Thoracic Spine
Editors: Morrey, Bernard F.; Morrey, Matthew C.
Title: Master Techniques in Orthopaedic Surgery: Relevant Surgical Exposures, 1st Edition
Copyright ©2008 Lippincott Williams & Wilkins
> Table of Contents > Section III – Spine > 13 – Thoracic Spine
13
Thoracic Spine
Matthew Morrey
Mark B. Dekutoski
Steve Cassivi
Ziya L. Gokaslan
ANTERIOR CERVICAL THORACIC APPROACHES
The four approaches used for the upper thoracic region
include first the high thoracotomy at the fourth rib which provides
excellent access to the lateral aspect of the anterolateral cervical
thoracic junction especially the sympathetic chain. This is, however, a
difficult approach for placement of anterior fixation. Second is the
modified anterior approach which resects the medial clavicle. This
exposure is fraught with significant shoulder morbidity albeit
downplayed for patients who are anticipated not to survive their
pathology. These exposures have fallen out of favor with the increasing
familiarity with the manubrial split accompanied by a lateral traverse
sternal split between the third and fourth rib. The full manubrial
split cervicothoracic approach allows anterior extension as low as the
diaphragmatic attachments. The modified anterior and manubrial split
are limited by the aortic arch which traverses approximately T3
vertebra. Fortunately, the aortal caval window approach can be used to
reach the anterior aspect of T3-T5, allowing for direct anterior
decompression, and by passing the plate under the aortic arch direct
anterior plate fixation is possible.
include first the high thoracotomy at the fourth rib which provides
excellent access to the lateral aspect of the anterolateral cervical
thoracic junction especially the sympathetic chain. This is, however, a
difficult approach for placement of anterior fixation. Second is the
modified anterior approach which resects the medial clavicle. This
exposure is fraught with significant shoulder morbidity albeit
downplayed for patients who are anticipated not to survive their
pathology. These exposures have fallen out of favor with the increasing
familiarity with the manubrial split accompanied by a lateral traverse
sternal split between the third and fourth rib. The full manubrial
split cervicothoracic approach allows anterior extension as low as the
diaphragmatic attachments. The modified anterior and manubrial split
are limited by the aortic arch which traverses approximately T3
vertebra. Fortunately, the aortal caval window approach can be used to
reach the anterior aspect of T3-T5, allowing for direct anterior
decompression, and by passing the plate under the aortic arch direct
anterior plate fixation is possible.
Indications
Anterior approaches of the cervical thoracic junction
are often necessary to address tumor pathology, deformity and anterior
column support. These approaches are often avoided due to limited
familiarity of the surgeon with the approach, which is paramount to
successful surgical intervention and avoidance of complications.
are often necessary to address tumor pathology, deformity and anterior
column support. These approaches are often avoided due to limited
familiarity of the surgeon with the approach, which is paramount to
successful surgical intervention and avoidance of complications.
Contraindications
Contraindications or limitations to the cervicothoracic
approaches are primarily related to the nature of the pathology of
spinal structures such as tumor pathology and with vascular involvement
postradiation changes which can substantially increase the risk of
intraoperative scarring compromising exposure and esophageal tissue
integrity.
approaches are primarily related to the nature of the pathology of
spinal structures such as tumor pathology and with vascular involvement
postradiation changes which can substantially increase the risk of
intraoperative scarring compromising exposure and esophageal tissue
integrity.
Anterior cervical thoracic approaches for tumor
involvement may require ligation of vascular and potential for a
dysfunctional limb.
involvement may require ligation of vascular and potential for a
dysfunctional limb.
Preoperative Planning
Collaboration between the access surgeon and the spinal
surgeon is useful. Adequate visualization of the neurologic structures
for direct decompression most commonly defines the caudal extent of the
exposure. When anterior fixation is only required to T1 or T2 an
extensile anterior lateral neck approach may be adequate. However, for
decompression of the T1 vertebra, a manubrial split is required to gain
adequate anterior access and fixation. The authors’ preference is to
conduct a right anterior neck approach to avoid the lymphatic duct and
the dominant left carotid artery. However, in the final analysis, the
specific pathology most commonly determines the approach selection.
surgeon is useful. Adequate visualization of the neurologic structures
for direct decompression most commonly defines the caudal extent of the
exposure. When anterior fixation is only required to T1 or T2 an
extensile anterior lateral neck approach may be adequate. However, for
decompression of the T1 vertebra, a manubrial split is required to gain
adequate anterior access and fixation. The authors’ preference is to
conduct a right anterior neck approach to avoid the lymphatic duct and
the dominant left carotid artery. However, in the final analysis, the
specific pathology most commonly determines the approach selection.
P.300
High Thoracotomy
Position
Typically the patient is placed prone with an axillary
roll and with the arm elevated and flexed anteriorly to allow for full
prepping of the arm and axilla.
roll and with the arm elevated and flexed anteriorly to allow for full
prepping of the arm and axilla.
Technique
-
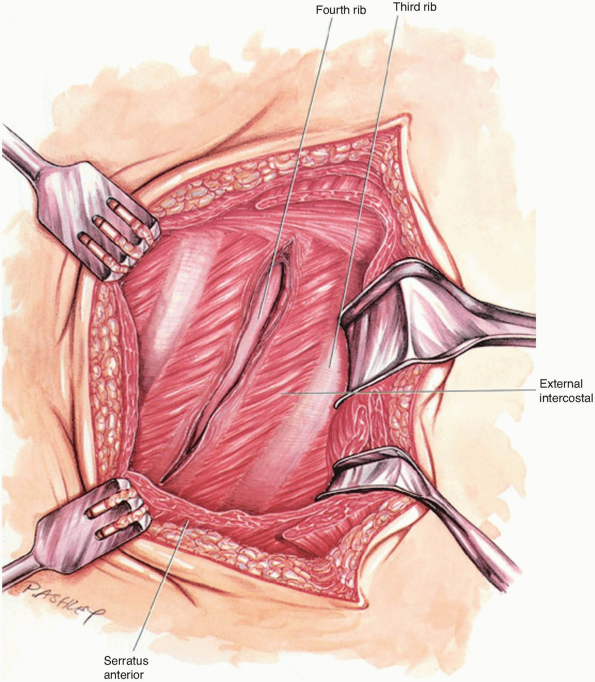
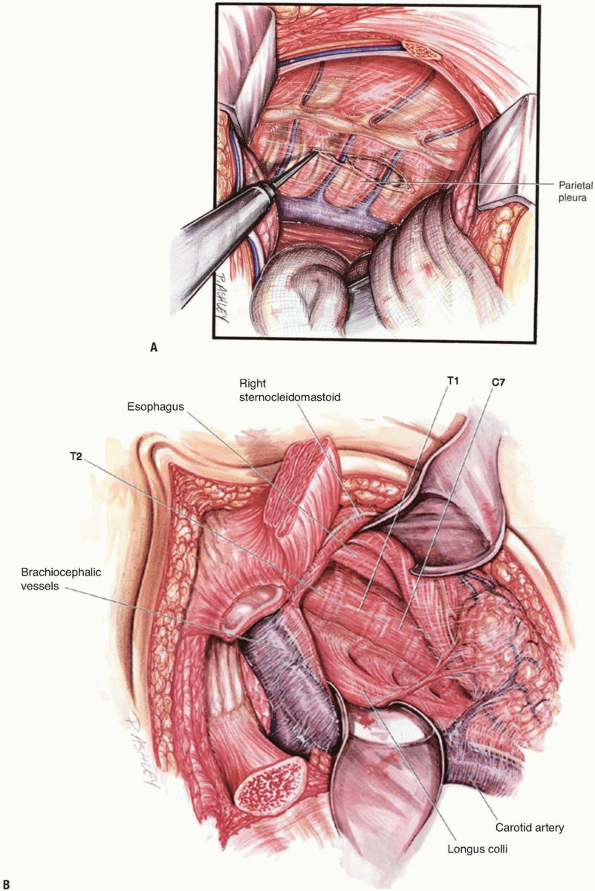
Incision: with the inferior border of the scapula defined, the incision courses over the mid-body of the scapula (Fig. 13-1).
-
The inferior muscular attachments of the
scapula are mobilized after transection and/or mobilization of the
trapezius dorsally. The latissimus dorsi muscle is retracted laterally
through this window (Fig. 13-2). -
The rhomboids are released and the fourth rib is identified by palpation.
-
An incision over the fourth rib is conducted while protecting the intercostal neurovascular structures anteriorly and cephalad (Fig. 13-3).
-
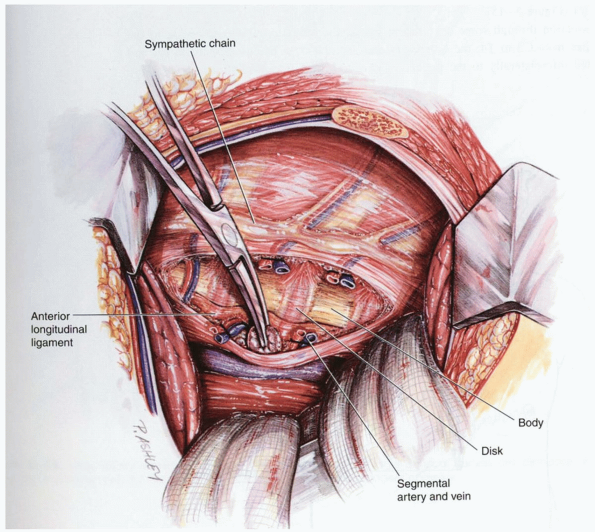
A dorsal osteotomy of the rib allows
further mobilization and retraction of the scapula. The scapula
retractor, along with chest wall retractors, allows for direct
visualization from C7 to the diaphragm (Fig. 13-4).-
Note: The right side of the chest allows for the greatest flexibility of the exposure.
-
P.301
 |
|
FIGURE 13-1
|
 |
|
FIGURE 13-2
|
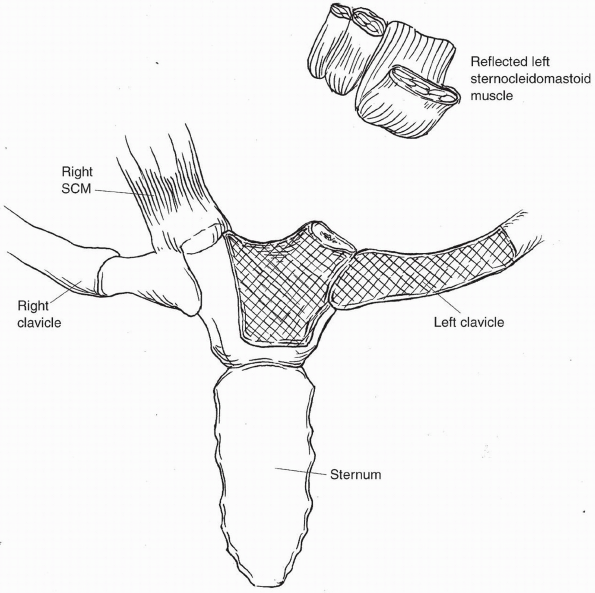
Direct Anterior Cervical Thoracic Approach
This is a modification of the anterior exposure with
resection of the medial clavicle. This approach employs the interval
between the strap muscles medially the sternocleidomastoid laterally,
the esophagus and trachea medially and the carotid sheath laterally.
Selection of a right or left approach is based on familiarity of the
surgeon and recognition that the recurrent laryngeal nerve is more
consistent on the left side than on the right side of the neck.
Further, hand dominance, familiarity, and the left sided lymphatic duct
all contribute to the decisions of a left or right approach.
resection of the medial clavicle. This approach employs the interval
between the strap muscles medially the sternocleidomastoid laterally,
the esophagus and trachea medially and the carotid sheath laterally.
Selection of a right or left approach is based on familiarity of the
surgeon and recognition that the recurrent laryngeal nerve is more
consistent on the left side than on the right side of the neck.
Further, hand dominance, familiarity, and the left sided lymphatic duct
all contribute to the decisions of a left or right approach.
 |
|
FIGURE 13-3
|
P.302
 |
|
FIGURE 13-4
|
Technique
-
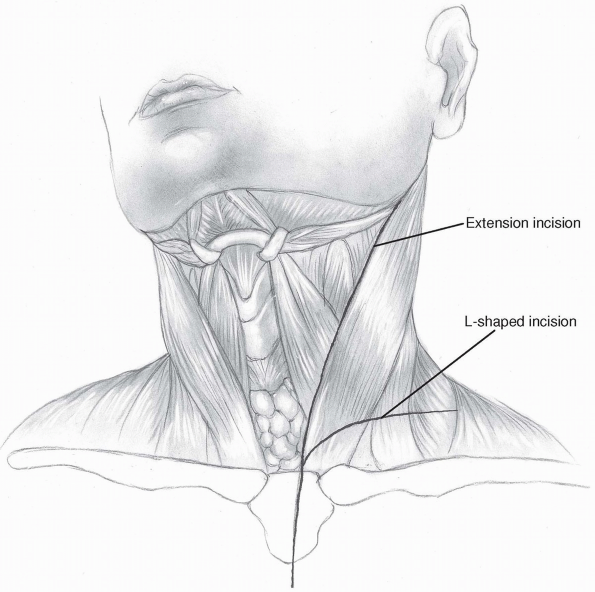
Incision: the incision may be extensive or more limited as shown in Figure 13-5.
-
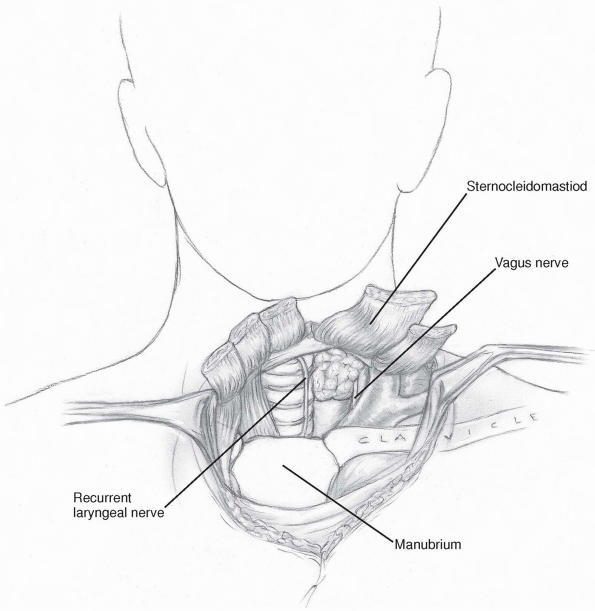
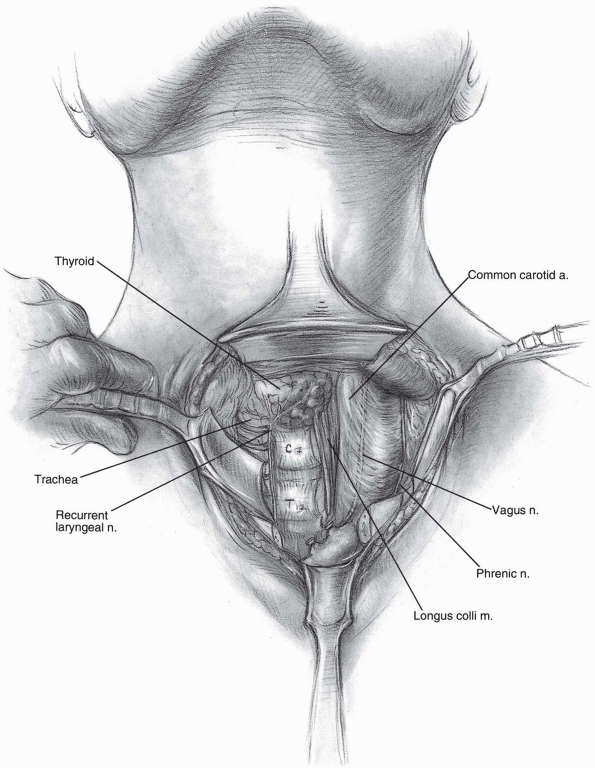
Once the anterior neck approach is
developed and the pharynx is identified and recurrent laryngeal nerve
typically deep to it. The inferior extent of this anterior dissection
will be the C-7 T-1 disc where upon a more extensile approach is
typically needed (Fig. 13-6). -
Resection of the medial clavicle is
conducted and the dissection is carried down lateral to the anterior
strap muscle which allows for continuation down onto the anterior
cervicothoracic junction (Fig. 13-7). -
Isolation and direct visualization of the
recurrent laryngeal nerve as it enters the tracheoesophageal group is
necessary to avoid transecting this structure (Fig. 13-8). -
The subclavian vein and phrenic nerve are readily identified and followed directly down to the spine (see Fig. 13-8).
 |
|
FIGURE 13-5
|
P.303
 |
|
FIGURE 13-6
|
 |
|
FIGURE 13-7
|
P.304
 |
|
FIGURE 13-8
|
P.305
 |
|
FIGURE 13-9
|
 |
|
FIGURE 13-10
|
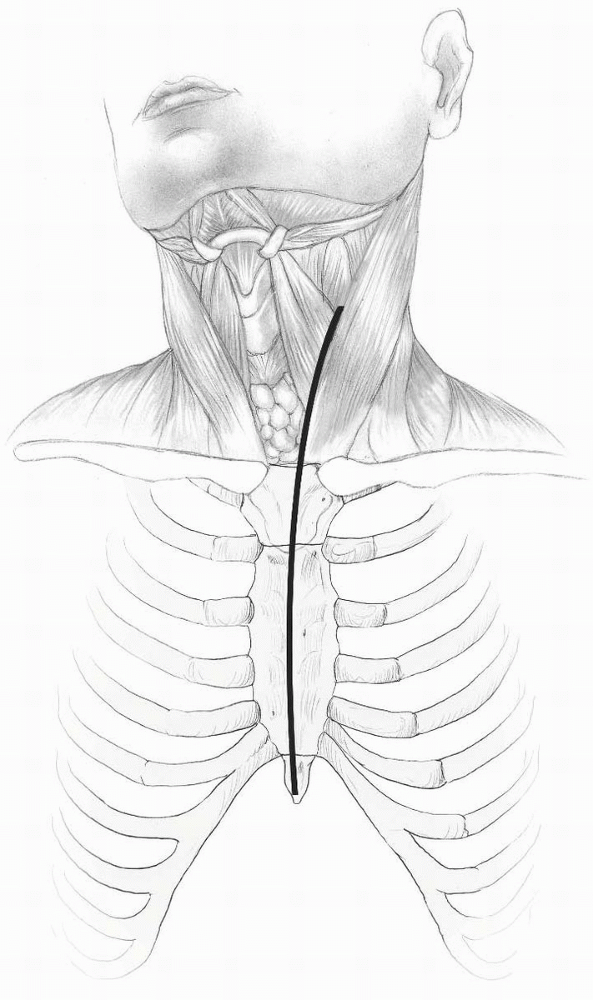
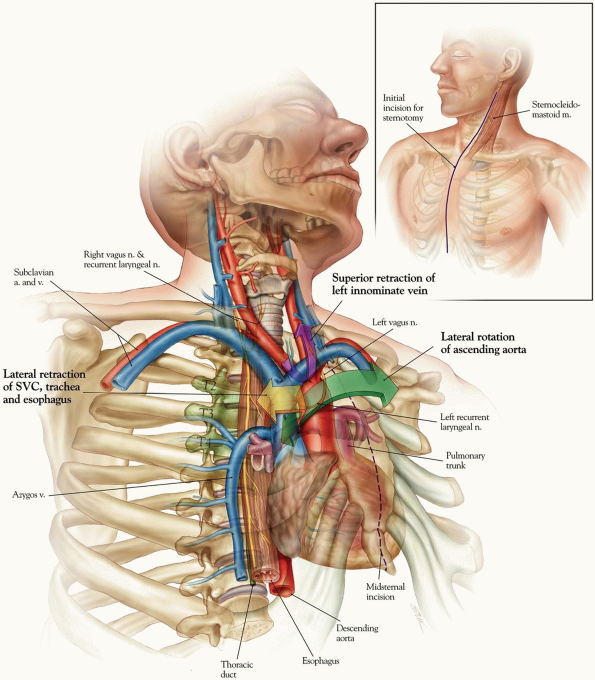
Sternal Split
The pathology, morbidity and recovery dictate the
selection of the direct anterior access by way of sternotomy.
Modification of the sternal split includes splitting the manubrium and
emerging laterally between the third and fourth ribs. By emerging
between the third and fourth ribs mobilization at this interval allows
more direct anterior access to the cephalad aspect of the aortic arch.
Should further dissection be necessary, the strap muscles are mobilized
taking care to protect the recurrent laryngeal and subclavian nerves.
This exposure provides greater consistency to access the anterior
anatomy and the most, direct approach for placement of implants and
visualization of neurological structures during decompression.
selection of the direct anterior access by way of sternotomy.
Modification of the sternal split includes splitting the manubrium and
emerging laterally between the third and fourth ribs. By emerging
between the third and fourth ribs mobilization at this interval allows
more direct anterior access to the cephalad aspect of the aortic arch.
Should further dissection be necessary, the strap muscles are mobilized
taking care to protect the recurrent laryngeal and subclavian nerves.
This exposure provides greater consistency to access the anterior
anatomy and the most, direct approach for placement of implants and
visualization of neurological structures during decompression.
Technique
-
Incision: with the patient supine,
incision begins typically over the anterior border of the
sternocleidomastoid and extends distally in the midline over the
manubrium and the sternum to the level of the zyphoid process (Fig. 13-9). -
Blunt dissection separates the posterior aspect of the sternum creating a retrosternal space.
-
The sternum is split longitudinally, usually with an oscillating saw.
-
A sternal retractor is used to separate the sternum taking care to avoid tearing the retropleural fascia (Fig. 13-10).
-
The dissection of the retropleural fascia allows exposure of the lower cervical and upper thoracic regions (Fig. 13-11).
-
Closure of the sternotomy is extremely
important. Nonunion can be very painful. This is performed in a
classical fashion with circumferential wire sutures.
P.306
 |
|
FIGURE 13-11
|
P.307
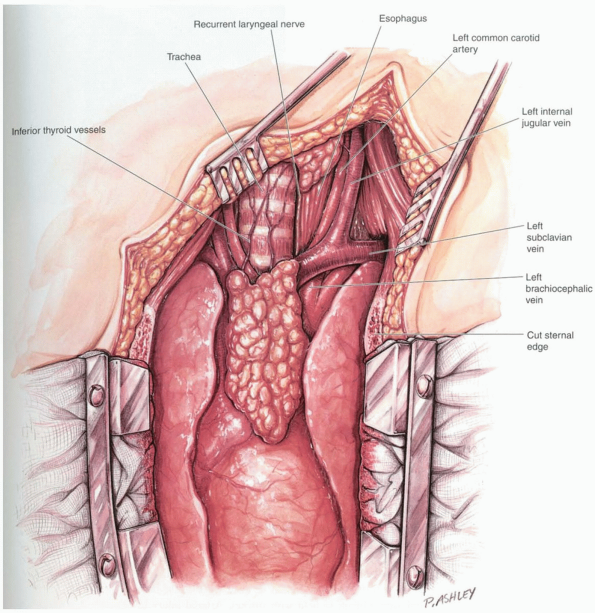
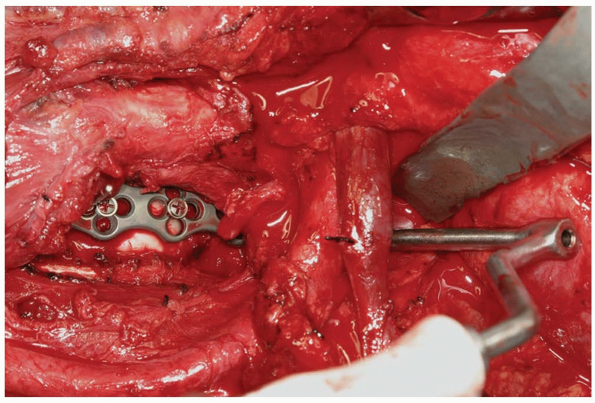
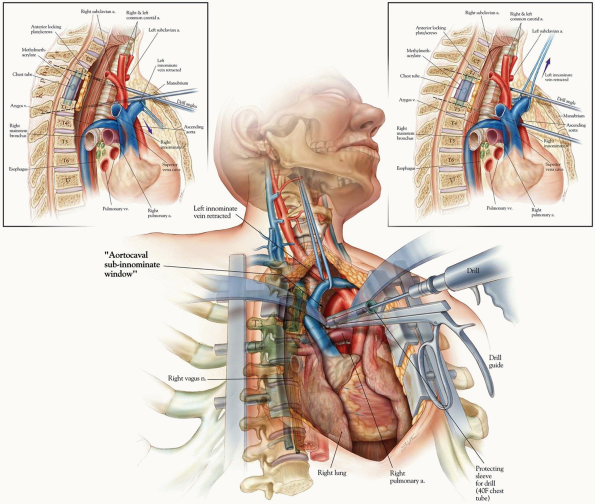
Interaortocaval Subinnominate Window
Indications
For proper anterior posterior screw orientation at the level of T3-T5.
Position
The patient is placed supine on the table.
Technique
-
Incision: the incision begins along the
anterior border of the sternocleidomastoid muscle and continues
distally over the sternum (Fig. 13-12). -
The medial border of the
sternocleidomastoid muscle is identified, the dissection is deepened to
expose the trachea thyroid and esophagus which are gently retracted to
the right. Note: Care is taken to protect the left recurrent laryngeal
nerve and the thoracic duct. -
Distally, the sternum is divided with an oscillating saw.
-
After splitting the thymus the left innominate (brachiocephalic vein) is isolated to the superior vena cava (Fig. 13-12).
-
The proximal innominate (bachiocephalic) artery is isolated.
-
The aorta is retracted to the patient’s
left and the superior vena cava to the patient’s right exposing the
T1-T3 vertebra. The procedure proceeds according to the nature of the
pathology (Fig. 13-13). -
The sternum is repaired with no. 5 titanium wires. The remainder of the closure is routine.
P.308
 |
|
FIGURE 13-12
|
For limited direct anterior decompression within the
window the author will use renal vein type rectractor blades. If a
drill or screws need to be passed via the aortocaval window a section
of 40F chest tube can be used to act as a soft tissue protector. The
clear tubing affords visualization and protection from the vascular
tissues.
window the author will use renal vein type rectractor blades. If a
drill or screws need to be passed via the aortocaval window a section
of 40F chest tube can be used to act as a soft tissue protector. The
clear tubing affords visualization and protection from the vascular
tissues.
 |
|
FIGURE 13-13
|
P.309
 |
|
FIGURE 13-13 (Continued)
|
P.310
ANTERIOR THORACOLUMBAR EXTENSILE APPROACH
Indications
-
Access to the anterior thoracic spine for an anterior condylar resection tumor
-
Anterior thoracic release for deformity and/or reconstruction
-
Note: This
exposure often requires the collaboration of an access surgeon and
spine surgeon. Proficiently in managing some conditions in the prone
position, the use of the operating endoscope and inner costal portals
is increasing.
-
Comment
A strong caution is advised against endoscopic
procedures for tumor pathology of the thoracic spine. Unfortunately,
early local recurrence from iatrogenic spread to the pleural cavity has
been documented with this approach. Contamination of the entire pleural
cavity will tend to occur from the dependent positioning, bleeding from
the tumor site, and by the seeding that results from the piecemeal
removal of the tumor.
procedures for tumor pathology of the thoracic spine. Unfortunately,
early local recurrence from iatrogenic spread to the pleural cavity has
been documented with this approach. Contamination of the entire pleural
cavity will tend to occur from the dependent positioning, bleeding from
the tumor site, and by the seeding that results from the piecemeal
removal of the tumor.
Position
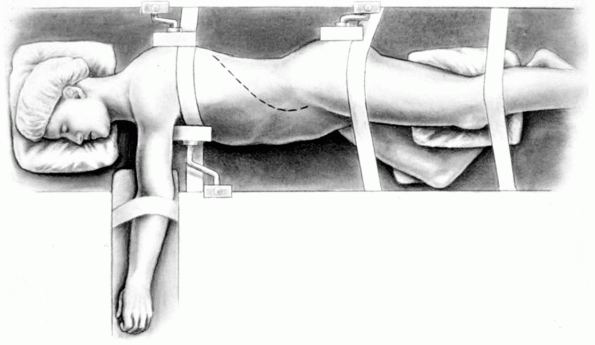
We typically position the patient with left side up so
as to avoid the interference with the liver. Stabilization is achieved
with radiolucent bolsters, the right hip is flexed and the left hip
extended. Taping of the pelvis and shoulder region reduces
intraoperative rolling of the patient. Thoracotomy can also be
accomplished in the prone position through a traditional anterolateral
approach with the arms in the abducted position most commonly used (Fig. 13-14).
as to avoid the interference with the liver. Stabilization is achieved
with radiolucent bolsters, the right hip is flexed and the left hip
extended. Taping of the pelvis and shoulder region reduces
intraoperative rolling of the patient. Thoracotomy can also be
accomplished in the prone position through a traditional anterolateral
approach with the arms in the abducted position most commonly used (Fig. 13-14).
Technique
-
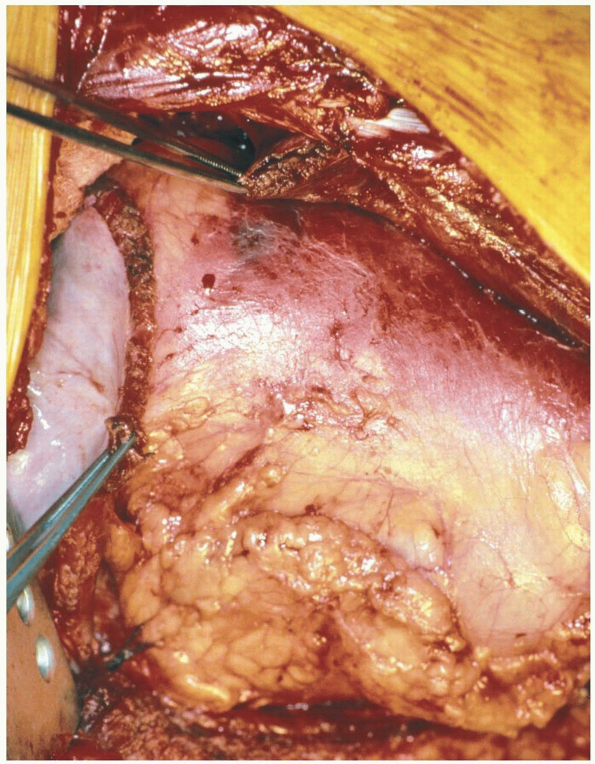
Incision: the curvilinear incision enters
through the 9th to 11th ribs depending on the pathology and anticipated
length of exposure (Fig. 13-15).
The extensile thoracoabdominal approach is typically carried out
cephalad to the 9th rib so as to allow for a direct visualization of
the dorsal diaphragmatic attachment. -
The latissimus dorsi muscle is split and dissection carried down to the intercostal area.
-
The dissection is carried over the rib to
protect the neurovascular bundle as in a standard thoracotomy fashion,
but with the patient in a prone position. -
The rib is exposed subperiosteally and as the intercostal nerve and vessels are protected, it is resected (Fig. 13-16).
-
A chest wall retractor is inserted and
with clipping and/or tying of intercostal vessels and with gradual
spreading, the thoracic contents are retracted away from the spine.-
Note:
Direct spinal access typically requires ligation of vessels
unilaterally and/or bilaterally. This can be done with safety; however,
efforts should be taken to maintain blood pressure above 60 to 70 mm
Hg. Further, if the patient has had radiation and/or myelopathic
changes, hypotension and vascular ligation can cause relative cord
ischemia and/or even paralysis.
-
-
Distally, the retroperitoneum can be entered over the tip of the 11th rib.
-
The costochondral cartilage is divided.
-
Direct blunt dissection by finger or gauge sponge inferior to the diaphragm is carried out in the retroperitoneum.
-
Carrying the incision more inferiorly
into the abdomen requires dividing the internal/external oblique
abdominal muscles as well as the transverse abdominal muscle. -
The reflection continues to the rib and
then down the lateral border of the rectus abdominus sheath to the
anterior-superior iliac spine. -
The retroperitoneam is now brought forward, typically with a sponge and a stick.
-
The quadratus lumborum, the femoral
nerve, and the iliopsoas muscle are identified coming anterior to the
iliac vessels and the bifurcation of the aorta is observed to the left.-
Note: Segmental vessels can be sectioned at the levels of pathology as necessary.
-
-
The diaphragm is released at the thoracolumbar junction (Fig. 13-17).
-
At this point the nerves to the posterior
diaphragm are spared if possible as they have significant contributions
to the sympathetic chain. Branches from the T11 and T12 splanchnic
innervate the diaphragm but may be taken unilaterally without
significant patient morbidity. -
The iliopsoas typically attaches at L-1
and is reflected from the midline laterally with careful avoidance of
dissection in the posterior third of the iliopsoas to avoid entry to
the lumbar plexus. The thoracolumbar vertebral bodies are now
accessible. -
Closure: The diaphragm is first repaired
with nonabsorbable sutures. The thoracic pleura through the rib bed is
closed and the lung inflated. -
A chest tube is used to maintain the reinflated lung.
-
The viscera is protected while the
abdominal musculature is closed in layers. Careful closure will lessen
the likelihood of abdominal hernia.
 |
|
FIGURE 13-14
|
 |
|
FIGURE 13-15
|
P.311
 |
|
FIGURE 13-16
|
P.312
 |
|
FIGURE 13-17
|
P.313
RECOMMENDED READING
Cohen
ZR, Fourney DR, Gokaslan ZL, et al. Anterior stabilization of the upper
thoracic spine via an “interaortocaval subinnominate window.” Case
report and description of operative technique. J Spinal Disord Tech 2004; 17(6):543-548.
ZR, Fourney DR, Gokaslan ZL, et al. Anterior stabilization of the upper
thoracic spine via an “interaortocaval subinnominate window.” Case
report and description of operative technique. J Spinal Disord Tech 2004; 17(6):543-548.
Grossfeld S, Winter RB, Lonstein JE, et al. Complications of anterior spinal surgery in children. J Pediatr Orthop 1997;17(1):89-95.
Hollinshead WH, ed. Anatomy for Surgeons. New York: Harper and Row, 1966.
Micheli LJ, Hood RW. Anterior exposure of the cervicothoracic spine using a combined cervical and thoracic approach. J Bone Joint Surg 1983;65A:992-997.
