Upper Extremity Nerve Injuries
that can occur during participation in sports activities. The most
common injuries experienced by athletes include contusions, sprains,
fractures, and dislocations. Less frequently, an athlete may suffer
from neurologic problems of the upper extremity, either in association
with the more common injuries noted previously, or as an isolated
entity. This chapter will discuss the various neurologic injuries that
may be encountered when providing care for an injured athlete.
organized array of structures that function to transmit electrical
impulses to and from the central nervous system as the body performs
its everyday activities. Sensory and motor nerves facilitate the
transmission of impulses in response to visual, auditory, and
physiologic stimuli from the environment. The components of the
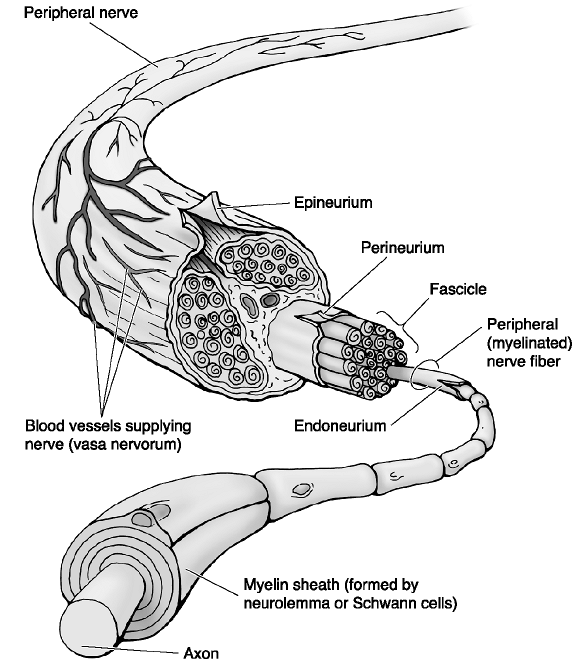
peripheral nerves include the axon, as the main conduit to and from the spinal cord, and the Schwann cell, which surrounds the axon as it courses throughout the body. Each Schwann cell is composed of myelin and is surrounded by endoneurium, with multiple axons forming a fascicle. Each fascicle is surrounded by perineurium, with multiple fascicles being surrounded by inner epineurium, and the entire nerve trunk is surrounded by the outer epineurium (Fig. 21-1). The significance of this organizational structure will become more relevant as we discuss the nature of nerve injuries.
extremity is helpful in understanding the patterns of injury that can
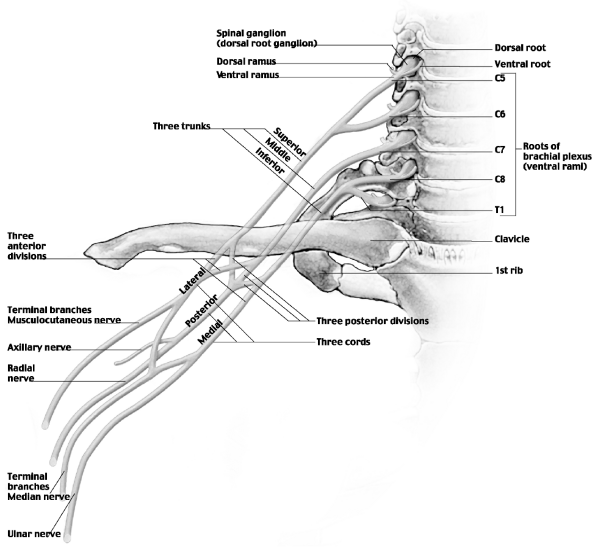
occur during sports participation. The brachial plexus
is the foundation for any discussion of the neurologic anatomy of the
upper extremity. The brachial plexus is formed by the cervical nerve
roots (from C5 to T1) as they exit the spinal cord in the cervical
spine. The roots combine to form trunks, then divisions, cords, and
finally the terminal branches (Fig. 21-2). The
terminology is based on the anatomical relationships to the vascular
anatomy of the shoulder and the clavicle as the nerves course distally
in the upper extremity. The manifestation of a nerve injury is
determined by the nature and location of the insult.
stresses that can result in traumatic injuries to the upper extremity,
including contusions, fractures, and dislocations. As the popularity of
“extreme” sports increases, physicians may see a rise in the number of
traumatic injuries, including those involving the peripheral nervous
system. Depending on the forces involved, nerves can be damaged by
blunt or penetrating trauma, traction from dislocations, or laceration
from fracture fragments. Peripheral nerves depend on their surrounding
microcirculation for normal function. Neurologic dysfunction in the
upper extremity can result from compression of a nerve by cysts,
ganglions, or entrapment from other soft-tissue or bony structures. The
local compression of a nerve can disrupt the normal microcirculation,
leading to ischemia and altered nerve conduction. Athletes who
participate in repetitive activities of the upper extremity can
experience nerve problems as an overuse injury. In that setting, the
recurrent stresses of a particular sport such as tennis or baseball can
cause damage to a nerve through traction on the nerve during the
motions of the activity. Several investigators have demonstrated
conduction abnormalities in rabbit tibial nerves that are stretched 6%
of their length, and that the intraneural vascular supply is occluded
at 15% lengthening. Finally, there is always the potential for
iatrogenic injury to the peripheral nerves that can occur during
surgical treatment of orthopaedic disorders of the upper extremity.
 |
|
Figure 21-1
Nerve anatomy of axon, Schwann cell, epineurium, endoneurium, and perineurium. (From Moore KL, Dalley AF II. Clinical Oriented Anatomy, 4th ed. Baltimore: Lippincott Williams & Wilkins, 1999.) |
the epidemiology of nerve injuries in sports. In a retrospective review
of 346 athletes involved in 27 different sports who were referred for
evaluation of neurologic problems, 86% of the injuries involved the
upper extremity. Most injuries occurred playing football, with
“burners” being the most common diagnosis. In a 5-year study of sports
injuries at an athletic clinic in Japan, there were only 28 peripheral
nerve problems among 9,550 athletes. Over an 18-year period, the
authors found that 5.7% of 1,167 peripheral nerve injuries were related
to sports, with most injuries involving the upper extremity.
that lead to various degrees of dysfunction, depending on the extent of
the inciting cause. In 1943, Seddon described three different types of
nerve injury and helped to form the foundation of our understanding and
treatment of these challenging problems.
and is described as a minor injury to the nerve, typically resulting
from blunt trauma, traction, or local compression. The pathologic
process consists of local demyelinization of the Schwann cell, without
disruption of the axon, leading to a conduction block. The effect of
this injury is a temporary loss of motor strength of the muscles and
occasionally sensory function of the dermatomes of the involved nerve.
There is no atrophy, or loss of normal reflexes, and spontaneous
recovery generally occurs within 3 to 4 weeks. The prognosis for
complete recovery is excellent.
disruption of the myelin sheath of the Schwann cell and the axon, but
with the outer epineurium remaining intact. In this scenario, there is
complete loss of motor and sensory function distal to the injury, with
atrophy, and absence of the muscle reflex. A process called “Wallerian
degeneration” takes place distal to the injury, involving loss of the
functional integrity of the nerve, whereas the structural integrity
remains intact. Because the epineurium remains in continuity, the nerve
has the innate ability to regenerate within the epineurial sheath. This
process has been measured to occur at the rate of 1 mm/day, or 1
inch/month, ultimately leading to return of normal, or near-normal
function.
which there is complete disruption of the myelin sheath, axon, and
epineurium. Patients with this injury will have no motor or sensory
function, with muscle atrophy, and loss of reflexes. Wallerian
degeneration occurs distal to the injury; however, because the
epineurial sheath is transected, there is little chance of nerve
regeneration and, consequently, little chance of functional recovery.
classification scheme noted previously can help in the diagnosis and
treatment of the patient, as well as offer an assessment of the
prognosis for recovery.
 |
|
Figure 21-2 Brachial plexus anatomy. (Courtesy of Anatomical Chart Co.)
|
sports-related neurologic injuries that impact the function of the
shoulder and upper arm. To enhance our understanding and evaluation of
these injuries, it is necessary to have a thorough knowledge of the
local anatomy. As discussed earlier, the brachial plexus is the origin
of the neurologic structures of the upper extremity. The peripheral
nerves supplying the muscles and sensory dermatomes of the shoulder and
arm arise from the brachial plexus as it courses distally from its
cervical and thoracic nerve root origins. Although any of the
individual nerves can be affected, we will concentrate on the more
common injuries that can occur during athletic activities, including
the brachial plexus, axillary nerve, musculocutaneous nerve,
suprascapular nerve, and long thoracic nerve.
neurologic dysfunction of the upper extremity that evolves from sports
injuries, but it is important to remember that there are numerous other
causes of neurologic abnormalities that must be considered when
evaluating patients, such as closed-head injury, stroke, multiple
sclerosis, muscular dystrophy, and a variety of other neurologic
diseases. A thorough discussion of these conditions is beyond the scope
of this chapter, and you are encouraged to review the appropriate
literature.
examination will depend on the initial presentation. The evaluation of
an unconscious athlete in the trauma room of an emergency room will
obviously be different from the evaluation of an athlete in your
office. The basic principles of a thorough exam should be followed
whenever possible, acknowledging the challenges and limitations
encountered in the emergency room setting.
-
The evaluation of a neurologic injury to
the upper extremity may begin on the playing field or sidelines during
a sports event, in the emergency room, or in a more controlled
environment, such as the office.-
A physician who provides coverage for
sporting events may witness a tackle, collision, or fall of sufficient
force to cause a neurologic injury. -
An injured athlete may be transferred
from the playing field to an emergency room for evaluation of a more
severe injury, or the athlete may present to your office with
complaints of pain, weakness, and possibly numbness of the upper
extremity without any inciting event.
-
-
In the treatment of an athlete, just as with any patient, the history will often give clues to the underlying problem.
-
Inquire as to whether there was a
traumatic event, and the specifics of the event, or whether the
symptoms developed insidiously.
-
-
Depending on the injury, the patient may
present with a variety of complaints, including pain, paresthesias,
numbness, weakness, fatigue, aching discomfort, and diminished athletic
ability.-
Patients may describe tingling, “pins and needles,” and burning as they relate their subjective complaints.
-
The symptoms may emanate from the cervical spine and radiate all the way to the hand.
-
-
Distinguish between symptoms that occur with activity and those that occur at rest, as well as with activity.
-
A competitive athlete may express frustration with his or her altered performance associated with the problem.
-
In many cases, the patient will be
anxious to resume sports participation as soon as possible, and there
may be a tendency to minimize symptoms and how they affect performance.
-
-
With pediatric patients, parents,
coaches, and trainers may be able to provide additional observations
related to the injury and subsequent problems experienced by the
patient.
-
A careful physical examination will
provide much of the information that will help elucidate the nature of
the condition that is causing the patient’s symptoms. -
When assessing neurologic abnormalities
of the upper extremity, it is important to remember that injuries to
the cervical spine can be manifested by dysfunction of the upper
extremity.-
It is imperative to thoroughly examine
the cervical spine of any athlete presenting with altered neurologic
function of the upper extremity. -
When possible, begin your examination
standing in front of the patient, but also be sure to examine the
patient from behind, looking for any muscle atrophy or loss of symmetry
that may be present. -
Look for any obvious bony abnormalities that might suggest a fracture or dislocation.
-
Palpate the cervical spine for any areas of tenderness or spasm, which may suggest an underlying injury.
-
Observe the range of motion of the cervical spine, taking notice of any limitations or pain reproduced during the motion.
-
Specific maneuvers to localize a particular nerve lesion will be discussed in the appropriate section.
-
-
Once the cervical spine evaluation is complete, the focus of the examination shifts to the shoulder and arm.
-
Compare active and passive range of
motion of the shoulder, elbow, wrist, and hand between the involved and
uninvolved extremity. -
Determine if any limitations in motion
are related to muscle weakness and an inability to move the involved
extremity, or if there may be limitations related to a contracture that
may suggest a longer time interval between the onset of symptoms and
the presentation in your office. -
Evaluate strength of the muscles of the
shoulder and throughout the upper extremity, including the periscapular
musculature, rotator cuff, elbow and wrist flexors and extensors, as
well as the muscles of the hand. -
Document any sensory deficits to light
touch, pinprick, and 2-point discrimination with a careful examination
of the dermatomes throughout the shoulder, and upper extremity, because
this may further localize the area of involvement. -
A check of the reflexes in the upper
extremity should complete the basic portion of the examination, noting
any discrepancies between the two upper extremities.
-
-
Although the history and physical
examination will provide much of the information necessary to suggest
the cause of a particular problem, additional information may be
helpful in arriving at a definitive diagnosis. -
If the clinical presentation includes a history of trauma, radiographs may be required to rule out a fracture or dislocation.
-
A computed tomography (CT) or magnetic
resonance imaging (MRI) scan may be appropriate to provide more
detailed information regarding the bony and soft-tissue structures of
the cervical spine, shoulder, and throughout the upper extremity. -
The role of nuclear medicine studies is
limited to an adjunct tool for assessing bony problems, such as occult
fracture, infection, neoplasm, or osteonecrosis, because these
conditions are rarely associated with neurologic dysfunction. -
The primary diagnostic tools for
evaluating neurologic abnormalities are the electromyogram (EMG) and
nerve conduction studies (NCS).-
The two tests combined allow the examiner to determine:
-
The presence of a nerve injury.
-
The anatomic region of the injury.
-
Whether the injury is acute or chronic.
-
Single or multiple nerve injuries.
-
The return of function after an injury.
-
Typically, it takes approximately 3 weeks
before any abnormalities will become measurable with an EMG/NCS, so
there is limited utility in the setting of an acute injury. -
It may be appropriate to obtain an
EMG/NCS early after an injury to determine the baseline measures in an
athlete with a history of previous neurologic dysfunction.
-
-
-
An EMG analyzes spontaneous and voluntary electrical activity in a muscle. Insertional activity refers to the electrical activity measured when the needle is inserted into a muscle or is moved within the muscle.
-
It is normal for there to be insertional activity.
-
Nerve damage can cause increased
insertional activity in cases of mild degeneration (neuropraxia) or
decreased insertional activity in cases of severe degeneration
(axonotmesis or neurotmesis).
-
-
Normally, there is no spontaneous activity in a muscle unless it is stimulated.
-
The presence of spontaneous activity in a muscle indicates an abnormal condition.
-
-
Spontaneous activity consists of fibrillation potentials and positive sharp waves,
and these may be seen in association with chronic denervation
(axonotmesis or neurotmesis) and also reinnervation after neurologic
injury. -
Motor unit potentials measure the number of muscle fibers stimulated by a particular axon.
-
After an injury—whether it is a
neuropraxia with conduction block, axonotmesis, or neurotmesis—there
will be diminished or absent motor unit potentials. -
As reinnervation occurs through
regenerated axons or collateral reinnervation, motor unit potentials
become larger and polyphasic in nature, allowing an objective
measurement of recovery.
-
-
NCSs measure the velocity, duration, and amplitude response of a peripheral nerve to an electrical stimulus.
-
-
Both motor and sensory components of a
nerve can be assessed, with abnormalities being associated with
prolonged latency (slower velocity) between the stimulus and a measured
response, along with prolonged duration and decreased amplitude of the
response.-
A summary of electrodiagnostic studies in peripheral nerve injuries is listed in Box 21-1.
-
-
Increased insertional activity
-
Fibrillation potentials
-
Positive sharp waves
-
Increased motor unit firing rate
-
Decreased number of motor units firing
-
Diminished motor nerve amplitude
-
Diminished sensory nerve amplitude
-
Prolonged latency
-
Slowed conduction velocity
with nerve injuries of the upper extremity, it is important to consider
the different options for treating acute versus chronic symptoms. There
are several scenarios that may necessitate emergent operative
treatment, including open fractures or dislocations, unreducible
dislocations, compartment syndromes, and injuries with neurovascular
compromise. Traumatic lacerations with neurologic symptoms may require
exploration and nerve repair. Alternatively, the majority of patients
who present with neurologic dysfunction of the upper extremity related
to sports may be managed nonoperatively, with a period of relative
rest, physical therapy, and if symptoms do not improve, surgery may be
appropriate. A more thorough discussion of the surgical alternatives
will follow the specific injuries discussed in the next section.
arises from the nerve roots C5 to T1 as they exit from the spinal cord
and travel distally in the neck, under the clavicle, and into the upper
arm. The nerve roots combine to form the upper, middle, and lower
trunks, then each trunk sends off an anterior and posterior division to
form the lateral, posterior, and medial cords. At various levels,
peripheral nerves branch off and continue to become motor and sensory
nerves of the shoulder, trunk, and upper extremity.
or penetrating trauma, traction from fractures or dislocations, and
laceration from fracture fragments. Be aware of the possibility of
vascular injuries in the setting of penetrating trauma or comminuted
fractures with significant displacement.
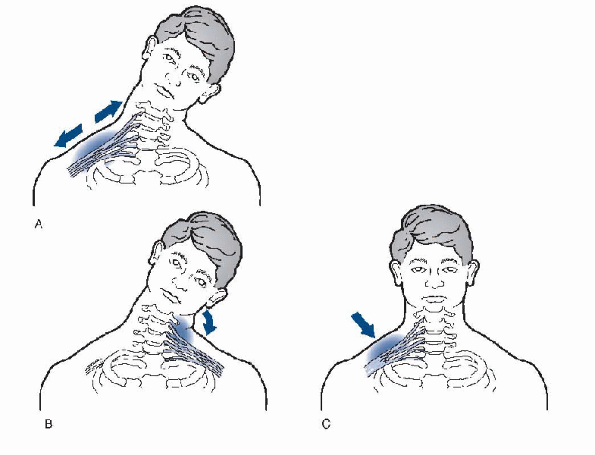
athletes participating in contact sports such as football, wrestling,
and hockey. These patients may suffer what is frequently referred to as
a “burner.” They will relate a history of striking another player, or
the ground, with their shoulder, often, as their head is pushed to the
contralateral side. Most frequently, a burner results from traction on
the upper roots of the plexus, C5 and C6, as the shoulder is pushed
downward, and the head is pushed to the opposite side (Fig. 21-3A).
Other mechanisms include a compression-type injury in which the head is
pushed to the same side as the symptomatic extremity (Fig. 21-3B), or a direct blow to the plexus from a helmet, a hockey stick, or lacrosse stick (Fig. 21-3C). It has been estimated that 20% to 65% of college football players experience a “burner” during their careers.
skateboarding, snowboarding, and mountain biking, the possibility of
high-energy trauma increases. Severe injuries are rare but can occur,
including scapulothoracic dissociation, in which the bony and
soft-tissue structures attaching the scapula to the trunk are
disrupted. This can include cervical root avulsions and vascular
injury. Clinical suspicion is warranted to rule out this devastating
injury.
weakness, and numbness of the upper extremity, including herniated
disc, cervical spine fracture or instability, and spinal cord contusion.
 |
|
Figure 21-3 Burner mechanism of injury.
|
-
Patients with a brachial plexus injury
can present with a variety of symptoms, depending on the nature of the
injury and the anatomic level of the injury. -
Patients who suffer burners report a
confluence of symptoms ranging from burning, “pins and needles,”
weakness, tingling, and numbness, all the way to temporary paralysis of
the upper extremity. -
The symptoms can last for a few seconds
to several minutes, and occasionally beyond that, and may radiate from
the shoulder to the hand and fingers. -
Patients with severe traumatic injuries
of the brachial plexus may present with pain, strength, and sensory
deficits related to the specific structures damaged by the injury.
-
The evaluation of patients with a
brachial plexus injury should begin with the cervical spine to make
sure there is no underlying damage that could result in a catastrophic
event if undetected. -
When assessing patients on the playing
field, spine precautions should be enacted for any athlete with a
suspected cervical spine injury. -
When a high-speed injury occurs, patients
should be treated following Advanced Trauma Life Support guidelines,
including controlling the airway, providing CPR when indicated, and
instituting spine precautions. -
Generally, a “burner” is not associated with neck pain or restricted motion of the cervical spine.
-
Brachial plexus injuries can be divided into supraclavicular and infraclavicular injuries.P.274
-
Those injuries that occur above the
clavicle, are supraclavicular, and are frequently associated with
Horner’s syndrome (ptosis, miosis, and anhydrosis). -
These are generally more severe injuries
and suggest the possibility of a cervical root avulsion, with loss of
autonomic function.
-
-
Passive and active range of motion should
be assessed throughout the shoulder and upper extremity, along with
careful evaluation of the motor strength, sensation and reflexes, in an
effort to localize the level of injury. -
If possible, examine the patient from behind, looking for muscle atrophy or scapular winging.
-
Peripheral pulses should be checked,
because these may be altered in more severe injuries such as
scapulothoracic dissociation or compartment syndrome. -
When there is no evidence of a traumatic
neck injury, the physician can perform Spurling’s test to differentiate
between cervical disc disease and a brachial plexus problem.-
Standing behind the patient, the examiner
hyperextends the patient’s cervical spine, flexes the head laterally
toward the involved side, and applies a downward force on top of the
head to axially load the spine. -
If the patient experiences symptoms
radiating into the arm, the result is positive, suggesting a cervical
nerve root impingement related to disc disease or foraminal narrowing
and not a brachial plexus problem.
-
-
Athletes with neck pain in association
with a burner should be evaluated with x-rays of the cervical spine to
rule out a fracture or other bony injury. -
If radiographs are nondiagnostic, then further evaluation with an MRI or CT scan may be indicated if neck pain persists.
-
Radiographs may be indicated to rule out fractures or dislocations of the upper extremity.
-
In the setting of high-energy trauma, the diagnostic workup should follow Advanced Trauma Life Support protocols.
-
Radiographs and CT scans will provide initial data regarding the injured structures.
-
If scapulothoracic dissociation is suspected, an arteriogram should be considered to rule out vascular injury.
-
After the life-threatening injuries have
been treated, additional information can be obtained with an MRI of the
cervical spine, the brachial plexus, and the shoulder if indicated.
-
-
There is little indication for an EMG/NCS in the acute setting, except as discussed previously.
-
Patients with symptoms that persist beyond 3 weeks should be referred for further evaluation.
-
Abnormalities may help to localize the level of involvement.
-
Patients will have normal sensory
responses and abnormal spontaneous activity in the paraspinal muscles
when the injury involves the cervical roots. -
Abnormal spontaneous activity in the
upper extremity muscles with normal activity in the paraspinal muscles
suggests a brachial plexus injury.
-
-
Most patients recover spontaneously from burners with little sequelae.
-
In some athletes, the symptoms can occur repeatedly with future contact episodes.
-
The treatment of a burner should include
keeping the athlete out of sports until the symptoms resolve and the
physical examination returns to normal. -
Encourage the patient to work on regaining full range of motion of the cervical spine and the upper extremity.
-
Any strength deficits should be addressed through a focused rehab program.
-
The athlete should be instructed on proper technique to avoid recurrent injury.
-
For football players, protective collars on the shoulder pads may lessen the likelihood of recurrence.
-
Patients need to be evaluated on a daily
basis for the first few days after injury and then weekly until the
symptoms have resolved. -
The treatment of a traumatic brachial
plexus lesion depends on the mechanism of injury, the associated
injuries, and the level of involvement.-
After the life-threatening injuries have
been stabilized, the orthopaedic injuries can be addressed, including
reduction of dislocations and fractures, and internal fixation when
appropriate. -
In severely injured patients, the
secondary survey may delineate the extent of neurologic deficits,
whereas additional diagnostic studies will provide information to aid
in planning the treatment. -
Initially, in the setting of a closed
injury without radiographic or electrophysiologic evidence of a nerve
root avulsion or nerve disruption, a shoulder sling may be appropriate
for comfort, along with physical therapy to help restore motion and
strength of the extremity. -
If functional deficits persist after 3 to
6 months, surgical alternatives include neurolysis, nerve repair, nerve
grafting, neurotization, nerve transfer, and muscle transfer.
-
idiopathic brachial neuritis—also known as acute brachial neuropathy,
neuralgic amyotrophy, brachial plexus neuropathy, and Parsonage-Turner
syndrome—which was named after two physicians who reported on 136
soldiers treated during World War II.
patient with this condition is between 30 and 70 years of age, with men
being affected twice as frequently as women. There is a belief that the
syndrome may be a sequela of a viral infection, although other possible
etiologies include heavy exertion, autoimmune disease, and recent
immunizations.
-
Patients can present with gradual or
occasional sudden onset of pain in the shoulder and upper arm, along
with varying degrees of muscle weakness and occasional sensory deficits. -
The symptoms can manifest with activity, as well as at rest.
-
Typically, the shoulder and upper arm muscles are affected; but in severe cases, the entire extremity can be involved.
-
The symptoms can mimic other conditions such as rotator cuff disease, cervical spine disorders, and compressive neuropathy.
-
Athletes with this condition may
demonstrate weakness and atrophy of several muscles of the shoulder
girdle and upper extremity, including muscles of the hand and wrist. -
Reflex and sensory deficits may be present.
-
The diagnosis of idiopathic brachial neuritis is based on the exclusion of other more common conditions.
-
Routine radiographs will generally provide little information.
-
An MRI scan of the shoulder should be
obtained to rule out rotator cuff disease, ganglion cysts that may
cause nerve compression, and to assess the presence of muscle atrophy. -
It may be appropriate to obtain an MRI of the cervical spine to evaluate any cervical disc disease.
-
The essential diagnostic tool is an EMG, typically showing changes 3 weeks after symptoms develop.
-
The findings of fibrillation potentials
and positive sharp waves indicate muscle denervation in association
with axonal neuropathy. -
Increased latencies and decreased active potentials are also noted.
-
 |
|
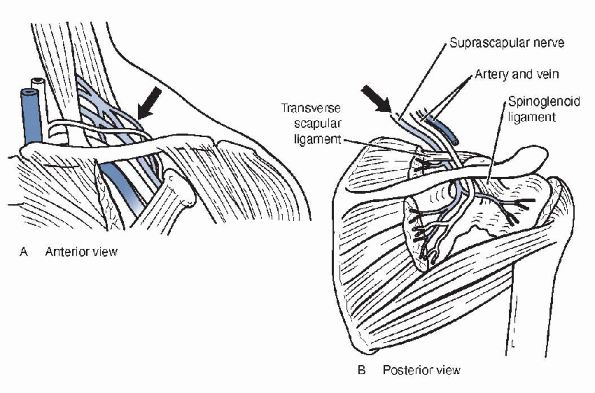
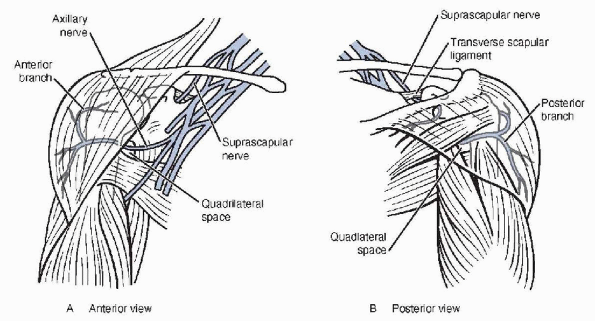
Figure 21-4 Anatomy of suprascapular nerve, anterior (A) and posterior (B) views, including suprascapular nerve and spinoglenoid notch.
|
-
Treatment of brachial neuritis consists
of analgesics, physical therapy to prevent arthrofibrosis, and work on
strengthening exercises to restore function. -
Spontaneous recovery generally occurs over several months, although occasionally the process may take several years.
-
Athletes can return to participation as their functional recovery allows.
physicians have recognized the subtleties of dysfunction that can occur
as a result of injuries other than rotator cuff disease and
glenohumeral ligament laxity. Although there is a long list of
differential diagnoses that need to be considered when evaluating
patients with shoulder problems, no list would be complete without
considering injury to the suprascapular nerve.
sensory innervation to the subacromial bursa, acromioclavicular joint,
and glenohumeral joint. The nerve traverses posteriorly, deep to the
trapezius, where it passes under the superior transverse scapular
ligament, through the suprascapular notch, before giving off a motor
branch to the supraspinatus muscle and sensory branches to the
subacromial bursa and acromioclavicular joint. The nerve continues
posteriorly and winds around the spine of the scapula as it enters the
spinoglenoid notch, under the spinoglenoid ligament. From there, the
nerve gives off a sensory branch to the posterior glenohumeral joint
and then terminates in motor branches to the infraspinatus muscle.
mechanisms such as fractures of the scapula and clavicle or penetrating
trauma. The nerve can become entrapped in either the suprascapular or
spinoglenoid notch, typically by a thickened superior transverse
scapular or spinoglenoid ligament, respectively (see Fig. 21-4).
The nerve may be compressed by a ganglion cyst in either notch or other
softtissue mass along its course. With athletes who participate in
repetitive overhead activities, the nerve is at risk for traction
injury associated with these sports. There have been several reports in
the literature noting the occurrence of suprascapular neuropathy in
volleyball players. As with many peripheral nerves, there is also a
risk of damage to the suprascapular nerve during shoulder surgery. In a
cadaver dissection, Warner et al. found that
the nerve could be injured if the supraspinatus and infraspinatus were
mobilized more than 3 cm. However, the occurrence of such injuries has
not been documented in the literature.
-
Typically, there is no specific injury that precedes the development of symptoms with suprascapular nerve problems.
-
Patients will usually complain of aching pain in the posterior aspect of the shoulder, often exacerbated by overhead activities.
-
Some patients may seek treatment because of weakness of the shoulder girdle.
-
With overhead athletes, diminished performance may be the impetus to seek medical consultation.
-
Occasionally, patients can be asymptomatic, and the only manifestation of the injury may be muscle atrophy.
-
A routine part of the physical
examination of any athlete with shoulder pathology is an assessment
from behind the patient, looking for atrophy of the muscles of the
shoulder girdle. -
With suprascapular nerve palsy, the physical findings will depend on the level of involvement.
-
If the nerve is entrapped in the
suprascapular notch, there may be atrophy of the supraspinatus and
infraspinatus, along with weakness of the external rotators, and a
positive supraspinatus test (see Fig. 15-3 in Chapter 15). -
Additionally, pain may be exacerbated with crossed adduction because this places the nerve under additional tension.
-
If the site of injury is the spinoglenoid
notch, the supraspinatus will be spared, and the patient may have
atrophy of the infraspinatus and weakness of the external rotators. -
Some patients, however, may not have any
weakness, as the teres minor can help to maintain strength against
resisted external rotation, and, in that situation, they may be
asymptomatic. -
Generally, patients will have normal range of motion of the shoulder unless limited by muscle weakness.
-
When considering suprascapular nerve
palsy in the differential diagnosis of posterior shoulder pain, an
EMG/NCS will provide diagnostic information, including the presence of
a nerve palsy, as well as the location of the lesion.-
It is important to localize the site of the nerve injury, because that will determine the surgical approach if necessary.
-
-
Routine x-rays of the shoulder will
generally offer little information for patients with suprascapular
nerve palsy, unless there is a clavicle or scapula fracture as an
underlying cause.-
If there is a question of a cervical radiculopathy, x-rays of the c-spine should be obtained to evaluate any abnormalities.
-
-
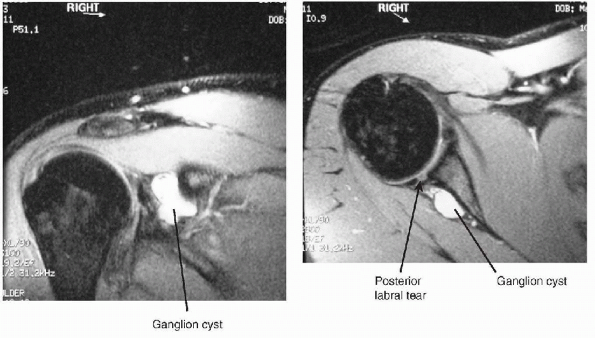
MRI (Fig. 21-5)
may be helpful in patients with suprascapular nerve palsy, looking for
a ganglion cyst in the suprascapular or spinoglenoid notch.-
These cysts can frequently be seen in association with a labral tear.
-
A routine MRI scan will delineate the
cyst, but an MRI arthrogram may be better at detecting labral pathology
associated with the cyst. MRI scans will also reveal the presence of
any other soft-tissue mass that may be a source of compression of the
nerve.
-
-
If the EMG or NCS is abnormal and the MRI
scan fails to show any abnormalities, the patient is most likely
suffering from entrapment of the suprascapular nerve in the
suprascapular or spinoglenoid notch, depending on the EMG/NCS findings.
-
The initial treatment of patients with
suprascapular nerve palsy includes avoidance of the activities that
produce symptoms, along with a physical therapy program to improve
flexibility and strength of the rotator cuff and scapular stabilizers. -
Anti-inflammatory medication and analgesics may be appropriate.
-
Several small studies have shown that
most patients can anticipate gradual relief of symptoms and improvement
in strength and muscle bulk over a period of 6 to 12 months. -
Nonoperative treatment is less likely to be successful in patients with a ganglion cyst.P.277
-
A review of the literature revealed less than 25% success with nonoperative treatment of these patients.
-
Mixed results have been reported with
ultrasoundand CT-guided aspiration of ganglion cysts associated with
suprascapular nerve palsy.
-
 |
|
Figure 21-5 MRI scans of cyst in spinoglenoid notch.
|
-
Surgical intervention should be
considered when pain symptoms and weakness persist despite nonoperative
management for 3 to 6 months. -
The surgical approach to treat
suprascapular nerve palsy is determined by the underlying pathology as
evaluated with EMG/NCS and MRI scan.-
When the MRI scan fails to reveal a cyst
or other soft-tissue mass, and the EMG/NCS show abnormalities of the
supraspinatus and infraspinatus—the site of involvement is the
suprascapular notch.
-
-
Surgical treatment is to release the superior transverse scapular ligament through a posterior approach to the shoulder.
-
The patient is placed on a beanbag in a lateral decubitus position, with the affected arm draped free.
-
The skin incision runs along the spine of
the scapula, with the trapezius being elevated superiorly, and the
underlying supraspinatus being reflected inferiorly to expose the
suprascapular notch. -
While protecting the underlying nerve and adjacent vascular structures, the ligament is released.
-
Numerous reports have demonstrated relief of pain and grad ual return of muscle strength with this intervention.
-
-
The decision to operate when the EMG/NCS
localizes the lesion to the spinoglenoid notch is based on pain
symptoms that occur with atrophy of the infraspinatus.-
Ferretti noted that, despite atrophy of
the infraspinatus muscle, a majority of volleyball players were able to
function without impairment. -
The surgical approach varies by exposing the nerve on both sides of the spinoglenoid notch.
-
The trapezius and supraspinatus are retracted superiorly, and the deltoid and infraspinatus are reflected inferiorly.
-
The spinoglenoid ligament is released under direct visualization while protecting the nerve.
-
On occasion, the spinoglenoid notch may need to be deepened to alleviate traction on the nerve.
-
-
If the MRI scan reveals a ganglion cyst,
arthroscopic examination of the glenohumeral joint is indicated to look
for and repair a labral tear, or other intra-articular abnormality that
may have led to the development of the cyst.-
It may be possible to decompress and
debride the cyst arthroscopically through the labral defect; however,
in some patients, the cyst may need to be excised through an open
approach.
-
-
Postoperatively, patients are placed in a
sling for 1 to 3 weeks, with early range of motion, depending on the
intra-articular findings at the time of surgery. -
The rehabilitation program includes
active and passive range-of-motion exercises, along with scapular
stabilization and rotator cuff strengthening. -
Most athletes return to sports within 2 to 4 months.
-
Even with successful resolution of
symptoms after surgical decompression of the suprascapular nerve,
nearly half of patients may have persistent atrophy.
injury of the shoulder. Considerable dysfunction of the upper extremity
can occur as a sequela of axillary nerve damage.
 |
|
Figure 21-6 Anatomy of the axillary nerve.
|
As the axillary nerve reaches the inferior surface of the
subscapularis, it curves posteriorly and inferiorly under the
glenohumeral joint. The nerve passes through the quadrilateral space (Fig. 21-6B),
where it divides into anterior and posterior branches. The posterior
branch supplies motor innervation to the teres minor and posterior
deltoid, and sensory innervation to the lateral aspect of the shoulder
via the superior lateral cutaneous nerve. The anterior branch curves
anteriorly and superiorly around the humerus, where it innervates the
middle and anterior deltoids. Anatomic studies have shown the axillary
nerve enters the middle deltoid approximately 5 cm below the lateral
edge of the acromion, a point to remember when performing surgery
through a deltoid-splitting approach.
injuries can occur through a variety of mechanisms, including traction,
blunt trauma, entrapment, and iatrogenic causes. The nerve is most
commonly injured after anterior dislocation of the glenohumeral joint,
with resultant traction and compression from the dislocated humeral
head. Several studies have shown the incidence of axillary nerve injury
after glenohumeral dislocation to range from 5% to 54%, with older
patients and shoulders left unreduced for several hours being more
susceptible. Displaced fractures of the shoulder may also damage the
nerve through traction or, in rare cases, laceration of the nerve from
fracture fragments. The axillary nerve can be damaged from blunt trauma
during contact sports such as football, and hockey, although this is a
less frequent scenario.
termed “quadrilateral space syndrome,” a condition in which the nerve
becomes entrapped by fibrous bands and hypertrophied muscle in the
quadrilateral space (teres minor, long head of triceps, teres major,
and humeral shaft).
various surgical procedures to correct shoulder pathology, including
anterior stabilization, arthroplasty, fracture fixation, rotator cuff
repairs, and arthroscopy. Surgeons need to identify and protect the
nerve from injury during open surgical techniques, and maintain an
awareness of proximity to the axillary nerve during arthroscopic and
open procedures. The nerve is more likely to be injured in revision
shoulder surgery, because the anatomy is frequently abnormal and scar
tissue may inhibit adequate visualization.
-
Manifestations of axillary nerve palsy
can include sensory and motor components, depending on the nature and
location of the injury, as well as the presence of any associated
involvement of the brachial plexus. -
Patients may present with weakness of the
shoulder, typically in flexion and abduction, along with numbness of
the lateral aspect of the shoulder. -
With quadrilateral space syndrome, the
athlete may complain of aching pain in the posterior shoulder, and
paresthesias of the lateral shoulder, without significant weakness. -
After surgical procedures of the
shoulder, diminished sensation over the lateral aspect of the shoulder
may be the earliest sign of axillary nerve injury because deltoid
function after surgery may be impaired by pain. -
Physical findings associated with
axillary nerve palsy are related to the degree of injury, ranging from
normal appearance and strength of shoulder flexion and abduction to
severe deltoid atrophy and weakness (Fig. 21-7). -
Patients will typically demonstrate altered sensation over the lateral aspect of the shoulder.
-
With any shoulder injury, it is important to document sensory deficits that may suggest axillary or other nerve dysfunction.
-
Range of motion of the shoulder may be impaired, depending on the underlying cause of the nerve injury.
-
Unless there is an associated brachial plexus injury, reflexes will be normal.
-
Patients with quadrilateral space
syndrome may present with no significant findings on exam, other than
tenderness of the posterior shoulder.
 |
|
Figure 21-7 Atrophy associated with axillary nerve palsy.
|
-
Routine x-rays of the shoulder are
indicated to reveal any fractures or dislocations that may be
associated with axillary nerve palsy.-
If the patient complains of neck pain, cervical spine films should be obtained.
-
-
The diagnostic test of most value will be
an EMG/NCS, looking for alterations of the deltoid and teres minor
function, along with the sensory changes that are common with axillary
nerve palsy.-
The electrophysiologic studies will also
elucidate any abnormalities of the brachial plexus that may suggest a
more significant problem. -
Because most axillary nerve palsies are
related to traumatic or iatrogenic causes, the test will be of little
benefit until 3 weeks or more after the injury. -
Abnormal findings are summarized in Box 21-1.
-
-
In evaluating quadrilateral space
syndrome, an arteriogram may provide additional information with
altered flow through the posterior circumflex artery as the arm is
brought into abduction and external rotation.
-
When an axillary nerve injury is diagnosed, the treatment is influenced by a variety of factors.
-
With closed injuries such as dislocations
or fractures, a prompt reduction is indicated to alleviate traction on
the nerve and lessen the risk of injury from a fracture fragment. -
A careful physical examination before treatment is necessary to document any baseline neurologic abnormalities.
-
The examination should be repeated after the reduction maneuver, and any changes should be noted.
-
-
If symptoms persist for more than 3
weeks, an EMG/NCS should be performed to assess any electrophysiologic
abnormalities, including the axillary nerve and the brachial plexus. -
Most injuries of the axillary nerve can
be managed nonoperatively with sling immobilization for a short period
of time, depending on the underlying injury, and a rehabilitation
program focusing on range-of-motion and strengthening exercises.-
The recovery of nerve function may take 3
to 6 months, depending on the initial injury, and a repeat EMG/NCS may
be indicated to provide objective evidence of recovery if an athlete
has ongoing symptoms and functional limitations.
-
-
If there is no clinical or
electrophysiological evidence of recovery by 3 to 6 months after a
closed injury, surgical exploration may be indicated.-
When an axillary nerve palsy occurs in
the setting of penetrating trauma, early exploration of the wound and
nerve repair within a few weeks of the injury may be indicated if the
EMG/NCS shows severe changes.
-
-
Patients who develop axillary nerve dysfunction after a surgical procedure can be managed with careful observation.
-
Frequently, the nerve can suffer a neurapraxia, resulting from traction during surgery.
-
An EMG/NCS should be obtained if no improvement is noted after 3 weeks.
-
If the results of the study suggest disruption of the nerve, exploration is indicated.
-
-
Surgical options depend on the findings
at the time of surgery and include primary nerve repair, neurolysis,
and sural nerve grafting.-
Patients are generally placed in a
lateral decubitus position because anterior and posterior approaches
may be necessary to perform a successful repair, frequently with sural
nerve grafting. -
There are a few studies in the literature reporting successful results in 50% to 100% of patients.
-
The best results were noted in patients who underwent surgery within 6 months of the injury.
-
-
For some patients, salvage procedures may
be indicated to treat severe deltoid atrophy and weakness that does not
resolve with nerve grafting and repair.-
In those patients, if the posterior
deltoid function is preserved, it may be possible to rotate the
posterior deltoid anteriorly on the acromion. -
Alternatively, a shoulder fusion can be
considered to provide a stable fulcrum for the upper extremity during
activities of daily living.
-
-
Athletes with quadrilateral space
syndrome can be treated using a rehab program that focuses on
stretching and strengthening as a part of anticipated recovery.-
Rarely, surgical decompression through a
posterior approach to the shoulder is indicated for patients who remain
symptomatic after nonoperative treatment. -
Cahill and Palmer achieved good or excellent results in 16 of 18 patients treated with decompression.
-
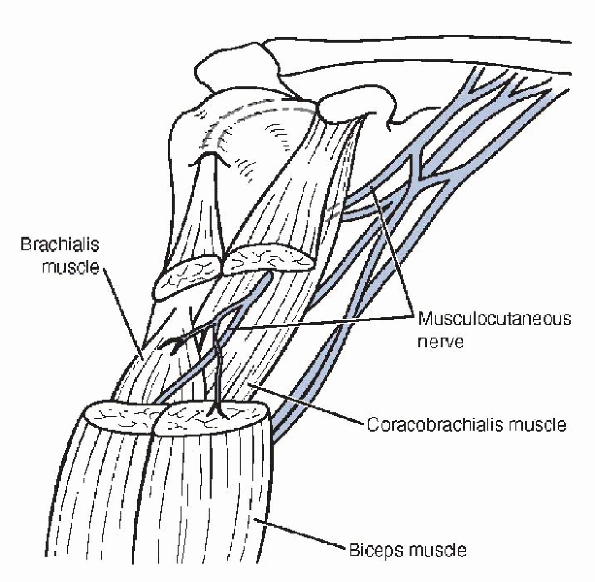
occurs with athletic activities. The nerve is more frequently injured
after trauma to the shoulder or surgical procedures around the shoulder
and has been reported to account for less than 2% of 14,000 nerve
injuries treated in World War II.
The nerve sends motor branches that enter the undersurface of the
coracobrachialis and brachialis muscles approximately 5 cm distal to
the coracoid process, as well as a motor branch to the biceps brachii
muscle (Fig. 21-8). The nerve courses distally
beyond the elbow, where it provides sensory innervation to the radial
aspect of the forearm via the lateral antebrachial cutaneous nerve.
injured as a result of traction from an anterior glenohumeral
dislocation. Rarely, patients can develop musculocutaneous nerve palsy
as a result of weight lifting, either from entrapment of the nerve
associated with hypertrophy of the biceps musculature or stretching and
compression of the nerve during repetitive biceps strengthening
exercises. More commonly, the musculocutaneous nerve can be injured
during shoulder surgery via a deltopectoral incision because retractors
are placed under the conjoined tendon to visualize the anterior aspect
of the glenohumeral joint. The nerve’s proximity puts it at risk for
injury. Entrapment of the lateral antebrachial cutaneous nerve
resulting in isolated sensory deficits has been reported in association
with racquet sports.
 |
|
Figure 21-8 Anatomy of the musculocutaneous nerve.
|
-
Patients with musculocutaneous nerve
dysfunction may present with weakness of elbow flexion and supination,
along with numbness of the radial aspect of the forearm.-
It is important to consider a biceps
tendon rupture, C5 to C6 cervical radiculopathy, or brachial plexus
injury in the differential diagnosis when evaluating patients with
symptoms suggesting injury to the musculocutaneous nerve.
-
-
After an acute event such as a shoulder
dislocation or anterior shoulder surgery, a patient with damage to the
musculocutaneous nerve may have weak elbow flexion and supination. -
It is possible that elbow flexion
strength deficits may be subtle, however, because of an intact
brachioradialis, which acts as a synergist, and that weakness of
supination may be the more predominant finding. -
Typically, there will be an absent biceps (C6) reflex and diminished sensation over the radial aspect of the forearm.
-
It is important to assess for diminished
sensation, altered reflexes, and weakness of other muscles around the
shoulder girdle and upper extremity that might suggest a broader injury
to the brachial plexus. -
In some patients, spontaneous recovery of
normal function can occur within hours after a musculocutaneous palsy
related to strenuous overuse.
-
Radiographs are indicated to assess for fractures or dislocations in the setting of traumatic injuries.
-
If dysfunction persists after 3 weeks of
symptoms, the primary diagnostic tool for evaluating musculocutaneous
nerve damage is the EMG/ NCS, looking for fibrillation potentials in
the biceps, positive waves, decreased voluntary motor unit action
potentials, and prolonged latency on nerve stimulation.
-
The treatment of musculocutaneous nerve
injury related to sports participation includes relative rest, with
gradual resumption of activities as symptoms resolve. -
Recovery may take several months, with
most patients regaining full function, although some atrophy and
sensory deficits may persist. -
For patients who show persistent weakness and EMG/NCS deficits after 3 months, surgical treatment should be considered.
-
Surgical options include neurolysis, primary nerve repair, and nerve grafting.
-
In the cases of injury related to trauma
or surgical procedures, surgical exploration led to 67% good results
after early nerve repair in a series of 85 patients.
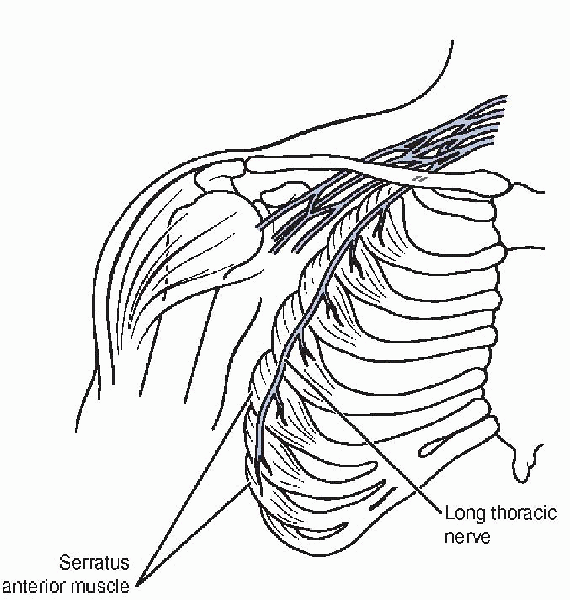
in a variety of sports, including volleyball, gymnastics, weight
lifting, hockey, and tennis.
immediately after they exit the intervertebral neuroforamina to form
the long thoracic nerve before it travels distally and laterally under
the clavicle and first rib. The nerve becomes more superficial as it
travels along the chest wall, where it innervates the serratus anterior
muscle. The serratus anterior arises from ribs 2 through 9, and inserts
on the medial (vertebral) border of the scapula (Fig. 21-9). The muscle helps to stabilize, protract, and elevate the scapula during shoulder motions.
from traumatic or nontraumatic causes. Because of the nerve’s
subcutaneous location, it is at risk of injury from a direct blow
during contact sports, or less commonly from direct pressure that can
occur when a patient lies on his or her side for a prolonged period of
time during a surgical procedure. Long thoracic nerve injury can occur
during various surgical procedures, including first rib resection for
thoracic outlet syndrome and axillary node dissection for breast
cancer. The nerve can also suffer repetitive microtrauma during
activities that cause traction on the nerve with overhead activities
such as volleyball, tennis, and baseball. The nontraumatic causes of
long thoracic nerve palsy include compression from adjacent bony and
soft-tissue structures as the nerve courses from the cervical spine to
the serratus anterior muscle. As discussed earlier in this chapter,
nerve compression can lead to ischemia of the microcirculation and
subsequent dysfunction. There have also been cases of long thoracic
nerve palsy after a viral illness and brachial neuritis.
 |
|
Figure 21-9 Anatomy of the long thoracic nerve and the serratus anterior muscle.
|
-
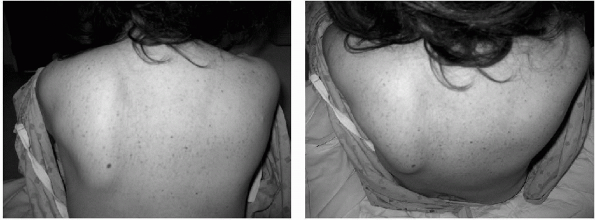
Patients with long thoracic nerve palsy
may present with diffuse complaints of aching pain in the shoulder,
neck, and scapular region, typically brought on by various overhead
activities. -
There may be some degree of weakness that can affect athletic performance such as throwing or tennis.
-
The athlete may notice deformity of the shoulder and back with efforts to lift the arm.
-
Patients typically do not complain of
numbness unless there is a more extensive process involved, such as
brachial neuritis, because the long thoracic nerve has no sensory
components -
The most obvious physical finding for patients with injury of the long thoracic nerve is scapular winging.
-
As the athlete attempts to forward flex the arm, the winging will typically become more pronounced (Fig. 21-10).
-
A wall push-up is a provocative maneuver that may exacerbate scapular winging.
-
-
Frequently, the patient may have loss of motion related to weakness of forward flexion and abduction of the shoulder.
-
As with many of the nerve injuries in
this chapter, the most useful diagnostic test is an EMG/NCS, which can
show the level and severity of the injury, as well as any recovery of
function. -
The test may also help differentiate
between other neurologic conditions, such as brachial neuritis or
spinal accessory nerve injury, which can also cause scapular winging. -
It may be reasonable to get plain
radiographs to look for any unusual bony abnormalities, such as a
cervical rib, which can cause compression of the nerve. -
More advanced imaging techniques such as MRI and CT are rarely indicated for this condition.
 |
|
Figure 21-10 Scapular winging.
|
-
In general, most patients with
dysfunction of the long thoracic nerve can be treated nonoperatively
because spontaneous recovery tends to occur over a period of 12 months
after the onset of symptoms. -
Patients should be restricted from the
causative sport and be referred for physical therapy to maintain range
of motion of the shoulder, along with strengthening exercises for the
scapular stabilizers and surrounding muscles that are trying to
compensate for the weakened serratus anterior. -
Some authors have attempted to stabilize the scapula with a special brace worn around the torso with limited success.
-
For patients whose symptoms or EMG
results do not improve after 1 to 2 years of nonoperative treatment,
surgery may be appropriate. -
The surgical options include pectoralis
major transfer, pectoralis minor transfer, rhomboid transfer, teres
minor transfer, scapulothoracic fusion, or scapular stabilization
without fusion. -
Several reports in the recent literature
present data on transfer of the sternal head of the pectoralis major,
augmented with autograft hamstrings, fascia lata, or allograft.-
The technique involves detaching the
sternal head portion of the pectoralis major from the humerus, creating
a longer construct by weaving an autograft hamstring, fascia lata or
allograft, and then passing the tendon through a hole created in the
inferior aspect of the scapula. -
Noerdlinger et al. reported that 75% of 15 patients in their study would undergo the procedure again.
-
Warner and Navarro reported satisfactory results in 7 of 8 patients using autogenous semitendinosus or gracilis augmentation.
-
In a series of 11 patients published by Connor et al., 91% of the patients were improved at an average follow-up of 41 months.
-
-
There have also been several articles
reporting successful treatment of scapular winging in a small series of
patients with neurolysis of the long thoracic nerve, or with nerve
transfer of the thoracodorsal or medial pectoral nerve to the long
thoracic nerve with favorable results.
nerve injuries around the shoulder associated with sports
participation. The spinal accessory nerve, cranial nerve 11, can also
affect function of the shoulder and upper extremity.
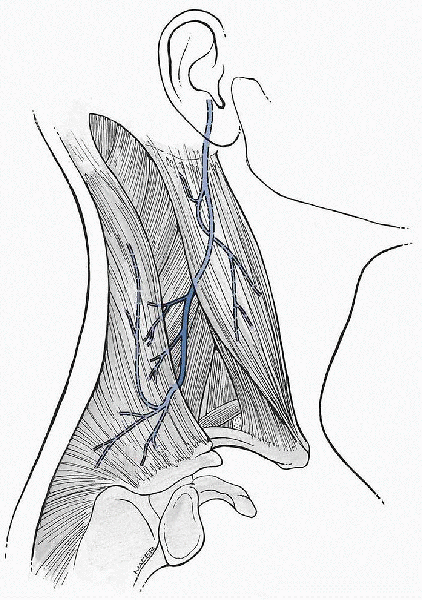
The nerve exits the base of the skull via the jugular foramen and
travels through the sternocleidomastoid muscle where it continues
subcutaneously along the floor of the posterior cervical triangle until
it reaches the trapezius. The trapezius is a large, broad muscle that
arises from the spinous processes of the neck, the upper and middle
back, and inserts along the spine of the scapula, the medial acromion
and the lateral clavicle. The muscle has three functional components:
(1) the upper portion elevates and laterally rotates the scapula, (2)
the middle portion stabilizes and retracts the scapula medially, and
(3) the lower portion depresses and downwardly rotates the scapula. As
the muscle facilitates scapular stabilization, elevation, and
depression, it is vital to the normal function of the shoulder and
upper extremity.
stick, or lacrosse stick. There have also been cases of spinal
accessory nerve palsy in patients wearing a shoulder sling for
prolonged periods of time. More commonly, injury occurs from
penetrating trauma, or during surgical procedures in the neck,
including lymph node biopsy, carotid endarterectomy, and tumor
resections. Weakness and scapular winging in the absence of trauma or
surgical intervention may suggest an underlying neurologic disease or
other process.
 |
|
Figure 21-11
Anatomy of the spinal accessory nerve. (From Agur AM, Dalley AF II. Grant’s Atlas of Anatomy, 11th ed. Philadelphia: Lippincott Williams & Wilkins, 2004.) |
-
An athlete suffering an injury to the spinal accessory nerve during sports may not experience any symptoms at first.
-
Subsequently, the patient may notice aching pain, along with weakness and difficulty lifting and abducting the arm.
-
Over time, the patient may notice drooping of the shoulder and loss of normal muscular contour.
-
-
Patients can develop pain secondary to
impingement of the rotator cuff, as well as pain from muscle spasm of
the levator scapula or rhomboids, which are working to compensate for
the trapezius dysfunction. -
As the shoulder droops, traction on the brachial plexus may cause discomfort.
-
Overhead athletes will generally experience diminished performance as a result of these previously described symptoms.
-
A patient with injury to the spinal
accessory nerve will typically have an abnormal contour of the shoulder
and neck related to atrophy of the trapezius muscle, the
sternocleidomastoid muscle, and associated drooping of the shoulder. -
When the athlete attempts to forward flex the shoulder, winging of the scapula may occur.
-
Typically, there will be weakness with
abduction and shrugging of the shoulder although, in some patients, a
strong levator scapulae can compensate somewhat. -
Shoulder range of motion should be assessed because patients can develop adhesive capsulitis.
-
The examination should conclude with a
thorough neurologic assessment of the entire extremity to rule out a
more involved process such as a brachial plexopathy or some other
neurologic condition.
-
As with most orthopaedic conditions, routine x-rays may be part of the patient evaluation.
-
Radiographs of the cervical spine, shoulder, and chest can be considered, with low expectation of any significant abnormalities.
-
-
Similarly, CT and MRI scans may offer
minimal information unless there is suspicion of cervical disc disease
or a neoplastic process. -
EMG/NCS will provide the most useful
information regarding the level of injury, the degree of involvement,
and any neurologic recovery that may occur.
-
Athletes suffering spinal accessory nerve palsy related to sports participation can generally be managed nonoperatively.
-
It may be appropriate to offer a sling initially for comfort, along with mild analgesics for pain.
-
A referral for physical therapy is
important to allow the patient to maintain shoulder range of motion, as
well as a strengthening program to focus on the surrounding musculature
to minimize drooping of the shoulder. -
Patients may benefit from modalities and transcutaneous nerve stimulation in an effort to alleviate pain symptoms.
-
There may also be a role for electrical muscle stimulation to help lessen muscle atrophy.
-
EMG/NCS should be repeated after several months to assess functional recovery.
-
If symptoms and strength do not improve
after 1 year, it is unlikely that continued nonoperative treatment will
offer any benefit. -
At that point, surgery should be considered in active patients.
-
-
Surgical treatment of spinal accessory nerve palsy consists of static or dynamic procedures to restore function.
-
Static procedures such as scapulothoracic
fusion or fasciodesis are designed to stabilize the scapula to the
chest wall or spinous processes, respectively. -
In a review article, Bigliani states that
the results of static procedures for spinal accessory palsy tend to
deteriorate with time as grafts stretch out.
-
-
Alternatively, several authors recommend dynamic procedures using local muscle transfers to mimic the function of the trapezius.
-
The “Eden-Lange procedure” involves
lateral transfer of the levator scapula, rhomboid minor, and rhomboid
major muscles, with each muscle substituting for various portions of
the dysfunctional trapezius.-
The Eden-Lange procedure originally
involved transfer of the levator scapula through the trapezius to the
lateral spine of the scapula, along with transfer of the rhomboid minor
and major to the infraspinatus fossa. -
The levator scapula mimics the upper
trapezius, the rhomboid minor, the middle trapezius, and the rhomboid
major the lower trapezius.
-
-
Bigliani has modified the procedure by
transferring the rhomboid minor to the supraspinatus fossa in an effort
to more closely reproduce the function of the middle trapezius.-
Together, the three muscles help to
restore mobility and the appearance of the shoulder girdle, although
return to sports is less predictable. -
As described by Bigliani, the technique
involves placing the patient in a lateral decubitus position, with an
incision between the spinous processes and the medial border of the
scapula. -
The trapezius is elevated off the
scapula, and the levator and two rhomboids are identified and detached
from the medial scapula border with a sliver of bone using an osteotome. -
The muscles are then mobilized toward the spinous processes to allow for advancement.
-
The next step in the procedure involves elevating the supraspinatus and infraspinatus from medial to lateral.
-
Drill holes are made in the supraspinatus and infraspinatus fossas 4 or 5 cm lateral to the medial border of the scapula.
-
The rhomboid minor is transferred to the
supraspinatus fossa, and the rhomboid minor is transferred to the
infraspinatus fossa, where they are sutured to the drill holes with
nonabsorbable sutures while maintaining the shoulder in 90 degrees of
abduction and the scapula in a reduced position. -
A second incision is then made along the spine of the scapula, medial to the posterolateral corner of the acromion.
-
The deltoid, trapezius, and supraspinatus
are elevated off the spine of the scapula, while protecting the
suprascapular nerve from injury. -
Drill holes are made in the scapular
spine 5 to 7 cm medial to the posterolateral corner of the acromion,
and the levator scapula is passed through the trapezius and sutured in
to place. -
Postoperatively, the patient is placed in an abduction brace for 4 weeks while undergoing rehabilitation.
-
-
E, Kurland LT, Mulder DW, et al. Brachial plexus neuropathy in the
population of Rochester, Minnesota, 1970-1981. Ann Neurol
1985;18:320-323.
LU, Compit CA, Duralde XA, et al. Transfer of the levator scapulae,
rhomboid major, and rhomboid minor for paralysis of the trapezius. J
Bone Joint Surg Am 1996;78:1534-1540.
PM, Yamaguchi K, Manifold SG, et al. Split pectoralis major transfer
for serratus anterior palsy. Clin Orthop Relat Res 1997; 341:134-142.
RR. Nerve anatomy and diagnostic principles. In: Pappas AM, ed. Upper
Extremity Injuries in the Athlete. New York: Churchill Livingstone,
1995:43-75.
MA, Cole BJ, Stewart M, et al. Results of pectoralis major transfer
with fascia lata autograft augmentation for scapula winging. J Shoulder
Elbow Surg 2002;345-350.
MR. Nerve injury about the shoulder in athletes. Part 1: suprascapular
and axillary nerve. Am J Sports Med 2004;32:3:803-819.
MR. Nerve injury about the shoulder in athletes. Part 2: long thoracic
nerve, spinal accessory nerve, burners/stingers, thoracic outlet
syndrome. Am J Sports Med 2004;32:1063-1076.
SP, Spinner RJ. Nerve problems about the shoulder. In: Rockwood CA,
Matsen FA, Wirth MA, et al., eds. The Shoulder. Philadelphia: WB
Saunders: 2004:1009-1031.
JP, Krushell RJ, Masquelet A, et al. Anatomy and relationships of the
suprascapular nerve: anatomical constraints to mobilization of the
supraspinatus and infraspinatus muscles in the management of massive
rotator cuff tears. J Bone Joint Surg Am 1992;74:36-45.
