Medial Epicondylitis
IV – Elbow Reconstruction > Part B – Evaluation and Treatment of
Elbow Disorders > 54 – Medial Epicondylitis
understood condition. It is frequently referred to as “golfer’s elbow.”
There have been few studies with proper design methodology or power to
scientifically delineate definitive treatment requirements. Medial
epicondylitis is perhaps the most common cause of medial elbow pain.
The term epicondylitis is really a
misnomer because there is minimal histologic evidence of inflammatory
disease. It most likely is a tendinosis, i.e., a degenerative condition
of the tendon. This tendinosis appears to be a failure of tendon
healing in the face of continual microtrauma. The diagnosis can be
difficult and may be found in conjunction with ulnar neuropathy at the
elbow.
is a repetitive overuse or stressing of the flexor pronator mass
musculature resulting in microtrauma. Degenerative changes involving
the musculotendinous unit of the medial epicondyle appear to be brought
about by a chronic repetitive concentric and eccentric loading of the
flexor pronator musculature. These repetitive eccentric and concentric
contractions load the muscle and tendon, causing microtrauma. These
microtears fail to heal and can build up over time. The degenerative
changes are usually seen in the pronator teres as well as the flexor
carpi radialis muscles. A single traumatic event such as a direct blow
or sudden-overload eccentric contraction can result in the development
of epicondylitis; however, the repetitive overuse theory is usually
attributed as the main cause. Activities that require repetitive
forearm pronation as well as wrist flexion have been associated with
causing medial epicondylitis.
golf, tennis, baseball, racquetball, bowling, football, archery,
javelin throwing, and weight lifting. However, this is not just an
athletic-type injury; some occupations require significant physical
activity. For example, butchers, carpenters, and plumbers are at
potential risk because of the repetitive forearm pronation and wrist
flexion involved with their occupations. It is thought that overload
from extrinsic valgus stresses and intrinsic muscular contractions can
predispose the flexor pronator mass musculature to injury and
accumulative microdegenerative trauma involving the pronator teres,
flexor carpi radialis, and occasionally the flexor carpi ulnaris. Most
commonly what is seen is a microtear in the interface between the
pronator teres and the flexor carpi radialis origins with subsequent
development of fibrotic granulation tissue.
frequently than its lateral counterpart, lateral epicondylitis. The
predominant age groups affected are fourth and fifth decades although
almost any age group can potentially be affected. However, it has not
been described in children. Male and female prevalence appears to be
equal in most studies. Other studies have suggested a 2:1
male-to-female ratio. Approximately 75% of patients are usually
symptomatic in their dominant extremity. Approximately 30% of patients
describe the pain being associated with an acute injury. Most patients,
roughly 70% of cases, describe a much more insidious onset of their
symptoms. Almost half of all cases will have some ulnar nerve symptoms
associated with them. Other conditions commonly seen in patients with
medial epicondylitis include an approximately 30% rate of prior history
of lateral epicondylitis, a 25% rate of history of carpal tunnel
syndrome, and a 20% rate of prior rotator cuff tendinosis. In younger
patients other causes of epicondylar pain should be ruled out prior to
considering this degenerative condition more commonly seen in
middle-aged adults. Other literature has suggested no predilection for
the dominant hand or between genders.
were posed and postulated in inflammatory conditions that involved
bursa, periosteum, synovium, and ligaments. The recent literature has
discounted these theories, and the
histologic
analysis of Nirschl and Pettrone has demonstrated normal collagen and
architecture disrupted by fibroblastic immature vascular response as
well as an incomplete reparative process. Importantly, there is a lack
of acute and chronic inflammatory cellular architecture. In the very
early stages of medial epicondylitis, there may be some inflammatory or
synovitis-type patterns present. However, more definitively in the
later stages there is evidence of microtearing with tendon
degeneration, with or without calcification, and failure to complete a
neovascular healing response. The pathologic tissue appears grossly
friable and has a gray to tannish color.
“angiofibroblastic hyperplasia” to describe such structural changes.
Nirschl has described four stages of epicondylar tendinosis. In stage
one there is generalized inflammation that can recede. In stage two the
injury is noted to have pathologic tissue changes of the
angiofibroblastic type. Stage three is noted to have degeneration that
results in structural failure. Finally, stage four can include
components of stages two and three but is also accompanied by marked
fibrosis or calcifications. The exact pathophysiology of medial
epicondylitis has not yet been established. It is agreed that the
injury results from microtearing of the tendon origin at the epicondyle
with failure of the usual reparative processes to mount a response. The
subsequent tendon tearing and degeneration changes the usual
musculotendinous biomechanics of the elbow, resulting in the pain and
dysfunction seen clinically.
medial epicondylitis based on the presence and severity of concomitant
ulnar neuropathy at the elbow. In their classification system, type 1A
includes patients without any associated ulnar nerve symptoms. Type 1B
has mild ulnar nerve signs or symptoms. In the type 2 medial
epicondylitis patient, there are moderate or severe ulnar nerve
symptoms with objective deficits noted on the physical exam as well as
denervation noted on electromyography.
come from various situations. Some are from the workplace and have an
environment that is consistent with repetitive activity. Others relate
it to being problematic with their athletic endeavors. When obtaining
the history, it is useful to divide patients based on the manner of
onset, provocative activities, localization of pain, and severity of
discomfort. Other specific characteristics to specifically ask about
include onset of pain with the date, time, and activity being
performed. For example, a golfer may recall a missed hit striking the
ground with the club that resulted in a sudden deceleration, or the
tennis player or racquetball player may remember a specific extra-hard
hit or serve that resulted in pain about the medial aspect of the
elbow. Is the patient able to localize the pain with one specific
finger to the medial epicondylar region or is he or she vague in where
the symptoms are located? Are symptoms better with rest and reproduced
with certain provocative activities? Do they have other areas of
significant pain about the upper extremity or neck or is it again
specifically localized to the medial epicondylar region? Is worker’s
compensation or other potential secondary gain involved? Do they
describe numbness and tingling in an anatomic or in a nonanatomic
distribution?
mechanically based in that the pain is exacerbated or reproduced by the
stress and strain of the wrist flexors and forearm pronators on the
medial side. Otherwise other conditions need to be considered (Table 54-1).
The most important injuries to exclude when evaluating a patient with
medial epicondylitis involve, again, the amount of ulnar nerve
involvement and any type of injury to the medial collateral ligament.
In overhead throwing athletes, this can be a challenging differential.
One technique for trying to differentiate medial tendon injury from
medial collateral ligament insufficiency is by placing a valgus force
to a slightly flexed elbow with the wrist in volar flexion and the
forearm pronated. This test usually does not elicit pain or demonstrate
laxity if the diagnosis is medial epicondylitis only. Other
considerations to think about are lower cervical radiculopathies
involving C7 through T1 that may cause radiating pain along the medial
aspect of the upper extremity.
patient relaxed and sitting. The patient frequently is able to help
identify the tenderest spot. Classic findings consist of exquisite and
repeatable localization of medial epicondylar tenderness with
palpation. Some patients may have maximal tenderness just distal to the
epicondylar region in the proximal flexor pronator mass. The medial
pain can be exacerbated with resisted pronation and flexion of the
wrist. The usual physical exam shows some tenderness over the anterior
aspect of the medial epicondyle. More than 90% of patients will have
pain with resisted pronation and more than 70% pain with resisted wrist
flexion. Wrist and elbow range of motion are typically normal. Local
injection of lidocaine or Marcaine results in near complete
obliteration of the discomfort.
including the Tinel sign over the ulnar nerve in the region of the
elbow, an elbow flexion test, ulnar nerve compression test, and
checking the ulnar nerve for subluxation about the medial epicondyle (Table 54-2)
Distally, function of the ulnar nerve needs to be assessed with
two-point discrimination in intrinsic strength and dorsal cutaneous
nerve status. Other things to check for include the cervical spine to
rule out a radiculopathy. The skin about the elbow should be inspected.
Palpation about the biceps insertion, brachialis, and lacertus needs to
be performed. The triceps insertion and olecranon should also be
palpated. Kurvers and Verhaar have noted that in their patient series,
approximately 20% of patients with medial epicondylitis for >12
months had flexion contractors ranging from 10 to 25 degrees.
Furthermore, 15% of their patient population had decreased active
supination range of motion by 5 to 15 degrees. Occasionally local
swelling and warmth may be present.
|
TABLE 54-1 Medial Elbow Pain Differential Diagnosis
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
TABLE 54-2 Ulnar Nerve Transposition Indications in Patients with Medial Epicondylitis
|
||||||
|---|---|---|---|---|---|---|
|
epicondylitis are usually normal. Approximately 20% to 25% of patients,
however, may have some soft tissue calcification in the proximity of
the medial epicondyle. Other patients, especially throwing athletes,
may have ulnar-sided traction spurs and medial collateral ligament
calcifications. Radiographs are also useful to rule out associated
conditions such as osteoarthritis as well as medial instability with
valgus stress views (if medial instability is suspected). An MRI
arthrogram can be helpful in differentiating medial collateral ligament
injury from medial epicondylitis. Other findings potentially seen on
radiographs are loose bodies, radiocapitellar and ulnar trochlear
arthritis, olecranon or coronoid impingement. In trying to
differentiate calcification to the medial tendon from the medial
collateral ligament, it should be noted that the calcifications in the
medial tendon are usually relatively superficial whereas those in the
medial collateral ligament are deep to the flexor pronator mass.
useful in cases where ulnar neuropathy is suspected clinically. This
can be used to document the severity of axonal changes. This can also
be used to show nerve conduction slowing in an absolute or relative
fashion compared with other nerves or the other side. The author’s
preference is to obtain electrodiagnostic studies with nerve conduction
velocities as well as electromyographic analysis. Surgical outcome can
be compromised by failing to address the ulnar neuropathy (Table 54-2).
In obtaining the MRI, make sure that the facility to be used has the
appropriate coils and imaging protocols as well as technical knowledge
to adequately evaluate the elbow; otherwise the study will be for
naught.
flexor pronator origin; this is at the anterior medial epicondyle. The
pronator teres originates in part from the superior interior medial
epicondyle; however, its main origin is from an intramuscular tendon
otherwise known as the medial conjoint tendon. In going from the radial
to ulnar aspect of the forearm, the musculature includes the pronator
teres, the flexor carpi radialis, the palmaris longus, the flexor
digitorum superficialis, and the flexor carpi ulnaris. The pronator
teres and flexor carpi radialis tendon and muscles are most afflicted
with the alteration of stretching and acceleration during throwing and
swinging.
the medial conjoint tendon and its associated pronator teres and flexor
carpi radialis origins. The medial conjoint tendon serves as the
landmark for the surgical excision of the pathology as well as a way to
identify and avoid the anterior oblique ligament. Medial conjoint
tendon arises from the anterior inferior epicondyle with an oblique
parasagittal orientation that traverses approximately 12 cm into the
proximal forearm. Any surgical dissection and elevation off the medial
epicondyle posterior to the medial conjoint tendon will violate the
anterior oblique ligament of the medial collateral ligament.
of the flexor pronator mass resulting in a flexion contracture.
Frequently 50% of these individuals will have some type of flexion
contracture and 30% will have an increased valgus angle compared with
their contralateral extremity. Of note, though, is that these features
have never been correlated with the recurrence of medial epicondylitis.
The ulnar nerve transverses posteromedially about the medial
epicondyle. Also, the medial antebrachial cutaneous nerve passes in
this zone. Occasionally the triceps can snap over the medial epicondyle
causing pain that is not related to medial epicondylitis, and this is
known as a snapping triceps syndrome.
epicondylitis. The purpose of this nonsurgical care is to relieve pain
and allow sufficient rehabilitation so that the
patient
can return to the previous activities. Current literature suggests that
roughly 5% to 15% of patients suffer recurring episodes of medial
epicondylitis. However, this may represent incomplete rehabilitation or
premature termination of the rehabilitative program. The initial
nonoperative treatment usually consists of rest, ice, nonsteroid
anti-inflammatories, local modalities, splinting, and cortisone
injections. The author’s preference for cortisone injection consists of
a water-soluble corticosteroid mixed with 2 mL of half percent plain
bupivacaine.
 |
|
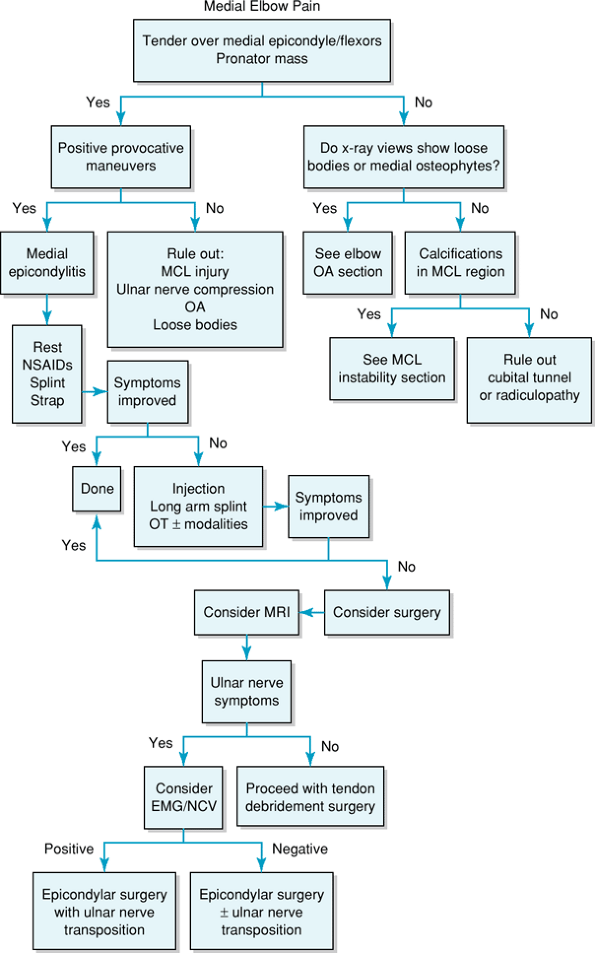
Figure 54-1
Algorithm for patient evaluation and treatment. MCL, medial collateral ligament OA; osteoarthritis; NSAIDs, nonsteroidal anti-inflammatory drugs; MRI, magnetic resonance imaging; EMG/NCV, electromyogram/nerve conduction velocity. |
The bupivacaine should substantially reduce the pain and this should
last for several hours. If the patient does not notice any relief from
the symptoms or minimal relief from the symptoms, then it is unlikely
the diagnosis is epicondylitis, assuming the injection was placed in
the proper location.
Most
cases of medial epicondylitis do benefit from the initial injection,
and this can last several months. However, repeat injections tend to
have a decreasing benefit. When performing an injection about the
medial aspect of the elbow for medial epicondylitis, care needs to be
taken to make sure the ulnar nerve is palpated and that the needle is
directed away from the cubital tunnel. I prefer to do the injection
with the elbow extended and the thumb of my nondominant hand over the
cubital tunnel.
is of sudden onset and severe. Usually a cock-up wrist splint resting
the wrist at approximately 10 degrees of extension is adequate. In
combination with the previously mentioned items, a 2-week course of
oral nonsteroid anti-inflammatories may also be helpful. A medial
counterforce brace can also be helpful for some patients, and the pad
of the brace needs to be anteromedial on the flexor pronator mass but
not medial or posterior medial over the ulnar nerve. If ulnar nerve
symptoms are exacerbated, the brace should be discontinued.
program can be initiated. This part of the rehabilitation starts with
wrist flexor and forearm pronator stretching and progressive isometric
exercises. Provocative activities, however, need to be avoided until
predisease strength is restored. Eccentric and concentric resistive
exercises are added once the flexibility, strength, and endurance of
the patient have improved adequately to tolerate the program. Success
rates of this combined approach range between 70% and 90%. The use of
modalities such as ultrasound and iontophoresis may help some patients
with their symptoms. However, there is no strong evidence in the
literature to support widespread use of one modality over another, and
no studies have shown modalities to provide prolonged long-term benefit.
relief of the patient’s symptoms the patient finds recurrence of the
symptoms inhibiting function of daily activities, then these patients
can be considered for surgical intervention. Patients with continued
minor or intermittent symptoms whose hobbies such as tennis or golf are
bothered but are not incapacitated in their activities of daily living
are marginal candidates for surgery. Contraindications to surgery would
be those patients who medically could not tolerate the surgery. The
other candidate obviously would be those patients who received no
benefit, even temporary, from an injection and are not able to
demonstrate or localize the pain to the medial epicondyle.
from surgery and it is rare for anyone to achieve 100% improvement.
Certainly strenuous or provocative activities that brought the symptoms
on before can still bring the symptoms on postoperatively. A rough rule
to give patients in counseling them about surgery is that 80% of
patients see 80% improvement in their symptoms. The author prefers to
try a minimum of 6 months of nonoperative treatment prior to
considering surgical intervention. Some authors recommend MRI or MRI
arthrogram as part of the preoperative planning to rule out any
concomitant pathology, to evaluate the condition of the tendons prior
to surgery, and to help focus on where the pathology may be present.
However, by no means is MRI mandated; this is a diagnosis that is made
clinically and not by imaging studies.
percutaneous epicondylar release and epicondylectomy; however, the
standard surgical treatment at this time consists of debridement of the
degenerative nidus in the tendon. This can be summarized as excising
the pathologic portion of the tendon, trying to enhance local
vascularity to promote healing, performing stout reattachment of any
elevated tissues to the medial epicondyle, repairing any tissue
defects, and surgically decompressing the ulnar nerve and
reconstructing the ulnar collateral ligament if needed. Nirschl and
Pettrone have performed a debridement of abnormal tendon tissue through
a longitudinal split of the medial tendon complex. The diseased tendon
can be identified and excised in an elliptical fashion. The tendon
origin is not disrupted.
greater exposure of the flexor origin and facilitated a complete
debridement. They used a curvilinear incision at the medial elbow
centered at the medial epicondyle. The interval between the pronator
teres and flexor carpi radialis is then identified. The medial tendon
is incised along the interval in the common flexor origin and is
reflected directly off the epicondyle with sharp dissection. The medial
collateral ligament is exposed but not disturbed. Any diseased and
abnormal tissue is sharply excised, and the epicondyle is prepared with
a rongeur to remove fibrous tissue. Small holes can be drilled in the
medial epicondyle that create a vascular bed. Care needs to be taken to
avoid entrapping any soft tissue around the drill. The common flexor
origin is then reattached to the bleeding bone surface with interrupted
stitches. Morrey describes his type 1A cases as requiring epicondylar
debridement only, whereas type 1B cases require debridement with or
without cubital tunnel decompression or transposition. Finally, his
type 2 cases receive debridement with submuscular transposition of the
ulnar nerve.
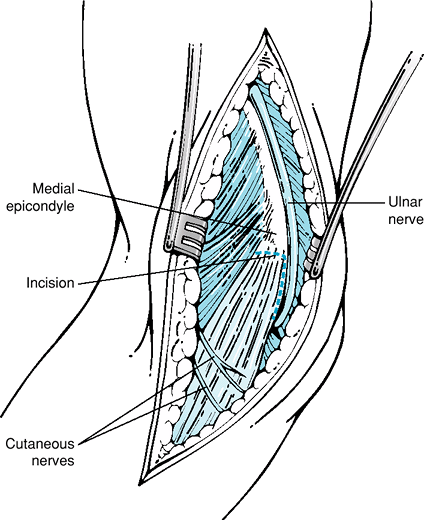
medial epicondyle. I usually apply a sterile tourniquet and use an arm
board. The medial antebrachial cutaneous nerve and its branches are
identified. The incision may be easily enlarged if ulnar nerve
transposition is to be considered. The common flexor pronator origin is
found along with the ulnar nerve, which is protected. Usually an
incision to the pronator teres and flexor carpi radialis interval is
developed longitudinally (Fig. 54-2). This
exposes the medial conjoint tendon. Again, care must be taken along the
posterior aspect of the medial conjoint tendon because that is where
the anterior oblique ligament lies. The degenerative tissue is then
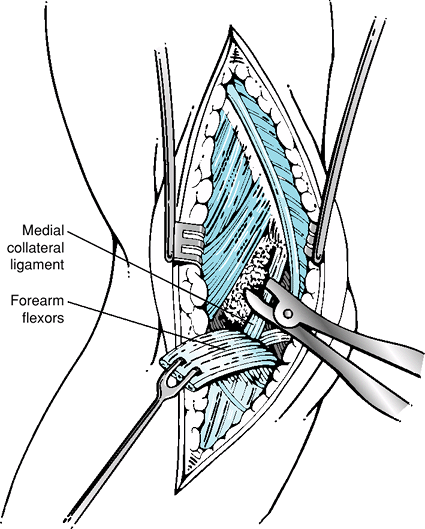
debrided with a rongeur as seen in Figure 54-3. The flexor pronator fascia is then repaired back to the retained rim
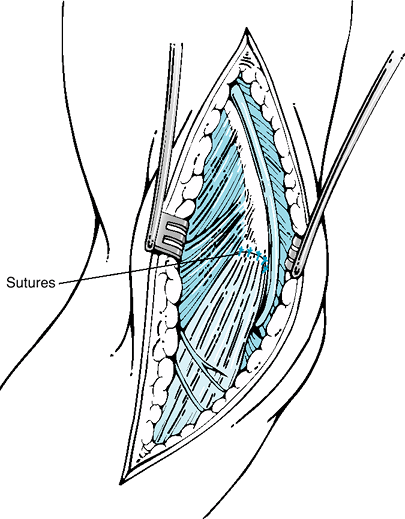
of fascia at its original position or in a slightly lengthened position
but not by more than >1 cm. The flexor pronator origin can be
reattached to the bleeding bony surface with either interrupted sutures
or through drill holes or with the attached adjacent flexor pronator
origin (Fig. 54-4).
 |
|
Figure 54-2
Anatomy and exposure of the medial epicondyle. Note the medial conjoint tendon, anterior oblique ligament, and medial antebrachial cutaneous nerve branches. |
 |
|
Figure 54-3 Note reflection of forearm flexors and debridement of degenerative tissue with a rongeur.
|
 |
|
Figure 54-4 The common flexor tendon is then reattached with interrupted sutures, creating a secure closure.
|
that is applied to the elbow and wrist with the elbow at 90 degrees of
flexion and the forearm in neutral rotation. At approximately 10 days
postoperatively, the splint is removed and any skin sutures are
removed. At this point gentle passive and active nonresistive range of
motion exercises are begun for the hand, wrist, and elbow. Gentle
isometric exercises are usually begun at 3 to 4 weeks postoperatively.
Finally at 6 weeks, more aggressive resistant wrist flexion and forearm
pronation are begun. Finally the progressive strengthening program is
initiated. A gradual careful return is encouraged. Total body and
extremity conditioning is encouraged throughout the entire
rehabilitative process. The average return for most patients to their
regular activities is 3 to 6 months postoperatively. However, in some
series this has been anywhere in the range from 3 to 24 months.
nerve with subsequent neuromas around the incision site. Other
complications involve injury to the ulnar nerve. Ulnar neuritis after
surgery is not uncommon for a short period of time. Scarring along the
cubital tunnel can lead to ulnar nerve symptoms developing
postoperatively. Medial collateral ligament injury can destabilize the
elbow and result in new symptoms that were not present preoperatively.
Excessive release and debridement of flexor fascia without careful
repair can lead to permanent flexor weakness. After surgery hematoma
formation can result, causing discomfort. Patients should be warned
about numbness around the incision area as well as potential numbness
in the forearm. The other potential complication of course relates to
failure to obtain improvement in the patient’s preoperative symptoms.
medial epicondylitis. Types 1A and 1B have roughly ≥90% good or
excellent results as reported in two studies and have slightly lower
rates in another two studies. Two thirds of patients can take ≤6 months
to obtain the good to excellent level, whereas the remaining third may
take up to ≤2 years. Type 2 with its associated ulnar nerve neuropathy
has a poorer prognosis. The results of type 2 medial epicondylitis are
related to the failure of the ulnar neuropathy to respond to the
surgical treatment. Cubital tunnel release alone as treatment for type
2 medial epicondylitis has been shown to be suboptimal. Vangness and
Jobe have reported the results of their surgical intervention with 86%
of patients having no limitation in use of the elbow. In their study,
isokinetic and grip-strength testing revealed no significant functional
loss. Gabel and Morrey have reported similar success rates after
surgical treatment of medial epicondylitis, but again found ulnar
neuropathy to be correlated with a poor prognosis. Using Nirschl
debridement technique Ollivierre et al. analyzed 50 cases of
intractable medial epicondylitis and found partial or complete pain
relief in all patients. Yet, one quarter of these patients were not
able to return to painfree participation after surgery.
enigmatic and problematic disease until surgeons have a better
understanding of the failure of the reparative mechanisms by which this
degenerative condition occurs. Nonoperative management remains the
mainstay of treatment, but surgical intervention is warranted in those
patients who fail nonoperative treatment and can no longer tolerate the
effect of their symptoms on their activities of daily living. Most
patients will have improvement in their symptoms after surgery.
