The Spine
The cervical spine is light, small, and flexible; the thoracic spine is
larger and relatively immobile because of its associated ribs. The
lumbar spine, especially the lower part, has more mobility than the
thoracic spine, but less than the cervical spine. Pathology is seen
most commonly in the cervical and lumbar spines, which are the most
mobile portions of the axial skeleton; they require surgery most
frequently.
through either an anterior or a posterior approach to treat pathology
of its anterior and posterior elements. Pathologies such as vertebral
body infection, fracture, and tumor often require anterior approaches.
There are many anterior approaches to the spinal column; we present the
basic ones that allow access to all the anterior parts of the spine.
posterior approaches are the most common, permitting access to all the
posterior spinal elements, as well as to the spinal cord and
intervertebral discs.
the ilium is the best site from which to obtain bone graft material,
this chapter concludes with the anterior and posterior approaches to
the ilium that are used in conjunction with spinal approaches.
the lumbar spine. Besides providing access to the cauda equina and the
intervertebral discs, it can expose the posterior elements of the
spine: the spinous processes, laminae, facet joints, and pedicles. The
approach is through the midline, and it may be extended proximally and
distally.
-
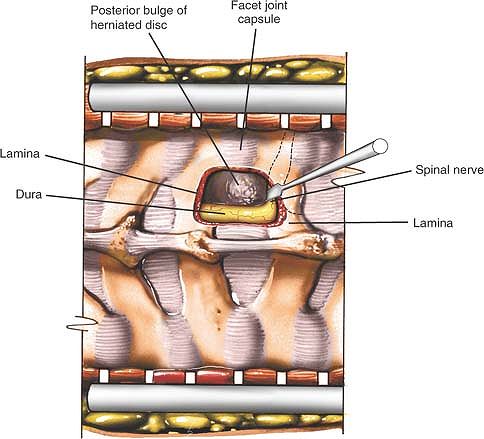
Excision of herniated discs1
-
Exploration of nerve roots2
-
Spinal fusion3,4
-
Removal of tumors5
-
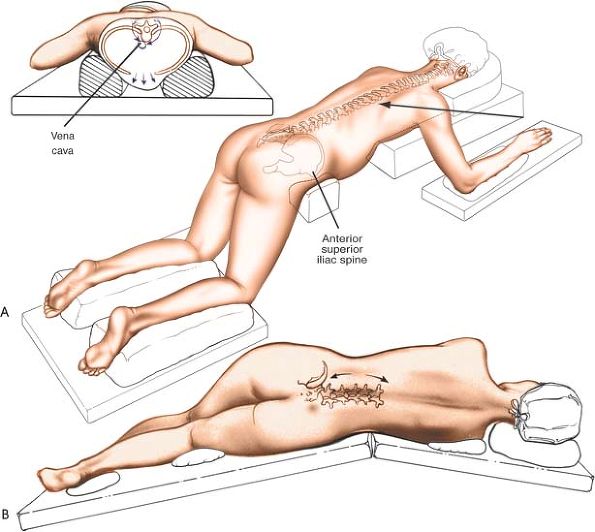
Logroll the patient into a prone
position. Be sure that bolsters are placed longitudinally under the
patient’s sides to allow the abdomen to be entirely free, reducing
venous plexus filling around the spinal cord by permitting the venous
plexus to drain directly into the inferior vena cava. The shoulders
should be placed at no more than 90° of abduction and should be
slightly flexed forward to relax the brachial plexus. Careful padding
of the ulnar nerve at the elbow and median nerve at the wrist must be
assured. Position the head and neck in a relaxed, neutral position and
be sure that no pressure is applied to the eyes. The lower extremities
should be padded carefully at the knees and feet. The hips are usually
flexed for decompression, as it allows for an increase in interlaminar
or interspinous distance and in neutral or slight extension for lumbar
fusions to restore normal lordosis. The knees are flexed, and we must
check that there is no pressure on the proximal fibula/common peroneal
nerve region (Fig. 6-1A). -
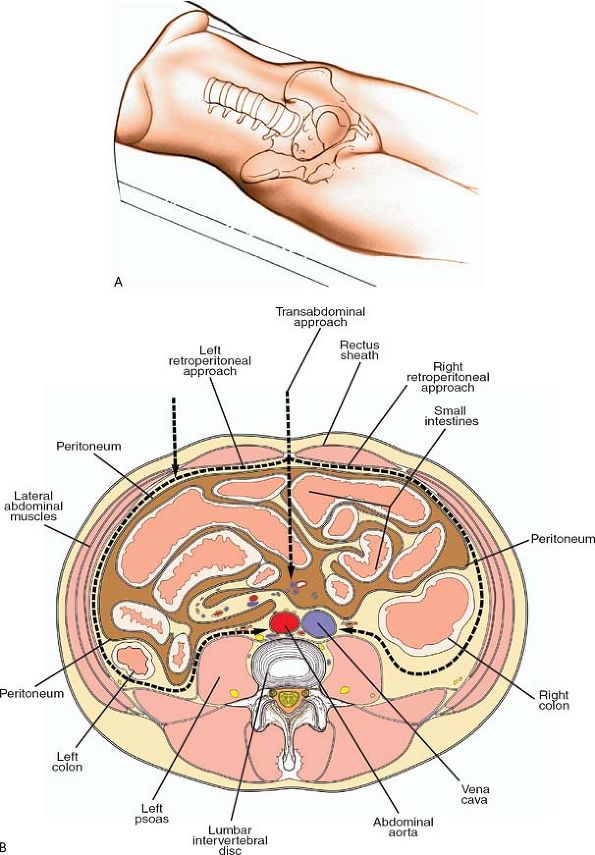
Place the patient on his or her side,
with the affected side upward. Flex the patient’s hips and knees to
flex the lumbar spine and open up the interspinous spaces. Make sure
that the patient is positioned with the involved spinal level over the
table break. Jackknifing the table can open further the intervertebral
space on the upper side of the patient by putting the lumbar spine into
lateral flexion. One advantage of this position is that it allows the
surgeon to sit. Extravasated blood drains down, away from the operative
field (see Fig. 6-1B).
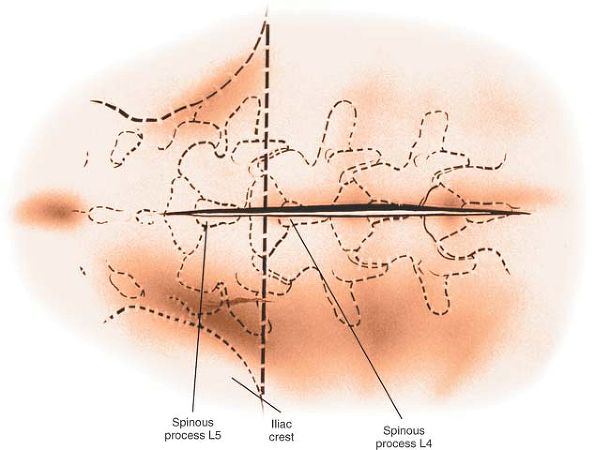
is in the L4-5 interspace. The line is only a rough guide, however; the
best means of determining the exact level is either to insert a small
needle into the spinous process and obtain a radiograph or to carry the
dissection distally and identify the sacrum.
above to the spinous process below the pathologic level. The length of
the incision depends on the number of levels to be explored (Fig. 6-2).
 |
|
Figure 6-1 (A) The position of the patient for the posterior approach to the lumbar spine. (B) Alternatively, place the patient in the lateral position with the affected side up.
|
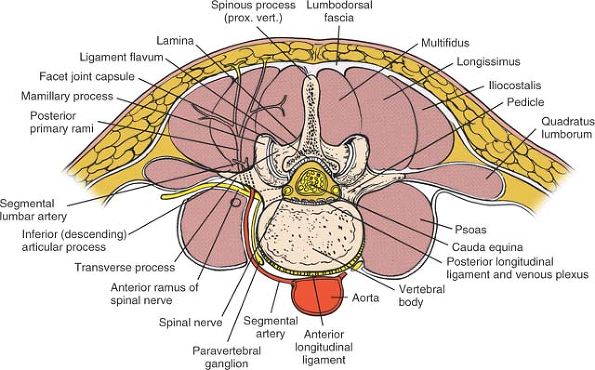
muscles (erector spinae), each of which receives a segmental nerve
supply from the posterior primary rami of the lumbar nerves.
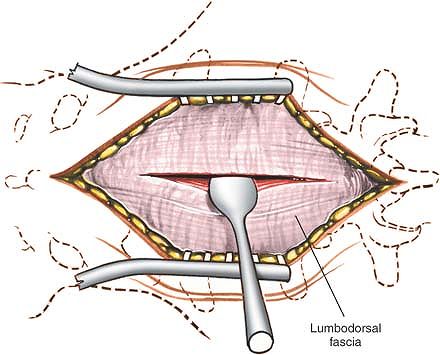
the skin incision until the spinous process itself is reached. Detach
the paraspinal muscles subperiosteally as one unit from the bone, using
a dissector, such as a Cobb elevator, or with cautery (Fig. 6-3).
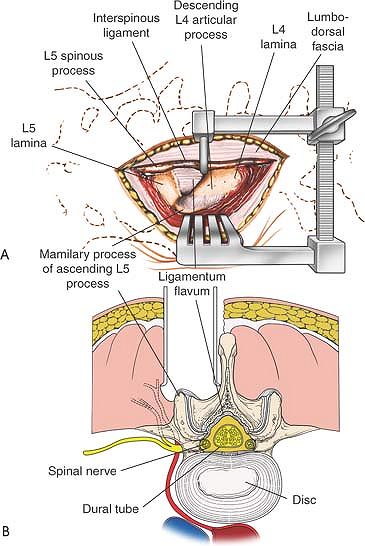
Dissect down the spinous process and along the lamina to the facet
joint. In a young patient, the tip of the spinous process is a
cartilaginous apophysis; it can be split in the midline, making
subperiosteal muscle removal easier (Fig. 6-4).
stripping the facet joint capsule from the descending and ascending
facets. To do this, strip the joint capsule in a medial to lateral
direction across the posterior aspect of the descending facet; then,
continue over the tip of the mamillary process of the more lateral
ascending facet. If the transverse processes must be reached, continue
dissecting down the lateral side of the ascending facet and onto the
transverse process itself (see Fig. 6-4).
transverse processes, are the vessels supplying the paraspinal muscles
on a segmental basis. These branches of the lumbar vessels frequently
bleed as the dissection is carried out laterally. Vigorous
cauterization of these
vessels
may be necessary to stop the bleeding. Note that the posterior primary
rami of the lumbar nerves, which also supply the paraspinal muscles
segmentally, run with these vessels. Loss of some of these nerves does
not totally denervate the paraspinal muscles, because they are
innervated segmentally (see Fig. 6-4).
 |
|
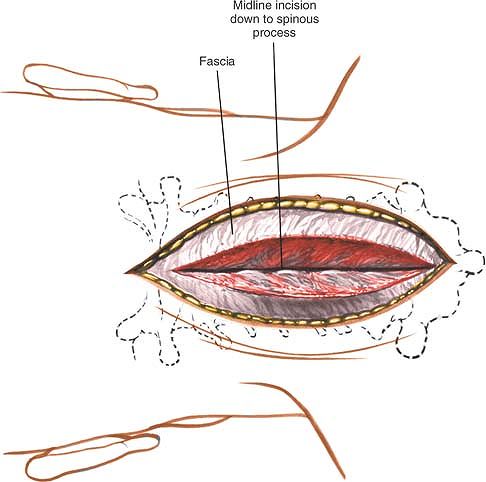
Figure 6-2
Make a longitudinal incision over the spinous processes, extending from the spinous process above to the spinous process below the level of pathology. A line drawn across the highest point of the iliac crest is in the L4-5 interspace. |
 |
|
Figure 6-3
Deepen the incision through the fat and fascia in line with the skin incision until the spinous process itself is reached. Detach the paraspinal muscles subperiosteally. |
 |
|
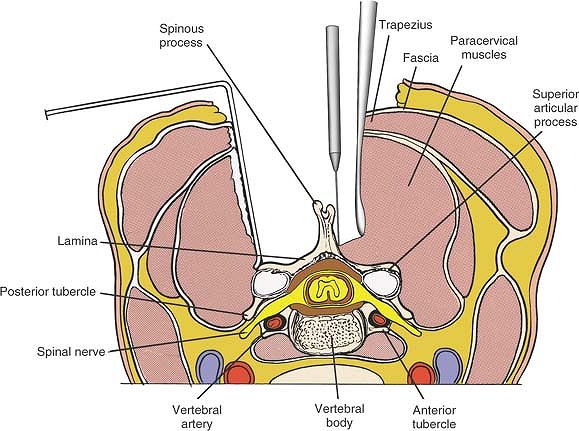
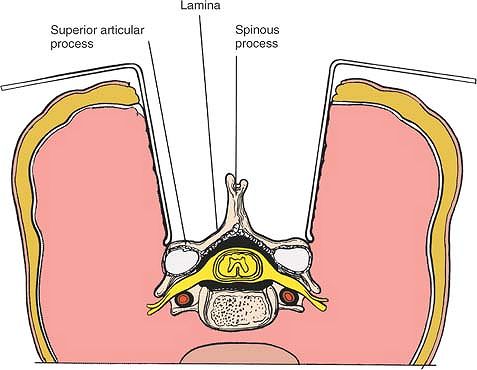
Figure 6-4 (A)
Dissect the paraspinal muscles from the spinous process and lamina to the facet joint. Remove the paraspinal muscles subperiosteally as one unit from the bone. (B) Continue dissecting laterally, stripping the joint capsule from the descending and ascending facets. Note the branches of the lumbar vessels that bleed during stripping of the muscles. |
 |
|
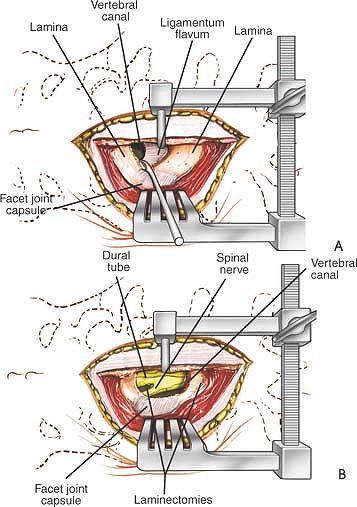
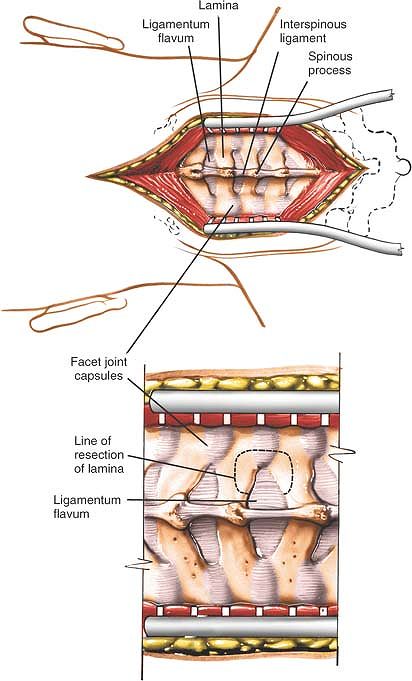
Figure 6-5 (A) Remove the ligamentum flavum by cutting its attachment to the superior or leading edge of the inferior lamina. (B)
Immediately beneath the ligamentum flavum and epidural fat is the blue-white dura. Identify the nerve root. Note the overlying epidural veins. |
to the superior, or leading, edge of the inferior lamina using either a
curette or sharp dissection. Immediately beneath are epidural fat and
the blue-white dura. Using blunt dissection and staying lateral to the
dura, carefully continue down to the floor of the spinal canal,
retracting the dura and its nerve root medially (Figs. 6-5, 6-6, 6-7 and 6-8).
protected. The more lateral the surgical field, the easier it is to
identify the nerve root and retract it so the disc space can be seen.
If a larger exposure is needed, incise part of the lamina on the distal
portion of the involved vertebra.
The bleeding can be stopped with Gelfoam or cotton patties soaked in
thrombin. Bipolar Malis cautery also may be used, although it must be
done with
great care because of the proximity of the nerve roots.
 |
|
Figure 6-6 (A) Insert a blunt dissector under the cut edge of the ligamentum flavum. (B)
Use a Kerrison rongeur to remove the distal end of the lamina. Note that the ligamentum flavum attaches halfway up the undersurface of the lamina. (C) Remove additional lamina and the remaining portion of the ligamentum flavum at its attachment to the undersurface of the lamina. |
the anterior aspect of the vertebral bodies may be injured if
instruments pass through the anterior portion of the annulus fibrosus
(see Fig. 6-21).6
-
To gain better exposure of the dura,
nerve root, and disc, remove additional portions of the lamina, both
from the leading edge of the lamina below and from the caudal edge of
the lamina above. A portion of the facet joint itself even can be
removed. Remember that it is safer to remove bone than to retract nerve
roots or dura excessively. If the wound is tight, dissect the
paraspinal muscles off the posterior spinal elements above and below
the exposed level to make the muscles easier to retract. -
To gain access to other parts of the
posterior aspect of the spine, carry the dissection as far laterally as
possible, onto the transverse processes. Complete lateral dissection
exposes the facet joints and transverse processes, permitting facet
joint fusion and transverse process fusion, if necessary (see Fig. 6-4).
proximally or distally and detach the posterior spinal musculature from
the posterior spinal elements. The approach can be extended from C1
down to the sacrum.
 |
|
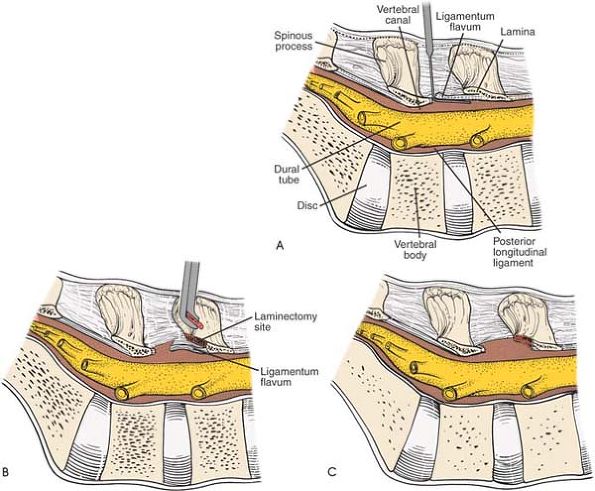
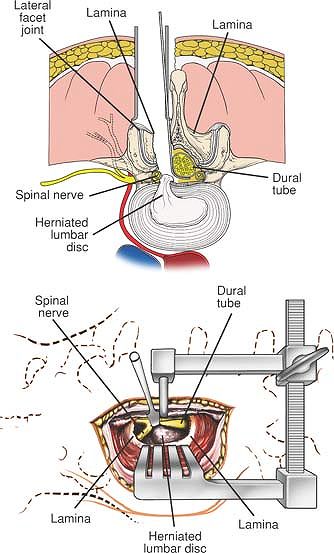
Figure 6-7 (A)
Using blunt dissection, carefully continue down the lateral side of the dura to the floor of the spinal canal; retract the dura and its nerve root medially. Reveal the posterior aspect of the disc. (B) Cross-section revealing the retraction of the dural tube and a herniated nucleus pulposus impinging on a nerve root. |
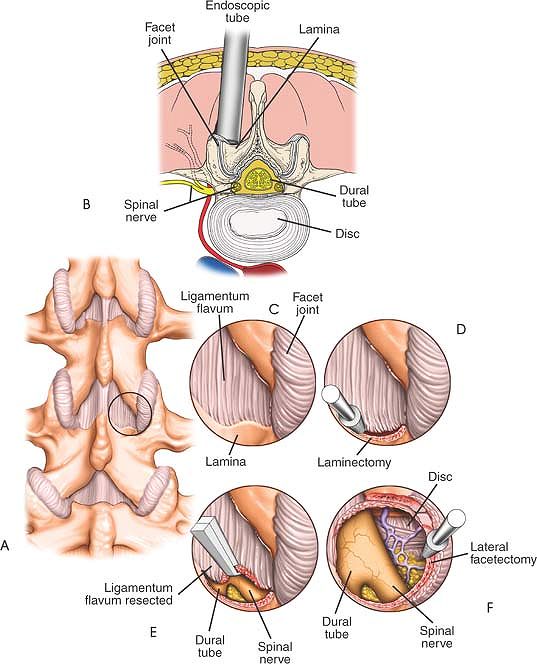
dilating/retracting tube and abutted against the lamina and medial
facet joint.7 The distal lamina and
ligamentum flavum are resected on the affected side to expose the nerve
root over the disc. Some of the medial facet can be resected to
decompress the lateral recess. The nerve root is then retracted
medially to expose the pathologic disc (Fig. 6-9).
 |
|
Figure 6-8 With the use of a microscope and retractor, a 3-cm incision can be used to expose the disc at a single level.
|
with landmarks and fluoroscopy because a very small incision is made.
Any deviation from the planned course may make it difficult to find the
pathology. If the incision is too medial, the spinous processes may
impede the proper positioning of the retracting tube. A tube that is
angled excessively will make it difficult to work and target the
microscope. This can be mitigated by using a tilting operating table.
Meticulous hemostasis is important, as the small access port can be
obscured easily by excessive bleeding.
differently to address pathologies in different locations, for example,
to access a sequestered disc, a far lateral disc, or to decompress a
contralateral spinal stenosis. Larger tubes are available if more
exposure is required. In the lordotic spine, a small change in the
angle of the tube can permit access to an adjacent level.
 |
|
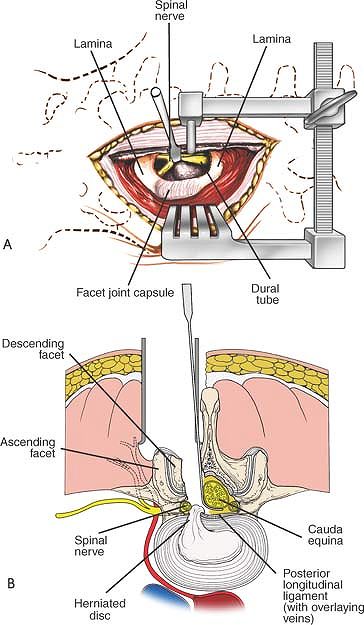
Figure 6-9 (A)
Localization of the level is performed with fluoroscopy. The starting point is 2 cm from the midline directly above the involved disc. (B) A 1- to 2-cm incision is made longitudinally. The fascia is incised. The erector muscles are split bluntly with dilating tubes. The retracting tube is positioned at the intersecting point of the lamina above the facet laterally and the ligamentum flavum medially and distally. (C) The proximal and distal lamina are thinned with a high speed burr. (D) The ligamentum flavum can be retracted medially or simply resected with a Kerrison rongeur is used to resect the caudad aspect of the lamina. (E) The ligamentum flavum can be retracted medially or simply resected with a Kerrison rongeur, exposing the dura. (F) The nerve root is exposed with the affected disc directly ventral to it. |
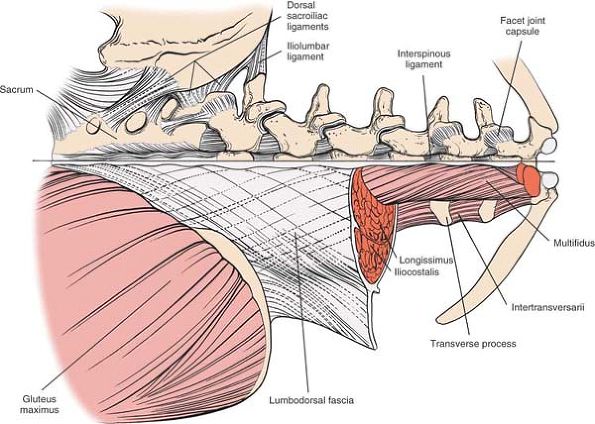
superficial and deep layers. The superficial layer consists of the
latissimus dorsi, a powerful muscle of the posterior axillary wall that
originates from the spinous processes and inserts into the
intertubercular groove of the humerus. The surgically important deep
layer consists of the paraspinal muscles and itself is divided into two
layers: the superficial portion, which contains the sacrospinalis
muscles (erector spinae), and the deep portion, which consists of the
multifidus and rotator muscles (Fig. 6-10).
 |
|
Figure 6-10
An overview of the musculature of the lumbosacral spine. In the lumbar spine, the sacrospinalis system is composed of the multifidi, longissimus, and iliocostalis muscles. Note the intertransversarii muscles located deeper. Note the dorsal sacroiliac ligaments. |
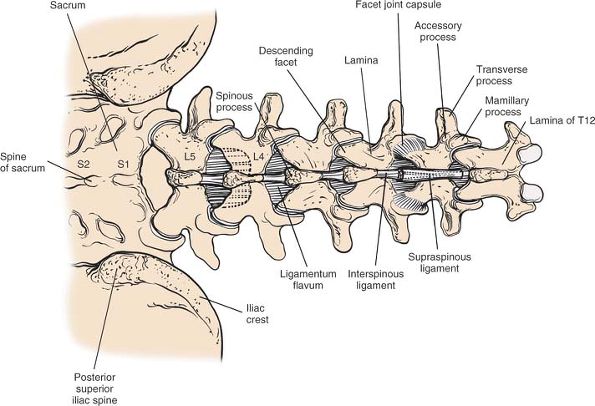
spinous processes in the lumbar area are thick. The distal end of the
tip of the spinous process is bulbous and extends slightly caudally.
Each process separates the paraspinal muscles on each side. In a
growing patient, the processes are capped by cartilaginous apophyses,
which, when split, make it easier to remove the paraspinal muscles
subperiosteally.
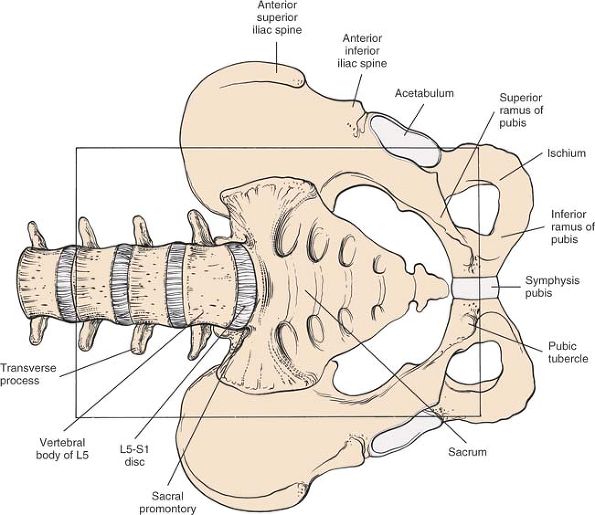
The broad iliac crests run posteriorly at a 45° angle toward the
midline. Because muscles either take origin from or insert into the
crest (none cross it), it has a palpable subcutaneous border. The
palpable, visible dimples over the buttocks lie directly over the
posterior superior iliac spines. A line drawn between the two posterior
superior iliac spines crosses the second part of the sacrum; a line
drawn between the highest points of the iliac crest crosses between the
spinous processes of L4 and L5 (Fig. 6-11).
 |
|
Figure 6-11
The bony anatomy of the lumbosacral spine and the posterosuperior aspect of the pelvis. The facet joint capsules, ligamentum flavum, and interspinous ligaments are shown. A line drawn across the crest of the ilium intersects the L4-5 interspinous space. A line crossing the posterior superior iliac spine intersects the second part of the sacrum. |
processes. It tends to heal with a fine, thin scar, because it is not
under tension after suturing and is attached firmly to underlying
fascia. No major cutaneous nerves cross the midline.
spinous processes. The fascia is a broad, relatively thick, white sheet
of tissue that forms a sheath for the sacrospinalis muscles and
attaches to the spinous processes (see Fig. 6-10).
It extends to the cervical spine, where it becomes continuous with the
nuchal fascia of the neck. Medially, it is attached to the spinous
processes of the vertebrae, the supraspinous ligaments, and the medial
crest of the sacrum. Inferiorly, it is attached to the iliac crests.
Laterally, it is continuous with the origin of the aponeurosis of the
transversus abdominis and latissimus dorsi muscles.
vertebra, connecting the spinous processes. They blend intimately with
the attachment of the dorsal lumbar fascia to the spinous processes (Fig. 6-14).
of muscle from bone. Because these muscles are detached in a single
mass, their critical feature, in regard to their surgical anatomy, lies
in their blood supply and not in their structure. The segmental lumbar
vessels branch directly from the aorta. They wrap around the waist of
each vertebral body and then ascend close to the pedicle, where they
divide into two branches. One supplies the spinal cord; the other,
larger branch then comes directly posteriorly to supply the paraspinal
musculature. During the approach, these vessels appear between the
transverse processes, close to the facet joints (see Fig. 6-11).
They often bleed as dissection is carried out. In addition, the
arteries branch within the muscle bodies, frequently creating a very
vascular field. For this reason, the dissection should be kept as close
to the midline as possible; no major vessels cross the midline, and the
plane is safe for use (Fig. 6-13; see Fig. 6-11).
 |
|
Figure 6-12
A sagittal section through the lamina of a lumbar vertebra. Note the origin and insertion of the ligamentum flavum as well as the supraspinous and interspinous ligaments. The nerve roots exit at the inferior aspect of the pedicle. |
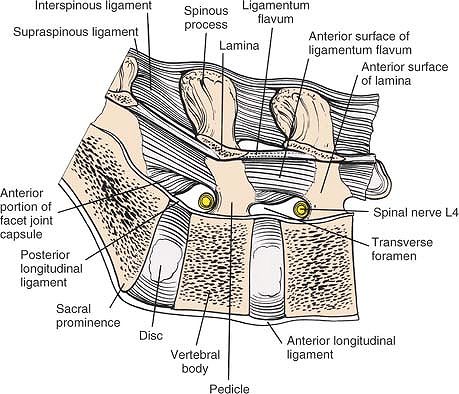
the deep layer. Consisting of yellow elastic tissue, the ligament takes
origin from the leading edge of the lower lamina and inserts into the
anterior surface of the lamina above, about halfway up onto a small
ridge (Fig. 6-12). The two ligamenta flava, one
from each side, meet in the midline, but generally do not fuse; the
plane between the ligamentum flavum and the underlying dura fat can be
entered most easily at that point. Because of its attachments, the
ligamentum flavum is removed best from the leading edge of the lower
lamina through sharp dissection or curettage (see Fig. 6-5A).
to the dura. Once the ligamentum flavum is entered, a thin spatula
should be placed beneath it to protect the underlying dura from being
torn (see Fig. 6-6A). The cord itself and the
nerve roots often are difficult to see as a result of bleeding from
epidural veins. The veins, which are thin-walled and easy to rupture,
even with blunt dissection, can be controlled by direct pressure using
a pattie or by bipolar cautery.
 |
|
Figure 6-13
Cross-section at the L3-4 disc space, looking distally. The segmental lumbar vessels branch directly from the aorta. They wrap around the waist of each individual vertebral body and then ascend close to the pedicle, where they divide into two branches. One branch supplies the cord; the other, larger branch proceeds directly posterior to supply the paraspinal musculature. During the surgical approach, these vessels appear between the transverse processes, close to the facet joints. Note that the posterior primary rami and the posterior branches of the lumbar vessels appear between the transverse processes close to the pedicle and descending facet. |
spine usually is reserved for fusing L5 to S1. It also may be used for
fusing L4 to L5, although it then involves mobilization of the great
vessels. Although the approach is simple in concept, the occasional
user may appreciate the assistance of a general surgeon who is more
familiar with the area exposed.8,9
Make sure that two areas remain bare for incision: one for the
abdominal incision, and one for harvesting an anterior iliac crest bone
graft. Insert a urinary catheter to keep the bladder empty. Use of
mechanical calf compression is recommended to decrease the risk of
thromboembolism.
 |
|
Figure 6-14 With the patient in the supine position (A), the anterior lumbar spine can be approached by a transperitoneal, left retroperitoneal, or right retroperitoneal path (B).
|
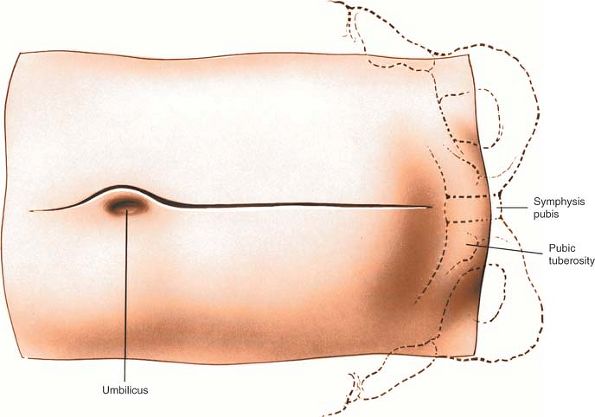
at the lower end of the abdomen through the fatty mons pubis. The pubic
tubercle, on the upper border of the pubis just lateral to the midline,
may be easier to palpate than the superior surface of the symphysis
itself.
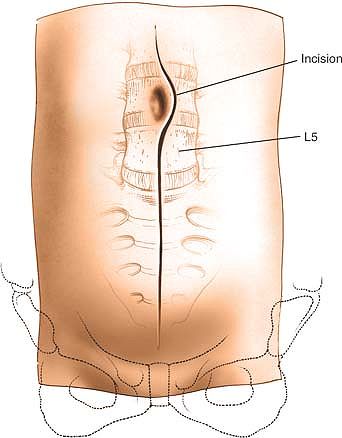
umbilicus to just above the pubic symphysis. Extend it superiorly,
curving it just to the left of the umbilicus and ending about 2 to 3 cm
above it. Heavier patients will require longer incisions (Fig. 6-15).
each side, segmentally supplied by branches from the seventh to the
12th intercostal nerves. Therefore, this incision can be extended from
the xiphisternum to the pubic symphysis.
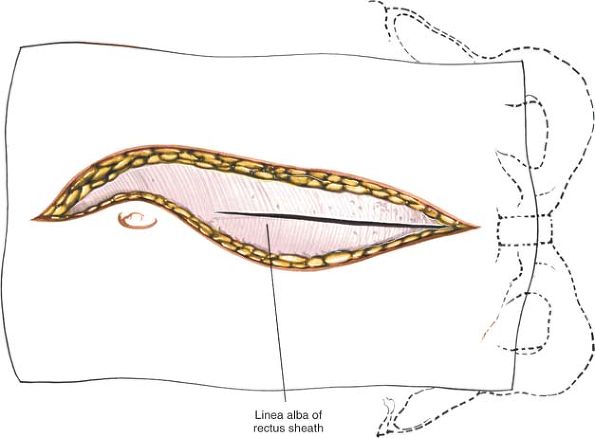
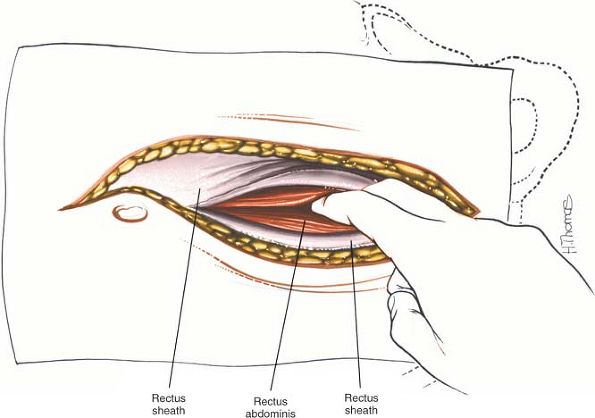
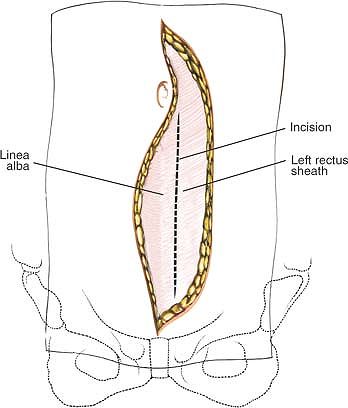
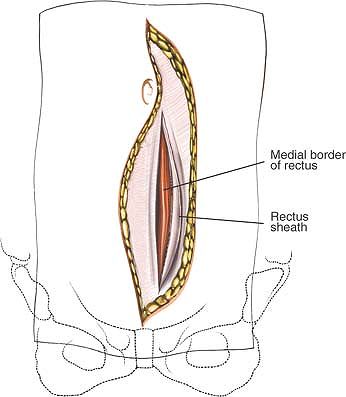
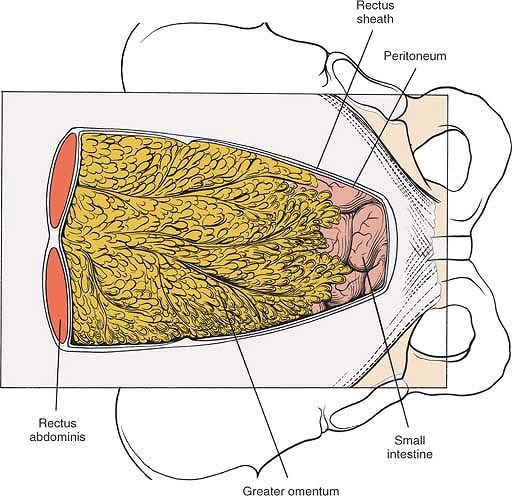
cutting through the fat to reach the fibrous rectus sheath. Incise the
sheath longitudinally, beginning in the lower half of the incision, to
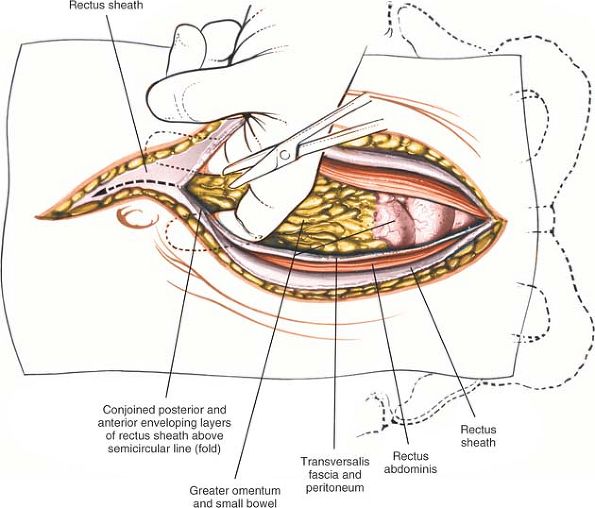
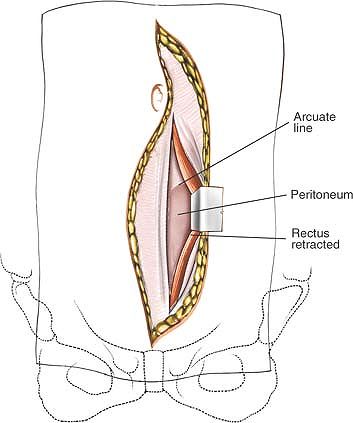
reveal the two rectus abdominis muscles (Fig. 6-16). Separate the muscles with the fingers to expose the peritoneum (Fig. 6-17).
Then, pick up the peritoneum carefully between two pairs of forceps
and, after making sure that no viscera are trapped beneath it, incise
it with a scissors (Fig. 6-18). Extend the
incision distally, but take care not to incise the dome of the bladder
at the inferior end of the wound. With one hand inside the abdominal
cavity to protect the viscera, carefully deepen the upper half of the
incision, staying in the midline and cutting through the linea alba,
the band of fibrous tissue that separates the two rectus abdominis
muscles in the upper half of the abdomen. Complete the exposure by
cutting through the peritoneum in the upper half of the wound (Fig. 6-19).
 |
|
Figure 6-15
Make a longitudinal midline incision from just below the umbilicus to just above the pubic symphysis. Extend it superiorly, to the left of the umbilicus. |
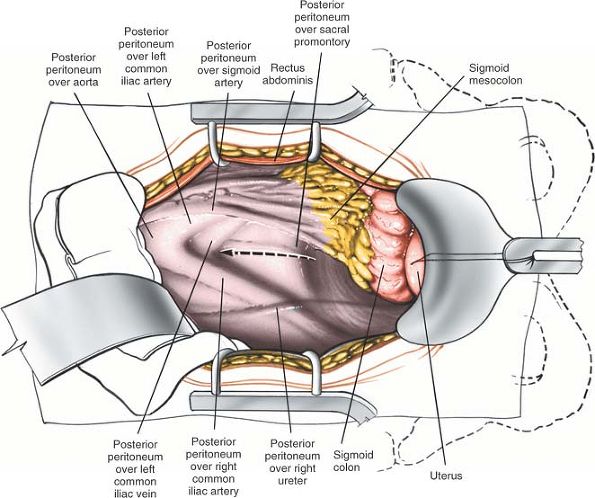
Perform a routine abdominal exploration. Next, put the operating table
in Trendelenburg’s position at 30° and carefully pack the bowel
in
a cephalad position, keeping it inside the abdominal cavity. Spread a
moist lap pad (swab) over it to prevent loops of bowel from slipping
free. It is much safer to keep the bowel within the abdominal cavity,
but do not pack it so tightly that vascular compromise is induced. In
women, the uterus may be retracted forward with a 0 silk suture placed
in its fundus and tied to the Balfour retractor.
 |
|
Figure 6-16
Deepen the wound in line with the skin incision by cutting through the fat to reach the fibrous rectus sheath. Incise the sheath longitudinally. |
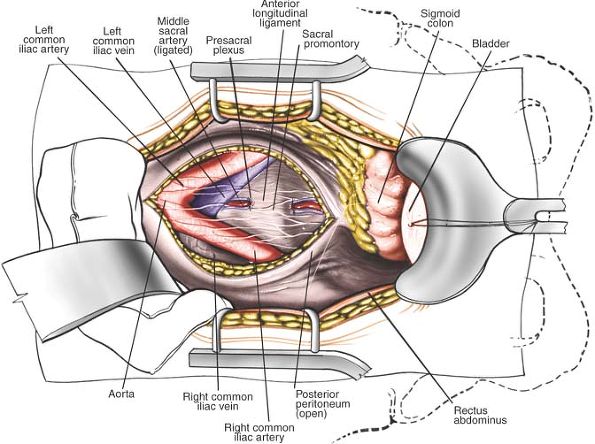
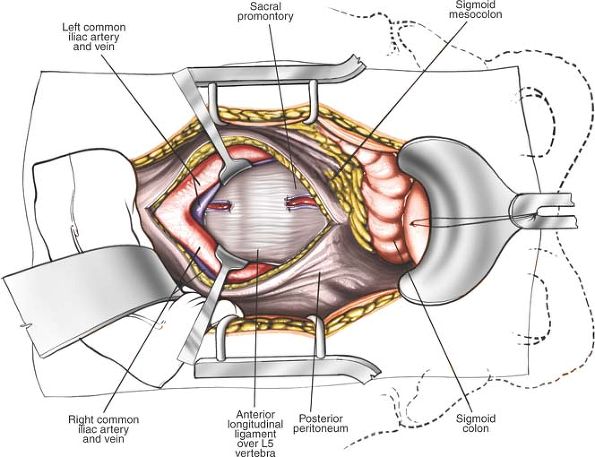
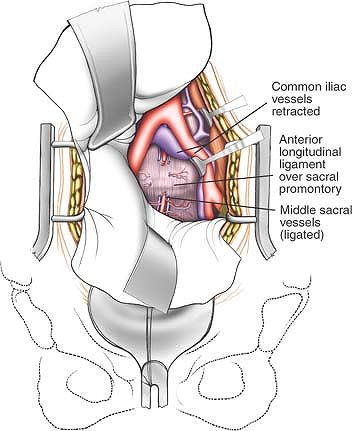
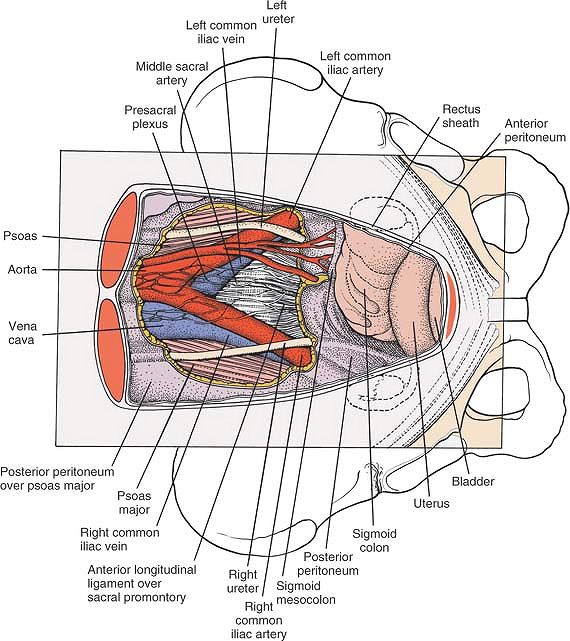
sacral promontory with a few milliliters of saline solution to make
dissection easier and to allow identification of the presacral
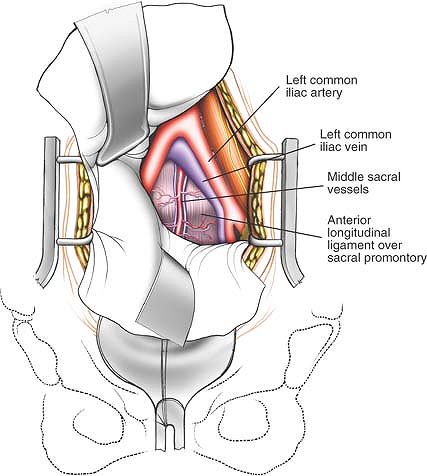
parasympathetic nerves that run down through this area. For the L5-S1
disc space, incise the posterior peritoneum in the midline over the
sacral promontory. The sacral artery runs down along the anterior
surface of the sacrum and must be ligated or clipped. The ureters
should be well lateral to the surgical approach.
the L5-S1 disc space either by palpating its sharp angle or by
inserting a metallic marker and taking a radiograph. The L5-S1 disc
space lies below the bifurcation of the aorta; it should be possible to
expose it fully without mobilizing any of the great vessels (Figs. 6-21 and 6-22).
exposure; mobilizing the great vessels is necessary, unless the
vascular bifurcation occurs much higher. Carefully incise the
peritoneum at the base of the sigmoid colon and mobilize the colon
upward and to the right to expose the bifurcation of the aorta, the
left common iliac artery and vein, and the left ureter. Identify the
aorta just above its bifurcation and gently begin blunt dissection on
its left side. Identify and ligate the fourth and fifth left lumbar
vessels, then divide them. Now, the aorta, vena cava, and left common
iliac vessels can be moved to the right, exposing the L4-5 disc space.
This exposure is difficult to achieve; a high incidence of venous
thrombosis has been reported with anterior surgery at this level. Take
care not to injure the left ureter, which crosses the left common iliac
vessels roughly over the sacroiliac joint. The ureter may have to be
moved laterally, but mobilize it only as much as necessary to reduce
the risk of postoperative ischemic stricture formation.
from below, working upward into the apex of the vascular bifurcation.
Isolate the left and right common iliac artery, placing umbilicus loops
around them. Retract the two arteries cephalad and laterally
to
expose the common iliac veins. Dissect into the confluence of the veins
and isolate the left common iliac vein with a loop. Gently retract the
venous structures to expose the disc space. Use only minimal retraction
to avoid injuring the intima, which may lead to venous thrombosis (see Fig. 6-22).
 |
|
Figure 6-17 With your fingers, separate the rectus abdominis muscles in the midline to expose the peritoneum.
|
 |
|
Figure 6-18 Pick up the peritoneum with forceps and incise it.
|
 |
|
Figure 6-19
With one hand inside the abdominal cavity to protect the viscera, carefully deepen the upper half of the incision, staying in the midline and cutting through the linea alba. |
 |
|
Figure 6-20
Use a self-retaining retractor to retract the rectus abdominis muscles laterally and the bladder distally. Carefully mobilize and retract the bowel in a cephalad position, keeping it inside the abdominal cavity. Observe the posterior peritoneum overlying the bifurcation of the great vessels and the promontory of the sacrum. Incise the peritoneum longitudinally. |
critically important to sexual function. Injury to the plexus at L5-S1
may cause retrograde ejaculation and injury more distal on the sacrum
or deep in the pelvis may cause importance. Therefore, dissection
should be carried out carefully, and only with a blunt peanut
dissector. The incision over the anterior part of the sacrum should be
made in the midline, and it should be long enough to allow for lateral
mobilization of these nerves with minimal trauma. Injecting saline
solution into the presacral tissue aids in identifying and preserving
these nerves (see Figs. 6-21 and 6-34).10,11,12
are tethered to the anterior surface of the lumbar vertebrae by the
lumbar vessels. These smaller vessels must be ligated and cut to allow
the great vessels to be lifted forward off the lumbar vertebrae,
exposing the L4-5 disc space (see Fig. 6-13). It is important to dissect these vessels out carefully without cutting them flush with the aorta.
If the vessels are cut flush, there will be, in effect, a hole in the
aorta, and the bleeding may be extremely difficult to control.
Mobilization of the venous structures should be undertaken very
carefully, because they are fairly fragile and easily traumatized.
Damage to these vessels may result in thrombosis; mobilization and
retraction should be kept to a minimum.
 |
|
Figure 6-21
Retract the posterior peritoneum to reveal the bifurcation of the aorta and vena cava. Ligate the middle sacral artery. Identify the presacral parasympathetic plexus overlying the aorta and the sacral promontory. |
laterally, particularly for exposure of the L4-5 disc space. It can be
identified easily by gently pinching it with a pair of non-toothed
forceps to induce peristalsis (see Fig. 6-34).
exposure in the pelvis. Careful mobilization of the great vessels is
crucial to exposure higher up (see Figs. 6-20 and 6-22).
xiphisternum, but the exposure of higher discs almost always is
performed better through a retroperitoneal approach.
 |
|
Figure 6-22 Mobilize the great vessels as needed for additional exposure. Expose the L5-S1 disc space subperiosteally.
|
distal to the midway mark between the umbilicus and symphysis. A more
distal incision is required for the L5-S1 disc because of its downward
orientation. The L4-5 disc is generally located a few centimeters from
the umbilicus, and the incision is made directly over the disc. L3-4 is
a few centimeters proximal to the umbilicus and is also approached with
an incision directly over it. The incisions can be transverse if only
one level is done or the more versatile incision for one or more level
is a midline longitudinal or slight oblique incision (Fig. 6-23).13
The inferior epigastric vessels are identified and preserved. Blunt
dissection is used to develop a plane dorsal to the rectus abdominis
and toward the lower quadrant. If exposing proximal to L5, the fascia
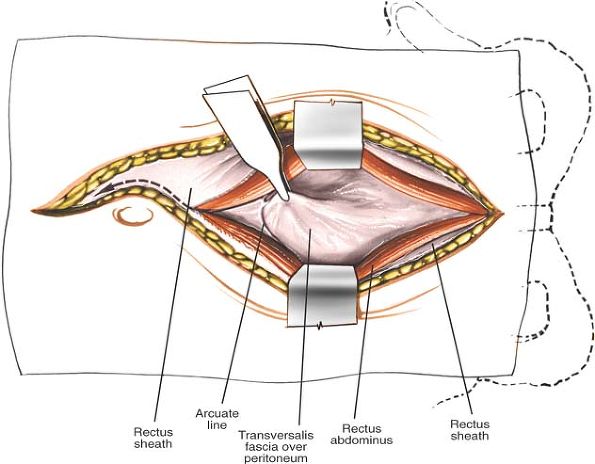
of the arcuate line is divided (Fig. 6-27).
 |
|
Figure 6-23
The landmarks for an anterior minimal access retroperitoneal approach are shown. The final localization should be done radiographically prior to the incision as the disc level may vary. The incisions can be transverse, longitudinal, or slightly oblique. The incisions for L3-4 and L4-5 are generally performed directly over the disc level, whereas the L5-S1 disc must be approached through a more distal incision given the downward orientation of the disc. |
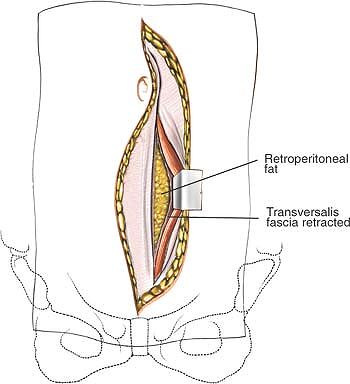
quadrant, retroperitoneal fat is eventually encountered; underneath it,
the psoas muscle can be seen. At this point, branches of the
genitofemoral nerve are readily identified lying on the psoas and just
medial is the common iliac artery. Retractors appropriate to the
direction of the incision and size should be determined (Fig. 6-28).
The ureter is generally seen on the underside of the peritoneum. The
peritoneum and ureter are retracted medially and the common iliac vein
is seen just dorsal to the artery and crossing from proximal-lateral to
distal-medial. Caution must be used not to damage the thin walls of the
vein, as it is easily the most fragile structure of this approach. The
soft tissues in front of the L5-S1 disc and sacral promontory are
bluntly pushed medially to expose the middle sacral vein(s) (Fig. 6-29).
The veins require clipping, cauterizing, and ligating to divide them
and mobilize the left iliac vein. To expose the L4-5 disc, the
dissection is moved proximal to the iliac vessels. A plane between
the
psoas and the iliac vessels is developed bluntly. The ascending
iliolumbar vein should be identified and ligated/clipped before
retracting the iliac vein.14
 |
|
Figure 6-24
The incision is continued to the ventral fascia of the rectus abdominus. The midline can be identified by the crisscrossing fibers of the fascia. |
 |
|
Figure 6-25 The rectus fascia is cut longitudinally on the medial edge of the muscle.
|
 |
|
Figure 6-26 The medial edge is identified and the rectus is lifted up and retracted to expose the dorsal fascia and the arcuate line.
|
 |
|
Figure 6-27
The epigastric vessels are identified and preserved. Blunt dissection is used to develop a plane dorsal to the rectus abdominis and toward the lower quadrant. If exposing proximal to L5, the fascia of the arcuate line is divided. |
 |
|
Figure 6-28
Continuing the blunt dissection toward the left lower quadrant, retroperitoneal fat is eventually encountered; underneath it, the psoas muscle can be seen. At this point, branches of the genitofemoral nerve are readily identified lying on the psoas and just medial is the common iliac artery. |
to sexual function. Dissection should be gentle and blunt with all the
soft tissues anterior to the disc moved as a unit with the
retroperitoneum. Bipolar cautery should be used selectively.
the psoas on the lateral vertebral body particularly when exposing
proximal to L5.
anterior surface of the lumbar vertebrae by the lumbar vessels. These
smaller vessels must be ligated and cut to allow the great vessels to
be lifted forward off the lumbar vertebrae, exposing the L4-5 disc
space (see Fig. 6-13). It is important to
dissect these vessels carefully, without cutting them flush with the
aorta. If the vessels are cut flush, there will be, in effect, a hole
in the aorta, and the bleeding may be extremely difficult to control.
Mobilization of the venous structures should be undertaken very
carefully, because they are fairly fragile and easily traumatized.
Damage to these vessels may result in thrombosis; mobilization and
retraction should be kept to a minimum.
 |
|
Figure 6-29
The soft tissues in front of the L5-S1 disc and sacral promontory are bluntly pushed medially to expose the middle sacral vein(s). |
retroperitoneal approach. It is generally easier to let the ureter be
moved medially with the rest of the retroperitoneum. It can be
identified by inducing peristalsis by gently pinching it with a pair of
nontoothed forceps.
aspect of T11 to S1. Exposing more proximal discs requires control and
division of the segmental vessels to mobilize the aorta and vena cava.
stages of dissection. The superficial stage consists of cutting the
skin and subcutaneous tissues down to the bowel. Below the skin lies
the linea alba, a fibrous structure in the midline that is identified
most easily in the upper abdomen. Cutting the linea alba in the lower
half of the abdomen exposes the rectus muscle, which can be separated
by finger pressure. Beneath it is the posterior rectus sheath and
peritoneum.
packing away the bowel, is the anatomy of the bowel and is not included
in this book.
retroperitoneal structures that lie anterior to the L4-5 and L5-S1 disc
spaces. These structures include the aorta, vena cava, common iliac
vessels, lumbar vessels, ureter, and presacral plexus.
 |
|
Figure 6-30 Superficial aspect of the distal rectus sheath. Note that the fibers of the external oblique appear laterally.
|
superficial to the linea alba. It usually is about halfway between the
pubic symphysis and the infrasternal notch, although it may be pulled
lower in obese patients.
externally by a groove in the midline of the abdomen. It divides one
side of the rectus abdominis muscle from the other. In the upper
abdomen, it actually separates the two muscles; cutting through it
leads directly down to the peritoneum, with neither muscle being
exposed. Below the umbilicus, the linea alba is less distinct; it does
not separate the two rectus muscles.
umbilicus. Because the skin is mobile and loosely attached to the
tissues immediately beneath it, it heals with a thin scar. The cleavage
or tension lines below the umbilicus appear in a chevron pattern, with
the apex of the V in the midline.
segmentally from T7 in the region of the xiphoid to T12 just above the
inguinal ligament. These segmental nerves do not cross the midline.
Therefore, midline incisions do not cut any major cutaneous nerves.
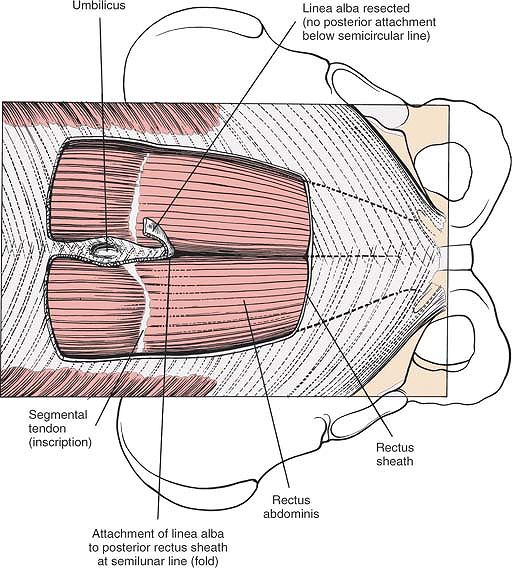
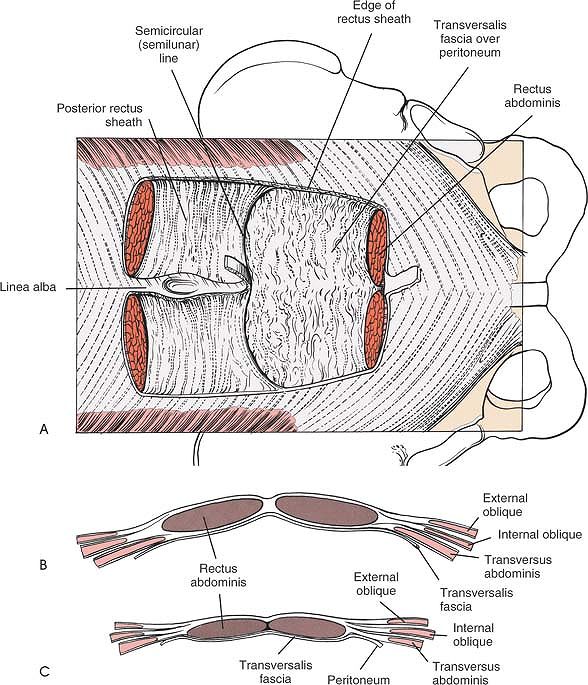
length of the entire abdomen, split into two muscles in the upper half
by the linea alba. The muscle is enclosed in a fascial sheath. Above
the umbilicus, the sheath has three elements: the aponeurosis of the
internal oblique splits to enclose the rectus muscle; the aponeurosis
of the external oblique passes in front of the rectus to form part of
the anterior sheath; and the aponeurosis of the transversus abdominis
fascia passes behind to form part of the posterior sheath. The inferior
margin of the posterior sheath is known as the semicircular line
(semicircular fold of Douglas). Below the umbilicus, all three
aponeuroses pass anteriorly, leaving a thin film of tissue posteriorly (Figs. 6-31 and 6-32).
 |
|
Figure 6-31
The anterior portion of the rectus sheath is resected, revealing the fibers of the rectus abdominis muscle. Distal to the semicircular line, the linea alba (which is shown elevated by sutures) overlies the muscle fibers of the rectus abdominis but does not separate them. Proximal to the semicircular line, the linea alba separates the rectus abdominis muscles by attaching to the posterior rectus sheath, which begins at the semicircular line. |
means that, in the upper half of the incision, the approach through
fibrous tissue leads directly down to the peritoneum, whereas in the
lower half, it leads to the rectus abdominis muscle. Because of this,
it is easier to open the abdomen in the lower half of the incision (Fig. 6-33; see Fig. 6-32).
 |
|
Figure 6-32 (A)
The rectus abdominis muscle has been resected. The posterior aspect of the rectus sheath ends just distal to the umbilicus. Its distal edge is called the semicircular line. The linea alba attaches to the posterior rectus sheath, thus separating the rectus abdominis muscles proximal to the semicircular line. (B) Cross-section above the semicircular line. Note that the rectus abdominis muscles are enveloped by the posterior and anterior rectus sheaths and separated from each other by the linea alba. (C) Cross section below the semicircular line. The rectus sheath exists only anteriorly. Posteriorly is the transversalis fascia and peritoneum. |
 |
|
Figure 6-33 The posterior rectus sheath has been removed to reveal the peritoneum and the abdominal viscera.
|
lower half of the rectus abdominis muscle. The artery lies between the
muscle and the posterior part of the rectus sheath. If the surgical
plane remains in the midline, this vessel should escape injury. If the
artery is damaged when the rectus muscle is mobilized, it can be tied
with impunity.
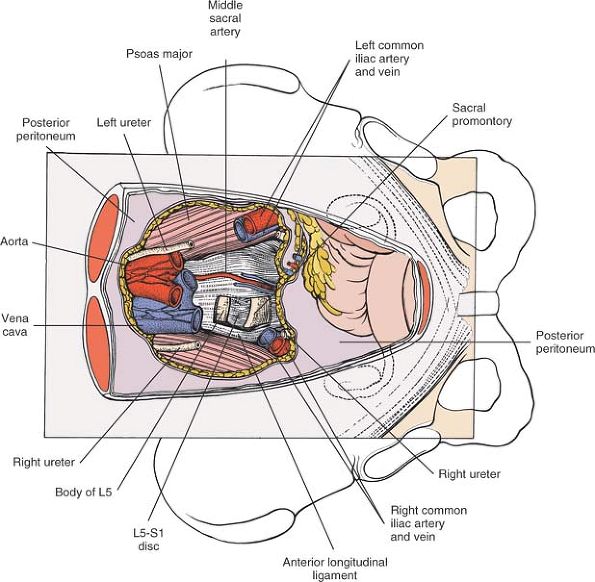
ends of the aorta and the vena cava from the vertebrae in the L4-5
vertebral area. The aorta divides on the anterior surface of the L4
vertebra into the two common iliac arteries. Just below this
bifurcation, the common iliac vessels divide in turn at about the S1
level into the internal and external iliac vessels. The internal iliac
is the more medial of the two (Fig. 6-34).
anterior parts of the lower lumbar vertebrae by the lumbar vessels.
These segmental vessels must be mobilized to permit the aorta and vena
cava to be moved (see Fig. 6-13). Because the
arterial structures are easier to dissect and more muscular than are
the thin-walled venous structures, the preferred approach to the L4-5
disc space is from the left, the more arterial side. The median sacral
artery originates from the aorta at its bifurcation at L4 and runs in
the midline, over the sacral promontory and down into the hollow of the
sacrum (see Fig. 6-34). The lumbosacral disc
usually lies in the V that is formed by the two common iliac vessels.
Nevertheless, the level at which the vessels bifurcate may vary; on
rare occasions, they may have to be mobilized to expose the L5-S1 disc
space.
common iliac artery, whereas the right common iliac artery lies below
and medial to the right common iliac vein. Therefore, special care must
be taken
when
mobilizing the left side of the vascular V, because the vessel closest
to the surgery is the thin-walled vein, not the artery (Fig. 6-35; see Fig. 6-34).
 |
|
Figure 6-34
The abdominal viscera has been retracted proximally, and the retroperitoneum has been resected to reveal the great vessels at their bifurcation, the ureters, and the presacral plexus. |
The nerves anterior to the L5-S1 disc are part of the superior
hypogastric plexus which receives sympathetic innervation from T11 to
L3 via the sympathetic chain and a plexus of nerves around the aorta.
Injury to these nerves may cause ejaculatory dysfunction in men
(retrograde ejaculation). More distally the plexus of nerve has
parasympathetic contributions from the pelvic nerves (S2,S3,S4) which
are important for erectile function in men. These nerves are more at
risk with surgeries anterior to the mid and lower sacrum as well as low
rectal and prostate procedures (see Figs. 6-34 and 6-35).15
 |
|
Figure 6-35
Portions of the major vessels have been resected to reveal the underlying L5-S1 disc space, the sacral promontory, and its overlying presacral plexus. |
psoas muscle. At the bifurcation of the common iliac artery over the
sacroiliac joint, it clings to the posterior abdominal wall, held there
by the peritoneum, and should be well lateral to the approach to the
L5-S1 disc space. It may have to be mobilized for exposure of the L4-5
disc space (Fig. 6-36; see Fig. 6-35).
 |
|
Figure 6-36 Osteology of the anterior aspect of the pelvis and lumbosacral spine.
|
lumbar spine has several advantages over the transperitoneal approach.
First, it provides access to all vertebrae from L1 to the sacrum,
whereas the transperitoneal approach is difficult to use above the
level of L4. Second, it allows drainage of an infection, such as a
psoas abscess, without the risk of a postoperative ileitis. Because of
the arrangement of the vascular anatomy of the retroperitoneal space,
however, it is slightly more difficult to reach the L5-S1 disc space
using the retroperitoneal approach.
-
Spinal fusion
-
Drainage of psoas abscess and curettage of infected vertebral body
-
Resection of all or part of a vertebral body and/or intervertebral disc and associated bone grafting
-
Biopsy of a vertebral body when a needle biopsy is either not possible or hazardous
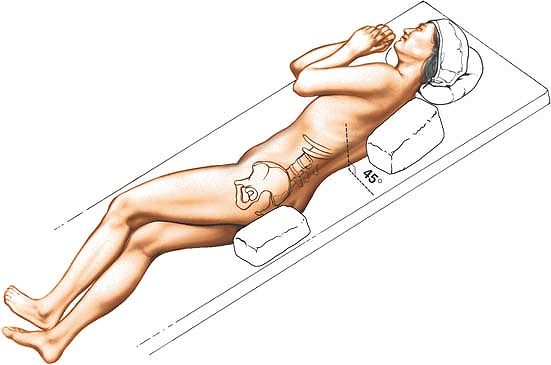
semilateral position. The patient’s body should be at about a 45° to
90° angle to the horizontal, facing away from the surgeon. Keep the
patient in this position throughout the surgery by placing sandbags
under the hips and shoulders or by using a kidney rest brace to hold
the patient. The angle allows the peritoneal contents to fall away from
the incision. Alternatively, place the patient supine on the operating
table and tilt the table at 45° to the horizontal away from the
surgeon. This position has the advantage of not putting the psoas
muscle on stretch (Fig. 6-37).
depending on whether the surgeon prefers to work on the “aortic side”
or the “caval side.”
 |
|
Figure 6-37 Place the patient in the semilateral position for the anterolateral (retroperitoneal) approach to the lumbar spine.
|
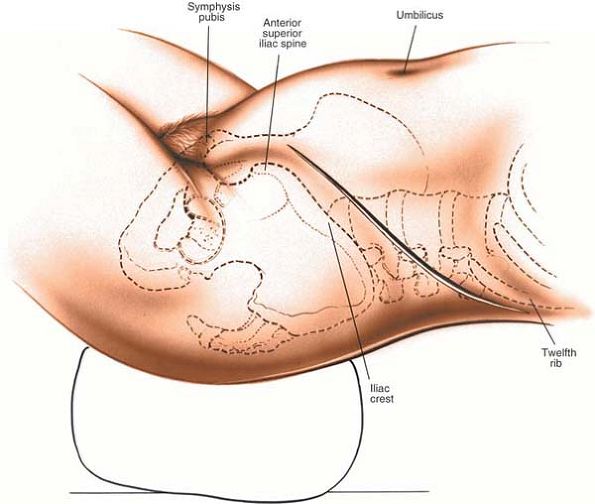
posterior half of the 12th rib toward the rectus abdominis muscle and
stopping at its lateral border, about midway between the umbilicus and
the pubic symphysis (Fig. 6-39).
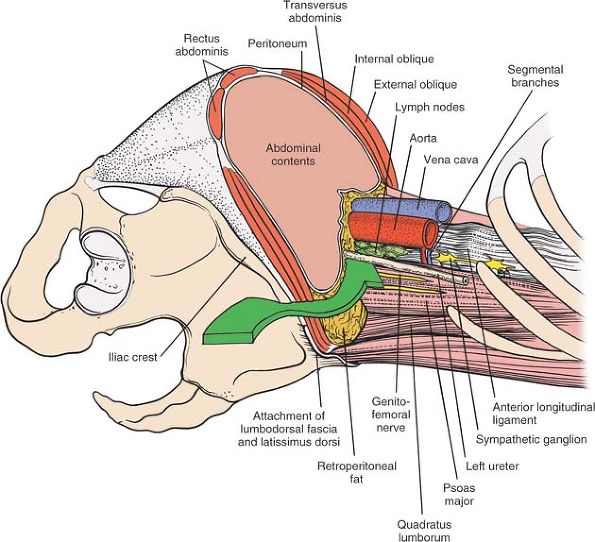
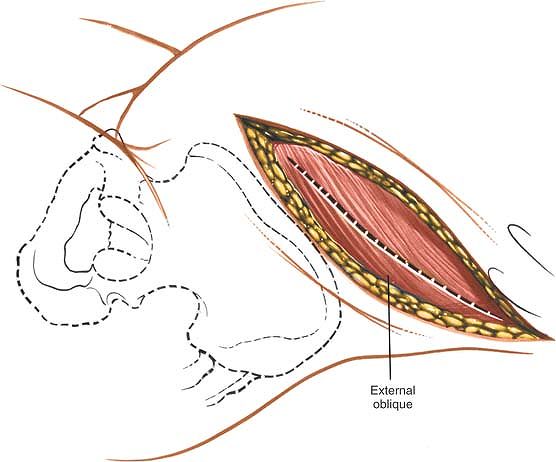
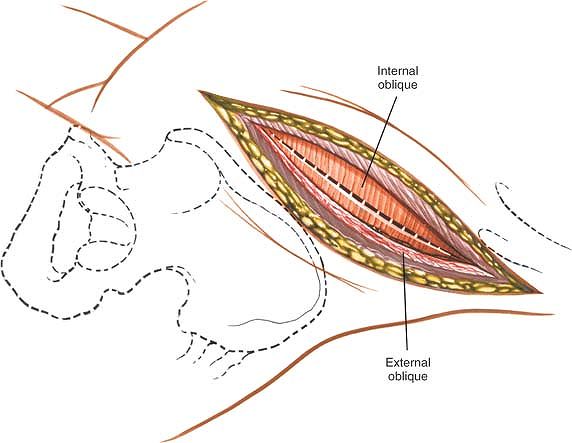
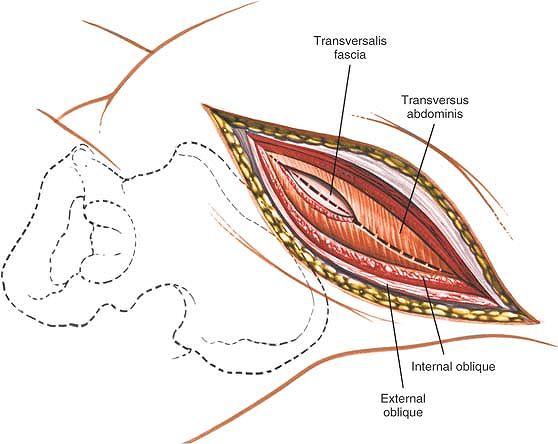
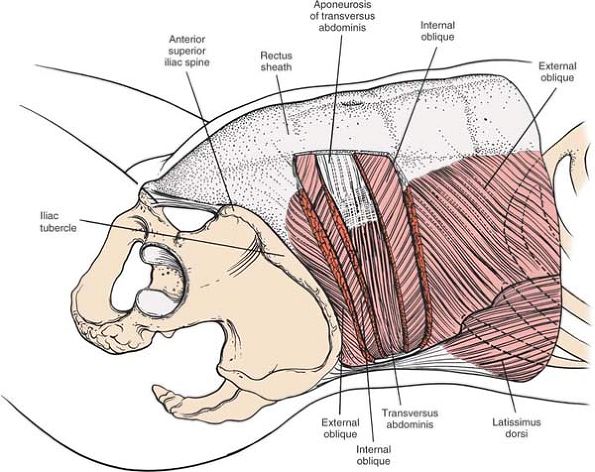
muscles of the abdominal wall (the external oblique, internal oblique,
and transversus abdominis) are divided in line with the skin incision.
Because all three muscles are innervated segmentally, significant
denervation does not occur (Fig. 6-38).
muscle. Divide the aponeurosis of this muscle in the line of its
fibers, which is in line with the skin incision. The muscle fibers of
the external oblique rarely appear below the level of the umbilicus
except in very muscular patients. If they are found there, the muscle
should be split in the line of its fibers (Fig. 6-40).
 |
|
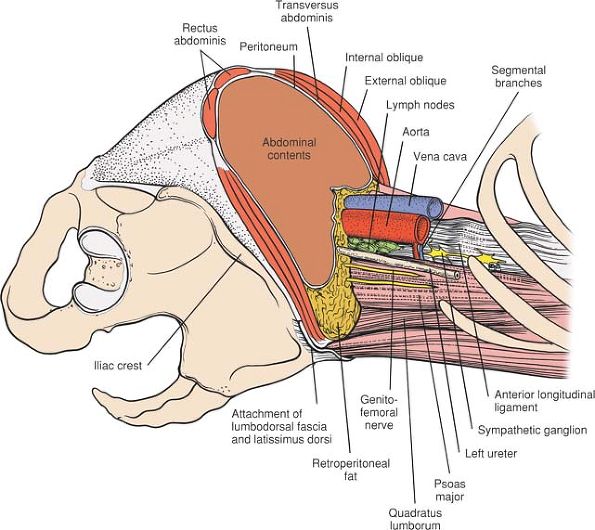
Figure 6-38 The anterior abdominal musculature and viscera have been transected and removed at the level of the iliac crest. The arrow indicates the route of surgery between the peritoneum anteriorly and the retroperitoneal structures posteriorly.
|
 |
|
Figure 6-39 Make an oblique flank incision extending down from the posterior half of the 12th rib toward the rectus abdominis muscle.
|
the skin incision and perpendicular to the line of its muscular fibers.
This division causes partial denervation, but if the muscle is closed
properly, postoperative hernias can be avoided (Fig. 6-41).
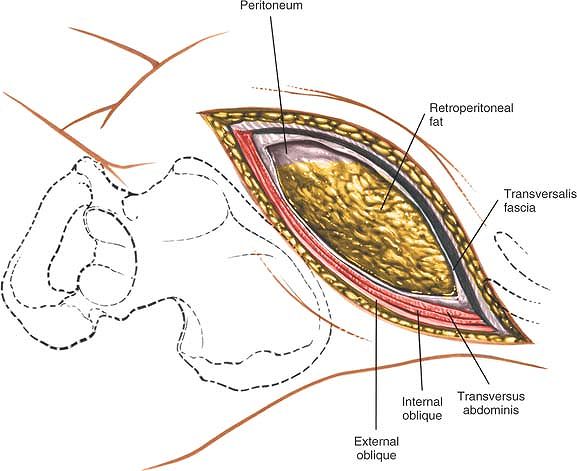
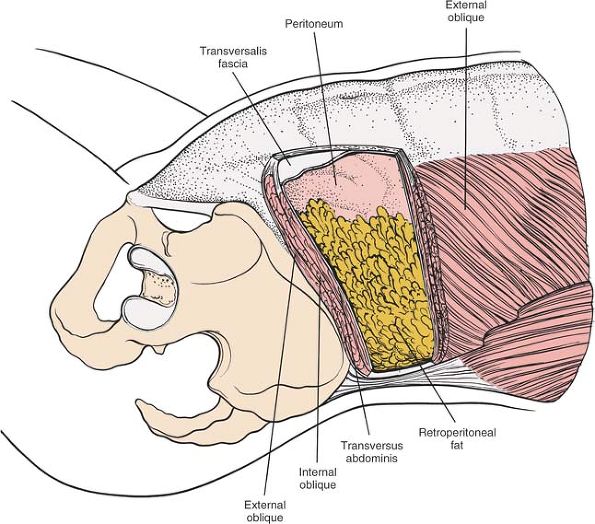
Under the internal oblique muscle lies the transversus abdominis
muscle. It, too, should be divided in line with the skin incision to
expose the retroperitoneal space (Figs. 6-42, 6-43, 6-47, and 6-48).
Carry out this dissection from either the left lower quadrant or the
right upper quadrant, depending on the side that needs to be exposed.
 |
|
Figure 6-40 Incise the external oblique muscle and aponeurosis in line with its fibers and in line with the skin incision.
|
 |
|
Figure 6-41 Divide the internal oblique in line with the skin incision and perpendicular to the line of its muscular fibers.
|
 |
|
Figure 6-42 Divide the underlying transversus abdominis muscle in line with the skin incision.
|
 |
|
Figure 6-43 In the anterior part of the wound, identify the peritoneum and its contents. Posteriorly, identify the retroperitoneal fat.
|
 |
|
Figure 6-44 Using blunt finger dissection, develop the plane between the retroperitoneal fat and fascia that overlie the psoas muscle.
|
 |
|
Figure 6-45 Mobilize the peritoneal cavity and its contents, and retract them medially.
|
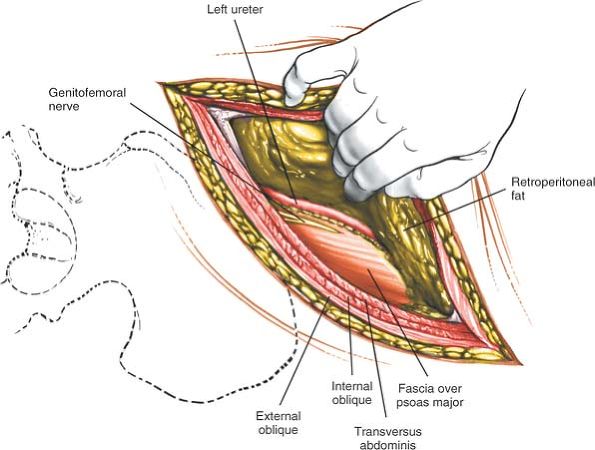
contents and retract them to the right upper quadrant. The ureter,
which is attached loosely to the peritoneum, is carried forward with it.
Any existing psoas abscess is easily palpable at this point. If one is
found, it should be entered from its lateral side with finger
dissection. Follow the abscess cavity with a finger directly to the
infected disc space or spaces. If there is no psoas abscess, follow the
surface of the psoas muscle medially to reach the anterior lateral
surface of the vertebral bodies.
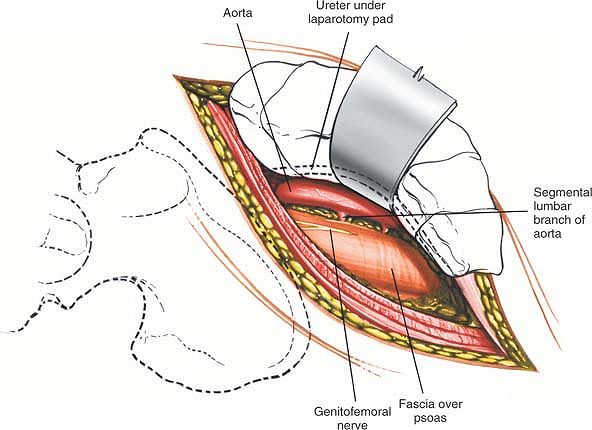
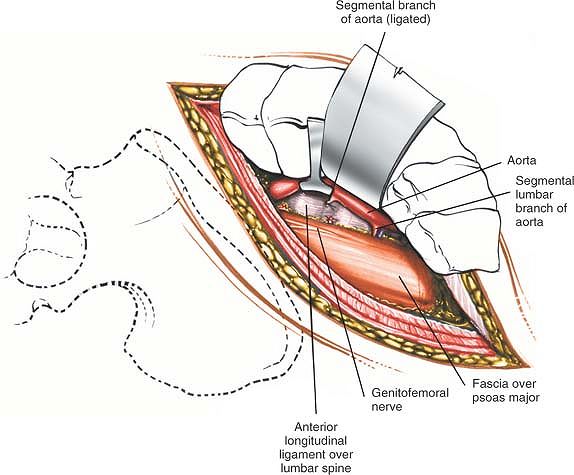
waist of the vertebral bodies by the lumbar arteries and veins. These
smaller vessels must be located individually on the involved vertebrae
and tied so that the aorta and vena cava can be mobilized and the
anterior part of the vertebral body reached. Make sure that the lumbar
vessels are not cut flush with the aorta; a slipped tie then would
prove hard to deal with (Figs. 6-46 and 6-49).
 |
|
Figure 6-46
Ligate the lumbar vessels (segmental branches of the aorta). Mobilize the aorta and vena cava to reach the anterior part of the vertebral body. |
on the lateral aspect of the vertebral body and on the most medial
aspect of the psoas muscle. It is easy to identify as the tissue is
cleared from the front of the vertebrae.
on the anterior medial surface of the psoas muscle, attached to its
fascia. Easily identifiable, it should be preserved (see Figs. 6-45 and 6-49).
if the peritoneal contents are retracted vigorously when the approach
is made from the right side. The aorta will come down on, and it is a
much tougher structure that is more resistant to injury.
 |
|
Figure 6-47
The external and internal oblique have been resected to reveal their relationship to each other and to the transversus abdominis muscle. |
medial aspect of the field between the peritoneum and the psoas fascia.
Because the ureter is attached not to the psoas fascia, but loosely to
the peritoneum, it normally falls forward with the peritoneum and its
contents, away from the operative field. If doubt exists regarding the
identity of the ureter, it should be stroked gently to produce
peristalsis (see Fig. 6-49).
visibility. They are self-retaining and offer excellent cephalad and
caudad exposure. If the incision does not comfortably expose the
involved vertebra, continue dissecting more posteriorly, taking
additional fibers of the latissimus dorsi, and even possibly the
quadratus lumborum, to allow more posterior exposure.
vertebrae. Parallel incisions may be made at higher levels for access
to the upper lumbar vertebrae, but they involve rib resection and
potentially are hazardous because of the proximity of the pleura and
the kidney. They should be performed in conjunction with a general
surgeon unless the orthopaedic surgeon has considerable experience in
this area.
 |
|
Figure 6-48 The transversus abdominis muscle is resected to reveal the peritoneum and the retroperitoneal fat.
|
 |
|
Figure 6-49
The abdominal muscles and viscera have been removed proximal to the level of the iliac crest to reveal retroperitoneal structures. Note the interval between the psoas muscle and the aorta. This interval provides access to the sympathetic chain and the anterior portion of the vertebral bodies. |
approach to the cervical spine, allowing quick and safe access to the
posterior elements of the entire cervical spine. It is used for the
following:
-
Posterior cervical spine fusion16
-
Enlargement of spinal canal (laminectomy or laminoplasty)
-
Treatment of tumors
-
Treatment of facet joint dislocations17,18
-
Nerve root exploration
-
Excision of some herniated discs
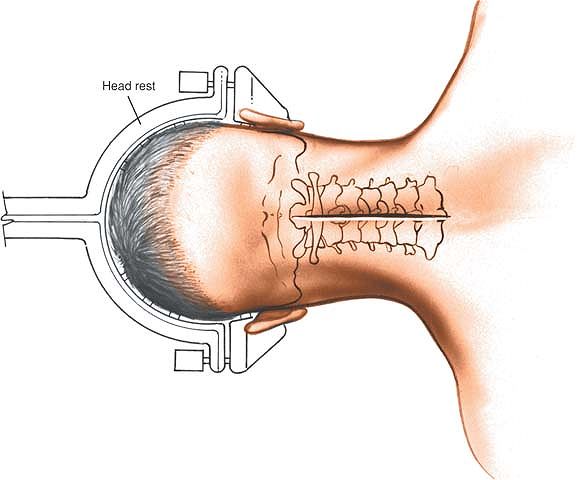
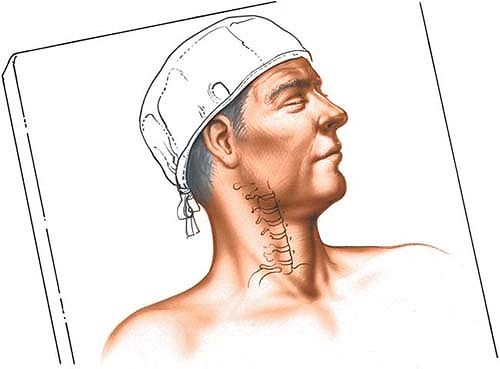
into a few degrees of flexion to open the interspinous spaces. Tongs
and a fixed brace are applied (Mayfield tongs or similar). This allows
for careful control of the head and neck position during the procedure,
minimizes the possibility of ocular pressure, and gives good access by
the anesthetist to the airway (Fig. 6-50).
has the advantage of decreasing venous bleeding, but it has been implicated as a cause of air emboli.
 |
|
Figure 6-50 The position of the patient for the posterior approach to the cervical spine.
|
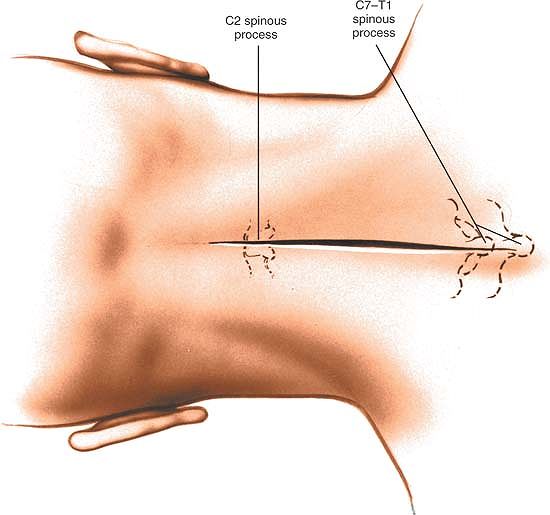
the most prominent landmarks in the vertebral arch. The C2 spinous
process is one of the largest cervical spinous processes, as are C7 and
T1. All three are quite palpable along the midline. Because it
sometimes is difficult to distinguish between C7 and T1 during surgery,
place a radiopaque marker (such as a needle) into the spinous process
at the level of the pathology before making the incision, so that the
exact location of the process can be identified. Sometimes placing a
second marker into C7 may be helpful. Because the distance between the
various cervical facet joints and interspaces is tiny, a significant
portion of the neck may be dissected unnecessarily unless the vertebra
being treated is identified, with the help of an x-ray film.
Use the needle that has been inserted into the spinous process as a
guide to and center point of the incision. Note that the skin of the
posterior cervical spine is thicker and less mobile than the skin of
the anterior neck, and that the resultant scar usually is broader;
however, hair usually covers most of the scar.
left and right paracervical muscles (which are supplied segmentally by
the left and right posterior rami of the cervical nerves).
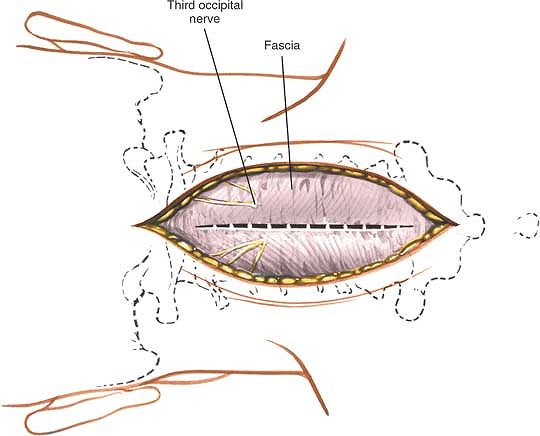
Minimal bleeding may come from venous plexuses that cross the midline;
these should be cauterized (Figs. 6-52 and 6-53).
unilaterally or bilaterally, depending on the exposure needed;
bilateral removal is done for a spine fusion and unilateral removal for
a herniated disc. Use a Cobb elevator or cautery, which can remove the
muscles from the bone without damaging them unduly (Fig. 6-54). Carry the dissection as far laterally as necessary to reveal the lamina and the facet joints (Figs. 6-55 and 6-56). If necessary, cauterize the segmental arterial vessel that runs between the facets.
 |
|
Figure 6-51 Make a straight incision in the midline of the neck, centering the incision over the area of pathology.
|
 |
|
Figure 6-52 Retract the skin flaps and incise the fascia in the midline. Note the position of the third occipital nerve.
|
 |
|
Figure 6-53 Continue the dissection down to the spinous processes through the nuchal ligament.
|
 |
|
Figure 6-54
Remove the paraspinal muscles subperiosteally from the posterior aspect of the cervical spine either unilaterally or bilaterally, depending on the exposure needed. Note that the vertebral artery is considerably anterior to the posterior facet joints. |
midline and cuts into muscles, however, notable bleeding can occur that
will require immediate cauterization. If the patient has significant
spina bifida, it is possible to enter the spinal canal, injuring neural
tissue.
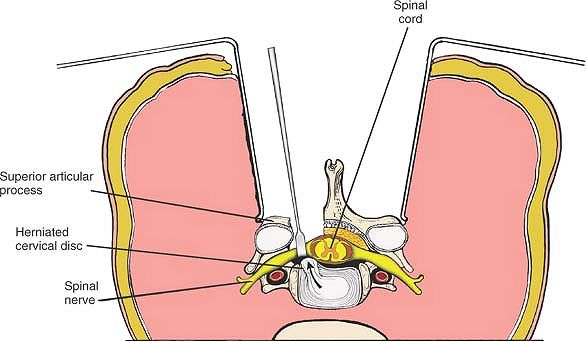
laminae. With a sharp blade, remove it from the leading edge of the
lamina of the inferior vertebra. Place a flat, spatula-shaped
instrument in the midline in the space between the two ligaments and
cut down on the ligamentum flavum, with the metallic unit separating
the ligamentum from the underlying dura. Perform a laminectomy, either
partial or complete, removing as much of the lamina as necessary to see
the blue-white dura, which lies immediately below it, probably covered
by epidural fat. Identify the posterior portion of the vertebral body,
the disc space, and the possibly herniated disc (Figs. 6-57 and 6-58).
Occasionally, the thin epidural veins surrounding the cord may bleed
significantly. The veins can bleed anywhere; they are hardest to
control between the anterior aspect of the cord and the posterior part
of the vertebral body.
 |
|
Figure 6-55 Bilateral exposure of the posterior cervical spine.
|
overzealously. If enough bone is removed during the laminectomy, both
medially and laterally, the exposure should be large enough to minimize
the need for cord retraction. The nerve roots themselves should be
retracted gently to prevent unnecessary tethering from postoperative
adhesions. Occasionally, the facet joint must be removed partially to
expose the nerve root.
of the cervical nerve roots supply the paraspinal muscles and sensation
to the overlying skin; they rarely are in danger. Even if a posterior
ramus must be cauterized, the nerve supply to the paracervical muscles
and skin is so rich that the denervation has no clinical effect.
profusely. Frequently, bipolar (or Malis) cauterization is the best way to control the venous bleeding.
 |
|
Figure 6-56
With a high-speed tool, then a small Kerrison rongeur, the caudal aspect of the lamina above, the rostral aspect of the lamina below, and the medial facet are removed. |
 |
|
Figure 6-57
Perform a laminectomy, partial or complete, removing as much lamina as needed. Gently retract the nerve root medially to identify the posterior portion of the vertebral body. |
 |
|
Figure 6-58 Identify the disc space and a possible herniated disc.
|
to the paracervical muscles may be cut or stretched as the muscles are
stripped past the facet joints. The muscles often contract, stopping
the small amount of hemorrhage; however, if the torn vessels can be
seen, they should be cauterized. The blood supply to the posterior
cervical muscles is generous. Cauterization causes no problem and
allows for a dry surgical field. Occasionally, a nutrient foramen of
the spinous processes or lamina may bleed. This can be controlled
easily with a dab of bone wax or cautery placed directly against the
foramen.
enclosed in a bony canal running through the transverse process
(transverse foramen). It is protected even if the transverse process is
dissected onto. If the process is destroyed as a result of infection,
tumor, or trauma, however, take great care not to enter the transverse
foramen (see Figs. 6-54 and 6-62).
addition, an extra vertebra may have to be dissected out proximally or
distally. The exposure may be expanded laterally by drawing the muscles
well out and past the facet joints and onto the transverse processes
without causing damage, except at C1 and C2. On occasion, the laminae
even may be exposed bilaterally and the laminectomy extended both
proximally and distally to improve exposure to the spinal cord and
nerve roots.
be extended proximally (staying in the midline plane) as high as the
occiput of the skull and as far distally as the coccyx via
subperiosteal removal of the paraspinal muscles.
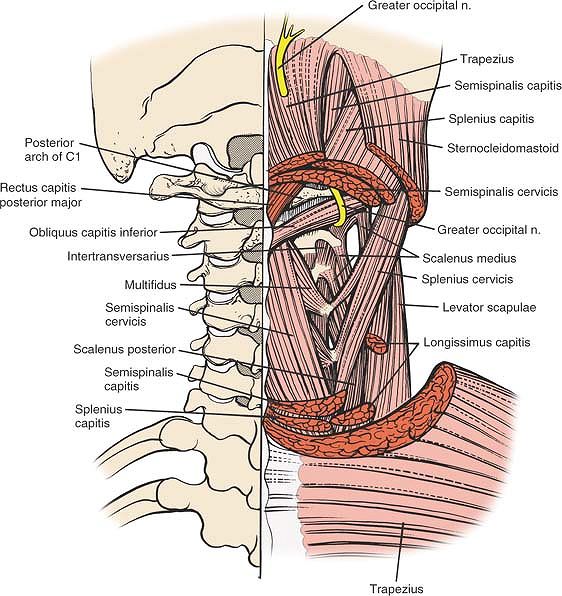
cervical spine run longitudinally and are supplied segmentally.
Although it is not critical to know the various individual posterior
muscles of the cervical spine, being aware of these muscles and their
layers is helpful. Because the approach itself is in the midline, it
disturbs no vital structures and is relatively safe.
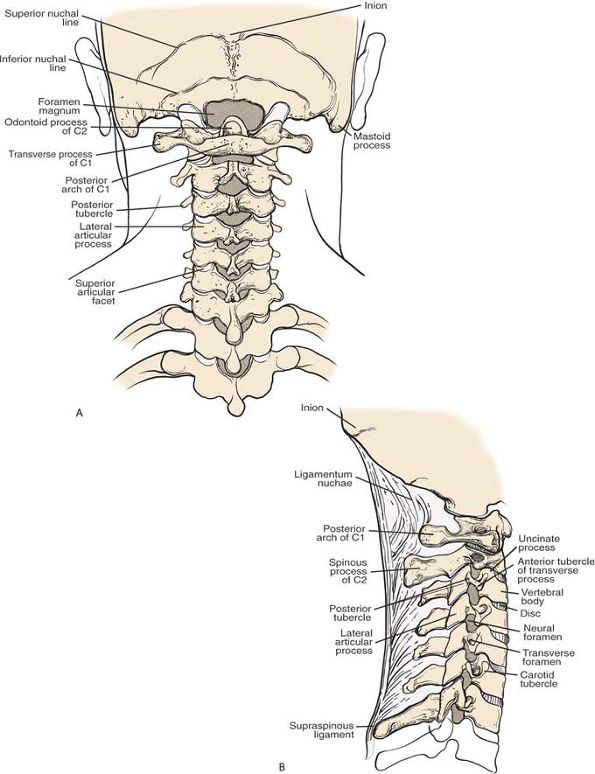
C6, are bifid. C2 is the largest proximal cervical spinous process; the
spinous processes of C3, C4, and C5 are relatively small. C7 is
thicker, is not bifid, and has a tubercle at its end. Because it is the
largest distal cervical spinous process, it is easy to palpate (see Fig. 6-63A).
caudad and posteriorly, serving as points of attachment for the
cervical muscles.
mobile than is the skin on the throat; it is attached directly to the
underlying fascia. The incision runs perpendicular to the tension line
of the skin, causing thicker scarring. Nevertheless, the wound usually
heals well, and, because the nape of the neck is covered with hair,
cosmetic concerns seldom are a problem.
takes origin from the occiput and inserts into the C7 spinous
processes, sending septa down to each of the cervical spinous processes
and dividing the more lateral paracervical muscles. The septum, which
is almost vestigial in humans, is well developed in quadrupeds, because
it helps the muscles support the head. It is the homologue of the
supraspinous ligament in the rest of the spine. Dissection through it
is safe, as long as it remains in the midline (see Fig. 6-63B).
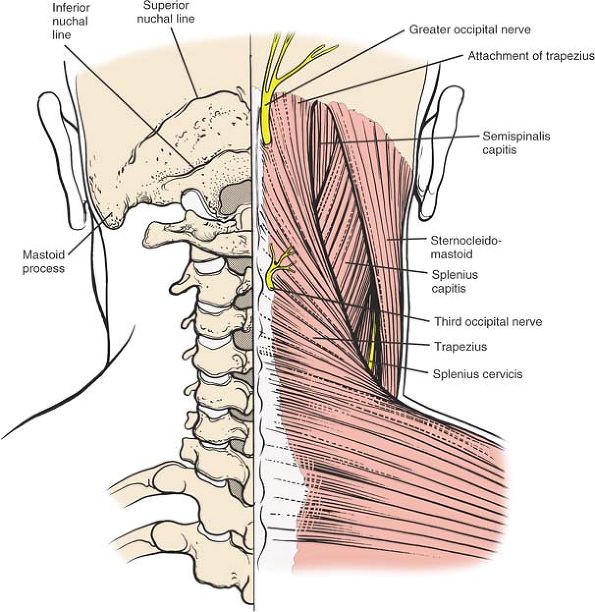
consists of the trapezius muscle, which takes origin from the superior
nuchal line and from all the spinous processes of the cervical spine.
The trapezius covers the entire cervical area; in common with its
counterpart in the lumbar spine, the latissimus dorsi, it is
essentially an upper limb muscle (Fig. 6-59).
filled by the splenius capitis, a relatively large, flat muscle that
takes origin from the midline (spine of C7, the lower half of the
ligamentum nuchae, and the upper three thoracic spinous processes) and
inserts into the occipital bone (Fig. 6-60).
 |
|
Figure 6-59
The superficial musculature of the cervical spine consists of the trapezius and the sternocleidomastoid muscles. Between these and deeper levels lies the intermediate layer, the splenius capitis. |
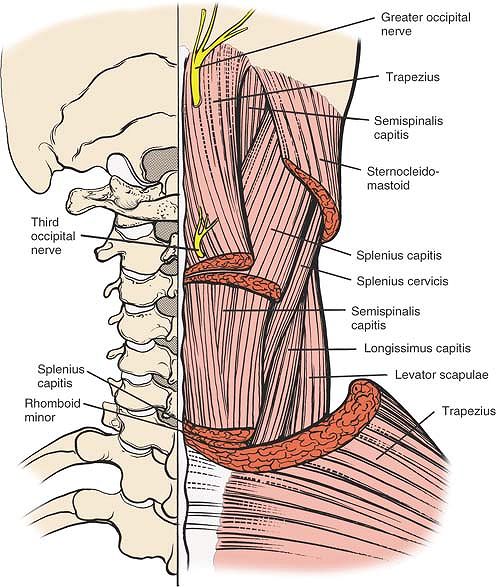
into three portions: superficial, middle, and deep. The superficial
portion consists of the semispinalis capitis, a relatively large muscle
that lies immediately beneath the splenius. The semispinalis capitis
takes its origin from the transverse processes of the cervical
vertebrae and inserts into the occipital bone. The middle portion of
the deep layer is filled by the semispinalis cervicis, which originates
from the transverse processes of the upper five or six thoracic
vertebrae
and
inserts into the midline interspinous processes. The deepest portion of
the deep layer consists of the multifidus muscles and the short and
long rotator muscles (Fig. 6-61).
 |
|
Figure 6-60
The superficial layer has been resected to reveal the splenius capitis, which also is resected partially. Deep to this are the semispinalis capitis, the longissimus capitis, the splenius cervicis, and, most laterally, the levator scapulae. |
medial to lateral at 45°. Lateral to the laminae are the joint
capsules, which completely surround the cervical facet joints. The
facet joints are in a frontal plane (Figs. 6-63B and 6-64).
canal is safe during this phase of the dissection. A wide, flat
instrument (such as a Cobb dissector) held transverse to the lamina
helps to protect the canal (see Fig. 6-54).
connects the lamina on one vertebra to the adjacent vertebra, filling
the space between the two. The ligaments are paired, one on each side,
and may be separated in the midline by a tiny space. They take origin
from the leading edge of the lower lamina and insert proximally into
small ridges on the anterior surface of the higher vertebra, about one
third up the anterior surface.
beneath the ligamentum flavum. Therefore, the ligament must be removed
carefully, so that the coverings of the cord (the outer dura, the
middle arachnoid, the inner pia) do not tear.
 |
|
Figure 6-61 The semispinalis capitis has been resected to reveal the deepest layer, the semispinalis cervicis, and the multifidi muscles.
|
posterior surface of the cervical vertebral bodies, within the
vertebral canal, and extends down through the entire spinal canal. The
ligament attaches to each vertebra and disc; it is broadest in the
cervical region. Over the ligament, on the floor of the canal, lie
large vertebral veins, comprising a nonvalvular venous plexus. These
may bleed and require cauterization.
vertebral artery. The artery runs upward in the neck through a series
of foramina in the transverse processes of the cervical vertebrae.
Vigorous decortication may breach the posterior walls of these foramina
and damage the artery, which carries a blood supply that is vital to
the hindbrain. The risks are far greater when the transverse processes
are involved in pathology. If the artery is damaged during dissection,
it should be packed to produce at least temporary control of bleeding.
In most situations, this will also produce definitive control;
occasionally, repair of the artery or legatum will be required (see Figs. 6-62 and 6-64).
 |
|
Figure 6-62
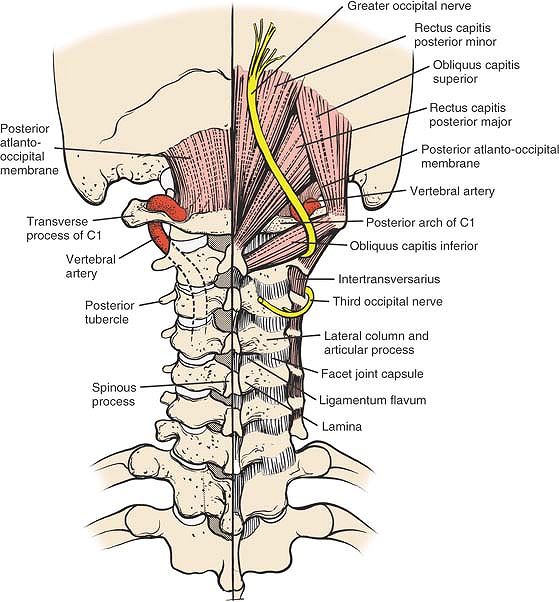
The muscles of the posterior triangle of the neck consist of the rectus capitis posterior minor and major, and the obliquus capitis superior and inferior. Note the course of the vertebral artery on the superior border of the arch of C1. It is lateral to the midline. The course of the vertebral artery in the transverse foramen distal to C1 is anterior to the facet joints. Rectus Capitis Posterior Major. Origin. Tendinous, from spinous process of axis. Insertion. Into lateral part of inferior nuchal line of occipital bone and immediately below this line. Action. Extends head and rotates it to same side. Nerve supply. Nerve branch of posterior primary rami main line of suboccipital nerve.
Rectus Capitis Posterior Minor. Origin. Tendinous, from tubercle of posterior arch of atlas. Insertion.
Into medial part of nuchal line of occipital bone and surface beneath it, and foramen magnum (only muscle to take origin from posterior arch of C1). Action. Extends head. Nerve supply. A branch of posterior primary main line of suboccipital nerve. Obliquus Capitis Inferior. Origin. From apex of spinous process of axis. Insertion. Into inferoposterior part of transverse process of atlas. Action. Rotates atlas; turns head toward same side. Nerve supply. Branches of posterior primary rami main line of greater occipital nerve.
Obliquus Capitis Superior. Origin. From tendinous fibers from upper surface of transverse process of atlas. Insertion. Into occipital bone between superior inferior nuchal lines; lateral to the semispinalis capitis. Action. Extends head and bends it laterally. Nerve supply. A branch of posterior primary division of greater occipital nerve (first cervical nerve).
|
 |
|
Figure 6-63 Osteology of the cervical spine in posterior (A) and lateral (B) views.
|
 |
|
Figure 6-64 Cross-section of the cervical spine. Note that the vertebral artery is anterior to the nerve root.
|
vertebrae C1 and C2, the atlas and the axis, is similar to that for the
rest of the cervical spine. Because the two vertebrae differ slightly
in their anatomy and function, however, they are discussed separately.
The uses for this approach are the following:
-
Spinal fusion19
-
Decompression laminectomy
-
Treatment of tumors
is the largest spinous process in the proximal part of the cervical
spine, it is hard to palpate except as a resistance. C1 has no spinous
process at all and is not palpable.
 |
|
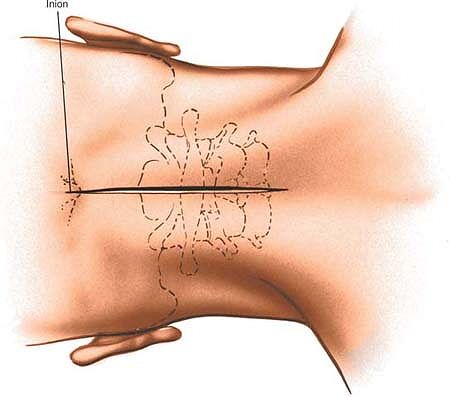
Figure 6-65 Make an incision in the midline from the external occipital protuberance inferiorly for 6 to 10 cm.
|
supplied by branches of the left and right posterior primary rami of
the proximal cervical nerve roots. The plane is internervous and
extensile.
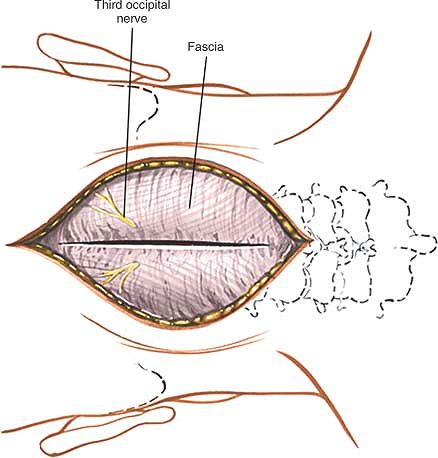
incising the fascia and nuchal ligament in the midline of the neck,
cutting down onto the large spinous process of C2 (Figs. 6-60 and 6-67).
Extend this fascial incision distally onto the spinous process of C3
and then proximally onto the tubercle of C1. Continue proximally,
cutting down onto the external occipital protuberance.
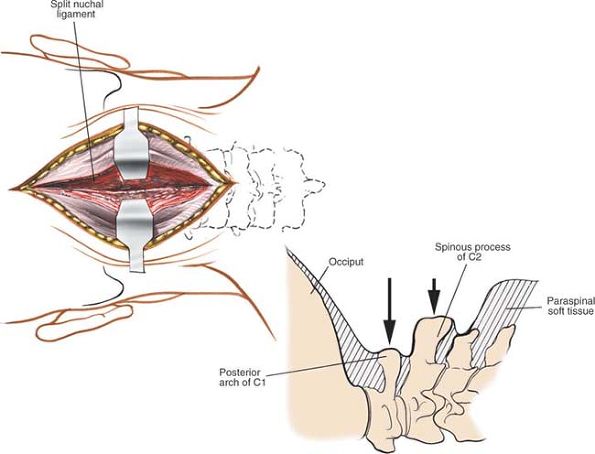
Use a wide dissecting instrument (such as a Cobb elevator) to avoid
inadvertently breaching the spinal canal. Note that the facet joints
between C1 and C2 are about an inch further anterior than are those
between C2 and C3. Carry the dissection up to the base of the occiput,
if necessary, to expose the superior margin of the ring of C1 (see Fig. 6-68).
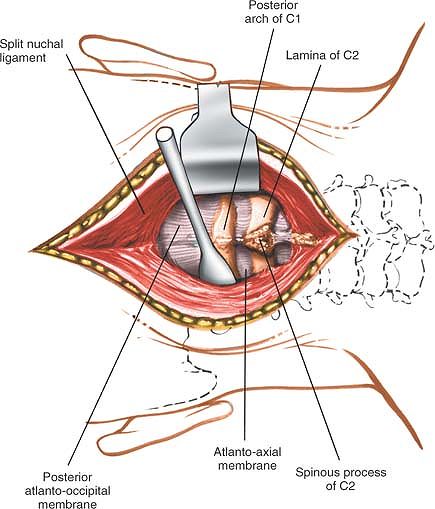
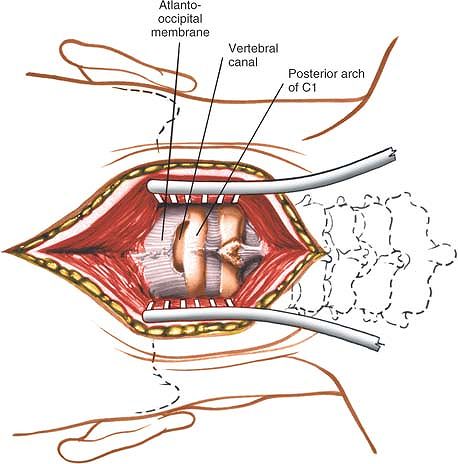
atlantoaxial ligament) can be removed from between C2 and C1, and the
posterior atlantooccipital membrane can be removed from between C1 and
the occiput (Fig. 6-69). This rarely is
necessary. Usually, separating these membranes from bone is all that is
needed to pass a wire underneath the arch of C1 so that the area can
retain bone graft. Once these posterior ligaments have been removed,
the dura of the cervical portion of the spinal cord is uncovered.
 |
|
Figure 6-66 Deepen the wound in line with the skin incision by incising the fascia and nuchal ligament in the midline of the neck.
|
between the dura and the bony ring at the level of C1-2, and the cord
rarely has to be retracted. Retracting the cord is extremely hazardous,
because overzealous retraction can cause death from respiratory
paralysis; in principle, it simply should not be retracted.
These nerves, which are branches from the posterior rami, supply a
large area of skin at the back of the scalp. They run upward from a
lateral position, and midline dissection does not damage them. Take
care when dissecting laterally to stay on bone and avoid damaging these
nerves.
the operative field. It passes from the transverse foramen of the
atlas, immediately behind the atlanto-occipital joint, and pierces the
lateral angle of the posterior atlantooccipital membrane. It is
vulnerable at that point during the approach (see Fig. 6-62).
paracervical muscles from their attachments to the skull. Extend the
incision distally and strip the muscles off the posterior bony elements
of C3.
approach to the spinous processes of the remaining cervical vertebrae.
Theoretically, the approach can be extended down to the coccyx.
 |
|
Figure 6-67 Incise the nuchal ligament down onto the large spinous processes of C2. Lateral view (inset). Note that the ring of C1 is further anterior than the spinous process of C2.
|
 |
|
Figure 6-68 Remove the paracervical muscles from the posterior elements of C1 and C2. Carry the dissection up to the base of the occiput.
|
 |
|
Figure 6-69 Remove the posterior atlanto-occipital membrane from between C1 and the occiput, if necessary.
|
of the upper cervical spine. As in other parts of the spine, the
muscles covering C1 and C2 lie in three layers. The outer layer
consists of the trapezius, a muscle of the upper limb. The intermediate
layer is made up of the paraspinal muscles, in this case, the splenius
capitis and the semispinalis capitis.
there are four pairs of small muscles that drive the unusual movements
that these joints are capable of. The riskiest part of surgery in the
area occurs in the deepest plane. The vertebral artery, which runs
through the foramen transversarium (still deeper) never should be seen
during dissection, but its position always must be kept in mind.
accommodating the insertions of the semispinalis cervicis and
multifidus, deep muscles that attach to it and stop, leaving the atlas
with almost no muscle attachment so that it is free to rotate around
the occiput. The posterior vertebral arch of C2 and its lamina, which
ascends to the spinous processes, are massive enough to support the
larger spinous process.
or inion, a large boss of bone in the center of the occiput, divides
the superior nuchal line, which extends from it to each side. The
superior nuchal line separates the scalp above from the area of
insertion of the nuchal muscles (see Fig. 6-63).
blood supply. Because the incisions run along the midline, they suffer
minimal tension. Cosmetically, they are difficult to see because of the
hairline.
extends from the external occipital protuberance to the spinous process
of the seventh cervical vertebra. A septum extends from its anterior
border; it attaches to the posterior tubercle of the atlas and all the
remaining spinous processes of the cervical spine (see Fig. 6-63B).
consist of the trapezius (in the superficial layer) and the splenius
capitis, which covers the semispinalis capitis and the longissimus
capitis (all in the intermediate layer; see Figs. 6-59 and 6-60).
processes before inserting into the base of the skull. Deep to it lies
the semispinalis cervicis, which inserts onto the axis.
of the suboccipital triangle, the rectus capitis posterior major and
minor, and the oblique capitis inferior and superior (see Fig. 6-62).
form the remaining posterior coverings of the cord, are homologues of
the original ligamentum flavum. The spinal canal at C1-2 is
particularly spacious, allowing extensive motion.
aspect of the suboccipital triangle: the greater occipital nerve (the
posterior primary ramus of C2) and the third occipital nerve (the
posterior primary ramus of C3; see Figs. 6-59 and 6-62). The most important structure in the suboccipital triangle is the vertebral artery.
This key blood supply to the hindbrain ascends in the neck through a
series of foramina in the transverse processes. At the level of the
atlas, it pierces the foramen transversarium of the atlas and then
turns medially behind the atlantooccipital joint. To enter the spinal
canal, it pierces the posterior atlanto-occipital membrane at its
lateral angle; therefore, it is extremely vulnerable during dissection
of the atlanto-occipital membrane (see Fig. 6-62).
anterior vertebral bodies from C3 to T1. It also allows direct access
to the disc spaces and uncinate processes in the region. It is used for
the following:
-
Excision of herniated discs (R.B. Cloward, personal communication, 1969)20
-
Interbody fusion (see the section regarding the anterior approach to the iliac crest for bone graft)
-
Removal of osteophytes from the uncinate processes and from either the anterior or the posterior lip of the vertebral bodies
-
Excision of tumors and associated bone grafting
-
Treatment of osteomyelitis
-
Biopsy of vertebral bodies and disc spaces
-
Drainage of abscesses
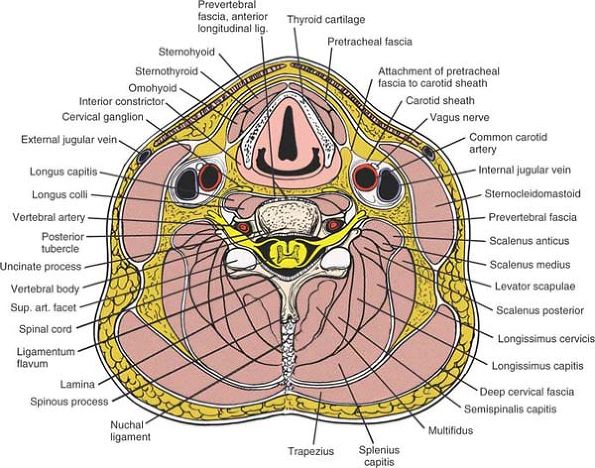
structure at risk during the anterior approach to the cervical spine.
The left recurrent laryngeal nerve ascends in the neck between the
trachea and the esophagus, having branched off from its parent nerve,
the vagus, at the level of the arch of the aorta. The right recurrent
laryngeal nerve runs alongside the trachea in the neck after hooking
around the right subclavian artery. In the lower part of the neck, it
crosses from lateral to medial to reach the midline trachea; therefore,
it is slightly more vulnerable during the exposure than is the left
recurrent laryngeal nerve. This is why some surgeons prefer left-sided
approaches, whereas others simply approach from the side of pathology.
 |
|
Figure 6-70
Place the patient supine on the operating table with a small sandbag between the shoulder blades to ensure an extended position of the neck. Turn the patient’s head away from the planned incision. |
small sandbag or roll between the shoulder blades to ensure extension
of the neck. Turn the patient’s head away from the planned incision to
provide good access to the side of the neck (Fig. 6-70).
Some cases may require application of halter traction so that it can be
used later if distraction is required. Elevate the table 30° to reduce
venous bleeding and make the neck more accessible. Place the patient’s
arm at his or her side after careful padding.
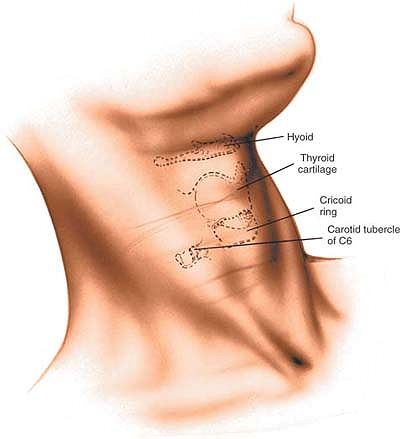
-
Hard palate–arch of the atlas
-
Lower border of the mandible–C2-3
-
Hyoid bone–C3
-
Thyroid cartilage–C4-5
-
Cricoid cartilage–C6
-
Carotid tubercle–C6
The sternocleidomastoid, an oblique muscle, runs from the mastoid
process to the sternum, just lateral to the midline of the neck. To
make it more prominent, turn the head away from the muscle in question,
into the operating position.
 |
|
Figure 6-71 Make an oblique incision in the skin crease of the neck at the appropriate level of the vertebral pathology.
|
transverse skin crease incision at the appropriate level of the
vertebral pathology (see above). The incision should extend obliquely
from the midline to the posterior border of the sternocleidomastoid
muscle. Such an incision has extreme cosmetic advantage (see Fig. 6-71).
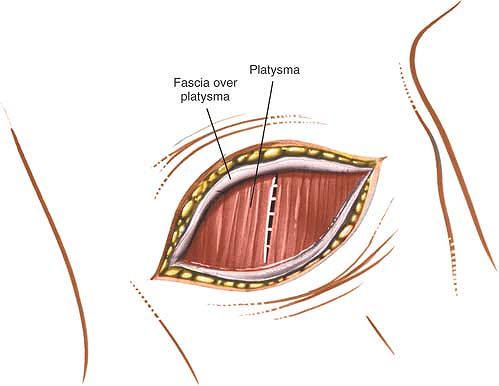
incising or dividing the platysma muscle causes no significant
problems; the muscle is supplied high up in the neck by branches of the
facial (seventh cranial) nerve.
sternocleidomastoid muscle (which is supplied by the spinal accessory
nerve) and the strap muscles of the neck
(which receive segmental innervation from C1, C2, and C3; see Fig. 6-74, cross section).
 |
|
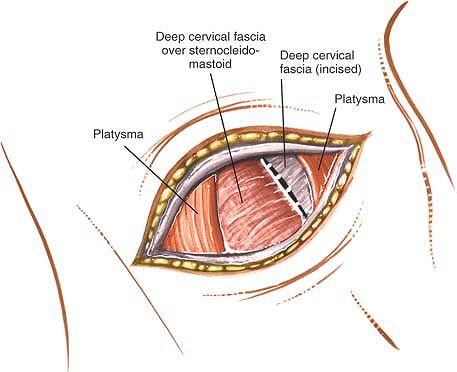
Figure 6-72
Incise the fascial sheath over the platysma in line with the skin incision. Split the platysma longitudinally, parallel to its long fibers. |
longus colli muscles, which are supplied separately by segmental
branches from the second to the seventh cervical nerves (see Fig. 6-76, cross section).
this reason, some surgeons inject the area with a dilute solution of
epinephrine (Adrenalin) before incising the skin.
 |
|
Figure 6-73 Identify the anterior border of the sternocleidomastoid and incise the fascia medially anterior to it.
|
Then, split the platysma longitudinally using the tips of the index
fingers, dissecting parallel to the long fibers. The platysma fibers
can also be divided with a knife. Identify the anterior border of the
sternocleidomastoid muscle and incise the fascia immediately anterior
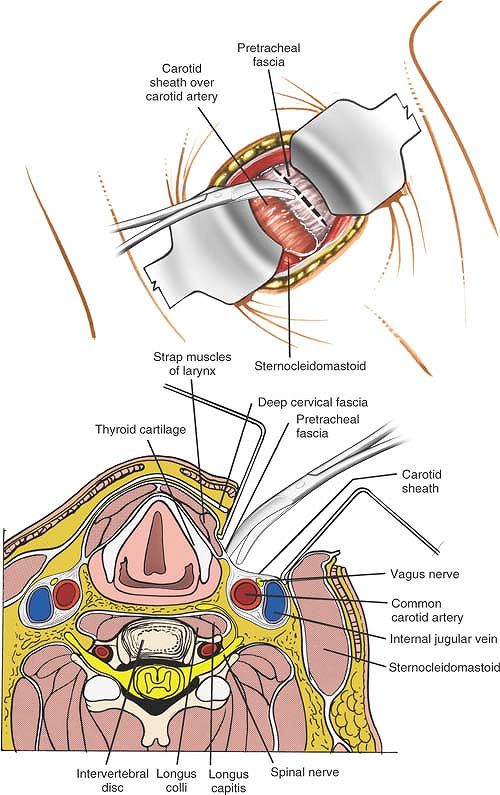
to it (Fig. 6-73). Using the fingers, gently retract the sternocleidomastoid muscle laterally. Retract the sternohyoid
and sternothyroid strap muscles (with the associated trachea and underlying esophagus) medially.
edge of the carotid sheath and the midline structures (thyroid gland,
trachea, and esophagus), cutting through the pretracheal fascia on the
medial side of the carotid sheath. Retract the sheath and its enclosed
structures laterally with the sternocleidomastoid muscle (Fig. 6-75).
 |
|
Figure 6-74
Retract the sternocleidomastoid laterally, and the strap muscles and thyroid structures medially. Cut through the exposed pretracheal fascia on the medial side of the carotid sheath. The cervical spine C3 through C5 (cross-section). Retract the sternocleidomastoid laterally and the strap muscles medially, and incise the pretracheal fascia immediately medial to the carotid sheath. |
and inferior thyroid arteries, may limit the extent to which this plane
can be opened up above C3-4. Occasionally, either or both of them may
have to be ligated and divided to open the plane.
 |
|
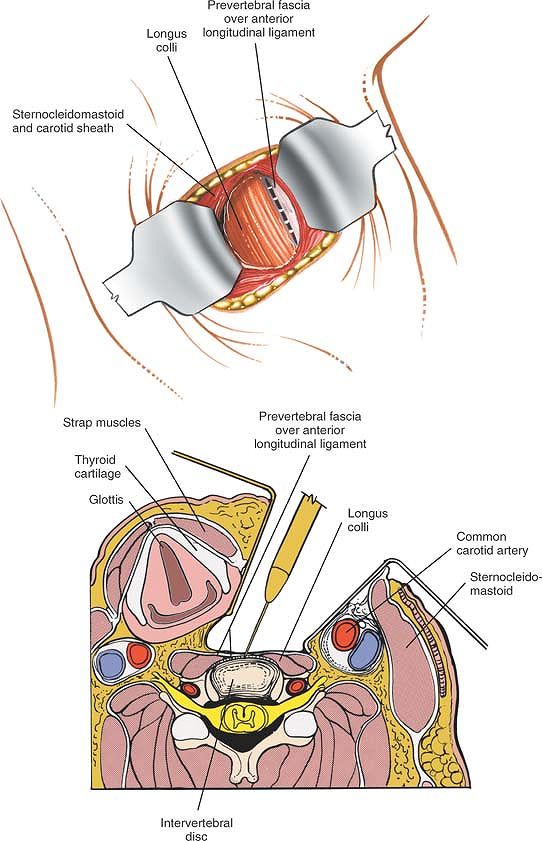
Figure 6-75
Retract the sternocleidomastoid and the carotid sheath laterally, and the strap muscles, trachea, and esophagus medially to expose the longus colli muscle and pretracheal fascia. Retract the sternocleidomastoid muscle and carotid sheath laterally, and the strap muscles and thyroid structures medially, then split the longus colli muscle longitudinally in the midline (cross-section). |
 |
|
Figure 6-76
Dissect the longus colli muscle subperiosteally from the anterior portion of the vertebral body and retract each portion laterally to expose the anterior surface of the vertebral body. The longus colli muscles are retracted to the left and right of the midline to expose the anterior surface of the vertebral body (cross-section). |
by blunt dissection, proceeding carefully in a medial direction behind
the esophagus, which is retracted from the midline.
the longus colli muscle and the prevertebral fascia. The anterior
longitudinal ligament in the midline can be seen as a gleaming white
structure. The sympathetic chain lies on the longus colli, just lateral
to the vertebral bodies (see Fig. 6-75).
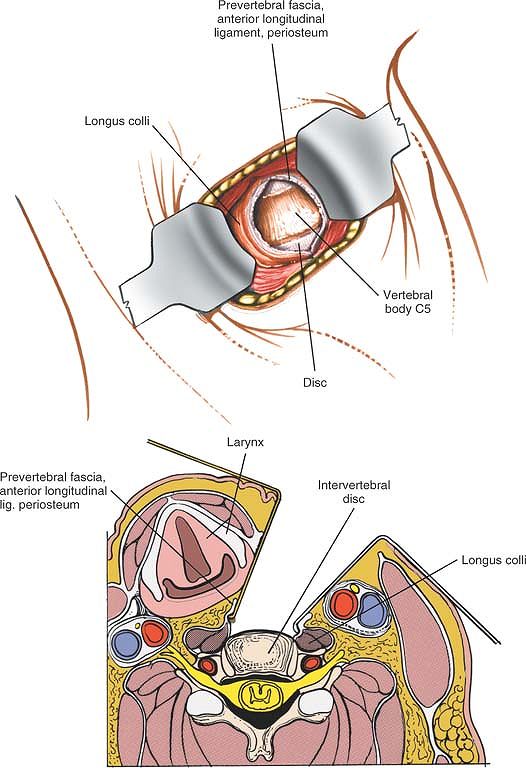
longitudinally over the midline of the vertebral bodies that need to be
exposed (see Fig. 6-75, cross section).
Then, dissect the muscle subperiosteally with the anterior longitudinal
ligament and retract each portion laterally (i.e., to the left and
right of the midline) to expose the anterior surface of the vertebral
body (Fig. 6-76).
Obtain a lateral radiograph after placing a needle marker in the
appropriate vertebral body to identify the level correctly. Make sure
that the retractors are placed underneath each of the longus colli
muscles, widening the exposure while protecting the recurrent laryngeal
nerve, trachea, and esophagus.
may be traumatized during the deepest layer of the approach. Protect it
by placing the retractors well under the medial edge of the longus
colli muscle (Fig. 6-79).
may be damaged or irritated, causing Horner’s syndrome. Protect them by
making sure that dissection onto the bone is subperiosteal from the
midline.
are protected by the anterior border of the sternocleidomastoid muscle.
Do not place self-retaining retractors in this area, or the sheath will
be endangered. If additional retraction is necessary, use hand-held
retractors with rounded ends (see Figs. 6-74, cross section, and 6-79).
lies in the costotransverse foramen on the lateral portion of the
transverse processes, should not be visible during the approach unless
the plane of operation strays well away from the midline (Fig. 6-81; see Fig. 6-76, cross section).
field in lower cervical approaches. If it is divided accidentally, it
may retract behind the carotid sheath, where it is difficult to
retrieve and tie off (see Fig. 6-80).
esophagus. Unless they are placed underneath the longus colli muscle,
the retractors used should be rounded and hand-held (see Fig. 6-76, cross section).
the longus colli muscle subperiosteally from the vertebral body. Take
care not to proceed too far laterally to avoid damaging the sympathetic
chain.
approach to the cervical spine lies in appreciating the three fascial
layers of the neck. The most superficial fascial layer is the investing
layer of deep cervical fascia. The fascia
surrounds the neck like a collar, but splits around the
sternocleidomastoid and trapezius muscles to enclose them. Posteriorly,
it joins with the ligamentum nuchae (nuchal ligament). The superficial
layer is incised along the anterior border of the sternocleidomastoid
muscle. Dividing the layer of fascia allows the sternocleidomastoid to
be retracted laterally and separated from the underlying strap muscles.
The only structures that lie superficial to it are the platysma muscle
(a remnant of the old panniculus carnosus, or muscle of the skin) and
the external jugular vein, which can be divided safely if it intrudes
into the operative field (Figs. 6-77 and 6-78).
which forms a layer between sliding surfaces. It invests the strap
muscles and runs from the hyoid bone down into the chest (see Fig. 6-78).
Its key relationship is with the carotid sheath, which encloses the
common carotid artery, the internal jugular vein, and the vagus nerve.
The pretracheal fascia is continuous with the carotid sheath at the
sheath’s lateral margin (see Figs. 6-77 and 6-79).
Hence, the pretracheal fascia must be divided on the medial border of
the carotid sheath so that the carotid sheath can be retracted
laterally and the midline structures can be retracted medially. Two
sets of vessels, the superior and inferior thyroid vessels, run from
the carotid sheath through the pretracheal fascia into the midline. On
rare occasions, the thyroid vessels have to be divided to enlarge the
exposure (see Fig. 6-80). The superior laryngeal nerve, however, which runs with the superior thyroid vessels, must be preserved.
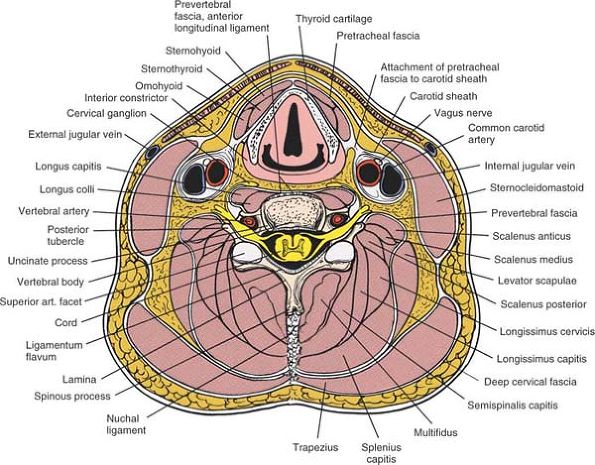 |
|
Figure 6-77
Cross-section at the level of C5. Note the deep cervical fascia, the pretracheal fascia, and the prevertebral fascia. Note the relationship of the pretracheal fascia to the carotid sheath. |
a firm, tough membrane that lies in front of the prevertebral muscles.
On its surface runs the cervical sympathetic trunk, which lies roughly
over the transverse processes of the cervical vertebrae. Beneath the
prevertebral fascia are the left and right longus colli muscles (see Figs. 6-77 and 6-80).
enlargement of the anterior tubercle of the transverse process of C6.
It is larger than all other vertebral tubercles (there is no anterior
tubercle of C7) and may be palpable. The tubercle of C6 is the key
surgical landmark in the anterior incision (Fig. 6-82).
palpable just beneath the thyroid cartilage. The only complete ring of
the trachea, it is opposite the C6 vertebral body (see Figs. 6-71 and 6-78).
runs obliquely down the side of the neck from the mastoid process to
the sternum and clavicle. It is enclosed in fascia, which must be
divided on the medial side before the muscle can be retracted
laterally. The nerve supply of the sternocleidomastoid comes from the
accessory nerve, which innervates the muscle from its posterior and
lateral surfaces. There is no danger of neurologic damage as long as
the dissection remains on the medial or anteromedial side of the
muscle. If it strays to the posterior side, however, the spinal
accessory nerve, which supplies not only the sternocleidomastoid, but
also the trapezius, can be damaged (see Fig. 6-78).
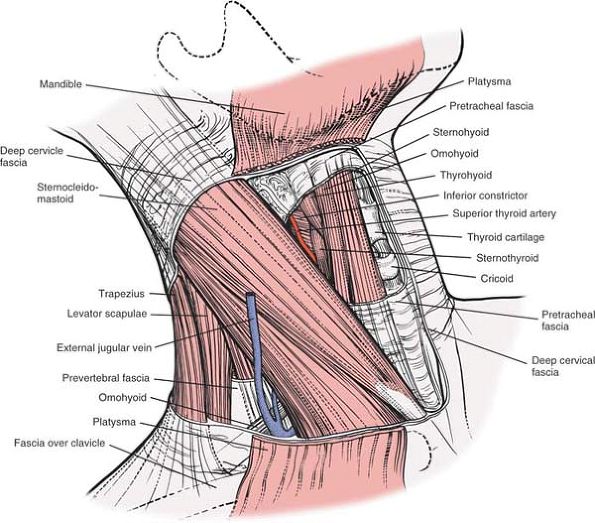 |
|
Figure 6-78
The platysma and deep cervical fascia have been removed. Note that the deep cervical fascia (investing fascia) encloses the sternocleidomastoid. The deeper pretracheal fascia encloses the strap muscles and thyroid structures. |
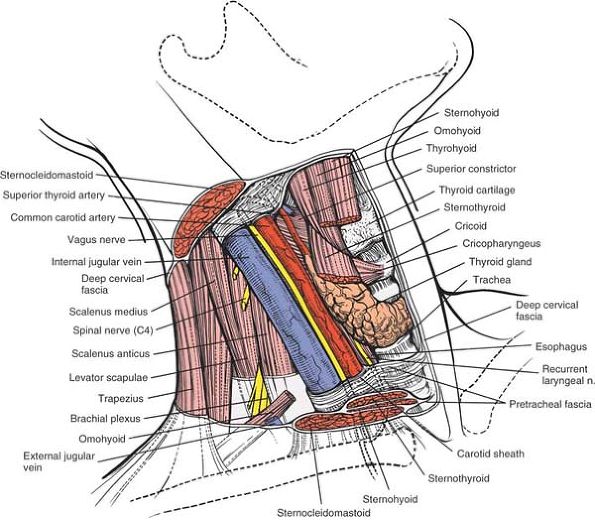 |
|
Figure 6-79
The sternocleidomastoid and strap muscles, and the pretracheal fascia have been resected. The carotid sheath and its contents have been exposed. The thyroid gland, cartilage, and trachea are seen. Note the course of the recurrent laryngeal nerve. |
cleavage lines of the skin of the neck. Inferiorly and anteriorly,
these lines run transversely, making the skin crease incision
advantageous. The skin on the anterior part of the neck is thinner and
more mobile than is the skin on the back of the neck, because of both
the loose subcutaneous tissue and the superficial fascia that remains
unconnected to the investing fascia of the neck. As a result, skin
retraction is easy; the skin incision can be moved to accommodate the
needs of the surgery. For extensive exposures, a longitudinal, slightly
oblique incision can be made parallel to the medial border of the
sternocleidomastoid muscle.
The muscle is difficult to denervate, because most of its nerve supply
comes from the cervical branch of
the
facial nerve and begins in the region of the mandible. In any case, the
muscle is not of great functional importance; sewing it carefully
during closure can improve the cosmetic appearance of the scar.
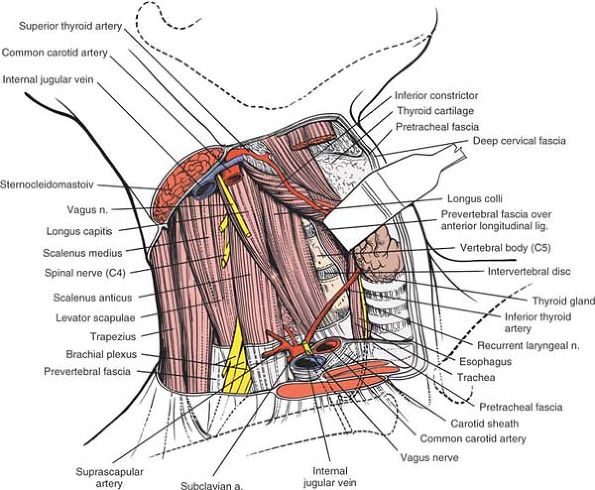 |
|
Figure 6-80
The carotid sheath and its contents have been resected. The larynx and its related structures are retracted medially. The longus colli and scalenus muscles with their overriding prevertebral fascia are seen. The sympathetic chain lies on the lateral border of the longus colli muscle. Note the position of the recurrent laryngeal nerve between the trachea and esophagus. |
The sheath contains the common carotid artery, which divides at the
upper border of the thyroid cartilage into internal and external
carotid arteries. It also contains the internal jugular vein and the
vagus nerve (see Fig. 6-79). After the plane
between the carotid sheath and the trachea and esophagus has been
entered, it is easy to develop by blunt dissection. The esophagus,
however, is a fragile structure that is damaged easily by injudicious
retraction.
the vertebral column, between C1 and T3. The muscles are pointed at
their ends and broad in the middle. They must be removed from the
vertebral bodies to expose the vertebrae. Removal does not denervate
them, because they are innervated segmentally and laterally from their
posterior surfaces. Running on the anterolateral surfaces of the longus
colli muscles is the
cervical sympathetic trunk, with its numerous ganglia. These must be avoided (see Figs. 6-77 and 6-80).
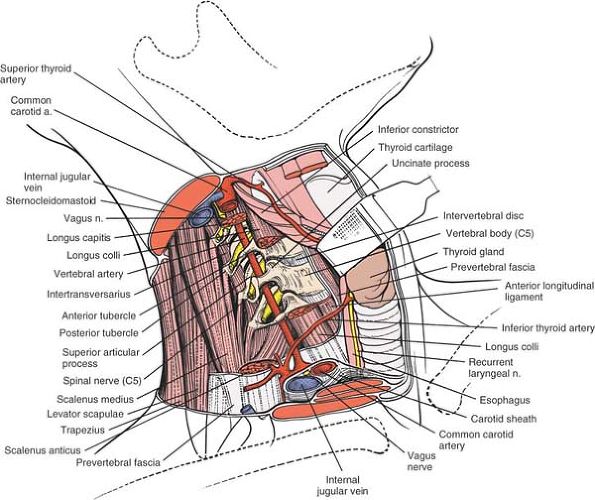 |
|
Figure 6-81
The longus colli, the longus capitis, and the scalenus anticus muscles have been resected to reveal the anterior portion of the vertebral bodies and transverse processes. Note the course of the vertebral artery through the transverse processes anterior to the nerve root. Note the course of the superior and inferior thyroid vessels. |
vagus nerve. The left recurrent laryngeal nerve descends into the
thorax within the carotid sheath. It curves around the aortic arch and
ascends back in the neck, running between the trachea and esophagus to
supply the larynx. The right recurrent laryngeal nerve descends within
the carotid sheath and curves around the subclavian artery before
ascending into the neck at a higher level than the left recurrent
laryngeal nerve. In addition, the right recurrent laryngeal nerve is,
on rare occasions, aberrant, leaving the carotid sheath at a higher
level and crossing the operative field at the level of the thyroid
gland (see Figs. 6-70 and 6-80).
Thus, left-sided approaches often are preferred. The nerves usually are
safe as long as retractors are placed correctly underneath the longus
colli muscles.
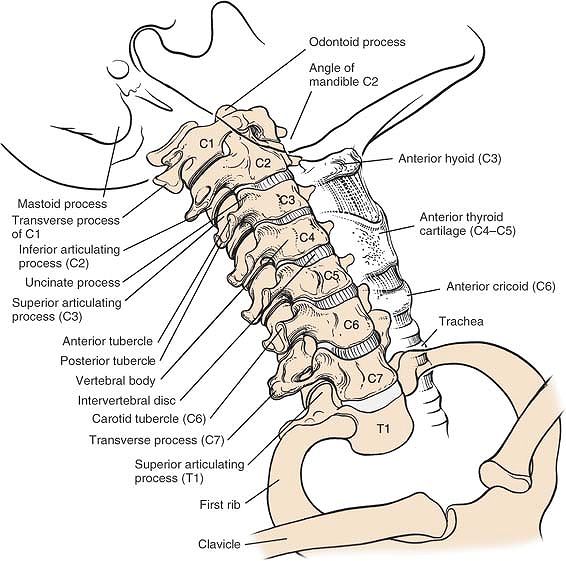 |
|
Figure 6-82 Osteology of the cervical spine, anterior view.
|
spine was developed for the drainage of tuberculous abscesses in this
part of the spine. Its major advantage is that it does not involve
major encroachment to the thoracic cavity. The approach is less
extensive than a formal thoracotomy and offers a poorer exposure. It
probably is best for limited exposures in patients who are at high
risk. This approach can also be combined with a
posterior/posterolateral approach to the spine to decompress the
vertebral canal circumferentially.
-
Abscess drainage22,23
-
Vertebral body biopsy
-
Partial vertebral body resection
-
Limited anterior spinal fusion
-
Anterolateral decompression of the spinal cord
-
Tumor debulking
bolsters positioned longitudinally on each side of the rib cage to
allow for chest expansion. Drape widely over the rib cage area so that
the rib cage can be exposed laterally (see Fig. 6-101).
any case, a needle should be placed into the spinous process of the
vertebra to be exposed so that a lateral x-ray film can pinpoint the
position. Remember that the spinous processes of the thoracic area are
long and slender, and tend to overlap the vertebrae below. Note that
the rib in the area to be exposed often is more prominent.
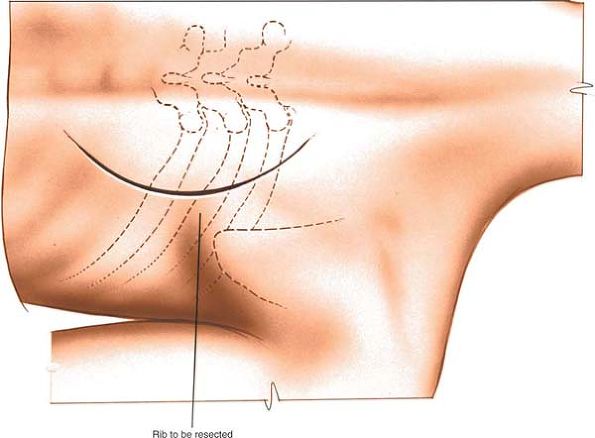 |
|
Figure 6-83
Make a curved linear incision lateral to the appropriate spinous process. Center the incision over the rib involved in the pathologic process. |
appropriate spinous process and 10 to 13 cm long. Center the incision
over the rib that is involved in the pathologic process (Fig. 6-83).
involves splitting the trapezius muscle and cutting through the
paraspinal muscles. Because the paraspinal muscles are innervated
segmentally, no significant denervation occurs. The trapezius receives
its supply from the spinal accessory nerve higher up.
skin incision, cutting through the trapezius muscle parallel with its
fibers close to the transverse processes. Deep to it are the paraspinal
muscles (Fig. 6-84).
resected all the way to bone. The plane often is bloody; a cutting
cautery (diathermy) is useful (Fig. 6-85).
dissection with a periosteal elevator (Fig. 6-86).
Dissect laterally along the superior border of the rib and medially
along the inferior border. Continue dissection subperiosteally on to
the anterior surface of the rib. Divide the rib about 6 to 8 cm from
the midline. Then, lift it up and carefully cut any remaining muscle
attachments and the costotransverse ligament. Twist the rib’s medial
end to complete the resection (Figs. 6-87 and 6-88). At this point, the field may flood with a gush of pus from the opened abscess cavity.
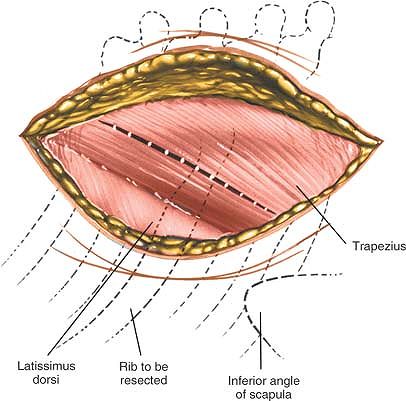 |
|
Figure 6-84 Incise the subcutaneous fat and fascia in line with the skin incision. Incise the trapezius muscle parallel with its fibers.
|
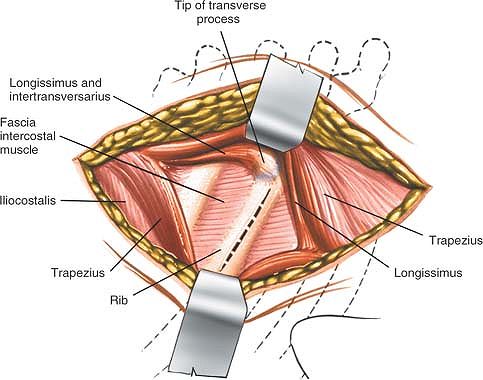 |
|
Figure 6-85
Cut down onto the posterior aspect of the rib to be resected. Strip the muscles laterally and medially onto the transverse process. Incise the periosteum over the rib. |
process; divide the process at its junction with the lamina and
pedicle, using a rongeur biting instrument. Remove the transverse
process to gain wider exposure (see Fig. 6-88, cross section).
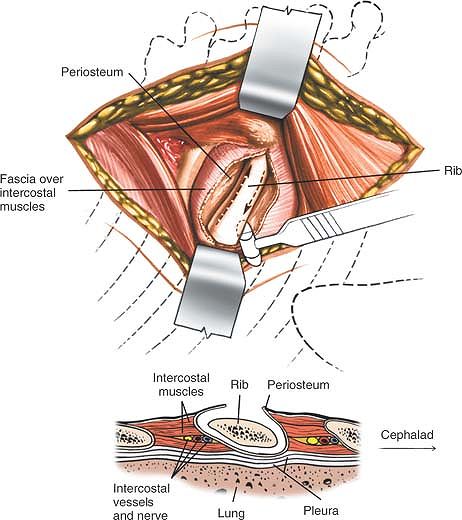 |
|
Figure 6-86 Separate all the muscle attachments from the rib, using subperiosteal dissection.
|
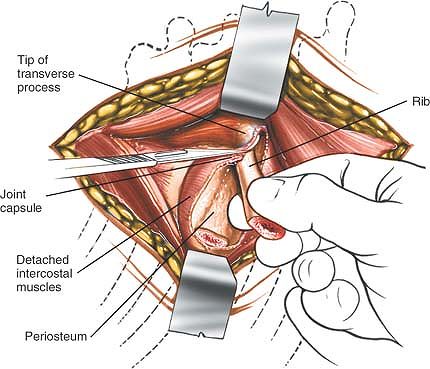 |
|
Figure 6-87
Divide the rib about 6 to 8 cm from the midline. Lift it up and carefully cut any remaining muscle attachments and the costotransverse ligament. |
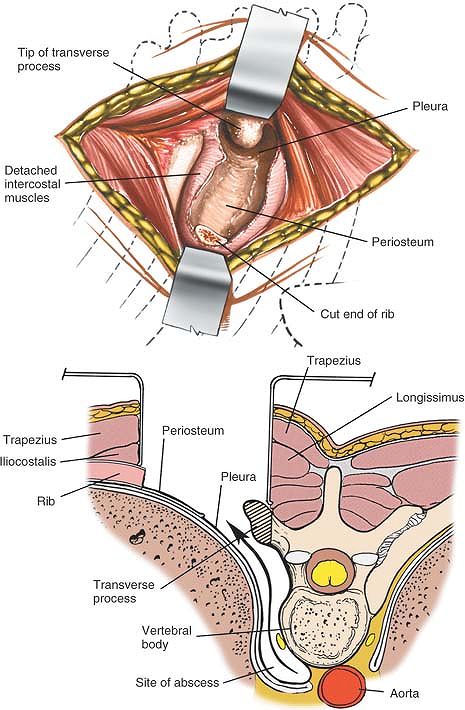 |
|
Figure 6-88
Twist the rib’s medial end to complete the resection and remove the rib. The abscess cavity now is exposed. The abscess cavity may extend along the lateral and anterior borders of the vertebra (cross-section). Resect the transverse process if greater exposure is necessary. |
palpation and dissection, removing the parietal pleura from the
vertebral body. Note that this plane is safe only if the pleura is
thickened by disease. Careful blunt dissection is essential to avoid
entering the pleural cavity. At this point, the vertebral body and disc
space should have been exposed.
often are damaged when the ribs are stripped. They lie on the inferior
border of the rib and should be ligated if they are cut (see Fig. 6-94).
thickened by infections of the underlying lung. As dissection proceeds,
damage to the pleura can be minimized by using blunt dissection to
strip the pleura from the anterolateral surface of the affected
vertebral body. The approach can cause a pneumothorax, however. If there is a sucking sound or a tear in the pleura, it should be treated by inserting a chest tube after closure.
muscles transversely in line with the transverse process to facilitate
retraction.
unrivaled exposure of the anterior portions of the vertebral bodies,
from T2 to T12. Nevertheless, this approach seldom is used, mainly
because of its dangers. A surgeon who uses the transthoracic approach
only occasionally should operate with a thoracic surgeon who is
accustomed to dealing with the hazards of the area.24,25
-
Treatment of infections, such as tuberculosis of the thoracic vertebral bodies26
-
Fusion of the vertebral bodies
-
Resection of the vertebral bodies for tumor and reconstruction with bone grafting
-
Correction of scoliosis
-
Correction of kyphosis
-
Osteotomy of the spine
-
Anterior spinal cord decompression
-
Biopsy
table, stabilizing the patient with a kidney rest or sandbags. Move the
hand and arm on the side to be approached above the patient’s head or
onto an airplane splint (Fig. 6-89). Place a
small pad in the axilla of the dependent side to avoid compression of
the axillary artery and vein. Feel for a radial pulse after
positioning; make sure that there is no venous obstruction in the arm.
The surgeon can be positioned in front of or behind the patient.
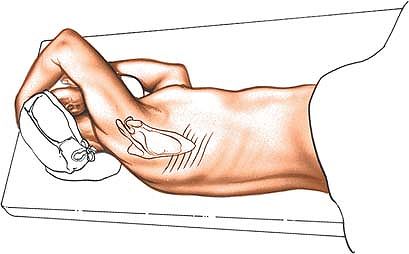 |
|
Figure 6-89
Place the patient on his or her side for the anterior transthoracic approach to the spine. On the side to be approached, move the patient’s hand and arm above his or her head. |
either side, approaching from the right side is easier because the
aortic arch and aorta can be avoided.
with the patient in the lateral position. Remember that the scapula is
mobile and the position of the tip will vary from patient to patient.
Palpate the spines of the thoracic vertebrae. They are long and slender. Observe the inframammary crease on the anterior chest wall.
the scapula and curve it forward toward the inframammary crease.
Complete the incision by extending it backward and upward toward the
thoracic
spine,
ending at a point halfway up the medial border of the scapula and
halfway between the spine and the scapula. The incision usually
overlies the seventh or eighth rib (Fig. 6-90).
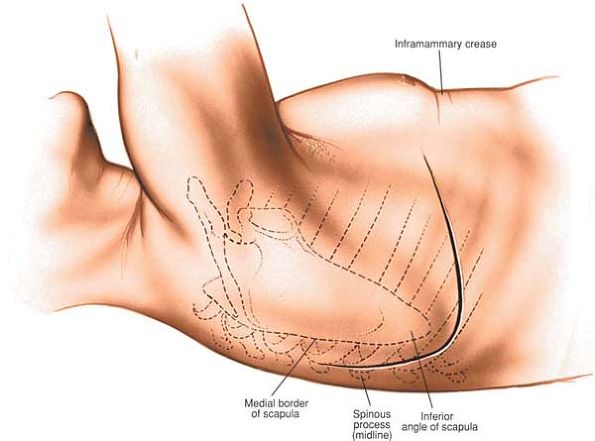 |
|
Figure 6-90
Begin the incision two fingerbreadths below the tip of the scapula. Curve the incision forward toward the inframammary crease. Complete the incision by extending it backward and upward toward the thoracic spine. The incision usually overlies the seventh rib. |
It seldom is necessary to cut the more posterior rhomboid muscles.
Because the operation is not performed in an intermuscular plane,
bleeding is a problem; cutting cautery (diathermy) can be used to
control it (Figs. 6-98 and 6-99).
intercostal space or by resection of one or more ribs. Rib resection
creates a better exposure, and the cut ribs can be used for bone
grafting.
location of the pathology to be treated. Unless the vertebrae involved
are low (between T10 and T12), use the fifth intercostal space (between
the fifth and sixth ribs) for entering the chest, because the scapula
easily overrides the healing site and will
not cause clicking. For pathology at T10 to T12, use the sixth
intercostal space, which provides better exposure of the lower
vertebral bodies. During its range of motion, however, the scapula may
have to jump over the callus formed at the healing site, causing a
click.
with cutting diathermy. Cut the periosteum on the upper border of the
rib and into the pleura in this line. Entering the pleura from above
the ribs avoids damage to the intercostal nerve and vessels, which lie
along its lower border (Fig. 6-94; see Fig. 6-93).
For greater exposure, strip all muscular attachments from either the
cephalad or the caudad rib (usually the fifth), using a periosteal
elevator or cautery, and resect the posterior three fourths of the rib
as far posterior as necessary (Fig. 6-95).
ribs apart; spread the ribs slowly to allow the muscles to adapt.
Incising the paraspinal muscles seldom is necessary. Ensure complete
hemostasis, especially in the posterior angle, before proceeding.
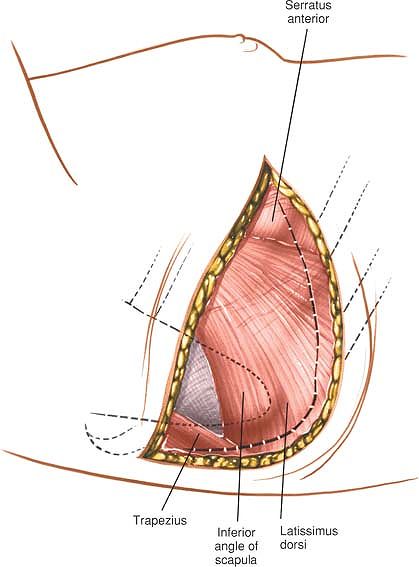 |
|
Figure 6-91 Divide the latissimus dorsi posteriorly in line with the skin incision.
|
gently retract it anteriorly, using moist lap pads to protect it. Under
it lies the posterior mediastinum. These make identification easier.
Incise the pleura over the lateral side of the esophagus so that the
esophagus can be retracted and the anterior part of the spine reached (Fig. 6-96).
The esophagus is easy to mobilize with finger dissection; retract it
from the anterior surface of the spine with two Penrose drains. The
intercostal vessels cross the operative field; one or more may have to
be tied off (Fig. 6-97). Tying off more
intercostal vessels than is necessary should be avoided, however,
because the blood supply to the spinal cord from these vessels varies.
Damage from ischemia may occur on rare occasions if more than two
sequential intercostal vessels are ligated close to the vertebral
bodies. Approaching the vertebral body from the right side obviates the
need to ligate both the left and right segmental intercostal arteries.
Approaching the vertebrae from the right side is safer and simpler than
is trying to move the aorta itself (Fig. 6-100B).
vulnerable at two stages. They are damaged most often during rib
resection, when they run along the undersurface of the rib; they also
may be damaged during exposure to the vertebrae within the chest and
must be tied off carefully before they are transected and allowed to
retract (see Figs. 6-94 and 6-100A).
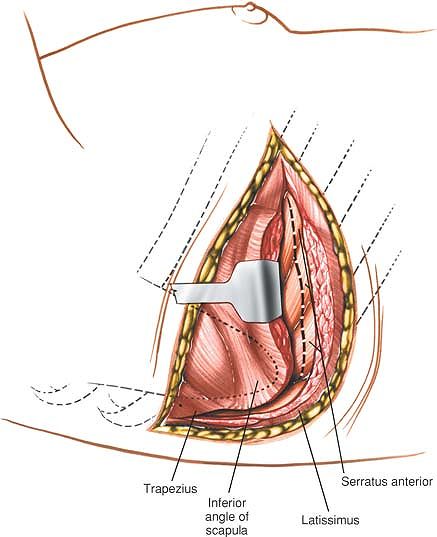 |
|
Figure 6-92 Divide the serratus anterior along the line of the skin incision down to the ribs.
|
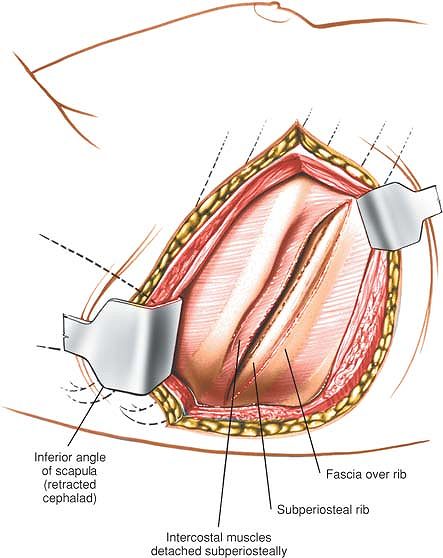 |
|
Figure 6-93
Elevate the scapula with the cut attached muscles proximally to expose the underlying ribs. Cut the periosteum on the upper border of the rib. |
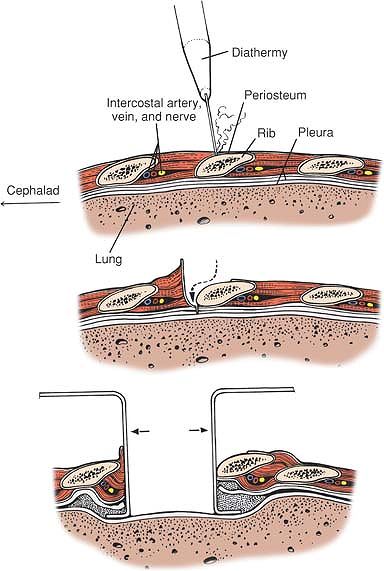 |
|
Figure 6-94
Enter the pleura from above the rib to avoid damage to the intercostal nerve and vessels that lie along this lower border. Insert a rib spreader to hold the ribs apart. |
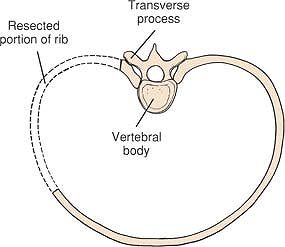 |
|
Figure 6-95 Resect the posterior three fourths of the ribs as far posterior as necessary for greater exposure.
|
provide good access to vertebrae from T2 to T12. In the lower part of
the incision, part of the diaphragm may need to be resected to enhance
the exposure. To accomplish this, remove the arcuate ligament from its
origin on the transverse process of L1. Note that the risks of surgery
increase in this area, because two major body cavities may be entered.
Reattach the diaphragm before closing.
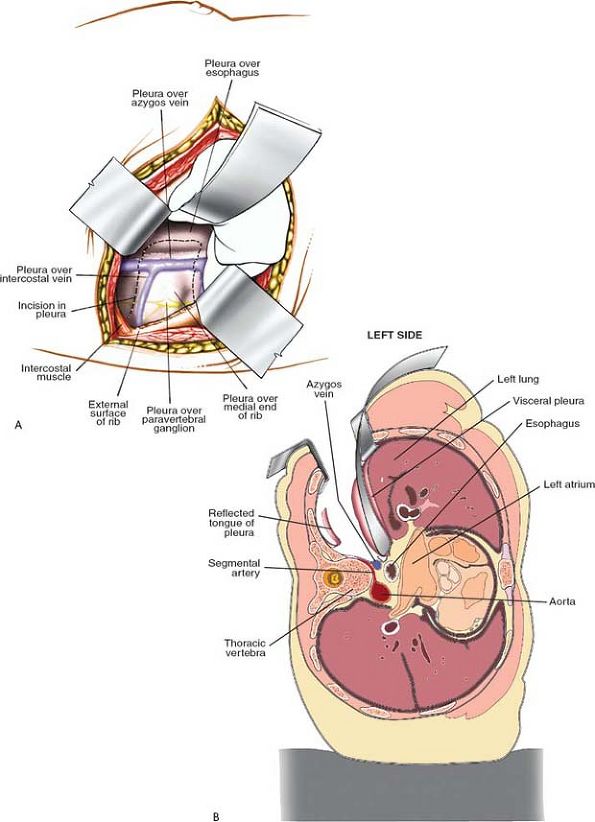 |
|
Figure 6-96
Retract the deflated lung anteriorly. Identify the esophagus over the vertebral bodies. Incise the pleura over the lateral side of the esophagus to enable it to be retracted. (A) View from surgeon standing dorsal to the spine. (B) Axial view of expoure with patient in the decubitus position. |
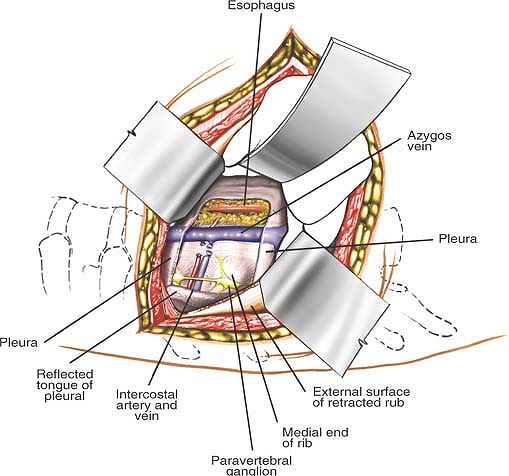 |
|
Figure 6-97
Mobilize the esophagus and retract it from the anterior surface of the spine. The intercostal vessels that cross the operative field are ligated. |
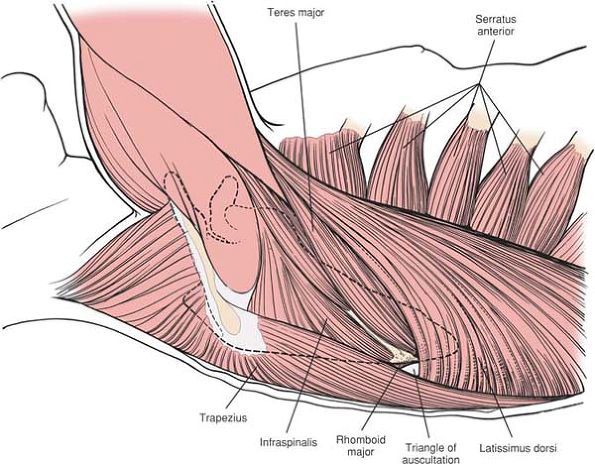 |
|
Figure 6-98 The superficial muscles of the posterolateral aspect of the thorax.
|
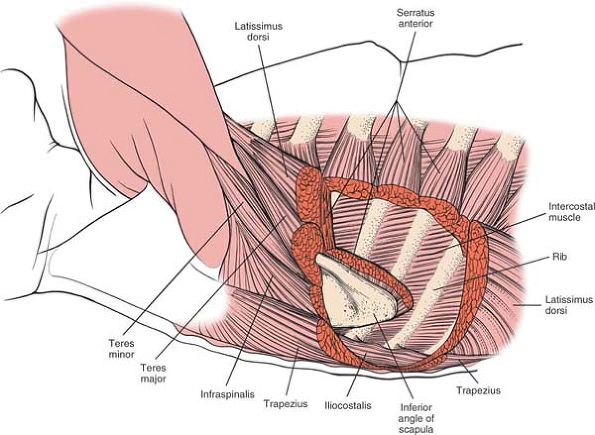 |
|
Figure 6-99
The superficial muscles of the posterior wall of the thorax (the trapezius, serratus anterior, latissimus dorsi, and teres major) have been resected to reveal the rib cage and the intercostal muscles. |
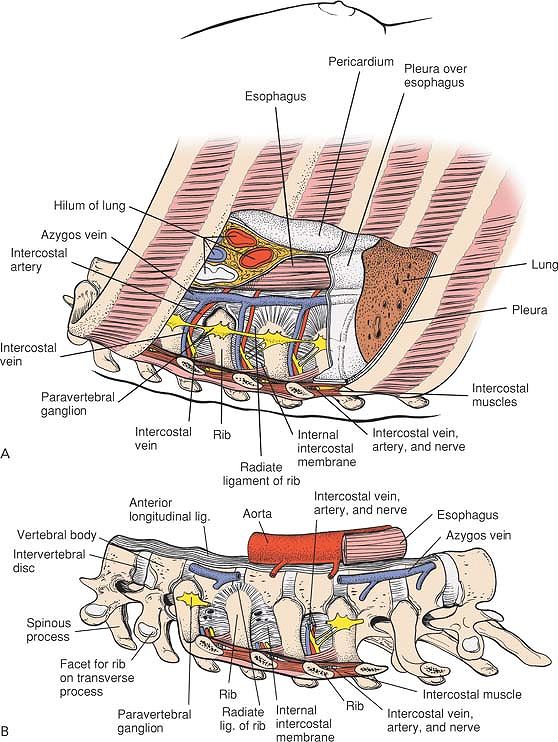 |
|
Figure 6-100 (A)
The ribs and lung have been resected, as well as the posterior pleura, to reveal the esophagus, azygos vein, and intercostal arteries and nerves. Note the position of the sympathetic chain. (B) A detailed view of the anterolateral aspect of the thoracic spine. It is surgically significant that the azygos vein and esophagus overlie the vertebral bodies and must be mobilized to expose them. |
is the approach used most frequently for the surgical treatment of
scoliosis.27,28,29,30,31
The approach is safe, avoiding vital structures, and allows direct
approach to the posterior aspect of the vertebral bodies in an
internervous plane.
-
Scoliosis surgery (see the section regarding rib resection and the posterior approach to the iliac crest for bone graft)
-
Posterior spine fusions (extensive and
limited; see the section regarding the posterior approach to the iliac
crest for bone graft) -
Removal of tumors of the posterior aspect of the vertebrae
-
Open biopsy
-
Stabilization of fractured vertebrae (see the section regarding the posterior approach to the iliac crest for bone graft)
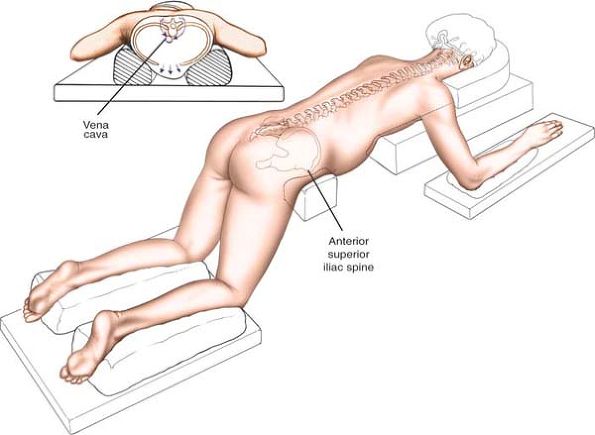 |
|
Figure 6-101
The position of the patient on the operating table for the posterior approach to the thoracic and lumbar spines. Place the bolsters so that the anterior abdominal wall clears the table; this allows emptying of the vertebral venous plexus to the vena cava. |
bolsters along each side so that the anterior chest wall clears the
table and the chest can expand. The bolsters should be long enough to
reach and support the anterior superior iliac spine so that the
anterior abdominal wall clears the table as well; this allows emptying
of the nonvalvular vertebral venous plexus into the vena cava, reducing
operative bleeding (Fig. 6-101).
mark the midline. The beginning of the gluteal cleft should be draped
with a clear plastic drape so that it still can be seen. The spinous
processes of C7 and T1 are the
largest
spinous processes in the lower cervical and upper thoracic spines. They
offer a guide to the location and level of the incision if the spinous
processes are counted down from C7.
lumbar spines that require surgery. Use the spinous processes of C7 and
T1 and the gluteal cleft as guides. A scalpel drawn along a
straightedge between these two points leaves an exact midline incision (Fig. 6-102).
(Frequently, the spinous processes are rotated away from the midline in
association with scoliosis; nevertheless, for cosmetic reasons, the
incision should be placed along the midline.)
posterior primary rami of the individual nerve roots in the thoracic
and lumbar spines. Because the incision is in the midline, it is truly
internervous; the nerves do not cross the midline.
whether they have deviated from the midline as they rotate in
scoliosis. Continue dissecting down to the middle of the spinous
processes and move the muscle origins to either side of the surface. In
children, split the spinous process apophyses longitudinally and
dissect them to each side of the processes with a Cobb elevator (Fig. 6-103).
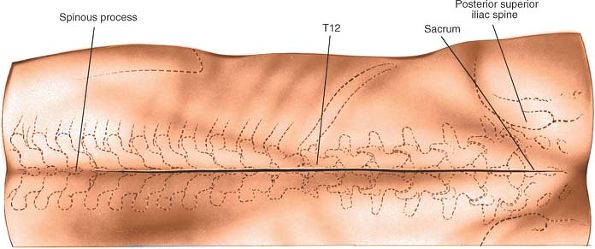 |
|
Figure 6-102 Make a straight midline incision over the thoracic and lumbar spines that require surgery.
|
In the thoracic area, work in a distal to proximal direction, in the
direction of the muscle fibers along the spinous process. After the
paraspinal muscles have been stripped from the spinous processes and
laminae, keep the dissection open with self-retaining retractors (Fig. 6-105).
rotators from the base of the spinous processes to the leading edges of
the laminae. Then, strip the muscles from the rest of the laminae
laterally, onto the transverse processes (Figs. 6-106 and 6-107).
emerge posteriorly from between the transverse processes, close to the
facet joints. Because of the significant overlap of innervation in the
paraspinal muscles, loss of an individual posterior primary ramus is
not harmful (see Figs. 6-106B and 6-111).
directly off the aorta appear between the transverse processes and
supply the paraspinal muscles. They bleed when muscles are stripped
from the transverse processes and must be
cauterized. The posterior primary rami are close to these vessels (see Figs. 6-106B and 6-111).
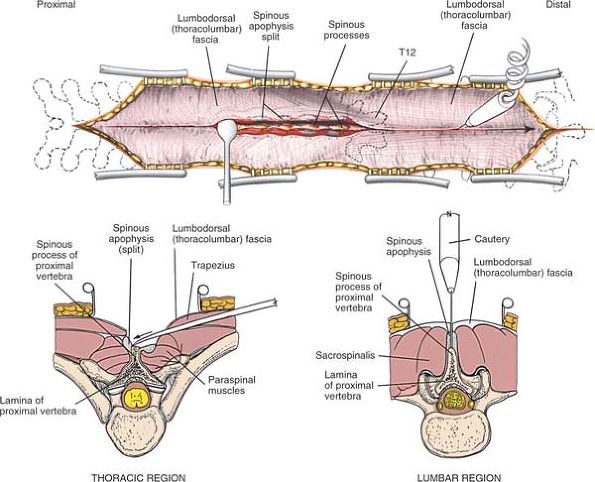 |
|
Figure 6-103
Dissect down onto the middle of the spinous processes. In children, split the spinous apophyses longitudinally and dissect them to either side with a Cobb elevator (inset). |
carry the dissection out onto the tips of the transverse processes. If
the area being worked in is tight, extend the incision one vertebra
higher or lower, whichever is appropriate.
the entire spine, from the cervical area to the coccyx. Because no
nerves cross the midline of the body, the nerves that segmentally
supply the paraspinal muscles remain safe.
12th (last) rib and dissect one level distal to it to locate the
transverse process of L1. Note that the last rib is mobile, a floating
rib without sternal attachment, whereas the transverse process of L1 is
quite rigid and firm, and does not yield to pressure. The rib also is
longer and more tubular than the transverse process (see Fig. 6-100).
After the last rib has been found, identify the nearby facet joints.
The descending facet joint of T12 is a lumbar facet joint, set in the
sagittal plane, whereas the ascending facet joint at the
upper end of T12 is a thoracic facet joint, set in a frontal plane (see Fig. 6-110).
Identifying the direction of facets, the last rib, and the first lumbar
transverse process provides a precise anatomic location. The only
alternative is to place markers in the spinous processes in the lumbar
area and to obtain a radiograph, or to carry the dissection distally
and identify the sacrum.
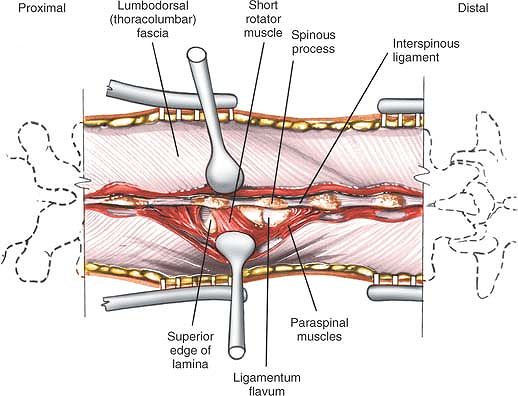 |
|
Figure 6-104 Remove the paraspinal muscles from the spinous processes and partially from the laminae by subperiosteal dissection.
|
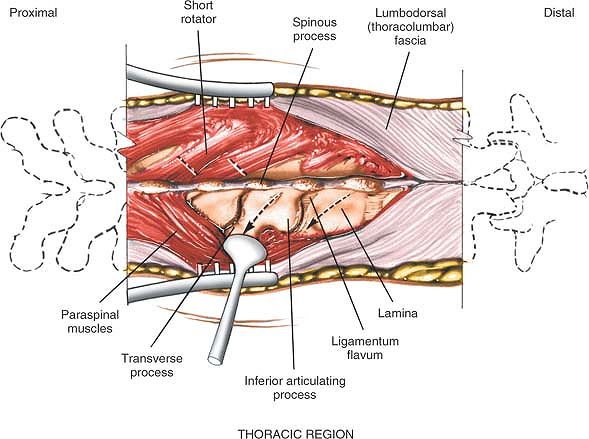 |
|
Figure 6-105
In the thoracic area, work from distal to proximal, in the direction of the muscle fibers along the spinous processes. With the use of Cobb elevators, remove the short rotators from the base of the spinous processes to the leading edges of the laminae. Then, strip the muscles from the rest of the laminae laterally onto the transverse processes. |
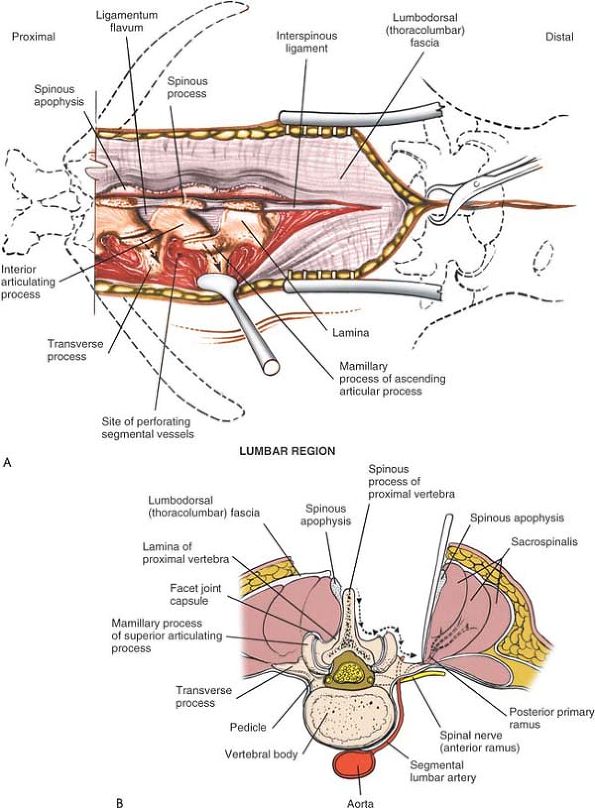 |
|
Figure 6-106 (A)
In the lumbar area, strip the paraspinal muscles from proximal to distal. Remove the joint capsule from medial to lateral. After crossing the mamillary process on the tip of the ascending facet, dissect laterally and caudally onto the transverse process. Be prepared to cauterize the segmental vessels that appear between the transverse processes. (B) Note that the transverse process is further anterior and distal than the mamillary process. |
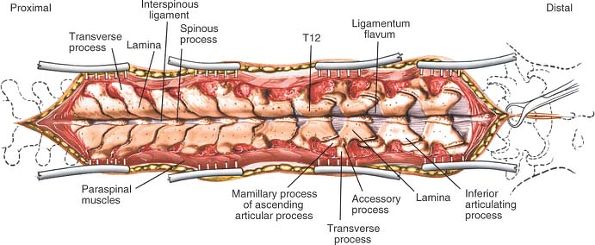 |
|
Figure 6-107
After you have stripped the paraspinal muscles from the spinous processes, laminae, and transverse processes, keep the dissection open with self-retaining retractors. |
each vertebral level, either in a proximal to distal direction or in a
distal to proximal direction. A half-inch osteotome may be used in
conjunction with the Cobb elevator to strip the facet joint capsules
from the ascending and descending facets, and to continue the
dissection laterally onto the transverse processes (see Fig. 6-106B).
-
Superficial layer: the mooring muscles that attach the upper extremity to the spine
-
Intermediate layer: the muscles of accessory respiration
-
Deep layer: the paraspinal muscle system, the intrinsic muscles of the back
surgical exposure of the spine, but the layering concept clarifies how
the anatomy relates to the dissection.
muscles can be subdivided into two layers: the most superficial layer
consists of the trapezius and latissimus dorsi; the deeper layer is
composed of the rhomboid major and minor.
consists of the serratus posterior superior and the serratus posterior
inferior, which are small, laterally placed muscles that attach to the
spine.
sacrospinalis muscles (erector spinalis) and a deep, obliquely running
layer consisting of the semispinalis, multifidus, and rotator muscles.
peripheral nerves: the trapezius by the spinal accessory nerve, the
rhomboids by the nerve to them from C5, and the latissimus dorsi by the
thoracodorsal nerve. They are not affected by a midline dissection.
at each level of the spine by the posterior rami of the thoracic and
lumbar nerves. Their nerve supplies usually are safe, but they may be
denervated partially by excessive lateral dissection.
processes in the region, with T1 being slightly larger. They point
directly posteriorly, with minimal caudal angulation, and are easily
palpable. The large L5 spinous process, which also has minimal caudal
angulation, can be palpated, but it cannot be differentiated from the
other equally large lumbar spinous processes. The gluteal cleft, which
runs between the protuberances of the gluteal (cluneal) muscles, is
easy to see.
than that on the anterior chest wall and abdomen. It usually heals with
a fine line scar because there is so little tension across the sutured
incision. The skin in the lumbar region (which is dissected
subcutaneously to leave the iliac crest accessible for a bone graft)
and the skin in the thoracic region (which is dissected subcutaneously
to reach the ribs) heal well, despite the subcutaneous dissection.
Dimpling of the skin over the iliac crest or ribs does not occur as
long as the thick, subcutaneous, fatty tissue layer is taken with the
skin to prevent it from adhering to the cut bony surfaces.
are much narrower than are those in the lumbar area, and more muscles
attach directly to their tips. As a result, dissection must approach
the tips of the spinous processes exactly in the midline, without
straying to either side. More bleeding occurs in the thoracic region,
mainly because of the direct attachment of muscle fibers from the
trapezius and rhomboid muscles; in the lumbar area, only the relatively
avascular lumbodorsal fascia attaches to the tips of the lumbar and
lower thoracic processes (Fig. 6-108). If the
patient has scoliosis with extensive vertebral body rotation, the
paraspinal muscles on the convex side of the curve may bunch up and
roll over the tips of the spinous processes, causing further bleeding
if the muscles are cut inadvertently during dissection.
portion and a deep portion. The superficial portion is made up of the
sacrospinalis muscle (the erector spinae), which runs longitudinally.
In the lumbar area, the muscle is a single mass; in the thoracic
region, it divides into three units, namely, from medial to lateral,
the spinalis, the longissimus, and the iliocostalis (see Figs. 6-108 and 6-111).
layers: superficial, intermediate, and deep groups. The superficial
group consists of the semispinalis muscles, which span about five
segments from origin to insertion. The intermediate group, the
multifidus muscles, spans about three segments. The deep group, the
rotator muscles, spans adjacent segments (Figs. 6-109 and 6-110; see Fig. 6-108).
The rotator muscles pass in a lateral to medial direction, with the
distal end of the muscle being more lateral. The resulting angle
between the muscle and its insertion makes stripping the muscles in a
caudad to cephalad direction in the thoracic region easier (see Figs. 6-105 and 6-108, 6-109 and 6-110).
In addition, because the spinous processes are angled more caudally in
the thoracic area than in the lumbar area (where they stand erect,
almost directly over the vertebral bodies), it is easier to dissect the
paraspinal muscles free from the thoracic spinous processes in a distal
to proximal direction. Finally, the short rotators take origin from the
caudal end of the spinous processes and are detached easily and
dissected out laterally onto the transverse processes (see Figs. 6-105 and 6-110).
of musculature in a distal to proximal direction. The transverse
processes become larger from T12 to T1.
of back muscles, the muscles of respiration; these are placed more
laterally.
lumbar nerves may be injured during dissection of the muscles,
particularly laterally between the transverse processes where the rami
are located. Although the loss of one or two posterior primary rami may
denervate the paraspinal muscles partially, the significant overlap of
the segmental nerve supply to these muscles prevents total denervation.
Excessive lateral retraction and cauterization at each level, however,
can cause muscle denervation.
lumbar and thoracic areas; they are located between the transverse
processes, close to the posterior primary rami. The vessels constitute
the main blood supply to the paraspinal muscles. Cauterizing
them
does not appear to cause significant loss of blood supply to the
muscles. If they are cut, they must be cauterized or tied off; they
branch directly from the aorta and may cause postoperative bleeding
under pressure (Fig. 6-111; see Figs. 6-105 and 6-106B).
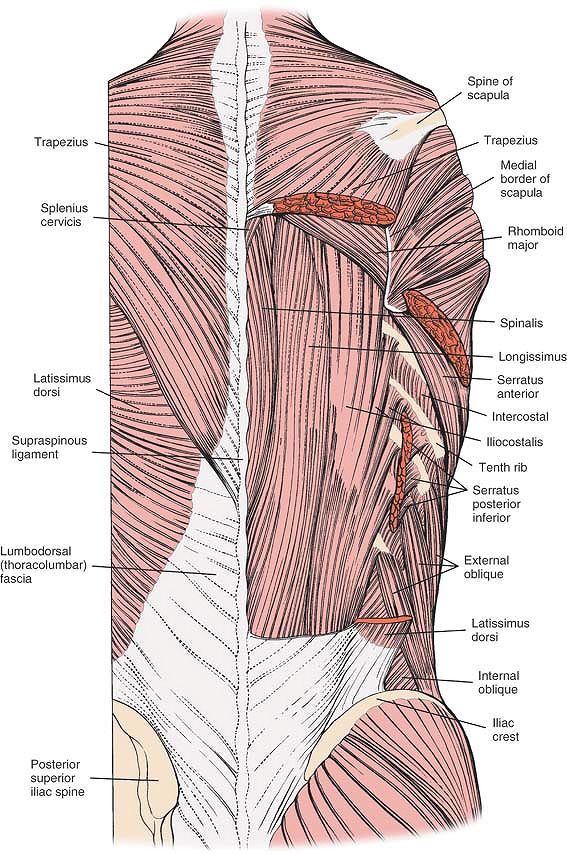 |
|
Figure 6-108
The musculature of the back. The most superficial layer is seen, including the trapezius, the latissimus dorsi, and the lumbodorsal fascia (left). The trapezius and latissimus dorsi have been resected to reveal the deep layer, the sacrospinalis muscles, including the spinalis, longissimus, and iliocostalis muscles (right). A portion of the rhomboid major muscle of the superficial layer is seen inserting into the medial border of the scapula. Trapezius. Origin.
From all spinous processes of the cervical spine except C1; from all spinous processes of thoracic vertebrae (T1-T12); and from superior nuchal line. Attachment to cervical spine is indirect, via ligamentum nucha. Insertion. Upper fibers from upper third of muscle, passing laterally and inferiorly to flattened posterior border of lateral third of clavicle and its upper surface. Intermediate muscle fibers pass laterally in a horizontal direction to adjacent part of upper surface of acromion and to associated upper lip of crest of spine of scapula. Lower fibers ascend, passing superiorly and laterally, inserting into tubercle on lower lip of spine of scapula. Action. Stabilizing muscle of shoulder girdle. Nerve supply. Spinal accessory nerve; cranial nerve XI. |
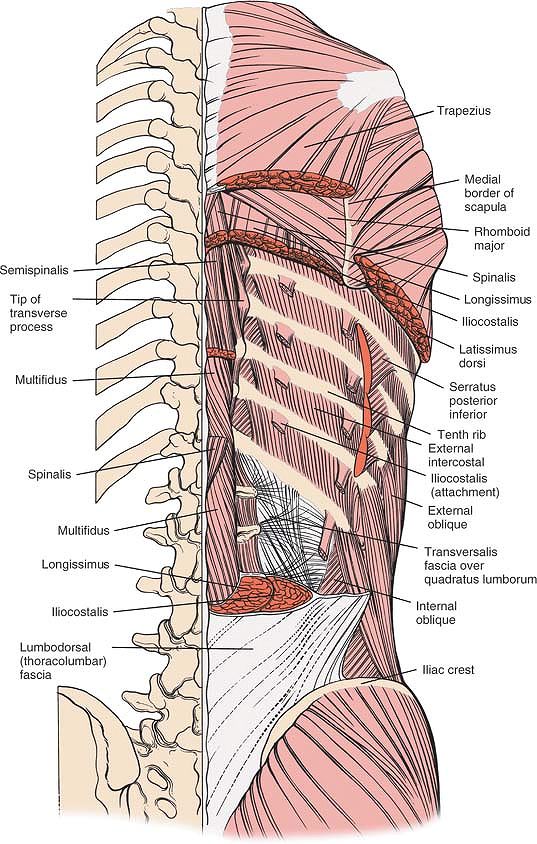 |
|
Figure 6-109
The sacrospinalis system has been resected to reveal the deep portion of the deep layer, which consists of the semispinalis and multifidi. Note the intertransversarii muscles and the insertion of the iliocostalis muscles into the borders of the ribs. |
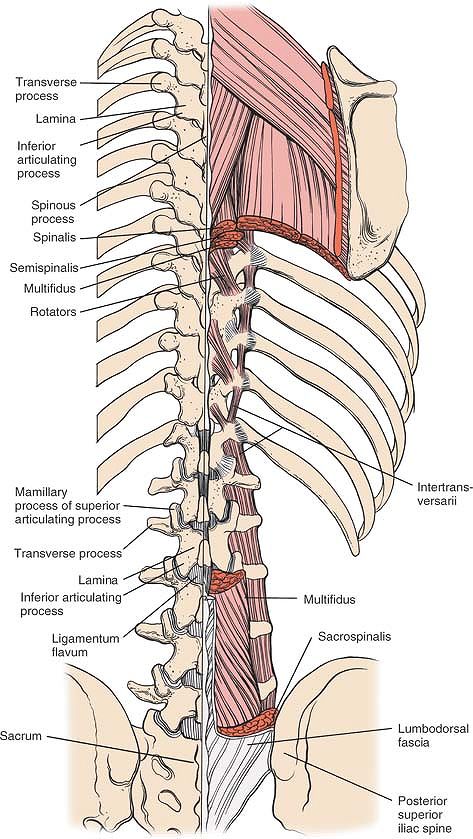 |
|
Figure 6-110
The muscles are resected further to reveal the deep muscles of the deep layer (i.e., the short rotators as well as the intertransversarii muscles and the interspinous muscles) and the facet joint capsules. |
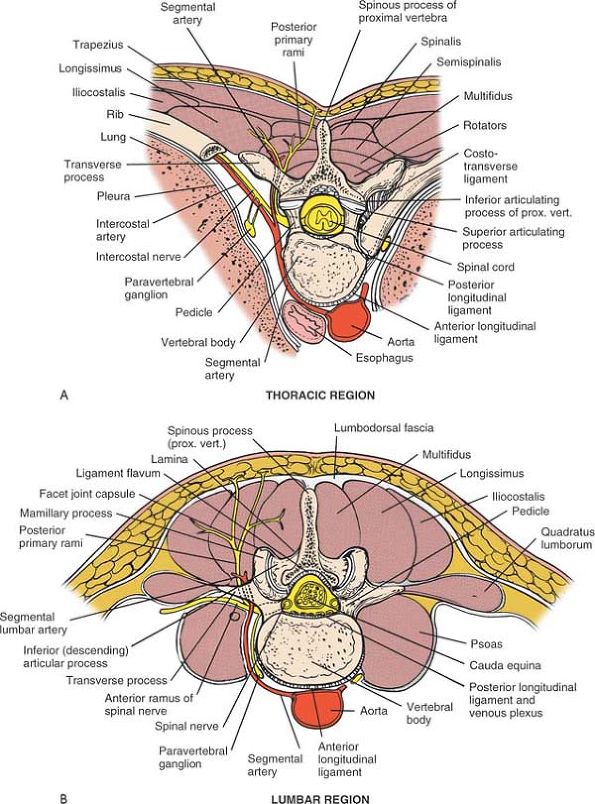 |
|
Figure 6-111 (A)
Cross-section through the level of a thoracic vertebra. Superficial and deep layers of the thoracic spine are visualized, as well as their nerve and blood supply. (B) Cross-section through the level of a lumbar vertebra. Note that the individual muscles of the sacrospinalis musculature are one paravertebral mass at this level. Note that the medial end of the cup-shaped ascending articulating process is closest to the lumbar nerve root. |
larger than their thoracic counterparts and protrude further
posteriorly. Their size is mainly the result of their large
articulating processes and large mamillary
processes
that sit on the posterior aspect of the ascending processes, extending
the bone even further posteriorly. The lumbar facet joints lie in the
sagittal plane (see Fig. 6-111B).
The joint capsules themselves are shiny, usually quite white, and are
continuous with the ligamentum flavum, which is yellow-white. In the
thoracic region, the joints are smaller, do not protrude as far
posteriorly, are flatter, and are placed in the frontal plane (see Fig. 6-111A). The facet joints are vulnerable during removal of the joint capsules.
edge of the inferior vertebra and extends upward to a ridge under the
lamina of the next vertebra, covers the blue-white dura and its layer
of epidural fat. The dura must be protected; any epidural tear must be
closed off (see Figs. 6-11 and 6-12).
to the lumbar nerve root. Arthritis of the medial end of the ascending
facet can cause compression of the nerve in the foramen. The nerve root
is safe during the foraminotomy if the anatomic arrangement of the
facet joints to the nerve root is appreciated. The nerve root should be
protected while the medial portion of the ascending process, the
portion that is close to the nerve root, is being removed (see Fig. 6-111B).
the ribs on the posterolateral aspect of the rib cage may have to be
resected to flatten out a hump caused by ribs that still protrude.
bolsters longitudinally on either side of the patient from the anterior
superior iliac spine to the shoulders to allow room for chest expansion
(see Fig. 6-101).
latissimus dorsi muscles. The trapezius is innervated by the spinal
accessory nerve and the latissimus dorsi is innervated by the long
thoracic (thoracodorsal) nerve. The deeper muscle, the iliocostalis
portion of the sacrospinalis, is innervated segmentally and, therefore,
is not denervated when it is split longitudinally.
subcutaneous tissue. Free them from the underlying fascia and retract
them laterally. Center the dissection over the most prominent, or
apical, rib. Extend it laterally to at least 12 cm from the midline,
and then proximally and distally to expose all the deformed ribs (Fig. 6-112).
downward toward the midline as far as the spinous process of T12.
Identify this muscle by its rolled, lateral free border. Dissect along
the lateral border and retract the muscle medially. The medial portion
of the fibers of the latissimus dorsi muscle and its aponeurosis run
almost perpendicular to and under the trapezius muscle; it takes origin
from the lower six thoracic spinous processes, as well as from the
lumbodorsal fascia. Dissect the muscle free with cautery and retract it
laterally (see Fig. 6-112).
muscles lies the iliocostalis, a longitudinal muscle with flattened
tendons in its musculature that insert into the lower borders of the
ribs. Split the iliocostalis muscle longitudinally over each of the
deformed portions of the ribs that are being removed, then dissect and
retract it medially and laterally in line with the ribs (Fig. 6-113).
dissector to push the split periosteum to the upper and lower borders
of the rib. With the special end of the dissector, strip the
intercostal muscles off the upper end of the rib in a medial to lateral
direction in the angle formed by the intersection of the external
intercostal muscles and the rib. Then, strip the intercostal muscles
from the lower end of the rib in a lateral to medial direction,
remaining in the angle formed by the origin of the external intercostal
muscle and the rib to discourage bleeding. By keeping the dissection in
a subperiosteal location, the neurovascular bundle, which will have
been freed from the lower border of the rib with the intercostal
muscles, will be avoided (Fig. 6-114).
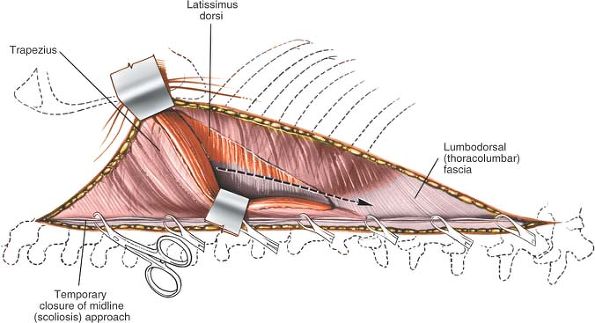 |
|
Figure 6-112
Retract the rolled lateral border of the trapezius muscle medially to expose the thin, aponeurotic medial portion of the latissimus dorsi. Incise the aponeurotic medial portion of the latissimus dorsi perpendicular to its fibers. |
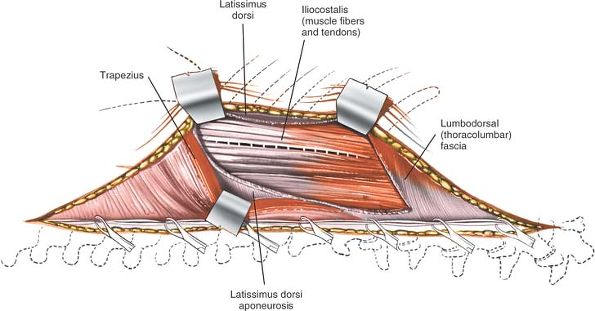 |
|
Figure 6-113
Retract the latissimus dorsi laterally and the trapezius medially to expose the underlying iliocostalis muscle. Incise the muscle longitudinally, parallel to its fibers. |
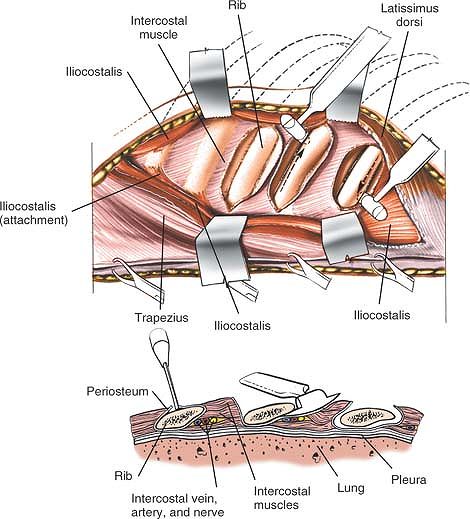 |
|
Figure 6-114
Dissect and retract the iliocostalis muscles laterally and medially from their insertion to expose the posterior aspect of the ribs. Incise the periosteum over the rib. Push the split periosteum to the upper and lower borders of the rib. With a special dissector, strip the intercostal muscles off the borders of the rib as well as anteriorly. |
patient’s breathing so that the visceral pleura can fall away from the
rib, minimizing the danger to the pleura during anterior dissection.
When the ribs have been uncovered completely, begin to resect them.
lies along the lower edge of the rib in the neurovascular groove.
Unless the dissection is kept in a subperiosteal location, it may be
cut inadvertently during the resection and the intercostal vessels will
have to be cauterized, causing possible segmental chest wall numbness
(see Fig. 6-114, inset).
1f that happens, plan to insert a chest tube immediately after the
wound is closed, while the patient is still in the operating room.
with blood flowing from the area of the spinal fusion into the lung. If
the two areas of dissection are connected, be prepared to insert a
chest tube to drain the blood.
portion of the rhomboid major muscle may have to be dissected to expose
the rib area more fully. Distally, the muscular belly of the
iliocostalis muscle may have to be split as it splits from the
sacrospinalis muscle.
lateral to its maximum deformity to the most medial end, without
removing its head and neck. The lateral portion of the resected rib
will drop forward, reducing the rib hump, but the medial portion, held
rigidly in place by the costotransverse and costovertebral ligaments,
will not move. That is why the rib should be resected as medially as
possible. Otherwise, the medial end of the rib will continue to stick
out posteriorly, causing continued deformity.
sympathetic effusion of a lung field. If this occurs, insert a chest
tube to drain the fluid.
continued oozing of blood. The wax does not prevent the ribs from
regenerating.
matchstick-sized pieces and used as graft material in a midline spine
fusion.
resecting the ribs will not produce a significant reduction in the rib
hump deformity.
WD: Neural Pathways and Central Sites Involved in Penile Erection:
Neuroanatomy and Clinical Implications, Neuroscience and Behavioral
Reviews (2000) p. 507–516.
R: Cervical, Thoracic and Lumbar Complications Anterior Approach,
Complications of Spine Surgery, Chapter 13, 1989, p. 246.
SA: Mini-open approach to the spine for anterior lumbar interbody
fusion: description of the procedure, results and complications. Spine
J 2:216, 2002
Groat WC: Anatomy and Physiology of the Lower Urinary Tract, Spinal
Cord Injury, Urologic Clinics of North America, Vol 20, no 3, Aug 1993
RA, Smith GW: Anterolateral cervical disc removal and interbody fusion
for cervical disc syndrome. Bull Johns Hopkins Hosp 96:223, 1955
AR, Stock FE, Fang HSY et al: Anterior spinal fusion: the operative
approach and pathological findings in 412 patients with Pott’s disease
of the spine. Br J Surg 48:172, 1980
PR: Treatment of scoliosis: correction and internal fixation by spine
instrumentation. J Bone Joint Surg [Am] 44:591, 1962
