Intertrochanteric Fractures
region extending from the extracapsular basilar neck region to the
region along the lesser trochanter before the development of the
medullary canal. Intertrochanteric and peritrochanteric are generic
terms for pertrochanteric fractures. Injury creates a spectrum of
fractures in this proximal metaphyseal region of bone, with damage to
the mechanically optimized placement of intersecting cancellous
compression and tensile lamellae networks and the weak cortical bone
with resulting displacement from the respective attachment of muscle
groups to the fracture fragments and an adjacent high mobility joint.
These structures are subject to multiplanar stresses after surgical
repair. This region of the femur shares many common biomechanical
properties with other short end-segment metaphyseal-diaphyseal
fractures with regard to the difficulty in obtaining stable fixation.
Although predominantly associated with low-energy older age patients,
high-energy trauma in young patients can result in similar patterns of
fracture.
interest globally. They are the most frequently operated fracture type,
have the highest postoperative fatality rate of surgically treated
fractures, and have become a serious health resource issue because of
the high cost of care required after injury. The reason for the high
cost of care is primarily related to the poor recovery of functional
independence after conventional fracture care in many patients.
Interestingly there has been no significant improvement in mortality or
functional recovery over the past 50 years of surgical treatment.
Paradoxically the last 50 years of acquiescence to the status quo of
hip fracture treatment are
related
to false assumptions that have been a hindrance to improvement in the
management of the hip fracture patient: (i) uncontrolled shortening and
varus collapse are acceptable in hip fractures but not other fractures;
(ii) reduction does not matter with sliding screw systems, as the
fracture will “collapse to stability” because rotation is not a problem
and placement of the head fixation takes precedence over fracture
reduction; (iii) union without implant failure overrides the
requirement of a stable anatomic reduction to the detriment of optimal
functional recovery; and (iv) the orthopaedic surgeon just fixes the
fracture, as opposed to treating the total musculoskeletal needs of the
patient. The reasons for these assumptions relate directly to the
historical evolution of hip fracture treatment and the arguments that
shaped our current understanding. A new paradigm regarding hip fracture
care and treatment is currently evolving, which hopefully will advance
our treatment goal back to optimal functional recovery and prevention
of future hip fractures.
incidence of hip fracture worldwide would double to 2.6 million by
2025, and 4.5 million by 2050.79 The
percentage increase will be greater in men (310%) than women (240%). In
1990 26% of all hip fractures occurred in Asia, whereas this figure
could rise to 37% in 2025 and 45% in 2050.143 Hagino et al. reported a lifetime risk of hip fracture for individuals at 50 years of age of 5.6% for men and 20.0% for women.82 Since 1986 in the Tottori Prefecture, Japan, the acceleration of hip fracture incidence continues for both genders.
decline in certain areas of the world, but the reason is unknown. In
Denmark the incidence of hip fractures has declined about 20% from 1997
to 2006; Nonetheless, this decline cannot be explained by
antiosteoporotic medications, whose effect should only be an
approximate reduction of 1.3% in men and 3.7% in women.2
Epidemiologic studies among Olmsted County, Minnesota, residents in
1980 to 2006 revealed that the incidence of a first-ever hip fracture
declined by 1.37%/year for women and 0.06%/year for men. The cumulative
incidence of a second hip fracture after 10 years was 11% in women and
6% in men.
fixation in the late twentieth century was to minimize implant failure
and avoidance of cutout of the femoral head and neck fixation
components. Because many of these fractures are associated with
osteoporosis, the current paradigm shift regarding hip fracture care
relates to three main strategies: (i) Prevention by aggressive
screening and treatment of patients with high risk for fragility
fracture; (ii) standardization of hip fracture centers with aggressive
early intervention and protocols to avoid complications; and (iii)
optimization of fracture reduction and new designs of implant component
fixation in osteoporotic bone with conceptual design changes in
fixation stability and augmentation of the bone-implant interface.
approximately 90% of community hip fractures in patients more than 50
years of age, with a higher proportion of women. Higherenergy hip
fractures are relatively rare; they are more common in men less than 40
years of age and are usually referred to regional trauma centers for
treatment.100 Cummings et al.43
noted that neither age-related osteoporosis, nor the increasing
incidence of falls with age sufficiently explains the exponential
increase in the incidence of hip fracture with aging.43 Their hypothesis was that four conditions correlated for a fall to cause a hip fracture:
(b) protective responses must fail; (c) local soft tissues must absorb
less energy than necessary to prevent fracture; and (d) the residual
energy of the fall applied to the proximal femur must exceed its
strength.
hip fractures. Fall with a rotational component is more common with
extracapsular hip fractures.98
associated injuries are most commonly distal radius and proximal
humerus fractures and minor head injuries that occur during the fall.
High-energy hip fractures are more commonly associated with ipsilateral
extremity trauma, head injury, and pelvic fractures. Associated
injuries or premorbid diseases may coexist with the fracture diagnosis.
Syncopal episodes resulting in a fall may bring attention to
cardiovasular and neurologic disease states. Primary neoplastic and
metastatic disease may reveal their presence with preceding hip
discomfort and subsequent fall resulting in fracture.
and inability to ambulate after a fall or other injury. The pain is
localized to the proximal thigh and is exacerbated by passive or active
attempts of hip flexion or rotation. Drug use, either illicit or
precribed pharmacologics, must be sought out as a confounding and
contributing factor. Nursing home and institutionalized patients must
be examined for the potential of neglect and abuse in the form of
previous fractures, and injuries in different states of repair and
decubiti.
shortening of the extremity and deformity of rotation in the resting
position compared with the contralateral extremity. Pain with motion or
crepitance testing is not elicited unless there are no physical signs
of deformity and radiographic studies are negative for an obvious
fracture. Pain with axial load on the hip has a high correlation with
occult fracture. The auscultation Lippmann Test is quite sensitive for
the detection of occult fractures of the proximal femur or pelvis.132
By placement of a stethescope bell on the symphysis pubis and tapping
on the patella of both extremities, variations in sound conduction
through the pelvis and hip from the patella result when there is any
discontinuity. A decreased tone or pitch implies fracture within this
arc of bone.
for surgery should include the following for all low-energy fractures
(osteopenic or fragility fractures): serum calcium, phosphate, and
alkaline phosphatase; a complete blood-cell count (CBC); 25
hydroxyvitamin D, thyroid-stimulating hormone (TSH); parathyroid
hormone (PTH intact); serum protein electrophoresis
(SPEP); and kidney-function tests, including blood urea nitrogen (BUN), creatinine, and glomerular filtration rate (GFR).45,206
complication includes: previous DVT/PE, anticoagulation medications,
immune deficiency disorders, malabsorption disease, angina or CVA
prodromal symptoms of atherosclerotic disease, and active infection
(pulmonary, genitourinary), which might result in sepsis
postoperatively. Protein-calorie malnutrition and vitamin D deficiency
are now recognized as serious risk factors for mortality and recovery.
Foster reports 70% mortality for patients with albumin less than 3
compared with a mortality rate of 18% in patents with albumin ≥3.61
Vitamin D deficiency is now viewed as an epidemic because of dietary
changes and lack of sunlight exposure; current recommendations are to
administer 50,000 IU of vitamin D immediately to all elderly patients
on admission with hip fracture.206
table lateral of the affected hip are usually recommended for diagnosis
and preoperative planning. Traction films are helpful is comminuted and
high-energy fractures in determining implant selection.117
Subtrochanteric extension requires full-length femoral AP and lateral
radiographs for implant length selection. If a long nail implant is a
consideration, then AP and lateral radiographs of the affected femur to
the knee are required, with special attention to femoral bow and
medullary canal diameter. Traction views with internal rotation may be
of benefit preoperatively as an aide in the selection of definitive
internal fixation.117
(MRI) scans are rarely required for displaced fractures but may be
useful in establishing the diagnosis in nonobvious fractures and
atypical fractures in high-energy trauma patients.181,209
The MRI does not necessarily require a full study, as the frontal
images are most often diagnostic. Nonetheless, complete studies usually
detect other diagnosis for hip pain in addition to occult fractures of
the proximal femur. MRI is preferred over the CT or the older
radionuclide scans because of a higher sensitivity and specificity for
a more rapid decision process.*
hip fractures occurs in the operative suite with fluroscopic C-arm
views. This technology gives the surgeon an excellent modality for
fracture analysis in complex fractures and immediate feedback as to the
stability of the fracture after the initial reduction. In many
institutions this has led to elimination of preoperative lateral
radiographs. Unfortunately this practice may also result in a change in
the selected type of fixation with inherent stress on the operative
team and resource management.
occurring from the basicervical to the level of the subtrochanteric
regions have not been particularly helpful in clinical situations.
Nonetheless, increased sugical complexity and recovery are associated
with unstable fracture patterns. Unstable characteristics include
posteromedial large separate fragmentation, basicervical patterns,
reverse obliquity patterns, displaced greater trochanteric (lateral
wall fractures), and failure to reduce the fracture before internal
fixation. Stability after surgical treatment connotes anticipated union
without deformity or implant failure. The current controversy of
implant selection is largely focused on what amount of deformity and
fracture site motion is still compatible with a functional recovery to
the patient’s preinjury status.
achieved reliable reproducible validity. In 1822 Astley Cooper (London)
described the first (pre-radiographic) classification of hip fractures:
intracapsular and extracapsular fractures (with the main complication
of nonunion and avascular necrosis in the first and the second of coxa
vara).
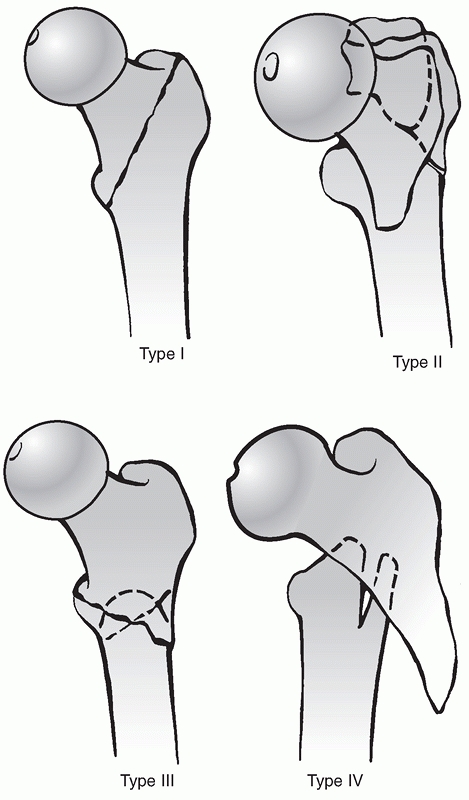
recommendation classification, predictive of the difficulty of
achieving, securing, and maintaining the reduction in four fracture
types: (i) Stable (two part); (ii) unstable with posteromedial
comminution; (iii) subtrochanteric extension into lateral shaft
extension of the fracture distally at or just below the lesser
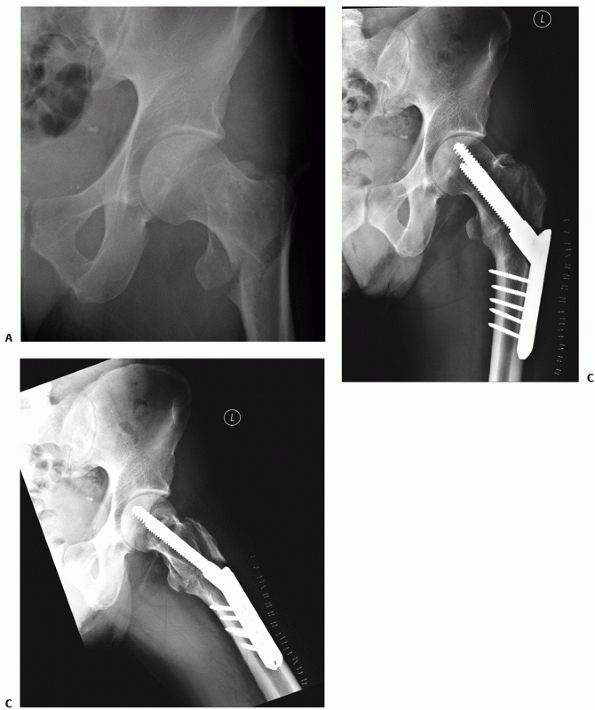
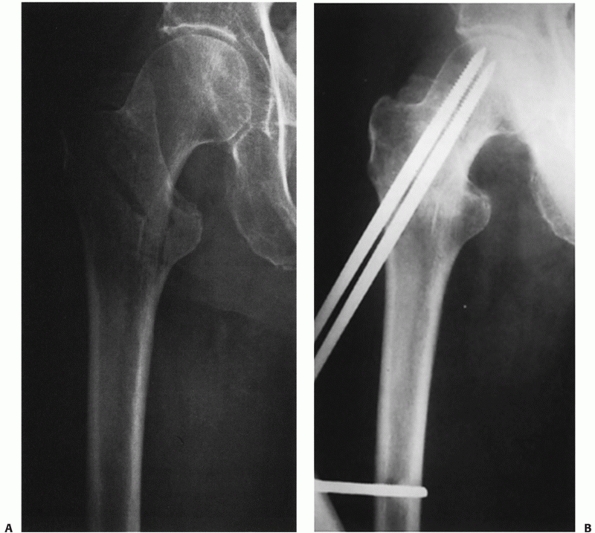
trochanter (the term reverse obliquity was coined by Wright);220 and (iv) subtrochanteric with intertrochanteric extension with the fracture lying in at least two planes (Figure 48-1).
They were the first to report the use of lateral buttress plating of
the greater trochanter to avoid medialization of the shaft in type 3
fractures, the need for two-plane fixation for type 4 subtrochanteric
fractures with a coronal fracture line, and the possibility
ofiatrogenic conversion of type 1 and 2 fractures to type 3 during
implant preparation and insertion.
 |
|
FIGURE 48-1
Boyd and Griffin classification: (i) stable (two-part), (ii) unstable comminuted, (iii) unstable reverse obliquity, (iv) intertrochanteric-subtrochanteric with two planes of fracture. |
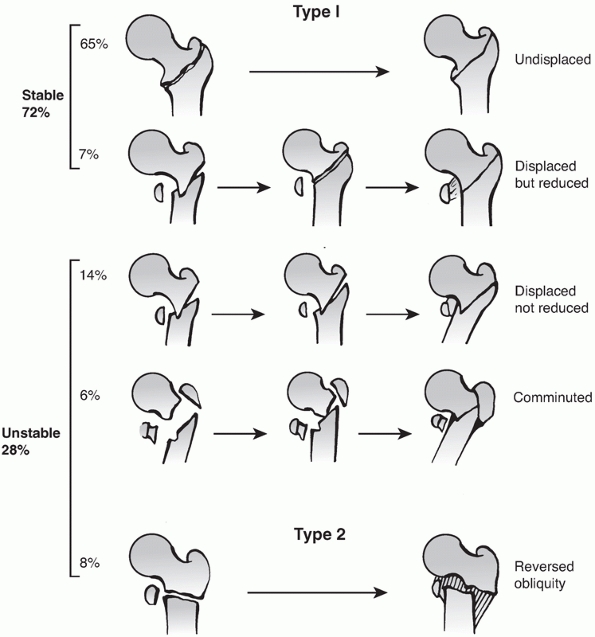
a post-treatment classification with five types described. He compared
nonoperative treatment and fixed angle device surgical treatment. He
documented that 72% of his fractures could be fixed in a stable
configuration. Stability was not achieved in 28% of the fractures; 14%
as a result of the fracture pattern or comminution and 14% of which he
felt the reduction was never achieved (Figure 48-2).
This paper was primarily used to argue the value of internal fixation
over nonoperative treatment of hip fractures, which was controversial
in England in the 1940s and 1950s.
et al. reported independently on a revision of the Evans classification
incorporating the lateral radiographic position of the posteromedial
fracture component and its relation to stability with sliding fixation
systems.104,122
Kyle et al. showed an increased rate of deformity and collapse with
increasing instability classification. Jensen et al. related the
ability to reduce the fracture and secondary displacement risk with a
CHS-type device in their classification system.
 |
|
FIGURE 48-2
Evans classification of trochanteric fractures. Type 1: Stable because either undisplaced or displaced but anatomically reduced to stability (intact medial cortex). Type 2: Unstable implies displaced and fixed in an unreduced position, comminuted with destruction of the anteromedial cortex, or reversed obliquity. |
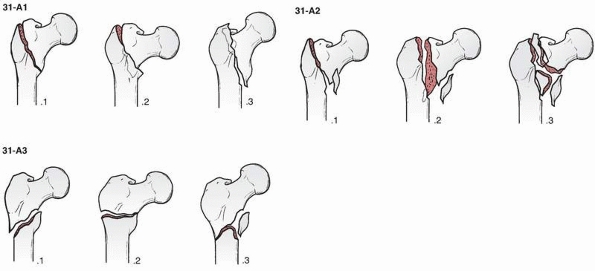
recent scientific articles and is a derivative of the Muller
classification (Figure 48-3). There is a higher
interobserver agreement with the AO/OTA classification than
Evans/Jensen, but neither meets the acceptable threshold for
reliability.64 The AO/OTA has nine
main types; however, correlation is best with only three categories;
also there is no lateral radiographic parameter with the AO/OTA
classification.156,175,188
Generally 31A1 fractures are thought of as the most stable, 32A2
fractures are more unstable, and 31A3 fractures are the most unstable
with plate device
fixation.
Unfortunatedly, the fifth digit of the classification has not been
found to be reliably identifiable in prospective evaluation.
 |
|
FIGURE 48-3
In the OTA alphanumeric fracture classification, intertrochanteric hip fractures comprise type 31A. These fractures are divided into three groups, and each group is further divided into subgroups based on obliquity of the fracture line and degree of comminution. Group 1 fractures are simple (two-part) fractures, with the typical oblique fracture line extending from the greater trochanter to the medial cortex. The lateral cortex of the greater trochanter remains intact. Group 2 fractures are comminuted with a posteromedial fragment. The lateral cortex of the greater trochanter, however, remains intact. Fractures in this group are generally unstable, depending on the size of the medial fragment. Group 3 fractures are those in which the fracture line extends across both the medial and lateral cortices. This group includes the reverse obliquity pattern. |
recent therapeutic-based classification, again derived from a
modification of the Evans and Jensen classification,120
primarily focusing on the stability of the lateral wall as a buttress
to minimize medialization and uncontrolled collapse after single screw
device fixation. Kyle has recently added another very unstable pattern
to his previous classification. In this variant, the fracture line
includes a separate femoral neck fracture; he concluded that this
variant should not be treated with a sliding hip screw device.121
combination of cortical and cancellous bone structure. The
well-vascularized pertrochanteric region is dependent on the structural
integrity of a laminated cancellous bone arcade from the femoral head
and epiphyseal scar, around Ward’s triangle to the lesser trochanter,
where the solid nature of the structure changes to a tubular construct
with the origin of the femoral medullary canal; the strong plate of
bone posteriorly is named the calcar femorale (Figure 48-4).65
This is the region most affected with the posteromedial fracture
comminution leaving only the anteromedial cortex potentially stable.
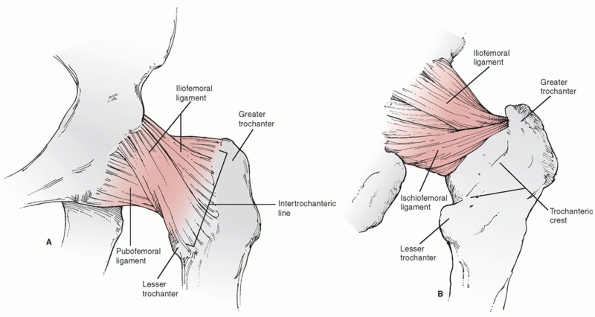
include the hip capsule and the musculotendinous junctions of the
gluteus medius and minimus (greater trochanter), iliopsoas (lesser
trochanter), pirifomis and short external rotators (posterior
trochanteric region from the greater trochanteric region to the lesser
trochanter), the oblique head of the rectus femoris (anterior capsule),
and the vastus lateralis (lateral femur distal to the greater
trochanter). The hip capsule is especially important in reduction of
pertrochanteric fractures and its continuity with the distal fragment
is the soft tissue attachment on which a stable reduction is possible (Figure 48-5).
fracture fragments is dependent on the musculotendinous attachment to
the respective fragments. The greater trochanter is abducted and
externally rotated by the gluteus medius and short exteral rotators,
the shaft is displaced posteriorly and medially by the adductors and
hamstrings. This accounts for the usual shortening and coxa vara
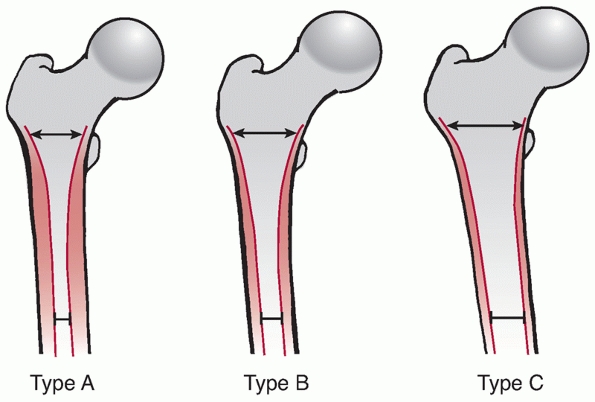
deformity of displaced fractures. With aging the morphology of the hip
changes with thinning of the cortex and expansion of the diameter of
the bone (Figure 48-4C). The younger hip
fracture patients has a relatively narrow metaphysis and a high narrow
isthmus with a very thick cortex in the diaphysis. Further aging
results in a slight widening and thinning of a cortex of the
metaphysis, with bone loss and a decreased thickness of the diaphyseal
cortical bone stock and a widening of the isthmus. In the advanced age
group, there is a very wide vacuous metaphysis proximally with loss of
tension and compression trabeculae, a loss of the constriction of the
isthmus, and a very round expanded tubular-shaped femur with a thin
cortex Three types of morphologic anatomy were grouped together by Dorr
et al. in 1983 referencing the selection of cemented versus
non-cemented arthroplasty femoral components48 (Figure 48-6).
The same rationale applies to implant selection for hip fracture
patients. Type A femurs occur primarily in young patients and have a
narrow metaphysis, thick cortex, and high constricting isthmus.
Excessive bone removal is required for intramedullary devices, and
either a plate-type construct or smaller-diameter reconstruction nail
may be more bone conserving. Type B fracture morphology has a wider
metaphysis and larger medullary canal, but relatively good cortex and
isthmus constriction. Type C is the most problematic in geriatric
populations with hip fractures: a wide metaphysis, wide medullary
canal, and loss of isthmus constriction in association with loss of
cortical diaphyseal bone stock. There
is
a trend to prefer long intramedullary implants in these patients;
however, care must be taken that the straightened thin diaphyseal
cortex may be at risk of perforation distally by long devices in the
anterior supracondylar area.157
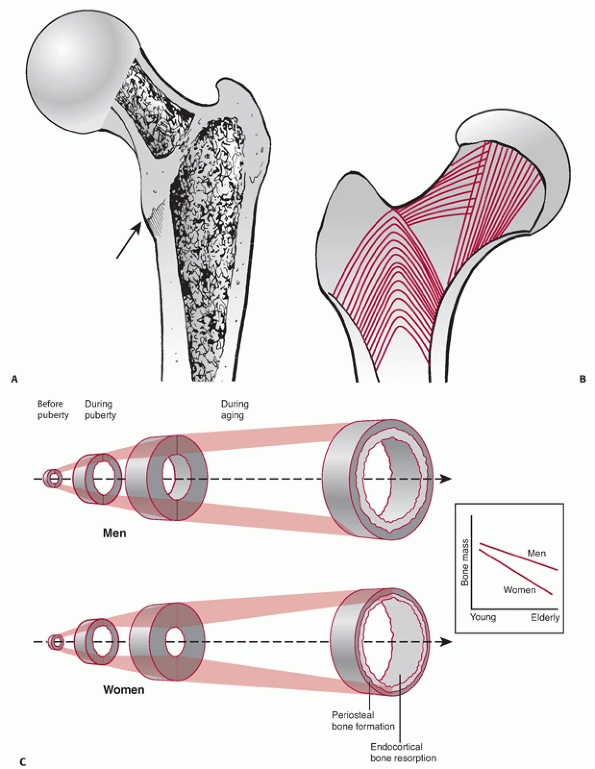 |
|
FIGURE 48-4 A. Posteromedial calcar shelf, which is usually damaged with unstable fracture patterns. B.
Ward crosssection of proximal femur. Best quality bone is within 10 to 30 mm of subarticular surface. Note tensile trabeculae between Ward’s triangle and greater trochanter. C. Changes in morphology of bone with age: adaptation to maintain whole bone strength. Note expansion of geometry and thinning of cortical bone with aging. (C adapted from Seeman E. Pathogenesis of bone fragility in women and men. Lancet 2002;359: 1841-1850, and Seeman E. Periosteal bone formation—a neglected determinant of bone strength. N Engl J Med 2003;349:320-323.) |
 |
|
FIGURE 48-5 A. Anterior hip capsule. Y-Ligament of Bigalow as structure for ligamentotaxis in closed reduction of stable Fractures. B. Posterior hip capsule. Note more-proximal position of capsule posteriorly and course of arteries to head.
|
nerve anteriorly and sciatic nerve posteriorly; however, they are
rarely encountered in surgical approaches for repair of pertrochanteric
fractures and are injured only rarely by penetrating trauma, usually by
displaced fracture fragments.49,112,140,152,179,212 Vascular injury affecting the femoral head is rarely involved in nonpenetrating injuries.192
Brodetti noted the rare possibility of injury to the vascularity of the
femoral head with femoral head fixation screws and nails with injection
studies, and found that the central and inferior locations were safe
zones.28 Avascular necrosis after
pertrochanteric fracture is extremely rare because of the relative
protected area of the medial circumflex artery with pertrochanteric
fractures, but may develop in 0.5% to 1% of pertrochanteric fractures
usually within 4 years of injury.13,69
 |
|
FIGURE 48-6
Dorr classification of morphology of femur. Type A corresponds to a small metaphysis, thick cortex, and high narrowed isthmus. Type B corresponds to a wider metaphysis, thinner cortex, and a tapering but wider isthmus. Type C corresponds to a wide metaphysis, thin cortex, and a straight or varus curvature in the diaphysis with loss of isthmus constriction. |
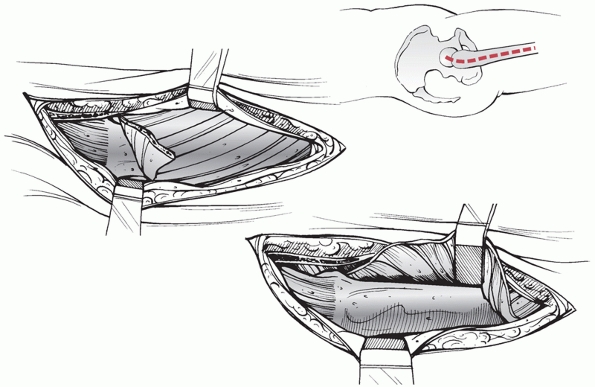
past 70 years for plate fixation. The patient is commonly operated on
with a fracture table and the leg and foot secured after closed
reduction. The entire proximal thigh from the iliac area to the distal
femur is prepared in the standard fashion. The incision length is based
on the length of the proposed plate-shaft component;
the
incision is started with reference from intraoperative C-arm
fluoroscopy views and is centered over the lesser trochanter. Commonly
the incision length is 5 to 10 cm in length. The iliotibial band is
incised and the proximal portion is extended sufficiently to develop
the area of the intertrochanteric line for palpation anteriorly. The
fascia of the vastus lateralis is incised near its attachment
posteriorly at the linea aspera. Leave sufficient fascia posteriorly (5
to 10 mm) for closure and to identify and obtain hemostasis of all
perforator arteriovenous structures. Reflect the vastus anteriorly,
exposing the lateral femoral shaft. There are no significant neurologic
or vascular structures at risk with this approach (Figure 48-7).
intersection of a line from the anterior superior iliac spine directed
posteriorly and a line parallel to the long axis of the femur. Overlay
a 3.2 guidewire on the skin anteriorly and laterally and confirm
alignment with the proximal femur with C-arm. Incise the skin proximal
to the greater trochanter. Usually a 3- to 5-cm incision is adequate.
The fascia is incised, but the gluteus medius fibers are not
dissected, as this approach is designed to minimize soft tissue damage
around the proximal femur. A targeting guide and trocar system protects
the gluteus medius. Separate incisions for the femoral head fixation
are made through the short version of the lateral approach to the femur
(Figure 48-8).
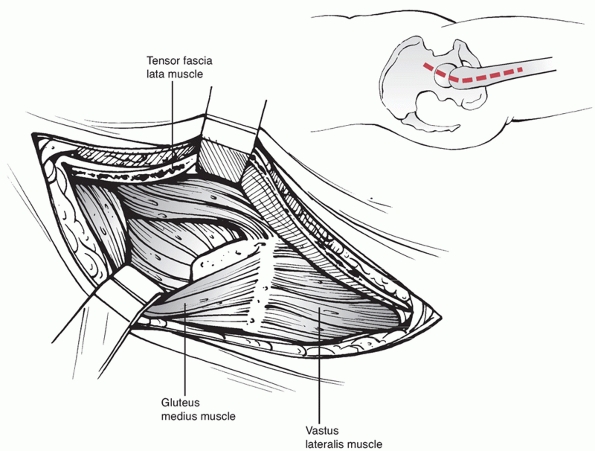
proximal expansion of the straight lateral approach previously
described. The muscular interval proximally is between the tensor
fasciae latae and the gluteus medius. The interval between these two
muscles is best begun distally and exposed proximally. Follow the
anterior border of the vastus lateralis proximally to reach the
anterior trochanteric ridge and hip capsule. The use of Schanz pins
drilled into the proximal femur is an aide in retraction for better
visualization and may be used for manipulation of the shaft. Further
capsulotomy and greater trochanteric osteotomy are rarely required for
pertrochanteric fracture management. The main vascular obstacle is the
ascending branch of the lateral femoral circumflex artery, which should
be isolated and ligated in the approach. Complete proximal dissection
of the gluteus medius and tensor fasciae latae interval to the iliac
crest is rarely necessary; the superior gluteal nerve to the tensor
fasciae latae is sacrificed with full proximal dissection; however,
this not clinically significant (Figure 48-9).
 |
|
FIGURE 48-7
Lateral surgical approach to the hip. Slight curvature of proximal extent of incision to allow palpation of the anterior cortex. Vastus lateralis reflection distally as needed for length of plate. |
treatment concepts regarding pertrochanteric fractures is critical to
advancing treatment modalities. Those who are ignorant of the past are
condemned to repeat its mistakes.
work of Pott and Cooper, who advocated supporting the thigh in a flexed
position. Early mobilization of the patient from bed rest to chair to
protective ambulation was the primary goal for survival of the patient.
They espoused “benign neglect of the
fracture” in an attempt to save life over limb.41 The other school was founded by Hugh Owen Thomas of Liverpool, who advocated immobilization and prolonged bed rest.20
 |
|
FIGURE 48-8
Intramedullary approach. Incision is placed center to slightly posterior to line of femoral shaft centered between the anterior superior and inferior iliac spines anteriorly. Incision length is 2 to 4 cm. |
type of fracture and advocated reduction and stabilization with
traction, abduction, and internal rotation, to better restore the
anatomy of the hip.217 This was
performed under general anesthesia; then the patient was placed in a
long leg hip spica cast to maintain the reduction. This basically moved
the treatment of hip fractures from a passive to an active role by the
surgeon.
 |
|
FIGURE 48-9 Watson-Jones approach. Key interval between TFL and G. Medius to visualize anterior femoral neck and capsule.
|
of the femur was a therapeutic derelict. The futility of conventional
treatment, demonstrated by Sir Astley Cooper, had been accepted as a
finality and permanent disability as an inevitable sequence of the
injury. Neglect of the fracture in the alleged interest of the patient
entailed no responsibility, either moral or legal. Positive treatment,
by contrast, could appeal only to adventurous spirits, because the
correction of deformity might
“break
up the sacrosanct impaction,” the only hope of union; whereas the
restraint of the plaster spica must endanger the life of the patient.
During the lapse of years, nonetheless, in spite of opposition and
inertia, the abduction treatment has come into general use, and
experience has disproved every assumption on which the negative
doctrine was based.
treatment with operative treatment, with the success of the
Smith-Petersen nail as the next progression to restore the limb and
decrease mortality.
fixation of the hip from a transtrochanteric insertion, but problems
with material compatibility and the rigors of surgery resulted in the
failure of these techniques.127 William Lane, Albin Lambotte, and Ernest Hey-Groves were the pioneers, who developed the modern principles of osteosynthesis.93,124,125,126
The advent of radiology prompted a re-evaluation of hip fracture
treatment, and in 1911 the Section of Surgery of the British Medical
Association reviewed a series of patients with the use of a new
technique of radiographic imaging and concluded that operative
treatment should be performed early when necessary and that function
seemed to be correlated with absence of radiographic deformity.93
The real modern era of internal fixation of hip fractures began with
the report of the technique by Smith-Petersen in 1925 and his invention
of the triflange nail for hip fractures.197
The triflange design controlled rotational instability and was strong
enough for patient mobilization. It was used for both trochanteric and
femoral neck fractures. Brittain using a very low placement on the
lateral cortex of the femur treated pertrochanteric fractures with the
Smith-Petersen nail, presaging the later high angle type devices.27,108
Sven Johansson in Sweden developed the technique simultaneously with
Westcott in the United States of a radiographic controlled insertion of
the Smith-Petersen Nail without arthrotomy 1932.68,215 This was termed blind nailing,
and began the movement toward minimally invasive surgery. Johansson
also is credited with developing the first cannulated Smith-Petersen
nail. In 1934 King and Henderson independently reported the use of
K-wires for provisional fixation, as described by Lambotte for guidance
and proper placement of the Smith-Petersen nail.90,115
It was not until the late 1930s and early 1940s that plate attachment
to the femoral head fixation truly lay the groundwork for the movement
from nonoperative to surgical treatment for pertrochanteric fractures.
Lawson Thornton is credited with the first attachable side plate bolted
to a Smith-Petersen nail205 in 1937.
Within 10 years there was an explosion of new devices. The Jewett Nail,
which was a triflange nail welded to a plate for shaft fixation.107
Jewett was the first to advocate the open reduction of the “lesser
trochanter” (posteromedial fragment) with separate screws to increase
the stability of the fracture. Blount in conjunction with Moore in the
1940s actually coined the terminology and concept of blade plates.22,144 Neufeld in California and Capener in the United Kingdom developed the fixed-angle type nail plate in 1944.33,203
Trochanteric buttress plates were first reported by Boyd and Griffin in
1949 (they were invented by Richardson at the Campbell Clinic) for
preventing medialization with the Neufeld plate in unstable fractures.26 Boyd reported on refinements of the buttress technique in 1961, including screw fixation into the trochanter.25
and 1940s was the belief that surgical fixation decreased mortality
from prolonged bed rest and eliminated the need for spica casts. Early
reports suggested that patients could be mobilized more rapidly and
with less hospitalization time. In 1949, Evans reported on the use of a
Neufeld nail type technique with open reduction compared with
nonoperative treatment for fractures and favored surgical repair on the
basis of four parameters that are still pertinent today: (i) Greater
pain relief and comfort of the patient; (ii) improved early patient
mobility; (iii) economy of bed control for nursing and hospital
efficiency; and (iv) lower mortality rate (18% compared with 33% for
nonoperative treatment).56
in the 1940s with the realization of the magnitude of the hip forces by
Inman and the effect of compression on healing by Eggers.51,103 Smith developed mechanical cadaver testing to reproduce fractures and determine the forces required for their causation.196
In a review of implant failures, Taylor and Neufeld proposed the need
for implants with sufficient fatigue life and the importance of stable
reductions.203 In 1956 Martz presented the first load to failure testing for common hip implants of the day.138
In analyzing stresses on the human femur, Martz pointed out that on
average walking subjects the femoral head to forces in the vicinity of
400 lb because of momentum and leverages. He applied the engineering
rule of thumb, calling for a safety factor of two, arriving at a force
of 800 lb (3200 Newtons) as adequate resistance to load of a proximal
fixation system. Foster advocated higher angle nail-plates to minimize
the load on the implants base on geometric assumptions on loading.60 Cleveland argued that even with optimized designs some small percentage of implant failure would still occur.40
He was the first to theorize that the rotation was unlikely for
pertrochanteric fractures to justify his design of a round nail plate
(fixed angle design) eliminating flanges on the femoral head component
for rotational control in distinction to previous derivative plates
from Smith-Petersen’s original concept. He believed it unlikely that
the proximal fragment of an intertrochanteric fracture could rotate
after the fracture was reduced, the nail inserted, and the plate fixed
to the shaft because of engagement of bone fragments at the fracture
site. He did not detect any evidence of rotation in the follow-up of
the 100 fractures included in the using his design and technique. He
also was the first to advocate full weight-bearing after surgery when
the implant’s fatigue resistance was adequate for unrestricted loading.
Interestingly, he used bolted shaft fixation screws through the plate.
system of drilling and insertion was invented by Godoy-Moreira and is
the precursor of this class of implants in 1938.73
As with other devices, it was originally designed for femoral neck
fractures with the focus of minimizing implant failure. The author also
believed that the compression generated by the screw and side bolt
would prevent any rotation or flexion at the fracture site.
Schummpelick et al. described an implant designed by E. Pohl in Kiel,
Germany (the same man who designed for G. Küntscher) of a sliding
cannulated system with a side-plate in 1952.190 Interestingly they did report telescoping of the implant
with collapse of the fracture, leading to a Trendelenburg gait in some
patients. They also reported on the concept of early weight-bearing
with the sliding hip screw.
the application of sliding with a nail plate device to minimize medial
penetration of the femoral head and early fatigue failure.139,178
Full weight-bearing was not advised for 4 to 6 months with these
devices. Interestingly Pugh attempted to classify the results on a
functional basis, but “because of the variations in age, as well as the
variation in the general physical status of these patients this was
deemed impractical. In the cases in which solid union occurred the
result was considered good or satisfactory.” The first commercially
available sliding compression hip screw in the United States was
introduced in 1956 in cooperation with K. Clawson of Seattle and
McKenzie of Scotland manufactured by Richards Manufacturing Company of
Memphis, Tennessee.38,39
Their modifications included a blunt-tipped cannulated screw design
coupled to a forged side plate of optional lengths and neck angles.
There was a keyed slot for enhanced rotational stability. The follow-up
series from Mullholland at Clawson’ institution (now Harborview Trauma
Center) in 1975 showed that functional status preoperatively correlated
with the postoperative recovery and mortality seemed to improve with
experience with the use of this device.151
patterns with proactive valgus oteotomies was popularized by Dimon and
Houston, Sarmiento, Harrington, and others in the 1960s to 1970s.47,87,187
Nonetheless, prospective studies and meta-analysis comparing the
results with sliding hip screws type designs showed no mortality or
functional improvement with osteotomies and a higher risk of blood loss.46,67,87,169
sliding devices was focused by Kyle et al. and Jensen et al., both of
whom reported independently on a revision of the Evans classification
incorporating the lateral radiographic position of the posteromedial
fracture component and its relation to stability with sliding fixation
systems.104,122
Kyle et al. showed an increased rate of deformity and collapse with
increasing instability classification. Nonetheless, they reported that
the use of a high-angle sliding nail technique with prophylactic
antibiotic, thromboembolism prophylaxis, and early mobilization was
acceptable for mortality and fixation failure. They did not advocate
the use of osteotomy. In their functional evaluation they considered
occasional pain, permanent limp, and use of a cane a good result.
Jensen et al. related the ability to reduce the fracture and secondary
displacement risk with a CHS type device in their classification
system. With anatomic reduction in both planes with a stable medial
cortex, no secondary displacement occurred. In nonanatomic and/or
unstable fractures they reported a 25% to 69% rate of secondary
displacement. In their statistical analysis, the correlation with
secondary displacement was not an unstable pattern but a lack of
reduction. Regarding the position of the tip of the device, Jensen et
al. advised placement over 10 mm from the articular surface and Kyle et al. within 10 mm to minimize cutout. The question that has persisted is how to address the secondary displacement problem.
failures led to a new approach to fixation. In the plate field, Medoff
introduced the biaxial compression hip screw for unstable fractures,
which actually allowed axial compression along the shaft reminiscent of
an Egger’s plate concept in addition to dynamic compression at the
screw plate interface in the head.142
This biaxial compression concept was proved effective to minimize
implant failure in unstable fractures, but with increased shortening of
the leg.135,213
The re-emergence of the importance of rotational instability as a
problem in 2000 prompted Gottfried to develop the PCCP plate system,
which consisted of a side plate with two constrained partially threaded
lag type screws reminiscent of a reconstruction nail-type pattern that
optimized the rotational stability of the hip and minimized damage to
the greater trochanter (lateral wall of the femur).75
Preliminary reports suggest that patients may have a trend toward
earlier functional recovery with this type of device, although further
studies are needed. Locked and hybrid locking plates have been applied
recently for unstable fractures with only preliminary reports thus far.
closed technique and fluoroscopic control with variable length femoral
geometry and enhanced proximal geometry to permit fixation with nails
or screws into the femoral head. They evolved from the Y-nail design of
G. Küntscher in 1940, described in the marrow nailing method in the
translation prepared by the U.S. naval forces, Germany technical
section in 1947, discovered in 2006.123
This was a nonlocking unreamed nail with an impaction-type nail
component for the femoral head driven through a perforation in the
centromedullary nail. The Zickel nail primarily developed for
subtrochanteric fractures was another impaction-type nail for the
femoral head, but with no distal locking capability. The TFN (Synthes,
Paoli, PA) is the most recent addition to this class of implant.
reconstruction nail were the start of two new classes of intramedullary
devices designed for the hip region; they coincided with the widespread
adoption and popularity of closed interlocking techniques in the 1980s
and 1990s. These devices made use of a compression screw inserted into
an intramedullary device instead of a nail for the femoral head
component. The gamma nail used an expanded head geometry of 17 to 18 mm
with a large single lag screw, and the reconstruction nail allowed a
smaller head geometry of 15 mm with two smaller lag screws for the head
component. Both devices have evolved over the past 20 years, with the
modern designs moving toward a 4- to 5-degree proximal bend with a
medial or tip trochanteric portal instead of a lateral trochanteric or
piriformis portal, respectively.
(Smith-Nephew, Memphis, TN) began clinical studies. It has a
trapezoidal cross-sectional geometry to protect the lateral wall of the
greater trochanter and a hybrid nail design similar to a hip prosthesis
stem for proximal nail stability in the shaft as well as linear
compression through an integrated screw construct in the femoral head,
resulting in much greater resistance to rotational instability and
cutout.
nonambulatory or chronic dementia patients with pain that is
controllable with analgesics and rest, terminal disease with less than
6 weeks of life expected, unresolvable medical comorbidites that
preclude surgical treatment, and active infectious diseases that
preclude insertion of a surgical implant. An exception to this
consideration are incomplete pertrochanteric fractures diagnosed by
MRI, which have been shown to heal with conservative
measures in selected patients.4,189
Nonoperative management must include attentive nursing care with
frequent positioning to avoid decubiti, attention to nutrition and
fluid homeostasis, and adequate analgesis/narcotic pain suppression.
Fracture callus formation at 3 weeks markedly decreases motion-related
pain, and by 6 weeks most patients can be lifted into a wheelchair or
reclining chair. Ambulatory capablility should not be anticipated after
nonoperative treatment. Meta-analysis of randomized trials does not
suggest major differences in outcome between conservative and operative
management programs for extracapsular femoral fractures, but operative
treatment appears to be associated with a reduced length of hospital
stay and improved rehabilitation.162
Opponents of nonoperative treatment even for nonambulatory patients
suggest that surgery is more effective for pain relief and does not
result in unacceptable increased mortality or complications.
excessively high risk of mortality form anesthesia and surgery, the
patient is nonambulatory and has minimal discomfort from the fracture,
or modern medical facilities are unavailable, then the strategy
previously discussed by Cooper20 of
rapid mobilization to chair and an upright chest position is
recommended. Mobilization is necessary to minimize decubitus,
pneumonia, and dementia. This form of treatment precludes any future
independent mobility.170
as soon as any correctable metabolic, hematologic, or organ system
instability has been rectified. Usually this is within the first 24 to
48 hours. The literature is inconclusive as to increased mortality
after this time, but patient suffering and hospital efficiencies demand
timely intervention. Holt et al. found that case mix variables (age,
gender, fracture type, prefracture residence, prefracture mobility, and
ASA scores) were the critical aspects of potential for mortality even
when corrected for time of fracture to treatment, admission time to
surgery, and grade of surgical and anesthetic staff undertaking the
procedure. Centers with experience and protocols for the rapid
diagnosis and treatment of hip fractures can effectively decrease the
hospitalization time and complication risks for these injuries.172,204 Interestingly, earlier surgery has not been found to be associated with a higher mortality or morbidity.113
Browne et al. found that surgeons with low volumes of experience (fewer
than seven cases per year) compared with high-volume hip fracture
surgeons (more than 15 cases per year) had higher rates of mortality
and complication, but that high- versus low-volume hospitals were
associated only with shorter hospital stay and lower nonfatal morbidity.30
|
TABLE 48-1 Classification of Plates
|
|||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
constructs, either nail or screws for the head fixation, nail
constructs with either nail or screws, external fixation, and
arthroplasty. Generically these options can be grouped to designs with
common biomechanical behaviors, techniques, complications, and results.
The literature is exhaustive, with series of specific techniques and
implants designs and a fair number of meta-analyses and randomized
prospective studies.
-
Impaction class: Impacted nail-type plate devices (e.g., blade plates, fixed angle nail plate devices)
-
Dynamic compression class: Large single
sliding screw or nail femoral head components with side plate
attachments (e.g., standard sliding hip screws) -
Linear compression class: Multiple head
fixation components controlling rotation and translation but allow
linear compression (e.g., Gotfried PCCP and the InterTAN CHS) -
Hybrid locking class: Multiple fixation
components with compression initially for fracture reduction followed
by locking screws which prevent further axial compression; these types
of fixation are the most stable (e.g., proximal femoral locking plates
[Synthes, Paoli, PA, and Smith-Nephew, Memphis]) (Table 48-1).
used for corrective osteotomies rather than as a primary treatment for
hip fractures. MacEachern reported on the difference of failure
mechanisms with medial penetration of the joint with the Jewett Nail
compared with the sliding hip screw.136
Attempts at modifying the results of nail plates with osteotomies fell
out of favor when comparisons were made with sliding hip screw devices
with anatomic reduction only giving equivalent results with less blood
loss and more rapid operative times.169
1999 meta-analysis, compared accurately fixed nail plates with sliding
implants involving a total of 2855 patients. Results showed an
increased risk of cutout (13% vs. 4%), nonunion (2% vs. 0.5%), implant
breakage (14% vs. 0.7%), and reoperation (10% vs. 4%) for fixed nail
plates in comparison with the sliding implants. In addition, patients
treated with fixed nail plates had a higher mortality and the survivors
were more likely to have residual pain in the hip and
impaired
mobility. The continued use of fixed nail plates gave way in the 1980s
to the unequivocal superiority of the sliding hip screw due to these
complications.36,166
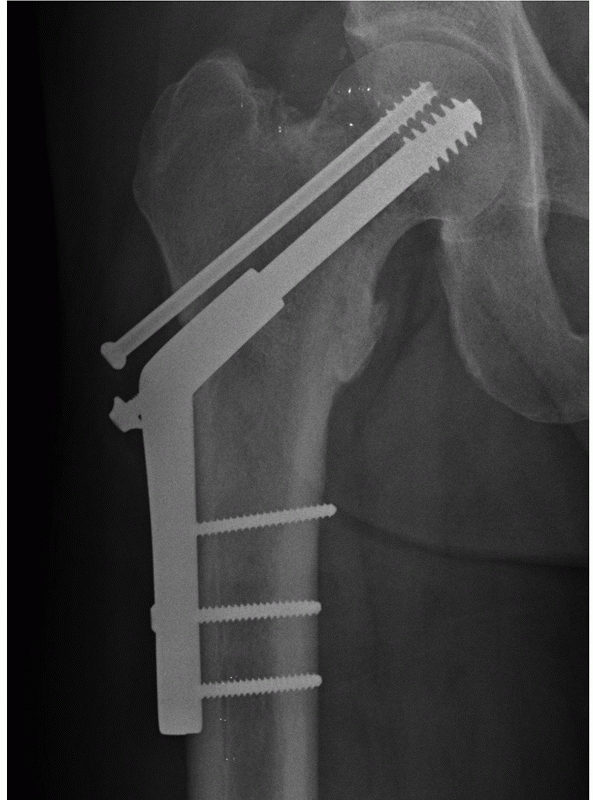
became the gold standard for hip fracture fixation, and many surgeons
still contend its usefulness in all fractures largely because of the
reports of Clawson, Mulholland, and meta-analysis studies by Parker et
al. from 2000 to now (Figure 48-10).164,167,168
In 1983 Rao evaluated 162 cases of unstable intertrochanteric fractures
treated by anatomic reduction and compression hip screw fixation. After
compression was applied, 90% of the fractures moved into medial
displacement position; 8% laterally displaced; and 2% maintained their
anatomic alignment. Loss of fixation with unacceptable varus angulation
of the fracture occurred in 4% of cases. One hundred ten patients were
bearing full weight an average of 3 weeks after operation. They stated
that the advantages of the sliding hip screw were that weight-bearing
could start early; the device was applicable to stable and unstable
intertrochanteric fractures with identical technique; and the fixation
maintained acceptable alignment.
nails with a center-center head position within 10 mm of the
subchondral bone for all fractures, anatomic reduction, prophylactic
antibiotics, prophylactic anticoagulation, and early ambulation,
without osteotomy or interfragmentary fixation except as a
consideration for unstable components in Kyle type 4 in conjunction
with delayed ambulation (although they noted its ineffectiveness). In
classifying their outcome data, they considered a “good result” as
normal hip range of motion, a noticeable limp, occasional pain, and
routine use of a cane; and with this definition they achieved a 96%
good and excellent functional result.
It has a standard lag screw/barrel component for compression along the
femoral neck. In place of the standard femoral side plate, it uses a
coupled pair of sliding components that enable the fracture to impact
parallel to the longitudinal axis of the femur. A locking set-screw may
be used to prevent independent sliding of the lag screw within the
plate barrel; if the locking set screw is applied, the plate can only
slide axially on the femoral shaft (uniaxial dynamization). If the
surgeon applies the implant without placement of the locking set screw,
sliding may occur along both the femoral neck and femoral shaft
(biaxial dynamization). For most intertrochanteric fractures, biaxial
dynamization is suggested.
 |
|
FIGURE 48-10 Compression hip screw components: lag screw, blunt tip, side-plate of fixed angle and cortical shaft screws.
|
 |
|
FIGURE 48-11 Medoff sliding plate.
|
sliding hip screw in a prospective randomized series of 160 stable and
unstable intertrochanteric fractures; follow-up averaged 9.5 months
(range, 6 to 26 months).213 Although
stable fracture patterns united without complication in both treatment
groups, there was a significantly higher failure rate with use of the
sliding hip screw for unstable fractures (14% vs. 3%). No differences
were observed between the two devices in terms of length of
hospitalization, return to prefracture ambulatory status, postoperative
living status, or need for postoperative analgesic medication.
Nonetheless, use of the Medoff plate for all fracture types was
associated with significantly greater blood loss and operating time.
series of intertrochanteric fractures stabilized using either a Medoff
plate or conventional sliding hip screw.153,154
In unstable fracture patterns, mean femoral shortening was
significantly greater with use of the Medoff plate (15 vs. 11 mm), but
the sliding hip screw was associated with more medialization of the
femoral shaft. All failures occurred in the sliding hip screw group.
Synthes) and the Medoff sliding plate (MSP) in patients with unstable
trochanteric or subtrochanteric fractures. They reported that the
ability to walk 15 meters at 6 weeks was significantly better in the
PFN group compared with the MSP group, with an odds ratio 2.2 (P
= 0.04, 95% confidence limit, 1.03 to 4.67). Reoperations were more
frequent in the PFN group (9%) compared with the MSP group (1%), but
there were no other significant differences.53
difference in mortality or functional recovery between compression hip
screws and intramedullary nails with single device fixation in the
femoral head. Interestingly the term malunion of a pertrochanteric fracture dropped out of usage after the 1970s and the emphasis was placed on implant failure.
under scrutiny for its application to all fractures. Haidukewych et al.
noted a higher rate of failure with sliding hip screws for reverse
obliquity intertrochanteric fractures caused by excessive medialization.85 Gotfried noted the high failure rate with associated lateral wall fractures with compression hip screws.76
The effect of shortening of the limb and changes in abductor function
with collapse has always been in the background of the hip literature.
collapse in 142 patients with intertrochanteric hip fractures fixed
anatomically with sliding hip screws, Bendo et al. found collapse (as
defined by strict radiographic criteria relating the height of the
femoral head to the greater trochanter and Doppelt’s criteria) was seen
in 26 of the unstable fractures. Of the patients with moderate or
severe collapse, 93% had a poor functional result, whereas all the
patients with minimal collapse remained asymptomatic. Although
postoperative fracture impaction of hips fixed with sliding screws may
promote early healing, a high rate of union, and a low rate of hardware
failure, excessive collapse is a problem that must be addressed.18
shortening with compression hip screws in non-geriatric patients with
compression hip screw fixation.177
The concern that many surgeons share is the question of functional
impairment with excessive dynamic collapse. Zlowodzki et al. recently
quantified a lower SF-36 score with shortening more than 5 mm in
femoral neck fractures;224 it may be
that the transitional displacement during the first 6 weeks after
surgery with compression side plates may be an underlying problem with
recovery after surgery. Kamath et al. documented significantly more
collapse with compression hip screws in basicervical fractures compared
with reconstruction nail type constructs.109
When the lesser trochanter was intact, plate fixation was associated
with ten times more collapse than nail fixation (8.1 vs. 0.7 mm); and
with complete displacement of the lesser trochanter, the relative
shortening was twice as much for the plate group versus the nail group
(16.1 vs. 8.1 mm). Su et al. reported a greater tendency to collapse
and pain increase with basicervical fractures compared with
intertrochanteric fractures treated with compression hip screws (Figure 48-12).200
Pajarinen et al. reported less deformity with nail devices compared
with SHS and recommended over correction of the hip into valgus to
anticipate the varus collapse with SHS.160
the stability of the compression hip screw with hydroxyapatite coating.
One hundred twenty patients with AO, A1, or A2 trochanteric fractures
were selected. Patients were divided into two groups and randomized to
receive a 135-degree four-hole dynamic hip screw fixed with either
standard lag and cortical AO/ASIF screws or HA-coated lag and cortical
AO/ASIF screws. Lag screw cutout occurred in four patients in with
conventional uncoated lag screws but no cutout occurred in the HA
group. The femoral neck shaft angle collapse from an average 134
degrees postoperatively to 127 degrees at 6 months in the standard CHS
group; but in the HA-coated group, the femoral neck shaft angle was 134
degrees postoperatively and 133 degrees at 6 months. The Harris hip
score was higher at 6 months in the coated group (60 vs. 71), although
the study was relatively small.146
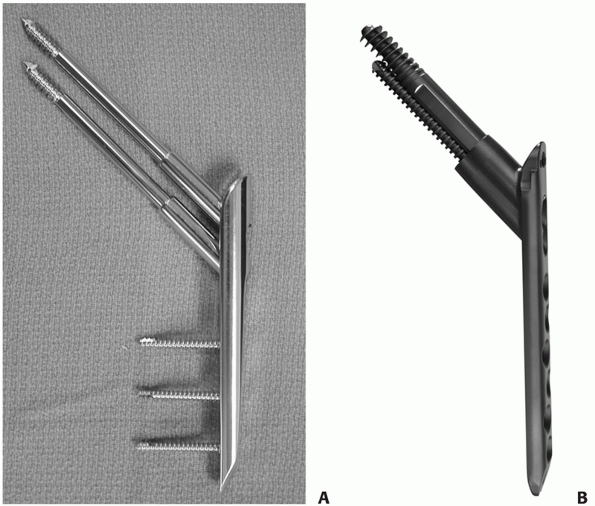
compression plating by adding enhanced rotational stability with
multiple screw fixation in the femoral head. Because the screws are
coupled to the plate, the rotational stability is much better than an
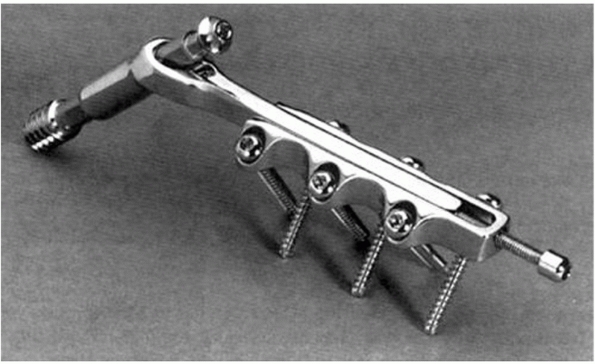
accessory screw adjacent to standard single screw fixation (Figure 48-13).
The percutaneous compression plate by Gotfried (Orthofix, McKinney, TX)
has two smaller-diameter lag screw/barrel components, which stabilize
the femoral head and neck. This device was designed with a minimally
invasive surgical technique. The two lag screw components (9.3- and
7.0-mm diameter) provide enhanced rotational stability of the proximal
fracture.77 The device is available
only in 135-degree angles. It was reported initially by Gotfried in 98
fractures with good results and no collapse, head penetration, or
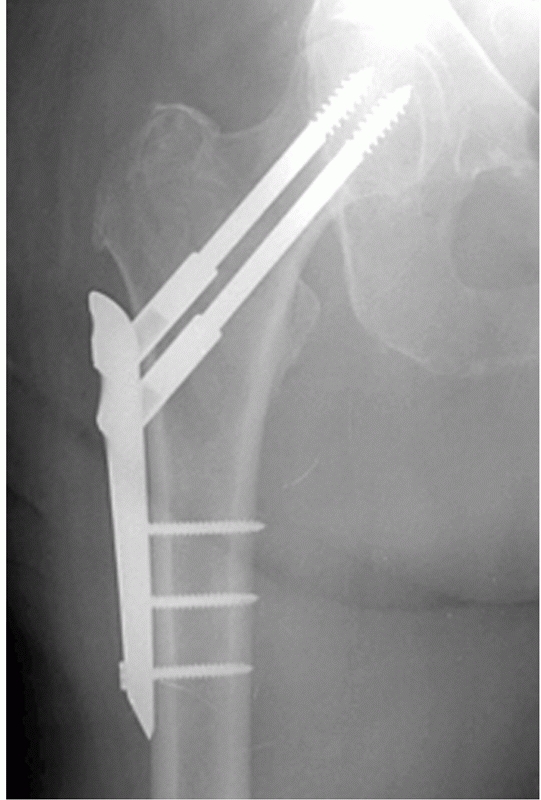
cutout. The InterTAN CHS (Smith-Nephew) consists of a 127- and
135-degree design with two integrated screws, with the option of locked
or standard shaft fixation.
 |
|
FIGURE 48-12
Healing short CHS AP radiograph. Healing of 31A1 fracture with shortening. Note accessory lag screw back out and compression screw prominence in soft tissues. |
comparing dynamic hip screw and PCCP that the pain score and ability to
bear weight were significantly better in the PCCP group at 6 weeks
postoperatively. Radiographically there was a reduced amount of medial
displacement in the PCCP group (two patients, 4%) compared with the CHS
group (10 patients, 18.9%).176 In a
recent presentation of a randomized prospective group of dynamic hip
screw versus PCCP, Yang documented improvements in pain and ambulatory
ability with improved SF-36 scores in the PCCP group.222
a meta-analysis review of comparative trials (1995 to 2006) comparing
the dynamic hip screw and the PCCP. There was a decreased trend in
overall mortality in the PCCP group [CI 0.84 (0.48 to 1.47)]. Similar
trends favoring the PCCP technique were seen with other outcomes. A
large randomized controlled trial was recommended. Other devices with
enhanced rotational stability, such as the InterTAN CHS
and the helical blade plate, are now being studied (Figures 48-14 and 48-15).
 |
|
FIGURE 48-13 A. Percutaneous compression plate (PCCP). B.
InterTAN CHS device. Similar to CHS design but incorporates compression mechanism in second inferior screw for enhanced rotational stability. |
with unstable fractures of the distal femur, the same concepts are
being applied to the proximal femur. The devices offer maximal
stability with initial compression, and fixed angle stability from
locking screws.106 Initial results
are mixed because of early failure rate with original plate designs and
three screw limitations. Newer devices with enhanced fixation strength
may be helpful in complex intertrochanteric fractures with
subtrochanteric extension (Figure 48-16).
 |
|
FIGURE 48-14
PCCP reduction and fixation. Note inferior placement of bottom screw and protection of the greater trochanter by distal plate position. |
piriformis fossa, lateral greater trochanter, or medial greater
trochanter. The femoral head portion of the fixation construct consists
of one or more screw or blade devices interlocked with the nail
component of the construct. Cephalomedullary nails are most commonly
indicated in pertrochanteric and subtrochanteric fractures, and
although there is occasional overlap of these regions, the personality
of the fracture will be predominantly one of these major types. These
nails are designed to have either a pirforimis portal for insertion,
usually with the shaft component straight in the AP plane, or a
trochanteric portal, with the shaft component laterally angulated
proximally. Modern trochanteric designs have moved to a 4-degree
proximal bend positioned above the lesser trochanteric region, which
seem to function best.158
-
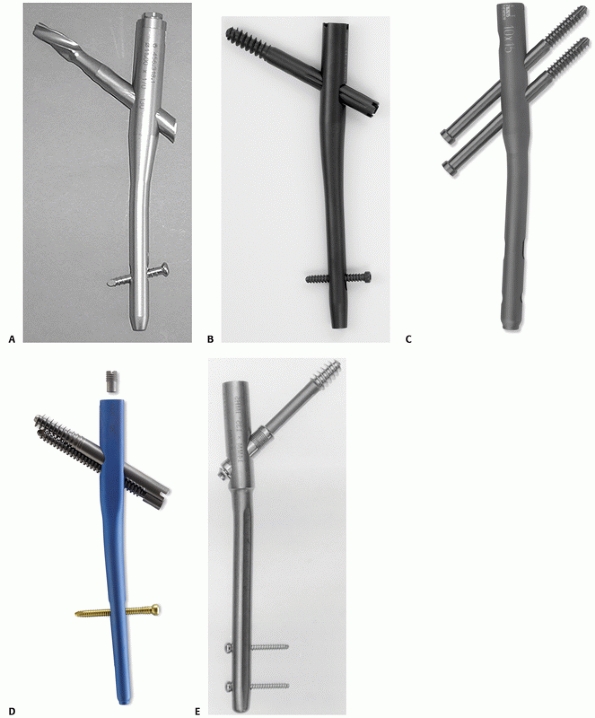
The impaction class or Y nail class originated with the Küntscher Y nail and current TFN Nail (Synthes) (Figure 48-17A).
-
The dynamic compression or gamma class
pioneered by the Grosse and Kempf Gamma Nail (Stryker-Howmedica), which
consists of a large head nail component (15.5 to 18 mm) with a single
large lag screw (Figure 48-17B and 17E). -
The reconstruction class developed by Russell and Taylor (Smith-Nephew) (Figure 48-17C), with a smaller head diameter (13 to 15 mm) and using two lag screws that are independent of each other.
-
The integrated class, consisting of a
nail design cross-section with the stability of a arthroplasty hip stem
and integrated two-screw construct with linear compression at the
fracture site, developed by Russell and Sanders (Smith-Nephew) (Figure 48-17D).
 |
|
FIGURE 48-15 InterTAN CHS case. A. Preoperative radiograph showing 31A2 fracture with greater trochanteric fracture lines and lesser trochanteric fracture. B. AP postoperative radiograph showing fixation. Stability of greater trochanter is maintained. C. Lateral postoperative radiograph.
|
mechanical failure in a series of 230 intertrochanteric femoral
fractures internally fixed with either a sliding hip screw or a
Küntscher Y-nail.44 The cutout rate
for the Y-nail was 8.8% versus 12.6% for the sliding hip screw overall.
Cutout was related to the quality of the fracture reduction; age,
walking ability, and bone density had no significant influence on
cutout. Center-center placement of the head component correlated with
less cutout, and posterior placement increased cutout with both groups.
Y-nail cutout or medial penetration increased with articular placement
less than 10 mm from the tip of the nail (23% Y-nail, 11% CHS), whereas
Y-nail medial penetration decreased with tip placement greater than 10
mm (3% Y-nail vs. 18% CHS).44
component for the femoral head of a helical blade design of 11 mm
inserted into a nail with a 17-mm proximal geometry. There are short
and long interlocking versions.66 In
a biomechanical study Sommers et al. showed better resistance to
rotation with the helical blade compared with single screw designs.198
The surgical technique precludes reaming of the femoral head, thus
saving bone stock and preventing instability of the fracture by a loose
nail. Gill et al.,72 comparing CHS
with TFN, revealed fewer blood transfusions with CHS and faster
operative time for the TFN group. Gardner et al. reported subtle
migration (approximately 2 mm) of the tip of the blade within the
femoral head in all fractures, but this did not preclude maintenance of
reduction and fracture healing. They noted that telescoping averaged 4
mm and did not affect stable fixation or fracture healing. All position
changes occurred within the first 6 weeks
postoperatively.66 Weil et al.214
reported medial penetration with the TFN analogous to the Y-nail type
penetrations described earlier. All eight clinical cases involved an
unstable intertrochanteric fracture pattern (AO/OTA 32A2).
 |
|
FIGURE 48-16 Hybrid locking plate system (Smith-Nephew, Memphis, TN).
|
1980s, an exhaustive series of studies have guided its use and
modifications. Although initially a lateral trochanteric entry nail
with a 10-degree angle and a short nail, the design is now in its third
major revision with decreases to 15.5 mm in head geometry from 17 mm.
Angulation has decreased to 4 degrees for a tip trochanter entry site,
and its distal geometry has been tapered for less risk of
periprosthetic femur fractures (its main detraction in early studies).
The IMHS is a similar class nail with a sliding sleeve in the barrel to
promote dynamic compression (Figure 48-17E).
The clinical studies must be referenced to the different designs and
time periods for correct analysis. Adams et al. reported a prospective
randomized study comparing a sliding hip screw with an intramedullary
nail for treatment of intertrochanteric fractures.3
Two hundred and three patients were stabilized with a short gamma nail,
197 received a sliding hip screw. Patients were followed for 1 year.
Use of the gamma nail was associated with a nonsignificant higher risk
of postoperative complications and equivalent union and functional
results.
|
TABLE 48-2 Classification of Nails
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
hip-screw device compared with the CHS was associated with
significantly less sliding of the lag-screw and subsequent shortening
of the limb in the region of the thigh. Patients whose fractures were
stabilized using the intramedullary hip screw experienced significantly
better mobility at 1 and 3 months follow-up. This difference was no
longer seen at 6 and 12 months, although patients who received the
intramedullary device enjoyed significantly better walking ability
outside the home at all time periods.
consensus regarding the superiority of the dynamic compression nails or
plate type devices and that future studies with the same devices are
unneccesasry.168 There is also
evidence that the complications with nail devices are more frequent.
Despite this evidence, the trend for intramedullary fixation has
increased in the United States.7
developed by Russell and Taylor in the early 1980s primarily for
complex subtrochanteric fractures and pathologic fractures. In 1991,
the Russell-Taylor reconstruction nail was first described for
intertrochanteric fractures in four cases.97
Different versions of this class have in common a smaller diameter head
(13 to 15 mm) with two lag screws of various diameters with long and
short interlocking versions. The original piriformis reconstruction
nail has been modified for medial trochanteric portal insertion, which
simplifies treatment for pertrochanteric fractures. Piriformis
reconstruction nails do no have optimal containment in the trochanter
because of their posterior placement in relation to the femoral head
and neck; they transfer essentially all the load to the head screws.
Trochanteric versions allow better containment of the nail in the
proximal femur and are optimally placed to minimize femoral neck
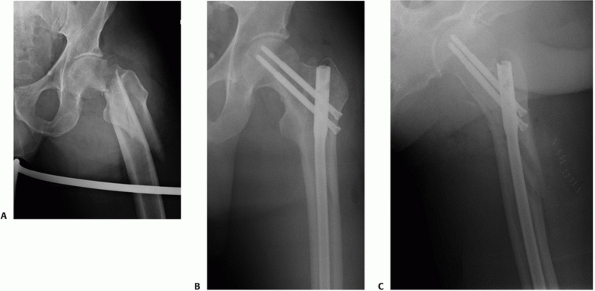
shortening (Figure 48-18).
the Variwall reconstruction nail for unstable intertrochanteric
fractures with 12 patients having subtrochanteric extension.191 Thirty-nine patients healed without deformity, shortening, or varus collapse.
series with CHS, demonstrated less blood loss and transfusion, no
cutout in the nail group, and all fractures united in the Holland
nail group.133
In a more complex group with both pathologic and multiple trauma cases,
Krastman et al. reported an 89% union rate with Holland nails in two
cases with screw penetration of the femoral head.118
The PFN (Synthes) was associated with a high implant failure rate and
the Z-effect of overpenetration of the cephalic screw proximally and
backing out of the inferior screw and has been discontinued in the
United States.10,31,59,194 The device brought attention to the differences in bone quality and effect of rotation with this type of fixation (Figure 48-19).199
 |
|
FIGURE 48-17 A. Short trochanteric fixation nail (TFN). B. Short gamma 3 intramedullary nail. C. Short trochanteric antegrade nail (TAN). D. Short InterTAN cephalomedullary nail with integrated screw design and hybrid stem design. E. Short intramedullary hip screw (IMHS).
|
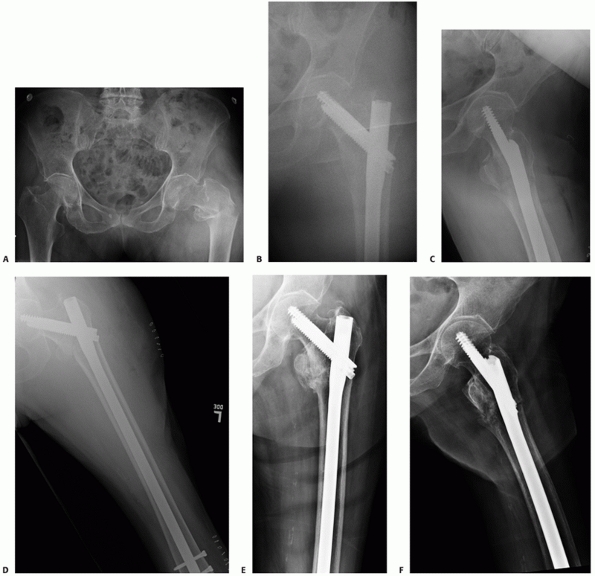
proximal femoral cross-section similar to a press-fit arthroplasty stem
for shaft stability, an integrated screw mechanism that provides linear
compression of the fracture while moving the stem toward the medial
femoral cortex with compression and stress relieving the lateral wall.
It is a trapezoidal design proximally with a 16-mm diameter that tapers
like a hip stem with a 4-degree bend for medial trochanteric insertion.
It is available in 125- and 130-degree
designs,
long and short. The short version includes dynamic locking above a
split tapered tip design to minimize implant stress in the diaphysis.
Like the gamma and Y-nail class nails, it is indicated for older
patients with pertrochanteric fractures with Dorr B and C type
morphology (Figure 48-20).
 |
|
FIGURE 48-18 A. 31A3 with subtrochanteric extension. B. Reduction and repair with long TriGen trochanteric reconstruction nail. C. Recon case lateral postoperative radiograph.
|
InterTan femoral head for the treatment of intertrochanteric fractures
that uses two screws in an integrated mechanism, allowing linear
intraoperative compression and rotational stability of the head/neck
fragment.182 One hundred consecutive
patients with an intertrochanteric fracture were treated with the new
trochanteric antegrade nail (Smith-Nephew). The mean age of the
patients was 81.2 years. Thirty-seven patients died. The average
surgical time was 41 minutes (13 to 95 minutes). All fractures healed
within 16 weeks (range, 10 to 16 weeks). Forty-eight remaining cases
had detailed radiographic analysis at healing that revealed no loss of
reduction, no uncontrolled collapse of the neck, no nonunions, no
femoral shaft fractures, and no implant failures. Two cases in the
series were poorly reduced and settled into varus malalignment. No
varus malposition was seen in the remaining 46 fractures. The mean
prefracture Harris hip score was 75.1 ± 13.4, and at the time of
follow-up was 70.3 ± 14.5 (P = 0.003); 58%
of the patients recovered prefracture status. They concluded that the
InterTAN device appeared to be a reliable implant with stability
against rotation and resultant neck malunions (shortening) through
linear intraoperative compression of the head/neck segment to the
shaft. Further studies are in process for comparative analysis.
 |
|
FIGURE 48-19
Demonstration of the “Z effect,” with one screw penetrating the hip joint and the other screw backing out of the nail. (Courtesy of Enes Kanlic MD, Texas Tech University Health Sciences Center, El Paso, TX.) |
fractures was evaluated in the 1950s, but its use was unsuccessful
because of high rates of pin-tract infections, subsequent pin
loosening, instability, and failure.12,78,119
Renewed interest in this technique occurred recently with the new
fixation designs and the addition of hydroxyapatite coated pin
technology. The addition of the HA coated half-pins with the Orthofix
pertrochanteric fixator by Moroni et al. has resulted in equivalent if
not better results than compression hip screws in 31A1-A2 osteoporotic
fractures.148 There were no pin
tract infections and equivalent functional results by the Harris hip
score comparisons (approximately 62 for both groups). More interesting
is the lower rate of varus collapse of on average 2 degrees versus 6
degrees for the CHS group. The CHS group averaged 2 units of blood
replacement versus none for the external fixation group. Surprisingly,
the external fixation group reported equivalent or slightly less pain
than the CHS group (Figure 48-21).
 |
|
FIGURE 48-20 A. 31A3 fracture with C-type morphology. B. Reduction and stabilization with InterTAN nail. Note alignment of nail paralleling the anterior cortex proximally. C. InterTAN case lateral postoperatively. D. Long nail selection due to wide diaphysis with loss of isthmus anatomy owing to aging and osteoporosis. E. Union without collapse or backing out of proximal fixation. F.
Note medialized nail position owing to integrated screw mechanism inducing translation of nail to medial cortex, unloading lateral wall. |
indicated in osteoporotic hip fractures in elderly patients, who may be
deemed at high risk for conventional open reduction and internal
fixation, or for those who cannot receive blood transfusions because of
personal conviction or religion. It may be superior to standard
compression hip screws in these patient groups.
arthroplasty, often with calcar replacement type components, is rarely
indicated in pertrochanteric fractures.211
Arthroplasty may be justified in neoplastic fractures, severe
osteoporotic disease, renal dialysis patients, and pre-existing
arthritis under consideration
for
hip replacement before the fracture occurred. Hemiarthroplasty, usually
cemented, has been reported to have a lower dislocation rate compared
with total hip arthroplasty. Haentjens et al. reported on 37 patients
more than 75 year old with unstable intertrochanteric or
subtrochanteric fractures from 1983 to 1986. Functional results were
rated as good to excellent in 75% of patients, but there was a
mortality rate of 36% and a dislocation rate of 44%.81
In a review of 29 THA and 5 HA patients with an average age of 80
years, Berend et al. reported 26/34 deaths within the study period of
12 years, with five patients requiring revision surgery for
dislocation. They did not believe their results supported the routine
use of arthroplasty in this elderly patient group.19
 |
|
FIGURE 48-21 A. Preoperative radiograph showing a pertrochanteric fracture in an 83-year-old woman. B.
Immediate postoperative radiograph. (From Moroni A, Faldini C, Pegreffi F, et al. Osteoporotic pertrochanteric fractures can be successfully treated with external fixation. J Bone Joint Surg Am 2005;87:47.) |
compared the mortality risk and complication rate after operative
treatment of pertrochanteric fractures with primary arthroplasty,
dynamic hip screw (DHS), or proximal femoral nail in this retrospective
study. Of these 283 patients, 132 were treated by primary arthroplasty,
109 with a DHS, and 42 with a PFN. Mortality was significantly
influenced by age, gender, and comorbidities, but not by fracture
classification. Primary hip arthroplasty did not bear a higher 1-year
mortality risk than osteosynthesis in a multiple regression analysis.
The main complication with DHS and PFN were cutting out of the hip
screw and nonunion, with a revision rate of 12.8%. With the
introduction of hemiarthroplasty instead of total hip arthroplasty, the
postoperative dislocation rate decreased from 12% to 0%. In a
randomized study, Kim et al. found a lower mortality and less blood
loss with a cephalomedullary nail compared with a cementless calcar
replacement arthroplasty with equivalent functional results.114
salvage operation for failed internal fixation than a first-line choice
in the geriatric fracture patient; and there is no level-one evidence
to show any difference between compression hip screw and arthroplasty,
with the exception of a higher blood transfusion rate with arthroplasty.165
treatment of fractures at the turn of the twentieth century, and they
are as applicable today as then.124,125 The first is exposure of the fracture, which today means visualization of the fracture deformity, and the safest approach to ensure reduction
and placement of the implant in the correct position. The second is reduction
of the fracture, which is critical to the stability and functional
recovery of the patient. Inadequate reduction is the major preventable
etiology for lost reduction and implant failure in pertrochanteric
fractures. The third step is provisional fixation in an anatomically reduced position;
this is frequently the most neglected step in hip fracture surgery.
This involves the reduction of the fracture and then maintenance of the
fracture with either provisional Kirschner pins and/or clamps to hold
the fracture in position while the bone is prepared for the definitive
implant. The last step is definitive fixation,
which should maintain the reduced fracture in an acceptable anatomic
and functionally correct position until fracture healing is complete.
elimination. The OTA/AO classification is a good starting point for
determination of fracture treatment. Conceptually, the 31 A1 fracture
can be treated with basically any of the previous implants if the bone
quality and morphology are acceptable. The most common plan is the
sliding hip screw system. Nevertheless, external fixation,
intramedullary nail techniques, and linear compression type devices
could be chosen for osteopenic individuals. External fixation might be
used for patients who are too ill for conventional open reduction based
on the suggestions from medical and anesthesia consultants. For 31A2
and A3, I prefer techniques with less potential for instability after
fixation (Figure 48-22).
optimize the size of the implant footprint for the bone stock
available. For Dorr A type fractures, with small canals, a plate device
or reconstruction class nail is chosen for bone conservation. For Dorr
B type fractures, either a short nail or side plate is equally
efficacious. For Dorr C type anatomy, a larger diameter
cephalomedullary nail may offer advantages. My personal preference is
to use a longer nail for A3 type fractures. The results with locking
plates are relatively recent and most reports have primarily been
descriptive in nature. The primary indication of these devices may be
A3 type fractures with multifragmentary type patterns (31 A 3.3) and
those with the extensive subtrochanteric extension. Trochanteric
buttress plating is helpful for compression hip screws to minimize
medialization of the shaft in unstable fractures or fixation of
displaced trochanteric wall fractures.
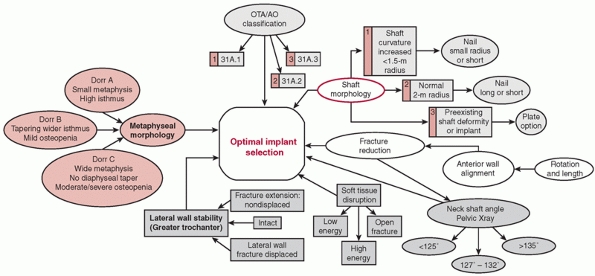 |
|
FIGURE 48-22 Implant selection variables.
|
normal femur may be helpful in selecting the correct length nail in
complex fractures (Figure 48-23). Determination
of preoperative neck-shaft angle and medullary canal diameter is
paramount to selection of the correct nail device, as different
manufacturers have different neck shaft angle and diameter nails.
Another important consideration is nail curvature for long nails. One
and a half to two meter radius nails are applicable to most situations.
It is important to note that multiple variables come into play in
deciding on the treatment of hip fracture. As the entry portal and hip
fracture nailing has moved from a piriformis or a lateral trochanteric
portal to a medial trochanteric portal at the tip of the trochanter,
the alignment of the curvature of the long nails is more compatible
with the distal femoral anatomy. For the intermediate sizes of bone,
either plate and screw devices or short intramedullary nails may be
appropriate.
best managed with a modern fracture table with image intensification
(C-arm) capabilities. Although the lateral decubitus approach may be
helpful for reverse obliquity patterns, the supine position is usually
preferred because of the ease of setup and radiographic visualization
in a familiar frame of reference. We prefer bilateral foot traction
with knees in extension with the legs scissored. The operative leg is
raised to approximately 20 to 30 degrees of flexion, and the
nonoperative extremity is extended 20 to 30 degrees. The legs are
pulled
in line with the body to avoid varus positioning of the hip. The C-arm
is brought in from the opposite side with the base parallel to the
operative extremity centered on the mid-femur such that the
cepalad-caudad movement of the C-arm gives good visualization of the
femoral head and shaft in AP and Lateral views. With this type of set
up, the true AP of the hip is usually obtained with 10 to 20 degrees of
rotation of the C-arm over the top, and the true lateral corresponds to
approximately 15 to 30 degrees over the horizontal position (Figure 48-24).
 |
|
FIGURE 48-23
Using contralateral extremity to measure nail selection for comminuted fracture. Nail package with anticipated nail length measured with intraoperative C-arm. Locate nail to lie at tip of greater trochanter to distal physeal scar. This length allows adequate length restoration. |
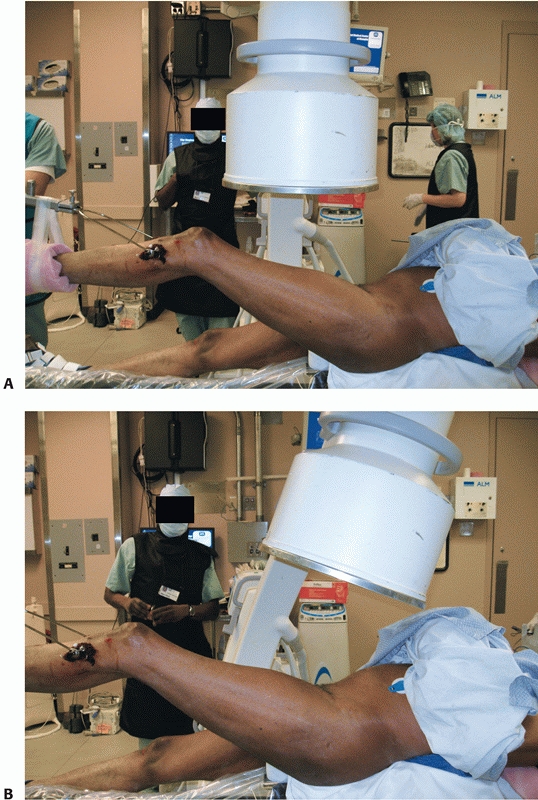 |
|
FIGURE 48-24 A. Conventional C-arm position will yield an oblique view. B. Correct C-arm position for flexion of the shaft. Make sure that C-arm axis is perpendicular to femoral axis. (continues)
|
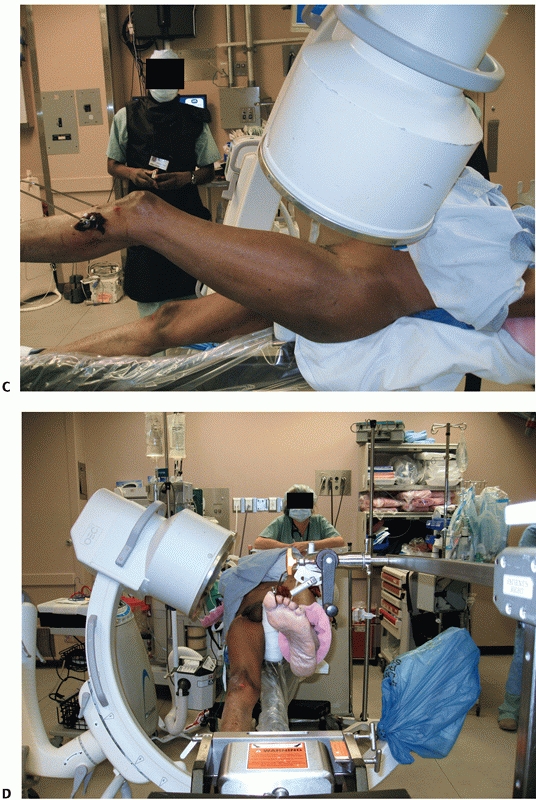 |
|
FIGURE 48-24 (continued) C. Correct C-arm position for anteversion. Tilt C-arm over leg 10 to 15 degrees to get the maximum length of the femoral neck. D.
Correct lateral C-arm to avoid excessive internal rotation. Obtain true lateral along neck anteversion without excessive internal rotation of leg. |
correct position for the hip fracture reduction but in studies by
Bannister et al. and May et al., pertrochanteric fractures may have an
equal chance of being reduced in neutral or external rotation and
external rotation was required in 25% of cases.11,141
Excessive internal rotation can lead to posterior gapping, further
destabilizing the fracture with a large posterior medial defect. The
focus on the anatomic reduction is paramount to success and should be
on the anterior medial cortex reduction. The author’s preferred
technique for the proximal femur involves a four-step technique:
-
After attachment to the foot positioner
with the perineal post attached, correct posterior sag at the fracture
with a posterior to anterior directed force and maintain. -
Flex the leg through the foot holder 20
to 30 degrees from neutral for intertrochanteric personality fractures
and 30 to 40 degrees for subtrochanteric personality fractures,
maintaining the posterior to anterior reduction force at the hip. -
Apply traction to restore length in line with the body. No varus.
-
Rotate the leg to align with the proximal
fragment, 5 to 15 degrees of external rotation for most subtrochanteric
fractures personalities and 0 to 10 degrees of internal rotation for
pertrochanteric fracture personalities.
for a lack of reduction. In 1963 Sarmiento called attention to the key
components of reduction of the pertrochanteric fracture:
if the fracture, whether simple or comminuted, has been reduced so that
there is an accurate fit of the fragments at the anteromedial cortex of
the femur. Absorption of the reduced medial cortex of the femur with
loss of stability is unlikely because of the great thickness and
strength of the medial
cortex.
Failure to obtain such reduction because of the degree of comminution
or technical difficulties precludes weight-bearing until bone union is
complete. Anatomical reduction of the medial and anterior cortices is
of great importance since the stability of the fracture and the
efficiency of the nail depend on the reduction of this portion of the
bone.186
common reason that obtained reductions are lost during fixation.
Provisional fixation must be placed so that it will not interfere with
the definitive fixation. Typically this can be achieved with 3.2
K-wires introduced away from the path of the definitive fixation.
Alternatively, fixation can be achieved in long oblique fractures by
K-wire fixation from the anterior longitudinal shaft region into the
medial femoral neck. The key is to position these K-wires such that
they do not interfere with the definitive preparation and fixation of
the bone. Weber-type clamps with a wide jaw may be inserted in a
limited open reduction in conjunction with a bone hook along the medial
cortex or medial to the greater trochanter to achieve fracture
reduction. If there is posterior displacement of the distal fragment,
there are no soft tissue structures to leverage and a manual reduction
of the shaft to an anterior position will be required. These
displacements require a combination of traction, translation of the
distal fragment, and some degree of rotational correction. Rotational
reduction is best evaluated by intraoperative radiographic views.
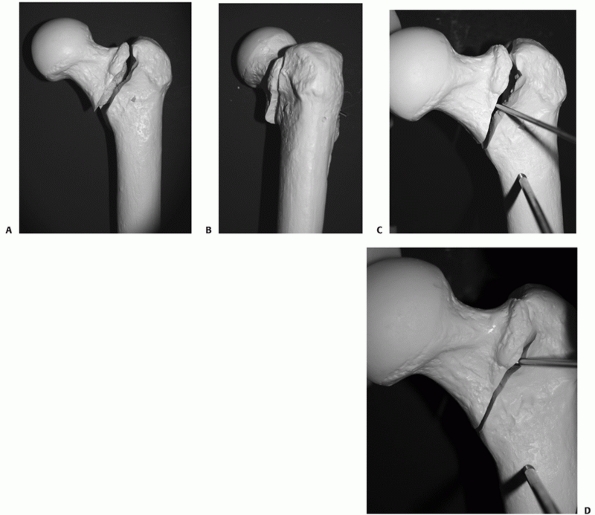 |
|
FIGURE 48-25 Stepoff deformity. A. Model of typical stepoff deformity showing overlap of anterior cortical surface. B. Lateral view showing overlap on lateral position. C. Reduction of the anterior cortex. Reduction of overlap with percutaneous pin with coach-lever maneuver. D. Reduction achieved.
|
Sarmiento’s focus on the anteromedial cortex and described reduction
techniques to facillitate the reduction. After a standard lateral
approach is made to the hip, the anterior reduction is assessed by
palpating the region of the intertrochanteric line anteriorly. Palpate
for a stepoff, which identifies where the posteriorly displaced shaft
overlaps the anteriorly displaced head and neck fragment (Figure 48-25A,B).
First pull the shaft laterally to disimpact it from the head and neck
fragment with a bone hook passed around the femoral shaft in a
subperiosteal manner distal to the lesser trochanter. With the shaft
displaced laterally, insert a narrow Jocher or key elevator between the
head and neck shaft pieces, and lever the head and neck piece
anteriorly, applying a posterior force to the shaft to align the two
fragments (Figure 48-25C,D). Adjustment in length and rotation of the limb may be required at this time. Release the laterally
directed traction on the shaft. Confirm the anterior reduction with
C-arm views. At this point, anteroposterior radiographic views of the
hip reveal an anatomic neck shaft junction —manifested as a “hairline
crack reduction.” On the lateral view, the anterior cortex line is
re-established. Secure the reduction with one or two 3.2-mm wires that
are directed away from the area of intended lag screw placement. Be
careful that the anterior reduction is not lost during insertion of the
hip compression screw, which tends to rotate the head and neck
fragment. Once all implants are positioned, the compression screw is
used to compress the reduction after removal of the provisional wires.
percutaneous Schanz pin in the anterior distal shaft component in
conjunction with a percutaneous ball spike pusher on the anterior
proximal cortex can effect a reduction. A K-wire can then be introduced
in a longitudinal direction from the anterior superior trochanter into
the distal shaft fragment for provisional fixation. Ookuma and Fukuda
reported that the anteromedial reduction can be obtained percutaneously
with a 3.2-mm wire inserted in the same fashion as described by Carr in
the open version. Furthermore, they developed a reduction
classification that confimed stability with only 2 mm collapse with
anteromedial reduction on the AP and lateral planes with two-part
fractures treated with the gamma nail, but greater than or equal to 5
mm displacement with intramedullary malreduction of the proximal medial
cortex into the distal medullary canal.155
fracture patterns. The head and neck to shaft reduction can be obtained
by manipulating the fracture in a manner similar to the side plate
technique. A lateral approach at the site of the lag screw insertion
can be made to allow placement of the bone hook or Weber clamps as
needed. A small accessory incision anterior to the femur at the level
of the femoral neck will allow insertion of the Jocher elevator or ball
spike pusher.
in the supine position with either a scissored leg traction setup or
with the affected leg extended and the contralateral leg abducted and
flexed out of the way of the C-arm. Slight flexion of the leg is
usually helpful. Traction should not be too powerful, as it may disrupt
any remaining soft tissue attachments and further destabilize the
fracture. The reduction steps are carried out as described previously.
A lateral incision is made after standard prep and drape centered from
the Vastus lateralis ridge approximately 6 cm distally in line with the
iliotibial band. Reflect the vastus lateralis near its origin on the
posterolateral surface the femur with care to obtain control of any
perforator vascular branches. The vastus is elevated anteriorly and
Hohmann retractors are placed for exposure of the lateral shaft. After
provisional fixation an anatomic reduction is secured with good
reduction of the anterior medial cortex and the position for the plate
is determined. A 3.2-mm K-wire is introduced over the anterior femoral
shaft under image control centered in the femoral neck into the femoral
head and tapped into the head. This will actually penetrate the capsule
of the head and is safe if kept on the anterior surface of the bone.
This gives the anteversion alignment of the proximal femur and also the
relative neck shaft angle, as originally described by Tronzo.208
Next a 3.2-wire using an appropriate angle guide, usually 125 to 135
degrees, is introduced at the level of the lesser trochanter in line
with the previous anteversion pin. In hard bone it is often helpful to
predrill with a 4.5-mm drill bit direct the guidewire into the femoral
head easier. The guidewire is then inserted centered on the AP and
lateral views in the femoral neck. It is important that the wire should
not be positioned too anteriorly or posteriorly from its entry portal
and should be centered on the AP and the lateral x-rays into the
femoral head. The wire should be advanced to within 5 to 10 mm of
subchondral bone to meet the requirements of the tip apex distance, as
described by Baumgaertner, of less than 25 mm. Next the length
measurement is taken; usually at this point a triple reamer type device
reams a path for the screw into the femoral head and also the expansion
of the lateral cortex for the plate to the selected depth. Usually a
screw will be selected that will be 5 mm less than the drill depth. If
the bone is dense it should be tapped and provisional fixation should
be applied to the fragment before tapping to ensure that there is no
loss of rotation because of the torquing of the tap. Insert the lag
screw with a cannulated attachment over the guidewire and seat the
screw to within 5 to 10 mm of subchondral bone. The selected plate is
usually of a 2- to 4-hole design; two holes for simple two-part stable
fractures, and the larger length for more unstable patterns or
osteoporotic bone. The plate is applied and inserted over the lag
screws. If the plate does not oppose itself easily to the bone, the
wrong angle may have been selected. Care should be taken not to force
the reduction of the plate to the bone, as this may result in gapping
of the medial cortex with induced instability. Attach the plate to the
femoral shaft with a standard drill bit (3.2- or 3.5-mm, depending on
the system) and a 4.5-mm cortical screw inserted in the proximal
platehole. Care should be taken that the plate is aligned with the
shaft of the femur to avoid offset or unicortical screws distally. Next
release traction and impact the plate with an impactor. Most systems
have compression screws that can be inserted through the plate into the
large lag screw. Apply compression after traction is released.
Excessive compression should be avoided, as it may disrupt the fixation
of the head and render it unstable. Also, in anticipation of up to 5 mm
of sliding, the screws should not be brought out so far that they
actually protrude past the plate, as this may cause postoperative pain
from the implant. Whether the compression screw device is left in place
is up to the surgeon; there are no clear data as to removal or
retention. The plate is then further secured with 4.5-mm screws with
bicortical fixation (Fig. 48-26A-C). Hemostasis
is confirmed and the wound is closed in layers in the standard fashion.
Drains are not routinely used unless the patient is on anticoagulant
therapy.
Intraoperative
confirmation of the reduction on the AP and lateral views and a
radiographic record obtained. The importance of provisional fixation
during screw insertion was pointed out by Mohan et al. in 1993. Their
study showed that malreduction occurred with tightening of the screw in
left-sided patients with malreduction (Fig. 48-26D,E).
 |
|
FIGURE 48-26 A. High-energy 31A fracture. B. Reduction and stabilization with CHS. Good position with good bone stock aids the stability of the fixation with CHS. C. Lateral postoperative radiograph. D. Malreduction with plate angle too high inducing medial opening of the fracture. E. Anterior translation of fracture with wrong angle plate.
|
fracture reduction, using a standard fracture table and the posterior
reduction device. Make a first stab incision of approximately 2 cm in
the lateral trochanteric area, followed by introduction of the plate,
connected to the introducer, which slides along the upper lateral
femoral shaft. The anteroposterior and lateral positions of the plate
are checked under an image intensifier and necessary corrections are
made. Make the second stab incision approximately 2 cm. Introduce the
percutaneous bone hook for reduction and clamping of the plate to the
femur. Insert the main sleeve through the lower oblique hole in the
plate. Insert the main guidewire into the femoral neck so that it is
approximately 2 to 3 mm proximal to the calcar on the anteroposterior
view and within the middle third of the femoral neck on the lateral
view. The butterfly pin is then fixed for temporary fixation of the
plate to the femur. The main guide and first sleeve are then replaced
by
the second sleeve and a 7.0-mm drill. A 7.0-mm hole is drilled. Next a
final drilling of 9.3 mm is performed for the screw barrel. The first
neck screw is screwed through the plate and the femoral neck up to the
subchondral bone, and the fracture is then compressed. Remove the main
sleeve, insert the short shaft sleeve to drill, and fix the three shaft
screws through the second incision. Remove the bone hook and butterfly
pin after insertion of the first shaft screw. The second, proximal,
neck screw is then placed in the same way as the first one. The
introducer is disconnected and removed. The wound is irrigated and
closed over a suction drain. Postoperatively, full weight-bearing is
permitted after surgery with crutches or walker.
replace the original sliding compression hip screw, and many designs
are now becoming available.
cephalomedullary surgical technique is based on three concepts of bone
and soft tissue conservation and nail implantation that minimize the
potential for malalignment: (i) Precision portal placement, (ii)
trajectory control, and (iii) portal preservation. A precise starting
point is the first criterion in assuring an accurate fracture reduction
of proximal fractures, whether the entry portal is a modified
trochanteric entry portal or a piriformis portal as defined by the
selected nail geometry. The medial trochanteric portal has become the
preferred portal for nail technqiues for hip fractures for both
mechanical stability and minimal soft tissue damage to the gluteus
medius.173 The proximal femur is
filled with a solid cancellous bone architecture from the femoral head
region until the level just below the lesser trochanter, where the
medullary canal begins. Trajectory control is the development of a
precise path for the nail through this solid cancellous bone, which
will restore the proximal alignment in the anteriorposterior and
medial-lateral planes. This correct trajectory parallels the anterior
lateral cortex of the proximal femur and allows nail juxtaposition
against a solid cortical structure. An incorrect trajectory will induce
malalignment with nail insertion and result in an unstable
juxtaposition against cancellous bone only, forcing the nail to migrate
to the posterior cortex and resulting in a flexion deformity of the
proximal fragment. Once the correct trajectory is established, the
portal and the lateral wall of the trochanter must be protected from
erosion and fragmentation by the subsequent instruments for fracture
reduction and canal preparation. Typically with the patient in a supine
position this erosion takes place in a posterolateral direction,
further contributing to a flexed and varus position of the proximal
fragment, with nail insertion occurring during reaming of the proximal
femoral component. A stepwise approach to canal preparation simplifies
the nail insertion technique.
protection to the region of the greater trochanter and insert a 3.2-cm
guide wire approximately 5 to 10 mm into bone in the lateral aspect of
the greater trochanter. This is a pivot pin about which a
honeycomb-type targeter can be adjusted to precisely place the
definitive guidewire pin at the tip of the greater trochanter. The
definitive guidewire should be just medial to the tip of the greater
trochanter on AP C-arm view and centerered in the femoral neck on the
lateral C-arm view. The definitive guidewire should be inserted 10 to
15 mm into the trochanter and does not have to be in correct canal
alignment because the definitve trajectory will be obtained in the next
step (Figure 48-27A,B).
end cutting capability (Channel Reamer, Smith-Nephew, Gamma3, Stryker),
approximating the proximal nail geometry diameter and introduce it over
the guidewire through the protective sleeve. Advance the rigid reamer
or channel reamer directed toward a point projected in the center of
the medullary canal just distal to the region of the lesser trochanter (Fig. 48-27C).
Advance the reamer stepwise confirming maintenance of trajectory. After
the reamer has been inserted approximately 20 mm, confirm the reamer’s
trajectory with a lateral C-arm view. The reamer should be directed
along the anterior cortex of the proximal femur. Insert the reamer
until it reaches the medullary canal just below the region of the
lesser trochanter. Remove the inner reamer and maintain the outer
reamer for protection of the proximal reamer during the next step.
similar curved cannulated device through the retained channel reamer to
the fracture site and thread it through the fracture site into the
distal fragment intramedullary canal with manipulation in appropiate
planes to align the fracture (Fig. 48-27E).
Insert a long guidewire to the knee if a long nail is desired,
confirming that the wire does not impinge on the anterior cortex
distally. Preferably the guidewire should be inserted distally for long
nails to the old physeal scar and centered on AP and lateral C-arm
views (Fig. 48-27F). Remove the reducer, and
maintain the guidewire position with an obturator proximally. Check the
length with an appropriate ruler, allowing for fracture distraction and
final nail position. Ream the diaphyseal region up to 1 mm over the
desired nail size; ream up to 2 mm for excessive anterior bows. The
proximal expansion of the nail should have already been reamed with the
entry portal reamer, but always confirm diameters. Remove the channel
reamer and insert the selected nail.
Fixation: Dynamic Compression Cephalomedullary Nail Designs (e.g.,
Gamma [Stryker-Howmedica], IMHS [Smith-Nephew])
creation, and canal preparation are as previously described. With the
correctly positioned guidewire and reduction obtained, proceed with
nail insertion. Using the proximal alignment guide, insert the nail to
a depth that will place the guidewire in a slightly inferior positon
from the center-center position in the head and neck and confirm
rotational alignment on the lateral radiograph (Fig. 48-28A-D).
The gamma nail does not encourage the forceful insertion of the nail
with a hammer, and this may cause difficulty with insertion and require
additional
proximal reaming to ensure sufficient depth insertion. Make a lateral
incision on the thigh in line with the anteversion postion of the nail
guide and insert the trocar to bone. Caution:
During this step anteversion may be misaligned. Do not insert the drill
for proximal screw fixation until both depth of insertion and
anteversion are certain. Drill a wire to within 5 mm of subchondral
bone, confirm fracture reduction, and measure length to lateral cortex.
If compression is desired (usually 5 mm), ream for the screw and select
a screw 5 mm shorter than measured. Insert the head fixation screw or
nail to the desired depth and confirm on AP and lateral C-arm views.
Insert the locking nut into the proximal nail canal and advance to the
lag screw (Fig 48-28E,F).
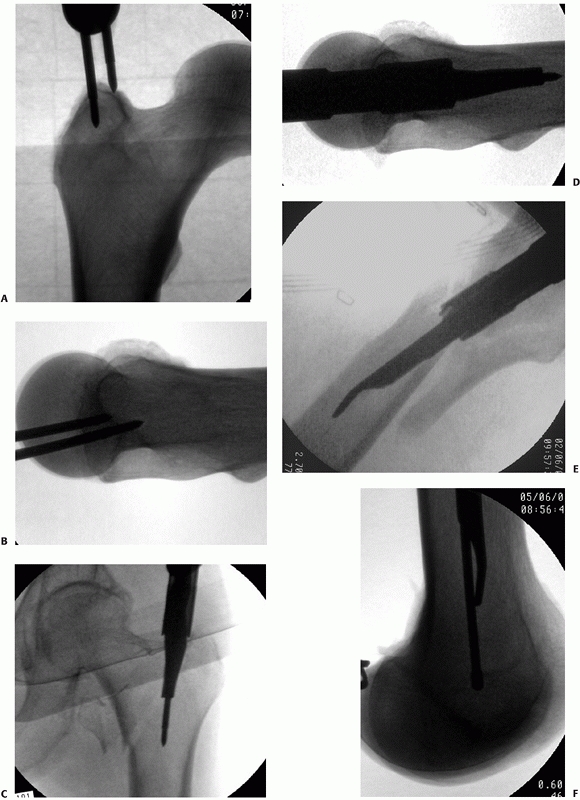 |
|
FIGURE 48-27 A.
AP guidewire options: tip of trochanter for most 4- to 5-degree angle nails or medial trochanter to minimize gluteus medius tendon damage and allow optimal compression with InterTAN nail. B. Lateral position should permit nail proximity to anterior cortex not posterior cortex and allow center position of head fixation. C. Medial trochanteric portal with reamer. D. Parallel anterior cortex with channel reamer for correct trajectory control. E. Reducer for subtrochanteric extension or segmental fractures. F. Use reducer to position distal guide wire centered on lateral radiograph to minimize risk of distal nail penetration. |
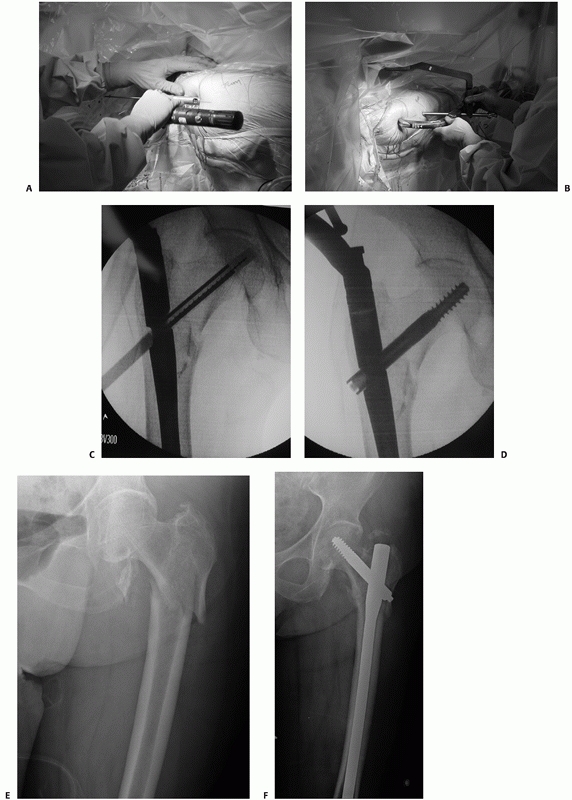 |
|
FIGURE 48-28 A. Placement of the nail by hand down the medullary canal. B,C.
Use of the sure-shot guide to help determine correct nail positioning to allow placement of the lag screw in the center of the femoral head and neck. D. Insertion of the lag screw through the intramedullary nail. E. Reverse obliquity 31A3 fracture. F. Anatomic reduction and optimal nail screw position. |
screw fixation preferably in a dynamic mode. One screw is sufficent for
most pertrochanteric fractures that do not extend below the lesser
trochanter. For distal extension, a long nail is preferable. Long nails
require distal interlocking with a free-hand technique.
Cephalomedullary Nails: Cephalomedullary Nail 2 Screw (Russell-Taylor
Reconstruction Nail, TriGen TAN [Smith-Nephew])
prepare the canal with a minimialy invasive technique as described
previously. For long trochanteric nails it is helpful to rotate the
nail 90 degrees anteriorly during the first half of the nail insertion
to minimize hoop stresses in the proximal femur; after partial
insertion rotate the nail to the anticipated anteversion required for
femoral head fixation (Fig. 48-29A,B). Insert
the last 5 cm of the nail after releasing distraction sufficient for
fracture apposition maintaining corrrect rotational alignment. Most
commercial guides use reference marks to align with the femoral head on
the lateral C-arm view. These same guides may be used for C-arm
verification of correct depth of insertion to allow optimal femoral
head fixation. Remove the long guide rod to proceed with interlocking.
Proximal interlocking will depend on the type of implant selected;
however, most designs recommend that the screw be placed as close to
center-center as possible. If a secondary screw is included in the nail
design, that is, reconstruction or InterTAN constructs, there is
usually sufficient room for the second screw inferiorly, but exercise
care in small patients.
C-arm to obtain a true lateral view of the hip. The nail guide and nail
are superimposed and the handle rotated until equal amounts of femoral
head are visualized anterior and posterior to the nail and guide. This
position will center the guidewire on the head from the lateral
reference point. Using the proximal guide, with the true AP view,
insert the nail until the depth centers the guidewire on the AP view.
Using the proximal targeting guide attached to the nail, insert the
distal-most proximal guidewire along the femoral calcar within 5 mm of
the inferior femoral neck centered on the lateral C-arm view to within
5 mm of subchondral bone (Fig 48-29C). Through
the proximal targeting guide attached to the nail, insert the most
proximal guide pin that will be close to the center postion of the
femoral head parallel to the first guide pin and confirm its position
with the C-arm. Remove the inferior guidewire, drill and ream for the
selected lag screw for the system, and insert the inferior screw (Fig 48-29D,E).
Next repeat the same steps for the proximal screw. Release traction
before final tightening of the lag screws to allow fracture compression
(Fig 48-29F). Proceed with distal interlocking with a free-hand image-guided technique.
with open procedures and is indicated in OTA/AO Class 31A1 to A2
fractures only (Figure 48-30). General
recommendations of a stable reduction confirmed with intraoperative
fluoroscopy under general or local anesthesia still apply. After
standard skin preparation, prophylactic antibiotics, a 2.0-mm K-wire is
introduced in the most cephalad portion of the femoral head and neck
subtending an angle of 110 to 130 degrees and centered on the lateral
radiograph. This wire serves as guidance and provisional stabilization
during the femoral head fixation pin placement. A 4.8-mm drill guide
and drill penetrate the lateral cortex through a percutaneous stab
incision. Advance the drill appproximately 3 cm under image
intensification control parallel to the path of the guidance K-wire
previously placed. Insert the first HA (hydroxyappatite coating) 6-mm
pin to within 10 mm of the articular surface and no more. Remove the
drill guide and K-wire and attach the proximal fixator Clamp and insert
the 6-mm trocar through the fixator body parallel to the proximal pin
on the lateral view and slightly convergent on the AP view. Advance the
drill guide through a second stab incision and advance the trocar to
bone. Repeat the drilling and HA coated half-pin insertion for the
second femoral head fixation. Clamp the proximal fixation 2 cm away
from the skin and tighten the proximal pin cluster assembly. For shaft
fixation, insert the 4.8-mm trocar and drill guide perpendicular to the
shaft, below the level of the lesser trochanter. Through a stab
incision, advance the trocar to bone and drill both cortices with a
4.8-mm drill. Insert the third HA coated pin confirming good screw
purchase in the near and far cortices. Check rotation of the distal
clamping array of the external fixator to ensure bicotical purchase of
the fourth and final pin. Repeat the same half-pin preparation and
screw insertion. Confirm fracture reduction, avoiding overdistraction
and tighten all connections securely. Confirm that with flexion and
extension of the hip there is no skin tension on the half-pins, and
extend the incision about the pins as necessary. Apply dry dressings
around the pin sites.
internal fixation, with mobilization within 24 hours after surgery with
walker or crutches and weight-bearing as tolerated. Pin sites are
cleaned twice weekly with saline solution. External fixation is removed
in the office without the need of anesthesia at 3 months
postoperatively. Ambuation progresses as tolerated.
to assess the construct and ensure stability. If adjustments are
necessary, these are best made while the patient is still under
anesthesia. Radiographs should reveal the entire fracture region,
including the entire implant construct. The patient is mobilized to a
chair upright postion the day after the operative procedure. Ambulation
is performed with supervision with weight-bearing as tolerated with a
walker or crutches with emphasis on heel-strike and upright balance
exercises. Multiple trauma or patients with other complications may
have delayed ambulation, but it should began as soon as possible to
minimize secondary complications. Delay in getting the hip fracture
patient out of bed is associated with poor function at 2 months and
worsened 6-month survival.195 Studies also reveal decreased rates of pneumonia, urinary tract infection, and dementia with early mobilization.110 Besides accelerating recovery, the ability to ambulate postoperatively is prognostic for survival rates.101 Specific fracture service and rehabilitation protocols reduce 30-day mortality rate from 22% to 7%.171
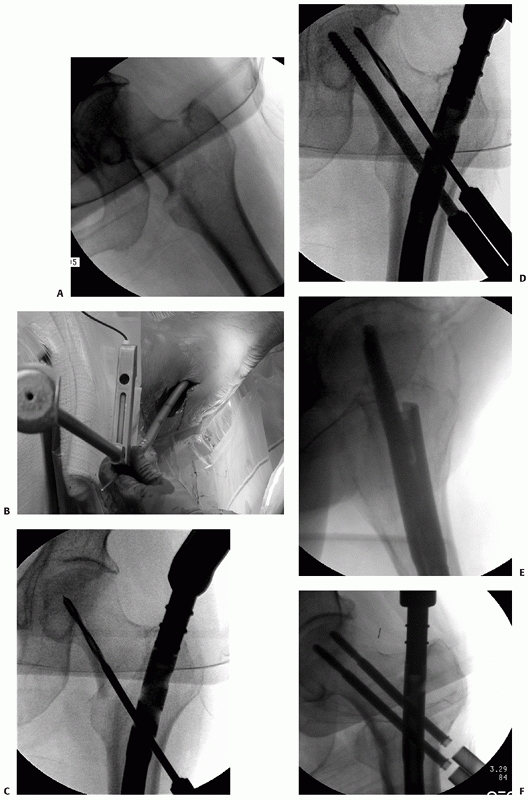 |
|
FIGURE 48-29 A. 31A1 fracture in Dorr A bone. B.
Trochanteric nails with a 5-degree proximal bend should be inserted with 90 degrees of internal rotation initially and then rotated externally at 50% insertion to minimize hoop stress at the insertion site. C. With recon technique the bottom guidewire should be inserted first and just above the inferior femoral neck. D. Inferior screw placed and drilling for proximal screw. E. Optimal lateral position of nail and screws. F. Final head fixation AP radiograph. |
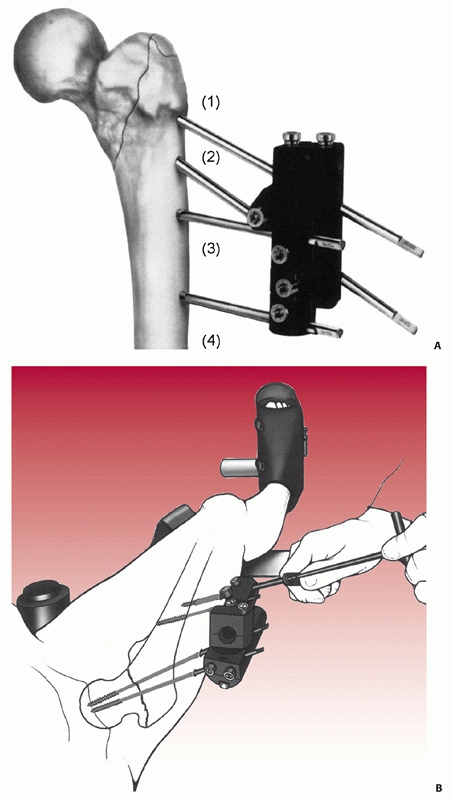 |
|
FIGURE 48-30 Orthofix pertrochanteric fixation. A. Pin positions 1 and 2 are in cancellous bone; pin positions 3 and 4 engage cortical bone. B.
The remaining pins are implanted, starting from pin position 2 (proximal) and ending with pin position 4 (distal), with use of the same surgical technique. (A from Moroni A, Faldini C, Pegreffi F, et al. Dynamic hip screw compared with external fixation for treatment of osteoporotic pertrochanteric fractures: a prospective, randomized study. J Bone Joint Surg Am 2005;87:755; B from Moroni A, Faldini C, Pegreffi F, et al. Osteoporotic pertrochanteric fractures can be successfully treated with external fixation. J Bone Joint Surg Am 2005;87:47.) |
optimal recovery and to assuage the fear of falling and lack of
independence. Weight-bearing stability of the implant construct
improves the functional ability of these patients.193
There must be sufficient stablity to allow aggressive physical therapy,
especially in cognitvely impaired patients with hip fracture.150 Koval has reported that patients autoregulate their weight-bearing.116
recovery. Patients with higher pain scores at rest had significantly
longer hospital lengths of stay, and were more likely to have physical
therapy sessions missed or shortened, less likely to be ambulating by
postoperative day 3, took longer to ambulate past a bedside chair, and
had significantly lower locomotion scores at 6 months.149
The issue here is adequate pain control and the importance of implant
stability. If an implant is unstable in the first 6 weeks after
surgery, pain and lack of mobility may affect long-term functional
recovery.
Hip abductors exercises bilaterally in conjunction with proper balance
and gait training are required. Resist the abandonment of crutches or
walker until normal gait is restored. Patients must be counseled to
report any increased swelling or respiratory distress as an emergency
because of the high risk of thromboembolic disease. On discharge,
prescribe vitamin D (minimum of 1000 IU daily); if the patient’s
vitamin D level is low, consider prescribing 50,000 IU weekly for 12
weeks. Fall prevention education and safe home checks should be
explained to the patient’s family or social support group. The patient
is re-evaluated with exam and radiographs at 2 weeks and then monthly
thereafter until fracture healing is documented and she or he has
maximized amublatory capabilities, usually by 6 months after injury.
plan to indentify secondary causes of osteoporosis, obtain bone density
testing, and initiate osteoporois pharmacotherapy if appropriate. The
FRAX calculator (http://www.shef.ac.uk/FRAX/) is a free service for
patients not on osteoporosis treatment and is helpful for patient
education and risk assessment.111
The AAOS, AOA, and Osteoporosis Foundation encourage the use of
fragility fracture and osteoporosis for diagnosis in the discharge
summary. Orthopaedic surgeons must treat the entire patient with the
same diligence we prescribe a rehabilitation program after any sports
injury, reconstructive surgery, or hand procedure.32
years or older found a rate of 1737 (19%) with postoperative medical
complications in 8930 patients.129
Interestingly, 81% of these patients had no medical complications after
hip fracture repair. Cardiac and pulmonary complications were most
frequent (8% and 4% of patients, respectively). Other complications
were gastrointestinal tract bleeding (2%), combined cardiopulmonary
complications (1%), venous thromboembolism (1%), and transient ischemic
attack or stroke (1%). Renal failure and septic shock were rare. After
the index complication, 416 patients had 587 additional complications.
Mortality was similar for serious cardiac or pulmonary complications
(30 day, 22% and 17%, respectively; 1 year, 36% and 44%, respectively)
and highest for patients with multiple complications (30 day, 29% to
38%; 1 year: 43% to 62%).129
imminent mortality, especially if they have had loved ones’ who have
died from hip fractures in the past. They have questions regarding
their ability to walk again or be independent enough to return to their
own home. Most surgeons consider union of any type to be a successful
treatment, whereas from a patient’s perspective it is a return to the
previous level of functional activity and home environment that is
desired.
recovery, and this is best addressed by the patient’s ability to trust
in the injured extremities’ support.17,159
Patients with improved mobility early in the postoperative period
develop better functional abilities at the 3- and 6-month periods.201
Ziden et al. reported multidimensional and dramatic changes in
patients’ life situations, including existential thoughts and
reappraisal of the years of life that remained. The results indicate
that the fracture seemed not only to break the bone, but also to cause
social and existential cracks leading some patients to a positive
socially interactive lifestyle and others to a depressive, defeatist
mentality with withdrawal and a diminished zest for life.223
controversy about proper prophylactic management and postoperative
therapy, considering the added cost and medical surveillance required
and the concern for major hemorrhagic postoperative events.6,71,86,88
Complicating management in the hip fracture patient population is the
preoperative frequency of platelet inhibitors and anticoagulants for
unrelated medical problems. Recommendations from the American College
of Chest Physicians, American Academy of Orthopaedic Surgeons, and
governmental agencies are not in agreement as to the best strategy.
Options include pentasaccharides, low-molecular-weight heparins,
adjusted dose warfarin, mechanical compression, and aspirin.207,216 Prophylaxis has been recommended for 4 to 6 weeks postoperatively because of reports of late pulmonary embolism and DVT.
thromboembolic event in the no treatment group was 12%, and in the
mechanical compression group was 4%.58
In 1984 Alho reported a prospective study for the expenditure of
hospital resources and the incidence of clinical venous thromboembolism
under prophylaxis with heparin, aspirin, or warfarin. Thromboembolic
complications were more frequent (P < 0.02) and hospital
costs clearly higher in the low-dose heparin-treated patient group
compared with the aspirin and warfarin groups. There were no distinct
differences between aspirin- and warfarintreated patients either in
results or costs. Nonetheless, carefully monitored treatment with
warfarin with Thrombotest always less than 0.20 appeared to be the most
effective prophylaxis in patients with hip fractures. They use aspirin
as a general prophylaxis in orthopaedic patients, and warfarin in
patients with established risk of thromboembolic complications.5
|
TABLE 48-3 Pearls and Pitfalls of Treatment of Pertrochanteric Fractures
|
||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
thromboprophylaxis with aspirin, and dextran 40 was compared in a
prospective review of 530 geriatric hip fracture patients treated
surgically. All patients were also treated with early mobilization with
weight-bearing as tolerated and above-knee elastic stockings. The
incidence of DVT (0.5%) and PE (2.6%) in the aspirin group was
essentially the same as the incidence of DVT (0.3%) and PE (2.4%) in
the dextran group. Neither mortality nor infection rates were
different. They reported the average cost for aspirin at $1.79 per
patient. The safety, cost, and ease of administration of aspirin may
make its use more desirable in their opinion.57
With this protocol they reported a DVT rate of 0.5% to 1.7%, pulmonary
embolism 0% to 2.0%, fatal pulmonary embolism 0% to 0.5%, and no
difference with regard to the effectiveness of each pharmacologic
treatment. Wound hematoma complications were increased with enoxaparin
(3.8%) versus aspirin (2.4%) and Dextran 40 (1.6%).
as well tolerated, and compared with placebo, it significantly reduced
delayed venous thromboembolism events from 35% to 1.4%. Based on these
findings, a 4-week fondaparinux treatment may become the standard
thromboprophylaxis after hip fracture surgery.55
to 1997 reflected significant increases in pharmaceutical
thromboembolic prophylaxis (from 45% to 81%) and early mobilization
(from 56% to 70%). There were reduced levels of pneumonia,
wound
infection, pressure sores, and fatal pulmonary embolism, but no change
was recorded in 3-month functional outcomes or mortality.62
anticoagulation, but 17% of patients are at risk of hemorrhage, and
some surgeons advocate mechanical methods as a safer option in this
population.174
internal fixation is reported to affect 1% of older patients and is
usually treated with total hip replacement. In young patients it is
treated with osteotomy, bone grafting, and implant revision (Fig 48-31).
Vidyadhara et al. reported on using closing lateral wedge valgus
intertrochanteric osteotomy in addition to dynamic hip screw
osteosynthesis in the successful management of seven patients with
varus trochanteric nonunion. Average preoperative coxa vara of 94
degrees (range, 85 to 104 degrees) had improved to a femoral neck shaft
angle of 139 degrees (range, 134 to 145 degrees) on postoperative
radiographs. All fractures and osteotomies had healed. The Harris hip
score improved from 34 (range, 22 to 47) to 89 (range, 83 to 95) at an
average of 11 months follow-up (range, 7 to 13 months).210 Other reports have high success rates with osteotomy and ORIF (82% success).137,185
Hadikewych et al. reported a 95% union rate with a combination of
techniques, including blade plate, DHS, DCS, and Zickel devices. They
added autogenous iliac bone graft in 17 cases versus three allografts;
19/20 nonunions healed with this strategy. Talmo has reported success
with total hip arthroplasty, with a Harris hip score average of 86 at
30 months in 10 patients (Figure 48-32).83,84,202
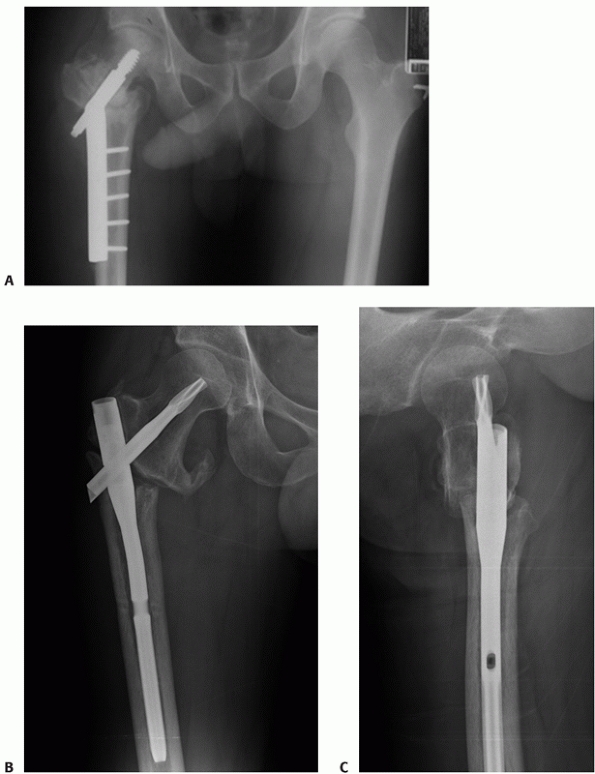 |
|
FIGURE 48-31 A. Nonunion of a 31A3 fracture with CHS displaying maximal shortening with medialization of the distal shaft fragment. B. Distraction nonunion with TFN. Repair requires open reduction, grafting, and compression fixation. C. TFN distraction nonunion on lateral radiograph.
|
approximate 5% of cases usually from a combination of implant fatigue
failure, shaft fixation failure with broken screws, femoral head medial
penetration, screw cutout, and disassembly of the device components.
With today’s stringent requirements for manufacturing and quality
control, manufacturing etiology for failure is extremely rare. Fatigue
failures associated with nonunion are most common.
characteristics of 27 patients with a trochanteric fracture treated
with a sliding hip screw in which fixation failure occurred, and
compared
them
with 74 patients having uneventful fracture union. Femoral
medialization was more common in specific fracture types, particularly
if there was comminution of the lateral femoral cortex at the site of
insertion of the lag screw. Femoral medialization was strongly
associated with fixation failure, with a sevenfold increase in the risk
of failure if medialization at more than one third occurred. This
author suggests that implants preventing femoral medialization in
specific types of trochanteric fracture merit further evaluation.163
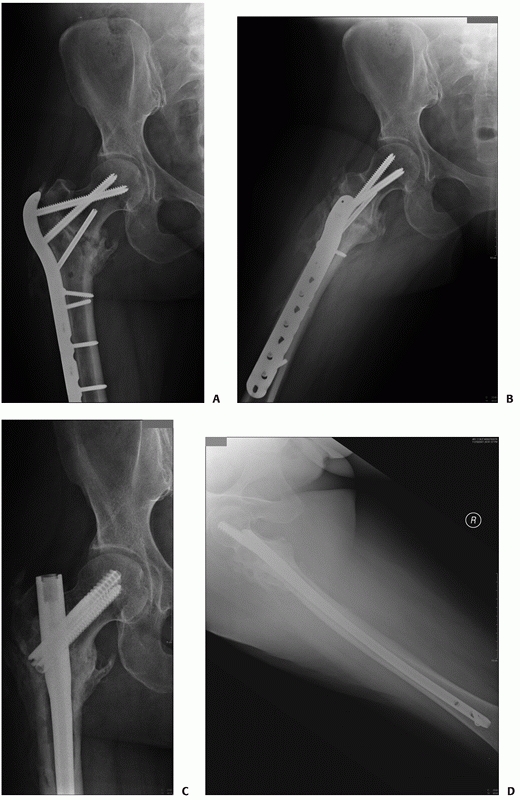 |
|
FIGURE 48-32 A. Nonunion with locking plate. Note deformation of screws. B. Locking plate nonunion, lateral. C. Revision with open reduction, inductive grafting, and compression with InterTAN nail. D. InterTAN revision and union shown on lateral radiograph.
|
complications manifested by collapse of the screw and varus migration
of the femoral head construct with final cutout failure in the worst
cases of screw and nail constructs. This occurs to a small degree in
all cases, as the sliding impaction was designed to minimize
catastrophic cutout, but frequently is compounded by lack of a stable
reduction. A center-center position of single screw devices minimizes
cutout as reported by many authors, but this is reduced to a
mathematical equation as the tip apex distance, as reported by
Baumgaertner16 (Figure 48-33).
that may occur around the lateral wall, the region of bone at the end
of a nail or side plate, or distally in the femur. These are problems
with tactics as the issue arises as to removal of the previous implant
or addition of further fixation. Gotfried and Palm et al. have
identified the seriousness of the lateral wall fracture, which
frequently occurs around a compression hip screw. These difficult
fractures require reattachment of the greater trochanter with buttress
plate techniques.80
Fractures distal to plates may be treated with retrograde nails with
removal of the inferior two to three screws of the sideplate to ensure
overlap of the fixation by the nail (Figure 48-34).
Periprosthetic fractures were more common with the first-generation
short trochanteric gamma nails, probably because of the large distal
diameter (up to 16 mm), larger proximal bend, and large distal locking
screws. Periprosthetic fracture rates as high as 17% have been
reported. With the newer design there has been a substantial drop in
periprosthetic femur fractures, but it remains a concern. Fractures
distal to short nails require revision to longer nails or locking
plates if the greater trochanter is also involved.
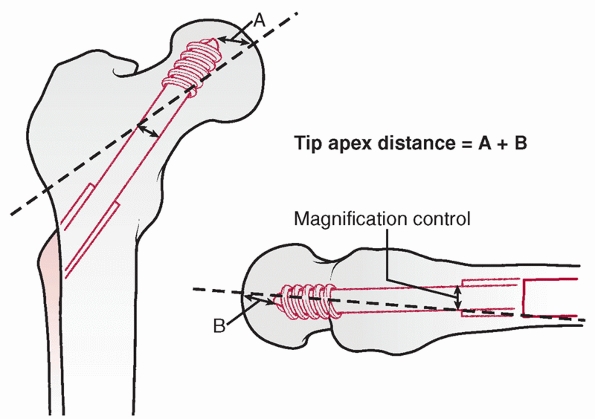 |
|
FIGURE 48-33
The tip-apex distance (TAD), expressed in millimeters, is the sum of the distances from the tip of the lag screw to the apex of the femoral head on both the AP and lateral radiographic views. |
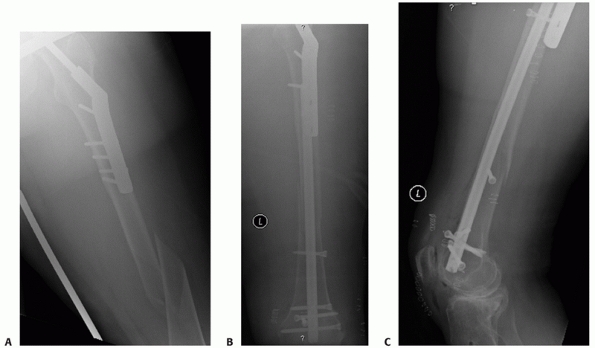 |
|
FIGURE 48-34 A. Peri-implant fracture of the femur below a CHS. Associated osteoarthritis of knee and osteoporosis in community ambulatory. B.
Treatment with retrograde locking nail overlapping sideplate by removal of distal plate screws percutaneously. Blocking screws are used to enhance construct stability and alignment. C. Lateral radiograph showing retrograde locking nail with blocking screws and overlap with plate. |
fractures relate to premature death, averaging 20% at 1 year, permanent
disability of 30%, inability to ambulate independently in 40%, and loss
of at least one activity of independent daily living (i.e., driving or
grocery shopping) in 80% of treated patients.42
trochanteric fractures treated with a sliding-screw technique and
followed clinically and radiographically for at least 1 year. Of 351
patients admitted from their homes, 209 (60%) were discharged to their
homes after an average of 18 days in the hospital. During the first
year another 61 (17%) patients returned home after rehabilitation in a
geriatric ward. Of 446 patients walking without support or with one
cane before surgery, 360 (80%) had regained the same mobility after 1
year. The 1-year mortality rate was 18%, whereas the 10-year rate was
74%. Forty-five (7.4%) were reoperated, 17 because of technical
complications, three because of infection, and three because of
nonunion. The deep infection rate was nine of 339 (2.7%) before and two
of 268 (0.8%) after the introduction of antibiotic prophylaxis.128
The reoperation rate was 3%. At the final follow-up, 81% of the
patients reported no or only limited pain at the hip, 55% had regained
their
prefracture walking ability, and 66% had attained their prefracture level of ADL function.
evaluated the associated excess mortality with a large nursing home
population in Germany. The crude incidence rates of admission to a
nursing home were 50.8/1000 person-years in women and 32.7/1000
person-years in men. The incidence rates increased with increasing age
categories and were highest in the first months after admission to the
nursing home. Mortality in patients with a hip fracture was increased
(women: hazard rate ratio for the first 3 months after fracture, 1.7
and men the hazard ratio, 2.14) but excess mortality was limited to the
first months after injury.
fast-track treatment and care program for hip fracture to optimize
patient care has been reported with components such as a switch from
systemic opiates to a local femoral nerve catheter block; an earlier
assessment by the anesthesiologist; and a moresystematic approach to
nutrition, fluid, and oxygen therapy, and urinary retention compared
with standard hospital care. In the intervention group, the rate of any
in-hospital postoperative complication was reduced from 33% to 20%
(odds ratio, 0.61, 95%; confidence interval; 0.4 to 0.9; P = 0.002). Rates of confusion (P = 0.02), pneumonia (P = 0.03), and urinary tract infection (P
= 0.001) were lower in the intervention group than the control group,
and length of stay was 15.8 days in the control group versus 9.7 days
in the intervention group. For community dwellers, 12-month mortality
was 23% in the control group. This study supports the concept of hip
fracture program to reduce the rate of in-hospital postoperative
complications and mortality. Randomized clinical trials are required to
validate and elucidate the elements of the program that have the
greatest effect on clinical outcomes and mortality.172
and is minimized by preoperative antibiotics, usually a cephalosporin
class drug. In immunocompromised and malnourished patients, standard
care involves isolation and sensitivity testing of the causative
bacteria and appropriate intravenous antibiotics in consultation with
an infectious disease specialist and standard débridement and
irrigation for wound care. If the implant is stable it should be
retained. A resection arthroplasty is rarely required.89
In 2008 Edwards et al. reported a 1.2% rate of deep wound infection and
1.1% superficial wound infection in a series of more than 3000 cases.
Fifty-seven of eighty infections (71.3%) were caused by Staphylococcus aureus
and 39 (48.8%) by MRSA (multiple organisms). No statistically
significant preoperative risk factors were detected. Length of stay,
cost of treatment, and predischarge mortality all significantly
increased with deep wound infection. The 1-year mortality in the total
series was 30%, and this increased to 50% in those who developed an
infection (P < 0.001). A deep infection
resulted in doubled operative costs, tripled investigation costs, and
quadrupled ward costs. MRSA infection increased costs, length of stay,
and predischarge mortality compared with non-MRSA infection.50
They recommended vigilance with a high index of suspicion for any signs
of wound inflammation or drainage. Oral antibiotics for 7 to 10 days
are suggested if the infection is superficial. Urgent formal surgical
débridement and irrigation are required for deep infection. Retain
stable implants. Antibiotic beads may be considered for defect
management. Wu et al. reviewed their experience with 23 pertrochanteric
osteomyelitis cases and presented a two-stage treatment protocol. They
used an external skeletal fixator or Buck’s traction after radical
débridement in the first stage and reconstruction in the second stage.
Only 12 of the 23 patients (52%) were successfully managed, and
infection recurred in four patients (17.4%) at final follow-up. The use
of external skeletal fixation was not recommended for managing
pertrochanteric osteomyelitis. Success using a two-stage protocol was
difficult to achieve.221
factor for recovery. Because of the avoidance of sunlight for fear of
skin cancer and the lack of vitamin D in the modern diet, vitamin D
deficiency has re-emerged as a health epidemic.94
Vitamin D deficiency causes muscle weakness. Skeletal muscles have a
vitamin D receptor and may require vitamin D for maximum function.
Performance speed and proximal muscle strength were markedly improved
when 25-hydroxyvitamin D levels increased from 4 to 16 ng/mL and
continued to improve as the levels increased to more than 40 ng/mL.21
A meta-analysis of five randomized clinical trials (with a total of
1237 subjects) revealed that increased vitamin D intake reduced the
risk of falls by 22%, compared with only calcium or placebo. The same
meta-analysis examined the frequency of falls and suggested that 400 IU
of vitamin D3 per day was not effective in preventing falls, whereas 800 IU of vitamin D3 per day plus calcium reduced the risk of falls.21 In a randomized controlled trial conducted over a 5-month period, nursing home residents receiving 800 IU of vitamin D2 per day plus calcium had a 72% reduction in the risk of falls as compared with the placebo group.29
surgical treatment in the mid-twentieth century but has remained stable
at 25% to 30% since then. In 2009 Abrahamsen showed that patients
experiencing hip fracture after low-impact trauma are at considerable
excess risk for death compared with nonfracture community control
populations. Hip fracture is associated with excess mortality (over and
above mortality rates in nonfracture community control populations)
during the first year after fracture, with studies suggesting a range
of 8.4% to 36%. This initial risk for mortality after hip fracture was
at least double that for the age-matched control population, became
less pronounced with advancing age, was higher among men than women
regardless of age, was highest in the days and weeks after the index
fracture, and remained elevated for months and perhaps even years after
the index fracture. These observations show that patients are at
increased risk for premature death for many years after a
fragility-related hip fracture and highlight the need to identify those
patients who are candidates for interventions to reduce their risk.1
mortality from the Scottish Hip Fracture Audit Database. Patients in
the 50-to 64-year group had significantly better outcome measures after
surgery for hip fracture in terms of survival and function. The
differences exist even after controlling for differences in patient
case-mix variables. Holt et al. developed a predictive formula
for
estimation of mortality at 30 and 120 days depending on age, ASA score,
gender, prefracture residence, prefracture mobility, and type of
fracture (Table 48-4).
|
TABLE 48-4 Predictive Mortality Variables
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
residence) + B(age) + B(sex) + B(type of fracture) + B(prefracture
mobility)
fracture patient aged 90 or over; ASA = 3; from a care home, assuming
other base characteristics (male, intracapsular fracture, walked
without aids before fracture) = 1/1 + e – (-4.79 + 0.80 + 0.53 + 1.96)
= 18.2%. This formula applies to Intracapsular, extracapsular,
subtrochanteric and pathologic fractures. Mortality in those more than
90 years old averaged 50% at 120 days.96
proximal femur were identified. The principal causes of death after hip
fracture were bronchopneumonia, cardiac failure, myocardial infarction,
and pulmonary embolism. Surgical intervention within 24 hours of injury
significantly reduced death from bronchopneumonia and pulmonary
embolism. Early mobilization reduced death from bronchopneumonia.174
to analyze functional recovery” to one in which we analyze and maximize
functional recovery. It is interesting that the Harris Hip Score has
been well validated as a hip quality measure. Recently, several authors
have reported results with this measure. Moroni et al. reported Harris
Hip Scores of 60/100 for external fixation and standard compression hip
screws, with increases to 70/100 with HA coated compression hip screw
devices. Ruecker et al. reported average Harris hip scores in the
78/100 range for preoperative function, and recovery to 70/100 with an
integrated screw nail device.
injury the surgeon treatment should first preserve life, second save
the limb, and finally maximize functional recovery. There is a
dichotomy of opinion regarding a surgeon’s and a patient’s perspective
after a broken hip. Globally surgeons feel that most surgeries are
equivalent and that patients are expected to have a lower demand and
lower mortality after surgery, and frequently their focus is on the
time of the surgical procedure and union of any type rather than the
total care of the patient. We have now arrived in a new century in
which functional recovery in previously independent community
ambulators is expected if not demanded, and the satisfaction of a
united fracture from the mid-twentieth century with reduced mortality
is not enough.
pertrochanteric fractures relates to appreciation of the relative
instability of the fracture construct with a single cephalic component
with osteoporotic bone stock, unstable fracture reductions, or
combinations thereof. It is appreciated that even with optimal screw
purchase in the correct position of the femoral head, any rotational
stability will lead to progressive collapse and progressive incremental
instability until the fracture heals in a varus position, the femoral
head motion results in femoral neck erosion and collapse until the
sliding screw reaches maximal collapse with resultant implant failure,
or cutout occurs. This is certainly more common in severe osteoporotic
patients and those with unstable reductions or comminuted fractures.
Uncontrolled dynamization has come to be appreciated as a cause for
bony erosion and progressive continuing collapse. This frequently
results in excessive dynamization, which weakens the abductors and
shortens the extremity and makes it more likely the patient will have
diminished function. The Baby Boomer generation patient with a hip
fracture expects a functional result equivalent to their friends’
experience with a total hip replacement.
ignored since Holt’s concept in 1963, has resurfaced with biomechanical
and clinical validation of the importance of rotational stability. New
techniques and devices are required to overcome the status quo.
fracture and the “next fracture.” Who can we save? Who can benefit from
prophylactic medications or even surgery? We know the major risk
factors for geriatric fractures, which include prior fragility
fracture, increased age, low bone mineral density, low body weight,
family history of osteoporotic fracture, glucocorticoid use, secondary
osteoporosis, liver and kidney disease, Crohn’s disease, rheumatoid
arthritis, hyperthyroid disease, antiepileptic medications, primary
hyperparathyroidism, and systemic inflammatory disease and smoking
tobacco products and now vitamin D.35,68
documented the drugs alendronate and risedronate as effective in
decreasing the risk of hip fractures. The AOA “own the bone” initiative
notes that patients with a hip fracture have at least one treatable
secondary cause of osteoporosis, usually low vitamin D (osteomalacia).
Similarly, 40% of women and more than 60% of men with osteoporosis have
a secondary condition and a treatable cause of their low bone density.
They recommend that we should develop admission and discharge fracture
care checklists that include the following recommendations:
-
Prescribe calcium (1200 mg daily).
-
Prescribe vitamin D (minimum of 1000 IU
daily). If the patient’s vitamin D level is low, consider prescribing
50,000 IU weekly for 12 weeks. -
Refer to physical medicine or physical therapy for fallprevention education.
-
Ask the family or friends to perform a home-safety check.206
for better instruments and implants. Moroni et al. have been
instrumental in the progress of HA-coated implants and the bone
reaction to these coatings.146,147,148
These types of devices have garnered little acceptance in the United
States as of yet. The application of bone in-growth coatings will
parallel the addition of new studies and strategies to convince
surgeons of their removal potential. The use of alendronate to augment
the ingrowth of HA components is also under study for the osteoporotic
patient.145
phosphate cements has been attractive since first described by Bartucci
et al. in 1985.15 The problem has
been the inability to demonstrate a functional improvement with the
increased stability hypothesized. In Bartucci’s experience patients
with PMMA had worse function at follow-up. The calcium phosphate
cements have also been tried but with the result in the most recent
meta-analysis primarily of decreased pain at the hip.9
It may be that the technique of application is incorrect. Recently the
trend has been to apply the cement in the femoral head and avoid the
fracture zone.8,37,54,74
As new techniques of delivery and cement composition are developed,
perhaps the addition of cements may prove more helpful in osteoporotic
fractures.
B, van Staa T, Ariely R, et al. Excess mortality following hip
fracture: a systematic epidemiological review. Osteoporos Int
2009;15:767-778.
B, Vestergaard P. Declining incidence of hip fractures and the extent
of use of antiosteoporotic therapy in Denmark 1997-2006. Osteoporos Int
2009.
CI, Robinson CM, Court-Brown CM, et al. Prospective randomized
controlled trial of an intramedullary nail versus dynamic screw and
plate for intertrochanteric fractures of the femur. J Orthop Trauma
2001;15(6):394-400.
AWK, Ostlere S. The MRI diagnosis and management of incomplete
intertrochanteric fractures of the femur. J Bone Joint Surg Br
2005;87(9):1253-1255.
A, Stangeland L, Rottingen J, Wiig JN. Prophylaxis of venous
thromboembolism by aspirin, warfarin, and heparin in patients with hip
fracture. A prospective clinical study with cost-benefit analysis. Ann
Chir Gynaecol 1984;73(4):225-228.
S, Buch K. Postdischarge symptomatic thromboembolic events in hip
fracture patients. Ann R Coll Surg Engl 2007;89(5):517-520.
JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip
fractures: changing pattern of practice. A review of the American Board
of Orthopaedic Surgery Database. J Bone Joint Surg Am
2008;90(4):700-707.
P, Rapp S, Claes L. A modified hip screw incorporating injected cement
for the fixation of osteoporotic trochanteric fractures. J Orthop
Trauma 2002;16(5):311-316.
SS, Zlowodzki M, Lelwica A, et al. The use of calcium phosphate bone
cement in fracture treatment. A meta-analysis of randomized trials. J
Bone Joint Surg Am 2008;90(6):1186-1196.
MS, Emms N, Thomas G. Proximal femoral nail failures in extracapsular
fractures of the hip. J Orthop Surg (Hong Kong) 2008;16(2):146-149.
JW, Ferreira CD, Freitas AA, Farah S. External fixation of
intertrochanteric fractures of the femur. Int Orthop 1995;19(4):217-219.
J, Fric V, Skala-Rosenbaum J, Dousa P. Avascular necrosis of the
femoral head in pertrochanteric fractures: a report of 8 cases and a
review of the literature. J Orthop Trauma 2007;21(4):229-236.
J, Sprindrich J, Skala-Rosenbaum J, et al. [Diagnosing occult
pertrochanteric fractures of proximal femur with MRI]. Rozhl Chir
2007;86(7):379-383.
E, Gonzalez M, Cooperman D, et al. The effect of adjunctive
methylmethacrylate on failures of fixation and function in patients
with intertrochanteric fractures and osteoporosis. J Bone Joint Surg Am
1985;67(7):1094-1107.
MR, Curtin SL, Lindskog DM, et al. The value of the tip-apex distance
in predicting failure of fixation of peritrochanteric fractures of the
hip. J Bone Joint Surg Am 1995;77(7):1058-1064.
C, Fleischer S, Hack A, et al. [Disabilities and handicaps due to hip
fractures in the elderly]. Z Gerontol Geriatr 1999;32(5):312-317.
JA, Weiner LS, Strauss E, et al. Collapse of intertrochanteric hip
fractures fixed with sliding screws. Orthop Rev 1994;Suppl:30-37.
KR, Hanna J, Smith TM, et al. Acute hip arthroplasty for the treatment
of intertrochanteric fractures in the elderly. J Surg Oerthop Adv
2006;14(4):185-189.
HAGE, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal
serum concentrations of 25-hydroxyvitamin D for multiple health
outcomes. Am J Clin Nutr 2006;84:18-28.
GA, Lizerbram EK, Crues JV 3rd. MR imaging in evaluation of suspected
hip fracture: frequency of unsuspected bone and soft-tissue injury.
Radiology 1995;197(1): 263-267.
S, Laan RF, Barton IP, et al. Effect of osteoporosis treatments on risk
of nonvertebral fractures: review and meta-analysis of
intention-to-treat studies. Osteoporos Int 2005;16(10):1291-1298.
A. The blood supply of the femoral neck and head in relation to the
damaging effects of nails and screws. J Bone Joint Surg Br
1960;42-B(4):794-801.
KCTC, Weinberg J, Bischoff-Ferrari HA, et al. A higher dose of vitamin
D reduces the risk of falls in nursing home residents: a randomized,
multiple-dose study. J Amer Geriatr Soc 2007;55(2):234-239.
AJJ A, Babst R. The PFNA proximal femur nail in treatment of unstable
proximal femur fractures—3 cases of postoperative perforation of the
helical blade into the hip joint. J Orthop Trauma 2008;22(10):731-736.
O, Brandi ML, Burlet N, et al. Postfracture management of patients with
hip fracture: a perspective. Curr Med Res Opin 2008;24(10):2841-2851.
JB. The anterior and medial reduction of intertrochanteric fractures: a
simple method to obtain a stable reduction. J Orthop Trauma
2007;21(7):485-489.
JA, Lacroix AZ, Wu L, et al. Serum 25-hydroxyvitamin D concentrations
and risk for hip fractures. Ann Intern Med 2008;149(4):242-250.
MA, Parker MJ. Fixed nail plates versus sliding hip systems for the
treatment of trochanteric femoral fractures: a meta analysis of 14
studies. Injury 1999;30(3): 157-163.
J, Koval KJ, Kummer FJ, Zukerman JD. Cement augmentation of
intertrochanteric fracture fixation: a cadaver comparison of 2
techniques. Acta Orthop Scand 1996; 67(2):153-157.
M, Bosworth DM, Thompson FR, et al. A 10-year analysis of
intertrochanteric fractures of the femur. J Bone Joint Surg Am
1959;41(8):1399-1408.
C. The crippling consequences of fractures and their impact on quality
of life. Am J Med 1997;103(2A):12S-17S; discussion 17S-19S.
T, Sher J, Horsman A, et al. Intertrochanteric femoral fractures.
Mechanical failure after internal fixation. J Bone Joint Surg Br
1990;72-B(1):26-31.
R, Greene D, Schelkun SR, Williams K. Osteoporosis disease management:
the role of the orthopaedic surgeon. J Bone Joint Surg Am
2008;90(Suppl4):188-194.
ARA, Paiement G, Newman N, et al. Unstable intertrochanteric fracture
of the femur. A prospective randomised study comparing anatomical
reduction and medial displacement osteotomy. J Bone Joint Surg Br
1993;75(3):445-447.
WW. False aneurysm of the profunda femoris artery following internal
fixation of an intertrochanteric femoral fracture. Injury
1978;9(3):249-251.
C, Counsell A, Boulton C, et al. Early infection after hip fracture
surgery: risk factors, costs, and outcome. J Bone Joint Surg Br
2008;90(6):770-777.
GSTO, Pomerat CM. The influence of the contact-compression factor on
osteogenesis in surgical fractures. J Bone Joint Surg Am
1949;31(4):694-716.
W, Miedel R, Ponzer S, et al. Quality of life after a stable
trochanteric fracture —a prospective cohort study on 148 patients. J
Orthop Trauma 2009;23(1):39-44.
WKTC, Larsson S, Ragnarsson B, et al. Functional outcome in treatment
of unstable trochanteric and subtrochanteric fractures with the
proximal femoral nail and the Medoff sliding plate. J Orthop Trauma
2007;21(1):18-25.
S, Frankenburg E, Goulet J, et al. Biomechanical evaluation of calcium
phosphate cement-augmented fixation of unstable intertrochanteric
fractures. J Orthop Trauma 2000;14(6):386-393.
BI. Improvements in the prevention of postoperative venous
thromboembolism in hip fracture patients. Orthopedics 2003;26(8
Suppl):s851-858.
DS, Zuckerman JD, Walters I, et al. Clinical efficacy of aspirin and
dextran for thromboprophylaxis in geriatric hip fracture patients. J
Orthop Trauma 1993;7(1): 1-5.
CG, Blachut PA, Salvian AJ, et al. Effectiveness of pneumatic leg
compression devices for the prevention of thromboembolic disease in
orthopaedic trauma patients: a prospective, randomized study of
compression alone versus no prophylaxis. J Orthop Trauma Feb
1995;9(1):1-7.
F, Kfuri M Jr, Paccola CA. Intramedullary fixation of pertrochanteric
hip fractures with the short AO-ASIF proximal femoral nail. Arch Orthop
Trauma Surg 2004;124(1):31-37.
JC. Trochanteric fractures of the femur treated by the vitallium
mclaughlin nail and plate. J Bone Joint Surg Br 1958;40-B(4):684-693.
MR, Heppenstall RB, Friedenberg ZB, et al. A prospective assessment of
nutritional status and complications in patients with fractures of the
hip. J Orthop Trauma 1990;4(1):49-57.
C, Todd C, Camilleri-Ferrante C, et al. Quality improvement for
patients with hip fracture: experience from a multisite audit. Qual Saf
Health Care 2002;11(3): 239-245.
W, Jonsson A, Buhren V, et al. Classifying intertrochanteric fractures
of the proximal femur: does experience matter? Med Princ Pract
2007;16(3):198-202.
MJBSM, Kopjar B, Helfet DL, et al. Radiographic outcomes of
intertrochanteric hip fractures treated with the trochanteric fixation
nail. Injury 2007;38(10):1189-1196.
MGR, Simpson AH. How effective are osteotomies for unstable
intertrochanteric fractures? J Bone Joint Surg Br Sep
1994;76(5):789-792.
S, Heaney RP, Boonen S, et al. Vitamin D inadequacy among
postmenopausal women: a systematic review. QJM 2005;98(9):667-676.
E, Ganz K, Krugel N, et al. Anatomy of the medial femoral circumflex
artery and its surgical implications. J Bone Joint Surg Br
2000;82(5):679-683.
F, Zimmermann-Stenzel M, Heisel C, et al. Trochanteric fractures in the
elderly: the influence of primary hip arthroplasty on 1-year mortality.
Arch Orthop Trauma Surg 2007;127(10):959-966.
JJ, Chin PC, Rafiei P, et al. Intertrochanteric hip fractures treated
with the trochanteric fixation nail and sliding hip screw. J Surg
Orthop Adv 2007;16(2):62-66.
F. A special stud-bolt screw for fixation of fractures of the neck of
the femur. J Bone Joint Surg Am 1940;22(3):683-697.
SB, Bauer TW, Carter D, et al. Norian SRS cement augmentation in hip
fracture treatment. Laboratory and initial clinical results. Clin
Orthop 1998(348): 42-50.
Y. The lateral trochanteric wall: a key element in the reconstruction
of unstable pertrochanteric hip fractures. Clin Orthop Relat Res
2004(425):82-86.
Y, Cohen B, Rotem A. Biomechanical evaluation of the percutaneous
compression plating system for hip fractures. J Orthop Trauma
2002;16(9):644-650.
Y, Frish E, Mendes DG, et al. Intertrochanteric fractures in high-risk
geriatric patients treated by external fixation. Orthopedics
1985;8(6):769-774.
RK, Sangwan K, Kamboj P, et al. Unstable trochanteric fractures: the
role of lateral wall reconstruction. Int Orthop 2009. (Epub ahead of
print)
P, Casteleyn PP, De Boeck H, et al. Treatment of unstable
intertrochanteric and subtrochanteric fractures in elderly patients.
Primary bipolar arthroplasty compared with internal fixation. J Bone
Joint Surg Am 1989;71(8):1214-1225.
H, Furukawa K, Fujiwara S, et al. Recent trends in the incidence and
lifetime risk of hip fracture in Tottori, Japan. Osteoporos Int
2009;20(4):543-548.
GJ, Berry DJ. Hip arthroplasty for salvage of failed treatment of
intertrochanteric hip fractures. J Bone Joint Surg Am
2003;85-A(5):899-904.
GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the
intertrochanteric region of the femur. J Bone Joint Surg Am
2001;83-A(5):643-650.
HH, Farrar MJ, McBirnie J, et al. Heparin, low-molecular-weight heparin
and physical methods for preventing deep vein thrombosis and pulmonary
embolism following surgery for hip fractures. Cochrane Database Syst
Rev 2000(2):CD000305.
FG Jr, Nelson CL, Puskarich-May CL. Effect of delayed admission to the
hospital on the preoperative prevalence of deep-vein thrombosis
associated with fractures about the hip. J Bone Joint Surg Am
1996;78(4):581-583.
T, Partanen J, Ristiniemi J, et al. Evaluation of 238 consecutive
patients with the extended data set of the Standardised Audit for Hip
Fractures in Europe (SAHFE). Disabil Rehabil 2005;27(18-19):1107-1115.
E Jr. Hip fractures in the trochanteric region: treatment with a strong
nail and early weight-bearing: a report of 100 cases. J Bone Joint Surg
Am 1963;45(4):687-705.
G, Smith R, Duncan K, et al. Outcome after surgery for the treatment of
hip fracture in the extremely elderly. J Bone Joint Surg Am
2008;90(9):1899-1905.
GK, Browner BD, Cole JD, et al. Initial experience with a second
generation locking femoral nail: the Russell-Taylor reconstruction
nail. Contemp Orthop 1991; 23(3):199-208.
JA, Parker MJ. Fractures of the hip: does the type of fall really
affect the site of fracture? Injury 1998;29(8):585-587.
M, Barwick C, Sinha AK, et al. Is magnetic resonance imaging (MRI)
necessary to exclude occult hip fracture? Injury 2007;38(10):1204-1208.
LC, Lo WH, Chen WM, et al. Intertrochanteric fractures in adults
younger than 40 years of age. Arch Orthop Trauma Surg
2001;121(3):123-126.
K, Ishii Y, Yagisawa K, et al. Postoperative ambulatory level after hip
fracture in the elderly predicts survival rate. Arch Orthop Trauma Surg
2000;120:369-371.
JV, Smith DK, Aufdemorte TB, et al. Anatomic significance of magnetic
resonance imaging findings in hip fracture. Clin Orthop Relat Res
1996(332):209-214.
GK, Gruson KI, Egol KA, et al. Thromboprophylaxis after hip fracture:
evaluation of 3 pharmacologic agents. Am J Orthop 2007;36(3):135-140.
GB, Ricci, WM. Stability of Intertrochanteric femur fracture fixation:
a critical ananlysis of extramedullary vs intramedullary implants and
the effect of lesser trochanteric involvement. 2009, in press.
H, Iqbal M, Mogallapu R, et al. Time to ambulation after hip fracture
surgery: relation to hospitalization outcomes. J Gerontol A Biol Sci
Med Sci 2003;58: 1042-1045.
SK, Kalra S, Khanna A, et al. Timing of surgery for hip fractures: A
systematic review of 52 published studies involving 291,413 patients.
Injury May 16 2009. (Epub ahead of print)
S-YK, Yong-Goo H. Cementless calcar-replacement hemiarthroplasty
compared with intramedullary fixation of unstable intertrochanteric
fractures. A prospective, randomized study. J Bone Joint Surg Am
2005;87(10):2186-2192.
KJ, Friend KD, Aharonoff GB, et al. Weight bearing after hip fracture:
a prospective series of 596 geriatric hip fracture patients. J Orthop
Trauma 1996;10(8):526-530.
KJ, Oh CK, Egol KA. Does a traction-internal rotation radiograph help
to better evaluate fractures of the proximal femur? Bull NYU Hosp Jt
Dis 2008;66(2):102-106.
PW, Breugem SJ, van Vugt AB. The Holland nail: a universal implant for
fractures of the proximal femur and the femoral shaft. Injury
2004;35(2):170-178.
RF, Ellis TJ, Templeman DC. Surgical treatment of intertrochanteric hip
fractures with associated femoral neck fractures using a sliding hip
screw. J Orthop Trauma 2005;19(1):1-4.
A. L’intervention opératoire dans les fractues recenes et anciennes
envisagée particuliérement au point de vue de l’osteosynthese avec la
description des plusiers techniques nouvelles. Paris; 1907.
B. Description of transfixion of femoral head by a transtrochanteric
nail (transl.). Verhand.d.deutsch Gesellsch. f. Chir. Kongress VII.
1878(1):92.
S, Friberg S, Hansson LI. Trochanteric fractures. Mobility,
complications, and mortality in 607 cases treated with the
sliding-screw technique. Clin Orthop Relat Res 1990(260):232-241.
VA, Hilsenbeck SG, Noveck H, et al. Medical complications and outcomes
after hip fracture repair. Arch Intern Med 2002;162(18):2053-2057.
KB, Eng AK, Chng SM, et al. Limited magnetic resonance imaging (MRI)
and the occult hip fracture. Ann Acad Med Singapore 2002;31(5):607-610.
NV, Fernando C, Elliott DS, et al. A prospective trial comparing the
Holland nail with the dynamic hip screw in the treatment of
intertrochanteric fractures of the hip. J Bone Joint Surg Br
2008;90(8):1073-1078.
O, Liebergall M, Mattan Y, et al. Early diagnosis of occult hip
fractures MRI versus CT scan. Injury 2005;36(6):788-792.
KC, Stigsson L, Hauggaard A. One-way compression along the femoral
shaft with the Medoff sliding plate. The first European experience of
104 intertrochanteric fractures with a 1-year follow-up. Acta Orthop
Scand 1995;66(4):343-346.
EM, Rand JA. Nonunion of intertrochanteric fractures of the femur
following open reduction and internal fixation. Results of second
attempts to gain union. Clin Orthop 1987(218):81-89.
DR, Maurer RC, Effeney D. Profunda femoris arterial laceration
secondary to intertrochanteric hip fracture fragments: a case report.
Clin Orthop 1981(161): 215-219.
JC. Displacement of trochanteric fractures and their influence on
reduction displacements of trochanteric fractures and their influence
on reduction. J Bone Joint Surg Br 1968;50-B(2):318-323.
RM. A new device for the fixation of unstable pertrochanteric fractures
of the hip. J Bone Joint Surg Am 1991;73(8):1192-1199.
LJ 3rd, Kearns AE, Atkinson EJ, et al. Secular trends in hip fracture
incidence and recurrence. Osteoporos Int 2009;20(5):687-694.
A, Faldini C, Hoang-Kim A, et al. Alendronate improves screw fixation
in osteoporotic bone. J Bone Joint Surg Am 2007;89(1):96-101.
A, Faldini C, Pegreffi F, et al. HA-coated screws decrease the
incidence of fixation failure in osteoporotic trochanteric fractures.
Clin Orthop Relat Res 2004(425): 87-92.
A, Faldini C, Pegreffi F, et al. Osteoporotic pertrochanteric fractures
can be successfully treated with external fixation. J Bone Joint Surg
Am 2005;87(Suppl 2): 42-51.
A, Faldini C, Pegreffi F, et al. Dynamic hip screw compared with
external fixation for treatment of osteoporotic pertrochanteric
fractures. A prospective, randomized study. J Bone Joint Surg Am
2005;87(4):753-759.
R, Magaziner J, McLaughlin M, et al. The impact of postoperative pain
on outcomes following hip fracture. J Gerontol A Biol Sci Med Sci
2003;103:303-311.
AM, Sherrington C, Lord SR, et al. Mobility training after hip
fracture: a randomised controlled trial. Age Ageing 2009;38(1):74-80.
PG, Geoghegan JG, Austin O, et al. Pseudoaneurysm of the profunda
femoris artery due to intertrochanteric fracture of the hip. Arch
Orthop Trauma Surg 1999; 119(1-2):117-118.
O, Ceder L, Hauggaard A. Femoral shortening in intertrochanteric
fractures. A comparison between the Medoff sliding plate and the
compression hip screw. J Bone Joint Surg Br 2001;83(4):572-578.
O, Ceder L, Lunsjo K, et al. Biaxial dynamization in unstable
intertrochanteric fractures. Good experience with a simplified Medoff
sliding plate in 94 patients. Acta Orthop Scand 1997;68(4):327-331.
Trauma Association Classification DaOCatACSC. Orthopaeidc Trauma
Association. Fracture and dislocation compendium, 2007. J Orthop Trauma
2007; 21(10):S31-32.
RFL. Penetration of the distal femoral anterior cortex during
intramedullary nailing for subtrochanteric fractures: a report of three
cases. J Orthop Trauma 2005; 19:656-660.
RFM, Marburger RA. A critical analysis of the eccentric starting point
for trochanteric intramedullary femoral nailing. J Orthop Trauma
2005;19:681-686.
VR, Banerjee S, Horan M, et al. Fear of falling more important than
pain and depression for functional recovery after surgery for hip
fracture in older people. Pshchol Med 2006;36(11):1635-1645.
J, Lindahl J, Savolainen V, et al. Femoral shaft medialisation and
neck-shaft angle in unstable pertrochanteric femoral fractures. Int
Orthop 2004;28(6):347-353.
SS, Mirza S, Bharadwaj G, et al. The percutaneous compression plate
versus the dynamic hip screw: a meta-analysis. Acta Orthop Belg
2008;74(1):38-48.
MJ. Trochanteric hip fractures. Fixation failure commoner with femoral
medialization, a comparison of 101 cases. Acta Orthop Scand
1996;67(4):329-332.
MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails
versus extramedullary implants for extracapsular hip fractures.
Cochrane Database Syst Rev 2000(2):CD000093.
MJ, Handoll HH. Replacement arthroplasty versus internal fixation for
extracapsular hip fractures. Cochrane Database Syst Rev
2000(2):CD000086.
MJ, Handoll HH. Extramedullary fixation implants and external fixators
for extracapsular hip fractures. Cochrane Database Syst Rev
2002(4):CD000339.
MJ, Handoll HH. Intramedullary nails for extracapsular hip fractures in
adults. Cochrane Database Syst Rev 2006;3:CD004961.
MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails
versus extramedullary implants for extracapsular hip fractures in
adults. Cochrane Database Syst Rev 2008(3):CD000093.
MJ, Handoll HH. Osteotomy, compression, and other modifications of
surgical techniques for internal fixation of extracapsular hip
fractures. Cochrane Database Syst Rev 2009(2):CD000522.
MJ, Handoll HH, Bhargara A. Conservative versus operative treatment for
hip fractures. Cochrane Database Syst Rev 2000(4):CD000337.
MJ, Pryor GA, Myles J. Eleven-year results in 2846 patients of the
Peterborough Hip Fracture Project: reduced morbidity, mortality, and
hospital stay. Acta Orthop Scand 2000;71(1):34-38.
SJ, Borgbjerg FM, Schousboe B, et al. A comprehensive hip fracture
program reduces complication rates and mortality. J Am Geriatr Soc. Oct
2008;56(10): 1831-1838.
E, Jahangir A, Mashru R, et al. Is there a gluteus medius tendon injury
during reaming through a modified medial trochanteric portal? A cadaver
study. J Orthop Trauma 2007;21:617-620.
H, Parker MJ, Pryor GA, et al. Classification of trochanteric fracture
of the proximal femur: a study of the reliability of current systems.
Reliability of the AO/ASIF classification for pertrochanteric femoral
fractures. Incidence of hip fracture in New South Wales: are our
efforts having an effect? Hip fractures in nonagenarians: perioperative
mortality and survival. Injury 2002;33(8):713-715.
A, Weil YA, Brocke L, et al. A prospective, randomised study comparing
the percutaneous compression plate and the compression hip screw for
the treatment of intertrochanteric fractures of the hip. J Bone Joint
Surg Br 2007;89(9):1210-1217.
P, Thalhammer G, Wozasek GE, Vecsei V. Femoral shortening after
surgical treatment of trochanteric fractures in nongeriatric patients.
J Trauma 2008;64(4): 982-989.
K, Amin A, Arora S, et al. Pseudoaneurysm of a branch of the profunda
femoris artery following distal locking of an intramedullary hip nail:
an unusual anatomical location. Hip Int 2008;18(3):231-235.
K, Becker C, Lamb SE, et al. Hip fractures in institutionalized elderly
people: incidence rates and excess mortality. J Bone Miner Res
2008;23(11):1825-1831.
PF, Gould ES, Lyden JP, Asnis SE. Diagnosis of occult fractures about
the hip. Magnetic resonance imaging compared with bone-scanning. J Bone
Joint Surg Am 1993;75(3):395-401.
AH, Rupprecht M, Gruber M, et al. The treatment of intertrochanteric
fractures: results using an intramedullary nail with integrated
cephalocervical screws and linear compression. J Orthop Trauma
2009;23(1):22-30.
TA, Mir HR, Stoneback J, et al. Avoidance of malreduction of proximal
femoral shaft fractures with the use of a minimally invasive nail
insertion technique (MINIT). J Orthop Trauma 2008;22(6):391-398.
MP, Madhavan P, Ravichandran KM. Nonunion of intertrochanteric
fractures of the femur. Treatment by modified medial displacement and
valgus osteotomy. J Bone Joint Surg Br 1995;77(1):90-92.
A. Intertrochanteric fractures of the femur: 150-degree-angle
nail-plate fixation and early rehabilitation: a preliminary report of
100 cases. J Bone Joint Surg Am 1963;45(4):706-722.
A, Williams EM. The unstable intertrochanteric fracture: treatment with
a valgus osteotomy and I-beam nail-plate. A preliminary report of 100
cases. J Bone Joint Surg Am 1970;52(7):1309-1318.
EM, Boruchov SD, Schmell EB, et al. Incomplete intertrochanteric
fractures: imaging features and clinical management. Radiology
1999;211(1):237-240.
W, Jantzen PM. A new principle in the operative treatment of
trochanteric fractures of the femur. J Bone Joint Surg Am
1955;37(4):693-698.
SS, Nargol AV, Port A. Unstable intertrochanteric fractures treated
with the Variwall reconstruction nail. Injury 1995;26(6):367-372.
ST, RG. The distribution and anastomoses of arteries supplying the head
and neck of the femur. J Bone Joint Surg Br 1965;47:560-573.
C, Lord SR, Herbert RD. A randomized controlled trial of weight-bearing
versus non-weight-bearing exercise for improving physical ability after
usual care for hip fracture. Arch Phys Med Rehabil 2004;85(5):710-716.
RK, Ljungqvist J, Bail H, et al. The new proximal femoral nail
antirotation (PFNA) in daily practice: results of a multicentre
clinical study. Injury 2008;39(8): 932-939.
AL, Penrod JD, Boockvar KS, et al. Early ambulation after hip fracture:
effects on function and mortality. Arch Intern Med 2006;166(7):766-771.
L. Hip fractures: the role of muscle contraction or intrinsic forces in
the causation of fractures of the femoral neck. J Bone Joint Surg Am
1953;35(2):367-383.
MR, Hall H, Kam BCC, et al. A laboratory model to evaluate cutout
resistance of implants for pertrochanteric fracture fixation. J Orthop
Trauma 2004;18(6): 361-368.
EJ, Kummer FJ, Koval KJ, et al. The “Z-effect” phenomenon defined: a
laboratory study. J Orthop Res 2007;25(12):1568-1573.
BW, Heyworth BE, Protopsaltis TS, et al. Basicervical versus
intertrochanteric fractures: an analysis of radiographic and functional
outcomes. Orthopedics 2006;29(10): 919-925.
J, Lenze E, Munin M, et al. Patient participation and physical activity
during rehabilitation and future functional outcomes in patients after
hip fracture. Arch Phys Med Rehabil 2009;90(4):618-622.
CT, Bono JV. Treatment of intertrochanteric nonunion of the proximal
femur using the S-ROM prosthesis. Orthopedics 2008;31(2):125.
HS, Armstrong D, Broad J, et al. Hip fracture in Auckland: contrasting
models of care in two major hospitals. Intern Med J 2009;39(2):89-94.
LL, Gliklich R, Kannan K, et al. The American Orthopaedic Association’s
“Own the Bone” Initiative to prevent secondary fractures. J Bone Joint
Surg Am 2008;90(1): 163-173.
S, Krska Z, Sedlar M, et al. [Comparison of various types of
pharmacological prevention of lower extremities deep vein thrombosis in
patients with proximal femoral fractures]. Rozhl Chir
2007;86(5):241-248.
RG. Use of an extramedullary guide pin for fractures of the upper end
of the femur. Orthop Clin North Am 1974;5(3):525-527.
KM, Hermann KL, Hasselqvist M, et al. The advantages of MRI in the
detection of occult hip fractures. Eur Radiol 2005;15(1):165-169.
S, Rao SK, Pandian S, et al. Closing lateral wedge valgus osteotomy
with dynamic hip screw for the treatment of varus nonunion of
pertrochanteric fracture: can restoration of biomechanics and
stabilization alone heal? Arch Orthop Trauma Surg 2009;129(6):827-832.
JP, Morton J, Schemitsch EH. The role of total hip replacement in
intertrochanteric fractures of the femur. Clin Orthop Relat Res
2004(429):49-53.
C. False aneurysm of the profundus femoral artery following nail-plate
fixation for intertrochanteric fracture of the hip. J Med Soc NJ
1975;72(7):623-624.
JM, Cramer KE, Karges DE. Comparison of the compression hip screw with
the Medoff sliding plate for intertrochanteric fractures. Clin Orthop
1998(348):79-86.
YA, Gardner MJ, Mikhail G, et al. Medial migration of intramedullary
hip fixation devices: a biomechanical analysis. Arch Orthop Trauma Surg
2008;128(2):227-234.
H. Preliminary report of a method of internal fixation of transcervical
fractures of the neck of the femur in the aged. VA Me Monthly
1932;59:197.
GH, Rana AJ, Terry MA, et al. Thromboembolic disease prophylaxis in
patients with hip fracture: a multimodal approach. J Orthop Trauma
2005;19(4):234-240.
R. A new method of treatment for fractures of the neck of the femur,
together with remarks on coxa vara. Ann Surg 1902;36:746.
R. A review of the campaign for the establishment of surgical
principles in the treatment of fracture of the neck of the femur. J
Bone Joint Surg Am 1938;20(4): 960-962.
JP, Goude W, Robbins SE, et al. An algorithm to standardise the
investigation of the undiagnosed traumatic painful adult hip: results
at 1 year. Ann R Coll Surg Engl 2005;87(3):181-184.
CH, Yuan LJ, Chan YS, et al. Conditions affecting treatment of
pertrochanteric osteomyelitis. Chang Gung Med J 2007;30(5):414-422.
EQ S, Trokhan S, Doseph D. Percutaneous compression plating compared to
sliding ip screw fixation of pertrochanteric hip fractures: a
prospective randomized study. OTA Annual Meeting. Denver; 2008.
L, Wenestam C, Hansson-Scherman M. A life-breaking event: early
experiences of the consequences of a hip fracture for elderly people.
Clin Rehabil 2008;22(9): 801-811.
M, Brink O, Switzer J, et al. The effect of shortening and varus
collapse of the femoral neck on function after fixation of
intracapsular fracture of the hip: a multicentre cohort study. J Bone
Joint Surg Br 2008;90(11):1487-1494.
