Knee Injuries: Acute and Overuse
acute and overuse injuries occur, and they require different
investigative processes to diagnose and treat them properly.
-
Subdivision of clinical categories
-
Acute injury is an injury that happens
where a single application of force creates the musculoskeletal damage.
This is common in athletics, motor vehicle trauma, etc. -
Acute or chronic injury is an injury that
results in a disabled state that can be quiescent over time and result
in a new injury episode at a later time. This new injury would
represent an acute injury. However, this new injury did not depend on
abnormal forces creating the injury but rather the fact that there was
pre-existing damage to the musculoskeletal tissue. Common examples
might be recurrent patella instability or recurrent shoulder
subluxation. -
Overuse injury is an injury that is
characterized by the absence of an injury or at least no injury
significant enough to explain the current clinical situation. This kind
of injury results from repetitive submaximal or subclinical trauma that
results in macro- or microscopic damage to a structural unit and/or its
blood supply. This overuse pattern can be seen in all musculoskeletal
tissue but is most common in bone (overuse pattern resulting in stress
fracture), bursal tissues (overuse pattern resulting in bursitis), and
tendon (overuse pattern resulting in tendonosis).
-
-
Clinical correlation. The clinical approach to a knee injury (acute/chronic/overuse) depends on four cornerstones:
-
History
-
Physical examination
-
Tests and their interpretations
-
Treatment
-
-
History
-
Mechanism of injury.
This helps to identify potential structures that may have been damaged
by the application of force, either direct (contact) or indirect
(twisting mechanism). If the injury was a contact injury, one should
look for external signs at the point of force application and what
structures might have been injured as that force continues. For
instance, a blow to the anterior tibia might create upper tibial
bruising. This force creates a posterior displacement of the tibia on
the femur, potentially injuring the posterior cruciate ligament.
Non-contact injuries frequently involve rotatory twisting; the lower
limb remains fixed as the upper body twists around the knee. -
Was a pop heard or felt? A pop is frequently associated with tearing of a ligament, most commonly the anterior cruciate ligament, or a bone bruise.
-
Return to play.
The degree of pain and/or disability cannot be used as a reliable
indicator of the seriousness of an injury. However, continued play with
little or no impairment in performance diminishes the likelihood of a
serious knee injury. -
Has the joint been previously injured?
Frequently this question uncovers an acute on chronic injury. Two
common examples are recurrent kneecap dislocation and recurrent
subluxation after initial anterior cruciate ligament injury. -
Joint swelling.
Knee joint swelling within 12 hours after an injury is, by definition,
hemorrhage into the joint. An effusion that occurs after 12 hours
suggests synovial fluid accumulation due to reactive synovitis, often
due to cartilage or meniscus damage. (see 6.b below). -
The differential diagnosis of an acute knee hemarthrosis (1) (what inside the knee can bleed?) is:
-
Ligament injury.
The anterior cruciate ligament (ACL) and posterior cruciate ligament
(PCL) are intraarticular/extra-synovial structures. The superficial
medial collateral ligament (MCL) is an extraarticular structure.
However, the deep MCL is a thickening of the joint capsule and is
intraarticular. In a complete tearing of the MCL, both structures are
torn. The lateral collateral ligament (LCL) is an extraarticular
structure. It is rare that this ligament is torn in isolation. The most
common ligament torn in acute hemarthrosis is the ACL (approximately
70%) (2). -
Peripheral meniscus tear.
The outer, or peripheral, one third of the meniscus is vascular, and a
tear in this region results in a hemarthrosis. Meniscus tears in this
zone have the potential for healing and are repairable. Tears in the
inner two thirds of the meniscus are more often associated with
synovial irritation leading to a serous effusion that arises later
(e.g., 24–48 hours) after the initial injury. -
Fractures.
Any fracture that involves the joint surface results in a joint
hemarthrosis. In addition to obvious condylar/patellar fractures,
occult osteochondral fractures can be a source of hemarthrosis. These
can include avulsion fractures of the PCL and ACL (more common in
developing adolescents) and fractures secondary to patella dislocation. -
Synovial/capsular tears.
Patella dislocations, even in the absence of fractures, are a source of
hemarthrosis as the medial patellofemoral ligament and medial
retinacular restraints are torn. Also, a significant contusion without
a frank fracture or ligament/meniscus injury can create synovial
bleeding. This is often considered a diagnosis of exclusion.
-
P.340 -
-
Physical Examination
-
Inspection
-
Swelling. The
absence of notable intraarticular swelling does not signify a less
severe injury. Severe ligament disruptions are associated with large
capsular disruptions, and fluid typically escapes into the surrounding
tissue. The absence of knee swelling may indicate an extraarticular
source of pain. -
Localized bruises and abrasions.
These can be useful to identify the point of application of force in a
contact injury. These can indicate the direction of the force, which
helps to indicate what structures may be injured.
-
-
Palpation
-
Direct palpation
of the injured area corresponds to the anatomic structure underneath
that area. This is most useful for diagnosis when surface anatomy is
directly correlated such as iliotibial band tendonosis and patella
tendonosis. Direct palpation of meniscal, patellofemoral, and MCL
structures can be useful in distinguishing a differential diagnosis.
The cruciate ligaments do not have a palpable attachment to the
capsule, and, therefore, direct palpation of these structures is not
possible. However, injury to the ACL is associated with anterolateral
subluxation of the tibia on the femur and, therefore, anterolateral
joint line tenderness is common. -
Patella subluxation/dislocation.
This is associated with tenderness along the patella retinaculum,
especially at the medial epicondyle where the medial patellofemoral
ligament (MPFL) inserts and/or along the superior medial portion of the
patella. Note that although the patella dislocates laterally, it is the
medial based structures that are injured and thus are painful when
palpated.
-
-
Range of motion.
This is best assessed with the patient in the supine position. When the
knee has an effusion, the knee’s resting position prefers approximately
30 degrees of flexion (where potential capsular distention is largest).
Full extension and full flexion should be compared to the opposite
side, presuming
P.341
that
side is normal. If the opposite side knee hyperextends, then an injured
knee that goes just to zero would be considered lacking full extension.-
A locked knee
is defined as the inability to obtain full passive motion of the joint
secondary to a mechanical block. This does not mean that the knee is in
one position, but rather that there is an inability to obtain full
motion. Common causes are a displaced meniscus tear or loose body. -
A pseudo locked knee
is defined as the inability to obtain full range of motion secondary to
pain or intraarticular knee swelling. A torn meniscus without
displacement can result in pain at the limits of flexion and/or
extension. If the patient’s knee “locks” in full extension and doesn’t
want to bend, the most common reason is an injury to the extensor
mechanism, resulting in pain when the patient attempts to engage the
kneecap in the trochlear groove. -
Active range of motion
assesses the integrity of the motor units surrounding a joint. Even in
a severely injured knee, the patient typically retains the ability to
lift his or her leg. Therefore, active straight leg raising and range
of motion should be assessed. Frequently missed acute knee injuries are
disruptions of the extensor mechanism, which include quadriceps tendon
and patella tendon injuries. In this instance, the patient will
generally be incapable of a straight leg raise.
-
-
Stability testing. The sine qua non of a ligament disruption is the presence of pathologic joint motion.
-
Straight plain instabilities
are the easiest instabilities to test on a knee. This represents the
ability to move the tibia away from the femur in four known planes.-
Medial instability is associated with injury to medial or tibial collateral ligament
-
Lateral instability is associated with injury to lateral or fibular collateral ligament
-
Anterior instability is associated with injury to ACL
-
Posterior instability is associated with injury to PCL
-
-
Rotary instabilities. This refers to the rotation of the tibia around its vertical or longitudinal axis (Fig. 24-1).
-
Anterolateral instability is associated with ACL injury
-
Posterolateral instability
is associated with structures of the posterolateral corner of the knee
(LCL, popliteal fibular ligament, popliteus tendon). These are
frequently associated with PCL and/or ACL injuries. -
Posteromedial injuries. These injuries are rare and are commonly associated with PCL injury with or without MCL injury.
-
Anteromedial injuries are associated with ACL/MCL injuries
-
-
Extensor mechanism instability
-
Apprehension sign.
Passive lateral movement of the patella causing pain and/or quadriceps
contraction is suggestive of patellofemoral subluxation/dislocation.
This maneuver is typically done with the leg in full extension,
quadriceps muscles relaxed. -
Straight leg-raising against gravity
confirms integrity of the extensor mechanism, including quadriceps
tendon, patella, and patella tendon. A “lag” sign represents the
difference between passive and active extension of the knee. A lag
signifies disruption and/or weakness of the extensor mechanism. -
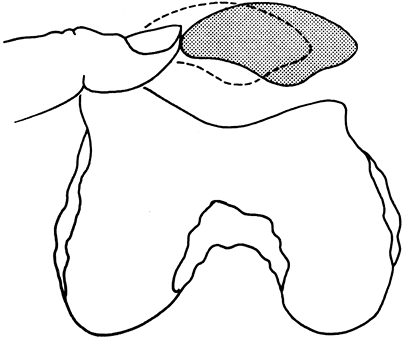
Medial/lateral patella restraints.
Stability testing of the patellofemoral joint involves assessing the
degree of passive patella motion in a medial and lateral direction of
the patella. This is typically measured against an imaginary midline of
the patella in the resting position (Fig. 24-2).
This maneuver tests the static restraints of the medial and lateral
extensor retinaculum complex. Any change from the patient’s “normal”
measured
P.342
against
their normal contralateral knee is suggestive of extensor mechanism
disruption. Most particularly, an increase in lateral patella motion
represents laxity or incompetence of the medial patella femoral
ligament and medial retinacular structures associated with past or
present patella dislocation.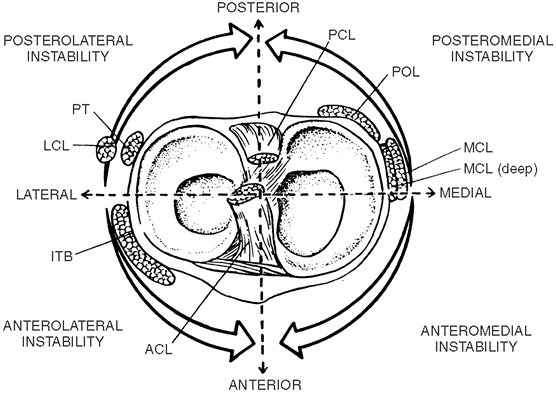 Figure 24-1.
Figure 24-1.
Rotatory instability of the knee. PCL, posterior cruciate ligament;
POL, posterior oblique ligament; MCL, medial collateral ligament; ACL,
anterior cruciate ligament; ITB, iliotibial band; LCL, lateral
collateral ligament; PT, popliteal tendon. (From Arendt, EA. Assessment
of the athlete with a painful knee. In: Griffin, LY, ed. Rehabilitation of the injured knee, 2nd ed. St. Louis, MO: Mosby, 1990, with permission.)
-
-
-
-
Tests and their interpretation
-
Plain radiographs
-
Anterior/posterior view.
The primary utility of this view is to rule out diagnoses and assess
overall tibiofemoral alignment. Standing views are preferred as they
best assess tibial-femoral joint space. If pain/swelling limits full
extension and/or full weight bearing, supine views are performed but
provide less information. -
Lateral view
evaluates the caudad/cephalad position of the kneecap. Patella alta, or
increase in the cephalad position of the kneecap, suggests a patella
tendon injury, especially when the injured side’s kneecap is higher
than the opposite side. Avulsion fractures, especially those of the
PCL, are typically visualized along the posterior aspect of the tibia
in this view. -
Axial view
evaluates the position of the patella in its relationship to the
femoral trochlear groove. Oftentimes, osteochondral fragmentation
following a patella dislocation can be visualized on this view.
Typically, one would see fragmentation of the medial patella facet
and/or lateral femoral condyle in an acute patella dislocation (Fig. 24-3). Different axial views have been established (Laurin’s, Merchant’s) (3).
The clinician should become familiar with one technique. Axial views
are a must for complete evaluation of all acute knee injuries.![]() Figure 24-2.
Figure 24-2.
Demonstrates one quadrant medial “glide.” The patella is divided
visually into four quadrants. Holding the patella between the
examiner’s thumb and index finger, the limits of medial and lateral
motion are assessed and recorded as “quadrants” of motion. (From
Halbrecht JL, Jackson DW. Acute dislocation of the patella. In: Fox JM,
Pizzo WD, eds. The patellofemoral joint. New York: McGraw-Hill, 1993, with permission.) -
Notch or tunnel view
is most useful for evaluation of avulsion fractures of the tibia,
osteochondritis dissecans, and loose bodies. This view is not standard
for an acute knee injury.
P.343 -
-
Magnetic resonance imaging (MRI)
for the knee. MRI has its largest application in evaluating meniscus
and cruciate ligament injury. The overall accuracy is greater than 90% (4).
An MRI is typically an adjunct test in the evaluation of an acutely
injured knee. It should be performed only if it will alter the
treatment protocol and is typically ordered by the physician who will
be giving definitive treatment. It should never be used in the absence
of a thorough and knowledgeable history and physical examination.
P.344
Posterolateral knee structures are not well visualized in the standard knee MRI views. Figure 24-3. Three types of fractures associated with patella dislocation. A: osteochondral fracture of the medial patella facet. B: osteochondral fracture of the lateral femoral condylar. C:
Figure 24-3. Three types of fractures associated with patella dislocation. A: osteochondral fracture of the medial patella facet. B: osteochondral fracture of the lateral femoral condylar. C:
Avulsion fragment of medial patella femoral ligament off medial
epicondyle (osseous-nonarticular). (From Halbrecht JL, Jackson DW.
Acute dislocation of the patella. In: Fox JM, Pizzo WD, eds. The patellofemoral joint. New York: McGraw-Hill, 1993, with permission.) -
TcMDP bone
scans are most useful in occult infections and to rule out stress
fractures. Their usefulness in diagnosing reflex sympathetic dystrophy
is variable. This is not a common diagnostic test ordered for acute
knee injuries. -
Computerized tomography (CT)
has few specific applications for routine imaging of acute knee
injuries. It continues to have utility for evaluating complex fractures
around the knee, especially those involving articular surfaces. When
used with contrast, it can be useful to evaluate the cartilage
integrity of osteochondral defects such as osteochondritis dissecans. -
Stress radiographs
can be utilized to document ligamentous disruption of the knee but are
infrequently performed. Stress radiographs can be useful to help
evaluate the stability of a fracture through the growth plate,
typically used within a surgical setting. Stress views of the knee are
recommended to evaluate the degree of PCL laxity, most often used in
the subacute or chronic setting.
-
-
General treatment
-
Joint aspiration
is rarely used to help with evaluation of an acute knee injury. It is
classically taught that fat dropules in a bloody aspirate helps to
diagnose a fracture through bone. When a tense effusion is present, an
aspiration can be therapeutic. Aspiration continues to be used when a
non-traumatic effusion is present and to rule out infection,
rheumatological diseases, especially crystalline deposit diseases such
as gout and pseudogout, and rarely synovial based tumors such as
pigmented villonodular synovitis. Aspirations for non-traumatic
effusions are usually complex with blood workup including complete
blood count (CBC) with differential, erythrocyte sedimentation rate
(ESR), C-reative protein (CRP), rheumatoid factor (RF), flourescent
antinucclear antibody test (FANA), and Lyme’s titer. -
Immobilization/crutches.
This is the safest way to protect an injured knee until a repeat
examination or a definitive diagnosis and/or treatment can be initiated
by the same or a referral physician. However, if no
significant/unstable fracture is present, removal of the brace to
perform gentle range-of-motion exercise is useful to help resolve an
effusion. Partial weight bearing, depending on the patient’s comfort
level and the working diagnosis can also be therapeutic and is
encouraged. A knee immobilizer may be indicated for the acute knee
injury when the patient’s knee is unstable or the pain is severe with
passive flexion. It is crucial to advise re-evaluation within a few
days as prolonged immobilization can precipitate atrophy and may turn a
small, self-limiting injury into a chronic problem. -
Reduction of swelling.
Strategies to reduce swelling should be included in the initial
treatment recommendation. These include ice, gentle passive or active
assisted range of motion, elevation, and compression. -
Repeat examination
is helpful in establishing a more firm diagnosis, especially when pain,
swelling, and/or apprehension limit the initial examination. -
Antiinflammatory medication
is commonly used to control pain. The efficacy in the reduction of an
acute effusion or inflammation of injured tissues is debated.
Antiinflammatory medications also change the role of platelet function
and can theoretically increase bleeding of an injured site. It is
recommended that this class of medications be used only for analgesic
reasons and should be taken as a prn drug.
-
-
Fractures of the patella
-
Anatomic considerations.
The patella is a sesamoid bone that is contained within the extensor
mechanism. Its main function is to provide a lever arm for superior
mechanical functioning of the extensor mechanism and to help stabilize
the limb in deceleration. The strong quadriceps muscle complex is
attached to its superior pole. -
Common types of fractures
-
Vertical fractures
of the patella frequently are due to a direct injury; infrequently they
represent an overuse injury of the patella. When they are associated
with no or minimal displacement, they do not constitute a disruption of
the extensor mechanism and can be treated conservatively. -
Chip fractures
of the medial border are commonly seen with a patella dislocation;
infrequently, they can be associated with direct trauma. This variety
will be more thoroughly discussed under patella dislocation.
-
Treatment
-
Undisplaced or minimally displaced fractures
may be treated symptomatically without surgery. However, they must be
protected from further damage. Immobilization in a knee immobilizer for
2 to 4 weeks is sufficient, with weight bearing as tolerated.
Quadriceps isometric exercises can be performed during this time.
Gentle, passive range of motion as per the patient’s comfort level is
recommended. -
For displaced fractures
involving the articular surface, an anatomic reduction is essential.
Open reduction and internal fixation of the fragments with a tension
band wire or lag screw is the treatment of choice (5). -
Comminuted fractures
require surgical treatment. A patellectomy is necessary if the entire
patella cannot be internally fixed to gain stability. If more than half
of the patella remains intact, then the comminuted pieces may be
excised and the tendon sutured just above the subchondral bone into the
remaining pole of the patella. Occasionally, fragments are large enough
to fix with tension band wiring or 2.7-mm cortical lag screws (5). -
If an osteochondral fracture
is suspected, an arthroscopy to inspect the joint and remove small
fragments of bone and cartilage may be of benefit. This is often the
result of a patella dislocation and will be more thoroughly discussed
below. At times, typically due to direct trauma, a large osteochondral
fragment can be present. If the chondral fragment has an osseous layer,
open or arthroscopic fixation should be attempted. This might be most
readily accomplished by using bioabsorbable implants. Cartilage
injuries are ominous for the future health of the joint; their
treatment is beyond the scope of this text (6,7). -
Postoperative treatment
must be individualized according to the type of fracture and the
security of the repair. Most knees are initially placed in a
compressive dressing with a posterior splint or knee immobilizer. If
rigid internal fixation is achieved and the patient is trustworthy,
early protective passive range of motion is initiated, progressing to
active motion. Typically, 6 weeks of some form of immobilization is
necessary for healing of the fracture(s). Quadricep muscle strength
within the limits of the allowed knee motion should be encouraged
throughout this time. -
The prognosis
of patella fractures depends on the degree of articular damage and the
ability to re-establish quadricep strength. Both are necessary for full
recovery of the extensor mechanism complex. If articular damage is
minimal, and good extensor mechanism strength can be restored, the
prognosis of patella fractures is excellent.
-
-
-
Patella dislocations
-
Mechanism of injury.
This injury can result from a direct blow but is more commonly
associated with a non-contact twisting injury involving an externally
rotated tibia combined with a forceful quadriceps contraction. The
patella is dislocated laterally which disrupts the medial retinaculum.
Spontaneous reduction frequently occurs when the patient instinctively
tries to straighten his or her leg. When the patella relocates,
osteochondral fragments can occur as the medial patella facet abuts the
lateral femoral condyle. These two areas, in particular, should be
scrutinized for osteochondral damage (see Fig. 24-3).P.346Medial patellar dislocations
are rare in knees which have not had previous surgery. It is most often
associated with iatrogenic causes, in particular a lateral retinacular
release (8). -
Physical examination.
The patient will invariably have medial retinacular tenderness,
especially at the medial femoral condylar region. If an attempt is made
to displace the patella laterally, the patient resists this (patella
apprehension test). A straight leg raising effort should be requested.
The patient should be able to lift the leg, although he or she will
report pain with this maneuver. This is frequently associated with
minimal extension lag (the difference between passive and active
extension). -
Radiographs.
An axial view is necessary for a complete evaluation of patellofemoral
or extensor mechanism injury. If the patient is seen prior to
spontaneous reduction of the patella, axial views will reveal the
dislocated patella. Once reduced, the axial view may reveal any
residual tilt and/or subluxation as well as the presence of
osteochondral fragmentation. Axial views taken in lower degrees of
flexion (Laurin’s 20-degree views or Merchant’s 30-degree views) will
be more likely to show minor degrees of continued subluxation (9,10,11,12,13,14).-
If the patella remains dislocated,
then a reduction should be performed without delay to relieve pain.
Achieve intravenous analgesia with morphine sulfate and a hypnotic
before reduction is attempted. Once the patient’s muscles are relaxed,
the knee is placed in full extension and the patella is reduced into
place by a gentle, medially directed pressure. Slight elevation of the
medial border of the patella during this maneuver is ideal. On occasion
the kneecap can be “trapped” by the condyle, and reduction can be
difficult. After appropriate prep of the skin, grabbing the kneecap
with a large towel clip and using it to gently unlever the kneecap can
be a useful maneuver for difficult reductions. Due to large hematomas
frequently associated with patella dislocations, and the fact that
there is a large retinacular tear medially, the use of local
intraarticular injections is not favored. General or regional block
anesthetic is rarely required. -
If a large associated hemathrosis is present, aspiration is suggested as this can be therapeutic in relieving pain.
-
There is no consensus in surgical treatment
for patella dislocations. There is universal agreement that, if it is
associated with radiographic osteochondral fragmentation, an
arthroscopy with irrigation and debridement or fracture repair is
advisable. Whether surgical repair of the injured retinacular
structures is necessary and/or whether it produces superior functional
outcome is unclear (12). -
When acute surgical repair is performed, it is directed at the medial retinacular structures, in particular the MPFL (12). Classically, this may also involve a lateral retinacular release and/or a medial transfer of the tibial tubercle (13), though these additional surgical procedures continue to be debated (13).
-
If there is no evidence of a fracture or continued radiographic subluxation/tilt, non-operative treatment
can be elected. Non-surgical treatment is directed at providing an
environment where the patella does not dislocate. Typically, the
patient should be treated initially with crutches and a knee sleeve,
encouraging gentle motion. In the presence of a significant
hemarthrosis, a compression dressing and immobilization in extension is
appropriate until early motion is comfortable. The knee sleeve is used
for 4 to 6 weeks while an aggressive quadriceps rehabilitation program
is pursued. Typically 6 weeks of monitored activities, keeping the knee
out of pivoting and twisting activities, is recommended. The most
important thing to accomplish in the first 6 weeks post-injury is
return of normal quadriceps strength. Return to full functional
activities should be based on functional strength rather than a
specific time period from the original injury (13).
-
-
Complications
-
Recurrent dislocation.
The main physical examination feature associated with recurrent
dislocation is continued quadriceps weakness. Recurrent dislocators
that have successfully accomplished strength comparable to their other
side will likely need surgical reconstruction to stabilize their
patella. Recurrent patella dislocations are frequently associated with
recurrent effusions at the time that the patient dislocates; a history
that “my knee gives out” following an initial patella dislocation may
represent quad weakness and not necessarily a re-dislocation. -
Degenerative joint changes
of the patellofemoral joint may occur when significant cartilage trauma
is present from the initial/recurrent patella subluxations.
-
P.347 -
-
Meniscus injuries about the knee
-
Anatomic concerns.
Menisci are C-shaped structures that rest on the medial and lateral
sides of the tibial plateau, whose main function is shock absorbency of
the tibial–femoral knee articulation. Because their outer perimeter is
thicker than their inner rim, some stability is afforded by their
anatomic construct as well. This added stability is most important when
cruciate ligament laxity is present. -
Mechanism of injury.
Most isolated injuries of the meniscus (not associated with ligamentous
injuries) occur with a rotatory stress on a weight-bearing knee.
Isolated meniscal injuries occur from trapping of the meniscus between
the femoral condyle and the tibia while the knee is weight bearing,
typically in flexion. A history of locking or clicking is helpful, but
it is frequently misleading.In a young patient (typically under age 30), significant
trauma is necessary to injure a meniscus. However, in the older knee, a
degenerative tear can occur from repetitive day-to-day activities. -
Physical examination
-
Joint line tenderness is typically
present along the medial (medial meniscus tear) or lateral (lateral
meniscus tear) joint lines. This joint line pain increases with
attempts at full extension or full flexion. -
The McMurray test.
An audible, palpable, and often painful clunk is produced when the knee
is extended from the full flexed position while the tibia is forcefully
externally rotated (medial meniscus) or internally rotated (lateral
meniscus). This sign is associated with a torn meniscus. Crepitus or
pain along the joint line and when this maneuver is performed, even in
the absence of an audible clunk, are also suggestive of a
medial/lateral meniscus tear. The reliability of this test is low,
though it is classically discussed in most textbooks (14). -
The presence of an effusion
is frequent in a meniscus tear. Typically the normal knee has less than
15 mL of fluid and is not detectable on physical examination. Small
amounts of fluid can be detected by “milking” the suprapatellar pouch,
looking for a fluid wave as one tries to push the fluid from the
lateral side of the knee to the medial side of the knee. This maneuver
is the best way to detect small amounts of swelling.The presence of an effusion limits complete extension of
the joint and may be a cause of a lack of full extension and /or
flexion.
-
-
Radiographs
-
A meniscus tear is not seen on plain x-ray.
However, in an older patient, medial or lateral joint space narrowing,
best seen on standing films, may give some indication as to the
likelihood of a degenerative meniscus tear. -
An MRI is
frequently requested to confirm the presence of a meniscus tear. The
MRI has high accuracy in diagnosing a meniscus tear (greater than 93%) (15,16).
-
-
Treatment
-
An isolated meniscus tear
in the repairable zone in a young person should generally be repaired.
The re-tear rate of a meniscus repair in a stable knee (not associated
with a ligamentous tear) has a higher re-tear rate
P.348
than
those meniscus tears associated with ligamentous instability when both
meniscus and ligament injuries are surgically treated (17). -
A symptomatic meniscus tear in the non-repairable zone
and/or a complex meniscus tear that persists despite conservative
management should be arthroscopically debrided. However, in the older
age group, consideration must be given to the fact that the symptoms
may be the result of osteoarthritis and cartilage wear and not from the
meniscal tear. -
In the older age group,
where one suspects a degenerative meniscus tear, the meniscus tear is a
reflection of generalized early arthritis of the knee joint. This
“tear” should be treated symptomatically according to the patient and
physician’s discussion. The presence of a degenerative meniscus tear on
MRI is not an indication to treat. If the symptoms associated with a
degenerative meniscus tear can be quieted down with rest, relative
rest, and/or medication, surgical treatment may not be necessary (18).
-
-
-
Ligamentous injuries of the knee
-
Anatomic considerations.
The cruciate ligaments are intraarticular/extra-synovial structures.
When the cruciate ligaments are torn they can create a hemarthrosis or
bleed into the joint. The LCL and superficial MCL are extraarticular
structures. The deep MCL is a thickening of the joint capsule and thus
is intraarticular. -
Mechanism of injury
-
Ligamentous injuries
can be the result of a direct or indirect trauma. Indirect trauma
frequently occurs when the body rotates around a relatively fixed
foot/leg. Direct injuries are a consequence of force directed to the
knee or limb. Typically, the ligament opposite the area of contact is
the ligament which is the most vulnerable. For instance, a blow to the
lateral side of the knee places the MCL most under stress for injury.
Straight plain instabilities (anterior, posterior, medial, lateral) are
most readily assessable by direct physical exam. Rotatory instability
of the knee (anterior lateral and posterior lateral) requires more
sophisticated physical exam skills. -
In an isolated tear of the MCL,
palpable discomfort can be detected anywhere along the ligament from
its origin on the medial femoral condyle to its insertion on the tibia
(approximately three finger breadths below the joint line). The deep
capsular ligament is a thickening at the joint line. Medial joint line
tenderness is also associated with MCL injuries. However, different
from a meniscal injury, an MCL injury would create pain to stressing
the knee in a valgus direction, as well as externally rotating the leg
with the knee flexed. Although attached to the medial meniscus, the
incidence of an in-substance medical meniscus tears in an isolated tear
of the MCL is low (19). -
Isolated injuries of the LCL
are rare. Frequently accompanying complete tears of the LCL are tears
of the posterolateral complex with or without cruciate involvement. If
one suspects a lateral/posterior lateral injury, physical examination
must include close inspection of peroneal nerve function distally in
the leg and foot region. Complete (grade 3) injuries to the
posterolateral region of the knee do not heal, and superior results are
present if the injury is addressed in the acute phase (with repair of
structures) rather than the chronic phase of this injury. Any increase
in external rotation of the tibia with the femur fixed that is
increased over the patient’s opposite uninjured knee should be suspect
for a posterolateral knee injury. This needs to be evaluated within
days of the injury by a surgeon competent in treatment of
multi-ligamentous injuries of the knee. -
Isolated tears of the PCL
are frequently associated with a hyperextension injury (indirect
injury) or a blunt contusion to the front of the tibia (direct injury). -
Isolated ACL injuries
can be sustained through a number of mechanisms, most commonly a
non-contact deceleration injury or landing from a jump. The potential
causal mechanisms in non-contact ACL injuries have been
P.349
the subject of intense research in the last decade (20).
Recent interventional studies suggest that neuromuscular training in
improving bent knee landing and pivoting can be helpful in injury
reduction (21).
-
-
Physical examination.
The amount of joint line opening or motion between the tibia and femur
that occurs with manual testing is graded according to American Medical
Association (AMA) guidelines (4): grade 1
injuries would be less than 5 mm of joint line opening; grade 2 are 5
to 10 mm; and grade 3 injuries (complete tear) are more than 10 mm of
opening (13).-
The main clinical motion test
for providing an analysis of the severity of MCL complex injuries is a
valgus stress test with the knee flexed at 30 degrees. The leg is put
over the side of the examining table, the fingers are placed on the
medial joint line to assess the amount of joint line opening and
rotation, and a valgus stress is applied to the knee. The reverse of
this, placing a varus stress on the knee, is the main clinical motion
test to analyze LCL instability. -
Typically injuries to the LCL also involve injury to the posterolateral complex.
Motion tests to determine the amount of injury to the posterior lateral
complex of the knee are the most complex of all knee exams. It is
beyond the scope of this text (22). -
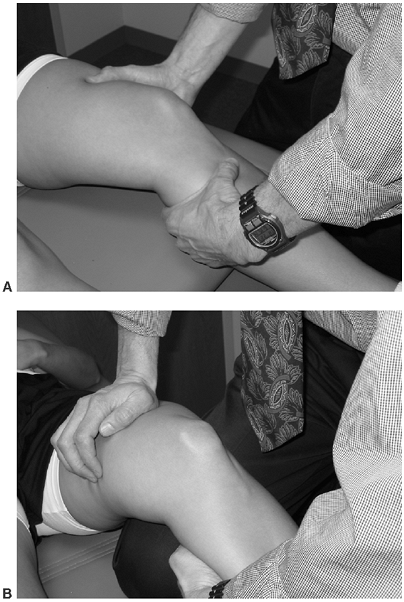
The main clinical motion test for an analysis of ACL injuries is the Lachman’s test (23) (Fig. 24-4).
This is performed with the knee in approximately 20 degrees of flexion,
with the leg in neutral rotation. The examiner holds firmly the distal
femur in one hand and the proximal tibia in the other hand, then one
places an anterior-directed force on the proximal tibia. Grading of
displacement of the tibia on the femur is along the AMA guidelines. In
addition to the Lachman’s exam, ACL injuries are associated with
anterior lateral rotatory tibial subluxation that is best evaluated
through the pivot shift maneuver or Losee maneuver (24).
The anterior drawer test (done at 90 degrees of knee flexion), though
historically cited, is not as reliable as the manual test for laxity of
the ACL (14). -
The main clinical motion test to detect injuries of the PCL is the posterior drawer test.
This is performed by placing the knee at 70 to 90 degrees of flexion. A
posterior force is applied to the tibia and the extent of translation
and the quality of the endpoint is recorded. Again, AMA guidelines are
used to assess the degree of translation. The key to this test is
accurately assessing the starting point of the tibia (25).Another useful test in assessing PCL laxity in an awake
patient is the “quads active” test: With the knee at 70 to 90 degrees
of flexion, the patient is asked to activate his or her quads with the
examiner holding the tibia in the position in which the tibia comes to
rest. Posterior motion from this starting point is then assessed. -
An acute knee examination should include all major ligamentous structures
within the knee. Significant anterior-posterior translation (>10 mm)
with the drawer or Lachman’s test may suggest an injury to both the ACL
and the PCL. Varus and valgus stress testing should be performed both
at 0 and 30 degrees of knee flexion. Asymmetry in varus or valgus
laxity that exists at 0 degrees of knee extension suggests a posterior
cruciate/posterior capsular injury as well as collateral ligament
injury. Varus or valgus asymmetry laxity existing at 30 degrees of
flexion but not at 0 degrees is indicative of at least an injury to a
collateral ligament.
-
-
Treatment
-
Isolated tears of ligamentous injuries
-
MCL. Isolated tears of the MCL can be treated conservatively (19,26).
For complete tears, progressive weight bearing on crutches, in a brace
limiting valgus stress for 4 to 6 weeks is recommended. In the absence
of a complete tear of the MCL, one can bear weight as pain and motion
permits. Complete recovery after isolated MCL injuries is the norm,
though distal MCL tears typically have more disability and take longer
to heal (26).![]() Figure 24-4.
Figure 24-4.
Lachman’s exam of the knee: This is a test for deciding the degree of
anterior translation of the tibia under the femur. The knee is held
firmly in place at 20 to 30 degrees of flexion by the examiner’s hand (A) or by resting the patient’s leg over the examiner’s knee (B).
With a firm hold of the proximal tibia, the examiner places an upward
or anteriorly directed force on the tibia, judging both the distance of
translation and the firmness of the endpoint. -
Isolated tears of the PCL
are frequently treated non-operatively. In the rehabilitation process,
special emphasis on quad strength is important to maintain a muscular
support to limit posterior displacement of the tibia. -
Isolated tears of the ACL
are prone to subluxation events when jumping and pivoting activities
are performed. In young active patients, or middle-aged patients that
have a high demand job or recreational aspirations, ACL reconstruction
is typically advised. The goal of ACL reconstruction is to prevent
future subluxation events which can be associated with meniscus and/or
cartilage damage. -
Multi-ligamentous knee injuries
most commonly involve the ACL/MCL or PCL with posterolateral injuries.
An operative treatment yields the best functional results in two
complete ligament knee injuries.
P.350P.351 -
-
-
-
Knee dislocations
-
Evaluation and treatment.
This relatively rare dislocation requires immediate reduction and
evaluation for joint stability. Reduction under anesthesia is sometimes
necessary (27,28).
Immediate and continuous evaluation of vascular status of the leg
reduction is important. If there is any question of the vascular
supply, most specifically if pulses are diminished or absent in the
affected limb, an arteriography must be performed immediately.
Prophylactic fasciotomy should be considered to prevent a compartment
syndrome following vascular repair, particularly if there is greater
than 6 hours from injury to vascular repair. If a vascular repair is
present combined with severe knee instability, an external fixator may
be applied to protect the vascular construct until definitive surgical
treatment of the torn ligaments ensues. -
Early reconstruction of torn ligaments offers the best outcomes (28).
If the injury is associated with a vascular repair and/or significant
disruption to the skin, a subacute reconstruction is indicated (0–3
weeks). Late surgical approach (more than 4 weeks) is more difficult
secondary to soft tissue scarring, particularly if it involves a
posterolateral corner, where individual structures can become more
difficult to dissect. In dislocated knees that are approached late
(more than 6 weeks), reconstructive efforts aimed at collateral
ligament injuries are frequently necessary (in deference to a primary
repair if done early). The cruciate ligament injuries are frequently
reconstructed in acute and late surgeries in deference to a repair.
Because of the typically severe nature of these injuries, allograft
tissue in deference to autograft tissue from the same or contralateral
knee is the norm.If the original injury has adequate joint surfaces and a
competent vascular system, functional use of the leg will parallel the
ability to get back satisfactory strength and motion. Acceptable
function for day-to-day activities is common following these injuries.
The ability to perform high-level activities following knee
dislocations is rare.
-
-
Extensor mechanism disruptions
-
Anatomic considerations.
The extensor mechanism consists of the quadriceps muscle complex,
quadriceps tendon, patella, patella tendon, and patella tendon
insertion into the tibial tubercle. Disruption of the extensor
mechanism along any one of its parts can result in failure of the
patient to perform a straight leg raising effort. A partial tear
frequently results in the patient’s ability to lift his or her leg, but
with a considerable lag (difference between passive and active
extension of the leg). -
Clinical considerations.
A quadricep tendon disruption is difficult to assess on physical
examination unless one requests a straight leg raising effort by the
patient. Quadricep tendon ruptures are a frequently missed cause of
acute knee injuries.Patella tendon disruptions
are often associated with an indirect trauma consisting of a forceful
quadriceps contraction against a relatively fixed lower limb. These can
be subtle injuries.If the rupture is below the inferior border of the
patella (i.e., in the patella tendon or at the tibial tubercle),
patella alta would be present, best seen on lateral knee x-rays.Extensor mechanism disruptions commonly occur in
patients with systemic illness such as diabetes or renal failure, or
with use of exogenous steroids (prednisone or anabolic steroids).
Cortical steroid injections for treatment of patella tendinosis has
been associated with an increased incidence of rupture. -
Treatment. The goal of treatment is to restore a functioning extensor mechanism to the knee. This is best accomplished surgically.
-
-
Physeal injuries. One cause of an acute knee injury in a growing adolescent is an injury to the physis.
-
A distal femur physeal injury,
particularly if it is a non-displaced injury, can be confused with a
collateral ligament injury. Pain is present, not only at the origin of
the collateral ligaments, but across the anterior aspect of the femur
or tibia, which is readily palpable in most children. X-rays can show
some widening and, at times, displacement of the physis. Stress x-rays
can confirm the diagnosis and assess the stability of the fracture
construct. Surgical reduction and stabilization for any displaced
physeal fracture is imperative. Stable injuries can be treated
non-operatively (29). -
The tibial apophysis
can avulse in the adolescent with closing growth plates. The tibial
growth plate fuses from posterior to anterior, and an avulsion of the
tibial tubercle frequently involves an interarticular fracture into the
joint. By history this injury is associated with a strong quadriceps
contraction; radiographically this injury is associated with patella
alta. Surgical reduction and fixation is advisable for the best outcome
when the tubercle is displaced.
-
-
Ligament avulsion.
Cruciate ligament avulsions, particularly the attachments of the ACL
and PCL onto the tibia, occur in the growing adolescent. When these are
associated with a large bony fragment, surgical reduction and fixation
is advised. The rehab will follow the course of a bone healing rather
than of a ligament reconstruction/revascularization. -
Osteochondritis dissecans
-
Definition.
Osteochondritis dissecans (OCD) is defined as an area of avascular bone
commonly presenting in the medial femoral condyle of a skeletally
immature child. The etiology of this area of avascularity is unknown.
Most commonly accepted theories are trauma, abnormal ossification
within the epiphysis, ischemia, or some combination of the above.
Approximately 40% of patients with OCD have a history of prior knee
trauma to a mild or moderate degree (21). The
medial condyle is involved 85% of the time versus 15% of the lateral
condyle. Fifty percent of loose bodies in the knee are associated with
OCD. -
Natural history.
The majority of juvenile lesions (presenting before closure of growth
plates) heal spontaneously. In the skeletally mature, there is a higher
incidence of bone fragmentation (subchondral fracture). This bone
collapse is in the area of the avascular bone and is felt to be because
of faulty lead transmission of bone just below the cartilage. In its
extreme form, the osteocartilaginous lesion can break away from the
healthy bone forming a loose body. Once there is a fracture of bone in
the area of avascularity, symptoms increase and the involved fragment
may become disengaged. -
Treatment
-
Juvenile osteochondral
lesions can generally be treated nonsurgically with rest or reduction
from high impact activities and repetitive deep knee bending. The goal
is to have the knee become pain free. The presence of an effusion is
indicative of possible disruption of the articular surface, signifying
the need for surgical evaluation. The patient and their family should
be informed to return to the doctor if recurrent effusions are present.
Following these patients in regular intervals (6–12 months) until
resolution of the lesion on x-ray is advised. -
Surgical treatment for adult OCD
(OCD after growth plate closure) is typically recommended. The type of
surgical treatment depends on the size and location of the OCD site and
the quality of the overlying cartilage. Options include drilling,
debridement, fixation, replacement, or excision. The discussion of this
is beyond the scope of this review (6).
-
-
-
Definition.
Repetitive submaximal or subclinical trauma that results in macro-
and/or microscopic damage to a tissue’s structural unit can result in
pain and/or dysfunction. Although clinicians refer to it as an “itis,”
an inflammatory response
P.353
is
not seen histologically. It is thought that damage to a tissue’s
structural unit and/or blood supply is a frequent cause of overuse
injuries.The most common form of overuse injury is from an
endogenous source, that being mechanical circumstances in which the
musculoskeletal tissue is subjected to greater tensile force or stress
than the tissue can effectively absorb. -
History.
Overuse injuries are characterized by the absence of an acute injury,
or at least no injury significant enough to explain the current
clinical situation. The most important feature to look for in the
patient’s history is a “change” in functional demand. A transitional
athlete/worker, defined as a person with a change in his or her
internal or external environment, is at high risk for development of
overuse injuries. These include:-
Change in intensity of repetitive activity (distance/time)
-
Change in frequency or duration of repetitive activity
-
Changes in equipment (footwear/surface changes including material composition and/or slope)
-
Changes in competitive climate/work climate/activity level
-
Changes in weather
-
Changes in lifestyle (puberty, aging, significant weight gain, and, for women, pregnancy and menopause)
-
-
Physical examination
-
Inspection
-
Alignment of
the limb is a must in evaluating any overuse injury of the lower
extremity. This includes tilt of the pelvis, rotation of the femur,
varus or valgus alignment of the knee, and pronation or supination at
the foot. Any change in “normal alignment” can cause tissue overload
anywhere along the kinetic chain. Some limb alignment features are
constitutional and cannot be changed short of surgery; others can be
modified. The two most common forms of modification are:-
An orthotic
may change the position of a flexible foot and thus can affect the
entire kinematic chain. Particularly, a flexible pronated foot can be
restored to normal alignment with the use of an orthotic. -
An anteriorly tilted pelvis is associated with increased internal femoral rotation and functional knee valgus. This can frequently be altered by appropriate hip abductor and extensor strengthening exercises (30).
-
-
Redness or warmth is not common in overuse injuries but may indicate the presence of an injured bursa or tendon.
-
Joint effusion is not common in overuse injuries. It indicates an intraarticular source of pathology.
-
-
-
Investigational tests
-
Strength tests. These can include:
-
Weakness compared to the contralateral limb
-
Concentric
(muscle shortens while contracting) muscle strength versus eccentric
(muscle lengthens while contracting) muscle strength in same muscle
group (see H.1.b). -
Agonist
(joint motion in one plane due to muscle contraction) versus antagonist
(the muscle group opposing or resisting joint motion caused by agonist
muscle) strength in same limb (i.e., quad to hamstring strength) -
Absolute strength and peak torque to body weight ratio compared to population norms
-
Endurance strength with a measure of muscle fatigability
-
-
Evaluation of flexibility, especially in key muscle groups, including quadriceps, hamstring, hip flexors, and Achilles tendon
-
-
Radiographs
-
Plain radiographs
are infrequently necessary for evaluation of overuse injuries.
Radiographic views of the patellofemoral joint, in particular axial
views, may be helpful to assess patella position. Standing knee views
show arthritic changes including bone spurs and joint space narrowing. -
MRI. The main
advantage of an MRI is its ability to view intra- versus extraarticular
pathology. Routine use of an MRI to diagnose overuse injuries is not
advantageous, although significant tendinosis and bursal edema can be
visualized by MRI.
P.354 -
-
Blood work
-
When there is a knee effusion that arises
spontaneously or is associated with other complaints (e.g., rash or
fatigue), then it is important to consider systemic diseases. Evaluate
for systemic disease, including collagen vascular disease and Lyme’s disease (see II.D.1).
-
-
Treatment
-
Reduce tissue irritation and pain with:
-
Analgesic non-narcotic medications [nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen]
-
Physical therapy modalities (ultrasound, e-stim, massage)
-
Rest or relative rest of the injured part (reduce activities, substitute activities, and protect the injured part)
-
Ice
-
Elevation and compression if swelling is present
-
-
Correct anatomical problems when possible (patella sleeves, orthotics, braces, rarely surgery).
-
Correct biomechanical errors
when possible (training sequence, sport style and form, strengthening
and stretching of musculoskeletal units, evaluation of workplace
station). -
Correct environmental concerns when possible (new shoes, change to a more absorbent surface, adequate clothing).
-
-
Sports-specific rehabilitation
-
Recovery of strength
-
Closed chain exercises
of the lower extremity are those exercises where the foot is supported
or planted during the exercise thus “closing the loop.” Leg press or
stand-up exercises such as partial squats are examples of closed chain
lower leg exercises. For lower extremity activities,
closed chained techniques are more functional and can obtain comparable
gains in quadriceps strength with less overuse of the patellofemoral
joint (30). -
Concentric/eccentric muscle strength. Concentric
muscle contractions occur when a muscle shortens as it contracts. In an
eccentric contraction, the muscle lengthens as contraction occurs.Eccentric strengthening has
long been favored for recovery of strength in the treatment of
tendinosis. For the patellofemoral joint, eccentric muscle activity is
an important part of functional use of the joint. Eccentric strength is
the main decelerator of the body, an important function of the
quadriceps complex.
-
-
-
The physician.
The physician’s role in diagnosing overuse injuries is to render an
injury with its appropriate treatment as well as educating the patient.
Patient education is the best treatment for the prevention of overuse
injuries in the future. -
The patient.
The patient’s role is to understand the causative factors in the injury
and to understand the progression from injury to wellness. This
includes activity modifications and their role in modifying their
activities. The patient needs to implement a paced return to full
activities.
-
Patella tendonosis
-
Patella tendonosis is a common overuse
injury that more typically affects the proximal attachment of the
patella ligament to the inferior pole of the patella, but can also
affect the distal end of the tendon. It is also called a jumper’s knee
because it occurs most frequently in athletes who require repetitive
eccentric quadricep contractions, as is common in jumping athletes, and
athletes who frequent heavy weight training. -
The case of patella tendonosis is generally considered to be chronic stress overload resulting in microscopic tears of the tendon with incomplete healing.
-
Treatment is
conservative and is the cornerstone of treatment for tendonosis. In
addition to the general scheme of treatment of overuse syndromes
outlined previously, the primary treatment emphasizes maximizing quad
strength and knee joint flexibility, reducing repetitive eccentric
quadriceps contraction exercises, and re-adding them in a paced
fashion. Infrequently, surgery is necessary for the patient with
recalcitrant disease. An MRI or ultrasound can be used to define the
area of the tendon affected by chronic tearing and subsequent
degeneration. Excising this area of the tendon can be useful (31).
Alternative schools of thought feel that the distal pole of the patella
impinges on the patella tendon, and excision of the distal pole can be
useful in treating this form of tendonosis (32).
P.355 -
-
Iliotibial band syndrome
-
Iliotibial band (ITB) syndrome (also known as ITB tendonosis)
is caused by excessive friction between the iliotibial band and the
distal lateral femoral condyle. The ITB functions as a weak extender of
the knee in near full extension, and a more powerful knee flexor after
30 degrees of knee flexion. The ITB is most stretched over the lateral
femoral condyle at 30 degrees of knee flexion. This condition is common
in runners and cyclists. -
Anatomic factors
have been implicated in ITB syndrome and include excessive foot
pronation, genu varum at the knee, tight lateral patella retinacular
structures, and an anterior tipped pelvis. Treatment is directed at
modification of the initiating causative factors and reducing the
excessive friction. Stretching of the ITB, treating foot pronation with
an orthotic, treating a tight lateral patella retinaculum with manual
therapy, and repositioning of an anterior tilted pelvis all can be
useful interventions when the patient has these physical examination
features.
-
-
Tibial tubercle apophysis (Osgood-Schlatter disease)
-
Clinical diagnosis.
This syndrome is usually seen in the rapidly growing athletic
adolescent with open growth plates at the knee. It is characterized by
point tenderness and enlargement of the tibial tubercle at the site of
the patella tendon insertion. A constant traction to this location
produces overgrowth of the tibial tubercle apophysis. X-ray evaluation
can be negative, or at times a prominent or irregular apophysis is
seen. Once the apophysis has closed, there frequently can be a free
bony particle anterior and superior to the tibial tubercle. -
Treatment.
The symptoms usually abate when the tibial tubercle fuses to the
diaphysis, and, therefore, every effort should be made to quiet this
injury down until full maturation is present in the developing
adolescent. Treatment depends on the severity of the disease. Nearly
all cases are managed by the proper balancing of activities against the
patient’s symptoms. This can follow the general treatment pattern of
overuse injuries as previously outlined. Surgical treatment is not
indicated. Aggressive treatment might occasionally involve limited use
of a knee immobilizer in recalcitrant cases where the patient is
dysfunctional in day-to-day activities, or non-compliant in activity
reduction.
-
-
Patellofemoral pain syndrome
-
Definition.
Patellofemoral pain syndrome is used to describe a constellation of
symptoms that are related to the patellofemoral joint. Typically, this
type of pain is considered an overuse syndrome, although the exact
etiology and nature of pain continues to be poorly understood.
Patellofemoral pain syndrome is that pain which originates in the
anterior knee structures, in the absence of an identifiable acute
injury (blunt trauma, dislocating or subluxing patella).Chondromalacia patella (CMP) is a term often used to
describe anterior knee pain, though use of this term to describe
clinical symptoms is not appropriate. CMP should be used only to
describe the pathological entity of cartilage softening on the
underneath side of the kneecap. Typically this could only be diagnosed
by surgical observation or MRI. The presence of cartilage softening
does not always result in the clinical symptom of pain. -
Pre-existing conditions.
Anatomic factors that can predispose a patient to patellofemoral pain
can include flexibility deficits of the limb, malalignment
P.356
of
the lower limbs including excessive femoral anteversion, high Q-angle,
rotation variations of the tibia, genu velgum at the knee, hind foot
valgus, and pes planus. Kneecap malalignment,
both static and functional, has been implicated in the etiology of
patellofemoral pain. However, there are a few population-based studies
to support the “malalignment theory kneecap pain.” Any one abnormality
may be trivial as a single entity. However, in combination with other
anatomic variables and associated with overtraining and overuse, they
frequently can lead to overuse injury (14).The role of malalignment and
the etiology of patellofemoral pain continue to be debated.
Radiographic imaging studies can reveal a patella that is malaligned
within the trochlear groove, as evidenced by a patella tilt and/or
subluxation. Some malalignment syndromes of the patella are residual
from a previous subluxing or dislocating event. However, other
malalignment syndromes can be present in the absence of an acute event,
and frequently are similar in both knees of the same person. It is felt
that patella malalignment, when constitutional in a person, can become
an overuse syndrome more readily and become a painful problem. -
Clinical presentation.
The most common clinical presentation of a patellofemoral pain syndrome
patient is pain on the anterior aspect of the knee that is aggravated
by prolonged sitting and stair climbing. Because the retinacular
structures of the patella extend both medially and laterally from the
patella, pain can also be associated with either medial- or
lateral-sided knee pain, therefore, it can create a very confusing
clinical presentation. It is infrequently associated with swelling.
Giving-way episodes can be reported; typically the giving-way episode
is with straight-ahead activities or stair-climbing, when one tries to
engage the quad and the quad “fatigues.” This should not be confused
with giving-way episodes associated with ligamentous instability, which
typically occur with planting, pivoting, or jumping activities.
Patients can also present with catching or clicking phenomena. This can
occur because of irritation of the knee-cap as it tracks in the
trochlear groove. Another common patient complaint is that the knee
“locks.” If the knee “locks” in full extension, this is a manifestation
of patellofemoral pain. The patient does not want to engage the knee
cap in the groove because of pain, and, therefore, keeps his or her leg
straight. If the knee is locked secondary to a loose body or torn
meniscus, it is always locked in some degree of flexion. -
Treatment.
Historically, non-surgical treatment has been the cornerstone for most
patellofemoral pain disorders. The primary goal of patellofemoral
rehabilitation is to reduce the symptoms of pain. This is done by a
combination of physical therapy modalities, improving quadriceps
strength, and endurance (see V. H). Other tools such as orthotics, knee sleeves, and McConnell taping can be used (33). Pelvic muscle strength, especially hip abductor and hip extensor strength, is essential for rotational control of the limb (23,30,34).
-
-
Pes anserinus bursitis
-
Definition.
The “pes” tendons are terminal insertions of three long thigh muscles,
one from each muscle group. These tendons come together to insert on
the anteromedial aspect of the proximal tibia, between the tibial
tubercle and the distal (tibial) attachment of the medial (tibial)
collateral ligament. The three tendons are sartorius (femoral
innervation), gracilius (obturator innervation), and semitendonosis
(sciatic innervation). They are powerful internal rotators of the leg
(tibia) and also aide in knee flexion. -
Clinical presentation.
The patient will present with soreness just below the medial knee,
which can be reproduced by direct palpation or resisted internal
rotation of the leg. In middle age, it can represent a referred pain
pattern from the knee due to medial knee arthritis. -
Treatment. In
addition to the rest, ice, compression, and elevation (RICE) principle
and physical therapy with modalities of stretching and strengthening, a
steroid injection at the bursa site can be helpful.
-
WG, James SL, Larson RL, et al. Patellofemoral disorders physical and
radiographic examination. Part II, radiographic examination. Clin Orthop 1984;185:178–186.
DW, Callaghan JJ, Sikes RA, et al. The accuracy of selective magnetic
resonance imaging compared with the findings of arthroscopy of the
knee. J Bone Joint Surg (Am) 1988;70:192–198.
CA, Dussault R, Levesque HP. The tangential x-ray investigation of the
patellofemoral joint: x-ray technique, diagnostic criteria and their
interpretation. Clin Orthop 1979;144:16–26.
DC, Meier SW. The case for advancement and repair of the medial
patellofemoral ligament in patients with recurrent patellar
instability. Oper Tech Sports Med 1999;7:81–89.
DH, Simel DL, Bates DW, et al. The rational clinical examination. Does
this patient have a torn meniscus or ligament of the knee? Value of the
physical examination. JAMA 2001;286:1610–1620.
LP, Li KC, Hollett MD, et al. Meniscal tears of the knee: accuracy of
detection with fast spin-echo MR imaging and arthroscopic correlation
in 293 patients. Radiology 1997;203:508–512.
ED, Wieslander SB, Stephensen S, et al. MRI preferable to diagnostic
arthroscopy in knee joint injuries. A double-blind comparison of 47
patients. Acta Orthop Scand 1997;68:277–281.
WDJ, Vittori JM. The incidence of healing in arthroscopic meniscal
repairs in anterior cruciate ligament-reconstructed knees versus stable
knees. Am J Sports Med 1992;20:176–181.
T, Gale D, Dewire P, et al. The clinical importance of meniscal tears
demonstrated in magnetic resonance imaging in osteoarthritis of the
knee. J Bone Joint Surg (Am) 2003;85:4–9.
EA, Dick R. Knee injury patterns among men and women in collegiate
basketball and soccer: NCAA data and review of literature. Am J Sports Med 1995;23(6):694–701.
RF, Terry GC. Injuries to the posterolateral aspect of the knee:
association of anatomic injury patterns with clinical instability. Am J Sports Med 1997;25:433–437.
JE, Yu JS, Kaeding CC. Recalcitrant patellar tendinitis: magnetic
resonance imaging, histologic evaluation, and surgical treatment. Am J Sports Med 1997;25:218–222.