Pelvis and Acetabulum
interconnecting ligaments. It consists of the two innominate bones,
which articulate anteriorly with each other at the pubic symphysis and
posteriorly with the body of the sacrum at the sacroiliac joint. The
bones are covered on each side by muscles, and the intraabdominal
contents make surgical exposure potentially complex. The presence of a
large subcutaneous surface (the iliac crest), however, allows safe
access to the ilium.
chapter, all of which provide access to the bone via its subcutaneous
portion. The anterior and posterior approaches to the iliac crest are
used almost exclusively for bone grafting. The anterior approach to the
pubic symphysis, and the anterior and posterior approaches to the
sacroiliac joints are performed rarely; their use is associated almost
exclusively with the open reduction and internal fixation of pelvic
ring fractures.
demanding approaches a surgeon can be asked to perform. They are nearly
always used for the reconstruction of the acetabulum following
fractures. Because each approach only gives access to a limited part of
the acetabulum, it is critically important that the correct approach is
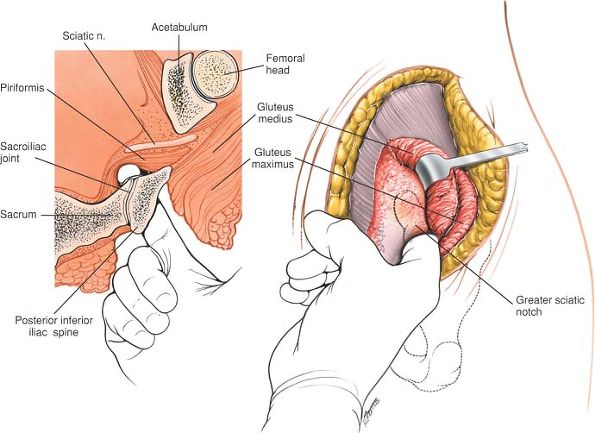
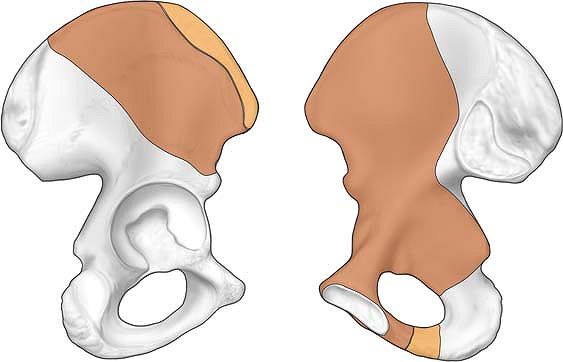
used for each fracture pattern (Fig. 7-1). This
requires accurate assessment of the anatomy of the fracture, using
radiographic techniques, including computerized tomography.1,2,3 The
use of a bone model is invaluable, especially when a surgeon is inexperienced.
 |
|
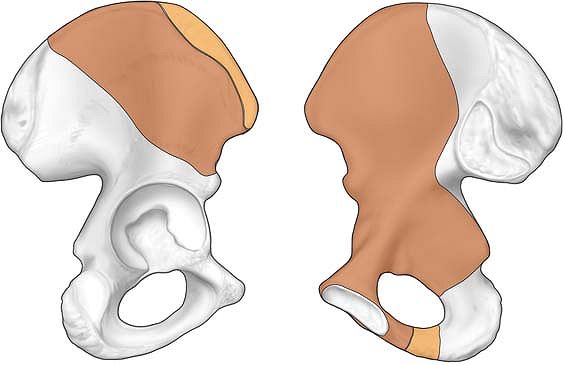
Figure 7-1
To appreciate the anatomy of the anterior and posterior columns of the acetabulum, hold a hemipelvis up against a light source. These two massive columns can then be appreciated in contrast to the thin central area of the wing of the ilium. |
access to the anterior column and medial aspect of the acetabulum. It
also allows visualization of the inner aspect of the pelvis from the
sacroiliac joint to the symphysis pubis. It does not allow access to
the posterior column or posterior lip (see Fig. 7-21).
to the posterior column, posterior lip, and dome segment of the
acetabulum. It allows very limited access to the anterior column of the
acetabulum and no access to the medial aspect of the acetabulum (see Fig 7-37).
approach is to be found immediately after the description of the
surgical approach. The applied surgical anatomy of the posterior
approach is found in Chapter 8 (see page 450).
the acetabulum, complex fractures may require the use of more than one
approach.
violent trauma. The tissues therefore are contused, and muscle planes
are often difficult to develop. The fractures themselves are difficult
to reduce, and control and specialized instruments are necessary to
ensure anatomical reduction and stable fixation. There is rarely, if
ever, indication to perform these approaches in an emergency situation.
Acetabular fractures are rare. Understanding of the anatomy of the
fracture is difficult, and surgical approaches are technically
demanding. The results of acetabular reconstruction depend largely on
the accuracy of the reduction of the fracture. For these reasons,
acetabular surgery, if at all possible, should be performed by
experienced surgeons working in centers large enough to attract a
sufficient volume of patients.
used grafts in orthopaedic surgery. The iliac crest is subcutaneous,
and cortical or corticocancellous grafts can be taken from it with ease
and safety for grafting in all parts of the body, including the spine.
It also is possible to remove pieces of the iliac crest, including both
cortices, for major bone reconstructions, especially in the head and
neck. For posterior spinal fusion work on conditions such as scoliosis,
the bone graft usually is taken from the posterior aspect of the iliac
crest.
the graft usually is taken in conjunction with other procedures, the
iliac crest should be draped as a separate unit. There is much to be
said for preparing this area routinely in all cases of open reduction
and internal fixation of long-bone fractures. Place a small sandbag
under the gluteal (cluneal) area of the side from which the graft will
be taken to elevate the crest and rotate it internally, making it more
accessible.
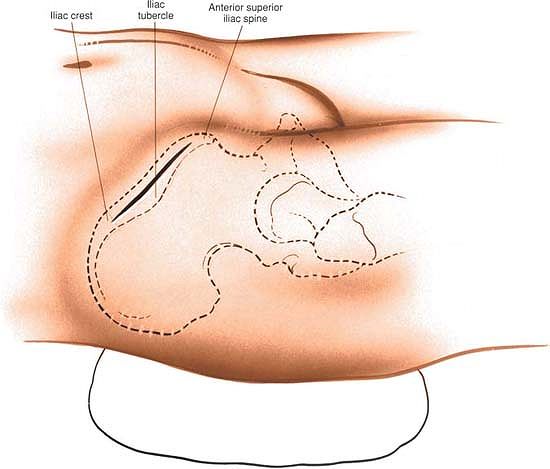
the most important landmark, is easily palpable. Continue palpating
along the crest of the ilium until its widest portion is reached, at
the iliac tubercle. The iliac tubercle marks the anterior portion of the ilium, the area containing the largest amount of cortical cancellous bone for graft material.
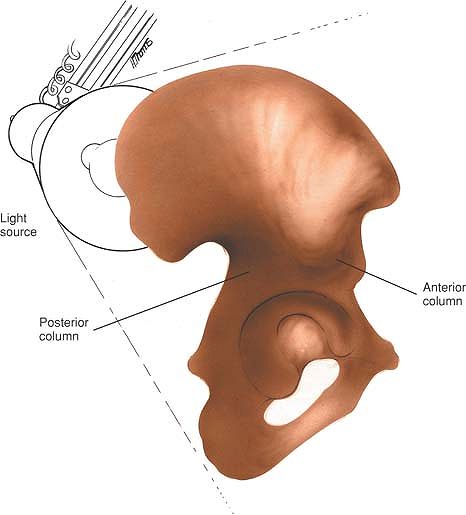
graft that is required. For an extensive bone graft make an 8-cm
incision parallel to the iliac crest and centered over the iliac
tubercle (Fig. 7-2).
crest, but do not cross it. Therefore, the crest offers a truly
internervous plane.
medius are the muscles affected most directly by grafts taken from the
anterior portion of the crest, because they originate from the outer
portion of the ilium and are supplied by the superior gluteal nerve.
The abdominal muscles take their origin directly from the iliac crest
and are supplied segmentally.
the crest still may be an avascular apophysis. If so, incise it and
remove the muscle through the crest in either direction with a Cobb
elevator. No apophysis will be present in adults.
 |
|
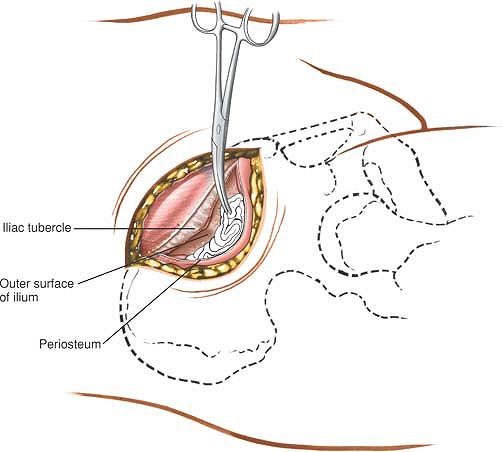
Figure 7-2 Make an 8-cm incision parallel to the iliac crest and centered over the iliac tubercle.
|
or iliac crest onto the anterior superior iliac spine itself; if this
occurs, the origin of the inguinal ligament may be detached and an
inguinal hernia may result.
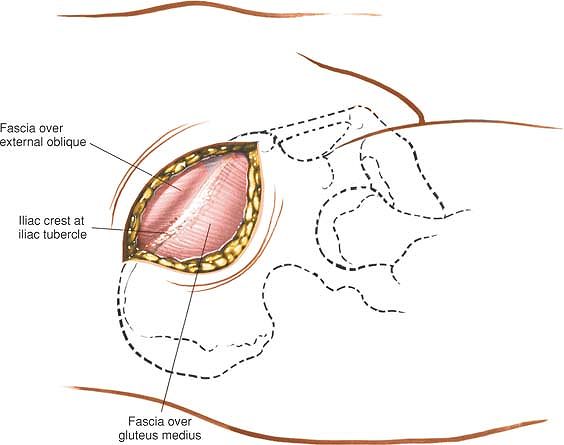
outer wall of the ilium. Initially, cut down onto the bone using a
scalpel. Follow the contour of the bone, sticking to it rigidly (Fig. 7-4).
Below the crest itself, the ilium narrows considerably, so the sharp
dissection will need to follow the contour of the bone carefully to
avoid straying out of plane and into trouble. After coming around the
corner of the crest onto the ilium, continue the dissection using blunt
instruments such as a Cobb elevator. The muscles will come away from
the bone easily. Alternatively, push a swab into the plane between the
iliac wing and the overlying muscles. Using a blunt instrument,
introduce more and more of the swab into the plane. The swab will act
as a tissue expander, pushing the muscle away from the bone, while at
the same time protecting the soft tissues. Corticocancellous strips may
be taken from either side of the bone, or a complete block of the ilium
can be removed. Pure cancellous bone can be taken by elevating a small
piece of the cortex of the crest. Be aware that the largest supply of
cancellous bone is directly underneath the subcutaneous surface of the
crest.
iliac spine should be left intact to preserve the normal appearance of
the pelvis. If the anterior superior iliac
spine is taken as graft material, the inguinal ligament might retract, causing an inguinal hernia.
 |
|
Figure 7-3 Retract the skin, identify the iliac crest, and incise the soft tissues overlying the iliac crest down to bone.
|
 |
|
Figure 7-4 Remove the origins of the gluteus minimus and medius muscles subperiosteally from the outer cortex of the ilium.
|
either the gluteal muscles from the outer cortex or the iliacus muscle
from the inner cortex. Placing a swab between the retractor and the
muscles creates a bloodless field and prevents little pieces of bone
graft from being lost in the depth of the wound. Great care must be
taken, however, to remove this swab before undertaking closure. The
incision may have to be lengthened on the iliac crest and additional
amounts of gluteus medius or iliacus stripped off to provide a better
view of the outer or inner cortex of the anterior portion of the ilium.
has been described in this section merely as a means of obtaining bone
graft.
during any posterior spine surgery that requires additional autogenous
bone to supplement the area to be fused. The grafts also may be used as
corticocancellous grafts for any part of the skeleton that needs fusion
or refusion.
bolsters running longitudinally to support the chest wall and pelvis,
allowing the chest wall and abdomen to expand without touching the
table. Place drapes distally enough so that the beginning of the
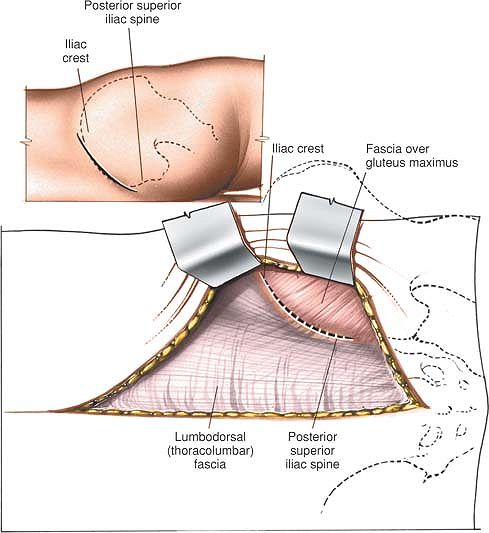
gluteal cleft and the posterior superior iliac spine can be seen (see Fig. 6-83).
performed, the midline incision can be extended distally to the sacrum.
Then, the skin and a thick, fatty, subcutaneous layer can be retracted
laterally. Using a Hibbs retractor, the flap should be dissected free
from the underlying lumbodorsal fascia until the posterior superior
iliac spine and crest can be palpated and seen (see Fig. 7-5).
but do not cross it. Therefore, the outer border of the iliac crest is
truly an internervous plane. The gluteus medius, minimus, and maximus
muscles take their origins from the outer surface of the ilium (the
gluteus medius and minimus are supplied by the superior gluteal nerve
and the gluteus maximus is supplied by the inferior gluteal nerve). The
segmentally supplied paraspinal muscles take their origin from the
iliac crest itself, as does the latissimus dorsi, which is supplied
proximally by the long thoracic nerve. Thus, an incision into the iliac
crest does not denervate muscles, even if it is not placed exactly on
the outer lip of the crest.
iliac crest is reached. In children, the iliac apophysis is white and
quite visible; it may be incised or split in line with the iliac crest,
using it as an avascular plane. In adults, the apophysis is ossified
and fused to the crest; the incision lands directly on the crest itself.
or muscles from the iliac crest both medially and laterally, to bare
the surface of the posterior portion of the crest.
 |
|
Figure 7-5
If lumbar spine surgery is being performed, extend the midline incision distally, retracting the skin laterally until the posterior superior iliac spine and crest can be palpated and seen. Incise the soft tissues overlying the crest down to bone. Make an 8-cm oblique incision, centered over the posterior superior iliac spine and in line with the iliac crest (inset). |
iliac crest. They can be avoided by placing the incision no more than 8
cm anterolateral to the posterior superior iliac spine. The nerves
supply sensation to the skin over the cluneal (gluteal) area. They are
composed of the posterior primary rami of L1, L2, and L3. Their loss
does not cause problems for the patient.
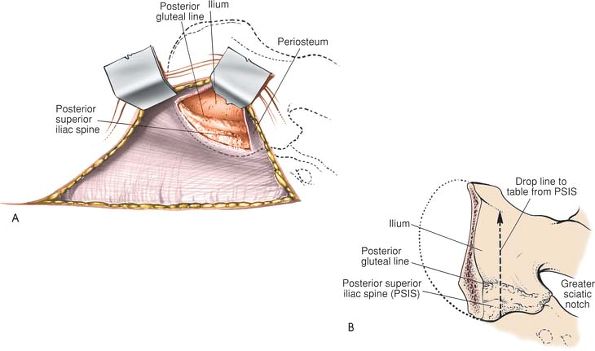
portion of the lateral surface of the ilium so that a large enough
graft can be obtained. Take care to stay in a subperiosteal plane while
passing from the iliac crest to the outer cortex of the ilium.
Proceeding 1.5 cm down the ilium in the area of the posterior superior
spine, the elevated posterior gluteal line can be seen and felt; pass
subperiosteally up over the line and then down its other side. Do not
err by letting the line direct the incision outward from bone into
muscle. A Taylor retractor will help the exposure by holding the
muscles laterally. Note that the posterior gluteal line separates the
origins of the gluteus maximus (posterior) from the gluteus medius
(anterior; Fig. 7-6).
which runs close to the distal end of the wound deep to the sciatic
notch; however, if an imaginary line is drawn from the posterior
superior iliac spine perpendicular to the operating table, and all work
is performed cephalad to it, both the notch and the nerve will be
avoided completely. If a larger graft is necessary, palpate the sciatic
notch itself before taking the graft (see Fig. 7-6B).
a branch of the internal iliac (hypogastric) artery, leaves the pelvis
via the sciatic notch, staying against the bone and proximal
to
the piriformis muscle. If a graft is taken too close to the sciatic
notch, the vessel may be cut and may retract into the pelvis. Nutrient
vessels from the artery supply the iliac crest bone along the
midportion of the anterior gluteal line, and the vessel may become an
osseous bleeder as it enters bone via the nutrient foramen. To control
bone bleeding, use bone wax on the raw cancellous surface of the pelvis
after the graft has been removed.
 |
|
Figure 7-6 (A) Subperiosteally, strip the musculature off the posterior portion of the lateral surface of the ilium. (B)
Proceeding down the outer surface of the ilium in the area of the posterior superior spine, the elevated posterior gluteal line can be seen and felt; pass subperiosteally up and over the line and then down its other side. Do not err by letting the line direct you outward from bone to muscle. If you draw an imaginary line from the posterior superior iliac spine perpendicular to the operating table and stay cephalad to it, you will avoid the sciatic notch and its contents. |
Breaking through the thick portion of the bone that forms the notch
disrupts the stability of the pelvis. Removal of bone from the false
pelvis proximal to the notch does not cause loss of stability (see Fig. 7-6B).
the bone to retract the gluteal muscles away from the bone and increase
the exposure. To increase the exposure further, lengthen the iliac
crest incision and strip more of the gluteal muscles from the outer
cortex to avoid working through a “keyhole.”
specifically for removing bone for graft material from the posterior
outer cortex of the ilium. Inner cortex also may be taken, but soft
tissues should not be stripped off the anterior (deep) aspect of the
ilium.
approach that is used almost exclusively for the open reduction and
internal fixation of a ruptured symphysis or internal fixation of a
displaced fracture of the superior pubic ramus. Other uses include
biopsy of tumors and treatment of chronic osteomyelitis.
associated with urologic damage, obtaining a urologic assessment is
advisable before undertaking open surgery, which often includes a
retrograde urethrogram. A urethral catheter must be inserted before
surgery. A full bladder will seriously interfere with the surgical
approach.
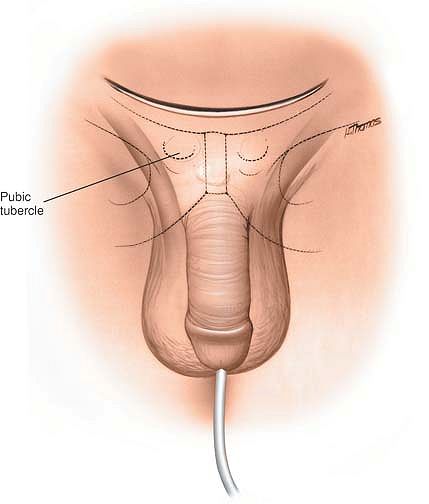
are easily palpable in all but the most obese patients. The pubic
symphysis will be palpable (as a gap) only in cases of rupture.
 |
|
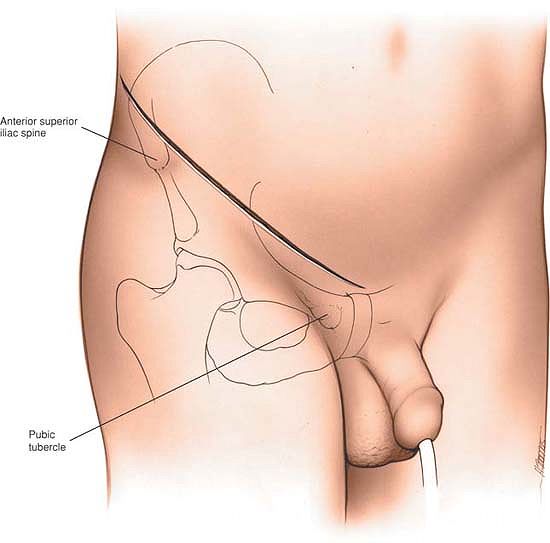
Figure 7-7
Palpate the pubic tubercles. Make a curved incision in the line of the skin crease, centering it 1 cm above the pubic symphysis. |
approach. Because the rectus abdominis muscles receive a segmental
nerve supply, they are not denervated, even though they are divided by
this approach.
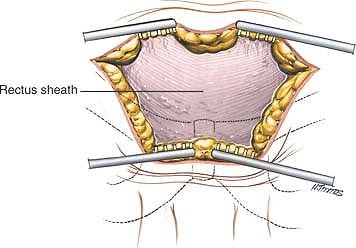
incision, deepening the incision down to the anterior portion of the
rectus sheath (Fig. 7-8). Identify, ligate, and
divide the superficial epigastric artery and vein that run up from
below across the operative field. Then, divide the rectus sheath
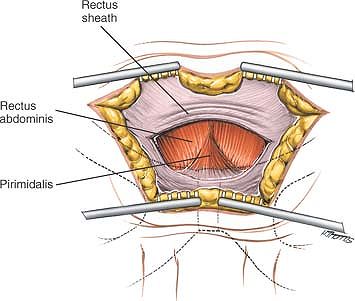
transversely,
about 1 cm above the symphysis pubis. The two rectus abdominal muscles now are visible (Fig 7-9).
In most cases of rupture of the symphysis pubis, one of these muscles
will have been detached from its insertion into the pubic symphysis.
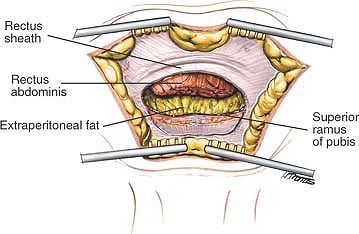
Divide the remaining muscle a few millimeters above its insertion into
the bone.
 |
|
Figure 7-8 Incise the fat in the line of the skin incision and retract the skin edges to reveal the anterior portion of the rectus sheath.
|
If access to the back of the symphysis is required, use the fingers or
a swab to push the bladder gently off the back of the bone. Palpation
of the posterior surface of the body of the pubis is useful to identify
the correct direction for the insertion of screws. This dissection is
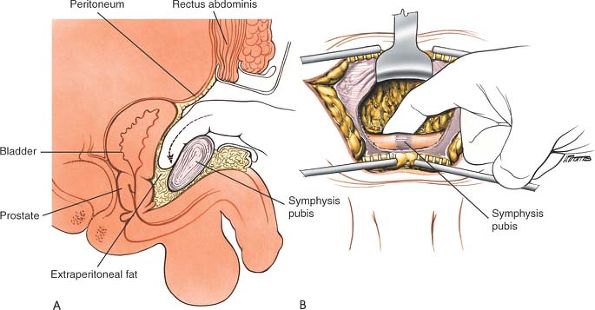
very easy to perform unless adhesions have formed due to damage to the
bladder. Such adhesions make it difficult to open up this potential
space (the preperitoneal space of Retzius) (Fig. 7-11). The pubic symphysis and superior pubic rami now are exposed adequately for internal fixation.
 |
|
Figure 7-9 Divide the rectus sheath transversely 1 cm above the symphysis pubis to reveal the rectus abdominis muscles and pyramidalis.
|
damaged during the trauma. If so, adhesions will have developed between
the damaged bladder and the back of the pubis. Mobilization of the
space of Retzius, therefore, may lead to inadvertent bladder rupture.
If fixation is considered in
the presence of urologic damage, it is best to operate in conjunction with an experienced urologic surgeon.
 |
|
Figure 7-10
Divide the rectus muscles 1 cm above their insertion and retract their cut edges superiorly to reveal the superior ramus of the pubis. |
in this area, it may be necessary to extend the skin incision and
superficial dissection in both directions to allow better visualization
of the deep structures in obese patients.
 |
|
Figure 7-11 (A) Open the plane behind the symphysis pubis, using your finger as a blunt dissector. (B) The pubic symphysis and superior pubic rami now are exposed.
|
safe, reliable access to that structure and allows anterior plates to
be positioned accurately across the joint. It also permits the exposure
of the inner wall of the ala of the ilium, allowing fixation of
associated iliac fractures. Paradoxically, although the sacroiliac
joint is one of the most posterior structures in the entire pelvic
ring, the anterior approach allows greater exposure and control than
does the seemingly more logical posterior approach, because of the
shape of the joint. Anteriorly, the joint is flat and directly
available, whereas posteriorly it is overhung by the posterior iliac
crest.
table and put a large sandbag under the buttock. The iliac crest should
be pushed up toward the surgeon. Support the opposite iliac wing with a
support attached to the operating table and then tilt the table 20°
away, allowing the mobile contents of the pelvis to fall away.
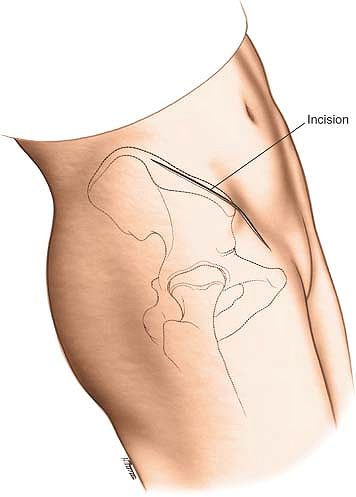
beginning 7 cm posterior to the anterior superior iliac spine (at about
the level of the iliac tubercle). Curve the incision forward until the
anterior superior iliac spine is reached. Continue the incision
anteriorly and medially along the line of the inguinal ligament for an
additional 4 to 5 cm (Fig. 7-12).
approach consists simply of stripping muscles off the pelvis; because
the bone is being approached via its subcutaneous surface, no muscle is
denervated.
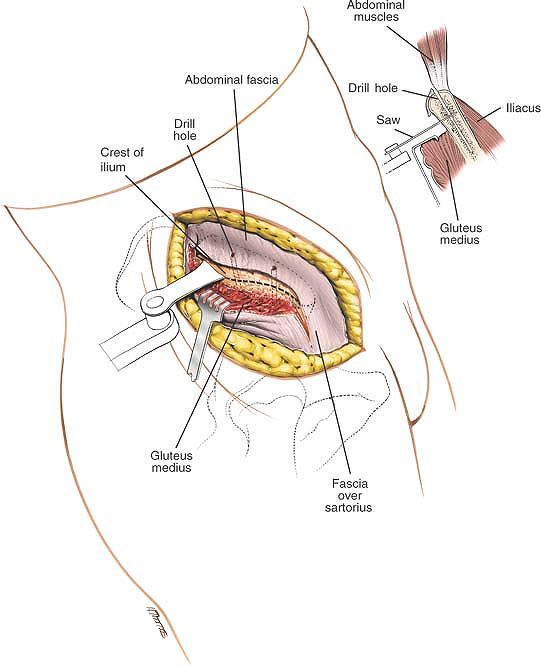
Expose the deep fascia overlying the glutei and tensor fasciae latae
muscles at the point where it attaches to the outer lip of the iliac
crest. Next, incise the periosteum of the entire anterior third of the
iliac crest and gently strip the muscles off the outer wall of the
pelvis to expose about 1 cm of the outer surface below the crest of the
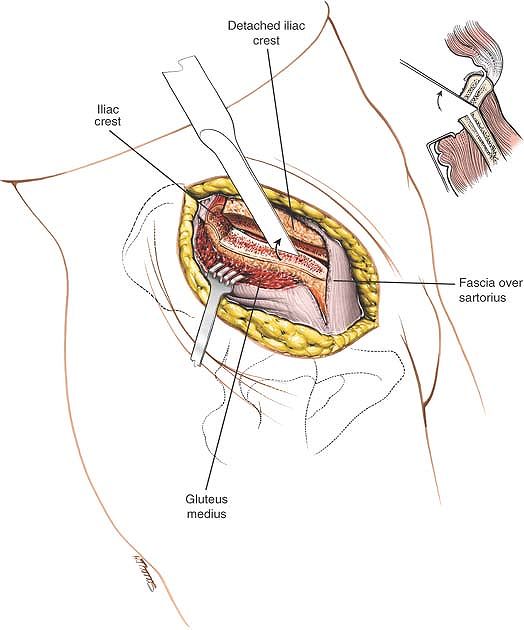
ilium. Predrill the iliac crest for easy reattachment. Using an
oscillating saw, transect the wing of the ilium at this level, cutting
only the outer cortex and the cancellous bone underneath (Fig. 7-13).
Next, crack the inner cortex with an osteotome. This allows the
anterior superior iliac spine to be detached along with the transected
portion of the iliac wing (Fig. 7-14).
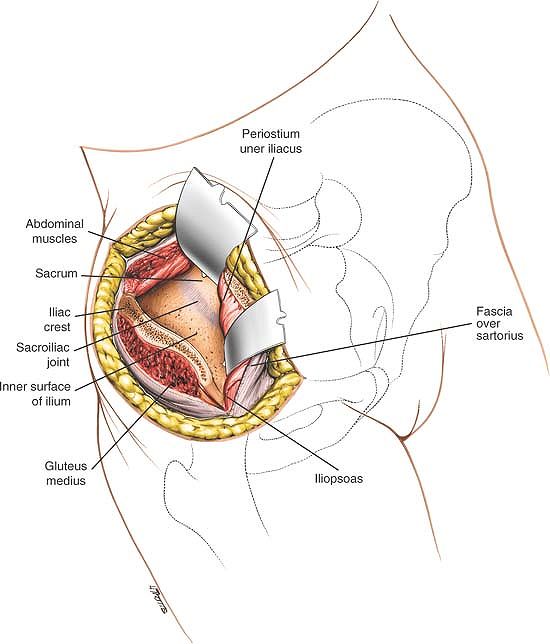
ilium; detach it by blunt dissection. As the dissection is deepened,
the detached anterior superior iliac spine, which still is attached to
the lateral end of the inguinal
ligament,
must be mobilized. This block of bone and muscle must be moved
medially; to accomplish this, divide some fibers of both the tensor
fasciae latae and sartorius muscles (Fig. 7-15).
Note that the lateral cutaneous nerve of the thigh is very close to the
anterior superior iliac spine and may have to be divided to permit this
mobilization.
 |
|
Figure 7-12
Make a curved incision over the iliac crest, beginning 7 cm posterior to the anterior superior iliac spine. Curve the incision anteriorly and medially along the line of the inguinal ligament for 5 cm. |
 |
|
Figure 7-13
Strip the muscles from the outer wall of the pelvis. Predrill the iliac crest. Divide the outer cortex 1 cm below the crest using an oscillating saw. |
iliacus muscle off the inner wall of the pelvis to expose the
underlying sacroiliac joint (see Fig. 7-15).
The distance is surprisingly short. As the muscle is stripped off, some
nutrient vessels will have to be detached from the inner wall of the
pelvis. Bleeding usually can be controlled by bone wax. Mobilizing the
iliacus muscle off the inside of the pelvis with a large bone block
allows the muscles to be reattached securely with screws during
closure. The muscle then resumes its anatomic position, and the dead
space beneath it is obliterated. Failure to securely reattach the iliac
crest will produce impaired function, a poor cosmetic result, possible
chronic pain, and a high risk of hematoma formation.
superior iliac spine. This will cause some numbness of the lateral aspect of the thigh.
 |
|
Figure 7-14 Crack the inner cortex using an osteotome to complete the iliac osteotomy.
|
they arise from the sacral foramina. For this reason, the dissection
cannot be carried further medially than the sacral foramina. The sacral
nerve roots are not usually exposed during this approach. They can be
at risk at two stages of the operation. If sharp pointed retractors
such as Homans are used medially, great care should be taken that the
point of these retractors is not inadvertently inserted into a sacral
foramen. Sacral nerve roots can also be entrapped under the medial end
of plates applied to the anterior surface of the sacroiliac joint.
Meticulous preoperative planning will allow you to know exactly how
many screw holes can be inserted safely into the sacrum without
endangering the sacral nerve roots. In most cases, only one screw can
be inserted.
the inner wall of the ilium. Bleeding from these vessels can be
controlled by pressure or bone wax.
posteriorly placed sacroiliac joint is adequate anterior dissection.
The lateral end of the inguinal ligament and its attached anterior
superior iliac spine must be mobilized to visualize the sacroiliac
joint adequately.
ilioinguinal approach that provides access to the entire anterior
column of the acetabulum. This approach is discussed in Chapter 8.
 |
|
Figure 7-15 Strip the iliacus from the inner wall of the pelvis to expose the underlying sacroiliac joint.
|
simple, safe approach that does not endanger any vital structures. Its
uses include open reduction and internal fixation of disruptions of the
sacroiliac joint, open reduction and internal fixation of fractures of
the ilium near the joint, and treatment of infections of the sacroiliac
joint or surrounding bones. The popularity of this approach has
diminished with the increasing use of percutaneous screw fixation
techniques. It is still, however, invaluable if adequate imaging is not
possible or if alternative techniques, such as plating, are used.
dislocations is difficult through this approach, especially the
correction of vertical displacement. Vertical displacement should be
corrected by longitudinal traction, preferably preoperatively.
demanding because of the shape of the joint and the presence of the
sacral nerve roots arising from the
sacral
foramina. Practice the direction of screw placement on a bone model
before surgery is attempted. During surgery, strict radiological
control of screw fixation using two plane C-arm imaging is mandatory.
Safe screw fixation can also be facilitated by the use of
computer-assisted surgery, if such technology is available to the
operating surgeon.
bolsters longitudinally to support the chest wall and pelvis; the
bolsters should allow the chest wall and abdomen to expand without
touching the table. Take great care during preparation and draping to
exclude the contaminated anal region from the operative field.
 |
|
Figure 7-16
Make a curved incision, beginning 3 cm distal and lateral to the posterior superior iliac spine. Cross the posterior superior iliac spine and continue along the crest to its highest point. |
crest, beginning 3 cm distal and lateral to the posterior superior
iliac spine. Extend the incision from this spot to the posterior
superior iliac spine and then continue along the crest to its highest
point (Fig. 7-16).
gluteus maximus and gluteus medius muscles must be detached partially
from their origins, but their individual neurovascular pedicles are
preserved easily.
incision. Anteriorly, small cutaneous nerves (the superior cluneal
nerves) may have to be cut, but they are of little clinical
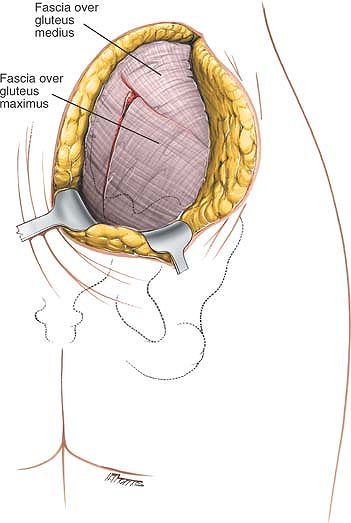
significance. Cut down into the outer border of the subcutaneous
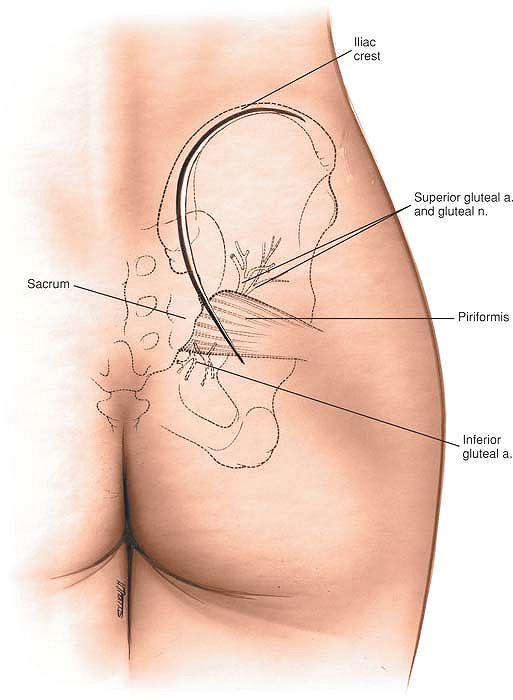
surface of the iliac crest to reveal the layer of fascia that covers
the gluteus maximus muscle. Detach the origin of the gluteus maximus
from the crest and carefully reflect the muscle downward and laterally (Fig. 7-17).
Two vital structures penetrate this muscle from its deep surface.
First, branches from the inferior gluteal artery, which emerge from the
pelvis, with the piriformis muscle through the greater sciatic notch,
penetrate the muscle. In addition, the inferior gluteal nerve emerges
from the notch beneath the piriformis to supply the muscle. Because it
is imperative that these two structures be preserved, they limit the
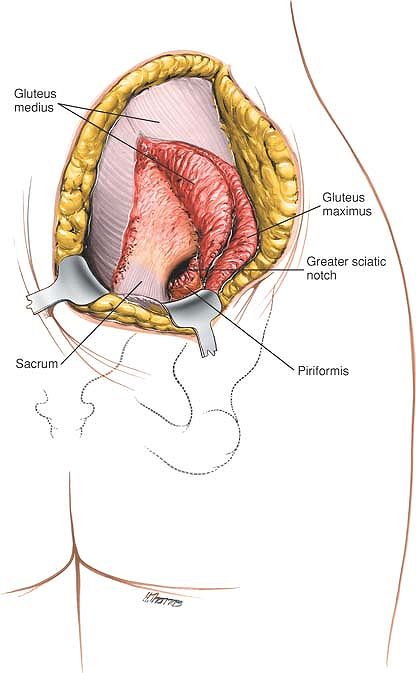
inferior mobilization of the muscle. As the gluteus maximus muscle is
reflected, the gluteus medius and piriformis muscles will be uncovered
as they emerge through the greater sciatic notch.
 |
|
Figure 7-17 Divide the subcutaneous fat and reflect the skin flap to reveal the fascia overlying the gluteus maximus and gluteus medius.
|
wing of the ilium. The muscle cannot be elevated much anteriorly
because its deep surface is tethered by its neurovascular bundle—the
superior gluteal nerves and vessels (Fig. 7-18). In cases of trauma, the ruptured sacroiliac joint or fracture is easily visible, but reduction is extremely difficult. To
evaluate any reduction, detach part of the origin of the piriformis
muscle from around the greater sciatic notch and insert a finger
through the notch to palpate the joint from its anterior surface. The
surface of the joint will feel smooth if it has been reduced (Fig. 7-19).
 |
|
Figure 7-18 Reflect the gluteus maximus muscle and the gluteus medius from the outer surface of the pelvis.
|
enters the deep surface of the gluteus maximus muscle. Overzealous
downward retraction of the muscle can cause a traction injury to this
nerve.
also enters the deep surface of the gluteus medius muscle. This limits
the forward retraction of this muscle, restricting the exposure of the
outer wing of the ilium. Excessive retraction of the muscle will injure
the superior gluteal nerve.
not endangered by the surgical approach but can be injured by
inaccurate screw fixation across the sacroiliac joint. Accurate x-ray
control of screw placement is mandatory.
gluteus medius and gluteus minimus muscles elevated from the outer side
of the iliac wing. This will enable more extensive fractures of the
wing and the ilium to be dealt with.
access via a subcutaneous portion of the bony pelvis. Thereafter,
access is afforded by stripping the muscular coverings off the bone
while remaining in a strictly subperiosteal plane. Using this
technique, the approaches avoid vital structures and, therefore, are
extremely safe. More muscles must be stripped and the view becomes
poorer, however, the further one proceeds from a subcutaneous part of
the bone. For this reason, these approaches are limited in the exposure
they provide. They cannot be extended and afford only limited access to
certain portions of the bony skeleton.
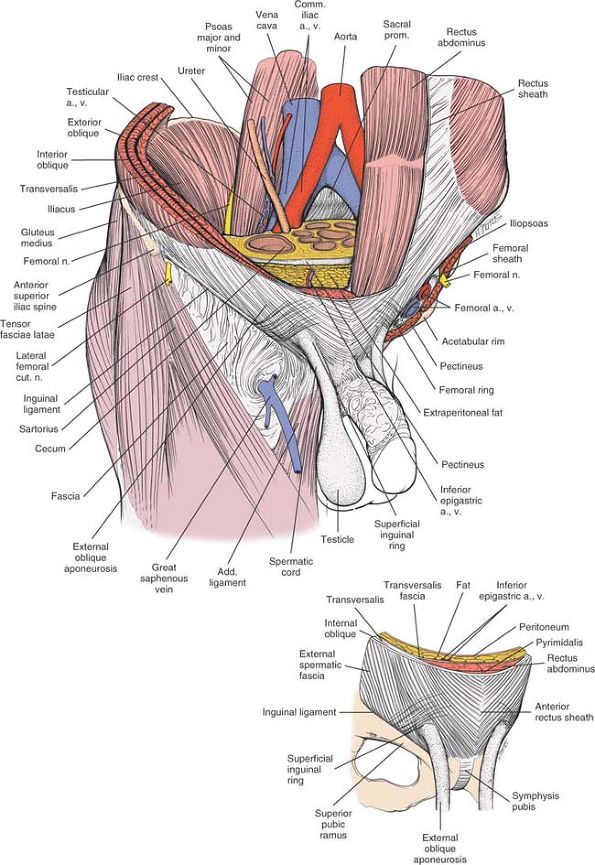
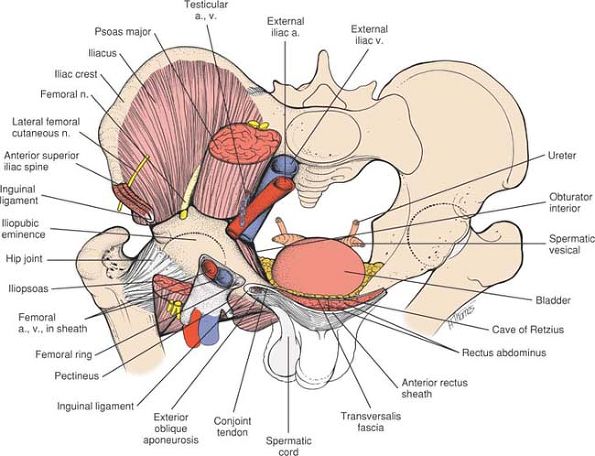
for access. The iliac crest has the external oblique and transversus
abdominis muscle arising from its surface. The wing of the ilium itself
is sandwiched between
two
masses of muscles, the glutei and tensor fasciae latae muscles on the
outer side, and the iliacus muscle on the inner side. The pubic
tubercles and upper parts of the superior pubic rami have the rectus
abdominis muscle attached to them, and these must be detached for
access to the superior surface of the structures.
is the site of insertion of the inguinal ligament and the sartorius
muscle. The anterior third of the iliac crest is the site of origin for
the external oblique, transversus abdominis, and tensor fasciae latae
muscles.
site of origin of the external oblique muscle. The posterior superior
iliac spine is marked by an overlying dimple. A line connecting these
dimples crosses the sacroiliac joint at the level of S2. The pubic
tubercle is the medial attachment of the inguinal ligament and the most
lateral part of the body of the pubis.
 |
|
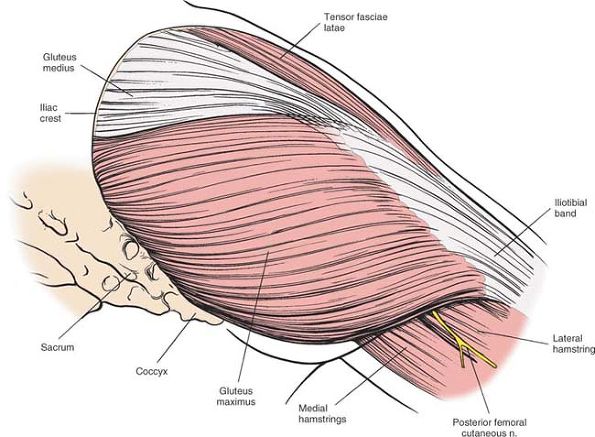
Figure 7-20 The superficial musculature of the posterior approach to the hip joint. The gluteus maximus predominates.
Gluteus Maximus. Origin.
From posterior gluteal line of ilium and that portion of the bone immediately above and behind it; from posterior surface of lower part of sacrum and from side of coccyx; and from fascia covering gluteus medius. Insertion. Into iliotibial band of fascia lata and into gluteal tuberosity. Action. Extends and laterally rotates thigh. Nerve supply. Interior gluteal nerve. |
of cleavage. Scars can be broad and ugly, however, but this rarely is
of clinical significance because they usually are covered with clothing.
consists of incising down onto the superficial portion of the bone. In
the iliac crest, this merely involves dividing the
overlying
fat. In the symphysis pubis, the rectus sheath must be opened. The
rectus sheath is a tough fibrous structure derived from all three
muscles of the anterior abdominal wall. It forms a tough anterior
covering to the underlying rectus muscle, which is easy to repair (see Fig 7-9).
anterior third of the iliac crest, but only from the outer aspect of
the posterior third of the crest.
detaching the origin of the tensor fasciae latae. Covering this muscle
is a thick layer of fascia that is continuous with the fascia covering
the gluteus maximus muscle. The tensor fascia latae, gluteus maximus
and the fascia can therefore be thought of as the outer layer of the
buttock anatomy (Fig. 7-20). This is analogous
to the position of the deltoid muscle in the shoulder. Deep to the
structures are the origins of the gluteus medius and gluteus minimus
muscles from the outer wing of the ilium. These can be lifted off the
bone entirely to provide a view of the wing of the ilium. It is
important to realize, however, that the rectus femoris muscle still
remains between the surgeon and the hip joint, thus limiting the
approach.
iliacus muscle. This can be lifted off the bone safely, providing
access down to the brim of the true pelvis.
joint, yet any movement is very difficult to demonstrate. The joint is
reinforced heavily by anterior and posterior supporting ligaments.
Approached from the front, the sacroiliac joint is perpendicular to the
plane of dissection. Approached from the rear, the joint is overhung by
the posterior iliac crest, making it oblique to the plane of
dissection. It is critically important to appreciate this obliquity
when planning the insertion of any screws that may be used to cross the
joint.
joint, but a secondary cartilaginous joint. Its superior surface is
readily accessible once the insertion of the rectus abdominis muscle
has been detached. Behind the symphysis pubis is a potential space
filled with loose areola tissue; this is known as the cave of Retzius.
This potential space lies between the symphysis pubis and the bladder,
and allows access to the inner surface of the pubis down to the muscles
of the pelvic floor.
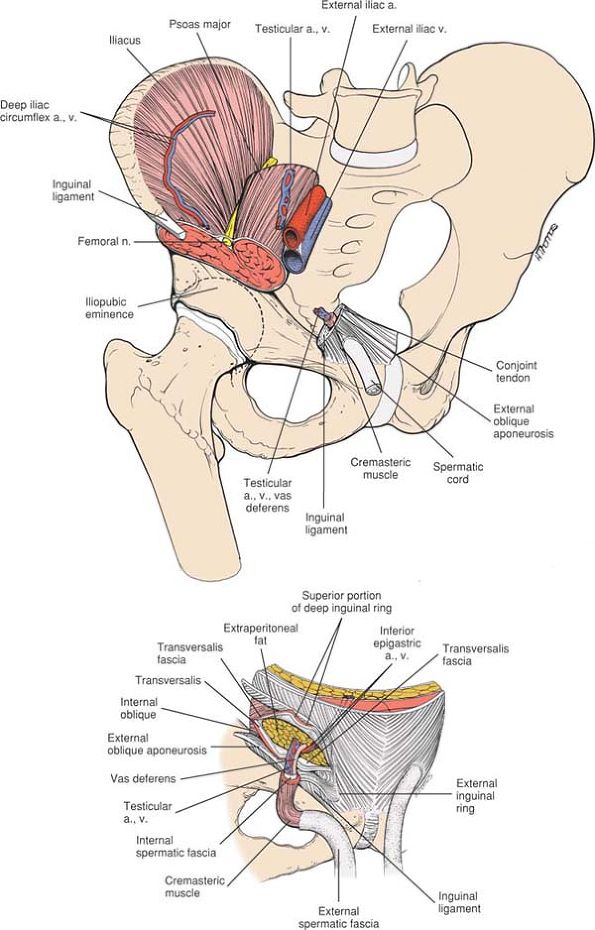
It allows visualization of the anterior and medial surfaces of the
acetabulum and is, therefore, suitable for exposure of anterior column
fractures of the acetabulum. It also allows insertion of screws into
the posterior column. The dissection involves isolating and mobilizing
the femoral vessels and nerve, as well as the spermatic cord in the
male and the round ligaments in the female. Because orthopaedic
surgeons usually do not operate in this area, operating in conjunction
with a general surgeon may be advisable. Alternatively, cadaveric
dissection should be performed before embarking on this exposure.
greater trochanter at the edge of the table. This allows the buttock
muscles and gluteal fat to fall posteriorly away from the operative
plane. Insert a urinary catheter. A full bladder will obscure vision.
thumbs medially along the inguinal creases and obliquely downward until
you can feel the pubic tubercle.
anterior superior iliac spine. Extend the incision medially, passing 1
cm above the pubic tubercle to end in the midline (Fig. 7-22).
 |
|
Figure 7-21
The ilioinguinal approach allows access to the anterior column and medial aspect of the acetabulum. It also allows visualization of the inner aspect of the pelvis from the sacroiliac joint to the symphysis pubis. |
 |
|
Figure 7-22
Make a curved anterior incision beginning 5 cm above the anterior superior iliac spine. Extend the incision medially, passing just above the pubic tubercle to end in the midline. |
 |
|
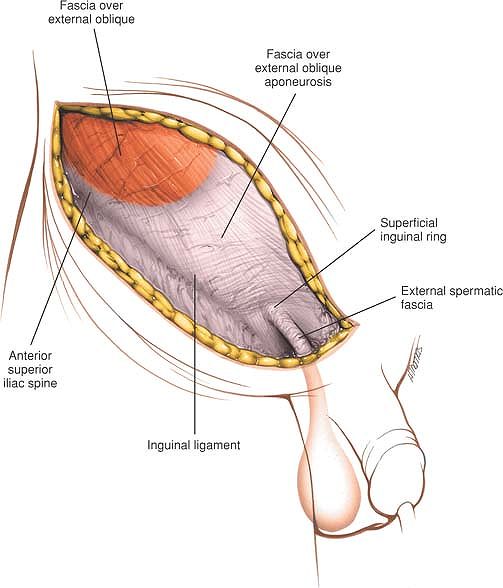
Figure 7-23 Dissect through subcutaneous fat in the line of the skin incision to expose the aponeurosis of the external oblique muscle.
|
consists essentially of lifting off muscular, nervous, and vascular
structures from the inner wall of the pelvis.
The lateral cutaneous nerve of the thigh will appear in the lateral
edge of the dissection. In most cases, the nerve will need to be
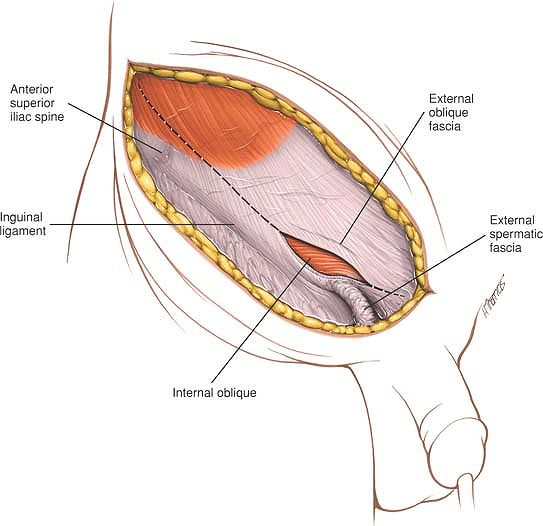
divided. Divide the aponeurosis of the external oblique muscle in the
line of its fibers from the superficial inguinal ring to the anterior
superior iliac spine (Fig. 7-24). This will
expose the spermatic cord in the male and the round ligament in the
female. Carefully isolate these structures in a sling (Fig. 7-25).
Continue the dissection medially, dividing the anterior part of the
rectus sheath to expose the underlying rectus abdominis muscle. Strip
the iliacus muscle from the inside of the wing of the ilium. Initially,
you will need to use sharp dissection, but once inside the pelvis, use
blunt dissection.
proximal to its insertion into the symphysis pubis. Using blunt
dissection, develop a plane between the back of the symphysis pubis and
the bladder. This space (the Cave of Retzius) is easily developed with
a finger.
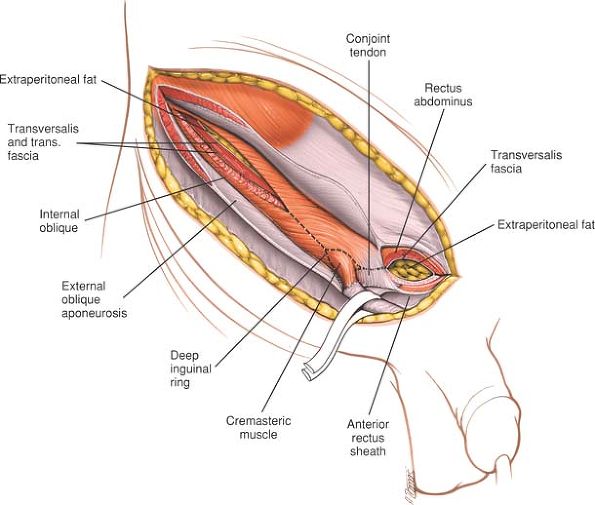
transversus abdominus muscles that form the posterior wall of the
inguinal canal (Fig. 7-26). Take care when approaching the deep inguinal ring; the inferior epigastric artery and vein cross the posterior
wall of the canal at the medial edge of the deep inguinal ring and must
be ligated at that point. Inadvertent division of these structures
results in profuse hemorrhage that is difficult to control. Now divide
those fibers of the transversus abdominus and internal oblique muscles
that arise from the lateral half of the inguinal ligament (Fig. 7-27).
 |
|
Figure 7-24 Divide the aponeurosis of the external oblique muscle from the superficial inguinal ring to the anterior superior iliac spine.
|
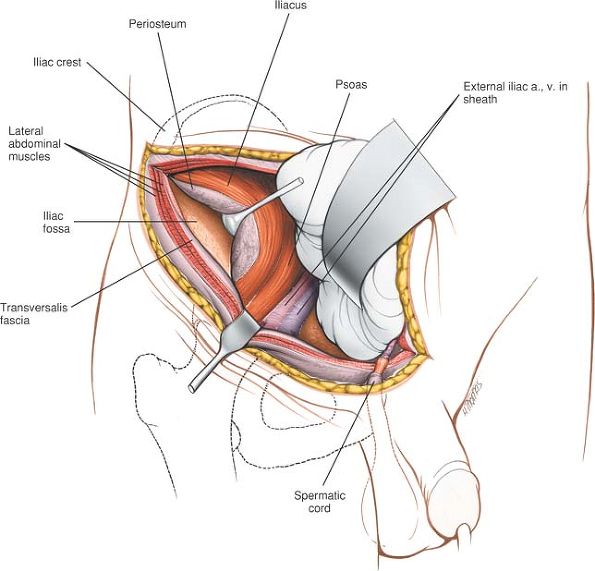
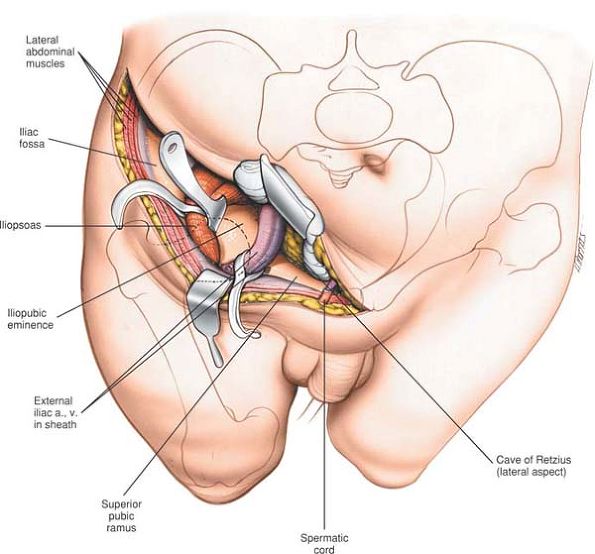
exposed. Using a swab, push the peritoneum upward to reveal the femoral
vessels, the femoral nerve, and the tendon of iliopsoas (Fig 7-28).
Isolate the femoral vessels together in the femoral sheath and protect
them with a sling. Pass a second sling around the tendon of iliopsoas
with the femoral nerve lying on top of it (Fig. 7-29).
Retract these structures either medially or laterally to gain access to
the underlying medial surface of the acetabulum and superior pubic
ramus (Fig. 7-30).
to the iliopsoas gives access to the inner surface of the ilium. The
middle window, medial to the iliopsoas but lateral to the femoral
artery and vein gives access to the quadrilateral plate. The medial
window, medial to the femoral artery and vein gives assess to the
superior pubic ramus and symphysis. For best visualization of the
medial window, the surgeon should move to stand on the opposite side of
the patient. Tilting the operating table also improves visualization of
the medial window.
beneath the inguinal canal lying on the iliopsoas muscle. Take care to
avoid vigorous retraction, as stretching the nerve will result in a
paralysis of the quadriceps muscle.
of the thigh will almost certainly have to be divided around the
anterior superior iliac spine at this stage of dissection. If it is
possible to retract it without compromising the exposure, do so.
Dividing the nerve will leave a patch of numbness on the outer side of
the thigh.
 |
|
Figure 7-25 Mobilize the spermatic cord or round ligament in a sling. The posterior wall of the inguinal canal is now exposed.
|
pass beneath the inguinal ligament are surrounded by a funnel-shaped
fascial covering called the femoral sheath. It is this sheath that
should be mobilized and held between slings rather than dissecting out
the artery and vein separately. Care should be taken on retraction of
these structures to minimize the risk of deep vein thrombosis. The
femoral sheath contains the femoral artery and vein, and medial to the
vein is a space known as the femoral canal. The femoral canal contains
efferent lymph vessels, but also provides a dead space into which the
femoral vein can expand. This space can also, however, contain a
femoral hernia, and this should be remembered when mobilizing the
structure.
crosses the operative field passing medial to the deep inguinal ring.
It will need to be ligated to allow access to the deeper structures.
The inferior epigastric vein may be
damaged during dissection at the medial end of the approach. It is
usually avulsed from the side of the femoral vein. This causes a
profuse hemorrhage and requires the sewing of the resultant vascular
defect in the side of the vein.
the vas deferens and testicular artery. Although it is easily
mobilized, it must be treated gently during the approach and the
closure to avoid ischemic damage to the testicle.
mobilized off the back of the symphysis pubis. Be aware that fractures
of the lower half of the anterior column, especially displaced fracture
of the superior pubic rami, may have caused bladder damage and
adhesions.
 |
|
Figure 7-26
Divide the rectus abdominal muscle 1 cm proximal to its insertion into the symphysis pubis. Divide the muscles forming the posterior wall of the inguinal canal. |
 |
|
Figure 7-27
Ligate and divide the inferior epigastric vessels. Complete the division of the muscular structures of the posterior wall of the inguinal canal. |
 |
|
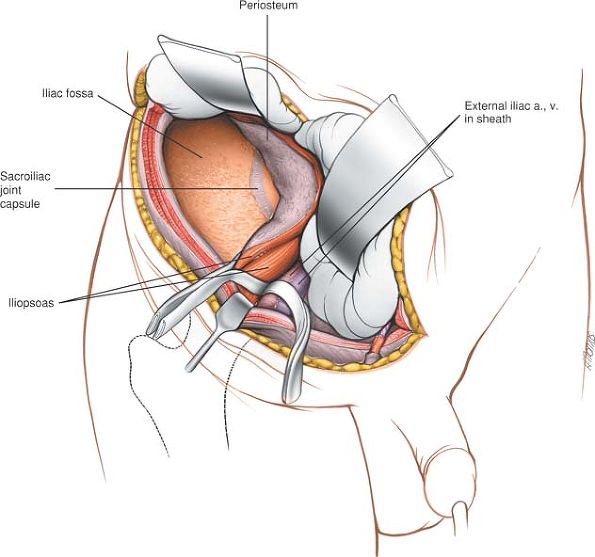
Figure 7-28
Using a swab, push the peritoneum upwards to reveal the femoral vessels. Mobilize the iliacus muscle from the inner aspect of the ilium. |
sacroiliac joint. Extend the skin incision posteriorly, following the
iliac crest. Using sharp dissection, cut down onto the bone. Then strip
off the origins of the iliacus from the inside of the ilium using blunt
dissection. Retract this iliacus medially to expose the inner wall of
the ilium and the sacroiliac joint (see Fig. 7-30).
 |
|
Figure 7-29
Continue stripping off the iliacus from the inner wall of the ilium to reveal the sacroiliac joint. Pass the sling around the femoral sheath. |
 |
|
Figure 7-30
Retract the iliopsoas and the femoral sheath either medially or laterally to reveal the medial surface of the acetabulum, the superior pubic ramus, and the inner surface of the ilium round to the sacroiliac joint. |
-
Lateral and posterior to the anterior superior iliac spine.
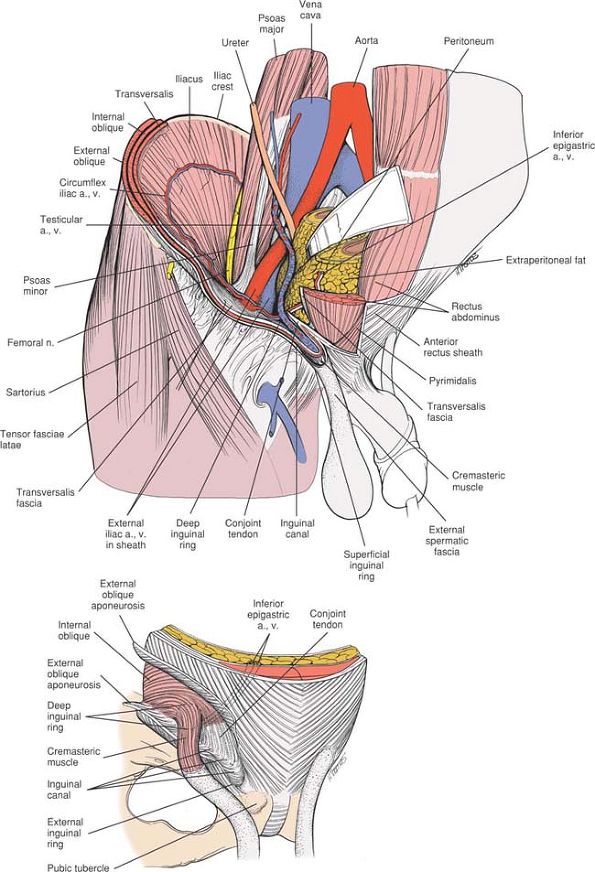
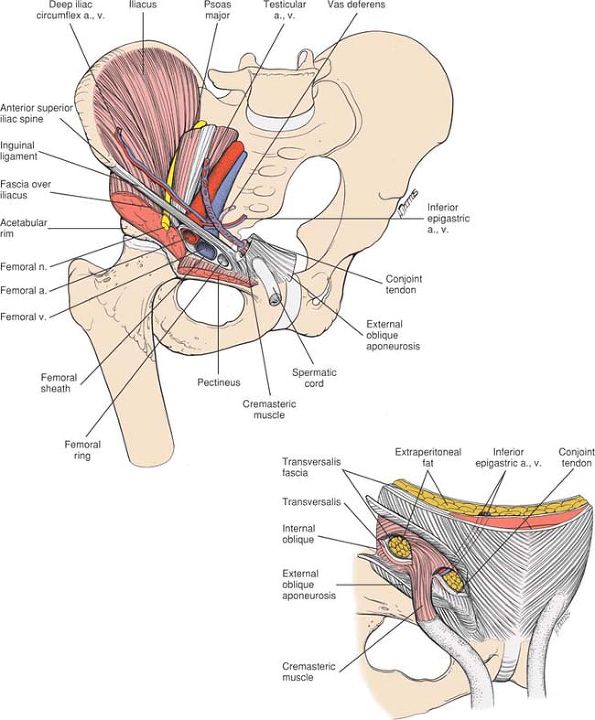
The dissection consists of detaching those muscles that arise from or
insert into the iliac crest and the inner wall of the ilium using
subperiosteal dissection. -
Medial and anterior to the anterior superior iliac spine.
The applied anatomy of the approach is that of the inguinal canal and
its related structures. Because pathology in this area nearly always
relates to herniae, both inguinal and femoral, it is usually an
unfamiliar ground for orthopaedic surgeons and, thus, is potentially
hazardous.
-
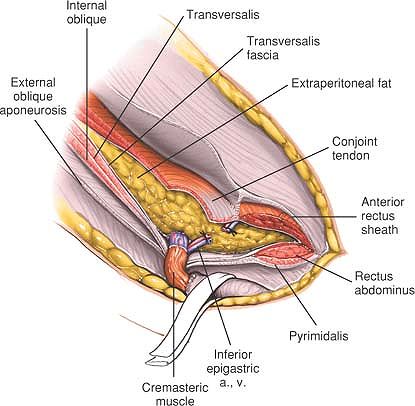
The external oblique
forms the outer layer of the muscles of the anterior abdominal wall. It
originates from the outer strip of the anterior half of the iliac crest. -
The internal oblique
forms the middle layer of the muscles of the anterior abdominal wall.
It originates from the center strip of the anterior half of the iliac
crest. -
The tensor fasciae latae arises from the outer lip of the anterior half of the iliac crest.
covered by the spermatic cord in the male and the round ligament in the
female.
cleavage in the skin. However, the extensive dissections involved may
leave rather broad scars. They are nearly always hidden by clothing.
which is the outer layer of the abdominal muscles, arises from the
lower eight ribs. It inserts as fleshy fibers into the anterior half of
the iliac crest. However, from the anterior superior iliac spine, it
becomes aponeurotic. The aponeurosis attaches to the pubic tubercle and
medially becomes fused with the aponeurosis of the opposite external
oblique muscle to form the anterior part of the rectus sheath.
Therefore, the splitting of the fibers of the external oblique muscle
and the incision of the anterior rectus sheath are both in the same
plane. There is a free lower border of this muscle between the anterior
superior iliac spine and the pubic tubercle. This free edge is called
the inguinal ligament. The aponeurosis curls back on itself to form a
gutter, and the free edge of this gutter is the origin of part of the
internal oblique and transversus abdominis muscles.
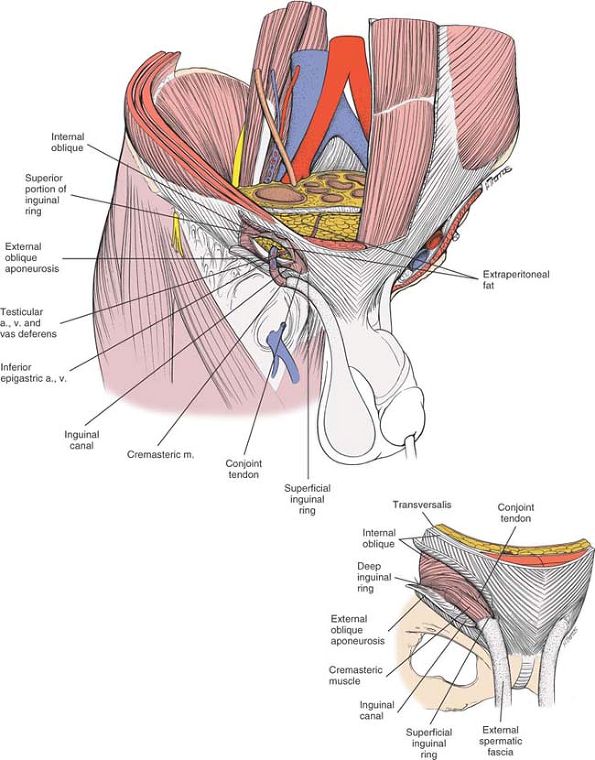
Dividing the fascia of the external oblique opens up the inguinal
canal, which is an oblique intramuscular slit running from the deep to
the superficial inguinal rings. These contain the spermatic cord in the
male and the round ligament in the female (Fig. 7-32).
fascia. In the region of this approach, however, the posterior layer of
fascia is inferiorly deficient. The anterior rectus sheath also
receives some tissue from both the internal oblique and transversus
abdominis muscles.
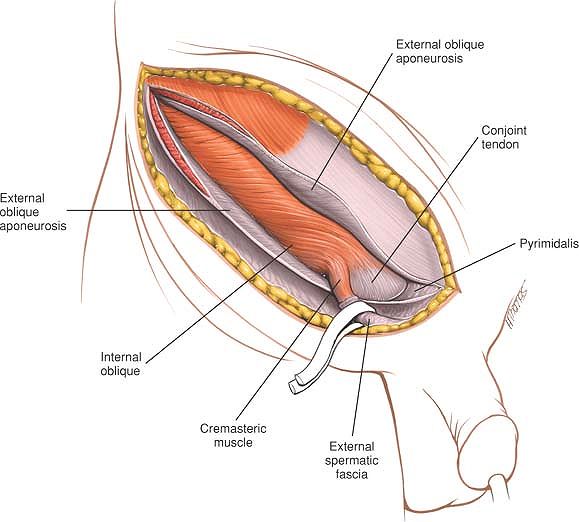
accompanied by its artery and the testicular artery and vein. As these
structures emerge through the abdominal wall, they get coverings from
each layer they pass through (Fig. 7-33). The
transversalis fascia covers the cord with a thin layer of tissue known
as the internal spermatic fascia. Passing through the transversus
abdominis and internal oblique, the cord gets covered with a layer of
muscle known as the cremasteric muscle. As it passes through the
external oblique at the superficial inguinal ring, it is covered by a
thin layer known as the external spermatic fascia. The round ligament
in the female is also covered by these three fascial layers. Both the
spermatic cord and round ligament can be mobilized easily in the
inguinal canal during the superficial surgical dissection.
 |
|
Figure 7-31
The superficial musculature of the inguinal region. Just above the pubic tubercle, there is a gap in the aponeurosis of the external oblique to allow the passage of the spermatic cord in the male and the round ligament in the female. This gap is known as the superficial inguinal ring (inset). |
 |
|
Figure 7-32
Dividing the external oblique muscle opens up in the inguinal canal. The spermatic cord is revealed covered by the cremasteric muscle, a muscle derived from the internal oblique muscle (inset). |
 |
|
Figure 7-33
As the testis migrates out through the anterior abdominal wall in fetal development, it and its vas deferens get coverings from each layer they pass through. The external oblique provides the external spermatic fascia. The internal oblique provides the cremasteric muscle and the transversus abdominis provides the internal spermatic fascia. The cord is retracted to reveal the posterior wall of the inguinal canal formed by the conjoint tendons (inset). |
posterior wall of the inguinal canal is seen. In the lateral half of
the inguinal canal, the rolled free edge of the external oblique
aponeurosis gives origin to muscle fibers from both the internal
oblique and the transversus abdominis. These muscle fibers arch up over
the spermatic cord and fuse to form a conjoint tendon that is attached
posterior to the spermatic cord into the pubic crest. Therefore, in the
medial half of the inguinal canal, its posterior wall consists of this
conjoint tendon, which needs to be divided for access to the underlying
structures. The spermatic cord exits from the abdominal cavity through
the deep inguinal ring to enter the inguinal canal. Lateral to the deep
inguinal ring, fibers of the internal oblique and transversus abdominis
arise from the inguinal ligament and also have to be divided (see Fig. 7-33). Medial to the deep inguinal ring lies the inferior epigastric artery,
which usually requires ligation. Deep to these muscles lies the thin
transversalis fascia, extraperitoneal fat, and finally the peritoneum (Fig. 7-35).
inguinal canal. Careful repair of all these structures on a
layer-by-layer basis is important to prevent the development of an
inguinal hernia.
arises from the anterior aspect of the lumbar spine and passes into the
thigh below the middle of the inguinal ligament. Between these two
muscles, the femoral nerve runs down into the thigh. It is intimately
related to the iliopsoas and is mobilized with the muscle to avoid
excessive retraction. Medial to the nerve, the femoral artery and vein
enter the thigh. As these vessels leave the abdomen, they take with
them a fascial layer derived from the extraperitoneal fascia. This is
known as the femoral sheath. In addition to the artery and vein, the
femoral sheath has a space in it, medial to the vein, known as the
femoral canal. This is used for the passage of lymphatic vessels and
also allows the vein to expand at times when the blood return from the
leg becomes increased.
Because the femoral artery and vein are enclosed in a common fascial
sheath, they should be mobilized together. Separate mobilization of the
femoral vein will traumatize it, leading to possible thrombosis.
from the pubic bones by a space known as the Cave of Retzius. It is
occupied by very thin tissue, the bladder, and, in the case of the
male, the prostate. The prostate can be easily mobilized from the back
of the pubis. However, in cases of fracture, there may be pathologic
adhesions in this area, and great care should be taken not to
accidentally produce a bladder rupture. A full bladder will make safe
access to this area impossible, and a urinary catheter inserted
preoperatively is vital (Fig 7-36).
 |
|
Figure 7-34
Deep to the inguinal ligament run the femoral nerve, the femoral vessel, as well as the psoas and iliacus muscles. Medial to the deep inguinal ring lies the inferior epigastric vessels (inset). |
 |
|
Figure 7-35 Division of the posterior wall of the inguinal canal reveals the extraperitoneal fat.
|
 |
|
Figure 7-36
The medial aspect of the acetabulum can be exposed by retraction of the iliopsoas and the femoral sheath. The inner aspect of the superior pubic ramus can only be visualized by careful mobilization of the bladder. |
It also allows direct visualization of the dorsocranial part of the
acetabulum, either through the fracture gap or via a capsulotomy. It is
by far the easiest of all acetabular approaches, and extensive blood
loss is not usually encountered. The approach does not allow access to
the anterior column. Its uses include reduction and fixation of:
-
Fractures of the posterior lip of the acetabulum
-
Fractures of the posterior column
-
Fractures of the posterior lip and posterior column
-
(Juxta- and infratectal) Simple transverse fractures
-
Transverse fractures with associated posterior lip fractures
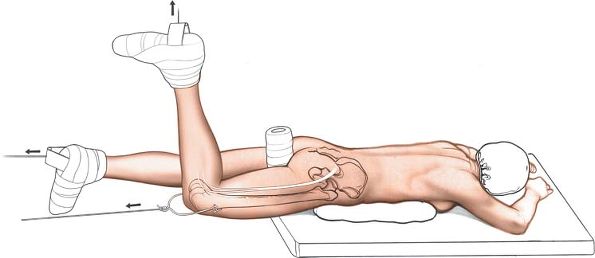
used for fractures of the posterior lip and/or posterior column, place
the patient in the lateral position.
If traction is to be used, place a skeletal pin transversely through
the lower end of the femur with the knee flexed to reduce the risk of a
traction injury to the sciatic nerve.
 |
|
Figure 7-37
The posterior approach to the acetabulum allows access to the posterior column, posterior lip, and dome segment of the acetabulum. |
natural tendency for the femoral head to move medially in cases of
transverse acetabular fracture. Operating in the lateral position,
therefore, makes reduction of these fractures more difficult. Reduction
of the fracture in this position can only be obtained by an assistant
lifting the femoral head out of the acetabulum. The use of the prone
position facilitates reduction of transverse fractures.
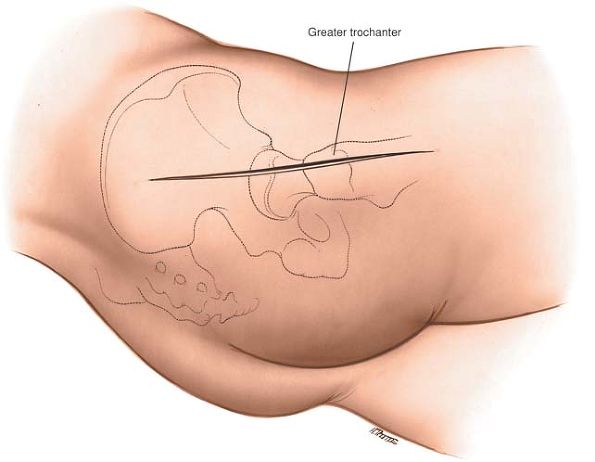
the thigh. Note that the posterior edge is easier to palpate than the
anterior one.
trochanter extending from just below the iliac crest to 10 cm below the
tip of the greater trochanter (Fig. 7-39).
 |
|
Figure 7-38
Position of the patient for posterior approach to the acetabulum. Note the flexed position of the knee to prevent stretching of the sciatic nerve. |
 |
|
Figure 7-39
Make a longitudinal incision centered on the greater trochanter extending from just below the iliac crest to 10 cm below the greater trochanter. |
 |
|
Figure 7-40
Incise the fascia lata in line with the skin incision. Extend the incision superiorly along the anterior border of the gluteus maximus muscle. |
However, the gluteus maximus that is split in the line of its fibers is
not significantly denervated because it receives its nerve supply well
proximal to the split.
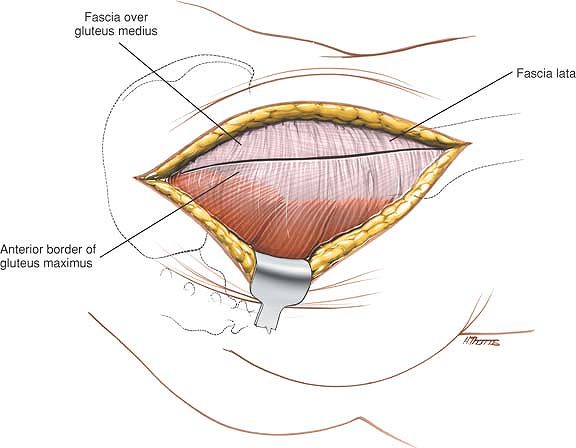
fascia lata in the line of the skin incision in the lower half of the
wound, and extend this incision superiorly along the anterior border of
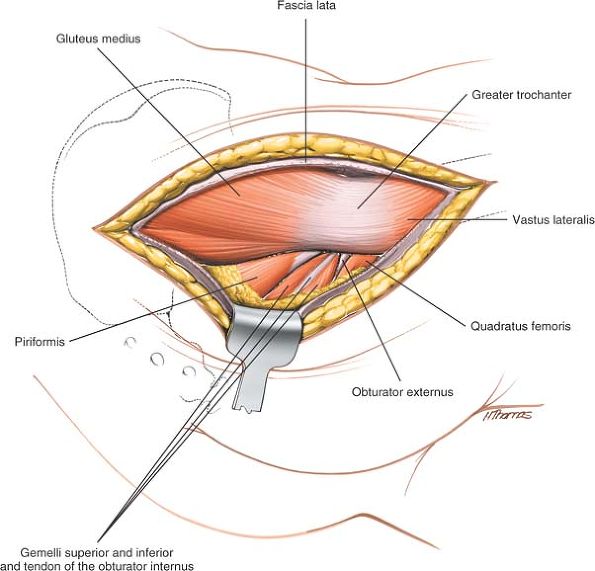
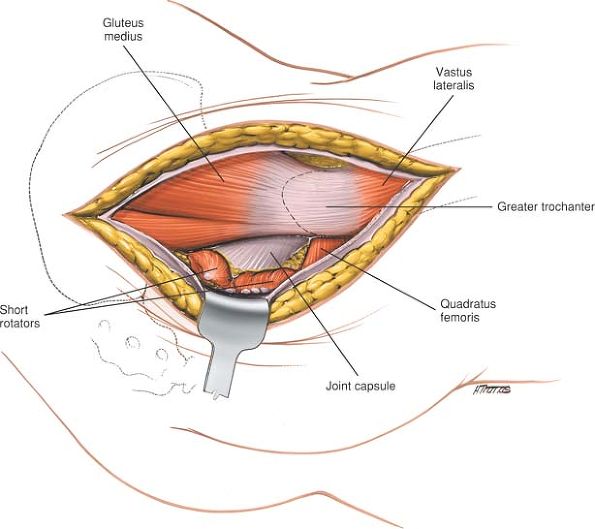
the gluteus maximus muscles (Fig. 7-40). Retract the split edges of the fascia to reveal the piriformis muscle and the short external rotators of the hip (Fig. 7-41). Partial detachment of the insertion of gluteus maximus from the femur will facilitate mobilization of this muscle.
rotators and the piriformis on the stretch and detach these muscles as
they insert into the femur (Fig. 7-42). Using
the short external rotator muscles as a cushion, carefully insert a
retractor into the greater sciatic notch. Do not apply great pressure
on this retractor as this will create a sciatic nerve palsy. Insert a
second retractor into the lesser sciatic notch to expose the posterior
column in its whole extent.
often torn or detached in cases of trauma. If the posterior capsule is
intact and a direct inspection of the joint is required, make a
T-shaped capsulotomy. Ensure that you avoid damage to the limbus when
incising the capsule.
by distracting the femoral head. This can either be achieved by
skeletal traction or with the help of a Schanz screw placed in the
femoral head.
adequately visualized and fixed at this stage. If you require more
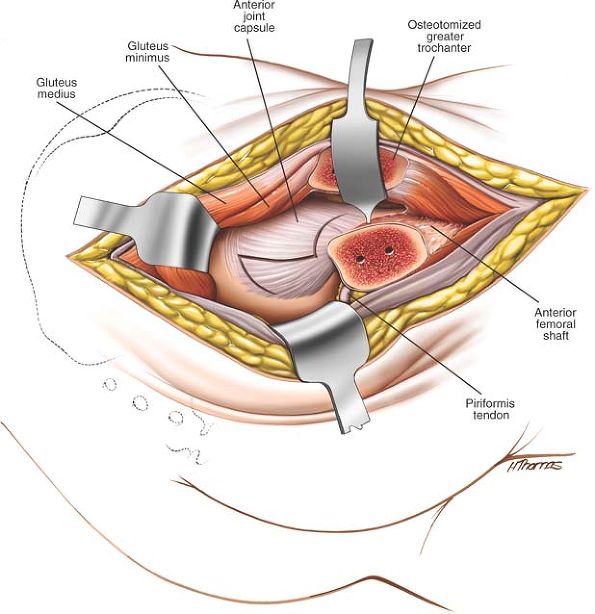
extensive exposure of the posterior column, perform an osteotomy of the
greater trochanter. Divide the greater trochanter from posterior to
anterior, removing a piece of bone 5 mm in size. This bone will have
the gluteal muscles attached to it superiorly and the vastus lateralis
attached to it inferiorly. Progressively evert the trochanter with its
attached muscles over the anterior surface of the femur using a sharp
retractor. The small remaining attachment of
gluteus
medius to the intertrochanteric ridge will now need to be released. If
difficulty is encountered mobilizing the fragment, the insertion of
piriformis may sometimes need to be partially released.
 |
|
Figure 7-41 Retract the split edges of the fascia to reveal the piriformis muscle and the short external rotators of the hip.
|
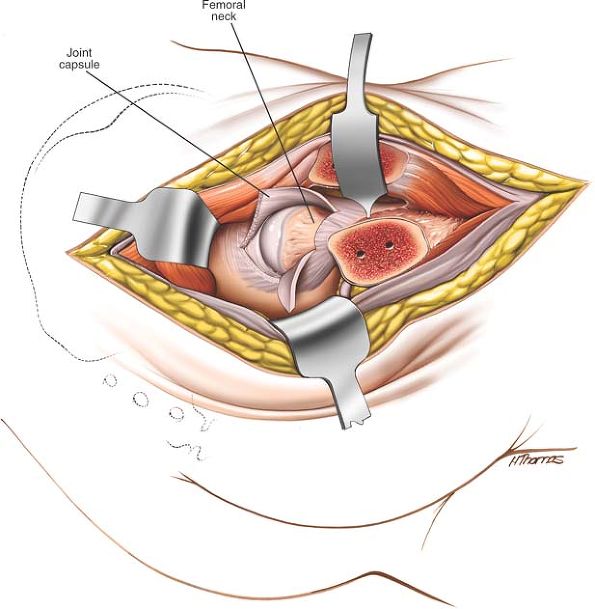
joint capsule, flex and externally rotate the hip. Mobilize the
insertion of gluteus minimus from the retroacetabular surface along the
superior capsule to its femoral insertion along the anterior aspect of
the trochanter (Fig. 7-43). If further exposure
of the anterior capsule is required, mobilize the proximal portion of
the vastus intermedius from the femur to allow access to the anterior
hip joint capsule (Fig. 7-44). This
trochanteric fragment can be reattached easily with screws during
closure. Note that trochanteric osteotomies are associated with
heterotopic bone formation in acetabular surgery.
contused by the original trauma. Great care must be taken throughout
the operation that the nerve is not forcibly retracted. The divided
external rotators will protect the nerve from direct trauma, but the
nerve may still be injured by indirect forces transmitted through the
retractor. The nerve is in most danger if a fracture table with
continuous traction is used. You must be certain that the knee is
flexed to avoid stretching the nerve.
leaves the pelvis beneath the piriformis. This vessel may be damaged by
the original fracture or the artery may be injured during
the
surgical dissection. If the artery is transected, it will retract into
the pelvis and bleeding will be brisk. To control the bleeding, apply
direct pressure, then turn the patient over into the supine position.
If the artery has retracted into the pelvis, vascular control can only
be achieved by tying off the external iliac artery via a
retroperitoneal approach.
 |
|
Figure 7-42 Divide the short external rotator muscles and the piriformis as they insert into the femur.
|
leaves the pelvis above the piriformis and enters the deep surface of
the gluteus medius. This attachment tethers the muscle, limiting the
amount of upward retraction of the muscle and prevents you from
reaching the iliac crest.
difficult because of the presence of an intact femoral head. In
addition to using longitudinal femoral traction, specialized femoral
head retractors are available that allow the head to be partially
dislocated, thereby facilitating clear visualization of the dome of the
acetabulum. It is critically important to obtain good visualization of
the inside of the joint because the screws used for internal fixation
may penetrate the joint.
level of the knee. Either split the vastus lateralis or elevate it from
the lateral intermuscular septum to allow exposure of the lateral
surface of the entire shaft of the femur.
 |
|
Figure 7-43
For access to the anterior hip joint capsule, flex and externally rotate the hip. Mobilize the insertion of the gluteus medius from the retroacetabular surface. |
 |
|
Figure 7-44
To complete exposure of the anterior capsule, mobilize the vastus intermedius from the femur. Perform a T-shaped capsulotomy of the anterior hip joint capsule to expose the femoral head and neck, together with the anterior lip of the acetabulum. |
KJ, Hoek van Dijke GA, Joosse P et al: External fixators for pelvic
fractures: comparison of the stiffness of the current systems. Acta
Orthop Scand 74:165, 2003
KA, Gautier E, Woo AK et al: Surgical dislocation of the femoral head
for joint debridement and accurate reduction of fractures of the
acetabulum. J Orthop Trauma 16:543, 2002
DC, Graney DO, Routt ML: Retropubic vascular hazards of the
ilioinguinal exposure: a cataveric and clinical study. J Orthop Trauma
10:156, 1996