Elbow Injuries
sustained by athletes, fractures still occur and must be treated
appropriately to allow the athlete to return to sport. Given the
current explosion of extreme sports, all types of fractures are now
being seen in the athletic population. The ultimate goal for the
treating physician is to identify the fracture and follow through with
proper care. Management of both the fracture and the soft-tissue
envelope is critical in the final outcome for injuries about the elbow.
texts hold true for the athlete with an elbow fracture. In general, all
athletes who are skeletally mature (closed physes—females aged 14 years
or older, males aged 15 years or older) can be treated with standard
rigid fixation. Rigid fixation supports osseous healing while allowing
for early passive and active assisted range of motion, which will
influence the overall outcome for athletes, especially throwing
athletes.
algorithms established in fracture texts, but rather to augment this
treatment by focusing on the athletic elbow.
the ulnohumeral and the radiocapitellar joints. The ulnohumeral
provides flexion and extension, while the radiocapitellar provides
supination and pronation. There also exists a third joint, between the
ulna and radius, which allows the radius to rotate around the ulna with
pronation and supination. Activities of daily living require a
flexion-extension arc of 30 to 130 degrees and 50 degrees of supination
and pronation. Anteroposterior (AP) stability of the elbow relies
heavily on the constrained ulnohumeral joint for static control.
Dynamic control is provided by the brachialis and biceps anteriorly and
the triceps posteriorly. The articular surfaces, as well as the radial
and ulnar ligamentous structures, also lend AP support. Valgus
stressors are resisted primarily through a combination the anterior
portion of the medial collateral ligament (MCL), the radial head, and
the anterior capsule. Varus stressors are primarily resisted by the
combination of the anconeus muscle and the lateral collateral ligament.
is the primary articular contact for the distal humerus. This articular
surface extends from the tip of the olecranon to the coronoid with one
significant interruption, a “bare area” that exists approximately
halfway between the tip and the
coronoid.
Along with the coronoid process, it makes up the greater sigmoid notch.
When in extension, the olecranon sits within the olecranon fossa of the
distal humerus and confers bony stability for the elbow. The olecranon
articulates with the trochlea of the humerus throughout the elbow arc
of motion. As the elbow moves into flexion, the bony stability
decreases, and the soft-tissue envelope of the elbow becomes the
primary dynamic and static stabilizing force for the elbow. The
olecranon serves as the insertion point for the triceps brachii and
anconeus muscles and the origin for ulnar aspect of the flexor carpi
ulnaris muscle.
|
TABLE 22-1 CLASSIFICATION OF OLECRANON FRACTURES
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||
blow to the olecranon or the indirect result of falling on an out
stretched arm. If the force is significant enough, the proximal aspect
of the olecranon will be displaced proximally with the triceps tendon.
The remainder of the ulna can move anteriorly with the radius,
resulting in a fracture dislocation of the elbow.
olecranon, none of which is universally accepted by orthopaedists. The
simplest one, created by Colton (1973), focuses on fracture displacement and type (Table 22-1). Schatzker’s (1987)
classification is relatively simple and may be the most useful to the
orthopaedist because it allows one to assess different treatment
options (Table 22-2 and Fig. 22-1).
Whichever scheme is chosen, the important aspect of the assessment is
fracture stability and overall condition of the articular surface.
|
TABLE 22-2 CLASSIFICATION OF OLECRANON FRACTURES
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||
 |
|
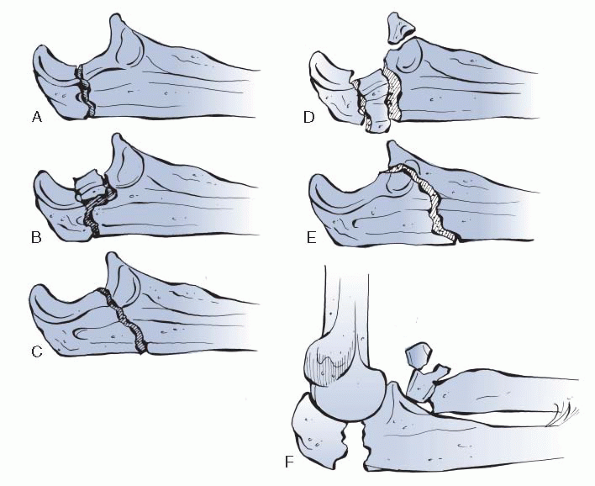
Figure 22-1 Schatzker classification of olecranon fractures. A: Transverse. B: Transverse impacted. C: Oblique. D: Comminuted. E: Oblique distal. F:
Fracture dislocation. (From Court-Brown C, McQueen M, Tornetta P III. Orthopaedic Surgery Essentials: Trauma. Philadelphia, Lippincott Williams & Wilkins, 2006.) |
-
Fractures of the olecranon tend to have a concomitant effusion due to intra-articular extension.
-
There can be a large amount of soft-tissue edema, which may make palpation of a step-off difficult.
-
When assessing the function of the elbow, the ability to actively extend the elbow is the most important test to conduct.
-
Failure of the extension mechanism usually results in the decision for surgical repair.
-
-
As with any fracture, a careful neuralgic examination should be performed, as well as a thorough inspection of the skin.
-
AP and true lateral views are needed.
-
Oblique lateral views can obscure the true extent of the intra-articular fracture.
-
Most olecranon fractures do not need more than clinical and radiographic workups.
-
Nondisplaced fractures can be treated in a long arm cast flexed between 45 and 90 degrees for 3 weeks.
-
This period of immobilization is then
followed by a protected range of motion (0 to 90 degrees) in a hinged
elbow brace until the fracture has united. -
Bony union takes approximately 6 to 8 weeks.
-
Once bony union is achieved, physical therapy should focus on obtaining full flexion.
-
For older patients, it is advisable to start range of motion before 3 weeks because they are more prone to stiffness.
-
These patients can be protected in the hinged brace or a sling to encourage earlier motion.
-
-
There are four established goals for operative fixation of displaced fractures:
-
Maintain power of the extensor mechanism
-
Avoid incongruity of the articular surface
-
Restore stability of the elbow
-
Prevent stiffness of the joint
-
-
How the surgeon achieves these goal depends on the fracture pattern and the surgeon’s experience.
-
Avulsion fractures can be treated with Kirschner (K) wire and tension band fixation.
-
The goal of tension band fixation is to
convert the tensile forces found along the dorsum of the olecranon into
dynamic compressive force across the articular surface. -
The approach for this and most other olecranon fractures is posterior, with the incision slightly lateral to the olecranon.
-
This helps to avoid a painful scar over the tip of the olecranon and keeps the approach away from the ulnar nerve.
-
The ulnar nerve does not need to be isolated or transposed, but its location should be palpated and noted throughout surgery.
-
-
Once through the soft tissue, the avulsed olecranon is usually readily identifiable.
-
The hematoma is evacuated and the joint copiously irrigated.
-
A trial reduction is conducted and held with reduction clamps.
-
K-wires are then passed antegrade through the avulsed tip and into the shaft of the olecranon.
-
The target point is the volar cortex just distal to the coronoid.
-
The position of the K-wires is checked with fluoroscopy.
-
-
Once satisfied with the reduction, the
drill hole in the ulna shaft is made for the tension band. It is placed
in the dorsal half of the shaft of the ulna distal to the fracture site. -
Next, 16- or 18-gauge wire is then passed
through the drill hole and passed dorsally over the ulna. A loop is
created on the radial side. -
A 14-gauge angiocatheter is passed between the triceps and tip of the olecranon from ulnar to radial.
-
This allows safe passage of the wire and protects the ulnar nerve.
-
-
Once passed, the ends are twisted
together, and tension is placed on the wire by tightening the loop and
the twisted ends simultaneously, which will result in increased tension. -
The wire knots are then cut to 3 to 4 mm
after being bent distally so that they lie along the radial and ulnar
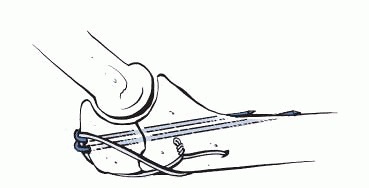
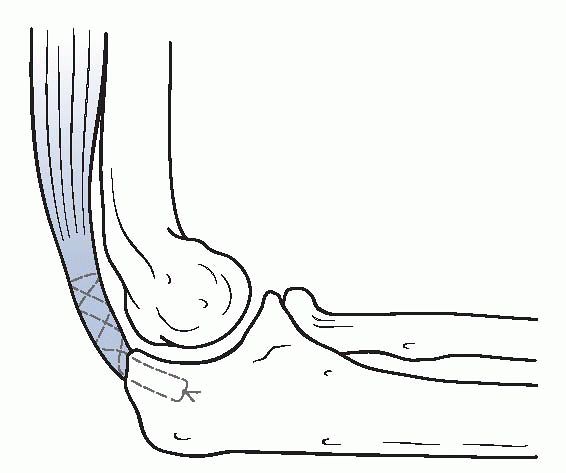
sides of the olecranon (Fig. 22-2). -
Once completed, the fixation is tested by bringing the elbow through a range of motion.
-
Final position of the hardware is checked with plain films.
-
The wound is copiously irrigated and then closed.
-
The arm is placed in a posterior splint.
 |
|
Figure 22-2
Example of tension band wiring of elbow. (From Court-Brown C, McQueen M, Tornetta P III. Orthopaedic Surgery Essentials: Trauma. Philadelphia, Lippincott Williams & Wilkins, 2006.) |
-
These fractures are treated in the same manner as the avulsion fractures.
-
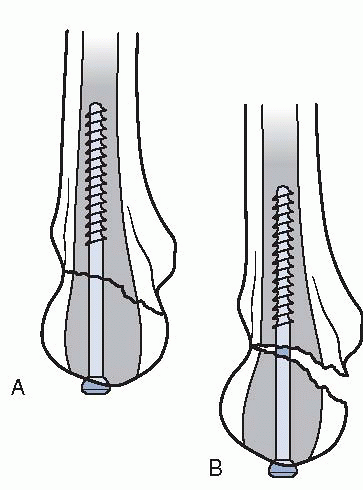
A 6.5 cancellous screw with a washer can be used in place of the K-wires (Fig. 22-3).
-
After the reduction, the triceps tendon is split in line with its fibers.
-
The olecranon and ulnar shaft are then
drilled and tapped for a 6.5 (4.5 can be used for a small ulna)
partially threaded cancellous screw. -
The cancellous screw needs to engage the cortex of the ulna shaft, usually requiring an 80 to 120 mm screw.
-
The tension is set and the screw tightened.
-
Care must be taken not to overseat the screw because this can translate the fracture.
-
-
Proponents of this technique cite
application of static and dynamic compression, security of the screw,
and strength of the construct as reasons to use the screw. -
Opponents believe that prominent hardware and potential overreduction and translation are reasons to avoid screw fixation.
 |
|
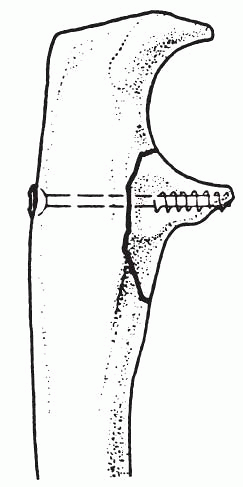
Figure 22-3 A: Proper placement of an intramedullary screw. B:
Placement of the screw slightly off the intramedullary axis results in fracture malreduction. (After Hak D, Golladay G. Olecranon fractures: treatment options. J Am Acad Orthop Surg 2000;8: 266-275. © 2000 American Academy of Orthopaedic Surgeons.) |
-
Fractures with minimal comminution are
amenable to fixation with K-wires and tension band, but great care must
be taken to avoid compressing the comminution and disrupting the arc of
motion between the trochlea and olecranon. -
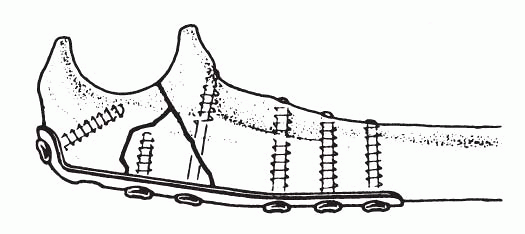
In cases with extensive comminution, it is best to treat the fracture with plates and screws.
-
These fractures usually require bone graft to support the articular surface.
-
Reconstruction plates, low-contact
dynamic compression (LCDC) plates, or preformed olecranon plates can be
helpful in dealing with these fractures (Fig. 22-4).
-
-
Once initial reduction is achieved, K-wires are used to hold the fragments in place.
-
Bone graft is added as necessary to support the articular surface.
-
The plates are then applied using AO technique.
-
Once again, care must be taken to avoid placing too much compression across the fracture.
-
-
These fractures are amenable to fixation with a lag screw and plate.
-
The lag screw is placed through a plate, from the tip of the olecranon to a point just distal to the coronoid process.
-
Screws are then placed, using AO technique, into the proximal aspect of the prebent plate.
-
The distal screws are then placed using AO compression techniques.
-
These fractures are fixed as noted
previously, but great care must be taken to avoid excess compression
when the lag screw and plate are being placed. -
In some instances, the lag screw or the compression through the plate may not be used to protect a severely comminuted fracture.
 |
|
Figure 22-4 Plate fixation of the comminuted fracture.
|
 |
|
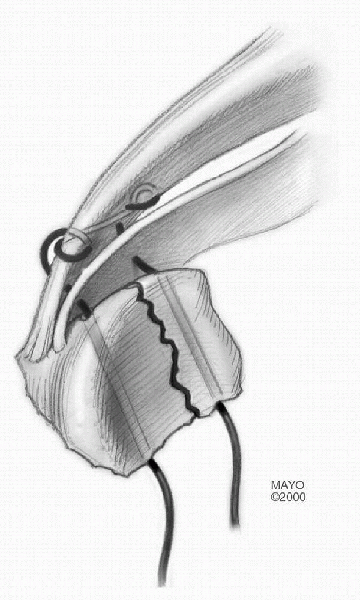
Figure 22-5
When excision and triceps advancement are performed, the triceps should be attached adjacent to the articular surface. (After Cabanela ME, Morrey BF. Fractures of the proximal ulna and olecranon. In: Morrey BF, ed. The Elbow and Its Disorders, 2nd ed. Philadelphia: WB Saunders, 1993:416. Modified with permission from the Mayo Foundation for Medical Education and Research. All rights reserved.) |
-
In some cases, adequate reduction is not achievable.
-
It is then advisable to excise the proximal end of the olecranon and repair the extensor mechanism.
-
When conducted, the triceps should be reattached adjacent to the articular surface (Fig. 22-5).
-
As described previously, all of these surgical cases will be placed in a long posterior splint after surgery.
-
After an early rest period (1 to 7 days), early motion is begun.
-
The extent and start time for early motion will depend on the fracture type and fixation used.
-
Fractures treated with tension banding are usually amenable to movement by day 7.
-
Hinged elbow braces or cast braces help to protect the repair.
-
-
More complicated fractures, those fixed
with neutralization plates, or patients who are unreliable should be
protected in a cast for 2 to 3 weeks. -
This period of immobilization is followed by passive and active assisted range of motion, as well as protection in a brace.
-
Once the patient demonstrates radiographic and clinical union, active range of motion is started.
-
About 76% to 98% of patients achieve good to excellent results.
-
Most experience a loss of extension (~10
degrees), flexion (~5 degrees), some pronation and supination (~5
degrees each), and loss of strength when compared with the
contralateral side. -
Poorer results have occurred with elderly patients, delayed surgery, malreduction, and extensive comminution.
-
The most significant complications occur due to painful hardware.
-
20% to 80% of patients will complain of hardware issues
-
30% to 70% of patients will require hardware removal
-
1% to 5% of all hardware will break
-
-
Other complications include infection (0% to 6%), ulnar neuritis (2% to 12%), and heterotopic ossification (2% to 13%).
of the radius. It is involved in both the flexion/extension and
pronation/supination arcs of motion. It forms articular joints with
both the capitellum, as well as the ulna via the sigmoid notch. The
highest level of force is exerted across the radiocapitellar joint at
full extension and across the radioulnar joint during pronation. The
radial head also provides stability to the elbow when a valgus force is
exerted.
of the radius, usually after a fall onto an outstretched arm. Fractures
also occur during an elbow dislocation or a direct blow to the
posterior aspect of a flexed elbow.
-
Most patients complain of pain along the
lateral side of the elbow with motion along the flexion/extension plane
or pronation/supination plane. -
With more severe injuries, there will be a mechanical block to motion, although pain with motion may mimic a mechanical block.
-
With higher-grade injuries, there is often gross edema around the elbow.
-
With type I injuries, pain may be the only pertinent physical finding.
|
TABLE 22-3 CLASSIFICATION OF RADIAL HEAD FRACTURES
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||
-
As with any suspected fracture, plain
films are the first line of a diagnostic workup. AP, lateral, and
oblique views of the elbow are obtained to diagnose the fracture. -
A radiocapitellar view, achieved by angling the x-ray tube 45 degrees cephalad with the forearm in neutral, may also be helpful.
-
If the patient complains of wrist or forearm pain, then films of the wrist and forearm should also be obtained.
-
If the fracture appears amenable to a
surgical procedure, it is often helpful to obtain a computed tomography
(CT) scan of the elbow as well.
-
Type I fractures are treated without surgical intervention.
-
The patient is placed in a sling for several days to recover from the acute trauma.
-
Aspirating the hematoma and injecting a local anesthetic can provide significant analgesia (Fig. 22-6).
-
Most patients will recover functional range of motion within 2 to 3 months.
-
Some may have a residual loss of extension, pain, or stiffness, even with a nondisplaced fracture.
 |
|
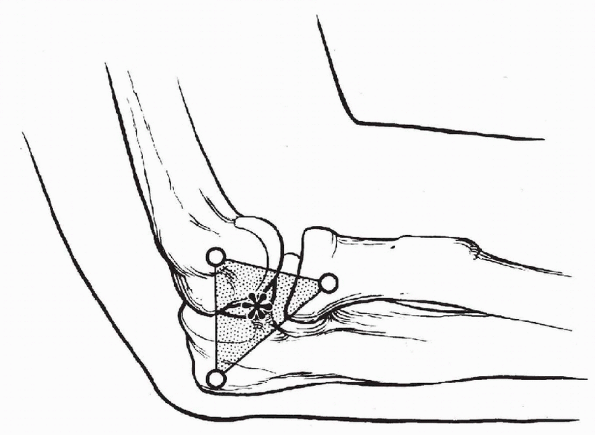
Figure 22-6
The landmarks for aspiration of the elbow joint are the radial head, lateral epicondyle, and tip of the olecranon. A needle inserted into the center of the triangle (asterisk) penetrates only the anconeus muscle and capsule before entering the joint. (From Mezera K, Hotchkiss RN. Fractures and dislocations of the elbow. In: Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2002:943.) |
-
All type II fractures should be
considered for open reduction with internal fixation (ORIF), especially
when the patient is less than 55 years old. -
Fractures associated with instability should be fixed at any age.
-
The best indication for fixation are type
II fractures that consists of <30% of the radial head or a “slice”
fracture that is displaced more than 3 mm. -
Some type II fractures will not have a mechanical block and may be treated similarly to type I.
-
Surgery to fix a type II radial head fracture is conducted through the classic Kocher approach to the lateral elbow.
-
Once the fracture is identified, the
hematoma is removed and care is taken not to strip any soft-tissue
attachments from the fracture fragments. -
The articular surface is then reconstructed and the reduction held with a 0.425 K-wire.
-
A 2.7 screw is inserted using AO technique.
-
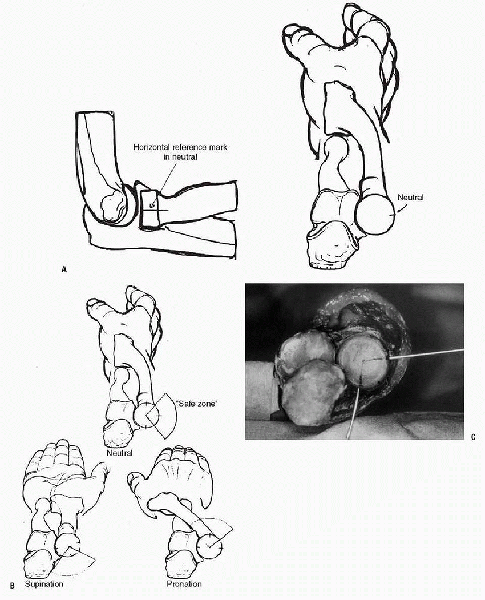
The screw should be placed through the
bare area on the radial head (located on the lateral aspect of the
radial head when the forearm is held in neutral) (Fig. 22-7).
-
-
A second screw should be placed if necessary.
-
On some occasions, a small T-plate can be used if the fracture fragment is large enough.
-
When associated with an Essex-Lopresti lesion, ORIF of the radial head fracture is especially helpful.
-
-
In the presence of severe comminution of the radial head, the only option is often excision.
-
When considering excision of the radial head, it is imperative to be sure that there is not a concomitant Essex-Lopresti lesion.
-
Without the radial head present, the radius will migrate proximally due to the incompetent interosseous ligament.
-
Because of this phenomenon, the space once occupied by the radial head must be accounted for.
-
-
Some success has been reported with delayed excision of the radial head, as well as with silicone implants.
-
Silicone implants have caused soft-tissue reaction and have other problems associated with them.
-
Titanium implants allow for maintenance
of the radial length when the radial head needs to be excised; however,
there has been some documented failure even with these prostheses. -
Indications for use of a metallic radial head are given in Box 22-1.
-
Because of the questionable outcomes with
prosthetic replacement, every effort should be made to save the radial
head, especially in the young athlete.
-
-
For patients who undergo ORIF of the
radial head, a posterior splint is used for 3 to 4 days and a passive
motion machine for 2 to 3 weeks. -
At 3 weeks, the patient is allowed to start active assisted and gentle active range of motion.
-
This range of motion should be along the extension and supination planes.
-
Flexion and pronation are avoided.
-
At 6 weeks, with evidence of healing, physical therapy is begun in all planes.
-
Complete healing usually occurs by 3 months, and motion is usually achieved by 12 months.
-
For patients who undergo a radial head replacement, motion is allowed on postoperative day 2.
-
Active assisted and passive range of
motion are initiated at first, followed by active range of motion.
Similar postoperative management is used for pure excisions of the
radial head.
-
Early complications include forearm
motion loss, poor fixation, loss of fixation, and injury to the
posterior interosseous nerve. -
Early fixation failure should be treated with delayed radial head excision (3 to 4 weeks later).
-
Late complications include nonunion, painful hardware, and elbow stiffness.
-
The plate, if used, may be removed safely after 6 months.
-
Heterotopic bone may form, especially in cases associated with head trauma and other associated elbow injuries.
-
The heterotopic bone can be dealt with once it has matured.
-
 |
|
Figure 22-7 The safe zone for hardware placement. A: A horizontal reference mark is first made with the forearm in the neutral position. B:
Two more horizontal marks are made in full pronation and full supination. By dividing each of these sectors in half, the safe zone is identified. C: An anatomical specimen showing the safe zone with the forearm in full supination. (After Hotchkiss RN. Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg 1997;5:1-10. © 1997 American Academy of Orthopaedic Surgeons.) |
-
Indications
-
Acute trauma
-
Type III radial head fracture associated with:
-
Elbow dislocation or Essex-Lopresti injury
-
Coronoid type II/III fx or olecranon type III fracture
-
After radial head excision with continued elbow instability
-
-
-
Reconstruction
-
With interposition arthroplasty if radial head removed and evidence of continued instability
-
Stabilization of the forearm and elbow after an Essex-Lopresti injury
-
Failed silicone radial head replacement if needed for stability
-
-
-
Contraindications
-
Acute trauma
-
Older patient (>65) with type III fracture without elbow instability or other associated injury
-
Open fracture of the radial head, olecranon, or open dislocation with a high risk of infection
-
Mason type I or II
-
Mason type III without elbow or forearm instability
-
-
Reconstruction
-
Poor radiocapitellar alignment
-
Proximal radial shaft fractures with comminution into the head
-
Disease or injury to the capitellum
-
-
-
Absolute Contraindications
-
Prior sepsis or question of wound contamination
-
Known sensitivity to makeup of prosthesis
-
Skeletal immaturity
-
Insufficient tissue to provide stability
-
Resected radius is malaligned with the capitellum
-
Morrey B, ed. The Elbow, 2nd ed. Philadelphia: Lippincot Williams &
Wilkins, 2002.)
become an important factor in determining and treating injuries to the
elbow. In general, at least 50% of the coronoid is required to maintain
elbow stability. Usually, overall elbow stability must take into
account ligamentous stability, radial head involvement, as well as the
coronoid. Injury to all three of these components, known as the
“terrible triad,” will be discussed later in the chapter. This section
will focus on the lower-grade injuries to the elbow that involve a
coronoid fracture.
|
TABLE 22-4 CLASSIFICATION OF CORONOID FRACTURES
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||
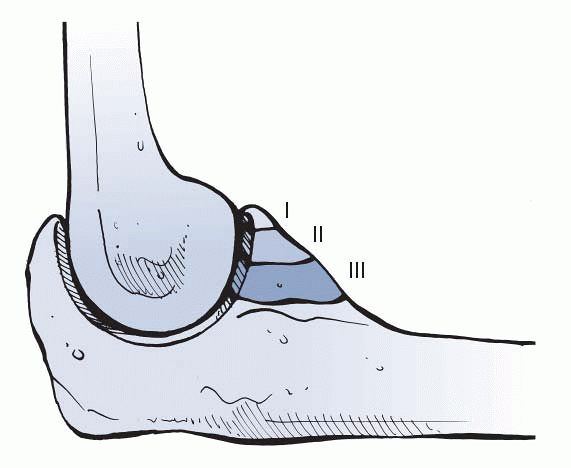
and extended elbow or direct impact of the coronoid against the
trochlea. The most widely accepted classification concerning the
coronoid is given in Table 22-4 and Figure 22-8.
-
Initial workup consists of x-rays. In
most cases of coronoid injuries, there will be pre- and postreduction
film (due to the elbow dislocation). -
After the reduction, it is important to
document the stability of the elbow, as well as the arc of motion in
which the elbow is stable. -
For patients in whom a more severe injury
is suspected, a magnetic resonance imaging (MRI) is usually helpful in
determining the extent of the ligamentous damage.
 |
|
Figure 22-8
Regan-Morrey classification of coronoid fractures. (From Court-Brown C, McQueen M, Tornetta P III. Orthopaedic Surgery Essentials: Trauma. Philadelphia: Lippincott Williams & Wilkins, 2006.) |
-
Type I injuries essential represent an elbow dislocation.
-
Once the ulnohumeral joint has been reduced, this fracture does not need to be addressed acutely.
-
Occasionally, the small avulsion can
cause anterior elbow discomfort or represent a loose body in the elbow
and can be dealt with arthroscopically.
-
This type of fracture can be approached from the posterior side.
-
The patient is placed supine and the operative arm is draped across the chest and over a bolster.
-
A posterior incision is made just medial to the tip of the olecranon.
-
This allows access to the fracture and ulnar nerve.
-
-
Once the subcutaneous flap is made, the ulnar nerve is identified.
-
The nerve can be left in place or released and transposed anteriorly.
-
If transposed, the intermuscular septum is released.
-
-
The soft tissues are elevated off the anterior septum, and the brachialis is elevated off the anterior surface of the humerus.
-
The pronator is elevated, but the flexor carpi ulnaris (FCU) is left for closure.
-
The MCL is identified and protected.
-
The muscle flap is elevated off the capsule and the brachialis is swept radially, exposing the capsule.
-
The capsule is split longitudinally, exposing the anterior joint and the coronoid fracture.
-
The fracture is reduced with bone-holding forceps and the fragment held with a 0.045 or 0.062 K-wire.
-
It is then stabilized with a 2.7 screw (Fig. 22-9).
-
-
In some cases, the fracture involves a more extensive medial piece of the ulna.
-
Screw fixation alone is not adequate and a contoured buttress plate should be added.
-
-
In cases in which the fracture fragments
are very small or comminuted, suture fixation may be the only available
means for fixation (Fig. 22-10).-
Drill holes are made in the fragments if
possible, and no. 2 or no. 5 sutures are passed through the drill holes
and the capsule. -
If possible, the insertion of the brachialis should be incorporated into the repair.
-
Retrograde drill holes are then made from
the subcutaneous border of the ulna to the base of the fracture near
the articular surface. -
The sutures are passed through and tied over the dorsal aspect of the ulna.
-
During the reduction, care should be taken to align the fragments as best as possible close to the joint surface.
-
-
Type II fractures with intact radial head and a grossly unstable ulnohumeral joint when flexed less than 50 to 60 degrees
-
Type II coronoid fractures associated with a radial head fracture and elbow dislocation (terrible triad)
-
Isolated anteromedial coronoid fracture
-
Patients who are more than 5 to 6 days postinjury with a reduced ulnohumeral joint (to avoid heterotopic calcification)
coronoid and complex instability of the elbow. In: Morrey BF, ed. The
Elbow. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 2002.)
 |
|
Figure 22-9
Lag screw fixation of the coronoid may be crucial to stability if the fracture is associated with dislocation. (After Heim U, Pfeiffer KM. Internal Fixation of Small Fractures, 3rd ed. Berlin, Springer-Verlag, 1988.) |
 |
|
Figure 22-10
Krachow suture technique. The stitch is used to secure the brachialis muscle, capsule, and fractured fragments. (From Morrey BF, O’Driscoll SW. Fractures of the coronoid and complex instability of the elbow. In: Morrey BF, ed. The Elbow, 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 2002:134.) |
injuries. The mechanism of injury is usually a fall onto an
outstretched arm. The median age for injury is 30 years old, and the
occurrence is spread between sports (40%) and high-energy accidents
(50%). Ninety percent are either posterolateral or straight posterior
and, if present, the most common associated fractures involve the
radial head and coronoid process.
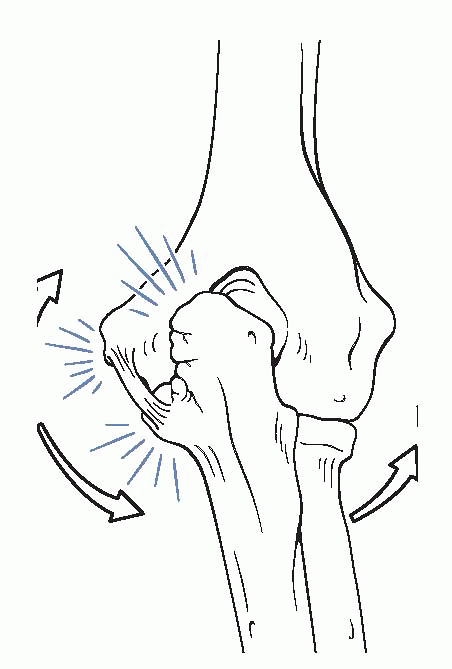
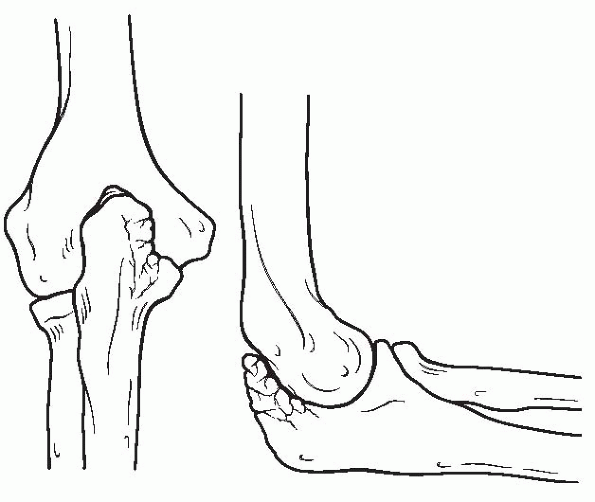
with direction, Morrey (2003) found classifying the dislocation as
perched or complete much more clinically relevant (Fig. 22-11). O’Driscoll et al. (1992)
found a significant difference in stability between a perched and
complete dislocation but could not find much significance between a
complete dislocation that was posterior, posterolateral, or anterior.
When a varus extension force is placed on an elbow, the lateral ulnar
collateral ligament (ULCL) is disrupted as the olecranon rotates and
moves posteriorly out of the fossa. If the force ends at this point,
the elbow is perched but still has some intrinsic stability due to the
intact MCL and the anterior capsule. When the force continues, the
olecranon completely dislocates, tearing the remaining soft-tissue
restraints. This creates a “ring of instability” and results in a much
more unstable elbow. A complete dislocation may also have other
associated injuries with it. Concomitant injury to the brachial artery,
ulnar and median nerves, radial head, and coronoid process have all
been reported.
-
As with other injuries about the elbow, the patient usually presents with pain, edema, and loss of motion.
-
A gross step-off posteriorly may be appreciated with complete dislocation.
-
Along with the elbow examination, a thorough neurovascular examination should be conducted.
-
The ipsilateral shoulder and wrist should
be examined because there is a 10% to 15% chance of an associated
injury to these joints.
-
AP, lateral, and oblique views of the elbow, along with proper films of other suspected sites of injury, should be obtained.
-
Postreduction films are essential.
-
If other fractures are noted after reduction, proper imaging of these injuries should be performed.
-
The first priority in treating an elbow dislocation is reduction.
-
For perched dislocation, the reduction can often be conducted with an intra-articular injection of a local anesthetic.
-
Once the joint has been anesthetized, longitudinal traction is placed on the affected arm at 45 degrees.
-
Pressure is then applied to the olecranon to guide it back into the fossa.
-
-
For a complete dislocation, the same
maneuver is used, but it is usually necessary to use either full-blown
conscious sedation or general anesthesia. -
Once reduced, x-ray confirmation needs to be made by obtaining an AP and true lateral views of the elbow.
-
These films need to be scrutinized for widening of the joint and possible fractures.
-
-
If adequately reduced, the next step is to determine the stable range of motion.
-
The elbow is then splinted in the appropriate position to confer stability.P.295
-
For perched dislocations, the elbow is splinted at 90 degrees for 2 to 3 days and then range of motion is started.
-
For complete dislocations, the elbow is protected for 5 to 10 days before starting therapy.
-
-
Immobilization for greater than 3 weeks results in loss of motion.
-
X-rays should be checked at least at weeks 1 and 3.
-
Dislocations that were thought to be unstable should be checked more often.
-
-
Perched dislocations usually achieve normal range of motion by 6 to 8 weeks.
-
Complete dislocations usually attain 80% to 90% of their motion by 3 months.
-
Any patient who displays a contracture of 50 degrees or more after 3 weeks should be placed in an extension brace.
-
Strengthening begins in earnest by 8 to 10 weeks.
 |
|
Figure 22-11 A: Complete dislocation. B:
Perched dislocation. (From Court-Brown C, McQueen M, Tornetta P III. Orthopaedic Surgery Essentials: Trauma. Philadelphia: Lippincott Williams & Wilkins, 2006.) |
-
Surgical intervention is reserved for
patients who require an extreme amount of flexion to remain reduced,
who fail to have a congruous reduction, or who have unstable fractures
associated with the dislocation. -
The most common fracture/instability
pattern is the “terrible triad,” which consists of an elbow
dislocation, as well as a radial head and coronoid fracture. -
Once the elbow dislocation is reduced,
the radial head and coronoid fractures need to be addressed as
described previously in this chapter. -
When dealing with these fractures, both the MCL and ULCL should be repaired to achieve the best possible outcome.
-
Multiple studies have looked into the repair of the ULCL, the MCL, and both ligaments.
-
Both ligaments play important roles in
elbow stability, with the MCL providing stabilization of the
ulnohumeral joint and the ULCL stabilizing the radiocapitellar joint. -
In instances of simple elbow dislocations, there is no merit in repairing the ligaments acutely.
-
-
For a completely dislocated elbow that
remains unstable despite the repair of the collateral ligaments, a
hinged external fixator may be the best option.
-
Stiffness and loss of motion are the most common outcomes following reduction and treatment for an elbow dislocation.
-
Most report a loss of up to 30 degrees of extension at 10 weeks and a final loss of 5 to 15 degrees.
-
Associated fractures of the radial head
and coronoid adversely affect this result. On rare occasions, the
primary concern is instability and not stiffness. -
Morrey (2003) reported that
posterolateral rotatory instability was the most common pattern among
his patients and that this diagnosis is not an easy one to make.-
In this instance, the ULCL needs to be reconstructed.
-
-
Many patients report general pain with activity.
-
This is most likely due to the trauma that the cartilage undergoes with the initial dislocation.
-
All complete elbow dislocations may have some osteochondral damage.
-
Patients may also lose up to 15% of their strength and feel that their injured side is inferior to the contralateral elbow.
-
-
Heterotopic ossification (HO) has also been documented after an elbow dislocation.
-
The best prevention of HO is to perform an early and definitive reduction.
-
Delayed treatment or multiple reduction attempts have been linked to the development of HO.
-
To help prevent postsurgical HO,
indomethacin SR 75 mg daily for 3 weeks, or a single postoperative dose
of radiation (700 cGy) can be used. -
When it does occur, it is best to remove the ossification once it has matured.
P.296 -
adolescents, adults can have olecranon stress fractures. The typical
patient is an overhead-throwing athlete with pain during the
acceleration and follow-through phases of throwing. This pain is
usually located directly posterior on the olecranon, although it can
also be found along the lateral border of the olecranon. Unlike
throwers with MCL laxity and pain, these athletes tend to have negative
valgus stress tests and pinpoint pain over the sites described.
-
Although x-rays may show the stress fracture, they are often negative.
-
If a fracture is suspected, MRI is currently the best study to evaluate the bone.
-
Both bone scans and CT have been used in the past, but neither have the same specificity and sensitivity as MRI.
-
MRI is helpful not only with initial diagnosis but also for following the healing of the fracture.
-
In general, MRI results depict poorly defined, patchy areas of low signal intensity continuous with the cortex on T1-weighted images and high signal intensity on STIR images.
-
In one study, all of the irregularity was noted in the posteromedial aspect of the olecranon.
-
-
Treatment for olecranon stress fractures is similar to stress fractures at other sites.
-
Initial treatment is to rest the arm and avoid throwing activities for 6 weeks.
-
Protecting the elbow in a hinged brace set between 20 degrees to full flexion for the first 4 weeks has been suggested.
-
Once the acute pain and discomfort resolves, the patient will begin on a physical therapy regimen.
-
This regimen is similar to that used for throwers with other injuries.
-
It focuses on rehabilitating the shoulder as well as the elbow.
-
If the athlete is able to work through
the program without pain, then a graduated throwing program is
initiated at 8 to 10 weeks.
-
For those athletes who have recurrent pain or who fail rehabilitation, then surgical options can be considered.
-
The treatment of choice is fixation with a 6.5 or 4.5 cannulated screw.
-
The screw can be placed through a small posterior incision at the tip of the olecranon.
-
The triceps is split, and a guidewire is passed antegrade down the shaft of the ulna.
-
The ulna is drilled and tapped, and the screw is placed in the standard fashion.
-
Once the acute surgical pain has resolved, the patient starts regaining range of motion.
-
Once healing is observed, the athlete enters the same program described for nonoperative treatment.
-
Occasionally, the hardware is painful and needs to be removed before the thrower is able to fully recover.
fracture in a juvenile gymnast. The diagnosis was made by
three-dimensional CT reconstruction of the coronoid. Treatment
consisted of withdrawing from athletic participation until the symptoms
resolved. Activities of daily living were allowed and splints were not
used.
athletic and nonathletic population. Due to the superficial nature of
the bursa, it can become quite inflamed, even after a minor injury to
the elbow. It can be either acute or chronic, septic or nonseptic.
-
Symptoms are usually initiated by trauma to the posterior elbow, although a specific history of trauma is not always evident.
-
The amount of swelling can be quite
dramatic and can be limited to a small area, causing an egg-like
appearance over the olecranon.
-
It is usually not painful, although in
the process of flexing the elbow, the patient may feel discomfort due
to stretching of the skin. -
The elbow range of motion is maintained.
-
Differential diagnosis includes tendonitis, arthritic flare, and pseudogout.
-
X-rays are usually done as a matter of course.
-
Soft-tissue swelling is usually evident.
-
There should be no sign of an effusion or fracture.
-
An aspiration can be conducted if the
swelling is so severe that it limits motion or if, in the elderly,
there is a question of pseudogout as the cause.-
In this case, the aspirate should be sent for culture, Gram stain, cell count, and crystals.
-
Bursal fluid should have a low white cell count with 80% monocytes.
-
 |
|
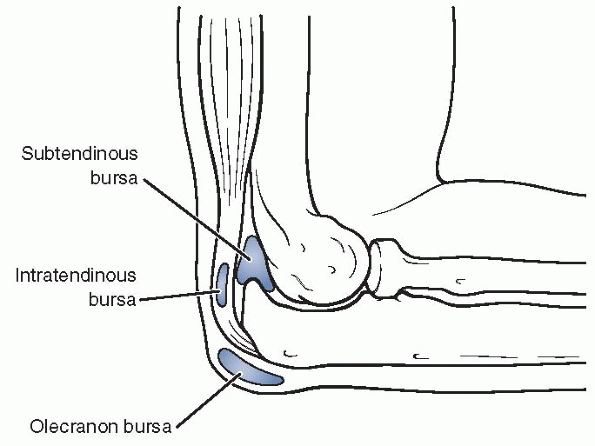
Figure 22-12
Bursae of the elbow joint: the superficial olecranon bursa; the intratendinous bursa, which is found in the substance of the tendon; and the subtendinous bursa, which lies between the tip of the olecranon and the triceps tendon. |
-
After several bouts of bursitis, the bursal lining can become quite thickened.
-
The thickened bursal tissue consists of villi that represent granulation tissue.
-
Early in the course, the chronic bursitis presents as soft, thickened tissue over the olecranon.
-
Eventually, the bursa becomes quite thickened and can contain multiple solid loose bodies.
-
Patients with septic bursitis can present in many ways.
-
Often, the patient will have had several days of insidious pain over the posterior aspect of the elbow.
-
He or she may recall trauma to the site; however, usually the trauma was so minor that they never registered it.
-
There may be a small abrasion over the bursa that served as the entry point for the bacteria.
-
He or she may have a history of fever,
chills, and other signs of a systemic infection, but most of the
symptoms are related to the local infection.
-
-
Cellulitis can travel both up the arm and down the forearm and can be accompanied by edema.
-
The posterior aspect of the elbow is very painful, and range of motion can be limited because of discomfort.
-
Every case of suspected septic bursitis should have an aspiration done.
-
Once again, the fluid should be sent for culture, Gram stain, crystals, and cell count.
-
The most common pathogen is Staphylococcus aureus.
-
-
Most acute bursitis can be treated conservatively.
-
Usually, ice packs and anti-inflammatory medication are enough to relieve the acute symptoms associated with the bursitis.
-
After 24 hours, warm packs can be used to help resorb the bursal fluid.
-
Some patients will need aspiration.
-
The bursal sac does not need to be openly drained, and a drain should not be placed after aspiration.
-
The bursal cells can line the tract of the drain and create a fistula.
-
-
After aspiration, a compressive dressing needs to be applied for 48 to 72 hours.
-
The patient should be advised that there
is a greater risk for recurrent bursitis after the first event, and
protective padding may be needed if the elbow is at risk of repetitive
trauma.
-
In most cases, patients have exhausted
the conservative treatment regimen described for acute bursitis. Many
present with an acute case superimposed on a chronic case of bursitis.-
In this instance, conservative treatment will not solve the problem.
-
-
The goal of operative treatment is to remove the entire bursal sac, as well as the loose bodies.
-
A posterior approach made slightly lateral to the olecranon is used.
-
An attempt is made to remove the entire bursal sac without disrupting the contents.
-
If there is an olecranon spur, it is removed.
-
Once removed, suturing the subdermal tissue to the underlying fascia obliterates the dead space.
-
-
An alternate approach is to close the
wound and then obliterate the dead space by passing mattress sutures on
either side of the incision.-
The skin is closed with suture, a
compressive dressing applied, and the elbow protected from flexion
greater than 45 degrees for 2 weeks.
-
-
Treatment usually consists of intravenous antibiotics, elevation, and analgesia.P.298
-
Until the pathogen and its sensitivities return, the antibiotic coverage is usually broad.
-
Once the sensitivities return, it can be tailored to the specific pathogen.
-
Most patients require 1 to 3 weeks of intravenous antibiotics, followed by several weeks of oral antibiotics.
-
-
In some cases, especially immunocompromised hosts, surgical treatment is warranted.
-
For those who get worse or fail to show
clinical improvement, surgical debridement similar to that described
earlier is conducted.-
A drain may be necessary for the first 24 hours for particularly aggressive infections.
-
The patient is placed in a compressive dressing and splint as outlined previously.
-
-
Morrey and Regan (2003) outlined a treatment plan that avoids the operating room in most cases.
-
The septic bursa is aspirated, and if the
aspirate is purulent or cloudy or if the patient is febrile, then the
bursa is lavaged, and 0.5 g of methicillin mixed in 10 cc of saline is
injected. -
The patient is then placed on proper oral antibiotics to treat Staphylococcus aureus.
-
If the fluid reaccumulates, a second aspiration is performed.
-
The elbow is splinted at 45 degrees.
-
If the patient has several bouts of the
septic bursitis, he or she is taken to the operating room for a formal
incision and drainage of the bursa.
-
describe the lesions around the medial aspect of the elbow. Medial
elbow injuries are quite common in a young patient population and are
related to increased tensile forces across the medial elbow in late
cocking and early acceleration phases of throwing. Year-round training,
breaking pitch, requiring more forceful flexion and pronation of the
wrist compared with standard straight pitch, and improper throwing
mechanics contribute to the development of medial-sided elbow injuries.
The affected patients are usually less than 10 years of age.
increased tensile stress on the medial epicondyle transmitted through
flexor pronator mass and MCL. This ultimately results in stress
fracture and separation of the medial epicondylar apophysis.
complaint in medial epicondylar apophysitis. It is also associated with
decrease in throwing velocity and the effectiveness of pitching. The
medial pain is generally worse with throwing but eventually can occur
with other activities.
-
On physical examination, characteristic
findings include medial tenderness over the epicondyle, swelling, and
occasionally flexion contracture. -
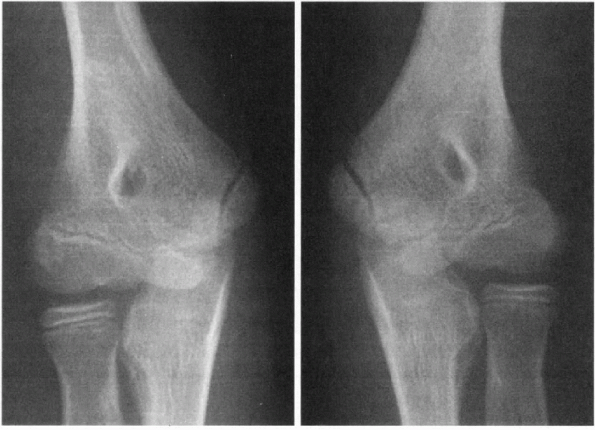
Early radiographic findings include irregular ossification of the medial epicondylar apophysis.
-
Later findings exhibit apophyseal enlargement, separation, and eventual fragmentation (Fig. 22-13).
-
Nonoperative treatment consists of rest
and nonsteroidal anti-inflammatory drugs (NSAIDs) for 2 to 4 weeks,
followed by stretching and range-of-motion exercises. -
Once motion is restored, strengthening is initiated with return to overhead activities at 6 weeks if pain-free.
-
Occasionally, pain persists secondary to inadequate period of rest.
-
In such cases, brief periods of
immobilization are appropriate to control inflammation and pain before
resumption of rehabilitation.
-
-
Shoulder rehabilitation is important to start at the same time to optimize the conditioning of the kinetic chain in throwers.
-
Throwing mechanics are examined and corrected if improper technique is used.
-
Number of pitches thrown and innings pitched must be monitored to avoid exacerbations of this condition.
-
-
In cases of acute avulsions of the medial
epicondyle, which usually result from extreme valgus loads during
throwing, treatment is guided based on fracture displacement.P.299-
Minimally displaced fractures are treated
by immobilization at 90 degrees for 2 to 3 weeks followed by
range-of-motion exercises. -
If the fragment is displaced greater than 5 mm, valgus stability is tested.
-
If instability is present, open reduction and internal fixation is performed with smooth K-wires.
-
-
In chronic medial apophysitis, nonoperative management is successful in returning patients back to sport.
-
Occasionally symptoms are recurrent, and the athlete has to miss a season.
-
In acute injuries, nonunions rarely occur from inadequate immobilization.
-
Late surgical excision may be indicated for pain.
-
Open reduction and internal fixation are
generally successful at restoring stability and prevention of future
radiocapitellar arthrosis.
-
 |
|
Figure 22-13
Comparison AP radiographs demonstrating left elbow medial epicondyle apophysitis with subtle widening in the throwing arm of a 10-year-old boy. (From Rudzki JR, Paletta GA Jr. Juvenile and adolescent elbow injuries in sports. Clin Sports Med 2004;23:581-608.) |
(OCD) of the elbow is much more common in the immature athlete. The
capitellum is the most common aspect of the elbow to be involved. In
the immature population, there are two entities that can involve the
capitellum. The first, Panner’s disease, is a self-limiting process
that involves general fragmentation and sclerosis of the capitellum. It
usually resolves without any long-term sequelae and is not associated
with overuse or repetitive elbow activity. It generally involves
children between the ages of 7 and 12 years old. The second, OCD,
usually presents itself between ages 11 and 15 years and is associated
with repetitive trauma. The area of the capitellum involved is well
defined. Unlike in Panner’s disease, the capitellum does not recover.
Instead, the area undergoes progressive flattening and fragmentation.
Fifty percent of the involved elbows will eventually develop
osteoarthritis.
 |
|
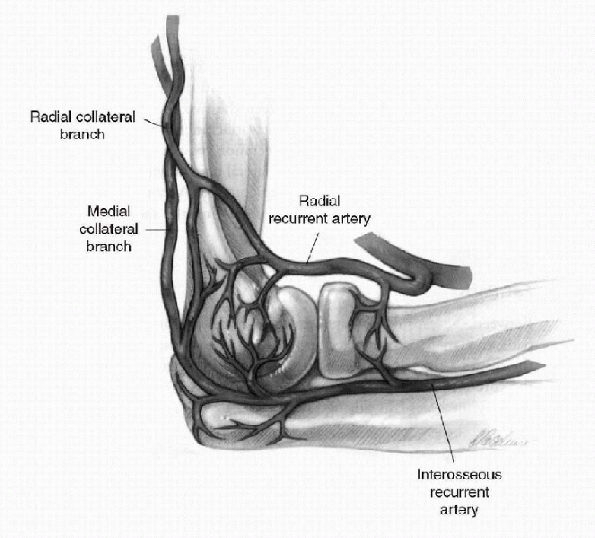
Figure 22-14
Lateral view of the right elbow showing the radial and interosseous recurrent arteries and the medial and radial collateral branches. (After Yamaguchi K, Sweet FA, Bindra R, et al. The extraosseous and intraosseous arterial anatomy of the adult elbow. J Bone Joint Surg Am 1997;79: 1653-1662.) |
Repetitive trauma clearly plays a role in its development. Multiple
studies have linked OCD with the trauma that occurs to the dominant arm
of male Little League pitchers. Studies have also linked the constant
stress of gymnastics on the immature elbow as a source of OCD in the
female athlete. Genetic predisposition may play a role in the
development of OCD. The nature of the vascular supply to the capitellum
may also play a role. The capitellum is supplied primarily by one or
two vessels traveling from posterior to anterior. There is no
metaphyseal collateral flow. The repetitive microtrauma experienced by
the elbow during pitching may be enough to disrupt the blood flow to
the capitellum and cause Panner’s disease or OCD (Fig. 22-14).
-
As described, the typical patient with Panner’s disease is 7 to 12 years old, whereas OCD affects children 11 to 15 years old.
-
With Panner’s disease, the child usually complains of stiffness and pain in the dominant elbow after activity.
-
The discomfort is relieved with rest.
-
-
With OCD, the patient may also experience pain and stiffness in the elbow.
-
As the fragmentation progresses, however, the child will start to demonstrate catching and locking of the elbow.
-
These symptoms are due to loose bodies within the joint.
-
-
Physical examination of the elbow usually reveals lateral elbow pain.
-
Although some may have pain specifically
over the capitellum, most usually have poorly localized pain over the
radiocapitellar joint.
-
-
Range of motion is limited, with a loss of extension more common than a loss of flexion.
-
Pain can be evoked with the active
radiocapitellar compression test, which involves pronation and
supination of the forearm while in full extension.
-
Diagnostic evaluation of an immature patient with elbow pain usually begins with radiographs.
-
AP and lateral x-rays are standard.
-
Early on in the disease process, these films may be negative.
-
-
Comparative views of the opposite elbow should be obtained.
-
AP radiographs at 45 degrees of flexion have been recommended to identify capitellar OCD lesions.
-
As the disease progresses, flattening and sclerosis are seen on the radiographs.
-
The classic lesion involves the anterolateral aspect of the capitellum.
-
-
Although radiographs can be quite helpful
with the diagnosis of an OCD, MRI is now the best method to detect and
define an OCD of the capitellum.-
MRI has the ability to detect the subtle bone marrow changes that occur early on in the disease process.
-
With progression, the MRI is also able to
define the separation of OCD from the underlying subchondral bone and
damage to the articular cartilage.
-
-
The diagnostic ability of the MRI can be enhanced with the addition of intra-articular contrast.
-
The contrast can show the separation between the lesion and the subchondral bone, denoting an unstable lesion.
-
Not all unstable fragments can be identified through this method, however.
-
-
MRI can allow for the misdiagnosis of a
pseudodefect, which occurs in the posteroinferior aspect of the
capitellum as opposed to an OCD, which usually occurs in the
anterolateral aspect of the capitellum. -
Classification in Table 22-5 is based primarily on MRI finding.
-
OCD lesions of the elbow can also be staged arthroscopically (Table 22-6).
-
Management of Panner’s disease is focused on relieving the symptoms.
-
By decreasing physical activity,
especially activities that load the lateral aspect of the elbow
(throwing, hand springs), the pain will usually resolve. -
For more intense cases, immobilization for 3 to 4 weeks may be necessary.
-
Long-term reports show excellent results for these patients.
-
-
Treating a young athlete with an OCD of the capitellum requires a review of both the clinical and radiographic evidence:
-
How old is the patient?
-
How long has the patient had lateral elbow pain?
-
Has the patient failed conservative treatment?
-
Does the patient demonstrate mechanical symptoms?
-
Is there evidence of an unstable lesion or loose body?
-
|
TABLE 22-5 CLASSIFICATION OF OSTEOCHONDRITIS DISSECANS OF THE ELBOW BASED ON MRI FINDINGS
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||
|
TABLE 22-6 CLASSIFICATION OF OSTEOCHONDRITIS DISSECANS OF THE CAPITELLUM
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
-
Whether viewed arthroscopically or established radiographically, type Ia lesions can be treated conservatively.
-
Cessation of all physical activity involving the affected arm is warranted.
-
Some advocate 3 to 6 weeks of protection in a hinged elbow brace with an anticipated return to activity by 3 to 6 months.
-
Others will allow strengthening of the
affected arm once the symptoms have resolved but will not return the
athlete to sports for at least 6 months.
-
-
Follow-up radiographs are obtained at 3 and 6 months.
-
In general, return to sports is based on
a clinical response rather than a radiographic response because the
radiographic changes may remain for months or years. -
If the symptoms return after the allotted period, the athlete is kept from athletics for additional time.
-
Pitchers may be changed to positional players, whereas competitive gymnasts may have to change to a different sport altogether.
-
Initial treatment of a type Ib lesion is the same as for a type Ia lesion.
-
For patients who fail conservative
treatment, have persistent pain, or who have developed an unstable
lesion, surgical intervention is warranted. -
An arthroscopic or possibly an open procedure through an anterolateral approach is conducted.
-
Bradley and Dandy (1989) described
subchondral drilling for lesions consisting of less than 55% of the
capitellum with less than a 60-degree angle. -
For larger, acute lesions, an attempt should be made to fix the lesion in situ with metallic or bioabsorbable implants.
-
Large lesions (greater than 70% with greater than 90 degrees on the lateral) have a poor outcome.
-
-
Chronic lesions with fragmentation should be debrided and drilled.
-
If the lesion is not completely detached, an attempt to fix it internally is made.
-
The subchondral bone is debrided, and
autograft from the ulna is used before fixing the lesion with a
metallic compression screw, which can be removed at 3 to 5 months.
-
-
For chronic, fragmented lesions, the area is debrided.
-
One must then consider use of an autograft or allograft osteochondral reconstruction.
-
-
Most patients with unstable type II lesions by radiographs, MRI, or arthroscopy will bypass the conservative treatment stage.
-
Surgical treatment is similar to that described for type Ib.
-
Chronic loose bodies are removed and the donor bed debrided.
-
Acute loose bodies may be fixed if the
patient had a previously documented OCD, and the displacement of the
fragment is clearly documented. -
For most patients, this is a salvage procedure, and they will be unable to return to sports.
-
This lesion is not usually encountered in the athletic population.
-
It represents damage to both the capitellum and radial head.
-
Treatment of the capitellar lesion, as described previously, can be undertaken when the radial lesion is small (<30%).
-
Debridement, drilling, or microfracture may all be useful in treating a radial lesion that is larger than 30%.
-
In the adult population, a radial head resection may be the best treatment option.
-
Most surgical patients were protected for
2 to 3 weeks in either a long arm cast or hinged brace. Passive and
active assisted range of motion was started at 3 weeks. -
For those with bony fragments reattached, active motion was not started until union was noted on radiographs.
-
For those with debridement only, active
range of motion was started once the patient had achieved full and
pain-free passive range of motion. -
Return to sport was allowed 6 months after surgery.
-
The outcome for patients with OCD of the capitellum depends on the type of lesion and the age of the patient.
-
Those diagnosed at an early stage and treated with an adequate rest period can do well.
-
Most patients, however, are diagnosed at the type Ib or II stage.
-
When followed out over the long term, these patients have a less favorable outcome.
-
-
For the youngest of our athletes, prevention is the still the best medicine.
-
Young throwers with good mechanics may be most at risk.
-
These athletes placed similar stresses on their shoulder and elbow as their professional counterparts.
-
Of all pitches, the fastball generates the most stress on the shoulder and elbow.
-
-
Box 22-3 contains recommendations for the young thrower with open physes.
-
For those with closed physes, the goal is still prevention.
-
Throwing athletes need to be well conditioned and should cross train to maintain conditioning.
-
Pitch counts should be monitored and controlled.
-
When discomfort is felt, the athlete should rest.
-
Medication can be used but should be used to help recover from and not cover up an injury.
-
During rehabilitation, it is important to incorporate elbow, shoulder, and scapular therapy on the throwing arm.
-
-
Limit number of pitches:9 to 12 years old: 6 innings per week13 to 15 years old: 9 innngs per week
-
Do not pitch or play when in pain
-
Do not medicate to play
Andrews JR. Kinetics of baseball pitching with implications about
injury mechanisms. Am J Sports Med 1995;23:233-239.)
apophysitis. During the acceleration phase of throwing, triceps
contractions put tensile forces on the olecranon. In childhood,
olecranon apophysitis usually occurs, whereas in adolescents, stress
fractures and avulsion of the olecranon apophysis may be seen.
-
Patients can present with acute (more common) or chronic pain and swelling over the posterior elbow.
-
Loss of terminal extension can also occur.
-
Athletes report decreased level athletic performance.
-
Symptoms are worse during physical activity, specifically during the acceleration and follow-through phases of throwing.
-
Physical examination findings include tenderness over the olecranon and pain with resisted extension.
-
It is important to assess valgus
stability of the elbow and palpate ulnohumeral articulation and
radiocapitellar articulation for tenderness.-
Overhead throwers may develop valgus
instability with resultant degenerative changes in the posterior
compartment and radiocapitellar articulation.
-
-
Radiographs characteristically demonstrate widening or fragmentation of the olecranon physis and sclerosis (Fig. 22-15).
-
Comparison to the contralateral side is useful in this age group to judge significant changes in the bone.
-
-
Absence of radiographic signs does not rule out this condition.
-
A technetium bone scan should be ordered when the level of suspicion is high to look for subtle stress fractures.
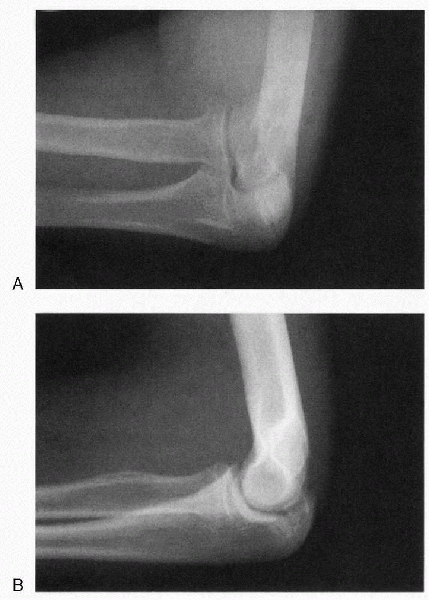 |
|
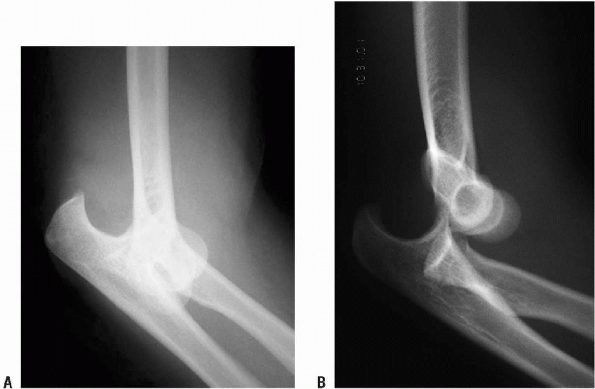
Figure 22-15 Radiocapitellar (A) and lateral (B)
radiographs of persistent olecranon apophysis. (From Rudzki JR, Paletta GA Jr. Juvenile and adolescent elbow injuries in sports. Clin Sports Med 2004;23:581-608.) |
-
Treatment is determined by severity of the injury.
-
Initial treatment includes rest, NSAIDs, cryotherapy, and activity modification.
-
Aggravating activities are avoided.
-
-
Once the symptoms are controlled, rehabilitation is initiated, focusing on range of motion and gradual strengthening.
-
Return to sport can usually occur in 6 weeks.
-
Occasionally, symptoms rebound and the
athlete has to be shut down from aggravating activity for longer period
of time and miss a season. -
In cases of chronic olecranon
apophysitis, physeal stress fractures, partial tears of the triceps,
and persistence of the apophysis into adulthood may occur.-
Persistent symptoms secondary to these conditions may require operative treatment.
-
-
In general, failure of apophyseal closure after 3 to 6 months of conservative treatment is an indication for internal fixation.
-
Usually, this is conducted through a
minimal posterior incision with placement of a cancellous screw. This
treatment is generally successful in achieving union.
-
Postoperatively, patients are immobilized
for 7 to 10 days with subsequent gradual active flexion and passive
extension exercises. -
At 6 weeks, active extension is allowed.
-
At 8 weeks, gradual strengthening begins and range-of-motion exercises are continued.
-
Return to athletic activity usually occurs in 3 months.
diagnosis, constituting only 1% to 2% of elbow arthritis. The diagnosis
is often a result of chronic overuse associated with repetitive motion.
Male to female ratio is 4:1, and the dominant extremity is affected 80%
to 90%, with bilateral involvement in 25% to 60% of cases. Common age
at the time of presentation is 50 years old, with variation from 20 to
65 years. Typical presentation in an athlete is a 35- to 45-year-old
male participating in a sport with intense repetitive motion of the
upper extremity.
-
The clinical presentation often consists
of a mildly limited range of motion (30 to 120 degrees), which may
compromise athletic performance (loss of extension in boxing), and pain
in terminal extension. -
It is important to ask the patient to
actively flex and extend elbows through arc of motion and determine at
which position symptoms occur.-
If pain occurs in the mid-arc of motion, as well as end-arc of motion, this may influence treatment options.
-
Forearm rotation is usually unaffected.
-
-
Ulnar nerve symptoms may be present and must be sought to make appropriate treatment plan.
-
The ulnar nerve must be palpated and checked for subluxation.
-
Tinel’s sign should be assessed.
-
-
Radiographic workup consists mainly of AP and lateral views.
-
These views usually demonstrate osteophyte formation at the coronoid and olecranon processes and in their respective fossae.
-
Loose bodies can also be seen around ulnar-humeral and radiocapitellar articulations.
-
Radial head involvement is evident in about 50% of cases.
-
-
Occasionally, cubital tunnel view may be useful if the ulnar nerve is involved based on physical examination findings.
-
Regular x-rays are usually all that is needed to establish diagnosis.
-
CT is useful as a preoperative tool to understand the exact location of osteophytes and plan surgical address.
-
Nonoperative treatment must be instituted
first, since the symptoms may be minimal and adjustment of technique or
activity may yield a satisfactory result. -
A course of anti-inflammatory medications may be helpful.
-
In athletic populations, activity
modification is usually not a realistic option, and recalcitrant
symptoms preventing sport participation justify surgical intervention. -
Several surgical options to treat primary osteoarthritis of the elbow exist.
-
Treatment depends on the ulnar nerve symptoms and the extent of the disease in the elbow joint.
-
Elbow arthroscopy is an option in experienced hands in patients who do not have ulnar nerve symptoms.
-
This technique allows removal of loose bodies and osteophytes, as well as capsulectomy in patients with limited motion.
-
Recent reports generally report quick recovery period and pain relief at the end-arc of motion is relieved in most cases.
-
Modest improvement of motion is also achieved but must be maintained with proper postoperative rehabilitation protocol.
-
Complications are rare but can be serious, involving surrounding neurovascular structures.
-
-
When motion is the dominating symptom, extensive capsulectomy must be performed, as well as osteophyte and loose body removal.
-
The posterior band of the MCL must be released to gain full flexion.
-
This can be performed safely when the ulnar nerve is protected through medial incision.
-
The ulnar nerve is identified and protected first.
-
After this crucial step, the elbow joint is entered from the medial side, and posterior and anterior capsulectomy are performed.
-
Osteophytes and loose bodies are removed.
-
The ulnar nerve is transposed or left in situ, depending on the preoperative symptoms.
-
-
Lateral column procedure accomplishes similar goals through the lateral approach.P.304
-
The ulnar nerve cannot be protected during this approach.
-
The joint is entered laterally and
anterior and posterior capsulectomy, and osteophyte and loose body
removal are performed in a similar manner.
-
-
In cases with extensive radiographic
disease, ulnohumeral arthroplasty allows access to the ulnar nerve and
circumferential removal of osteophytes and loose bodies.-
A posterior approach is used, and the ulnar nerve is identified and protected.
-
The medial edge of the triceps is
reflected and posterior capsulectomy, as well as removal of osteophytes
and loose bodies, is performed. -
Olecranon fossa is debrided with a trephine.
-
The resultant smooth curvature allows
access to the prominent coronoid process, osteophytes, and loose bodies
in the anterior compartment of the joint.
-
-
Interposition arthroplasty and total
elbow replacement are potential options for patients with extensive
disease and pain throughout the arc of motion.-
After these procedures, the patients are
advised not to return to activities that put any significant stresses
on the elbow joint.
-
-
The results of both the medial and
lateral open approaches, as well as the arthroscopic approach, are
similar and achieve reliable pain relief and improvement in range of
motion between 30 and 60 degrees.-
Recurrence of motion loss may occur and must be addressed by a judicious postoperative rehabilitation program.
-
Other reported complications include
intra-articular bleeding and nerve palsy. Fortunately, these
complications are rare but serious and usually can be prevented by
meticulous surgical technique.
-
-
With ulnohumeral arthroplasty, pain
relief is achieved in about 90% of patients, and modest improvement in
motion can be achieved.-
This motion can be lost in the postoperative period, as with other procedures described previously.
-
Recurrence of symptoms and radiographic changes occur in 20% of patients at 10 years after surgery.
-
Ulnar nerve symptoms occur in 10% of patients post-operatively.
-
-
Loose bodies within the elbow joint can occur in two distinct populations.
-
In the athletic population,
overhead-throwing athletes can develop loose bodies as the result of
the repetitive overhead motion and the stress that it places on the
elbow. -
Other patients can develop loose bodies as the result of trauma or degenerative arthritis in the elbow.
-
-
In the overhead-throwing athlete,
persistent valgus extension overload can cause impingement between the
posteromedial olecranon and the medial aspect of the olecranon fossa (Figs. 22-16 and 22-17).-
As in other parts of the body, the
repetitive stress can result in the development of osteophytes along
the posteromedial olecranon.
-
-
Some patients can have concomitant MCL pain, which can cloud the diagnosis.P.305
-
Throwing athletes with MCL pain generally
have discomfort at the medial epicondyle, whereas patients with valgus
extension overload will experience pain more proximally near the tip of
the olecranon. -
Both can experience pain during the early
acceleration phase of throwing and both can experience pain with a
valgus stress in the office.
-
 |
|
Figure 22-16
Medial tension overload secondary to repetitive valgus stress at the elbow, resulting in attenuation of the UCL complex medially, lateral radiocapitellar compression, and extension overload within the posterior compartment. (After Kvitne RS, Jobe FW. Ligamentous and posterior compartment injuries. In: Jobe FW, ed. Techniques in Upper Extremity Sports Injuries. Philadelphia: Mosby-Year Book, 1996:414.) |
 |
|
Figure 22-17
Valgus-extension overload of the posterior compartment results in posteromedial osteophytes within the olecranon fossa. (After Miller CD, Savoie FH III. Valgus extension injuries of the elbow in the throwing athlete. J Am Acad Orthop Surg 1994;2:261-269. © 1994 American Academy of Orthopaedic Surgeons.) |
-
In the valgus extension overload test,
the examiner repeatedly forces the slightly flexed elbow rapidly into
full extension while applying a valgus stress (see Fig. 15-28 in Chapter 15).-
A positive test points to the presence of posteromedial osteophytes.
-
-
Standard AP, lateral, and oblique films should be obtained.
-
Up to 30% of loose bodies can be missed on standard films.
-
When considering the possibility of an MCL tear, an MRI is usually obtained. This will also help to delineate the loose bodies.
-
When an overhead thrower is diagnosed
with valgus extension overload and osteophytic changes, the first line
of treatment is conservative. -
Rest, ice, and anti-inflammatory medication may reduce the discomfort.
-
If a loose body accompanies the osteophytic changes, arthroscopy is the treatment of choice.
-
Elbow arthroscopy can be conducted with the patient supine, lateral, or prone.
-
The most important factor for elbow arthroscopy is placement of the portals.
-
Unlike other major joints, the elbow has several neurovascular structures that lie very close to all possible portal sites.
-
Because of the possible injury to these structures, some basic principles for elbow arthroscopy should be followed (Box 22-4).
-
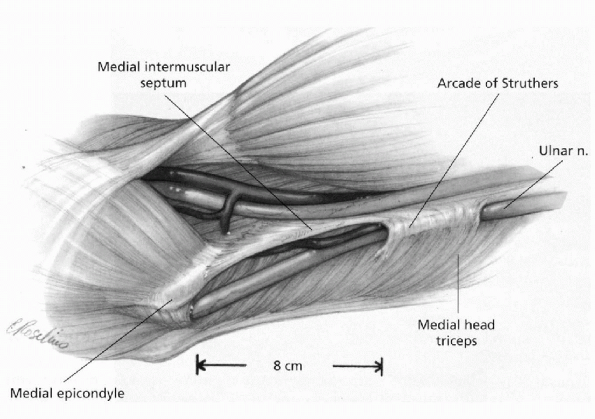
The anteromedial portal has the highest risk as a result of the proximity of the ulnar nerve (Fig. 22-18).
-
The most important aspect of placement of this portal is to stay anterior to the intermuscular septum.
-
A portal 2 cm above and 1 to 2 cm anterior to the medial epicondyle has been described, but this places the ulnar nerve at risk.
-
The standard anteromedial portal is made
2 cm distal and 2 cm anterior to the medial condyle. This portal places
the brachial artery, ulnar nerve, and median nerve at risk.
P.306 -
-
Laterally, four portal sites have been described.
-
The standard site is located 1 cm distal and 3 cm anterior to the lateral epicondyle.
-
The midanterolateral portal, the proximal anterolateral portal, and the straight lateral portal have all been described.
-
The straight lateral, or soft spot, can also be used to distend the joint before the start of arthroscopy.
-
-
Three posterior portals exist for inspection of the posterior elbow.
-
The posterocentral portal is 3 cm above the tip of the olecranon.
-
Both medial and lateral gutters, as well as the olecranon fossa, can be observed through this portal.
-
-
The proximal posterolateral portal is located along the lateral gutter anywhere from the olecranon tip to 3 cm proximal.
-
The inferior posterolateral portal is created at the level of the radiocapitellar joint within the lateral gutter.
-
-
-
After the removal of the loose bodies, the spurs along the medial aspect of the olecranon and within the fossa can be addressed.
-
Usually, the central and proximal posterolateral portals are used for this purpose.
-
-
Care must be taken to protect the ulnar nerve and the triceps tendon.
-
In this instance, suction should never be used when the shaver or other instrument is within the medial gutter.
-
 |
|
Figure 22-18
The ulnar nerve courses around the medial aspect of the elbow. Proximally, the nerve passes beneath the arcade of Struthers, runs along the medial intermuscular septum, enters the cubital tunnel around the medial epicondyle, and passes through the two heads of the FCU. (From Doyle JR, Botte MJ. Elbow. In: Hand and Upper Extremity Surgery. Philadelphia, Lippincott Williams & Wilkins, 2003: 389.) |
-
Avoid penetrating the subcutaneous tissue with the scalpel blade when making a portal
-
Flex the elbow 90 degrees to insert an arthroscopic sheath
-
Outline bony landmarks before capsular distention
-
Measure precisely the portal placement from the appropriate landmarks
-
Direct the arthroscopic sheath and trocar directly toward the center of the joint during insertion
-
Local anesthesia is not recommended
-
Postoperative neurovascular examination is mandatory
-
All patients are started on immediate range of motion.
-
After return of full range of motion, strengthening of the upper extremity is started.
-
For overhead athletes, this includes incorporation of shoulder and scapular rehabilitation into the recovery phase.
-
-
Most throwing athletes can begin rehabilitative throwing by 6 to 8 weeks.
-
Anticipated return to sport is 3 to 4 months.
-
Arthroscopic removal of loose bodies has up to a 90% success rate.
-
Even more favorable results have been reported when loose body removal is accompanied by ulnohumeral arthroplasty.
-
The most common complications are as follows: Persistent drainage from the arthroscopy portals
-
Deep infection
-
Minor contractures
-
Transient palsies
-
Permanent nerve damage
-
-
Permanent nerve damage has been reported for each of the three nerves around the elbow.
musculoskeletal junction, incontinuity tendon tear, and at the tendon
insertion to the radial tuberosity. Avulsion from the radial tuberosity
is the most common location of injury. This injury occurs routinely in
male patients with dominant extremity involvement in 80% of the cases.
resistance to elbow flexion at around 90-degree position. Anabolic
steroids and chronic degenerative changes in the tendon are common
predisposing factors. Radiographic findings of radial tuberosity
spurring are the result of degenerative process at the tendon-bone
junction (Fig. 22-19). Previous history of pain
in antecubital fossa may represent pre-existing partial rupture.
Systemic conditions, such as hyperparathyroidism and lupus
erythematosus associated with tendon disorders elsewhere, may
predispose to biceps tendon rupture.
-
Clinical presentation usually consists of
acute sudden pain in antecubital fossa followed by a dull ache that can
persist for several weeks. -
The usual patient is a young or middle-aged male, healthy and physically fit.
-
On physical examination, ecchymosis and obvious characteristic biceps deformity with attempted contraction are noted.
-
Diminution of strength must be determined and compared with the contralateral side.
-
Supination strength is mostly affected by flexion strength.
-
Grip strength diminution is also common.
-
-
If the deformity is not present, partial
rupture may have occurred, and crepitus is usually present with
pronation and supination of the forearm.
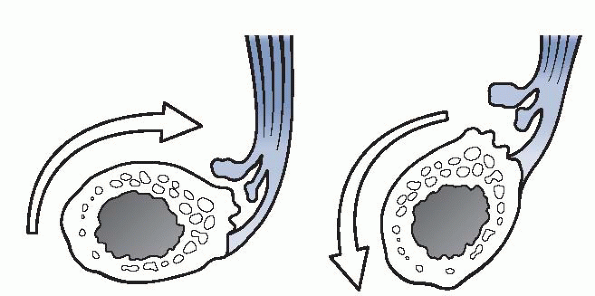 |
|
Figure 22-19
Pathophysiology of the distal biceps rupture. Hypertrophic changes at the radial tuberosity cause irritation of the tendon, predisposing it to degenerative changes and rupture during pronation and supination. (After Davis WM, Yassine Z. An etiologic factor in the tear of the distal tendon of the biceps brachii. J Bone Joint Surg Am 1956;38:1368.) |
-
Radiographic evaluation usually will demonstrate edema in soft tissues and degenerative changes of radial tuberosity.
-
Routine MRI is not necessary but is
occasionally helpful in cases with vague previous traumatic episodes
when the injury may not be acute, resulting in tendon contraction and
disappearance into the muscular substance.
-
In cases of acute disruption, operative repair is clearly superior to the nonoperative management.
-
Partial ruptures can be treated nonoperatively initially; however, if chronic pain develops, surgical approach may be necessary.
-
The two-incision approach popularized by
Morrey and the single incision anterior approach using various devices
securing soft tissue to bone are the two most common techniques of
distal biceps repair. -
In the two-incision technique, the tendon
is identified, secured with stitches, and passed with a hemostat along
the biceps tendon tract right next to the radius without exposure of
the ulna.-
The second incision is made over the hemostat, radial tuberosity is prepared, and repair is performed through the bone tunnels.
-
Exposure of the ulna is associated with increased incidence of heterotopic ossification.
-
-
The anterior single-incision approach has become more popular since the advent of suture anchors.
-
The anterior approach is used, and usually two suture anchors are secured in the radial tuberosity.
-
The suture limbs from the anchors are
passed through the tendon using various techniques, and the tendon is
repaired back to the radial tuberosity.
-
-
After repair of the tendon in the more
common insertion avulsion injuries, the arm is usually immobilized for
5 to 7 days at 90 degrees of flexion and then passive and active
gradual motion is begun. Strengthening is started at 3 months
postoperatively. -
For tendon tears in continuity and for
tears at the musculotendinous junction imbricating repair, graft
augmentation is usually necessary.-
These tears are very rare, and no reports on the results of treatment have been published.
-
The repair is usually protected for 3 weeks, and then gradual motion is begun over next 3 months.
-
-
In chronic injuries when the tendon has
retracted into the muscle belly, allograft reconstruction with repair
to the radial tuberosity is an option for patients who require
restoration of strength.-
Various graft tissues have been described, including fascia lata, semitendinosus tendon, and Achilles tendon allograft.
-
Rehabilitation focuses on protection of the graft and restoration of motion in the first 3 months.
-
Gradual strengthening is started after 3 months.
-
If the needs of the patient are satisfied with decreased supination strength, simple repair to the brachialis may be sufficient.
-
Rehabilitation is much simpler with no restriction on pronation and supination postoperatively.
-
-
The repair of the tendon in avulsion
injuries, regardless of the technique, results generally in restoration
of normal flexion and supination. -
Complications include radial nerve,
posterior interosseous nerve, and musculocutaneous nerve injury, which
are more associated with anterior approach. -
Heterotopic ossification is more common after the two-incision technique.
-
Meticulous passage of the tendon without exposure of the ulna prevents the occurrence of heterotopic ossification.
-
If the osseous bridge develops,
successful resection can be performed 8 to 9 months after the repair.
Recurrence of the tendon avulsion is very rare.
ruptures. This injury occurs in both men and women, with a male/female
ratio of 3:2. This injury can occur in a wide spectrum of ages, with a
mean of 33 years. The three sites of injury are muscle belly,
musculotendinous junction, and boney avulsion of the tendon, which is
the most common.
secondary to previous surgical release and repair. Traumatic rupture
most often occurs due to excentric contraction of the triceps of a
flexing elbow as it commonly happens during a fall. Uncoordinated
contraction of the triceps during physical activity may also cause this
injury. Direct blows to the distal triceps have also been reported to
result in tendon rupture. This is a much more rare mechanism of
traumatic injury. Spontaneous ruptures are usually secondary to other
inflammatory or systemic conditions affecting the strength
of
the tendon and its insertion to bone. Local inflammatory
conditions—such as olecranon bursitis and rheumatoid arthritis and
systemic conditions like secondary hyperparathyroidism, lupus
erythematosus, osteogenesis imperfecta, and renal osteodystrophy—have
been implicated in association with tendon ruptures. Triceps deficiency
after triceps detachment and repair as part of another procedure (e.g.,
total elbow arthroplasty) occurs rarely and its incidence depends on
the repair technique, which is beyond the scope of this chapter.
-
Patients usually present with acute onset of pain at the posterior elbow and variable weakness of extension.
-
Some residual extension may be preserved secondary to the anconeus confluence with triceps.
-
Extension against gravity, however, is usually absent in complete tendon ruptures.
-
Palpable defect can be palpated depending on the amount of retraction of the tendon.
-
Swelling and ecchymosis are common findings.
-
Neurovascular examination is usually
normal, although subluxation of the ulnar nerve with triceps tendon
rupture has been previously reported. -
Partial ruptures can be more difficult to
diagnose because of preservation of extension and less pain, compared
with complete ruptures.-
These patients can also present late because of delayed weakness, compared with the contralateral side.
-
-
Radiographic examination—including AP, lateral, and oblique views—is useful for several reasons.
-
Olecranon bony avulsions can often be noted and assist in establishing diagnosis.
-
Concomitant fractures, especially the radial head, have been reported.
-
-
MRI, although not routinely performed, can provide information about the extent of partial tears.
-
Surgical repair is the treatment of choice for complete tendon ruptures.
-
A common finding is the preservation of the lateral tendinous portion in continuity with anconeus.
-
Nonabsorbable sutures through drill holes provides strong repair.
-
Care must be taken medially to avoid injury to the ulnar nerve.
-
-
Partial ruptures can be treated nonoperatively.
-
One must make sure that most of the
tendon is still in continuity because later reconstructive options are
not as reliable in achieving good results.
-
-
Delayed reconstructive options include various fascial flaps and V-Y lengthening techniques.
-
We generally use anconeus slide alone or in conjunction with allograft tissue.
-
For significant tendon retraction, Achilles tendon is an ideal choice.
-
It provides secure fascial attachment
proximally to the triceps and distally allows boney fixation to the
olecranon with a screw.
-
-
Postoperatively, the arm is protected at 90 degrees of flexion for 3 weeks, and gentle active motion is allowed subsequently.
-
Strengthening is begun at 3 months.
-
Strength is often slow to gain, with 80% recovery at 6 months even for acute repairs.
-
Results have been generally good with repair or reconstruction up to 1 year after injury.
-
Strength is restored even though its recovery may take up to 6 to 8 months.
-
Terminal 5-degree loss of extension strength is a common finding.
-
Complications are not frequent and
include olecranon bursitis, loss of terminal extension strength, and
delayed recovery of strength.
than its medial counterpart. The peak incidence is in the fourth and
fifth decades of life. The prevalence rates are similar in males and
females. Seventy-five percent of cases occur in the dominant extremity.
The condition has been named “tennis elbow” because of the initial
implication of racket sports as the primary cause of the lateral
epicondylitis. Ten to 50% of tennis players experience this condition
at some point in their career. Many other sports and occupational
activities have been found to cause lateral epicondylitis. The common
etiologic factor is repetitive forearm activity and wrist motion,
especially forced extension. The pathologic lesion is located at the
origin of the common extensor tendon of the forearm consisting of
extensor carpi radialis longus, extensor carpi radialis brevis,
extensor digitorum communis, and the extensor carpi ulnaris.
Specifically, extensor carpi radialis brevis is the most commonly
involved
tendon in this disorder. It originates off the lateral epicondyle,
lateral collateral ligament, annular ligament, the investing fascia,
and the intermuscular septum. Electromyographic studies have shown
increased activity in the extensor muscles of the forearm in
professional and collegiate tennis players during ground strokes. These
muscles stabilize the wrist in acceleration and follow-through phases.
The greatest activity was noted in extensor carpi radialis brevis. In
athletes, improper technique and equipment have been implicated as
potential causative factors. In tennis, leading with the elbow, hitting
the ball late and off-center on the racket, has been associated with
increased incidence of lateral epicondylitis. Improper grip size,
racket weight, and racket stringing can also generate higher loads on
the extensor muscle origin.
epicondylitis seems to be tendinosis. The initial trauma to the tendon
causes intrasubstance microtear, which fails to heal secondary to
continued repetitive aggravating activity. The result is the formation
of the reparative vascular granulation tissue in the tendon. Nirschl
has described this tissue as “angiofibroblastic dysplasia” and proposed
a classification system for this process (Table 22-7).
-
Typical presentation consists of insidious onset of lateral elbow pain often associated with repetitive activity.
-
The pain often radiates distally through the forearm.
-
Patients often report weakness and difficulty carrying items in their hand.
-
Rarely is there a history of acute traumatic event associated with symptoms.
-
-
Physical examination must include the entire upper extremity and cervical spine.
-
The shoulder must be thoroughly examined
because degenerative disorders in the elbow are often associated with
overuse conditions in the shoulder. -
Range of motion of the elbow is usually normal.
-
Patients have tenderness to palpation,
with the greatest tenderness 2 to 5 mm distal to the lateral epicondyle
over the extensor carpi radialis brevis.-
Pain is increased with resisted wrist extension and maximal wrist flexion while the elbow is extended.
-
-
Resisted wrist extension creates tension in the diseased tendon, and maximal flexion puts the tendon on stretch.
-
Grip strength is often diminished, compared with the contralateral side.
-
The radiocapitellar joint must be palpated to evaluate for plica and potential chondral damage with loose body formation.
-
Tenderness over radiocapitellar joint is generally more distal than lateral epicondylitis tenderness.
-
-
Posterior interosseous nerve entrapment
often presents with similar symptoms and has been reported to actually
coincide with lateral epicondylitis in 5% of the cases.-
Patients with posterior interosseous
nerve entrapment usually demonstrate pain with resisted supination when
a nerve is entrapped in the supinator, or resisted long finger
extension when a nerve is entrapped in the extensor digitorum communis. -
Differentiating these diagnoses from lateral epicondylitis is a difficult task.
-
|
TABLE 22-7 STAGES OF THE DEVELOPMENT OF LATERAL EPICONDYLITIS
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
-
Radiologic workup occasionally reveals calcification in the extensor origin.
-
The presence of calcification does not alter the treatment and has no reported influence on prognosis.
-
-
MRI has limited value, although some
reports indicate that the size of the tear and degeneration of the
tendon can be reliably determined on MRI.
-
Nonoperative approach is the mainstay of treatment for lateral epicondylitis and is usually divided into three phases.
-
The first phase focuses on control of associated synovitis and pain.
-
Rest, activity modification, cryotherapy, NSAIDs, and cortisone injections can be used to control symptoms.
-
Physical therapy modalities such as friction massage, manipulation, phonophoresis, and iontophoresis may also control symptoms.
-
Counterforce bracing decreases the force on the tendon origin by controlling the musculotendinous unit expansion.
-
-
The second phase is focused on rehabilitation, including stretching, range-of-motion exercises, and strengthening.
-
It is important to include shoulder
rehabilitation, especially in athletes to avoid disuse atrophy and
preserve healthy kinetic chain.
-
-
The third phase
focuses on functional rehabilitation, sports-specific exercises,
correction of improper technique and equipment, and interval program of
activity to return an athlete to competition.
-
Operative treatment is offered for those rare patients who fail nonoperative treatment.
-
The goal of surgical treatment is to remove the diseased portion of the tendon and preserve lateral collateral ligament.
-
Multiple techniques have been described
over the years. Currently, open, arthroscopic, and percutaneous
techniques are used to address the lateral epicondylitis surgically. -
Open technique uses a lateral approach over the lateral epicondyle.
-
The interval between extensor carpi
radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) is
identified, and ECRL is elevated to reveal the ECRB tendon. -
The degenerative tissue is often located on the undersurface of the ECRB tendon.
-
The tendon is split, and the degenerative tissue is excised.
-
Surgical address of concurrent posterior interosseous nerve (PIN) entrapment can be performed at the same time if indicated.
-
Different subsequent steps can be used, and multiple reports have shown successful results with different techniques.
-
The origin of the tendon can be
reattached to the epicondyle. The epicondyle can be drilled and
rongeured to increase the vascular supply, the tendon can be
lengthened, synovial fringe can be excised, and the tendon can be
released without reattachment. -
All these techniques have shown similar outcomes and depend on the surgeon’s preference.
-
-
-
Arthroscopic lateral release is another surgical approach that has become available with the advent of arthroscopic techniques.
-
The advantage of arthroscopic technique is that concomitant intra-articular pathology can be addressed at the same time.
-
The patient is placed in either a supine, lateral decubitus, or prone position.
-
Proximal medial portal is created after the elbow is distended.
-
Diagnostic arthroscopy of the anterior compartment is performed.
-
Three types of lateral capsular lesion associated with lateral epicondylitis have been described.
-
Type 1 has intact lateral capsule.
-
Type 2 demonstrates a linear rent in the capsule.
-
In type 3, the entire lateral capsular origin is peeled off and reflected distally with ECRB visible behind it (Fig. 22-20).
-
-
The proximal lateral portal is created
with an out-side-in technique. Shaver and bipolar or monopolar
radiofrequency probes can be used to debride the lateral capsule and
the origin of the ECRB until the ECRL is visible. -
Care must be taken to stay over the anterior 50% of the radial head to avoid injury to the lateral collateral ligament.
-
The posterior compartment can be inspected through various posterior portals.
-
-
Percutaneous release have also been reported, with similar results as open procedures.
-
The procedure can be performed in the office.
-
The patient is given local anesthetic
injection. Onecentimeter incision is made transversely just distal to
the lateral epicondyle. -
Common extensor origin is incised with a scalpel just distal to the lateral epicondyle.
-
Hemostasis is controlled and the wound is closed.
-
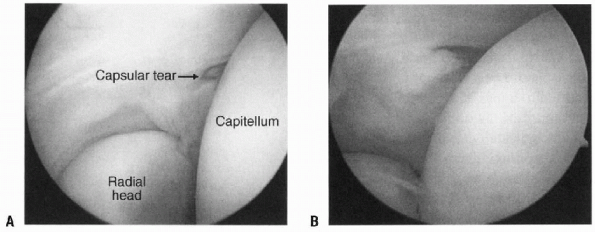 |
|
Figure 22-20 A:
Arthroscopic view of the lesion associated with lateral epicondylitis. The arthroscope is in the proximal port looking laterally into the anterior chamber of the elbow joint. B: A type 3 lesion. (From Whaley AL, Baker CL. Lateral epicondylitis. Clin Sports Med 2004;23:677-691.) |
-
The postoperative rehabilitation after
open approach includes early immobilization for 7 to 10 days, with
subsequent range-of-motion and isometrics exercises for 3 to 4 weeks. -
Gradual strengthening starts at that point.
-
After arthroscopic approach, range of motion and isometrics are started immediately.
-
Progressive strengthening starts at 4 weeks.
-
Patients often return to work in 2 to 4
weeks, depending on their vocation. Rehabilitation after percutaneous
release is similar.
-
The results of the nonoperative treatment are successful in up to 90% of the patients.
-
Regardless of the nonoperative approach, most patients seem to improve with time up to 1 year.
-
Arthroscopic and percutaneous approaches seem to be associated with faster recovery and return to occupational activities.
-
Posterolateral rotatory instability is a fairly recently described condition.
-
In this condition, the ulna and the
radial head rotate externally on the distal humerus when the forearm is
in maximal supination and the elbow is in slight flexion (see Fig. 15-31 in Chapter 15).-
This occurs when static and dynamic stabilizers of the lateral elbow are deficient.
-
-
The static stabilizer on the lateral side of the elbow is the LCL complex.
-
The complex consists of lateral ulnar
collateral ligament (LUCL), radial collateral ligament (RCL), annular
ligament, and accessory lateral collateral ligament (Fig. 22-21). -
The LUCL and RCL originate at the lateral epicondyle and are indistinguishable at this location.
-
The LUCL inserts on the crista supinatoris on the ulna, where distinct broad attachment of the ligament can be identified.
-
O’Driscoll described the LUCL as the “essential lesion” in posterolateral rotatory instability (PLRI).
-
-
The pathoanatomy of injury is a continuum of softtissue disruption that occurs in elbow dislocation.
-
In stage 1, LUCL is disrupted creating PLRI.
-
Stage 2 involves further disruption of the anterior and posterior capsule.
-
In stage 3A, the posterior band of the
ulnar collateral ligament (UCL) is torn and the elbow dislocates,
pivoting on the anterior band of the UCL. -
The anterior band is disrupted in stage 3B.
-
-
There is controversy as to what static stabilizers must be deficient for PLRI to occur.
-
Several studies pointed out that the proximal origin of the LCL complex (LUCL and RCL) must be detached for the PLRI to occur.
-
It seems that proximal detachment is much more significant in creation of instability as opposed to distal injury.
-
-
-
The dynamic stabilizers preventing PLRI are also not very clear.
-
The structures that have been implicated
in providing dynamic stability include lateral triceps, anconeus,
extensor muscles of the forearm, brachialis, intermuscular septum
between extensor digitorum communis and extensor digitorum quinti, and
deep fascial bands of extensor carpi ulnaris.
-
-
Disruption of the static and dynamic
stabilizers can occur in three different scenarios: elbow dislocation,
acute varus injury to the elbow, and iatrogenic causes.-
Elbow dislocation is the most common cause of PLRI.
-
Acute varus injury of the elbow can occur in elderly patients during falls.P.312
-
Repetitive stretching of the LCL rarely occurs, as it does to its medial counterpart, the UCL.
-
However, congenital or traumatic
conditions of the elbow, leading to cubitus varus, can cause gradual
stretching of the LCL resulting in PLRI.
-
-
Iatrogenic causes of LCL injury include
surgical procedures for lateral epicondylitis and radial head excision
or replacement when the LCL is inadequately repaired back to the
lateral epicondyle.
-
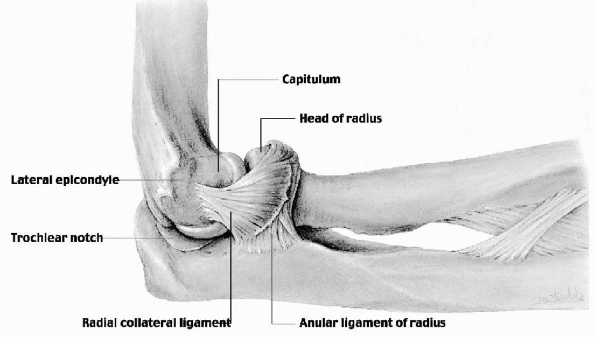 |
|
Figure 22-21
Radial (lateral) collateral ligament. The fan-shaped lateral ligament is attached to the anular ligament of the radius, but its superficial fibers continue on to the ulna. (From Moore KL, Dalley AF II. Clinical Oriented Anatomy, 4th ed. Baltimore: Lippincott Williams & Wilkins, 1999.) |
-
Clinical presentation of patients with PLRI is highly variable.
-
Presenting symptoms can be anywhere from pain to frank recurrent elbow dislocations.
-
Most of the time, patients present with pain when loading the elbow.
-
This is especially noted when the forearm
is supinated and elbow slightly flexed, such as when pushing off with
arms while getting up out of a chair. -
Symptoms of snapping, popping, and giving way can also be present.
-
It is important to ask about previous injuries and surgical procedures on the involved elbow.
-
A high index of suspicion and awareness about possibility of PLRI is important to avoid missing this diagnosis.
-
Physical examination may appear remarkably normal.
-
The range of motion is usually normal.
-
Tenderness is likely to be absent of traumatic event to the elbow, which occurred a long time before presentation.
-
Routine varus and valgus stress usually does not show any abnormal laxity.
-
-
Specific provocative tests have been shown to be helpful in making diagnosis.
-
These are difficult to perform in an awake individual.
-
The most sensitive test is the lateral pivot shift test of the elbow (see Fig. 15-31 in Chapter 15).
-
The patient’s shoulder is flexed and
maximally externally rotated with the examiner standing above the
patient’s head. The forearm is maximally supinated with valgus stress
on the elbow flexed at 90 degrees. Axial load is provided by the other
arm of the examiner, and the elbow is extended and apprehension
response or frank radial head subluxation may occur. This may create a
dimple in the skin overlying the radiocapitellar joint. When the elbow
is flexed again past 40 degrees, the radial head reduces and may
produce an audible and palpable clunk. -
The test is considered positive, even if
the maneuver elicits pain, since the patient’s guarding may prevent
actual subluxation of the radial head.
-
-
The posterolateral drawer test is another test for PLRI (Fig. 22-22).
-
The elbow is flexed to 30 or 90 degrees,
and the forearm is translated in anterior and posterior directions
relative to the distal humerus to create subluxation of the ulnohumeral
joint. Pivoting of the lateral forearm around intact medial structures
will occur in PLRI. -
The test is positive if instability is felt by both the examiner and the patient.
-
-
Another two tests consist of the patient
pushing up from either a prone position or from a chair with palms
supinated. The same maneuvers are performed with forearms pronated.-
If maneuvers are painful when the forearms are supinated and nonpainful when they are pronated, the tests are positive.
-
-
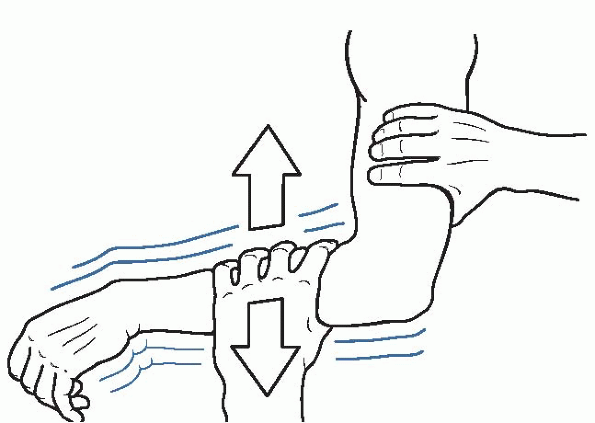 |
|
Figure 22-22
Lateral translation, which consists of superior and inferior stress to the lateral aspect of the flexed elbow while the forearm is fully supinated. (After Morrey B, O’Driscoll S. Lateral collateral ligament injury. In: Morrey BF, ed. The Elbow and Its Disorders, 3rd ed. Philadelphia: WB Saunders, 2000:556-562. Modified with permission from the Mayo Foundation for Medical Education and Research. All rights reserved.) |
-
Radiographic studies usually do not show
any abnormalities unless there is cubitus varus secondary to previous
fracture or congenital deformity. -
Stress views while applying varus stress
or posterolateral pivot shift can demonstrate LCL complex laxity and
radial head subluxation. -
MRI is rarely useful, although special sequences may demonstrate LCL pathology.
-
There is no successful nonoperative treatment for deficient LCL complex and PLRI.
-
Less active patients who modify their activity may adapt and accept the limitations of function.
-
In active patients, treatment of PLRI is surgical.
-
Examination under anesthesia is important
because this is the only time when a physician can truly assess the
extent of instability without the patient’s guarding. -
Repair of the LCL complex is indicated in
children, adolescents, and adults, with adequate ligamentous tissue for
repair back to the lateral epicondyle.-
A lateral 8- to 10-cm incision is made along the supracondylar ridge proximally and anterior to the anconeus distally.
-
The Kocher approach provides excellent exposure to the LCL complex and radiocapitellar joint.
-
If the tissue of the LUCL and RCL is
adequate, two nonabsorbable no. 2 or no. 5 sutures are placed in the
tissue in locked fashion. -
Three bone tunnels are created starting on the lateral epicondyle and exiting over the posterolateral supracondylar ridge.
-
Sutures are passed through the bone
tunnels and tied over the bone bridge, whereas the elbow is held in
valgus and 40 degrees of flexion, with the forearm in pronation. -
Anterior and posterior capsules are
plicated, and the extensor muscles, anconeus, and lateral triceps are
repaired back to the lateral epicondyle and lateral supracondylar ridge.
-
Most of the patients have attenuated ligamentous structures and require reconstruction of the LUCL.
-
Graft choices include ipsilateral
palmaris longus, contralateral palmaris longus, gracilis tendon,
semitendinosus tendon, fourth toe extensor tendon, plantaris tendon, or
a 3-mm-wide strip of the Achilles tendon. -
The approach is similar to the approach described for the repair.
-
The LUCL is split longitudinally along its fibers to identify the origin of the lateral epicondyle.
-
Ulnar tunnel and two lateral epicondylar tunnels are created.
-
The graft is passed through the tunnels.
-
The elbow is held at 40 degrees of flexion and full pronation, and the graft is sutured to itself.
-
Muscles and skin are repaired in the same manner as described for LCL repair.
-
-
Postoperative care after repair or
reconstruction initially consists of immobilization with elbow at 90
degrees of flexion and forearm in full pronation for 2 weeks. -
A brace is placed after 2 weeks; and
motion is allowed with block of extension at 60 degrees, 45 degrees,
and 30 degrees at 2-week intervals over a 6-week period. -
At 8 weeks, the brace is removed, but supination, extension, and varus forces are avoided.
-
Generally, patients return to activity at 9 months.
-
Long-term data on LUCL reconstruction are limited.
-
Repair of the ligaments when the tissue is adequate, and reconstruction restored stability in 89% of the patients in one report.
-
About 73% of the patients in this report achieved good or excellent results.
-
The results were better in patients with
a history of trauma, subjective complaints of instability, and
reconstruction with autograft tissue.
associated with medial-side tension injuries in adults. The spectrum of
the pathology includes tendonitis of the volar-pronator mass, medial
epicondylitis, ulnar nerve traction injuries, hyperextension valgus
overload, and UCL injuries. These conditions become more prevalent with
age and often interfere with athletes’ performance. Just as most of
overuse conditions, the medial-sided elbow disorders in athletes often
respond to rest, NSAIDs, and physical therapy. About 50% of athletes
undergo operative intervention to return to sports, however.
its counterpart, lateral epicondylitis. Consequently, much less
literature has been written about medial epicondylitis. The underlying
pathologic process seems to be similar; however, the anatomy in the
region of the medial elbow, specifically in close proximity of the
anterior oblique band of the UCL and the ulnar nerve, make medial
epicondylitis unique in terms of diagnostic workup and treatment.
life, with equal rates in males and females. Dominant extremity is
involved 75% of the time. Just as others overuse diagnosis, medial
epicondylitis is associated with repetitive stress over the medial side
of the elbow. Throwing athletes put tremendous strain over the medial
side of the elbow as described previously. The volar flexor-pronator
mass absorbs significant amount of the forces placed across the elbow
leading to degenerative changes at the musculotendinous region and the
tendon-bone junction at the medial epicondyle. This disorder has also
been associated with other sports, such as golf, tennis, bowling,
racquetball, football, weight lifting, and javelin throwing. Certain
occupations such as carpentry and plumbing have increased incidence of
medial epicondylitis most likely secondary to repetitive forearm
pronation and wrist flexion.
the tendinous origin of the flexor-pronator muscles, the ulnar nerve,
and the anterior band of the UCL. One must be aware of intimate
association of this structures and concomitant pathology that can
occur. The pronator teres and flexor carpi radialis are the most
lateral muscles of the flexor pronator mass and originate from the
anterior aspect of the medial epicondyle. These tendons are most
commonly involved in the pathologic process of the medial
epicondylitis. Proximity of the ulnar nerve often creates concomitant
pathology of ulnar nerve irritation and entrapment. The distal portion
of the cubital tunnel, between the two heads of the
flexor
carpi ulnaris, is the most common location of nerve compression. The
proximity of the UCL and the common mechanism of increased valgus
strain responsible for medial epicondylitis and degeneration of the UCL
make valgus instability an important part of differential diagnosis.
to the lateral epicondylitis. The three stages described for the
lateral epicondylitis most likely take place on the medial side.
-
Patients usually present with insidious pain over the medial elbow.
-
Pain is worse with forceful flexion and pronation of the wrist.
-
In athletes, pain is associated with
repetitive activity such as throwing and can be associated with other
pathologic processes such as ulnar neuritis and UCL insufficiency.
-
-
Range of motion is usually normal
initially, but with time, flexion contracture can develop and is very
common in overhead athletes. -
On physical examination, patients can have swelling and warmth over medial epicondyle.
-
Tenderness is usually present about 8 to
10 mm distal and anterior to the medial epicondyle over the pronator
teres and flexor carpi radialis tendons.-
Pain is exacerbated with resisted flexion and pronation.
-
-
Ulnar nerve neuritis and UCL deficiency may present in similar fashion or coexist in athletic population.
-
Thorough examination of the ulnar
nerve—including Tinel’s, elbow flexion test, and palpation of the
nerve—is an important part of the examination. UCL should be examined
by palpation along its course and using provocative tests: the valgus
stress test, the milking maneuver, and the Mayo valgus stress test,
described earlier.
-
-
Radiographic workup is usually negative but may reveal calcifications and traction spurs.
-
EMG testing is useful in patients with concomitant ulnar nerve symptoms.
-
MRI or magnetic resonance arthrography is
useful in athletes to assess the status of the UCL and evaluate the
origin of the volar-pronator muscle mass when acute rupture is
suspected.
-
Nonoperative approach to medial
epicondylitis is the mainstay treatment for this condition. It is
divided in three phases, similar to the lateral epicondylitis.-
The goal of the first phase is to control the inflammation and alleviate pain.
-
The patient is to stay away from offending activities.
-
Complete rest is discouraged to avoid atrophy.
-
The medial elbow is iced 3 to 4 times a day for 15 to 20 minutes.
-
A short course of NSAIDs and cortisone
injection into the subaponeurotic fatty recess may also be helpful to
alleviate pain from concomitant synovitis. -
Ultrasound and high-voltage galvanic
stimulation have been used to relieve pain; however, these modalities
have not undergone the scrutiny of prospective, randomized studies to
determine their efficacy. -
Counterforce bracing is also helpful to
decrease the intrasubstance tension in the tendon by limiting the
contractile expansion of the musculotendinous unit.-
The brace is worn during daily activities and may also be helpful in returning to athletic activity.
-
-
-
The second phase of the nonoperative treatment is focused on rehabilitation.
-
This phase is initiated as soon as the pain is controlled.
-
The first goal is to establish painless full range of motion.
-
Stretching and isometrics are instituted at this time.
-
As the strength and flexibility are restored, concentric and excentric strengthening exercises are begun.
-
The goal is to achieve greater strength than at the time of preinjury when tendinous injury occurred.
-
Shoulder and elbow rehabilitation is also
very important, especially in athletes before sport-specific and
vocational activities.
-
-
The third phase is focused on a safe return of an athlete back to competition.
-
Equipment and proper technique must be monitored to ensure prevention of recurrent symptoms.
-
Various equipment factors related to
increased incidence of lateral and medial epicondylitis have been
identified in different sports. -
The main goal is to decrease the vibration transmission and valgus stress to the medial elbow.
-
Experienced coaches, trainers, and
physicians can ensure safe return to the sport by using a structured
interval program focusing on flexibility, strength, and endurance.
-
-
-
Surgical treatment is offered when 3 to 6 months of nonoperative treatment fails.
-
In high-level athletes with tendon origin
avulsion, the operative treatment is offered sooner because return to
sport with such injury, especially throwing, is most likely
incompatible with conservative treatment. -
The goal of the surgical approach is to excise the degenerative tissue, enhance the vascular environment of the
P.315area, reattach the healthy tendon, and address concurrent ulnar nerve and UCL pathology.
-
The medial approach is used, and care must be taken to avoid injury to the medial antebrachial cutaneous nerve.
-
The degenerative tissue is excised
through the longitudinal muscle-splitting approach or transverse
approach, leaving tendon origin on the medial epicondyle. -
The bone bed can be rongeured and drilled to enhance the vascular supply to the area.
-
The defect is closed, and the tendon is
reattached to the epicondyle through bone tunnels or to the stump of
the tendon tissue that was left intact during the approach. -
Ulnar nerve and UCL pathology is addressed through the same approach if warranted.
-
Layered closure is performed, and the elbow is splinted at 90 degrees of flexion in neutral forearm rotation.
-
-
Postoperative rehabilitation includes immobilization for 7 to 10 days until wound heals.
-
Passive and active range of motion is started at this point.
-
Isometrics are initiated at 3 to 4 weeks, and resistive strengthening started at 6 to 8 weeks.
-
Athletes generally return to their sport in 3 to 6 months.
-
Results of nonoperative treatment are variable.
-
Older reports have shown a success rate
of 85% to 90%, but others have reported recurrence of symptoms in 26%
to 40% of the patients.
-
-
Surgical treatment after failed nonoperative management results in 88% to 96% of successful treatment.
-
Most athletes are able to return to their previous level of competition.
-
Results are better in patients without concurrent ulnar nerve pathology.
-
Objective strength deficits may occur but do not seem to result in functional compromise.
-
stability of the elbow. In extension, olecranon articulation with
olecranon fossa contributes to stability of the joint in the coronal
plane. Extensive valgus forces combined with hyperextension, which
occurs in throwing athletes, result in increased pressure between the
medial olecranon and the medial half of the olecranon fossa. This
process results in formation of osteophytes and loose bodies in
olecranon fossa and on the medial surface of the olecranon. Medial
ligamentous laxity exacerbates this condition.
-
Clinical presentation usually constitutes
pain medially and posteriorly, especially during acceleration and
deceleration phases of throwing. -
Patients may report catching, locking, and sharp painful episodes in terminal extension.
-
Terminal extension is often limited secondary to osteophytes and loose bodies.
-
Pain radiating down the ulnar side of the
forearm and tingling may represent ulnar nerve irritation secondary to
olecranon osteophytes. -
Physical examination usually demonstrates tenderness along the medial ulnohumeral articulation.
-
Crepitus and locking can be observed with active motion of the elbow.
-
Range of motion is often limited in extension due to impinging osteophytes.
-
Valgus testing and milking maneuver are important to assess anterior band of medial collateral ligament.
-
Testing for Tinel’s sign should be performed to check for ulnar nerve irritation.
-
Ulnar nerve instability must be checked for, especially prior to any surgical intervention.
-
Palpation of the radiocapitellar joint,
secondary stabilizer to valgus stress, is also important because
increased pressure in this articulation can cause articular damage and
loose body formation.
-
Radiographic workup includes AP, lateral, and axillary views.
-
Loose bodies and osteophytes can often be identified with these routine views.
-
MRI is often useful to further identify
loose bodies and osteophytes, as well as provide information about
surrounding soft-tissue structures.
-
Initially, treatment consists of rest,
NSAIDs, physical therapy focusing on excentric elbow flexors
contractions, modalities, supervised pitching mechanics, and gradual
throwing program as symptoms allow. -
Increased valgus stress at the elbow
during pitching was correlated with shoulder abduction angle at stride
foot contact and elbow angle at the peak of the elbow valgus stress. -
Modification of pitching mechanics may decrease the valgus stress seen at the elbow.
-
Operative options include open removal of osteophytes and loose bodies through posterior incision and arthroscopic approach.
-
The arthroscopic option results in less
morbidity, faster recovery, and offers the advantage of inspection of
the entire joint to address any additional pathology. -
The portals used for posterior compartment include the
P.316posterolateral portal, located 3 cm proximal to olecranon tip along the
lateral border of the triceps, and the direct posterior portal, located
3 cm proximal to the olecranon tip through the middle of the triceps
tendon.-
The posterolateral portal is usually used as a viewing portal, and the direct posterior portal is used as a working portal.
-
-
Care is taken to remove only osteophytes and preserve native olecranon.
-
When working medially, special attention
should be paid to avoid injury to the ulnar nerve traveling in the
cubital tunnel close to the medial osteophytes.
-
Postoperative rehabilitation consists of immediate active flexion and extension exercises.
-
Care is taken to gain full extension to prevent build of scar in the space created after resection.
-
At 6 weeks, the gentle throwing program is initiated, with return to competition allowed around 3 to 4 months postoperatively.
-
Open and arthroscopic treatments showed successful results in about 90% of patients.
-
In general, patients with posterior impingement alone do better than patients who developed degenerative changes in the joint.
-
One of the concerning findings is that in
professional baseball players, resection of the medial olecranon may
unmask valgus instability secondary to incompetent medial collateral
ligament.-
In one of the reports, 25% of players required subsequent MCL reconstruction.
-
-
Medial olecranon osteophytes may provide increased valgus stability in patients with incompetent MCL.
-
Resection of these osteophytes leads to further damage of the MCL secondary to increased demand during throwing.
-
Increased sequential resection of the olecranon places increased strain on the MCL.
-
These results further stress the
importance of careful medial resection of osteophytes, leaving only the
native olecranon intact.-
The exact amount of safe resection is currently unknown.
-
-
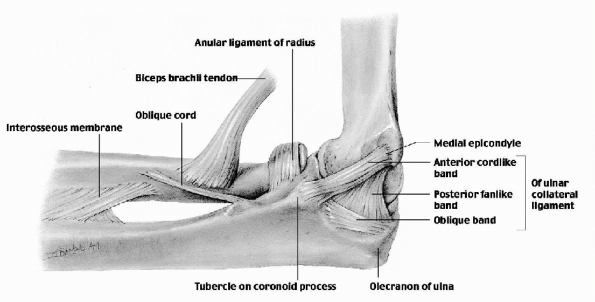 |
|
Figure 22-23
Ulnar (medial) collateral ligament. The anterior band (part)—a strong, round cord—is taut when the elbow joint is extended. The posterior band is a weak, fan-like ligament that is taut in flexion of the joint. The oblique fibers merely deepen the socket for the trochlea of the humerus. (From Moore KL, Dalley AF II. Clinical Oriented Anatomy, 4th ed. Baltimore: Lippincott Williams & Wilkins, 1999.) |
The anterior bundle is the primary stabilizer of elbow to valgus
stress. Throwing athletes with injury to the anterior bundle of the
ligament have pain and decreased athletic performance.
anterior band of the UCL during throwing. The greatest stresses occur
during late cocking and early acceleration phases of throwing. During
the acceleration phase, the elbow flexes from 90 to 120 degrees and
rapidly extends at 40 msec to the ball release. The angular velocity of
the elbow during this interval of time is 4,500 deg/sec. The forces
placed on the UCL often exceed its tensile strength. Improper throwing
mechanics, poor flexibility, and inadequate conditioning may result in
additional cumulative stress transmitted to UCL complex. This mechanism
of throwing puts repeated stress on the anterior band of UCL, resulting
in stretching, attenuation, and sometimes frank failure of the ligament.
-
Two types of presentations can occur in athletes with UCL injury.
-
The more common presentation consists of
gradual onset of medial pain during the late cocking and early
acceleration phases of throwing. -
Sometimes athletes can experience
first-time medial pain after a particularly intense and prolonged
period of throwing, after which they continue having medial pain and
can subsequently throw at only 50% to 75% of their normal level. -
Occasionally, an athlete experiences acute pain and pop after a throw and is unable to continue throwing.
-
-
It is important to collect as detailed a
history as possible including time of onset of symptoms and phase of
throwing when symptoms are most bothersome.-
Changes in training regimen, accuracy, velocity, stamina, and strength, as well as prior injuries, are important information.
-
About 85% of athletes experience symptoms during the acceleration phase of throwing.
-
-
Any neurologic and vascular symptoms must be sought.
-
Ulnar neuritis is commonly associated
with UCL insufficiency and it is important to assess the symptoms,
especially motor abnormalities, because it may influence treatment.
-
-
If there is an effusion of the elbow, the
joint is held at 70 to 80 degrees of flexion corresponding to the
greatest capsular volume. -
Carrying angle formed by the axial line of the humerus and the forearm is assessed.
-
Increased carrying angle may be secondary
to previous trauma, congenital abnormalities, as well as adaptive
changes in throwers secondary to the stretching of the medial
structures.
-
-
Range of motion is assessed both actively and passively, taking note of any contractures, crepitus, and pain.
-
Flexion contractures are present in 50% professional throwers and are considered normal adaptations.
-
-
Palpation on bony anatomy and soft tissue is also an important part of the examination.
-
Tenderness of the volar-pronator mass is
common in throwing athletes and should alert the physician to the
possibility of valgus instability.
-
-
Palpation of the UCL is performed with the elbow flexed 50 to 70 degrees, allowing the volar-pronator mass to move anteriorly.
-
Palpation is performed along the entire course of the ligament.
-
Pain on palpation may indicate a spectrum of pathology from intrasubstance tearing to frank rupture.
-
Some athletes may have rupture of the flexor-pronator muscle origin associated with UCL injury.
-
These patients will have pain on
palpation at the medial epicondyle and pain with resisted wrist
flexion, as well as weakness of wrist flexion.
-
-
-
The ulnar nerve should also be palpated along its course from the raphe of Struthers to the flexor ulnaris muscle mass.
-
Ulnar nerve instability is checked by palpation while moving the elbow from extension to flexion.
-
-
Stability of the elbow is assessed with
the valgus stress test performed at 20 to 30 degrees of flexion to
unlock the olecranon from the olecranon fossa (see Fig. 15-28 in Chapter 15).-
Opening of greater than 1 mm or pain may indicate abnormality in UCL.
-
This opening medially is difficult to
detect on manual testing, which may explain why studies by experienced
clinicians have noted the ability on physical examination to detect
valgus elbow laxity preoperatively of 26% to 82% of patients.
-
-
-
The milking maneuver produces a valgus stress to the joint in flexion and is helpful in assessment of UCL (see Fig. 15-29 in Chapter 15).
-
The affected elbow is flexed beyond 90
degrees, and the opposite hand of the patient is placed under the elbow
being tested to grasp the thumb of the affected hand, thereby exerting
a valgus stress on the affected elbow. -
The UCL is palpated by the examiner for tenderness and joint space opening during this maneuver.
-
This technique of examination is thought
to be more sensitive at 90 degrees of flexion, based on the increased
valgus rotation of the elbow at this position, as compared with the
30-degree position.
-
-
Another test for UCL insufficiency is the Mayo valgus stress test (Fig. 22-24).
-
The athlete’s shoulder is placed in an abducted and externally rotated position.
-
The elbow is then taken through its flexion-extension arc of motion while imparting a valgus force to the elbow.
-
During this maneuver, pain is usually felt at a specific and reproducible point within the flexion arc of 80 to 120 degrees.
-
This reproduces the pain of throwing in the athlete because of close replication of forces.
-
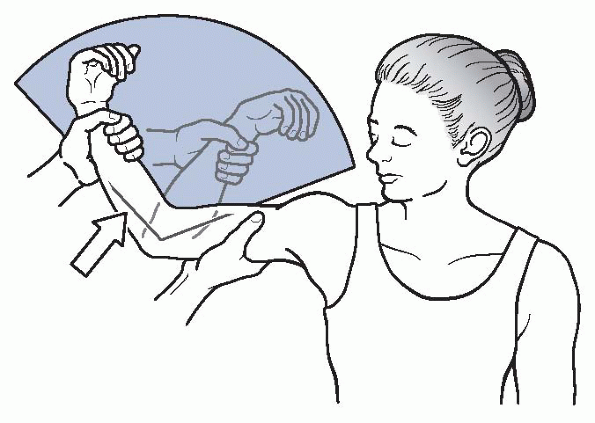 |
|
Figure 22-24
Mayo valgus stress test for UCL instability. A positive result is pain between 80 and 120 degrees. (After Safran MR. Injury to the ulnar collateral ligament: diagnosis and treatment. Sports Med Arthrosc Rev 2003;11:20.) |
-
Radiographic workup includes AP, lateral, axial, and two oblique views of the elbow.
-
Stress radiographs may be helpful to assess medial joint line opening, compared with the uninjured side.
-
Radiographs are evaluated for olecranon
osteophytes, loose bodies, and calcification within the ligament
(indicating potential previous injury). -
Diagnostic imaging for evaluation of soft tissue around the elbow, specifically UCL, continues to be a controversial topic.
-
The options include nonenhanced MRI, and CT and magnetic resonance arthrograms.
-
-
CT and magnetic resonance arthrograms showed similar sensitivity and specificity in diagnosis of complete and partial tears.
-
Nonenhanced MRI seems to be less accurate
for partial tears, although some reports demonstrated good sensitivity
and specificity using special sequences.
-
Nonoperative treatment of UCL injuries leads to satisfactory results in nonthrowing athletes.
-
In general, high-demand professional throwing athletes do not do well with nonoperative approach.
-
The nonoperative treatment begins with a
period of “active rest” (2 to 6 weeks) when the athlete stays away from
throwing and modalities focusing on control of inflammation and
range-of-motion exercises are instituted. -
Shoulder rehabilitation is an important
part of elbow recovery because any weakness or soreness at the shoulder
level places increased demand at the elbow during throwing. -
After pain in the elbow is resolved, strengthening of the flexor-pronator muscles is initiated.
-
Progressive strengthening of all muscle groups in the upper extremity is initiated after pain is controlled.
-
Plyometrics and functional exercises are started with an interval-throwing program initiated at 3 months.
-
Return to competition is allowed when the entire rehabilitation program is completed without pain.
-
Operative treatment of UCL injuries is
indicated in patients with complete rupture of UCL based on history,
physical examination, and imaging studies who want to return to active
throwing sports. -
The operative approach is also offered to
throwing athletes with partial tears who failed a comprehensive
nonoperative treatment described previously. -
Occasionally, nonthrowing athletes continue having symptoms of valgus instability despite nonoperative treatment.
-
Operative treatment constitutes reconstruction of the anterior band of the UCL.
-
Based on multiple reports, reconstruction
allows higher return to throwing and better overall results compared
with ligament repair. -
Jobe et al. (1986)
were the first to report on reconstruction of the anterior band of UCL
using graft tissue in the figure-of-eight fashion placed through bone
tunnels in the medial epicondyle of the humerus and the proximal ulnar
and suturing the graft to itself.-
This procedure allowed 10 of 16 athletes to return to the previous level of competition.
-
Several concerns with the approach
described in this chapter included detachment of the flexor-pronator
mass and routine submuscular ulnar nerve transposition.
-
-
Subsequently, several authors reported various modifications of the original surgical technique.
-
Modifications included a muscle-slitting
approach through the flexor-pronator mass with subcutaneous ulnar nerve
transposition or without ulnar nerve transposition, and utilization of
the Krakow stitch in the graft with fixation in the medial epicondyle
through the single bone tunnel (docking procedure).
-
-
Arthroscopic evaluation can be useful
before the open approach to confirm valgus instability and check for
concomitant pathology (e.g., olecranon osteophytes, loose bodies). -
Positioning of the patient for the arthroscopic portion is a matter of preference of the surgeon.
-
The anterior compartment is examined either from one of the medial or lateral portals.
-
Valgus stress is applied, and medial joint opening is confirmed.
-
The posterior compartment can be evaluated after that through the posterolateral portal.
-
The posterior portal can be established if osteophytes or loose bodies need to be removed.
-
-
After the arthroscopic portion of the procedure is finished, a medial approach to the elbow is used.P.319
-
Care must be taken to avoid injury to the medial antebrachial cutaneous nerve.
-
Depending on the surgeon’s preference,
the ulnar nerve can be dissected and protected throughout the procedure
for subsequent transposition. -
A muscle-splitting approach is less traumatic and allows adequate visualization of the anterior band of the UCL.
-
The anterior band is identified and split along its length.
-
Valgus stress is applied, and the opening of the medial joint space is confirmed.
-
Ulnar tunnels are made 3 to 4 mm distal to the sublime tubercle.
-
The ulnar nerve must be meticulously protected during placement of the inferior drill hole.
-
Proximally, the surgeon has a choice to
use either two tunnels and passing the graft in the figure-of-eight as
described in the original technique by Jobe or using a single tunnel
and fixing graft tissue over a bone bridge (docking procedure). -
Ulnar nerve transposition is performed if significant ulnar nerve symptoms were present preoperatively.
-
Subcutaneous transposition seems to cause less postoperative ulnar nerve symptoms, compared with submuscular transposition.
-
-
Postoperatively, the elbow is immobilized
for 7 to 10 days, with subsequent institution of active shoulder,
elbow, and wrist range-of-motion exercises. -
Progressive strengthening is initiated at 4 to 6 weeks.
-
The elbow is protected from valgus stress for 4 months.
-
It is important to include shoulder rehabilitation exercises early and continue them throughout the rehabilitation program.
-
Rotator cuff strengthening is initiated at 2 months post-operatively.
-
Progressive interval-throwing program is started at 4 months.
-
Return to competition occurs usually around 12 to 18 months.
-
Before the UCL reconstruction described
by Jobe, rupture of the anterior band of the UCL in a throwing athlete
was a career-terminating event. -
Several reports have documented the
results of the anterior band of the UCL reconstruction using Jobe’s
technique with or without modifications. -
The reconstruction allows return to a previous level of activity in 63% to 97% of throwing athletes.
-
Postoperative complications most commonly involve injury to the medial antebrachial cutaneous nerve and ulnar nerve irritation.
-
Recurrent instability due to stretching or rupture of the graft is uncommon.
EL Jr, Dugas JR, Wolf RS, et al. Elbow injuries in throwing athletes: A
current concepts review. Am J Sports Med 2003;31: 621-635.
MC, Schwartz MA, Ciccotti MG. Diagnosis and treatment of medial
epicondylitis of the elbow. Clin Sports Med 2004;23: 693-705.
FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral
ligament in athletes. J Bone Joint Surg Am 1986;68:1158-1163.
K, Burton K, Rodner C, et al. Lateral compression injuries in the
pediatric elbow: Panner’s disease and osteochondritis dissecans of the
capitellum. J Am Acad Orthop 2004;12:246-254.
J, Morrey BF, O’Driscoll SW. Ligamentous repair and reconstruction for
posterolateral rotatory instability of the elbow. J Bone Joint Surg Br
2005;87:54-61.
J. Fractures of the olecranon. In: Schatzker J, Tile M, eds. The
Rationale of Operative Fracture Care. Berlin: Springer-Verlag, 1987.
RJ III, Urquhart ER, Altchek DW. Medial collateral ligament tears in
the throwing athlete. Instr Course Lect 2004;53:579-586.
