CHAPTER 71 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 71 – Multiligament Knee Reconstruction
Christopher D. Harner, MD
Knee dislocations are rare but severe injuries. The diagnosis and management of multiligament knee injuries remain challenging and complex. Knee dislocations can occur from trauma of relatively high or low energy and can be overlooked in the setting of polytrauma with a spontaneous reduction of the knee before the time of presentation. These injuries usually result in damage to at least three of the four major ligaments of the knee, commonly involving both the anterior (ACL) and posterior cruciate ligaments (PCL) and either the medial collateral ligament (MCL) or the lateral collateral ligament (LCL) and the posterolateral corner (PLC).[6]
Knee dislocations are also associated with neurologic and vascular insults. The incidence of popliteal artery injury after knee dislocation is estimated to be between 32% and 45%. [7] [17] Neurologic damage may occur in 16% to 40% of all knee dislocations. [10] [17] Classification of these injuries is based on the direction of tibial translation in relation to the femur: anterior, posterior, medial, lateral, or rotatory.[6]
Historically, multiligament knee injuries have been treated with cast immobilization. Advances in imaging, clinical awareness, and surgical techniques have led to improved diagnosis and management of these injuries. Results of existing studies are difficult to compare, given the different populations of patients (including the severity of injuries), the different techniques used for treatment of cruciate and collateral ligament injuries, and the various outcome measurements and rating scales. Some controversy still exists concerning the timing of surgery, the decision of ligament repair versus reconstruction, and the surgical technique in the management of multiligament knee injuries.
A complete history can be difficult to obtain from an obtunded or sedated polytrauma patient, but it is important nonetheless. The mechanism of injury can provide insight into the direction of dislocation and focus attention to other potentially injured structures in the knee. High- or low-energy trauma may cause a knee dislocation, and this aspect should be noted. The time of injury and the time at onset of symptoms of neurologic or vascular compromise are vital to obtain and to document. Previous knee injuries and treatments should also be recorded.
After the evaluation and treatment of the trauma patient, a thorough examination of the uninvolved and involved knees is performed. For an unreduced dislocated knee, a neurovascular examination is conducted and documented. If there is no apparent vascular compromise, anteroposterior and lateral radiographs are obtained to note the direction of dislocation and to exclude periarticular or intraarticular fractures. Conscious sedation is administered, and a gentle closed reduction is performed.
Several components of the physical examination are crucial in determining whether emergent arteriography or surgery is required. All aspects of the examination should be compared with the contralateral knee. A deteriorating neurovascular status may represent ongoing leg ischemia or compartment syndrome; therefore, serial examinations are imperative.
| • | Note open wounds, abrasions, and soft tissue injuries. | |
| • | Dimpling of skin (may be present in irreducible knee dislocations) | |
| • | Previous incisions |
| • | Assess dorsalis pedis and posterior tibialis pulses with palpation, Doppler study, and ankle-brachial indices. | |
| • | Assess capillary refill, color, and temperature of affected extremity. |
| • | Test motor and sensory function in lower extremity. |
| • | Anterior tibial translation at 30 and 90 degrees | |
| • | Posterior tibial translation at 90 degrees | |
| • | Varus and valgus stress at 0 and 30 degrees | |
| • | Posteromedial and posterolateral rotatory instability |
| • | Bone injuries: bone contusion, avulsion fractures, periarticular or intraarticular fractures | |
| • | Meniscal injury | |
| • | Articular cartilage injury |
| • | Acute cases: anteroposterior and lateral radiographs | |
| • | Chronic cases: anteroposterior, lateral, and 45-degree flexion, weight-bearing radiographs |
| • | Magnetic resonance imaging to evaluate ligament and capsular injuries, meniscal tears, and occult fractures | |
| • | Arteriography for any concerns with the vascular supply to the extremity |
Indications and Contraindications
Absolute indications for surgery include open knee dislocations, open fracture-dislocations, and irreducible knee dislocations. Compartment syndrome may occur after the initial injury or after revascularization and should be treated emergently. Vascular injuries warrant a consultation with a vascular surgeon and require immediate intervention. For nonemergent cases, surgery is generally recommended for most patients with multiligament knee injuries.
Surgery for multiligament knee injuries is contraindicated for patients with an active infection, sedentary lifestyle, advanced osteoarthritis of the knee, severe medical comorbidities, and intraarticular or periarticular fractures of the involved knee.
Other Preoperative Considerations
Ligamentous Repair Versus Reconstruction
The majority of multiligament knee injuries involve disruption of both cruciate ligaments and either medial- or lateral-sided injuries. Tibial avulsions of the cruciate ligaments are treated with repair; however, most cruciate ligament injuries are intrasubstance tears and are best managed with ligament reconstruction. If any bundles of the ACL or PCL remain intact, these are preserved, and a single-bundle cruciate ligament augmentation is performed.
For MCL, LCL, and PLC tears, primary repair may be attempted within 3 weeks of injury. For femoral- or tibial-sided MCL ruptures, repair can be performed with a screw and spiked soft tissue washer or suture anchors. Acute LCL and PLC intrasubstance tears may be repaired primarily with nonabsorbable suture, whereas avulsions from the fibular head may be treated with suture anchors or sutures tied through transosseous tunnels.
More chronic medial or lateral ruptures are less amenable to repair secondary to muscle contracture and scar formation. In these cases, repair with graft augmentation or ligament reconstruction is performed.
The timing of multiligament knee surgery is debated. Factors affecting this decision include the vascular status of the lower extremity, the condition of the skin and soft tissues, the presence of other intraarticular injuries, the associated traumatic or systemic injuries, the capsuloligamentous structures injured, and the extent of these injuries.[5]
In general, multiligament knee surgeries are performed 2 to 3 weeks after injury. This interval is chosen to allow time for soft tissue and capsular injuries to heal and to decrease the likelihood of fluid extravasation with arthroscopy, yet to operate before significant scar formation and soft tissue contractures occur.[9] Some combined cruciate and medial ligamentous injuries can be managed with initial bracing of the MCL and later reconstruction of the ACL and PCL. With so many variables to consider, the timing of surgery must be tailored to the individual patient.
Multiligament reconstruction procedures may be performed under general epidural or regular anesthesia with intravenous sedation, depending on the preferences of the surgeon, the anesthesiologist, and the patient. Preoperative femoral and sciatic blocks are routinely performed to assist in postoperative pain relief. The patient is positioned supine on the operating room table. A Foley catheter is passed, and all extremities are well padded. A gel pad is placed under the ipsilateral hip. A padded bump is taped to the foot of the table to hold the knee flexed at 90 degrees without manual assistance. A side post with bump is placed lateral at the proximal thigh to support the leg in flexion. A tourniquet is placed on the proximal thigh but not routinely used.
Surface Anatomy and Skin Incisions
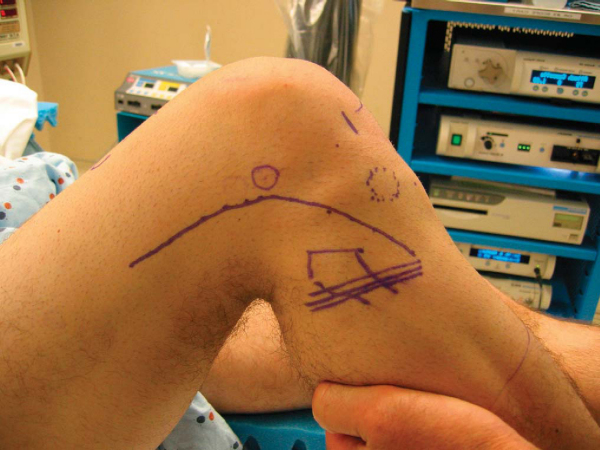
The following are surgical landmarks for multiligament knee reconstruction (
Fig. 71-1
| • | Patella and patellar tendon | |
| • | Medial and lateral femoral epicondyles | |
| • | Medial and lateral joint lines | |
| • | Fibular head | |
| • | Path of common peroneal nerve | |
| • | Tibial tubercle and Gerdy tubercle |
The knee is flexed to 90 degrees, and the vertical arthroscopy portals are delineated. If patellar height is considered normal, the anterolateral portal is placed just lateral to the lateral border of the patellar tendon at the level of the inferior pole of the patella. The anteromedial portal for outflow is positioned approximately 1 cm medial to the medial border of the superior aspect of the patellar tendon. An outflow portal may be used superolaterally. For PCL reconstruction, an accessory posteromedial portal is established just proximal to the joint line and posterior to the MCL under spinal needle localization. The incision for the cruciate ligament tibial tunnels is positioned approximately 2 cm distal and medial to the superior portion of the tibial tubercle. The femoral tunnel incision for the PCL graft is marked over the proximal anteromedial knee. If an MCL repair or reconstruction is to be performed, a curvilinear incision is planned from the tibial tunnel incision extending proximally above the medial epicondyle. If a posterolateral dissection is required, a curvilinear incision is made from the lateral aspect of the lateral femoral condyle to just anterior to the fibular head. The proposed incisions are then cleaned with sterile povidone iodine (Betadine) paint and then injected with a 0.25% bupivacaine with 1:100,000 diluted epinephrine.
Examination Under Anesthesia and Diagnostic Arthroscopy
An examination under anesthesia is then performed. The nonoperative knee is examined, followed by the operative knee. The alignment and range of motion are assessed with specific attention to terminal extension and flexion. A thorough ligamentous examination is conducted to determine the patterns of laxity. Once the leg is prepared and draped, the dorsalis pedis artery is palpated and marked, and a hole is cut in the stockinette for access to the pulse throughout the case (
Fig. 71-2
).
|
|
|
|
Figure 71-2 |
The arthroscopic equipment is prepared, and the fluoroscopy machine is later draped. A complete diagnostic arthroscopy is performed to assess for intraarticular pathologic changes, including inspection of the menisci and articular surfaces. The intercondylar notch is examined for any remaining intact bundles of the cruciate ligaments, which are preserved for augmentation.
Specific Steps (
Box 71-1
)
1 Graft Selection and Preparation
Findings from the history, physical examination, imaging studies, examination under anesthesia, and arthroscopic examination are combined to determine which structures require repair or reconstruction. Options for graft selection include allograft and autograft (
Fig. 71-3
). Whereas autograft offers potentially more rapid incorporation, decreased infection risk, and decreased cost, use of allograft tissue has no donor site morbidity, offers a variety of graft sizes, and decreases operative time. At our institution, allograft tissue is preferred in multiligament knee reconstruction surgery. In general, hamstring autograft is not harvested in the setting of a medial ligament injury.
|
|
|
|
Figure 71-3 |
For ACL reconstruction, bone–patellar tendon–bone allograft provides sufficient strength with good osseous fixation. The bone plugs are usually fashioned to 11×25 mm; the graft width is 11 mm. Smaller-diameter grafts may be used in augmentation cases. Drill holes are placed in both bone plugs for passage of No. 5 nonabsorbable sutures. Alternatively, soft tissue allograft may also be used. Soft tissue grafts are doubled on themselves over a closed endoloop with the EndoButton (Smith & Nephew, Inc., Andover, Mass) removed. This is done to maximize the amount of graft within the tunnel, which has been shown in a dog model to improve pullout strength.[8] All grafts are placed on the tensiometer and kept moist in a damp sponge.
For PCL reconstruction, Achilles tendon or tibialis anterior allograft is preferred. Achilles tendon grafts offer a bone plug for rigid femoral fixation, which is fashioned to 11×25 mm. A No. 5 nonabsorbable suture is passed through bone plug drill holes, and another suture is used to whipstitch the tendinous portion of the graft. For augmentation of the anterolateral or posteromedial bundles, tibialis anterior allograft or hamstring autograft may also be used.
Reconstruction of the LCL is performed with Achilles tendon allograft or remaining graft from the bone–patellar tendon–bone allograft initially used for the ACL reconstruction. The bone plug is sized to 7 to 8 mm in diameter. The PLC is reconstructed with tibialis anterior allograft or hamstring autograft.
2 Cruciate Ligament Tunnel Preparation
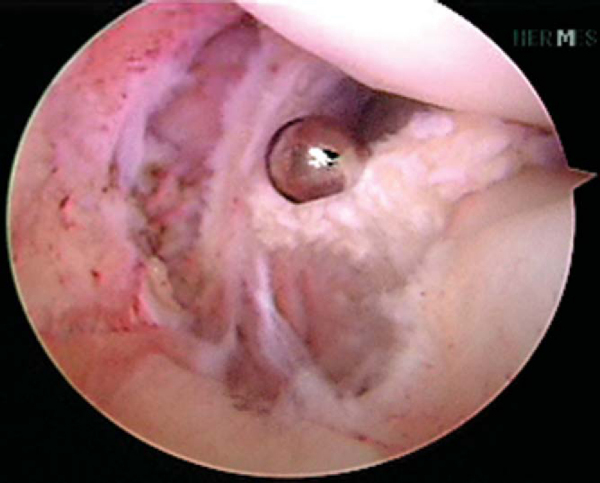
The tibial tunnel of the PCL reconstruction is addressed first. A 70-degree arthroscope is placed through the anterolateral portal and used to visualize the PCL tibial footprint. A spinal needle is used for establishment of the posteromedial portal. A transseptal portal is established as described by Ahn et al. [1] [2] The PCL footprint is exposed by débridement of the surrounding synovial tissue with a PCL curet and arthroscopic shaver (
Fig. 71-4
). Care is taken to avoid injury to the neurovascular bundle posteriorly. The 30- and 70-degree arthroscopes are frequently exchanged in the posteromedial and anterolateral portals, respectively, for adequate visualization. A PCL drill guide is set to 50 to 55 degrees, and its placement posteriorly is confirmed with fluoroscopy and arthroscopy. A vertical incision is made over the anteromedial aspect of the proximal tibia (or the anterolateral aspect if an ACL reconstruction is not required and a lateral incision will be performed).
|
|
|
|
Figure 71-4 |
The guide wire is passed under fluoroscopic guidance to the posterior tibial cortex and then through the cortex under arthroscopic visualization. The wire exits the tibia along the sloped face of the posterior tibial fossa, in the distal and lateral aspects of the PCL footprint. A parallel drill guide may be used to optimize placement of the guide wire.
Both ACL and PCL guide wires are placed before drilling of the tibial tunnels. To prepare the ACL tibial tunnel, the ACL stump is débrided and any intact bundles are preserved. An ACL guide is set to 45 degrees, and a guide wire is drilled into the center of the ACL footprint. A lateral fluoroscopic image is obtained to confirm correct placement of both wires.
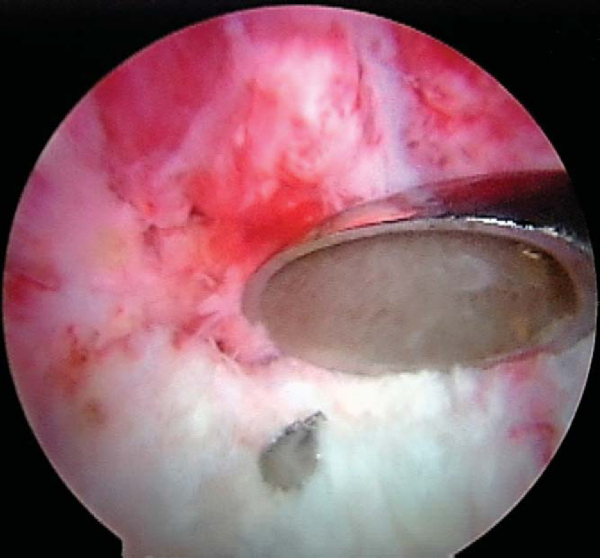
A cannulated compaction drill is passed over the wire to drill the PCL tibial tunnel; a curet is placed over the guide wire posteriorly for protection from neurovascular injury (
Fig. 71-5
). Final drilling of the posterior cortex is done by hand. Serial tunnel dilators are passed to match the size of the graft. The tibial tunnel for the ACL is drilled in similar fashion. The tibial tunnels between the ACL and PCL are at least 1 to 2 cm apart.
|
|
|
|
Figure 71-5 |
Femoral tunnel preparation for PCL reconstruction involves identification and débridement of the PCL femoral insertion. For single-bundle PCL reconstruction, a guide wire is inserted through the anterolateral portal in the center of the PCL insertion site. A cannulated compaction drill is inserted by hand to avoid injury to the patellar chondral surface and to confirm tunnel location in relation to the articular cartilage of the medial femoral condyle. The drill is passed to a depth of 25 to 30 mm, and sequential dilators are passed up to the graft diameter. A smaller drill is used to drill through the cortex for graft passage. Separate tunnels are drilled and smaller grafts are used if double-bundle PCL reconstruction is to be performed.
For placement of the ACL femoral tunnel, a notchplasty is performed, and the over-the-top position is identified with a curet. An anteromedial portal technique with the knee flexed to 120 degrees is preferred for placement of the femoral ACL tunnel (
Fig. 71-6
). An angled awl is placed in the 10-o’clock or 2-o’clock position for the right or left knee, respectively, to make a starting hole 5 to 6 mm anterior to the posterior wall. A guide wire is then advanced into the medial wall of the lateral femoral condyle through the starting hole. The compaction drill is again used to make a hole 25 to 30 mm in depth, the cortex is broached with a smaller drill, and serial dilators are passed (
Fig. 71-7
).
|
|
|
|
Figure 71-6 |
|
|
|
|
Figure 71-7 |
3 Cruciate Graft Passage and Proximal Fixation
The compartments of the leg should be checked regularly during the arthroscopic portion of the procedure. Graft passage may be performed arthroscopically “dry” if there is concern about fluid extravasation. An 18-gauge bent wire loop is passed through the PCL tibial tunnel and retrieved through the anterolateral portal with a pituitary rongeur. The leading No. 5 suture is then pulled anterograde through the tibial tunnel as the wire loop is removed. A Beath pin is inserted through the anterolateral portal into the PCL femoral tunnel. The leading sutures for the femoral side of the PCL graft are passed through the eye of the Beath pin and pulled proximally with the pin into the tunnel. For the ACL, the graft is passed in retrograde fashion through the tibial tunnel. The leading femoral-sided suture limbs are passed through the tibial tunnel with a pituitary rongeur and grasped through the anteromedial portal with another pituitary rongeur. A Beath pin is passed through the ACL femoral tunnel with the lead sutures, and the graft is pulled into the femoral tunnel.
Femoral fixation for both grafts is performed with a post. A 4.5-mm AO cortical screw and washer are used for the ACL, and a 6.5-mm cancellous screw and washer are used for PCL fixation. The lead sutures may be tied over the post, or the screw may be passed through a closed endoloop attached to the graft. Careful planning should ensure that these screws are placed at different levels within the distal femur. Alternatively, interference screws may be used.
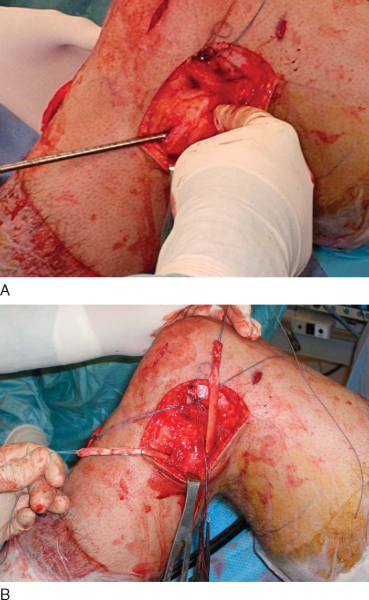
A hockey stick lateral incision is made to address injuries to the PLC. The iliotibial band is retracted anteriorly, and the biceps femoris muscle and tendon are retracted posteriorly. The common peroneal nerve is identified and protected throughout the procedure. Acute bone avulsion injuries of the LCL, popliteus, iliotibial band, or biceps tendon are generally repaired to bone with suture anchors. For irreparable, intrasubstance, or chronic PLC ruptures, reconstruction is recommended.
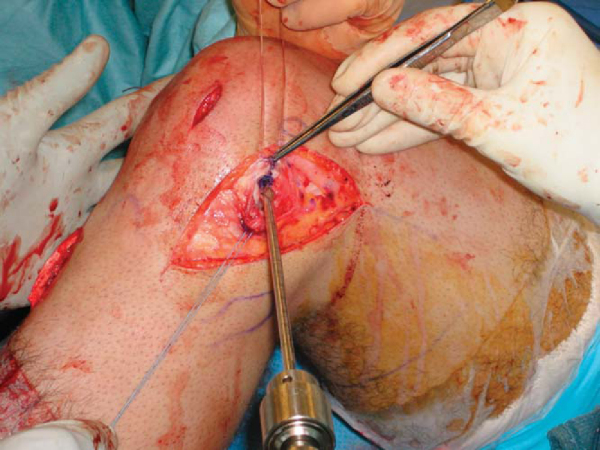
LCL reconstructions are performed with allograft passed through a bone tunnel in the fibular head (
Fig. 71-8
) and into a blind femoral tunnel measuring 7 to 8 mm in diameter. No. 2 nonabsorbable suture may be placed in whipstitch fashion in the native popliteus and LCL for advancement with the graft into the femoral tunnel (
Fig. 71-9
). A small drill is used to penetrate the medial femoral cortex, and a Beath pin may be used to pass the leading sutures to the medial side. The graft and native tissue are pulled into the femoral tunnel, and the sutures are tied over a post on the medial femur (or the post from the femoral PCL fixation). Native tissue is sutured to graft tissue to augment the reconstruction.
|
|
|
|
Figure 71-8 |
|
|
|
|
Figure 71-9 |
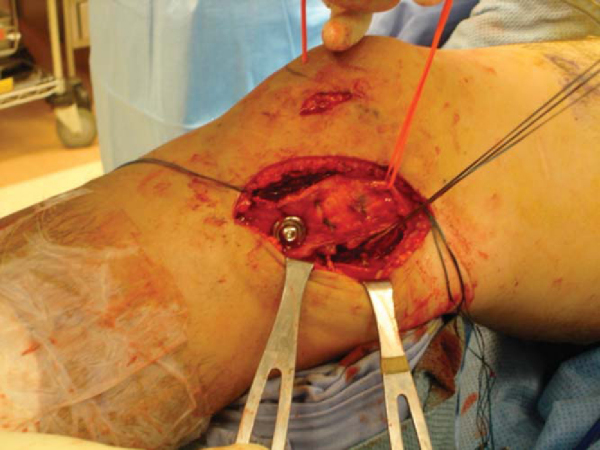
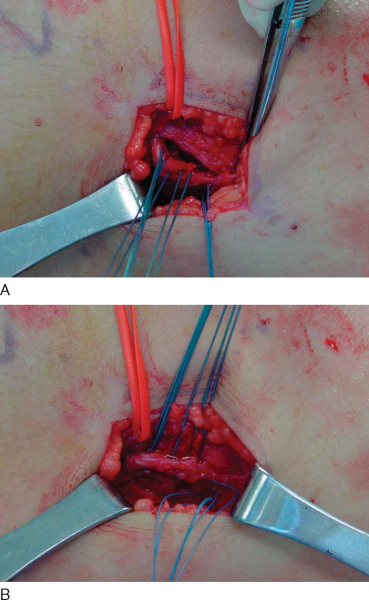
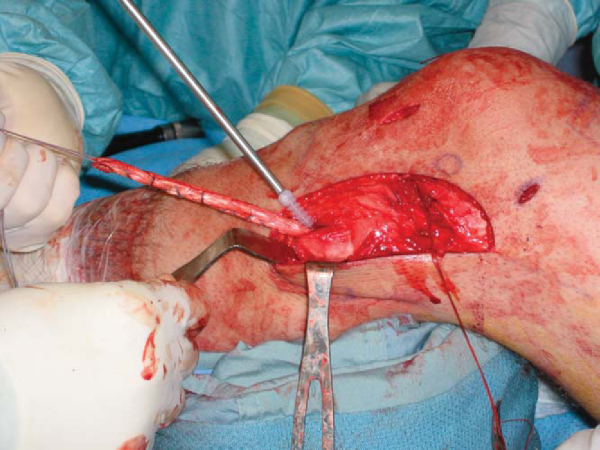
If a medial-sided injury is to be addressed, a curvilinear incision is extended from the anteromedial proximal tibial incision. Peripheral medial meniscal tears may be repaired through this incision. The MCL is usually repaired in grade III injuries. For femoral or tibial avulsion injuries, the ligament is repaired to a prepared bone bed with suture anchors or a screw and spiked soft tissue washer or both for deep and superficial layers (
Fig. 71-10
). Intrasubstance tears may be primarily repaired in acute cases or reconstructed with augmentation of native tissue in chronic cases. The posterior oblique ligament (POL) may be injured in cases of posteromedial rotatory instability. The POL is separated from the posterior MCL and the underlying meniscus. The peripheral meniscus is rasped, and a suture repair is performed through the anteriorly advanced POL. The anterior flap of the POL is advanced and imbricated deep to the posterior MCL with cottony Dacron sutures (
Fig. 71-11
).
|
|
|
|
Figure 71-10 |
|
|
|
|
Figure 71-11 |
6 Graft Tensioning and Distal Fixation
The order of distal fixation is as follows:
| • | PCL | |
| • | ACL | |
| • | Lateral structures | |
| • | Medial structures |
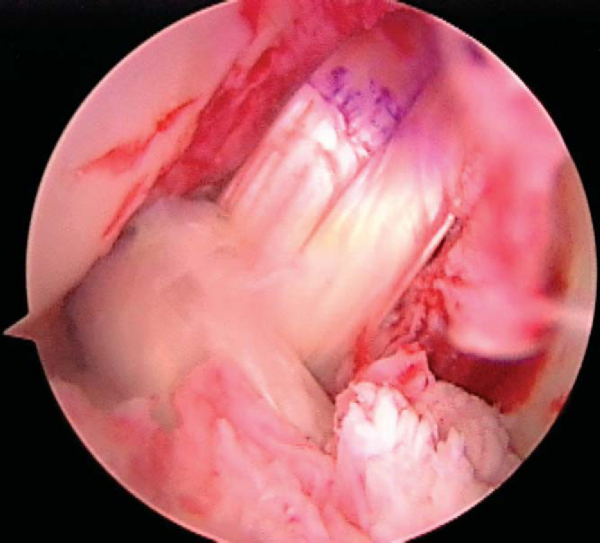
Single-bundle PCL reconstructions are tensioned at 90 degrees of flexion to approximate the anterolateral bundle. An anterior tibial force is applied to reduce the tibia on the femur. The lead sutures of the graft may be tied over a 4.5-mm AO screw and washer, or an interference screw may be used. Tension and tibial fixation of the ACL graft are performed in full extension. Fixation may be achieved with a screw and washer post or an interference screw. The position of the graft and the fixation are checked arthroscopically (
Fig. 71-12
) and clinically.
The PLC graft is tensioned at 30 degrees of knee flexion with internal rotation of the tibia. Fibular fixation of reconstructed LCL or popliteofibular ligament may be performed with an interference screw (
Fig. 71-13
). The reconstructed MCL is also tensioned at 15 to 30 degrees and may be fixed with a screw and washer or an interference screw. The POL advancement is tensioned at full extension. After final fixation, the knee’s range of motion is assessed, and final fluoroscopic images are obtained.
|
|
|
|
Figure 71-13 |
All incisions are irrigated with antibiotic solution. Deep layers are closed with 0 nonabsorbable suture, subcutaneous tissues are approximated with 2-0 nonabsorbable suture, and skin is closed with staples. The arthroscopic portals are closed with 3-0 nylon suture. The dorsalis pedis pulse is palpated or assessed by sterile Doppler study if necessary, and the leg is palpated to assess the compartments. A standard surgical dressing is placed with a bias stockinette wrap. A hinged knee brace is applied and locked in extension.
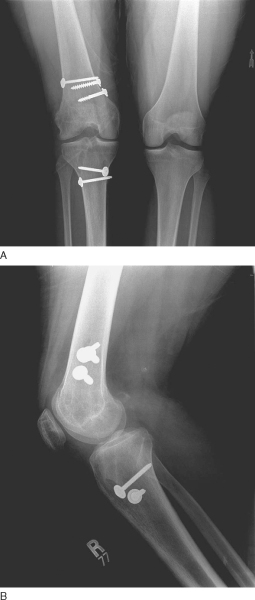
The patient is discharged from the hospital on the following day and returns in 7 to 10 days for staple or suture removal and radiographs (
Fig. 71-14
). Dressing changes are performed with posterior tibial support to avoid stress to the reconstructed PCL.
|
|
|
|
Figure 71-14 |
The rehabilitation program for multiple ligament knee reconstruction is as follows. [3] [9]
| • | Immediate partial weight bearing is allowed with the brace locked in extension. | |
| • | Quad sets, straight-leg raises, and calf pumps are done while the patient is in the brace. | |
| • | Closed-chain exercises (mini-squats) are performed with the brace unlocked, with a goal of 90 degrees of flexion by 4 weeks. The brace is locked in extension with ambulation. | |
| • | Unlock the hinged knee brace at 4 weeks and advance to full weight bearing. | |
| • | Avoid active knee flexion with hamstrings for 6 weeks to prevent posterior tibial translation; avoid open-chain hamstring exercises for 12 weeks. | |
| • | Quadriceps strengthening, including limited arc open-chain knee extension exercises, begins after 4 weeks. | |
| • | Active-assisted range of motion and stretching begin at 6 weeks. | |
| • | Discontinue the brace at 6 weeks. | |
| • | The goals are full extension and 100 degrees of flexion by 12 weeks. If progress is unsatisfactory, manipulation under anesthesia may be performed. | |
| • | Low-impact aerobic activities are permitted at 8 to 12 weeks; running is permitted at 6 months if quadriceps strength is 80% of the contralateral side. | |
| • | Return is allowed to heavy labor in 6 to 9 months and to sports in 9 to 12 months. |
| • | Neurovascular injury, including popliteal vessels, peroneal and saphenous nerves (missed and iatrogenic injuries) | |
| • | Compartment syndrome (missed and iatrogenic injuries) | |
| • | Tibial plateau fracture (missed and iatrogenic injuries) | |
| • | Infection | |
| • | Arthrofibrosis | |
| • | Residual laxity due to failure to recognize or to treat all injured components, failure of graft incorporation, or recurrent rupture of graft |
| PEARLS AND PITFALLS | |||||||||
|
Management of the dislocated knee has changed with the advancement of arthroscopic techniques. Some authors have shown improved clinical results in comparing operative with nonoperative treatment of multiligament injuries. [16] [21] However, comparison of studies involving multiligament reconstruction is difficult for a number of reasons. There are variations in the populations of patients in these studies; some include or exclude patients with neurovascular injuries, many include both acute and chronic ligament injuries, and the different ligament injury combinations in each study are widely varied. In addition, different surgical techniques have been used in different studies. These variables include ligament repair or reconstruction, open or arthroscopic techniques, choice of graft tissue, single- or double-bundle cruciate reconstruction,[19] and method of PCL reconstruction. Finally, use of different clinical outcomes also limits comparisons between studies. Postoperative knee stability has been evaluated with physical examination, side-to-side differences with KT-1000 arthrometer measurements, and stress radiography. Functional results are reported in different rating scales. The Meyers scoring system was developed for knee dislocations and is based on subjective ratings. [12] [13] However, it does not account for functional or objective scores and is less strict than other knee-scoring systems.[20] A list of studies involving surgical treatment, including bicruciate ligament injuries and their results, is shown in
Table 71-1
. [4] [9] [11] [14] [15] [18] [20]
| Author | Number of Knees | Mean Followup | Clinical Results |
|---|---|---|---|
| Harner et al[9] (2004) | 31 | 44 months | Meyers: 23/31 (74%) good–excellent |
| IKDC: 0 normal, 11 (35%) nearly normal, 12 (39%) abnormal, 8 (26%) severely abnormal | |||
| Fanelli and Edson[4] (2002) | 35 | 2-10 years | Significant improvement over Tegner, HSS, and Lysholm preoperative scores |
| Ohkoshi et al[15] (2002) | 9 | 40 months | IKDC: 0 normal, 7/9 (78%) nearly normal, 2/9 (22%) abnormal |
| Mariani et al[11] (2001) | 14 | 36 months | IKDC: 3 (20%) normal, 7 (47%) nearly normal, 3 (20%) abnormal, 1 (7%) grossly abnormal |
| HSS: 12/14 (86%) good–excellent | |||
| Wascher et al[20] (1999) | 13 | 38 months | Meyers: 11/13 (85%) good–excellent |
| IKDC: 6 (50%) nearly normal, 5 (42%) abnormal, 1 (8%) grossly abnormal | |||
| Noyes and Barber-Westin[14] (1997) | 11 | 58 months | 3/7 (43%) good–excellent (acute only rated) |
| Shapiro and Freedman[18] (1995) | 7 | 51 months | Meyers: 6/7 (86%) good–excellent |
|
Meyers, Meyers knee dislocation rating system; IKDC, International Knee Documentation Committee from; HSS, Hospital for Special Surgery Knee ligament rating scale. |
1.
Ahn JH, Chung YS, Oh I: Arthroscopic posterior cruciate ligament reconstruction using the posterior transseptal portal.
Arthroscopy 2003; 19:101-107.
2.
Ahn JH, Ha CW: Posterior transseptal portal for arthroscopic surgery of the knee joint.
Arthroscopy 2000; 16:774-779.
3.
Chhabra A, Cha PS, Rihn JA, et al: Surgical management of knee dislocations. Surgical technique.
J Bone Joint Surg Am 2005; 87(suppl 1, pt 1):1-21.
4.
Fanelli GC, Edson CJ: Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year followup.
Arthroscopy 2002; 18:703-714.
5.
Fanelli GC, Edson CJ, Orcutt DR, et al: Treatment of combined anterior cruciate–posterior cruciate ligament–medial-lateral side knee injuries.
J Knee Surg 2005; 18:240-248.
6.
Fanelli GC, Orcutt DR, Edson CJ: The multiple-ligament injured knee: evaluation, treatment, and results.
Arthroscopy 2005; 21:471-486.
7.
Good L, Johnson RJ: The dislocated knee.
J Am Acad Orthop Surg 1995; 3:284-292.
8.
Greis PE, Burks RT, Bachus K, Luker MG: The influence of tendon length and fit on the strength of a tendon-bone tunnel complex: a biomechanical and histologic study in the dog.
Am J Sports Med 2001; 29:493-497.
9.
Harner CD, Waltrip RL, Bennett CH, et al: Surgical management of knee dislocations.
J Bone Joint Surg Am 2004; 86:262-273.
10.
Helgeson MD, Lehman Jr RA, Murphy KP: Initial evaluation of the acute and chronic multiple ligament injured knee.
J Knee Surg 2005; 18:213-219.
11.
Mariani PP, Margheritini F, Camillieri G: One-stage arthroscopically assisted anterior and posterior cruciate ligament reconstruction.
Arthroscopy 2001; 17:700-707.
12.
Meyers MH, Harvey Jr JP: Traumatic dislocation of the knee joint. A study of eighteen cases.
J Bone Joint Surg Am 1971; 53:16-29.
13.
Meyers MH, Moore TM, Harvey Jr JP: Traumatic dislocation of the knee joint.
J Bone Joint Surg Am 1975; 57:430-433.
14.
Noyes FR, Barber-Westin SD: Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Use of early protected postoperative motion to decrease arthrofibrosis.
Am J Sport Med 1997; 25:769-778.
15.
Ohkoshi Y, Nagasaki S, Shibata N, et al: Two-stage reconstruction with autografts for knee dislocations.
Clin Orthop Rel Res 2002; 398:169-175.
16.
Richter M, Bosch U, Wippermann B, et al: Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations.
Am J Sports Med 2002; 30:718-727.
17.
Rihn JA, Cha PS, Groff YJ, Harner CD: The acutely dislocated knee: evaluation and management.
J Am Acad Orthop Surg 2004; 12:334-346.
18.
Shapiro MS, Freedman EL: Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation.
Am J Sports Med 1995; 23:580-587.
19.
Stannard JP, Riley RS, Sheils TM, et al: Anatomic reconstruction of the posterior cruciate ligament after multiligament knee injuries. A combination of the tibial-inlay and two-femoral-tunnel techniques.
Am J Sports Med 2003; 31:196-202.
20.
Wascher DC, Becker JR, Dexter JG, Blevins FT: Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Results using fresh-frozen nonirradiated allografts.
Am J Sports Med 1999; 27:189-196.
21.
Wong CH, Tan JL, Chang HC, et al: Knee dislocations—a retrospective study comparing operative versus closed immobilization treatment outcomes.
Knee Surg Sports Traumatol Arthrosc 2004; 12:540-544.