Lateral Epicondylitis
IV – Elbow Reconstruction > Part B – Evaluation and Treatment of
Elbow Disorders > 53 – Lateral Epicondylitis
although most likely a symptom of overuse microtrauma (a small tear) to
the common wrist extensor tendon origin, usually the extensor carpi
radialis brevis (ECRB). A commonly used term, epicondylitis
inaccurately implies an inflammatory process. Numerous pathologic
studies have confirmed vascular proliferation and focal hyaline
degeneration in surgical specimens, most likely as a result of
disrupted healing response, with fibrosis and granulation tissue
forming rather than normal tendon. Nirschl has also used the term
“angio-fibroblastic tendinosis” to describe the pathologic changes.
This process leads to progressive shortening of the tendon, which may
increase the chance of reinjury. Other authors have postulated that it
may be a degenerative process with vascular compromise and hypoxia,
similar to that found in rotator cuff pathology. A possible link to
fluoroquinolone ingestion has also been proposed. Excessive eccentric
loading may be a factor in the etiology of tendinopathy, as fewer
muscle fibers are recruited to perform the work, which increases the
stress load on each, resulting in an elevated risk for injury.
annual incidence between 1% and 3% in the general population. In one
study, which attempted to identify industries at high risk for work
related disorders of the neck, back, and upper extremity, epicondylitis
was found to be the only one in which claims increased over a
near-10-year period. Most likely the process is a cumulative one,
resulting from the use of heavy hand-held tools or a combination of
vigorous work, abnormal posture of hands and arms, and repetition. It
is also very common in the dominant extremity of a typically average
recreational athlete involved in racquet sports who may have a faulty
single-handed backhand ground stroke. The commonly used term “tennis
elbow” is unfortunately misleading, though, as only a small percentage
(5% to 10%) of patients afflicted with this disorder play at all.
extensor carpi radialis brevis–extensor digitorum communis (EDC)
complex laterally. Pathologic specimens of patients operated on for
this condition have not revealed any evidence of acute or chronic
inflammation, although in vitro analysis of painful tendons has
revealed the presence of interleukin-1 and cytokines. This molecular
inflammation cascade could be a source of pain and dysfunction. One
study in which catheters were inserted into tendons with tendinosis
showed no prostaglandin E2, a component of inflammation. Higher levels
of glutamate, a potent pain modulator in the central nervous system,
were found, though, which may also be a source of pain in tendinosis.
Although it is debatable whether radial nerve entrapment (analogous to
carpal tunnel syndrome) causes the forearm discomfort seen in many
cases of lateral epicondylitis, decompression of the posterior
interosseous nerve may also be necessary to relieve the forearm pain
and tenderness associated with lateral epicondylitis.
is poorly understood. Magnetic resonance images in patients with
lateral epicondylitis have demonstrated thickening with separation of
the ECRB tendon from the radial collateral ligament and abnormal signal
change on the T1-weighted sequences. There were no associations between
pathological signal intensity within the ECRB tendon on T1- and
T2-weighted sequences, however, and the degree of self-reported pain.
In one arthroscopic study, 31.3% of patients were noted to have a type
I lesion, characterized as fraying of the undersurface of the ECRB;
31.3% had a type II lesion noted by linear tears within the ECRB; and
37.5% had a type III lesion, consisting of a partial or complete
avulsion of the ECRB origin. Therefore, an overuse injury resulting in
progressive disruption of the tendinous origin of the ECRB may produce
an excessive inflammatory response during the healing process leading
to pain and possible swelling and compression of the posterior
interosseous nerve. If overuse of the tendon leads to the pain that
patients experience, rest should decrease symptoms. Unfortunately,
injections of the muscle with botulinum toxin, providing
temporary paralysis of the painful common extensor origin, showed no benefit over placebo.
who report insidious onset of symptoms with no clear recollection of a
traumatic event. The pain is localized to the lateral aspect of the
elbow and proximal forearm. It is typically aggravated with activities
such as lifting an object with the arm extended away from the body and
the forearm in a pronated position. Tenderness along the lateral aspect
of the elbow is present. Although rest pain is unusual, patients often
experience pain and stiffness in the morning while initially attempting
to mobilize their elbow and wrist with their daily activities.
Secondary stiffness of the elbow and wrist is uncommon, and if present,
should prompt suspicion for an underlying articular disorder.
Furthermore, any mechanical symptoms such as catching, locking,
popping, or giving way may indicate an internal derangement of the
elbow joint. Lateral epicondylitis is rare in patients in their teenage
years or younger and should prompt a more aggressive workup.
typically seen. Although swelling may be seen in a thin individual, it
is uncommon. Tenderness is typically present about 1 cm anterior and
distal to the lateral epicondyle, which is easily palpated in most
patients. Although patients may also experience tenderness in the
proximal forearm musculature, this may also indicate a coexisting
radial tunnel syndrome, particularly if the tenderness is in the area
of the radial tuberosity. Elbow motion is typically full, smooth, and
painless, although some patients with severe epicondylitis may
experience lateral elbow pain in full extension. If pain is present
with passive forearm rotation, combined with elbow flexion and valgus
stress, a radiocapitellar plica may be the cause. Elbow stability
should be assessed with a posterolateral pivot shift maneuver while the
patient is in a supine position. A careful neurologic exam should be
performed, although it is unusual to find any deficits, even in a
patient in whom radial tunnel syndrome is suspected. Pain in terminal
extension with a bounce maneuver, especially in a throwing athlete,
might be related to impingement from an olecranon spur. A common
finding in tennis elbow is pain in the region of the lateral epicondyle
during resisted extension of the middle finger (the Maudsley test).
This may be owing to disease in the EDC muscle rather than compression
of the radial nerve or disease within the ECRB. A positive chair test
may be identified if pain is exacerbated when the patient lifts a chair
with the affected arm in extension. If unilateral symptoms are present,
diminished grip strength compared with the opposite side is often
found, most likely is a reflection of painful wrist extension.
lateral epicondylitis is unclear. In one study, standard
anteroposterior, lateral, and radiocapitellar views of the elbow in
patients with a diagnosis of lateral epicondylitis demonstrated
calcification along the lateral epicondyle in 7%. In only two of the
294 sets of films did the radiographs alter management. The author
concluded that obtaining radiographs as an initial step in the
evaluation of patients with lateral epicondylitis is not necessary.
Certainly in patients who present with atypical symptoms such as night
pain and mechanical abnormalities, radiographs are recommended.
the diagnosis of tennis elbow, magnetic resonance imaging (MRI) is a
more sensitive modality to diagnose and evaluate treatment response,
although rarely necessary in my opinion. MRI of epicondylitis
demonstrates tendon thickening with increased T1 and T2 signal, but
these findings may be seen in a small minority of asymptomatic
individuals. Tears of the extensor origin may be identified, and
anconeus edema, previously demonstrated on MRI in epicondylitis, is
rarely found. Increased marrow T2 signal within the involved epicondyle
is occasionally seen. Abnormalities of the lateral collateral ligament
complex and areas of osteochondritis dissecans, which can also produce
lateral elbow pain, may also be identified with MR imaging. CT scan and
isotope bone scan may be helpful in distinguishing lateral
epicondylitis from bony tumors such as osteoid osteoma.
to manual work and high baseline pain. If modifications to reduce
physical demands during recovery cannot be realized, than operative
treatment may eventually be necessary. One concept that is important to
make the patient understand, however, is that (assuming all other
diagnostic possibilities have been excluded) lateral epicondylitis is a
condition in which pain may secondarily effect function. The surgical
solutions proposed to correct it, therefore, are elective with very
focused goals. If patients can live with their pain, or modify their
activities in such a way as to make their symptoms tolerable, then
surgery may not be advisable.
encourage healing of the abnormal tissue that produces pain. Most
successful nonsurgical treatment programs center on the concept of an
adequate, progressive rehabilitative resistance exercise program.
Nonetheless, many modalities have been described in an attempt to
hasten or improve the healing process. Unfortunately, many of these
interventions have been advocated on the merit of insufficient
evidence, contradicting results, insufficient power, short-term
follow-up, or a low number of studies per intervention. They
may,
therefore, not actually produce results superior to rest alone, which
can be expected to result in improvement in 80% to 85% of patients.
Although rest is important with respect to avoiding symptom-provoking
activities, complete rest is ill advised as muscle atrophy may begin
within 6 days of complete disuse.
commonly used nonoperative treatment modality. In one systematic review
of many studies on various modalities (laser therapy, electrotherapy,
exercises, mobilization techniques, and ultrasound), weak evidence for
efficacy was found only for ultrasound. Other studies have failed to
demonstrate any additional benefit of including phonophoresis with a
topical corticosteroid to ultrasound. With strengthening, eccentric
contraction should be emphasized. Eccentric strengthening may help to
heal tendinopathies by stimulating mechanoreceptors and tenocytes to
produce collagen. Animal experiments have shown that eccentric loading
improves tendon collagen alignment and simulates formation of collagen
cross-linkage to improve tensile strength. In addition, tendon cells
respond to an eccentric mechanical load by up-regulation of gene
expression for synthesis of collagen proteins. One large Dutch
randomized, controlled study found that, after 12 months, the success
rate in the physiotherapy group (91%) was significantly higher than an
injection group (69%), but only slightly higher than in a
“wait-and-see” group (83%).
Overload of the wrist extensors, which is considered to be a major
pathogenic factor in lateral epicondylitis, has been shown to be
reduced by braces. Forearm/hand splints are not more effective than
elbow bands as a treatment for lateral epicondylitis, and currently no
definitive conclusions can be drawn concerning the effectiveness of
orthotic devices for lateral epicondylitis.
anti-inflammatory medications (NSAIDS), despite the growing evidence
that the condition is noninflammatory. Nonetheless, these medications
may be helpful in decreasing the level of pain, at least in the short
term, but must be weighed against the risks of gastrointestinal adverse
effects. There is also evidence that topical NSAIDS are similarly
effective in the short term, and without the gastrointestinal risks.
These compounds can typically be produced at many pharmacies or
apothecary shops. A direct comparison between topical and oral NSAID
has not been made, though. Some authors have expressed concern,
however, as NSAIDS may inhibit the inflammatory response necessary for
tissue repair. One study demonstrated that when NSAIDS were compared
with placebo, tendon strength was reduced at 28 days.
corticosteroid injections providing only short-term relief at best,
lateral epicondylitis is the most common extra-articular use for
corticosteroid injections by orthopedic surgeons. A meta-analysis
review found superior short-term effects of corticosteroid injections
for lateral epicondylitis, but it was not possible to draw firm
conclusions on the effectiveness of injections owing to the lack of
high-quality studies. No beneficial effects were found for intermediate
or long-term follow-up. Other authors have reported on the use of an
injection of autologous blood, felt to possibly provide the necessary
cellular and humoral mediators to induce a healing cascade, with a
reported 80% success rate. A double-blind, randomized, controlled trial
comparing injections of botulinum toxin type A with those of a placebo
(normal saline solution) in the treatment of chronic tennis elbow
failed to find a significant difference between the two groups.
Acupuncture also may provide improved pain relief in the short term
when compared with placebo, but no clear long-term benefit has been
demonstrated.
shock wave therapy as an alternative treatment for chronic lateral
epicondylitis of the elbow. The mechanism of action of shockwave
therapy is not fully understood but may stimulate the healing process
of damaged tendons and encourage revascularization, release of local
growth factors, and the recruitment of appropriate stem cells to the
area. Although some studies comparing low-dose or low-energy shockwave
therapy with sham treatment demonstrated improvement in pain scores,
most other studies have failed to demonstrate a clear benefit of this
treatment modality.
of lateral epicondylitis have shown that surgical intervention is
necessary in only 5% to 10% of patients. Only those patients with
persistent or recurrent local pain and muscle weakness, nonresponsive
to conservative measures for at least 6 months, should be considered
for surgery. Symptoms of radial tunnel syndrome can resemble those of
tennis elbow and result from compression of the radial nerve by the
free edge of the supinator muscle or closely related structures in the
vicinity of the elbow joint. It can be difficult to objectively
differentiate these two disorders, and they may often occur
simultaneously. Radial tunnel syndrome should be strongly considered in
patients who have failed to respond to previous extensor release or
debridement. Differential diagnostic injections can be helpful in
distinguishing these two problems or confirming the presence of both.
The first injection is given at the point of maximal tenderness, near
the lateral epicondyle typically 1 cm anterior and 1 cm proximal with 3
to 4 mL of 1% plain lidocaine. After 5 to 10 minutes have elapsed, the
patient is re-examined, and if pain is eliminated with provocative
maneuvers (resisted wrist extension). and tenderness over the radial
tuberosity region is diminished, then a diagnosis of lateral
epicondylitis alone is appropriate. If, however, pain and tenderness
persists, an injection is given toward the radial tuberosity with the
forearm in supination with a long 25- or 27-gauge needle (Fig. 53-1).
Once the needle strikes bone, it is redirected anteriorly and 10 mL of
1% plain lidocaine (a reasonable volume of local anesthetic is
important) is injected. After 10 minutes, the patient is re-examined
and if a posterior interosseous nerve palsy has been produced and pain
is relieved, a posterior interosseous nerve decompression is included
in the surgical plan. If pain persists following both injections,
suspicion is raised for intra-articular pathology such as degeneration
of the orbicular ligament or a redundant synovial fold, in which case a
confirmatory intra-articular injection can be
performed. This is particularly helpful in patients who have failed previous surgery for lateral epicondylitis.
case the patient is placed in the supine position with an arm board. If
there is any suspicion of instability or intra-articular pathology, an
examination under anesthesia is included, as well as a possible
arthroscopy. The presence of a palmaris longus is confirmed, or
alternate graft choices are discussed with the patient in advance
 |
|
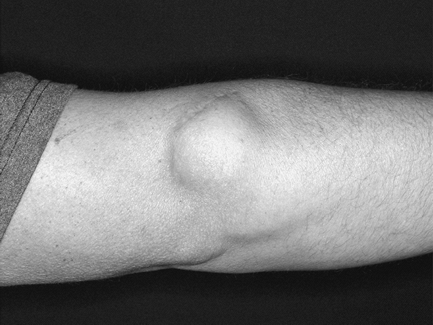
Figure 53-1
With the forearm in supination, a fine gauge (1.5 in.) needle is directed anterior to the radial tuberosity in this patient with persistent pain after a previous open release of the extensor origin (surgical scar marked with indelible pen depicted by solid black arrow) suspected of having radial tunnel syndrome. |
and has a significant advantage of cost savings. Local anesthetic is
injected at the point of origin of the ECRB. An 11 blade is then used
to release the extensor origin from the epicondyle. The goal is to
achieve about a 1-cm distal muscle slide to a new resting length.
Immediate motion is allowed in a soft dressing. A more popular
technique involves excising the abnormal tissue through an open
incision, which I prefer to perform under a Bier block anesthetic. A
longitudinal split is made between extensor carpi radialis longus
(ECRL) and EDC tendons. After elevating the origin of the ECRL, the
grayish-yellow pathologic tissue in the origin of the ECRB has a
distinct fish-flesh appearance and consistency in contrast to the
normal glistening longitudinal tendinous tissue (Fig. 53-2).
It is excised in an elliptical fashion, with care taken to avoid injury
to the underlying lateral collateral ligament. The underlying lateral
epicondyle is then excoriated with a curette, and a small drill is used
to create some channels for bleeding to promote scar and healing. One
randomized double-blind comparative prospective trial has shown,
however, that drilling conferred no benefit and actually caused more
pain, stiffness, and wound bleeding than not drilling.
with absorbable sutures to prevent a synovial cutaneous fistula from
developing postoperatively (Fig. 53-3). The
defect in the extensor tendon is then reapproximated. A soft,
compressive dressing is applied and immediate gentle range of motion is
encouraged. Alternatively, complete release of the extensor mechanism,
debridement of abnormal tissue, with reattachment of the extensor
origin back to lateral epicondyle out through drill holes can be
performed. A V-Y lengthening, or slide, of the common extensor origin
has also been described with good results. One must limit lifting and
activities for 6 weeks following these latter two procedures to prevent
detachment of the extensor origin in the postoperative period. In
patients with persistent pain requiring revision surgery, or in whom a
synovial cutaneous fistula has developed after a previous release, a
wider debridement of the extensor origin may be performed with coverage
using a vascularized rotational pedicle flap of the anconeus muscle.
 |
|
Figure 53-2 Intraoperative photograph of a patient with refractory epicondylitis. Solid black arrow depicts area of tendon degeneration; open arrow depicts longitudinal rent in extensor carpi radialis brevis (ECRB) tendon.
|
 |
|
Figure 53-3
Patient with a persistent subcutaneous synovial fluid collection after extensor origin debridement and arthrotomy, in whom the joint capsule was not repaired. |
a popular technique. This is accomplished using proximal medial and
proximal lateral portals. It has an added advantage of addressing any
intra-articular pathology, which has been reported in 19% to 70% of
patients. Baker et al. have classified the arthroscopic appearance of
these lesions as follows: type 1, a normal-appearing undersurface of
the capsule; type 2, a horizontal rent in the capsule; or type 3,
complete rupture of the capsule with exposure of the ECRB tendon. The
capsule is removed to allow visualization of the origin of the extensor
muscles and tendon. The debridement is then performed from proximal to
distal and is complete when all visible abnormal tissue is excised,
exposing muscle fibers with a healthy appearance. Elbow stability is
not compromised as long as resection does not extend posteriorly to an
intra-articular line bisecting the radial head. Contraindications to
arthroscopic debridement include significant calcific tendonitis,
previous ulnar nerve transposition since visualization must be from the
medial side (proximal-medial portal), and significant ankylosis, which
may lead to inadequate joint distention and an increased risk of
vascular injury because of inadequate displacement from the portal site
from incomplete distention. Denervation (Wilhelm technique) has also
been reported as an effective method for relieving pain, and is
accomplished blindly by detachment of certain muscles, as well as
simultaneous indirect decompression of the posterior interosseous nerve.
release of the lateral collateral ligament, as this structure is
confluent with the origins of the ECRB and EDC. When performing a
percutaneous release, the surgeon should keep a thumb over the
posterolateral aspect of the radiocapitellar joint to avoid extension
of the scalpel. If a posterior interosseous nerve decompression is
performed, direct injury or neurapraxia, particularly involving
branches to the EDC, is possible. One must keep in mind during an
arthroscopic release that cadaveric studies have demonstrated varying
courses of the lateral and posterior antebrachial nerves, which place
these superficial sensory nerves at risk during portal placement. The
radial nerve is also about an average of 5 mm from the proximal lateral
portal. Painful neuromas of the posterior antebrachial nerve have also
been reported after open releases and can be treated with neuroma
resection and implantation of the nerve proximally into the
brachioradialis muscle. Synovial cutaneous fistulas can result if the
capsule has been violated to a significant degree and not repaired
sufficiently. Heterotopic ossification after lateral epicondylectomy,
although rare, has also been reported.
pain are limited by methodologic weaknesses in selection and definition
of the study population, length of follow-up, and analysis of
prognostic factors. Outcome scores, such as proposed by Roles and
Maudsley or DASH (Disabilities of the Arm, Shoulder, and Hand), are not
routinely used, and even objective data such as grip-strength
measurements with an extended elbow are seldom reported. Systematic
reviews of interventions have confirmed that there is a surprising lack
of published controlled trials of surgery for lateral elbow pain.
Without a control group, it is very hard to draw any conclusions about
the effectiveness of a given modality of treatment, since the natural
history of the syndrome is uncertain.
debridement or releases ranges from 78% to 97%, 91% to 96% after
percutaneous releases, and 85% to 90% after denervation. Reported rates
involving return to work average about 5 weeks following open, 9 to 21
days for percutaneous, and 6 to 15 days after arthroscopic releases.
When reported, grip-strength improvements range from 30% to 100%, with
a good result considered >90% compared with the uninvolved side. One
prospective, randomized, controlled trial comparing formal open release
with percutaneous tenotomy showed significant improvements in patient
satisfaction, time to return to work, the DASH score, and sporting
activities in the percutaneous group. In another retrospective
comparison, 69% of open cases and 72% of arthroscopic cases had good or
excellent outcomes. Patients treated with arthroscopic release returned
to work earlier than patients treated with open release did, and they
required less postoperative therapy. Poorer results have been reported
in patients seeking compensation.
CL Jr, Murphy KP, Gottlob CA, et al. Arthroscopic classification and
treatment of lateral epicondylitis: two-year clinical results. J Shoulder Elbow Surg. 2000;9:475–482.
JP, Andersen JH. Prognostic factors in lateral epicondylitis: a
randomized trial with one-year follow-up in 266 new cases treated with
minimal occupational intervention or the usual approach in general
practice. Rheumatology (Oxford). 2003;42:1216–1225.
MJ, Santini AJ, Hughes PJ, et al. Botulinum toxin injection in the
treatment of tennis elbow. A double-blind, randomized, controlled,
pilot study. J Bone Joint Surg Am. 2005;87:503–507.
H, Guibert R, Joncas J, et al. Lack of scientific evidence for the
treatment of lateral epicondylitis of the elbow. An attempted
meta-analysis. J Bone Joint Surgery Br. 1992;74:646–651.
