Primary Benign Tumors
percentage of patients who seek medical attention for symptoms
originating in the spine. Delays in diagnosis can occur if a physician
is not aware of the features that distinguish spinal tumors from
nonneoplastic spinal disorders. Advances in imaging techniques allow
earlier diagnosis and more sophisticated preoperative evaluation and
staging of spinal tumors. Advances in systemic therapy, surgical
implants, biomaterials, and surgical procedures have improved greatly
short-term and long-term outcomes in tumor patients. The principles of
orthopaedic oncology that apply to the extremities may not always be
applicable to the spine.
all bone tumors and are much less common than metastatic lesions.
Benign primary lesions affecting the spinal column are far less common
than malignant primary tumors. Diagnosing primary benign tumors of the
spine requires a high index of suspicion. Spinal tumors occur in
patients of all ages and at any level of the spine. Primary spinal
tumors in children and adolescents are usually benign. Benign tumors
are rare in elderly patients. In one series of patients with primary
spinal tumors, nearly 70% of patients age 18 years or younger had
benign spinal lesions. Of tumors in patients older than age 18 years,
only 20% were benign. The mean age at diagnosis was 20.9 years for
patients with benign tumors.
and posterior elements of the spine, with a slight overall predilection
for the posterior elements. Location of the lesion is an important
factor in determining the type of tumor. Osteoid osteoma and
osteoblastoma have a tendency to affect the posterior elements, whereas
eosinophilic granuloma (EG) and hemangioma tend to involve the
vertebral body.
presenting with primary benign spinal tumors. In one series, pain was
the chief complaint in nearly 85% of patients with spinal tumors. Pain
usually is localized to the site of the lesion in the neck or back, but
radicular pain is not atypical. The pain is characterized classically
as progressive, gradual in onset, worse at night, and often unrelated
to activity. Occasionally, patients may associate the onset of symptoms
with a traumatic episode, which may be the case when fracture occurs in
an already compromised vertebra. Pathologic fracture also should be
considered, however, when patients report the acute onset of pain in
the absence of severe trauma. In the case of nerve root compression by
tumor or as the result of vertebral collapse, patients may present with
radicular symptoms. Less commonly, patients may have weakness; bowel or
bladder incontinence; palpable mass; or constitutional symptoms such as
fevers, chills, night sweats, weight loss, and anorexia. Spinal
deformity also may result from spinal tumors. Focal kyphosis can result
from any tumor that causes vertebral body collapse. Scoliosis is a
common presentation of osteoid osteoma and osteoblastoma in younger
patients.
diagnosing primary spinal tumors. Focal tenderness is more common with
spinal tumors than in nonneoplastic disease. Thorough inspection of the
entire spine, including the forward bending test, is essential to look
for any curvature of the neck or back. Torticollis or scoliosis,
especially when associated with pain, can be attributed to spinal
tumors. Although a tumor rarely presents with a palpable mass, it is
important to palpate along the spinous processes from occiput to sacrum
and the paraspinous areas. Subtle findings, such as a stiff neck or
back, may be the only clues to recognizing a benign spinal tumor.
in establishing a diagnosis. Complete blood cell count, erythrocyte
sedimentation rate, and C-reactive protein level usually are obtained.
In most patients with benign primary spinal tumors, the results of
laboratory studies are normal.
identifying benign spinal tumors. Before a bone lesion can be detected
by plain radiography, at least 30% to 50% bone loss must be present. If
scoliosis is evident radiographically, spinal tumor must be included in
the differential diagnosis. Technetium bone scanning is much more
sensitive than biplanar radiography because it measures bone activity
and can identify small lesions before extensive bone loss. Computed
tomography (CT) has become a valuable imaging tool, particularly in
evaluating bone anatomy and determining the amount of canal compromise
after pathologic fracture of the spine. CT is not the best screening
tool, however, because it does not image the entire spine. Magnetic
resonance imaging (MRI) has become the criterion standard in the
diagnosis of primary benign spinal tumors. MRI can detect the presence
of a bone lesion, identify the presence of neural compression, and
determine the involvement of the surrounding soft tissue. This
information is crucial for treatment planning.
-
Osteochondroma
-
Osteoid osteoma
-
Osteoblastoma
-
Hemangioma
-
Aneurysmal bone cyst (ABC)
-
EG and giant cell tumor (GCT)
presentation, location, imaging characteristics, and treatment. Each
tumor type is discussed individually, with the exception of osteoid
osteoma and osteoblastoma, which are differentiated primarily by size.
or radicular or referred-type pain into the extremities, osteoid
osteoma and osteoblastoma should be included in the differential
diagnosis. Osteoid osteoma and osteoblastoma are identical
histologically and have similar clinical presentations. Pain usually is
the first and only complaint of patients with these lesions. The pain
associated with osteoid osteoma classically is relieved with aspirin
when it involves the extremities, but this finding is not as consistent
when the spine is involved. The only physical examination findings that
may be present are spinal stiffness and spinal curvature in the form of
scoliosis or torticollis. A few features distinguish between these two
benign lesions (Table 10-1).
cause for the deformity needs to be sought when pain is an associated
complaint. Benign osteoid osteoma and osteoblastoma may be the most
common causes of scoliosis provoked by pain. These tumors, which often
are difficult to view radiographically, tend to involve the cancellous
lamina and pedicle of the vertebra but have been found in rib heads
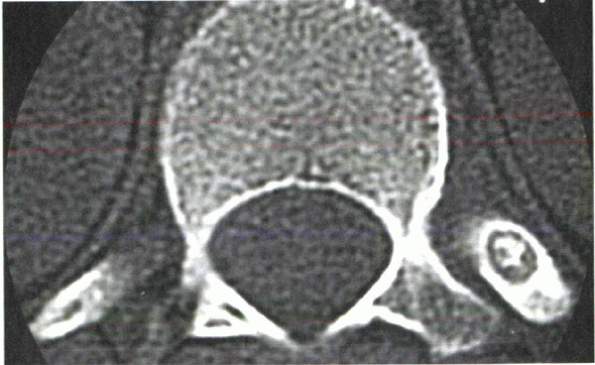
adjacent to thoracic vertebrae (Fig. 10-1).
|
TABLE 10-1 DISTINGUISHING FEATURES OF OSTEOID OSTEOMA AND OSTEOBLASTOMA
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
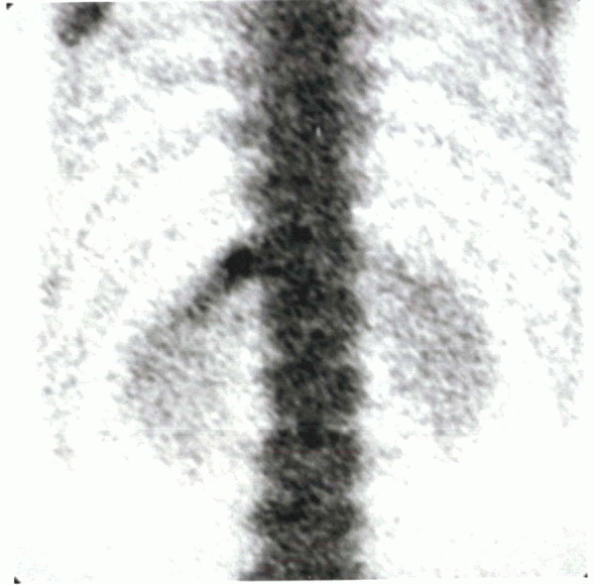
produce pain even before they are visible radiographically. Technetium
bone scanning is nearly 100% accurate in locating these lesions, even
when plain radiographs are negative, by showing a nonspecific but
intense focal uptake of activity (Fig. 10-2).
When these tumors are evident radiographically, they classically are
located on the concavity of the deformity and near the apex. The
painful lesion leads to muscle spasm on the ipsilateral side of the
spine and increases pressure on the vertebral epiphyseal growth plate.
The resulting growth retardation coupled with the continued growth of
the contralateral vertebral epiphysis may result in true rotatory
scoliosis.
-
Early diagnosis
-
Complete excision
-
Relief of pain
-
Correction of deformity
suspicion. Despite the fact that the natural course of osteoid osteoma
may lead to spontaneous remission, a lesion should be removed when it
is diagnosed because the time interval
before
remission can range from 2 to 8 years, and the scoliosis can become
structural during that time. Complete surgical resection via a
posterior approach usually is curative. Patients often note immediate
relief. Resolution of scoliosis also has been reported extensively in
the literature. In patients who develop symptoms at or around skeletal
maturity, complete resolution of scoliosis after excision is the norm.
In skeletally mature individuals, the deformity is thought to be merely
a postural response to the painful stimulus. Because these patients
have no vertebral rotation, the deformity resolves instantaneously
after the lesion is excised. In a growing child, the interrelationships
of the age of onset of symptoms, duration of symptoms, severity of
deformity, and time interval to skeletal maturity have a direct bearing
on whether scoliosis resolves after removal of the painful stimulus.
The crucial time span between the onset of symptoms and surgical
excision has been reported to be 12 to 15 months. Complete or almost
complete resolution of the spinal deformity occurred in nearly every
patient treated before or within the crucial period. When diagnosis was
delayed beyond 18 months, permanent deformity was the rule. Early
diagnosis and complete excision of osteoid osteomas and osteoblastomas
of the spine can reduce the duration of pain and may reverse associated
deformity.
 |
|
Figure 10-1
Axial CT scan shows osteoid osteoma in the rib head of the 12th thoracic vertebra. The patient was a 12-year-old boy with a 1-year history of back pain and mild spinal asymmetry. He was treated with en bloc excision. |
 |
|
Figure 10-2 Technetium bone scan shows focal uptake in T12 rib head.
|
the body. The spine is one of the more common locations for these
lesions, with only the skull and pelvis being involved more frequently.
EG, a granulomatous process of unknown cause, destroys focal areas of
bone. The disease occurs more frequently in young people than in adults.
and without a history of serious trauma. In contrast to most benign
tumors, the onset of pain usually is relatively sudden. Cervical
lesions often present with associated torticollis. Neurologic deficits
as a result of EG of the spine have been reported but are not common.
The radiographic appearance is variable when EG involves the spine.
Changes range from early cavitation and destruction of the body or
neural arch to partial collapse, producing wedge-shaped deformities,
and finally to uniform and complete collapse of a vertebral body. This
uniform collapse is called vertebra plana (Fig. 10-3).
Vertebra plana also can be attributed to other lesions, but it
classically is associated with EG. EG always must be considered in the
differential diagnosis of a lytic vertebral lesion, especially in
children.
 |
|
Figure 10-3
Sagittal MRI shows collapse of C3 vertebral body consistent with vertebra plana in a 10-year-old boy with a 3week history of neck pain and torticollis. |
tissue analysis. Needle biopsy seldom is used today because of the
tendency for negative results or inadequate amounts of recovered
tissue. Open biopsy is preferred to establish the diagnosis of EG.
Reports in the literature have shown satisfactory healing of these
lesions with simple biopsy or even immobilization.
is a self-limited disease, and simple biopsy and curettage alone
frequently are sufficient to stimulate regression of the lesion.
Radiotherapy also has been successful in treating this disease, even
with associated neural deficit. Surgical decompression is rarely
necessary. Spinal stabilization sometimes is necessary when open biopsy
destabilizes a vertebral segment.
ABCs are neither aneurysms nor cysts, but the name has remained.
Similar to EGs, ABCs are found in nearly every bone in the body, with a
slight predilection for the spine.
The
cause of this condition also is unknown. These lesions tend to affect
adolescents and have a slightly higher incidence in females.
 |
|
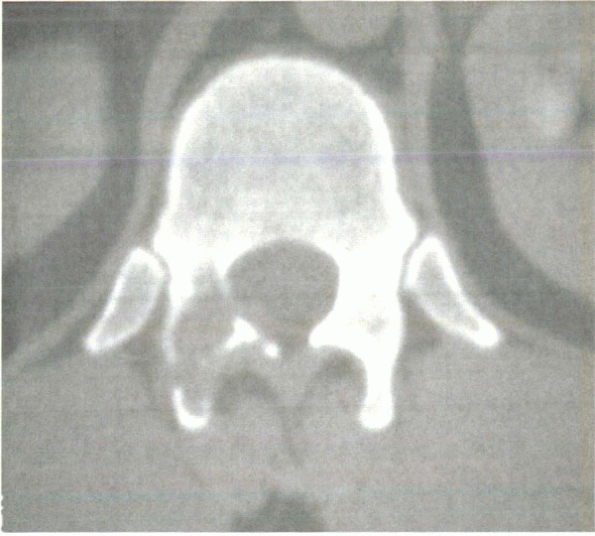
Figure 10-4
Axial CT scan shows an aneurysmal bone cyst involving the posterior elements. The lesion is lytic and expansile with blown-out, thinned cortex. This 35-year-old patient presented with a 6-week history of sudden-onset back pain. |
features associated with a typical ABC. Depending on the size of the
lesion, the complete spectrum of neurologic signs also has been seen in
patients with an ABC of the spine. Because of their tendency to expand,
ABCs are associated more frequently with neural deficits than any of
the aforementioned benign spinal tumors. They also may invade adjacent
vertebrae. These lesions are identified easily on radiographs.
and is an expansile, osteolytic cavity that often contains fine strands
of bone surrounded by an eggshell of blown-out cortex (Fig. 10-4).
Approximately 60% of ABCs involve the posterior elements, and the
remainder involve the vertebral body. They are most common in the
lumbar spine. Destruction of a vertebral body leading to vertebra plana
has been observed in patients with ABC.
deterioration has been reported as a result of hemorrhage from the
needle tract. Open biopsy is recommended to establish a diagnosis,
usually at the same setting as definitive treatment. Complete excision
at the time of biopsy reduces the risk of recurrence. A quarter of ABCs
recur with incomplete resection. ABC is a benign condition in which
disappearance has occurred spontaneously and with simple biopsy, making
treatment controversial. If neurologic deficits are present, surgical
decompression with excision of the tumor is recommended. Surgical
instrumentation and fusion is indicated only when instability develops
either from the extent of the lesion or from the surgical debulking.
The prognosis tends to be excellent overall in the treatment of ABC of
the spine.
hemangioma is relatively common. Autopsy studies have shown an overall
incidence of 10% of the population. Most cases are asymptomatic and
undiagnosed. Pain and neural deficit have been reported in association
with hemangioma of the spine but not typically. Less than 1% of
vertebral hemangiomas are believed to be symptomatic. The thoracic
spine is the usual location for these lesions, and multiple-level
involvement is common. The diagnosis of hemangioma frequently can be
made on the basis of plain radiographs.
on anteroposterior and lateral views of the spine because of the
thickened trabeculae of the affected vertebral body. Pathologic
compression fractures also can occur in patients with hemangiomas. CT
provides further information about cord impingement or pathologic
fracture. MRI also can be helpful for surgical planning. Vertebral
hemangioma can present as a cold defect on bone scintigraphy.
because most lesions are asymptomatic, incidental radiographic
findings. Radiotherapy is the most common treatment for symptomatic
lesions and has an antiinflammatory effect on these benign,
slow-growing tumors. Radiotherapy is easy to use and is a highly
effective analgesic treatment modality. In the rare patient who
requires surgical decompression, it should be preceded by angiography,
and preoperative embolization should be done whenever possible.
Surgical excision may be difficult because of the vascularity of the
tumor. Radiotherapy often is used to supplement the surgery in cases of
subtotal resection.
that arise from any zone of endochondral bone formation. They develop
by progressive endochondral ossification in anomalous foci of
metaplastic cartilage in the periosteum. They make up almost 10% of all
bone tumors and 40% of all benign tumors. Osteochondromas are common in
the appendicular skeleton but occur rarely in the spine (<5%). These
lesions can be solitary or multiple when they occur as part of the
genetic disorder called hereditary multiple exostoses.
cervical spine; the C2 vertebra is the most common location. OCs also
originate in the thoracic and lumbar spine but rarely in the sacrum. In
the case of multiple exostoses, the incidence of lesions occurring in
the thoracic region increases.
neural arch of the vertebra. Vertebral body involvement is uncommon.
Slow growth of the tumor can result in protrusion into the neuroforamen
or spinal canal. The plain radiograph of osteochondroma is
characteristic: a sessile or pedunculated osteoblastic mass adjacent to
the marrow and the cortex of the bone from which it arises. When the
spine is involved, the mass may be difficult to discern because of
obstruction by the surrounding bone column. CT and MRI can be used to locate the lesion.
Neurologic symptoms also occur frequently in vertebral osteochondroma,
as a consequence of the tendency for expansile growth into the spinal
foramen. Occasionally a palpable mass can be detected on physical
examination of the spine. There also is a case report in the literature
of scoliosis resulting from a thoracic osteochondroma.
-
Surgical decompression, when indicated
-
Complete resection of the tumor
deficits and eliminates the potential risk of sarcomatous degeneration,
which reportedly occurs in 1% of the solitary lesions and in 5% to 15%
of multiple osteochondromas.
GCT constitutes 2% to 8% of all primary bone tumors but accounts for
less than 1% of all vertebral tumors. GCT is found more commonly in the
sacrum and less frequently in the anterior portion of the spinal
column. Patients with GCT of the spine usually present with focal pain
and neurologic deficit caused by the locally aggressive nature of the
lesion. Pathologic compression fractures also are common and can result
in relatively acute onset of pain. Patients often have symptoms for
several months, however, before presenting to a physician.
radiographs, but spinal GCT usually presents as an osteolytic lesion
involving the vertebral body. Although the radiographic appearance may
be similar to ABC and metastatic disease, the diagnosis usually can be
made if all information is taken into consideration. Although ABC and
GCT appear as expansile osteolytic lesions, ABC tends to present in the
posterior elements, and GCT almost always is situated anteriorly. The
age at diagnosis in patients with GCT is usually 15 to 30 years, and
metastatic tumors generally present later in life. CT scans define the
bony anatomy more clearly and show osteolysis and possibly soft tissue
extension. CT is especially important in the preoperative evaluation of
these tumors because complete resection is crucial to eradication of
local disease.
tumors. Some authors believe that GCT is moderately malignant in
nature. Despite its benign histologic appearance, transformation to
malignancy or recurrence after high-dose irradiation was reported in
the early 1970s. More recent studies indicate that radiotherapy can be
used safely and effectively to treat GCT, especially as a supplement to
surgical excision. Optimal treatment of GCT of the spine is
controversial.
excision; however, this is not always possible in the spine. The
proximity of the spinal lesion to vital structures makes en bloc
resection difficult. Intralesional excision may be necessary, and
adjuvant therapy is recommended. The options for adjuvant treatment
include:
-
Cement implantation
-
Using a high-speed bur around the periphery of the lesion
-
Irradiation
after resection or curettage and radiotherapy, although additional
procedures were required in some patients because of local recurrence.
With more aggressive surgical excision, radiotherapy is unnecessary,
and good disease-free intervals have been obtained.
tumors tend to occur in young patients and are diagnosed less commonly
in adults. A high index of suspicion is essential for early diagnosis
and improved overall patient satisfaction. The interval between the
onset of symptoms and eventual diagnosis and treatment has prognostic
importance. The clinical presentation usually provides clues to alert
the physician to suspect spinal neoplasm. Although benign spinal tumors
may remain asymptomatic for extended periods, when symptoms develop,
they usually are a consequence of one or more of the following:
-
Expansion of the cortex by tumor mass
-
Compression of the spinal cord or nerve roots
-
Pathologic fracture
-
Spinal instability
of the spine and usually is curative. In planning the surgical
approach, the anatomic extent of the lesion must be understood, and the
need for stabilization or reconstruction must be anticipated. Improved
imaging techniques have assisted greatly in this process. In general,
vertebral body lesions should be approached anteriorly, and posterior
tumors should be approached from behind.
features that distinguish it from the others and assist in making the
correct diagnosis. When the diagnosis is made, the appropriate
treatment can be applied. With advances in imaging techniques,
equipment, biomaterials, and surgical procedures, prognosis and
outcomes have improved greatly in the management of these lesions.
BA, Rooholamini SA. Scoliosis caused by benign osteoblastoma of the
thoracic or lumbar spine. J Bone Joint Surg 1981; 63A:146-155.
S, Gasbarrini A, De Iure F, et al. Symptomatic vertebral hemangioma:
the treatment of 23 cases and a review of the literature. Chir Organi
Mov 2002;87:1-15.
AO, Pozo JL, Hutton PA, et al. The behaviour pattern of the scoliosis
associated with osteoid osteoma or osteoblastoma of the spine. J Bone
Joint Surg 1984;66B: 16-20.
HH, Nicholson JT, Nixon JE. Vertebra plana and eosinophilic granuloma
of the cervical spine in children. Spine 1978;3: 116-121.
