Pediatric Wrist and Hand
-
Rare, although carpal injuries may be
underappreciated owing to difficulties in examining an injured child
and the limited ability of plain radiographs to detail the immature
skeleton. -
The adjacent physis of the distal radius
is among the most commonly injured; this is protective of the carpus as
load transmission is diffused by injury to the distal radial physis,
thus partially accounting for the rarity of pediatric carpal injuries.
-
The cartilaginous anlage of the wrist
begins as a single mass; by the tenth week, this transforms into eight
distinct masses, each in the contour of its respective mature carpal
bone. -
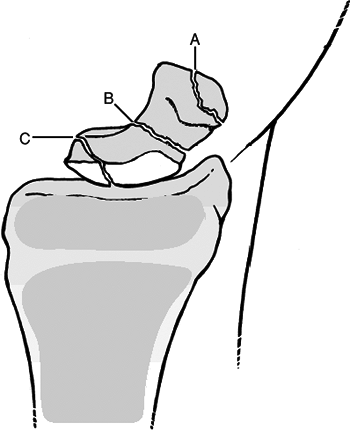
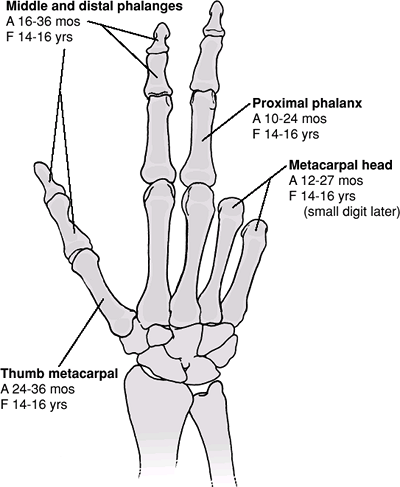
The appearance of ossification centers of
the carpal bones ranges from 6 months for the capitate to 8 years of
age for the pisiform. The order of appearance of the ossification
centers is very consistent: capitate, hamate, triquetrum, lunate,
scaphoid, trapezium, trapezoid, and pisiform (Fig. 46.1). -
The ossific nuclei of the carpal bones
are uniquely protected by cartilaginous shells. As the child matures, a
“critical bone-to-cartilage ratio” is reached, after which carpal
fractures are increasingly common (adolescence).
-
The most common mechanism of carpal injury in children is direct trauma to the wrist.
-
Indirect injuries result from falls onto
the outstretched hand, with consequent axial compressive force with the
wrist in hyperextension. In children, injury by this mechanism occurs
from higher-energy mechanisms, such as falling off a moving bicycle or
fall from a height.
-
The clinical presentation of individual
carpal injuries is variable, but in general, the most consistent sign
of carpal injury is well-localized tenderness. In the agitated child,
however, appreciation of localized tenderness may be difficult, because
distal radial pain may be confused with carpal tenderness. -
A neurovascular examination is important,
with documentation of distal sensation in median, radial, and ulnar
distributions, appreciation of movement of all digits, and assessment
of distal capillary refill. -
Gross deformity may be present, ranging from displacement of the carpus to prominence of individual carpal bones.
 |
|
Figure
46.1. The age at the time of appearance of the ossific nucleus of the carpal bones and distal radius and ulna. The ossific nucleus of the pisiform (not shown) appears at about 6 to 8 years of age. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Anteroposterior (AP) and lateral views of the wrist should be obtained.
-
Comparison views of the uninjured, contralateral wrist may be helpful.
-
The scaphoid is the most commonly fractured carpal bone.
-
The peak incidence occurs at age 15
years; injuries in the first decade are extremely rare, owing to the
abundant cartilaginous envelope. -
Unlike adults, the most common mechanism
is direct trauma, with extraarticular fractures of the distal one-third
the most common. Proximal pole fractures are rare and typically result
from scapholunate ligament avulsion. -
Clinical evaluation: Patients present with wrist pain and swelling, with tenderness to deep palpation overlying the
P.555
scaphoid and anatomic snuffbox. The snuffbox is typically obscured by swelling.![]() Figure 46.2. Three types of scaphoid fractures. (A) Distal third. (B) Middle third. (C) Proximal pole.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 46.2. Three types of scaphoid fractures. (A) Distal third. (B) Middle third. (C) Proximal pole.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Radiographic evaluation: The diagnosis
can usually be made on the basis of AP and lateral views of the wrist.
Oblique views and “scaphoid views,” or views of the scaphoid in radial
and ulnar deviation of the wrist, may aid in the diagnosis or assist in
further fracture definition. Technetium bone scan, magnetic resonance
imaging, computed tomography, and ultrasound evaluation may be used to
diagnose occult scaphoid fractures.
| Type A: | Fractures of the distal pole |
| A1: | Extraarticular distal pole fractures |
| A2: | Intraarticular distal pole fractures |
| Type B: | Fractures of the middle third (waist fractures) |
| Type C: | Fractures of the proximal pole. |
-
A fracture should be presumed if snuffbox
tenderness is present, even if radiographs do not show an obvious
fracture. Initial treatment in the emergency setting should consist of
a thumb spica splint or cast immobilization if swelling is not
pronounced. In the pediatric population, a long arm cast or splint is
typically necessary for adequate immobilization. This should be
maintained for 2 weeks at which time repeat evaluation should be
undertaken. -
For stable, nondisplaced fractures, a
long arm cast should be placed with the wrist in neutral deviation and
flexion/extension and maintained for 6 to 8 weeks or until radiographic
evidence of healing has occurred. -
Displaced fractures in the pediatric
population may be initially addressed with closed reduction and
percutaneous pinning. Distal pole fractures can generally be reduced by
traction and ulnar deviation. -
Residual displacement >1 mm,
angulation >10 degrees, or scaphoid fractures in adolescents
generally require open reduction and internal fixation. A headless
compression screw or smooth Kirschner wires may be used for fracture
fixation, with postoperative immobilization consisting of a long arm
thumb spica cast for 6 weeks.
-
Delayed union, nonunion, and malunion:
These are rare in the pediatric population and may necessitate
operative fixation with bone grafting to achieve union. -
Osteonecrosis: Extremely rare in the
pediatric population and occurs with fractures of the proximal pole in
skeletally mature individuals. -
Missed diagnosis: Clinical suspicion
should outweigh normal appearing radiographs, and a brief period of
immobilization (2 weeks) can be followed by repeat clinical examination
and further radiographic studies if warranted.
-
This extremely rare injury occurs primarily from severe, direct trauma (e.g., crush injury).
-
Clinical evaluation reveals tenderness to
palpation on the volar wrist overlying the distal radius and lunate,
with painful range of motion. -
Radiographic evaluation: AP and lateral
views of the wrist are often inadequate to establish the diagnosis of
lunate fracture because osseous details are frequently obscured by
overlapping densities.-
Oblique views may be helpful, but computed tomography, or technetium bone scanning best demonstrate fracture.
-
-
Treatment
-
Nondisplaced fractures or unrecognized
fractures generally heal uneventfully and may be recognized only in
retrospect. When diagnosed, they should be treated in a short arm cast
or splint for 2 to 4 weeks until radiographic and symptomatic healing
occurs. -
Displaced or comminuted fractures should
be treated surgically to allow adequate apposition for formation of
vascular anastomoses. This may be achieved with open reduction and
internal fixation, although the severity of the injury mechanism
typically results in concomitant injuries to the wrist that may result
in growth arrest.
-
-
Complications
-
Osteonecrosis: Referred to as
“lunatomalacia” in the pediatric population, this occurs in children
less than 10 years of age. Symptoms are rarely dramatic, and
radiography reveals mildly increased density of the lunate with no
change in morphology. Immobilization of up to 1 year may be necessary
for treatment, but it usually results in good functional and
symptomatic recovery.
-
-
Extremely rare, but the true incidence
unknown owing to the late ossification of the triquetrum, with
potential injuries unrecognized. -
The mechanism of fracture is typically direct trauma to the ulnar wrist or avulsion by dorsal ligamentous structures.
-
Clinical evaluation reveals tenderness to palpation on the dorsoulnar aspect of the wrist as well as painful range of motion.
-
Radiographic evaluation: Transverse
fractures of the body can generally be identified on AP views in older
children and adolescents. Distraction views may be helpful in these
cases. -
Treatment
-
Nondisplaced fractures of the triquetrum
body or dorsal chip fractures may be treated in a short arm cast or
ulnar gutter splint for 2 to 4 weeks when symptomatic improvement
occurs. -
Displaced fractures may be amenable to open reduction and internal fixation.
-
-
No specific discussions of pisiform fractures in the pediatric population exist in the literature.
-
Direct trauma causing a comminuted fracture or a flexor carpi ulnaris avulsion may occur in late adolescence.
-
Radiographic evaluation is typically unrevealing, because ossification of the pisiform does not occur until age 8 years.
-
Treatment is symptomatic only, with immobilization in an ulnar gutter splint until the patient is comfortable.
-
Extremely rare in children and adults.
-
The mechanism of injury is axial loading
of the adducted thumb, driving the base of the first metacarpal onto
the articular surface of the trapezium with dorsal impaction. Avulsion
fractures may occur with forceful deviation, traction, or rotation of
the thumb. Direct trauma to the palmar arch may result in avulsion of
the trapezial ridge by the transverse carpal ligament. -
Clinical evaluation reveals tenderness to
palpation of the radial wrist, accompanied by painful range of motion
at the first carpometacarpal joint with stress testing. -
Radiographic evaluation: Fractures are
difficult to identify because of the late ossification of the
trapezium. In older children and adolescents, identifiable fractures
may be appreciated on standard AP and lateral views.-
Superimposition of the first metacarpal
base may be eliminated by obtaining a Robert view or a true AP view of
the first carpometacarpal joint and trapezium.
-
-
Treatment:
-
Most fractures are amenable to thumb spica splinting or casting to immobilize the first carpometacarpal joint for 3 to 5 weeks.
-
Rarely, severely displaced fractures may
require open reduction and internal fixation to restore articular
congruity and maintain carpometacarpal joint integrity.
-
-
Fractures of the trapezoid in children are extremely rare.
-
Axial load transmitted through the second
metacarpal may lead to dislocation, more often dorsal, with associated
capsular ligament disruption. Direct trauma from blast or crush
injuries may cause trapezoid fracture. -
Clinical evaluation demonstrates
tenderness proximal to the base of the second metacarpal with painful
range of motion of the second carpometacarpal joint. -
Radiographic evaluation: Fractures are
difficult to identify secondary to late ossification. In older children
and adolescents, they may be identified on the AP radiograph based on a
loss of the normal relationship between the second metacarpal base and
the trapezoid. Comparison with the contralateral, normal wrist may aid
in the diagnosis. The trapezoid, or fracture fragments, may be
superimposed over the trapezium or capitate, and the second metacarpal
may be proximally displaced. -
Treatment
-
Most fractures may be treated with a splint or short arm cast for 3 to 5 weeks.
-
Severely displaced fractures may require
open reduction and internal fixation with Kirschner wires with
attention to restoration of articular congruity.
-
-
Uncommon as an isolated injury owing to its relatively protected position.
-
A fracture of the capitate is more
commonly associated with greater arc injury pattern (transscaphoid,
transcapitate perilunate fracture-dislocation). A variation of this is
the “naviculocapitate syndrome,” in which the capitate and scaphoid are
fractured without associated dislocation. -
The mechanism of injury is typically
direct trauma or a crushing force that results in associated carpal or
metacarpal fracture. Hyperdorsiflexion may cause impaction of the
capitate waist against the lunate or dorsal aspect of the radius. -
Clinical evaluation reveals point
tenderness as well as variable painful dorsiflexion of the wrist as the
capitate impinges on the dorsal rim of the radius. -
Radiographic evaluation: Fracture can
usually be identified on the AP radiograph, with identification of the
head of the capitate on lateral views to determine rotation or
displacement. Distraction views may aid in fracture definition as well
as identification of associated greater arc injuries. Magnetic
resonance imaging may assist in evaluating ligamentous disruption. -
Treatment: Splint or cast immobilization
for 6 to 8 weeks may be performed for minimally displaced capitate
fractures. Open reduction is indicated for fractures with extreme
displacement or rotation to avoid osteonecrosis. Fixation may be
achieved with Kirschner wires or compression screws. -
Complications
-
There are no specific discussions in the literature concerning hamate fractures in the pediatric population.
-
The mechanism of injury typically
involves direct trauma to the volar aspect of the ulnar wrist such as
may occur with participation in racquet sports, softball, or golf. -
Clinical evaluation: Patients typically
present with pain and tenderness over the hamate. Ulnar and median
neuropathy can also be seen, as well as rare injuries to the ulnar
artery. -
Radiographic evaluation: The diagnosis of
hamate fracture can usually be made on the basis of the AP view of the
wrist. Fracture of the hamate is best visualized on the carpal tunnel
or 20-degree supination oblique view (oblique projection of the wrist
in radial deviation and semisupination). A hamate fracture should not
be confused with an os hamulus proprium, which represents a secondary
ossification center. -
Treatment: All hamate fractures should be
initially treated with immobilization in a short arm splint or cast
unless compromise of neurovascular structures warrants exploration.
Excision of fragments is generally not necessary in the pediatric
population. -
Complications
-
Symptomatic nonunion: May be treated with excision of the nonunited fragment.
-
Ulnar or median neuropathy: Related to
the proximity of the hamate to these nerves and may require surgical
exploration and release.
-
-
Biphasic distribution: These injuries are
seen in toddlers and adolescents. The injuries are typically crush
injuries in toddlers and are typically related to sports participation
in adolescents. -
The number of hand fractures in children
is higher in boys and peaks at 13 years of age, which coincides with
participation of boys in organized football. -
The annual incidence of pediatric hand
fractures is 26.4 per 10,000 children, with the majority occurring
about the metacarpophalangeal joint. -
Hand fractures account for up to 25% of all pediatric fractures.
-
As a rule, extensor tendons of the hand insert onto epiphyses.
-
At the level of the metacarpophalangeal
joints, the collateral ligaments originate from the metacarpal
epiphysis and inset almost exclusively onto the epiphysis of the
proximal phalanx; this accounts for the high frequency of Salter-Harris
Type II and III injuries in this region. -
The periosteum of the bones of the
pediatric hand is usually well developed and accounts for intrinsic
fracture stability in seemingly unstable injuries; this often serves as
an aid to achieving or maintaining fracture reduction. Conversely, the
exuberant periosteum may become interposed in the fracture site, thus
preventing effective closed reduction.
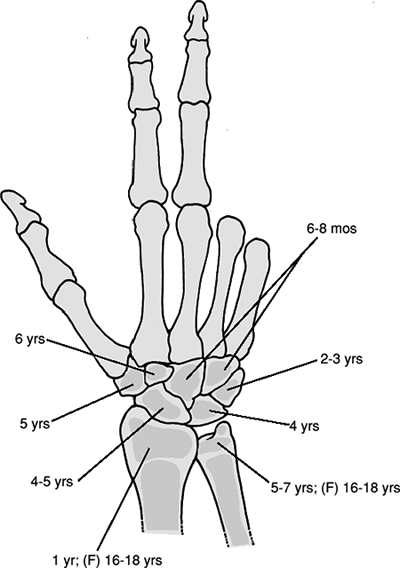
 |
|
Figure 46.3. Appearance of secondary ossification centers (A). Fusion of secondary centers to the primary centers (F).
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
The mechanism of hand injuries varies
considerably. In general, fracture patterns emerge based on the nature
of the traumatic force:-
Nonepiphyseal: torque, angular force, compressive load, direct trauma
-
Epiphyseal: avulsion, shear, splitting
-
Physeal: shear, angular force, compressive load
-
-
The child with a hand injury is typically
uncooperative because of pain, unfamiliar surroundings, parent anxiety,
and “white coat” fear. Simple observation of the child at play may
provide useful information concerning the location and severity of
P.561
injury. Game playing (e.g., “Simon says”) with the child may be utilized for clinical evaluation. -
History: A careful history is essential because it may influence treatment. This should include:
-
Patient age.
-
Dominant versus nondominant hand.
-
Refusal to use the injured extremity.
-
The exact nature of the injury: crush, direct trauma, twist, tear, laceration, etc.
-
The exact time of the injury (for open fractures).
-
Exposure to contamination: barnyard, brackish water, animal/human bite.
-
Treatment provided: cleansing, antiseptic, bandage, tourniquet.
-
-
Physical examination: The entire hand
should be exposed and examined for open injuries. Swelling should be
noted, as well as the presence of gross deformity (rotational or
angular). -
A careful neurovascular examination is
critical, with documentation of capillary refill and neurologic status
(two point discrimination). If the child is uncooperative and nerve
injury is suspected, the “wrinkle test” may be performed. This is
accomplished by immersion of the affected digit in warm, sterile water
for 5 minutes and observing corrugation of the distal volar pad (absent
in the denervated digit). -
Passive and active range of motion of
each joint should be determined. Observing tenodesis with passive wrist
motion is helpful for assessing digital alignment and cascade. -
Stress testing may be performed to determine collateral ligament and volar plate integrity.
-
AP, lateral, and oblique radiographs of
the affected digit or hand should be obtained. Injured digits should be
viewed individually, when possible, to minimize overlap of other digits
over the area of interest. -
Stress radiographs may be obtained in cases in which ligamentous injury is suspected.
-
The examiner must be aware that
cartilaginous injury may have occurred despite negative plain
radiographs. Treatment must be guided by clinical as well as
radiographic factors.
-
“Fight-bite” injuries: Any short, curved
laceration overlying a joint in the hand, particularly the
metacarpal-phalangeal joint, must be suspected of having been caused by
a tooth. These injuries must be assumed to be contaminated with oral
flora and should be addressed with broad-spectrum antibiotics. -
Most pediatric hand fractures are treated
nonoperatively, with closed reduction using conscious sedation or
regional anesthesia (e.g., digital block). Hematoma blocks or fracture
manipulation without anesthesia should be avoided in younger children. -
Finger traps may be utilized with older children or adolescents but are generally poorly tolerated in younger children.
-
The likelihood of iatrogenic physeal
injury substantially increases with repeated, forceful manipulation,
especially when involving late (>5 to 7 days) manipulation of a
paraphyseal fracture. -
Immobilization may consist of short arm
splints (volar, dorsal, ulnar gutter, etc.) or long arm splints in
younger patients to enhance immobilization. With conscientious
follow-up and cast changes as indicated, immobilization is rarely
necessary beyond 4 weeks. -
Operative indications include: unstable
fractures, in which the patient may benefit from percutaneous Kirschner
wire fixation; open fractures, which may require irrigation,
debridement, and secondary wound closure; and fractures in which
reduction is unattainable by closed means—these may signify interposed
periosteum or soft tissue that requires open reduction. -
Subungual hematomas that occupy >50%
of the nailplate should be evacuated with the use of a needle, cautery
tip, or heated paper clip. DaCruz et al. reported a high incidence of
late nail deformities associated with failure to decompress subungual
hematomas. -
Nailbed injuries should be addressed with
removal of the compromised nail, repair of the nailbed with 6-0 or 7-0
absorbable suture, and retention of the nail under the nailfold as a
biologic dressing to protect the healing nailbed. Alternatively,
commercially made stents are available for use as dressings.
-
Pediatric metacarpal fractures are classified as follows:
-
Fractures include the following:
-
Epiphyseal fractures
-
Physeal fractures: Salter Harris Type II fractures of the fifth metacarpal most common
-
Collateral ligament avulsion fractures
-
Oblique, vertical, and horizontal head fractures
-
Comminuted fractures
-
Boxer’s fractures with an intraarticular component
-
Fractures associated with bone loss
-
-
Most require anatomic reduction (if possible) to reestablish joint congruity and to minimize posttraumatic arthrosis.
-
Stable fracture reductions may be
splinted in the “protected position,” consisting of metacarpophalangeal
flexion >70 degrees and interphalangeal joint extension to minimize
joint stiffness. -
Percutaneous pinning may be necessary to
obtain stable reduction; if possible, the metaphyseal component
(Thurston-Holland fragment) should be included in the fixation.
-
-
Early range of motion is essential.
-
Fractures of the fourth and fifth metacarpal necks are commonly seen as pediatric analogs to boxer’s fractures in adults.
-
The degree of acceptable deformity varies according to the metacarpal injured, especially in adolescents:
-
More than 15-degree angulation for the second and third metacarpals is unacceptable.
-
More than 40- to 45-degree angulation for the fourth and fifth metacarpals is unacceptable.
-
-
These are typically addressed by closed
reduction using the Jahss maneuver by flexing the metacarpophalangeal
joint to 90 degrees and placing an axial load through the proximal
phalanx. This is followed by splinting in the “protected position.” -
Unstable fractures require operative
intervention with either percutaneous pins (may be intramedullary or
transverse into the adjacent metacarpal) or plate fixation
(adolescents).
-
Most of these fractures may be reduced by closed means and splinted in the protected position.
-
Operative indications include unstable
fractures, rotational deformity, dorsal angulation >10 degrees for
second and third metacarpals, and >20 degrees for fourth and fifth
metacarpals, especially for older children and adolescents in whom
significant remodeling is not expected. -
Operative fixation may be achieved with
closed reduction and percutaneous pinning (intramedullary or transverse
into the adjacent metacarpal). Open reduction is rarely indicated,
although the child presenting with multiple, adjacent, displaced
metacarpal fractures may require reduction by open means.
-
The carpometacarpal joint is protected
from frequent injury owing to its proximal location in the hand and the
stability afforded by the bony congruence and soft tissue restraints. -
The fourth and fifth carpometacarpal
joints are more mobile than the second and third; therefore, injury to
these joints is uncommon and usually results from high-energy
mechanisms. -
Axial loading from punching mechanisms typically results in stable buckle fractures in the metaphyseal region.
-
Closed reduction using regional or
conscious sedation and splinting with a short arm ulnar gutter splint
may be performed for the majority of these fractures, leaving the
proximal interphalangeal joint mobile. -
Fracture-dislocations in this region may
result from crush mechanisms or falls from a height; these may
initially be addressed with attempted closed reduction, although
transverse metacarpal pinning is usually necessary for stability. Open
reduction may be necessary, especially in cases of multiple
fracture-dislocations at the carpometacarpal level.
-
Fractures are uncommon and are typically related to direct trauma.
-
Metaphyseal and physeal injuries are the most common fracture patterns.
-
Structures inserting on the thumb metacarpal constitute potential deforming forces:
-
Opponens pollicis: broad insertion over
metacarpal shaft and base that displaces the distal fragment into
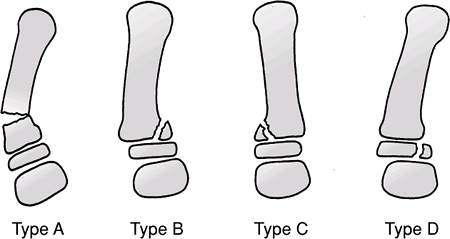
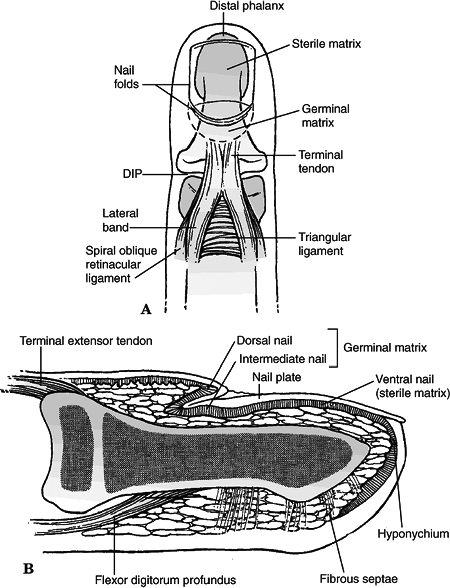
relative adduction and flexion![]() Figure
Figure
46.4. Classification of thumb metacarpal fractures. (A) Metaphyseal
fracture. (B,C) Salter-Harris Type II physeal fractures with lateral or
medial angulation. (D) Salter-Harris Type III fracture (pediatric
Bennett fracture).(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Abductor pollicis longus: multiple sites
of insertion including the metacarpal base, resulting in abduction
moment in cases of fracture-dislocation -
Flexor pollicis brevis: partial origin on
the medial metacarpal base, resulting in flexion and apex dorsal
angulation in metacarpal shaft fractures -
Adductor pollicis: possible adduction of the distal fragment
-
-
These typically result from direct trauma.
-
Closed reduction is usually adequate for
the treatment of most fractures, with postreduction immobilization
consisting of a thumb spica splint or cast. -
Anatomic reduction is essential for
intraarticular fractures and may necessitate the use of percutaneous
pinning with Kirschner wires.
-
Type A: fractures distal to the physis
-
They are often transverse or oblique, with apex-lateral angulation and an element of medial impaction.
-
They are treated with closed reduction
with extension applied to the metacarpal head and direct pressure on
the apex of the fracture, then immobilized in a thumb spica splint or
cast for 4 to 6 weeks. -
Up to 30 degrees of residual angulation may be accepted in younger children.
-
Unstable fractures may require
percutaneous Kirschner wire fixation, often with smooth pins to cross
the physis. Transcarpometacarpal pinning may be performed but is
usually reserved for more proximal fracture patterns.
P.565 -
-
Type B: Salter-Harris Type II fracture, metaphyseal medial
-
The shaft fragment is typically angulated
laterally and displaced proximally owing to the pull of the abductor
pollicis longus; adduction of the distal fragment is common because of
the pull of the adductor pollicis. -
Anatomic reduction is essential to avoid growth disturbance.
-
Closed reduction followed by thumb spica
splinting is initially indicated, with close serial follow-up. With
maintenance of reduction, immobilization should be continued for 4 to 6
weeks. -
Percutaneous pinning is indicated for
unstable fractures with capture of the metaphyseal fragment if
possible. Alternatively, transmetacarpal pinning to the second
metacarpal may be necessary. Open reduction may be required for
anatomic restoration of the physis.
-
-
Type C: Salter-Harris Type II fracture, metaphyseal lateral
-
These are similar to Type B fractures,
but they are less common and typically result from more significant
trauma, with consequent apex medial angulation. -
Periosteal buttonholing is common and may prevent anatomic reduction.
-
Open reduction is frequently necessary for restoration of anatomic relationships.
-
-
Type D: intraarticular Salter-Harris Type III or IV fractures
-
These are the pediatric analogs to the adult Bennett fracture.
-
They are rare, with deforming forces
similar to Type B fractures, with the addition of lateral subluxation
at the level of the carpometacarpal articulation caused by the
intraarticular component of the fracture. -
Nonoperative methods of treatment widely
variable in results. Most consistent results are obtained with open
reduction and percutaneous pinning or internal fixation in older
children. -
Severe comminution or soft tissue injury may be initially addressed with oblique skeletal traction.
-
External fixation may be used for contaminated open fractures with potential bone loss.
-
-
The physes are located at the proximal aspect of the phalanges.
-
The collateral ligaments of the proximal
and distal interphalangeal joints originate from the collateral
recesses of the proximal bone and insert onto both the epiphysis and
metaphysis of the distal bone and volar plate. -
The volar plate originates from the
metaphyseal region of the phalangeal neck and inserts onto the
epiphysis of the more distal phalanx. -
The extensor tendons insert onto the dorsal aspect of the epiphysis of the middle and distal phalanges.
-
The periosteum is typically well
developed and exuberant, often resisting displacement and aiding
reduction, but occasionally interposing at the fracture site and
preventing adequate reduction.
 |
|
Figure
46.5. Anatomy about the distal phalanx. (A) The skin, nail, and extensor apparatus share a close relationship with the bone of the distal phalanx. Specific anatomic structures at the terminal aspect of the digit are labeled. (B) This lateral view of the nail demonstrates the tendon insertions and the anatomy of the specialized nail tissues. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Type A: physeal
-
Of pediatric hand fractures, 41% involve
the physis. The proximal phalanx is the most frequently injured bone in
the pediatric population. -
The collateral ligaments insert onto the
epiphysis of the proximal phalanx; in addition to the relatively
unprotected position of the physis at this level, this contributes to
the high incidence of physeal injuries. -
A pediatric “gamekeeper’s” thumb is a
Salter-Harris Type III avulsion fracture, with the ulnar collateral
ligament attached to an epiphyseal fragment of the proximal aspect of
the proximal phalanx. -
Treatment is initially by closed reduction and splinting in the protected position.
-
Unstable fractures may require
percutaneous pinning. Fractures with >25% articular involvement or
>1.5 mm displacement require open reduction with internal fixation
with Kirschner wires or screws.
P.567 -
-
Type B: shaft
-
Shaft fractures are not as common as those surrounding the joints.
-
Proximal phalangeal shaft fractures are
typically associated with apex volar angulation and displacement,
created by forces of the distally inserting central slip and lateral
bands coursing dorsal to the apex of rotation, as well as the action of
the intrinsics on the proximal fragment pulling it into flexion. -
Oblique fractures may be associated with
shortening and rotational displacement. This must be recognized and
taken into consideration for treatment. -
Closed reduction with immobilization in
the protected position for 3 to 4 weeks is indicated for the majority
of these fractures. -
Residual angulation >30 degrees in
children <10 years of age, >20 degrees in children >10 years
of age, or any malrotation requires operative intervention, consisting
of closed reduction and percutaneous crossed pinning. Intramedullary
pinning may allow rotational displacement.
-
-
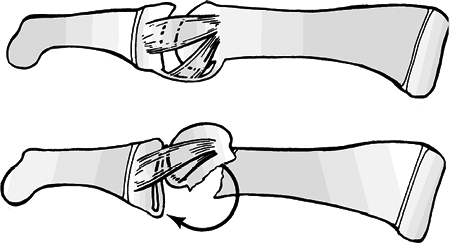
Type C: neck (Fig. 46.6)
-
Fractures through the metaphyseal region of the phalanx are commonly associated with door-slamming injuries.
![]() Figure
Figure
46.6. Phalangeal neck fractures often are unstable and rotated. These
fractures are difficult to reduce and control by closed means because
of the forces imparted by the volar plate and ligaments.(From Wood BE. Fractures of the hand in children. Orthop Clin North Am 1976;7:527–534.) -
Rotational displacement and angulation of
the distal fragment are common, because the collateral ligaments
typically remain attached distal to the fracture site. This may allow
interposition of the volar plate at the fracture. -
Closed reduction followed by splinting in
the protected position for 3 to 4 weeks may be attempted initially,
although closed reduction with percutaneous crossed pinning is usually
required.
P.568 -
-
Type D: intraarticular (condylar)
-
These arise from a variety of mechanisms,
ranging from shear or avulsion resulting in simple fractures to
combined axial and rotational forces that may result in comminuted,
intraarticular T- or Y-type patterns. -
Open reduction and internal fixation are
usually required for anatomic restoration of the articular surface.
This operation is most often performed through a lateral or dorsal
incision, with fixation using Kirschner wires or miniscrews.
-
-
These injuries are frequently associated
with soft tissue or nail compromise and may require subungual hematoma
evacuation, soft tissue reconstructive procedures, or nailbed repair. -
Pediatric distal phalangeal fractures are subclassified as follows:
-
Physeal
-
A mallet finger may result from a
fracture of the dorsal lip with disruption of the extensor tendon.
Alternatively, a mallet finger may result from a purely tendinous
disruption and may therefore not be radiographically apparent. -
Treatment of Type A and nondisplaced or minimally displaced type B injuries is full-time extension splinting for 4 to 6 weeks.
-
Type C, D, and displaced Type B injuries
typically require operative management. Type B injuries are usually
amenable to Kirschner wire fixation with smooth pins. Type C and D
injuries generally require open reduction and internal fixation.
-
-
Volar (reverse) mallet injuries
-
These are associated with flexor
digitorum profundus rupture (“jersey finger:” seen in football and
rugby players, most commonly involving the ring finger). -
Treatment is primary repair using heavy
suture, miniscrews, or Kirschner wires. Postoperative immobilization is
continued for 3 weeks.
-
-
Extraphyseal
Type A: Transverse diaphyseal Type B: Longitudinal splitting Type C: Comminuted P.569-
The mechanism of injury is almost always direct trauma.
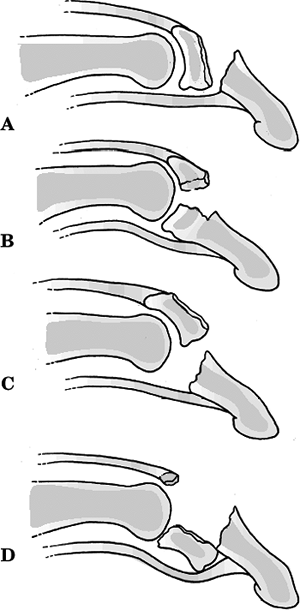 Figure 46.7. (A–D) Malletequivalent physeal fracture types.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 46.7. (A–D) Malletequivalent physeal fracture types.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Nailbed injuries must be recognized and addressed.
-
Treatment is typically closed reduction
and splinting for 3 to 4 weeks with attention to concomitant injuries.
Unstable injuries may require percutaneous pinning, either
longitudinally from the distal margin of the distal phalanx or across
the distal interphalangeal joint (uncommon) for extremely unstable or
comminuted fractures.
-
-
Impaired nail growth: Failure to repair
the nailbed adequately may result in germinal matrix disturbance that
causes anomalous nail growth. This is frequently a cosmetic problem,
but it may be addressed with reconstructive procedures if pain,
infection, or hygiene is an issue. -
Extensor lag: Despite adequate treatment,
extensor lag up to 10 degrees is common, although not typically of
functional significance. This occurs most commonly at the level of the
proximal interphalangeal joint secondary to tendon adherence.
Exploration, release, and or reconstruction may result in further
cosmetic or functional disturbance. -
Malunion: Apex dorsal angulation can
disturb intrinsic balance and also can result in prominence of
metacarpal heads in palm with pain on gripping. Rotational or
angulatory deformities, especially of the second and third metacarpals,
may produce
P.570
functional and cosmetic disturbances, thus emphasizing the need to maintain as near an anatomic relationship as possible. -
Nonunion: Uncommon but may occur
especially with extensive soft tissue injury and bone loss, as well as
in open fractures with gross contamination and infection. -
Infection, osteomyelitis: Grossly
contaminated wounds require meticulous debridement, appropriate
antibiotic coverage, and possible delayed closure. -
Metacarpophalangeal joint extension
contracture: This may result if splinting is not in the protected
position (i.e., metacarpophalangeal joints at >70 degrees), owing to
soft tissue contracture.