Nonacute Elbow, Wrist, and Hand Conditions
-
History. As
with any medical problem, the history of events leading up to the
patient’s visit to the physician with an upper extremity problem is
critical. The history should contain family history, social history,
personal medical history unrelated to the musculoskeletal system,
infectious disease history, and risk behavior history. Some additional
key facts to record include the following:-
Handedness. Is the patient right- or left-handed?
-
Work-relatedness.
If the patient believes a problem is related to work or a series of
events, it is the physician’s job to document the patient’s beliefs.
The physician can do this by “quoting” the patient exactly. It is not the physician’s job or duty to question the veracity of a patient’s complaint. -
Mechanism of onset.
Record the details of the incident or accident as completely as
possible. This is particularly relevant for motor vehicle accidents.
Record details such as whether the patient was in the car, whether the
air bags were deployed, whether the steering wheel was bent
(particularly if the injured person was the driver), and the amount of
damage done to the car. -
Date of most recent tetanus booster. This is important with any direct trauma. Do not assume that another first examiner has resolved this issue.
-
-
Physical examination
-
General. At first glance, the upper extremity is a mirror of the lower. But, several key differences are obvious:
-
The shoulder has more freedom of motion and is consequently less stable than the hip.
-
The “patella” of the elbow is fused to the ulna as the olecranon.
However, it performs a similar function to the patella in that it
increases the “lever arm” for the attached muscle (triceps in the arm,
quadriceps in the leg). -
The elbow and wrist
participate equally in guiding forearm rotation (supination and
pronation). A similar motion is not available in the lower extremity. -
The wrist has more motion and less bony stability than the ankle.
-
The fingers are longer in proportion to the palm than the toes in relationship to the midfoot.
-
The thumb is longer and is opposable to the digits.
-
-
Region specifics
-
Elbow
-
The elbow joint moves in a hinge manner
at its articulation between the humerus and ulna. Thus, the
ulnar-humeral articulation is uniaxial. In addition to its critical
role in forearm rotation, the radius can transmit load to the humerus
in “high-strength” situations. This issue is even more important if the
elbow ligaments are injured. In general, the elbow gains minimal
stability from muscle support and is reliant upon ligament support to
guide joint motion. -
Examination of this joint should document
the active and passive arc of flexion and extension. Varus (lateral
ligament loading) and valgus (medial ligament loading) should be
assessed. -
Standard radiographs include anteroposterior (AP) and lateral views.
-
-
Forearm
-
Rotation of the forearm is guided by bone
support at the proximal and distal radioulnar joints (PRUJ and DRUJ,
respectively). Additional stability and guidance for this motion is
provided by the interosseous membrane. -
Examination should record the active and
passive arc of supination and pronation. Crepitance or pain at the PRUJ
or DRUJ should be noted. Pain or swelling in the mid-forearm should be
assessed. -
Standard radiographs include AP and lateral views.
-
-
Wrist
-
The wrist moves in a multiaxial manner.
The carpus is divided into a proximal (scaphoid, lunate, triquetrum)
and distal (hamate, capitate, trapezoid, trapezium) row. Some of the
key intercarpal articulations have more easily described relationships
(the scaphoid moves relative to the lunate in flexion and extension).
However, taken as a whole, the wrist is multiaxial and its motion is
highly dependent on ligament function. There is no direct attachment of
an extrinsic (forearm based) muscle or tendon to the bones of the
proximal wrist. Thus, these bones (scaphoid, lunate, and triquetrum)
are 100% dependent on ligament integrity for function. -
Examination
should record passive and active arcs of flexion, extension, radial
deviation, and ulnar deviation. Obvious pain or crepitance should be
recorded as specifically as possible. -
Standard radiographs
include posteroanterior (PA) or AP and lateral views. If the scaphoid
is the focus of attention, AP and lateral views of the scaphoid should
be specifically requested. These are oblique to the normal PA and
lateral views of the wrist.
-
-
Hand
-
The hand
contains uniaxial (interphalangeal), multiaxial-stabilized (metacarpal
phalangeal), and multiaxial-unstabilized (first and fifth
carpometacarpal) articulations. Thus, these joints have varying degrees
of ligamentous or muscle stability requirements. For example, the
proximal interphalangeal joint of the index finger is dependent on
ligament support. Whereas, the index finger’s metacarpophalangeal joint
can be partially stabilized by hand intrinsic muscle support. -
Examination
should record active and passive arcs of flexion and extension for all
joints. Thumb examination should additionally include ability to abduct
(palmar and radial), adduct, retropulse (extend), and oppose. Joint
stability should be tested and any masses or tenderness noted. -
Standard radiographs
include PA and lateral views. Note: To obtain a lateral view of a
finger, the adjacent digits need to be moved aside. Similar to the
scaphoid, “normal” thumb views are oblique to the hand. -
Note: Always examine the opposite or unaffected side. This is particularly important when assessing stability.
-
P.284 -
-
-
Developmental birth conditions
-
Radial agenesis.
Absence of the radius can be full or complete. Occasionally, this
longitudinal deficiency is accompanied by thumb agenesis. An even more
rare condition is presence of the radius and absence of the ulna. In
either event, stability of the wrist is compromised. The deformity is
often characterized with a “club hand.” The absence of the radius would
then be termed a radial club hand. Full assessment of this condition
requires complete assessment of the child to include renal,
cardiovascular, neural, and other musculoskeletal regions (shoulder,
elbow, and hand). If the child has associated anomalies, correction of
the deformity at the forearm carpal articulation may actually
compromise function. Thus, any direct treatment must consider the whole
forearm and carpal articulation. -
Syndactyly
-
This is the most common congenital hand condition (1 in 2,000 live births). The cause is not known. It is divided into simple (soft-tissue joining of two or more digits with no associated bone or joint anomaly) and complex
(joining of two or more digits to include soft tissue and bones or
joints) categories. Further subdivision is possible based on the length
of the syndactyly. Complete syndactyly involves the whole length of the finger, whereas incomplete
syndactyly does not. Simple syndactyly differences are often completely
correctable. The complex differences, however, can occur in combination
with other congenital differences (Apert syndrome). -
In general, surgical correction of this
difference should be performed as soon as is anesthetically feasible.
Correction of a multiple finger difference is done in stages.
Limitations of correction are often related to digital blood supply;
usually, full-thickness skin grafts are required at surgery.
-
-
Polydactyly
-
This difference is classified into preaxial duplication
(involvement of the thumb), central duplication (index, middle, or ring
involvement), and postaxial duplication (small finger involvement). Postaxial duplication
has a clear genetic component and is seen in as many as 1 in 300 live
births. Correction of this difference usually involves excision. The
degree of duplication and joint involvement determines the complexity
of the procedure. -
Treatment methods
for thumb duplication generally focus on excision of an unstable
duplicate thumb. Duplication of the thumb has been characterized to
occur in at least seven different patterns. The outcome of thumb
reconstruction depends on the ability to create a thumb of appropriate
length, rotation, stability, and mobility and to integrate the thumb
into the child’s daily routine. It is on this basis that earlier
correction is generally recommended.
-
-
Madelung’s deformity.
First described by Malgaigne in 1855 and later by Madelung in 1878,
this difference of growth related to the distal epiphysis of the radius
is believed to be congenital in nature, although it is usually not
noted before adolescence. It is a rare, genetic condition transmitted
in an autosomal dominant pattern. Because of incomplete growth of the
radius, the clinical presentation may be prominence of the ulnar head
(distal ulna). Alternatively, abnormal forearm rotation may be the
presenting complaint. At present, pain may not be a component. The
method of surgical correction (shortening of the ulna versus
lengthening of the radius) is less important than the goal of obtaining
and preserving stable, painless forearm rotation with full and
unrestricted use of the wrist. -
Brachial plexus
-
The brachial plexus comprises a
coalescence of cervical and upper thoracic spine nerve roots. It
traverses the space between neural foramina and the infraclavicular
region where it again separates into individual nerves. Birth injuries
relating to the brachial plexus are thought to represent an avulsion or
stretch of the upper (Erb’s), lower (Klumpke’s),
or both aspects (combined) of the brachial plexus. These injuries occur
generally in the process of vaginal delivery of the child. -
Critical to the examination
of any child with a presumed brachial plexus lesion is verification of
normal shoulder bony anatomy. The physician should document this by way
of physical examination and shoulder radiographs confirming the
shoulder (glenohumeral joint) is located. -
Occasionally a child with nothing more than a fractured clavicle (birth related)
will be mistaken to have a brachial plexus injury. Thus, it is
important to include the clavicle in the physical examination of the
infant. Generally speaking, a single AP chest radiograph suffices to
detect such a fracture in the neonate. -
Management of brachial plexus injuries at birth should include the following:
-
Documentation of glenohumeral joint status (located)
-
Documentation of passive mobility of all upper extremity joints, including cervical spine mobility
-
Documentation of observed active motion in shoulder, upper arm, elbow, forearm, wrist, and hand
-
Initiation of twice-daily active-assisted “whole-arm” mobilization program to be completed by the care team or parents
-
Plan for follow-up examination on a
frequent interval to verify understanding and completion of passive and
active-assisted exercises and available joint motion (both passive and
active—looking for change or improvement)
-
-
The prognosis
for many brachial plexus injuries is for complete or near complete
recovery. Children whose function remains compromised are evaluated and
occasionally operated upon within the first 6 to 18 months of age. The
treating physician who cannot document substantial improvement early
(less than 6 months of age) should arrange further evaluation by an
upper extremity specialist.
P.286 -
P.285 -
-
Delayed presentation of developmental differences
-
Cerebral palsy
-
Patients with cerebral palsy constitute
the largest group of pediatric patients with neuromuscular disorders.
The frequency varies from 0.6 to 5.9 patients per 1,000 live births.
Difficulties related to this problem persist into adulthood. However,
unlike many neuromuscular disorders, this condition does not progress.
Relative progression of the disorder may occur in relation to growth,
weight gain, or onset of degenerative change. However, any real
progression should cause review of the original diagnosis. Generally,
the problem relates to prenatal, natal, or early postnatal brain
injury. The injury can express itself in a wide pattern, ranging from
single limb to whole body involvement. Two clinical types of injury are
seen:-
Spastic type—represents an injury to pyramidal tracts in the brain. Exaggerated muscle stretch reflex and increased tone are seen.
-
Athetoid type—probably a lesion in the basal ganglia. Continuous motion of the affected part is present; this type is more rare.
-
-
Diagnosis is
the first component of treatment. In cases with lesser involvement,
diagnosis may not be obvious until the child fails to reach normal
motor milestones or has difficulty with coordinated tasks. In some
cases, the diagnosis is suspected because of early “under-use” of a
part. For example, a child does not have a strong hand preference
before 18 months of age. -
Treatment of
cerebral palsy should always focus on functional improvement. Surgery
generally has a cosmetic benefit, but the initial goal should be to
improve a specific function. Intelligence and sensory awareness of the
child are the two biggest determinants for functional improvement after
surgery. Improvements of arm function are possible by improvement in
the position of the shoulder, elbow, forearm, wrist, hand, and thumb.
Three of the more successful surgeries are release of an internal
rotation/adduction spastic contracture involving the shoulder,
release/rebalancing of a flexed and pronated spastic wrist/forearm, and
release/rebalancing of a thumb into palm deformity.
-
-
-
Nerve. Nerve
tissue is responsible for communication in two directions between the
brain and the external environment (peripheral). Like the brain, nerve
function is highly dependent on oxygen. Although depolarization of a
single axon is energy independent, repolarization of the axon is
dependent on adenosine triphosphate to run the Na+/K+ pump to “recharge” the axon potential. Thus, although local loss of O2 will not cause death of the peripheral axon cell body, local loss of O2 will affect the ability of the axon to conduct information. This change in conduction is generally transient, depending on O2 availability. However, frequent episodes of
P.287
reduced O2
can produce permanent change in function. Common sites for nerve
dysfunction to occur in the arm are the carpal canal (median nerve),
the cubital tunnel (ulnar nerve), and the arcade of Froshe (posterior
interosseous branch of the radial nerve).-
Carpal tunnel syndrome (CTS)
-
Fig. 20-1
depicts the carpal tunnel as seen from end on. The carpal tunnel is
seen to be formed by the three bony borders of the carpus (trapezium,
lunate, hook of hamate) and the transverse carpal ligament. As such, it
is a defined space with a fixed volume. Changes in the fixed volume can
occur as a result of actual changes in the bony outline resulting from
late effects of trauma or arthritis. Also, relative change in volume
available can be the result of mass effect occurring from tendon or
muscle swelling or synovitis, presence of an anomalous muscle, or
presence of an actual mass (e.g., lipoma). The patient with reduction
in available volume is less able to tolerate or accommodate increases
in pressure within the carpal canal. Thus, in patients with reduced
carpal canal volume, provocative maneuvers such as Tinel’s (tapping or
percussion of a nerve in a specific location), Phalen’s (flexion of the
wrist causing indirect nerve pressurization), or Durkin’s compression
test (manual pressure by examiner upon the median nerve) are more
likely to be positive. -
Presenting complaint is most commonly pain in the median nerve distribution. Pain is often exacerbated at night or by specific activities (1).
As the syndrome advances, numbness occurs in the distribution of the
median nerve. Weakness of the thenar muscles with associated wasting is
a late stage event. -
Laboratory testing.
Radiographs to check for degenerative joint disease (DJD) or old
fractures are occasionally of benefit. The most widely accepted
diagnostic method is electrodiagnostic testing [electromyogram/nerve
conduction velocity (EMG/NCV)]. This test can document slowing of nerve
P.288
conduction
and early muscle denervation. The EMG is most specific if the symptoms
have been present for at least 1 month. Given the association of
hypothyroidism and rheumatologic discorders, testing of the thyroid
stimulating hormone (TSH) and rheumatoid factor (RF) should be strongly
considered. Finally, carpal tunnel syndrome is very common in
pregnancy, and symptoms frequently resolve after delivery.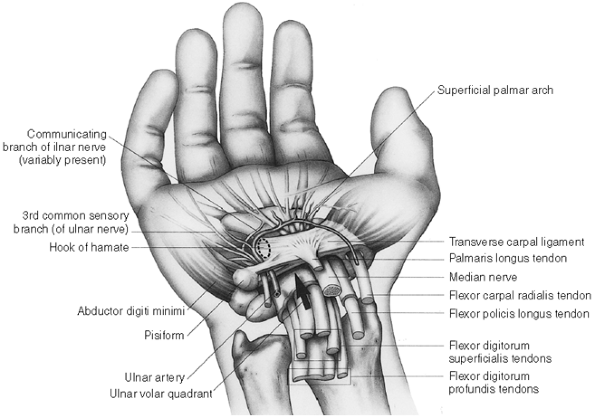 Figure 20-1.
Figure 20-1.
The carpal tunnel is bounded by bone on three sides and by the ligament
(transverse carpal) on one side. Guyon’s canal overlies the ulnar side
of the carpal tunnel. The median nerve lies in the radial volar
quadrant of the carpal canal. Generally, it is immediately below or
slightly radial to the palmaris longus. -
Treatment of
CTS focuses on relief of pain. Initial therapy can include medication
to relieve pain and swelling [nonsteroidal anti-inflammatory drugs
(NSAIDs)], splint support, and exercises to increase mobility. No test
or study has shown definite value for NSAIDs in management of CTS,
except as they are related to relief of pain. An injection of
corticosteroid into the carpal tunnel may be effective. There is some
benefit from vitamin B6 and C oral therapy. -
Surgery for
relief of CTS symptoms is generally successful, with patient
satisfaction exceeding 95% and complications less than 1%. The surgery
can be completed by a variety of methods (open surgery versus
percutaneous or arthroscopic-assisted release) without a clear benefit
to one method versus another, as long as complete longitudinal division
of the transverse carpal ligament is achieved along the ulnar half (1,2,3,4). Return to unrestricted activity after CTS surgery requires 4 to 8 weeks.
-
-
Cubital tunnel syndrome
-
The cubital tunnel
is formed by the bony borders of the medial epicondyle and medial ulna
and overlying soft-tissue constraints including the entrance between
the ulnar and humeral head of the bipennate flexor carpi ulnaris. It is
a defined space with a fixed volume. Changes in the fixed volume can
occur as a result of actual changes in the bony outline as a result of
late effects of trauma or arthritis (osteoarthritis or rheumatoid
arthritis). Relative change in volume available can be the result of
mass effect occurring from tendon and muscle swelling or synovitis.
Laxity of the soft-tissue–supporting structures can allow the ulnar
nerve to migrate out of the cubital tunnel and over the medial
epicondyle during flexion. This motion is often referred to as
subluxation of the ulnar nerve and produces a “Tinel-like” distal
sensory disturbance. -
Presenting complaint is most commonly pain in the distribution of the ulnar nerve distribution (5).
Pain is often exacerbated at night or by specific activities. As the
syndrome advances, numbness occurs in the distribution nerve. Weakness
or atrophy of the hypothenar muscles is a late stage event. -
Laboratory testing
(thyroid function tests and rheumatoid factor) and radiographs (DJD,
old fractures) are occasionally of benefit. The most widely accepted
diagnostic test method is electrodiagnostic testing (EMG/NCV). This
test can document slowing of nerve conduction and early muscle
denervation. Again, the EMG is most sensitive if symptoms have been
present for at least 1 month. -
Treatment of cubital tunnel syndrome focuses on relief of pain (6).
Initial therapy can include medication (NSAIDs) to relieve pain and
swelling, provision of antielbow flexion splint support or pad, and
exercises to increase mobility. No test or study has shown definite
value for NSAIDs in management of cubital tunnel syndrome, except as
related to relief of pain. -
Surgery for
relief of cubital tunnel symptoms is substantially less successful than
surgery for relief of CTS. The surgery can be completed by a variety of
methods (small versus large surgical exposure) without a clear benefit
to one method versus another as long as the point of observed nerve
compression is released (7). The patient returns to unrestricted activity 12 to 24 weeks after surgery.
-
-
PIN compression/other
-
The PIN (posterior interosseous) branch of the radial nerve travels through a defined space with a fixed volume. The tightest region of this
P.289
space is formed by a fascial connection at the proximal margin of the
two heads of the supinator muscle in the proximal forearm (arcade of
Froshe). Changes in the fixed volume can occur as a result of actual
changes in the bony outline that result from late effects of trauma or
arthritis. Relative change in volume available can be the result of
mass effect occurring from tendon and muscle swelling or synovitis,
presence of an anomalous muscle, or presence of an actual mass (e.g.,
lipoma). The most common cause of nerve irritation in this region is
believed to be the result of thickening of the facial margin in
response to time (age) and stress. -
Presenting complaint
is most commonly pain in the general region of the supinator muscle.
Pain is often exacerbated at night or by specific activities. As the
syndrome advances, numbness does not occur. Weakness of the PIN
innervated muscles with associated wasting is a late stage event. -
The most widely accepted diagnostic test
method is electrodiagnostic testing (EMG/NCV). PIN compression with
this test is of substantially less benefit when compared with other
nerve compression syndromes. Nonetheless, it shows muscle denervation
in some cases. -
Treatment of
PIN syndrome focuses on relief of pain. Initial therapy can include
medication to relieve pain or swelling (NSAIDs) and exercises to
increase mobility. Splints may exacerbate the problem if placed over
the nerve. Wrist splints to reduce load on wrist extensors (the wrist
extensors cross over the supinator) are occasionally helpful. As with
the other nerve compression syndromes, no test or study has shown
definite value for NSAIDs in management of PIN syndrome. -
Surgery for
relief of PIN symptoms is substantially less successful than surgery
for relief of CTS. A variety of surgical approaches have been
described. The arcade of Froshe is identified and released. Return to
unrestricted activity after surgery requires 12 to 24 weeks.
-
-
Other. Nerve
compression can essentially occur wherever a nerve exits or enters a
fascial plane/transition zone. The foregoing are the most common sites.
Knowledge of extremity anatomy will aid the student in assessing other
sites of suspected nerve entrapment.
-
-
Muscle and tendon.
Muscles and tendons work together to generate and transmit force. The
effect of load transfer depends on stable points of origin and
insertion. Thus, at least three locations of function failure are apparent: (1) bone–muscle origin, (8) muscle–tendon junction, and (9) tendon–bone insertion. An example of each is provided.-
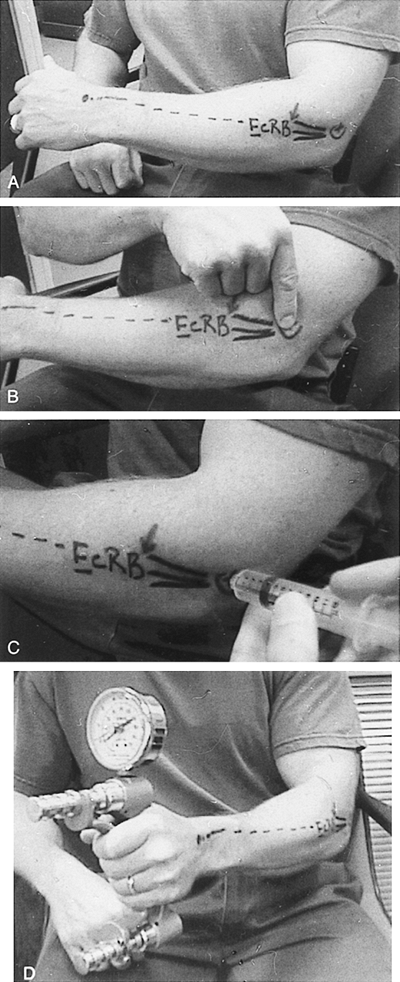
Bone–muscle origin interface failure: lateral epicondylitis (Fig. 20-2)
-
Failure of the muscle origin
of forearm extensors (lateral) or flexors (medial) is a common
condition. The condition is uncommon in youths or persons of advanced
age. It is occasionally seen in conjunction with working activities.
Most often, the condition begins after a period of repetitive stress. -
Presenting complaint
is usually pain focused at the muscle origin. Resisted use of the
muscle aggravates the condition. The pain usually subsides with rest.
Swelling is rarely present; no mass is seen with this condition. Range
of motion may be uncomfortable; but a full active or active-assisted
range of motion should be possible. -
Laboratory testing
is of no particular value. Screening roentgenograms may be obtained but
are generally normal for age. An injection test may be of confirmatory
benefit (9). This is performed as outlined in Fig. 20-2.
In this situation, the hope is that a precise injection of lidocaine
with steroid into the area of extensor origin will eliminate or
significantly alleviate the pain. -
Treatment of
epicondylitis focuses on reducing the stress at the “inflamed”
interface. Theoretically, if the stress is low enough, the healing
process can succeed in healing the injured interface. Thus, use of
splints (Froimson barrel or forearm band) to reduce the load on the
injured muscle origin, massage to increase the blood supply for
healing, and stretching exercises to increase muscle excursion are all
measures that are likely to
P.290P.291
provide success. The value of injections versus oral NSAIDs, rest, and splint support has not been clarified.![]() Figure 20-2. A: The path of the extensor carpi radialis brevis (ECRB) from lateral epicondyle to the base of the third metacarpal. B: The center of the epicondyle is the usual pain foci. C:
Figure 20-2. A: The path of the extensor carpi radialis brevis (ECRB) from lateral epicondyle to the base of the third metacarpal. B: The center of the epicondyle is the usual pain foci. C:
Injection of lidocaine at the painful site. This should eliminate the
pain. The injection is into the muscle origin, below the fascia. D:
Postinjection strength testing usually reveals greater strength after
pain is eliminated (successful injection). (From Putnam MD, Cohen M.
Painful conditions around the elbow. Orthop Clin North Am 1999;30(1):109–118.)
-
-
Muscle–tendon pathway failure results in trigger finger, trigger thumb, and de Quervain’s tenosynovity.
-
The junction
between a specific muscle and its tendon is a potential site of
failure. However, failure or pain at this location is uncommon in the
upper extremity. Achilles tendinitis represents a condition occurring
in the lower extremity. A similar condition does not occur in the upper
extremity with any frequency. Problems along the tendon pathway,
however, do occur. -
Commonly referred to as trigger digits,
snapping of flexor tendon function caused by bunching of the flexor
synovium at the annular one (A1) pulley does occur. This condition is
seen more often in older patients, although a congenital version is
also common. The condition occurs more often in patients with diabetes.
Patients with active tenosynovitis (rheumatoid arthritis) may have a
condition that is often confused for tendon triggering. But, rheumatoid
arthritis and synovitis in other patients can be distinguished from
true trigger digit by the inability to obtain complete active flexion.
This is the result of too much synovium “blocking” the active flexion
of the digit (the excursion of the flexor tendon is blocked). In the
case of de Quervain’s tenosynovitis, the problem is focused within the
first dorsal extensor compartment of the wrist. The pathophysiology is
the same, but this condition results in pain and crepitus along the
tendon rather than triggering. The problem and degree of discomfort
varies with time of day and activity. -
Clinical diagnosis
of trigger dysfunction is made based on pain or tenderness, crepitance,
and locking focused at the A1 pulley of a specific digit. -
Laboratory studies
are essentially within normal limits. Radiographic studies are not
generally useful. In the case of de Quervain’s tenosynovitis, a special
clinical test (Finkelstein’s) is routinely performed. Finkelstein’s
test is positive if ulnar wrist deviation combined with thumb adduction
and flexion of the metacarpal phalangeal joint reproduces the patient’s
complaint of pain. -
Treatment of
trigger digit and de Quervain’s synovitis includes rest, stretching
exercises, steroid injection into the tendon sheath, and surgical
release of the tendon sheath (3,4,5,6,7,8,11).
If conservative care fails, response to supportive modalities is
variable. In up to 60% of patients, the condition resolves after
steroid injection (12). Surgical release of the sheath is thought to be 95% effective in those who fail to respond to lesser treatments (13).
-
-
Tendon–bone insertion failure results in mallet finger and biceps rupture.
-
Failure at
the distal point of muscle action can occur as a result of attrition or
age-related change, or excessive load. Occasionally, both methods are
involved. Patients are usually seen for diagnosis soon after the
failure occurs. Pain is usually less an issue than is weakness or
dysfunction. -
These conditions are diagnosed
based on findings observed on clinical examination. Laboratory studies
and roentgenographic findings are generally normal, the exception being
when the extensor tendon involved with a Mallet finger pulls off a
piece of the proximal aspect of the distal phalanx (thus, a “bony
Mallet”). Larger tendon ruptures can be further clarified using
magnetic resonance imaging (MRI) if there are unclear physical findings. -
Treatment is
based on the ability to reposition the specific insertion and maintain
this in a resting position. For the terminal extensor–mallet finger, 6
weeks of a conservative extension splint treatment is generally
successful (8,10).
Conversely, distal biceps ruptures will not heal without surgery
because the tendon cannot be reliably positioned. However, because the
muscle is a supporting elbow flexor (not the only elbow flexor),
patients who do not require forceful supination (the biceps is the
prime supinator) may choose to forego repair (and tolerate the
functional limitations).
-
-
-
Joint.
Painless, stable joint function is maintained by a combination of
healthy cartilage, retained shape of the joint surface, ligamentous
integrity, and muscle/tendon strength. Change in any of these four
factors begins a process of increasing joint wear and dysfunction.
Aging alone causes changes in the surface of the joint that accelerate
wear. Most arthritic conditions of the arm
are a combination of load, genetics, and history. However, it is
occasionally possible to point to a single event many years earlier
that has gradually led to joint dysfunction. Processes such as
rheumatoid arthritis are usually the sole cause of dysfunction. Even in
these diseases, isolated or cumulative trauma can play a role.-
Thumb carpometacarpal (CMC) (Fig. 20-3),
wrist, and elbow DJD occur with decreasing frequency. Thumb CMC DJD may
be the most common site of arthritic presentation. In any of the upper
extremity sites, the most common presenting complaint is pain. To the
degree that a specific joint is unstable, incongruous, or both, motion
and stress aggravate symptoms. Certain activities and prior injury may
predispose to arthritis, but underlying genetics is likely the most
predominant cause. -
Diagnosis is
a combination of history, examination, laboratory study, and plain
radiographs. MRI or computed tomography (CT) methodology is rarely
useful. Most patients complain of pain after activity that is relieved
by rest. Oral NSAIDs are of some benefit. However, care must always be
taken with long-term administration of these medications, particularly
in elderly patients. -
Treatment begins with supportive splints and hot/cold modalities. Hand-based flexible splints are particularly helpful for thumb CMC.
-
At some point, many patients can no longer “tolerate” the pain. This is the time to consider surgery.
Unlike the lower extremity, upper extremity arthritic surgery can offer
patients reliable joint rebuilding procedures without resorting to
joint replacements. An example of such an excisional arthroplasty is
shown in Fig. 20-4. Such procedures report greater than 90% success rate relative to pain relief. -
In the event that first-stage arthritic procedures do not work, newer and increasingly durable total joint replacement options are becoming available for the elbow, wrist, and the proximal interphalangeal joints.
-
-
Bone.
Skeletal support is essential for function of the legs and arms. As
such, immediate change (fracture) or gradual change (e.g., avascular
necrosis, tumor) will alter the function of the arm or leg. Gradual
change is rarely as painful as acute or fracture change in bone
support. This may explain the late presentation for treatment of
patients whose slow change process has progressed to the point at which
curative or reconstructive treatment is no longer an option. Avascular
necrosis of bone is a condition in which presentation and diagnosis are
often delayed. As such, it is a good model to discuss the workup of
bone pain.-
Avascular necrosis, Kienböck’s (lunate) (Fig. 20-4), Presiser’s (scaphoid), and Panner’s (humeral capitellum)
are focal avascular lesions of bone seen in the upper extremity.
Genetics, overload, endocrine and systemic illness, and steroid use may
play contributory roles. Patients usually have pain in the focal area
and, on testing, it is usually possible to document a reduction in
motion. Age of presentation varies from adolescence to late adulthood.
Plain radiographs may reveal a change in bone density. In more advanced
cases, the shape of the bone is altered. Change in shape is a precursor
to diffuse arthritis.-
Conservative treatment
starts with making a definite diagnosis. This is true for any
unexplained pain in bone. If the diagnosis confirms a focal change in
bone vascularity without change in bone shape, initial treatment may
focus on joint support. However, many patients, particularly those with
Kienböck disease, do not gain sufficient pain relief from splints, and
other joint “unloading” treatments are sought. -
Surgical treatments
for these processes can be broken down into treatments that reduce load
on the injured bone segment, debride the injured bone segment, or
replace/excise the injured bone segment. These treatments are likely to
relieve pain in more than 80% of patients; however, full functional
recovery rarely occurs.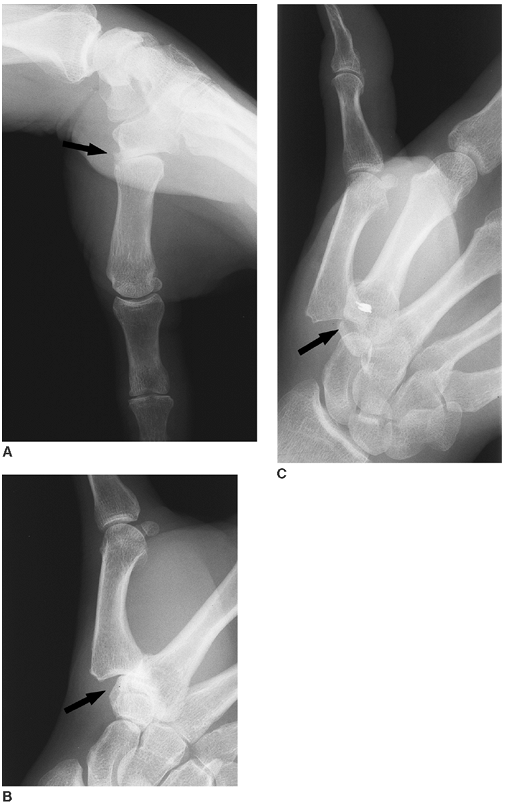 Figure 20-3. A and B: Loss of normal space between the metacarpal and trapezium typical of basilar joint thumb arthritis. C:
Figure 20-3. A and B: Loss of normal space between the metacarpal and trapezium typical of basilar joint thumb arthritis. C:
After trapezial resection and stabilization of the first to second
metacarpal, a new space for thumb carpometacarpal motion has been
“created.”![]() Figure 20-4. A: Posteroanterior (PA) wrist radiograph showing “collapse” of the lunate. B:
Figure 20-4. A: Posteroanterior (PA) wrist radiograph showing “collapse” of the lunate. B:
Magnetic resonance imaging study of the same wrist from the same point
in time showing essentially no vascular signal within the lunate
marrow. C: PA wrist radiograph showing the capitate “seated” in the lunate fossae after excision of the lunate.
-
-
-
Tumors. The
upper extremity is the site of a variety of tumors, many of which are
rare, some appearing almost exclusively on the hand and the arm, and
still others are common to all regions of the body. Although most
tumors of the upper extremity are benign, few present simple
therapeutic problems. The close anatomic relation of the tumor to the
nerves, vessels, and muscles in the upper extremity presents a great
challenge to the treating surgeon.-
Surgeons who treat hand and upper extremity tumors must be familiar with the wide range of possible diagnoses.
Tumors that look innocent may not be; every mass should be considered
potentially dangerous. This section focuses on primary malignant bony
tumors of the upper extremity: diagnosis, evaluation, pathology, and
treatment recommendations. -
Symptomatic tumors,
especially those that have increased in size, must be diagnosed and
then classified as to stage. The patient’s clinical and family history,
the physical characteristics of the lesion, and diagnostic images
provide information to determine whether the growth is aggressive and
should be “staged.” -
Diagnostic strategies
to accurately stage the lesion should be pursued before obtaining a
biopsy. Appropriate evaluation includes a detailed history and
proficient physical examination, imaging, and laboratory studies. The
history should determine the length of time a lesion has been present,
associated symptoms, and any incidence of family history. Physical
examination requires detailed evaluation of the entire limb and
testing, especially for sensibility, erythema, fluctuance, range of
motion, tenderness, and adenopathy. -
There are a few lesions that have significant associated blood chemistry changes.
These include the elevated sedimentation rate of Ewing’s sarcoma and
the serum protein changes in multiple myeloma. Serum alkaline
phosphatase is elevated in metabolic bone disease and in some
malignancies. A serum immunoelectrophoresis determines whether multiple
myeloma is present. -
Imaging
further aids in determining the location of the tumor and the presence
or absence of tumor metastasis. There are a variety of imaging
techniques that are useful tools.-
Plain films and tomography.
Radiographs are of great importance in the diagnosis of bone tumors.
Excellent technique is required to ensure good resolution of bone and
adequate soft tissue surrounding the lesion. Plain films are the
benchmark in predicting presence and location of bone involvement.
Tomography or CT affords improved resolution. -
MRI has
recently developed as one of the more important tools for diagnosing
bone tumors. It offers excellent delineation of soft-tissue contrast as
well as the ability to obtain images in axial, coronal, and sagittal
planes. Additionally, MRI can visualize nerve, tendon, and vessels and,
with advanced protocols, cartilage can also be evaluated.
-
-
Classification of lesions.
Correct treatment must always take into consideration the location and
size of the tumor, the histologic grade and clinical behavior, and the
potential for metastasis. If a lesion increases in size or becomes
symptomatic, or if the physical or radiographic appearance suggests an
aggressive lesion, appropriate staging studies including a tissue
diagnosis (biopsy) must be obtained. -
Specific tumors
-
Benign
-
Lipoma. This
common tumor occasionally presents in the hand or wrist as a firm mass
within a nerve or vascular passageway. As such, it may be associated
with carpal tunnel syndrome. Its nature may be suspected based on
clinical examination alone (mass). To understand its dimensions and
relationship to adjacent tissues, an MRI scan is usually obtained.
Excision (marginal) is the treatment of choice. -
Enchondromas (Fig. 20-5)
of the hand are common; they are sometimes multiple and often present
after a fracture. Initial treatment in this circumstance is aimed at
satisfactory fracture healing. They can clinically be confused with
osteochondromas. Radiographic examination easily differentiates the two
processes. Most randomly identified lesions can be observed; any lesion
associated with pain or increasing size in adulthood should be more
carefully studied. Treatment is either observation or intralesional
excision. Occasionally, previously benign lesions recur or undergo
malignant transformation (Fig. 20-5). Any such lesion should be biopsied and carefully considered for wide excision.
-
-
Malignant
-
Melanoma. The hand, wrist, and forearm are common sites of melanoma. Any change in a pigmented lesion warrants biopsy.
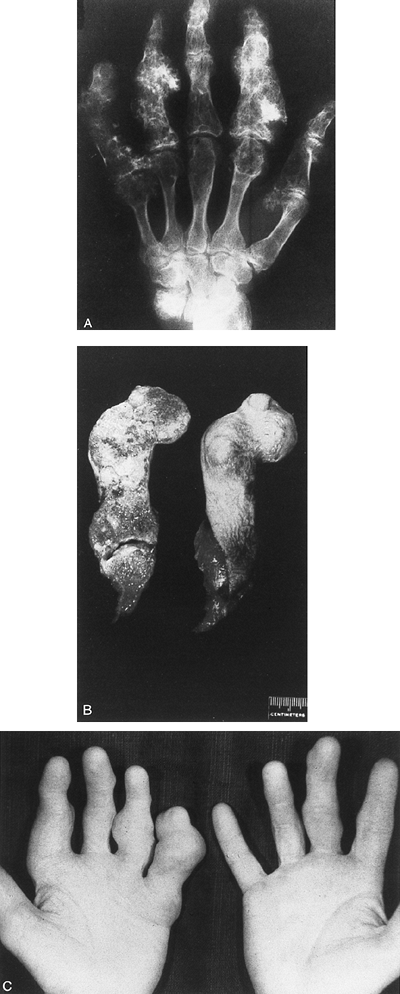 Figure 20-5. A: Posteroanterior radiograph showing bone changes consistent with multiple enchondromas. B: Longitudinal section of the small finger. Pathology seen was consistent with low-grade chonorosarcoma. C:
Figure 20-5. A: Posteroanterior radiograph showing bone changes consistent with multiple enchondromas. B: Longitudinal section of the small finger. Pathology seen was consistent with low-grade chonorosarcoma. C:
Preoperative clinical photo showing multiple digit enlargements. In
this case, the patient noted rapid enlargement of the small finger
during several months before surgery. (From Putnam MD, Cohen M.
Malignant bony tumors of the upper extremity. Hand Clin 1995;11(2):265–286.) -
Osteosarcoma and chondrosarcoma.
Malignant bone lesions do occur in the arm. Most distal lesions are
likely to represent degenerative change of benign processes (Fig. 20-5).
Any bone or enlarging soft-tissue mass must always receive a complete
evaluation (staging and biopsy) leading to a definitive diagnosis.
P.296P.297 -
-
-
Metastasis.
Lesions from elsewhere appearing as metastasis are the most common form
of malignancy in the hand. This should be kept in mind, particularly
for the patient who is not known to have a malignancy and whose lesion
is not in keeping with local origin. A search for the primary tumor is
appropriate.
P.295 -
-
Other factors: Workmen’s compensation.
The hand is often the first tool in and last tool out of a dangerous
situation. As such, it is the frequent site of workplace injuries (14).
Not all injuries are clearly documented. It is the physician’s
responsibility to remain the patient’s advocate while at the same time
remaining an objective observer. Occasionally, these tasks are in
conflict. Three simple rules apply in these situations:-
Remain a dispassionate recorder of medical facts.
-
Search for an accurate diagnosis.
-
Offer no treatment without a specific diagnosis.
-
JN, Keller RB, Simmons BP, et al. Maine carpal tunnel study: outcomes
of operative and nonoperative therapy for carpal tunnel syndrome in a
community-based cohort. J Hand Surg (Am) 1998;23:697–710.
JP, Fink K, Sullivan SD. Conservative versus surgical treatment of
mallet finger: a pooled quantitative literature evaluation. J Am Board Fam Pract 1998;11:382–390.
G, Herbert R, Hearns M, et al. Evaluation and management of chronic
work-related musculoskeletal disorders of the distal upper extremity. Am J Ind Med 2000;37:75–93.
Quervain F. On a form of chronic tendovaginitis by Dr. Fritz de
Quervain in la Chaux-de-Fonds. 1895. Illgen R, Shortkroffs, trans. Am J Orthop 1997;26:641–44.