Head Injuries
received increasing attention. This is the result of the early
retirement of well-known professional athletes, such as Steve Young,
Troy Aikman, Pat Lafontaine, Merrill Hodge, and others who have
sustained multiple concussions. There is an increasing awareness of the
frequency and effects of head injury in sports. This chapter will
provide information to help physicians, coaches, and trainers to
diagnose, treat and, hopefully, prevent head injuries in athletes.
concussion. Multiple definitions of concussion exist. The word itself
is derived from the Latin verb concussus,
which means “to shake violently.” The Committee on Head Injury
Nomenclature of the Congress of Neurological Surgeons defines
concussion as “a clinical syndrome characterized by immediate and
transient posttraumatic impairment of neural function, such as
alteration of consciousness, disturbance of vision, equilibrium, etc.,
as a result of brainstem involvement.” As Kelly has stated, a
concussion is a “trauma-induced alteration in mental status that may or
may not involve loss of consciousness.” The American Orthopaedic
Society for Sports Medicine defines concussion as “any alteration in
cerebral function caused by a direct or indirect (rotation) force
transmitted to the head resulting in one or more of the following acute
signs and symptoms: a brief loss of consciousness, light-headedness,
vertigo, cognitive and memory dysfunction, tinnitus, blurred vision,
difficulty concentrating, amnesia, headache, nausea, vomiting,
photophobia, or balance disturbance. Delayed signs and symptoms may
also include sleep irregularities, fatigue, personality changes,
inability to perform usual daily activities, depression, or lethargy.”
physiologic disturbance without structural damage, animal and human
data have shown that neurochemical and structural changes with loss of
brain cells can occur. A neurochemical cascade begins within minutes
after a concussion and can continue for days. It is during this period
that neurons remain in a vulnerable state, susceptible to minor changes
in cerebral blood flow, increases in intracranial pressure, and anoxia.
Animal studies have shown that, during this susceptible period, a
decrease in cerebral blood flow that normally would have little
consequence can produce extensive neuronal cell death.
This syndrome occurs in an athlete who has sustained an initial head
injury, most often a concussion, and returns to play while still
symptomatic and sustains a second head injury. The second impact to the
symptomatic brain can result in a loss of cerebral autoregulation,
leading to rapid cerebral vascular congestion, increased intracranial
pressure, and brain herniation. The condition typically occurs in
adolescents aged 14 to 16 and is uncommon in adults. It appears to have
a common pathophysiology with “diffuse cerebral swelling” or “malignant
brain edema” syndrome in children.
school football alone accounts for about 250,000 brain injuries each
year. Approximately 1 in 20 high school football players sustain a
concussion in a given season. Head injury accounts for 75% of all
fatalities in high school football. Of these fatalities, the majority
(74.4%) are the result of subdural hematomas. Between 1980 and 1993, 35
football players succumbed to the second impact syndrome.
During a single season of Canadian intercollegiate ice hockey, the
incidence of concussion was 1.55 per 1,000 athletic exposures.
Concussion rates among college soccer players are estimated to be about
1 per 3,000 athletic exposures. Concussions occur in many other sports,
including wrestling, lacrosse, motor sports, bicycling, diving,
basketball, baseball, field hockey, gymnastics, rugby, volleyball,
track and field, and softball. One study sampling students from a
boarding school with mandatory sports participation reported that 97%
of athletes aged 14 to 19 years had sustained at least one
sports-related concussion.
In the National Football League, it is estimated that 100 to 120
concussions occur per year, or about one every two to three games. In
professional soccer, 52% of players have reported at least one
concussion in their career. The National Hockey League (NHL) has seen
an increase in the number of concussions, with the rate from 1997 to
2002 more than triple that of the preceding decade. Multiple theories
have been proposed for the increase, such as bigger, faster players,
new equipment, and harder boards and glass. Fortunately, the rate has
reached a plateau since 1997, which was the year the NHL instituted its
concussion program.
may be at higher risk for concussion. For example, the concussion rate
for collegiate soccer players is estimated at 1 per 3,000 athletic
exposures, whereas the rate for high school players has been reported
at 1 per 2,000 exposures. Among Canadian amateur hockey players aged 15
to 20, 60% have reported sustaining a concussion during either a
practice or a game. Authors have expressed concern that injury during
adolescence may impair the plasticity of the developing brain.
|
TABLE 7-1 1989-1998 NCAA INJURY SURVEILLANCE SYSTEM CONCUSSION DATA
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||
gender differences in regard to concussion rates. In high school
sports, females were found to be at higher risk for sustaining a
concussion than males competing in the same sport. The rate in soccer
was 1.14 concussions per 100 player-seasons in females and 0.92 per 100
player-seasons in males. In basketball, females had a rate of 1.04
concussions per 100 player-seasons, whereas males had a rate of 0.75
per 100 player-seasons. In softball, the rate was 0.46 for females and
0.23 for males. This trend does not remain at all levels. At the
collegiate level, the concussion rate for soccer and basketball players
appears to be nearly identical. At the Olympic level, 89% of male and
43% of female soccer players have reported a prior history of
concussion.
divided into several categories: primary injury, secondary injury,
inflammatory response, and repair/regeneration process. The primary
injury generally occurs after an external impact to the head. Contact
forces can cause a focal injury, such as a skull fracture, epidural
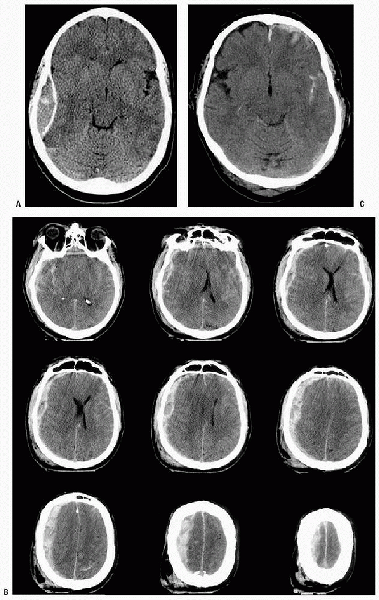
hematoma, subdural hematoma, or coup or contra coup injury (Fig. 7-1).
Inertial or accelerative forces to the head can cause these focal
injuries, as well as more diffuse injury such as diffuse axonal shear.
brain injury and is associated with the production and release of
neurochemicals that alter cerebral blood flow, ion homeostasis, and
metabolism. After a concussion or minor traumatic brain injury,
disruption of the neuronal cell membrane, stretching of axons, and
opening of potassium channels lead to an efflux of potassium out of
affected neurons. Depolarization of neurons leads to release of
glutamate, which further induces an efflux of potassium. The
extracellular potassium leads to a release of excitatory amino acids
and further depolarization, both serving to further increase
extracellular potassium. Increased adenosine triphosphate (ATP) is
required to restore the imbalance in potassium and membrane potential.
Glucose utilization increases, leading to a state of hyperglycolysis
that in rat studies lasts several hours but in humans may last
significantly longer. Lactate levels increase, which can cause neuronal
damage and lead to increased vulnerability to cell damage.
influx of calcium into neuronal cells. Elevated intracellular calcium
may activate proteases and cause cell damage or death. Oxidative
phosphorylation slows, which results in decreased ATP availability and
a further increase in glycolysis. Cerebral blood flow has been seen to
decrease 50% after concussion. This drop may further impair the
neurons’ ability to maintain a normal electrolyte balance.
magnesium, which may not return to normal for four days. Decreased
magnesium can cause a further influx of calcium. It is also associated
with impairment of glycolysis, oxidative phosphorylation, and protein
synthesis.
 |
|
Figure 7-1 A: Computed tomography (CT) scan appearance of epidural hematoma. B: CT scan appearance of subdural hematoma. C: CT scan appearance of subarachnoid hematoma.
|
|
TABLE 7-2 EVIDENCE-BASED CLASSIFICATION SCHEMES FOR CONCUSSION
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||
days after the concussion. In the hours to weeks after injury, damage
may be seen in both the microtubule and neurofilament structure.
Structural changes may occur, such as focal axonal swelling and axonal
bulbs. This swelling is also referred to as a “retraction bulb” because
the axonal ending appears severed from its distal segment and is
characteristic of diffuse axonal injury.
release of oxygen free radicals. Stimulation of cyclooxygenase,
monoamine oxidase, and nitric oxide synthase can result in the
production of these oxygen free radicals, which can cause cell membrane
damage through lipid peroxidation and result in release of arachidonic
acid. Production of leukotrienes and thromboxane B2 from the
arachidonic acid cascade has been shown to cause neurodegeneration and
result in poor outcomes in experimental models. Animal studies have
used ibuprofen and indomethacin, inhibitors of cyclooxygenase, to limit
the arachidonic acid cascade. These compounds have been shown to
improve cerebral metabolism and reduce neurologic dysfunction in mice
after brain injury.
concussion, also referred to as minor traumatic brain injury. Several
attempts have been made to classify concussions based on their
severity, with guidelines for return to play. The most commonly used
classifications have three grades, with a type 1 described as mild,
type 2 as moderate, and type 3 as severe. The classification schemes
vary somewhat, but are all based on clinical presentation of the
athlete and duration of symptoms. Table 7-2 provides a comparison of two commonly used classifications.
-
The athlete who has sustained a severe
head injury is usually easy to identify. Typically, there has been a
significant impact or acceleration/deceleration to the head, and the
athlete may be rendered unconscious. -
The challenge lies in identifying the athletes who have sustained less severe head injuries, such as a grade 1 concussion.
-
The impact to the head may not seem out of the ordinary or may not have been seen at all by the team physician or trainer.
-
Athletes often minimize symptoms in an
effort to remain in play but may use terms such as “having my bell
rung” or feeling “in a fog” (Box 7-1). -
Classic acute symptoms include headache, dizziness, nausea, and difficulty concentrating.
-
Athletes may seem to have a vacant stare or ask repetitive questions and express emotional lability.
-
It is not unusual for the athlete to develop a sense of euphoria after such an injury.
-
-
The initial approach to an unconscious
athlete is similar to that for any traumatized patient, and the “ABCs”
(Airway, Breathing, and Circulation) should be followed. -
It is important to assume the athlete
also sustained a neck injury until proven otherwise, and spine
precautions should be followed. -
The facemask on football helmets can be
removed, but usually the rest of the helmet is left on and used to help
stabilize the neck. -
For less-severe injuries, a detailed sideline examination can be performed.
-
A neurologic examination should include
an assessment of level of consciousness, speech, balance, memory
(antegrade and retrograde and to event), and orientation to person,
place, and time.
-
-
Athletes should not return to play until
symptoms have resolved both at rest and with exertion, such as running
a sideline sprint.-
One recent study found that some high
school athletes, whose symptoms were thought to have cleared quickly
postconcussion, scored below their baseline on neuropsychologic testing
at 48 hours, suggesting that perhaps no athlete with a documented
concussion should return to play the same day.
-
-
The use of neuropsychologic testing has received increasing attention.
-
Given the wide variation among
individuals on these tests, it is necessary to have a preseason
baseline evaluation for comparison after a traumatic brain injury. -
A decline in neuropsychologic test
results has been shown to correlate with severity of postconcussive
symptoms at 1-week postinjury.
-
-
Athletes who have sustained a prolonged
loss of consciousness, or exhibit neurologic deficits, should be
triaged to a medical center for further evaluation. -
Abbreviated neurologic examinations, such
as the Glasgow Coma Scale, are useful in predicting outcome after a
severe head injury (Table 7-3). -
On arrival at a medical center, a full
neurologic examination should be performed, including assessment of
mental status, speech, memory, motor and sensory function, cranial
nerve function, and reflexes (normal and abnormal). -
A computerized tomography scan is helpful in the evaluation of potential intracranial hemorrhage and skull fracture.
-
Magnetic resonance imaging will identify more diffuse injury, such as diffuse axonal shear.
-
Because the subject may not lend
him/herself to prospective, randomized studies, the guidelines for
return to play after a traumatic brain injury are based largely on
retrospective analysis and judgment. -
A primary goal is to avoid secondary
injury, such as a more severe concussion, or worse yet a second impact
syndrome. It is for this reason that athletes who remain symptomatic
after even a grade 1 concussion should not return to play. -
Another goal is prevent the long-term
effects of multiple minor traumatic brain injuries that can lead to
permanent changes, such as the classic description of “dementia
pugilistica” seen in boxers. It is with these aims in mind that the
guidelines in Table 7-4 were developed. -
Factors other than the concussion severity must be weighed in the return-to-play decision.
-
The athlete’s concussion history: the
total number, time between injuries, and severity of the blow causing
the concussion are all important factors. -
When making the return-to-play decision,
one should consider all pieces of the concussion puzzle and, when in
doubt, err on the side of caution: “If in doubt, sit them out.”
-
-
A relatively recent finding is that
athletes who possess the apolipoprotein E4 allele may be at increased
risk after minor traumatic brain injuries.-
This allele is already well known to
correlate with the incidence of Alzheimer’s disease. There is
increasing evidence that patients who have the apolipoprotein E4 allele
have a worse outcome after head injury and may be predisposed to
earlier-onset of dementia after repetitive concussions. -
Knowing an athlete has this allele may factor into the retirement decision after head injury.
-
|
TABLE 7-3 GLASGOW COMA SCALE
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
-
The first step in medical treatment is making an accurate diagnosis.
-
Intracranial hematomas may require prompt craniotomy and removal, but their treatment is beyond the scope of this chapter.
-
On the field, treatment of athletic head
injuries begins with preparation, including having appropriate
personnel and equipment available.-
For the unconscious athlete, full spine precautions should be followed, including use of a spine board and cervical collar.
-
Maintaining an adequate airway is of primary concern.
-
The facemask should be removed and, if there is respiratory compromise, on-the-field intubation may be required.
-
Continuous blood pressure monitoring is performed, and cardiopulmonary resuscitative equipment should be available if needed.
-
The shoulder pads should be loosened in the front to allow for chest compressions and defibrillation.
-
For patients in whom a spine injury is
suspected, the Inter-Association Task Force for Appropriate Care of the
Spine-Injured Athlete has outlined four instances in which the athletic
helmet and chin strap should be removed (Box 7-2). -
The awake athlete for whom cervical spine injury has been ruled out can be helped to a sitting position.
-
If stable in the sitting position, the athlete may be helped off the field for more detailed examination.
-
-
The primary focus is preventing a second
impact that could have more severe consequences. For this reason, the
athlete should not return to competition until asymptomatic, both at
rest and with exertion.
|
TABLE 7-4 GUIDELINES FOR RETURN TO PLAY AFTER CONCUSSION
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
If the helmet and chin strap do not hold the head securely, such that immobilization of the helmet fails to immobilize the head
-
If the design of the helmet prevents adequate airway management even after removal of the facemask
-
If the facemask cannot be removed in a reasonable amount of time
-
If the helmet prevents immobilization for transportation in an appropriate position
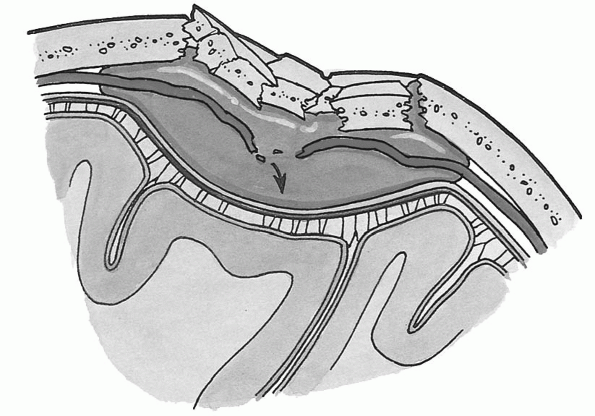
expanding intracranial hematomas. Although subdural is the most common
intracranial hematoma resulting in death after athletic head injury,
the epidural hematoma can be a rapidly fatal lesion without immediate
surgical treatment. Epidural hematoma classically results from injury
to the middle meningeal artery (Fig. 7-2),
whereas a subdural hematoma occurs after disruption of the venous
connections between the dura and the brain. The patient with an
epidural hematoma may sustain an initial loss of consciousness,
followed by an awake and more lucent period, and then quickly develop
loss of mental status and lapse into coma.
well as to try to minimize the cumulative effects that multiple
concussions can cause. Boxing is perhaps most recognized for this, with
fighters having been described as permanently “punch drunk” or
suffering from “dementia pugilistica.” The cumulative effects of minor
traumatic head injuries are becoming better understood in many other
sports as well. Athletes who have sustained prior concussions appear
more prone to future head injury, often with less force required to
cause impairment. In one prospective study of high school football
players, those players who had sustained three prior concussions were
9.3 times more likely to demonstrate on-field signs (such as loss of
consciousness, anterograde amnesia, and confusion) with a concussion,
compared with players sustaining their first concussion.
 |
|
Figure 7-2
Extradural or epidural hemorrhage between the endosteal layer of the dura and the calvaria may follow a blow to the head. Typically, a brief concussion results, followed by a lucid interval of some hours. This is followed by drowsiness and coma. Most bleeding from the torn meningeal arteries results in an extradural or epidural hematoma—a slow, localized accumulation of blood. As the blood mass increases, compression of the brain occurs, necessitating evacuation of the blood and occlusion of the bleeding vessels. (From Moore KL, Agur A. Essential Clinical Anatomy, 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 2002.) |
between high school and college age athletes. In one prospective study,
high school athletes with concussion showed prolonged memory
dysfunction, compared with college athletes with concussion. By three
days postconcussion, the college athletes scored similar to
aged-matched controls on neuropsychological testing. At seven days
postconcussion, the high school athletes still scored below agematched
controls. The exact cause for this age difference is not fully
understood. Children have shown a more diffuse and prolonged cerebral
swelling after traumatic brain injury, compared with adults. It is
hypothesized that the immature brain is more sensitive to excitotoxic
brain injury and may show prolonged metabolic dysautoregulation.
return to play but is clearly open to individual variation and clinical
judgment. Duration of posttraumatic amnesia is one factor in the Cantu
scale of concussions. In one study, the athletes who self-reported
memory problems at 24 hours postconcussion were an indicator of the
severity of the concussion. Athletes who reported memory problems on
followup examination in general had longer duration of symptoms, scored
worse on neurocognitive tests, and had more overall symptoms. All
postconcussion signs and symptoms are important, as is their duration.
Thus, grading of a concussion should ideally await resolution of
symptoms.
is prevention. The increased attention on head injuries in sports has
made athletes, trainers, physicians, and fans more aware of the
potential dangers of brain injury in sports. Football was one of the
first sports to focus on prevention of head and neck injury, as
evidenced by the rule change in 1976 prohibiting initial contact with
the head (“spear tackling”). The number of fatalities as a result of
head injuries in football has declined from a high of 162 during the
10-year span from 1965 through 1974 to a low of 32 during the 10 years
from 1985 through 1994.
means of rule changes, improved protective equipment, and better data
collection to analyze outcomes. The NHL began data collection on head
injury when it instituted its concussion program in 1997. Improved
equipment, such as the Bull Tough helmet (Bull Tough, San Antonio, TX),
seems to help decrease the incidence of head injury in professional and
amateur bull riders (Fig. 7-3). Equally
important is the increasing realization by athletes that returning to
competition while symptomatic from a concussion could lead to
significant worsening of their symptoms and even second impact syndrome.
with football resulting in the highest overall number per year in the
United States. What may seem to be a minor injury, such as a grade 1
concussion, can cause metabolic and potentially structural changes in
the brain, thus making it more susceptible to further insult.
Appropriate identification and on-the-field management of head-injured
athletes can limit further injury. There appears to be age- and
gender-related differences in the rate and severity of head injury in
athletics. Through increased data collection and analysis,
rule changes, education, and equipment development, hopefully, the incidence of head injury in athletics will decline.
 |
|
Figure 7-3 Bull Tough headgear. (Courtesy of www.bulltough.com.)
|
MA, Archer P. Survey analysis to assess the effectiveness of the Bull
Tough helmet in preventing head injuries in bull riders: a pilot study.
Clin J Sports Med 2002;12:360-366.
MW, Lovell MR, Iverson GL, et al. Cumulative effects of concussion in
high school athletes. Neurosurgery 2003;51: 1175-1179.
RJ, Cantu RC. Return to play following sports-related mild traumatic
brain injury: the role of neuropsychology. Appl Neuropsychol
2003;10:48-55.
M, Collins MW, Lovell MR, et al. Does age play a role in recovery from
sports-related concussion? A comparison of high school and collegiate
athletes. J Pediatr 2003;142:546-553.
G, Schaadt G, McAllister DR. On-the-field evaluation of an athlete with
a head or neck injury. Clin Sports Med 2003;22: 445-465.
CK, Schatz P. Current issues in the identification, assessment, and
management of concussions in sports-related injuries. Appl Neuropsychol
2003;10:4-11.
RC. Head and neck injuries in football: mechanisms, treatment, and
prevention. Baltimore: Williams & Wilkins, 1973.
