Distal Radius Fractures: External Fixation
injuries in clinical practice. They tend to occur in a bimodal fashion
with a peak associated in children and adolescents as well as elderly
patients. Nonarticular fractures of the distal radius and most
epiphyseal fractures in children are typically treated, with
predictable success, by cast immobilization. With increasing age,
osteoporosis and falls lead to fragility fractures of the distal
radius, particularly in women. These fractures often have significant
fracture comminution with instability, making closed treatment less
successful. In young patients with normal bone stock, these fractures
are often caused by motor vehicle accidents or a fall from a height,
and they often result in highly comminuted fracture patterns. While
many of these fractures can be reduced by closed means, comminution and
instability lead to loss of reduction and malunion.
reduction and casting defines fracture instability. Many authors have
proposed criteria to predict which fracture patterns are inherently
unstable and may benefit from surgical treatment. Lafontaine et al (1)
proposed five factors that indicated fracture instability: (a) initial
dorsal angulation greater than 20 degrees, (b) dorsal comminution, (c)
radiocarpal intra-articular involvement, (d) associated ulnar
fractures, and (e) age greater than 60 years. In their experience,
patients with three or more of these factors had a high incidence of
reduction loss with cast treatment. Nesbitt et al (2)
used the criteria of Lafontaine et al and determined that age was the
only significant risk factor in predicting instability. In patients
over the age of 58 years, there was a 50% risk for secondary
displacement, while patients over 80 years had a 77% increased risk. In
addition to the Lafontaine factors, carpal malalignment and
postreduction incongruity (the combination of articular step-off and
fracture gap) have been shown to have a negative impact on functional
outcome (3,4).
unstable distal-radius fractures have become available, especially the
use of anatomically designed plates for the volar, radial, and dorsal
aspects of the radius. In the past, external fixation had been the
workhorse for unstable distal-radius fractures which had been judged to
be too unstable for cast treatment. With
advances
in internal fixation, external fixation is used more commonly as an
adjunctive procedure to other fixation techniques. These techniques
include Kirschner (K) wire fixation, Kapandji pin technique,
arthroscopically assisted articular-surface reduction (5)
and the placement of fragment-specific miniplates. These techniques are
frequently augmented with metaphyseal bone fillers such as cancellous
allograft chips and hydroxyapatite cement. Thus, external fixation
devices that span the fracture can be used to neutralize the forces
around the wrist and to protect the fracture reduction obtained by
other direct or indirect means.
be used as both the reduction tool and the neutralization device. This
is accomplished through the use of dorsally applied half pins which can
directly manipulate and reduce displaced fragments. This construct
combines the principle of Kapandji, dorsal, and blocking pins with the
security of half pins locked to the frame. It also improves restoration
of palmar tilt, which is difficult to accomplish with spanning frames (6).
information gathering on hand dominance, occupational requirements,
medical co-morbidities, and patient expectations, are important factors
in crafting a treatment strategy. The mechanism of injury and a careful
examination of the limb allow the surgeon to assess soft-tissue
integrity. Any signs or symptoms of increased compartment pressure or
evolving neurological deficits mandate that any splints or cast be
removed for more precise evaluation and treatment. Furthermore, it is
necessary to check the forearm and elbow for instability and the
possibility of combined fracture-dislocation patterns such as Galeazzi,
Monteggia, or Essex-Lopresti injuries. The carpus should be carefully
palpated to determine if any focal sources of pain or deformity can be
found in carpal injuries or dislocations. The hand should also be
carefully evaluated for signs and symptoms of injuries to the
metacarpals and phalanges.
sensation and motor integrity should be documented and the results
assessed. The encompassing, and often incorrect assumption of
“neurovascularly intact,” should not be used when evaluating patients
with a distal radius fracture.
digits, especially the basal joint of the thumb, should be noted. Often
joints with preexistent stiffness are adversely affected by the
postfracture swelling, pain, and immobilization, and as a result hand
function is compromised.
closed distal-radius fractures. However, the surgeon should caution
patients about the small risk of late, extensor pollicis longus (EPL)
tendon ruptures.
asking the patient to grasp, and to confirm anterior interosseous nerve
integrity, by paying particular attention to the flexor pollicis longus
(FPL) and flexor digitorum profundus (FDP) to the index finger.
Abducting and adducting the second ray will confirm ulnar-nerve
intrinsic function. Tip pinch will confirm median nerve thenar function.
lateral, and oblique radiographs should be obtained. True lateral
x-rays of the wrist are more difficult to obtain when the wrist is
immobilized in flexion and ulnar deviation. Contralateral films can be
helpful in assessing the normal radial and ulnar lengths as well as
radial inclination of the wrist.
useful in predicting the magnitude of the forces involved as well as
the displacement and comminution. Traction films obtained in the
emergency room or operating room will allow assessment of articular
incongruities such as scaphoid or lunate die-punch injuries. Traction
films can also reveal subtle, combined, carpal bone and or ligamentous
injury (i.e., transradial styloid-perilunate instability).
all distal-radius fractures. Although most ulnar styloid fractures heal
uneventfully with a fibrous union, some ulnar-styloid fractures are
associated with distal radioulnar joint (DRUJ) instability. Ulnar
styloid fractures that occur through the base and those displaced
greater than 2 mm have highest likelihood of associated DRUJ
instability (8). However, DRUJ stability is assessed following stabilization of the radial fracture.
radial length to within 2 to 3 mm of uninjured wrist. Radial
inclination is approximately 21 degrees and radiocarpal congruence is
within 1 mm. The lateral view should demonstrate a collinear
relationship with the radial shaft and lunocapitate axis: There should
be no more than 5 to 10 degrees of articular dorsal tilt and preferably
neutral or inclined toward the normal 10-degree palmar tilt.
reduction of the distal radius. Residual angular or rotational
instability, such as dorsal, intercalated, segment instability (DISI),
is usually a sign of laxity of the extrinsic capsular ligaments, which
can occur secondary to a loss of axial length or from rupture. The
peri-articular shear fractures, either dorsal or palmar, are
essentially ligamentous injuries that require secure repositioning of
the fracture to effect stable reduction. Assessment of the break in the
carpal arcs, as described by Sarmiento et al (9), should be recognized; these breaks may be unmasked by traction films taken in the emergency or operating room.
necessary for preoperative planning. In fact, standard two dimensional
CT scans done prior to reduction may create more confusion in
interpreting the position of unstable, unreduced fragments. We prefer a
traction film taken in the operating room for its simplicity in
preoperative planning.
well as a thorough review of the radiographs, surgical or nonsurgical
treatment is recommended. Based on criteria elaborated previously, we
attempt to identify stable and unstable fracture patterns. The ultimate
treatment plan is based upon the patient’s expectations, functional
requirements, and medical conditions; each plays a role in the
indication for surgery. With regard to marked loss of radial length,
radial inclination, and reversal of palmar tilt, numerous studies have
shown measurable deficits in the objective and subjective outcomes
following cast treatment. These differences in outcomes are magnified
when loss of articular congruence and carpal subluxation are found (3,4). Treatment decisions should be made in the context of the entire person and not on the radiographic findings alone.
seen in the emergency room undergo a closed reduction and application
of a sugar tong splint with application of a Bier block or a fracture
hematoma injection. If a hematoma block is used, one must remember to
also inject the ulnocarpal joint to achieve complete anesthesia of the
injury. The ulnar side of the wrist joint is almost always involved in
a distal radius fracture through an ulnar styloid fracture or
peripheral triangular, fibrocartilage complex (TFCC) tear.
radiographs show restoration of radial length, minimal loss of palmar
tilt, and most important, good cortical apposition and minimal fracture
comminution. The wrist is held in slight flexion, ulnar deviation, and
neutral forearm rotation. Weekly follow-up x-rays for the first 3 weeks
are necessary to guard against loss of reduction. The palmar extent of
the cast must always be contoured to allow for full
metacarpal-phalangeal joint flexion. Casting usually continues for 6
weeks followed by transitional splinting with a removal prefabricated
splint. If finger motion can be maintained, then little formal
occupational therapy is required. If stiffness or swelling in the
immediate postreduction period is significant, then supervised
occupation therapy is recommended.
then surgical management is indicated in all but the most elderly or
infirm. In most cases, it is better to perform primary osteosynthesis
rather than late three-dimensional osteotomy and grafting.
treated with external fixation, few should be treated with a spanning
construct alone. The fracture morphology usually will dictate if
additional or augmented fixation is necessary (10).
This may include Kapandji dorsal intrafracture K wire pinning,
transradial styloid-interosseous pinning, and metaphyseal-bone filler
support with allograft or hydroxyapatite-based bone cements (11).
In minimally comminuted fractures, with sufficient distal-fragment bone
stock, a non–joint-spanning external fixation may be a superior
technique for restoring the radial length, inclination, and palmar tilt
(6). Dorsal volar-shearing type fractures, such
as Smith and volar Barton, should be treated with a buttress plate.
Scaphoid or lunate die-punch injuries should be treated with elevation
of fragments and subchondral support which can often be performed with
arthroscopic assistance (12).
anesthesia with either an infraclavicular or axillary block. This is
performed with nerve stimulation assistance to avoid transaxillary
arterial puncture. Regional anesthesia allows full muscle relaxation
and postsurgical pain relief for 8 to 12 hours.
the arm is abducted and placed on a radiolucent arm board. A C-arm
image intensifier must be available. A first generation cephalosporin
is given intravenously prior to the inflation of the arm tourniquet,
which is used in all cases. If a penicillin allergy exists, vancomycin
is substituted.
pressure is set at 250 mm Hg in the adult, but for very large or small
circumference limbs, it may be adjusted to within 70 mm Hg of mean
systolic pressure. Tourniquet times should be limited to less than 120
minutes to limit muscle weakness from prolonged tissue ischemia.
traction apparatus attached to the arm board to assist in preliminary
fracture reduction. The traction apparatus can also be used to
facilitate intraoperative traction radiographs. It can also help with
the application of adjunctive K wire fixation prior to the distraction
through the completed external-fixation construct.
near the foot of the bed. The overhead traction tower may also be used
to facilitate the arthroscopic examination.
of the distal fragment, we employ a combination of K wire insertion
techniques following fracture reduction. The Kapandji technique is
useful in providing a prop or support to prevent gradual fracture
resettling that is secondary to dorsal cortex incompetence. We use two
or three dorsal, intrafocal 0.625 K wires. The K wires are introduced
by hand directly into the fracture site and up to but not through the
palmar cortex. Respecting the dorsal extensor tendon, we place one wire
radial to the fourth dorsal compartment and another ulnar to the fourth
compartment. The power wire driver is used to assist this process if
the bone is particularly dense. The pin is then directed distally to
affect a clockwise rotatory force to correct the dorsal displacement
and reversal of palmar tilt. Once this is accomplished, the K wire is
then driven in a retrograde fashion to engage the palmar cortex and is
thus stabilized against migration. The force and direction of the
Kapandji pins tends to translate the distal radius fragment in a palmar
direction. This tendency is accentuated when the palmar cortex is
comminuted. To prevent this secondary deformity of overreduction, one
must place a transradial, styloid, intramedullary pin. Following
placement of the K wires, we favor a neutralizing, spanning,
external-fixation frame until fracture union. We prefer to leave K
wires percutaneous to allow for ease of removal in the outpatient. The
K wires are cut, with 2 to 3 cm protruding from the skin, and then pin
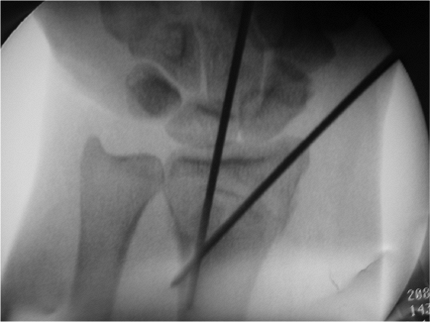
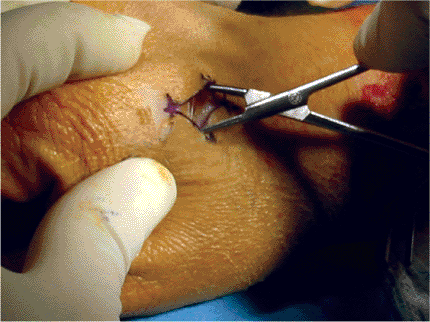
caps are applied (Figs. 12.1 and 12.2).
 |
|
Figure 12.1. Dorsal Kapandji and radial styloid pins placed.
|
 |
|
Figure 12.2. Fluoroscopic image of Kapandji and radial styloid pins.
|
made regarding the presence and magnitude of residual, metaphyseal,
bone loss. Many patients with severe osteopenia will have significant
bony defects that can lead to late settling and reduction loss despite
proper placement of K wires (11). Placing a
bone filler or substitute is effective and avoids the morbidity of an
iliac-crest bone graft. We use freeze-dried, allograft, cancellous-bone
chips, which can be crushed and placed into the void with an impaction
grafting technique. This will supplement the fixation with rapid
incorporation and remodeling (7). This
technique also decreases the stress on the K wire and external fixation
construct, and therefore, it can prevent late settling and loss of
radial length even after the external fixation frame is removed. One
can also use hydroxyapatite cements, which provide similar mechanical
support, but with some reduction in bone remodeling that is secondary
to slow, and perhaps, incomplete resorption (10).
and fourth dorsal compartments just ulnar to Lister’s tubercle. The
proximal extensor retinaculum is divided. The EPL is retracted radially
and the extensor digiti communis (EDC) is retracted ulnarly. The
fracture site is visualized and used as the window for bone grafting. A
cavity is then created within the fracture site. This is done by
compacting and compressing the cancellous bone within the metaphysis of
the distal radius. The crushed cancellous bone chips are then place
into the void. They are then impacted with an elevator against the
subchondral surface until the entire void is filled with the allograft
chips (Figs. 12.3 and 12.4).
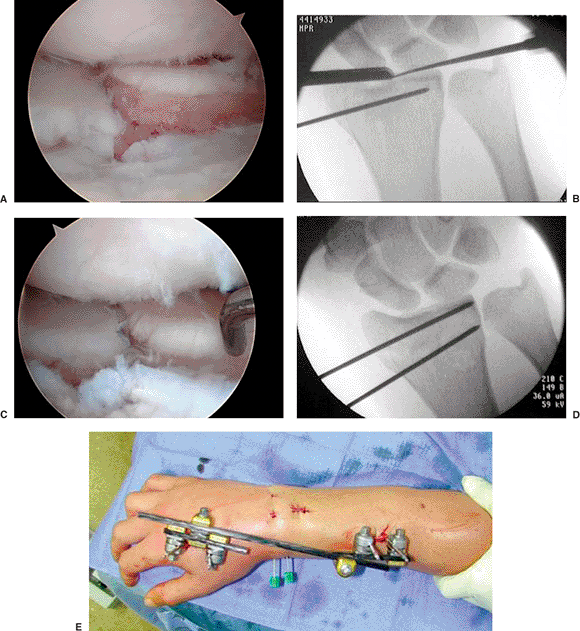
selected articular-fracture fragments. These injuries can be reduced
from the metaphyseal side with elevators as a prelude to bone or bone
substitute grafting. However, certain fractures will not reduce this
way and arthroscopy is less invasive than a formal arthrotomy.
Arthroscopy is performed with vertically applied traction. This setup
allows for intraoperative fluoroscopy and extra-articular K wire
elevators can be used to fine tune the reduction (Fig. 12.5).
index and long fingers and is generally set at 4.5 kg. Care is taken to
pad and protect the ulnar nerve. Arthroscopy portals are outlined with
a skin marker and follow the dorsal compartment intervals. The
workhorse portals are the 3–4 and 4–5, but all may be used. Dorsal
veins are noted so that they are avoided during portal creation.
 |
|
Figure 12.3. Metaphyseal void under fluoroscopy.
|
 |
|
Figure 12.4. Bone graft placement in the metaphyseal void under fluoroscopy.
|
joint is then distended with 3 to 5 cc of normal saline injected
through the 3–4 portal. Joint triangulation is tested with an 18-gauge
needle. The portals are then created with a nick-and-spread method to
protect the articular cartilage from iatrogenic injury. A 2 to 3 mm
incision is made with a no. 11 blade and then a small, curved hemostat
is used to penetrate the dorsal joint capsule. A hemostat is spread
wide enough to allow a 2.7-mm blunt trochar and cannula to be inserted
into the 3–4 portal. Visualization is usually obscured with clotted
blood in the joint. This is rapidly cleared with pressurized joint
lavage set at a maximum of 25 mm Hg. A synovial shaver can also help
clear joint debris quickly. In many patients, there is an articular
defect on the carpal side of the injury from axial load and impaction.
One major additional benefit of arthroscopy is the ability to evaluate
intercarpal ligament injuries, as well as TFCC tears, which are common
and often unrecognized (13). Extra-articular
placement of joystick K wires and bone elevators allows reduction and
elevation of fragments, which can then be secured by subchondral wires
and supported by a spanning, external, fixation frame and a bone graft
or filler as indicated (Fig. 12.6).
 |
|
Figure 12.5. Arthroscopic setup.
|
 |
|
Figure 12.6. A. Visualization of the fracture site. B. Fluoroscopic image with instruments in place. C. After arthroscopically assisted articular reduction of the fracture site. D. K wires used to hold together the reduction. E.
After arthroscopically assisted reduction, an external fixator is placed. Note the midline dorsal incision where the metaphyseal bone graft was placed. |
fracture has been accomplished, a decision to proceed with either
non–joint-spanning or joint-spanning external fixation is made. If the
distal fracture fragment is large enough, we always prefer to use a
non–joint-spanning external fixator. However, if the fracture fragment
is too small or if there is too much comminution, then we will use a
spanning external fixator.
external fixation as the best way to control radial length,
inclination, and most of all, the restoration of palmar tilt (6). The studies of Bartosh and Saldana (14)
clearly demonstrate the difficulty of attaining full correction of
palmar tilt with a spanning device: the palmar capsule is symmetrically
tensioned and thus limits the correction to neutral tilt.
can be used with the spanning and the nonspanning external fixators.
The proximal pins are placed about 10 cm proximal to the tip of the
radial styloid. They are positioned in the bare interval of the
midradius between the brachioradialis and the extensor carpi-radialis
longus muscles. Pin placement is done through a limited open approach
to insure identification and protection of the radial sensory and
lateral antebrachial-cutaneous nerves (15). The
limited open approach also insures that the pilot holes and half pins
are placed in the central axis of the radial shaft. To minimize the
risk of heterotopic ossification, one must be careful not to violate
the interosseous membrane with the drill or half pins. We prefer
self-tapping pins that engage the distal cortex. Prestressing the pins
during the assembly of the external fixator is unnecessary and may lead
to resorption of the bone around the pins and subsequent premature
loosening.
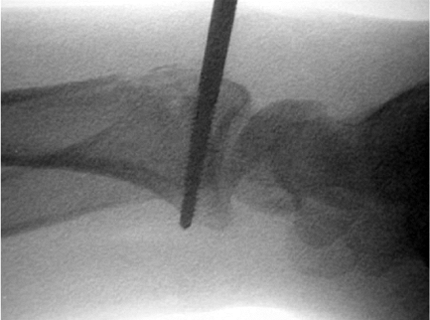
placement is finalized. Most fractures that have at least 6 mm of
cortex proximal to the subchondral plate can accept the 3 mm threaded
half pins. If the fracture is amenable to a non–joint-spanning external
fixator, a longitudinal, transradial, styloid, K wire is placed to
prevent overtranslation of the distal fragment. The pins should be
inserted through 2-cm longitudinal incisions that are placed between
the dorsal compartments. Because most distal-radius fractures include a
radial styloid and/or scaphoid facet fragment and an ulnar or lunate
facet fragment, the two distal half pins must stay within the limits of
those fracture fragments. For the protection of all soft tissues,
including cutaneous nerves and tendons, we prefer to use small
incisions instead of percutaneous placement of the half pins. Pilot
holes (1.5 mm) are drilled for the self-tapping 3-mm half pins. It is
important to use the designated soft tissue sleeves to facilitate pin
placement, and to be secure, the half pins must engage the palmar
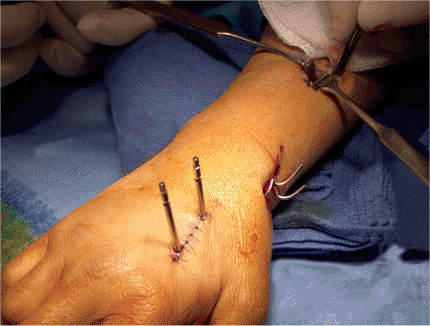
cortex (Fig. 12.7).
 |
|
Figure 12.7. The distal pins in the nonspanning external fixator engaging the palmar cortex.
|
 |
|
Figure 12.8. A,B. Final construct of non–joint-spanning external fixator.
|
is applied with pin-to-rod connectors. A moderate amount of traction is
applied to unload the previously placed adjunctive K wires and/or
metaphyseal bone filler. We use graphite rods because they are light
and radiolucent (Fig. 12.8).
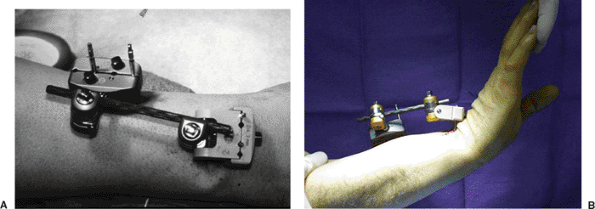
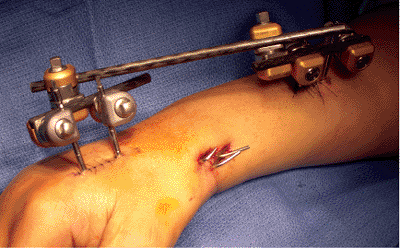
employed, then a joint-spanning external fixator is created. The
metacarpal pin placement should also be done through a limited open
approach (Fig. 12.9). The incision is
positioned over the proximal third of the second metacarpal and is
centered in the bare area between the first dorsal interosseous muscle
and the extensor tendon to the index finger. To avoid the possibility
of a stress fracture, the pilot holes for the 3-mm half pins must be
placed in the center of the cylindrical metacarpal shaft. The more
proximal pin of the pair can be oriented to cross the bases of the 2nd
and 3rd metacarpals. This enables four cortices to be captured because
the bases of these two are in close proximity, and there is no
violation of the interossei muscles. The metacarpal pins must be kept
in the proximal third of the second metacarpal. This pin placement
prevents encroachment upon the metacarpal-phalangeal joint capsule or
interference with the smooth gliding of the lateral bands. The
orientation of these pins should be 45 degrees to the long axis to
permit full abduction and extension of the thumb (15).
As noted previously, to have maximal purchase for the duration of the
frame application, one must ensure that the terminal threads of the
self-tapping half pins engage the far cortex fully (Fig. 12.10).
 |
|
Figure 12.9. Dissection of metacarpal pin-placement site using a limited open incision.
|
 |
|
Figure 12.10. Location of proximal and distal screw site placement.
|
 |
|
Figure 12.11. Final frame assembly.
|
the muscle interval closed over both the proximal and distal pin
groupings. The skin should be closed by the orientation that provides
the least skin tethering because most of the pin-skin interface
problems are due to excessive traction on the skin. Poor closures can
cause wound necrosis, which ultimately leads to local pin-tract
infection and early pin loosening.
The pin clamps and connecting bars are placed close to the skin to
minimize the profile and to make it easy to wear shirts and coats. The
final wrist position need not be in the classic Cotton-Loder ulnar
deviation and wrist flexion as the ligamentotaxis effect is not
required for maintenance of reduction. The distal fragment must not be
overpronated in the spanning frame. Overpronation of the distal
fragment will restrict restoration of supination. A few degrees of
volar flexion and ulnar deviation are all that usually are necessary.
Tighten all remaining pins and bar clamps.
of the distal radioulnar joint. If dorsopalmar translation is greater
than on the contralateral wrist, arthroscopic evaluation and repair of
the TFCC ligaments may be indicated. Alternatively, the position of the
forearm in the fixator may be adjusted to increase stability.
Occasionally, K wire fixation of the distal radioulnar joint may be
necessary.
pins, and early motion of the fingers and thumb is encouraged. Index MP
flexion or thumb abduction and extension should not be discouraged.
Final intraoperative x-rays should not demonstrate any carpal
distraction at either the proximal or midcarpal articulations. Surgical
incisions are infiltrated with 0.5% Marcaine as a postoperative
analgesic. Palmar plaster splints may be used to control wrist motion
if a non–joint-spanning fixation frame is employed.
and pain management. In the morning of the first postoperative day,
patients are seen by an occupational therapist to review finger, elbow,
and shoulder range of motion exercises. They are encouraged to use
their fingers, elbow, and shoulder for activities of daily living. The
use of a sling is used intermittently for comfort and to control
swelling. Pin sites are cleaned with hydrogen peroxide and cotton tip
applicators.
removal and x-rays. They can now shower and have water run over their
fixator. If patients have limited finger mobility or are reluctant to
use their hands, formal, supervised, hand therapy is begun.
and pins are removed under local anesthesia. Hand therapy is
intensified with emphasis on functional tasks and the return to
previous activities. Most patients can transition to a home program at
2 to 4 months after surgery, but gains in strength can continue for up
to 1 year.
pin track infection. Most can be managed by pin care and oral
antibiotics. If the pins loosen, they must be replaced if the frame is
still required. Modern frames have excellent articulations and usually
will not loosen. It is important to check for frame tightness at each
postoperative visit.
stiffness early in the postoperative period. They should be
aggressively treated to avoid arthrofibrosis. This is not a complex
regional pain syndrome (CRPS) as is often suggested. If a CRPS is
present, a multimodal and interdisciplinary approach is used and may
include regional blocks, pain management, and even manipulation under
anesthesia prior to the onset of unyielding capsular contractures.
MM, Hajducka C, Court-Brown CM. Redisplaced unstable fractures of the
distal radius: a prospective randomised comparison of four methods of
treatment. J Bone Joint Surg Br 1996;78(3):404–409.
K, Hattori Y, Otsuka K, et al. Intra-articular fractures of the distal
aspect of the radius: arthroscopically assisted reduction compared with
open reduction and internal fixation. J Bone Joint Surg Am 1999;81(8):1093–1110.
MM. Redisplaced unstable fractures of the distal radius. A randomised,
prospective study of bridging versus non-bridging external fixation. J Bone Joint Surg Br 1998;80(4):665–669.
M, Chapman CB, Roh M, et al. Treatment of unstable distal radius
fractures with cancellous allograft and external fixation. J Hand Surg [Am] 1999;24(6):1269–1278.
MM, Lawton JN, Blazar PE. Ulnar styloid fractures associated with
distal radius fractures: incidence and implications for distal
radioulnar joint instability. J Hand Surg [Am] 2002;27(6):965–971.
SW, Austin G, Lorenze M, et al. A biomechanical comparison of different
wrist external fixators with and without K-wire augmentation. J Hand Surg [Am] 1999;24(3):516–524.
TE, Wagner W, Hanel DP, et al. Intrafocal (Kapandji) pinning of distal
radius fractures with and without external fixation. J Hand Surg [Am] 1998;23(3):381–394.
RA, Saldana, MJ. Intraarticular fractures of the distal radius: a
cadaveric study to determine if ligamentotaxis restores radiopalmar
tilt. J Hand Surg [Am] 1990;15(1):18–21.
