PRINCIPLES OF AMPUTATION IN CHILDREN
same principles as in adults, require special considerations and
techniques because of continuing growth (1).
This chapter reviews the general disorders requiring amputation and
specific techniques useful in the skeletally immature patient.
on the ultimate success of a pediatric amputation, particularly in the
younger child. For example, a 6-year-old child who has a successful
above-knee amputation will have an extremely short stump at maturity
because of loss of the distal femoral physis. In addition, stumps in
children tend to become narrow and conical with growth, and this may
subsequently lead to poor rotational control of a prosthesis.
overgrowth. Overgrowth probably results from distal apposition of bone
by the active periosteum, although the exact mechanism is not
understood. Overgrowth is not dependent on the physis, and
epiphysiodesis will not arrest it. Overgrowth never occurs after
disarticulation. Terminal overgrowth is most severe before 6 years of
age, and several revisions (three or more) may be required during the
growing years. Overgrowth is not seen after about 12 years of age. The
bones most likely to exhibit overgrowth are the humerus, fibula, and
tibia. The exact incidence depends on the diagnostic categories of the
reported series (congenital or traumatic). Many surgical remedies for
overgrowth, such as capping, osteotomy, and surgical cross-union, have
been attempted and discarded; the only effective treatment seems to be
surgical revision of the pointed distal bone and its overlying bursa.
the pediatric amputee than for the adult amputee. The congenital
amputee, born without the limb segment, accepts the condition as
normal. Children who lose a limb traumatically generally rehabilitate
quickly when a prosthesis is fitted. The main requirement of the child
is function and durability, often with little concern for appearance or
body image. However, parental acceptance of congenital or acquired
amputations may be difficult. Feelings of guilt or inappropriate fears
may require specialized
counseling.
Phantom limb and phantom pain, common in the adult amputee, are rare in
children and generally absent in the congenital amputee.
surgical techniques, and the special aspects of prosthetic fittings
during growth have led to multidisciplinary child amputee clinics in
centers throughout the country (6). The value
and success of this approach has been documented, and the surgeon
should consider referral to a regional center if one is available.
-
Preserve the physis. Amputations through
the metaphysis (such as above-knee or distal forearm level) or
diaphysis are not recommended in children because of the progressive
relative shortening of the residual limb. This is most critical in the
femur, but it is applicable to other long bones as well. -
Disarticulate when possible.
Disarticulation completely eliminates the problem of terminal
overgrowth and subsequent revision surgery. -
Preserve stump shape. The pediatric
amputation stump becomes conical with growth, so preservation of bony
architecture such as a short segment of proximal fibula or the distal
condyles of the humerus will assist in subsequent rotational control of
the prosthesis. -
Be creative with soft-tissue coverage.
Pediatric amputees rarely suffer from the wound-healing problems that
commonly affect dysvascular adult amputees. Split-thickness skin can
often be successfully used in the child to preserve an otherwise
satisfactory stump without adequate skin coverage. The split-thickness
skin graft can hypertrophy and become sufficiently strong to withstand
the shear forces of prosthesis use.
knows no other body image and has a remarkable ability to use a
prosthesis to enhance function (5,8).
Although the child automatically accepts the limb deficiency as normal,
parents are often emotionally overwhelmed by depression and guilt.
Early referral of the family to a regional child amputee clinic
facilitates the counseling and acceptance by the family that is as
necessary for a satisfactory outcome as orthopaedic or prosthetic
management.
to a different level, but revision of stumps for terminal overgrowth is
common, particularly for the humerus. Conversion of the upper extremity
is rarely necessary. It is usually unnecessary to remove upper
extremity nubbins, which the child may find useful for holding small
objects or activating powered prostheses. Lower extremity conversion
should be done to enhance prosthetic fitting if it facilitates
ambulation, but durability and function, not cosmesis, are the goals.
In general, useful deformities should be retained.
the child is sitting independently, usually at about 6 months. Initial
upper extremity terminal devices are passive, but they can be activated
when grasping becomes important (1.5 to 2 years of age). Lower
extremity prostheses are fitted when the child begins pulling to stand
or cruising. A fixed knee with waistband suspension is used for
above-knee amputees. Frequent length adjustments of the prosthesis will
be required with growth. Children will discard upper-limb prostheses if
they perceive them to be nonfunctional, and children with multiple limb
deficiencies often reject prostheses because they interfere with the
specialized movements required by daily living activities.
is considerable evidence that the typical child with a traumatic
amputation comes from a socially dysfunctional background. Most are
boys from single-parent homes who are rebellious or running away from
home. The psychological ability of these patients to undergo extensive
treatment, revision of level, and rehabilitation is often very limited.
Be sensitive to these psychosocial issues and obtain consultation early
from appropriate professionals.
necessary to consider amputation at a more proximal level rather than
subject the child to an emotionally draining series of heroic
procedures to preserve length. Traumatic amputees may not tolerate
multiple procedures or extensive rehabilitation efforts if they do not
have the emotional base of support of a functioning family system.
and terminal overgrowth, particularly of the tibia, is often a problem.
Many of these patients will wait until they can no longer tolerate
their prosthesis before presenting for a revision of the overgrown
stump, making smooth coordination of surgery and prosthetic fitting
difficult.
lost soft tissue from a degloving injury proximal to the bony
amputation level. Occasionally, it is appropriate to sacrifice bone
length if considerations warrant it. However, other options include
extensive use of split skin graft (much better tolerated in children
than in adults), tissue expanders, or microvascular free tissue
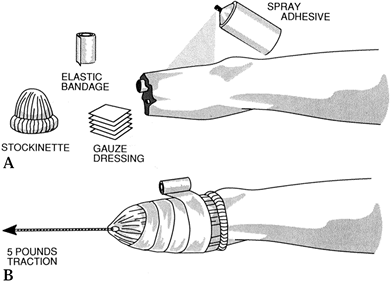
transfer. Skin traction (Fig. 175.1) over a 1- to 2-week period can add several centimeters of full-thickness circumferential skin and allows
inspection of the open wound for appropriate care in the interim.
 |
|
Figure 175.1. Technique of application of skin traction after traumatic amputation.
|
rapid mobilization of the trauma patient, while minimizing pain and
reducing the tendency to form contractures.
coverage while salvaging the most distal amputation level possible.
Extensive use of split-thickness skin is often successful in the child.
Stump breakdown is less of a problem in the child than in the adult.
Attempt to preserve length if at all possible. Proximal joint stiffness
seems to be more of a problem in burn amputees than in other amputees,
and it should be addressed early and aggressively in the rehabilitation
effort.
has become technically feasible in older children, but amputation is
still often necessary for local control of tumors. Amputation also may
be the treatment of choice for malignant tumors in children younger
than 10 years because skeletal growth is disturbed by limb-sparing
techniques. Amputation is usually indicated when a pathologic fracture
occurs through a malignant lesion.
as any tumor procedure, with the goal being complete local control of
the lesion for cure or palliation. Adjuvant chemotherapy or radiation
therapy may be appropriate.
added psychological stress to the family and child of adjuvant
treatments in the addition to limb loss, these children should receive
aggressive, early rehabilitation. Rigid dressings and immediate pylons
can ease the immense emotional strain of the diagnosis and treatment.
Use interim prostheses early, as chemotherapy and weight loss may
postpone definitive fitting.
division of bones, and treatment of sectioned nerves) for amputations
in children are generally the same as the techniques in adults (see Chapter 120, Chapter 121 and Chapter 122). However, amputations in skeletally immature patients present special considerations.
contour of the shoulder girdle, but most children reject prosthetic
fitting attempts. Mid-humerus and longer levels allow artificial limb
function, but the stump will become thin and conical, so every attempt
should be made to maintain its shape by preserving the distal humeral
condyles if possible. Marquardt (7) has
described a right-angle osteotomy 5 cm proximal to the end of the
above-elbow stump to assist with prosthesis suspension and rotational
control. Above-elbow amputees have a high incidence of terminal
overgrowth, and parents should be warned of the likelihood of multiple
revisions.
excellent amputation option for children. It eliminates the problem of
overgrowth, and the preservation of the distal humeral condyles aids in
prosthetic fitting. As puberty approaches, consider epiphysiodesis of
the distal humeral epiphysis. This provides shortening of the amputated
limb in comparison to the contralateral limb, allowing internal
prosthetic elbow hinges.
stump. Preserve as much length as possible. Even short below-elbow
stumps, distal to the biceps insertion on the radius, can aid with
prosthetic stabilization and internal prosthetic control.
in the child. It does not restrict pronation–supination, and overgrowth
does not occur.
hemipelvectomy and hip disarticulation are applicable to children. As
in adults, the prosthetic rejection rate after hemipelvectomy or hip
disarticulation is high (see Chapter 120 and Chapter 122).
is a poor option for children because of loss of the distal femoral
physis. The relative shortening of the leg with growth is dramatic and
is worsened by the problem of terminal overgrowth.
and lack of terminal overgrowth make knee disarticulation an ideal
amputation level in the child. The patella may be retained. Suture the
hamstrings to the cruciate stump and oversew the quadriceps tendon to
them. This tenodesis preserves the strength of the muscles for walking
and prevents their slippage around the distal bone end.
years in boys) approaches, do a distal femoral epiphysiodesis to allow
slight shortening, which facilitates prosthetic design using an
internal hinge. Consult a prosthetist to determine the optimal amount
of shortening for prosthetic fitting.
prosthetic ambulation potential, because above-knee amputees require
more energy for prosthetic ambulation than do below-knee amputees. As
most pediatric amputees will become geriatric amputees, it is desirable
to salvage the knee joint in pediatric amputation surgery if possible.
However, below-knee amputations have specific problems in children.
Terminal overgrowth of the tibia and fibula are almost inevitable, and
multiple revisions are the rule. Varus angulation in younger children
occurs often and may be severe enough to require tibial osteotomy. The
thin, conical stump makes rotational control difficult.
Patellar-tendon-bearing prosthesis is a misnomer in the growing child,
because the rapid change in length makes nearly all prostheses
essentially end-bearing. For all of these reasons, ankle
disarticulation is preferable to below-knee amputation if at all
possible.
the same for the child as for the adult, except that the skin flaps can
be widely variable because the vascular supply in children is so rich.
If possible, avoid scars directly over the end of the stump.
Split-thickness skin is remarkably well tolerated in the child and may
hypertrophy to give good results in maturity, even at this
weight-bearing level. Preserve the fibula if at all possible, even if
it is very short. The broad shape of the combined proximal tibia and
fibula enhances rotational prosthetic control. Surgical cross-union and
other techniques to prevent terminal overgrowth do not work and may
lead to proximal migration of the fibula.
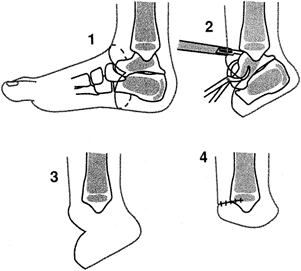
children, the similar procedure of ankle disarticulation carries the
same name by popular usage (Fig. 175.2). The
pediatric Syme amputation, while having the benefits of a
disarticulation, can be difficult to perform well because of the late
problem of posterior heel-pad migration (2).
Modern prosthetic technique allows fitting of bulbous stumps, which
often taper with maturation. The main use of the Syme amputation is in
congenital anomalies, especially fibular hemimelia and proximal femoral
focal deficiency. I prefer the Boyd amputation, described in the next
section, over the Syme.
 |
|
Figure 175.2. Technique of pediatric Syme amputation. See text for details.
|
-
Perform surgery with a pneumatic
tourniquet. Between points just distal to the medial and lateral
malleoli, connect an anterior incision dorsally and a plantar incision
directly inferiorly (Fig. 175.2). Carry the
incisions, without extensive subcutaneous undermining, straight down to
bone, ligating vascular structures and tagging the anterior tibial and
toe extensor tendons. -
Grab the talus with a towel clip and
plantar-flex it to its extreme. With a scalpel directed toward the
bone, carefully dissect out first the talus and then the os calcis
P.4467
in
a similar manner. Avoiding any injury to the subcutaneous tissue is
critical to the success of the operation. Ensure that the excision
includes the cartilaginous apophysis of the posterior os calcis. -
Sever the Achilles tendon and allow it to
retract into the leg. Trim the cartilaginous malleoli transversely to
the level of the tibial plafond with a scalpel. Suture the anterior
tibial and toe extensor tendons to the anterior edge of the heel pad to
prevent posterior migration. Avoid the temptation to trim the dog-ears
over the malleoli: They will remodel. Trimming may jeopardize the
vascular supply to the heel flap. -
Close the skin and subcutaneous tissue
with fine absorbable suture over a suction drain, and apply an
above-knee rigid plaster dressing with molding over the femoral
condyles.
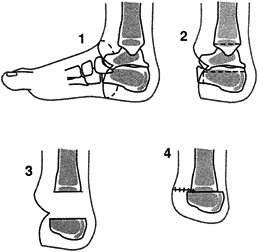
amputation, preserves the posterior os calcis and thus stabilizes the
heel pad (Fig. 175.3) (3).
Take care to place the heel in a plantigrade position and to divide the
Achilles tendon, so that the heel does not drift into plantar flexion.
If properly done, the Boyd produces an excellent end-bearing stump
without the problem of terminal overgrowth. Boyd amputations produce a
bulbous stump that may improve with growth.
 |
|
Figure 175.3. Technique of Boyd amputation. See text for details.
|
-
Make a skin incision in a fashion similar
to that for the pediatric Syme amputation. Tagging the anterior tendons
is unnecessary. Disarticulate the midfoot and forefoot from the talus
and calcaneus. Grab the talus with a towel clip and carefully shell it
out by plantar-flexing it and releasing soft-tissue attachments to the
talus with a small scalpel. The subcutaneous tissue must not be damaged
during this procedure. -
Shave the distal tibial articular surface
transversely until the ossific nucleus of the distal tibial epiphysis
is exposed, using a scalpel or fine osteotome (usually just held by
hand; a mallet is unnecessary). Similarly, shave the superior surface
of the os calcis down to cancellous bone, making it flat parallel to
the weight-bearing surface of the heel. Shorten the anterior end of the
os calcis. Sever the Achilles tendon and allow it to retract; this
prevents late plantar flexion drift of the os calcis. -
Approximate the raw surfaces of the
tibial epiphysis and os calcis while bringing the os calcis forward
(anterior) slightly. Hold them together with one or more smooth
Kirschner wires inserted through the heel pad. If the Boyd amputation
is being combined with a knee fusion for proximal femoral focal
deficiency, the heel can be fixed with a longitudinal Rush rod passed
up the heel, tibial canal, and through the knee fusion site. Use bone
graft from discarded bones if desired. Ensure that the weight-bearing
surface of the heel is plantigrade; avoid even slight plantar flexion. -
Close the wound over a suction drain
using fine absorbable stitches for all layers (I use 4-0 polyglycolic
acid), and bend the pin(s) externally to avoid migration. Immobilize
the limb in a spica cast or long-leg cast, depending on age. -
Remove the pins at 4–6 weeks and continue
immobilization in a long-leg cast (molded over the femoral condyles)
until radiographic union.
usually traumatic; this is not a desirable level for an elective
amputation. In managing these injuries, sever the Achilles tendon to
help prevent equinus contracture, and anchor extensor tendons, if
available, to the anterior bony structures. Conversion to a
higher-level (Boyd or pediatric Syme) amputation is often required (4).
level, are very well tolerated by children and require only a
space-filling prosthetic shoe insert.
management of pediatric amputations come from the improper applications
of adult amputation principles to the child. Adult principles fail to
take into account the need to
preserve
epiphyses for normal growth, to preserve distal shape for prosthetic
control, or to be creative with skin coverage so that length is not
traded for simplicity of initial wound closure. The complication of
terminal overgrowth following through-bone amputations in children is
predictable and requires surgical revision at 2- to 4-year intervals
until growth ceases. Painful neuromas and phantom pain are very rare
and generally occur only when the amputation is acquired in
adolescence. Management is the same as adults (see Chapter 120 and Chapter 121).
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
CN, Hamilton RC, Tellicore RJ. The Juvenile Amputee Program: Its Social
and Economic Value. A Follow-up Study after the Age of 21. J Bone Joint Surg Am 1969;51:1135.
