Anesthesia
and a high degree of safety is a building block of patient reassurance
and a hallmark of modern outpatient surgery. The methods to be
described are effective and safe in emergency rooms, outpatient
settings, as well as in more formalized operating theaters. Emphasis
upon outpatient surgery has dramatically increased the desirability of
effective regional and local anesthesia methods that can be used by
operating surgeons and anesthesiologists. In many of the settings where
surgery is performed today, there is not an anesthesiologist
available—or even necessary. This is an additional stimulus to the
operating surgeon to become proficient in the administration of local
and regional anesthesia.
-
Determine the patient’s allergy status to the drugs.
-
Despite the fact that genuine allergies
to local anesthetics are exceedingly rare, if the patient describes an
allergy to a local anesthetic, the surgeon should not use it, even if
the history is inconclusive or vague.-
If the patient is right, and a reaction occurs, the physical and legal consequences can be serious.
-
-
If a local anesthetic agent is necessary
for medical or other reasons, the surgeon should consider using an
alternative drug or skin testing. -
Of the two types of local anesthetics,
esters, being derived from para-aminobenzoic acid (PABA), are far more
likely to produce an allergic reaction than amide-type agents are. -
Symptoms of allergic reactions include
itching, burning, tingling, hives, erythema, angioedema, dyspnea, chest
discomfort, wheezing, coughing, sneezing, shock, and tachycardia. -
Much more commonly, the patient will not
have had a true allergic reaction to the local anesthetic, but rather
symptoms associated with one of the following:-
Inadvertent direct intravenous or
arterial injection of the agent or a drug overdose. These symptoms can
include convulsions, disordered speech, tachycardia, or bradycardia. -
Reaction to local agents containing epinephrine (palpitations, severe anxiety, tachycardia).
-
A vasovagal reaction.
-
An anxiety-hyperventilation event.
-
-
One can choose another type and perform a skin test.
-
Otherwise, consult an anesthesiologist and proceed with another method.
-
-
Ensure the site of injection is sterile.
-
Do not inject directly into a wound. This increases the risk of implanting and spreading bacteria.
-
Inject more proximally to avoid multiple needle sticks and the resulting multiple punctures and patient discomfort.
-
Block a peripheral nerve well proximal to the site of surgery.
-
This will result in less needle sticks and a larger area of anesthesia.
-
-
Know the anatomy.
-
Knowing the location of peripheral nerves is necessary to accomplish a successful regional nerve block.
-
The sensory distribution of peripheral nerves is reasonably consistent.
-
Figure 8-1 represents the distribution of the three major peripheral nerves in the upper extremity.
-
It is important to know this anatomy so
as to be able to perform a neurologic examination prior to inducing
anesthesia for the purpose of making a proper diagnosis. -
A patient’s injury may have resulted in
damage to a nerve, and that fact should be known before surgery so that
one can select a proper treatment plan and choose the appropriate
peripheral nerve, or nerves, to block.
-
-
Take care in choosing the needle bore and type.
-
One has to balance the issues of pain versus effectiveness and safety.
-
We tend to assume that needles of small
diameter cause less pain. However, the disposable needles we use are so
sharp that patients cannot tell the difference between one with a gauge
of 25 or 22. -
There are several advantages to using a larger-bore needle.P.117
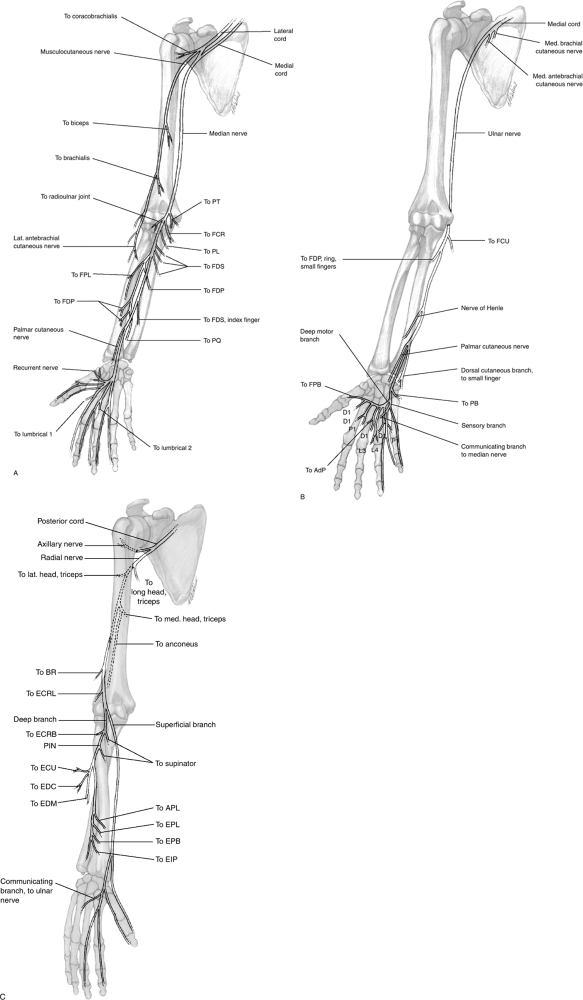 Figure 8-1 The anatomy of the major nerves of the upper extremity, showing their sensory and motor components. (A) Median nerve. (B) Ulnar nerve. (C) Radial nerve.
Figure 8-1 The anatomy of the major nerves of the upper extremity, showing their sensory and motor components. (A) Median nerve. (B) Ulnar nerve. (C) Radial nerve.-
Increased stiffness of the needle allows the surgeon to direct it more effectively.
-
There is less chance of breaking it or having to deal with retrieving a broken needle.
-
One obtains useful information feedback from rate of flow.
-
Because there is greater resistance to flow in a small-bore than in a large-bore needle, one has to push harder on the plunger.
-
If the surgeon uses a small-bore needle,
he or she may not be able to distinguish between being in a tendon or
the space around a peripheral nerve. -
A large-bore needle will give the surgeon important information about the location of the end of the needle.
-
-
Smaller diameter needles will penetrate the substance of a peripheral nerve more easily than larger diameter needles.
-
Axons will be damaged if a needle is inserted into the substance of a peripheral nerve.
-
Also, the patient will usually have severe pain upon penetration.
-
When the surgeon and the patient both move violently because of pain or surprise, additional damage can be done to the nerve. -
-
For all peripheral nerve blocks, one should use needles designated “blunt tip,” when available.
-
This is especially important when doing infraclavicular and axillary blocks.
-
The angle of the bevel is 30 to 45 degrees instead of the usual “sharp tip” needles, which are beveled at 12 to 15 degrees.
-
Using a blunt-tip needle further reduces the chance of penetrating the epineurium and injecting into the substance of the nerve.
-
Experience has shown that the blunt-tip
needle is more likely to push or roll the nerve out of the way, rather
than perforating or impaling it. -
Injecting into the substance of a peripheral nerve may cause significant mechanical injury.
-
-
-
Inject the local anesthetic slowly and steadily.
-
Avoid fast and forceful injections, especially with larger volume blocks.
-
Remember, nerves can usually recover from
mechanical trauma from needle contact, but needle insertion plus
deposition of local anesthetic injected under high pressure can
significantly damage nerve fascicle architecture and compromise its
microvasculature, with devastating permanent results. -
Always inject smaller volumes of local
anesthetic (3 to 5 mL) at a time, with intermittent aspiration to rule
out a direct intravascular injection. -
When aspirating on a syringe for blood,
some smaller veins may collapse, even with the tip of the needle in the
lumen of the vessel. -
Patient response is the key to diagnosis of intravascular injection of local anesthetic agent.
-
Never inject local anesthetic when high resistance to the injection is encountered.
-
Withdraw the needle, reassess surface landmarks, reinsert the needle, and try again.
-
Painful paresthesias and resistance to injection strongly suggest an intraneural injection.
-
-
-
Do not inject into a vein or artery.
-
Many peripheral nerves are in close association with veins and arteries.
-
In some locations, such as the axillary
sheath, the median nerve at the elbow, and the ulnar nerve at the
wrist, the relationships are intimate. -
The old and true admonition to withdraw the plunger of a syringe before injecting applies yet again.
-
-
Consider the time it takes for local or
regional anesthesia to become effective, and use this period to further
your relationship with the patient.P.120-
Because anesthetic materials take a few
minutes to become fully effective, there is a potential time gap in the
operating room schedule.-
Anesthesia should preferably be administered in an anteroom to the operating room.
-
Nurses in this setting can prepare the
patient so that the surgeon can administer the anesthetic immediately
after the preceding operation. -
The anesthetic will be acting while the paperwork and room preparation is proceeding.
-
If one assumes a 20-minute turnover time, there will be adequate time for the anesthetic to become effective.
-
-
This is an important time to establish a
doctor-patient relationship in the surgical environment, before the
patient is separated from the operating team by a wall of draping cloth.-
Giving the anesthetic well before the operation gives the surgeon time to reassure the patient and to discuss the process.
-
When administering the anesthetic, the
surgeon has time to chat, describe the process, and answer questions
that all patients have. -
The patient may remember the surgeon only
in a white coat in an office. Often, patients will not even recognize
the surgeon in a scrub suit. -
Preoperative contact with the operating
surgeon is in itself reassuring to patients, even though an anesthetic
agent is being injected. -
The patient will be reassured by knowing that anesthesia is complete before being rolled into the operating room.
-
If the surgeon has to administer
additional injections after the patient has been blinded to the process
by drapes and other items, the patient may lose confidence and become
anxious.
-
-
Making the patient as comfortable as possible in the operating room can enhance the feeling of reassurance.
-
Keeping the environment warm and quiet is helpful.
-
A pillow for the head and behind the knees adds comfort.
-
The arm board should be placed so that
the arm is not abducted more than perpendicular to the trunk, in order
to reduce shoulder stiffness or pain.
-
-
-
Confirm that anesthesia is accomplished by using light touch.
-
Pinching or sticking skin merely produces more pain and unnecessary anxiety in the patient.
-
If the patient feels light touch, the
anesthetic is not adequate. If the patient does not feel light touch,
anesthesia is complete. -
This method must be used in children, or
the additional pain or threat thereof will bar any possibility of
cooperation. Adults appreciate the same consideration. -
The examiner has to be careful to not
stimulate a proprioceptive response from the patient by moving skin or
joints in an area not anesthetized. Many patients will respond if they
feel anything, including a proprioceptive sensation.
-
-
Remember that managing anesthesia for children is different from that for adults.
-
Children have minimal tolerance for pain
and threatening surgeons. And one is wise to assume that they have food
in their stomachs. -
In many emergency situations, local
anesthesia is the safest method for obtaining anesthesia for children,
but successful administration requires the surgeon to be skilled at
management of the psychological and technical issues. -
In the more controlled operating room
environment, anesthesiologists, equipment, and premedication are
available. Adults appreciate efficient, minimally painful, and
effective anesthesia, too.
-
-
Consider use of a pneumatic tourniquet when more distal blocks (wrist and digits) are used.
-
Most patients can tolerate a tourniquet without parenteral drugs for up to 20 minutes.
-
The pressure should not exceed 225 to 250 mm Hg.
-
If the systolic pressure is so high that
bleeding occurs in spite of the tourniquet pressure set as described,
one should probably not be doing surgery except in an emergency
situation. -
The tourniquet can be deflated and
reinflated 5 to 10 minutes later if necessary, but one should carefully
choose operations that can be performed with confidence within the 10
to 20 minute time limit. -
Planning approaches, reviewing
radiographs, and other such procedures should be done before inflating
the tourniquet, and wound irrigation, bleeding control, and closure can
be done after the tourniquet has been deflated.
-
onset of anesthesia but is short acting. Using epinephrine can increase
the time of effective anesthesia. The latter drug may produce some
unpleasant side effects to deal with in an outpatient setting,
including drowsiness, lightheadedness, and vertigo. If blood
concentration continues to rise, one sees agitation and excitement, and
then, seizures. Fortunately, these symptoms are not common, but one
must be prepared. One complication reported from the use of epinephrine
with local anesthetic agents when used for digital nerve blocks is
ischemia of the digit caused by vasoconstriction of the digital
arteries. Most of these unfortunate effects can be avoided by using
mepivacaine, which has a longer effect without using epinephrine.
12 hours. During that time, the patient will be relieved of pain from
the injury or operation. However, the surgeon will have placed the
patient at risk. Consider, for example, if the operation were performed
successfully and a dressing or cast applied after wound closure—and
then the patient developed a compartment syndrome. By the time the
patient and surgeon were aware that there was a problem, it would be
too late to prevent necrosis of soft tissue. Surgeons depend on careful
observations to warn of an impending compartment syndrome. Usually, the
first warnings come from the patient who complains of inordinate pain.
If that information is not available because of the anesthetic, the
first indication that a problem exists will come too late to reverse
the course of the injury. A better choice of agent is mepivacaine. It
will provide adequate anesthesia for an operation and recovery up to 3
to 4 hours. Then the patient will be able to alert the surgeon if the
pain is so severe that it cannot be adequately controlled by 30 to 60
mg of codeine, or its equivalent. There will be sufficient time to
relieve pressure from the cast or dressing, or to do a fasciotomy if
needed, to prevent soft tissue necrosis.
and if the sites to be operated upon are located within the digits or
palm, a wrist block would suffice. However, the surgeon must be aware
of the tourniquet time. An axillary or infraclavicular block is usually
more comfortable for the patient, and provides better flexibility for
the surgeon if the tourniquet time will extend beyond 10 to 20 minutes.
in addition to the operated extremity for skin, bone, vessel, or tendon
graft material or distant skin flap, one could still use regional
anesthesia if the patient and anesthesia services are prepared to use a
general anesthetic when needed, or if the other site can be
anesthetized with regional or local anesthesia. Otherwise, proceed with
general anesthesia from the outset.
cooperation is required or useful, such as tenolysis of adhesions to
tendons or tendon balancing, as in quadregia, a combination of regional
anesthesia (wrist block) and sedation/pain relief to control tourniquet
pain (ischemia) is used. This requires coordination with
anesthesiology. The tourniquet time must be monitored so that the
extremity is not paralyzed at the time one needs the patient to
contract muscles. Paralysis occurs about 30 minutes after a tourniquet
is applied. If the tourniquet is deflated for 5 minutes, patients can
respond to commands to contract muscles. For example, if you were doing
a tenolysis of a profundus tendon in a digital flexor sheath, you
should ask the patient to slowly make a fist. If the regional
anesthesia is adequate and sufficient analgesia has been supplied by
the anesthesiologist to block pain from the tourniquet, then the
patient should be able to contract the muscles and move the tendon
being tenolysed. The procedure described is exceptionally useful when
orchestrated properly.
use. There are four reasons why the procedure should be abandoned. Any
procedure that places the patient at unnecessary risk, places the
surgeon in the disadvantageous position of restricting options
unnecessarily, or favors the person giving the anesthesia over the
patient and the surgeon, should not remain in use. The person
administering the anesthetic is assured of rapid and easily obtained
success, but if an error is made, it can be fatal to the patient. The
surgeon cannot consider deflating the tourniquet to evaluate bleeding
potential, or for any other reason, before the operation is completed,
as anesthesia will be lost as soon as the tourniquet is deflated.
Bleeding control, wound closure, and other end-of-operation procedures
will have to be done with supplemental anesthetic injected locally, and
with attendant discomfort and anxiety for the patient. These are
sufficient reasons to discourage the use of intravenous regional
anesthesia. Let’s add a fourth and more important reason: there are
other methods that are safer for the patient and can be performed
quickly and easily if the surgeon takes the time to become proficient
and efficient using them.
environment because of the risk of pneumothorax (reported up to 6%)—and
the resulting need for assistance, positive pressure breathing, and the
possibility that a chest tube may have to be inserted. These methods
can be used effectively for shoulder operations, as well as for upper
extremity operations when experienced personnel and proper facilities
are available.
-
The length of the clavicle is palpated from its manubrial attachment to the coracoid process, and bisected in half.
-
The axillary artery pulsation is palpated in the apex of the axilla.
-
The surgeon stands on the patient’s side
opposite the side to be blocked, with the patient’s head turned
laterally away from that side, with his or her arm abducted 90 degrees
at the shoulder, and with the forearm supine. -
The infraclavicular area is prepped and draped.
-
A skin wheal is raised 2 to 3 cm below the inferior border of the midpoint of the clavicle.P.122
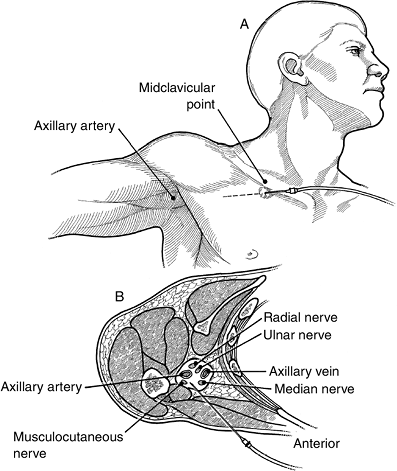
![]() Figure 8-2 The technique of a brachial plexus block, by the infraclavicular approach.
Figure 8-2 The technique of a brachial plexus block, by the infraclavicular approach. -
A nerve stimulator is used to more precisely localize the plexus, usually at a depth of 6 to 8 cm.
-
A 10 cm insulated nerve-stimulating
needle is then advanced through the skin wheal oriented laterally at a
45 degree angle. It enters tangentially, and away from the rib cage (to
reduce the risk of a pneumothorax), and is inserted in the direction of
the axillary artery pulsation (Figure 8-2).-
Initial muscle twitches elicited will be from the pectoralis major/minor.
-
Once the needle has traversed the
pectoralis muscles, stimulation of the brachial plexus cords will
produce characteristic muscle contractions at the wrist, and will
indicate entry of the needle into the sheath. -
Stimulation of median nerve twitches in particular seems to yield consistently higher success rates.
-
-
The surgeon stabilizes the needle,
aspirates carefully for blood, and injects an appropriate volume and
concentration of local anesthetic.
-
Mepivacaine 1.25% to 1.5% (35 to 45 mL) will provide 3 to 4 hours of anesthesia.
electrical stimulation. Safety, effectiveness, and ease of performance
make this the method of choice in an outpatient setting and in the
emergency room. If electrical stimulation is not available, one should
use the axillary approach instead of the infraclavicular approach.
(Compare with other methods: simplicity, repeatability, effectiveness,
risks, effect of obesity on the process, etc.) Also, the axillary
approach to the brachial plexus can be used more safely than the
supraclavicular and infraclavicular approaches in an outpatient setting.
-
All effective proximal nerve blocks are
produced by placing the anesthetic agent within the perivascular space
(axillary sheath). -
It does not matter where one enters the
space. If the volume is sufficient, the anesthetic agent will
infiltrate to all four nerves in the sheath. -
The T2 nerve is not located within the
axillary sheath. Since it supplies sensibility to the medial arm, one
should consider placing a weal of anesthetic material transversely
across the proximal arm on the medial surface to relieve pain that
could be caused by tourniquet pressure. -
Confirmation of proper needle placement within the axillary sheath can be achieved by any of the following methods:
-
Eliciting paresthesias in the distribution of the median, ulnar, and radial nerves
-
Using a nerve stimulator
-
Dividing the neurovascular bundle into
four quadrants, and depositing four aliquots of local anesthetic in
each sector around the artery after “fascial clicks” have been
obtained. Such clicks are the feedback resistance felt on perforating
the axillary sheath, which is more noticeable if one uses a “blunt”
needle.
-
one must always withdraw the plunger to be certain that there is no
blood returning through the needle.
-
The patient lies supine with the upper extremity abducted 90 degrees with or without elbow flexion.
-
The axillary artery pulse is palpated as
far proximal as possible in the apex of the axilla. Overzealous digital
pressure, or having the patient rest the hand behind the head, can
obscure the pulse. -
The axillary fold is prepped with Betadine or chlorhexidine solution, and the area is draped with sterile towels.
-
The two-finger fixation technique (using
the tips of the non-dominant index and long fingers) is used to
identify the margins of the pulse, retract the overlying skin and soft
tissue, and help immobilize the needle prior to and during the
injection. -
A skin wheal is raised over the most prominent area of the axillary artery pulse.
-
With the two fingertips gently applied
over the pulse, a 22-gauge, 3-to-5-cm conventional needle connected to
an intravenous extension set tubing (or alternatively, a 21-gauge
butterfly needle with such tubing already attached) is advanced either
perpendicular to, or at a more oblique angle with, the needle tip
oriented toward the axilla. The needle should intentionally puncture
the anterior wall of the axillary artery until bright red blood with a
pulsatile pressure head can be seen entering the extension tubing or
can be readily aspirated into the syringe.P.123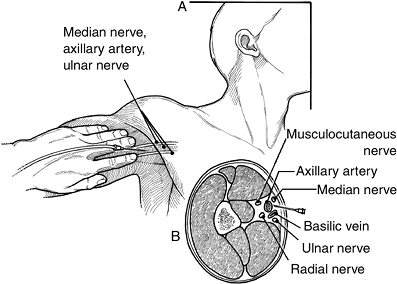 Figure 8-3 Technique of a brachial plexus block, by the axillary approach.
Figure 8-3 Technique of a brachial plexus block, by the axillary approach. -
The needle is then slowly advanced 1 cm
or more to deliberately puncture the posterior wall of the artery until
no more blood flows into the tubing or syringe (Figure 8-3). The needle tip can then be assumed to be residing in the posterior part of the neurovascular sheath. -
Because the axillary sheath is believed
to have discontinuous connective tissue septae that compartmentalize or
impede the free diffusion of local anesthetic, one should inject half
of the total dose of local anesthetic at this location. Do so after
careful confirmation that the needle tip is not inside the axillary
artery lumen. -
One slowly withdraws the needle through
the artery while aspirating for blood into the syringe. The
reappearance of blood in the tubing or syringe confirms that the needle
tip is back in the lumen of the axillary artery. -
The surgeon continues withdrawing the
needle until it exits the artery. At this location one should inject
the remaining one-half of the dose of local anesthetic agent. -
After the needle is withdrawn completely,
the patient’s arm is adducted to the side, and continuous digital
pressure is applied to the injection site to promote spread of the
anesthetic agent. -
A single needle
puncture into the axillary sheath often results in an adequate axillary
block, but it is not as frequently effective as either the
transarterial or the two-needle methods.-
To use the single needle method, it is
only necessary to place the needle into the axillary sheath and then
inject 35 to 45 mL of mepivacaine slowly. -
In the process of inserting the needle
into the sheath, one may inadvertently puncture the axillary artery. In
case this happens, merely adjust the technique to a transarterial
method.
-
-
When performing a transarterial
axillary block, one deliberately pushes the needle toward the axillary
artery, passes through it, and, after withdrawing the plunger to be
certain that the tip of the needle is not in either artery or vein,
injects the sheath as described above.-
This method yields a high degree of
success. Experience with it suggests that there are not often
complications unless one injects the agent into the artery. If this
happens, seizures and other complications can occur.
-
-
A technique that is preferred to either of the above is the two-needle
method. It is especially useful in urgent and outpatient settings where
there may not be expert help available to help deal with the
complications from other techniques. The advantage of the two-needle
method is that one can avoid the need to search for landmarks after the
first injection, which would hide and distort the anatomy because of
tissue inflation.-
A short 22-gauge blunt-tip needle is
attached to a syringe to use as a handle, and, for aspiration, to be
sure that the needle tip is not in a vessel. -
The two needles are directed into the
axillary sheath, one above and one below the artery. A “click” is often
felt when penetrating the axillary sheath. -
The axillary artery is superficial and
should be identified as far proximal in the axilla as possible. This is
the best site for injection. All four major nerves are located within
the axillary sheath at this level. Recall from our previous discussion
that there is a need for a block of T2 nerve root.
-
-
1% or 1.5% mepivacaine (Polocaine/Carbocaine), 30 to 40 mL.
-
When injecting, one can apply digital
pressure distal to the site of injection to force more of the fluid
into the proximal portion of the perivascular space. -
It takes about 20 to 30 minutes for the anesthetic to become effective, so one should arrange to use the time efficiently.
-
If the anesthesia department is planning
to perform the block, the patient should be sent for in plenty of time
for the anesthesiologist to prepare for and perform the block. -
If the surgeon is doing the block, he
should do it immediately following the proceeding case, and then do
other paper work, surgical preparations, and other things afterward.
the upper extremity high enough to prevent pain from a tourniquet. It
will also give the surgeon the flexibility to inflate and deflate the
tourniquet as needed, do surgery for 2 to 3 hours, and still have
sufficient pain relief to last for an additional hour after surgery.
Complications from infraclavicular and axillary blocks are rare and are
related to intravascular injection of the anesthetic agent.
It would be a rare event that would call for such blocks to be used
instead of an axillary or other more proximal block. The median and
radial nerves in the arm and forearm are deep within the tissue, and
lack easily identifiable landmarks. Multiple punctures and an
electrical
stimulator
would be needed to be successful. It is more comfortable for the
patient if the axillary block method is used. Also, the success rate is
higher.
 |
|
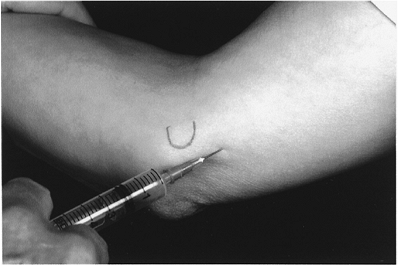
Figure 8-4 Ulnar nerve block at the elbow. The mark on the skin is over the medial epicondyle.
|
-
The ulnar nerve proximal to the medial
epicondyle of the elbow is an exception because it is accessible. In
this situation, the nerve is easily palpated just proximal to the
medial epicondyle. -
Inserting the needle about 2 to 3 cm
proximal to the medial epicondyle and parallel to the nerve, and
injecting the agent along side of the nerve at this site, will block it
successfully. -
One should not inject posterior to the
epicondyle because the nerve is often fixed in the cubital tunnel.
Injecting into the cubital tunnel increases the risk that the needle
might penetrate the substance of the nerve and cause permanent damage.
Also, the hydraulic pressure that is produced by injecting into the
partially closed space of the cubital tunnel may cause permanent damage
to the ulnar nerve by acute severe compression.
tunnel, and the needle tip is located adjacent to the easily palpated
ulnar nerve at this site (Figure 8-4).
-
Mepivacaine, 1%, 5 to 7 mL.
bleeding during a procedure on the hand when some type of peripheral
block has been performed. It is possible for the surgeon to inflate a
tourniquet to 25 to 50 mm Hg above systolic pressure for about 20
minutes. If more time is required, one will have to deflate the
tourniquet, wait about 5 minutes to restore comfort, and begin again.
This can be repeated, but the surgeon is likely to push the patient
beyond his or her tolerance of pain caused by ischemia. One should
reserve this method for operations that can be performed safely within
the 20-minute time limit. The surgeon should not let overconfidence
dictate his choice to use this method. If one anticipates that more
than 20 minutes will be required to perform an operation with care
within the time limit, an axillary block should be undertaken instead.
It is a very unhappy scene in the operating room when the surgeon is
trying to complete an operation while the patient is complaining of
pain, moving around on the table, and threatening to get off the table
and leave
-
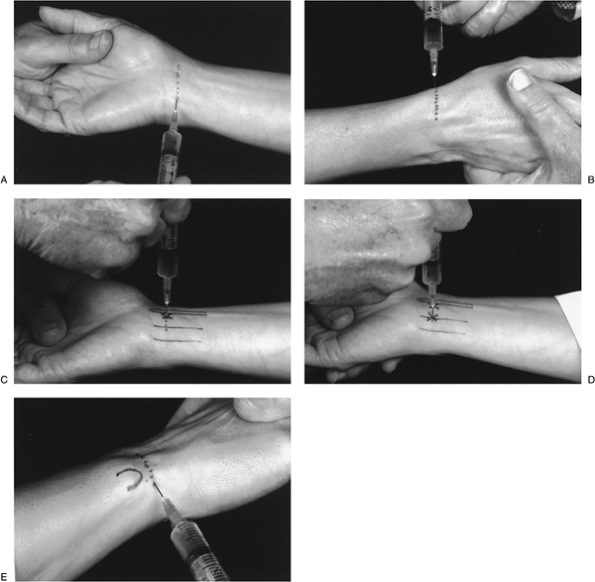
The first step is to raise a subcutaneous
wheal across the flexor surface of the distal forearm about 2 cm
proximal to the wrist flexion crease (Figure 8-5A). -
At this location, the anesthetic material
will block the last branch of the lateral antibrachial cutaneous nerve
and the palmar sensory branch of the median nerve, producing a numb
area for the subsequent injection to block the median and ulnar nerves. -
A second wheal should be raised over the radial styloid to block the sensory branches of the radial nerve (Figure 8-5B).
-
One can return to the volar site and inject through the first wheal to block the median and ulnar nerves.
-
The median nerve block is accomplished by
inserting a 22-gauge needle tip at a location 1.5 to 2 cm proximal to
the wrist flexion crease and 1 cm ulnar to the palmaris longus. -
The needle tip is inserted perpendicular
to the skin about 1.5 cm and is located within the ulnar bursa. Thus,
the median nerve is bathed by the agent and not put at risk of
perforation (Figure 8-5C). -
About 5 to 7 mL of mepivacaine is injected.
-
The ulnar nerve is blocked by inserting
the needle at the same distance proximal to the wrist flexion crease as
the median nerve block. -
The insertion should be at the radial edge of the flexor carpi ulnaris (FCU) tendon, to a depth of about 1.5 cm (Figure 8-5D).
-
Aspiration is especially important before injecting the agent because the ulnar artery and veins are very close to the nerve.
-
About 5 to 7 mL of mepivacaine will be sufficient.
-
A complete wrist block using this method will ensue within about 20 minutes.
-
A wrist block will, of course, paralyze
all of the intrinsic muscles. There may be occasions when preserving
function of the small muscles is useful, as in reconstructive
operations on the extensor hood mechanism.-
In such cases, digital blocks and use of an arm tourniquet for a short time will be a better choice.
-
Also, one can coordinate the anesthetic
with anesthesiologist as mentioned above, so that the tourniquet can be
kept in place for longer than 20 minutes.
-
-
Five to 7 mL of 1% mepivacaine is used at
the median and ulnar nerve sites, and 3 to 4 mL is administered in a
weal raised over the radial sensory nerve and the dorsal sensory nerve
from the ulnar nerve (Figure 8-5B and E).
 |
|
Figure 8-5 Wrist block. (A)
A wheal is raised to block the sensory branch of the median nerve and produce a numb area for subsequent injection of the median and ulnar nerves. (B) Technique to block the sensory branch of the radial nerve. (C) Block of the median nerve (X). (D) Block of ulnar nerve (second X). (E) Block of the dorsal sensory branch of the ulnar nerve (∈ mark on skin indicates distal ulna). See text for details of injection techniques. |
hand except for a small quarter-size area at the base of the thumb on
the volar side of the thenar eminence supplied by the branches of the
lateral antebrachial cutaneous nerve. A weal placed proximal to this
site just proximal to the wrist flexion crease will complete the block
if needed. The purpose of this subcutaneous injection of 3 to 5 mL is
to block the branches of the medial antebrachial cutaneous nerves and
the sensory branch of the median nerve that supply sensation to the
base of the thumb and palm, and to anesthetize the sites of injection
for the median and ulnar nerve blocks. Some examples of operations that
lend themselves to this type of anesthesia are carpal tunnel release
and trigger finger release. Longer operations where patient cooperation
is necessary, such as tenolysis in digits and palm, should be performed
using a wrist block, with sedation and pain control by anesthesia, so
that the tourniquet can be used as
needed and the patient can move the tendons undergoing tenolysis at the surgeon’s request.
 |
|
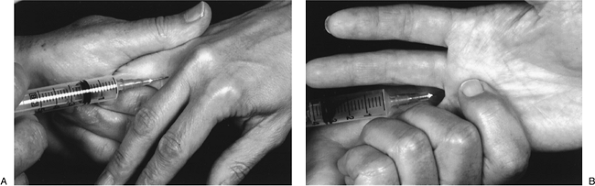
Figure 8-6 (A) Technique for finger nerve block. (B)
Palmar view of the finger nerve block, showing technique for palpating the flow of the anesthetic material into the web space and lumbrical canal. |
wide area of anesthesia. This approach avoids “circumferential” digital
block, with its implied risk of arterial spasm and necrosis of the
digit. Epinephrine is not used in any type of
finger or thumb nerve block because of its potential for
vasoconstriction and circulatory compromise. Polocaine/Carbocaine may be injected with a 22-gauge needle.
-
Assuming the person administering the
anesthetic is right handed, he or she should grasp the finger or
fingers on the left side of the web space to be injected, place the
pulp of his or her index finger in the patient’s palm between the
metacarpal heads (over the lumbrical canal), insert the 22-gauge needle
parallel to the metacarpals and into the lumbrical canal, and inject
about 3 mL of Polocaine/Carbocaine into the lumbrical canal (Figure 8-6A). -
With the index finger, the surgeon should feel the lumbrical canal inflate (Figure 8-6B), confirming that the agent is in the correct space volar to the transverse metacarpal ligament.
-
The next web space is injected in the same manner.
-
Thus, there is a block of both digital
nerves to the digit, as well as numbness on the contiguous sides of the
adjacent digits. This reduces the sensory feedback that the patient has
to tolerate. -
Additional anesthesia to the digit is
produced by raising a weal transversely across the base of the digit
about 1 cm proximal to the MCP joint as described elsewhere. -
The radial digital nerve to the index
finger is also superficial enough to be easily palpated over the first
lumbrical muscle belly. -
Two or 3 mL of anesthetic agent placed in
a transversely oriented wheal located about 1 to 2 cm proximal to the
metacarpal head will accomplish the block. -
The situation is a bit different in the
case of the ulnar digital nerve to the little finger, as it is under
fat resting upon the short flexor muscles of the hypothenar group.-
One cannot palpate the nerve, so the
injection should be done from the ulnar side of the palm with the
needle directed volar to the hypothenar muscles and into the fat
between the muscles and the skin. -
Two to 3 mL of anesthetic agent will produce a successful block.
-
-
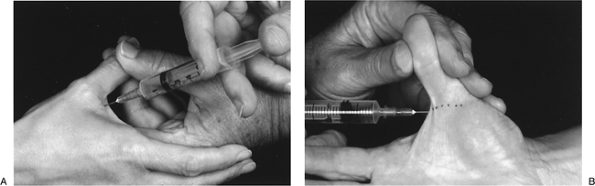
In the case of the thumb, the weal can be
placed at the level of the mid shaft of the metacarpal or more
proximal. This includes doing so at the wrist in order to completely
block the radial sensory nerve at the level of the radial styloid. -
The digital nerves to the thumb are so
superficial that they are easily palpated beneath the skin on either
side of the flexor pollicis longus. -
Raising a weal transversely across the
flexor surface of the thumb at or just proximal to the MCP joint
flexion crease easily blocks them (Figure 8-7).
-
Three mL of mepivacaine is used at each
site, and a weal is placed on the dorsum of the palm about 1 cm
proximal to the metacarpal head.
produce pain relief for about 3 hours. Some examples of operations that
lend themselves to this type of anesthesia are any operation at or
distal to the PIP joint (so there is space for a tourniquet at the base
of the digit). A surgeon could use a
tourniquet applied more proximally if he or she was very confident that the procedure would take no longer than 20 minutes.
 |
|
Figure 8-7 Technique for thumb nerve block. (A) Note the convenient and less painful site of injection for a digital nerve block of the thumb. (B)
The digital nerves of the thumb are located in the subcutaneous tissue, and are easily anesthetized by injecting a wheal of anesthetic across the flexor surface of the thumb at the MCP joint flexion crease. |
have not heard of the law or think they are above the law would use
rubber bands for a temporary tourniquet for bleeding control during
operation on a digit. The rest of us know that there is a considerable
risk that we could put a dressing over the bands and forget them—and if
this happens, when the anesthetic has worn off, the patient will
complain of inordinate pain because the digit has been rendered
necrotic by prolonged ischemia. We reduce our risk of this happening by
using a wider Penrose drain clamped with a hemostat, which will remind
us to remove it before applying a dressing. The hemostat is too large
to fit inside of most dressings. There is a device being marketed that
looks like a finger cot. The device will exsanguinate the digit as it
is rolled into place on the digit and provide ischemia during the
operation. It has the same inherent drawback that a rubber band has. It
can be hidden by dressings, and is not recommended.
is appropriate, relatively painless, and complete. One must arrange the
sequencing of care so that the process is efficient, unhurried, and
sufficient time is allowed for the anesthetic agent to become effective.