Olecranon Fractures: Open Reduction Internal Fixation
Direct forces drive the olecranon into the distal humerus, often
producing comminuted fractures with depressed joint fragments, similar
to a tibial plateau fracture. Olecranon fractures, which occur
indirectly through the contraction of the triceps muscle, generally
produce transverse or short oblique fracture patterns.
less than 2 mm of joint gap or step-off, intact, active-elbow
extension, and no significant fragment motion with elbow flexion.
Fractures are displaced if they do not meet these criteria (1).
reconstruction of the articular surface, restoration of the elbow
extensor mechanism, preservation of elbow motion and function, and
prevention or avoidance of complications (2).
The indications for operative treatment include displaced fractures,
injuries with elbow extensor-mechanism disruption, and open fractures.
Indications for conservative treatment include nondisplaced fractures,
injuries where the elbow extensor mechanism is intact, and poor overall
medical condition of the patient.
internal fixation (ORIF) and fragment excision with elbow
extensor-mechanism reconstruction (2,3,4).
For displaced fractures, the treatment goals are met most often with
internal fixation techniques. These techniques consist primarily of
tension band wiring or plate osteosynthesis.
but they are occasionally found in the polytrauma patient. With
isolated fractures, a history of a fall with elbow pain is the most
common presenting complaint. Physical examination reveals a painful,
swollen elbow, and in displaced fractures, a palpable defect is often
identified. Crepitus with elbow motion may also be present. The
inability to extend the elbow against gravity suggests loss of the
integrity of the elbow extensor mechanism. Neurovascular evaluation
should include particular attention to the ulnar nerve. The proximity
of the ulnar nerve places it at risk for injury, especially when direct
forces are involved in the accident.
view and a true lateral view. When the olecranon fracture is part of an
elbow fracture dislocation, traction radiographs are used to evaluate
the injury as well. The lateral radiograph reveals the extent of the
fracture and the presence of comminution or joint depression. The
integrity of the radial head–capitulum articulation is examined, and
subluxation or dislocation of the semilunar notch from the trochlea is
noted. The AP radiograph is examined for sagittal fracture lines that
are not well visualized on the lateral view. Comparison radiographs can
be helpful in complex fracture patterns.
surgical tactic developed. The preoperative plan begins with a tracing
of the fracture fragments. The fragments are then reduced on paper. The
need for bone graft to support depressed intra-articular fragments is
determined. The proposed fixation is added. The method of fixation
chosen is dependent on the fracture geometry and the experience of the
surgeon. The surgical tactic is a sequential outline of the planned
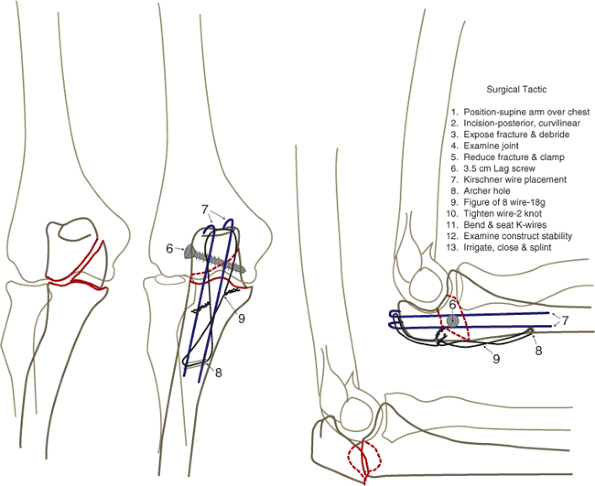
procedure and is added to the drawing (Fig. 8.1).
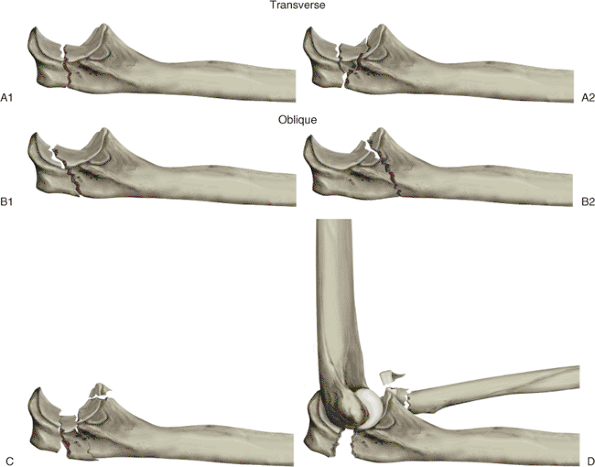
The fractures are divided into three types: extra-articular (21-A),
articular and involving the surface of one bone (21-B), and articular
and involving the surface of both bones (21-C). Extra-articular
avulsion fractures are type 21-A
while
intra-articular fractures are type 21-B. A more detailed description of
this classification is found in the Orthopaedic Trauma Association’s Fractures and Dislocation Compendium (5).
 |
|
Figure 8.1. Preoperative plan. This is a tracing from the radiographs: ulna (blue); fixation (red); and humerus/radius (black).
|
Transverse and oblique fractures may have a depressed joint segment
similar to that seen in tibial plateau fractures. Depressed segments
are elevated and may require bone graft or other support to maintain
elevation. Oblique fractures can be oriented proximally or distally.
Lag screws are frequently used with oblique fractures. Comminuted
fracture patterns usually occur in isolation, but the radiographs must
be scrutinized to rule out a fracture dislocation of the elbow.
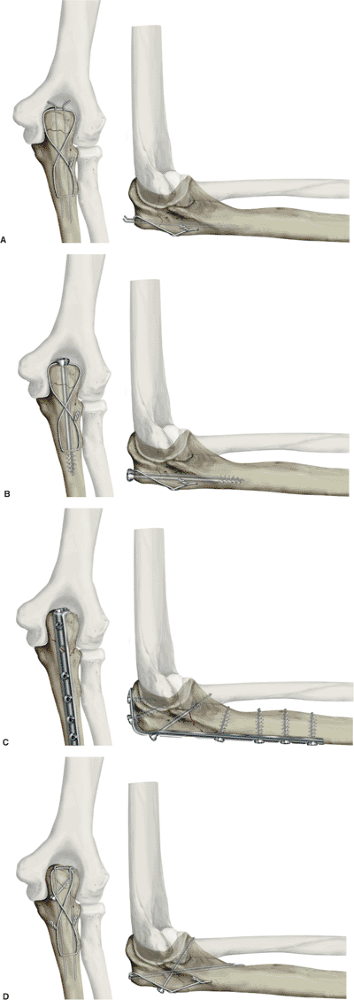
A tension band construct may consist of two Kirschner (K) wires with a
figure-of-eight wire or cable, or it may be made of an intramedullary
screw with a figure-of-eight wire. Alternatively, a lag screw and
dorsal plate (3.5-mm semitubular or reconstruction) can be used (Fig. 8.3A–C).
The cable is easier to place and has a low-profile crimp rather than
two prominent wire knots. A figure-of-eight wire alone does not provide
sufficient stability to resist physiologic loading (21). Advocates of the lag screw–dorsal plate technique cite less operative time, better reductions, fewer
hardware symptoms, less postoperative loss of reduction, and lower incidence of infection (7,10,20,26).
The lag screw–neutralization plate construct consists of a lag screw
across the fracture and a radial, ulnar, or dorsal neutralization
plate. Two K wires with a figure-of-eight wire will also neutralize the
lag screw (Fig. 8.3D).
 |
|
Figure 8.2. Olecranon fractures: (A1) transverse, (A2) transverse with joint depression, (B1) proximal oblique, (B2) distal oblique, (C) comminuted, (D) fracture-dislocation. (From
McKee
MD, Jupiter JB. Trauma to the adult elbow and fractures of the distal humerus. In: Browner BD, Jupiter JB, Levine AM, et al, eds. Skeletal trauma. Philadelphia: W.B. Saunders; 1992:1455–1522 ; Fig. 41-16.) |
clinical experience, the surgeon must determine which fixation
technique to employ for a given fracture. In the absence of
complications, outcomes for each of the fixation techniques are
comparable (12,21).
However, biomechanical and clinical evidence suggests that certain
techniques may be advantageous when applied to specific fracture
patterns.
 |
|
Figure 8.3. Tension-band constructs. A. Two K wires with a figure-of-eight wire (33). B. Medullary screw with a figure-of-eight wire (33). C. Dorsal plate with lag screw. D. Two K wires that engage the anterior cortex plus lag screw. (A and B from
Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg 1985;67A:1396–1401
; C and D from Helm U. Forearm and hand/mini-implants. In: Muller ME, Allgower M, Schneider R, et al, eds. Manual of internal fixation. Berlin: Springer-Verlag; 1991:453–484
, Fig. 8.6.) |
treatment for transverse, noncomminuted, olecranon fractures, but they
may also be used in some comminuted fracture patterns. In commonly used
constructs, intramedullary K wires or an intramedullary screw, combined
with either braided cable or monofilament wire, are used. In terms of
biomechanics, tension band techniques are thought to convert the force
generated by the elbow extensor mechanism into a dynamic compressive
force along the articular surface of the
semilunar notch during active elbow motion (7).
Although the validity of this biomechanical principle has been recently
challenged, the clinical efficacy of tension band techniques is well
documented (15,18,22).
A plate, often in conjunction with a lag screw, can also be used in
oblique fractures. Whereas proximal oblique fractures are effectively
treated with either tension band wiring or interfragmentary lag screws
with a neutralization plate, the interfragmentary lag-screw
fixation-neutralization plate construct has been demonstrated to
possess a biomechanical advantage in treating more distal oblique
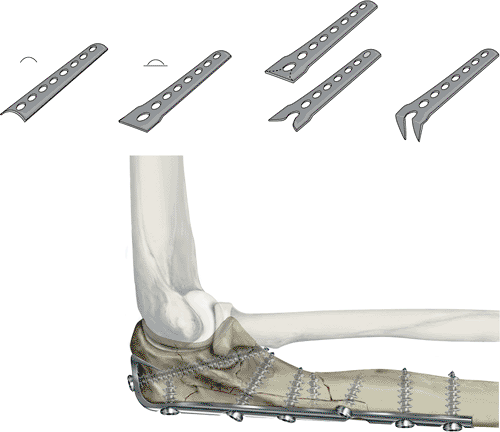
fractures (14). Because of the subcutaneous location of the olecranon, mini and small fragment plates are indicated (Fig. 8.4D). Recently, olecranon-specific peri-articular plates have been developed as have standard locking plates.
require joint elevation and bone grafting. Larger joint depressions may
require adjunctive fixation with miniscrews or
plates,
K wires, and absorbable pins. A lag screw and a 3.5-mm plate or two K
wires with a figure-of-eight wire are indicated for proximal and distal
oblique fractures. Bone graft, lag screws, and a dorsal-neutralization
3.5-mm semitubular hook (see Fig. 8.4D),
reconstruction, or compression plate all are required for comminuted
fractures. Repair or reconstruction of the associated injuries in
comminuted olecranon fractures is also required.
 |
|
Figure 8.4. Hook plate. A. One end of a 3.5-mm semitubular plate is B. flattened with a mallet and bending irons. C. A wire cutter is used to cut away a portion of the distal plate hole. D.
The two cut ends are then bent to 90 degrees. The plate is then contoured to the olecranon. Two holes are placed in the proximal olecranon to ease insertion of the hooks into the fragment. E. Cut portions of the plate are bent 90 degrees. (From Mast JW, Jakob R, Ganz R. Planning and reduction techniques in fracture surgery. Berlin: Springer-Verlag; 1989
; Figs. 3.17 and 4.37.) |
Although some authors have demonstrated maintenance of elbow stability
with excision of up to 80% of the trochlear notch, others have
demonstrated a linear decline in elbow stability with increasing
amounts of bone excision. Furthermore, several investigators have shown
that fragment excision results in relatively elevated joint pressures
in comparison to those found after internal fixation (7,18,28). Whenever possible, the amount of resected bone should be minimized.
dislocations of the elbow are beyond the scope of this chapter, we
implore the surgeon to be vigilant in the identification of associated
radial-head fractures, coronoid fractures, and Monteggia
fracture-dislocations. When treating olecranon fractures, these
additional injuries must be addressed because they may compromise the
elbow function if left untreated.
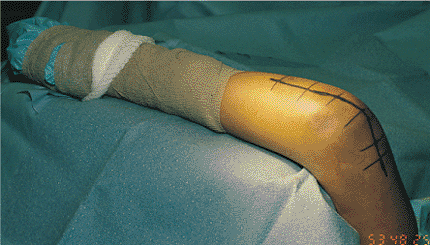
either regional (Bier or axillary block) or general anesthesia is
administered. A tourniquet is applied, and the arm is placed in an arm
holder across the patient’s chest (Fig. 8.5).
Antibiotic prophylaxis consists of a cephalosporin for closed injuries,
and for open injury, an aminoglycoside or penicillin (or both) are
added to cefazolin. A c-arm image intensifier is positioned at either
the head or foot of the table on the side of injury.
A sterile Kerlex dressing (Kendall Healthcare Products, Mansfield, MA)
is wrapped around the wrist, and a weighted speculum attached to the
end of the Kerlex is passed off the table (Fig. 8.7).
The weighted speculum provides enough traction to maintain the arm on
the arm holder with the dorsal surface exposed. This eliminates the
need for an assistant to hold the arm. As an alternate, the patient may
be placed in a lateral decubitus position with the arm over a post. The
elbow rests in flexion. The elbow is then extended to aid in the
reduction. An iliac crest is also prepped and draped if the
preoperative plan specifies the need for a bone graft.
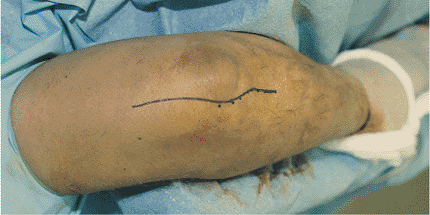
subcutaneous border of the ulna to the olecranon area, where it is
curved radially around the tip of the olecranon and then extended
proximally in the midline 3 to 5 cm.
 |
|
Figure 8.5. The patient’s arm is placed across the chest on an arm holder. A tourniquet is applied.
|
 |
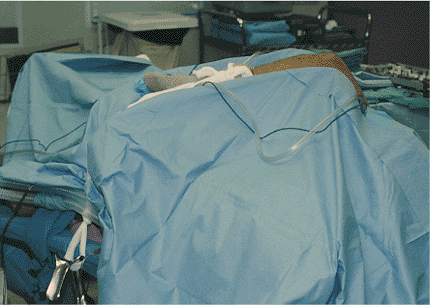
|
Figure 8.6. The patient’s arm is prepped and draped for surgery and placed on the arm holder.
|
 |
|
Figure 8.7.
A sterile Kerlex is wrapped around the patient’s forearm. A weighted vaginal speculum is attached to the Kerlex. The traction holds the arm on the arm holder. |
 |
|
Figure 8.8.
The skin incision is begun distally along the ulnar subcutaneous border and is curved radially around the tip of the olecranon and extended proximally in the midline. |
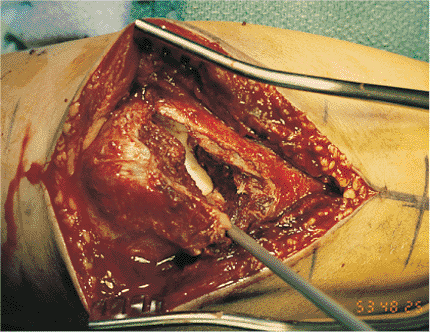
subcutaneous flap is elevated over the tip of the olecranon from radial
to ulnar. The dorsal component of the fracture line is now usually
visible (Fig. 8.9). Two millimeters of
periosteum is reflected from either side of the fracture lines to
simplify visualization and fracture reduction. Distally, muscle origins
are reflected extraperiosteally as needed. The fracture lines are
cleaned of clot and debris. The joint is visualized by retracting the
proximal fragment. The joint is cleaned of clot and debris.
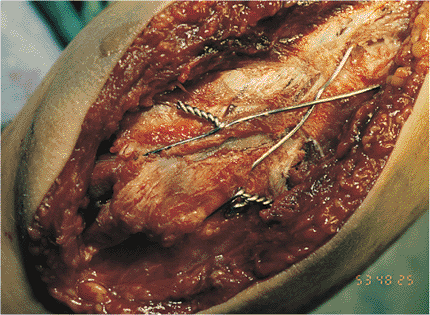
depressed articular component, if present. Bank or autogenous bone
graft is used if necessary to support the depressed fragments.
Small-screw fixation can be added if necessary. The fracture is then
reduced and temporarily held in place with K wires or pointed reduction
clamps. Additional lag screws are used if needed (Fig. 8.10). The fixation construct is determined by the preoperative plan.
guide (Fig. 8.11).
The K wires are over-inserted 1.0 to 1.5 cm and then are backed out to
ease seating to the final depth. The K wires are placed down the
intramedullary canal of the ulna. Alternately, the K wires can engage
the anterior cortex of the ulna (see Fig. 8.3D),
which may diminish pin migration. Intraoperative radiographs are
obtained to verify the reduction and fixation position. We have
abandoned the technique of anterior cortical engagement because
precisely estimating the K wire length is technically difficult but
necessary for preventing forearm rotational impingement or
neurovascular injury should the K wire excessively protrude through the
anterior cortex.
 |
|
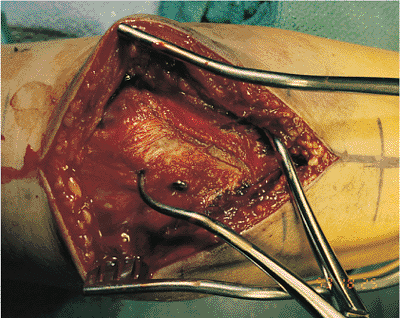
Figure 8.9.
The incision is carried down to the fascia and periosteum. A subcutaneous flap is developed radially with the skin over the tip of the olecranon. The dorsal component of the fracture line is now visible. |
 |
|
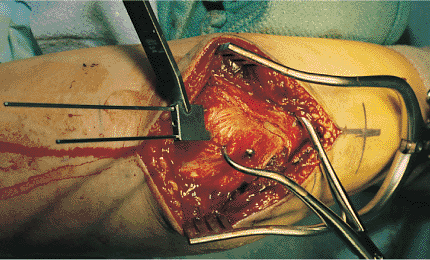
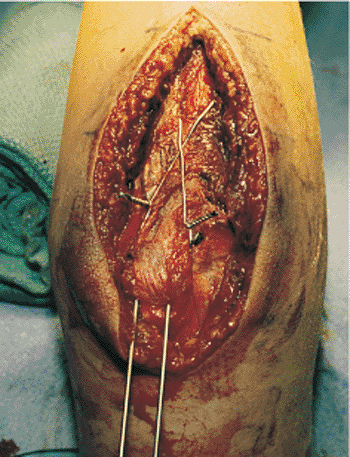
Figure 8.10.
The fracture is reduced and held in place with a pointed reduction clamp. In this case, one lag screw is placed across the fracture. |
the ulna approximately 3 to 4 cm distal to the fracture (distal anchor
hole). This drill hole is approximately halfway between the volar and
dorsal surfaces of the ulna. Anterior placement of this drill hole has
been advocated based on a mathematical analysis (24).
The anchor hole may be drilled before or after fracture reduction and K
wire placement. Drilling the distal anchor hole before K wire placement
avoids the potential complication of the drill hitting the K wires but
does not eliminate the possibility that the K wires will prevent
tension-band-wire placement in the distal anchor hole.
distal drill hole. This wire is then crossed over the dorsal surface of
the olecranon. A small loop is added to the wire proximal to the point
where the wire crosses the dorsal olecranon surface on the radial side (Fig. 8.12).
A 14-gauge angiocatheter is then passed from ulnar to radial side
between the triceps tendon and the tip of the olecranon to help avoid
injury to the ulnar nerve. The needle is removed. The radial limb of
the figure-of-eight wire is inserted into the angiocatheter (see Fig. 8.12), and the angiocatheter is gently pulled back out (Fig. 8.13). The figure-of-eight wire is now located anterior to the triceps insertion, which has been shown to be the optimal position (8).
This portion of the wire is twisted to the other end of itself. Two
knots are now present in the wire, one knot on each side of the ulna.
provides more uniform tension to the bone-implant construct. The knots
are cut to a length of 3 to 4 mm, bent down, and buried in the soft
tissues (Fig. 8.14). The K wires are bent dorsally just past 90 degrees with a metal suction tip (Fig. 8.15) and cut, leaving 3 to 4 mm of wire remaining past the bend. By using a wire pliers, the K wires are bent over to 180 degrees (Fig. 8.16) and rotated until
the short portion of the bent wire is anterior. The K wires are then seated with a mallet and nail set (Fig. 8.17).
 |
|
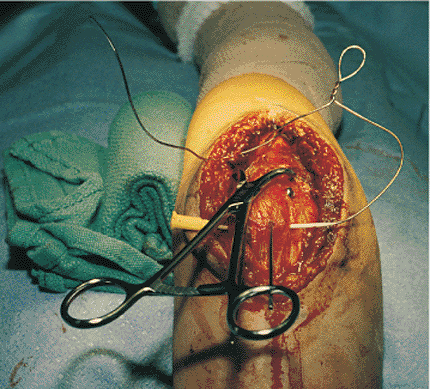
Figure 8.11.
The preoperative plan in this case included a tension band construct with K wires and a figure-of-eight wire. Two 1.6-mm K wires are placed across the fracture site with a parallel drill guide. |
 |
|
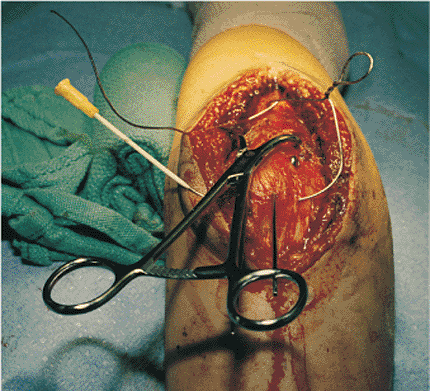
Figure 8.12.
The figure-of-eight anchor hole is placed in the distal fragment. A wire is passed through the hole and crossed over the dorsal cortex of the ulna. A twist with a loop is placed into the limb of the wire that is now radial. A 14-gauge angiocatheter is passed from ulnar to radial side anterior to the triceps tendon along the tip of the olecranon. The needle is removed. The radial limb of the wire is put into the angiocatheter. |
 |
|
Figure 8.13.
With gentle pushing on the wire, the angiocatheter is removed. The figure-of-eight wire now lies anterior to the triceps tendon on the tip of the olecranon. This end of the wire is twisted to itself. |
 |
|
Figure 8.14.
By using two needle holders, the figure-of-eight wire is tightened by twisting the loop on the radial side and the knot on the ulnar side. The twists are cut to a length of 3 to 4 mm. |
small crimp instead of figure-of-eight wire. The cable sleeve is placed
along the ulna so that the soft tissues can easily cover it, making it
less prominent. In theory, the cable has the ability to achieve greater
tension in a more symmetric fashion than the figure-of-eight wire. Care
must be exercised to avoid applying too much tension on the cable,
resulting in fragment crushing and loss of reduction.
obtained. The fracture is examined through a full range of elbow motion
to verify stability (Fig. 8.18). The wound is
irrigated and closed in layers. A drain is not used if adequate
hemostasis is obtained after tourniquet release. The arm is placed into
a posterior plaster splint. Antibiotics are continued for 24 hours.
 |
|
Figure 8.15. The two K wires are bent dorsally to 90 degrees with a metal suction tip and a heavy needle holder.
|
 |
|
Figure 8.16. The K wires are then cut, leaving 3 to 4 mm past the bend. A heavy needle holder is used to bend the K wires to 180 degrees.
|
 |
|
Figure 8.17.
The bent K wires are rotated 180 degrees so that the short end of the bend is now anterior. The K wires are seated with a nail set. |
Advocates of this technique point out that static and dynamic
compression are applied, that the screw is less likely to back out, and
that this fixation is the strongest biomechanical construct (12,16,21).
Disadvantages include prominent hardware and loss of reduction as the
screw engages the distal ulnar canal, causing fragment translation.
A 6.5-mm cancellous (32-mm thread length) or 4.5-mm malleolar screw is
used. A washer is used to help anchor the figure-of-eight wire
proximally. The triceps tendon is split in line with its fibers. The
pilot hole is drilled, starting at the tip of the olecranon, and
subsequently tapped. An alternative method is to leave the fracture
displaced and to drill the pilot hole retrograde into the proximal
fragment. The fracture is then reduced and held in place with clamps.
The pilot hole is identified in the proximal fragment and the drill bit
is inserted through it into the distal fragment.
proximal fragment can occur. Before final seating of the screw, the
figure-of-eight wire is inserted as described. The wire is passed
around the screw below the triceps tendon. After the wire is tightened,
the screw is
seated.
The washer is located on the bone deep to the triceps tendon. This
technique avoids injury to the triceps tendon during final seating of
the screw. The procedure continues as described.
 |
|
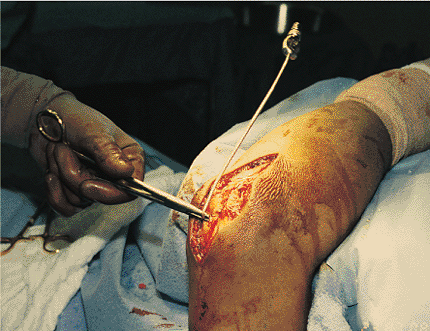
Figure 8.18. The reduction and quality of fixation is evaluated as the arm is placed through a range of motion.
|
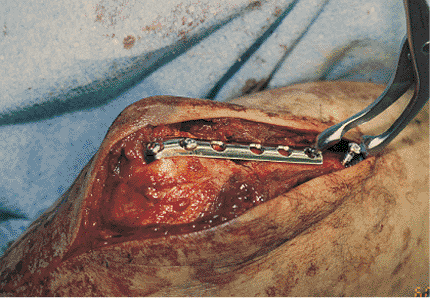
through the plate, across the fracture, and placing a plate on the
dorsal surface of the olecranon (see Fig. 8.3C).
It is especially useful with oblique fractures in the sagittal plane.
The lag screw is usually inclined from just distal to the tip of the
olecranon to the coronoid process. The plate is bent around the tip of
the olecranon, and two screws are placed proximally. The plate is
tensioned by first placing a screw distal to the end of the plate. One
limb of a Verbrugge clamp is then placed around the screw head, and the
other hooks the last hole in the plate (Fig. 8.19).
Closing the clamp applies tension to the plate. As an alternative, an
articulated tensioning device can be used to tension the plate. Three
to four screws are then added distally. The procedure continues as
described previously. The use of a peri-articular plate with or without
locking screws can be very helpful.
comminuted fractures. Care is taken to avoid devascularization of bone
fragments. Reduction proceeds in a step-wise fashion. Temporary
fixation is achieved with K wires. The quality of the reduction,
proposed final fixation, and bone is now assessed. If the fracture
cannot be reduced, a spanning or bridging plate can be considered, or
the fragments excised, and the triceps tendon advanced.
reduction, then final fixation is applied. K wires are replaced with
lag screws. Bone graft is used to support osteochondral fragments. A
dorsal plate is then applied to neutralize the lag screws. Several
custom-designed plates are currently available. In addition, locking
plates now offer other alternatives for fixation. While their role
needs to be better defined biomechanically before advocating routine
use, we have found locking plates very useful when the fracture is
comminuted or is in osteopenic bone. A pelvic reconstruction plate can
also be shaped to fit dorsally to the tip of the olecranon. In another
alternative, a 3.5-mm semitubular plate is fashioned into a hook plate
(see Fig. 8.4A–C) and shaped to fit dorsally to the tip of the olecranon (Fig. 8.4E).
The hooks engage the olecranon at the most proximal point. This
supplies additional points of fixation. The quality of fixation is
assessed by moving the elbow neutral to 120 degrees. Closure continues
as previously described.
room immediately, where irrigation and debridement of the injury are
completed. The open wounds are extended as needed. Fixation proceeds as
previously described. Part of the wound is left open, but the joint may
be closed over a suction drain. The patient is returned to the
operating room on postinjury days 2 and 4 for wound and fracture
irrigation and debridement. Wound closure is completed on postinjury
day 4. Wound closure is accomplished by
delayed
primary closure, skin graft, local rotational flap, or free-tissue
transfer as needed. Antibiotics are used for 24 hours after each wound
manipulation.
 |
|
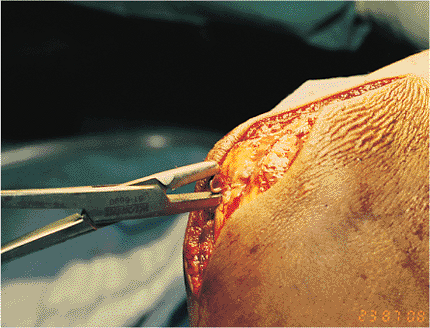
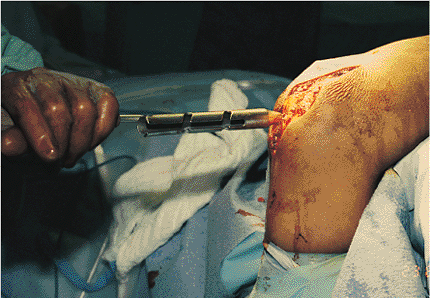
Figure 8.19.
The fracture is reduced and a plate applied. A screw is placed into the ulna. A Verbrugge clamp is applied to the screw and the plate. Closing the clamp puts tension on the plate. This is unmeasured tension and care must be taken so the fracture is not displaced. |
phases: initial, motion, and strengthening. Initially, the limb is
splinted at 90 degrees for 3 to 5 days to promote soft-tissue healing.
The second phase (motion) depends on the fixation used. Patients with
fractures fixed with the tension band principle begin early active
motion on day 5. A cast brace is used as needed; the decision is based
on fixation quality and patient reliability. Fractures fixed with the
lag screw–neutralization principle are placed in a long arm cast for a
total of 2 to 3 weeks. A cast brace is used for an additional 3 to 4
weeks. Active and active-assisted motion exercises continue until the
patient enters phase three. Isometric and isotonic exercises are
started early as dictated by patient tolerance.
for entering this phase are radiographic evidence of progression to
union, clinical evidence of union (no pain with physiologic stress),
and an active range of motion of at least 75% of the contralateral
elbow (75% of normal with bilateral injuries). The patient begins a
progressive-resistance program designed to strengthen the entire upper
extremity. Functional capacity evaluations are used for return to work
for manual laborers.
of fixation and the intraoperative stability achieved. If stable
fixation is achieved, even in comminuted fractures, then the protocol
continues as described. If the quality of fixation will not withstand
early motion, then the arm is splinted for 3 weeks. The rehabilitation
protocol then continues as described and is adjusted if needed.
olecranon fractures are related to the hardware. Hardware symptoms are
present in 22% to 80% of cases (7,10,13,26,29,31,32,33).
K wire migration occurs in up to 15% of the cases. Hardware removal is
required in 20% to 66% of fractures. Hardware failure occurs in 1% to
5% of cases.
used, several steps may help avoid symptoms related to the implants. K
wires are over-inserted 1 cm and then backed up to ease deep final
seating. The K wires are bent 180 degrees before final seating so that
the bent portion of the wire penetrates the tip of the olecranon,
making the wires less prominent. K wires that engage the anterior
cortex may prevent the wires from backing out (23).
The figure-of-eight wire knots should be buried in the surrounding
muscle to avoid their prominence. The use of plate fixation may
decrease the incidence of hardware-related complaints and the need for
subsequent hardware removal (25,34).
However, hardware prominence, symptoms, and removal may be unavoidable
in this very superficial area. The preoperative discussion should
include a description of the hardware-related symptoms and the frequent
necessity for hardware removal.
infection is reduced with the use of perioperative antibiotics and in
open fractures with attention to the soft tissues and wound closure.
Acute infection is managed with irrigation and debridement as needed,
antibiotics, and wound closure or soft-tissue reconstruction (tissue
transfer).
of the cases. The ulnar nerve is not routinely exposed during ORIF, but
the surgeon’s constant awareness of its location minimizes the
possibility of injury. Observation is usually all that is required as
symptoms either quickly resolve or improve with time. Late neurolysis
may reduce symptoms in some patients.
fractures. Indomethacin is recommended to help prevent heterotopic
ossification in fractures at risk (associated, severe, soft-tissue
injury,
or elbow dislocation). Significant heterotopic ossification is treated
with delayed resection and prophylactic irradiation.
JB, Mehne DK. Trauma to the adult elbow and fractures of the distal
humerus. In: Browner BD, Jupiter JB, Levine AM, et al, eds. Skeletal trauma: fractures, dislocations, ligamentous injuries. Philadelphia: W. B. Saunders; 1992:1125–1176.
MD, Seiler JG, Jupiter JB. The application of the limited contact
dynamic compression plate in the upper extremity: an analysis of 114
consecutive cases. Injury 1995;26:661–666.
M, Whitelaw GP, Cimino W, et al. Postoperative complications of tension
band wiring of olecranon fractures. Paper presented at: The Eighth
Annual Orthopaedic Trauma Association Meeting; October, 1992;
Minneapolis, Minnesota.
BR, Ede DE, Brown TD. Fractures of the olecranon: an in vitro study of
the elbow joint stresses after tension-band wire fixation versus
proximal fracture fragment excision. J Trauma 2002;53:1088–1093.
GP, Novak VP, Jinnah RH, et al. Biomechanical evaluation of tension
band placement for the repair of olecranon fractures. Clin Orthop 1997;335:325–330.
MJ, Williams JL, Marshall MP, et al. Biomechanical comparison of
fixation methods in transverse olecranon fractures: a cadaveric study. J Orthop Trauma 1997;11:565–572.
NC, Garnham IR, Wolinsky PR, et al. Posterior olecranon plating:
biomechanical and clinical evaluation of a new operative technique. Bull Hosp Joint Dis 2002;61:27–31.
