Cervical Radiculopathy
root dysfunction. Abnormalities in motor, sensory, or reflex function
of a specific nerve root often are attributable to the herniation of
disc fragments from the intervertebral disc and resultant compression
of the nerve root by this fragment. The diagnosis begins with a
thorough history and physical examination. Accurate diagnosis depends
on an understanding of the differential diagnosis, which includes
peripheral nerve entrapment syndromes and primary diseases of the
neuromuscular system. The physician also should be familiar with the
natural history of cervical radiculopathy, because most patients with
radiculopathy improve with nonoperative treatment. For patients not
responding to nonoperative therapies, several surgical options are
described in this chapter, along with indications, results, and
complications.
commonly in men 30 to 50 years old; age is the most significant risk
factor. Other risk factors include frequent lifting, driving, working
overhead (i.e., painting a ceiling), and smoking. Genetics also plays a
role, with individuals predisposed to cervical radiculopathy presenting
at an earlier age. Radiculopathy most commonly occurs without
antecedent trauma, but trauma may aggravate an asymptomatic “abnormal”
disc.
pathogenesis of cervical radiculopathy. There are seven cervical
vertebrae, which can be divided into the upper and lower cervical
spine. The upper cervical spine consists of the atlas, or C1, and the
axis, C2. These two levels rarely are involved in producing
radiculopathy. Radiculopathy of the cervical spine occurs most
frequently in the lower cervical spine, defined as the intervertebral
space of C2-3 to the intervertebral space of C7-T1. The C5-6 level is
the most common site of compression, followed by C6-7. The five
vertebral bodies of the lower cervical spine are similar in their
anatomy. Each motion segment (a motion segment consists of a single
intervertebral disc and the vertebra above and below) consists of five
articulations. These articulations include the intervertebral disc
anteriorly, the two facet joints posteriorly, and the two neurocentral
joints, which lie along the posterolateral border of the vertebral
body. The neurocentral joints also are called the joints of Luschka
(or uncovertebral joints) and are osseous projections directed upward
from the superior aspect of the inferior vertebral body and articulate
with the uncinate process. These articulations are not true joints
because they lack an articular capsule, but they can become arthritic.
Because of their interposition between the disc and the intervertebral
foramen, the neurocentral joints can cause impingement via mechanical
compression of nerve roots as they exit the neural canal. The facet
joints are oriented at 45 degrees in the sagittal plane and neutral in
the coronal plane. The facet joints are true diarthrodial joints
complete with a synovial membrane, articular cartilage, and fibrous
capsule.
joints in relation to the intervertebral foramina. The intervertebral
foramen comprises the vertebral body, intervertebral disc, and
neurocentral joint anteriorly and the facets posteriorly. The superior
and inferior pedicles constitute the superior and inferior borders of
the foramina. As the nerve root enters the foramen medially, it lies at
the level of the superior articular facet of the inferior vertebrae.
The nerve courses inferiorly and laterally and forms the dorsal root
ganglion within the lateral aspect of the neural foramen. With an
understanding of this anatomy, it becomes clear how a disc herniation
or arthritic hypertrophy of either the joints of Luschka or the facet
joints may impinge mechanically on an exiting nerve root to cause
radiculopathy. The process of degenerative change of these joints is
called spondylosis, which is discussed more thoroughly in Chapter 13.
well studied. The structural components of the disc include the nucleus
pulposus and the anulus fibrosus, surrounded on the superior and
inferior sides by cartilaginous end plates. The nucleus pulposus is a
centrally located structure, occupying approximately 30% to 60% of the
volume of the entire disc. It consists of a loose array of type II
collagen arranged in an irregular meshwork. An extracellular matrix of
proteoglycans
gives
the nucleus an elastic quality that accommodates compressive forces.
The proteoglycans, primarily chondroitin sulfate and dermatan sulfate,
are hydrophilic and maintain a high water content (70% to 90%) within
the disc. As a person ages, the character of the nucleus pulposus
changes. The ratio of proteoglycans changes, with a decrease in
chondroitin sulfate, and an increase in dermatan sulfate and subsequent
loss of water content. The nuclear composition undergoes age-related
changes and no longer optimally can transmit, modify, and distribute
forces evenly.
function, resisting tensile stresses of motion and transmitted forces
from the nucleus. The anulus consists of type I collagen fibers
peripherally and some type II fibers centrally. The anulus is formatted
in concentric laminated bands of these collagen fibers, which attach to
the vertebral body end plates and insert into the anterior longitudinal
ligament and posterior longitudinal ligaments. The anulus’ water
content remains steady throughout life, but it, too, undergoes
degeneration. Circumferential tears in the anulus begin to present
around the 20s and progress to fraying and splitting of the collagen
fibers. With the progression of degeneration, there is continued loss
of the fluid properties of the nucleus, which undergoes a gradual
replacement with fibrous tissue. This process occurs from the 30s to
the 50s. By the 60s, there is advanced degeneration of the
intervertebral disc, and the disc loses its ability to attenuate shock
and vibration and to distribute loads evenly. Some environmental
factors contribute to disc degeneration, such as driving, lifting, and
smoking.
deformation of the dorsal root ganglion or nerve root. This mechanical
deformation—be it compression or stretch of the involved nerve
root—causes release of substance P, phospholipase 2, and vasoactive
intestinal polypeptide from the cells of the nucleus pulposus, which
act to inflame the affected nerve root. These chemical mediators lead
to paresthesia and sensory or motor deficit.
-
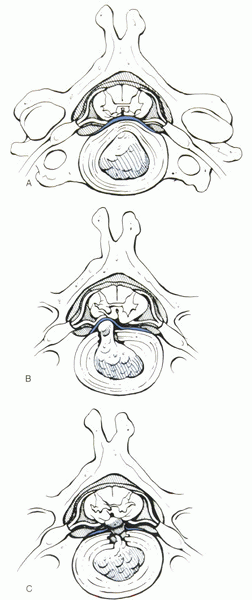
First, the
nucleus pulposus may be a protrusion, with a radial tear in the anulus
allowing for the nuclear material to force the outer annular fibers to
bulge out and encroach on neural elements. -
Second, there
is an extruded disc. In this scenario, nuclear elements have herniated
through the anulus but are restrained by the posterior longitudinal
ligament. -
Third, there
is the sequestered disc, wherein nuclear material is directly
compressing the neural elements, having herniated through the outer
annular fibers and the posterior longitudinal ligament (Fig. 14-1).
from the degenerative changes of spondylosis. Hard discs
are posterior or posterolateral osteophytes that commonly cause spinal
stenosis and radiculopathy in patients older than 55 years of age. The
acute soft disc herniation is most common
in men age 30 to 50. Disc herniations are categorized by their location
relative to the neural canal—foraminal, posterolateral, and midline
herniations—with posterolateral herniations being the most common
cervical disc herniation.
 |
|
Figure 14-1 Three common types of cervical disc herniation. (A) Central protrusion, with the outer anulus remaining intact. (B)
Posterolateral extrusion, with the anulus having a tear and the nucleus being restrained by fibers of the posterior longitudinal ligament. (C) Central sequestered fragment, lying posterior to the posterior longitudinal ligament. (From Jenis L, An H. Cervical disc disease. In: Chapman MW, ed. Chapman’s orthopaedic surgery, 3rd ed. Philadelphia: Lippincott Williams & Wilkins. 2001:3749.) |
specific symptoms and signs. The neuroanatomy of the cervical spine is
unique in that the nerve roots exit above the pedicle of the same
number, with the exception of C8, which exits below the pedicle of the
same level. C5 exits above the pedicle of C5 in the C4-5 interspace.
Compare this with the thoracic and lumbar spines, where the nerve root
exits below the pedicle of the same number: The L4 nerve root exits
below the L4 pedicle at the L4-5 interspace. The location of the
herniation determines the presenting symptoms. Intraforaminal or
lateral herniations most commonly manifest as pure radicular pain (pain
in a dermatomal or radicular distribution). Posterolateral herniations,
between the posterior edge of the uncinate process and the lateral
border of the posterior longitudinal ligament, often present with motor
deficits in the affected myotome. Midline herniations often are
responsible for myelopathy, compressing directly on the cord itself.
suspected radiculopathy because there is an extensive differential
diagnosis to be considered. Symptoms of cervical radiculopathy may
develop acutely, with an initial episode of neck pain followed by
radiation of pain in a dermatomal pattern or weakness in the affected
extremity. Referred trapezial and periscapular pain often accompanies
the radicular component. The patient may describe positions that
alleviate symptoms, such as rotating the head away from the affected
side, effectively enlarging the intervertebral foramina of the involved
side, and the abducted shoulder sign, in which the patient describes
pain relief with the affected shoulder abducted and the hand resting on
top of the head.
observation of the patient, noting the position of the head and neck
contours. Next the painful area of the neck is identified by palpation,
checking for muscle spasm. In assessing range of motion, cervical
flexion may alleviate symptoms, whereas extension may exacerbate the
patient’s symptoms. The range of motion in a normal patient involves
the following:
-
Flexion—chin to chest
-
Extension—looking directly at the ceiling
-
Rotation—chin in line with the shoulder
-
Lateral bending—45 degrees to each side
diagnosis of cervical radiculopathy and differentiating the diagnosis
from shoulder pathology, peripheral nerve entrapment syndromes,
vascular syndromes, and lesions above the foramen magnum. The Spurling
maneuver involves turning the patient’s head toward the affected side,
then applying axial compression, recreating symptoms of radiculopathy.
The shoulder abduction sign often is observed as the patient enters the
physician’s office, with the affected arm abducted fully at the
shoulder and the hand placed squarely on the head. The jaw jerk reflex
is a tap on the temporomandibular joint, which, if hyperactive,
indicates pathology above the foramen magnum.
presentation of radiculopathy is nerve root specific, so a review of
individual nerve root findings follows.
-
Radiculopathy is rare above C2 and presents with occipital headaches and jaw pain without any neurologic deficit.
-
C3 radiculopathy most commonly involves
the C2-3 disc and presents with pain and numbness in the back of the
neck around the mastoid process and the pinna of the ear. No weakness
or reflex change is readily detectable. The pain often is accompanied
by an occipital headache and must be differentiated from a tension
headache. -
Compression of the C4 nerve root
typically involves the C3-4 disc. There is more motion at this level
than C2-3 and is more often involved. Pain and numbness at the base of
the neck at the trapezium muscle predominates. Although the phrenic
nerve is innervated by C3-5, involvement of the diaphragm is unusual
secondary to bilateral denervation. There are no readily detectable
weaknesses or reflex changes, with the exception of some weakness in
neck extension with involvement of the levator scapula muscle. -
Disc herniations at C4-5 impinge on the
C5 nerve root. This impingement typically presents with pain or
numbness radiating down the side of the neck to the top of the shoulder
to the lateral aspect of the deltoid muscle. The difficulty with C5
radiculopathy is differentiating it from intrinsic shoulder pathology,
so a complete shoulder examination is mandatory. In a rotator cuff
tear, there is weakness of the supraspinatus, infraspinatus, teres
minor, or subscapularis. A shoulder examination shows weakness in
abduction with external rotation, adduction with external rotation, or
a posterior push-off test in a tear of one of the rotator cuff muscles.
In a C5 radiculopathy, there is often weakness of the deltoid without
involvement of the rotator cuff muscles. In advanced cases of C5
compression, the deltoid can become markedly atrophied. Although the
biceps reflex frequently is associated with C5, findings of decreased
reflexes here are unreliable findings. -
Radiculopathy at C6 involves the C5-6
disc and is the most common site of herniation in the cervical spine.
It presents as pain radiating down the lateral side of the arm and
forearm to the tip of the thumb and index finger. There is weakness of
the biceps muscle, which often is subtle in its presentation. The
examining physician should check not only elbow flexion, but also
supination of the forearm. There also is a weakness of wrist extension.
With C6 radiculopathy, there often is a diminished
P.117brachioradialis reflex and possibly a decreased response of the biceps reflex.
-
C7 is the second most common site of
cervical radiculopathy. The offending disc is at C6-7. Pain or numbness
or both radiate down the middle of the forearm to the middle finger,
with possible involvement of the index and ring fingers. There is a
weakness in the triceps muscle and a loss of wrist flexion strength.
Patients also may have decreased push-off strength. The triceps reflex
is diminished. -
Disc protrusions affecting C8 originate
from the C7-T1 interspace. This relatively uncommon herniation is
associated with numbness on the medial aspect of the forearm to the
ring and small fingers. Pain is an infrequent complaint at this level.
The intrinsic muscles of the hand, the lumbricals and the interossei
muscles, weaken and atrophy, affecting finger flexion, abduction, and
adduction. Weakness of grip strength results. No reflex changes are
associated with this level.
symptoms. Exceptions to this practice are red flag cases, and include
patients with progressive weakness, intractable pain, trauma, suspected
infection, or tumor. A review of the patient’s symptoms always should
include a history of fever, chills, weight loss, and past malignancy.
Plain radiographs often reveal the age-related changes of spondylosis,
which are ubiquitous in patients older than age 40. Greater than 70% of
radiographs show spondylotic or degenerative change in patients by age
70. Plain films may not be helpful in securing the diagnosis. When
indicated, anteroposterior, lateral, and right and left oblique views
should be ordered. Plain radiographs help to rule out tumor, infection,
or fracture. Radiographs also show sagittal alignment. The oblique
views are useful in evaluating the foramina; a narrowed foramen has a
figure-of-eight appearance. Flexion/extension films may be helpful if
trauma is involved or if instability due to severe facet degeneration
is present.
imaging study of choice for cervical radiculopathy. A 1.5 Tesla magnet
or higher is preferred. The test is noninvasive and is useful for
diagnostic confirmation and preoperative planning. T1-weighted and
T2-weighted images should be obtained. T1-weighted images show
herniated discs and bone spurs as hypointense, making it more difficult
to discern these structures from bone and ligament. T2-weighted images
often are more revealing, creating a myelographic picture of the spinal
cord and roots (Figs. 14-2 and 14-3).
MRI tends to overestimate stenosis and, similar to radiographs, should
be used with strict clinical correlation. Asymptomatic disc
degeneration and herniation commonly are encountered in individuals
older than 30 years.
who are claustrophobic or when MRI is contraindicated or nondiagnostic.
In an acute disc herniation, CT-myelography reveals extradural filling
defects, cord flattening, and obstruction of flow to affected nerve
roots in an axial plane (Fig. 14-4).
Disadvantages include inability to differentiate between hard and soft
disc protrusions, inability to assess pathology below a complete
myelographic block, and invasiveness.
 |
|
Figure 14-2
Axial T2 weighted MRI reveals a posterolateral soft disc herniation. The disc is impinging on the left nerve root (the right side of the MRI image) and effectively reducing the foraminal area. |
nonradicular pathology. Electromyography (EMG) and nerve conduction
velocity studies detect motor changes secondary to compression.
Demyelination must be present for nerve conduction tests to show
decreased amplitude. This rarely occurs in radiculopathy; it occurs
more commonly in peripheral nerve entrapment syndromes. Nerve
conduction studies evaluate peripheral nerves and their responses to
surface electrodes. The amplitude and the latency (time between the
stimulus and response) are measured and compared against normal
controls. EMG uses intramuscular needle electrodes to evaluate muscle
function. A peripheral neuropathy, such as carpal tunnel or cubital
tunnel syndrome,
would
present with fibrillations and sharp waves on EMG. EMG is not useful
until 4 weeks after injury; normal (latent) responses are obtained
before 4 weeks. These tests may be ordered in patients with unusual
presentations, diabetes, suspected neurologic syndromes, or suspected
peripheral nerve entrapment syndromes.
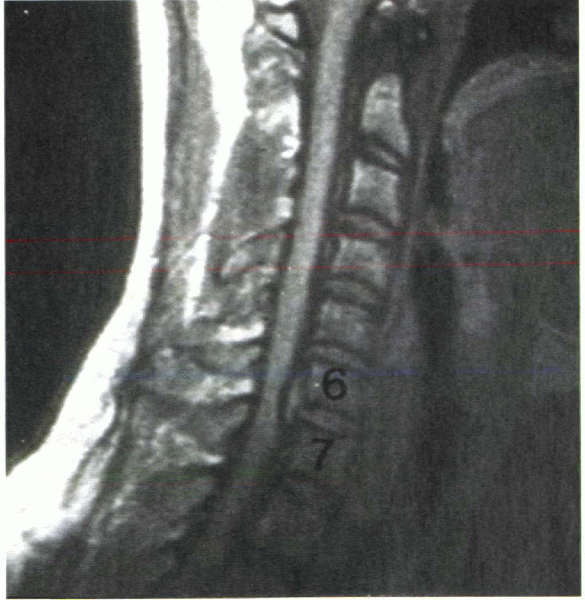 |
|
Figure 14-3 T2-weighted MRI reveals soft disc herniations at C4-5, C5-6, and C6-7.
|
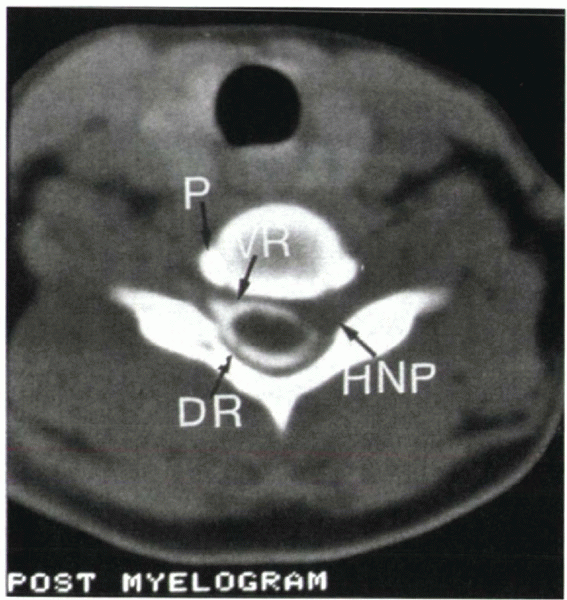 |
|
Figure 14-4
CT-myelogram shows a herniated nucleus pulposus (HNP). Note the loss of contrast material in the left nerve root, representing compression of the exiting nerve root. DR, dorsal root; VR, ventral root; P, uncinate process of the vertebral body. |
alert the physician to the possibility of a tumor or infection.
Systemic signs of weight loss, night sweats, lack of energy, fever, and
chills also are strong indicators of possible tumor or infection.
the branches of the brachial plexus. Ulnar, median, posterior, and
anterior interosseous nerve compressions can mimic radiculopathy.
Pronator syndrome, involving the median nerve, may present similar to a
C6-7 radiculopathy. Specific EMG and nerve conduction velocity studies
are helpful in ruling out these entities, showing a change in
potential, 3 weeks after injury.
distinguish from radiculopathy. Rotator cuff tears, impingement
syndromes, bursitis, tendinitis, arthritis, and shoulder instabilities
can present with nonspecific shoulder and arm pain. A detailed shoulder
examination is necessary to clarify the diagnosis.
lower cervical roots by a cervical rib or vascular compression of C8
and T1. Bruits in the lower cervical spine and a cervical rib on
radiographs are clues to the diagnosis. Syringomyelia is a cystic
dilation within the spinal cord itself often resulting from trauma or
secondary to Chiari malformations and tumor. A syrinx typically
presents with weakness and atrophy of the hands with a loss of pain and
temperature sensation and sparing of light touch. A headache often
precedes neurologic findings. The presence of syringomyelia can be
confirmed with MRI.
deficits similar to myelopathy. Multiple sclerosis is associated with
visual changes and upper motor neuron lesions that wax and wane over
time. MRI may reveal focal plaques consistent with multiple sclerosis.
Serum and cerebrospinal fluid with increased oligoclonal bands and
immunoglobulins help to confirm this diagnosis. Amyotrophic lateral
sclerosis often presents in people in their 50s through 70s with
painless weakness beginning about the shoulder girdle and progressing
to complete motor loss without sensory involvement. Lesions above the
foramen magnum, such as cerebrovascular insults or brain tumors, also
may present with deficits that must be differentiated from cervical
radiculopathy.
function, provide stability, and resolve neurologic deficits.
Understanding the natural history of cervical radiculopathy is
important in formulating a treatment plan. Lees and Turner found, that
45% of cases of radiculopathy occurred as single episodes, 30% recurred
with intermittent episodes, and 25% had persistent radiculopathy.
DePalma and Rothman reported that 29% of patients had complete relief
of symptoms, 49% had partial relief, and 22% had no relief. Gore’s
retrospective review showed that 32% of patients had persistent pain.
and advising the patient to avoid lifting and extension movements about
the neck. Soft cervical collars may be used for 1 to 2 weeks. These
braces do not stop cervical motion effectively, but they serve more
effectively as reminders to the patient that a problem exists.
Medications are employed effectively to relieve inflammation, including
aspirin, nonsteroidal antiinflammatory drugs, short-term oral steroids,
and epidural steroid injections. Epidural steroids have been shown to
provide short-term symptom relief, but currently there is no evidence
of long-term symptomatic relief. Physical therapy plays an active role
in conservative treatment. Isometric muscle strengthening and
stretching and modalities such as heat, traction, ultrasound, and
massage are helpful. Traction usually provides some relief of radicular
pain and accompanying spasms. Active exercise that is limited by the
patient’s symptoms serves to keep the neck from becoming deconditioned.
Chiropractic care may be considered in patients without significant
spondylosis at the initial onset of symptoms.
of nonoperative treatment. A progressive neurologic deficit with
confirmatory imaging studies consistent with the clinical picture is an
absolute operative indication. The results of operative intervention
for axial neck pain are inferior to the results for radiculopathy, with
operative results for radiculopathy being 70% to greater than 90% good
to excellent. Mitigating factors that should be considered include
workers’ compensation cases, mental health issues such as depression,
and substance abuse. These factors have a negative impact on treatment,
with surgical results for these patients lagging behind results of
other patients.
spine—anterior and posterior—and there are several factors to consider
in selecting one over the other. Single-level or double-level
involvement is addressed best with an anterior approach, whereas
multiple-level involvement may be addressed better by a posterior
approach. The location of the impingement and the contour of the spine
also are important to consider. Central herniations place the cord at
risk if approached posteriorly, so an anterior approach is recommended.
A unilateral soft intraforaminal disc may be approached posteriorly
with a laminofacetectomy and foraminotomy. Laminoplasty, wherein the
posterior elements are hinged open like a door, employs a right-sided
or left-sided osteotomy at the intersection of the lamina and the
lateral mass. This approach is most effective for unilateral
radiculopathy at multiple levels with accompanying stenosis.
Laminoplasty is contraindicated in patients who have lost physiologic
lordotic contour of the cervical spine. Laminectomies are an
alternative for multiple-level radiculopathies but are employed more
commonly in myelopathic patients with central stenosis. If instability
is present, laminectomy should be followed by posterolateral fusion to
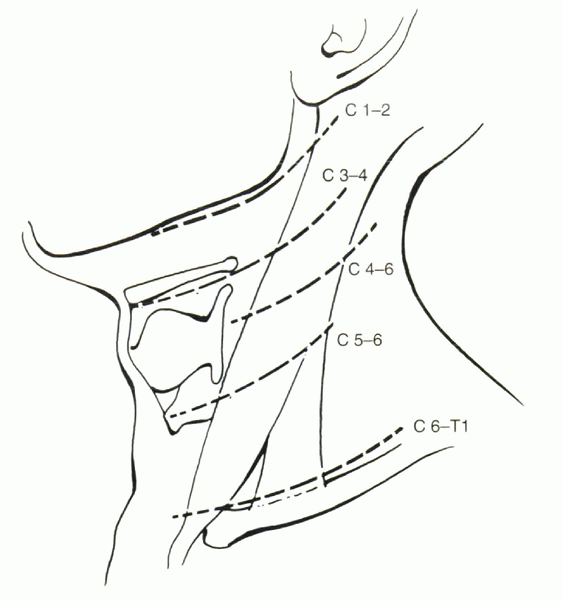
avoid subsequent kyphotic collapse. The anterior approach is the most
common surgical approach for cervical radiculopathy. A transverse
incision is used for one-level to two-level discectomies, and a
longitudinal incision is used for three or more levels. A left-sided
approach is preferred because of the predictability of the recurrent
laryngeal nerve on this side. The nerve courses between the esophagus
and the trachea and is protected. The thoracic duct of the lymphatic
system inserts at the confluence of the jugular and subclavian veins on
the left side and must be avoided in low-level discectomies. When
approaching from the left, the level of the incision is determined by
palpating anatomic landmarks: The hyoid bone is at the C3 level, the
thyroid cartilage is at C4-5, and the cricoid cartilage is at C6 (Fig. 14-5).
to 90% satisfactory results. Tricortical autograft harvested from the
patient’s iliac crest remains the gold standard, providing stability,
osteoinductivity, and osteoconductivity. Allograft, usually patella or
fibula, has shown to be as effective in single-level fusions as
autograft, without the morbidity associated with graft harvest.
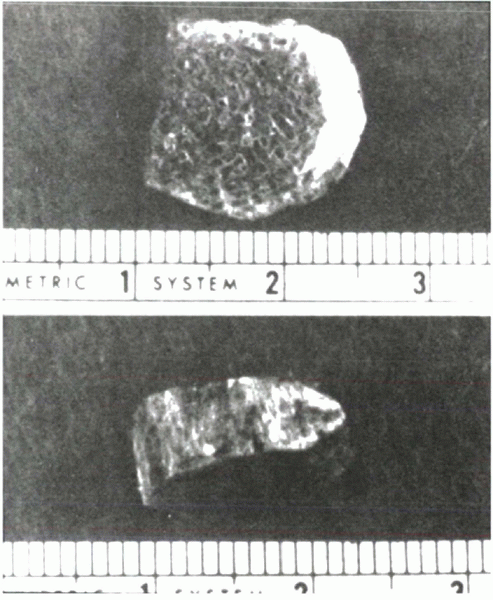
Tricortical grafts:
 |
|
Figure 14-5
Landmarks for the incision of the Smith-Robinson approach for anterior cervical discectomy and fusion. C1-2 is at the level of the mandible. C3 is at the level of the hyoid. C4-5 is at the level of the superior and inferior borders of the thyroid cartilage. C6 is at the level of the cricoid cartilage. C7-T1 exposure is just above the clavicle. (From Fischgrund J, Herkowitz H. In: Bradford DS, ed. Master techniques in orthopaedic surgery: spine. Philadelphia: JB Lippincott, 1997:92.) |
-
Offer some immediate stability to the
motion segment Eventually lead to interbody fusion (which may arrest or
reverse spur formation). Posterior osteophytes often resorb after solid
fusion. -
Can increase the dimension of the neuroforamina by distraction (Figs. 14-6 and 14-7).
multiple-level discectomies but does not improve the fusion rate in
single-level anterior cervical discectomy and fusions. Plating should
be used for multiple-level interbody fusions, single-level fusions in
smokers, single-level fusions in which allograft is employed, and
pseudarthrosis repair. In practice, plating allows for a more
aggressive rehabilitation and decreased duration of immobilization (Fig. 14-8).
Postoperative immobilization consists of a cervical orthosis for 6
weeks if plating is not used and less than 2 weeks if plating is
employed. If an anterior plating system is placed, an orthosis is used
for 1 week.
well defined. They range from graft harvest complications to permanent
neurologic injury, with an overall complication rate of 6.7%. Autograft
harvest site complications are the most
commonly
cited and include pain, hematoma, infection, abdominal herniation, and
injury to the lateral femoral cutaneous nerve (meralgia paresthetica).
 |
|
Figure 14-6
Anteroposterior radiograph after a three-level anterior cervical discectomy and fusion with tricortical grafts for multiple-level herniations. The anterior plate assists with stability and improves fusion rates, especially in multiple-level operations. |
anteriorly (0.7% to 2.8%); this may be due to the abundant blood supply
of the neck and the relatively atraumatic tissue dissection involved in
the Smith-Robinson exposure. Prophylactic antibiotics, usually a
first-generation cephalosporin, given 1 hour before surgery reduce the
risk of infection. Conditions associated with an increased risk of
infection include diabetes, malnutrition, immunocompromised status,
rheumatoid arthritis, malignancy, alcoholism, and poor dentition.
occur in less than 2% of all anterior cervical discectomies. Hoarseness
may be encountered secondary to excessive traction or, more seriously,
division of the recurrent laryngeal nerve. The recurrent laryngeal
nerve on the right side courses transversely across the spine at the
C6-7 level, exposing it to injury with sharp dissection or retraction.
For this reason, we recommend the left-sided approach, in which the
recurrent laryngeal nerve courses in the tracheoesophageal groove and
is protected by the trachea and esophagus. Transient sore throat and
difficulty swallowing commonly are seen in the immediate postoperative
period and usually resolve within 1 to 2 weeks. Esophageal injury is a
rare but potentially lethal injury. Injury may be evidenced by saliva
or food in the wound, dysphagia, and increasing neck pain. A perforated
esophagus is diagnosed with an esophagogram. Late perforations may be
related to prominent hardware. Finally, the thoracic duct of the
lymphatic system enters the subclavian vein on the left side. Low,
lateral approaches on the left potentially can injure the duct. If the
thoracic duct is damaged, it should be double ligated. Clinically this
injury presents with an expanding mass similar to that of a hematoma.
Surgical exploration may be necessary to address the lymphatic drainage.
 |
|
Figure 14-7
Tricortical bone graft. Autograft tricortical graft is harvested from the iliac crest. Allograft tricortical graft often is taken from donor fibula or patella. Typical dimensions for a man would be 8 mm high × 14 mm deep × 14 mm wide. |
important to seat the graft properly. Graft collapse can be avoided by
harvesting with a power saw to avoid microfactures that can occur when
osteotomes are used. Grafts that are too thick may lead to collapse;
grafts that are too thin may predispose to pseudarthrosis. Grafts
should be 2 mm greater than the intervertebral space. If the graft
collapses or migrates, revision surgery is advised. Neurologic injury,
dysphagia, kyphosis, and respiratory distress all are possible
complications of graft extrusion.
irreparable damage done to the neural structures before surgery, wrong
level of surgery, or an inadequate decompression. The level of surgery
always should be checked with an intraoperative radiograph. Neurologic
injury can occur during or shortly after surgery. Implant malposition
or displacement should be considered and evaluated with radiographs and
CT-myelography in patients with postoperative neurologic deficit.
graft, is related directly to the number of levels fused. One-level
fusion has a pseudarthrosis rate of 5% to 10%; two-level, 10% to 15%;
and three-level, 20% to 30%. Rates also are increased with smoking and
the use of allograft. Pseudarthrosis may be diagnosed in a patient
experiencing continued mechanical cervical pain. Motion at the graft
segment seen on flexion/extension lateral films and a lack of bony
trabeculae across the end plates confirm the diagnosis. Pseudarthrosis
can be asymptomatic; surgical indications are based on the degree of
instability and its attendant risk of injury to the spinal cord.
 |
|
Figure 14-8 Lateral view of the same patient as in Figure 14-7, 6 months postoperatively. Note the beginning of a fusion anteriorly.
|
rely on the physician’s knowledge of cervical anatomy and understanding
of the differential diagnoses that may mimic its signs and symptoms.
When cervical radiculopathy is diagnosed, nonoperative therapies should
begin, including physical therapy and short-term use of a soft cervical
collar. Plain radiographs show the degree of degeneration and the
sagittal alignment and help to rule out neoplastic and infectious
conditions. MRI and CT-myelography help confirm the diagnosis and
detect the source of compression. Surgery is indicated in patients with
progressive neurologic deficits or intractable, persistent pain for
more than 3 months. The surgical results in patients with cervical
radiculopathy are 70% to 90% good to excellent.
SD, McCowin PR, Davis DO, et al. Abnormal magnetic-resonance scans of
the cervical spine in asymptomatic subjects: a prospective
investigation. J Bone Joint Surg 1990;72A:1178-1184.
NE. A review of laminoforaminotomy for the management of lateral and
foraminal cervical disc herniations or spurs. Surg Neurol
2002;57:226-234.
MJ, Albert TJ, Smith MD. Cervical radiculopathy: diagnosis and
nonoperative management. J Am Acad Orthop Surg 1996;4:305-316.
