Forearm Fractures: Open Reduction Internal Fixation
permits elbow, forearm, and wrist motion. Loss of normal angular
alignment results in loss of forearm supination and pronation (1,2).
Angular deformity in single bone fractures of the forearm with
associated soft-tissue injury result in dislocation. Isolated ulna
fractures are often referred to as Monteggia fractures and are
recognized as having an associated injury or dislocation of the
proximal radioulnar joint. Isolated fractures of the radius are
accompanied by a distal radioulnar joint (DRUJ) dislocation and are
often called a Galeazzi fracture. Open reduction and internal fixation
(ORIF) of displaced forearm fractures in the skeletally mature patient
remains the standard treatment for displaced forearm fractures.
Internal fixation allows for maintenance of fracture alignment during
healing while the patient performs functional range of motion with the
arm. Outcomes following internal fixation provide better results than
nonoperative treatment (3,4,5,6,7,8).
remain the exception to this general rule. The “night stick” fracture,
as it is commonly called, does not have the degree of soft-tissue
injury recognized in other fractures of the forearm, and the likelihood
of acute instability of the distal or proximal radioulnar articulations
is absent. Fractures involving the distal third of the ulna should be
evaluated closely and observed carefully over time as angular deformity
can result in significant functional impairment at the DRUJ. Operative
fixation of isolated ulna fractures, regardless of injury mechanism, is
recommended in open fractures, fractures angulated greater then 10
degrees in any plane, and in fractures with greater than 50%
comminution (9).
necessary for developing a treatment plan. A detailed history related
to mechanism of injury, hand dominance, occupation,
previous
injury, and associated medical problems is required. The entire
extremity needs to be carefully examined for associated injuries.
Circumferential inspection of the extremity should be performed to
identify the presence of an open fracture as well as to assess the
extent and severity of the soft-tissue injury. Any violation of the
skin in reasonable proximity to the fracture should be enough to
consider the injury an open fracture. Ecchymosis, fracture blisters,
and edema suggest that the soft tissue absorbed significant energy and
the index of suspicion for compartment syndrome should be high.
Palpation for tenderness and instability should be performed from the
shoulder to the hand. The elbow, wrist, and carpal bones should receive
special attention.
scaphoid fractures, and carpal instability are common. Neurological
examination should be focused and include the motor and sensory status
of the radial (posterior interosseous, superficial radial), ulnar, and
median nerves. Vascular examination should focus on the perfusion of
the extremity and should include palpation of the brachial radial and
ulnar pulses.
application of splinting material, should consist of orthogonal
radiographs (AP and lateral) that include both the wrist and the elbow.
In situations when the physical examination indicates additional injury
or radiographs are inadequate or inspire suspicion that associated
injuries exist, joint specific views of the wrist and elbow should be
obtained. Radiographic evaluation should never inhibit the overall care
of the patient. In the patient with multiple injuries as well as in the
patient with soft-tissue injury or neurological or vascular compromise,
a provisional reduction and splint should be applied prior to obtaining
radiographs. Traction radiographs often facilitate evaluation of
comminuted fractures. Difficult to obtain without proper sedation,
these radiographs are best obtained following induction of anesthesia
prior to surgery. Stress radiographs of the joints for associated
instability can also be obtained at this time, and fluoroscopy is often
helpful in this regard.
physical examination consists of basic open-fracture wound management
(if present) and gross realignment and splint immobilization of the
forearm to limit pain and further soft-tissue injury while definitive
fracture fixation is pending. In cases of marked angulation or vascular
compromise, realignment should be performed immediately. In a Monteggia
fracture with a dislocated radial head, gentle traction and supination
with conscious sedation or regional anesthesia (Bier block) is
necessary to reduce the dislocation. In most other situations, adequate
analgesia will permit gross realignment and splint application of the
forearm. A long-arm posterior splint is preferred. A sugar tong splint,
while adequate in many patients, can result in unnecessary skin
breakdown in the supracondylar area. Following any manipulation, the
neurological and vascular status of the extremity should be reevaluated
and documented.
condition of the soft tissues and the general condition of the patient.
Internal fixation is warranted on an emergent basis for open fractures,
impending or frank compartment syndrome, and irreducible dislocation
with impending skin breakdown or neurological deficit. In other
situations, the surgery can be performed in a more elective setting.
The reduction, however, becomes more difficult with time, and
additional soft-tissue dissection may be required to achieve reduction
when fracture fixation is delayed beyond 72 hours. Several studies on
open fractures have shown no increased morbidity with immediate plate
fixation (6,10). Repeat
irrigation and debridement are dictated by the severity of the
soft-tissue injury and viability following initial plate fixation. In
the patient with multisystem trauma and an open forearm fracture,
external fixation following irrigation and debridement may be used as a
temporizing measure until the patient’s general condition is allowed to
improve.
3.5-mm plate that allows for dynamic compression and application of lag
screws through the plate. These implants are available in full contact
and limited contact designs. They are available in either titanium or
stainless steel from a variety of manufacturers. In theory, low-contact
plates limit devitalization of the underlying bone, and titanium
decreases the likelihood of stress shielding. Excellent results can be
achieved with any of these implant choices. Recently, locked
compression plates have been introduced as a fixation option. Their
role in diaphyseal fractures of the forearm remains
undefined and to a large extent appears to be unnecessary except in cases of significant osteoporosis (11). In adults, reconstruction and one-third tubular plates are contraindicated.
should be determined following full evaluation of radiographs and
characterization of the fracture pattern. Implant templates are
available to aid in this process and should be used liberally.
Traditional technique has called for the use of plates that can obtain
a minimum of 6 cortices of fixation on either side of the fracture. The
use of long plates with spaced screws is also an option. More
important, a well thought-out surgical plan should be developed to
achieve reduction and fixation. This is paramount when utilizing
indirect reduction aids to restore length and alignment.
cases, general anesthesia is preferred so that accurate postoperative
assessment of neurological function and evaluation for compartment
syndrome can be ensured. The patient is positioned supine and the arm
is placed on a radiolucent arm board. Following the induction of
anesthesia, a nonsterile tourniquet is applied, and in the case of
comminuted fractures, traction radiographs are obtained by applying
longitudinal traction to the hand while an assistant or the surgeon
applies counter traction in the upper arm.
fashion. In the case of open fractures, the tourniquet is not utilized
so that further anoxic injury to the traumatized soft tissue can be
avoided. In closed fractures, the limb is exsanguinated and the
tourniquet is inflated to 250 psi. Surgical incisions are then drawn on
the extremity, and the fracture site is localized with the C-arm and
marked. In general, the least comminuted fracture is approached first
to aid in the indirect reduction of the other fracture(s). In
noncomminuted fractures, the radius is generally approached first. Loop
magnification may be utilized for volar forearm dissections to better
recognize and control bleeding vessels. Bipolar cautery is utilized
when the surgeon is working in close proximity to the nerves, and small
ligature clips are utilized liberally during the dissection.
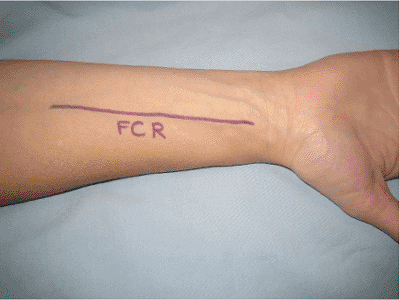
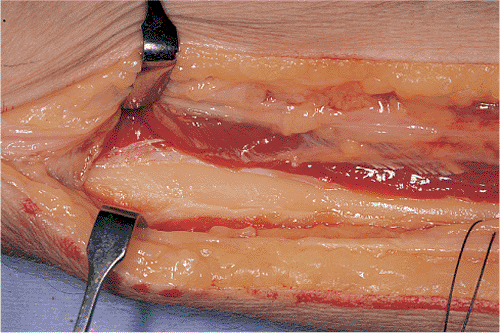
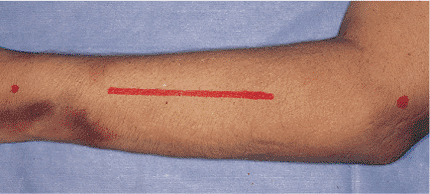
a volar approach based on the flexor carpi radialis (FCR) is utilized.
The surgical incision is located just radial to the FCR tendon (Fig. 10.1).
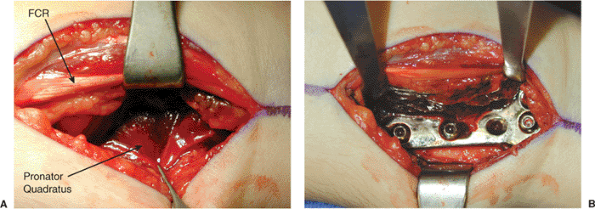
Following the skin incision, the FCR tendon sheath is split
longitudinally and the FCR tendon is retracted ulnarly. The floor of
the tendon sheath is then incised. The flexor pollicis longus (FPL) is
then encountered and
retracted
ulnarly; this action adds further protection to the median nerve. The
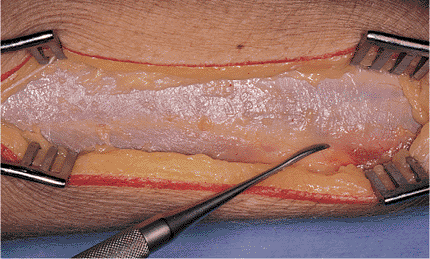
pronator quadratus is then incised, elevated from the periosteum, and
retracted ulnarly to expose the distal third of the radius (Fig. 10.2). This exposure offers the benefit of avoiding direct dissection of the radial artery, which the FCR sheath protects.
 |
|
Figure 10.1. The surgical incision is based just radial to the FCR tendon.
|
 |
|
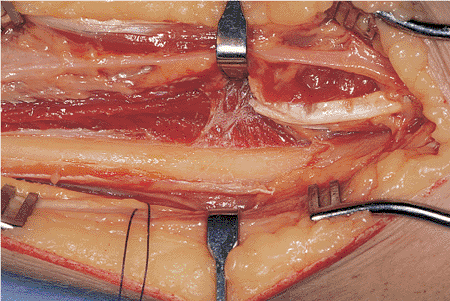
Figure 10.2. A. The floor of the tendon sheath is incised. The FPL is encountered and retracted ulnarly. B. The pronator quadratus is elevated from the periosteum and retracted ulnarly.
|
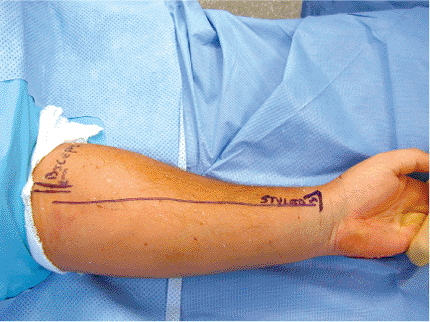
Adequate exposure can be obtained from the biceps tuberosity to the
distal-radial articular surface. The surgical skin incision extends
from the biceps tendon to the radial styloid, generally following the
lateral aspect of the FCR (Fig. 10.3). In the
distal aspect of the incision, the radial artery is in close proximity
to the volar fascia, and careful scissor dissection initiated
proximally and proceeding distally will keep the surgeon from injuring
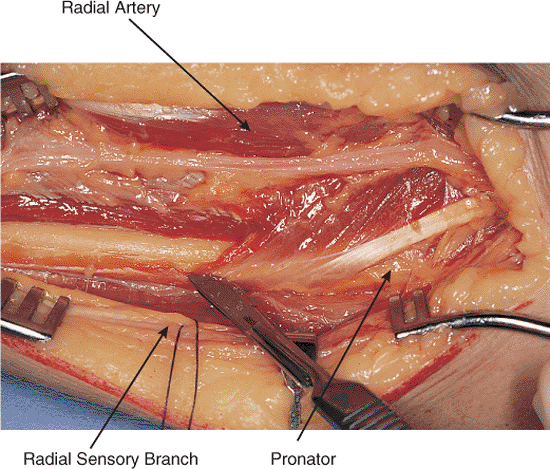
this structure. The proximal plane between the brachioradialis and the
FCR should be developed (Fig. 10.4).
direction dictated by associated soft-tissue conditions. Loop
dissection is tremendously helpful when dissecting the radial artery
because it allows for recognition of the small vascular branches that
are associated with the artery and their subsequent clip ligature or
cautery.
nerve is found on the under surface of the proximal brachioradialis. It
pierces the fascia and emerges on the superficial surface of the
brachioradialis. Deep dissection distally includes incising the
pronator quadratus
from its radial attachment such that it is dissected off the underlying periosteum and retracted ulnarly along with the FPL (Fig. 10.5).
 |
|
Figure 10.3. The surgical incision is based just radial to the FCR tendon.
|
 |
|
Figure 10.4.
The volar fascia is opened to expose the brachioradialis and the FCR muscles. The interval between these muscles is developed bluntly. The sensory branch of the radial nerve courses beneath the brachioradialis and pierces the volar fascia in the distal third. |
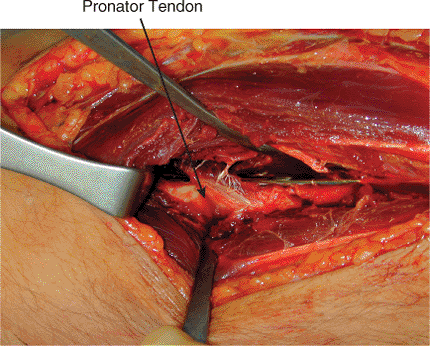
In an alternative, the pronator teres attachment can be preserved and
the tendon can be elevated from the volar surface of the radius to
accommodate a submuscular/tendinous plate (Fig. 10.7).
elevator and retracted radially while the flexor digitorum
superficialis is elevated and retracted ulnarly to expose the
biceps tuberosity (Fig. 10.8). In this area, bipolar cautery should be utilized secondary to the proximity of the posterior interosseous nerve.
 |
|
Figure 10.5.
The distal third of the radial shaft is exposed with retraction of the brachioradialis radially and FCR ulnarly. The radius is relatively flat in this zone, and the plate generally needs minimal contouring. |
 |
|
Figure 10.6. The pronator teres has been elevated sharply to expose the middle third of the radius.
|
radius that offers complete access from the radial head to the distal
articular surface (13). Secondary to the risk
to the posterior interosseous nerve and irritation caused by dorsal
plate fixation of the overlying tendons, this approach is used less
frequently than the FCR or Henry approaches. The dorsal approach is
reserved for open fractures with a dorsal-based soft-tissue lesion,
fractures that require exploration of the posterior interosseous nerve,
and select proximal-third radial fractures. The skin excision extends
from the lateral epicondyle to the ulnar aspect of Lister’s tubercle (Fig. 10.9).
 |
|
Figure 10.7.
The pronator attachment can be preserved and the tendon can be elevated from the volar surface of the radius allowing submuscular/tendinous placement of a plate. |
 |
|
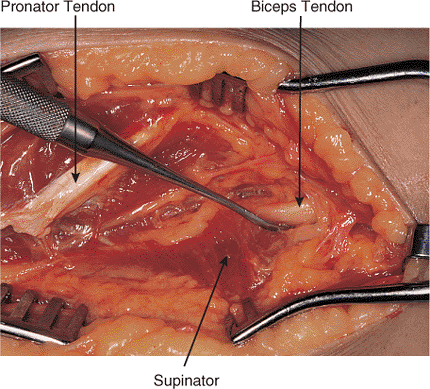
Figure 10.8.
The Henry approach can be extended to the proximal third of the radius if needed. The probe shows the insertion of the bicipital tendon. |
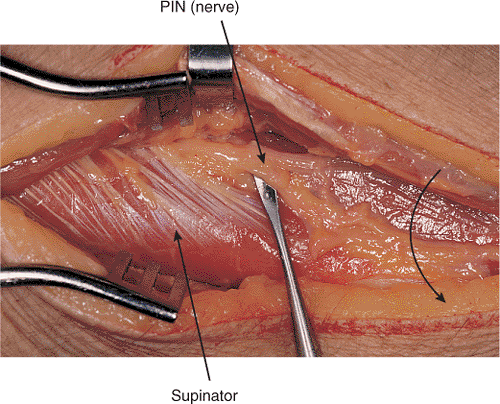
(ECRB) and the extensor digitorum comminus (EDC) is developed
proximally. The interval between the muscles is more easily recognized
in the distal forearm (Fig. 10.10). Once this
interval is developed, the posterior interosseous nerve (PIN) is
localized as it emerges from the mid substance of the supinator muscle.
The nerve must be dissected out of the supinator while care is taken to
protect the branches of the nerve to the supinator muscle (Fig. 10.11).
 |
|
Figure 10.9.
The dorsal approach to the radius is marked along a line from the lateral humeral epicondyle to the ulnar side of Lister’s tubercle. |
beneficial. The arm is supinated to expose the attachment of the
supinator and the pronator teres, both of which are detached and
subperiosteally elevated toward their origins. As the approach is
developed distally, the abductor pollicis longus (APL) and the extensor
pollicis brevis are obliquely crossing the radius (Fig. 10.12).
The muscles are elevated from the underlying periosteum and retracted
either radially or ulnarly to facilitate exposure. In the most distal
aspect of the approach, the interval between the ECRB and the extensor
pollicis longus (EPL) is developed. As with all approaches to the
forearm, the extent of dissection is based on the fracture location and
the length of the plate to be utilized.
dorsal approach to the entire ulna. The arm is flexed on the table to
provide access to the subcutaneous border and needs to be supported
during dissection (Fig. 10.13). The interval is
between the extensor carpi ulnaris (ECU) and the flexor carpi ulnaris.
To avoid subcutaneous placement of internal fixation, the ECU is
retracted and the dorsal aspect of the ulna is exposed (Fig. 10.14).
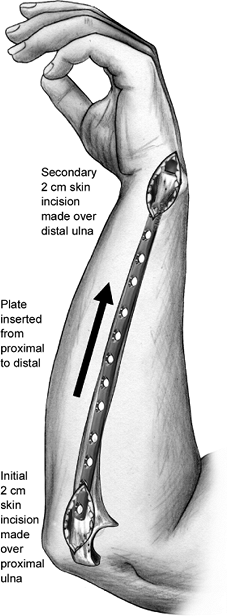
percutaneous plate placement, particularly in comminuted fractures.
Following indirect reduction of the ulna by either plate fixation of
the radius or provisional reduction utilizing an external fixator, 2-cm
incisions
are
made along the subcutaneous border of the ulna, and the overlying skin
is mobilized from the deep tissue with an elevator directed toward the
fracture. The plate is then inserted along the bone until it is exposed
in the opposite incision. The process is visualized with an image
intensifier. The plate is then secured to the bone with screws via the
two small incisions and strategically placed stab incisions along the
subcutaneous border of the ulna (Fig. 10.15).
When placed percutaneously in this manner, plates lie along the
subcutaneous border and thus increase the likelihood of symptoms
related to the internal fixation.
 |
|
Figure 10.10. The dorsal investing fascia is examined to define the interval between the ECRB and the EDC.
|
 |
|
Figure 10.11. The forearm is pronated, which brings the PIN closer to the operative field and may increase the risk for injury.
|
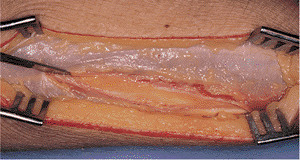
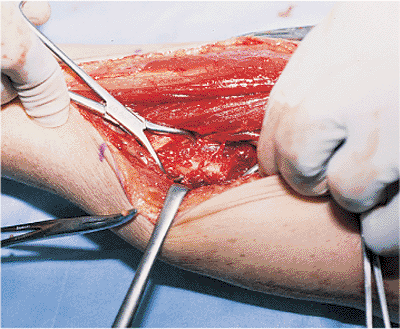
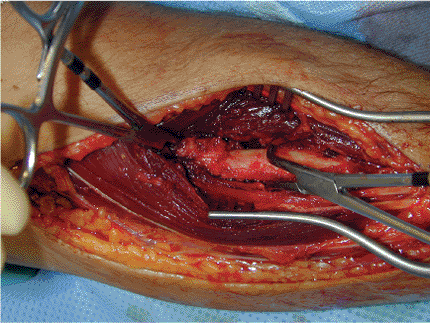
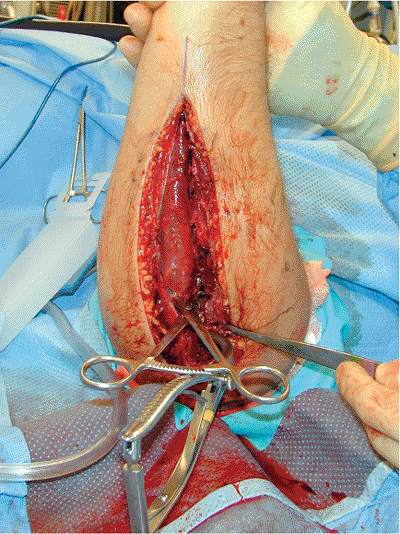
reduction and internal fixation. Soft tissues are retracted with right
angle retractors or strategically placed (extraperiosteally when
possible) small Homan retractors. Broad retractors should be avoided to
eliminate unnecessary soft-tissue stripping (Fig. 10.16). In transverse and short, oblique
fracture patterns, direct reduction followed by lag screw and
compression plating techniques are recommended. Pointed reduction
forceps or serrated reduction forceps are used to grasp the bone and
draw it out to length; the fracture is then reduced under direct
visualization (Fig. 10.17).
 |
|
Figure 10.12.
The dorsal fascia is incised along this interval. The APL crosses the dorsal surface of the radius obliquely in the distal portion of the exposure. |
 |
|
Figure 10.13.
The subcutaneous approach to the ulna is marked with the elbow flexed and the forearm in neutral rotation. The fracture site should be palpated to determine the midpoint of the incision. |
 |
|
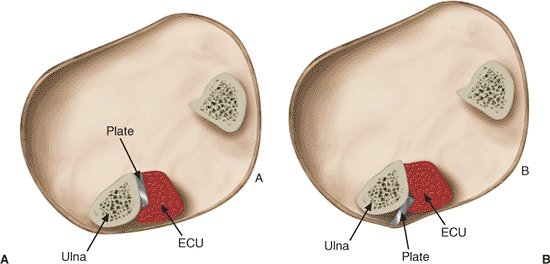
Figure 10.14. A.
The plate along the subcutaneous border of the ulna should be placed so that it lies beneath the ECU and is recessed dorsal to the subcutaneous border of the ulna. B. This reduces painful symptoms related to a prominent plate that most frequently occurs when the forearm is placed on a rigid surface. |
a reduced position by placing the pointed reduction forceps
perpendicular to the fracture line. Compression across the fracture
should then be obtained with a lag screw. When the fracture orientation
permits, lag screw fixation through the plate (after compression of the
fracture with the plate) will enhance the stability of the construct.
In transverse fractures, a contoured plate is secured to the bone with
a bicortical screw in the most distal aspect of the plate after the
surgeon ensures it is centered on the bone. Opposite the fracture, an
additional bicortical screw is
placed
in an eccentrically drilled hole to compress effectively the fracture
as it is tightened. Prior to final tightening, the clamps anchoring the
plate to the bone should be loosened or removed to allow the plate to
slide in relationship to the compressing screw. The clamps are then
removed and two additional screws are placed in the neutral position on
either side of and in close proximity to the fracture. Additional screw
fixation is unnecessary in bone of regular quality. In poor quality
bone, a minimum of six to eight cortices of fixation should be obtained
on either side of the fracture or use of a locked plate device should
be considered.
 |
|
Figure 10.15.
An incision measuring 2 cm is made over the subcutaneous proximal ulna and carried down to the periosteum. The subcutaneous tissue is elevated from the periosteum by pushing a plate along the subcutaneous border of the ulna. With the plate inserted, a separate 2-cm incision is made over the plate at the distal ulna. The plate is then centered on the bone at both ends and screws are placed. If additional screws are required closer to the fracture, stab wounds are made over the plate and screws are inserted percutaneously. |
 |
|
Figure 10.16.
Exposure is facilitated through the use of right-angle retractors and small Weber clamps. Extensive dissection of soft tissue with wide exposure of the fracture site is avoided. |
 |
|
Figure 10.17.
Pointed reduction forceps or serrated reduction forceps are used to grasp the bone and draw it out to length. The fracture is reduced under direct visualization. |
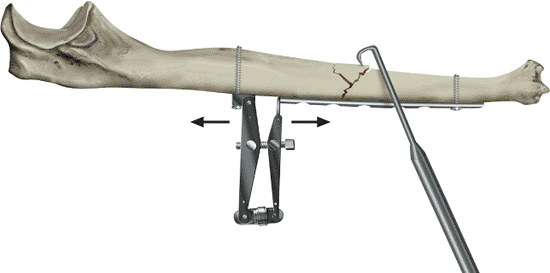
reduction techniques and the application of a bridge plate. In this
situation, individual reductions of the comminuted fragments are
avoided and dissection in the area of the main fracture should be
limited. Restoration of length and alignment can be obtained by several
methods. The fracture can be brought out to length by the surgeon
grasping the bone with pointed reduction forceps or serrated reduction
forceps on opposite sides of the fracture, drawing it out to length,
and then clamping the plate to the bone to maintain length while screw
fixation is obtained.
length and alignment include application of the plate to the distal
aspect of the bone with one or two screws placed in the neutral
position, then the application of a push-pull screw in the proximal
aspect of the plate. A tension distraction device or a lamina spreader
is then utilized to push the fracture out to length. During this
process, two loosely applied clamps placed perpendicular to one another
around the plate will control alignment during the distraction process (Figs. 10.18 and 10.19).
When the bone is appropriately brought out to the correct length, two
screws are placed in the neutral position; one in close proximity to
the fracture and one in the most proximal aspect of the plate. With
good indirect technique, bone grafting is not required even in
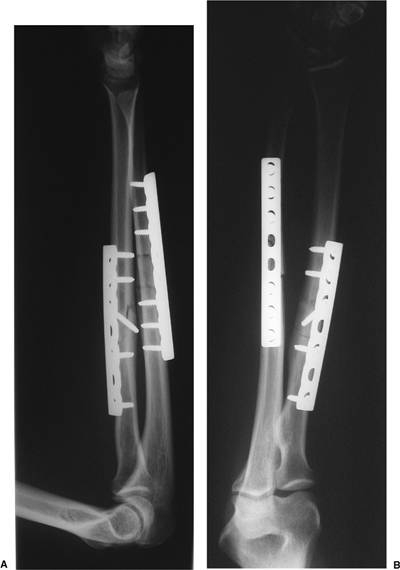
comminuted fractures (Fig. 10.20) (14).
the range of motion and the stability of both the proximal and distal
radial and ulnar articulations should be checked. In Galeazzi
fractures, if the DRUJ is stable through a full range of motion no
immobilization is required. If it is only stable in supination, the
extremity should be initially splinted and then casted in supination
for 6 weeks. If the DRUJ is unstable in all positions, the joint should
be reduced and pinned with a 2.0-mm Kirschner (K) wire, and ulnar
styloid fractures should be repaired. The extremity should then be
immobilized in a cast in the reduced position for 6 weeks.
reduced, the fracture reduction needs to be carefully checked to ensure
that anatomic length of the ulna has been restored. If
the
radial head remains dislocated and the ulna has been correctly reduced,
then the proximal radioulnar joint should be explored and the annular
ligament reconstructed. If the joint is reduced and stable, then no
additional immobilization is required, but if it is unstable, then it
should be reduced in a stable position, usually supination, for 6 weeks.
 |
|
Figure 10.18.
Indirect reduction of the ulna is depicted. A laminar spreader and screw are used for distraction of the fracture. The dental pick is used to tease the wedge fragment into position. The laminar spreader is then gradually released, and the fracture is compressed with an eccentrically placed screw. |
 |
|
Figure 10.19.
A lamina spreader is utilized to push the fracture out to length. During this process, two loosely applied clamps placed perpendicular to one another around the plate will control alignment. |
range of motion under anesthesia suggests residual mal-alignment of the
fracture. In all cases, full length radiographs should be obtained in
the operating room to ensure accurate fracture reduction. The
tourniquet, if utilized, should be deflated prior to closure and
hemostasis obtained. The
deep
structures, such as the pronator teres, supinator, and pronator
quadratus, are placed back in their anatomic locations but do not
require repair. The fasciae on both the volar and dorsal exposures are
not closed to decrease the likelihood of a compartment syndrome
following closure. The skin is then closed with an interrupted no. 2-0
absorbable suture in the subcuticular layer and either a running
subcuticular stitch or interrupted nonabsorbable suture.
 |
|
Figure 10.20. A,B.
A both-bone forearm fracture treated with compression plating of the radius and bridge plate fixation of the ulna is shown. A long plate with minimal screw insertion was utilized to minimize bone devitalization. |
radioulnar joint, the surgical incision sites are dressed, and with the
wrist in neutral or slight dorsiflexion, a light, volar, wrist splint
is applied. This postoperative immobilization is provided to rest the
soft tissues and increase the comfort of the patient in the immediate
postoperative period. The splint is discontinued on the first
postoperative visit, and active-assisted range of motion of the upper
extremity is initiated at that time as tolerated. The patient is
encouraged to begin using the extremity for activities of daily living,
with restrictions against lifting objects greater than 10 to 15 pounds.
The lifting restriction is eased at 6 to 10 weeks depending on clinical
and radiographic signs of fracture union, and typically all
restrictions are removed at approximately 3 to 4 months. Return to work
is encouraged with restrictions in the first 7 to 10 days following
surgery, and return to sport is allowed 4 to 6 months following injury.
Radiographs are obtained on the second postoperative visit, typically 6
weeks following injury, then on a 4 to 6 week basis thereafter until
union.
retained indefinitely unless complications arise related to internal
fixation. Hardware removal before 1 year should be avoided. When it is
performed, the patient should be carefully counseled regarding the
inherent risk of nerve injury and refracture (15,16).
EH, Richards RR. The effect of malunion on functional outcome after
plate fixation of both bones of the forearm in adults. J Bone Joint Surg Am 1992;74:1068–1078.
F, Chow SP. A prospective, randomized trial comparing the limited
contact dynamic compression plate with the point contact fixator for
forearm fractures. J Bone Joint Surg Am 2003;85(12):2343–2348.
RR, Schmeling GJ, Schwab JP. The necessity of acute bone grafting in
diaphyseal forearm fractures: a retrospective review. J Orthop Trauma 1997;11(4):288–294.
