Femoral Neck Fractures
Intracapsular femoral neck fractures account for about 50% of all hip
fractures. The lifetime risk of sustaining a hip fracture is high and
lies within the range of 40% to 50% in women and 13% to 22% in men.
Life expectancy is increasing worldwide, and these demographic changes
can be expected to cause the number of hip fractures occurring
worldwide to increase from 1.66 million in 1990 to 6.26 million in 2050.62 The estimated annual cost of treating these fractures is enormous and a significant burden to any healthcare system.
undisplaced intracapsular hip fracture, which is almost invariably
treated with internal fixation; however, only 15% of these fractures
are undisplaced. The remainder are displaced and occur predominantly in
elderly female patients. Despite the ubiquitous nature of these
fractures there is still a surprising degree of variation in treatment.
Options include reduction and fixation, unipolar arthroplasty, bipolar
hemiarthroplasty, and total hip arthroplasty. Any of the arthroplasty
options may be cemented or uncemented. Recent surveys of practice
indicate widespread variation in the use of these options.19,54,117,140
In recent years, however, a number of randomized trials have been
published that have provided better evidence on which to base treatment
choices. As a generalization these trials have suggested that for the
majority of patients with a displaced fracture an arthroplasty is the
best choice, and that a modern design of arthroplasty is better that
older designs of unipolar hemiarthroplasties.
years. There is some racial variation in the incidence. They are less common in black races233 and more common in white females than males.197 Currently these fractures are most common in the white populations of Europe and North America.127 The incidence increases exponentially with age.72 The risk of a second hip fracture within 2 years approaches 10% in women and 5% in men.16,41 In patients who sustain a second hip fracture it is the same type of hip fracture in more than 70%.86
Epidemiologic studies have identified numerous risk factors associated
with an increased risk of sustaining a hip fracture. These include,
among other factors, a low BMI (less than 18.5), low sunlight exposure,
low recreational activity, smoking, a history of previous osteoporotic
fracture, maternal history of hip fracture, and corticosteroid
treatment.58,122,126,209,210
incidence of these fractures would increase until 2050. More recent
epidemiologic studies from Europe have reported that the incidence of
osteoporotic fractures may have leveled off,41,197 and there is even evidence that the incidence may be reducing.41,128 One study has predicted that the incidence and absolute numbers of hip fractures will fall.147 Whether these changes in the incidence are secondary to preventive measures or other therapeutic modalities is uncertain.
that increase the risk of falls in the elderly and those that
predispose to changes in bone mass. The main risk factors linked to
reduction in bone mass have already been given. Reduction in bone mass
caused by osteoporosis has an unequivocal link with hip fracture and is
present in more than 84% of patients with femoral neck fracture. A
reduction of bone mass at the hip of one standard deviation doubles the
risk of hip fracture.56 The
reduction in bone mass is caused by osteoporosis in most patients.
Other metabolic disorders of bone such as osteomalacia and renal
osteodystrophy also render the femoral neck more susceptible to
fracture, but they are much less prevalent.39
The risk of falling increases with age because of the increasing
prevalance of risk factors for falling in older age groups. These
include muscle weakness, abnormal gait or balance, neurologic disease,
deteriorating eyesight, and medication with sedative or cardiovascular
side effects.60,102
The direction of the fall is also important. Older patients who are
fitter tend to fall forward and are more likely to sustain distal
radial fractures or other upper limb fractures. More infirm elderly
patients are more likely to fall sideways, in which case the force of
the fall is sustained directly on the trochanteric region.
patients. The usual cause is a simple fall with an applied force being
transmitted to the femoral neck via the greater trochanter, resulting
in the fracture.145 An alternative
mechanism is external rotation of the leg with increasing tension in
the anterior capsule and iliofemoral ligaments. As the neck rotates,
the head remains fixed and a fracture occurs. This mechanism accounts
for the posterior neck comminution observed in many of these fractures.
The usual site of the fracture is in the weakest part of the femoral
neck, located just below the articular surface. Quantitative computed
tomography (CT) has confirmed site-specific bone loss within the
femoral head and neck with maximal bone loss in the more proximal and
superolateral areas, which accounts for the site of fracture.51
energy trauma. These injuries are more common in younger patients, in
whom much greater force is required to cause the fracture.78
Head-on vehicle collisions may be responsible. The use of clipless
pedals on bikes has become popular, and these hamper the ability to
quickly disengage the foot in the event of an accident, making a fall
on the trochanter, and a hip fracture, more likely. In younger
patients, the injury more frequently affects men. Finally the femoral
neck is a well-recognized site for stress fractures, and these occur as
a result of repetitive cyclical loading, which eventually exceeds the
strength of normal bone.83
injuries. Nonetheless they may be associated with distal radial
fractures and proximal humeral fractures in elderly patients.
Approximately 3% to 5% of hip fractures occur in younger patients; a
proportion of these follow high-energy trauma, and other fractures may
be present. Ipsilateral femoral shaft and neck fractures are a
well-recognized combination in these patients172,223,252 and it is estimated that femoral neck fractures occur in 2% to 6% of femoral shaft fractures.
at risk, is the concomitant presence of significant medical
comorbidities. Data from prospective population studies indicate that
70% of patients with femoral neck fractures have an ASA grade of 3 or 4
at presentation, because of associated medical problems. Some of these
are acute, such as stroke or myocardial infarction, and may be
implicated in the cause of the fracture.
fall as the cause of injury. In 2% to 3% of cases there is no history
of trauma,114 and the injury may be
pathologic or a stress fracture. Stress fractures can occur in younger
patients and are typically associated with heavy repetitive physical
activity in male patients or the triad of anorexia nervosa,
osteoporosis, and amenorrhea in female patients. The femoral neck is
not a particularly common site of stress fractures, and accounts for
only 3% of these injuries.262 There is usually a history of prodromal symptoms in patients with stress fractures.
patients there is cognitive impairment and there may be an unreliable
history of the nature or timing of injury. In view of the significant
rate of concomitant medical comorbidities, a careful history of
previous medical problems is important. An acute medical event or
deterioration of a pre-existing condition may have contributed to the
fall, causing the hip fracture, and this possibility always should be
considered. Osteoporosis is a feature in most patients with this
injury, and treatment may be required in the postoperative period. Any
other medical condition associated with osteoporosis may influence
decision making and needs to be considered. In a significant proportion
of younger patients with these fractures there are medical
comorbidities and risk factors that predispose to the injury. These
risk factors include alcohol abuse, steroids, renal failure, rheumatoid
arthritis, and endocrine diseases, all of which are associated with
decreased bone mineral density in younger patients.
fracture. There may be no obvious deformity, with the only finding
being a painful range of motion of the hip. In displaced femoral neck
fractures the affected leg is typically shortened and externally
rotated. All motions of the hip are painful. Associated neurovascular
injuries are exceptionally rare in the typical elderly patient but
should be sought in younger patients with high-energy injuries.
Physical findings do not differ significantly from extracapsular hip
fractures, and clinically the two hip fracture groups are
indistinguishable. Anterior hip dislocation is also associated with
shortening and external rotation of the hip, but this is a are much
rarer injury, which seldom occurs in elderly patients. Patients with
very limited mobility may have flexion contractures of the hip or knee
if they are normally bed- or wheelchair bound, and this may pose a
problem positioning the patient for surgery. Pressure sores should also
be noted, as these increase the risk of wound infection and may impede
postoperative mobilization depending on their location.
commonly undertaken in these patients. There were several theoretical
reasons for doing so. It was considered that the relative
immobilization of the limb would be helpful in reducing pain. The
traction might also reduce the risk of further local soft tissue
injury, help maintain reduction, and increase the chance of a better
reduction being achieved at the time of surgery in patients undergoing
reduction and internal fixation. Several published trials*
have compared preoperative traction with no traction. No conclusive
benefits have been shown for the use of traction in terms of pain
relief, ease of fracture reduction, or quality of reduction achieved at
the time of surgery; therefore, it is no longer recommended.
 |
|
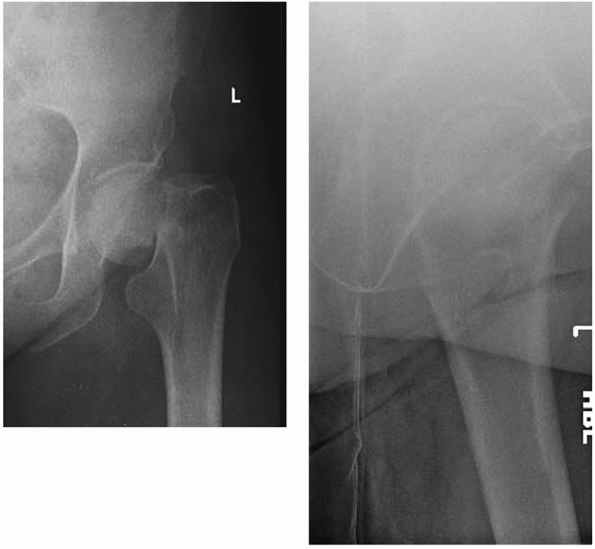
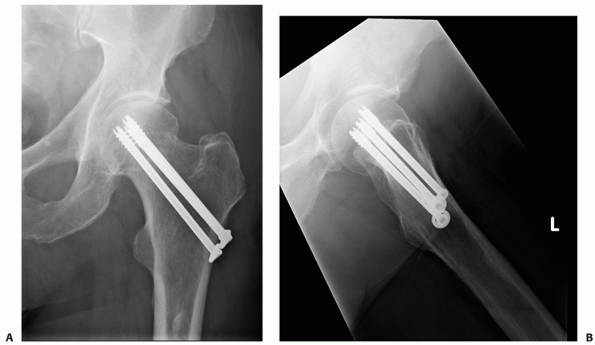
FIGURE 47-1 AP and lateral radiographs of a displaced femoral neck fracture.
|
patients some hematologic screening investigation is routinely
required. These include a full blood count, blood grouping, and serum
electrolyte analysis. Additional haematologic or biochemical
investigations may be appropriate depending on the associated medical
problems. An ECG wil be carried out in patients over the age of 60
years or younger patients with any history of cardiac problems.
Nonetheless, there is not much evidence that extensive preoperative
investigation of cardiac status alters management. Ricci et al.207
carried out a retrospective study of 235 patients with hip fractures. A
total of 35 (15%) underwent preoperative cardiac investigation. This
did not alter perioperative management in any case but did result in a
mean delay of 3 days to surgery in these patients.
Anteroposterior (AP) and lateral radiographs are required. In the
majority of cases the diagnosis is clear on the AP radiograph.
Nonetheless the degree of displacement can be difficult to discern in
some patients and in others there may be doubt about the diagnosis. The
lateral radiograph may be difficult to acquire because of pain, but it
is useful in determining whether the fracture is present and whether it
is displaced. In 2% of cases the fracture may be difficult or
impossible to visualize on plain radiographs. In the past a technitium
bone scan was often considered a useful investigation in this situation.76
Although it is usually positive in cases with a femoral neck fracture,
there is the possibility of a false-negative in osteopenic bone if the
investigation is carried out within 48 to 72 hours of the fall. It is
also sensitive but not specific. CT
scanning is a more accurate investigation, but exposes the patient to further radation.
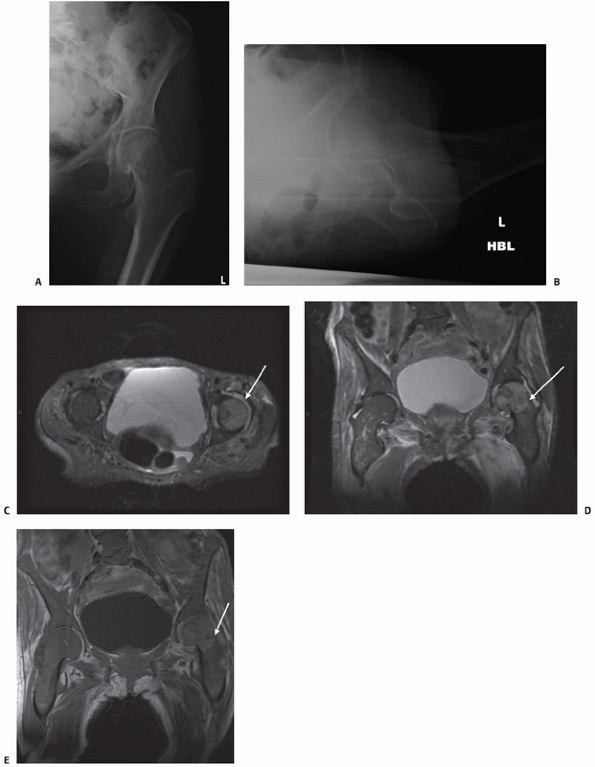
is probably the most useful additional form of imaging in modern
practice (Fig. 47-2). It has been shown to be more accurate than a bone scan75,92,208 in the early stages after injury and there is no radiation.177
It also picks up soft tissue problems that may be causing hip pain in
the absence of a fracture. Nonetheless for the majority of patients
plain radiographs are adequate for clinical decision making.
 |
|
FIGURE 47-2 A 78-year-old patient presented with painful left hip after a fall. There was no fracture clearly visible on the AP (A) or lateral (B) radiographs. A transverse MRI scan (C) showed a haemarthrosis of the left hip joint and AP MRI images showed an undisplaced intracapsular hip fracture (D,E).
|
patients because most patients are elderly and there is a high
incidence of cardiorespiratory problems. Distal radial fractures and
proximal humeral fractures are not unusual in these patients, and
apppropriate radiographs should be obtained if there is clinical
suspicion of a fracture in these locations. Even low-energy falls in
older patients may be associated with intracranial trauma. If the onset
of confusion coincides with the fall causing the hip fracture and there
is evidence of cranial trauma, a CT scan is needed to rule out a
remedial intracranial lesion.
mentioned. The use of dual energy photoabsorptiometry (DEXA) scans may
be appropriate in some patients. They are not necessary in patients
over the age of 70 years with a hip fracture. By definition, these
patients have osteoporosis and should be considered for prophylactic
treatment.
femoral neck fractures. Some authors have distinguished the fractures
based on their anatomic location, dividing intracapsular fractures into
subcapital and transcervical types.13
However, the bone in the transcervical region is much stronger than
that in the subcapital region, and it is doubtful if many fractures
actually occur in the transcervical region.9,133 Also the exact location of the fracture is difficult to determine on the basis of plain radiographs.6,89,133
The majority of fractures undoubtedly occur in the subcapital region.
In any event, the location of the intracapsular fracture has not been
shown to influence management or outcome.203
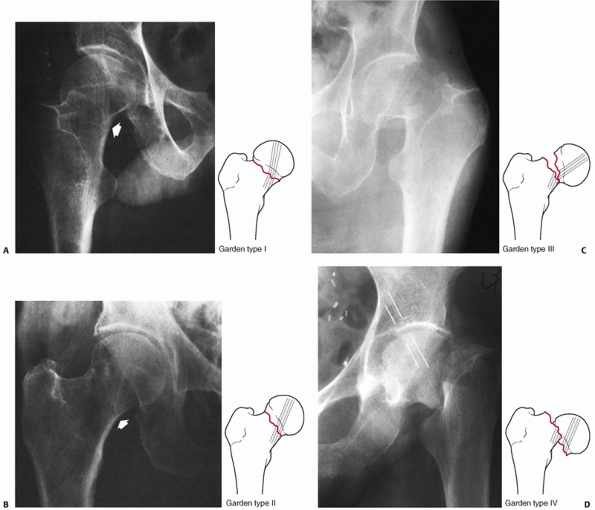
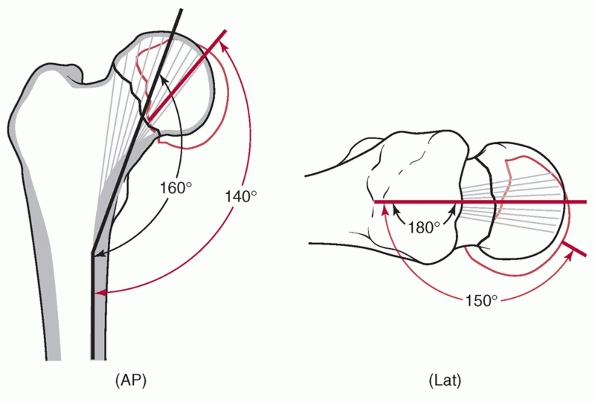
The degree of displacement is the more important consideration and this
is the basis of the more commonly used used classification systems.
The divisions are based on the degree of displacement, which is judged
on the anteroposterior radiograph by determining the relationship of
the trabecular lines in the femoral head to those in the acetabulum. In
the nonfractured hip, the trabecular lines in the femoral head are in
the same orientation as those of the acetabulum. The Garden I fracture
is a valgus impacted subcapital fracture. The fracture is incomplete
with a lateral fracture line that does not breach the medial cortex.
The trabecular lines in the femoral head therefore form an angle with
those in the acetabulum. In the Garden II fracture the fracture is
complete but undisplaced, and the trabecular lines in the head are
colinear with those in the acetabulum and the femoral neck distal to
the fracture. Garden III subcapital fractures are incompletely
displaced fractures. The femoral head has not lost contact with the
femoral neck, but the head is varus and extended, resulting in
angulation of the trabecular lines. The angulation is in the opposite
direction to that described for Garden I fractures. Finally, the Garden
IV fracture is completely displaced, and the trabecular lines line up
as the femoral head returns to a neutral position within the
acetabulum. The femoral neck has lost contact with the head and rotates
externally, so the trabecular lines in the neck are not colinear with
those in the head.
probably the most frequently utilized classification system in the
orthopaedic literature pertaining to femoral neck fractures.276
Unfortunately, like many other orthopaedic radiologic classifications,
interobserver and intraobserver level of agreement are not ideal.
Frandsen et al.81 evaluated the
classification and found that the level of interobserver agreement was
only 22% across all four grades. Surgeons demonstrated high levels of
agreement in determining whether fractures were undisplaced (Garden I
or II) or displaced (Garden III or IV), but the level of agreement was
much poorer when they were asked to subdivide cases across all four
groups. Another criticism of the classification is the small number of
cases fulfilling the criteria for Garden II fractures. In a multicenter
trial of 1503 femoral neck fractures,11
only 19 (1.2%) were classified as type II fractures. Also the outcome
for undisplaced (type I and II) fractures was independent of the grade
assigned. Similarly, most displaced fractures (type III and IV) are
treated by arthroplasty and the outcome is independent of the grade of
displacement.73,136
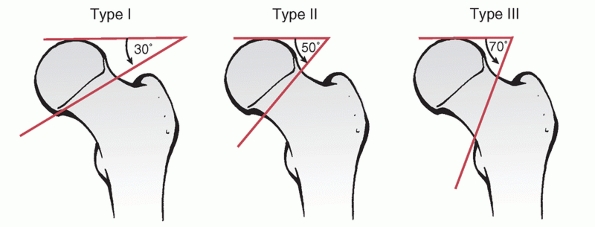
He described three separate fracture types based on whether the
fracture plane was vertical, oblique, or transverse. It was proposed
that the classification would be predictive of fixation failure or
nonunion with an increasing angle of fracture. The type I fracture
subtends an angle of 30 degrees or less. Type II fractures are between
30 and 50 degrees, and type III fractures are greater than 50 degrees.
This classification has been evaluated in a number of clinical studies
and has not been shown to be reliable either in describing the fracture
or predicting outcome.35,173,179
One limitation is that fractures with a vertical plane are actually
rather rare and the majority of fractures are closer to transverse in
orientation. It may be a more relevant classification for the younger
patient.150 In these patients the
fracture is often sustained as a result of high-energy trauma and
vertical fracture lines are more common. Liporace et al.146
recently described a series of Pauwel type III fractures. The mean age
in their series was 42 years, which is considerably younger than the
mean age for the general hip fracture population. The classification
relates the prognosis to the angle of the fracture plane—as the angle
increases the fracture instability increases and complications of
fracture healing and fixation are more likely.
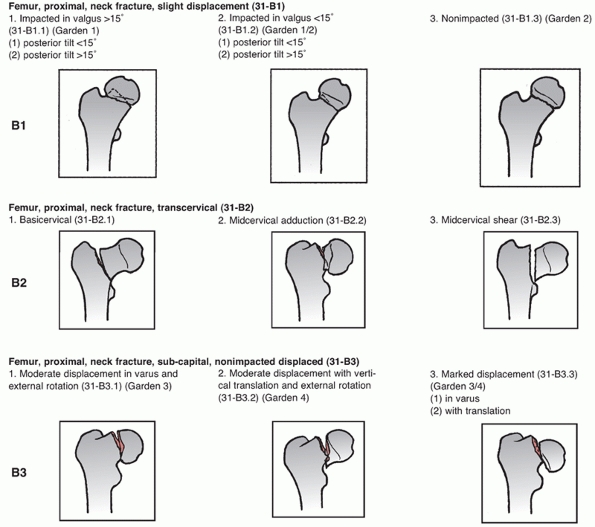
is an alphanumeric system based on the bone, the location of the
fracture, and the fracture morphology (Fig. 47-5).
The femoral neck is designated 31B. The B1 group describes undisplaced
femoral neck fractures, the B2 group contains transcervical fractures,
and the B3 group describes displaced subcapital fractures. Although
this system of classification provides a comprehensive method of
classifying fractures in general, it has not proved to be popular for
femoral neck fractures. Its complexity limits its usefulness in routine
clinical practice. Although it has been proposed to be a useful tool
for research purposes, it has not stood up to scrutiny for this use.
Blundell et al.26 found very poor
levels of agreement within the subdivisions of the classification.
Surgeons were able to divide the fractures into the main three groups:
undisplaced subcapital fractures, basal cervical fractures, and
displaced subcapital fractures, but levels of agreement within
subgroups were very poor. Moreover it was not found to be useful in
selecting treatment, nor was it predictive of outcome.
It
appears therefore that this classification, although theoretically
attractive, will prove impractical for use either in clinical practice
or as a research tool.
 |
|
FIGURE 47-3
The Garden classification of femoral neck fractures. Type I fractures can be incomplete, but much more typically they are impacted into valgus, and retroversion (A). Type II fractures are complete, but undisplaced. These rare fractures have a break in the trabeculations, but no shift in alignment (B). Type III fractures have marked angulation, but usually minimal to no proximal translation of the shaft (C). In the Garden type IV fracture, there is complete displacement between fragments and the shaft translates proximally (D). The head is free to realign itself within the acetabulum, and the primary compressive trabeculae of the head and acetabulum realign (white lines). |
 |
|
FIGURE 47-4
The Pauwel classification of femoral neck fractures is based on the angle the fracture forms with the horizontal plane. As fracture type progresses from type I to type III, the obliquity of the fracture line increases and, theoretically, the shear forces at the fracture site also increase. |
 |
|
FIGURE 47-5
The OTA classification of femoral neck fractures. The B1 group fracture contains nondisplaced to minimally displaced subcapital fractures. The B2 group includes transcervical fractures through the middle or base of the neck, and the B3 group includes all displaced nonimpacted subcapital fractures. Subgroups further specify fracture geometry. The diagrams represent common examples of the defined fracture pattern. |
based on judging the stability of the fracture have been proposed but
have not been widely accepted. For the purposes of evaluating outcome,
it is clear that surgeons are good at deciding if the fracture location
is intracapsular or extracapsular (basal cervical) and whether the
fracture is displaced or undisplaced. These are in fact the essential
points in determining treatment and are predictive of the likely
complications. At the present time newer classifications have not been
proved to be superior to these simple groupings. Older classifications
are either of limited applicability in most patients (Pauwels) or in
the case of the Garden classification, still widely used but of limited
reliability. Most clinical studies are concerned with undisplaced or
displaced femoral neck fractures and the subdivisions of these groups
based on various classification systems, is not a reliable guide to
treatment or prognosis.
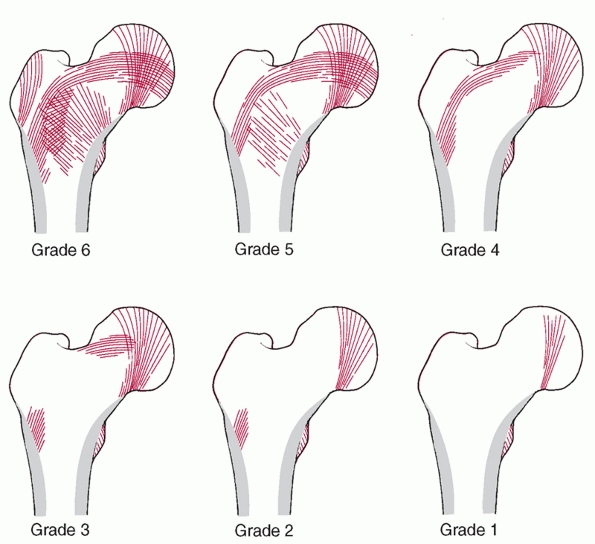
which is a method of estimating the degree of osteoporosis by fitting
the pattern of proximal femoral trabecular lines into six separate
categories. Several studies have evaluated the usefulness of this
classification134,232
and found it unreliable. It shows poor interobserver and intraobserver
levels of agreement. More importantly, it does not correlate with bone
mineral density as measured by DEXA scans. It is of little practical
value in modern orthopaedic clinical practice.
 |
|
FIGURE 47-6
Singh Index grades osteopenia from normal (grade 6; all trabecular groups are visible) to definite (grade 3; thinned trabeculae with a break in the principal tensile group) to severe (grade 1; only the primary compressive trabeculae are visible, and they are reduced) based on the ordered reduction in trochanteric, tensile, and ultimately primary compressive trabeculae. The grade is determined from a true AP projection of an intact proximal femur. (Adapted from Singh M, Nagrath AR, Maini PS. Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Joint Surg 1970;52A:457-467, with permission.) |
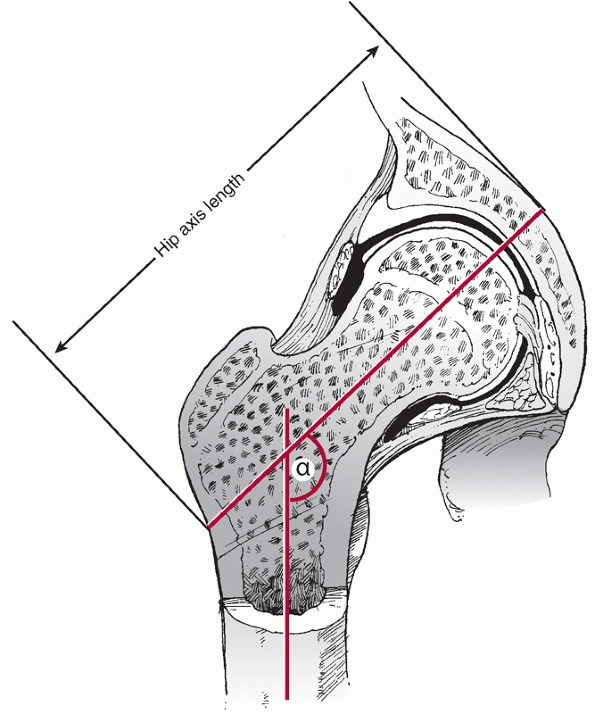
the case of the femoral neck, the relationship to the femur and hip
joint is characterized by anteversion of the femoral neck in the
transverse plane and the femoral neck shaft angle in the coronal plane.
The femoral neck subtends an angle with the femoral shaft of between
130 and 135 degrees in the normal hip. An angle less than this is
referred to as coxa vara and an increased angle is termed coxa valga.
Femoral neck anteversion describes the angle subtended by the femoral
neck to the the transcondylar axis, which is usually between 15 and 25
degrees. In addition to these two angles, hip axis length and femoral
neck width have also been shown to have an influence on the risk of
femoral neck fracture. The hip axis length is the distance from the
lateral aspect of the trochanteric region along the axis of the femoral
neck to the inner table of the pelvis (Fig. 47-7). An increase in hip axis length and femoral neck width and lower neck shaft
angles are associated with an increased risk of femoral neck fracture.32
Hip axis lengths are known to be longer in white females compared with
those of Asian and black populations, which may partly explain the
increased susceptibility to femoral neck fracture in this group.57
 |
|
FIGURE 47-7
Hip axis length and neck shaft angle (α). A longer hip axis length is associated with a greater lever arm and greater force being applied to the femoral neck during a fall. A lower neck shaft angle is seen in coxa vara and will also increase the risk of femoral neck fracture for the same reason. |
consideration when reduction and fixation is selected as a method of
treatment. Increased femoral anteversion may be present and
occasionally coxa varus or valgus, which will influence implant
placement. The internal trabecular system of the femoral head was
described by Ward.265 They are
oriented along lines of stress, and the thickest come from the calcar
region and radiate into the lower part of the femoral head. The calcar
femorale is a dense vertical plate of bone extending from the
posteromedial portion of the femoral shaft under the lesser trochanter
radiating to the greater trochanter and reinforcing the posteroinferior
portion of the femoral neck.101,110 The presence or absence of trabecular lines form the basis of the classification of osteoporosis described by Singh.
 |
|
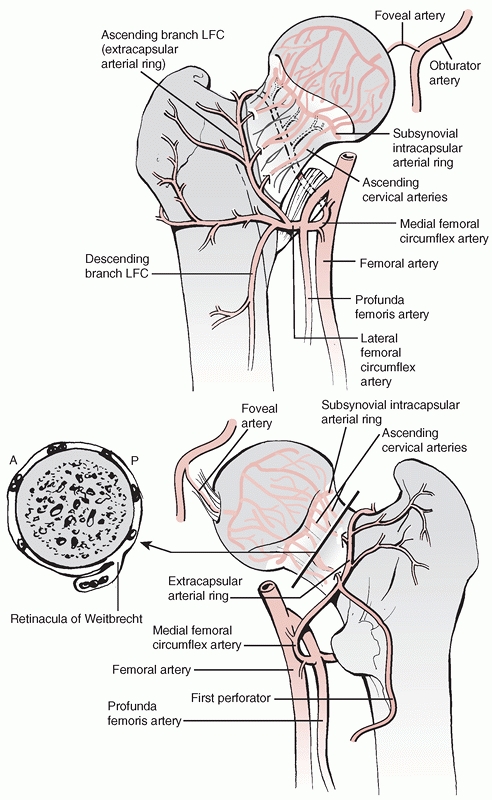
FIGURE 47-8 Vascular anatomy of the femoral head and neck. (Top) Anterior aspect. (Bottom) Posterior aspect. LFC, lateral femoral circumflex artery.
|
There are three sources: capsular vessels, intramedullary vessels, and
a contribution from the ligamentum teres. In the adult the most
important source of femoral head blood supply is derived from the
capsular vessels. These vessels arise from the medial and lateral
circumflex femoral arteries. These are in turn branches of the profunda
femoris in 79% of patients. In 20% of patients one or other of these
vessels arises from the femoral artery, and in the remaining 1% both
vessels arise from the femoral artery.260
The medial and lateral femoral circumflex arteries form an
extracapsular circular anastomosis at the base of the femoral neck, and
the ascending
cervical
capsular vessels arise from this. They penetrate the anterior capsule
at the base of the neck at the level of the intertrochanteric line. On
the posterior aspect of the neck they pass beneath the orbicular fibers
of the capsule to run up the neck under the synovial reflection to
reach the articular surface. Within the capsule these are referred to
as retinacular vessels.
There are four main groups (anterior, medial, lateral, and posterior),
of which the lateral group is the largest contributor to femoral head
blood supply. The most important retinacular vessels arise from the
deep branch of the medial femoral circumflex artery.52,124,221,253
These vessels supply the main weight-bearing area of the femoral head.
The contributions of the lateral femoral circumflex artery and
metaphyseal vessels are much less important by comparison.115,124,221,253,254 At the junction of the articular surface of the head with the femoral neck there is a second ring anastomosis termed the subsynovial intra-articular ring.45
The terminal branches of the deep branch of the medial femoral
circumflex artery penetrate the femoral head 2 to 4 mm proximal to the
articular surface on its postero-superior aspect.93
They enter the femoral head just below the articular margin.
Displacement of the femoral head because of a fracture in this area
will damage these vessels, jeopardizing the blood supply to the femoral
head and resulting in an increased risk of avascular necrosis if the
head is retained.90 Claffey46 has shown that the risk of avascular necrosis is greatly increased if the important lateral retinacular vessels are damaged.
Some additional blood supply in the adult reaches the head via the
medullary bone in the neck. Clearly these latter vessels will be as
vulnerable to disruption in any displaced fractures as are the
retinacular vessels. Although the vessels entering the head through the
ligamentum teres contribute to femoral head blood supply, their
contribution is generally not sufficient to maintain complete
vascularity of the entire head.115
After a displaced fracture, revascularization of the femoral head
occurs by revascularization from areas of the head with retained blood
supply and ingrowth of vessels from the metaphysis.36,37,46
capsule has no cambial layer in its fibrous covering to participate in
callus formation during fracture healing. Fracture union depends on
endosteal healing alone, which is one of the reasons prolonged union
times are commonly seen in these fractures.
intertrochanteric line over the anterior aspect of the femoral neck,
but posteriorly the lateral half of the femoral neck is extracapsular.
Three important condensations of the hip joint capsule are considered
ligamentous stabilizers of the hip. The ischiofemoral ligament controls
internal rotation in flexion and extension. The lateral arm of the
iliofemoral ligament has dual control of external rotation in flexion
and both internal and external rotation in extension. The pubofemoral
ligament controls external rotation in extension with contributions
from the medial and lateral arms of the iliofemoral ligament.155
Increased tension in the iliofemoral ligament is considered to have a
role in both the pathogenesis of femoral neck fractures and the
posterior neck comminution characteristic of the injury.
femoral, sciatic, and superior gluteal nerves. The anteromedial part of
the joint is supplied by the obturator nerve. The anterior capsule
receives sensory innervation from the femoral nerve. The posterior
aspect of the joint is supplied by the sciatic nerve and there is a
contribution to the posterolateral capsule from the superior gluteal
nerve. This has some relevance for pain control after hip fracture.
Femoral nerve blockade is commonly used, but this produces incomplete
pain relief. Much of the pain relief derived from femoral nerve
blockade is secondary to the reduction of muscle spasm.
into the lesser trochanter. When the femoral neck is intact,
contraction of this muscle also produces internal rotation. If the
femoral neck is fractured the muscle pull will result in external
rotation of the femoral shaft. External rotation of the hip is also
caused by the action of piriformis, the gemelli and obturator internus.
Abduction is produced by the gluteal muscles, which are supplied by the
superior gluteal nerve. Damage to this nerve, and particularly to the
inferior division of the nerve, may occur in the direct lateral
approach to the hip. This may contribute to the development of a
Trendelenberg gait after arthroplasty for fracture.
adductor compartment, which are supplied by the obturator nerve. These
include adductor longus, adductor magnus, and adductor brevis. These
muscles are not of particular importance in femoral neck fractures, but
may contribute to the characteristic leg shortening of the leg seen
with a displaced intracapsular fracture.
approach to the hip. It involves making an incision along the iliac
crest, which is then extended inferiorly from the anterior superior
iliac spine. The gluteal muscles are detached from the external wing of
the ileum and a plane is developed between tensor fascia lata and
sartorius. This allows access to the anterior aspect of the hip joint.
The reflected head of rectus femoris is detached to gain direct access
to the capsule. This surgical approach is useful for fixation of
femoral head fractures, but is not routinely used in the management of
femoral neck fractures.
access to the hip joint via an intermuscular plane. A lateral incision
is made in line with the femur that extends up to the iliac crest. It
angulates in a posterior direction to finish 8 to 10 cm anterior to the
posterior superior iliac spine. The fascia is divided in line with the
incision. A plane is developed between the anterior edge of the gluteal
muscles and tensor fascia lata that allows access to the anterior
capsule of the hip joint. This approach has most commonly been used in
femoral neck fractures when
open
reduction is necessary. It can be used for hip arthroplasty or
hemiarthroplasty, but access is limited and in particular it is not
ideal for femoral stem placement. The direct lateral or posterior
approaches are preferable for arthroplasty.
after a displaced intracapsular fracture. There is a higher rate of
dislocation associated with total hip arthroplasty following hip
fracture than with total arthroplasty performed for primary
osteoarthritis of the hip. The direct lateral exposure is associated
with a lower rate of dislocation after arthroplasty than the posterior
approach and it is the preferred approach for hip fracture patients if
total hip arthroplasty is being carried out. Variations on this
approach have been described by a number of authors. In general the
patient is placed in the lateral position and a longitudinal incision
is made centered on the greater trochanter. After division of the
fascia the trochanteric bursa is excised. An incision can then be made
through the tendon of gluteus medius extending distally to reflect the
vastus lateralis off the femur. At the proximal end of the trochanter
the gluteal muscles are split in line with their fibers. Care should be
taken not to carry this split too proximally or injury to the superior
gluteal nerve is a risk. This risk is increased if dissection is
performed more than 5 cm proximal to the trochanter. The approach can
then be developed by dissecting down to bone and then reflecting the
tissues in an anterior direction until the capsule is incised around
the base of the neck. The alternative is to divide the gluteus medius
and minimus tendons separately, which exposes the hip joint capsule,
which is then incised separately. The hip can then be exposed by
flexion and external rotation of the femur, which delivers the
fractured femoral neck out of the joint, thereby allowing access to the
fractured head in the acetabulum. Once this is removed,
hemiarthroplasty or total arthroplasty can be carried out.
the patient in the prone or lateral position. The former position is
popular for acetabular fracture surgery, but for arthroplasty the
lateral position is preferable to facilitate correct positioning of the
components. The approach is made through an incision centered on the
greater trochanter, which extends distally down the shaft and
proximally toward the posterior superior iliac spine. The more proximal
part of the approach, which provides access to the sciatic notch and
posterior column of the acetabulum, is not routinely required for
femoral neck surgery. The fascia is divided in line with the incision.
Above the level of the trochanter the gluteus maximus is split. More
distally the exposure is facilitated by partial division of the gluteus
maximus insertion into the linea aspera. The sciatic nerve should be
indentified and protected. The short external rotators of the hip are
divided starting proximally with piriformis. The obturator internus and
the gemelli are then divided and reflected posteriorly, where they lie
over the sciatic nerve. The capsule can then be incised to expose the
femoral head and neck. The neck is accessed by flexing the knee to 90
degrees and internally rotating the femur.
for both hemiarthroplasty or total hip arthroplasty. It also has the
advantage of being extensile both proximally and distally. None-theless
this facility is not often required during femoral neck fracture
surgery. The main disadvantage of this approach is that it is
associated with a higher rate of dislocation than the anterior or
anterolateral approaches. Although the risk is acceptably low in
osteoarthritic patients, it is much higher in patients undergoing total
arthroplasty for femoral neck fracture and this is a significant
drawback of this approach.
the medial approach and the Charnley transtrochanteric approach, but
these have no place in femoral neck fracture surgery. Trochanteric
osteotomy is best avoided, particularly in elderly patients because of
the frequent problems associated with trochanteric reattachment.
cases and 97% of patients are over 60 years of age; therefore, the
clinical decision-making process in most cases concerns the optimum
choice of treatment for a displaced femoral neck fracture in an elderly
patient. Although undisplaced fractures are only 15% of the total,
surgeons encounter them fairly frequently because of the rate of
femoral neck fractures in the population.
femoral neck fractures; some authors have recommended this method of
treatment and reported good results.200
Patients can be mobilized to weight-bearing with crutches and the
fracture can be expected to heal in 4 to 6 weeks. The advantage of this
method is that it avoids surgery, but most studies show there is a
significant risk of displacement during nonoperative treatment. The
risk of displacement varies from 19% to 46%49,224,261 in reported studies. In the only comparative study, Cserháti et al.55
compared nonoperative with operative treatment of undisplaced femoral
neck fractures. Operatively treated patients had much better outcomes.
The duration of hospitalization was a week shorter, full weight-bearing
began 11 days earlier, and there were no early displacements in the
operative group compared with 20% in the nonoperative group. In a
smaller, noncomparative study, Parker and Pryor178 reported nonunion in twice as many patients treated nonoperatively compared with operatively treated patients. Conn and Parker49
reported failure in 19% of nonoperatively treated patients at 1 year,
but two more recent studies reported secondary displacement in more
than 40% of cases.224,261 The mean time to displacement was 23 days in one of these studies,261 but displacement occurred up to 24 weeks after injury in some patients.
nonoperative treatment of these fractures. It can be considered in
patients with cardiac or psychiatric problems, stroke, renal failure,
multiple disseminated malignancies, and those who chose nonoperative
treatment.112 Occasionally patients present late after the injury, in which case nonoperative treatment is also an option.
 |
|
FIGURE 47-9 A. AP and (B) lateral radiographs of a displaced intracapsular hip fracture well-healed 9 months after fixation with three cannulated screws.
|
treatment of choice for the undisplaced intracapsular hip fracture.
There are a large number of implants available from which to choose. In
modern orthopaedic practice the usual choice is either a cannulated
screw system (Fig. 47-9) or a sliding hip screw device with a short plate. These have superseded older devices such as hook pins,241 Knowles pins,238 and the Watson-Jones nail,195 even though these implants were documented as having results comparable with more modern implants.
usually straightforward. The patient is placed supine on the operating
table and a fluoroscope is used to obtain anteroposterior (AP) and
lateral images of the hip. This is facilitated by flexion and abduction
of the contralateral hip. The surgical exposure required is minimal and
the procedure can be undertaken percutaneously. If the procedure is
performed open, a short linear incision is made from just inferior to
the vastus lateralis ridge of the greater trochanter for approximately
5 cm. The guidewires can then be introduced into the femoral neck using
a fluoroscope to guide their position. Most surgeons who use a
cannulated screw system prefer to use three screws, but there is some
evidence that two screws may be as effective.135
The optimum position of the screws has also been a source of debate,
particularly whether they should be parallel or divergent. Once again,
convincing evidence to suggest screw position greatly influences
outcome is lacking. Perhaps surprisingly, a recent study showed more a
favorable outcome if screws were used with rather than without washers.275
devices with cannulated screw implants for these fractures. Two
meta-analyses have addressed the issue of implant selection,180,183
analyzing more than 25 trials comparing implants. The conclusion of
these meta-analyses was that there was no clear evidence of superiority
of any one implant for fixation of these fractures. Cannulated screw
systems do have the advantage of a less invasive surgical exposure with
less blood loss and pain47,142 and are the most popular choice.
as tolerated. Serial radiographs should be taken to document union,
which can be expected to occur in more than 90% of cases. The rate of
nonunion in most series is low but it does occur, and Table 47-1
shows that overall a rate of about 6% can be expected. Despite the fact
that these are undisplaced fractures, there is a definite rate of late
avascular necrosis that, according to the literature, varies from 1.6%
to 22.5% (Table 47-1).40,42,49,168,188 Younger patients should be followed up to detect this complication, but long-term follow-up may be impractical
in older patients. The functional outcome of patients with undisplaced
femoral neck fractures reflects the low complication rate and is
generally good. The majority of patients return to their prefracture
level of mobility and residence.248
|
TABLE 47-1 The Results of Studies Investigating Internal Fixation of Undisplaced Femoral Neck Fractures
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
with undisplaced fractures, in which there is general agreement
regarding treatment, there is considerable variation in surgical
practice in the treatment of displaced femoral neck fractures. Three
recent surveys of European and North American orthopaedic surgeons
evaluated how surgeons treated displaced fractures.19,54,117
The results showed that most surgeons believed that reduction and
internal fixation was the treatment of choice for displaced fractures
in patients less than 60 years old. Almost all surgeons preferred
arthroplasty in patients more than 80 years old. There was much more
variation in patients between the age of 60 and 80 years, with surgeons
using reduction and internal fixation, unipolar hemiarthroplasty,
bipolar hemiarthroplasty, and total hip replacement. In the past few
years, a number of randomized trials have evaluated these treatment
options and have provided better evidence on which to base clinical
decisions regarding the optimum treatment.
neck fractures is now less popular with surgeons. The main reason for
this is the high failure rate associated with this procedure because of
fixation failure, nonunion, and avascular necrosis. Nonetheless it is
still widely used, and is the treatment of choice in younger patients.
to that described for undisplaced femoral neck fractures once the
fracture is reduced. The usual method of reduction is to apply gentle
traction and internal rotation to the leg. This is an essential point,
because a common error is to apply excessive traction with forceful
rotation to the leg. This may result in a valgus reduction, which is
very difficult to correct by closed means. The correct technique is to
place the patient on the traction table and apply minimal traction and
rotation in the first instance. Radiographs can then be taken to verify
the position of the fracture. If the fracture is incompletely reduced,
then small incremental increases in both traction and internal
rotation, checking the position after each adjustment, can be carried
out until the reduction is judged adequate.
 |
|
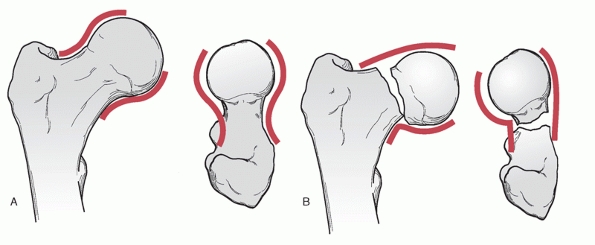
FIGURE 47-10 Lowell148
demonstrated that the cortices of an anatomically aligned femoral head and neck will project shallow S- or reverse S-shaped curves on both x-ray views (A). Malalignment is demonstrated by a flattening of one curve and a sharp apex on the opposite side (B). These findings are usually easier to appreciate intraoperatively with fluoroscopy than are the primary compressive trabecular alignments needed to measure an alignment index. |
views. The junction of the convex femoral head and neck should produce
an S-shaped curve in all planes148 (Fig. 47-10).
A perfect reduction may not be possible if there is comminution of the
femoral neck, which is not unusual. On the AP view, a valgus reduction
is preferable to a varus reduction. A valgus reduction is inherently
more stable, whereas a varus reduction is associated with a much higher
risk of fixation failure.10 What
constitutes an acceptable reduction is debatable, but a 20 degree varus
reduction is associated with a 55% risk of failure and Arnold4
recommended that there should be less than 20 degrees of posterior
angulation to minimize the risk of fixation failure. The risk of
avascular necrosis has also been shown to be lowest with anatomic
reduction. Either varus or valgus reduction increases the risk.43
This is based on measurement of bony trabecular alignment on the
postoperative AP and lateral radiographs. On the AP view, the angle
subtended by the central axis of the medial trabecular system in the
head and the medial cortex normally should be 160 degrees. On the
lateral view, the central trabecular axis in the head is in line with
the femoral neck, an angle of 180 degrees. Garden90
reported good results when the angle was between 155 and 180 degrees on
either view. The risk of fixation failure and avascular necrosis
increased when the angle was outside this range. Failure to achieve a
stable reduction is most commonly caused by posterior comminution of
the femoral neck.9,89,90,220
This is not under the control of the surgeon; if an acceptable
reduction cannot be achieved, the use of an arthroplasty should be
considered.
 |
|
FIGURE 47-11
The Garden alignment index. An angle of 160 to 180 degrees on both anteroposterior (AP) and lateral images was considered acceptable by Garden. Anatomic (black) and unacceptable (red) reductions are shown. |
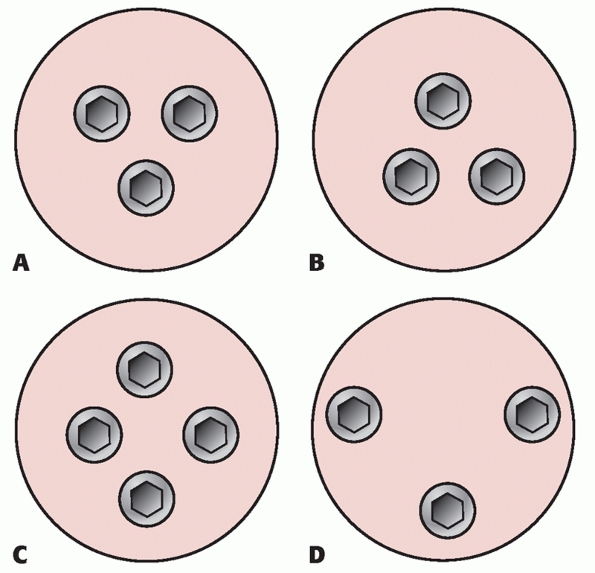
with either cannulated screws or a sliding hip screw and short side
plate. Although two screws may be adequate for undisplaced fractures,
three cannulated screws are a safer choice for a displaced fracture,21,135
and this is the most common technique in current use. Most surgeons use
a parallel pin placement and a triangular configuration, although
evidence for the superiority of one particular pin configuration is
lacking (Fig. 47-12). Postoperatively patients
can be mobilized with touch weight-bearing for 6 weeks. Older patients
are unable to cooperate with instructions to remain non-weight-bearing,
so this is impractical. It should also be remembered that the forces
across the hip joint are greater with complete non-weight-bearing than
with touch weight-bearing; therefore, non-weight-bearing mobilization
is illogical.
usually takes longer than 6 months in the majority of cases. Barnes et
al.11 reported union in only 14.5%
of patients with displaced fractures at 6 months. Patients require
regular radiographs until this time to ensure that the fracture is
uniting uneventfully. Avascular necrosis tends to manifest itself after
fracture union and is most commonly seen in the second year after
injury.11 Younger patients should be followed up for 2 years with radiographs on a 6-month basis to detect this complication.
 |
|
FIGURE 47-12 Configuration of screws used to internally stabilize a femoral neck fracture.
|
femoral neck fractures are considerably inferior to the results
reported for undisplaced fractures treated by fixation. There is a high
incidence of postoperative complications. These are mainly owing to
fixation failure, nonunion, and avascular necrosis. Although avascular
necrosis is a well-recognized complication, the majority of
reoperations are for early fixation failure in osteoporotic bone and
nonunion.149 Table 47-2
shows that the literature indicates that nonunion varies between 6.5%
and 31.8%, with an average of about 25%, whereas avascular necrosis
varies between 3.7% and 32.7%, but averages about 11%.
arthroplasty in displaced fracture. The results of these studies are shown in Tables 47-3, 47-4 and 47-5. Table 47-3 shows the prevalence of dislocation after internal fixation, hemiarthroplasty, and total hip arthroplasty. Table 47-4 shows the prevalence of revision surgery, and Table 47-5
shows the mortality associated with the three procedures. The results
have been remarkably uniform. Reduction and internal fixation compares
unfavorably with arthroplasty in terms of reoperation rates and
functional outcome. The reoperation rates for reduction and fixation in
these trials have been notably higher than previously published studies
and vary from 33% to 50%.
|
TABLE 47-2 The Results of Studies Investigating Reduction and Internal Fixation of Displaced Femoral Neck Fractures
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
|
TABLE 47-3 The Rates of Dislocation in Eight Randomized Controlled Trials
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
contribute to the high failure rate of internal fixation. The level of
the fracture in the femoral neck has not been shown to make any
difference as long as the fracture is intracapsular.203 As indicated, there is no clear evidence that one particular implant has any advantage over another.180,183 Nonetheless the quality of reduction does have an influence. In particular, a varus reduction has been estimated44 to increase the risk of failure fourfold.
|
TABLE 47-4 The Rates of Revision Surgery in Eight Randomized Controlled Trials
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
On this basis it has been suggested that ancillary measures such as
aspiration of the hip joint capsule or open reduction might be useful
to decompress the hemarthrosis and improve the quality of reduction.
Nonetheless, clinical studies have failed to show evidence that
aspiration or capsulotomy to drain the hemarthrosis is actually of any
benefit.
reduction and compression in these fractures, but there is no
convincing evidence that either technique enhances results.182
The use of fracture compression using a sliding hip screw was compared with no compression in one study.80
No benefit was conferred by compression of the fracture. Open reduction
of femoral neck fractures has been compared with closed reduction in
two studies.97,255
The open reduction took longer, but there was no significant difference
in the quality of fracture reduction between the open and closed
groups. This was reflected in the outcome, with no significant
differences being noted in the mean time to union or the rates of
nonunion and avascular necrosis. Therefore, open reduction should
mainly be reserved for young patients with higher-energy trauma in whom
an adequate closed reduction cannot be achieved and arthroplasty is not
a desirable option.
|
TABLE 47-5 The Mortality Rates in Eight Randomized Controlled Trials
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
the femoral head are seen within 6 hours of the fracture, but osteocyte
cell death occurs quite slowly and may not be complete until 2 to 3
weeks after the fracture occurs.36,37
Thus fixation may well be successful even if it is not undertaken soon
after the patient presents with a femoral neck fracture. Barnes et al.11
found that timing of surgery had no influence on the rates of avascular
necrosis and nonunion in patients treated with reduction and fixation
up to 7 days after injury. In contrast to this finding, Jain et al.118
compared early fixation (within 12 hours of injury) to delayed fixation
(more than 12 hours) and recorded an incidence of AVN in 16% of the
delayed group compared with none in the early fixation group.
without complications are usually associated with acceptable functional
results. In patients who develop complications the results are
frequently not satisfactory and there is a high rate of revision
surgery to deal with the complications.248
In the majority of cases revision surgery is needed to deal with
fixation failure and nonunion rather than avascular necrosis. In
patients with healed fractures the result is sometimes not
satisfactory. Femoral neck shortening after fixation can occur in up to
one third of patients in the absence of any healing complication.277 This adversely affects hip abductor muscle function, which may contribute to poor results in these cases.
initially treated with reduction and fixation may be converted to a
total hip replacement secondarily because of failure of fixation.
Nonetheless the evidence suggests that secondary total hip replacement
in this situation is associated with a higher rate of complications
than a total hip arthroplasty (THA) carried out as a primary procedure.
McKinley and Robinson157 compared
secondary THA with an age- and sex-matched cohort who had received THA
as a primary procedure for displaced subcapital hip fracture. They
recorded a significantly higher rate of infection, dislocation, and
loosening in the group that had the procedure carried out as revision
for failed fixation. Other studies evaluating secondary THA without a
comparison group concluded that their results were acceptable, but the
rates for common complications in most series are higher than those
reported for primary THA.20,82,169,170,266
Current evidence indicates that if THA is used, superior results can be
expected in patients in whom the procedure is the primary operation.
been widely used for femoral neck fracture for many years. Although
modern prostheses are available, a surprising number of cases are still
carried out using older, unsophisticated implants such as the Austin
Moore and Thompson prostheses (Figs. 47-13 and 47-14).
The procedure has a number of advantages. The surgery is technically
relatively straightforward, and it eliminates the risks of nonunion and
fixation failure, which contribute to the high rate of revision surgery
associated with reduction and internal fixation.
patient in the lateral position. Most surgeons choose a posterior or
direct lateral approach. Lateral approaches may result in some abductor
weakness, but there is a lower risk of dislocation.130,259
Once the hip joint is exposed, the femoral neck is delivered into the
wound and the femoral neck is cut. The femoral head can then be removed
from the acetabulum. The
femoral
canal is reamed and the chosen prosthesis inserted. Although older
implants such as the uncemented Austin Moore are cheap and easy to use,
they are not ideal implants in fitter patients. The lack of modularity
means that it is necessary to judge the leg length and hip soft tissue
tension correctly at the time of insertion, as this cannot be varied
later. Proximal femoral fractures can occur at the time of insertion.222
This complication can be minimized by completely excising the hard
residual femoral neck bone, which is located laterally at the base of
the greater trochanter. This allows the prosthesis to be pressed into
the softer cancellous bone in the lateral region, thereby avoiding
excess pressure on the calcar, which may result in fracture. Once the
implant has been inserted, reduction can be accomplished. Forceful
maneuvers, especially rotation, should be avoided to minimize the risk
of a periprosthetic femoral shaft fracture. Once the implant is
reduced, the capsule can be repaired and the wound closed.
 |
|
FIGURE 47-13 An Austin Moore prosthesis.
|
 |
|
FIGURE 47-14 A Thompson prosthesis.
|
This shows that although unipolar hemiarthroplasty avoids the problems
of fixation failure, nonunion, and avascular necrosis that are
associated with reduction and fixation, it exposes the patient to the
risks of arthroplasty. Nonetheless because of the large head diameter
the risk of dislocation is low, averaging between 3% and 4%, and wound
infection rates should be on the order of 1%. Table 47-6 also shows that the revision rate averages approximately 4%, and around 70% of patients have excellent or good results.
increased risk of proximal femoral fracture at the time of insertion,
and the incidence of this has been reported to be up to 12%.267 Cemented stems also have been associated with better functional outcomes and less thigh pain.77,185,229
Long-term survival of these implants has been good, mainly because of
the limited life expectancy of the patients who sustain femoral neck
fractures. In one long-term study the survival rate was 94% at 5 years
and 83% at 12 years.171 This has to
be interpreted in light of the high mortality of these patients, as 81%
died within the study period. Most patients with these implants may
never survive to develop symptoms from stem loosening or acetabular
protrusio. Most authors now agree that the use of these older
uncemented designs should be confined to patients with very limited
mobility and functional demands.
has become a very popular alternative to unipolar hemiarthroplasty. A
wide range of modern bipolar cemented and uncemented stems are
available. Bipolar heads have a number of proposed advantages. There is
an articulation between the inner head and shell and between the shell
and acetabulum. This dual articulation was proposed to reduce the risk
of wear and acetabular protrusio. Some studies have suggested that in
some designs, the prosthesis ceases to function as it was intended and
for practical purposes the implant behaves as a unipolar implant in a
proportion of patients.27,69,113,194 There is some evidence that the function of the articulation varies with the diameter of the inner head. Brueton et al.33
investigated motion with two bipolar designs, one with a 22-mm inner
head and one with a 32-mm inner head. The prosthesis with the smaller
head diameter exhibited predominantly intraprosthetic motion compared
with the larger-diameter head, in which motion was mainly
extra-prosthetic. They recommended selection of a bipolar design with a
smaller-diameter inner head on the basis of these findings.
hemiarthroplasty implants are available in cemented and uncemented
designs. The surgical approaches and techniques are identical to those
already described for unipolar hemiarthroplasty. Modern bipolar
hemiarthroplasties have a modular design with a variety of inner
head-neck lengths. Trial heads and neck additions are available with
some implants. This makes precision in judging tissue tension and leg
length easier at the time of surgery. If a cemented stem is used modern
cementing techniques with a medullary plug and cement pressurisation
should be used.
|
TABLE
47-6 The Results of Studies Investigating the Use of Unipolar Hemiarthroplasty in the Treatment of Displaced Femoral Neck Fractures |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
shows the results of bipolar hemiarthroplasty for femoral neck
fractures, which generally have been good. The complication rates are
higher than those reported for hip arthroplasty in osteoarthritis but
still acceptably low. Table 47-7 shows that
the dislocation rate in a number of large studies averaged less than 3%
and the infection rate less than 1%. Early mortality in this group of
patients tends to be high, but one study of prosthetic survival found
that the 10-year survivorship was 93.6%, which is comparable with the
outcome after total hip arthroplasty for osteoarthritis.106
Revision for protrusio is actually very rare and has been reported in
less than 2% of cases. Functional outcome is seldom reported in much
detail. Most authors use relatively crude measures of outcome, although
the Harris hip score has been used in a number of studies reporting
good to excellent results in 65% to 96% of patients. Table 47-7 shows that the the rate of excellent and good outcomes averages about 80%.
 |
|
FIGURE 47-15 AP radiograph of cemented bipolar hemiarthroplasty.
|
unipolar with bipolar hemiarthroplasty have failed to show any
advantage for the bipolar design. Eight studies have compared the
outcome of unipolar and bipolar hemiarthroplasty.* Most of
these compared a cemented unipolar implant with a cemented bipolar
implant, but three compared the use of an Austin Moore implant with a
bipolar implant.153,216,257
There was no difference in the reported rates of dislocation, deep
infection, reoperation rates, or other general complications such as
deep venous thrombosis. Levels of mobility also showed no significant
differences.
the implications are different. In the case of a unipolar
hemiarthroplasty a closed reduction is usually possible. The same does
not apply to a bipolar hemiarthroplasty. The bipolar head is mobile,
and this mobility often prevents a successful closed reduction.
Attempts at closed reduction can result in dissociation of the two
articulating components.201 In most cases of dislocation an open reduction of the bipolar prosthesis is required.
Most of these studies have involved the use of older implants such as
the Austin-Moore and Thompson prostheses. Uncemented implants were
found to be significantly faster to perform but the perioperative
complication rates were no different. Function tended to be better with
cemented stems. Most studies reported better mobility and less pain in
patients with a cemented implant. Nonetheless studies involving more
modern uncemented implants have found no differences.219 More data are needed on outcomes associated with modern designs of uncemented stem.
for displaced intracapsular hip fractures in the past. Total hip
replacement is the most complex operative treatment option for
a
displaced femoral neck fracture. It is a longer operation than the
other operations that have been discussed and, depending on the implant
used, may be the most expensive operative procedure. Many patients who
sustain this injury are not natural choices for total hip arthroplasty
(THA) as most are elderly, have limited mobility, and 25% to 30% have
some degree of cognitive impairment. In addition the initial experience
with THA for intracapsular fractures was not very encouraging. Early
reports detailed high rates of loosening and dislocation.99,100,246 This led to pessimism about the use of THA, and most surgeons are still reluctant to consider it as a treatment option.19
Nonetheless, there is now an accumulating body of evidence that
supports the use of THA in suitable patients, and some recent trials
have indicated that the functional outcome may be more favorable than
other procedures.
|
TABLE
47-7 The Results of Studies Investigating the Use of Bipolar Hemiarthroplasty in the Treatment of Displaced Femoral Neck Fractures |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
have been associated with a high rate of failure after reduction and
internal fixation. THA should be considered particularly in rheumatoid
arthritis, in which there may be involvement of the acetabulum in the
disease. The results of fixation in patients with rheumatoid arthritis
are very poor, with high rates of failure.239,242
Displaced subcapital fractures are very rare in osteoarthritic
patients, but for the same reason should be treated in fit patients
with a total arthroplasty.
consideration. Most surgeons still regard reduction and fixation as the
treatment of choice in patients under the age of 60 years.19 Reduction and fixation of these injuries in younger patients is normally successful.107
Nonetheless, a proportion of these patients are medically unwell with
conditions that predispose to a higher risk of failure. These problems
include steroid treatment, alcoholism, and other conditions associated
with osteoporosis. Patients with these risk factors have a higher risk
of fixation failure and nonunion. Total hip arthroplasty is probably a
better choice in these patients. In displaced subcapital fractures in
patients under the age of 50 years the incidence of nonunion and AVN in
one study was 37%,107 although not all patients with AVN required conversion to arthroplasty.
lateral or posterior surgical approach as described for
hemiarthroplasty. Some aspects of the procedure differ from THA in the
osteoarthritic hip. The acetabular anatomy is not distorted by
osteophytes and the bone is osteoporotic rather than sclerotic, as in
osteoarthritis. Therefore, particular care is required in preparation
of the acetabulum. It is easy to overream and remove excessive bone
from the anterior and posterior walls or the acetabular floor. Cautious
reaming is necessary with regular visual evaluation of the amount of
bone removed. Capsulectomy
is
performed in the osteoarthritic hip to facilitate exposure and hip
mobility. This is not required in hip fractures and the capsule should
be conserved to allow repair at the end of the procedure. Cementing of
the socket can be carried out using standard techniques. In uncemented
sockets the desire for a tight impaction fit must be balanced against
the risk of pelvic fracture if the chosen implant diameter is too large
for the osteoporotic bone to accommodate it without a stress fracture.
Finally, malposition of the acetabular component must be avoided to
minimize the risk of postoperative dislocation. The femoral stem
preparation and insertion are as described for hemiarthroplasty. The
choice of femoral head may differ from THA undertaken for
osteoarthritis and many surgeons choose a slightly larger head diameter
(30 to 32 mm) for hip fracture patients to reduce the risk of
dislocation. After reduction a careful capsular repair will also reduce
the risk of dislocation.
 |
|
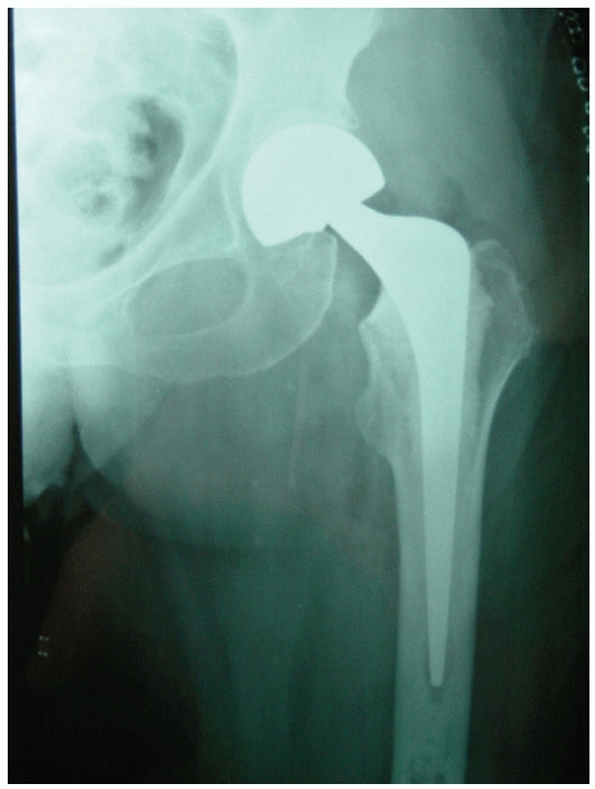
FIGURE 47-16 A cemented total hip arthroplasty used to treat a femoral neck fracture in a fit older patient.
|
hemiarthroplasty or internal fixation, and one concern surgeons had was
that the mortality rate would be higher. Nonetheless, the 30-day
mortality in a series of more than 7000 patients undergoing THR for hip
fracture was 2.4%,189 which compares favorably with the mortality rate of other procedures. Data from the Norwegian hip registry144
suggest that there is a slight increase in standard mortality ratio
compared with the non-THA population (SMR = 1.11). Randomized trials
have not shown a higher mortality with THA compared with other
treatment options.* It seems that mortality is more
influenced by increasing age and medical comorbidities than the
magnitude of the surgical procedure.
relatively short follow-up periods, often only 2 years. Three studies
have carried out longer-term follow-ups and calculated the 10- and
20-year survivals of THA after femoral neck fracture. These studies
indicate that the 10-year survival of THA is in excess of 90%.
Tarasevicius et al.247 reported
10-year survival rates of more than 90% for both stem and cup in THA in
a series of 135 patients. The implant used had no influence on outcome.
Mabry et al.151 reported 93% 10-year
survival and 76% 20-year survival of Charnley cemented implants used to
treat femoral neck nonunion. An age of less than 65 years and obesity
were associated with an increased risk of loosening. Lee et al.141
reported survival rates of 95% at 5 years, 94% at 10 years, 89% at 15
years, and 84% at 20 years for cemented THA used as primary treatment
for intracapsular hip fracture. These survival rates are slightly less
favorable than for THA carried out for primary osteoarthritis, but
nevertheless still represent excellent long-term results.
THA has consistently been shown to be superior to reduction and
internal fixation in relation to functional outcome and cost. The
complication rate in these trials after THA has been much lower than
with reduction and internal fixation. Reoperation rates with reduction
and fixation average approximately 40% compared with approximately 5%
after THA (Table 47-4). Mortality averages approximately 20% after internal fixation compared with approximately 12% after THA (Table 47-5). The rates of dislocation are shown in Table 47-3,
but it must be remembered that the studies differ in their definition
of dislocation. Most dislocations actually occur after the revision
hemiarthroplasty or THA operation used to treat the failed internal
fixation. Some studies do not report this and the true dislocation rate
is difficult to determine. In one study the hip complication rate was
10 times higher with reduction and fixation compared with THA.23
Randomized trials comparing THA with hemiarthroplasty have found that
THA was associated with better function and a lower rate of revision
surgery, but the numbers of cases in published studies have been small.25,130
have been published comparing the outcome of THA after femoral neck
fracture.18,149,185,215
These also have reached similar conclusions to the randomized trials.
THR is associated with a low rate of complications and better
functional outcome than other methods of treatment.
Nonetheless, about half of the patients are somewhat older, usually age
between 40 and 60 years. These patients often have predisposing
conditions that render them more liable to sustain a hip fracture.
These factors include chronic diseases associated with osteoporosis,
steroid treatment, and alcohol abuse.274
If the fracture is undisplaced, it may be treated by reduction and
internal fixation as a scheduled urgent procedure. A displaced
intracapsular hip fracture in a young patient requires more urgent
treatment. These fractures should be treated by reduction and fixation
as soon as possible. In most patients closed reduction is satisfactory.
If closed reduction is not adequate, open reduction can be considered.
This is usually performed through a Watson-Jones approach,91
which conserves the femoral blood supply. A capsulotomy in line with
the femoral neck can be performed to visualize the fracture. Reduction
can be assisted by applying traction to the femur using a bone hook on
the greater trochanter to disimpact the fracture. Control of the
proximal fragment can be achieved by inserting a 2-mm Kirschner wire
into the femoral head, which can act as a joystick and allow
manipulation of the head to facilitate reduction. Nonetheless, although
this maneuver may facilitate a better anatomic reduction, this may be
at the expense of increasing the rate of nonunion. The overall rate of
nonunion in younger patients after open reduction has been shown to be
11%, in comparison with 5% for closed reduction.59
patients are good in most cases, but rates of nonunion and avascular
necrosis are significant. The results of a number of studies are given
in Table 47-8. In these studies nonunion rates
vary from 0% to 7.2%, but average 3.6%, and avascular necrosis varies
from 2.5% to 40.9%, but averages 24.2%. A recent metaanalysis59
estimated the overall rates of nonunion and avascular necrosis to be
8.9% and 23%, respectively. Although intuitively early reduction and
fixation would seem advisable, there is no
strong relationship between timing of surgery and nonunion or avascular necrosis. In their series, Jain et al.118
reported no AVN in 15 patients fixed within 12 hours compared with 26%
in patients with a delay to fixation (6/23). Nonetheless, in another
large series255 and in a meta-analysis of the literature,59
there was no relationship between the timing of surgery and development
of nonunion or AVN. The quality of reduction has an influence on the
rate of complications. In particular, a varus reduction has been shown
to be associated with a 13-fold increase in the likelihood of fixation
failure.44
|
TABLE
47-8 The Results of Studies Investigating Reduction and Internal Fixation of Displaced Femoral Neck Fractures in Patients Less Than 60 Years Old |
||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
reported that the nonunion rate with fixed angle devices was 8%
compared with 19% with sliding devices. The numbers in the study were
not large, but a fixed angle device may be a better choice for these
very unstable patterns in younger patients.
Nonetheless, it may occur as an iatrogenic injury because of
injudicious placement of the proximal entry point for antegrade femoral
nailing. Between 2% and 6% of femoral neck fractures in young adults
have an ipsilateral hip fracture.2,252,269,270
The injury is easily missed, particularly if the fracture is
undisplaced or the radiographs of the proximal femur are inadequate or
of poor quality. Careful scrutiny of the radiographs is necessary in
all cases. If the fracture is recognized before surgery, the options
are:
-
Antegrade femoral nailing with a cephalomedullary nail, allowing simultaneous fixation of the femoral neck and shaft
-
Fixation of the femoral neck fracture with cannulated screws and retrograde intramedullary nailing of the femoral shaft fracture
-
Fixation of the femoral neck fracture with cannulated screws and plating of the femoral shaft fracture
this situation the femoral neck fracture takes priority. It is very
important to reduce and fix this fracture anatomically. If the femoral
neck fracture is undisplaced I usually choose an antegrade
cephalomedullary femoral nail. If the femoral neck fracture is
displaced and any difficulty is anticipated in achieving a closed
reduction I prefer screw fixation for the femoral neck fractures
followed by retrograde nailing for the femoral shaft fracture. I
reserve plating of the femoral shaft fracture for cases where the shaft
fracture is in the distal third of the bone. The treatment of femoral
shaft fractures is discussed in Chapter 50.
with rheumatoid arthritis because of the osteoporosis associated with
the condition. In published reports the results of reduction and
fixation in these cases have been poor.105,239 Hadden et al.105
reported only eight satisfactory results in 27 displaced fractures in
rheumatoid patients treated with reduction and internal fixation.
Similarly, Stromqvist et al.239
reported complications in 19 of 20 displaced fractures treated by
reduction and fixation. The experience of other authors has been
similar.5,28,111
Unless the patient is very young or the fracture is undisplaced,
intracapsular hip fractures in these patients should be treated with an
arthroplasty. Satisfactory results have been reported with both bipolar
and total hip prostheses.
fractures or insufficiency fractures. The former occur in normal bone
as a result of repetitive cyclical loading and the latter occur in
osteoporotic bone secondary to normal physiologic loading. Fatigue
fractures most frequently occur in young adults, and have been reported
in military recruits, with an prevalence varying from 3% to 8%.87,196 Insufficiency fractures occur in elderly patients and are estimated to account for 2% to 3% of hip fractures.114
Most proximal femoral stress fractures are intracapsular in location.
The fracture is often incomplete and is located either on the superior
or inferior surface of the femoral neck (Fig. 47-18).
Fractures on the superior surface of the neck are tension fractures and
are more liable to become complete and displaced. They should be
treated with internal fixation. Compression fractures, on the inferior
surface of the femoral neck, are more common in younger patients. They
are inherently more stable and may initially be treated nonoperatively
with 6 to 8 weeks of protected weight-bearing. If the fracture
fails to heal internal fixation is indicated. Stress fractures are discussed further in Chapter 19.
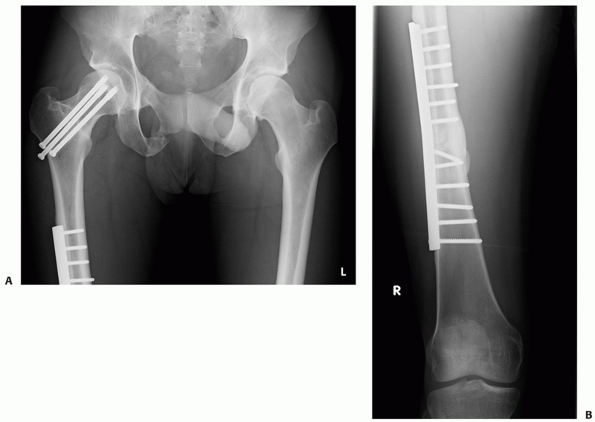 |
|
FIGURE 47-17 Ipsilateral femoral neck (A) and femoral shaft (B) fractures treated by plating and screw fixation.
|
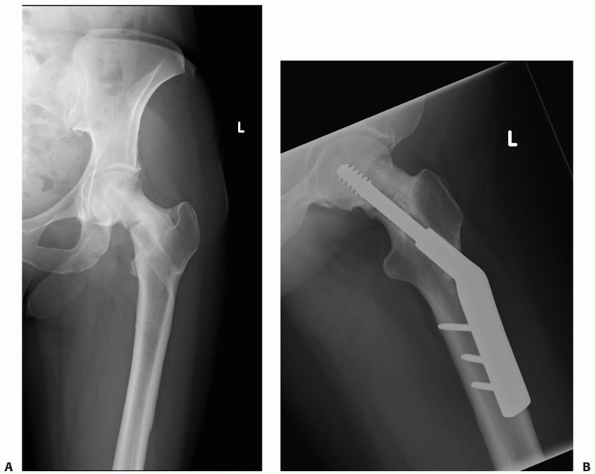 |
|
FIGURE 47-18 A.
AP and lateral radiographs of a 48-year-old woman with an inferior femoral neck stress fracture. The patient had previously undergone fixation of the fracture with a sliding hip screw but the fracture recurred after implant removal. B. The fracture healing after further sliding hip screw fixation. |
intertrochanteric or subtrochanteric fractures in Paget disease.
Nonetheless the disease can produce a coxa vara deformity and this is
associated with an increased risk of failure with reduction and
internal fixation. The results in the literature are strongly in favor
of arthroplasty for patients with Paget disease who present with a
displaced intracapsular fracture. Dove66 reported a nonunion rate of 75% after fixation, and Milgram161 and Grundy103
also reported a high complication rate after fixation. Although
arthroplasty is the preferred option, it is often not a straightforward
undertaking. The bone may be sclerotic and very vascular and the
surgery may be technically difficult. If the acetabulum is involved in
the disease process the results of hemiarthroplasty are not as good,12,167 and total hip replacement is a better choice.227
are less common than those in the pertrochanteric region. They should
be suspected in patients with a previous history of carcinoma with a
predilection for bony spread (lung, breast, prostate, kidney, thyroid),
those patients who present with minimal or no history of trauma, and
those with evidence of a lytic lesion in the femoral neck. Depending on
the location of the primary tumor, some additional preoperative
investigations and preparation may be necessary. Hypercalcemia may be
an accompanying feature that needs to be corrected before surgery.
Imaging of the rest of the skeleton is necessary to diagnose disease
elsewhere. It is particularly important to establish that the
ipsilateral femoral shaft is free of disease because the presence of
other metastatic lesions in the femur will clearly influence surgical
management.
fracture secondary to metastatic disease, an arthroplasty is the most
appropriate treatment. For patients with limited functional demands or
life expectancy, a bipolar hemiarthroplasty is a reasonable choice.
Patients with a more favorable prognosis and better function should be
considered for total hip arthroplasty. The presence of additional
lesions in the proximal femur may necessitate proximal femoral
replacement. Metastatic fractures are discussed further in Chapter 20.
or other neurologic conditions occasionally sustain a femoral neck
fracture. If this is undisplaced, then internal fixation is the
treatment of choice. Careful radiologic assessment of the femoral neck
is required. Some degree of dysplasia is often present. The femoral
neck and head are frequently hypoplastic, limiting the space for
implants. In cerebral palsy there is often marked anteversion of the
femoral neck, which needs to be anticipated when fixation is
undertaken. For patients with displaced fractures internal fixation may
still be the treatment of choice in younger patients. In older patients
an arthroplasty may be a better choice. Preoperative templating in
these patients is advisable to ensure that appropriate stem sizes are
available at the time of surgery.
a number of considerations: whether the fracture is displaced or
undisplaced and the age of the patient, in addition to the cognitive
state, functional demands, and the presence of other medical
comorbidities. A rational decision based on good clinical evidence can
be made for most of patients. My approach to treatment selection is
summarized in the algorithm illustrated in Fig. 47-19.
cannulated screw fixation irrespective of age or other considerations.
The majority of these fractures heal uneventfully after this treatment
and the procedure can be carried out with a very limited surgical
exposure associated with low postoperative morbidity. I generally use
three screws in parallel alignment on the AP and lateral views.
Although nonoperative treatment is an option, the risk of displacement
is considerable. Unless the patient presents late and is completely
asymptomatic I do not manage any of these injuries nonoperatively. I
follow up independently mobile patients until there is evidence of
fracture union.
with displaced fractures: younger patients; fit older patients; and
older patients with lower functional demands owing to cognitive
impairment, limited mobility, or medical comorbidities.
prefer early reduction and internal fixation with cannulated screws.
When feasible I operate as soon as possible after admission, although
the evidence in support of urgent surgical intervention is limted.
There is evidence to suggest that internal fixation up to 1 week after
fracture has similar results to procedures performed on an urgent
basis. Therefore I consider reduction and fixation in younger patients,
even those presenting within this time frame after injury. I prefer to
use cannulated screws rather than a sliding hip screw device with a
short side plate. There is no difference in outcome, but the cannulated
screws are a less bulky implant. I use three cannulated screws,
although as discussed the evidence that this is superior to the use of
two screws is limited. Implant position has been debated, but there is
evidence that parallel placement on the AP and lateral radiographs is
associated with good results. I usually place the screws in an
inferior, central, and superior position on the AP view and superimpose
them in the central portion of the head on the lateral view.
Postoperatively patients can be mobilized touch weight-bearing on
crutches. As has been discussed, non-weight-bearing mobilization is not
logical. This actually increases the forces across the hip in patients
who can comply, but most elderly patients are unable to tolerate
non-weight-bearing
mobilization
anyway. These patients require regular orthopaedic follow-up to ensure
that fracture healing occurs uneventfully and to detect complications,
particularly fixation failure, nonunion, and avascular necrosis. I
review younger patients at 6 weeks, 3 months, and 6 months
postoperatively. Thereafter I review patients on a 6-month basis until
they are 2 years postsurgery. If no complications are evident at this
stage, patients can be discharged. This follow-up schedule may be
impractical in older patients. Follow-up to fracture union is advisable
and patients can be referred back to the surgeon if complications
develop.
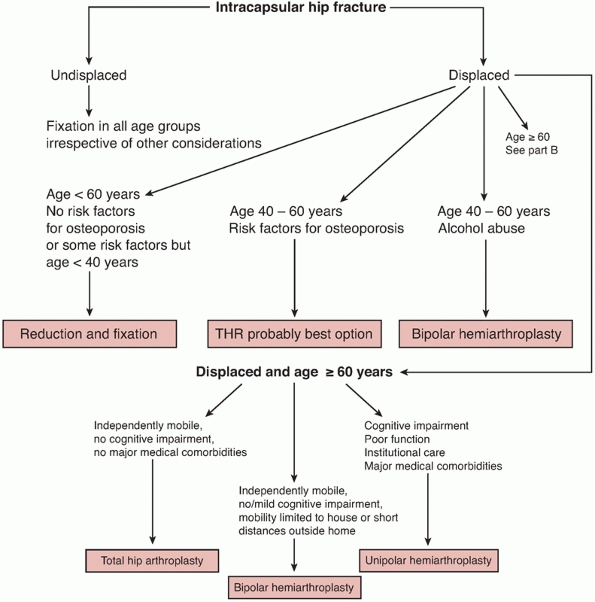 |
|
FIGURE 47-19 Algorithm for treatment of femoral neck fractures.
|
predisposing to osteoporosis or alcohol abuse, I often consider some
form of arthroplasty, particularly if the patient is more than 40 years
of age. The failure rate of internal fixation in these patients is very
high. Patients with renal failure, rheumatoid arthritis, or those who
are on long-term corticosteroid treatment are very poor candidates for
fixation. If the level of function is good in these patients I prefer
total hip arthroplasty. Patients with a history of chronic alcohol
abuse are at high risk for dislocation after total hip arthroplasty,
especially if alcohol withdrawal symptoms develop in the early
postoperative period. Consequently I treat the fracture in these
patients with a cemented bipolar hemiarthroplasty if there is evidence
of ongoing alcohol abuse at the time of admission.
there is now an accumulating body of evidence from randomized trials to
support the use of total hip arthroplasty for fit older patients with a
displaced intracapsular hip fracture. In patients more than 60 years
old who are independently mobile in the community, I now use this
treatment option as my first choice. Many surgeons might be reluctant
to consider total hip arthroplasty for patients in their sixties, but
the evidence from randomized trials indicates that failure of fixation
is no different from that in patients more than 70 years of age. The
functional outcome is also better after total hip arthroplasty.
a cemented total hip arthroplasty. I use a single dose of a broad
spectrum antibiotic at induction of anesthesia to prevent infection and
a low molecular weight heparin for DVT prophylaxis. Postoperatively,
patients are mobilized weight-bearing as tolerated. The risk of
dislocation is higher than with THR for osteoarthritis, and patients
need to be carefully instructed by the physiotherapist about
precautions to minimize the risk of dislocation. Because these patients
are fit and active, I routinely follow up at 6 weeks, 3 months, 6
months, and 1 year postoperatively to detect any postoperative
complications at an early stage.
with a displaced intracapsular hip fracture who are completely
independent community ambulators with no cognitive impairment merit
consideration of this treatment option. The recommendation to use total
hip arthroplasty applies to a very limted number of patients in most
orthopaedic units. An orthopaedic unit with a catchment population of
250,000 will treat 250 to 300 hip fractures a year. Half of these will
be intracapsular and 85% of this group will be displaced. Even with a
workload of 300 hip fractures per year, only about 20 patients would
fulfill the criteria for total hip arthroplasty.
female patients. The prevalence of significant medical comorbidities is
about 70%, and 25% to 30% have a degree of cognitive impairment. The
results of reduction and fixation are very poor in this group and I no
longer use this procedure for these patients. My preference is to use a
modern cemented bipolar hemiarthroplasty for the majority of these
patients. Although there is no evidence to support the use of a bipolar
prosthesis rather than a unipolar prosthesis I consider that the
modularity of modern bipolar prostheses is advantageous in achieving
correct leg length and soft tissue tension at the time of surgery. Even
patients with dementia may be mobile within the home environment or
community, and a modern cemented implant is associated with better
function than an older uncemented implant such as the Austin Moore or
Thomson hemiarthroplasty. The latter implants are now obsolescent.
Their use should be confined to patients with very limited mobility who
are institutionalized in whom the main objective of surgery is pain
relief rather than function.
prophylaxis are as described for total hip arthroplasty.
Postoperatively patients can be mobilized weight-bearing as tolerated.
Arrangements for follow-up of these patients will vary. If the patients
have been in the hospital for a sufficient duration of time to detect
early wound problems, I do not routinely follow them up as outpatients.
If there has been any wound problem, then early outpatient review is
advisable to detect any sign of deep infection.
-
Consider the possibility of predisposing
causes in younger patients that may contraindicate fixation such as
alcohol abuse, rheumatoid arthritis, or steroid use. -
Gentle positioning on the table is important to avoid increasing fracture displacement.
-
Employ cautious application of traction with slight internal rotation.
-
Avoid excessive traction to minimizes the risk of valgus reduction.
-
Three cannulated screws are adequate for fixation.
-
Avoid multiple drill holes in the lateral cortex, which increases the risk of postoperative subtrochanteric fracture.
-
Do not use older designs (Austin Moore/Thompson) in active patients.
-
Employ a lateral approach to minimize the risk of dislocation.
-
Cut the neck to allow collar support.
-
Carefully ream and insert the implant to avoid splitting the femur.
-
A modular prosthesis is preferred to achieve correct soft tissue tension and leg length.
-
If the femoral shaft splits during reaming, employ cerclage wires and convert to a cemented stem.
-
Employ a gentle reduction maneuver, avoiding excess rotational force to avoid femoral shaft fracture.
-
Use total hip arthroplasty in fit active patients without cognitive impairment.
-
Avoid total hip arthroplasty in alcohol abusers.
-
Use a lateral approach to minimize the risk of dislocation.
-
Cautiously ream the acetabulum to avoid medial wall penetration or overreaming of the anterior/posterior wall.
-
Consider using an uncemented prosthesis in patients with cardiovascular morbidity to minimize the risk of cement reaction.
-
Displaced or undisplaced fracture
-
Age of patient
-
Cognitive state
-
Functional demands
-
Medical comorbidity
-
Conditions/medication predisposing to osteoporosis
The results from clinical trials, reported series, hip fracture audits,
and national databases or joint registries estimates a 15% hospital
mortality and 30% mortality at 1 year. There is no significant
difference in mortality rates for pertrochanteric and intracapsular
neck fractures.95 These mortality rates are four to five times higher than in the comparable non-hip fracture population of the same age.272
In patients with significant cognitive impairment, the 1 year mortality
rises to 50%. Not surprisingly, the presence of concomitant medical
comorbidities increases the risk of death after surgery. This applies
particularly to patients with significant cardiorespiratory conditions.70,129,164,193 Renal impairment with elevated urea and creatinine was associated with double the 1-year mortality in one study.143 Women have a lower rate of mortality than men.129,138,164,193,209 The mortality rates for undisplaced fractures are higher if they are treated with a hemiarthroplasty as opposed
to internal fixation. Sikand et al.225 reported a 38% mortality at 1 year after hemiarthroplasty compared with 11% for fixation for undisplaced fractures.
operative workload of orthopaedic trauma, and delays to surgery are
common because of the volume of cases. The relationship of mortality to
delay to surgery remains controversial. Dolk63
analyzed a small series and found no difference in mortality between
patients who had immediate surgery and those who had surgery up to 48
hours after admission. Orosz et al.175
compared mortality and complication rates in patients having surgery
within 24 hours and after that period. They found no difference in
mortality or functional outcome, but patients who had early surgery had
less pain and a showed a trend to lower complication rates. Similarly,
larger population studies have not shown any reduction in mortality if
surgery is performed within 24 hours of admission.152,243 Nonetheless, a number of studies have looked at longer delays. Doruk65 reported a significant increase in mortality with delays beyond 5 days, and Moran et al.162
found a significant increase in mortality with delays beyond 4 days. It
may be that shorter delays are important but the effect is less and has
not been picked up in these studies with cohorts of 2000 to 4000
patients.
found an odds ratio of 1.27 increase in mortality for a 24-hour delay
to surgery after adjustment for comorbidity. Based on the available
evidence, it seems that mortality can be reduced with early surgery,
and the aim for most patients should be to have surgery within 48 hours
of admission.
influence mortality, but the effect is weaker than might be expected.
Bhandari et al.18 assessed this in a meta-analysis of studies comparing arthroplasty with fixation.*
The average mortality rates in the first 4 months were 9% (range, 4% to
20%) for arthroplasty compared with 6% (range, 0% to 12%) for fixation.
At 1 year the average mortality rates were 23% (range, 4% to 48%) for
arthroplasty compared with 20% (range, 0% to 65%) for fixation. These
slight differences did not achieve statistical significance. The type
of arthroplasty used had no influence.
with internal fixation than arthroplasty. The operation is shorter,
requires a minimally invasive surgical exposure, and the implants used
are smaller. In comparative studies infection rates after internal
fixation range from 0% to 10% compared with arthroplasty infection
rates of 0% to 18%.18 Infection
after internal fixation usually has less serious consequences than deep
infection after arthroplasty. Removal of the implants after fracture
healing may be all that is required. There is also the option of later
conversion to arthroplasty if the fracture fails to unite. Deep
infection after arthroplasty is a very difficult management problem in
these elderly frail patients. The options of excision or exchange
arthroplasty are further major interventions and are likely to be
poorly tolerated in patients with medical comorbidities. Excision
arthroplasty to control infection is generally associated with very
poor postoperative mobility. Older patients are usually wheelchair
bound after this procedure. Immediate exchange arthroplasty has quite
good results after arthroplasty for osteoarthritis with eradication of
infection in 85% of cases. The results are not likely to be as good in
the hip fracture population, as this population is much frailer;
However, there is little published information about this problem.
or total hip arthroplasty has to take a number of factors into account,
including the age of the patient as well as functional demands, medical
comorbidities, and the infecting organism. If the organism is sensitive
to common antibiotics, one option is nonoperative management if the
patient is frail with an attempt being made to suppress the infection
with low-dose antibiotic therapy. Unfortunately, organisms such as MRSA
are relatively frequent in this population and this organism is a
common cause of deep infection in these cases.159
Nonoperative management with antibiotic suppression is less likely to
be successful in the presence of this or other resistant organisms.
hip with replacement of some of the implant, such as the the bipolar
head, if applicable. In some patients deliberate creation of a fistula
to allow drainage in the inferior part of the wound is an option if
excision and reimplantation are not planned in the short to medium
term. In fitter patients who can tolerate more major surgery, my
preference is to carry out an excision arthroplasty and reimplantation
when the infection is under control. This is also the best option for
infections resulting from resistant organisms in which antibiotic
suppression options may be limited, or where they are unwanted side
effects of antibiotic therapy. Posttraumatic osteomyelitis is discussed
further in Chapter 24.
complication of hip fracture and the surgery required to treat the
injury. Zahn et al.273 found
venographic evidence of deep venous thrombosis (DVT) in 13/21 (62%) of
patients whose surgery had been delayed beyond 48 hours. Other authors
have estimated that one third to one half of patients with a hip
fracture will develop DVT.104,218 Nonetheless, larger studies244 have indicated that the prevalence of symptomatic DVT may be lower than this. Todd250 recorded a 6% prevalence of DVT and a 2% prevalence of fatal pulmonary embolism. In a review of the literature Gillespie et al.94
reported that radiographically proved DVTs occurred in 45% and
clinically apparent DVT in 7% of patients. Nonfatal pulmonary emboli
occurred in 8% and fatal pulmonary emboli in 4% of patients. There is
an accumulating body of evidence to support the view that DVT
prophylaxis is effective in reducing the risk of DVT in patients with
hip fracture. The most commonly used options for prophylaxis after hip
fracture include aspirin, heparin, dextran, and pneumatic compression
devices.
compression devices has been shown to reduce the risk of asymptomatic
deep venous thrombosis after hip fracture in a meta-analysis108 of trials assessing the effectiveness of these devices. The prevalence of DVT was reduced from 19% to
6%. There was no demonstrable effect on symptomatic DVT or mortality.
heparin or low molecular weight heparin. Aspirin has been shown to be
more effective than placebo in DVT prevention. A meta-analysis of trials108
using aspirin has indicated that it is effective in reducing
asymptomatic DVT (42% to 36%), symptomatic DVT (1.5% to 1%), all
pulmonary emboli (1.6% to 0.8%), and fatal pulmonary emboli (0.8% to
0.4%). These conclusions were based mainly on the largest trial, which
was the PEP study198 in which the authors calculated that aspirin prevented four fatal pulmonary emboli per 1000 hip fracture patients.
carried out a meta-analysis of 31 trials evaluating various
combinations of heparin and pneumatic compression devices.
Unfractionated and low molecular weight heparins reduced the incidence
of DVT from 42% in control groups to 26%. There was no demonstrable
reduction in either pulmonary embolism or mortality. Five trials
compared unfractionated and low molecular weight heparin, but no
conclusive differences were shown. Five trials of mechanical pumping
devices were methodologically flawed but appeared to show a reduction
in the incidence of DVT (7% vs. 22%). Compliance may be an issue with
these devices.
 |
|
FIGURE 47-20 A. AP and lateral (B) radiographs of an undisplaced intracapsular hip fracture. C. AP radiograph at 3 months showing collapse with loss of fixation and nonunion.
|
hip fracture patients. Many of these patients are already elderly and
are taking multiple pharmacologic agents, and the risks associated with
warfarin administration make it an unpopular choice for this group.
agent (heparin, aspirin, or mechanical pumps) is justified, as these
agents appear to protect against DVT after hip fracture. There is some
evidence that the risk of pulmonary embolus is reduced, but this is
uncertain. Based on current evidence, low molecular weight heparin or
aspirin is probably the safest choice for thromboprophylaxis in
patients with a femoral neck fracture, supplemented by a pneumatic
compression device if this is tolerated by the patient.
are the main modes of failure after fixation of displaced or
undisplaced femoral neck fractures. The two problems are difficult to
distinguish because most displaced fractures take a long time to heal
after fixation, which increases the risk of fixation failure. The
incidence is low in undisplaced fractures, and failure of fixation is
a rare complication. Nonunion is more common, and is reported to be between 3.1% and 8.8% but averages about 6% (Table 47-1) . Both complications are much more frequent after reduction and fixation of displaced fractures (Table 47-2). The incidence of nonunion and/or fixation failure requiring revision surgery averages about 40% in displaced fractures (Table 47-4).
the patient presents with increasing hip pain, shortening of the leg
owing to collapse and loss of reduction, and radiologic evidence of
fixation failure. In the majority of cases the best option for
treatment is conversion to an arthroplasty. In fit patients I prefer
total hip replacement. In older patients conversion to a
hemiarthroplasty is an alternative if the acetabulum is normal.
Infection is an occasional contributory cause and should be considered
in all cases. If there is any evidence of infection, excision
arthroplasty may have to be considered in the first instance with an
arthroplasty undertaken at a later stage.
to either a hemi- or total arthroplasty is a straightforward solution
to the problem. Studies that have compared the outcome of primary
versus revision fixation do not bear this out.15,24,84,157
The rates of dislocation and infection are approximately double those
seen after primary arthroplasty for femoral neck fracture. The
functional outcome is also inferior and there is evidence that the
survivorship of these revision prostheses is shorter. In one randomized
trial comparing internal fixation with bipolar and total hip
arthroplasty, the arthroplasty complication rate in the fixation group
was identical to the two arthroplasty groups, reflecting the higher
rates of arthroplasty complications in patients with failed fixations
converted to arthroplasty.130
be the ideal first choice, particularly if the patient is under 40
years and has no other medical comorbidities. In these patients the
alternatives include revision of fixation, a vascularized bone graft,
or a valgus osteotomy if the nonunion or fixation failure is recognized
before complete displacement of the head occurs.237
Revision of fixation augmented by a vascularized bone graft is a
reasonable option if there has been no loss of reduction. Meyers et al.160 described the use of a vascularized quadratus femoris graft to prevent avascular necrosis after femoral neck fracture (Fig. 47-21). It is now more commonly used to achieve union in patients with delayed or nonunion,264 and has been reported to be successful in achieving union in 95% of cases.
posterior capsulotomy is performed. The femoral neck nonunion is
identified and all fibrous tissue cleared from the nonunion site. The
quadratus femoris insertion on the posterior aspect of the femur is
elevated with a length of 4 cm, a width of 1.5 cm, and a depth of 1 cm.
A trough to receive the bone block is cut into the posterior aspect of
the femoral neck bridging the nonunion site. The bone block is placed
in the trough and fixed in place with screws.
presents with some loss of reduction with the femoral head displacing
into a varus position. In this situation the best option is a proximal
femoral valgus osteotomy.192,237
This procedure converts the fracture plane from a vertical orientation
to a transverse one with compression created at the site of the
nonunion (Fig. 47-22). Careful preoperative
planning is necessary. The usual aim is to change the femoral neck
angle to 150 degrees. This degree of correction is sufficient to
restore the fracture to a transverse orientation in most cases. A blade
plate is the most popular fixation device for this procedure. I
generally use a 130-degree blade plate, but the exact implant depends
on the correction required. The channel for the blade is made before
the osteotomy, which is carried out at the level of the lesser
trochanter. A wedge of bone is then excised to achieve the correction
and the blade plate is used to fix the osteotomy. Marti et al.154
reported on 50 younger patients treated with this technique. Seven
failed and required conversion to an arthroplasty. The remainder healed
but there was radiographic evidence of AVN in 22 (44%) at a mean
follow-up of 7 years, although most of the patients with this
complication were reported to be asymptomatic. More recently Sringari237 reported union in 18 of 20 (90%) patients treated with a valgus osteotomy.
show that avascular necrosis is a well-recognized complication of
femoral neck fracture, but is not frequently encountered in clinical
practice. This is because of a gradual increase in the use of
arthroplasty rather than internal fixation to treat these injuries over
the past two decades. The declining incidence of this complication is
reflected in three studies published in separate decades. Barnes et al.,11
in a study of more than 1500 femoral neck fractures treated by internal
fixation reported an incidence of AVN in 24% of women and 15% of men.
The incidence was lower in undisplaced fractures (16%) compared with
displaced fractures (27.6%). In the meta-analysis of Lu-Yao et al.,149
the incidence of fixation failure and nonunion was 33% compared with a
rate of AVN of 16% (95% CI 11% to 19%). By the time of publication of
the meta-analysis of Bhandari et al.,18
the reported rate of AVN had declined to a mean of 6.9% (range, 0% to
22%). There are several possible explanations for the decline in the
incidence of this problem. There has been a gradual reduction in the
widespread use of reduction and fixation for displaced fractures. The
incidence of AVN is lower with undisplaced fractures. Surgeons may now
be choosing patients more carefully for reduction and fixation so that
only patients with a favorable prognosis are treated with this
technique.
radiographic appearances, but these may not be evident for a long
period of time. Single photon-emission computed tomographic (SPECT)
scanning has been shown to be an accurate predictor of AVN if uptake is
less than 90%.240 MRI scanning will
detect the problem before plain radiographs but it is not an accurate
predictor of AVN in the early weeks after injury.7,236
Fractures treated by reduction and fixation take a long time to heal
and AVN usually presents after union. Barnes et al.11
noted it to be most common in the second year after injury, but
presentation later than this may occur occasionally. The occurrence of
AVN does not always require intervention. Barnes et al. reported that
of their cases, 24.3% were asymptomatic and 46.4% had
an
acceptable level of disability. This left 29.2% of patients with
significant disability; 60% of these underwent further surgery. More
recent studies have reported very similar rates of asymptomatic
patients who require no surgery.168
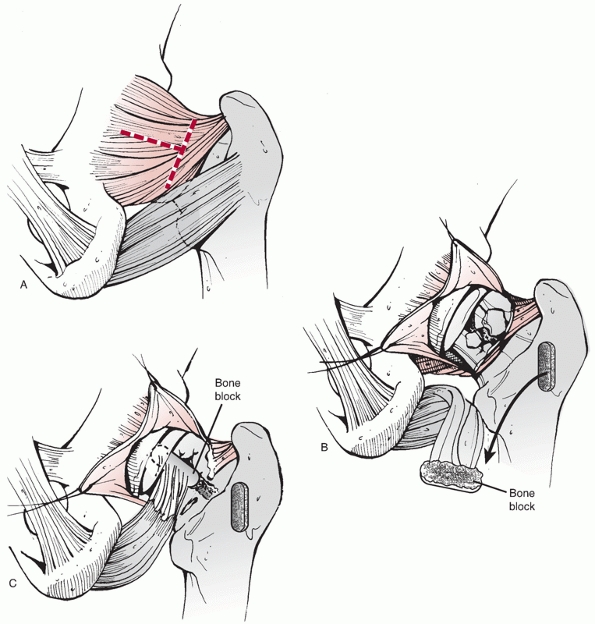 |
|
FIGURE 47-21 Meyer’s graft. A. “T” incision of the posterior capsule. B. Mapping out the quadratus femoris graft. C.
The trough is curetted out from the intertrochanteric line up into the femoral head. A small tunnel is created up under the articular surface of the femoral head to lever the graft into position. Once the graft is inserted, a 3.5-mm cancellous screw and washer are inserted from posterior to anterior to compress the graft and support the comminuted posterior cortex. |
typical radiographic signs of increased femoral head density or
collapse. In symptomatic cases, the usual treatment option is
conversion to an arthroplasty. For most patients a total hip
arthroplasty is the best choice because the segmental collapse of the
head is often associated with degenerative changes in the acetabulum.
Furthermore, many patients now treated with reduction and fixation are
young and the best long-term outcome is probably associated with a
modern total hip prosthesis. If the acetabular surface is well
preserved or the patient is elderly with limited functional demands or
medical comorbidities, then a hemiarthroplasty is a reasonable
alternative.
show that dislocation rates with unipolar hemiarthroplasties and
bipolar hemiarthroplasties are similar and average about 3%. As
discussed, the dislocation rate after total hip arthroplasty is higher
than the rate reported for hemiarthroplasty. Nonetheless the incidence
of dislocation after total hip arthroplasty has declined steadily.
Lu-Yao et al.149 quoted a rate of 11%, which declined to 6% in the subsequent meta-analysis of Bhandari et al.18
In more recent randomized trials evaluating the use of total hip
arthroplasty for femoral neck fracture the prevalence has been similar (Table 47-3).
There may be a number of contributory factors to explain the decline in
reported dislocation rates after THR. There has been a tendency to
avoid using implants with small femoral heads, such as the Charnley
prosthesis, which are associated with higher dislocation rates. Another
factor that may contribute to the lower prevalence of dislocation is
the availability of more surgeons with specific arthroplasty expertise
to carry out the procedure.
patients undergoing arthroplasty for osteoarthritis. Technical errors
at the time of surgery with implant malposition are perhaps the
most
common cause. Older prostheses such as the uncemented Austin Moore may
loosen and change position if the patient is active or has another
fall. Patient noncompliance with the usual arthroplasty precautions is
more common in this group than in the osteoarthritic group.
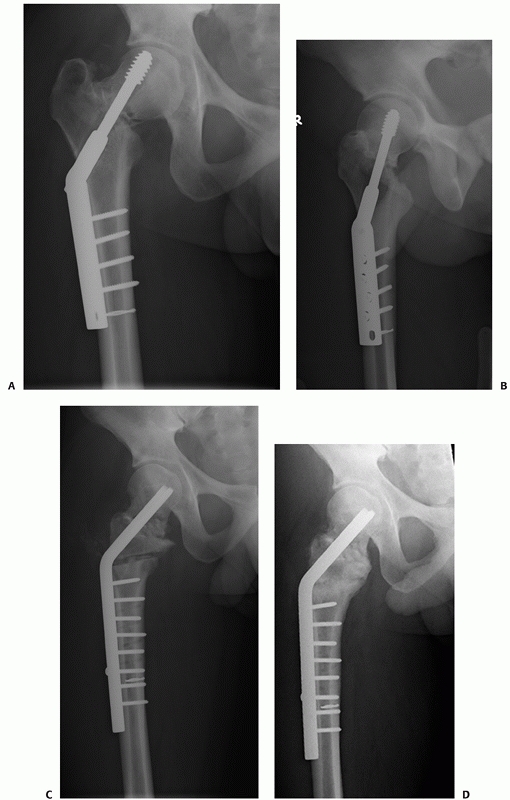 |
|
FIGURE 47-22 (A,B)
AP and lateral radiographs of a displaced intracapsular hip fracture 4 months after treatment with a sliding hip screw that has been inserted incorrectly. The fracture has not been reduced and coxa vara is present. The hip screw is too high and the plate is unnecessarily long. C. AP radiograph showing correction of deformity with a valgus osteotomy. A 130-degree blade plate was used with a closing wedge subtrochanteric osteotomy to change the femoral neck angle to 150 degrees. D. AP radiograph 9 months after osteotomy. The osteotomy and the femoral neck fracture have united and there is no sign of avascular necrosis. |
total hip implants. The bipolar hemiarthroplasty is much more difficult
to reduce closed, although it is usually worth attempting. A particular
risk with closed reduction of bipolar implants is dissociation of the
bipolar head from the stem, which makes closed reduction impossible. In
cases of recurrent dislocation or irreducible dislocation an open
reduction is required. In this situation careful preoperative planning
is necessary. It may be obvious from the preoperative assessment there
is a malposition of the orginal implant, in which case revision of the
prosthesis is likely to be necessary to prevent further episodes of
dislocation.
arthroplasty surgery even in the hip fracture population. Long-term
follow-up studies of these patients are uncommon and consequently there
are limited data on loosening and revision rates. The high early
mortality, limited life expectancy, and elderly demographics of the
population undergoing arthroplasty for femoral neck fracture mean
long-term follow-up is uncommon. Ravikumar and Marsh204 reported mortality rates of 85% and 91%, respectively, for hemiarthroplasty and THR in a 13-year follow-up.
evaluated the survivorship of hemiarthroplasty. They recorded an
overall survivorship of 90% at 5 years and 85% at 10 years. The
prostheses studied were the Austin Moore, the Christiansen, and the
Hastings. The latter two are bipolar designs. The rate of loosening
after unipolar hemiarthroplasty has been higher than bipolar
hemiarthroplasty.271 The risk of
loosening after bipolar hemiarthroplasty is low. In five studies
reporting this outcome the revision rate for loosening was 1.6%.15,17,96,106,176
studied long-term outcome of THR for femoral neck revision and reported
93% 10-year survival and 76% 20-year survival. These results are
comparable with those reported for OA.
functional demands in the majority of these patients, the requirement
for late revision owing to aseptic loosening is low. Most revision
arthroplasties are needed within the first 2 years because of
dislocation or infection. The favorable long-term results of THR in the
few studies with sufficient follow-up may reflect a bias in patient
selection, as the operation is usually considered for fitter patients,
who may be expected to have a lower risk of early complications and a
better prospect of longer-term survival.
concentrated on surgical measures of outcome rather than functional
measures. Older studies tend to use fairly crude outcome measures, such
as pain and level of mobililty, which are documented in a rudimentary
fashion.
reported that patients had better outcomes after either
hemiarthroplasty or total hip arthroplasty. Overall 71% of patients
with reduction and internal fixation had no pain at 2 years, compared
with 86% of patients after bipolar hemiarthroplasty, and 90% of
patients with a total hip arthroplasty. Data from studies published up
to that time had insufficient long-term data to document pain after the
2-year postinjury period. An analysis of more recent, larger trials
shows an emerging pattern favoring a better functional outcome
following modern designs of arthroplasty. A comparison of internal
fixation with an uncemented Austin Moore hemiarthroplasty showed that
pain was greater at 1 year with the hemiarthroplasty.22,184 In a three-way comparison of the Austin Moore with fixation and cemented hip replacement, Skinner et al.231
reported a higher incidence of pain at 1 year in the Austin Moore group
(12% vs. 27%). Nonetheless, in trials comparing cemented implants with
fixation, pain was significantly less at 4 months and 1 year in the
arthroplasty groups compared with fixation.130,131,213,249
subcapital fractures tend to regain mobility better than those with
displaced fractures. Most patients with undisplaced fractures return to
their previous level of mobility unless there are complications.
Patients with displaced femoral neck fractures have a less favorable
outcome in this respect. Poor prognostic factors for return of mobility
are increasing age, cognitive impairment, and any degree of impaired
mobility before fracture. The choice of treatment also influences
mobility. Some trials comparing internal fixation with arthroplasty in
displaced fractures have shown superior levels of mobility in patients
in the arthroplasty groups. This probably reflects the high rate of
early complications in patients treated with reduction and fixation.
This consideration must be set against the relatively short-term
follow-up in many of these trials, which may bias assessment in favor
of arthroplasty. Nonetheless, one might expect that with a 2-year
follow-up, which is a feature of more recent larger trials, the effect
of early complications in the fixation group might dissipate. This is
the case, and overall the proportion of patients regaining their
previous level of mobility after fixation or arthroplasty is 46%.119,184,213,231,249
Even in these trials mobility was still poorer in the fixation groups
at 2 years. In a longer-term follow-up of arthroplasty versus fixation,
Blomfeldt et al.25 did not demonstrate any improved mobility in the fixation group.
hemiarthroplasty have tended to indicate better levels of mobility with
the total hip arthroplasty group. The reasons for this are unclear and
may be multifactorial. More clinical data are needed. The reduction in
mobility no doubt contributes to the fact that between 15% and 20% of
patients do not return to their previous residence.119,184
reviewed the literature and carried out a cost-effectiveness analysis
based on reported outcomes. They predicted that arthroplasty would be
more cost-effective than reduction and fixation. The studies, which
have incorporated an assessment of the economic cost of treatment
modalities, have tended to analyze and compare the hospital costs of
fixation or arthroplasty. Soreide235 found bipolar hemiarthroplasty to be 1.6 times more expensive than fixation, and Johansson et al.121
found no difference in cost between fixation and total hip replacement.
These findings are in distinction to the other published work, which
has generally shown fixation to be the more expensive option. Parker et
al.184 found that three AO screws
were more expensive than the uncemented Austin Moore hemiarthroplasty.
Two randomized trials have been published that incorporated an economic
analysis. Rogmark et al.214 reported that arthroplasty (total or hemi) was more cost-effective than reduction and fixation. Keating et al.130,131
compared the costs of THA with cemented bipolar hemiarthroplasty and
fixation. Over a 2-year follow-up period THA was the most
cost-effective procedure. The poor economic performance of fixation
against arthroplasty in these studies is explained by the high rate and
cost of revision surgery in this group. Although the implant costs
associated with reduction and fixation are clearly less, the main
burden of expenditure in these patients is accounted for by the
duration of hospital stay. This has not been found to be any shorter
for reduction and fixation compared with arthroplasty, and the costs
associated with high readmission rates for revision surgery heavily
outweigh any financial advantage of the lower implant cost. Although
these findings might seem counterintuitive at first, it should be borne
in mind that in these patients the main cost driver is the duration of
time in hospital rather than the implant costs, which represent a small
percentage of the overall cost of treatment. The reason that fixation
has been shown to be more expensive in more detailed studies is that
the cost is driven up in this group by the high requirement for
revision surgery and subsequent readmission.
inexorable rise in the incidence of these fractures may be reaching a
plateau or even declining. Nonetheless there is no doubt that they will
continue to form a considerable component of the orthopaedic trauma
workload for the foreseeable future. Formerly the main controversy in
management of these fractures was centered on the debate of fixation
versus arthroplasty. Since publication of the 6th edition of Rockwood
and Green, there has been a gradual move within the orthopaedic
community toward the use of arthroplasty for a greater proportion of
these patients. Nonetheless, it seems likely that fixation will always
have a role in treatment of these fractures. It remains the treatment
of choice for younger patients with displaced fractures and for any
patient with an undisplaced fracture who is fit for surgery. The
optimum arthroplasty choice remains a source of debate. The bipolar
hemiarthroplasty is probably the most commonly used implant, but there
is no evidence that it is superior to a unipolar implant. Its continued
popularity is probably explained by the appeal of modularity to the
operating surgeon.
total hip arthroplasty is justified, as seems to be the case based on
recent comparative trials. There has been widespread use of old and
outmoded uncemented arthroplasties for these fractures. This may
account for the evidence supporting the use of cemented rather than
uncemented stems in these patients. Trials providing information on the
results of newer designs of modern uncemented prostheses can be
expected and may support their use. Nonetheless, the results may not be
comparable to their use in osteoarthritic patients. The majority of
patients with intracapsular fractures have osteoporosis and wide
femoral medullary canals, which may not be the ideal for uncemented
stems. Now that arthroplasty is established as the preferred treatment
method for the majority of these patients, clinical research is
required to provide evidence on which arthroplasty is associated with
the best functional outcome, the lowest economic tariff, and the lowest
incidence of surgical complications.
A. Concurrent ipsilateral fractures of the hip and femoral shaft: a
meta-analysis of 659 cases. Acta Orthop Scand 1996;67:19-28.
GH, Harper WM, Connolly CD, et al. Preoperative skin traction for
fracture of the proximal femur. J Bone Joint Surg Br 1993;75(5):794-796.
WD. The effect of early weight bearing on the stability of femoral neck
fractures treated with Knowles pins. J Bone Joint Surg 1984;66A:847-852.
T, Nagaya I, Miyake N, et al. The treatment of intracapsular hip
fractures with total hip arthroplasty in rheumatoid arthritis. Bull
Hosp Jt Dis 1993;53(2):29-33.
SE, Gould ES, Bansal M, et al. Magnetic resonance imaging of the hip
after displaced femoral neck fractures. Clin Orthop Relat Res
1994;(298):191-198.
RP, Squires B, Gargan MF, et al. Total hip arthroplasty and
hemiarthroplasty in mobile, independent patients with a displaced
intracapsular fracture of the femoral neck. A randomized, controlled
trial. J Bone Joint Surg Am 2006;88(12):2583-2589.
AP, Davison JK. Traumatic osteonecrosis of the femoral head following
intracapsular fracture:incidence and earliest radiological features.
Clin Radiol 1977;28: 407-414.
L, Kreder HJ, Berry GK, et al. Subcapital hip fractures: the Garden
classification should be replaced, not collapsed. Can J Surg
2002;45(6):411-414.
JG, Kok WL, Alho A. Primary and secondary Charnley-Hastings
hemiarthroplasty in displaced femoral neck fractures and their
sequelae. Ann Chir Gynaecol 1996;85(1):72-76.
SD, Samelson EJ, Hannan MT, et al. Second hip fracture in older men and
women: the Framingham Study. Arch Intern Med 2007;167(18):1971-1976.
HP, Shah AR, Harding SH, et al. Cementless bipolar hemiarthroplasty for
displaced femoral neck fractures in the elderly. J Arthroplast
2004;19(7 Suppl 2): 73-77.
M, Devereaux PJ, Swiontkowski MF, et al. Internal fixation compared
with arthroplasty for displaced fractures of the femoral neck: a
meta-analysis. J Bone Joint Surg Am 2003;85:1673-1681.
M, Devereaux PJ, Tornetta P 3rd, et al. Operative management of
displaced femoral neck fractures in elderly patients. An international
survey. J Bone Joint Surg Am 2005;87(9):2122-2130.
O, Karaeminogullari O, Kulecioglu A. Results of conversion total hip
prosthesis performed following painful hemiarthroplasty. J Int Med Res
2000;28(6):307-312.
R, Törnkvist H, Ponzer S, et al. Internal fixation versus
hemiarthroplasty for displaced fractures of the femoral neck in elderly
patients with severe cognitive impairment. J Bone Joint Surg Br
2005;87(4):523-529.
R, Törnkvist H, Ponzer S, et al. Comparison of internal fixation with
total hip replacement for displaced femoral neck fractures. Randomized,
controlled trial performed at four years. J Bone Joint Surg Am
2005;87(8):1680-1688.
R, Törnkvist H, Ponzer S, et al. Displaced femoral neck fracture:
comparison of primary total hip replacement with secondary replacement
after failed internal fixation: a 2-year follow-up of 84 patients. Acta
Orthop 2006;77(4):638-643.
R, Törnkvist H, Eriksson K, et al. A randomised controlled trial
comparing bipolar hemiarthroplasty with total hip replacement for
displaced intracapsular fractures of the femoral neck in elderly
patients. J Bone Joint Surg Br 2007;89(2):160-165.
CM, Parker MJ, Pryor GA, et al. Assessment of the AO classification of
intracapsular fractures of the proximal femur. J Bone Joint Surg Br
1998;80(4):679-683.
RM, Pellicci PM, Lyden JP. Bipolar hemiarthroplasty for fracture of the
femoral neck. Clinical review with special emphasis on prosthetic
motion. J Bone Joint Surg Am 1988;70(7):1001-1010.
E, Ouellette G, Hastings D. Failure of internal fixation of displaced
femoral neck fractures in rheumatoid patients. J Bone Joint Surg Br
1991;73(1):7-10.
A, Aylin P. Mortality associated with delay in operation after hip
fracture: observational study. BMJ 2006;332(7547):947-951. Epub 2006
Mar 22.
TJ, Smith-Hoefer E, Hooper A, et al. The displaced femoral neck
fracture. Internal fixation versus bipolar endoprosthesis. Results of a
prospective, randomized comparison. Clin Orthop 1988;230:127-140.
RN, Craig JS, Hinves BL, et al. Effect of femoral component head size
on movement of the two-component hemi-arthroplasty Injury
1993;24(4):231-235.
SJ, Anderson GH, Jagger C, et al. Unipolar or bipolar prosthesis for
displaced intracapsular hip fracture in octogenarians: a randomised
prospective study. J Bone Joint Surg 1996;78B:391-394.
M. A histological study of avascular necrosis of the femoral head after
transcervical fracture. J Bone Joint Surg 1965;47B:749-776.
M. The histological appearances of late segmental collapse of the
femoral head after transcervical fracture. J Bone Joint Surg
1965;47B:777-791.
HA, Osorio PQ, Comando D. Classification and diagnosis of intracapsular
fractures of the proximal femur. Clin Orthop Relat Res 2002
Jun;(399):17-27.
T, Guilley E, Herrmann FR, et al. Incidence of hip fracture over a
10-year period (1991-2000): reversal of a secular trend. Bone
2007;40(5):1284-1289. Epub 2007 Jan 4.
K, Howard LG, Potter TA, et al. A study of 104 consecutive cases of
fracture of the hip. J Bone Joint Surg 1953;35A:729-735.
D, Jaglal SB, Schatzker J. Predictors of early failure of fixation in
the treatment of displaced subcapital hip fractures. J Orthop Trauma
1998;12:230-234.
DI, Crofts CE, Saleh M. Femoral neck fracture fixation. Comparison of a
sliding screw with lag screws. J Bone Joint Surg 1990;72B:797-800.
M, Bruckner J. The outcome of Austin Moore hemiarthroplasty for
fracture of the femoral neck. Am J Orthop 1997;26:681-684.
KS, Parker MJ. Undisplaced intracapsular hip fractures: results of
internal fixation in 375 patients. Clin Orthop Relat Res 2004
Apr;(421):249-254.
CN, Levine D, O’Doherty J, et al. Unipolar versus bipolar
hemiarthroplasty for the treatment of femoral neck fractures in the
elderly. Clin Orthop 1998;348:67-71.
N, Loveridge N, Parker M, et al. Intracapsular hip fracture and the
regionspecific loss of cortical bone: analysis by peripheral
quantitative computed tomography. J Bone Miner Res 2001;16(7):1318-1328.
PT, Khan RJ, MacDowell A, et al. A survey of the treatment of displaced
intracapsular femoral neck fractures in the UK. Injury
2002;33(5):383-386.
P, Kazár G, Manninger J, et al. Non-operative or operative treatment
for undisplaced femoral neck fractures: a comparative study of 122
non-operative and 125 operatively treated cases. Injury
1996;27(8):583-588.
SR, Black DM, Nevitt MC, et al. Bone density at various sites for
prediction of hip fractures. The Study of Osteoporotic Fractures
Research Group. Lancet 1993; 341:72-75.
SR, Cauley JA, Palermo L, et al. Racial differences in hip axis lengths
might explain racial differences in rates of hip fracture. Osteoporosis
Int 1994;4:226-229.
DS, Parker MJ, Chojnowski A. Complications after intracapsular hip
fractures in young adults. A meta-analysis of 18 published studies
involving 564 fractures. Injury 2005;36(1):131-141.
P, Favier F, Grandjean H, et al. Fall related factors and hip fracture:
the EPIDOS prospective study. Lancet 1996;348:145-149.
JN, Calder SJ, Anderson GH, et al. Treatment for displaced
intracapsular fracture of the proximal femur: a prospective, randomised
trial in patients aged 65 to 79 years. J Bone Joint Surg
2001;83B:206-212.
LD, Glousman R, Hoy AL, et al. Treatment of femoral neck fractures with
total hip replacement versus cemented and noncemented hemiarthroplasty.
J Arthroplast 1986;1(1):21-28.
H, Mas MR, Yildiz C, et al. The effect of the timing of hip fracture
surgery on the activity of daily living and mortality in elderly. Arch
Gerontol Geriatr 2004;39(2): 179-185.
N, Nilsson LT, Strömqvist B, et al. Hemarthrosis after femoral neck
fracture fixation. Acta Orthop Scand 1988;59(5):526-529.
S, Ostgrd SE. Risk factors influencing mortality after bipolar
hemiarthroplasty in the treatment of fracture of the femoral neck. Clin
Orthop Relat Res 1991 Sep;(270): 295-300.
L, Gullberg B, Alexander E, et al. Methodology of Medos-Multicenter
study of hip fracture incidence: Validity and relevance consideration.
Bone 1993;14:S45-49.
RJH, Broughton NS, Desai K, et al. Bipolar hemiarthroplasty for
subcapital fracture of the femoral neck. A prospective randomized trial
of cemented Thompson and uncemented Moore stems. J Bone Joint Surg
1991;73B:322-324.
PD, Wilson C, Lyons K. Comparison of MRI with bone scanning for
suspected hip fracture in elderly patients. J Bone Joint Surg
1994;76B:158-159.
J, Colhoun E, Johnston D, et al. Bone scanning for suspected hip
fractures. A prospective study in elderly patients. J Bone Joint Surg
1987;69B:251-253.
MA, Orkazai SH, Okusanya O, Devitt AT. Intracapsular fractures of the
femoral neck in younger patients. Ir J Med Sci 2005;174(4):42-45.
PA, Andersen PE, Christoffersen H, et al. Osteosynthesis of femoral
neck fracture: the sliding screw plate with or without compression.
Acta Orthop Scand 1984; 55(6):620-623.
PA, Andersen E, Madsen F, et al. Garden’s classification of femoral
neck fractures. An assessment of inter observer variation. J Bone Joint
Surg 1988;70B: 588-590.
H, Nilsson LT, Stromqvist B, et al. Secondary total hip replacement
after fractures of the femoral neck. J Bone Joint Surg Br
1990;72(5):784-787.
MAR, Todd RC, Pirie CJ. The role of fatigue in the pathogenesis of
senile femoral neck fractures. J Bone Joint Surg 1974;56B:698-702.
F, Madsen JE, Aksnes E, et al. Comparison of re-operation rates
following primary and secondary hemiarthroplasty of the hip. Injury
2007;38(7):815-819. Epub 2006 Dec 4.
F, Nordsletten L, Madsen JE. Hemiarthroplasty or internal fixation for
intracapsular displaced femoral neck fractures: randomised controlled
trial. BMJ 2007; 335(7632):1251-1254. Epub 2007 Dec 4.
VK, Anand S, Dhaon BK. Management of displaced femoral neck fractures
in young adults (a group at risk). Injury 1998;29(3):215-218.
CA, Kozin SH, Levy AS, Brody LA. The use of MRI in the diagnosis of
occult hip fractures in the elderly: a preliminary review. Orthopedica
1994;17:327-330.
E, Ganz K, Krügel N, et al. Anatomy of the medial femoral circumflex
artery and its surgical implications. J Bone Joint Surg Br
2000;82(5):679-683.
W, Murray D, Gregg P, et al. Risks and benefits of prophylaxis against
venous thromboembolism in orthopaedic surgery. J Bone Joint Surg
2000;82B:475-479.
VB, Lyden JP, Cornell CN, Bochner RM. Bipolar hemiarthroplasty for
fracture of the femoral neck. J Orthop Trauma 1991;5(3):318-324.
DH. The evolution of a personal philosophy for the treatment of
displaced subcapital fractures. J Bone Joint Surg 1988;70(Br)1:161.
CG, Jones JR. Primary total hip replacement for displaced subcapital
fracture of the femur. J Bone Joint Surg Br 1988;70(4):639-643.
JA, Kelsey JL, Strom BL, et al. Risk factors for falls as a cause of
hip fracture in women. The Northeast Hip Fracture Study Group. N Engl J
Med 1991;324:1326-1331.
DA, Berkman SA. Venous thromboembolic disease after hip surgery. Risk
factors, prophylaxis and diagnosis. Clin Orthop Relat Res
1989;242:212-231.
GJ, Israel TA, Berry DJ. Long-term survivorship of cemented bipolar
hemiarthroplasty for fracture of the femoral neck. Clin Orthop Relat
Res 2002;(403): 118-126.
GJ, Rothwell WS, Jacofsky DJ, et al. Operative treatment of femoral
neck fractures in patients between the ages of fifteen and fifty years.
J Bone Joint Surg Am 2004;86-A(8):1711-1716.
HH, Farrar MJ, McBirnie J, Tet al. Heparin, low molecular weight
heparin and physical methods for preventing deep vein thrombosis and
pulmonary embolism following surgery for hip fractures. Cochrane
Database Syst Rev 2002;(4):CD000305.
WM, Gregg PJ. The treatment of intracapsular proximal femoral
fractures: a prospective randomised trial (Abstract). J Bone Joint Surg
1992;74(Suppl 3):282.
MY, Shinomiya F, Okada M, et al. Intracapsular hip fractures in
patients with rheumatoid arthritis. Int Orthop 2003;27(5):294-297.
M, Adunski A, Chechick A. Nonoperative treatment of intracapsular
fractures of the proximal femur. Clin Orthop Relat Res 2002
Jun;(399):35-41.
JP, Meadows TH, Davies DR, et al. A radiological assessment of
interprosthetic movement in the Charnley-Hastings hemiarthroplasty.
Injury 1988;19(1):18-20.
WW, Lacey T, Schwartz RP. A study of the gross anatomy of the arteries
supplying the proximal portion of the femur and acetabulum. J Bone
Joint Surg Am 1950; 32-A:856-866.
R, Healy WL, Lemos DW, et al. Displaced femoral neck fractures in the
elderly: outcomes and cost effectiveness. Clin Orthop Relat Res
2001;(383):229-242.
R, Schwartz B, Macaulay W, et al. Surgical treatment of displaced
femoral neck fractures in the elderly: a survey of the American
Association of Hip and Knee Surgeons. J Arthroplast
2006;21(8):1124-1133.
R, Koo M, Kreder HJ, et al. Comparison of early and delayed fixation of
subcapital hip fractures in patients sixty years of age or less. J Bone
Joint Surg Am 2002;84-A(9): 1605-1612.
J, Rasmussen T, Christensen S, et al. Internal fixation or prosthetic
replacement in fresh femoral neck fractures. Acta Orthop Scand
1984;55:712.
R, Doshe A, Karlsson J. Preoperative treatment in patients with hip
fractures is not useful. Clin Orthop Relat Res 2000;(378):169-173.
T, Jacobsson SA, Ivarsson I, et al. Internal fixation versus total hip
arthroplasty in the treatment of displaced femoral neck fractures: a
prospective randomised study of 100 hips. Acta Orthop Scand
2000;71(6):597-602.
O, Gullberg B, Kanis JA, et al. Risk factors for hip fracture in
European women: the MEDOS Study. Mediterranean Osteoporosis Study. J
Bone Miner Res 1995;10(11): 1802-1815.
B, Sernbo I, Carlsson A, et al. Social function after cervical hip
fracture. A comparison of hook-pins and total hip replacement in 47
patients. Acta Orthop Scand 1996;67:431-434.
J, Judet R, Lagrange J, et al. A study of the arterial vascularisation
of the femoral neck in the adult. J Bone Joint Surg Am 1955;37A:663-680.
J, Johnell O, Gullberg B, et al. Risk factors for hip fracture in men
from southern Europe: the MEDOS study. Mediterranean Osteoporosis
Study. Osteoporos Int 1999; 9(1):45-54.
A, Papakitsou E, Dretakis K, et al. Mortality rates of patients with a
hip fracture in a southwestern district of Greece: ten-year follow-up
with reference to the type of fracture. Calcif Tissue Int
2006;78(2):72-77. Epub 2006 Feb 6.
JF, Grant A, Masson M, et al. Displaced intracapsular hip fractures in
fit, older people: a randomised comparison of reduction and fixation,
bipolar hemiarthroplasty and total hip arthroplasty. Health Technol
Assess 2005;9(41):iii-iv, ix-x, 1-65.
JF, Grant A, Masson M, et al. Randomized comparison of reduction and
fixation, bipolar hemiarthroplasty, and total hip arthroplasty.
Treatment of displaced intracapsular hip fractures in healthy older
patients. J Bone Joint Surg Am 2006;88(2): 249-260.
GR, Parvizi J, Vegari DN, et al.Total hip arthroplasty for acute
femoral neck fractures using a cementless tapered femoral stem. J
Arthroplasty 2006;21(8): 1134-1140.
VC, Kesselaer SM, Clevers GJ, et al. Evaluation of the Singh index for
measuring osteoporosis. J Bone Joint Surg Br 1996;78(5):831-834.
P, van den Bent RP, Krijnen P, et al. Two cannulated hip screws for
femoral neck fractures: treatment of choice or asking for trouble? Arch
Orthop Trauma Surg 2006;126(5):297-303. Epub 2006 Apr 21.
H. Arthroplasty led to few failures and more complications than did
internal fixation for diplaced fractures of the femoral neck. J Bone
Joint Surg Am 2002;84: 2108.
JO. Treatment of intracapsular fractures of the femoral neck in
Denmark: trends in indications over the past decade. Acta Orthop Belg
1999;65(4):478-484.
BP, Berry DJ, Harmsen WS, Sim FH. Total hip arthroplasty for the
treatment of an acute fracture of the femoral neck: long-term results.
J Bone Joint Surg Am 1998; 80(1):70-75.
YS, Chen SH, Tsuang YH, et al. Internal fixation of undisplaced femoral
neck fractures in the elderly: a retrospective comparison of fixation
methods. J Trauma 2008; 64(1):155-162.
JR, Hassan SK, Wenn RT, Moran CG. Mortality and serum urea and
electrolytes on admission for hip fracture patients. Injury
2006;37(8):698-704. Epub 2006 Jun 30.
SA, Engesaeter LB, Havelin LI, et al. Mortality after total hip
replacement: 0-10-year follow-up of 39,543 patients in the Norwegian
Arthroplasty Register. Acta Orthop Scand 2000;71(1):19-27.
P. Type of displacement in fractures of the femoral neck and
observations on impaction of fractures. J Bone Joint Surg
1949;34B:184-189.
F, Gaines R, Collinge C, Haidukewych GJ. Results of internal fixation
of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am
2008;90(8): 1654-1659.
O, Berglund K, Larsson L, Toss G. Changes in hip fracture epidemiology:
redistribution between ages, genders and fracture types. Osteoporos Int
2002;13(1): 18-25.
Yao GL, Keller RB, Littenberg B, et al. Outcomes after displaced
fractures of the femoral neck. A meta analysis of one hundred and six
published reports. J Bone Joint Surg 1994;76A:15-25.
TM, Prpa B, Haidukewych GJ, et al. Long-term results of total hip
arthroplasty for femoral neck fracture nonunion. J Bone Joint Surg Am
2004;86-A(10):2263-2267.
SR, Beaupre LA, Johnston DW, et al. Lack of association between
mortality and timing of surgical fixation in elderly patients with hip
fracture: results of a retrospective population-based cohort study. Med
Care 2006;44(6):552-559.
RK, Schuller HM, Raaymakers EL. Intertrochanteric osteotomy for
non-union of the femoral neck. J Bone Joint Surg Br 1989;71:782-787.
HD, Savage A, Braly BA, et al. The function of the hip capsular
ligaments: a quantitative report. Arthroscopy 2008;24(2):188-195. Epub
2007 Nov 26.
JI, Barrios C, Gomar-Sancho F. Intracapsular hip pressure after femoral
neck fracture. Clin Orthop Relat Res 1997 Jul;(340):172-180.
JC, Robinson CM. Treatment of displaced intracapsular hip fractures
with total hip arthroplasty: comparison of primary arthroplasty with
early salvage arthroplasty after failed internal fixation. J Bone Joint
Surg Am 2002;84-A(11): 2010-2015.
J, Girou E, Lortat-Jacob A, et al. Surgical site infection after
surgery to repair femoral neck fracture: a French multicenter
retrospective study. Infect Control Hosp Epidemiol
2007;28(10):1169-1174. Epub 2007 Aug 29
MH, Harvey JP Jr, Moore TM. The muscle pedicle bone graft in the
treatment of displaced fractures of the femoral neck: indications,
operative technique, and results. Orthop Clin North Am 1974;5:779-792.
CG, Wenn RT, Sikand M, et al. Early mortality after hip fracture: is
delay before surgery important? J Bone Joint Surg Am 2005;87(3):483-489.
J, Alter AH, Elconin KB, et al. Transcervical fractures of the hip
treated with the Bateman bipolar prosthesis. Clin Orthop Relat Res
1990;(251):48-53.
S, Yamamoto S, Ishibashi H, Nakamura K. Factors associated with
mortality following hip fracture in Japan. J Bone Miner Metab
2006;24(2):100-104.
G, Adolphson P, von Sivers K, et al. Bone and muscle mass after femoral
neck fracture. Arch Orthop Trauma Surg 1997;116:470-474.
M, Radford P, Langstaff R. Preoperative traction for hip fractures in
the elderly: a clinical trial. Injury 1993;24(5):317-318.
KE, Papadakis SA, Kateros KT, et al. Long-term outcome of patients with
avascular necrosis, after internal fixation of femoral neck fractures.
Injury 2003;34(7): 525-528.
LT, Stromqvist B, Thorngren KG. Secondary arthroplasty for
complications of femoral neck fracture. J Bone Joint Surg Br
1989;71(5):777-781.
LT, Jalovaara P, Franzen H, et al. Function after primary
hemiarthroplasty and secondary total hip arthroplasty in femoral neck
fracture. J Arthroplasty 1994;9(4): 369-374.
AR, Rao J, Parker MJ. Prosthesis survivorship and clinical outcome of
the Austin Moore hemiarthroplasty: an 8-year mean follow-up of a
consecutive series of 500 patients. Injury 2006;37(8):734-739. Epub
2006 Apr 18.
CW, Oh JK, Park BC, et al.Retrograde nailing with subsequent screw
fixation for ipsilateral femoral shaft and neck fractures. Arch Orthop
Trauma Surg 2006;126(7): 448-453. Epub 2006 Jun 21.
BC, Maurer SG, Aharonoff GB, et al. Unipolar versus bipolar
hemiarthroplasty: functional outcome after femoral neck fracture at a
minimum of thirty-six months of follow-up. J Orthop Trauma
2002;16(5):317-322.
GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for
hip fracture and patient outcome. JAMA 2004;291(14):1738-1743.
S, Jensen TT, Bonde G, Mossing NB. The uncemented bipolar
hemiarthroplasty for displaced femoral neck fractures. 6-year follow-up
of 171 cases. Acta Orthop Scand 1991;62(2):115-120.
MJ, Blundell C. Choice of implant for internal fixation of femoral neck
fractures. Meta analysis of 25 randomised trials including 4,925
patients. Acta Orthop Scand 1998;69:138-143.
MJ, Pryor GA. Internal fixation or arthroplasty for displaced cervical
hip fractures in the elderly: a randomised controlled trial of 208
patients. Acta Orthop Scand 2000; 71:440-446.
MJ, Banajee A. Surgical approaches and ancillary techniques for
internal fixation of intracapsular proximal femoral fractures. Cochrane
Database Syst Rev 2005 Apr 18; (2):CD001705. Update of: Cochrane
Database Syst Rev 2000;(3):CD001705.
MJ, Stockton G. Internal fixation implants for intracapsular proximal
femoral fractures in adults. Cochrane Database Syst Rev
2001;(4):CD001467.
MJ, Khan RJ, Crawford J, Pryor GA. Hemiarthroplasty versus internal
fixation for displaced intracapsular hip fractures in the elderly. A
randomised trial of 455 patients. J Bone Joint Surg Br
2002;84(8):1150-1155.
MJ, Gurusamy K. Arthroplasties (with and without bone cement) for
proximal femoral fractures in adults. Cochrane Database Syst Rev 2006
Jul 19;3:CD001706. Update of: Cochrane Database Syst Rev
2004;(2):CD001706.
MJ, Handoll HH. Pre-operative traction for fractures of the proximal
femur in adults. Cochrane Database Syst Rev 2006 Jul 19;3:CD000168.
MJ, Gurusamy K. Internal fixation versus arthroplasty for intracapsular
proximal femoral fractures in adults. Cochrane Database Syst Rev 2006
Oct 18;(4):CD001708.
MJ, Raghavan R, Gurusamy K. Incidence of fracture-healing complications
after femoral neck fractures. Clin Orthop Relat Res 2007;458:175-179.
J, Ereth MH, Lewallen DG. Thirty-day mortality following hip
arthroplasty for acute fracture. J Bone Joint Surg Am
2004;86-A(9):1983-1988.
KK, Ashford RU, Frasquet-Garcia A, et al. Müller straight stem total
hip arthroplasty for fractured neck of femur. Injury
2006;37(8):727-733. Epub 2006 Feb 28.
MB, Jørgensen HL, Hansen K, Duus BR. Factors affecting postoperative
mortality of patients with displaced femoral neck fracture. Injury
2006;37(8):705-711. Epub 2006 Jun 12.
JE, Christie J. Undisplaced fracture of the neck of the femur: results
of treatment of 100 patients treated by single Watson-Jones nail
fixation. Injury 1988;19(2):93-96.
HK, Ruohola JP, Weckström M, et al. Long-term outcome of undisplaced
fatigue fractures of the femoral neck in young male adults. J Bone
Joint Surg Br 2006; 88-B(12):1574-1579.
M, Vahlberg T, Isoaho R, et al. Incidence of fractures and changes over
time among the aged in a Finnish municipality: a population-based
12-year follow-up. Aging Clin Exp Res 2007;19(4):269-276.
embolism prevention (PEP) trial collaborative group. Prevention of
pulmonary embolism and deep venous thrombosis with low dose aspirin.
PEP Trial. Lancet 2000;355:1295-302. commentary 1288-89.
TJS, Laine HJ, Tarvainen T, Aho H. Thompson hemiarthroplasty is
superior to Ullevaal screws in treating displaced femoral neck
fractures in patients over 75 years. A prospective randomised study
with 2-year follow-up. Ann Chirurg Gynaecol 2001; 90:225-228.
EL. Marti RK. Non-operative treatment of impacted femoral neck
fractures. A prospective study of 170 cases. [see comment]. J Bone
Joint Surg Br 1991;73(6): 950-954.
PJ, Hodgkinson JP, Meadows TH, et al. Treatment of displaced subcapital
fractures with the Charnley-Hastings hemiarthroplasty. J Bone Joint
Surg Br 1989;71(3): 478-482.
FJ, Chapman CB, Herrera MF, et al. Bipolar or unipolar hemiarthroplasty
for femoral neck fractures in the elderly? Clin Orthop 2003;414:259-265.
DT, Parker MJ. Does the level of an intracapsular femoral fracture
influence fracture healing after internal fixation? A study of 411
patients. Injury 2001;32(1): 53-56.
KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip
arthroplasty for displaced subcapital fractures of femur—13 year
results of a prospective randomised study. Injury 2000;31:793-797.
S, Thorngren K-G. Preoperative traction for hip fracture: a randomized
comparison between skin and skeletal traction in 78 patients. Acta
Orthop Scand 1998;69(3): 277-279.
S, Bjarnetoft B, Thorngren K-G. Preoperative skin traction or pillow
nursing in hip fractures: a prospective, randomized study in 123
patients. Disabil Rehabil 2005; 27(18-19):1191-1195.
WM, Della Rocca GJ, Combs C, et al. The medical and economic impact of
preoperative cardiac testing in elderly patients with hip fractures.
Injury 2007;38(Suppl 3):S49-52.
PF, Gould ES, Lyden JP, et al. Diagnosis of occult fractures about the
hip. Magnetic resonance imaging compared with bone scanning. J Bone
Joint Surg 1993;75A: 395-401.
JA, Biggs ML, Cauley J. Adjusted mortality after hip fracture: From the
cardiovascular health study. J Am Geriatr Soc 2006;54(12):1885-1891.
J, Aragaki AK, Kooperberg C, et al. Factors associated with 5-year risk
of hip fracture in postmenopausal women. JAMA 2007;298(20):2389-2398.
CM, Court-Brown CM, McQueen MM, et al. Hip fractures in adults younger
than 50 years of age: epidemiology and results. Clin Orthop
1995;312:238-246.
M, Schon M, Fredin H. Treatment of displaced femoral neck fractures: a
randomised minimum 5 year study of screws and bipolar hemiarthroplasty
in 100 patients. Acta Orthop Scand 2003;74(1):42-44.
C, Carlsson A, Johnell O, Sernbo I. A prospective randomised trial of
internal fixation versus arthroplasty for displaced fractures of the
neck of the femur. Functional outcome for 450 patients at 2 years. J
Bone Joint Surg Br 2002;84(2):183-188.
C, Carlsson A, Johnell O, Sernbo I. Costs of internal fixation and
arthroplasty for displaced femoral neck fractures: a randomised study
of 68 patients. Acta Orthop Scand 2003;74(3):293-298.
C, Johnell O. Orthopaedic treatment of displaced femoral neck fractures
in elderly patients. Disabil Rehabil 2005;27(18-19):1143-1149.
LL, Miller BJ, Dupuis PR, et al. A prospective randomised study
comparing bipolar hemiarthroplasty and hemiarthroplasty in elderly
patients with subcapital fractures. (Abstract) J Bone Joint Surg
1992;74(Suppl 3):282.
JE, Chen FS, Hiebert R, et al. Efficacy of preoperative skin traction
in hip fracture patients: a prospective, randomized study. J Orthop
Trauma 2001;15(2):81-85.
S, Rebecatto A, Bolgan I, et al. Hip fractures in elderly patients
treated with bipolar hemiarthroplasty. Comparison between cemented and
cementless implants. J Orthop Traumatol 2005;6:80-87.
S, Thomson RG. The distribution and anastomoses of arteries supplying
the head and neck of the femur. J Bone Joint Surg Br 1965;47B:560-573.
KM, Parker MJ. Austin Moore hemiarthroplasty: technical aspects and
their effects on outcome, in patients with fractures of the neck of
femur. Injury 2002;33(5): 419-422.
MS, Kumar MA, Ireshanavar SS, et al. Ipsilateral hip and femoral shaft
fractures treated with intramedullary nails. Int Orthop
2007;31(1):77-81. Epub 2006 Jun 2.
M, Kunzheng W, Zhichao T, et al. Outcome of non-operative management in
Garden I femoral neck fractures. Injury 2006;37(10):974-978. Epub 2006
Aug 24.
M, Wenn R, Moran CG. Mortality following surgery for undisplaced
intracapsular hip fractures. Injury 2004;35(10):1015-1019.
JM, Barrington R. Internal fixation versus hemiarthroplasty for the
displaced subcapital fracture of the femur. A prospective randomised
study. J Bone Joint Surg Br 1981;63:357-361.
BR, McLauchlan GJ, Robinson CM, et al. Epidemiology of fractures in
15,000 adults: the influence of age and gender. J Bone Joint Surg Br
1998;80(2):243-248.
GK, Deshmukh RG. Uncemented Austin-Moore and cemented Thompson unipolar
hemiarthroplasty for displaced fracture neck of femur—comparison of
complications and patient satisfaction. Injury 2006;37(2):169-174. Epub
2006 Jan 17.
M, Nagrath AR, Maini PS. Changes in trabecular pattern of the upper end
of the femur as an index of osteoporosis. J Bone Joint Surg (Am)
1970;52A:457-467.
P, Riley D, Ellery J, et al. Displaced subcapital fractures of the
femur: a prospective randomized comparison of internal fixation,
hemiarthroplasty and total hip replacement. Injury 1989;20(5):291-293.
MD, Cody DD, Goldstein SA, et al. Proximal femoral bone density and its
correlation to fracture load and hip-screw penetration load. Clin
Orthop Relat Res 1992;(283): 244-251.
S, Walter S, Jensen JS. Moore hemi-arthroplasty with and without bone
cement in femoral neck fractures. A clinical controlled trial. Acta
Orthop Scand 1982; 53(6):953-956.
O, Molster A, Raugstad TS. Internal fixation versus primary prosthetic
replacement in acute femoral neck fractures: a prospective, randomized
clinical study. Br J Surg 1979;66:56-60.
KP, Spritzer CE, Harrelson JM, et al. Magnetic resonance imaging of the
femoral head after acute intracapsular fracture of the femoral neck. J
Bone Joint Surg Am 1990; 72:98-103.
T, Jain UK, Sharma VD. Role of valgus osteotomy and fixation by
doubleangle blade plate in neglected displaced intracapsular fracture
of neck of femur in younger patients. Injury 2005;36(5):630-634. Epub
2005 Jan 23.
KH, Broos PL. Internal fixation of femoral neck fractures. A follow-up
study of 118 cases. Acta Chir Belg 1987;87(4):247v251.
B, Brismar J, Hansson LI, et al. Technetium 99m-methylenediphosphonate
scientimetry after femoral neck fracture. A 3 year follow-up study.
Clin Orthop Rel Res 1984;182:177-189.
B, Hansson LI, Nilsson LT, et al. Hook pin fixation in femoral neck
fractures. A two year follow up study of 300 cases. Clin Orthop
1987;218:58-62.
R, Liski A. Quality effects of operative delay on mortality in hip
fracture treatment. Qual Saf Health Care 2005;14(5):371-377.
S, Benum P, Nesse O, et al. [Femoral neck fractures in the elderly. A
comparison of 3 therapeutic methods]. Tidsskr Nor Laegeforen
1985;105:492-495. Norwegian.
MF, Winquist RA, Hansen ST. Fractures of the femoral neck in patients
aged between twelve and forty-nine years. J Bone Joint Surg Am
1984;66:837-846.
WH, Armour PC. Primary total hip replacement for displaced subcapital
fractures of the femur. J Bone Joint Surg 1985;67-B(2):214-217.
S, Jermolajevas V, Tarasevicius R, et al. Total hip replacement for the
treatment of femoral neck fractures. Long-term results. Medicina
(Kaunas) 2005;41(6): 465-469.
J, Ponzer S, Svensson O, et al. Internal fixation compared with total
hip replacement for displaced femoral neck fractures in the elderly. A
randomized, controlled trial. J Bone Joint Surg Br 2003;85(3):380-388.
J, Zethraeus N, Svensson O, et al. Quality of life related to fracture
displacement among elderly patients with femoral neck fractures treated
with internal fixation. Orthop Trauma 2002;16(1):34-38.
CJ, Freeman CJ, Camilleri-Ferrante C, et al. Differences in mortality
after fracture of the hip: the East Anglian audit. BMJ 1995;310:904-908.
SM, Favero KJ. Femoral neck fractures in skeletally mature patients,
fifty years old or less. J Bone Joint Surg Am 1985;67(8):1255-1260.
P 3rd, Kain MS, Creevy WR. Diagnosis of femoral neck fractures in
patients with a femoral shaft fracture. Improvement with a standard
protocol. J Bone Joint Surg Am 2007;89(1):39-43.
A, Jain P, Mishra P, et al. Delayed internal fixation of fractures of
the neck of the femur in young adults. A prospective, randomised study
comparing closed and open reduction. J Bone Joint Surg Br
2004;86(7):1035-1040.
Dortmont LM, Douw CM, van Breukelen AM, et al. Cannulated screws versus
hemiarthroplasty for displaced intracapsular femoral neck fractures in
demented patients. Ann Chir Gynaecol 2000;89:132-137.
Thiel PH, Snellen JP, Jansen WBJ, et al. Moore prosthesis versus
Bateman bipolar prosthesis: a prospective randomised clinical study. J
Bone Joint Surg 1988;70(4):677.
Vugt AB, Oosterwijk WM, Goris RJ. Osteosynthesis versus endoprosthesis
in the treatment of unstable intracapsular hip fractures in the
elderly. A randomised clinical trial. Arch Orthop Trauma Surg
1993;113:39-45.
CC, Smulders TC, van Walsum AD. High secondary displacement rate in the
conservative treatment of impacted femoral neck fractures in 105
patients. Arch Orthop Trauma Surg 2005;125(3):166-168. Epub 2005 Jan 12.
G, Hoerer D, Groisman G, et al. Stress fractures of the femoral neck
following strenuous activity. J Orthop Trauma 1990;4(4):394-398.
SW, Jakob RP, Gautier E. Ten year patient and prosthesis survival after
unipolar hip hemiarthroplasty in female patients over 70 years old. J
Arthroplasty 2003;18(5): 587-591.
JP, Schemitsch E. The use of Meyer’s graft in the prevention and
treatment of femoral neck nonunions. Presented at the meeting of the
AAOS, New Orleans; 2003.
D, Hubble M, Sarris I, et al. Revision of failed hemiarthroplasty for
fractures at the hip. Int Orthop 1998;22(3):165-168.
PC, Moore WR, Shooter DR, et al. Early prosthetic complications after
unipolar hemiarthroplasty. ANZ J Surg 2006;76(6):432-435.
RG, Hinves BL. The Hastings bipolar hemiarthroplasty for subcapital
fractures of the femoral neck. A 10-year prospective study. J Bone
Joint Surg Br 1990; 72(5):788-793.
M, Chao EY, Ilstrup DM, et al. Fixed-head and bipolar hip
endoprostheses. A retrospective clinical and roentgenographic study. J
Arthroplasty 1987;2:327-341.
W, Seigne R, Bright S, et al. Audit of morbidity and mortality
following neck of femur fracture using the POSSUM scoring system. N Z
Med J 2006;119(1234): U1986.
HR, Skinner JA, Porteous MJ. The preoperative prevalence of deep vein
thrombosis in patients with femoral neck fractures and delayed
operation. Injury 1999;30(9): 605-607.
M, Weening B, Petrisor B, et al. The value of washers in cannulated
screw fixation of femoral neck fractures. J Trauma 2005;59(4):969-975.
M, Bhandari M, Keel M, et al. Perception of Garden’s classification for
femoral neck fractures: an international survey of 298 orthopaedic
trauma surgeons. Arch Orthop Trauma Surg 2005;125(7):503-505.
M, Ayieni O, Petrisor BA, Bhandari M. Femoral neck shortening after
fracture fixation with multiple cancellous screws: incidence and effect
on function. J Trauma 2008;64(1):163-169.
