The Painful Total Knee Arthroplasty
II – Knee > Part C – Operative Treatment Methods > 27 – The
Painful Total Knee Arthroplasty
normally a progressive decrease in pain and a reciprocal increase in
function. Persistent and/or progressive pain is disconcerting to both
the patient and surgeon. The causes of pain following TKA are often
related to patient anatomy, implant design, and/or surgical technique.
as high as 47%; however, only 5% to 7% of patients experience
persistent pain. The most common causes of pain are soft tissue
tenosynovitis, patella-related complications, malalignment, infection,
component loosening, instability, synovitis, and complex regional pain
syndrome (CRPS). Less common causes include scarring and retained
cement/osteophytes. Patients with preoperative functional limitations,
severe pain, low mental health score, or multiple medical comorbidities
are more likely to have a painful TKA and a poorer overall outcome.
careful history and clinical examination are prerequisite in making the
definitive diagnosis. Diabetic patients may have a higher propensity to
infection and neuropathic pain. Establishing the time interval between
TKA and development of pain can help with the diagnosis. For example,
presence of pain persisting since surgery suggests infection,
instability, prosthetic malalignment, or nonarticular causes. When
prosthetic infection is suspected, one should inquire about fever,
chills, and recent history of invasive procedure (e.g., dental
treatment, urologic procedures).
and global tenderness is often due to either infection or prosthetic
loosening. Constant pain is typically associated with infection,
whereas pain associated with mechanical activity is often due to either
inflammatory causes or mechanical derangement. Pain that is experienced
with weight bearing, but improves with rest, often is caused by
prosthetic loosening.
tenderness and assessing for range of motion (ROM) and stability.
Although effusion can be seen in synovitis, erythema and warmth are
more often related to joint sepsis. Presence of crepitus is often
indicative of either soft tissue impingement or severe polyethylene
liner failure leading to metal-on-metal articulation. In addition to a
thorough musculoskeletal evaluation, neurologic and vascular
assessments are important.
 |
|
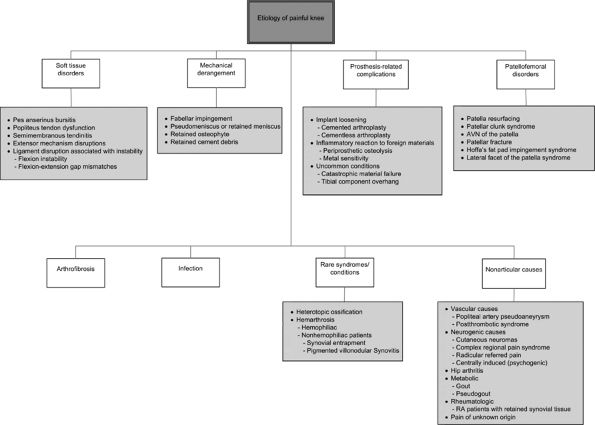
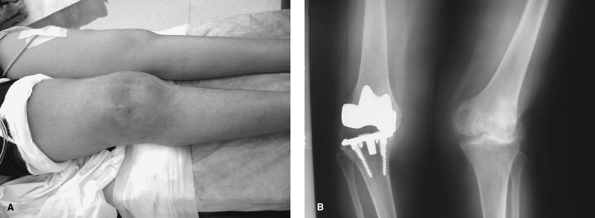
Figure 27-1 Etiology of the painful knee following total knee arthroplasty (TKA).
|
 |
|
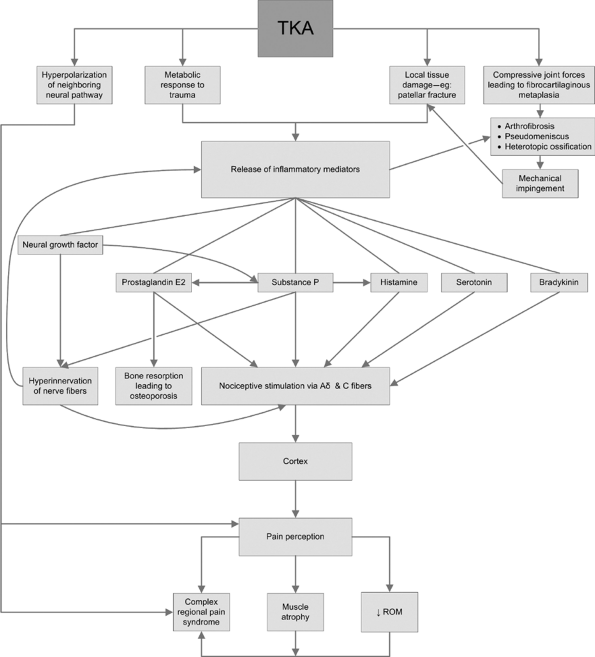
Figure 27-2 Pain pathogenesis in total knee arthroplasty (TKA).
|
 |
|
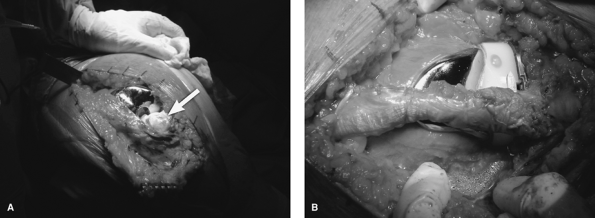
Figure 27-3 Intraoperative photographs of a 60-year-old woman who fell on her knee, suffering a painful extensor mechanism disruption. A: The small avascular patella was attached to the quadriceps tendon by thin fibrotic tissue. B:
The extensor mechanism disruption was addressed using a tendo-Achilles allograft. A Krackow stitch repair of the soft tissue ends was performed with the knee in extension. (Courtesy of Patrick Meere, MD.) |
that lies deep to the tendons of the sartorius, gracilis, and
semitendinosus. Pes anserinus bursitis is an underdiagnosed condition
in which patients (often obese females) complain of a tender
anteromedial knee mass (2 inches inferior to the medial joint line).
Pain is exacerbated with stair climbing. Although nocturnal symptoms
predominate, patients may complain of knee stiffness with limited
flexion lasting ≤1 hour during daily activities. Most symptoms are
secondary to overuse. Infrequently, symptoms can be caused by
anteromedial overhang of the tibial component, varus coronal
malalignment of the TKA components, or irritation of the pes anserinus
bursa by polyethylene debris. First-line treatment consists of rest,
nonsteroidal anti-inflammatory drugs (NSAIDs), and injection of steroid
and local anesthetics (e.g., lidocaine).
be caused by chronic subluxation of the popliteus tendon over a
retained lateral femoral condylar osteophyte or prominent overhang of
the posterolateral condyle of the femoral prosthesis. This condition
has been reported in about 0.2% of TKA patients. Patients present with
lateral knee pain often associated with either a catching sensation or
an audible snap at the posterolateral knee. Occasionally recurrent knee
effusions mimic symptoms of a septic joint. Women
are
more likely to have this condition because their relatively smaller
femoral geometry may lead to oversizing of the prosthetic component in
the medial-lateral plane. Intraoperatively, retained osteophytes, if
present, should be excised. In addition, following capsular closure of
the knee, the surgeon should perform flexion-extension maneuvers;
diagnosis of popliteus tendon dysfunction is suggested by an audible
popping sound. If no obvious source of the entrapment is apparent, the
popliteus tendon may be released from its femoral insertion.
examination; diagnostic arthroscopy may also be required. Conservative
treatment options are usually ineffective. Patients may be treated with
arthroscopic release of the popliteus tendon from its femoral insertion
site, which often provides complete symptom resolution.
about 1% of TKA patients. Symptoms include posteromedial knee pain that
develops several months following surgery. The pain intensifies with
activity, especially during standing from a seated position. Patients
with considerable preoperative varus deformity are at risk because
restoration of the mechanical axis is associated with an increase in
tension on the semimembranosus tendon. Another possible cause of
semimembranosus tendonitis is frictional irritation of the reflected
segment of the tendon inferior to the posteromedial joint line,
particularly in conjunction with osteophytes at the semimembranosus
groove.
steroid and local anesthetic injections, surgical detachment and
excision of the reflected portion of the tendon may be considered. Some
authors recommend release of the tendon at the semimembranous groove
with lengthening of the tendon to preserve dynamic knee stability.
tendon ruptures), both of which are uncommon, can be either indirect or
direct. Indirect injuries are further subclassified as high-velocity
injuries (e.g., motor vehicle accidents) and low-velocity injuries
(e.g., slip during daily activities). Hyperflexion with excessive
loading causes indirect disruptions. Direct disruptions result from
extensor mechanism laceration. Patients typically present with anterior
knee pain, weakness, and difficulty negotiating stairs. The patellar
tendon ruptures at a force 17.5 times body weight, but detachment of a
damaged tendon may occur with less force. Risk factors for these soft
tissue disruptions include previous cortisone injections and medical
conditions that compromise connective tissue integrity, such as
rheumatoid arthritis, chronic renal failure, and diabetes mellitus.
Acute disruptions are associated with inflammation and significant pain
and can be managed with direct repair; however, rerupture rates are
high, and hence one should consider augmentation with autogenous
grafts. Neglected ruptures of the patellar or quadriceps tendon
typically require direct repair with additional augmentation with
either autogenous (e.g., semitendinosus or extended medial
gastrocnemius–Achilles tendon) or allograft tissues
(quadriceps-patella–achilias tendon–tibial tubercle or achilias
tendon–calcaneal bone block) (Fig. 27-3).
with symptoms of instability and pain with deep-flexion activities
(e.g., stair descent or chair transfer). In
posterior-cruciate–retaining designs, this has been classically
described as flexion instability due to rupture of the posterior
cruciate ligament. In posterior-stabilized knees, flexion instability
may be secondary to fracture of the polyethylene
stabilizing
cam or an excessively large flexion gap created at the time of index
TKA. Additional clinical features include intra-articular effusion,
posterior tibial subluxation (sag), and pain. Tenderness is often
present over the extensor mechanism, pes anserinus tendon complex,
and/or distal iliotibial band. In highly symptomatic cases, revision
arthroplasty may be considered (Chapter 28).
consequences on knee stability and kinematics. Unsatisfactory coronal
alignment can result in unequal loading of the knee and lead to
collateral ligament strain. For example, excessive valgus is associated
with medial collateral ligament strain and tenderness. Revision
arthroplasty is often required and is discussed in the next chapter.
located within the origin of the lateral gastrocnemius tendon and is
present in 12% of adults. When the fabella is >2 cm in diameter
(mean diameter, 1 cm), there is a risk of fabella impingement following
TKA. Symptoms can develop days to months after TKA and are due to the
fabella catching on either the posterior femoral, tibial, or
polyethylene component. Patients complain of pain at the posterolateral
knee (especially with flexion), effusion, palpable popliteal mass, and
a sensation of catching. This sensation may be accompanied by a
snapping sound. Recurrent impingement leads to articular erosion and
notching of the fabella. The adjacent synovial tissue may be laden with
birefringent polyethylene particles. In patients with a large fabella
identified on preoperative radiographs, intraoperative assessment for
possible impingement is accomplished by ranging the knee and listening
for an audible snap. If present, the fabella may be excised with
electrocautery. Patients presenting with symptoms occasionally get
relief with local anesthetic injections. Excision of the fabella via a
small posterolateral incision may be required if symptoms are
refractory to conservative measures.
can catch and impinge in the tibiofemoral compartment. The suggested
pathogenesis includes the production of fibrocartilage from metaplastic
transformation of retained meniscal remnants or redundant
intra-articular synovium subject to repetitive joint compressive
forces. Patients with this condition present with persistent joint line
tenderness (posterolateral or posteromedial) about 3 to 6 months
following an initially uneventful postoperative course. Patients
complain of pain aggravated with stair descent, sometimes accompanied
by a catching sensation with knee flexion. Conservative treatment
modalities such as physical therapy, bracing, and local anesthetic
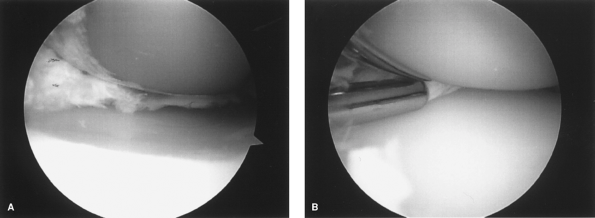
injections may provide modest relief. Arthroscopic excision of the
meniscal tissue typically provides immediate and long-lasting remission
of symptoms (Fig. 27-4).
 |
|
Figure 27-4
Arthroscopic views of medial pseudomeniscus in a 58-year-old man who presented with recurrent posteromedial pain and an associated snapping sensation. A: Before treatment. B: Arthroscopic shaver being used to debride the impinging pseudomeniscus. |
all TKAs. However, if large osteophytes remain at the distal femur or
proximal tibia, problems can arise. Patients usually present with
persistent pain, crepitus, and a knee effusion. Routine radiographs are
often negative. Surgical management consists of arthroscopy or open
arthrotomy with excision of these osteophytes. Debridement of an
associated synovitis may also improve symptoms.
primary TKA. The posterior aspect of the knee is the most common site
and can lead to pain at this location. With the increasing number of
surgeons using smaller incisions for TKA, limited surgical exposure may
result in poor visualization of the posterior compartments with
subsequent retention of fragments. Patients can present as late as
several months after TKA with severe, sharp pain associated with a
popping sensation, effusion, and decreased range of motion. Radiopaque
cement debris usually can be seen on
radiographs. Arthroscopic techniques can be used to remove cement fragments, resulting in symptom resolution.
components can develop secondary to polyethylene, metal, and/or cement
debris. If the debris particles are <15 µm in diameter, they can be
ingested by macrophages, which then release numerous inflammatory
mediators, including prostaglandin E2, tumor necrosis factor α, and
interleukins-2 and -6. The resulting inflammatory response with
subsequent activation of osteoclasts is responsible for osteolysis.
Patients present with effusion, pain, and instability. Revision TKA is
often the only solution to this significant problem.
confirmed on epicutaneous testing, is associated with nickel (Ni),
chromium (Cr), cobalt (Co), and CrCoNi alloys and occurs in 8% to 15%
of the general population. Metal sensitivity, an allergic reaction of
the periprosthetic tissues to metals, has been correlated to contact
dermatitis with possible symptom exacerbation following use of
conventional prostheses. Clinical features may include eczematid
dermatitis, generalized allergic vasculitis, aseptic loosening, and
bone necrosis resulting in pain. Pathologic evaluation of tissues can
reveal either a cell-mediated immune response or a preponderance of
immunoglobulin E antibodies. The frequency of clinically relevant
allergic responses to knee implants is unknown, but probably very low.
In at-risk patients, titanium-containing or ceramic prostheses may be
considered owing to their decreased immunogenic potential.
the femoral component and the polyethylene tibial tray.
High-molecular-weight polyethylene that has been sterilized by gamma
irradiation in air is at the highest risk for catastrophic failure.
Modular tibial inserts with suboptimal locking mechanisms can develop
wear at the backside of the polyethylene tray. Polyethylene material
failure is often associated with a painful chronic effusion and usually
occurs many years following TKA. In cases with a metal-backed patella,
the thin polyethylene segment can dissociate or wear through, leading
to metal-on-metal articulation. Patients present with a grinding or
squeaking noise and metallosis. Revision of the patella and sometimes
the femoral component usually is required.
oversizing the tibial component with respect to the underlying bony
surface. This technical error can result in painful incursion and
subsequent inflammation of the collateral ligaments. The medial
collateral ligament is more frequently involved than the lateral
collateral ligament. Patients who fail medical management, including
NSAIDs and/or local anesthetic injection, may be considered for
revision surgery.
of controversy. Approximately 10% of patients with a nonresurfaced TKA
have some persistent anterior knee pain. This may develop several years
following the index TKA. If all other diagnoses for anterior knee pain
have been excluded, the patella may be resurfaced, especially if the
clinical features are suggestive of either inflammatory arthropathy or
patellofemoral arthrosis.
patella resurfacing; it is often due to a tight lateral retinaculum,
weak vastus medialis, or more commonly an internally rotated femoral
and/or tibial component. If conservative treatment options are
unsuccessful, either an extensor mechanism realignment procedure or
revision arthroplasty may be required.
association with first-generation posterior-stabilized knee designs and
is infrequently encountered today. These first-generation implants had
a sharp transition between the anterior flange and the intercondylar
notch of the femoral component. The condition is characterized by
chronic irritation of the quadriceps tendon at the superior aspect of
the patella, where the tendon can abut the femoral housing. An
inflammatory nodule may form at the junction of the quadriceps tendon
and the proximal pole of the patella. When extending the knee from a
fully flexed position, at approximately 30 to 40 degrees, patients
experience crepitation and catching, frequently accompanied by pain.
Treatment consists of arthroscopic or open debridement of the nodule,
which is usually successful.
complicated by patellar fracture in the postoperative period. The
incidence is increased with use of a patellar implant with a large
central peg or by cutting the patella too thin. Bony resection should
match the new prosthetic implant thickness. The minimum postresection
thickness is approximately 11 mm. Fracture also may be associated with
osteonecrosis of the patella.
following use of mobile bearing TKAs. Compression of the
well-innervated fat pad by the anterior border of the polyethylene
insert results in anterior knee pain and can be associated with limited
ROM. Imaging modalities such as ultrasound and positron emission
tomography (PET) scan can aid in confirming the diagnosis.
Intraoperative findings suggestive of fat pad impingement include
tissue necrosis and sometimes an imprint of the components. If revision
surgery is undertaken, it is recommended that the fat pad be removed.
of the lateral patellar facet can lead to painful irritation of the
exposed arthritic patellar surface. Patients may complain of anterior
knee pain and can have increased radionucleotide uptake over the
patella on bone scans. Sunrise view of the patella may indicate
abutment of the lateral facet of the patella against the lateral flange
of the femoral component. Patella revision may be required for
persistent symptoms.
 |
|
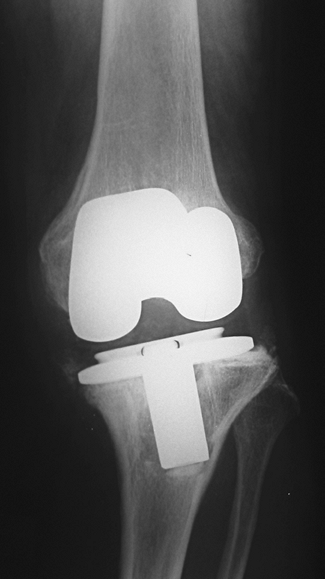
Figure 27-5 A 39-year-old woman with a history of rheumatoid arthritis who had an uneventful cementless total knee arthroplasty. A
Four years following the index procedure, she presented with a red and inflamed knee joint; sepsis was confirmed by aspiration and cultures. B Anteroposterior radiograph indicating component loosening secondary to joint infection. |
typically have a flexion contracture of >15 degrees and/or cannot
bend the knee >75 degrees. The incidence of painful postoperative
stiffness has been reported to be as high as 10%. Factors associated
with knee stiffness include limited preoperative knee ROM, multiple
previous knee surgeries, biologic predisposition, history of diabetes,
postoperative hemarthrosis, poor patient motivation, inadequate
postoperative rehabilitation, improper/insufficient bone cuts,
component malposition, tight flexion or extension gap, “overstuffing”
of the tibiofemoral or patellofemoral joint, posterior femoral/tibial
osteophytes, incorrect component size, a tight posterior cruciate
ligament, and heterotopic ossification. Histologic analysis of
arthrofibrotic tissue reveals a large population of ovoid and
spindle-shaped cells in a dense collagen matrix. Macroscopic variants
include simple fibrous bands, exuberant parasynovial fibrous
hypertrophy (often in the intercondylar notch), and extensive
panarticular scar formation. With diminished ROM, quadriceps work is
increased with walking (67 degrees is required for normal gait).
Patients may encounter difficulty negotiating stairs and rising from a
chair, as these tasks require 85 and 95 degrees of flexion,
respectively. Surgical intervention can be early or late. For patients
with stiffness within 6 to 12 weeks following TKA, manipulation under
anesthesia can be performed. Patients with chronic stiffness may be
treated with an arthroscopic or open lysis of adhesions. Revision
arthroplasty may be necessary if implant-related causes have been
diagnosed.
to be 1% to 2%. Susceptibility factors include a compromised immune
system, obesity, smoking, peripheral vascular disease, venous
insufficiency, history of skin ulcers, use of oral steroids, multiple
previous surgeries, rheumatoid arthritis, history of knee infection,
and recurrent urinary tract infection. Infections following TKA can be
categorized as superficial or deep. The deep infections can be further
subdivided into direct and hematogenous (seeding from distant infection
site). The most common organisms are Staphylococcus aureus (coagulase-positive) and Staphylococcus epidermis
(coagulase-negative). Patients may present with pain, swelling, febrile
episodes, erythema, decreased ROM, and sometimes wound drainage (Fig. 27-5).
infections are identified early (<6 weeks) with well-fixed
components, an attempt can be made to perform an open, radical
debridement with exchange of the tibial insert. Polyethylene exchange
is important because the glycocalyx “slime” layer that deposits on the
polyethylene bearing can promote recurrence. In cases diagnosed beyond
6 weeks, the following options are considered: primary exchange,
two-stage (delayed) exchange, resection arthroplasty, arthrodesis, or
amputation. If reimplantation (primary or two-stage) is considered,
organism-specific antibiotic-impregnated cement should be used. The
most predictable results are achieved with the two-stage exchange
method.
Antibiotic suppression can be used in patients with stable implants who
are not suitable candidates for surgical intervention and who are
infected with a low-virulence organism.
first three postoperative months. It occurs in 5% to 15% of TKA
patients, although it is symptomatic in <1% of patients.
Presentation is variable and may consist of vague discomfort,
stiffness, and, in very rare cases, persistent pain and snapping. New
bone formation is evident on radiographs within 3 months following
surgery and usually does not change after the first year.
surgery, high-risk patients may be given prophylaxis using either a
course of indomethacin or radiation. In the occasional patient who
experiences symptoms that fail to respond to conservative therapy,
surgical excision of the HO may be necessary.
(mean 2 years) following TKA. The incidence is approximately 5%, and
the underlying cause is frequently unknown. In some cases, the
pathogenesis is characterized by synovial proliferation secondary to
polyethylene, metal, or cement debris, which can frequently bleed owing
to entrapment or microtrauma. Tissue histology reveals focal synovial
hyperplasia containing histiocytes and hemosiderin deposits. Other
possible causes include clotting disorders such as hemophilia, chronic
use of anticoagulants, remnant posterior cruciate ligament stump
trauma, intercondylar notch fibrosis, pigmented villonodular synovitis,
juxta-articular arteriovenous malformation, tumor, component loosening,
and knee instability (including flexion instability).
decreased range of motion. Coagulation studies are often normal. In the
acute setting, knee aspiration is diagnostic and typically reveals
bright red blood. In rare cases angiography may aid in identifying the
source of bleeding. Initial management consists of short-term rest,
application of ice, limb elevation, splinting, and discontinuation of
anticoagulant medication. In patients who fail conservative treatment
or who have recurrent hemarthrosis, arthroscopic synovectomy can be
considered. In refractory cases, implant revision may provide a
satisfactory long-term outcome.
complications (0.03% to 1.2%). Pseudoaneurysm of the popliteal artery
is a rare and painful vascular complication that, if untreated, can
result in loss of the operated limb. About 40% of cases are diagnosed
within 1 month of disease onset. Symptoms include a painful and
pulsatile mass that produces bruits and/or thrills and is usually
associated with ecchymosis overlying the popliteal region. In addition,
distal pulses may be weak. Magnetic resonance imaging (MRI) can be used
to confirm the diagnosis of popliteal artery pseudoaneurysm.
thrombosis (DVT) secondary to stasis, endothelial damage, and increased
blood viscosity (the Virchow triad). DVT may precipitate chronic venous
insufficiency, and patients may present with a painful, swollen lower
limb, sometimes associated with ulceration. Clinical findings can be
confirmed with venous Doppler studies. Patients should be treated with
compression stockings and referred to a vascular specialist.
secondary to a cutaneous neuroma. A neuroma may develop when the
infrapatellar branch of the saphenous nerve, medial femoral cutaneous
nerve of the thigh, or medial/lateral retinacular nerves are divided at
the index procedure. Conservative measures for neuropathic pain include
topical steroids, iontophoresis, transcutaneous electrical stimulation,
and medications. If symptoms last >6 months, nerve blocks and
selective denervation procedures may be considered.
reflex sympathetic dystrophy (RSD) or Sudeck atrophy, is a diagnosis of
exclusion and arises from autonomic dysfunction. It is a complex
interplay of four factors: a local trigger (e.g., surgical trauma),
psychologic factors, systemic factors associated with pain exacerbation
(e.g., peripheral neuropathy), and sympathetically maintained pain. It
is thought to occur in about 0.5% of TKA patients. There is a wide
variation in disease presentation. Symptoms may include intense burning
or prolonged pain in nonanatomic distributions, sensory abnormalities
such as allodynia or hyperalgesia that are out of proportion to the
physical examination findings, edema, sudomotor disruptions such as
sweating, trophic changes such as smooth, shiny skin, cold intolerance,
vasomotor disturbances such as hyperhidrosis and coolness to the touch,
stiffness, and weakness. Patients with anxiety and severe pain
preoperatively are more likely to develop CRPS. Although there may be a
psychologic overlay in CRPS, it is unclear whether the psychologic
factors predispose patients to this condition or are a result of this
syndrome. Although diffuse pain and hypersensitivity suggest the
presence of CRPS, the extensive variability of clinical symptoms
warrants a thorough workup to exclude other causes (e.g., mechanical,
prosthetic, or soft tissue causes).
be appreciated on plain radiographs. Technetium-99m bone scans may
reveal increased uptake in affected regions. Sympathetic block is
useful, both as a diagnostic and therapeutic modality.
medications, and physical therapy. Narcotics and benzodiazepines are
contraindicated in these patients. Instead, anesthetic sympathetic
blockade can provide long-term pain relief. Lumbar sympathectomy can be
attempted for recalcitrant symptoms.
and none is applicable. The incidence of severe pain without
identifiable cause following TKA is about 6%. Associated clinical
factors may include history of multiple procedures, fibromyalgia,
unreasonable patient expectations, injuries with workers’ compensation
issues, and patients who had minimal joint disease as determined
radiographically prior to TKA.
basic laboratory tests to rule out infection. The usual tests consist
of the following:
-
Erythrocyte sedimentation rate (ESR)
-
Returns to normal 3 to 6 months following
TKA. Thus, interpretation of this test in the context of the early and
intermediate painful TKA may be difficult. -
ESR of >30 has a sensitivity of 80% and a specificity of 63% in predicting infection.
-
-
C-reactive protein (CRP)
-
An acute-phase protein that returns to normal within 3 weeks following TKA.
-
The most useful laboratory test to rule out infection.
-
-
Complete blood count (CBC)
-
Often normal but can be useful when reviewed with ESR and CRP.
-
Lymphocyte count of <1,500 cells/mm2 is associated with a more than threefold risk of wound complications.
-
-
Knee aspiration
-
All aspirated fluid should be sent for
microscopy and cultures (aerobic and anaerobic bacteria, fungi, and
tubercle bacilli). Gram stain has limited sensitivity (10%). -
For diagnosis of infection, knee aspiration has a positive-predictive value of 89.5% and a negative-predictive value of 84.5%.
-
Use of antibiotics increases the
false-negative rate. Ideally antibiotics should be stopped at least 2
weeks prior to aspiration when chronic infection is suspected.
-
-
Synovial biopsySynovial biopsy can be performed either arthroscopically
or open. The following conclusions can be made based on high-power view:-
A count of ≥10 polymorphonuclear leucocytes (PMNs) per high-power field (HPF) is predictive of infection.
-
A count of 5 to 9 PMNs per HPF is not always consistent with infection.
-
A count of <5 PMNs per HPF reliably excludes infection.
-
-
Conventional radiographs
-
Anteroposterior (AP), lateral, and
sunrise views to assess for malposition, patella tilt, periprosthetic
fractures, and radiolucent lines. -
Checking for radiographic signs of loosening:
-
Tibial component bone/cement interface is
broken down into five to seven zones, depending on whether or not a
stem is present (as seen on AP view). -
Femoral component bone/cement interface
is broken down into five to seven zones, depending on whether or not a
stem is present (as seen on lateral view). -
Patellar component bone/cement interface
is broken down into three to five zones, depending on number of
fixation lugs (as seen on sunrise view). -
The width of radiolucent lines for each
zone is measured in millimeters. The total widths are added for each
zone for all three components. -
For each component, if the cumulative
total widths are ≤4 and these lines have been nonprogressive on
subsequent radiographs, the component is not significant for implant
loosening; cumulative total widths of 5 to 9 should be followed
closely, as loosening is likely; cumulative total widths of ≥10 signify
failure or impending failure.
-
-
Special films may occasionally be required:
-
Full-length radiograph: To assess overall limb alignment.
-
Oblique films: To evaluate for periprosthetic osteolysis.
-
Dynamic fluoroscopy: To confirm mechanical derangement (e.g., fabella impingement), component loosening, and instability.
-
Fluoroscopically positioned radiographs:
May be obtained to gain perfectly tangential views of uncemented
implant bone/prosthesis interfaces. These radiographs are useful in
evaluation of uncemented knee component loosening.
-
-
-
Arthrography
-
An invasive nonspecific test that may help diagnose component loosening (especially tibial).
-
Current use is limited and superseded by other tests described below.
-
-
Ultrasound
-
Permits dynamic, real-time evaluation of moving structures such as muscles and tendons.
-
Often unavailable.
-
-
Sinography
-
Can be used to determine whether a draining sinus communicates with the knee joint.
-
-
Technetium-99m bone scintigraphy
-
Although a negative scan rules out
significant knee pathology, a positive scan is nonspecific. Positive
scans are seen most commonly in infection, component loosening, stress
fracture, and bone remodeling.
-
-
Computed tomography scan
-
Significant metal artifact can arise.
-
Newer reformatting software allows for
artifact suppression and improved imaging of bone/cement and
cement/implant interfaces and allows for better quantification of
osseous defects.
-
-
Magnetic resonance imaging
-
Conventional MRI sequences have extensive metallic susceptibility artifact.
-
Newer metal subtraction software programs
aid in diagnosis of various soft tissue and bone-related causes of
painful TKA, e.g., collateral ligament disruptions, bursitis,
synovitis, fat pad scarring, intramuscular hematoma, pigmented
villonodular synovitis, and osteolysis.
-
examination, diagnostic procedures, and possible treatment options of
painful TKA is presented in Figure 27-6.
 |
|
Figure 27-6 Diagnostic evaluation and management of pain following TKA.
|
patients presenting with pain following TKA can be a diagnostic
challenge even for the experienced surgeon. A systematic approach is
essential to elucidating the cause of a painful TKA. Patients with
definable causes of knee pain following TKA such as loosening,
malalignment, oversized components, or heterotopic ossification improve
most predictably from surgical intervention. Revision TKA performed
prior to defining a specific cause for the patient symptoms can lead to
inferior functional results and persistent or worsened symptoms.
