Forearm Fractures: Intramedullary Nailing
relatively common injuries that usually occur after intermediate or
high-energy trauma. With widespread dissemination of the methods of
fixation advocated by the AO/ASIF, plate fixation of these injuries has
become the gold standard. Numerous authors have shown high rates of
union and excellent functional outcomes after plate osteosynthesis of
these fractures. The chief drawbacks with this fixation method are the
long incisions and wide exposure necessary to reduce and fix the
fractures. Radial nerve palsies are common after open reduction and
internal fixation (ORIF), and refracture rates of the forearm vary from
1% to 20% and are most common in the proximal one third. Furthermore,
the resultant scar can be a significant cosmetic deformity,
particularly in female patients.
to replace conventional plate fixation. Rather, it is indicated in a
small subgroup of patients in whom nailing may be more advantageous
than plate osteosynthesis. The indications for intramedullary nailing
of the radius and ulna include segmental fractures, gunshot fractures
with severe comminution, refracture of the forearm after plate removal,
fracture occurring above or below an existing plate, unstable fractures
in children or adolescents, and fractures in athletes who participate
in contact sports.
intramedullary canal measures less than 3 mm at the narrowest point.
Fractures less than 3 cm from the proximal or distal end of the bone
should not be nailed because of inadequate fixation of the short
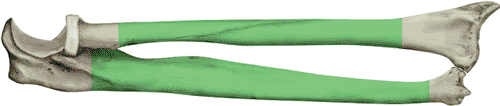
segment of bone (Fig. 11.1). Nailing should be
avoided in patients with preexisting deformity of the forearm that
would preclude nailing without an osteotomy. Finally, nailing is not
the fixation method of first choice to stabilize corrective osteotomies
or treat nonunions.
 |
|
Figure 11.1.
Portion of radius and ulna that can be treated with an interlocking forearm nail. At least 3 cm of intact bone on either end must be present. |
after multiple trauma. In the severely injured patient, basic and
advanced trauma life support (ATLS) and a full trauma evaluation and
resuscitation are mandatory. Once life-threatening and limb-threatening
injuries have been addressed, the injured arm is carefully evaluated.
The entire upper extremity is inspected for open wounds, ecchymosis,
abrasion, deformity, and other injury. The limb is palpated from
shoulder to fingers by the surgeon looking for areas of tenderness or
fracture crepitus. Ipsilateral injuries to the shoulder, upper arm,
elbow, wrist, and hand commonly occur after high-energy trauma. The arm
is critically examined to ensure that a compartment syndrome does not
exist. If the surgeon has any doubt, the compartment pressure should be
measured. After the lower leg, the forearm is the second most common
site for a compartment syndrome. The axillary, brachial, radial, and
ulnar pulses should be palpated and compared with those of the opposite
side. The sensory and motor components of the radial, medial, and ulnar
nerves must be documented. In patients with proximal injuries, the
function of the brachial plexus requires evaluation. If the fracture is
open, the wounds should be sterilely dressed, the limb splinted, and
intravenous antibiotics administered. The patient should be brought to
the operating room as soon as possible for irrigation and debridement.
entire injured and uninjured forearm are obtained to determine proper
nail length, diameter, and radial bow. Three methods of determining
correct nail length are used: First, the patient’s uninjured arm is
measured with a tape measure from the tip of the olecranon to the ulnar
styloid, and 1 cm is subtracted from the measurement; second, a nail of
known length is intraoperatively placed against the affected bone while
traction is used to keep the bone to the appropriate length, and the
fit of the nail is checked fluoroscopically; or third, the fit is
checked preoperatively through the use of radiographic templates with
known magnification parameters. Because the radial head is often
difficult to palpate, the radial length can be determined by
subtracting 2 cm from the ulnar length.
computed tomography (CT) scanning, or other imaging modalities, are not
helpful in preoperative planning.
because the relaxation obtained improves the chances of achieving a
closed reduction. Closed nailing is more successful if surgery is done
within 72 hours of injury. The patient is placed supine on an operating
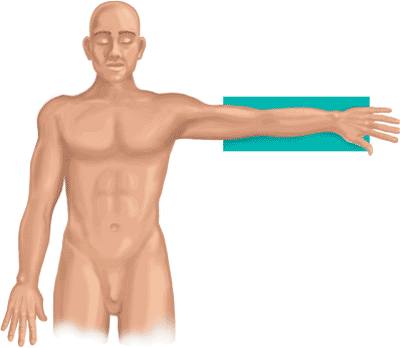
table, and a radiolucent arm table is used to support the extremity (Fig. 11.2).
A mobile, C-arm, image intensifier is brought in from the head of the
table. The surgeon sits at the axilla while the assistant is positioned
at the end of the hand table. For ulnar nailing, the shoulder is
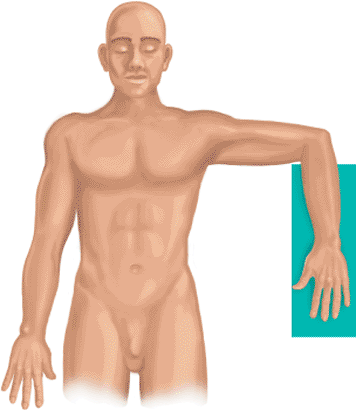
abducted and internally rotated, and the elbow is flexed to 90 degrees.
The elbow is “bumped” with a stack of towels for easier access to the
olecranon (Fig. 11.3).
open method. Closed nailing is preferable because it preserves blood
supply and enhances fracture healing. Closed reduction is achieved by
longitudinal traction or direct pressure at the fracture site. Traction
devices
with finger traps have not been successful. The surgical assistant
should wear sterile lead gloves to minimize radiation exposure to
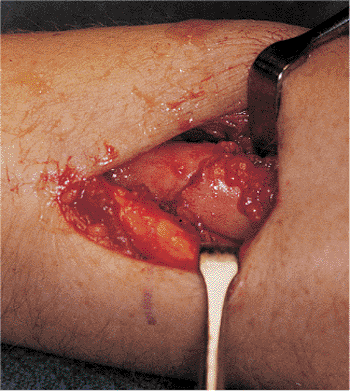
his/her hands. When the fracture fragments are locked in bayonet
apposition, a mini–open technique through a 2- to 4-cm incision may be
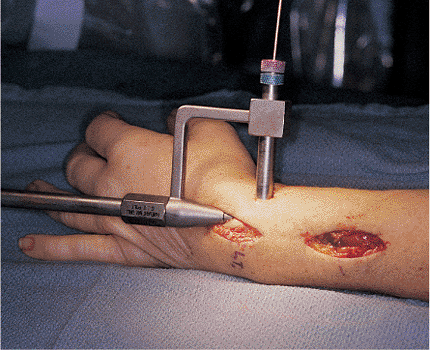
used to reduce the fragments (Fig. 11.4).
 |
|
Figure 11.2.
The patient is positioned supine with a radiolucent arm board. The surgeon sits facing the axilla, while the image intensifier comes in from the head of the table. A stack of towels is placed under the wrist. |
 |
|
Figure 11.3.
With nailing of the ulna, the elbow is bent 90 degrees for access to olecranon, where the surgeon will place the entry portal. A stack of towels is placed under the elbow. |
loss. If both bones are fractured, the radius is approached first.
However, both bones are prepared for nailing before nailing is
initiated in either bone. A 1.5-cm incision is made just lateral to
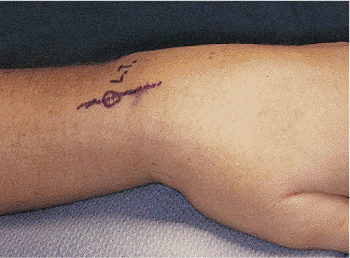
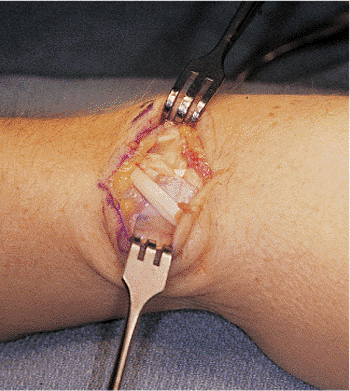
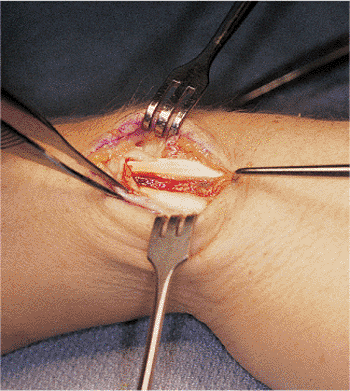
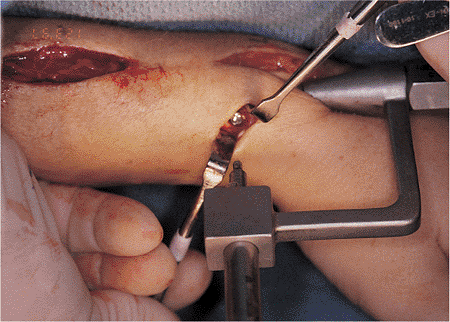
Lister’s tubercle at the distal radius (Fig. 11.5). The extensor pollicis longus (EPL) tendon is identified and
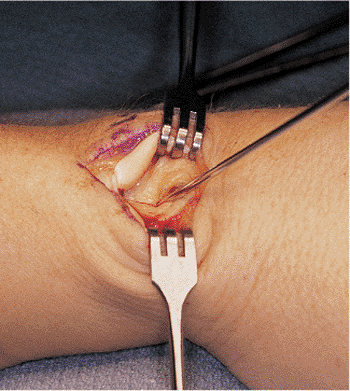
released from its sheath around Lister’s tubercle (Fig. 11.6). The interval between the short and long wrist extensors is identified (Fig. 11.7).
The surgeon must identify the distal edge of the radius to avoid
inadvertent insertion through the scaphoid. The medullary canal is
entered obliquely through a 2.0-mm pilot drill hole at the dorsal
margin of the radius (Fig. 11.8). The wrist is flexed and placed over a stack of towels to prevent inadvertent perforation of the volar cortex (Fig. 11.9). The entry portal is enlarged with a cannulated 6.0-mm reamer (Fig. 11.10).
 |
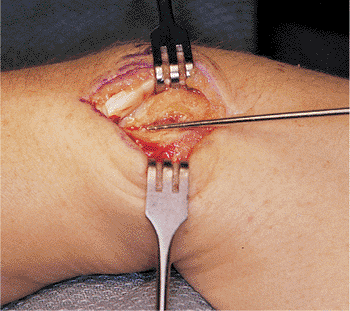
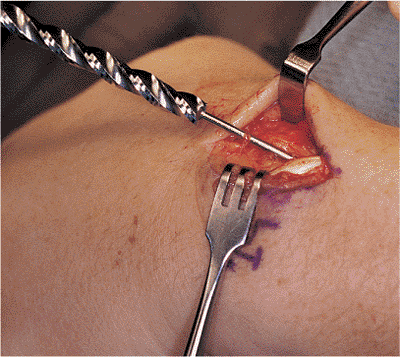
|
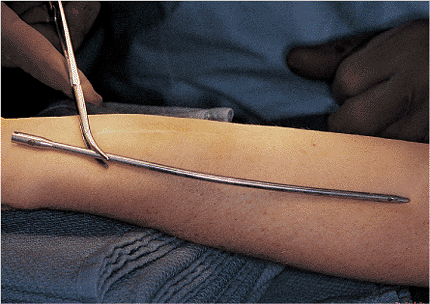
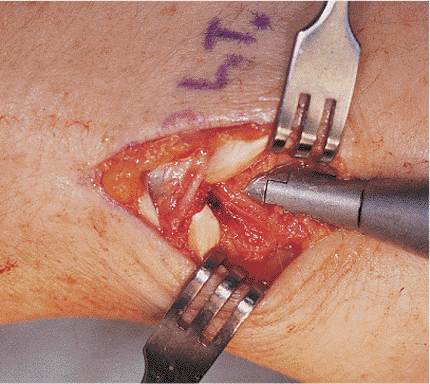
Figure 11.4. A 4-cm mini–open incision is used to reduce a completely displaced fracture of the radius.
|
 |
|
Figure 11.5. A 2-cm incision is centered over Lister’s tubercle for creation of an entry portal into the radius.
|
 |
|
Figure 11.6. The extensor retinaculum is divided to expose the EPL tendon. The EPL tendon is then released from its surrounding sheath.
|
 |
|
Figure 11.7. The interval between the extensor carpi radialis longus (ECRL) is developed. The EPL is retracted radially with the ECRL.
|
third, the point of insertion for the ulna is toward the radial side of
the olecranon, and is made approximately 5 mm from the lateral cortex.
A l-cm incision is made with the 2.0-mm drill to access the medullary
canal, and then a 6-mm cannulated reamer is used.
 |
|
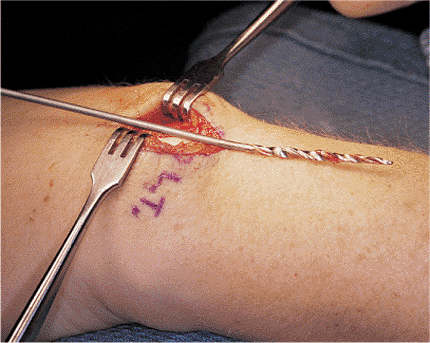
Figure 11.8.
The 2.0-mm guide pin is introduced at a point 5 mm from the distal edge of the radius. The pin is started vertically so entry into the bone can be gained. |
 |
|
Figure 11.9. The wrist is flexed, and the pin is brought into a more horizontal direction to avoid penetration of the volar cortex.
|
 |
|
Figure 11.10. To enlarge the entry portal, the surgeon introduces a 6-mm cannulated reamer over the 2.0-mm trocar wire.
|
nailing because they help the surgeon avoid nail incarceration. Both
hand and power reamers are available (Fig. 11.11).
Small end-cutting and side-cutting reamers are manufactured by Smith
& Nephew Richards (Memphis, TN). The narrowest portion of the
intramedullary canal may range from 3 to 7 mm. Preoperative canal
sizing is used to determine whether reaming is necessary before nail
insertion. The medullary canal should be overreamed by 0.5 to 1.0 mm to
prevent nail incarceration, fracture comminution, or distraction at the
fracture site.
fractures should be reduced and prepared before either bone can be
nailed; otherwise, the stability of the nailed bone may make reduction
of the other fracture difficult. When closed nailing is performed, the
rotational control obtained by the interference fit of the nail is less
important than it is with open nailing. If open nailing is performed,
the canal may be reamed from the fracture site (Fig. 11.12). After the last reamer is used, it is replaced with a 2.4-mm, straight, guide rod. The
radius is reduced and temporarily stabilized with a guide rod. The ulna is prepared in a fashion similar to that of the radius.
 |
|
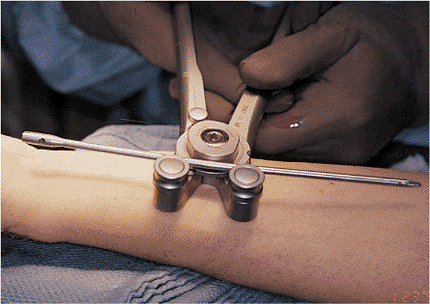
Figure 11.11.
A hand reamer with a 15-degree bend is used to help skate off the volar cortex. Reamers are available in sizes from 3.0 to 5.5 mm in 5-mm increments. |
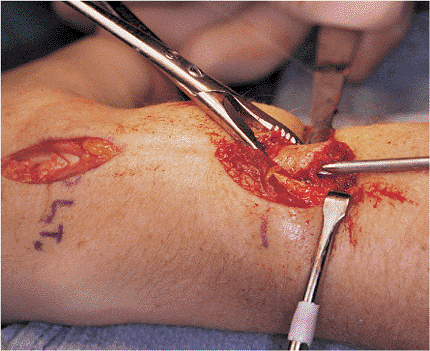 |
|
Figure 11.12. To prepare the canal at the fracture site, the surgeon uses a power reamer during an open nailing.
|
materials and shapes. Some are made of stainless steel, and others are
comprised of titanium. Some are prebent to conform to the normal
dorsoradial bow of the radius and lateral ulna bow. Other nails are
straight and must be contoured with a nail bender before insertion. The
radial nail should be contoured with respect to the normal dorsoradial
bow. The angle to which the nail should be bent can be determined
through radiographs of the uninjured forearm. This process is similar
to that used to bend reconstruction plates before implantation (Fig. 11.13). After proper nail contouring (Fig. 11.14),
orientation of the implant with respect to anatomy is most important.
After assembly of the nail on the driver and drill guide (Fig. 11.15),
the nail is inserted with hand pressure or light hammering. Proper
rotational alignment is confirmed by the use of the image intensifier.
Orientation of the bicipital tuberosity and the radial styloid is
helpful in confirming correct rotation of the radius. In addition, at
the completion of the procedure, an intraoperative check of the arc of
forearm rotation is essential to prevent malreduction. The nail is
seated so that the driving end is countersunk just below the cortex (Fig. 11.16).
 |
|
Figure 11.13. A nail bender is used to contour the radial nail.
|
 |
|
Figure 11.14.
The nail is bent to re-create the dorsoradial bow. The amount of bow can be determined by preoperatively measuring the radiographs of the uninjured radius. |
or dynamically (screws at only one end). Fracture stability, expected
patient compliance, and appropriate level of postoperative
immobilization all must be considered. For unstable fracture patterns,
possible noncompliant patients, and patients who desire to be free of
any postoperative immobilization, static locking should be performed
for optimal rotational control and length maintenance. If the surgeon
has any doubt about the length or rotational stability of the fracture,
static interlocking should be done.
One, 2.7-mm, fully threaded, locking screw is placed through a
targeting guide on the driving end of the nail. In the radius, this
screw is placed from radial to ulnar through a 1-cm incision (Fig. 11.18).
The soft tissues are spread to make sure the drill guide is firmly on
bone to avoid injury to the superficial branch of the radial nerve. To
avoid injury to the ulnar nerve, the driving end screw is placed from
ulnar to radial through a l-cm incision of the ulna.
done with the aid of an image intensifier in magnification mode. A
perfect circle view of the hole is obtained. To avoid injury to the
posterior interosseous nerve, the surgeon makes an incision to expose
the bone in the proximal radius. To decrease the possibility of injury
to the posterior interosseous nerve, the arm should be kept in neutral
position with the hole no more than 3 cm from the end of the radius.
The length of the screw is measured from a calibrated drill, and a
unicortical 2.7-mm screw is inserted.
 |
|
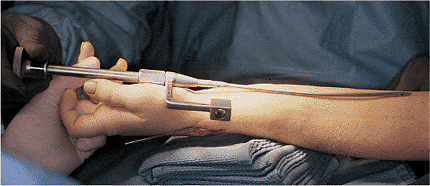
Figure 11.15.
The nail driver and proximal targeting guide are assembled. Orientation of the nail in relation to the normal, dorsal, radial bow is shown. |
 |
|
Figure 11.16. The nail is seated so that the female end is countersunk just below the cortex to avoid irritation of the extensor tendons.
|
 |
|
Figure 11.17.
A 1.5-cm incision is made to insert the driving-end interlocking screw. Drill and screw guides must be placed onto bone to avoid injury to the superficial branch of the radial nerve. |
the arm is checked, and the arc of rotation is recorded. Both screw
holes are checked via image intensification to ensure proper position
of the nail and screws.
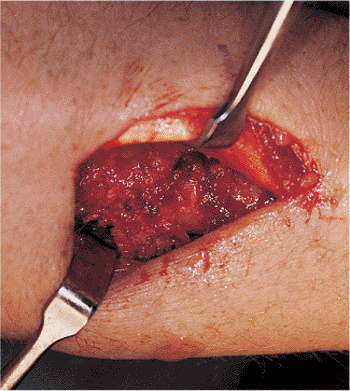
necessary. If nailing is done as an open procedure, a primary bone
graft should be done, especially if comminution, a bone defect, or any
distraction or gap at the fracture site is present. When small amounts
are needed, bone from the reamed area at the entry portal may be
sufficient (Fig. 11.19). Cancellous
bone from the distal radius or proximal ulna can also be used. If
larger amounts of bone are needed, an iliac-crest bone graft should be
obtained. We have no experience with the use of bone-bank grafts or
synthetic bone in conjunction with forearm nailing.
 |
|
Figure 11.18.
A driving-end interlocking screw is shown seated on bone. Image intensification is used to verify that the screw has engaged the hole in the nail. |
 |
|
Figure 11.19. Bone graft obtained from the reamed entry portal is used to pack around the fracture site through the mini–open incision.
|
 |
|
Figure 11.20.
To reduce swelling and control pain, a bulky hand dressing is postoperatively incorporated via use of a sugar-tong splint that provides even compression. The dressing is removed at 2 postoperative weeks for suture removal. |
then a long-arm posterior splint or sugar-tong splint is applied for 2
weeks (Fig. 11.20). In noncompliant patients or
in patients whose nailing was done as an open procedure or was
dynamically locked, the arm is immobilized for 4 to 6 weeks. Heavy
lifting and twisting should be avoided for 3 months. Patients are
followed up at monthly intervals to determine clinical outcomes and
assess radiographic evidence of healing. Recreational activities such
as golf or tennis are permitted at approximately 6 months. Hardware
removal is not recommended unless the patient is severely symptomatic.
at the Los Angeles Medical Center, both retrospective and prospective
reviews have been completed to evaluate forearm nailing by Langkamer
and Ackroyd; Marek; and Rush and Rush. Union rates of 97% have been
reported with good and excellent results in 25 patients. This compares
favorably with results of other series of forearm fractures treated
with plating. All studies emphasized the need for proper patient
selection and careful surgical technique with attention to detail. Ulna
nailing was described successfully by De Pedro et al.
were found in his series of patients treated with intramedullary
nailing. Street et al reported a 93% union rate in their series of
patients
treated with a square forearm nail. Studies by DePedro et al have
correlated accuracy of reduction and the restoration of radial bow in
forearm fractures with return of function.
nail incarceration, iatrogenic comminution of the fracture, fracture
distraction, nonunion, and cortical perforation during reaming or nail
insertion. Successful nailing eliminates the problem of refracture
after implant removal, which has been reported with plating of forearm
fractures. The major complication of nonunion can be minimized if (a)
closed nailing is done whenever possible, (b) distraction at the
fracture site is avoided, and (c) bone grafting is done when open
nailing is necessary in comminuted fractures. Radiographic evidence of
consolidation at the fracture can be slow and should not limit
restoration of function. Technical problems such as nail incarceration,
fracture distraction, iatrogenic comminution, and cortical perforation
are preventable with careful attention to surgical technique and
preoperative planning.
surgeon can avoid it by making sure that the nail advances with each
blow of the hammer. A change in pitch should alert the surgeon that the
nail may be too tight. Removal of the nail with a vise grip or
splitting of the cortex may be necessary to remove an incarcerated
nail. This correction is followed by overreaming of the canal by 1 mm
and reinsertion of the nail with static locking.
be prevented by proper canal preparation. Overreaming by 0.5 to 1.0 mm
will minimize this problem. If either of these occurs during open
nailing, then bone grafting is recommended.
osteosynthesis. Hypertrophic nonunion does not require bone grafting.
Atrophic nonunions should be treated with plating and supplemental,
cancellous, bone grafts.
the entry portal into the radius. Flexion of the wrist to 90 degrees
over a stack of towels will prevent the drill or reamer (or both) from
exiting through the volar cortex.
 |
|
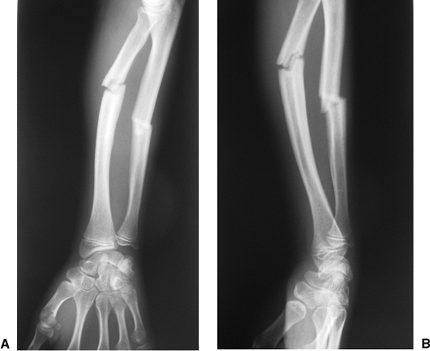
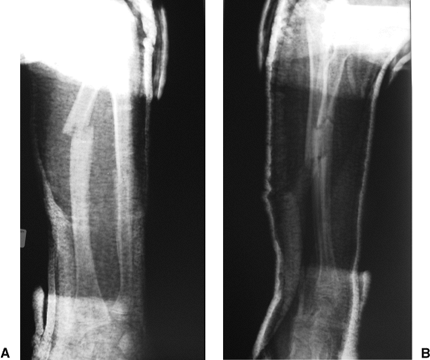
Figure 11.21. AP (A) and lateral (B) radiograph of preoperative radius and ulna.
|
 |
|
Figure 11.22. Preoperative AP (A) and lateral (B) radiograph after closed reduction.
|
 |
|
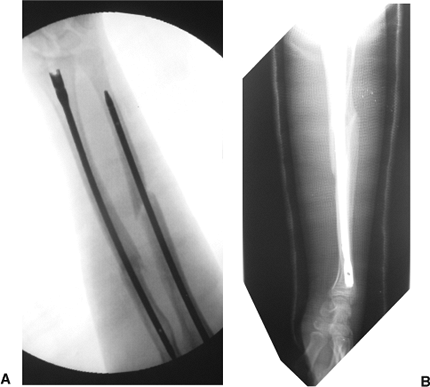
Figure 11.23. Postoperative AP (A) and lateral (B) radiographs after closed nailing.
|
Y, Salai M, Checkik A, et al. Closing intramedullary nailing for the
treatment of diaphyseal fore-arm fractures in adolescence: a
preliminary report. J Pediatr Orthop 1985;5:143–146.
D, Plut J, Wood W. Intramedullary forearm nailing. Paper presented at:
American Academy of Orthopaedic Surgeons Exhibit, 1979.
M, Zinar DM: Intramedullary fixation of forearm fractures using the
Street square forearm nail. Paper presented at: American Academy of
Orthopaedic Surgeons meeting; 1990; New Orleans, LA.
DM, Wolgin M, et al. Prospective evaluation of forearm i.m. nailing.
Paper presented at: American Academy of Orthopaedic Surgeons Meeting;
1992; Washington, DC.
