Tarsometatarsal Lisfranc Injuries: Evaluation and Management
injury is the knowledge that the injury will do poorly with
nonoperative treatment. Conceptually, tarsometatarsal injuries that
will lead to a loss of the arch or significant deformity if treated
conservatively should be treated surgically; these include both
displaced injuries and subtle injuries that have instability in two
planes. The decision to treat a tarsometatarsal injury surgically is
based on both physical examination and radiographic studies.
depend on the tarsometatarsal joints to make the foot sufficiently
rigid to support the body, much as the apical blocks of ice support an
igloo. Unstable tarsometatarsal injuries that compromise this
structural integrity may result in deformity of the foot. In the
majority of displaced injuries, the metatarsals displace dorsally and
laterally on the tarsal bones, which produces pes planus with forefoot
abduction. As a result, when weight is borne on the foot, it collapses.
During heel lift, further deforming forces that act on the midfoot tend
to exacerbate the deformity. For the metatarsals to displace in this
direction, the plantar tarsometatarsal (Lisfranc) ligaments must be
disrupted. Operative treatment is indicated when an ambulatory patient
has an injury that renders the foot mechanically unsound, deformed, or
both.
are apparent on the plain x-rays and who have all the stabilizing
ligaments disrupted are candidates for surgery. When the injuries are
subtle or apparently nondisplaced, operative treatment is indicated
only when two-plane instability is detected on clinical examination or
stress x-rays. Because the foot functions in weight bearing, the
integrity of the plantar ligaments is of greater importance than that
of the dorsal ligaments.
nonambulatory individuals, patients with serious vascular disease
unlikely to heal a surgical incision but who have no significant
deformity, or an injury that is unstable in only the transverse plane.
Lisfranc injuries with only bone injuries can be treated by closed
means or by closed reduction with percutaneous pinning. When deformity
and compromised circulation is found, the surgeon faces a dilemma.
Leaving a deformity puts the patient at risk for ulceration, while
treating it surgically puts the patient at risk for wound-healing
problems. In this circumstance, a vascular surgeon may be consulted to
evaluate whether an inflow procedure would be beneficial prior to
orthopedic intervention.
physician must decide whether sufficient energy produced the injury or
whether an underlying neuropathic condition exists. Trivial injuries
that cause significant displacement should stimulate an investigation
into a possible neuropathic condition. A Charcot neuropathic foot has
different indications for treatment and calls for different technique
than does a foot without preexisting neuropathy. For treatment of a
Lisfranc injury in the presence of peripheral neuropathy, more fixation
will be required, and a longer period of postoperative protection is
indicated.
injuries in orthopedics in which the maxim “the eye doesn’t see what
the mind doesn’t search for” is most appropriate. Swelling and
tenderness in the midfoot with no obvious fracture should trigger a
high index of suspicion. Instability should be determined by physical
examination. The physician grasps the metatarsal heads and applies a
dorsal force to the forefoot while the other hand palpates the
tarsometatarsal joint. Dorsal subluxation or dislocation of the bases
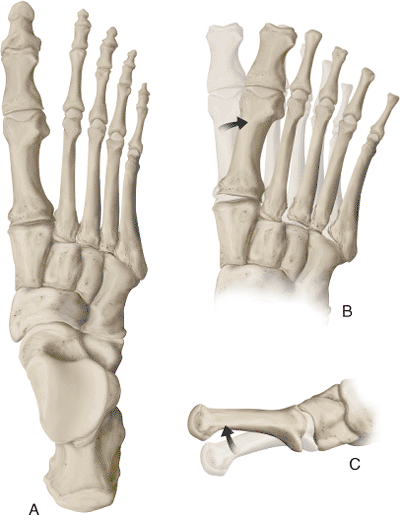
of the metatarsals suggests instability (Fig 36.1).
If the first and second metatarsal can be displaced medially or
laterally as well, global instability is present, and surgical
treatment is needed. Low-energy injuries interrupt the medial capsule
but do not disrupt the plantar ligaments. When the
plantar
ligaments are intact, no dorsal subluxation will occur with stress
examination. These injuries may be treated nonoperatively or with less
rigid fixation at the discretion of the examining surgeon.
 |
|
Figure 36.1. A–C. Diagrammatic representation of a dorsal view of the foot. The metatarsal bases are forced laterally and dorsally.
|
fracture, x-rays made while the patient is not weight bearing may be
deceptively benign. The ligaments are torn with initial displacement;
however, when the deforming force is removed, the foot may spring back
into a neutral position, concealing gross instability. The physician
should be suspicious whenever midfoot gross swelling and pain is found.
films, subtle tarsometatarsal injury is suggested. The first and most
reliable image shows disruption in the continuity of a line drawn from
the medial base of the second metatarsal to the medial side of
intermediate cuneiform on the anteroposterior (AP) and oblique views (Fig. 36.2A).
the interval between the first and second ray; these x-rays should
arouse suspicion. If tenderness is evident upon palpation, stress views
should be obtained.
of the base of the fourth metatarsal should line up with the medial
side of the cuboid on the oblique view. This is a soft sign because the
cross section of the metatarsal base is not equal to the cross section
of the cuboid. As a result, a step-off may be present if the angle of
the beam is slightly misdirected. On the lateral view, the metatarsals
are aligned with the cuneiforms at the dorsal cortex. When ligament
injury is extant, the metatarsals are typically dorsally displaced in
relation to the cuneiforms.
a line tangential to the medial aspect of the navicular and medial
cuneiform, can be found on two views. The disruption will show on the
intersection of the base of the first metatarsal on an AP view taken
during weight bearing. In addition, views taken during abduction stress
reliably predict disruption of the Lisfranc ligamentous complex.
dorsalis pedis and posterior tibial pulses, the integrity of the skin,
and the habitus of the foot. Tendon entrapment may be demonstrated by
an altered, uncorrectable position of the toes or midfoot. Intact or
altered sensation should be documented.
lateral view of the foot under weight bearing, as well as an oblique
view. Oblique views are essential in evaluating a midfoot injury and
should be included in the foot trauma series. If the presence,
location, or degree of injury is uncertain, stress x-rays should be
taken in two planes. Typically they are done through use of fluoroscopy
so the surgeon can make certain that the correct plane is achieved for
the image. When the index of suspicion is high, the stress
roentgenogram is performed in an operating room (OR), so that if the
injury is confirmed, surgery can be done under the same anesthetic.
unit is brought into the OR suite. The table is bent at the knees so
the foot is relatively parallel to the floor. While wearing lead
gloves, the surgeon grasps the first and second metatarsal heads with
one hand and the hind foot with the other. With the thumb placed over
the cuboid to act as a fulcrum, the forefoot is abducted and an AP
x-ray is obtained. Instability is present if a gap occurs on the medial
side of the first or second tarsometatarsal joint, or disruption of the
MCL is produced (see Fig. 36.2D).
uncertainty exists. This is done with the surgeon grasping the midfoot
with one hand and the forefoot with the other, and acutely
plantarflexing through the tarsometatarsal joint. The fluoroscopy unit
is oriented across the
table
and an image is obtained. Although the tarsometatarsal joints may
angulate, they should not open asymmetrically. Subluxation indicates
that the joints are unstable.
 |
|
Figure 36.2. A. An AP x-ray demonstrating a subtle Lisfranc injury. The base of the second metatarsal is displaced laterally. B.
This lateral x-ray, taken under nonweight-bearing conditions, shows that the dorsal cortex of the second metatarsal is subluxed dorsally relative to its cuneiform. C. A scout view is used to confirm that the foot is in the correct position for assessing the tarsometatarsal joints. D. The stress x-ray reveals instability in the first, second, and probably third tarsometatarsal joints. E. An intraoperative fluoroscopic image taken after fixation reveals that the third metatarsal is stable. F. Six weeks following surgery, the reduction appears anatomic and the clinical position of the foot is good. G. Alignment of the metatarsal bases is restored in both planes. |
These injuries are not rare, but because they are subtle, out of the
plane of standard x-rays, and not well described, they are easily
missed. Treatment follows the same principles as those at the Lisfranc
level. Stress views in the AP plane are used to confirm the injury.
Because little motion is characteristic of most of the intercuneiform
joints, any significant motion is abnormal. If the instability is great
enough to allow subluxation of the midfoot, it should be treated.
Displacement of the intercuneiform joints leads to deformity that is
poorly understood and difficult to treat.
and stress views are obtained when there is uncertainty, additional
imaging modalities should not be necessary. Computed tomographic (CT)
scans of the midfoot are difficult to interpret. The role of the
magnetic resonance imaging (MRI) scan has not been established.
 |
|
Figure 36.3. A. An AP x-ray of a left foot with severe Lisfranc injury. All five metatarsals are displaced laterally. B. The lateral view, taken under nonweight-bearing conditions, shows a dorsal dislocation.
|
surgical intervention is necessary. These include the amount of
soft-tissue swelling, the availability of imaging studies, and the
degree of displacement. Surgery should be done emergently only in the
presence of a compartment syndrome, an open injury, or a deformity that
threatens the integrity of the skin. Open injuries should be stabilized
as soon as possible. If emergency stabilization threatens the survival
of the limb, the soft tissue may be treated and the bony stabilization
performed when the safety of the soft-tissue envelope is restored. If
gross instability is found, stabilizing the bone may help the soft
tissue to heal, as it does in long-bone fractures.
greater trochanter to rotate the limb internally to a neutral position.
A second roll is placed beneath the popliteal fossa. Knee flexion
allows plantarflexion of the foot for easier exposure and imaging.
while the surgeon takes care to avoid damage to the dorsal cutaneous
nerves. The first tarsometatarsal joint is exposed between the long and
short hallux-extensor tendons (see Fig. 36.4C).
Typically, one finds significant hemorrhage in this area, making
identification of the structures somewhat difficult. The capsule may be
enfolded into the joint and should be removed and preserved for later
reapproximation. A small periosteal elevator is placed along the medial
side of the first tarsometatarsal joint to confirm its reduced
position. The enfolded joint capsule is removed medially so that the
medial edge of the joint can be seen. Because the displacement is most
often dorsal and lateral, the first metatarsal usually reduces with a
plantar and medial force. When the first metatarsal is reduced relative
to the medial cuneiform, a Kirschner (K) wire is placed across the
joint at its periphery, preventing loss of reduction before definitive
fixation (see Fig. 36.4D).
The K wire is placed in the area of the joint that will not be used for definitive fixation.
 |
|
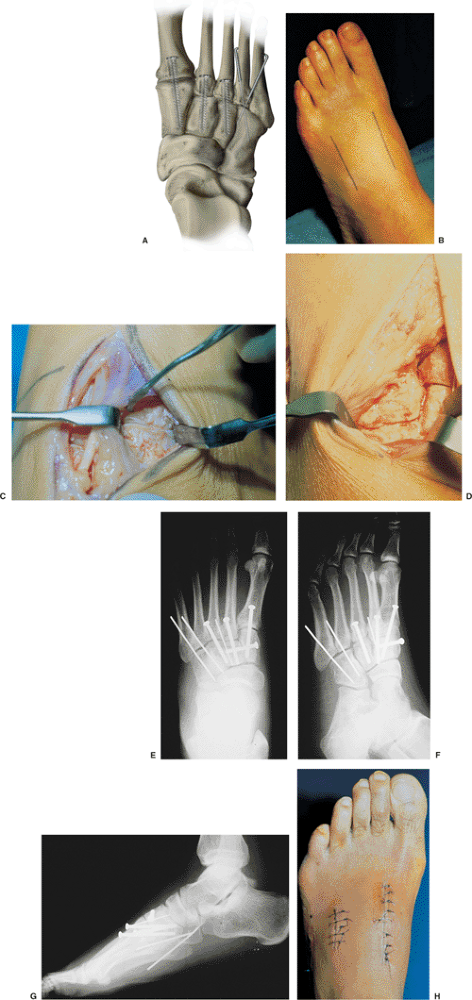
Figure 36.4. A.
Idealized fixation. A small screw, usually 3.5 mm, transfixes the base of the metatarsal and cuneiform. The screw should be directed from distal to proximal and begin approximately 15 mm from the joint or a little farther in the first ray. If an intercuneiform injury is present, an additional screw is directed from medial to lateral. B. The preferred position of the two dorsal incisions. C. This figure shows the intraoperative exposure through the more medial of the two dorsal incisions. D. Intraoperative photograph showing the base of the second metatarsal reduced into its mortise. E. The 3.5-mm screws bridge the first, second, and third tarsometatarsal joints and the joint between the medial and intermediate cuneiform. The fourth and fifth tarsometatarsal joints are transfixed by 0.062-inch K wires. F. This oblique view shows that the base of the fourth metatarsal, on its medial side, lines up with the medial side of the cuboid. G. A lateral x-ray of the same foot as in (F) shows that the dorsal cortex of the metatarsal and tarsal bones are aligned. H. A postoperative photograph of the operated foot at 2 weeks after surgery. |
should check for injury between the medial and middle cuneiforms.
Although not as common as Lisfranc-level injuries, disruption of the
medial/middle cuneiform junction is the most common of the intertarsal
disruptions (Fig. 36.5A). If first-second
intertarsal instability is found, it should be addressed before the
tarsometatarsal repair because it is difficult to secure the
metatarsals to mobile tarsals. Under direct vision, the cuneiforms are
reduced and held together with a pointed reduction clamp. Through a
small stab wound, the surgeon drills from medial to lateral, beginning
in the middle of the dorsal one third of the medial cuneiform. This
starting position is necessary because the middle cuneiform is smaller
in its dorsoplantar and proximal-to-distal direction than is the medial
cuneiform (see Fig. 36.5F). This approach also
allows the surgeon to keep the screw out of the way of the screws that
will traverse the tarsometatarsal joints. The drill hole is measured,
and a 3.5-mm screw is placed from medial to lateral. The screw should
not be placed into the lateral cuneiform (see Fig. 36.5C,D).
mortise between the three cuneiforms. This is accomplished by directly
reducing the base of the second metatarsal against the intermediate
cuneiform. If the surgeon has difficulty reducing it, interposition of
bone may be found plantarly. Occasionally, part of the base of the
second metatarsal is avulsed by the Lisfranc plantar ligament and
blocks reduction of the second metatarsal (see Fig. 36.5A).
A small elevator is used to push the fragment plantarly and medially.
When it is reduced, a large, pointed, reduction clamp is placed from
the base of the second metatarsal to the middle of the medial cuneiform
and compressed. A K wire is placed at the periphery of the joint to
maintain the position. The dorsal cortex of the second metatarsal is
notched 12 to 15 mm from the joint and a hole prepared for the 3.5-mm
screw with a 2.5-mm drill. Before advancing the drill, the surgeon
should center it over the second toe and advance it in a position
almost parallel to the plantar surface of the foot. This is necessary
because the intermediate cuneiform is quite small in cross section, and
if the screw is directed too plantarly, it may completely miss the
cuneiform. To prevent subluxation as the screw is advanced across the
joint, the drill hole should be tapped before a 3.5-mm cortical screw
is inserted. When the screw has been seated, the K wire is removed.
relative to the medial cuneiform. If it has moved or is overreduced, it
should be repositioned and a K wire placed at the edge of the joint.
Again, the surgeon drills, taps, and places a 3.5-mm cortical screw.
This screw should start 15 to 20 mm from the joint, but it need not be
quite parallel to the plantar surface of the foot because the shape of
the medial cuneiform is greater in the dorsoplantar direction. This
screw should be approximately 40 mm in length. If the measured length
is less than 30 mm, the starting hole was placed too close to the joint
or the drill was directed obliquely out of the cuneiform. A screw this
short may not provide adequate purchase in the cuneiform.
evaluated. If it requires fixation but the fourth does not, no further
incision is required. A full-thickness flap is developed through the
original incision until the third tarsometatarsal joint can be
visualized. It will usually follow the second into a reduced position.
It is held in place with a reduction clamp, and the screw is placed
through a small stab wound. However, if the third and fourth metatarsal
bases both require reduction and fixation, a second incision will be
helpful. A longitudinal incision is made over the base of the fourth
ray parallel to the first incision (see Fig. 36.4B).
Depending on the size of the extensor brevis muscle, the surgeon may be
able to elevate the lateral border of the muscle. If it is too large,
the muscle belly is split bluntly in line with its fibers so that the
tarsometatarsal joints are visualized. The third metatarsal base should
be reduced first. Again, a K wire is placed as provisional fixation.
Definitive fixation is provided by a 3.5-mm cortical screw.
mobile, the goals of treatment are slightly different than for the
other joints. These joints must be held in place only long enough for
the surgeon to develop a scar capsule. Screws may break because of the
motion in this joint. The fourth and fifth tarsometatarsals are held in
place and pinned with 0.062-inch
K wires (Figs. 36.4E–G and 36.5C–E). K wires may be used obliquely when reduction is difficult or intertarsal injuries require fixation (see Fig. 36.4A).
 |
|
Figure 36.5. A.
An AP x-ray of a left foot with Lisfranc injury and intercuneiform disruption. Note the avulsion fracture at base of second metatarsal. B. The lateral view, taken under nonweight-bearing conditions, shows dorsal dislocation and cuneiform fracture. C. A postoperative AP view with intercuneiform fixation. Tarsometatarsal fixation with 4.0-mm cortical screws and lateral K wire fixation. D. Postoperative lateral view, taken under nonweight-bearing conditions, shows dorsal placement of intercuneiform screw fixation, which allows adequate room for crossed 4.0-mm cortical screw fixation in the first ray. E. Oblique view confirms anatomical reduction of fourth and fifth metatarsal-cuboid joints. F. Coronal weight-bearing CT cut at the level of the medial and middle cuneiforms demonstrates rapid plantar tapering of the middle cuneiform. This relationship necessitates dorsal screw placement for intercuneiform fixation. |
They most commonly present as a fracture through the metaphysis of the
metatarsals. When unstable, the fracture should be stabilized, and then
the joint evaluated. If fractures are present without concomitant
ligament injuries, reduction and pinning may be adequate, because
fractures get sticky within 3 weeks and heal within 6 weeks. A common
pattern includes a joint disruption at the first ray, a fracture
through the second metatarsal base, and a joint injury at the third.
Because the second metatarsal is recessed into a mortise between the
cuneiform, it fractures and leaves the base attached to the ligaments.
If the first and third rays are stabilized across the joint, the second
requires only reduction and sometimes pinning for 4 weeks. When
fractures pass through the metatarsal bases and the joint is intact,
treatment is not so involved: Reduction and pinning with K wires may be
enough. Unlike the ligaments, fractures heal reliably in 6 weeks. The K
wire can be left in place until the fracture becomes stable. Once the
fracture is healed, mechanical stability is restored.
have resulted in the development of newer implant technology. The
4.0-mm cortical screw is 15% stronger in bending than the 3.5-mm
cortical screw (Table 36.1). The strength
advantage results primarily from the core diameter of 2.9 mm for the
4.0 mm cortical screw versus 2.4 mm for the 3.5-mm cortical screw. This
newer screw has proven useful in crowded Lisfranc constructs while in
theory it also reduces hardware failure (see Fig. 36.5C–E).
absorbable screws in an attempt to minimize both the incidence of
symptomatic hardware and subsequent surgical procedures for hardware
removal. Results appear safe in small numbers at short-term follow-up.
The efficacy of these implants has yet to be tested for maintenance of
reduction in long-term follow-up.
splint at the end of the operation. The patient is discharged when he
or she safely masters ambulation with crutches or a walker, and pain
control is achieved with oral agents. The length of stay is dependent
on associated injuries, the fragility of the patient, and the degree of
swelling. The range varies from outpatient surgery to 4 or 5 days as an
inpatient. Sutures are removed 10 to 14 days after surgery. If the
injury was isolated, the patient reliable, and fixation secure, the
splint is replaced with a removable brace. If any of these three
factors is absent, a short-leg non–weight-bearing cast is recommended
for an additional 4 weeks.
areas so the surgeon can document the alignment and assess fracture
healing. Postoperative imaging should include a simulated
weight-bearing AP and lateral as well as an oblique view. For most
injuries, partial weight bearing is instituted with the patient wearing
a removable protective boot at 6 weeks. Self-directed physical therapy
(PT) is begun at this time. Swimming is encouraged, and riding an
exercise bike is allowed. Depending on the stability and fixation, the
patient is encouraged to gradually advance to full weight bearing over
the 2 to 4 weeks after the protective boot is implemented. At 8 to 10
weeks, the patient can begin wearing a regular shoe if the foot is not
too swollen. The screws are left in place for a minimum of 16 weeks.
first through third tarsometatarsal joints, they may be left
permanently in place. If the joint has become sufficiently stiff, the
screws will not be symptomatic. However, a small amount of motion
frequently occurs, which causes the screws to loosen. If this happens,
the screws can often be removed under local anesthesia in the office or
outpatient center.
stockings may be beneficial. Initially the patient may begin by wearing
athletic shoes. As activity level increases, a standard work shoe may
replace the athletic shoe for a few hours a day in increasing amounts
until normal shoes can be tolerated. The process may be facilitated by
a custom-molded full-length insole of a nonrigid material such as cork
or pelite.
work in an office. They should return to work in 3 to 4 months if they
are involved in heavy labor activities. Patients should avoid
jumping-type recreational activities, such as basketball and
volleyball, and running for 9 to 12 months. The degree of work and
recreational activities depends on the amount of trauma, the degree of
articular surface injury, and the quality of the bone. Most patients
will continue to have some symptoms in the foot for up to 2 years. Many
will have life-long symptoms. Only 12% will need midfoot arthrodesis if
bony Lisfranc injuries are anatomically
reduced
and held rigidly. A slightly higher trend toward midfoot arthrosis can
be found in those with pure ligamentous injuries. If symptoms are
mechanical (i.e., midfoot pain during heel rise), a custom,
full-length, semirigid insole may be beneficial. Generally, this should
be fabricated when the patient has returned to full weight bearing and
the swelling has resolved.
dislocations include intercuneiform injuries, tendon entrapment, and
vascular injury. The interval between the medial and intermediate
cuneiform is the most common, associated, intercuneiform, joint injury.
The tibialis anterior is the most commonly entrapped tendon. The
tibialis anterior tendon inserts in part on the base of the first
metatarsal. As the first metatarsal is displaced laterally, it takes
the tendon with it. As the deforming force is removed, the metatarsal
moves medially, and the tendon is trapped by the medial cuneiform. This
complication is treated during open reduction. At the time of surgery,
the anterior tibia tendon will be in the way of reduction and can be
reduced to its normal position. The most common vascular injury is to
the plantar branch of the dorsalis pedis, where it is tethered between
the first and second metatarsal. Damage to this vessel, however, is of
little clinical significance; however, some historic references
document the potential for more severe injuries that result in forefoot
ischemia.
superficial peroneal nerve also may occur. Because the tissues are
edematous and displaced and hemorrhage is significant in the
subcutaneous tissue, identification of these small nerves is
challenging. Care should be taken to preserve the nerves, and patients
should be warned preoperatively that nerve injury is possible. If one
of these nerves is divided during surgery, the proximal end can be
tucked into the extensor brevis muscle belly or the two ends can be
reapproximated.
direct trauma. There is little muscle to absorb the load or augment the
blood flow. Patients should be warned that eschar may develop in areas
that were injured and may include the surgical incision. It is uncommon
for these soft-tissue problems to require free tissue transfer, but
skin grafts are common in direct injuries. Full-thickness wounds are
managed with dressing changes until an adequate bed of granulation
tissue is generated to support a split-thickness graft.
it occurs and is painful or leads to instability, it must be treated.
Sometimes, in spite of nonunion, “splinting” by the surrounding
structures is sufficient such that symptoms are minimal and surgical
treatment is unnecessary.
to loss of the arch and abduction of the forefoot. Great care should be
taken to plantarflex and adduct the metatarsals adequately. To lessen
the likelihood of incomplete reduction, the surgeon must be certain
that the first metatarsal is brought medially and plantarly before
trying to reduce the second metatarsal. A prominent cuneiform may be
observed on the dorsomedial aspect of the foot when the first
metatarsal is incompletely plantarflexed and adducted. At times this
deformity may also be due to unrecognized intercuneiform injury.
HS, Manos RE, Buoncristiani A, et al. Abduction stress and
weightbearing radiography of purely ligamentous injury in the
tarsometatarsal joint. Foot Ankle 1998;19(8):537–541.
