Jones Fracture
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Jones Fracture
Jones Fracture
Bill Hobbs MD
Simon C. Mears MD, PhD
Description
-
Fracture of the base of the 5th metatarsal of the foot
-
Injuries may be acute or stress fractures.
-
-
Classification is by location of the fracture (1).
-
Tuberosity avulsion fracture: No involvement of the 4th to 5th intermetatarsal joint
-
True Jones fracture: Proximal metaphyseal
fracture with involvement of the 4th to 5th intermetatarsal joint up to
the metaphyseal–diaphyseal junction -
Diaphyseal fracture (pseudo-Jones
fracture): At the proximal diaphysis, distal to the tuberosity of the
peroneus tertius insertion
-
General Prevention
Early radiographs for athletes complaining of lateral
foot pain so that treatment measures can be initiated to decrease
prolonged symptoms.
foot pain so that treatment measures can be initiated to decrease
prolonged symptoms.
Epidemiology
-
Common in athletes
-
Metatarsal fractures occur at all ages (mean age, 42 years) (2).
-
Occurs more often in females than males
-
63% of all metatarsal fractures involve the 5th metatarsal (2).
Incidence
1.8% of professional football players sustain a Jones fracture (3).
Risk Factors
-
Athletics
-
Falls
-
Osteoporosis is a risk factor for foot fractures (4).
Etiology
-
Avulsion fracture: Inversion or internal rotation injury of the foot
-
Jones or diaphyseal fractures: Indirect
trauma (inversion or internal rotation injuries) or direct trauma, such
as dropping a heavy object on the foot
Signs and Symptoms
Pain and swelling along the lateral border of the foot occur with point tenderness at the base of the 5th metatarsal.
Physical Exam
-
Pain over the lateral forefoot with palpation and weightbearing
-
Swelling and redness also common
Tests
Imaging
Plain, AP, lateral, and oblique radiographs of the foot are obtained to determine the level and displacement of the fracture.
Pathological Findings
The watershed blood supply to the metaphyseal–diaphyseal
junction makes fractures in this area more susceptible to nonunion and
requires more aggressive treatment of the Jones fracture than do other
metatarsal fractures.
junction makes fractures in this area more susceptible to nonunion and
requires more aggressive treatment of the Jones fracture than do other
metatarsal fractures.
Differential Diagnosis
-
Lisfranc injury (dislocation of tarsometatarsal joints)
-
Stress fracture of the 5th metatarsal diaphysis (Fig. 1)
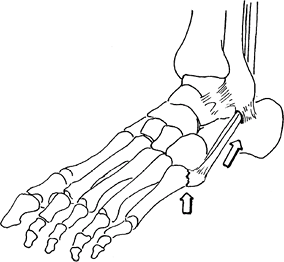 Fig.
Fig.
1. Avulsion fracture of the 5th metatarsal bone (as shown here) must be
differentiated from Jones fracture, which occurs more distally.
General Measures
-
Treatment varies by fracture type.
-
Tuberosity avulsion:
-
Symptomatic management involves
weightbearing as tolerated with a hard-soled shoe, cast, or splint,
even with considerable displacement (>1 cm). -
Clinical union often occurs by 3 weeks.
-
Nonunion is rarely symptomatic; if problematic, resect the fragment and reattach the peroneus brevis tendon.
-
-
Diaphyseal fracture:
-
The patient is nonweightbearing in a
below-the-knee cast until radiographic union occurs (usually 8 weeks),
followed by 6 weeks of limited activity.
-
-
Jones fracture:
-
Most are treated with a nonweightbearing below-the-knee cast for 4–6 weeks.
-
Competitive athletes may undergo
percutaneous screw fixation with weightbearing after 2 weeks and may
return to sports after pain and tenderness have resolved (8 weeks).
-
-
Activity
Activity is as-tolerated with the previously mentioned
external supports, except for diaphyseal fractures, for which patients
should remain nonweightbearing for 6–8 weeks.
external supports, except for diaphyseal fractures, for which patients
should remain nonweightbearing for 6–8 weeks.
Special Therapy
Physical Therapy
Rarely indicated
Surgery
-
Diaphyseal fractures:
-
May be treated with percutaneous placement of a malleolar screw for earlier return to activity
-
-
Jones fracture:
-
Screw fixation for Jones fractures in competitive athletes
-
A cannulated screw can be placed percutaneously.
-
-
Avulsion fracture
-
Symptomatic nonunion may be treated with excision of the fragment and reattachment of the peroneus brevis tendon.
-
P.203
Prognosis
-
The prognosis is excellent for avulsion fractures (5).
-
Jones fractures treated nonoperatively have approximately a 40% chance of not healing (6).
-
Treatment of Jones fractures with
intramedullary fixation is thought to result in a higher rate of
healing and earlier return to function for athletes (7).
Complications
-
Nonunion of fracture
-
Recurrent fractures are more common in highly competitive athletes.
-
Returning to sport before full healing is thought to increase the rate of nonunion even with surgical treatment (8).
Patient Monitoring
-
Patients are followed at 1-month intervals until the fracture heals and they return to full weightbearing.
-
Delayed union occurs when the healing at the fracture site has not occurred by 6–8 weeks.
-
The fracture is judged to be a nonunion if no evidence of additional healing is noted and pain is present at the fracture site.
References
1. Torg
JS, Balduini FC, Zelko RR, et al. Fractures of the base of the fifth
metatarsal distal to the tuberosity. Classification and guidelines for
non-surgical and surgical management. J Bone Joint Surg 1984;66A:209–214.
JS, Balduini FC, Zelko RR, et al. Fractures of the base of the fifth
metatarsal distal to the tuberosity. Classification and guidelines for
non-surgical and surgical management. J Bone Joint Surg 1984;66A:209–214.
2. Petrisor BA, Ekrol I, Court-Brown C. The epidemiology of metatarsal fractures. Foot Ankle Int 2006;27:172–174.
3. Low K, Noblin JD, Browne JE, et al. Jones fractures in the elite football player. J Surg Orthop Adv 2004;13:156–160.
4. Hasselman CT, Vogt MT, Stone KL, et al. Foot and ankle fractures in elderly white women. Incidence and risk factors. J Bone Joint Surg 2003;85A: 820–824.
5. Konkel
KF, Menger AG, Retzlaff SA. Nonoperative treatment of fifth metatarsal
fractures in an orthopaedic suburban private multispeciality practice. Foot Ankle Int 2005;26:704–707.
KF, Menger AG, Retzlaff SA. Nonoperative treatment of fifth metatarsal
fractures in an orthopaedic suburban private multispeciality practice. Foot Ankle Int 2005;26:704–707.
6. Mologne TS, Lundeen JM, Clapper MF, et al. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med 2005; 33:970–975.
7. Rosenberg GA, Sferra JJ. Treatment strategies for acute fractures and nonunions of the proximal fifth metatarsal. J Am Acad Orthop Surg 2000;8: 332–338.
8. Larson CM, Almekinders LC, Taft TN, et al. Intramedullary screw fixation of Jones fractures. Analysis of failure. Am J Sports Med 2002;30: 55–60.
Additional Reading
Fetzer GB, Wright RW. Metatarsal shaft fractures and fractures of the proximal fifth metatarsal. Clin Sports Med 2006;25:139–150.
Codes
ICD9-CM
825.25 Metatarsal fracture
Patient Teaching
-
Stress the importance of following weight limitations to prevent nonunion and delay in return to normal activities.
-
Stress to athletes that training should not begin after a Jones fractures until healing can be seen radiographically.
Activity
Patients with stress injuries should resume activity slowly.
Prevention
Athletes should monitor training activity to avoid repetitive stress injury.
FAQ
Q: Is a cast or splint needed for a fracture of the base of the 5th metatarsal?
A:
The need for immobilization depends on the fracture type. Avulsion
fractures require only symptomatic treatment. A splint may be used if
the patient has a lot of pain. Jones fractures should be treated with
immobilization; consideration should be given to intramedullary
fixation.
The need for immobilization depends on the fracture type. Avulsion
fractures require only symptomatic treatment. A splint may be used if
the patient has a lot of pain. Jones fractures should be treated with
immobilization; consideration should be given to intramedullary
fixation.
