Distal Humerus Intra-articular Fractures: Open Reduction Internal Fixation
– Upper Extremity > 7 – Distal Humerus Intra-articular Fractures:
Open Reduction Internal Fixation
uncommon injuries. Despite improved surgical techniques and implants,
operative management does not guarantee an excellent clinical result.
Indications for surgery include all displaced fractures in adults who
are medically stable for surgery. Nonoperative management of displaced
intra-articular fractures of the distal humerus are associated with
unacceptably high rates of malunion, nonunion, and elbow joint
stiffness, often leading to loss of independence and subsequent
disability. The goal of surgery are identical to those of all
intra-articular fractures: stable fixation to allow early joint motion
in an anatomical position with healing of the fracture.
choice for most fractures, some injuries in the osteoporotic elderly
are probably best treated with primary elbow arthroplasty.
Contraindications to surgery include selected grade-IIIB open
fractures, active infection, extreme comminution such as found in
gunshot wounds, lack of equipment, and surgeon inexperience.
extremity is performed. A detailed neurovascular examination as well as
the status of the patient’s compartments are documented. In multiply
injured patients, evaluation of the head, chest, abdomen, and spine are
essential. In many patients, concomitant injuries take precedence over
the distal humeral fracture(s).
invariably show the fracture. However, a complete understanding of the
fracture is difficult secondary to collapse of
elbow
anatomy caused by fracture displacement. In many cases, adequate
radiographs may only be obtainable while patient is in traction and
under intravenous sedation or anesthesia. Computed tomography (CT) is
occasionally performed preoperatively. CT may reveal associated
injuries of the radial head or neck that will alter the surgical plan.
Coronal plane fractures of the anterior portion of the articular
surface of the distal humerus are also identifiable by CT. As with
plain radiographs, CT scans are most helpful when major fracture
displacement has been corrected and the arm splinted. With the
exception of open fractures, the vast majority of intra-articular
fractures of the distal humerus are done semi-urgently.
fractures, results can be improved with the creation of a surgical
plan. This involves a written step-by-step surgical tactic outlining
each step of the operation, including the placement of screws, plates,
bone grafts, and so forth. The creation of a preoperative plan ensures
that needed implants can be ordered and will be available. In addition,
when a preoperative plan is utilized, surgery and tourniquet times can
be reduced and the need for bone graft clarified.
small diameter screws (1.5 through 2.4 mm) for comminuted
peri-articular fragments as well as 3.5-mm compression and
reconstruction plates and screws. Peri-articular and/or locking plates
can be extremely useful. In some patients, 3.5-mm screws directed from
medial to lateral in the supra-articular region will exceed the 50-mm
maximum length available in the standard, small fragment instrument
tray. Therefore, supplemental screw lengths should be readily available
along with an accompanying extra-long 2.5-mm drill bit.
in the articular reconstruction. A medium, serrated, reduction clamp is
helpful during medial plate application. In patients with extensive
comminution, the iliac crest should be prepped and draped or bank bone
graft should be available.
although regional anesthesia is occasionally employed. Prophylactic
intravenous antibiotics are given before the procedure. Surgery can be
done with the patient in the lateral or prone position. I prefer the
lateral decubitus position. The arm is supported over a padded
small-diameter post that will allow intraoperative flexion of the elbow
to 110 degrees (Fig. 7.1). The entire upper
extremity, flank, and iliac crest are prepped in the same field through
the utilization of pairs of U-shaped split drapes. The arm is
exsanguinated and a sterile tourniquet applied.
The
tourniquet is later removed after the articular reconstruction is
complete. A c-arm image intensifier must be available so fracture
reduction and screw placement can be assessed.
 |
|
Figure 7.1.
The patient is placed in the lateral decubitus position with the arm draped over a padded roll; this position allows for intraoperative flexion of the ulna to 110 degrees. |
the midpoint of the arm and extending over the dorsal surface of the
ulna onto the proximal forearm. The incision is placed slightly medial
or lateral to the tip of the olecranon (Fig. 7.2.).
The ulnar nerve is identified and followed proximally to where it
emerges from the medial intermuscular septum and distally to where it
enters the flexor carpi ulnaris. The nerve is protected with a
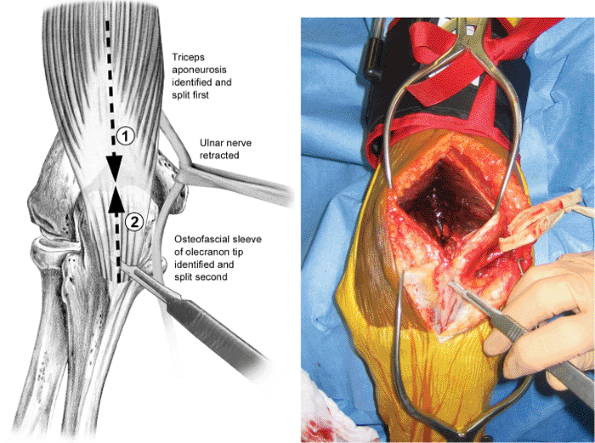
moistened Penrose drain (Fig. 7.3).
with either a formal olecranon osteotomy or a triceps slide. For most
patients, I prefer a modified Morrey triceps-splitting approach; the
split is extended longitudinally down the fascial sleeve of the
proximal
forearm.
This approach provides excellent access to the distal humerus and
decreases some of the complications associated with an olecranon
osteotomy. The extended triceps-splitting approach may be desirable
when there is transverse disruption of the extensor mechanism (which
often occurs in open fractures) and the distal humeral-shaft-fracture
fragment protrudes posteriorly through the triceps tendon.
 |
|
Figure 7.2. The anatomy is marked with ink pen on the skin. A longitudinal incision is made slightly lateral to the tip of the olecranon.
|
 |
|
Figure 7.3.
The ulnar nerve is protected with a Penrose drain. The split in the triceps tendon is connected to the split in the forearm fascia by sharp elevation of the olecranon medially and laterally. |
olecranon fossa and is carried down to the bone. The split is extended
through the posterior fat pad of the elbow joint down to the tip of the
olecranon. To expose the humeral shaft, the triceps muscle mass is
split proximally using medial and lateral countertraction and a
vertically oriented, sharp, half-inch periosteal elevator. Proximal
extension is dictated by the extent of the fracture into the diaphysis.
If the distal humerus must be exposed through the lower diaphysis, the
radial nerve must be identified and protected.
left intact while attention is turned to the most distal portion of the
incision. The interval between the flexor carpi ulnaris and extensor
carpi ulnaris is split down to the ulnar shaft. Sharp subperiosteal
dissection from distal to proximal exposes both sides of the ulna. The
depth of dissection should be to the ulnohumeral joint line medially
and to the proximal radioulnar joint laterally; the dissection should
be maintained proximal to the annular ligament of the radius.
the dense tendinous attachments remaining at the tip of the olecranon
with several, fresh, knife blades. This is most successfully performed
by proceeding toward the olecranon both proximally and distally.
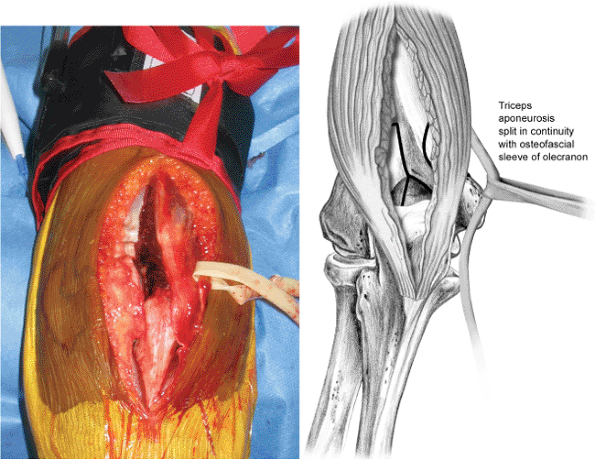
In this way, the entire extensor mechanism is opened longitudinally and is later repaired side to side (Fig. 7.4).
Small rents in the extensor mechanism, exposing a portion of the
olecranon, will not impede healing or eventual extensor function.
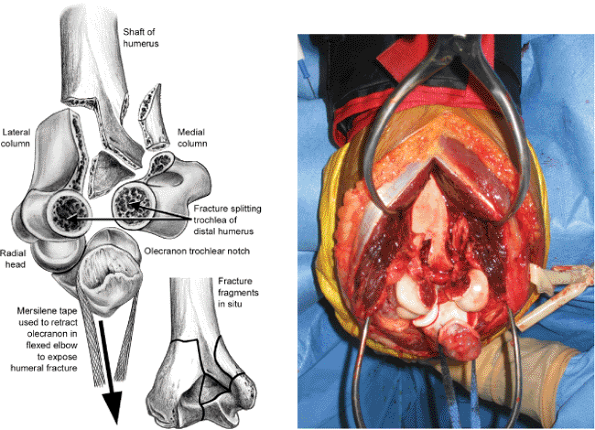
then passed around the trochlear notch of the ulna and is used to apply
longitudinal distraction to the ulna (along the axis of the humeral
shaft) as the forearm is flexed approximately 110 degrees. The entire
articular surface of the distal humerus is now exposed and the fracture
may be addressed (Fig. 7.5).
over the proximal ulna is incised and elevated 15 mm distal to the
olecranon tip. A shallow Chevron osteotomy is planned. A 2.0-mm
Kirschner (K) wire is used to drill multiple holes along the plane of
the planned osteotomy, which is completed with an osteotome. The
olecranon and the entire triceps muscle can then be reflected
proximally, exposing the entire posterior aspect of the distal humerus.
At the conclusion of the case, the osteotomy is stabilized with a
6.5-mm screw or tension band wire technique.
attachments to fracture fragments as they are cleansed of adherent clot
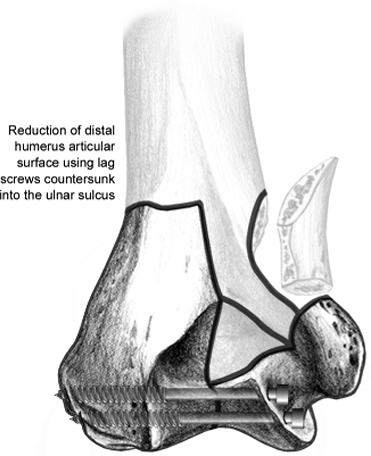
using a dental pick and forceps. Fracture reconstruction then proceeds
from distal to proximal. The articular fragments are pieced together
and provisionally held with multiple K wires. A large, pointed,
tenaculum clamp often facilitates reduction. Two screws are placed
transversely from medial to lateral through the ulnar sulcus (Fig. 7.6).
These screws are countersunk to avoid ulnar nerve irritation. Safe
sites for screw entry are limited, and many surgeons prefer to use
4.0-mm cannulated screws.
may distort the trochlear fragments leading to ulnotrochlear
incongruence. In this case, it is important to fix the trochlea
at
the appropriate width using interposition bone graft and fully threaded
positioning screws rather than lag screws. In typical instances, at
least one of the trochlear fracture fragments will also remain attached
to its respective epicondyle. This side should be used to fasten the
articular surface to its respective humeral column.
 |
|
Figure 7.4. The triceps-splitting approach is complete.
|
 |
|
Figure 7.5.
The fracture is exposed by flexing the ulna 110 degrees and applying longitudinal traction through the trochlear notch with the cord of a laparotomy sponge. |
 |
|
Figure 7.6.
The first step in reconstruction: the articular surface is reduced and stabilized with lag screws countersunk medially into the ulnar sulcus. |
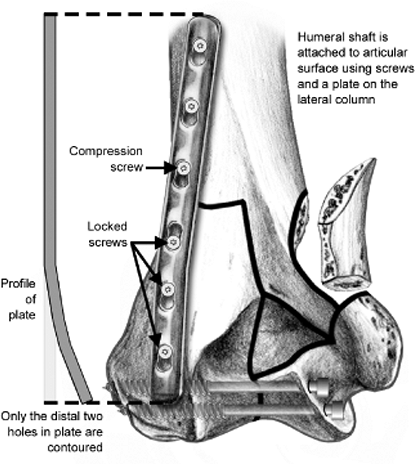
The next step in the reconstruction is realigning and reattaching the
articular surface to the distal humeral metaphysis. Plates on both the
lateral and medial column are recommended. Plates are contoured to lie
posterior on the lateral column and medial on the medial column.
Whenever possible, compression plates are used at both sites to
increase stability. However, a reconstruction plate placed medially is
often necessary. Locking plates are advantageous especially on the
lateral column where distal fixation is otherwise limited to short,
unicortical, cancellous screws with conventional low-compression
dynamic-compression (LCDC) plates.
lateral columns into the humeral shaft to reduce and stabilize the
metadiaphyseal component of the injury. Often definitive reduction and
compression to the shaft can only be performed after one of the plates
has been applied distally.
site of the two most distal holes. The proximal portion of the lateral
plate is usually left straight. (Fig. 7.7) The
lateral plate is placed as distal as possible to the edge of the
capitulum without impinging on the radial head when the elbow is fully
extended. Placing the lateral plate posteriorly provides a stable
construct and avoids the additional soft-tissue stripping required to
place the plate on the lateral aspect of the distal humerus. In
severely comminuted or osteoporotic fractures, however, the addition of
a third plate along the lateral aspect of the lateral column may
improve stability.
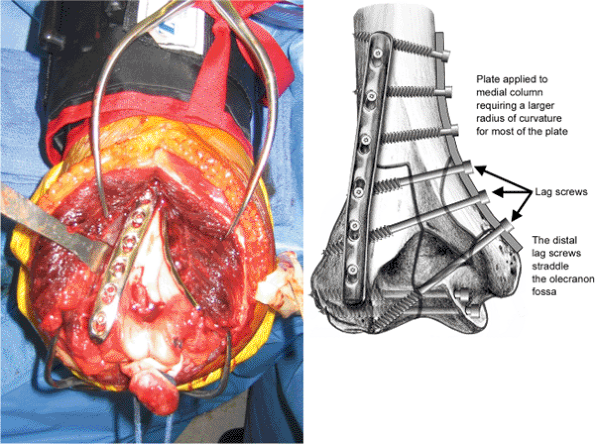
radius over most of the plate. The distal tip of the plate will lie
superior to the most prominent portion of the medial epicondyle. Stable
fixation can be compromised if the medial epicondyle is separated from
the articular fragments by fracture. In this case, specially designed,
anatomically congruent plates that curve around the medial epicondyle
may have an advantage over standard or
reconstruction
compression plates. It is very difficult to contour a compression plate
around the medial epicondyle and is not recommended.
 |
|
Figure 7.7.
The second step in reconstruction: the less comminuted column (in this case, lateral) is used to attach the articular surface to the shaft. Only the distal two holes in the lateral plate should be contoured; the proximal portion should be straight. |
epicondyle, an alternative fixation construct may be used. Purchase in
the small distal fragment may be improved via a contoured 3.5-mm
reconstruction plate that curves around the posterior aspect of the
medial column occupying the ulnar sulcus. If the curve in the plate is
sufficient, the two distal screws may be inserted orthogonally to each
other and can interlock within the bone.
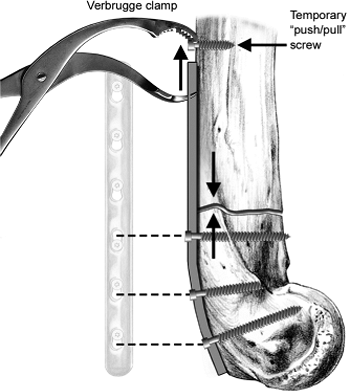
increased by fixing the reconstructed articular surface to the shaft
under compression. This can be performed by using the offset drill
guide in the oblique holes of the compression plate. In another
alternative, a unicortical push-pull screw may be inserted temporarily
proximal to the plate. A Verbrugge clamp is then used to pull the plate
toward the screw, achieving considerable compressive stability (Fig. 7.8).
screws as possible through plates and into the distal fragments. In
ideal situations, screws placed from medial to lateral through the
medial plate are anchored into a fragment on the lateral side that is
fixed by the lateral plate. To maximize distal screw length, two screws
are passed through the medial plate straddling the olecranon fossa (Fig. 7.9).
during placement of hardware from the medial to lateral direction. The
extra length facilitates protection of the bulky soft-tissue envelope
traversed by the drill. Calibrations on the drill bit and self-tapping
screws may eliminate the need to measure and tap.
plate should roughly equal the number of screws achieved distally for a
balanced fixation construct. The elbow joint is reduced and taken
through a normal range of motion while the fixation is observed.
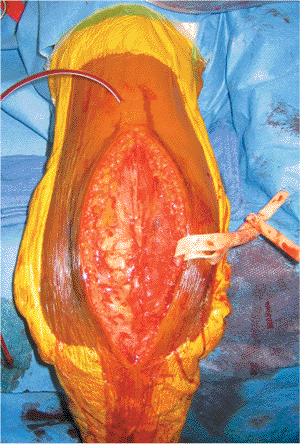
through the proximal triceps split. The extensor mechanism is repaired
with resorbable suture, and the ulnar nerve is allowed to resume its
normal anatomic position (Fig. 7.10). If the
demands of fixation require screw heads or tips protruding into the
ulnar sulcus beneath the medial epicondyle, then an anterior
subcutaneous transposition of the ulnar nerve is performed.
 |
|
Figure 7.8.
Stability is increased by applying the columnar plates under compression. Laterally, a Verbrugge clamp and push-pull screw may be used. |
in the operating room. The arm is immobilized in a plaster splint with
the elbow flexed 90 degrees and supinated.
 |
|
Figure 7.9. The final step in reconstruction: a medially applied medial column plate.
|
24 hours. The suction drain is removed the day following surgery, and
the patient is encouraged to begin active finger exercises. The splint
is removed on the third postoperative day, and the wound is recovered
with sterile dressings and a padded elbow sleeve. A sling is used for
comfort and is removed at least three times daily so the patient can
begin active and assisted range of motion in the elbow. Skin sutures
are removed in 7 to 10 postoperative days, and formal physical therapy
may begin.
Resistive strengthening is avoided until the fracture has healed and
functional range of motion has been achieved, typically at 12 weeks.
Dynamic splinting is sometimes helpful in regaining terminal extension
of the elbow. Postoperative radiographs are checked at 3, 6, 12, and 24
weeks after surgery.
by pain and inability to mobilize the patient. Late failure of fixation
may be associated with delayed union or nonunion. The
use
of compression plates rather than reconstruction plates may enhance the
longevity of the fixation construct and reduce the risk of fixation
failure.
 |
|
Figure 7.10. The triceps split has been repaired in continuity with the forearm fascial sleeve. A suction drain is in place.
|
osteotomy, such as nonunion, may be reduced by using the extended
triceps-splitting exposure described.
extensive wound debridement, lavage, and intravenous antibiotics are
required. Stable internal fixation should be retained if possible until
union occurs. If the infection cannot be eradicated in the presence of
the hardware, then after the fracture heals, the implants may need to
be removed.
J, Diederichs G, Arzdorf M, et al. A biomechanical evaluation of
methods of distal humerus fracture fixation using locking compression
plates versus conventional reconstruction plates. J Orthop Trauma May-June 2004;18:286–293.
