Open Fractures
injuries. While the goals of treatment are similar to those in adults,
the methods used to achieve these goals may differ. Children heal more
quickly, have significant remodeling potential, and generally have
fewer premorbid conditions than adults. However, open physes and size
limitations preclude many of the fixation options available for adult
fractures.
-
Occur as a result of higher energy injuries
-
Associated injuries seen in 25% to 75% of children with open fractures
-
Motor vehicle accidents, pedestrians/bicyclists hit by vehicles, and falls are common causes.
-
10% of all polytraumatized children have open fractures.
-
While pediatric fractures are extremely common, open fractures fortunately account for only 2% of the total.
-
Higher energy trauma results in higher grade injuries.
-
Higher energy required to cause an open fracture results in increased comminution and soft tissue stripping.
-
Communication with the external environment allows foreign material and bacteria to contaminate the fracture site.
-
Necrotic soft tissue and bone are easily
infected and poor antibiotic penetration in these areas makes
controlling any infection difficult. -
Fracture stabilization of unstable fractures prevents further soft tissue damage, and allows for neovascularization and healing.
-
Mechanism
-
Time of injury
-
Medical history
-
Tetanus immunization
-
Head-to-toe evaluation of entire patient to rule out other injuries—remember your ABCs!
-
Detailed evaluation of injured extremity, including skin condition
-
□ Neurologic exam
-
□ Vascular exam
-
□ Size and configuration of wound
-
□ Amount of contamination
-
□ Tissue pressure measurements if compartment syndrome suspected
-
-
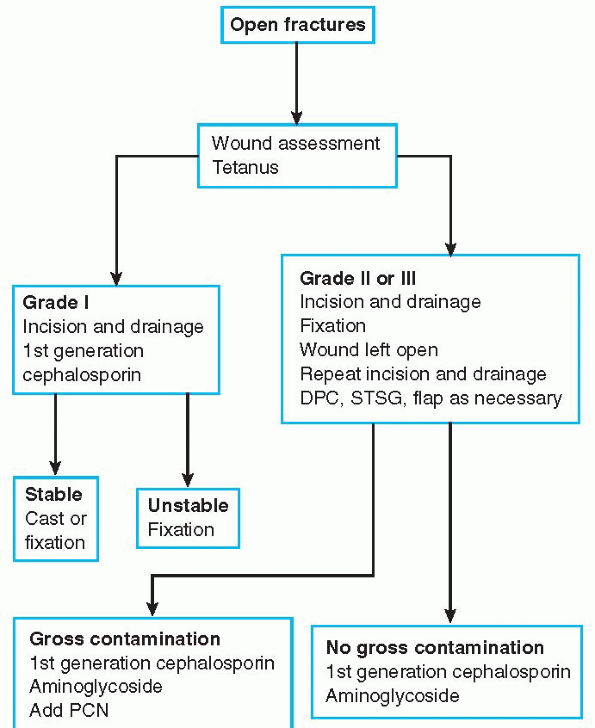
The diagnostic workup of open fractures is considered in Algorithm 14-1.
|
TABLE 14-1 CLASSIFICATION OF OPEN FRACTURES
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
 |
|
Algorithm 14-1 The diagnostic workup of open fractures in children.
|
-
Antibiotics:
-
□ Broad-spectrum cephalosporin for grade I and II injuries
-
□ Aminoglycoside added for Gram-negative coverage in grade III injuries
-
□ Penicillin or clindamycin added for severely contaminated injuries (i.e., farm injuries)
-
-
Tetanus toxoid
-
Wound coverage with sterile dressing to prevent further contamination
-
Splinting of injured extremity to prevent further soft tissue damage
-
An open fracture is a surgical emergency.
However, life-threatening injuries must be evaluated and treated first.
Operating room treatment is then considered. -
Wound margins are extended for visualization and débridement of all contaminated tissue.
-
Contaminated and necrotic tissue is thoroughly débrided and irrigated, devitalized bone is removed and the wound is left open.
-
Routine use of perioperative cultures has
not been shown to be effective and is not recommended. Primary closure
of open wounds and retention of devascularized fragments in children
are controversial and data limited, therefore a conservative course is
recommended. -
Stable fractures with minor soft tissue
injury may be splinted or casted. However, unstable fractures or those
with significant soft tissue injury benefit from operative
stabilization. -
Because children are smaller and
generally heal quickly, implants do not necessarily need to meet the
biomechanical requirements of implants used in adults. Kirschner-wires,
flexible intramedullary nails, external fixation, and small plates and
screws are commonly used. -
Delayed primary closure, split thickness
skin grafting, or free tissue transfers are performed once a stable,
clean wound is obtained. Despite the increased technical challenge of
smaller vessels in pediatric free tissue transfer, the general health
status and lack of premorbid conditions make success more likely and
excellent results have been reported.
-
While good outcomes of lower grade
injuries in most published studies dealing with open fractures in
children have been reported, the risk of complications is increased
with higher fracture grades. -
Delayed union, nonunion, infection, and compartment syndrome are all found with increasing frequency in higher grade injuries.
-
□ Delayed union is reported in 5% to 33%
of all open tibia fractures in children and nonunion rates of 0% to 16%
have been documented. -
□ Bone healing complications in open forearm fractures in children have been reported in 22% of patients.
-
□ The effect of age on delayed union and
nonunion is controversial, with some studies finding an increased rate
of delayed union and nonunion in older children.
-
-
Lawnmower injuries in children may be
devastating. Shredding injuries are associated with a high risk of
amputation and poor long-term results. -
Open physeal injuries frequently occur as a result of direct trauma and growth arrest is more likely.
-
Compartment syndrome
-
Delayed union
-
Nonunion
-
Infection
-
Limb length discrepancy
-
Angular deformity
-
Motion loss
-
The less rigid implants used and the usual activity levels of children dictate a period of immobilization and protection.P.179
-
□ Children are unlikely to develop
permanent stiffness, and immobilization to allow fracture healing
rarely compromises final range of motion. -
□ Implants are removed after fractures heal and before bony overgrowth occurs.
-
-
While physical therapy may be required in
older children or children with severe soft tissue injuries, it is
often unnecessary in young children or children with lesser degrees of
injury. -
▪ The potential for overgrowth and limb
length discrepancy in long bone fractures and growth arrest and
deformity in physeal injuries requires long-term follow-up and regular
radiographic review in children.
SL, Smith G, Sponseller PD, et al. Severe type III open fractures of
the tibia in children. J Pediatr Orthop 1996;16:627-634.
KE, Limbird TJ, Green NE. Open fractures of the diaphysis of the lower
extremity in children. J Bone Joint Surg (Am) 1992;74:218-232.
HJ, Armstrong P. The significance of peri-operative cultures in open
pediatric lower extremity fractures. Clin Orthop 1994;302:206-212.
