The Facial Nerve
cranial nerve (CN VII) has two components: the motor root, which makes
up about 70% of the fibers, and the sensory root, which accounts for
30%. The motor portion innervates the muscles of facial expression and
the muscles of the scalp and ear. The sensory root (nervus intermedius
of Wrisberg) contains both sensory and autonomic fibers. It carries
parasympathetic secretory fibers to the submandibular and sublingual
salivary glands and to the lacrimal gland. Its most important sensory
function is to mediate taste from the anterior two-thirds of the
tongue. Anatomically the motor division of the nerve is separate from
the sensory and parasympathetic portions.
expression arises from the lower third of the contralateral precentral
gyrus in the facial area of the motor homunculus and descends in the
corticobulbar tract into the pons, then decussates to converge on the
facial nuclei. The portion of the nucleus that innervates the lower
half to two-thirds of the face has predominantly contralateral
supranuclear control; the portion that innervates the upper third to
half has bilateral control.
assessment of the actions of the muscles of facial expression. A great
deal can be learned from simple inspection. At rest the face is
generally symmetric, at least in young individuals. With aging, the
development of character lines may cause asymmetry that does not
indicate disease. Note the tone of the muscles of facial expression,
and look for atrophy and fasciculations. Note the resting position of
the face and whether there are any abnormal muscle contractions. Note
the pattern of spontaneous blinking for frequency and symmetry. A
patient with parkinsonism may have infrequent blinking and an immobile,
expressionless, “masked” face. Facial dystonia causes an abnormal fixed
contraction of a part of the face, often imparting a curious facial
expression. Progressive supranuclear palsy may cause a characteristic
facial dystonia with knitting of the brows and widening of the
palpebral fissures (omega sign). Synkinesias are abnormal contractions
of the face, often subtle, synchronous with blinking or mouth
movements; they suggest remote facial nerve palsy with aberrant
regeneration. Spontaneous contraction of the face may be due to
hemifacial spasm (HFS). Other types of abnormal involuntary movements
that may affect the facial muscles include tremors, tics, myoclonic
jerks, chorea, and athetosis.
note whether there is any asymmetry in forehead wrinkling or in the
width of the palpebral fissures with the face at rest. A flattened
nasolabial fold with symmetric forehead wrinkles suggests a central
(upper motor neuron) facial
palsy;
a flattened nasolabial fold with smoothing of the forehead wrinkles on
the same side suggests a peripheral (lower motor neuron) facial nerve
palsy. Eyelid position and the width of the palpebral fissures often
provide subtle but important clinical clues. A unilaterally widened
palpebral fissure suggests a facial nerve lesion causing loss of tone
in the orbicularis oculi muscle, the eye closing sphincter; this is
sometimes confused with ptosis of the opposite eye. It is a common
misconception that facial nerve palsy causes ptosis.
expression as the patient talks, smiles, or frowns. Have the patient
grin, vigorously drawing back the angles of the mouth and baring the
teeth. Note the symmetry of the expression, how many teeth are seen on
each side and the relative amplitude and velocity of the lower facial
contraction. Have the patient close her eyes tightly and note the
symmetry of the upper facial contraction. How completely the patient
buries the eyelashes on the two sides is a sensitive indicator of
comparative orbicularis oculi strength.
the eyebrows, singly or in unison, and noting the excursion of the brow
and the degree of forehead wrinkling; close each eye in turn; corrugate
the brow; puff out the cheeks; frown; pucker; whistle; alternately
smile and pucker; contract the chin muscles; and pull the corners of
the mouth down in an exaggerated frown to activate the platysma. The
platysma can also be activated by having the patient open the mouth
against resistance or clinch the teeth. The patient may smile
spontaneously after attempting to whistle, or the examiner may make an
amusing comment to assess emotional facial movement. Because of their
paucity of facial expression, patients with Parkinson disease may fail
to smile after being asked to whistle: the whistle-smile (Hanes) sign.
detect mild weakness. It is difficult to pry open the tightly shut
orbicularis oculi in the absence of weakness. Vigorously pulling with
the thumbs may sometimes crack open a normal eye. If the examiner can
force the eye open with her small fingers, then the orbicularis oculi
is definitely weak. Likewise, it is difficult to force open the tightly
pursed lips in a normal individual. When the orbicularis oris sphincter
is impaired, the examiner may be able to force air out of the puffed
cheek through the weakened lips. With stapedius weakness, the patient
may complain of hyperacusis, especially for low tones.
The peripheral receptors are the taste buds embedded in the tongue
epithelium, and to a lesser extent in the soft palate and epiglottis.
Taste is also carried through CN IX and probably CN X. There are four
primary tastes, in order of decreasing sensitivity in humans: bitter,
sour, sweet, and salty. A fifth modality, umami (delicious or savory),
may exist in response to compounds of some amino acids. The many
flavors encountered in life are a combination of the four primary
tastes plus olfaction and oral sensory information (“mouth feel”).
Sweet and salty substances are most commonly employed for clinical
bedside testing due to their ready availability. Cranial nerve VII only
subserves taste on the anterior two-thirds of the tongue. When the
tongue is retracted into the mouth, there is rapid dispersion of the
test substance outside the area of interest. The tongue must therefore
remain protruded throughout testing of an individual substance, and the
mouth must be rinsed between tests.
tongue protruded, instructions must be clear in advance. A damp
applicator stick may be dipped into a packet of sugar, artificial
sweetener or salt and coated with the test substance, then placed on
one side of the patient’s tongue and rubbed around. The patient signals
whether she can identify the substance. Most patients will identify the
test substance in less than 10 seconds. Taste sensation is less on the
tip of the tongue, and the substance is best applied to the dorsal
surface at about the junction of the anterior and middle third of the
tongue. The sweetness of artificial sweeteners such as saccharine and
aspartame is more intense, and they may make better test substances
than ordinary sugar.
|
TABLE 12.1 Possible Causes of Disturbed Taste
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
taste is the evaluation of facial nerve palsy. If a patient with a
peripheral pattern of facial weakness has impaired taste, the lesion is
proximal to the junction with the chorda tympani. A lesion at or distal
to the stylomastoid foramen (e.g., in the parotid gland) does not
affect taste.
hypogeusia, taste perception is blunted or delayed. Perversions or
abnormal perceptions of taste are parageusias. Some causes of disturbed
taste are listed in Table 12.1.
movements, account for the preponderance of clinical abnormalities of
facial nerve function. Changes in sensation, primarily taste, and in
secretory function sometimes occur as a sidebar, but are rarely if ever
the major manifestation of disease of CN VII. Changes in these
functions can help to localize the lesion along the course of the
nerve. The major branches in sequence are the greater superficial
petrosal, nerve to the stapedius, and chorda tympani, after which the
nerve continues to the facial muscles. The mnemonic tear-heartaste-face
may help recall the sequence.
peripheral, or lower motor neuron; and central, or upper motor neuron.
Peripheral facial palsy (PFP) may result from a lesion anywhere from
the CN VII nucleus in the pons to the terminal branches in the face.
Central facial palsy (CFP) is due to a lesion involving the
supranuclear pathways before they synapse on the facial nucleus. PFP
results from an ipsilateral lesion, whereas CFP, with rare exception,
results from a contralateral lesion.
 |
|
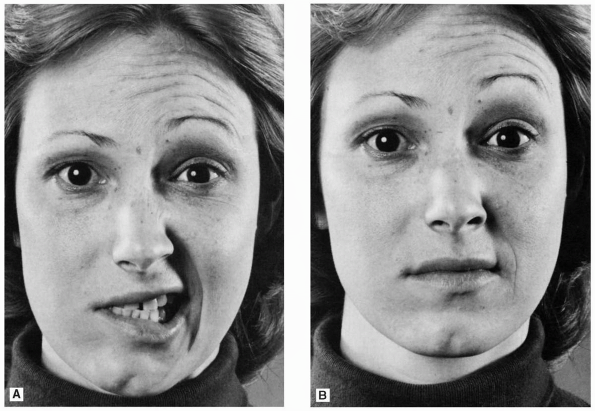
FIGURE 12.1 • A patient with a peripheral facial nerve palsy on the right. A. Patient is attempting to retract both angles of the mouth. B. Patient is attempting to elevate both eyebrows.
|
of facial expression on the involved side, both upper and lower face,
and the paralysis is usually complete. The affected side of the face is
smooth; there are no wrinkles on the forehead; the eye is open; the
inferior lid sags; the nasolabial fold is flattened; and the angle of
the mouth droops (Figure 12.1). The patient
cannot raise the eyebrow, wrinkle the forehead, frown, close the eye,
laugh, smile, bare the teeth, blow out the cheeks, whistle, pucker,
retract the angle of the mouth, or contract the chin muscles or
platysma on the involved side. She talks and smiles with one side of
the mouth, and the mouth is drawn to the sound side on attempted
movement. The cheek is flaccid and food accumulates between the teeth
and the paralyzed cheek; the patient may bite the cheek or lip when
chewing. Food, liquids, and saliva may spill from the corner of the
mouth. The cheek may puff out on expiration because of buccinator
weakness. The facial asymmetry may cause an apparent deviation of the
tongue. A patient with an incomplete PFP may be able to close the eye,
but not with full power against resistance. Inability to wink with the
involved eye is common. The palpebral fissure is open wider than
normal, and there may be inability to close the eye (lagophthalmos).
During spontaneous blinking, the involved eyelid tends to lag behind,
sometimes conspicuously. Attempting to close the involved eye causes a
reflex upturning of the eyeball (Bell phenomenon). The iris may
completely disappear upwardly.
fine vibrations palpable with the thumbs or fingertips resting lightly
on the lids as the patient tries to close the eyes as tightly as
possible. Labials and vowels are produced by pursing the lips; patients
with peripheral facial weakness have a great deal of difficulty in
articulating these sounds. Because of weakness of the lower lid
sphincter, tears may run over and down the cheek, especially if there
is corneal irritation because of inadequate eye protection. A lack of
tearing may signal very proximal involvement, above the origin of the
greater superficial petrosal nerve. With severe weakness, the eye never
closes, even in sleep.
and spontaneous contraction. There is no dissociation. With a severe
lesion, the passage of time may lead to atrophy of the involved
muscles. With PFP the motor limb of the direct corneal reflex is
impaired but the consensual is intact; in the opposite eye the direct
response is intact and the consensual impaired (Table 12.1);
in other words, the involved eye does not blink no matter which side is
stimulated, and the normal eye does blink no matter which side is
stimulated. In comatose or otherwise uncooperative patients, facial
movements can be elicited by painful pressure over the supraorbital
nerves, or by other painful stimuli applied to the face to elicit an
avoidance response.
same with lesions anywhere along the course of the nerve proximal to
the pes anserinus. Diagnostic localization depends on the associated
findings, such as hyperacusis, decreased tearing, impaired taste, and
involvement of neural structures beyond CN VII. The most common cause
of PFP by far is Bell palsy.
follows a viral infection or an immunization. Symptoms often begin with
pain behind the ear, followed within a day or two by facial weakness.
There is peripheral facial weakness involving both upper and lower
face. The paralysis is complete in approximately 70% of patients. About
25% of patients report some degree of facial numbness that is often
dismissed as an odd sensation related to the immobility. Depending on
the relationship of the lesion to the geniculate ganglion, to the
takeoff of the chorda tympani, and to the takeoff of the branch to the
stapedius, patients may note loss of taste sensation on the ipsilateral
anterior two-thirds of the tongue, dryness of the eye, or hyperacusis
for low tones.
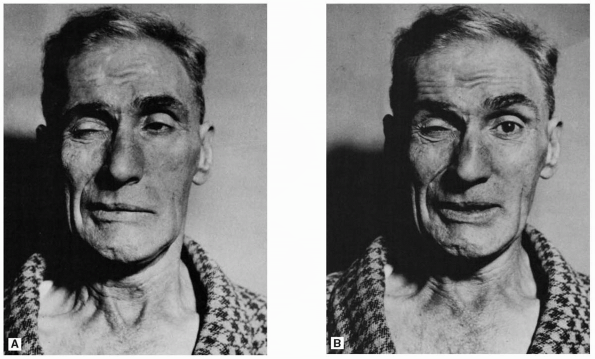
after traumatic nerve injury. Axons destined for one muscle regrow to
innervate another, so that there is abnormal twitching of the face
outside the area of intended movement. On blinking or winking, the
corner of the mouth may twitch. On smiling the eye may close (Marin
Amat sign, Figure 12.2). These synkinesias can be
prominent in some patients; more often they are subtle, such as a
slight twitch of the orbicularis oris synchronous with blinking of the
eye. Aberrant regeneration may also involve autonomic and taste fibers.
The syndrome of crocodile tears is a gustatory-lacrimal reflex,
characterized by tearing when eating, especially highly flavored foods.
It is due to misdirection of salivary axons to the lacrimal gland. Frey
auriculotemporal syndrome is similar, but with sweating and flushing
over the cheek rather than lacrimation.
 |
|
FIGURE 12.2 • Facial synkinesias following right peripheral facial paralysis. A. Patient attempting to close the eye. B. Patient attempting to retract the angle of the mouth.
|
involving the motor neurons of the CN VII nucleus in the pons include
motor neuron disease and Möbius syndrome. In spinobulbar muscular
atrophy (Kennedy syndrome), facial fasciculations and facial weakness
are often prominent. Facial nerve paralysis, unilateral or bilateral,
may be congenital. Möbius syndrome (congenital oculofacial paralysis)
is the association of congenital facial nerve palsy with paralysis of
the extraocular muscles, especially the lateral rectus, due to
hypoplasia or aplasia of the cranial nerve nuclei.
may cause PFP. There are usually associated findings to indicate the
lesion is intramedullary. Many disorders may affect the intrapontine
fibers of CN VII. Ischemic lesions are common. Because of the proximity
of the nucleus and fibers of CN VII to the nucleus and fibers of CN VI,
pontine lesions frequently cause both an ipsilateral facial paralysis
and an ipsilateral lateral rectus paralysis.
acoustic neuroma and meningioma, commonly extend to involve CN VII, the
nervus intermedius, CN VIII, CN V, the cerebellar peduncles, and the
cerebellum. There is usually hearing loss, facial sensory changes,
ipsilateral ataxia, and nystagmus. In Ramsay Hunt syndrome (herpes
zoster oticus) the PFP is due to a reactivation of varicella zoster
virus involving the geniculate ganglion. There may be vesicles on the
tympanic membrane, in the external auditory canal, on the lateral
surface of the pinna and in the cleft between the ear and mastoid
process.
increased risk of developing acute PFP. Slowly progressive facial
weakness can occur with neoplasms involving either the pons or the
facial nerve peripherally. Both HIV infection and Lyme disease can
occasionally present with facial neuropathy. PFP due to Lyme disease is
particularly prone to be bilateral. Fractures of the petrous bone due
to closed head injury may injure the facial nerve. Melkersson syndrome
(Melkersson-Rosenthal syndrome) is characterized by recurrent attacks
of facial palsy, nonpitting facial and lip edema, and a congenitally
furrowed and fissured tongue (lingua plicata, scrotal tongue); it is
sometimes familial and usually begins in childhood. Its cause is
unknown.
bilateral PFP; it is much less common but much more ominous than
unilateral PFP. Bilateral facial weakness can also occur because of
neuromuscular disorders, including myasthenia gravis, bulbospinal
neuronopathy, and muscle disease. Myopathic facies are particularly
typical of facioscapulohumeral muscular dystrophy.
VII, the differential diagnosis includes bilateral Bell palsy,
sarcoidosis, Lyme disease, diabetes, head trauma, HIV infection,
Guillain-Barré syndrome, Miller Fisher syndrome, carcinomatous or
lymphomatous meningitis, tuberculous or fungal meningitis, pontine
tumor, Melkersson-Rosenthal syndrome, pseudotumor cerebri, Möbius
syndrome, and a long list of other conditions.
palsy (CFP), there is weakness of the lower face, with relative sparing
of the upper face. The upper face has both contralateral and
ipsilateral supranuclear innervation, and cortical innervation of the
facial nucleus may be more extensive for the lower face than the upper.
The paresis is rarely complete.
prior to their synapse on the facial nerve nucleus will cause a CFP.
Lesions are most often in the cortex or internal capsule. There is
considerable individual variation in facial innervation, and the extent
of weakness in a CFP may vary from the lower half to two-thirds of the
face. The upper face is not necessarily completely spared, but it is
always involved to a lesser degree than the lower face.
in a CFP, the patient is always able to close the eye, Bell phenomenon
is absent, the corneal reflex is present, and the orbicularis oculi
reflex may be exaggerated. In CFP the lower face is weak, the
nasolabial fold is shallow, and facial mobility is decreased. However,
the lower face weakness is never as severe as with a PFP, which
suggests that there may be some direct cortical innervation to the
lower face as well as the upper. Separating CFP and PFP is rarely
difficult.
voluntary; and (b) emotional, or mimetic. In most instances of CFP, the
facial asymmetry is present both when the patient is asked to smile or
show the teeth, and during spontaneous facial movements such as smiling
and laughing. However, spontaneous movements and deliberate, willful
movements may show different degrees of weakness. When asymmetry is
more apparent with one than the other, the facial weakness is said to
be dissociated. Facial asymmetry more apparent with spontaneous
expression, as when laughing, is called a mimetic, emotive, or
emotional facial palsy; weakness more marked on voluntary contraction,
when the patient is asked to smile or bare her teeth, is called a
volitional facial palsy. Volitional facial palsy may result from a
lesion in the cortex or in the subcortical corticobulbar pathways as
they go through the internal capsule, the cerebral peduncle, or the
pons above the facial nucleus. Facial weakness seen only with emotional
movements most commonly results from thalamic or striatocapsular
lesions, usually infarction, rarely with brainstem lesions.
movements rather than weakness. Common disorders causing abnormal
facial movements include aberrant regeneration due to facial nerve
palsy, blepharospasm, hemifacial spasm, and facial myokymia. Hemifacial
spasm (HFS) usually arises de novo, due to intermittent compression by
an ectatic arterial loop in the posterior circulation, most often a
redundant loop of the anterior inferior cerebellar artery. The
compression is usually near the anterior aspect of the root exit zone;
arterial pulsations are thought to cause demyelination and focal nerve
damage leading to ephaptic transmission and ectopic excitation.
Hemifacial spasm usually develops in older patients. Twitching usually
begins in the orbicularis oculi, and initially may be subtle and
difficult to distinguish from facial synkinesias. Fully developed HFS
causes repetitive, paroxysmal, involuntary, spasmodic, tonic, and
clonic contractions of the muscles innervated by the facial nerve on
the involved side of the face. The mouth twists to the affected side,
the nasolabial fold deepens, the eye closes, and there is contraction
of the frontalis muscle (Figure 12.2).
Synkinesias due to aberrant regeneration following PFP may cause
movements resembling HFS. The essential difference is that synkinesias
are provoked by a voluntary movement, whereas HFS is a spontaneous,
involuntary contraction. Blepharospasm causes involuntary twitching
that primarily involves the orbicularis oculi and frontalis muscles.
Blepharospasm is most often idiopathic or “essential” and is a form of
focal dystonia. It is most often bilateral. Tic, or habit spasm, can
cause a movement resembling HFS or blepharospasm. Bizarre grimacing
movements of the face are usually habit spasms.
quivering that has a rippling, wormlike, appearance. It is usually
unilateral. Facial myokymia has been reported with numerous conditions,
most intrinsic to the brainstem. It is a classic feature of multiple
sclerosis, but may also occur with pontine tumor, Guillain-Barré
syndrome, and other conditions. Disease of the basal ganglia or
extrapyramidal system may involve the facial muscles causing
hypokinesia or hyperkinesia. Parkinson disease causes hypokinesia.
Forms of facial hyperkinesias include dyskinesias,
choreiform,
athetoid, dystonic, grimacing, and myoclonic movements and tremors.
Oral-facial dyskinesias are common, most often as a tardive
manifestation of psychoactive drug use.
are not a common part of facial nerve lesions. Taste may be affected
with lesions of the facial nerve proximal to the takeoff of the chorda
tympani. Geniculate neuralgia causes paroxysmal pain deep in the ear,
sometimes radiating to the face. Cranial nerve VII is involved in
lacrimation and salivation; lesions of the nerve at or proximal to the
geniculate ganglion can cause abnormalities of these functions.
