Fractures of the Pelvis
This chapter includes simple apophyseal avulsion fractures, stable and
unstable pelvic ring fractures, and acetabular and triradiate
fractures. The nature and treatment of pediatric pelvic fractures are
challenging to describe and summarize, as they are dependent on
changing anatomy and bone structure with age.
appreciation of the high-energy mechanism of injury and the associated
injuries to other systems including the neurovascular structures,
abdominal viscera, genitourinary system, musculoskeletal system, and
central nervous system. The rate of concomitant injury to peripelvic
soft tissues is between 58% and 87%.15,24,29,69,80
The mortality rate in children with pelvic fractures ranged from 2.4%
to 14.8% in a large series collected from level 1 pediatric trauma
centers.7,15,19,29,37,52,55,67,69,80,92,94
In a recent study comparing pelvic fractures in adults and children,
there was no difference in mortality or injury to concomitant
peripelvic soft tissues between the groups.32 The authors found no difference in the trauma severity as expressed by the Injury Severity Score between children and adults.32
Central nervous system head injury was cited as the most common cause
of death in two recent large single-institution retrospective studies
of pediatric pelvic fractures.15,80 Other causes of death include multiorgan failure and visceral injuries.15,37,52,80
In children, hemorrhage from pelvic fracture-related vascular injury
was the cause of death in only 0.3% to 0.7% compared with 3.4% in
adults.37 Thus, the majority of deaths are not directly linked to the pelvic injury itself in children and adults.32
has been nonoperative based on the concept that the growing pelvis is
likely to remodel and anatomic reduction and fixation are therefore not
required. There is a trend toward operative treatment of unstable
fractures as new retrospective reviews have revealed significant long
term morbidity from malunion associated with nonoperative management.42,93
In addition, disruption of the immature pelvis may injure the
triradiate cartilage. Damage to the triradiate cartilage has the
potential to cause acetabular deformity
because of growth derangement.42
Long-term studies suggest a need for operative anatomic reduction to
lessen the chance of late deformity due to malunion, instability, or
growth disturbance.
understanding of pediatric pelvic fractures, the natural history, and
recommended treatments.
In the largest consecutive series of pediatric pelvic fractures from a
single urban level 1 trauma center, the most common mechanism of injury
was pedestrian struck by a motor vehicle (60%), followed by passenger
in a motor vehicle (22%), and falls (13%).80 Sporting activities account for between 4% and 11% of pelvic fractures in other series.69,92
Child abuse is a rare cause of pelvic fracture, but isolated fracture
of the pelvis may be the only skeletal manifestation of child abuse.64 Radiographs of the pelvis should be included in any skeletal survey for child abuse.1 Avulsion injuries most commonly occur secondary to athletic injuries, especially soccer, gymnastics, and track.
elasticity, they deform more and absorb more energy than adult bones
before fracture.18 In addition,
there is greater elasticity in the sacroiliac joints and symphysis
pubis in children, and greater energy is required to cause a fracture
in an immature pelvis than in an adult pelvis.80
Thus, the presence of a pelvic fracture in a child is a marker of
severe injury that should alert the clinician to search actively for
other injuries including abdominal, genitourinary, neurologic, and
other fractures.15
high-energy trauma, multisystem injuries are common. Between 58% and
87% of pelvic fractures have at least one and often several associated
injuries.15,24,29,69,80 Of the 57 consecutive children with pelvic fractures reported by Grisoni et al.,29
58% had one or more other body area injuries in addition to the pelvic
fracture. This included nonpelvic fractures (49%), neurologic injury
(26%), significant hemorrhage requiring transfusion (21%), abdominal
injury (14%), thoracic injury (7%), and genitourinary injury (4%). The
incidence of associated injuries increases with the severity of the
pelvic fracture. Bond et al.7 noted
that the location and number of pelvic fractures were strongly
associated with the probability of abdominal injury: 1% for isolated
pubic fractures, 15% for iliac or sacral fractures, and 60% for
multiple fractures of the pelvic ring. However, a study by Grisoni et
al.29 found no association between
multiple pelvic fractures and associated abdominal injuries. Almost all
authors agree that the outcome of patients with pelvic fractures is
largely determined by the associated injuries rather than the pelvic
fracture itself.7,15,24,29,37,52,69,80,91,94
reported the highest incidence of head injuries in 48% of the 54
patients in their series, ranging from mild concussion to brain death.
The two largest single institution studies of pediatric pelvic
fractures reported closed head injuries in 39%15 and 44% of patients.80 The correlation of pelvic fractures with head injury has been noted by others as well.92
Brain injury merits the highest priority because it is the leading
cause of death and major cause of long-term morbidity in patients with
pelvic fracture.
often require blood transfusions, exsanguination is rarely the primary
cause of death, which is distinctly different from the adult situation.
In three recent studies, each with between 57 and 166 patients, the
incidence of transfusion was between 20% and 30%15,19,29 and similar to adult rates of transfusions.19
In none of these studies did children die of an exsanguinating pelvic
fracture or associated vascular injury. In a recent study, only one
pediatric patient (0.7%) had mortality directly related to
exsanguination from the pelvic injury.32
Direct vascular injury with marked superior displacement of the
hemipelvis can injure the superior and inferior gluteal arteries at the
sciatic notch. Other studies of pelvic fractures in children have
documented retroperitoneal hemorrhage from disruption of branches of
the iliac artery adjacent to a grossly disrupted sacroiliac joint in
children.52,65
Children are thought to have lower incidence of exsanguinating
hemorrhage compared with adults because of a more effective
vasoconstrictive response in younger patients with nonatherosclerotic
blood vessels.37 The study by McIntyre et al.52
was the only study of pelvic fractures in children that correlated the
risk of life-threatening hemorrhage to pelvic fracture complexity. In
children with unstable fracture patterns or uncontrolled hypotension in
spite of adequate resuscitation and transfusion, external fixation,
angiography, and selective embolization may be indicated. In 90% of
studied cases, the pelvic bleeding is venous thus directly proceeding
to arteriography will not usually be helpful. A simple external
wrapping may reduce pelvic volume enough to tamponade bleeding and
preclude or delay the need for operative measures. When the abdomen is
opened either surgically or traumatically, direct packing of the
retroperitoneum may arrest life-threatening hemorrhage.82
examined for vaginal and rectal lacerations. The incidence of these
injuries is between 2% and 18% in children with pelvic fractures,6,55,68,87 and early detection and repair or diversion may prevent pelvic infection or abscess formation.56
The incidence of injury to the lower urinary tract (47%), vaginal
laceration (33%), and rectal laceration (66%) is significantly
increased in open fractures.54 Some
studies warn of a high rate of association of urogenital injury with
multiple pelvic fractures and anterior pelvic fractures,7,91
but the largest series to address this issue found no association
between pelvic fracture type or instability and urinary tract injury.87 Hematuria is noted on initial urinalysis in 14% to 52% of children with pelvic fractures.15,67,87
The incidence of significant lower urinary tract injuries including
bladder rupture or urethral tear has been between 4% and 15% in
retrospective studies.7,,44,55,67,68,69
The two largest singlecenter retrospective studies of pediatric pelvic
fractures reported a 1% incidence of lower urinary tract injury in
association with pelvic fracture.80,87
Although controversial, most authors agree that microhematuria can be
followed expectantly, whereas patients with gross hematuria or
significant local findings on physical examination should undergo
formal urologic assessment.
This assessment should include abdominopelvic computed tomography (CT), retrograde urography, and cystography.87
injury and hollow viscera is between 14% and 21% in children with
pelvic fractures.7,15,19,55,80
Rapid diagnosis and treatment of severe abdominal injury is important
because abdominal injury ranks second to head injury as the cause of
death in children with pelvic fractures.15 The presence of extremity fracture concomitant with pelvic fracture is associated with increased risk of abdominal injury.94 CT scan best demonstrates injury to organs, viscera, and mesentery after blunt injury to the abdomen.15 The incidence of abdominal injury with pelvic fracture is similar in children (13.7%) and adults (16.7%).19 Ultrasonography and diagnostic peritoneal lavage may be helpful in the diagnosis of intra-abdominal injury and vascular injury.76
in a study of 79 children with pelvic fractures, found that the
presence of any additional fracture was a significant indication that
head or abdominal injury was also present and that transfusion would be
required in the first 24 hours after injury. The patients with an
additional fracture had twice the frequency of death, thorax injury,
laparotomy, and other nonorthopaedic procedures compared with the group
with pelvic fractures alone. Vazquez and Garcia94
suggested that this easily identifiable risk factor can help identify
patients at risk who may benefit from early transfer to a regional
pediatric trauma center.
hemipelvis or iliac wing may result in damage to the lumbosacral plexus
or sciatic nerve. The incidence of lumbosacral plexus injury is low,
between 1% and 3%.24,68,91
Myelography with computed axial tomography or magnetic resonance
imaging (MRI) can be helpful in assessing plexus injury or root
avulsion. Complete neurologic examination of the extremities, sphincter
tone, and perianal sensation should be routine and documented.
with a thorough history and physical examination. Dangerous associated
injuries to the head injury, chest, abdomen, and genitourinary tract
take precedence over the pelvic fracture in evaluation and treatment.
The examination of the pelvic area begins with a visual inspection.
Areas of contusion, abrasion, laceration, ecchymosis, or hematoma,
especially in the perineal and pelvic areas, should be recorded.
spine, crest of the ilium, sacroiliac joints, and symphysis pubis
should be palpated. Pushing posteriorly on the anterior superior iliac
crest produces pain at the fracture site as the pelvic ring is opened.
Compressing the pelvic ring by squeezing the right and left iliac wings
together also causes pain, and crepitation may be felt if a pelvic
fracture is present. Pressure downward on the symphysis pubis and
posteriorly on the sacroiliac joints causes pain and possibly motion if
there is a disruption. Pain with range of motion of the extremities,
especially the hip joint, may indicate articular involvement. Careful
examination of the head, neck, and spine should be performed to assess
for spinal injury and closed head injury. A complete neurovascular
examination including peripheral pulses should be part of the initial
survey. A careful genitourinary evaluation must be performed because of
the intimate relationship between the pelvis and the bladder and
urethra. Rectal exam is indicated in significantly displaced fractures
or if there is any blood in the perineal area, but recent studies have
found a poor sensitivity for diagnosing injury with a routine rectal
exam in pediatric patients.77
pelvic trauma should be performed before obtaining survey radiographs.
If the patient is stable, scout views of the cervical spine, chest, and
pelvis should be obtained quickly. Once the primary survey is completed
and the patient is stable, region-specific radiographs should be
obtained of any area with signs of trauma on secondary assessment.
significant fracture-dislocation, multiple radiographic views can be
deferred. A single anteroposterior radiograph will provide a lot of
information about pelvic ring stability in the acute situation.90
The presence of sacroiliac displacement on the anteroposterior view
indicates instability and the possibility of associated major
hemorrhage. If there is an indication of an unstable injury on the
anteroposterior view, two other views, the inlet and outlet views,
should be obtained. These evaluate the pelvic ring by taking views that
are approximately at right angles to each other.90
The inlet view is obtained by directing the x-ray beam caudally at an
angle of 60 degrees to the x-ray plate. The inlet view is best for the
determination of posterior displacement of a hemipelvis. The outlet
view is obtained by directing the x-ray beam in a cephalad direction at
an angle of 45 degrees to the x-ray plate. The outlet view best
demonstrates superior displacement of the hemi pelvis or vertical
shifting of the anterior pelvis.90
Internal and external rotation (Judet or oblique) are reserved for
fractures of the acetabulum. Comparison views of the contralateral
apophysis may be helpful in evaluating avulsion fractures.
pelvis, especially at the sacroiliac joint, sacrum, and acetabulum.
Most authors agree that CT scanning is indicated if there is doubt
about the diagnosis on plain radiograph or if operative intervention is
planned.81 It has been shown that
plain films alone could reliably predict the need for operative
intervention, but the addition of CT scanning changed the injury
classification in 15% and the management in 3% of patients.11
Some of the advantages of CT over plain radiographs include optimized
imaging with CT reconstruction and improved fracture definition. This
aids in decision making between conservative and operative treatment
and improves the selection of operative approach.49
Others have noted that CT scans of the pelvis are more sensitive than
plain radiographs in all anatomic areas including the iliac region,
pubis, sacroiliac joint, hip, sacrum, and soft tissues.30
Many trauma centers routinely obtain CT scans of the abdomen and pelvis
looking for visceral injury. Including CT cuts through the bony pelvis
may obviate the need for dedicated pelvic screeing radiographs. MRI
offers similar benefits, with the advantages over CT in delineating
soft tissue injuries, absence of ionizing radiation, and fractures of
cartilaginous structures such as posterior wall fractures associated
with hip dislocations.71 Rarely, a radioisotope bone scan is useful for the diagnosis of nondisplaced
pelvic fractures and in the identification of acute injuries in
children and adults with head injuries or multiple-system injuries.35,90
|
TABLE 20-1 Torode and Zieg Classification of Pelvic Fractures in Children
|
|||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||
in the anatomy with age makes the comparison of incidence, mechanism of
injury, morbidity and mortality, and outcome difficult among studies
using different systems. In addition, many of the classifications do
not include triradiate cartilage injury, which may be associated with
the pelvic fracture. Although many recent studies of children’s
fractures use the Torode and Zieg92 (Table 20-1 and Fig. 20-1) or Tile et al.90 classifications (Table 20-2)
or both, the basic classifications, (a) mature or immature pelvis and
(b) stable or unstable fracture, are very useful information for making
treatment decisions. Regardless of the classification system that is
used, if there is a break in the anterior and posterior pelvic ring, an
extremely misshapen pelvis, a displaced posterior ring injury, or a
displaced triradiate fracture, the pelvis is unstable.
|
TABLE 20-2 Tile and Pennal Classification of Pelvic Fractures
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|
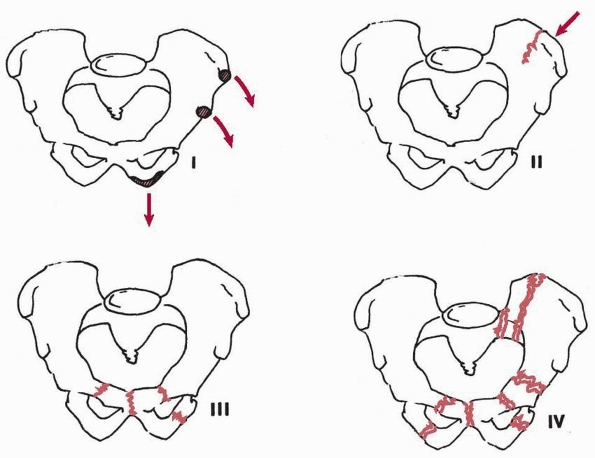
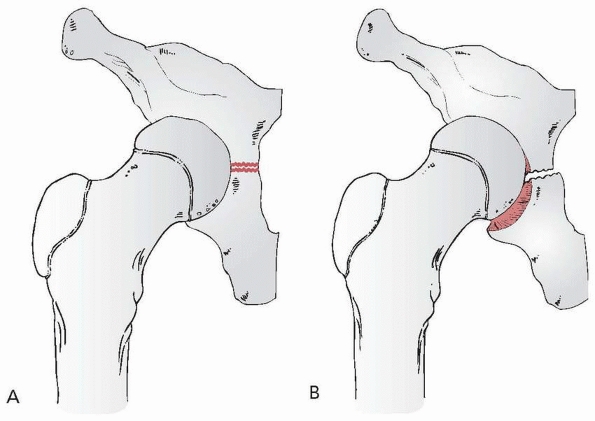
FIGURE 20-1 Torode and Zieg92
classification of pelvic fractures in children: type I, avulsion fractures; type II, iliac wing fractures; type III, simple ring fractures; type IV, ring disruption fractures. |
reviewed radiographs of 133 children and adolescents with pelvic
fractures and classified them into two groups: immature (Risser 0 and
all physes open) and mature (closed triradiate cartilage). They
suggested that in the immature group, management should focus on the
associated injuries because the pelvic fractures in this group rarely
required surgical intervention.79 Fractures in the mature group were best classified and treated according to adult pelvic fracture classification
and management principles. Thus, pelvic fractures in patients with
closed triradiate cartilage should follow adult fracture
classifications and treatment protocols.11,62,90 Torode and Zieg92
retrospectively reviewed 141 children with pelvic fractures and
classified the injuries on the basis of the severity of the fractures
as well as associated prognosis. Their classification does not include
acetabular fractures (see Table 20-1 and Fig. 20-1). The morbidity, mortality, and complications were greatest in the type IV group with segmental instability of the pelvis.
classified pelvic fractures in children into three categories: (i)
uncomplicated or mild fractures, (ii) fractures with visceral injury
requiring surgical exploration, and (iii) fractures with immediate,
massive hemorrhage often associated with multiple and severe pelvic
fractures. This classification system emphasizes the importance of the
associated soft tissue injuries, but does not account for the mechanism
of injury or the prognosis of the pelvic fracture itself. Watts95
classified pediatric pelvic fractures according to the severity of
skeletal injury: (a) avulsion, caused by violent muscular contraction
across the unfused apophysis; (b) fractures of the pelvic ring
(secondary to crushing injuries), stable and unstable; and (c)
acetabular fracture associated with hip dislocation.
classified pelvic fractures according to the direction of force
producing the injury: (a) anteroposterior compression, (b) lateral
compression with or without rotation, and (c) vertical shear. This
classification was modified and expanded by Tile et al. (see Table 20-2).90 Burgess et al.11
further modified the Pennal system and incorporated subsets to the
lateral compression and anteroposterior compression groups to quantify
the amount of force applied to the pelvic ring. They also created a
fourth category, combined mechanical injury, to include injuries
resulting from combined forces that may not be strictly categorized
according to the classification scheme of Pennal.
Orthopaedic Trauma Association/AO classification, which is divided into
bone segments, type, and groups (Table 20-3).62
The Orthopaedic Trauma Association/AO system classifies pelvic
fractures on the basis of stability versus instability, and surgical
indications are based on the fracture types. Surgery is rarely
indicated for type A fractures, whereas anterior or posterior surgical
stabilization or both may be indicated for types B and C. Numerous
subtypes are included, and further details are described in the chapter
on adult pelvic fractures.
|
TABLE 20-3 AO/Association for the Study of Internal Fixation Classification of Pelvic Fractures
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
the pelvis of a child and that of an adult. First, a child’s pelvis is
more malleable because of the bone is more elastic and less brittle,
the joints are more elastic, more of the pelvis is cartilaginous rather
than bony, and the cartilaginous structures are better able to absorb
energy than bone.58 Second, the
elasticity of the joints may allow significant displacement and
resultant fracture in only one area rather than the traditional concept
of a mandatory “double break” in the ring for a displaced fracture.58,66
Third, avulsion fractures of an apophysis occur more often in children
and adolescents than in adults because cartilage is weaker in tension
and shear compared with bone. Fractures of the acetabulum through the
triradiate cartilage also occur more often for the same reason.66,94
Fourth, fractures through physeal cartilage in children can result in
late growth arrest, leg-length discrepancy, and late deformity (e.g., a
fracture through the triradiate cartilage with resultant “bony bar”
formation and ultimately a deficient and dysplastic acetabulum).58
ossification centers: the ilium, ischium, and pubis. The three centers
meet at the triradiate cartilage and fuse at approximately 16 to 18
years of age (Fig. 20-2).58
The pubis and ischium fuse inferiorly at the pubic ramus at 6 or 7
years of age. Occasionally, at approximately the time of fusion of the
ischium to the pubis, an asymptomatic lucent area is noted on
radiographs in the midportion of the inferior pubic ramus. This, termed
ischiopubic synchondrosis, is a normal variant with a benign natural
history. It is often bilateral and does not require treatment. The
condition is often confused with a fracture of the pelvis.
crest, ischial apophysis, anterior inferior iliac spine, pubic
tubercle, angle of the pubis, ischial spine, and lateral wing of the
sacrum. Secondary ossification of the iliac crest is first seen at 13
to 15 years and fuses to the ilium at 15 to 17 years of age. The
secondary ossification center of the ischium is first seen at 15 to 17
years and fuses at 19 years of age, although sometimes as late as 25
years of age. A center of ossification may be present at the anterior
inferior iliac spine at approximately 14 years, fusing at 16 years of
age.58,95
Knowledge about the location, age of appearance, and fusion of the
secondary centers is important in differentiating them from true
fractures.
ischium, and pubis that merge to become the triradiate cartilage.
Interstitial growth in the triradiate part of the cartilage complex
causes the acetabulum to expand during growth and causes the pubis,
ischium, and ilium to enlarge as well. The concavity of the acetabulum
develops in response to the presence of a spherical head. The depth of
the acetabulum increases during development as the result of
interstitial growth in the acetabular cartilage, appositional growth of
the periphery of this cartilage, and periosteal new bone formation at
the acetabular margin.63 At puberty,
three secondary centers of ossification appear in the hyaline cartilage
surrounding the acetabular cavity. The os acetabuli, which is the
epiphysis of the pubis, forms the anterior wall of the acetabulum. The
epiphysis of the ilium, the acetabular epiphysis,63,95 forms a large part of the superior wall of the acetabulum. The small secondary center of the ischium is rarely
seen. The os acetabuli, the largest part, starts to develop at
approximately 8 years of age and expands to form the major portion of
the anterior wall of the acetabulum; it unites with the pubis at
approximately 18 years of age. The acetabular epiphysis develops in the
iliac acetabular cartilage at approximately 8 years and fuses with the
ilium at 18 years of age, forming a substantial part of the superior
acetabular joint surface (Fig. 20-3).
The secondary center of the ischium, the smallest of the three,
develops in the ninth year, unites with the acetabulum at 17 years, and
contributes very little to acetabular development. These secondary
centers should not be confused with avulsion fractures or loose bodies
in the hip joint.
 |
|
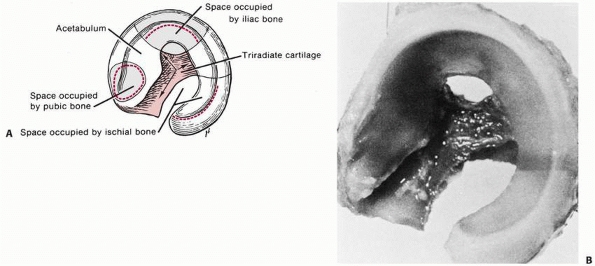
FIGURE 20-2 A.
Triradiate-acetabular cartilage complex viewed from the lateral side, showing the sites occupied by the iliac, ischial, and pubic bones. B. Normal acetabular cartilage complex of a 1-day-old infant. The ilium, ischium, and pubis have been removed with a curet. The lateral view shows the cup-shaped acetabulum. (From Ponseti IV. Growth and development of the acetabulum in the normal child. Anatomical, histological, and roentgenographic studies. J Bone Joint Surg Am 1978;60(5): 575-585, with permission.) |
 |
|
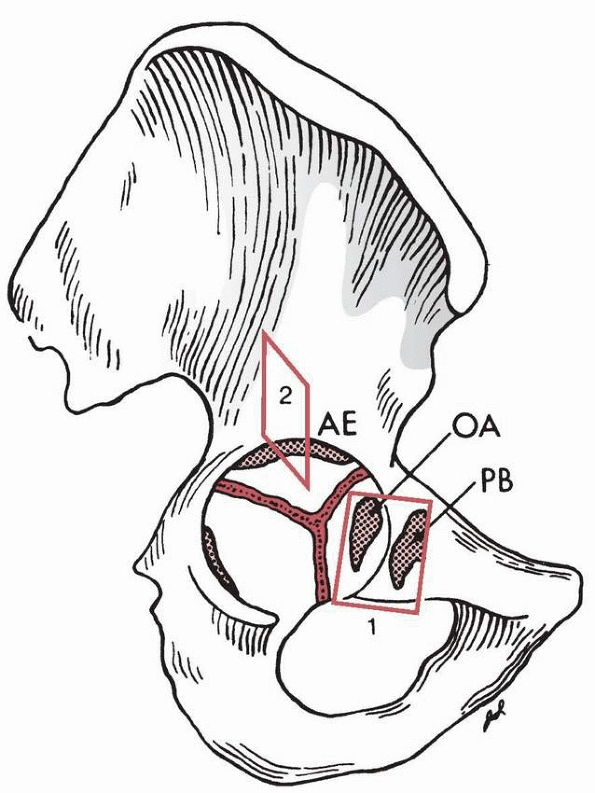
FIGURE 20-3
Right innominate bone of an adolescent. The os acetabuli (OA) is shown within the acetabular cartilage adjoining the pubic bone (PB); the acetabular epiphysis (AE), within the acetabular cartilage adjoining the iliac bone; and another small epiphysis (not labeled), within the acetabular cartilage adjoining the ischium (left). (From Ponseti IV. Growth and development of the acetabulum in the normal child. Anatomical, histological, and roentgenographic studies. J Bone Joint Surg Am 1978; 60(5):575-585, with permission.) |
adolescent athletes as a result of forceful contraction of the attached
muscle while the athlete is actively engaged in activities such as
kicking, running, or jumping.23,53,70
As these injuries are painful, but not disabling, the incidence of
avulsion fractures is most certainly underrepresented in large
hospital-based clinical series because most of these injuries are never
seen in the emergency room. The incidence in two large recent series
was approximately 4%.67,69
Chronic repetitive traction on the developing iliac apophysis may
result in an incomplete avulsion fracture or apophysitis without a
history of acute trauma.16,26
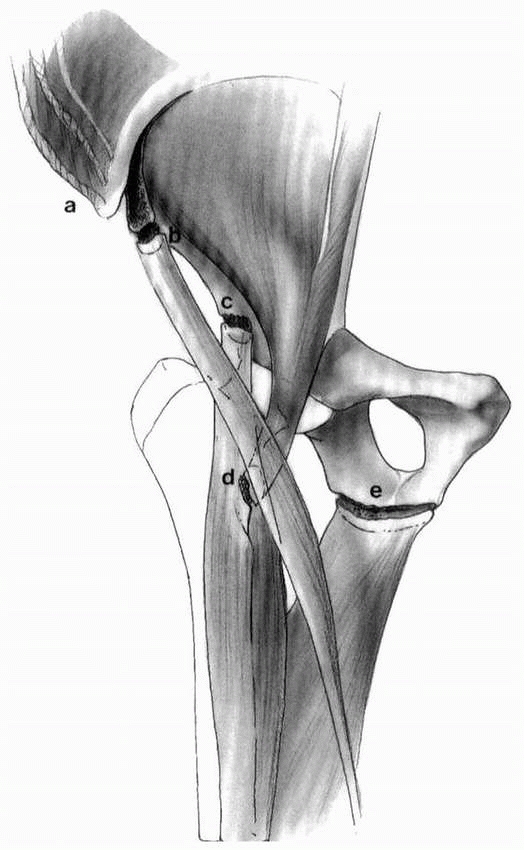
The sartorius muscle originates at the anterior superior iliac spine,
the direct head of the rectus femoris at the anterior inferior iliac
spine, and the hamstrings and adductors from the ischial tuberosity (Fig. 20-4).
50% were ischial avulsions, 23% were avulsions of the anterior superior
iliac spine, and 22% were avulsions of the anterior inferior iliac
spine. Avulsions of the lesser trochanter (3%) (Fig. 20-5) and iliac apophysis (2%) accounted for the rest.
through large muscles, which have their origins on the pelvic
apophyses. This may be active contraction as in sprinting or jumping,
or avulsion may result from sudden passive traction such as performing
splits in gymnastics or dance.53 The
distribution of fracture patterns with respect to sporting activity
reveals that gymnastics are responsible for the greatest number of
acute ischial tuberosity avulsion fractures, whereas soccer is
responsible for the greatest numbers of anterior superior and anterior
inferior iliac spine avulsion fractures.70
Iliac apophysitis is most frequently associated with long distance
running and thought to result from either repetitive muscle traction
injury or stress fractures of the apophysis.16
 |
|
FIGURE 20-4 Locations for pelvis apophyseal fractures. A. Iliac apophysis from external oblique. B. Anterior superior iliac spine avulsion attached to sartorius. C. Anterior inferior iliac spine avulsion from recuts; femoris attachment. D. Lesser trochanter avulsion from iliopsoas attachment. E. Ishial tuberosity avulsion from hamstring muscles.
|
tenderness at the site of the avulsion fracture. Motion is limited due
to guarding, and pain may be mild or marked. In the case of repetitive
stress injury, pain and limitation of motion usually are gradually
progressive. In patients with ischial avulsions, pain at the ischial
tuberosity can be elicited by flexing the hip and extending the knee
(straight-leg raising). In this position, as the hip is moved into
abduction, the pain increases. Patients may also have pain while
sitting or moving on the involved tuberosity.
 |
|
FIGURE 20-5 Avulsion fracture of the lesser trochanter.
|
spine, radiographs show displacement of the apophysis. In patients with
anterior inferior iliac spine avulsions, radiographs show minimal
distal displacement of the fragment. Further displacement is probably
prevented because of tethering by the conjoined tendon, as the
reflected head of the rectus femoris muscle is intact. Contralateral
views can be obtained and compared to ensure that this fragment is not
actually a secondary center of ossification, either the os acetabuli or
acetabular epiphysis. In the case of ischial tuberosity avulsion,
radiographs typically reveal a semilunar fragment displaced distally
compared with the opposite ischial tuberosity. The intact sacrotuberous
ligament resists significant displacement.
of ossification before the center is fused with the pelvis, primarily
in children ages 11 to 17 years,23,53,86
comparison views of the contralateral apophysis should be obtained to
ensure that what appears to be an avulsion fracture is not in reality a
normal adolescent variant. Later, exuberant callus formation can
occasionally mimic a malignant neoplasm.4
Recognition of the initial fracture is important to avoid unnecessary
evaluations such as CT, MRI, and radionuclide scans, and inappropriate
biopsy.
satisfactorily with conservative nonoperative management including
rest, partial weight bearing on crutches for 2 or more weeks, and
extremity positioning to minimize muscle stretch. Two small series of
adolescents with pelvic avulsion fractures treated conservatively
concluded that nonsurgical treatment was successful in all patients,
and all patients returned to preinjury activity levels.23,53
Others have suggested that conservative nonoperative treatment is
associated with a significantly higher incidence of functional
disability and inability to return to competitive athletic activity.86
On long-term follow-up of 12 patients with ischial avulsions, 8
reported significant reduction in athletic ability and 5 had persistent
local symptoms.86 In the largest
series published to date, only 3 of 198 competitive adolescent athletes
with pelvic avulsion fractures were treated operatively.70
Anecdotally, long-term functional disability and inability to return to
preinjury activity levels have been reported in the setting of
conservatively managed ischial avulsion fractures.73,86
Controversy exists surrounding the acute management of ischial avulsion
fractures, but most agree that excision of the ischial apophysis is
indicated in the setting of chronic pain and disability. Some authors
recommend open reduction and internal fixation of those rare acute
pelvic avulsion fragments displaced more than 1 to 2 cm (Fig. 20-6).48
reported only 7 (12%) in 57 fractures. However, this fracture often
occurs in conjunction with other fractures of the pelvis, and thus the
overall incidence
of iliac wing fractures is probably significantly higher than the incidence of isolated iliac wing fractures.
 |
|
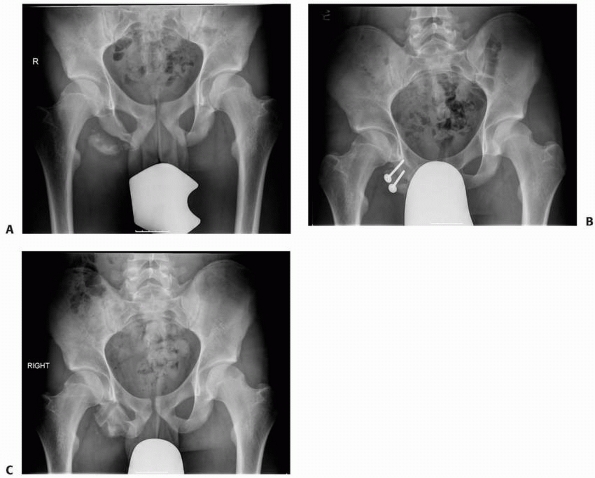
FIGURE 20-6 A. A painful ischial apophyseal nonunion in an athlete. B. Fixation of the apophysis. C. Healed apophysis after implant removal. (Courtesy of Dr. David C Scher, Hospital for Special Surgery, NY.)
|
but it can occur medially or proximally. Severe displacement is rare as
the iliac wing is tethered by the abdominal muscles and the hip
abductors. Pain is located over the wing of the ilium, and motion at
the fracture site may be noted. A painful Trendelenburg gait may be
present because of spasm of the hip abductor muscles. A fracture of the
wing of the ilium may be overlooked on an underexposed radiograph of
the pelvis where the ilium is poorly seen as a large area of
radiolucency.
by the associated injuries. Symptomatic treatment is all that is
necessary for treatment of the fracture itself. This should be followed
by partial weight bearing on crutches until the symptoms are completely
resolved. Regardless of comminution or displacement, these fractures
usually unite without complications or sequelae (Fig. 20-7).
reported that 56% of pelvic fractures in their series of 166
consecutive pediatric pelvic fractures were simple ring fractures
(excluding acetabular fractures) and were caused by a motor vehicle
striking a pedestrian in 60%. Single ramus fractures are more common
than multiple ramus fractures, and the superior ramus is fractured more
often than the inferior ramus (Fig. 20-8).67
clinical examination reveals tenderness and sometimes crepitus at the
fracture site. CT scanning or inlet and outlet radiographic views are
helpful in determining whether there are any other pelvic fractures
presenting in the pelvic ring. If there is significant displacement of
the pubic rami, a second fracture through the pelvic ring should be
suspected. However, because of the plasticity of bone and elasticity of
the symphysis and sacroiliac joints in children, more displacement can
be expected than in adults
with
a similar injury. In the immature pelvis, ramus fractures may extend
into the triradiate cartilage. Treatment of theses patients is usually
symptomatic, and progressive weight bearing is allowed. These are
stable injuries and do not require surgery.
 |
|
FIGURE 20-7 Stable fracture of the iliac wing.
|
 |
|
FIGURE 20-8 A. Stable superior pubic ramus fracture. The patient was allowed full weight bearing as tolerated. B. Radiographs show complete fracture union and remodelling.
|
rami comprised 18% of pediatric pelvic fractures in the series of 120
pediatric pelvic fractures reviewed.15
Although these fractures are generally stable, they may be associated
with injuries of the abdominal viscera, especially the genitourinary
system (e.g., bladder rupture).22
There is a high incidence of associated head injury, which correlates
with the mechanism of injury, which is very often a motor
vehicle-pedestrian incident.92
pattern, and other associated fractures should be expected. A general
evaluation should be followed by examination of the pelvis and lower
extremities, with special attention to abrasions, contusions,
lacerations, and ecchymosis about the pelvis. Palpation reveals
discomfort anteriorly, and crepitus at the fracture site may be noted.
adults. However, in children, the fracture almost always unites with
adequate remodeling of even the most displaced fractures. For this
reason, symptomatic treatment and progressive weight bearing on the
involved side is all that is necessary.
is extremely rare in children. The fracture occurs from external force
to the ischium, most commonly in a fall from a considerable height. The
fracture usually is minimally displaced, and treatment consists of
symptomatic treatment and progressive weight bearing (Fig. 20-9).
 |
|
FIGURE 20-9 A. Nondisplaced fracture through the left ischium and contralateral pubic ramus fracture. B.
Follow-up radiograph shows mild displacement and incongruity of the acetabulum and complete healing of the superior pubic ramus fracture. Either displacement of the fracture fragments or premature closure of the triradiate cartilage could have contributed to the incongruity of the femoral head in the acetabulum. |
occur in adolescents and young adults from chronic, repetitive stress
to a bony area or during the last trimester of pregnancy. Stress
fractures of the pubis are likewise uncommon, but a small series of
stress fractures, primarily in the inferior pubic rami, has been
reported. Chronic symptoms and pain increased by stress may be noted in
the inferior pubic area. Radiographs may show no evidence of fracture
for as long as 4 to 6 weeks, and then only faint callus formation may
be visible; however, MRI or a technetium bone scan may reveal increased
uptake early.35 Treatment should consist of avoiding the stressful activity and limited weight bearing for 4 to 6 weeks.
The radiographic appearance of the synchondrosis at the ischiopubic
junction may be misinterpreted as a fracture. Caffey and Ross12,43
noted that bilateral fusion of the ischiopubic synchondrosis is
complete in 6% of children at 4 years of age and in 83% of children at
12 years of age. The presence of the synchondrosis itself is common and
usually asymptomatic. Bilateral swelling of the synchondrosis was also
noted in 47% of children at age 7 years. Irregular ossification and
clinical swelling at the ischiopubic synchondrosis has been called
ischiopubic osteochondritis or van Neck disease. If this
syndrome is noted in a child older than 10 years of age, it should be treated as a repetitive stress injury (Fig. 20-10).
 |
|
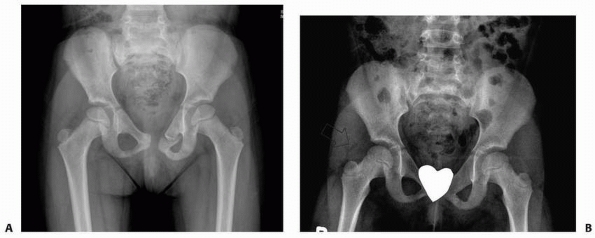
FIGURE 20-10
Radiograph of the pelvis of a 9-year-old child. Although the differentiation could not be made between a fracture and fusion of the right ischiopubic ossification at the time of radiograph, the patient was asymptomatic and the mass was considered a variant of normal development. |
because they usually occur in association with disruption of the
posterior ring near the sacroiliac joint. Although significant force
appears to be necessary to disrupt or fracture the symphysis pubis,
isolated disruption of the symphysis pubis can occur.95
There is normally some elasticity at the symphysis, even in adults (0.5
mm in men, 1.5 mm in women), and there is probably even more in
children, depending on maturity. In children and adolescents, diastasis
greater than or equal to 2.5 cm or rotational deformity greater than 15
degrees suggests significant instability and the need for reduction.27
symphysis; the legs are externally rotated and often pain is worse in
the supine position than in the side-lying position.95 Motion of the hips in flexion, abduction, external rotation, and extension is restricted and painful (fabere sign).
The two sides may be offset vertically or front-to-back. Disruption may
occur near or through the symphysis pubis. Because of normal variation
of the width of the symphysis in children, the extent of traumatic
separation may be difficult to evaluate. Watts95
suggested radiographs with and without lateral compression of the
pelvis. More than 1 cm of difference in the width of the symphysis
pubis between the two views suggests a symphyseal separation.
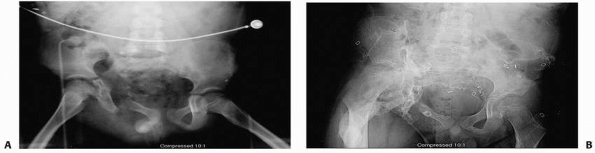
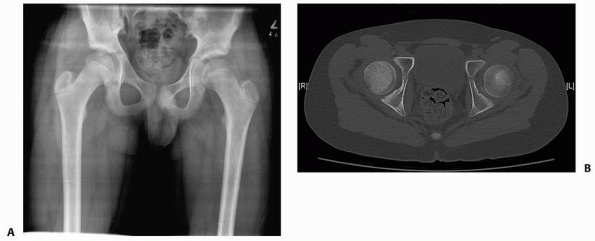
Radiographic evaluation including CT should be performed to
specifically exclude sacroiliac joint disruption and triradiate
cartilage fracture because both of these injuries may occur in
association with symphysis pubis separation (Fig. 20-11).58
 |
|
FIGURE 20-11 A. Fracture adjacent to the symphysis pubis with symphysis pubis separation. B. CT scan showing no posterior instability.
|
 |
|
FIGURE 20-12 Radiograph of the pelvis after plating of the pubic symphysis that also includes acetabular fixation.
|
significant displacement (2 cm) or posterior injury should be
symptomatic. If there is wide diastasis, reduction and external
fixation with an anterior frame will provide immediate stability and
allow early mobilization.2 Open
reduction and internal fixation with a plate may be considered if a
fixator is too bulky or restricts access to the abdomen (Fig. 20-12).
joint are rare, probably even less common than isolated fractures at
the weaker symphysis pubis. More commonly, posterior disruptions of the
pelvic ring require a concomitant disruption of the anterior pelvis.
These double-ring disruptions are considered unstable. Sacroiliac
dislocations differ from those in adults in several ways. In children,
disruptions tend to be incomplete
because
the anterior sacroiliac ligaments tend to tear incompletely. The
sacroiliac joint may also fail through the epiphysis of the ilium
adjacent to the joint.58 A fracture through the relatively weak physeal cartilage may leave the sacroiliac joint technically intact.20
Associated vascular and neurologic injuries may occur. Lumbosacral
nerve root avulsions have been described in children with this fracture.76
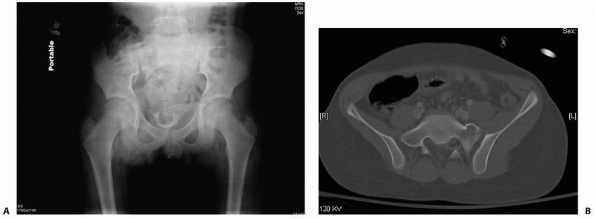
Derangement of the sacroiliac joint should be suspected after
high-velocity trauma with impact to the posterior pelvis. In patients
with these injuries, the fabere sign is markedly positive on the
ipsilateral side.20,33
Comparison views of both sacroiliac joints should be carefully
evaluated looking for asymmetry of the iliac wings or the clear space
at the sacroiliac joint. Offset of the distal articular surface is an
indication of sacroiliac joint disruption. Because it is rare to have
an isolated posterior injury, in the case of a seemingly isolated
sacroiliac disruption, special views including inlet and outlet, or
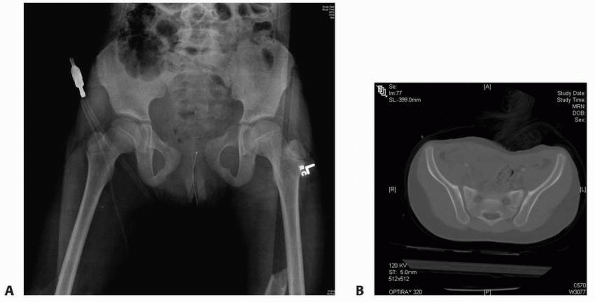
axial, CT scan are indicated to look for anterior ring fracture (Fig. 20-13).
crutches are sufficient treatment for isolated subluxations or
fractures. Heeg and Klasen33
reported sacroiliac joint dislocations in 18 children, 10 of whom had
extensive degloving injuries of the posterior pelvis. Ten were treated
nonoperatively, six with open reduction and internal fixation, one with
open reduction but no internal fixation, and one with external
fixation. Long-term sequelae included occasional back pain in six,
daily back pain in three, and incomplete neurologic recovery in six.
 |
|
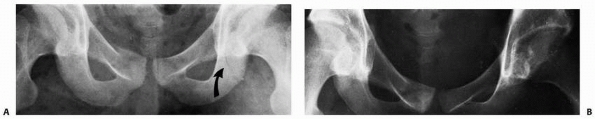
FIGURE 20-13 A 4-year-old with a pelvis fracture primarily with posterior involvement. A. Pelvic outlet radiograph showing a posterior injury at the sacroiliac joint. B. CT scan showing the minimal posterior SI widening. C. CT scan showing no anterior ring injury.
|
-
Double anterior injury with bilateral
pubic ramus fractures (the straddle or floating injury) or disruptions
of the pubis with an associated second break in the anterior ring -
Double fractures in the pelvic ring with
anterior and posterior, disruptions through the bony pelvis, sacroiliac
joint, or symphysis pubis (Malgaigne fractures) -
Multiple crushing injuries that produce at least two severely comminuted fractures in the pelvic ring
rami (straddle fractures) cause a floating anterior arch of the pelvic
ring that is inherently unstable (Fig. 20-14).
Disruption of the symphysis pubis with unilateral fractures of the rami
causes similar instability. This fracture pattern frequently is
associated with bladder or urethral disruption.58
rami can occur in a fall while straddling a hard object, by lateral
compression of the pelvis, or by sudden impact while riding a motorized
cycle. The floating fragment usually is displaced superiorly, being
pulled in this direction by the rectus abdominis muscles.95 Radiographically, an inlet view most accurately determines the amount of true displacement of the floating fragment.
are not grossly displaced, these injuries should heal and remodel
without any orthopaedic intervention. Because these injuries do not
involve the weight-bearing portion of the pelvis, there is no residual
leg-length discrepancy. Skeletal traction is unnecessary, and a pelvic
sling is contraindicated because of the possibility that compression
will cause medial displacement of the ilium.58,95
 |
|
FIGURE 20-14 Example of a straddle fracture.
|
result in instability of the hemipelvis. These unstable fractures are
often accompanied by retroperitoneal and intraperitoneal bleeding.
There has been a 35% to 60% incidence of concomitant abdominal injury
in these unstable pelvic fractures versus 11% to 18% in more stable
pelvic fractures.7,93
Bilateral anterior and posterior fractures are the most likely fracture
pattern to cause severe hemorrhage. Initial treatment involves
resuscitation with fluids and blood and stabilization of the child’s
overall condition before treatment of the pelvic fractures.91
implied that the majority were from anteroposterior compression forces.
Other possibilities are direct lateral compression force and indirect
forces transmitted proximally along the femoral shaft with the hip
fixed in extension and abduction.
pelvic fractures, leg-length discrepancy and asymmetry of the pelvis
also may be present because of displacement of the hemipelvis. Inlet
and outlet radiographs and CT scan reveal the amount of pelvic
displacement. The degree of residual pelvic asymmetry can be described
by the method of Keshishyan.42 With
this method, pelvic asymmetry is determined by the difference in length
(in centimeters) between two diagonal lines drawn from the border of
the sacroiliac joint to the contralateral triradiate cartilage.
 |
|
FIGURE 20-15
An unstable pelvis fracture with fractures in both the anterior and posterior ring of the pelvis. The left hemipelvis is displaced and rotated. |
depending on the type of fracture and the amount of displacement. For
fractures with minimal displacement, symptomatic treatment,
weight-bearing restrictions, and close follow-up for displacement are
suggested (Fig. 20-16). Spica casting can be used in the younger child.
Historically and in general, operative treatment of pelvic fractures in
children has not been routinely recommended because of the following:
(a) exsanguinating hemorrhage is unusual in children, so operative
pelvic stabilization to control bleeding rarely is necessary5,55;
(b) pseudoarthrosis is rare in children and fixation is not necessary
to promote healing; (c) the thick periosteum in children tends to help
stabilize the fracture, so surgery usually is not necessary to obtain
stability67; (d) prolonged immobilization is not necessary for fracture healing57;
(e) significant remodeling may occur in skeletally immature patients;
and (f) long-term morbidity after pelvic fracture is rare in children.29,39,55 Many of these assumptions are correct and some have proven to be untrue.
unstable displaced fracture to prevent long-term morbidity. There are
several reasons for advocating more aggressive treatment for unstable
pelvic fractures in children. The ability of the immature pelvis to
remodel has been overestimated in the past. Residual pelvic and
acetabular deformity may have a poor long-term outcome.82
The long-term musculoskeletal morbidities include leg-length
discrepancy, back pain, scoliosis, pelvic asymmetry, and sacroiliac
arthrosis.82,83
The short-term morbidity of pelvic fracture in children centers on
pain, immobility, loss of independence, and effects of associated
injuries. Signorino et al.78 studied
short-term outcome parameters after pelvic fracture in children. They
found that in three important domains—self-care, mobility, and
cognition—children tended to return to near normal status by 6 months
postinjury.
persistent obliquity of the pelvis and damage to the pelvic floor.
Smith et al.83 followed 20 patients
with open triradiate cartilages and unstable pelvic fracture for a mean
of 6.5 years. They were evaluated using the Short Musculoskeletal
Function Assessment (SMFA) questionnaire, physical exam, and
radiographs. Pelvic asymmetry did not remodel even in younger patients.
Eighteen patients were treated operatively with external fixation,
internal fixation, or a combination of both, and pelvic asymmetry of no
more than 1 cm was achieved in 10 of them. Patients who had no more
than 1 cm of pelvic asymmetry had no lumbar or sacroiliac pain, no or
mild sacroiliac tenderness, no Trendelenburg sign, no lumbar scoliosis,
and lower (better) bother and dysfunction scores on the SMFA compared
with patients with more pelvic asymmetry. All patients with greater
than 1.1 cm of pelvic asymmetry had three or more of the following:
nonstructural scoliosis, lumbar pain, a Trendelenburg sign, or
sacroiliac
joint
tenderness and pain. Patients with fewer associated injuries and pelvic
asymmetry of no more than 1 cm had better clinical results. They
concluded that fractures associated with at least 1.1 cm of pelvic
asymmetry following closed reduction should be treated with open
reduction and internal or external fixation in order to improve
alignment and the long-term functional outcome.83
 |
|
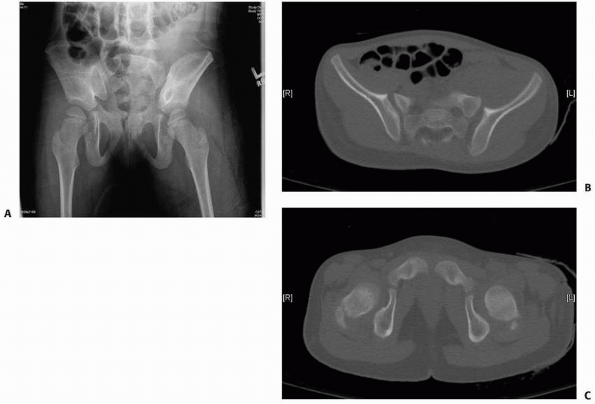
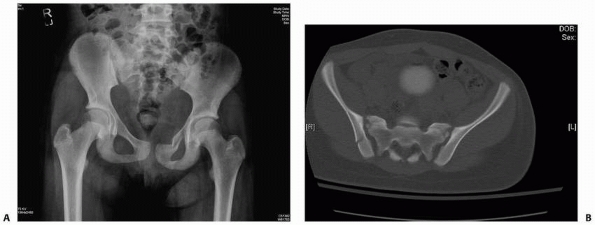
FIGURE 20-16 A potentially unstable pelvis fracture with anterior and posterior injury. A. The radiograph shows a left superior and inferior ramus fracture. B.
The CT scan shows a minimally displaced fracture adjacent to the sacroiliac joint. This is also an example where both CT and plan radiographs can be used to evaluate the injury and help decide on displacement and treatment. This patient was treated nonoperatively with follow-up making sure there was no displacement. |
a long-term (2 to 25 years) follow-up of 17 children with
nonoperatively treated unstable pelvic fractures, reported moderate to
severe pelvic asymmetry in eight patients. Measured leg-length
discrepancies between 2 and 5 cm were reported in 5 patients. These
authors emphasized that reduction of the pelvic ring fractures should
be as anatomic as possible because healing in malposition resulted in
unsatisfactory results in half of the cases. McDonald51
found that that one third of 15 skeletally immature patients with
unstable fractures treated nonoperatively had residual pain. Heeg and
Klasen7 retrospectively followed 18
children at an average of 14 years after injury. Ten were treated with
bedrest and 8 surgically. Nine patients had a leg-length discrepancy of
greater then 1.0 cm and 3 patients reported daily back pain.7 Rieger and Brug69
concluded that the principles of operative management should not differ
much between children and adults due to their review of long-term
morbidity in unstable fractures. Nierenberg et al.,57
however, reported excellent or good results after conservative
treatment of 20 unstable pelvic fractures in children despite
radiographic evidence of deformity. They suggested that treatment
guidelines for unstable pelvic fractures are not the same for children
as for adults, and recommended that external or internal fixation
should be used only when conservative methods fail.57 Silber and Flynn,79
in a retrospective review of 166 consecutive children with pelvic
fractures, found that all 4 patients who required open reduction and
internal fixation had a mature pelvis with a closed triradiate
cartilage. The average age of the children that required operative
fixation was 14.3 years versus 8.7 years in those children that did not
require operative fixation. These reviews suggest that younger children
with an immature pelvis are unlikely to require operative intervention;
however, treatment of children with unstable pelvic fractures and
treatment of adolescents with a “mature” pelvis should follow adult
treatment guidelines.
patients treated nonoperatively for unstable pelvic fractures. At 7.4
years follow-up, in addition to various orthopaedic complaints, 23
patients had genitourinary dysfunction including urethral stricture,
urinary incontinence, and erectile dysfunction. Thirty-one patients
were diagnosed with 41 psychiatric illnesses, including dysthymic
disorder, social phobia, posttraumatic stress disorder, and major
depression. They felt that long hospital stays and urologic
complications are associated with serious psychologic problems, and
thus should be considered during selection of treatment modality.
Baessler et al.3 studied symptoms of
pelvic floor dysfunction after pelvic trauma. Twenty-four women who had
sustained AO type B and C fractures completed questionnaires at a
median age of 24 years. Sixteen women reported new symptoms. Bladder
symptoms occurred in 12, bowel problems in 11, and sexual dysfunction
in 7 of 17 sexually active women. They concluded that pelvic fracture
is a risk factor for pelvic floor dysfunction.3
then maintaining reduction until healing. Reductive maneuvers may
include manipulation, traction, or open reduction. After successful
reduction is obtained, casting, traction, external fixation, or
internal fixation can be used to maintain the reduction. Spica casting
is most suited to small children. Skeletal traction may be suited to
children who can tolerate prolonged recumbency or who are unable to
tolerate internal fixation. Anterior external fixation is achieved by
placing one or two pins in the supra-acetabular bone on each side (Fig. 20-17).72
Pins can be placed open or percutaneously. External fixation has been
advocated to stabilize an unstable fracture, maintain accurate
reduction, achieve earlier ambulation, and decrease pain secondary to
instability. Keshishyan et al.42 advocated external fixation of complex pelvic fractures, especially in children with polytrauma, and Gordon et al.27
suggested external fixation or open reduction and internal fixation in
children older than 8 years of age because spica casting is poorly
tolerated in older children. Symphysis plating via a Pfannenstiel
approach is a good alternative for anterior ring external fixation. It
is less bulky then external
fixation
and can often be performed when the surgeons are repairing the bladder
or laparotomy, which is not uncommon with a widely displaced symphysis.
 |
|
FIGURE 20-17
Fixation of an unstable pelvis fracture with external fixation. One or two pins are placed in the iliac wing. The stating point is 1 to 2 cm posterior to the anterior superior iliac spine. An anterior to posterior supra-acetabular pin may also be used. |
Open reduction can be achieved through an anterior retroperitoneal
approach in the iliac fossa in the supine position. Fixation is by
small screws or plate. Alternatively, reduction and fixation can be
done prone through a posterior approach. Holden et al.36
determined after a review of the literature that fractures with at
least 2 cm of displacement must be reduced and stabilized. They felt
that external fixation is not ideal for vertical shear injuries, but it
is appropriate when emergent stabilization is needed to control blood
loss.36 Internal fixation with anterior pubic symphysis plating and percutaneous sacroiliac screw fixation may be required.36 Stiletto84 (Fig. 20-19)
reported good results after open reduction and internal fixation of
unstable pelvic fractures in two toddlers. AO small-fragment
instrumentation was used in both. During a 7-year period, Karunaker et
al.40 operatively treated 18
unstable pelvic and acetabular fractures in children. Their results
suggest that unstable pelvic and acetabular fractures in the skeletally
mature patient should be managed by the same principles used in the
adult population. Clinical and radiographic follow-up at a mean of 2
years in their group showed that adolescents recover full function with
minimal deficits and residual pain if anatomic or near-anatomic
reductions are achieved. Unstable pelvic and acetabular fractures in
skeletally immature patient were also successfully managed operatively
with a low incidence of complications. No sacroiliac or triradiate
growth arrests were identified at 3 years of follow-up. They felt that
operative intervention is warranted in skeletally immature patients
with significant deformity of the pelvis at the time of injury to
prevent late morbidities.40
 |
|
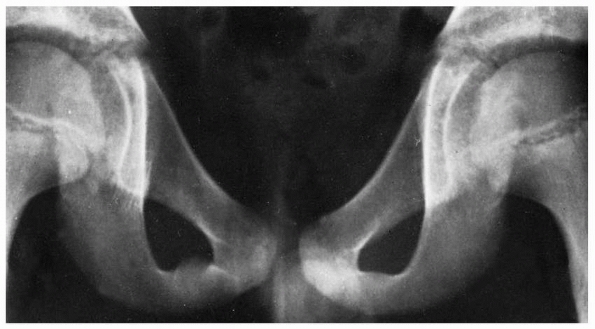
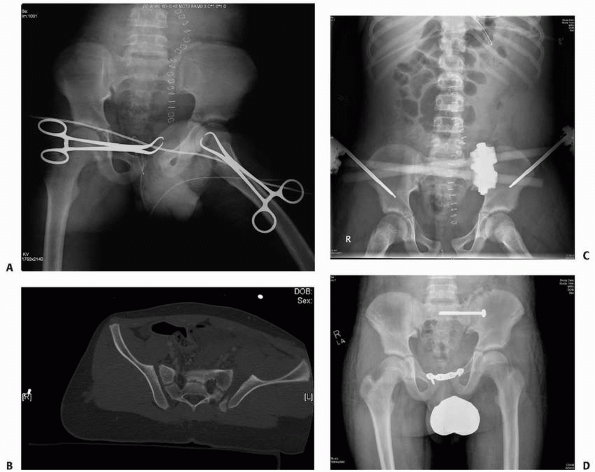
FIGURE 20-18 A.
Multiple trauma in this 12-year-old child included three fractures of the pubic rami, disruption and fracture of the sacroiliac joint on the right, and a femoral shaft fracture on the right. B. CT shows fracture of the ilium and disruption of the sacroiliac joint. C. After open reduction and internal fixation of the sacroiliac joint and closed intramedullary nailing of the femoral shaft fracture. Note femoral nail inserted through the tip of the greater trochanter. |
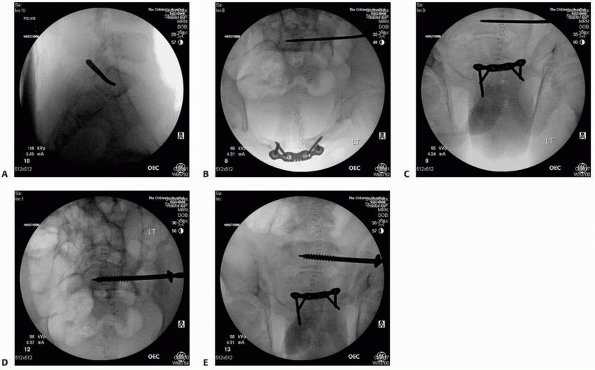
sacroiliac screws. Insertion of sacroiliac screws requires expertise
and image guidance. The patient is placed prone on a radiolucent table.
A lateral image of S1 can find the stating point for the guidewire.
Then a fluoroscopic 40-degree pelvic inlet and 40-degree pelvic
outlet views are obtained to direct the guidewire across the sacroiliac joint into the body of S1(Fig. 20-20).
One 6.5-mm cannulated screw is optimal. In the pediatric patient, the
narrow corridor for safe screw placement makes the procedure difficult.83 In the patient with a small corridor, the use of screw placement with CT guidance has been described.97 The use of cannulated screws facilitates accurate placement.
 |
|
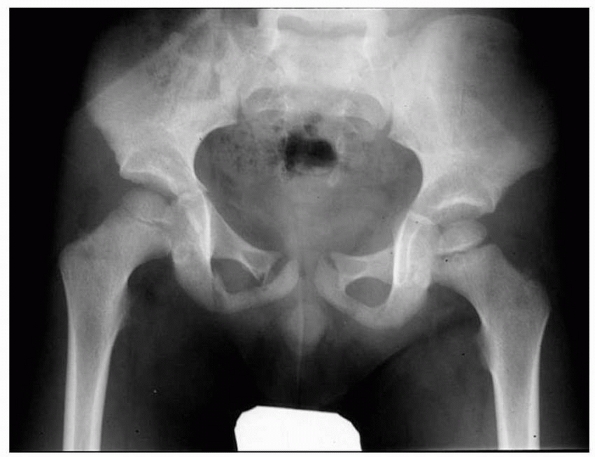
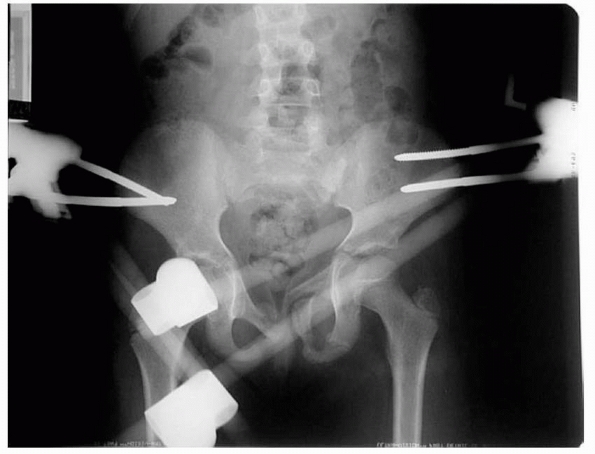
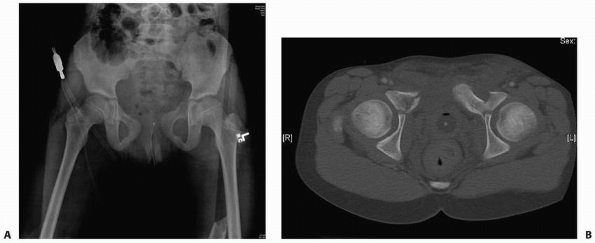
FIGURE 20-19 This radiographic series highlights treatment of the unstable pelvic fracture with hemodynamic instability. A.
Anteroposterior pelvis radiograph of a 12-year-old male who was a pedestrian hit by a car. There is a wide symphysis and a displaced fracture adjacent to the left sacroiliac joint. The towel clips seen on radiograph are to hold a sheet (sling) around the pelvis to help temporarily control hemorrhage. B. CT scan showing the displaced posterior injury. C. Pelvis radiograph after an anterior external fixation was placed urgently to stabilize the pelvis. This along with resuscitation stabilized the hemodynamic status. D. Once the patient had stabilized, the external fixation was converted to anterior internal fixation with a plate on the symphysis pubis and the posterior instability was treated with a sacroiliac screw. |
do not need operative intervention. When the pelvis is more mature,
adult guidelines should be followed. There is data to suggest that
significant residual deformity may lead to a poor outcomes so unstable
fracture patterns may benefit from operative reduction. The following
are indications for operative fixation of pelvic fractures in children:
(i) in the case of severe instability in which the goals are to control
pain associated with motion of fragments, to control bleeding, and to
facilitate mobility and patient transfer; (ii) in the case of
associated visceral or soft tissue injuries that could not be managed
without a stable skeleton; and (iii) in the case of a displaced (>1
cm) unstable fracture which is likely to lead to long-term mechanical
problems.
adult pelvic fractures and should be part of pediatric pelvic
fractures. The team should be aware of the large incidence of
concomitant injuries to the head, thorax, and abdomen. The urogenital
system should be carefully evaluated specifically evaluating for open
fractures. If there is hemodynamic instability, the trauma surgeon,
orthopaedic surgeon, radiologist, and blood bank should work together
to stabilize the patient. The orthopaedic surgeon can provide temporary
relief with pelvic wrapping, external fixation, or wound packing
depending on the treatment of other injuries. If needed, operative
fixation can be done in the same session as surgery for associated
injuries or it can be timed later when the patient is stabilized.
with an immature pelvis and operative in children with an unstable
fracture pattern and a mature pelvis or closed triradiate cartilage.79 For toddlers, we prefer symptomatic treatment
that may include a spica cast for immobilization and comfort. In the
younger child with severe displacement, femoral traction on the
displaced side of the hemipelvis may be indicated if operative
reduction with implants may not be technically feasible. There is
growing body of evidence that unstable pelvic fractures treated
nonoperatively have poor results. Fracture reduction is indicated in
unstable fractures. The challenge is deciding what is unstable, the
uncommon incidence of these fractures, and the methods of fixation. The
technical principles are identical to those used for unstable pelvic
fractures in adults. Torode and Zieg Class IV injuries with
displacement and/or pelvic ring fractures with displacement of more
than 1 cm and anterior and posterior ring fractures should have
reduction and fixation. Open reduction of the sacroiliac joint or a
posterior iliac injury can be performed with a combination of plate
and/or screws. The approach can be anterior in the iliac fossa or
posterior depending on the fracture characteristics. Sacroiliac screws
can be used in the immature pelvis. The anatomy and size of S1 must be
adequate for screw placement. Imaging, including the use of fluoroscopy
for placement of the screws, is necessary. In older adolescents,
treatment should follow the guidelines for the treatment of adult
fractures, including a combination of internal and external fixation
for fracture stabilization and early mobilization. With a widened
symphysis, anterior external fixation or plating is recommended along
with posterior stabilization.
 |
|
FIGURE 20-20 Placement of a sacroiliac screw. A. Fluoroscopic lateral image of S1 to percutaneously localize the starting point for the guidewire. B.
Fluoroscopic 40-degree inlet view showing the direction of the guidewire for anterior and posterior placement in the sacroiliac body. C. Fluoroscopic 40-degree outlet view showing location of the guidewire in relation to the S1 foramen. D. Inlet view after screw placement. E. Outlet view showing screw placement in the body of S1. |
 |
|
FIGURE 20-21 A. Open pelvis fracture with severe displacement. B. The soft tissue injury precluded pelvic reduction and fixation. This radiograph shows remarkable late deformity.
|
pelvis is severe and, in addition to multiple breaks in the pelvic
ring, apparent or occult fractures of the sacrum may be present, with
or without neurologic involvement (Fig. 20-21). Massive hemorrhage,
although common in adults with severe pelvic fractures,19 is much less common in children with pelvic fractures.79
Nevertheless, up to 20% of children with crushed open pelvic fractures
in one series died within hours of admission secondary to uncontrolled
hemorrhage.54 The overall need for
blood transfusion in two large retrospective series including all types
of pediatric pelvic fractures was between 21% and 33%.19,29 In the setting of hypovolemic shock, however, emergency measures may be necessary.
blood loss before operative intervention. Occasionally, an external
fixator will be applied spanning the iliac crests in order to limit the
pelvic volume and thereby tamponade persistent bleeding. The rare
patient may also require arterial embolization and placement of an
inferior vena cava filter before operative intervention. It is
important to recognize injuries with marked comminution because mobile
fracture fragments may penetrate viscera (e.g., the bladder or
abdominal viscera) or lacerate the vagina or rectum.
reported that 13% of 116 pediatric pelvic fractures seen over a 12-year
period were open injuries. Fourteen of the 15 children were struck by
motor vehicles, and one sustained a gunshot wound. Five children with
stable fractures were treated nonoperatively, and 10 with unstable
fractures were treated operatively: external fixation alone (8
patients), combined external fixation and internal fixation (3
patients), and internal fixation alone (2 patients). Three of the
children died secondary to uncontrollable hemorrhage (2 patients) and
chest injury (1 patient). Eleven of the 12 surviving children had deep
wound infection or sepsis, and 3 had premature physeal closure.
Mosheiff and colleagues54 emphasized
that the treatment of the soft tissue injuries depends on stabilization
of the pelvis and that external fixation is often insufficient, and
posterior internal fixation and stabilization are often necessary.
reported two sacral fractures and seven sacroiliac
fracture-dislocations in their 54 patients. Sacral fractures are
probably more common than reported, but because they are obscured by
the bony pelvis and the soft tissue shadows of the abdominal viscera,
and because they are rarely displaced, they may be overlooked. Nine of
166 patients (5.4%) with pelvic fractures in the series by Silber et al.80
had associated sacral fractures, none with nerve root involvement.
There are two general types of sacral injuries. Spinal type injuries
may present as crush injury with vertical foreshortening of the sacrum
or horizontal fractures across the sacrum. These fractures may be
significant because they may damage the sacral nerves, resulting in
loss of bowel and bladder function. Alar type injuries are generally
vertical fractures through the ala or foramina. There fractures are
significant in that they may represent the posterior break of the
double ring fracture.
 |
|
FIGURE 20-22 A. An example of an anterior posterior pelvic radiograph where the sacral fracture is not well visualized. B. CT scan of the patient showing the sacral fracture.
|
clinically. Pain and swelling may be present, usually over the sacrum.
Rectal examination elicits pain on palpation. Occasionally, the
fracture fragments may be felt. Manual attempts at reduction should be
avoided because of the risk of rectal tear.
radiographs. The fracture can be oblique, but most are transverse with
minimal displacement and occur through a sacral foramen, which is the
weakest part of the body of the sacrum. Minimal offset of the foramen
or offset of the lateral edge of the body of the sacrum is an
indication of sacral fracture. Lateral views are helpful only if there
is anterior displacement, which is rare. A 35-degree caudad view of the
pelvis may reveal a fracture of the body of the sacrum. CT and MRI
scans are best in the identification of sacral fractures missed on
plain radiographic images.28,30,75
In one study comparing radiographs with CT scans in a consecutive
series of 103 pediatric trauma patients with pelvic radiographs and
pelvic CT scans, only three sacral fractures were identified with plain
radiographs whereas nine sacral fractures were identified with CT (Fig. 20-22).30
Sacral fractures are generally managed expectantly and treated
symptomatically. In rare cases, pinched sacral nerve roots may need to
be decompressed.
pain. The possibility of fracture must be entertained. Because the
coccyx is made up of multiple small segments, is obscured by soft
tissue, and naturally has a crook in it, it is difficult to determine
on
radiographs whether a coccygeal fracture has occurred, especially in a
child. These fractures rarely have associated injuries. Clinically,
patients describe immediate, severe pain in the area of the coccyx.
Pain on defecation may be present as well as pain on rectal
examination. Because radiographic identification is difficult, the
diagnosis should be made clinically by digital rectal examination.
Exquisite pain may be elicited, and an abnormal mobility of the
coccygeal fragments may be noted. Acute symptoms may abate in 1 to 2
weeks, but may be remarkably persistent. The differential diagnosis is
between fracture and coccydynia. Lateral radiographs of the coccyx with
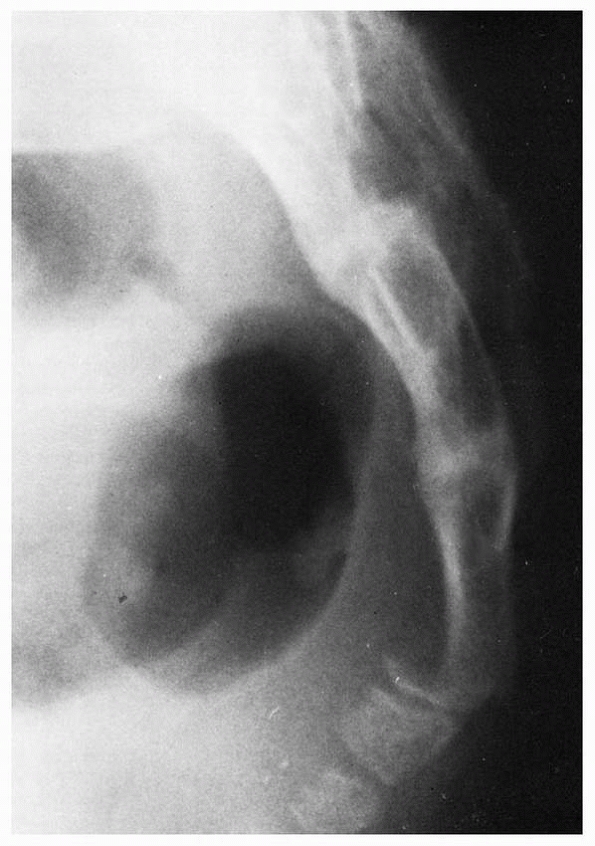
the hips flexed maximally may reveal a fracture (Fig. 20-23).
Apex posterior angulation of the coccyx is normal variant, and should
not be falsely interpreted as a fracture or dislocation. CT and MRI
scanning may be helpful in differentiating between physeal plates and
fracture lines.8 Treatment is
symptomatic only and consists of activity restriction and
pressure-relieving doughnut cushion for sitting with an expectation of
resolution in 4 to 6 weeks.
 |
|
FIGURE 20-23 Lateral radiograph with the hips maximally flexed reveals displaced coccygeal fracture in a 14-year-old boy.
|
 |
|
FIGURE 20-24 A. Pelvis radiograph showing a pelvis fracture with the left superior ramus injury propagating towards the triradiate cartilage. B. CT scan showing the ramus fractures propagating into the triradiate cartilage.
|
The remarkable difference between acetabular fractures in children and
adults is the presence of the triradiate cartilage in growing children.
This critical physeal area is responsible for acetabular growth and
development, acts as a stress riser in the pelvic ring, and is
susceptible to permanent damage. The mechanism of injury of acetabular
fractures in children is similar to that in adults: The fracture occurs
from a force transmitted through the femoral head. The position of the
leg with respect to the pelvis and the location of the impact determine
the fracture pattern; the magnitude of the force determines the
severity of the fracture or fracture-dislocation. Patients with
high-energy injuries usually have major associated injuries. Fractures
of the acetabulum are intimately associated with pelvic fractures. Some
acetabular fractures involve only the hip socket. Others represent the
exit point of a fracture of the pelvic ring. Pelvic fractures,
particularly ramus fractures, may propagate into the triradiate
cartilage (Fig. 20-24).
Their classification system is used to help determine the prognosis of
a triradiate cartilage injury that may result in a deformity of the
acetabulum with growth. The anatomy of the triradiate is such that the
superior weight-bearing portion of the acetabulum is separated from the
inferior third by the superior arms of the triradiate cartilage. These
superior arms are usually the ones involved in a fracture. In the
Bucholz classification, a type I or II injury occurs from a traumatic
force to the ischial ramus, pubic ramus, or proximal femur resulting in
a shearing force through the to superior arms of the triradiate
cartilage. If there is a metaphyseal bone fragment, this is a type II
fracture. A type V injury is a crush injury to the physis.10,47 Watts95
described four types of acetabular fractures in children: (i) small
fragments that most often occur with dislocation of the hip, (ii)
linear fractures that occur in association with pelvic fractures
without displacement and usually are stable, (iii) linear fractures
with hip joint instability,
and (iv) fractures secondary to central fracture-dislocation of the hip.
 |
|
FIGURE 20-25 Types of triradiate cartilage fractures. A. Normal triradiate cartilage. B. Salter-Harris type I fracture.
|
similarly to those in adults who are usually classified by the system
of Judet et al.38 and Letournel and Judet.46
A more comprehensive system is the AO comprehensive fracture
classification, which groups all fractures into A, B, and C types with
increasing severity. Type A acetabular fractures involve a single wall
or column; type B fractures involve both columns (transverse or
T-types) and a portion of the dome remains attached to the intact
ilium; and type C fractures involve both columns and separate the dome
fragment from the axial skeleton by a fracture through the ilium. Both
of these classification systems are discussed in more detail in
Rockwood and Green’s, Fractures in Adults, Chapter 36, Volume 2, of
this series in relation to adult fractures.
displacement of acetabular fragments after fracture. Inlet, outlet, and
45-degree oblique (Judet) views often are often needed to show
displacement. CT scanning is even better to show displacement and can
detect retained intra-articular fragments which can prevent concentric
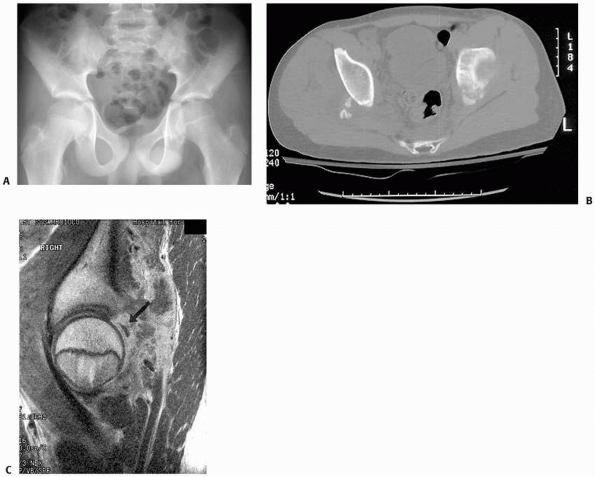
reduction (Fig. 20-26).13
Three-dimensional CT reconstructions can give an excellent view of the
overall bony fracture pattern but often underestimate the magnitude of
cartilaginous fragments, especially of posterior wall fractures in
children.71 Rubel et al.71
recommend MRI as an adjunctive imaging study for all pediatric
acetabular fractures because MRI discloses the true size of largely
cartilaginous posterior wall fragments in children (Fig. 20-27).
 |
|
FIGURE 20-26 A. Postreduction anteroposterior pelvis radiograph of a 12-year-old with the left hip appearing nonconcentric. B. CT scan showing a bony fragment from the posterior wall impeding reduction.
|
children are two. The first is to restore the mechanics of the hip. The
second is restoring alignment of the triradiate cartilage in hopes of
ensuring normal growth. The mechanical goals of treatment for
acetabular fractures in children are the same as for adults: to restore
joint congruity and hip stability. Schlickewei et al.72
noted that there are a variety of injury patterns and limited evidence
of outcomes for any specific treatment. Thus, each fracture should be
evaluated on an individual basis with the following guidelines: (i)
anatomic reduction will likely result in a good long-term outcome; (ii)
MRI is the best tool for identifying closure of the triradiate
cartilage; and (iii) patients should be informed on the possible growth
arrest and secondary associated problems such as joint subluxation or
dysplasia.72
Non-weight-bearing ambulation with crutches can be used for
nondisplaced or minimally (≤1 mm) displaced fractures. Because
weight-bearing forces must not be transmitted across the fracture,
crutch ambulation is appropriate only for older children
who
can reliably avoid weight bearing on the injured limb. Non-weight
bearing usually is continued for 6 to 8 weeks. In younger children,
this may be shortened to 5 to 6 weeks.
 |
|
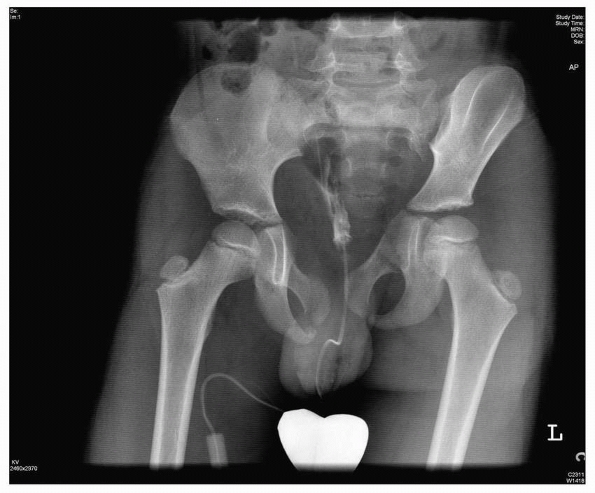
FIGURE 20-27 A. Postreduction radiograph of a left hip dislocation in a 12-year-old boy. B. CT scan demonstrates small ossified posterior wall fragments. C. Sagittal MRI demonstrates 90% posterior wall involvement with intra-articular step-off (black arrow).
(From Rubel IF, Kloen P, Potter HG, Helfet DL. MRI assessment of the posterior acetabular wall fracture in traumatic dislocation of the hip in children. Pediatr Radiol 2002;32(6):435-439, with permission.) |
recommended accurate reduction and internal fixation of any displaced
acetabular fracture in a child. They noted that the presence of
incomplete fractures and plastic deformation may make accurate
reduction difficult or impossible; they recommended that incomplete
fractures be completed and that osteotomies of the pubis, ilium, or
ischium be made if necessary for accurate reduction of the acetabulum.27
In children with open physes, all periacetabular metallic implants
should be removed 6 to 18 months after surgery. Improved outcomes with
early (<24 hours) fixation of acetabular fractures in adults have
been reported,61 and Gordon et al.27
noted that early fixation (before callus formation) is especially
important to prevent malunion in young patients in whom healing is
rapid (Fig. 20-28).
Linear growth of the acetabulum occurs by interstitial growth in the
triradiate part of the cartilage complex, causing the pubis, ischium,
and ilium to enlarge. The depth of the acetabulum develops in response
to the presence of a spherical femoral head and interstitial growth of
the acetabular cartilage. Growth derangement of all or part of the
triradiate cartilage as a result of fracture and a triradiate physeal
bar may result in a dysplastic acetabulum. Since the ilioischial limb
of the triradiate contributes the most to acetabular growth, injury to
the ilioischial limb of the triradiate cartilage has a greater
potential for late acetabular deformity that an anterior iliopubic limb
injury.25
bridge) of the triradiate cartilage has been reported after trauma to
the acetabulum. Heeg34 reported
acetabular deformity and subluxation of the hip in 2 of 3 patients with
premature fusion of the triradiate cartilage. Peterson and Robertson60
reported formation of a physeal osseous bar in a 7-year-old boy 2 years
after fracture of the lateral portion of the superior ramus at the
junction with the triradiate cartilage. After excision of the osseous
bridge, the physis remained open. Although the injured physis closed
earlier than the contralateral side, there was only a slight increase
in the thickness of the acetabular wall and lateral displacement of the
femoral head. Peterson and Robertson60
emphasized that early recognition and treatment are essential before
premature closure of the entire physis and development of permanent
osseous deformity (Fig. 20-30).60
The typical dysplastic changes seen after trauma to the triradiate
cartilage differ significantly from developmental dysplasia and include
both lateralization of the hip joint and acetabular retroversion.21
noted two main patterns of physeal injury in nine patients with
triradiate cartilage injury: a Salter-Harris type I or II injury, which
had a favorable prognosis for continued normal acetabular growth, and a
crush injury (Salter-Harris V), which had a poor prognosis with
premature closure of the
triradiate
cartilage caused by formation of a medial osseous bridge. In either
pattern, the prognosis depended on the child’s age at the time of
injury. In young children, especially those younger than 10 years of
age, acetabular growth abnormality was common and resulted in a
dysplastic acetabulum. By the time of skeletal maturity, disparate
growth increased the incongruity of the hip joint and led to
progressive subluxation. These authors found that acetabular
reconstruction was frequently necessary to correct the gradual
subluxation of the femoral head.10
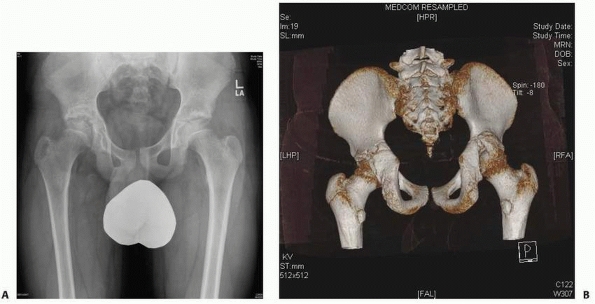 |
|
FIGURE 20-28 A.
Pelvic radiograph of a 12-year-old 1 year after an acetabular fracture. The fracture is a malunion with subluxation of the hip joint. B. Three-dimensional CT scan showing the malunited fragment. |
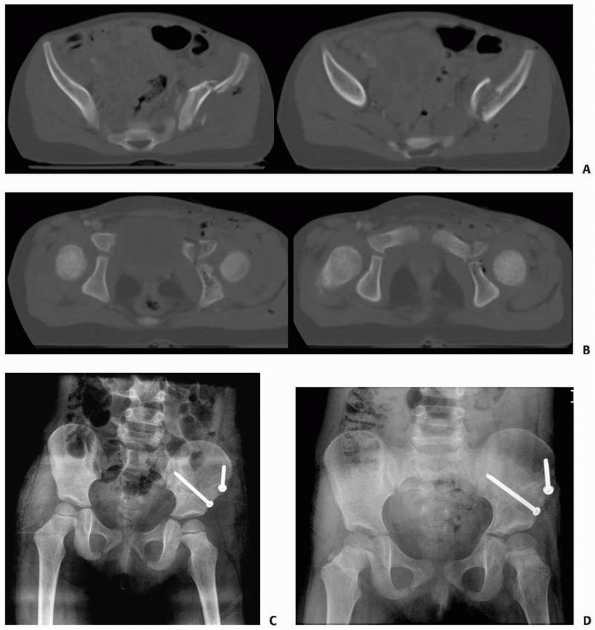 |
|
FIGURE 20-29 A. CT scan of a 7-year-old with a displaced pelvic wing fracture B. CT scan showing the fracture propagation into the triradiate cartilage. C. Anatomic reduction of the triradiate cartilage with open reduction and internal fixation. D. Despite anatomic reduction, a medial osseous bridge bar spans the triradiate cartilage.
|
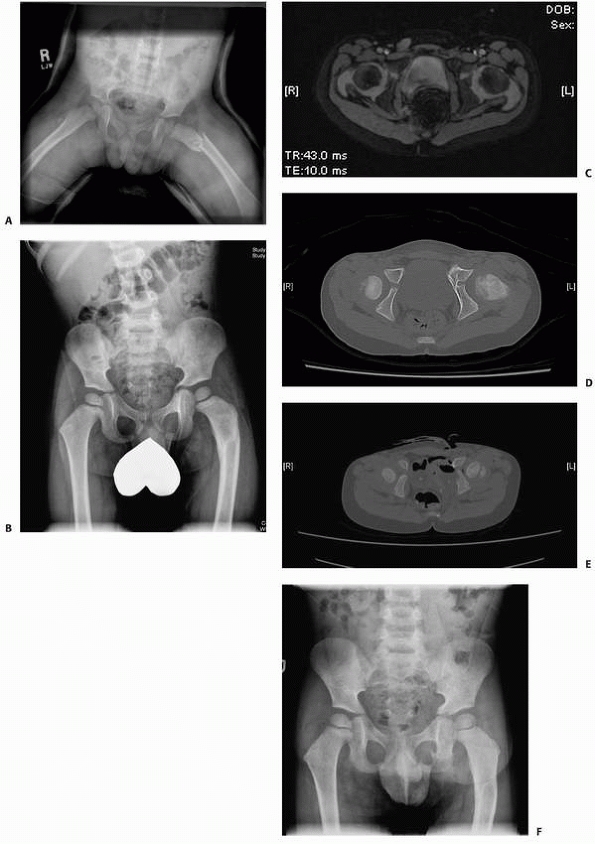 |
|
FIGURE 20-30 A. Radiograph of a 2-year-old with a ramus fracture that involves the triradiate cartilage. B. Six months after the injury, there is indication of a physeal bar on the medial aspect of the triradiate cartilage. C. MRI confirming the presence of a physeal bar. D. CT scan confirming the physeal bar. E.
CT scan confirming the physeal bar excision. This procedure was performed through an ilioinguinal approach and CT-guided excision. F. Radiograph of the pelvis after bar excision. |
|
TABLE 20-4 Surgical Exposure for Operative Fixation of Acetabular Fractures
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||
of the fracture and the direction of the displacement as determined on
the preoperative radiographs and CT scans (Table 20-4).27
Fractures of the posterior wall or posterior column can be approached
through a Kocher-Langenbeck approach with the patient either in the
lateral decubitus position (isolated posterior wall fracture) or supine
(associated posterior column fracture) (Fig. 20-31).
Anterior column injuries can be approached through an ilioinguinal
approach. Some transverse fractures may require an extended iliofemoral
approach.17 The extended lateral
approaches, which include the extended iliofemoral and triradiate
approaches, should be avoided as much as possible because of the risk
of devascularization of the ilium and heterotopic bone formation.31
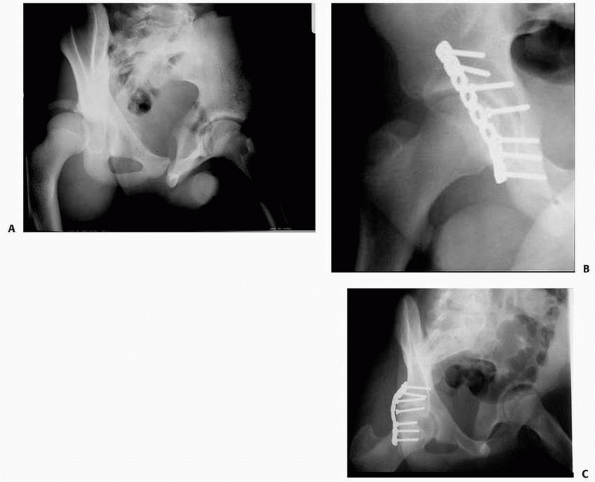 |
|
FIGURE 20-31 A. Radiograph of a football injury with posterior acetabular fracture and dislocation. B,C. Postoperative radiographs after a posterior approach and plating.
|
described the use of CT image-guided fixation of acetabular fractures
in 10 patients, including bilateral posterior wall fractures in a
14-year-old girl. They cite as advantages of image-guided surgery
reduced operating time (×20% reduction), less extensive surgical
dissection, reduced fluoroscopic time, and compatibility with
traditional fixation techniques. Most important, it allows accurate and
safe placement of screws
and
pins for acetabular fixation. This technology is attractive, but
anatomic reduction of the joint surface and secure fixation outweigh
the benefits of surgical convenience.
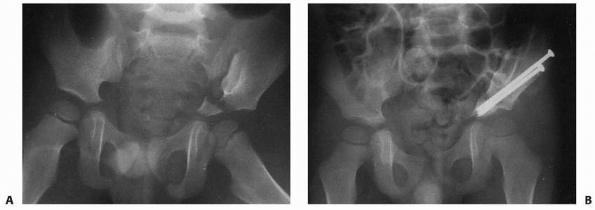 |
|
FIGURE 20-32 A. Fracture of the wing of the ilium with extension into the dome of the acetabulum in a 3-year-old boy. B.
After reduction and fixation with two cannulated screws. (From Habacker TA, Heinrich SD, Dehne R. Fracture of the superior pelvic quadrant in a child. J Pediatr Orthop 1995;15(1):69-72, with permission.) |
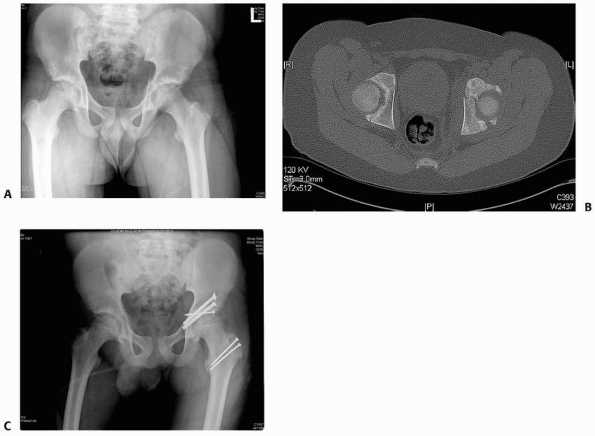 |
|
FIGURE 20-33 A. Radiograph of a 13-year-old with an acetabular fracture though the closing triradiate cartilage. B. CT scan showing the fracture in the region of the triradiate and posterior wall. C. Postoperative radiograph of the fracture fixed with cannulated screws via a surgical hip dislocation approach.
|
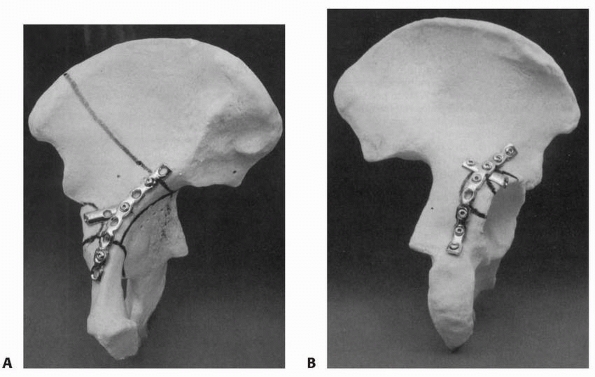 |
|
FIGURE 20-34 A. Anterior column plate and additional wall “hook” plate. B.
Posterior wall buttress plate and hook plate. (From Gordon RG, Karpik K, Hardy SEA. Techniques of operative reduction and fixation of pediatric and adolescent pelvic fractures. Oper Tech Orthop 1995;5:95-114, with permission.) |
weeks. If radiographs show adequate healing at that time, the cast is
removed and free mobility is allowed. In an older child with stable
fixation, crutches are used for protected weight bearing for 6 to 8
weeks. If radiographs show satisfactory healing, weight bearing is
progressed as tolerated. Return to vigorous activities, especially
competitive sports is delayed for at least 3 months.
an acetabular fracture looking for a triradiate closure. If the
radiographs indicate a physeal bar, CT and MRI can be obtained to
confirm the diagnosis. If the patient is less the 10 years of age, a
triradiate bar excision should be performed.
fracture leading to long-term morbidity and premature triradiate
closure after acetabular fracture. Because of the rapid healing in
young children, loss of reduction and nonunion usually are not
problems. Other reported complications include osteonecrosis, traumatic
arthritis, sciatic nerve palsy, heterotopic ossification, and stenosis
of the birth canal in female patients. Because of the possibility
dystocia during childbirth, pelvimetry is recommended before pregnancy.
Rieger and Brug69 reported one
female patient who required cesarean section because of ossification of
the symphysis pubis after nonoperative treatment of an open-book
fracture. Schwarz et al.74 reported
leg-length discrepancies of 1 to 5 cm in 10 of 17 patients after
nonoperative treatment of unstable pelvic fractures; 5 had low back
pain at long-term follow-up. Nine of 10 patients with lumbar scoliosis
had low back pain. McDonald51
reported that one third of 15 skeletally immature patients treated
nonoperatively with unstable pelvic fractures had residual pain. Heeg
and Klassen33 reviewed 18 children
with unstable pelvic fractures and reported that 9 had a leg-length
discrepancy greater the 1 cm and 3 had back pain.
children is residual deformity, which may lead to leg-length
discrepancy, sacroiliac joint arthrosis, back pain, lumbar scoliosis,
incompetency of the pelvic floor, and distortion of the birth canal.
The complications of acetabular fracture late hip instability, hip
arthrosis, and triradiate growth that may lead to joint subluxation or
dysplasia.
K, Bircher MD, Stanton SL. Pelvic floor dysfunction in women after
pelvic trauma. Br. J Obster Gynecol 2004;111:499-502.
ST, Hinds RB. Pseudotumor of the ischium. A late manifestation of
avulsion of the ischial epiphysis. J Bone Joint Surg Am
1972;54(3):645-647.
SJ, Gotschall SC, Eichelberger MR. Predictors of abdominal injury in
children with pelvic fracture. J Trauma 1991;31(8):1169-1173.
DR, Hayman LA, Herrick RC, et al. Postnatal maturation of the sacrum
and coccyx: MR imaging, helical CT, and conventional radiography. AJR
Am J Roentgenol 1998;170(4):1061-1066.
GA, Willis MC, Firoozbakhsh K, et al. Computed tomography image-guided
surgery in complex acetabular fractures. Clin Orthop Relat Res
2000;370:219-226.
AR, Eastridge BJ, Young JW, et al. Pelvic ring disruptions: effective
classification system and treatment protocols. J Trauma
1990;30(7):848-856.
J, Ross SE. The ischiopubic synchondrosis in healthy children: some
normal roentgenologic findings. Am J Roentgenol Radium Ther Nucl Med
1956;76(3):488-494.
Ng BK, Ying SY, et al. A 10-year study of the changes in the pattern
and treatment of 6493 fractures. J Pediatr Orthop 1999;19(3):344-350.
AH. Extensile acetabular approaches. In Canale ST, ed. Campbell’s
Operative Orthopaedics. Vol. 1. 10th ed. St. Louis: Mosby, 2003:77-86.
D, Karaiskakis M, Velmahos GC, et al. Pelvic fractures in pediatric and
adult trauma patients: are they different injuries? J Trauma
2003;54(6):1146-1151.
V, Daneman A, Krajbich I, et al. CT appearance of sacroiliac joint
trauma in children. J Comput Assist Tomogr 1985;9(2):352-356.
C, Zurbach J, Hersche O, et al. Pathomorphologic characteristics of
posttraumatic acetabular dysplasia. J Orthop Trauma 2000;14(7):483-489.
R, Weiss R, Hallel T. Acetabaular dyspasia and hip dislocation after
selective premature fusion of the triradiate cartilage. J Bone Joint
Surg Br 1984;66(3):334-336.
RW, Hansen CA. Incomplete avulsion of a portion of the iliac epiphysis:
an injury of young athletes. J Bone Joint Surg Am 1973;55(6):1301-1302.
RG, Karpik K, Hardy S.Techniques of operative reduction and fixation of
pediatric and adolescent pelvic fractures. Oper Tech Orthop
1995;5:95-114.
D, Wardell S, Sarwark S, et al. Fatigue fractures of the sacrum in
children: two case reports and a review of the literature. Skeletal
Radiol 1993;22(7):515-518.
OD, Mahboubi S, Stafford PW,et al. The utility of the pelvic radiograph
in the assessment of pediatric pelvic fractures. J Trauma
2003;55(2):236-239.
O, Strohm PC, Culemann U, et al. Mortality in patients with pelvic
fractures: results from the German pelvic injury register. J Trauma
2008;64(2):449-455.
M, Visser JD, Oostvogel HJ. Injuries of the acetabular triradiate
cartilage and sacroiliac joint. J Bone Joint Surg Br 1988;70(1):34-37.
SD, Gallagher D, Harris M, et al. Undiagnosed fractures in severely
injured children and young adults. Identification with technetium
imaging. J Bone Joint Surg Am 1994;76(4):561-572.
R, Judet J, Letournel E. Fractures of the acetabulum: classification
and surgical approaches for open reduction. Preliminary report. J Bone
Joint Surg Am,1964;46: 1615-1646.
EP Jr, Nelson DS, Carroll KL, et al. A prospective evaluation of the
clinical presentation of pediatric pelvic fractures. J Trauma
2001;51(1):64-68.
M, Goulet JA, Mueller KL, et al. Operative treatment of unstable
pediatric pelvis and acetabular fractures. J Pediatr Orthop
2005;25(1):34-38.
RA, Rozinov VM, Malakhov OA, et al. Pelvic polyfractures in children.
Radiographic diagnosis and treatment. Clin Orthop Relat Res
1995;320:28-33.
A, Fogarty E, Dowling F. The pelvic fracture in childhood: a report
supporting nonoperative management. Injury 1995;26(5):327-329.
F, Ong B, Mohaideen A, et al. Development and injury of the triradiate
cartilage with its effects on acetabular development: review of the
literature. J Trauma 2003; 54(6):1245-1249.
D, Fishman EK, Ney DR, et al. Acetabular and pelvic fractures in the
pediatric patient: value of two- and three-dimensional imaging. J
Pediatr Orthop 1992;12(5): 621-625.
RC Jr, Bensard DD, Moore EE, et al. Pelvic fracture geometry predicts
risk of life-threatening hemorrhage in children. J Trauma
1993;35(3):423-429.
CA, Fischer RP, Cotler HB, et al. Selective management of pediatric
pelvic fractures: a conservative approach. J Pediatr Surg
1987;22(6):538-540.
G, Volpin G, Bialik V. Pelvic fractures in children: a follow-up in 20
children treated conservatively. J Pediatr Orthop B 1993;1:140-142.
HA, Robertson, RC. Premature partial closure of the triradiate
cartilage treated with excision of a physical osseous bar. Case report
with a 14-year follow-up. J Bone Joint Surg Am 1997;79(5):767-770.
T. Pelvic ring injuries: assessment and concepts of surgical
management. In: Ruedi TP, Murphy W, eds. AO Principles of Fracture
Management. New York: Thieme, 2000:391-439.
IV. Growth and development of the acetabulum in the normal child.
Anatomical, histological, and roentgenographic studies. J Bone Joint
Surg Am 1978;60(5):575-585.
SA, Helikson MA, Shorter N, et al. Pelvic fractures in children-review
of 120 patients with a new look at general management. J Pediatr Surg
1980;15(6):727-734.
F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent
competitive athletes: prevalence, location, and sports distribution of
203 cases collected. Skeletal Radiol 2001;30(3):127-131.
IF, Kloen P, Potter HG, et al. MRI assessment of the posterior
acetabular wall fracture in traumatic dislocation of the hip in
children. Pediatr Radiol 2002;32(6): 435-439.
J, Olix ML. Functional disability following avulsion fracture of the
ischial epiphysis. Report of two cases. J Bone Joint Surg Am
1972;54(3):641-644.
G, Mower WR, Bergman J, et al. Poor test characteristics for the
digital rectal examination in trauma patients. Ann Emerg Med
2007;50(1):25-33.
P, Densmore J, Werner M, et al. Pediatric pelvic injury: functional
outcome at 6-month follow-up. J Pediatr Surg 2005;40(1):107-112.
JS, Flynn JM. Changing patterns of pediatric pelvic fractures with
skeletal maturation: implications for classification and management. J
Pediatr Orthop 2002;22(1): 22-26.
J, Flynn JM, Koffler KM, et al. Analysis of the causes, classification,
and associated injuries of 166 consecutive pediatric pelvic fractures.
J Pediatr Orthop 2001;21(4): 446-450.
JS, Flynn JM, Katz AM, et al. Role of computed tomography in the
classification and management of pediatric pelvic fractures. J Pediatr
Orthop 2001;21(2):148-151.
W, Shurnas P, Morgan S, et al. Clinical outcomes of unstable pelvic
fractures in skeletally immature patients. J Bone Joint Surg Am
2005;87(11):2423-2431.
RJ, Baacke M, Gotzen L. Comminuted pelvic ring disruption in toddlers:
management of a rare injury. J Trauma 2000;48(1):161-164.
M, Arslan H, Necmioglu S, et al. Long-term outcomes of conservatively
treated pediatric pelvic fractures. Injury 2004;35(8):771-781.
M, Carty H. Avulsion fractures of the pelvis in children: a report of
32 fractures and their outcome. Skeletal Radiol 1994;23(2):85-90.
GJ, Kaplan GW, Lerman SL, et al. Lower genitourinary injury and pelvic
fractures in pediatric patients. Urology 2002;59(1):123-126.
M, Helfet DL, Kellam J, eds. Fractures of the Pelvis and Acetabulum.
3rd ed. Baltimore: Lippincott Williams & Wilkins, 2003.
VT. Orthopaedic treatment of fractures of the long bones and pelvis in
children who have multiple injuries. Instr Course Lect 2000;49:415-423.
J, Gardner M, Gaines B, et al. Early functional outcomes in children
with pelvic fractures. J Pediatr Surg 2000;35(6):1002-1005.
WD, Garcia, VF. Pediatric pelvic fractures combined with an additional
skeletal injury is an indicator of significant injury. Surg Gynecol
Obstet 1993;177(5):468-472.
B, Smith WR, Towers J, et al. Iliosacral screw fixation of the
posterior pelvic ring using local anaesthesia and computerised
tomography. J Bone Joint Surg Br 2003;85(3): 411-418.
