Hip Dislocations and Fractures of the Femoral Head
significant force to dislocate. Thus, pure hip dislocation or
dislocation with femoral head fracture is generally a result of
high-energy trauma and is often accompanied by associated injuries that
must be sought out.78 Suraci167
reported that 95% of patients presenting with hip dislocation after a
motor vehicle accident had an associated injury requiring inpatient
management. In addition to a standard trauma evaluation, a meticulous
musculoskeletal and neurologic examination and detailed radiographic
assessment is necessary to avoid missing injuries.
Some, such as cartilage damage at impact and injury to the femoral head
vascular supply, are beyond the control of the surgeon. Others, such as
the timing and accuracy of the reduction, are variables that can be
positively affected by recognizing and treating the dislocation as an
emergency. Complications are common and include avascular necrosis
(AVN), arthritis, neurologic injury, heterotopic ossification, and
redislocation.3,11,18,28,32,42,67,77,123,173
Even if short-term complications such as loose body wear and AVN are
avoided, the long-term outcome of hip dislocation is not predictably
good. The incidence of unsatisfactory results, primarily as a
consequence of arthritis, has been reported as high as 50%.32,193
The treatment of hip dislocations and femoral head fractures is
directed toward avoiding complications by emergent reduction and by
providing a congruent and stable joint.
risk for hip dislocation than restrained drivers.27 Other mechanisms include falls, pedestrians struck by motor vehicles, industrial accidents, and athletic injuries.41,49,112,120,162,167,170
|
TABLE 46-1 Direction of Hip versus Injury Pattern
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
||||||||
the individual’s anatomy all affect the direction of the dislocation
and whether a fracture-dislocation or pure dislocation occurs (Table 46-1).21,28,34,39,42,43,44,94,95,124,128,162,179 Posterior dislocations outnumber anterior dislocations by approximately nine to one.11,32,170,193
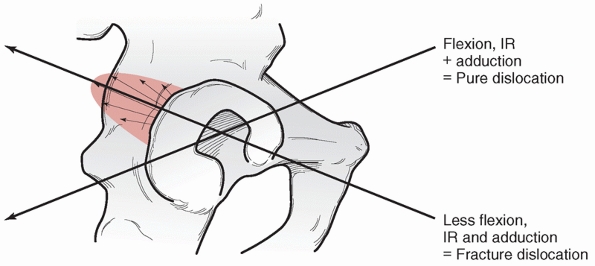
The typical mechanism for a posterior dislocation is a deceleration
accident in which the occupant’s knee strikes the dashboard with the
knee and hip flexed. Letournel94,95
used vector analysis to explain that the more flexion and adduction the
hip is in when a longitudinal force is applied through the femur, the
more likely a pure dislocation will occur( Fig. 46-1).94,95
Less adduction or less internal rotation favor a fracture-dislocation,
which may occur with a posterior wall fracture or a shearing injury of
the femoral head as the head impacts against the posterior wall. The
latter case results in a Pipkin-type injury with a fragment of the
femoral head remaining in the acetabulum and the intact portion
dislocating posteriorly.
plays a large role in the type of injury is supported by Upadhyay and
colleagues,179 who studied the
femoral anteversion in patients with hip dislocations and
fracture-dislocations. They observed a decrease in femoral anteversion
and even femoral retroversion in patients who sustained
fracture-dislocations compared to a normal population and even less
femoral anteversion in patients who sustained pure dislocations.
Decreased anteversion acts to place the head in a more posterior
position as does internal rotation, both tending to produce a pure
dislocation. Conversely, greater anteversion and less internal rotation
led to fracture-dislocation.
 |
|
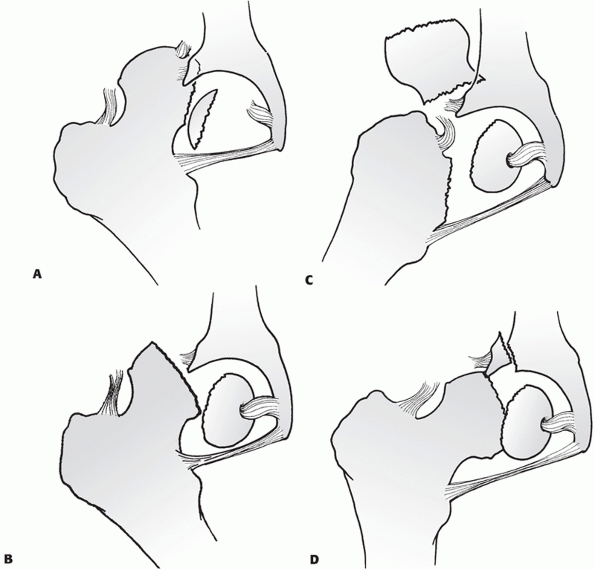
FIGURE 46-1
The position of the hip during axial loading determines the type of injury. Increasing flexion, adduction, and internal rotation favors pure dislocation, while lesser degrees of each leads to fracture-dislocation. (Adapted from Letournel E, Judet R. Fractures of the Acetabulum. 2nd ed. New York: Springer Verlag, 1993.) |
This mechanism may be present in deceleration injuries in which the
occupant is in a relaxed position during impact with the legs flexed,
abducted, and externally rotated, as well as in motorcycle accidents
where the legs are frequently hyperabducted. Using cadavers, Pringle
and Edwards128 were able to cause
anterior hip dislocations by hyperabduction and external rotation. The
degree of hip flexion determined the type of anterior dislocation, with
extension leading to a superior pubic dislocation and flexion resulting
in an inferior obturator dislocation.
reported on eight American football players who sustained a posterior
hip subluxation, primarily from a fall on the knee with the hip
adducted. They describe a characteristic triad of magnetic resonance
imaging (MRI) findings, including a small posterior wall fracture,
rupture of the iliofemoral ligament, and hemarthrosis as being
diagnostic.112 Aspiration was
recommended for large hemarthrosis as two of the eight went on to
severe AVN and hip replacement. Matsumoto et al.106
reviewed a large experience of skiing and snowboarding injuries. The
incidence of dislocation from snowboarding was five times higher than
skiing (0.45 vs. 0.09/100,000). Additionally, snowboarding injuries
were more commonly posterior dislocations and 30% had femoral head
fractures.
less obvious in mechanism than high-energy trauma. They occur in
patients with osteopenia, but may occur in healthy adults when
beginning a new exercise regimen.16,26,93,138,155,166,185
These are reported as “subchondral impaction” or “insufficiency”
fractures, but represent a significant injury to the femoral head. Song
et al.155 and Visuri et al.185
have reported a combined 17 cases of insufficiency fracture in military
recruits. Most were diagnosed on MRI, but several presented with
collapse seen on plain radiographs. Fourteen of the 17 had good
results, but two went on to total hip arthoplasty.
without femoral head fracture have been reported, as well as cases of
femoral head with and without femoral neck fractures without
dislocation.4,35,70,79,80,104,109,137,145,174
|
TABLE 46-2 Common Associated Fractures
|
|||||||
|---|---|---|---|---|---|---|---|
|
head fracture should be presumed to have multiple injuries. Up to 95%
of these patients have injuries that require inpatient management
independent of their dislocation.167 Intra-abdominal, head, and chest trauma are common associated injuries. Additionally, Marymont et al.102
described the association of thoracic aortic injury in combination with
posterior hip dislocations. Despite a typical presentation, including
extremity deformation, the diagnosis of hip dislocation may be delayed
due to more life-threatening associated injuries.
head, neck, or shaft fractures, acetabular fractures, pelvic fractures,
knee injuries, ankle and foot injuries, and neurologic injury (Table 46-2).
Knee injuries including posterior dislocation, cruciate ligament
injuries, and patellar fractures are common with posterior hip
dislocations due to direct trauma with the dashboard at impact (Fig. 46-2). Tabuenca et al.169
reported that 25% of 187 patients with hip dislocations and fracture
dislocations sustained a major knee injury. Seven of these injuries
were not diagnosed at the time of the initial hospital stay. Patients
should be treated with spinal precautions until the spine has been
radiographically cleared of injury. In the absence of femoral shaft or
neck fractures, the position and mobility of the extremity may indicate
a dislocation. In a posterior dislocation, the leg is flexed, adducted,
and internally rotated (see Fig. 46-1). Any
motion of the hip, particularly attempts to extend or externally rotate
the hip, is exceedingly painful. Conversely, anterior dislocations
present with the extremity externally rotated with varied amounts of
flexion and abduction.
 |
|
FIGURE 46-2
Photograph of a patient presenting after a dashboard injury. The patient sustained an open knee injury from the incident. The leg is flexed and internally rotated, indicating possible posterior dislocation. |
hip dislocation. Proper diagnosis of these injuries and their potential
influence on treatment is paramount. This begins with associated
fractures that may affect the ability of the surgeon to obtain a closed
reduction by manipulation of the lower extremity. Nondisplaced femoral
neck fractures are the most difficult of these to diagnose and are a
major potential pitfall. High quality radiographs of the femoral neck
in profile (15-degree internal rotation view) and sometimes computed
tomography (CT) scan are needed to rule out occult femoral neck
fracture before manipulative closed reduction is attempted. Fixation of
the neck may be needed prior to attempts at closed reduction of the hip
(see Fig. 46-27).
countertraction impossible, necessitating open reduction of the
dislocation (Fig. 46-3). Injury to the knee is
usually apparent on careful clinical examination and confirmed with
radiographic evaluation. Associated fractures of the hip itself, such
as acetabular wall fractures and femoral head fractures, may require
surgical intervention even if the hip dislocation is reduced closed.
Femoral head fractures or loose bodies from the head or acetabulum may
cause an incongruent reduction of the hip. Acetabular wall fractures
may allow for clinical instability even in the face of a congruent
reduction and require fixation. While this chapter
does
not cover the indications and techniques of posterior wall reduction
and fixation, the determination of hip stability in the presence of a
posterior wall fracture is important. This is discussed below (see “Current Treatment Options”), and is included in the treatment algorithm.
 |
|
FIGURE 46-3
A 23-year-old with an open hip fracture-dislocation with associated pelvic fractures including a symphyseal dislocation, and an ipsilateral fracture-dislocation of the sacroiliac joint. |
begin by palpation of all long bones and joints of the affected
extremity and a meticulous neurologic and vascular examination.
Emphasis on the prereduction function of the sciatic nerve is paramount
in posterior dislocations as the nerve can be injured during reduction.12,41,72,90,161,162
Careful testing of all branches is required, including foot eversion,
as weakness in the peroneals may be an isolated finding. Posterior
dislocations are associated with posterior knee dislocations, and,
although rare, anterior dislocations may injure the femoral vessels,
necessitating a careful assessment of distal pulses. Finally, the spine
and pelvis should be examined. While injury to these areas may be
clinically apparent, they cannot be ruled out without radiographic
studies.
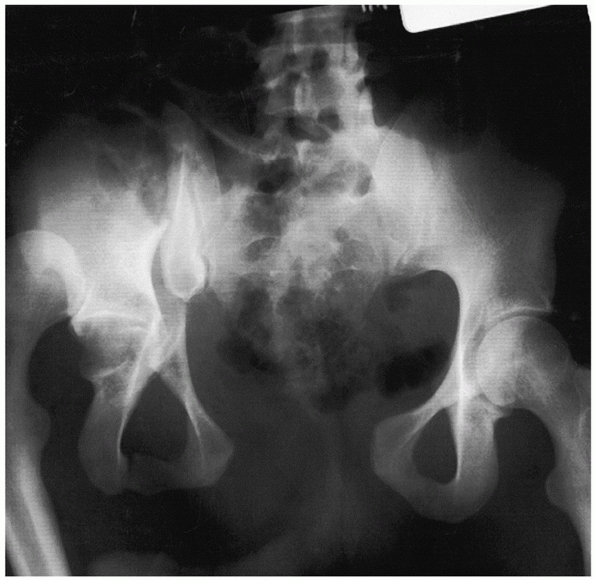
(AP) pelvis radiograph. This is usually taken as part of the initial
trauma workup before orthopaedic consultation is obtained and can help
to direct treatment. The diagnosis of hip dislocation should be
apparent on this single radiographic view (Fig. 46-4).
The key to the diagnosis on the plain AP pelvis is the loss of
congruence of the femoral head with the roof of the acetabulum. On a
true AP view, the head will appear larger than the contralateral head
if the dislocation is anterior and smaller if posterior. The most
common finding in the case of a posterior dislocation is a small head
that is overlapping the roof of the acetabulum. In an anterior
dislocation, the head may appear medial to or inferior to the
acetabulum.
rotation is also detectable on the single AP view. The lesser
trochanter is more apparent and the femoral neck is seen in profile
when the femur is internally rotated (see Fig. 46-4).
It is critical that the initial radiograph be of good quality and
carefully inspected for associated injuries before a reduction is
attempted. In particular, associated femoral neck fractures, which may
be nondisplaced, must not be overlooked. Likewise, associated femoral
head fractures are usually visible as a retained fragment in the joint.
Acetabular fractures and pelvic ring injuries are also visible on the
plain AP radiograph. Additional radiographic assessment is not usually
indicated before attempts at reduction unless a femoral neck fracture
cannot be ruled out or there is a clinical suspicion of a femur, knee,
or tibial injury that will affect the ability to use the extremity to
manipulate the hip. In such cases, biplanar radiographs of all
questionably affected areas must be obtained.
 |
|
FIGURE 46-4 The trauma AP pelvis radiograph of the patient in Fig. 46-2
demonstrates a posterior dislocation of the right hip. Note the superior location of the femoral head and the internally rotated proximal femur. |
the hip are deferred until after the hip is reduced, unless the hip is
irreducible. If the hip cannot be reduced, then it is advantageous to
obtain a preoperative radiographic series and CT scan to help in the
diagnosis of offending structures and to look for the possibility of
loose bodies in the joint or associated fractures that would require
removal or fixation during open reduction.
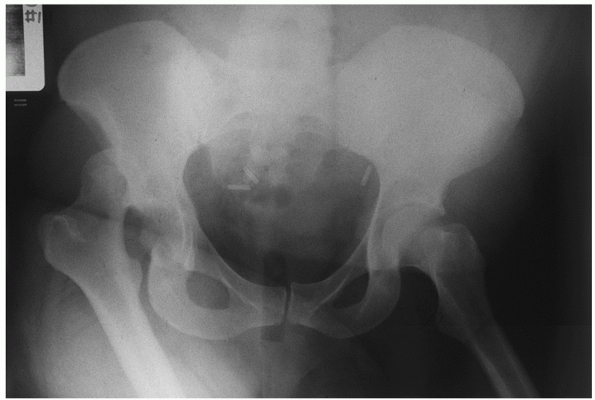
pelvis are obtained. Radiographs should include AP, both Judet
(45-degree oblique) views (Fig. 46-5), and an
inlet and outlet of the pelvis. It is best to focus the beam in the
center of the pelvis, as this allows for a direct comparison of the
affected hip with the normal hip when examining congruence and joint
space. When evaluating each of these views, the first issue is whether
there is a concentric reduction of the hip. The use of the
contralateral hip is necessary to answer this question. The congruence
of the hip is evaluated by comparing the relationship of the femoral
head to the roof on each view and comparing it to the contralateral
side. This relationship should show no loss of parallelism.
Additionally, the joint space should be equal to the contralateral hip.
The evaluation of these views for pelvic and acetabular fractures is
discussed elsewhere in the text.
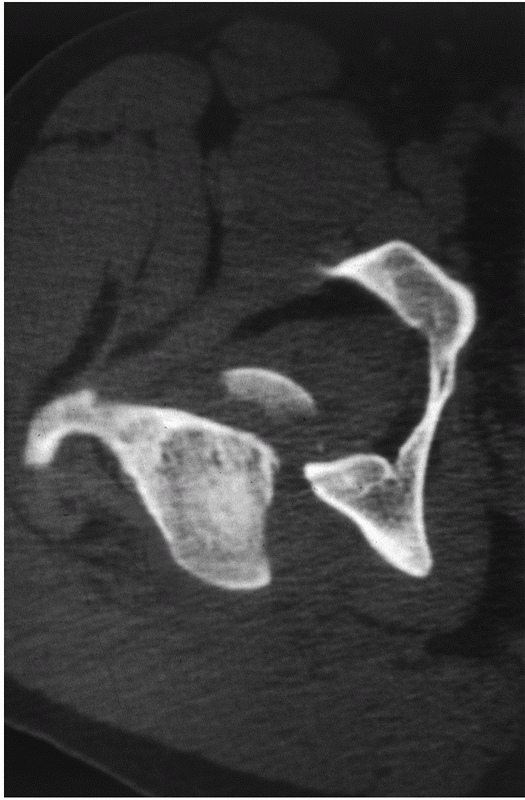
The CT scan is more sensitive in detecting small intra-articular
fragments, femoral head fractures, femoral head impaction injuries,
acetabular fractures, and joint incongruity.5,36,46,100,119,158,192 It has been demonstrated that intra-articular fragments are better visualized on CT than plain films. Hougaard et al.67
reported six cases of minor acetabular fracture and six cases of
retained intra-articular fragments visualized on CT and not visible on
plain radiographs in patients after closed reductions of posterior hip
dislocations. Additionally, Baird and colleagues5
demonstrated CT to be more sensitive than plain radiographs in
identifying 2-mm methylmethacrylate beads placed in cadaveric hips. The
congruence of the hip is also easily evaluated using CT. The head
should be in the center of the subchondral ring of the acetabulum as it
becomes visible, appearing as a bullseye.173
A difference of as small as 0.5 mm in the distance from the anterior,
articular surface to the femoral head has been reported to indicate a
subluxation of the hip.18 Impaction
injuries and femoral head fractures are much more easily seen on the
postreduction CT. The quality of the reduction of femoral head
fractures is also apparent and determines treatment. The CT scan also
aids in directing follow-up radiographic analysis in the case of
reduced femoral head fractures. Moed and Maxey111
suggested the use of specific angled radiographs based on the CT
determination of the fracture direction when obtaining follow-up
radiographs of femoral head fractures treated nonoperatively.
 |
|
FIGURE 46-5
A 53-year-old woman with a posterior hip dislocation demonstrating fragments in the joint prior to hip reduction and an inferior femoral head fracture (A). The postreduction AP and Judet views (B-D) demonstrate a widened joint space compared with the normal side and an incongruent reduction. Note that there are fragments both superior and inferior in the joint and that there is a loss of parallelism of the femoral head and acetabular articular surfaces. |
planning operative intervention when necessary in cases of concomitant
fracture, irreducible dislocation, or incongruent reduction. The
location, size, and number of free intra-articular fragments and the
location and size of femoral head fragments is clearly delineated,
allowing for accurate planning of operative procedures. Although CT is
very sensitive in identifying small, retained fragments, not all
intra-articular fragments will affect the treatment plan. This is
discussed in greater detail below (see “Current Treatment Options”).
performed MRI examinations of both hips in 18 patients after traumatic
dislocation at an average of 13 days postreduction. Trabecular changes
were noted in eight (44%) of the hips. However, since no follow-up data
are available for these patients, the usefulness of MRI in predicting
AVN or arthritis was not established. This is further manifest because
MRI changes of AVN may not be present before 6 to 8 weeks. MRI is also
useful in diagnosing insufficiency or impaction injuries from overuse,
and appears to be more sensitive than CT in detecting these lesions.17 A typical pattern of low density band with edema and contrast enhancement proximal and distal to the band is seen.177
The use of single photon emission computed tomography (SPECT) has been
shown to aid in distinguishing avascular changes from impaction
injuries of the femoral head.56
Despite its usefulness in this differentiation, SPECT has not been
helpful in predicting AVN when used in the peri-injury time frame. Yue
et al.195 studied 54 dislocations and
fracture dislocations pre- and postreduction and then followed the
patients for a minimum of 1 year. The average time to reduction of the
hip was 4 hours. They found that low blood flow patterns were seen in
early and late reductions, but that these patterns did not predict AVN
at an average of 24 months.
hip dislocations. All of these schemes include subtypes for important
associated injuries. The first distinction is whether the hip
dislocation is anterior or posterior. Anterior dislocations are
described by their anatomic location, being superior, including pubic
or subspinous, or inferior, including obturator, thyroid, and perineal
locations.2,8,19,20,30,54,152,159,164,188
In anterior dislocations, femoral head impaction injuries are more
common than shearing injuries. These are more apparent on the CT images
than on plain films (Fig. 46-6).
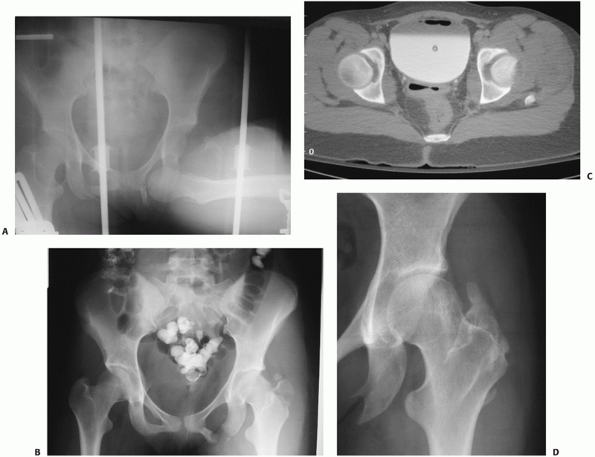 |
|
FIGURE 46-6
AP radiograph of a 16-year-old girl demonstrating an inferior anterior dislocation with greater trochanter fracture and femoral head impaction (A). The superolateral impaction is visualized on the postreduction AP (B), but more clearly seen on the CT (C). After the patient was stabilized, open elevation of the depressed articular surface was performed, using bone graft for support. At 2 years, the head has remodeled and the patient had excellent function (D). (Courtesy of William R Creevy, MD.) |
anterior dislocations. Two original classification schemes have been
described for posterior dislocations. Thompson and Epstein170 and subsequently Stewart and Milford162 both described systems incorporating associated fractures (Table 46-3).
The Stewart and Milford scheme specifically addresses postreduction
stability in the case of acetabular fracture, which has prognostic
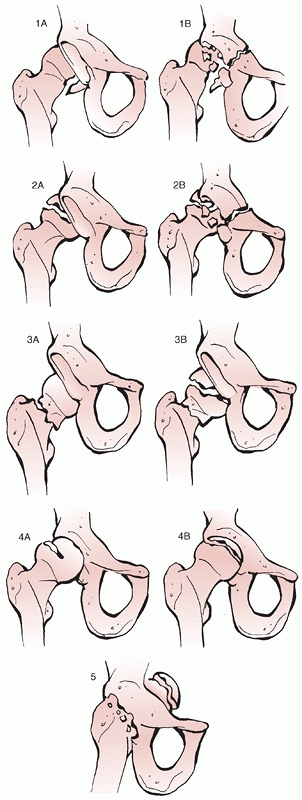
implications.68,162 Epstein’s type 5 dislocation includes a femoral head fracture. This type has been subdivided by Pipkin into four types (Table 46-4; Fig. 46-7).124 This scheme is commonly used and is important in decision making.
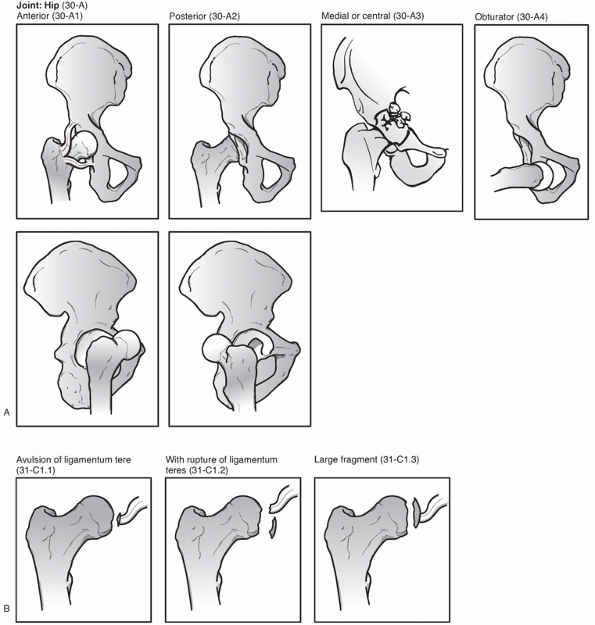
Brumback’s classification takes into account the size of the head
fragment, the direction of the dislocation, as well as the stability of
the hip (Fig. 46-8). Finally, the Orthopaedic Trauma Association’s comprehensive fracture classification scheme includes hip dislocations (Fig. 46-9).
|
TABLE 46-3 Classification Schemes for Posterior Hip Dislocations
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||
 |
|
FIGURE 46-7 The Pipkin classification of dislocations with femoral head fractures (see Table 46-3). Type I (A), type II (B), type III (C), and type IV (D).
|
|
TABLE 46-4 Pipkin Classification
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
|
TABLE 46-5 Brumback Classification of Femoral Head Fractures
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||
are whether there is an associated fracture and whether the hip is
stable after reduction. In each scheme, the presence of an acetabular
fracture requiring reduction and fixation is noted. For the purpose of
this text, these injuries are considered to be acetabular fractures and
are discussed in Chapter 45. This chapter
focuses on pure dislocations that are stable after reduction (whether
that be open or closed) and those with associated femoral head
fractures.
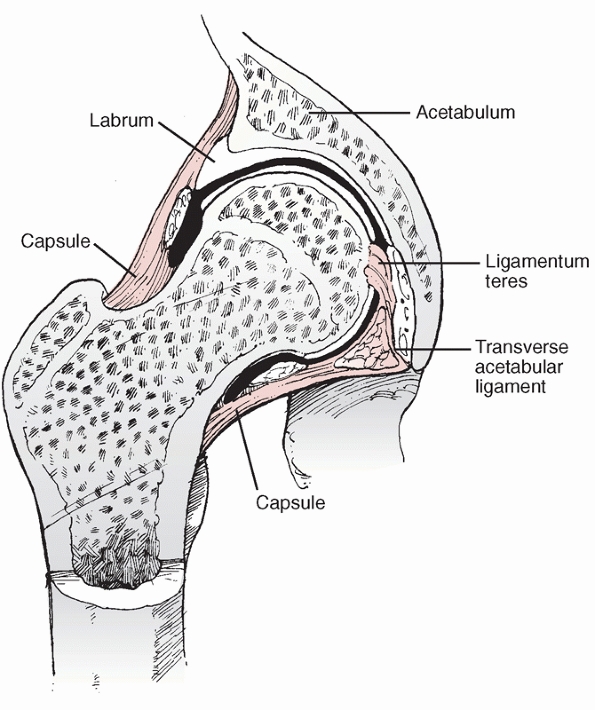
The head rotates within the acetabulum and is incompletely covered. The
depth of the acetabulum is supplemented by the fibrous labrum, which
makes the joint functionally deeper and more stable (Fig. 46-10).
The labrum adds more than 10% to the coverage of the femoral head,
creating a situation that keeps the head more than 50% covered during
motion.9,65,66,115,135 It takes more
than 400 N of force just to distract the hip joint.46
The capsule of the hip is strong and extends from the rim of the
acetabulum to the intertrochanteric line anteriorly and the femoral
neck posteriorly. The longitudinal fibers are supported by spiral
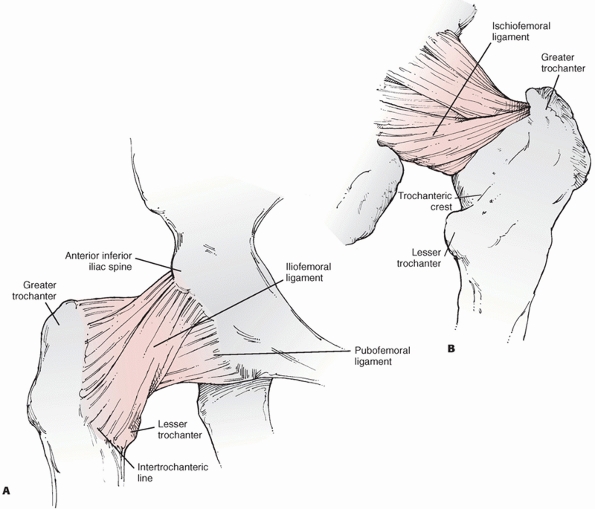
capsular thickenings called ligaments. Anteriorly, the iliofemoral or Y
ligament originates from the superior aspect of the joint at the ilium
and anterior inferior iliac spine. It runs in two bands inserting along
the intertrochanteric line superiorly and just superior to the lesser
trochanter inferiorly. The inferior capsule is further supported by the
pubofemoral ligament, which takes its origin from the superolateral
superior ramus and inserts on the intertrochanteric line deep to the Y
ligament (Fig. 46-11A).65,108
 |
|
FIGURE 46-8
The Brumback classification of hip dislocations with femoral head fractures. (Adapted from Stannard JP, Harris HW, Volgas DA, et al. Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Rel Res 2000;377:44-56.) |
 |
|
FIGURE 46-9 The Orthopaedic Trauma Association classification of hip dislocations (A) and femoral head fractures (B).
|
just inferior to the head medially and extends to the base of the
greater trochanter laterally. The ischiofemoral ligament within the
capsule posteriorly originates at the junction of the inferior
posterior wall with the ischium. It runs obliquely lateral and superior
to insert on the femoral neck with the capsule (see Fig. 46-11B).65,108 In addition to these ligaments, the short external
rotators lie on the posterior capsule, providing additional support.
 |
|
FIGURE 46-10 Coronal section of the hip of a child demonstrates the added depth that the labrum provides over the femoral head.
|
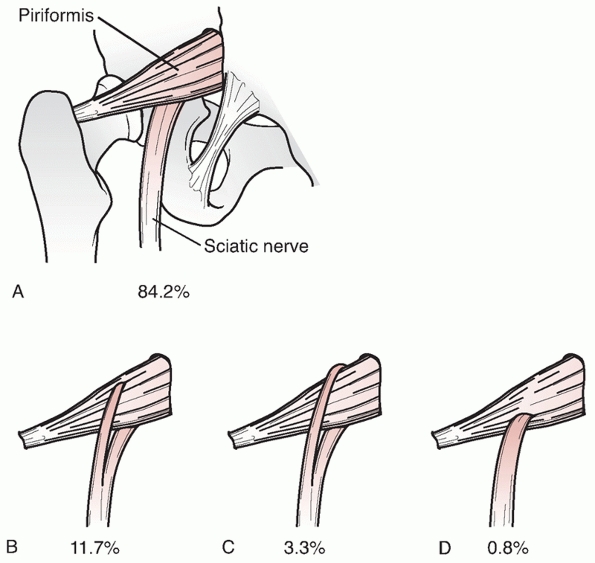
hip joint. The sciatic nerve warrants the most attention, as it is most
at risk. This nerve runs posteriorly to the joint, emerging from the
greater sciatic notch deep to the piriformis and superficial to the
obturator internis and gemelli muscles. In 85% of people, the nerve is
a singular structure located in the normal position. In 12%, it divides
prior to exiting the greater sciatic notch, and the peroneal division
passes through, rather than deep to, the piriformis muscle.7
In 3%, the nerve divisions surround the piriformis, and in 1%, the
entire nerve passes through the piriformis. With posterior dislocation,
the nerve may be stretched or directly compressed.
obturator foramen with the obturator artery. The femoral nerve lies
medial to the psoas in the same sheath and can be injured with anterior
dislocation.
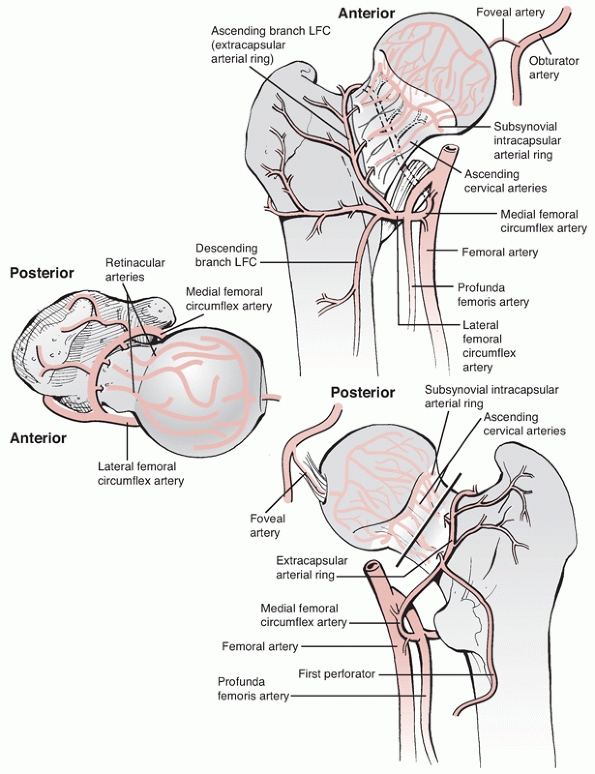
important factor in hip dislocations. In adults, the primary blood
supply to the head derives from the cervical arteries. These arteries
originate from the extracapsular ring at the base of the femoral neck (Fig. 46-12).
This ring is formed by contributions from the medial femoral circumflex
artery posteriorly and the lateral femoral circumflex anteriorly.71
The capital vessels traverse the capsule close to its insertion on the
neck and the trochanteric ridge and ascend parallel to the neck,
entering the head adjacent to the inferior articular surface.23,59,65
The superior and posterior vessels, which are derived primarily from
the medial femoral circumflex artery, have been shown to be the
dominant blood supply to the femoral head.52,55,75
In addition to the cervical vessels, a minor contribution to the head
arises from the foveal artery, a branch of the obturator artery that
lies within the ligamentum teres. This artery makes a significant
contribution to the epiphyseal portion of the femoral head vasculature
in approximately 75% of hips.27
vessels supplying the head, making the collateral circulation
important. Yue et al.196 did
injection studies of six cadaveric hips after forceful dislocation and
relocation. Filling defects were demonstrated at the junction of the
external iliac and common femoral arteries and at the circumflex
vessels as compared with the normal hip. However, this change in the
extraosseous blood supply did not provide a consistent change in the
intraosseous supply to the head, presumably due to collateral
circulation.
least a portion of the capsule must be disrupted. Labral tears or
avulsions and muscular injury are common.89 Pringle and Edwards128
examined the soft tissue injuries in cadavers in which they induced hip
dislocations. They found that the capsule may be stripped as a cuff
from either the acetabulum or femur by a rotational force or be split
by direct pressure. A combination of these capsular injuries may take
place resulting in an L-shaped lesion.
directly posteriorly or inferoposteriorly depending on the amount of
flexion at the time of the injury. The Y ligament is generally intact
with the capsule stripped from its acetabular attachment posterior to
it. However, in some cases, the Y ligament may be avulsed with a
fragment of bone.14
of the hip, and the capsule is disrupted anteriorly and inferiorly.
Although rare, in extremely high-energy injuries, the femoral vessels
can be injured or an open dislocation can occur.87
Avulsions are most common. When the hip dislocates, a small fragment
remains attached to the ligamentum teres, avulsing from the head. These
fragments, if small and within the fovea, are of minimal concern. More
severe injuries to the head involve a shearing mechanism or impaction
injury. Impaction is more common after anterior dislocation and may be
quite large (see Fig. 46-6).28
Shear injuries are usually the result of a posterior dislocation that
occurs with less adduction and internal rotation, forcing the head
against the rim of the posterior wall. In these cases, the head fails
in shear rather than the posterior wall fracturing. Because of the
mechanism, the fracture fragment is sheared from the anteromedial head,
with the fracture line running from anterolateral to posteromedial (Fig. 46-13).
These head fragments may be attached to the ligamentum teres and remain
in a relatively normal position or can be free of soft-tissue
attachments within the joint.
from comminution of associated fractures, shearing of cartilage, and
extra-articular fragments being pulled into the joint during the
reduction.
stability of the hip is derived from its role as the fulcrum about
which the large muscles that surround it act. These muscular actions
tend to force the femoral head into the acetabulum, taking advantage of
its depth. The capsule is loose compared to other joints allowing for
greater motion in multiple directions.
 |
|
FIGURE 46-11 The hip capsule and its thickenings (ligaments) as visualized from anteriorly (A) and posteriorly (B).
|
inferiorly. The articular cartilage, which resembles a horseshoe, is
thickest laterally and peripherally.79,136 This coincides with descriptions of the loading pattern of the acetabulum as being primarily peripheral.117
The articular cartilage of the head is thickest on the medial and
central surfaces. The position that the head takes within the
acetabulum is affected by the normal anteversion of the femoral neck on
the shaft of 12 degrees and by the neck-shaft angle, which averages 125
degrees.48 The neck-shaft angle
allows for freedom of motion by providing offset of the femur from the
pelvis. Variation in the neck-shaft angle is common, and can affect the
loading pattern of the hip. Likewise, deviation in anteversion affects
the position of the head within the acetabulum.
simple activities and are caused primarily by the force of the muscles
acting about the joint. During double leg stance, because few muscles
are necessary for balance, the joint reaction force is approximately
one third of body weight. This is in contradistinction to normal gait,
where the joint reaction force can reach six times body weight. With
respect to the rehabilitation of patients with hip joint injury, it is
important to note that due to the weight of the leg, the joint reaction
force on the hip in swing phase can be greater than body weight.48
Of equal importance to the hospitalized or injured patient is that the
act of getting on a bedpan can generate more than two times body weight
through the joint. The least force through the hip is with toe touch
weight bearing, which allows the ground to support the weight of the
leg rather than the hip musculature. The biomechanics of hip
dislocation include the factors of force of injury, native hip anatomy
such as anteversion, and the position of the
hip
at impact. Less anteversion and a position of internal rotation at
impact favor pure dislocation over fracture dislocation. This topic was
more completely reviewed above (see Mechanism of Injury).
 |
|
FIGURE 46-12
The vascular supply to the femoral head arises from the medial and lateral circumflex vessels, which create a ring giving rise to the cervical vessels. A minor contribution comes from the obturator artery via the ligamentum teres. (Modified from Gardner MJ, Suk M, Pearle A, et al. Surgical dislocation of the hip for fractures of the femoral head. J Orthop Trauma 2005;19:336.) |
when the hip is dislocated anteriorly or if there is an associated
femoral head fracture that needs to be reduced and stabilized. If an
irreducible dislocation is being addressed, then an anterolateral
approach is usually undertaken. This will avoid a dissection too close
to the femoral vessels, which are displaced by the dislocated femoral
head. Likewise, this is the approach of choice if a displaced femoral
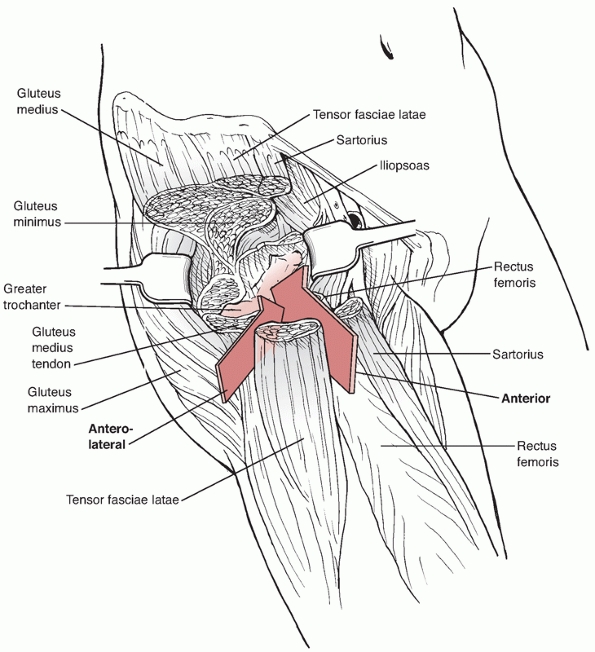
neck fracture is present. The deep interval is the same as the
Smith-Petersen approach, but the superficial dissection is lateral to,
rather than medial to, the tensor muscle (Fig. 46-14).
of the anterior aspect of the joint, the neck, and the anterior
acetabulum.
The
vessels may be protected and the hip reduced. The rectus, capsule,
labrum, bony fragments, and even the psoas tendon have been implicated
in irreducible anterior dislocations. Each of these structures must be
evaluated in the case of an irreducible anterior dislocation. Flexion
to relax the anterior structures makes the procedure easier. Often a
joker or other curved retractor can be used to lever a tight structure
over the head and allow for reduction. If there is no tendon blocking
the reduction, then distraction of the hip will provide for easier
digital inspection of the joint to remove fragments, capsule, labrum,
or avulsed muscle. This distraction is performed in flexion and mild
rotation using a bone hook on the trochanter to pull laterally.
Complete anesthetic paralysis of the patient is required.
 |
|
FIGURE 46-13
The fracture line of the femoral head is typically 25 to 45 degrees off the coronal axis with the free fragment located anteromedially. |
 |
|
FIGURE 46-14
The Smith-Petersen (direct anterior) and the Watson-Jones (anterolateral) approaches to the hip take the same deep interval but pass on different sides of the tensor in their superficial dissections. The anterior approach is well suited for femoral head fractures while the anterolateral approach is best for irreducible anterior dislocations. |
nonconcentric reductions. If careful radiographic and CT evaluation
after closed reduction demonstrates that the incongruent reduction is
caused by something located anteriorly in the joint, then an anterior
approach will allow for removal of the structure without redislocating
the hip. This is true regardless of the direction of the hip
dislocation. An excellent example of this is a type I femoral head
fracture in which the fracture fragment is causing an incongruent
reduction. A Smith-Petersen approach is used to access the anterior of
the joint. Distraction can be provided manually by an assistant or by
use of a femoral distractor from the anterior inferior iliac spine to
the trochanter. The fragment can be removed easily and the capsule
repaired. Likewise, soft tissue or bony fragments located in the front
of the joint are easily removed via this method.
reduction internal fixation (ORIF) of large femoral head fractures or
impaction injuries, which are usually located anteriorly. Either the
direct anterior or anterolateral approach can be used. If a large
impaction injury is present, then it can be elevated and grafted for
support via a window created at the articular margin.86
More commonly, a Pipkin type II fracture is present. If not
anatomically reduced after closed reduction, then ORIF is performed.
Since these fragments may remain attached to the ligamentum teres,
which provides blood supply for the fragment, the reduction should be
obtained with the hip reduced. If reduction is not possible with the
remaining femoral head in the acetabulum, it may be surgically
dislocated for the reduction without substantially increasing the rate
of AVN.131 An extensive radial
capsulotomy with vertical extension is required to obtain full
exposure. The fracture fragment is cleaned on its undersurface of all
clots, and the fracture bed is curetted. The joint is cleaned of all
free fragments before fixation is performed. External rotation of the
hip along with extension and mild abduction usually brings the bed into
direct view. Reducing the fragment is sometimes difficult because the
bed is typically circular and the fragment is thin and contains few
irregularities on its edge. It is paramount that the reduction is
anatomic, as an error in rotation may widen the head creating an
incongruent joint. One landmark that is commonly a useful key to the
reduction is the fovea. If an edge of the fracture fragment has some of
the fovea attached, this can be reduced first and aid the surgeon to
gain the correct rotational position. It is also prudent to temporarily
fix the fragment and get fluoroscopic views to confirm the reduction
prior to definitive fixation. If the rotation of the fragment is
incorrect, it will often be visible as a bulging of the head, or a lack
of circular shape, indicating a re-reduction is needed. After the
reduction is achieved, the fragment is fixed. Whatever method is used
must maintain a smooth joint surface. Screws must be seated below the
articular surface. Suture anchors and resorbable implants may be used
for especially narrow fragments.
obtained before closure to confirm an anatomic reduction regardless of
the procedure performed.
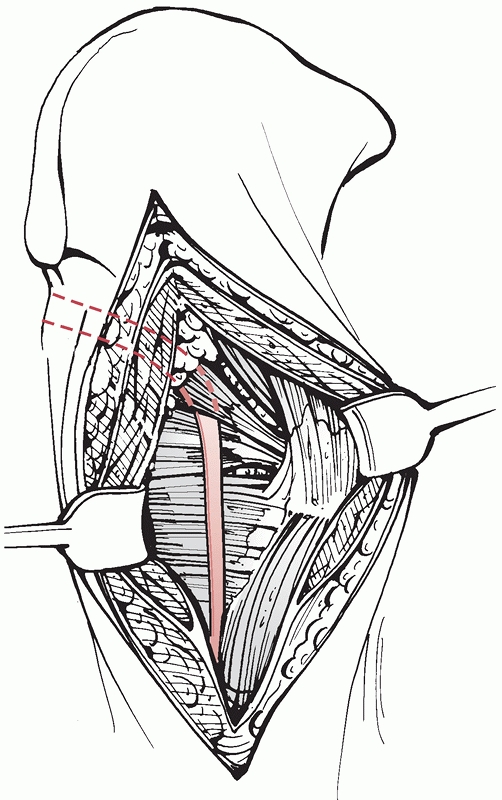
irreducible posterior dislocation, a nonconcentric reduction with
posterior interposition, or dislocation associated with posterior wall
fracture requiring fixation.
fractures is frequently performed with the patient prone, open
reduction of an irreducible dislocation of the hip is easiest with the
patient in the lateral position.95,96
A Kocher-Langenbeck approach exposes the posterior aspect of the hip
and allows for direct exposure and protection of the sciatic nerve.
Identification of the sciatic nerve is the first step of the procedure,
as it may be trapped or injured by the dislocation or the reduction. In
the face of an irreducible dislocation, the piriformis tendon, maximus
muscle, ligamentum teres, labrum, capsular attachment, or bony fragment
may prevent reduction. The sciatic nerve may be tented over the
dislocated head, which is apparent immediately upon splitting the
gluteus maximus muscle. The nerve must be identified at this point in
the procedure. This is best accomplished by finding it distal to the
area of the disruption. To achieve this, the gluteus maximus tendon can
be released at its distal insertion (Fig. 46-15).
This takes pressure off the muscular envelope and makes identification
of the sciatic nerve more straightforward. The nerve is located medial
to the maximus insertion and dorsal to the quadratus femoris muscle.
Gentle extension of the hip will take tension off the nerve and the
posterior structures. Likewise, the knee should be kept flexed at 90
degrees at all times to relax the tension on the nerve. Once the nerve
is identified distal to the hip joint, it is followed proximally and
freed from impingement. The nerve emerges as one branch from under
(anterior to) the piriformis tendon and passes behind (dorsal to) the
obturator internus tendon in 84% of cases (Fig. 46-16).7
In other cases, it may be two branches and either surround or traverse
the piriformis tendon. In either case, the tendon must be followed back
to its origin from the greater sciatic notch to ensure its safety.
After this, the piriformis tendon may be released from the greater
trochanter. This will enable the reduction if the piriformis was
wrapped under the head and provide better exposure of the joint if
necessary. Offending structures are removed from the hip joint and the
hip is reduced. If the superior posterior wall is entrapped, it may be
attached to the iliofemoral ligament or labrum.14
Prying the fragment inferiorly and posteriorly is possible with distal
and lateral traction on the femoral head via the trochanter. Posterior
wall fragments or labrum that is stuck
in
the joint is difficult to free and, on occasion, must be forced
anteriorly on its pedicle to remove it. The intact portion of the
labrum is always the anchor of these fragments so identification is
imperative in determining the direction of removal. If the labrum is
intact superiorly, then the fragment must come out superiorly, and vice
versa.
 |
|
FIGURE 46-15
The sciatic nerve runs medially to the insertion of the gluteus maximus tendon and posteriorly to the quadratus. It is safest to identify the nerve distally in the wound by releasing the maximus tendon when performing an open reduction of the hip. |
 |
|
FIGURE 46-16 A-D.
The sciatic nerve is a single structure that emerges from the greater sciatic notch anterior to the piriformis in 84% of cases. In 16%, a portion of the nerve passes through the piriformis or posterior to it, placing it at greater risk. |
removed from the joint, and the nerve is safely retracted, the hip may
be reduced. Again, high-quality radiographs in the operating room are
needed to confirm a congruent reduction as evacuation of the joint is
challenging. Care should be taken to avoid damage to the medial femoral
circumflex vessel within the quadratus femoris. If dissection of this
muscle is necessary, it should always be performed from the acetabular
side. Once the hip is reduced, labral detachments can be repaired using
suture anchors to a freshened cancellous bed.47,172
Small posterior wall fractures are also fixed since the exposure is
already available. Spring plates may be used for fragments too small to
accept lag screws. Finally, débridement of any damaged muscle,
particularly the gluteus minimus, may help prevent heterotopic
ossification.132 Repair of all tendons is followed by a careful closure over drains.
 |
|
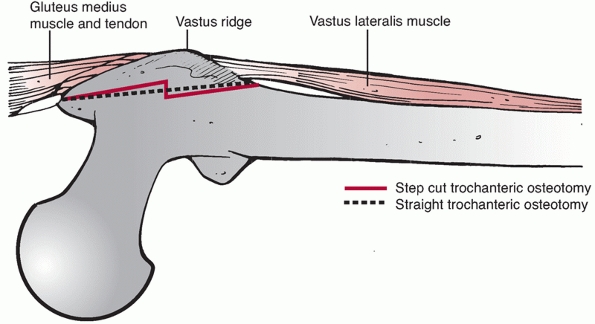
FIGURE 46-17 Diagram of trochanteric osteotomy. The osteotomy can be made as a straight cut (dashed line) or as a step cut (solid line).
In either case, proximally the osteotomy starts within the tendon of the gluteus medius in the middle of the tip of the trochanter and ends just distal to the vastus ridge. |
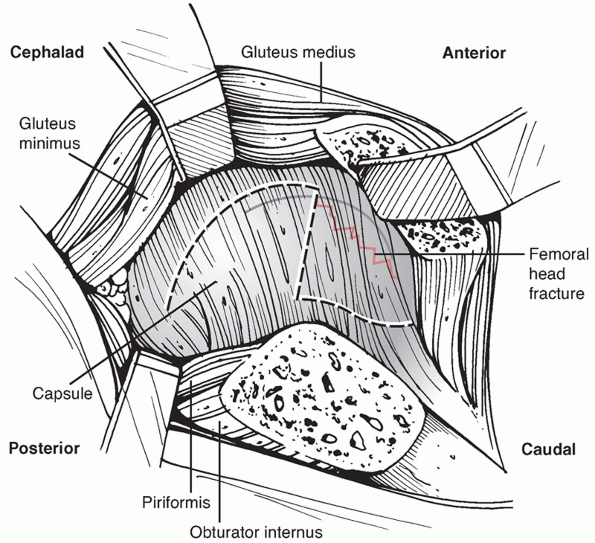
dislocate the hip can be used to treat all four types of Pipkin
fractures. The approach, as described by Ganz,50
respects the blood supply to the femoral head and gives excellent
access to the femoral head as well as to the articular side of the
acetabulum. This approach is particularly useful for the treatment of
combined femoral head and acetabular fractures.117,121
is used to prevent iatrogenic damage to the gluteus maximus muscle. For
optimal exposure, the interval between the TFL and gluteus maximus is
divided as proximally as possible and extended to the insertion of the
gluteus maximus tendon on the posterior femur distally. Alternatively,
a transgluteal approach similar to a standard Kocher-Langenbeck
approach can be used to expose the lateral portion of the femur. The
posterior portion of the trochanter is identified and prepared for the
digastric osteotomy. The posterior portion of the gluteus medius is
palpated and the proximal end of the osteotomy should be performed in
the middle of the tip of the trochanter and the gluteus medius tendon.
This prevents the osteotomy from injuring the main branch of the medial
femoral circumflex artery (MFCA) on the obturator externus or the
anastomosis of the internal gluteal artery and the MFCA, which lies on
the posterior border of the piriformis tendon.52,55 The osteotomy exits distal to the vastus ridge and can be performed as a straight or as a step osteotomy (Fig. 46-17).6,143
Once the osteotomy is made, it is elevated anteriorly, the remnant of
the gluteus medius is released from the intact tip of the trochanter,
and superior border of the piriformis tendon is identified. The gluteus
minimus is then dissected off the capsule posteriorly. Anteriorly, to
help elevate the vastus lateralis and intermedius off the anterior
capsule and anterior femur the hip is slowly abducted, externally
rotated, and flexed. The hallmark
of the digastric osteotomy is continuity above and below the shallow bone with an intact soft tissue sleeve.
can be palpated a Z-shaped capsulotomy is performed along the superior
anterior portion of the femoral neck. At the anterior rim of the
acetabulum, the capsulotomy is curved posteriorly and follows along the
acetabular rim. The anterior limb of the capsulotomy goes inferiorly
along the intertrochanteric ridge in a manner that leaves a cuff of
tissue along the ridge to allow for reattachment at closure (Fig. 46-18).
With the capsulotomy performed, a bone hook is placed around the
femoral neck and, as an assistant flexes and externally rotates the
femur, the bone hook is used to subluxate and then dislocate the hip.
If the ligamentum is intact to the femoral head it needs to be
transected to allow for full dislocation and visualization of the
femoral head. This is a safe procedure with respect to the blood supply
of the head. With the hip dislocated, the leg is externally rotated and
the foot is placed in a sterile bag anteriorly. External rotation
allows for more exposure of the femoral head. Fracture fragments and
areas of impaction, which usually occur adjacent to the fracture edges,
can be addressed.
expose the entire hip joint, an increased ability to address areas of
impaction (Fig. 46-19), visualize the reduction
circumferentially, increased ability to treat concomitant labral
detachments, and an improved ability to ensure implant placement is not
intra-articular (Fig. 46-20). Additionally, the
surgical dislocation approach allows for the treatment of femoral head
fracture with or without associated fractures of the femoral neck or
acetabulum.62,83,154
Complete dislocation of the femoral head allows for a thorough
débridement of loose bodies from the hip joint. Avulsions or tears of
the acetabular labrum are repaired to the acetabular rim with suture
anchors, as described for the treatment of femoroacetabular
impingingement.45 Surgical dislocation has primarily been described for the treatment of femoroacetabular impingement50 and acetabular fractures.149,150
More recently, some authors have reported using a surgical dislocation
approach for all femoral head fracture, in particular when there is an
associated acetabular fracture.85,154
 |
|
FIGURE 46-18
Diagram of capsulotomy for a surgical dislocation. The capsulotomy is Z-shaped with the transverse portion inline with the femoral neck in the superior anterior portion of the joint. The distal limb should be on the femoral side and the proximal portion going posteriorly should be along the acetabulum, keeping the capsulotomy away from the MFCA. (Modified from Gardner MJ, Suk M, Pearle A, et al. Surgical dislocation of the hip for fractures of the femoral head. J Orthop Trauma 2005;19:336.) |
series of 12 patients with femoral head fractures treated with surgical
dislocation, no patient had a nonunion of the trochanteric osteotomy
after the primary surgery for fracture fixation. One patient did have a
nonunion after a third hip revision for an arthroplasty 6 years
following a Pipkin type IV injury. Ganz50
also reported no cases of AVN in his series, demonstrating that the
approach does not cause AVN in the elective setting. Solberg154 reported one case of AVN in a Pipkin IV fracture, and Henle62
had two cases of AVN also in type IV injuries, making it difficult to
determine if there was a causal relationship of the approach with this
complication.
is an attempt at a closed reduction. The reduction should be considered
an emergent procedure and includes patients with concomitant femoral
head fractures or acetabular fractures.11,68,72,86,88,95,129,161,171
As previously discussed, nondisplaced femoral neck fractures and other
injuries that preclude using the lower extremity to manipulate the hip
are a contraindication to standard closed reduction. For dislocations
without associated fractures that result in a congruent reduction by
closed means, nonoperative management is usually definitive (Table 46-6). However, irreducible dislocations, those with incongruent reductions,
and those with associated fractures may require subsequent operative management.
 |
|
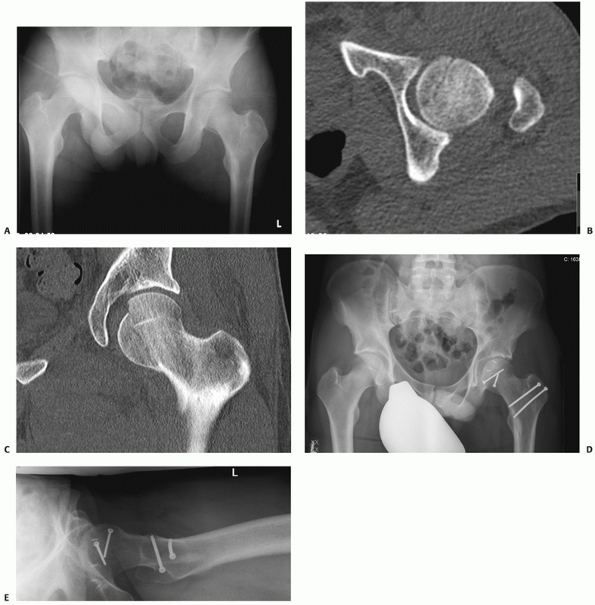
FIGURE 46-19
A 25-year-old male who sustained a Pipkin type II injury and at the time of open reduction using surgical dislocation approach, a labral avulsion was identified and repaired with suture anchors. Injury films include and AP (A) pelvis and CT (B,C) scan. Postreduction films (D,E) include a AP pelvis and lateral hip. (Courtesy of Lorenz Büchler, MD, from Inselspital, University of Bern, Switzerland.) |
Regardless of the technique, the patient must be completely relaxed. If
the patient is already intubated due to other injuries, then the
reduction may take place in the emergency department with proper
monitoring after paralytic agents are given. In other circumstances,
the reduction should be performed in the operating room unless one is
not available. This provides the safest situation for control of the
patient’s airway. In rare circumstances, the reduction may need to be
performed in the emergency department under conscious sedation. It is
best to have an emergency physician or anesthesiologist present to
control the airway during the procedure and to monitor the patient’s
oxygenation. Although not uniformly agreed upon, most authors believe
that no more than two closed reduction attempts should be made to avoid
further damage to the femoral head.11,28,41,161,162,181
Another advantage of performing the reduction in the operating room is
the use of real time fluoroscopy to aid in the reduction. The position
of the head with respect to the acetabulum can be visualized well if
there is difficulty reducing the hip, and adjustments based on the
position can be made.
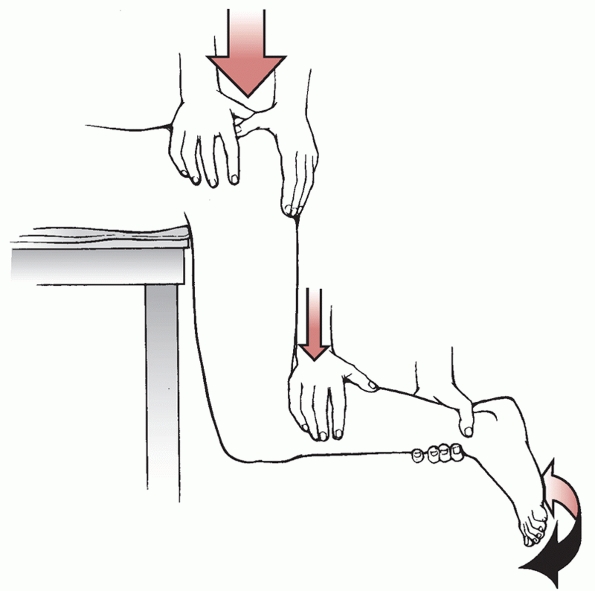
on the operating table with the hips flexed at the end of the bed and
the legs hanging over. The assistant stabilizes the pelvis and prevents
the patient from sliding off the table. The surgeon keeps the knee
flexed to 90 degrees and applies downward pressure on the leg in a
steady fashion (Fig. 46-21).
The gravity of the leg along with the downward pressure reduces the
hip. Gentle rotation during the maneuver may assist the femoral head to
walk over the rim of the acetabulum into the reduced position.
 |
|
FIGURE 46-20 A. AP radiograph of the right hip in a 36-year-old male with a Pipkin type IV injury. B.
An intraoperative picture of the femoral head demonstrating areas of impaction and cartilage damage. The picture is looking at the inferior aspect of the femoral neck taken from the front of the patient in the lateral position. C. This shows the femoral head from the opposite side of the table, standing behind the patient and looking in the caudal direction. (Courtesy of Prof. Alessandro Massé, San Lugi Ospedale, Torino, Italy.) |
|
TABLE 46-6 Patterns Treated Nonoperatively
|
||||
|---|---|---|---|---|
|
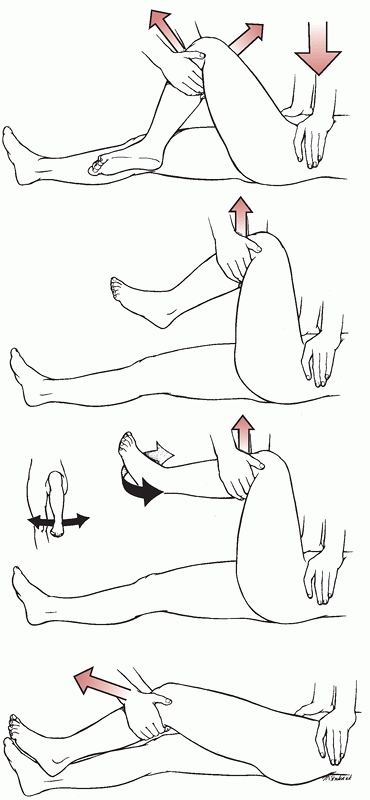
is appropriate even in the face of other traumatic injuries. It is
performed with the patient in the supine position and uses the familiar
traction and countertraction techniques that are used to reduce other
joints. The patient is placed supine on a stable table. The assistant
stabilizes the pelvis, usually by pushing down on the anterior superior
iliac spine while pushing laterally on the inner proximal thigh. The
surgeon then flexes the knee and the hip to relax the hamstrings.
Steady longitudinal traction is then applied with the extremity in
internal rotation and adduction. While the traction is being applied,
the leg is gently rotated, allowing the reduction (Fig. 46-22).
Several modifications of this technique have been described. The “East
Baltimore Lift” utilizes several assistants in an attempt to make the
reduction less demanding on the surgeon.141 Performing the reduction in the lateral position has been suggested to diminish the risk of lower back injury to the surgeon.24
 |
|
FIGURE 46-21 The Stimson164 gravity method of reduction.
|
dislocation, after the reduction is accomplished the hip is extended
and externally rotated and a knee immobilizer is placed on the leg.
These measures will maintain the hip reduced while postreduction
studies are obtained.
technique. Traction is continuously applied in line with the femur with
gentle flexion. Along with a lateral push on the inner thigh, internal
rotation and adduction are used to reduce the hip (Fig. 46-23).
If the dislocation is superior, then distal traction is applied until
the head is at the level of the acetabulum and gentle internal rotation
is applied. Extension may be necessary when reducing anterior
dislocations.30
careful to use continuous traction rather than short jerky motions. By
using continuous distraction and gentle manipulation, the reduction is
achieved while minimizing additional trauma. Sudden forceful movements
can cause fractures of the neck and damage the articular surface of the
femoral head.126,173
after the reduction is obtained, a full set of radiographs and 2-mm CT
through the hip should be obtained. These studies determine if the
reduction is congruous. If the hip is congruous and there are no
associated fractures of the acetabulum or femoral head that require
surgery, then nonoperative management is generally definitive. This is
the case even if there are small fragments of bone retained in the
fovea of the hip joint. As long as there are no fragments making
contact with the articular surface of the head during movement and the
fragments are not between the articular surfaces of the head and
acetabulum, small fragments do not require débridement (Fig. 46-24). These bony fragments are attached to the ligamentum teres and are not free to move within the joint.
fractures exist that do not require fixation or cause instability of
the hip. Two types of injury fall into this category: Pipkin type I
femoral head fractures, which do not create incongruity, and small
posterior wall fractures that do not allow for instability. The amount
of posterior wall that can be affected without causing instability is
debated. If greater than 35% of the posterior wall is affected, the
loading pattern of the hip is altered and may lead to arthritis.118
On the basis of cadaveric studies, most authors would recommend ORIF of
these fractures. A more complete discussion of this topic and
techniques of fixation is included in Chapter 45
on acetabular fractures. For the purpose of this discussion, we will
consider only posterior wall fragments that do not necessarily require
reduction and fixation based on their size. If the posterior wall
fragment is small enough that fixation may not be required, stability
testing can be performed
to ensure that the hip is stable.173
With the patient asleep or sedated, the hip is brought through a range
of motion under fluoroscopy. It is flexed and internally rotated and
then pressure is placed posteriorly in line with the femur. AP and
obturator oblique views are taken. Any change in the congruous
relationship of the head to the roof indicates posterior subluxation,
and the hip should be considered unstable (Stewart and Milford type
III) (Fig. 46-25). In a small series, Tornetta172
reported a fragment consisting of only 15% of the posterior wall caused
instability. If the hip is found to be stable, then nonoperative
management may be chosen as definitive.
 |
|
FIGURE 46-22 The Allis1 reduction technique for posterior hip dislocations.
|
 |
|
FIGURE 46-23 The Allis1 maneuver for anterior dislocations.
|
fractures may also be treated nonoperatively. In cases of inferior
femoral head fractures (Pipkin type I), the fracture fragment does not
affect the weight-bearing surface. These fracture fragments are not
loaded during normal gait and therefore may be treated as loose bodies.69,124,160
If the fragments are well reduced or in a position that does not create
an incongruent reduction of the hip, they can be left in place. Thus,
fixation or excision is not necessary if the reduction of the hip is
congruent. These injuries may be treated with the same nonoperative
protocol as a pure hip dislocation.
 |
|
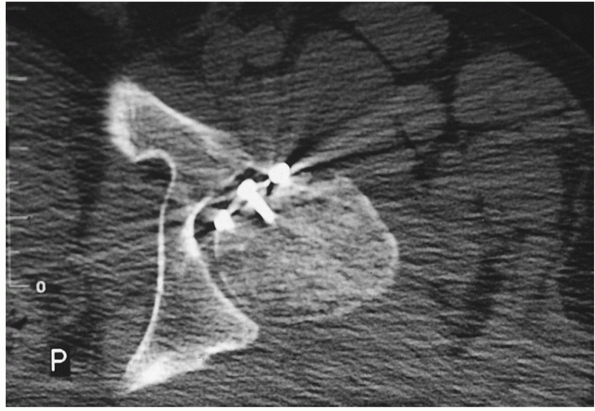
FIGURE 46-24
The postreduction CT of a patient after posterior dislocation demonstrates a small, insignificant fragment in the fovea centralis, which does not affect the congruous hip reduction and does not require removal. Fragments are considered insignificant if they clearly do not impinge on the head. |
The indications for open reduction are an irreducible dislocation,
sciatic nerve injury caused by a reduction attempt, and cases of
incongruent reduction.
reduction. Approximately 2% to 15% of dislocated hips are irreducible
via closed means.27 The offending structure may be a bony impingement or soft tissue interposition (Table 46-8).
Anterior dislocations are associated with interposition of the rectus
femoris, the iliopsoas, the anterior hip capsule, or the labrum.41,61,74,76,98,99,191 Buttonholing though the capsule and bony impingement in the obturator foramen have also been reported.140,173
In posterior dislocations, the causes of irreducibility are
buttonholing though the posterior capsule, and interposition of the
piriformis, gluteus maximus, ligamentum teres, labrum, or large bone
fragments.14,20,25,72,81,116,122,151 Metha et al.107
reported on irreducible fracture-dislocations of femoral head without a
fracture of the posterior acetabular wall and reported this occurred in
about 10% of femoral head fracture-dislocations. In all cases, the
displaced proximal femur had herniated through a posterior-superior
traumatic interval between the acetabular rim and the labrum.107
identifying the offending structure and planning the surgery. If well
coordinated, the additional CT cuts can be done during the trauma CT
scan and not require a second examination. A full series of radiographs
and the fine-cut CT are desirable before performing the open reduction;
however, substantial delays should not be accepted. If the reduction of
the hip will be significantly delayed by obtaining the CT scan, then it
can be deferred until after the open reduction is performed.
a nonconcentric reduction is not an emergency. The head is contained
within the acetabulum and the blood supply to the head that is not
thrombosed or torn is restored.147,196
Thus, the time to obtain all preoperative studies is available,
allowing for the most controlled circumstance for the surgery.
Incongruent reductions occur if there are bony fragments or soft tissue
interposed in the acetabulum, preventing a congruous reduction. Free
fragments located between the femoral head and acetabular articular
cartilage must be removed (Fig. 46-26). The
postreduction CT will demonstrate the location, size, and number of
offending bony fragments allowing better planning of the procedure.
Fragments treated by débridement include avulsions from the femoral
head, inferior femoral head fractures (Pipkin type I), loose fragments
from the posterior wall, and cartilage fragments sheared from the
femoral head.20,22,25,41,122,151,156,170 Pure hip dislocations,
because there are no free bony fragments, have a lower rate of
nonconcentric reduction than fracture dislocations of the hip, which
generate more bony debris.11,72,129,170
 |
|
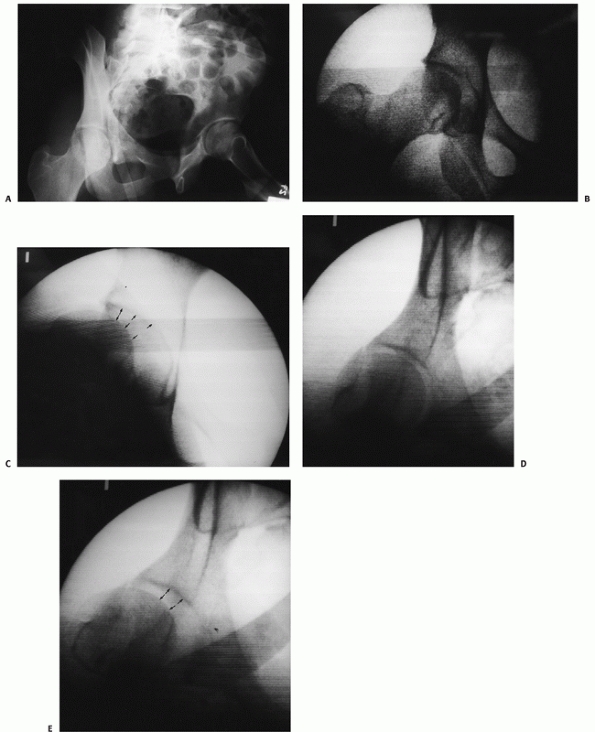
FIGURE 46-25
The obturator oblique view of a patient after closed reduction of a posterior hip dislocation with associated small posterior wall fracture (A). In the operating room with the patient asleep, the AP view of the hip demonstrates a congruent relationship of the head to the roof (B). With flexion of the hip, the head subluxes away from the roof (arrows) and becomes incongruous, indicating instability (C). The posterior subluxation is also evident on the obturator oblique view (D,E). |
|
TABLE 46-7 Patterns Treated with Open Reduction and Débridement
|
|||||
|---|---|---|---|---|---|
|
leaving femoral head and neck fractures to be discussed here. In the
rare case of a young patient with an associated femoral neck fracture
and hip dislocation, the dislocation requires open reduction and the
hip fracture should be fixed acutely. If the fracture is not displaced,
then fixation of the neck may precede reduction of the hip if it can be
accomplished expeditiously (Fig. 46-27). If the
neck fracture is displaced, then the femoral head reduction will enable
reduction of the neck and should be performed emergently. The treatment
of this combination injury becomes different in the older population.
For elderly patients, a hemiarthroplasty may be favorable to ORIF as
the hip dislocation adds to the likelihood of AVN.
may also be candidates for ORIF. Specifically, Pipkin type II fractures
in which the fracture line extends cephalad to the fovea into the
weight-bearing surface of the femoral head require accurate alignment.
In many cases, these fractures align well with reduction of the hip as
they are held in their normal position by the ligamentum teres.68
The postreduction CT of the joint in conjunction with the AP and Judet
views will demonstrate any displacement. If the reduction is near
perfect, then nonoperative management has been recommended (Fig. 46-28).15,78,124,168 If the fragment is not anatomically reduced, then ORIF is performed (Fig. 46-29).
Fixation of these fractures can be challenging, as the fragment is
frequently shallow, having been caused by a shearing mechanism.
|
TABLE 46-8 Causes of Irreducible Dislocation
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
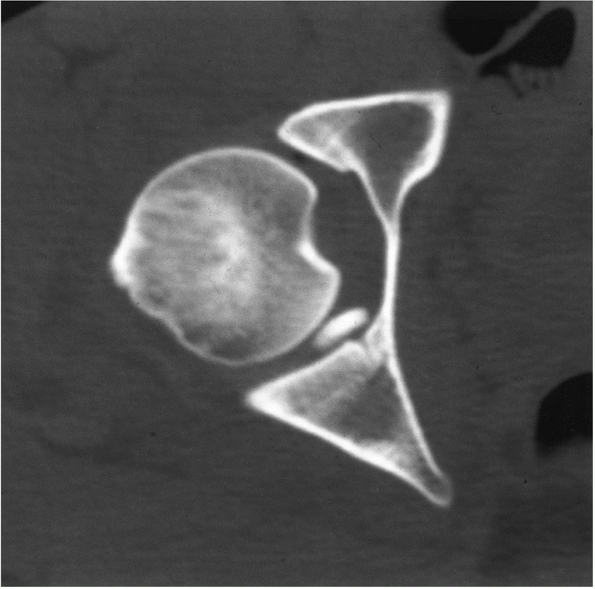
FIGURE 46-26
CT scan demonstrating a fragment of bone interposed between the femoral head and posterior articular surface that requires removal. |
debated. Because the fracture is caused by the femoral head impinging
on the posterior wall of the acetabulum in an internally rotated
position, the fracture fragment of the head is located anteromedially.
Moed and Maxey111 demonstrated that
the fracture angle in these cases is usually between 25 and 45 degrees
off the sagittal plane, creating an anteromedial fragment. Although
Epstein had recommended débridement of the joint via a posterior
approach to utilize the already damaged capsule, this may not apply to
femoral head fractures.162,168,170
To reduce and fix an anteromedial fracture of the femoral head from a
posterior approach, the hip may require redislocation. Even with the
femoral head out of the acetabulum, anatomic reduction may be difficult
without disrupting the ligamentum from the femoral head fragment,
potentially devascularizing it. Positioning the intact posterolateral
head against the anteromedial fragment without disrupting its soft
tissue is extremely difficult, and at best visualization of only a
portion of the fracture is possible. In contradistinction to the
posterior approach, an anterior approach allows for direct
visualization of the femoral head fragment without redislocating the
hip. External rotation of the hip allows for cleaning of the fracture
bed and accurate reduction of the fragment. Since the major blood
supply to the femoral head arises from the posterior cervical branches,
which may be damaged, there is a concern for anterior surgical
dissection.
Swiontkowski and colleagues168
compared the anterior and posterior approaches in the management of
femoral head fractures meeting operative criteria. The incidence of AVN
was not increased in hips treated via the anterior approach versus the
posterior approach. The anterior approach allowed for an easier
reduction and better visualization. Of note, however, there was a
slightly higher rate of heterotopic ossification after anterior
approaches that did not affect outcome. Likewise, Stannard et al.157
found a higher rate of AVN after posterior than anterior approach for
treatment of femoral head fractures. Four of five patients treated via
a posterior approach developed AVN to some degree.
 |
|
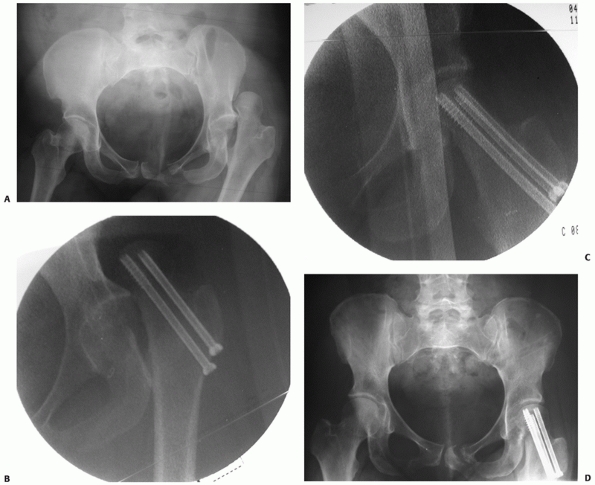
FIGURE 46-27
AP radiograph of a 36-year-old who sustained a posterior hip dislocation, impaction of the femoral head, and a minimally displaced valgus femoral neck fracture in addition to type 2 anteroposterior compression pelvic injury (A). The patient was brought emergently to the operating room where the femoral neck was fixed with percutaneous screws prior to the reduction (B). After fixation, the hip was able to be reduced closed (C). At 6 months, the patient had no signs or symptoms of AVN and minor posterior pelvic pain (D). |
has also been described to treat these fractures. More commonly used to
treat the prearthritic condition of femoroacetabular impingement the
approach is ideal for treating femoral head fractures. Siebenrock149,150
has also reported using this approach to treat acetabular fractures.
More recently, his colleagues reported on a series of 12 patients with
femoral head fractures treated with surgical dislocation.62
In this group, 83% had good to excellent outcomes as compared with 21
patients treated through other approaches (Watson-Jones,
Smith-Petersen, and Kocher-langenbeck) at their institution in whom
only 56% of patients had good to excellent outcomes.83 Other authors have also described this technique for femoral head fractures,51 in particular those with combined posterior wall lesions.51,85,154
While this is a logical approach for the treatment of femoral head
fractures, thus far only small numbers of patients have been reported
on. As more patients are treated with this approach, better comparisons
with other approaches will be possible in terms of the complication
rates and medium- to long-term outcomes.
 |
|
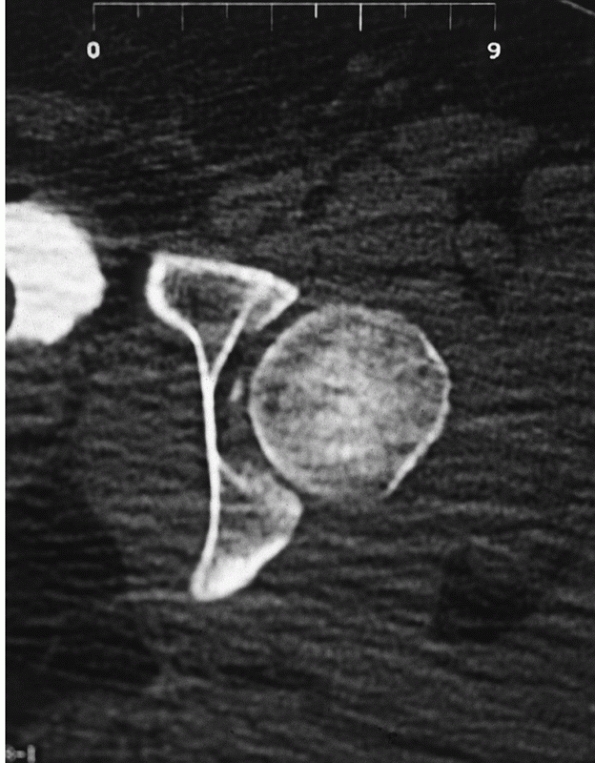
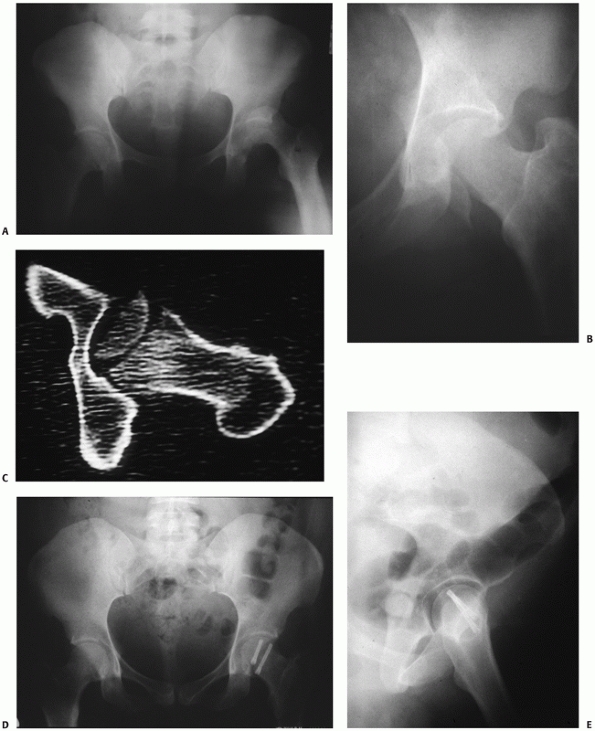
FIGURE 46-28 AP view of posterior hip dislocation with associated femoral head fracture (A).
CT scan after reduction of the hip demonstrates an anatomic reduction of the fragment at the level of the fovea and a congruent joint (B). The injury was treated nonoperatively, and at 2 years the patient has no pain and no arthritis (C). |
shallow nature of the fragment. Techniques that allow for subarticular
fixation are necessary. These include the use of screws with no heads,
such as Herbert screws or Acutrax screws, countersinking screws with
heads, resorbable pin fixation, and suture repair. Regardless of the
chosen technique, it is imperative that the fixation is in subchondral
bone and does not protrude (Fig. 46-30). Stannard et al.157
recently reported a high failure rate of cannulated 3.0-mm screws made
to screw into special washers (Synthes, Paoli, PA) and recommended
against their use.
femoral head impaction injury. Recent biomechanical studies have shown
that a 2-cm2 area must be present to significantly affect the contact force distribution in the hip.84 If such an injury exists, the impacted area can be elevated and grafted as described by Mast.103 This should be considered if an impacted area of 2 cm2 exists in the weight-bearing portion of the head (see Fig. 46-6D).
a congruent and stable hip. The initial management is directed at
reducing the head to within the confines of the acetabulum in order to
minimize the ischemia of the femoral head and subsequent AVN. If
irreducible, then immediate open reduction is necessary. After the
femoral head is within the confines of the acetabulum, the hip will
fall into one of three categories: congruent reduction without
associated fracture, congruent reduction with associated fracture, or
incongruent reduction. The ultimate management will then be determined
by whether the associated fracture requires fixation, and the stability
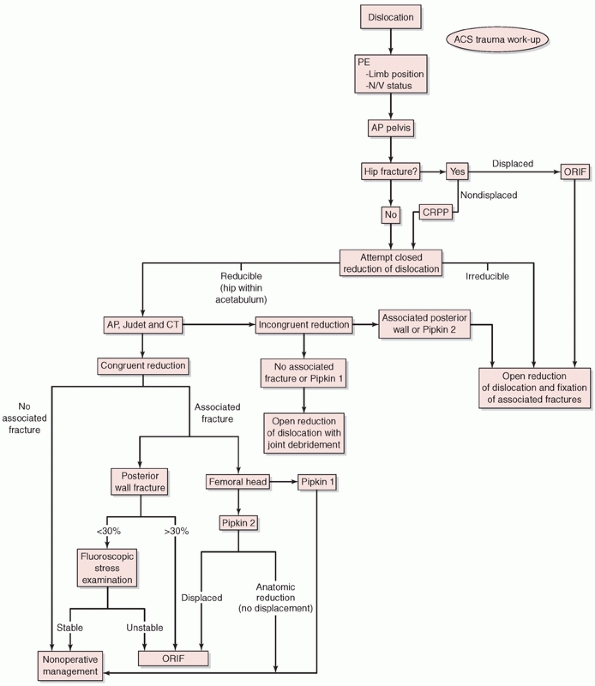
of the hip as shown in the algorithm (Fig. 46-31).
attempt at closed reduction should be performed. This is typically
performed in the operating room, but can be performed in the emergency
department if the patient is already intubated. Regardless of the
direction of the dislocation, the reduction is attempted by traction in
line with the femur and gentle rotation. An Allis1 maneuver is tried next if the dislocation is posterior, and the Walker modification of the Allis1
technique if the dislocation is anterior. If the hip is irreducible,
then immediate open reduction is necessary. The hip is approached from
the side of the dislocation, posterior for posterior dislocation via a
Kocher-Langenbeck approach, and anterior for an anterior dislocation
via a Smith-Petersen or Watson-Jones approach. If open reduction is
necessary, then joint débridement and treatment of all associated
fractures are performed simultaneously. This includes ORIF of the
acetabular wall or type II femoral head fractures and removal of joint
debris or type I femoral head fractures allowing for a congruent
reduction.
 |
|
FIGURE 46-29 AP radiograph of a patient with a Pipkin type II posterior fracture dislocation of the hip (A). After reduction of the hip, the femoral head fragment was not reduced and the hip was not reduced concentrically (B). CT scan demonstrates the femoral head fragment to be rotated 180 degrees (C). The fracture was reduced and fixed with large Herbert screws via an anterior approach (D,E).
|
 |
|
FIGURE 46-30
Example of screws used to fix an anatomically reduced femoral head fragment that may not be seated below the articular surface of the head and can cause wear of the acetabulum. (Courtesy of J. Sledge.) |
postreduction studies including AP and Judet views of the hip and a CT
with 2-mm cuts are obtained to determine the congruence of the
reduction and the postreduction position of any associated fractures.
congruent with symmetric joint space to the contralateral hip on all
plain films and the CT scan, then nonoperative management is
definitive. A short period of protected weight bearing is all that is
necessary (see Postoperative Care).
is incongruent, then the offending structure needs to be removed. The
postoperative radiographs and particularly the CT will demonstrate any
bony fragment interfering with the reduction. Careful analysis of the
CT is imperative in planning surgery to remove the fragments. During
surgery it is difficult to determine whether the joint is completely
free of fragments, so knowledge of the number, location, and size of
bony fragments makes the procedure much easier. Other than joint
débridement, no specific stabilization of the joint is necessary at
this time. However, if the labrum is avulsed from the acetabular rim,
repair via suture anchors to a freshened cancellous surface may provide
improved stability (Fig. 46-32). After the procedure, the treatment is the same as after successful closed reduction.
the hip reduction is incongruent, then an open reduction of the hip is
necessary with removal of debris as described above. The posterior wall
is fixed at the same time through the same incision. If the hip is
congruently reduced and the posterior wall is fractured, then the next
question is whether the posterior wall should be fixed. While the
techniques for fixation of posterior wall fractures is covered
elsewhere in this text, the determination of which fractures should be
fixed and which may be treated nonoperatively must be understood. This
is a controversial question and there is no definitive answer. Olson et
al.118 have demonstrated that a
posterior wall articular defect as small as 27% leads to an alteration
in the joint contact forces. Likewise, they demonstrated that the
largest change in contact forces occur with any posterior wall fracture
as compared with the intact acetabulum and that the size of the wall
fragment is less important. Although not clearly demonstrated in any
clinical series, in theory posterior wall fractures that affect the
joint mechanics and increase the contact forces in the roof may lead to
arthritis. Based on these findings and the low morbidity secondary to
advances made in acetabular fracture fixation, posterior wall fractures
that affect greater than 30% of the posterior articular surface are
generally fixed.
reported that 83% of patients with posterior wall fractures allowing
for instability of the hip went on to arthritis if treated
nonoperatively. Hips with fractures that allowed for instability that
were reduced and fixed developed arthritis at a rate similar to
dislocations without associated fractures.32,68
These hips represent the Stewart and Milford type III injury. Thus,
determination of instability in the face of posterior wall fractures
with hip dislocations is paramount. The authors believe that any
posterior wall fracture that allows for hip instability should be fixed
regardless of the size. Several authors have examined the relationship
of posterior wall fragment size and instability and made distinct
recommendations.18,77,183
In all of these studies, specific sizes of posterior wall fractures
were found to be unstable, but a large ambiguous zone is also reported.
The soft tissue injury associated with the fracture is thought to cause
this ambiguity and cannot be assessed directly by plain radiography or
CT scanning. Based on the inconsistency of these studies, the
significant ambiguity, and the importance of hip stability to long-term
outcome, the author utilizes a fluoroscopic stress examination to
determine hip stability in all posterior wall fractures that do not
require fixation on the basis of fragment size.172
This is performed with the patient under general anesthesia in the
operating room on a radiolucent table. The hip is brought through a
range of motion under fluoroscopy (Fig. 46-33).
Any change in the congruent relationship of the head to the roof is
considered instability. The hip is flexed and internally rotated and
enough pressure to rock the pelvis is applied in line with the femur in
an attempt to displace the head posteriorly. This stress test is
repeated in the AP and obturator oblique positions (see Fig. 46-25). If instability exists, then the posterior wall is reduced and fixed (Fig. 46-34).
If the hip is shown to be stable, then nonoperative management is
prescribed as in patients without associated posterior wall fractures.
reduction is assessed. If incongruent, then an open reduction is
necessary. As opposed to cases of posterior wall fracture, the open
reduction of a dislocation with femoral head fracture may be performed
anteriorly. Regardless of the size of the femoral head fracture, the
reduction is via the anterior approach.
Swiontkowski et al.168
demonstrated no increase in the rate of AVN if an anterior approach is
utilized. The authors prefer a Smith-Petersen approach to come directly
down on the hip joint. The radial portion of the capsulotomy is done on
the acetabular side to avoid damaging the cervical vessels (Fig. 46-35).
Since the femoral head fragment is located anteriorly, it is directly
visualized via this method. The ultimate treatment of the fracture is
dependent on its size. If the fragment is large and affects the
weight-bearing surface (type II), then it is reduced and fixed with
Herbert screws recessed beneath the articular surface. If the fragment
is small and caudal (type I), then excision is preferred (Fig. 46-36).
 |
|
FIGURE 46-31 Algorithm for the management of hip dislocation and femoral head fractures.
|
fracture is present, then the treatment is determined by the size and
reduction of the femoral head fracture. If the fracture fragment is
small (type I), then it may be treated nonoperatively regardless of its
position (Fig. 46-37). If the fracture affects
the weight-bearing region of the head, then an anatomic reduction is
desirable. The reduction should be assessed on plain films and on 2-mm
CT cuts. If there is a near anatomic reduction and the hip is
congruent, then close observation is possible using a CT-guided view
(see Fig. 46-28).95 If the reduction is not anatomic, then ORIF is chosen as above (see Fig. 46-29).
Finally, the addition of a posterior wall acetabular fracture makes the
management one step more complicated. If the posterior wall needs to be
fixed, then the femoral head can be fixed after surgical dislocation of
the hip from the posterior approach prior to the fixation of the
posterior wall. If the acetabular fracture is small, as is typically
seen, then fixation of the femoral head is done from anteriorly (Fig. 46-38).
 |
|
FIGURE 46-32
If open reduction of the hip is necessary, then avulsed labral tears can be repaired using suture anchors after freshening the cancellous bed (A,B). |
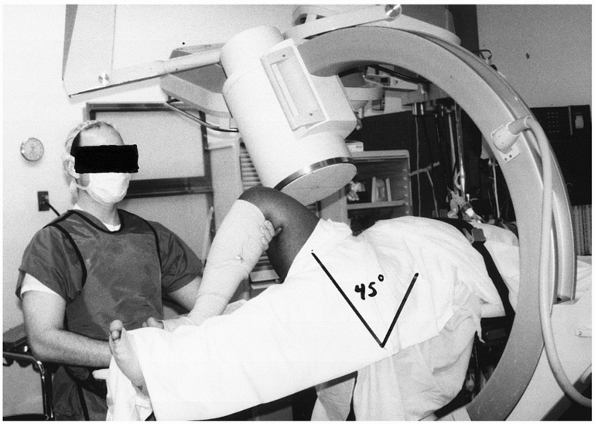 |
|
FIGURE 46-33
Method of performing fluoroscopic stress view in the operating room for a posterior wall fracture. This is the same patient as in Fig. 46-25. The photograph depicts the obturator oblique view with the image intensifier at a 45-degree angle to the body. |
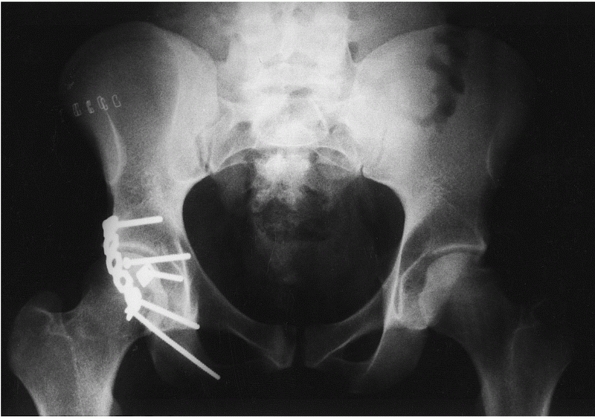 |
|
FIGURE 46-34 Postoperative radiograph of the patient in Figs. 46-25 and 46-33 after ORIF of the small posterior wall fragment that allowed for instability. The hip was stable after fixation.
|
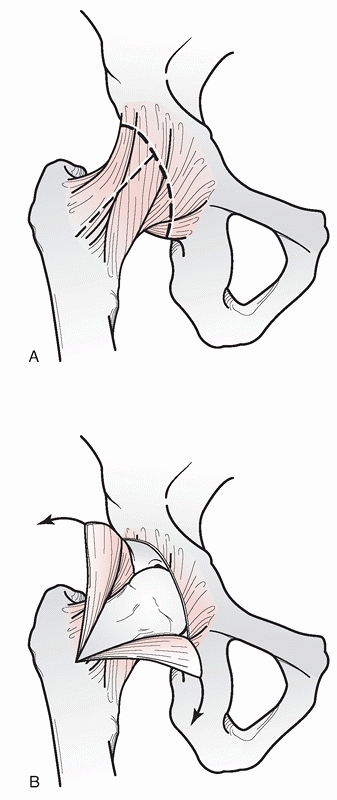 |
|
FIGURE 46-35
If an anterior approach is used for fixation of a femoral head fracture, the radial portion of the capsulotomy should be performed on the acetabular side and the vertical limb directed parallel with the femoral neck (A). This allows for the best visualization of the femoral head and spares the cervical vessels (B). |
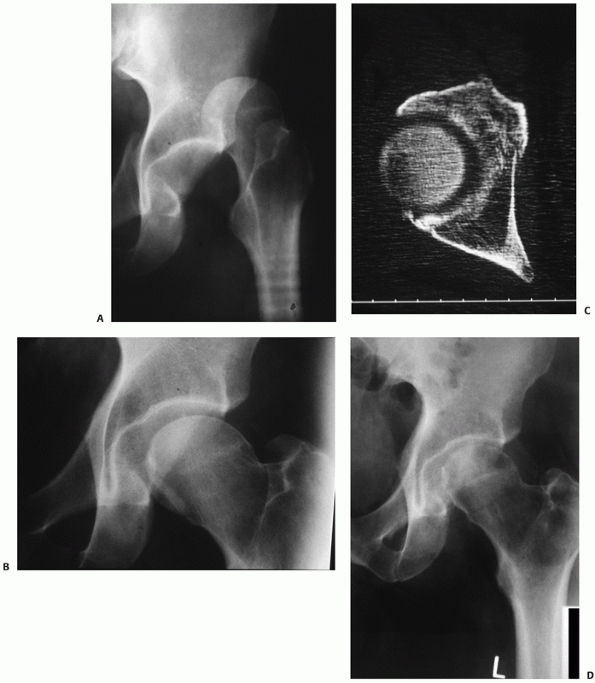 |
|
FIGURE 46-36 AP radiograph of a posterior hip dislocation with a small inferior femoral head fragment (A). Postreduction AP (B) and CT (C)
demonstrate that the joint is incongruently reduced and the joint space is widened due to the impingement of the Pipkin type I fracture. The fragment was excised and the joint débrided. The patient has an excellent result at 4 years (D). |
The primary question is whether weight bearing should be delayed. It
has been postulated that early weight bearing may cause greater
collapse in cases of hip dislocation complicated by AVN.165 This has not been demonstrated in a prospective fashion,
but has some merit on historical grounds.11 Several authors have examined the use of MRI to detect changes within the femoral head after dislocation.32,89
Although changes within the femoral head have been demonstrated, the
long-term outcome of patients with these changes has not been
determined. These studies indicate that MRI may have future use in
predicting which patients may develop AVN and therefore help to
determine whether early weight bearing is a risk for degree of
collapse. However, at this point, there is no consistent way to predict
eventual AVN. Since the rate of AVN is highest in hips reduced after 6
hours, it may be reasonable to delay full weight bearing in these cases
for 8 to 12 weeks. In the absence of fracture fixation, patients
requiring open reduction may be treated with the same protocol as after
successful closed reduction.
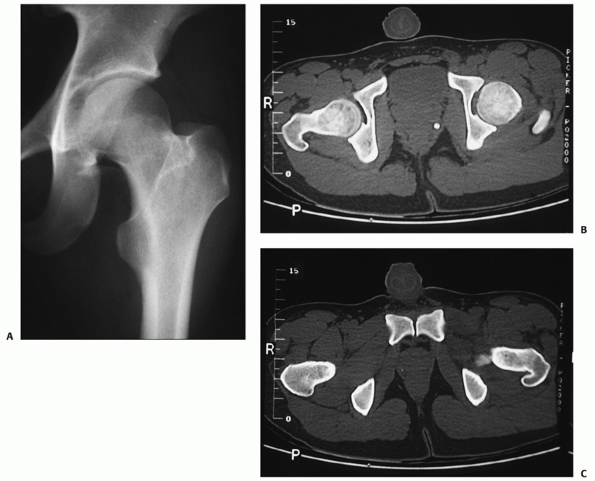 |
|
FIGURE 46-37
AP radiograph of a 24-year-old man after closed reduction of a posterior hip dislocation with associated inferior femoral head fracture (Pipkin type I). The femoral head fracture is displaced, but is not impinging on the reduction of the hip, which is concentric (A). The CT scan confirms that the reduction of the hip is concentric (B) and shows the femoral head fragment to be located inferiorly (C). The fragment was left in place and the patient was treated nonoperatively. |
hours, the standard postreduction regimen includes a brief period of
rest for several days to 2 weeks followed by mobilization. Continuous
passive motion is desirable to avoid the intra-articular adhesions and
arthritis that come from long immobilization.175
Extremes of motion are avoided for 6 to 8 weeks to allow for capsular
healing. Likewise, early mobilization of patients is best for their
overall condition. Patients should be out of bed to a chair within a
few days and up on crutches or a walker within 1 week. Typically, the
affected side is allowed toe touch weight bearing to provide the least
stress to the hip joint by resting the leg on the ground during
ambulation. As patients’ strength returns and they are able to better
control the limb, weight bearing is increasingly permitted. Most
patients can achieve full weight bearing by 6 weeks.
strengthening the hip musculature. In particular, therapy should
concentrate on the abductor muscles to diminish the patient’s need for
ambulatory assistive devices. After muscle strength is restored,
proprioceptive training and coordination exercises will help the
patient regain maximal function.
fractures fixed is determined by the associated injury. In the case of
posterior wall acetabular fractures or femoral head fractures, active
hip motion may be deferred for approximately 6 weeks. Passive motion is
encouraged via a continuous passive motion machine. Toe touch
ambulation begins immediately and continues for 10 to 12 weeks. Therapy
to strengthen the hip musculature is instituted when full weight
bearing begins.
are treated based on the type of fixation and the type of fracture
without regard for the dislocation (see Chapter 47).
 |
|
FIGURE 46-38
The trauma AP pelvis of a 37-year-old man demonstrates a posterior hip dislocation with femoral head fracture and small posterior wall fracture (A). The femoral head fragment remained displaced on the postreduction films (B,C). The obturator oblique view nicely profiles the significant displacement of the femoral head fracture and the narrow posterior wall fracture (C). The CT clarifies the plane of the femoral head fracture in the typical direction (D). Intraoperative obturator oblique demonstrates a congruent head to roof relationship (E), but on flexion and internal rotation, the head subluxates (F). Repeat stress examination after femoral head fixation from an anterior approach reveals a stable joint, and the posterior wall was treated nonoperatively (G). |
initial assessment is avoiding complications. The most dangerous of
these is a missed associated injury. Specifically, nondisplaced hip
fractures that may be displaced with attempts at closed reduction must
be identified. Likewise, significant knee ligament injuries may occur,
necessitating vascular assessment of the leg. Complete neurologic and
vascular assessment will provide a necessary baseline for the
postreduction examination. Sciatic nerve dysfunction at the time of
presentation is reported in up to 19% of patients and is more common in
fracture dislocations than pure dislocations.42,64,72,123,161,162,170 The peroneal division is most often affected, so peroneal strength must be tested.161
If the sciatic nerve is injured at the time of the dislocation, then
reduction of the head is more imperative, as this may take pressure off
the nerve. Functional recovery occurs in approximately 70% of cases and
is related to the degree of initial injury, with complete palsies
having a worse prognosis than partial palsies.40,41,62,72,125,140,144,153,162,176
If recovery does not occur, patients may be offered tendon transfer at
the ankle if they do not wish to use a walking ankle-foot orthosis.
Exploration of the nerve is generally not recommended.
function of the limb should be reassessed. Specifically, the sciatic
nerve function needs to be documented. If nerve function was normal
before the reduction and significantly impaired after the reduction,
then surgical exploration of the nerve is recommended to ensure it is
not trapped within the joint.58
must be clearly documented with the use of plain films and CT.
Likewise, small fragments interposed within the articular surface must
not be missed as third-body wear will occur quickly. For this reason,
if the head is generally reduced within the acetabulum but is
incongruous, a femoral traction pin should be placed and the hip
distracted using skeletal traction to avoid articular damage until the
offending structures can be removed.
there is an associated fracture. If a large posterior wall fracture
exists that may engender instability, then the hip should be placed in
skeletal traction with the hip minimally flexed to maintain reduction
until stability testing can be performed.
It is reported in 1.7% to 40% of various series. If the hip is reduced
to within the confines of the acetabulum within 6 hours of the
dislocation, then AVN rates are 0% to 10%.
multifactorial. In part, the cervical vessels to the head and the
contributions from the ligamentum teres are damaged at the time of
injury. Secondarily, an ischemic insult to the femoral head while it is
dislocated affects outcome. The mechanism of AVN has been studied in
rabbits. Shim147 and Duncan and Shim33
have demonstrated femoral head ischemia in adult rabbits caused by
dislocation. Contrary to previous beliefs, they found that the cervical
vessels to the head are not normally disrupted by the dislocation, but
do not provide adequate circulation due to spasm of the larger vessels
or of the cervical vessels themselves. Early reduction restored the
vascular supply to the head better than late reduction, in some cases
almost to the level of the contralateral hip based on angiographic
studies. Yue et al.196 found a
similar kinking effect in human cadavers. Extrapolated to the clinical
situation, this work indicates that the majority of AVN is secondary to
the initial ischemia of the femoral head, not to torn vessels, and that
emergent reduction may reduce the incidence of AVN. This parallels the
clinical findings of many authors who report much lower rates of AVN if
the hip is reduced within 6 hours (Table 46-9).11,133,162
usually present within 2 years, but have been seen to occur as late as
5 years postinjury.173 The diagnosis
may be difficult until collapse is present, particularly if the patient
develops heterotopic ossification, as this may obscure the radiographic
findings. Fortunately, as opposed to AVN secondary to systemic illness
or medications or idiopathic AVN, posttraumatic AVN may be highly
localized. It is therefore more amenable to treatment by osteotomy than
global AVN. The treatment begins with a period of motion and non-weight
bearing to diminish the amount of collapse once the diagnosis is made.
|
TABLE 46-9 Results, Avascular Necrosis, and Arthritis
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
New evidence from the lab suggests that a prolonged dislocation time
will increase in chondrocyte apoptosis with increasing time to
reduction in a rat model for hip dislocation.37 Fracture dislocations are also more likely to develop arthritis.40,43,113
Dislocations with associated femoral head fractures may develop
arthritis in 50% of patients. The higher rates of arthritis in fracture
dislocations may be in part from chondrocyte damage, as marginal
cartilage injury is common in cases of fracture dislocation.13,95 Repo and Finely134 were able to induce chondrocyte death by applying a 20% to 30% strain. Similarly, Borelli et al.175 demonstrated subchondral fractures and decreased metabolic activity in cartilage exposed to a compression injury.
who reported on 50 patients after dislocation without associated
fracture: 38 were posterior and 12 anterior. Despite all but one of the
hips being reduced within 6 hours (mean 70 minutes), they reported a
26% incidence of arthritis at an average of 8 years postdislocation.
Six of the seven patients without associated severe injury had a good
or excellent result as compared with only three of eight who had a
severe associated injury. In contradistinction to other reports, they
found no increase in the incidence of arthritis with length of
follow-up. They also reported that the majority of patients with
radiographic signs of AVN did not manifest radiographic signs of
arthritis.
This complication is also commonly reported after posterior wall
fractures. It is likely due to posterior muscle injury from the
dislocation in combination with surgical trauma. In cases of femoral
head fracture, Swiontkowski et al.168
demonstrated a higher incidence of HO after ORIF via an anterior
approach than a posterior approach. In cases of posterior dislocation,
the use of indomethacin may diminish the rate of clinically significant
HO. The other choice is to use radiation therapy, usually 700 Gy in one
dose. This method is very effective in decreasing the rate of HO, but
is not favored in young patients.10,110 HO seems to be related to significant trauma in addition to a dislocation with Pape et al.121 reporting a rate of 60% that was not related to a surgical procedure having been performed. Similarly, Nork et al.131 reported a 58% rate of HO in patients treated for femoral head fractures via an anterior approach.
recently reported on three patients who required late excision of an
inferior femoral head fracture due to pain and limitation of motion.
These patients were initially treated with non-weight bearing and then
gradual ambulation. In each case, the inferior fragment was excised
restoring motion.
It is usually from HO either compressing the nerve or causing it to be
stretched. It is important to continue to examine the nerve function at
each postinjury visit, as early decompression may favor neurologic
return.
been reported. Good to excellent results have been demonstrated in 48%
to 95% of patients (see Table 46-9).32,72
At least part of this variation is due to the types of dislocation
reported, the length of follow-up in the various studies, and the
criteria used for assessing them. Upadhyay et al.180 and Hougaard and Thomsen68
found increasing rates of arthritis with longer follow-up. In most
series, a good result indicated no limp or limp only after a long
workday, no more than 25% restriction of motion, no interference with
activities of daily living, and no radiographic evidence of arthritis
or AVN. Although only small numbers of patients have been studied, it
appears that anterior dislocations without femoral head injury fare
better than posterior dislocations.2,28,32 Dreinhofer et al.32 reported 75% acceptable results after anterior dislocation and only 48% after posterior dislocation. Vecsei et al.184
reported 87 dislocations in 82 patients. Of 43 patients followed for
between 6 months and 19 years, 17 (40%) developed arthritis, but only
one had AVN. All dislocations were reduced within 6 hours. Of the 29
otherwise healthy patients, 8 had occasional pain and another 6 had
limited motion and pain.
found high rates of complications in patients with an injury severity
score of greater than 18, including 5/17 with early arthritis and 7/17
with AVN.121 Additionally, 64%
developed HO, which did not appear to correlate with open procedures.
Patients who performed heavy labor may also be at increased risk of
poor outcome.180 Likewise,
associated fractures may adversely affect outcome.
Fracture-dislocations have a poorer prognosis than pure hip dislocation.168
found no cases of arthritis or AVN in simple dislocations reduced
within 6 hours. Additionally, there may be an association of sciatic
nerve injury with delays in reduction of the hip in patients
transferred to a major center after dislocation.63
poor results reported. The type of femoral head fracture and their
management does correlate with outcome. Matejka et al.105
followed 51 patients with femoral head fractures for a minimum of 24
months. Thirty of the 38 with complete follow-up had been treated with
fixation or excision of the fragment. Eleven developed AVN and 16
arthritis, with 11/30 going on to total hip arthoplasty. Yoon et al.195
followed 30 patients for 3-10 years after injury. Smaller fragments
were excised (n = 14) and larger ones fixed (n = 16). Overall, good or
excellent results were found in 21 clinically and radiographically.
Marchetti et al.101 reported no
excellent, 67% good, 18% fair, and 15% poor results in 33 patients at
an average of 49 months. Results for Pipkin type I and II fractures
were better than type III and IV fractures (p <0.02). Finally, Dreinhofer et al.31
reported similar results to those they found in pure hip dislocations.
Twenty-six patients followed for an average of 5 years (2-11) resulted
in 6 with arthritis, 5 with AVN, and 8 with HO. By the Thompson and
Epstien170 criteria, 15/26 had fair or poor results.
evaluated the clinical and radiographic outcome of 22 patients at an
average of 24 months after injury using the SF12 outcome scale.
Radiographic findings correlated well with SF12 scores, with poor
results having an average physical score of 29 as compared with over 42
for all other groups. Outcome was not different, with only small
groups, for patients managed with ORIF of the head (typically larger
more proximal fractures) versus excision (smaller inferior fragments),
or an anterior versus posterior approach. AVN had a substantial
negative effect on outcome with an average physical score of 27 for the
5 patients who developed it as compared with 44 for those that did not.
Nork and colleagues131 evaluated 37
patients treated with ORIF (21) or excision (13) via an anterior
approach at a minimum of 40 months using the musculoskeletal functional
assessment (MFA). Half of the patients had small posterior wall
fractures of less than 10%, which did not affect the stability of the
joint. Fifty-eight percent developed HO, and 6% developed AVN. Nineteen
patients who were evaluated using the MFA had results similar to other
isolated lower extremity injuries (average 22.7). Their results were
lower than population based norms in 8/10 subcategories. With a small
number of patients in each group, no associations could be made related
to management or injury type.
femoral head fractures with combined acetabular fractures. In two
separate studies, Solberg154 and Zlowodzki197
both reported excellent and good outcomes in Pipkin IV injuries when
using the surgical dislocation approach with a trochanteric osteotomy.
Each study only evaluated 12 patients, but 21 of the 24 patients were
reported to have an excellent or good outcome after 2 years. These two
small reports suggest functional improvements may be seen with this
approach but further evaluation of the long-term outcomes is necessary.
reduction of the hip in a paralyzed patient and ideally is performed in
the operating room and within 6 hours of injury. Understanding the
factors that affect outcomes is still a work in progress. The cartilage
damage at the time of injury has been demonstrated to be an important
predictor of arthritis and a predictor of total hip replacement.28
The use of MRI has been shown to help recognize soft tissue injuries
and insufficiency fractures of the femoral head but its role in the
evaluation of acute hip dislocations and recognizing these cartilage
lesions remains unclear. In the future, as improvements are made in
detecting cartilage damage and early arthritis, MRI may be a useful
tool for following these patients after dislocation and recognizing
early arthritic changes.
In this study, 39 hips underwent arthroscopy for the débridement of
loose bodies. In 14 hips, there was no radiographic evidence of loose
bodies.114 Although hip arthroscopy
is not indicated for every hip dislocation, it may provide a role in
the treatment of these injuries in the future, particularly in the
débridement of loose bodies in the face of the stable, concentric hip.
the femoral head or the acetabulum significantly change the treatment
and outcome of a hip dislocation. The use of the transtrochanteric or
surgical dislocation approach has shown some promise in improving the
outcome of these injuries. The increased use of the surgical
dislocation approach for femoral head fractures with or without an
associated acetabular fracture has demonstrated some improved outcomes
compared to the more traditional anterior and posterior approaches.51,62,85,154
The improvements in clinical outcomes seen with this approach are
encouraging, but more follow-up and comparison studies are needed.
Additionally, the use of bioresorbable pins has been reported to be
useful in the treatment of nine femoral head fractures.130 In this study, they used biodegradable poly-L/DL lactide pins for fixation.130
The use of biodegradable pins for femoral head fractures has some
advantages, particularly allowing for better imaging of the hip, but
much more work has to be done to provide enough evidence that these are
safe and dependable devices.
RA, Schobert WE, Pais MJ, et al. Radiographic identification of loose
bodies in the traumatized hip joint. Radiology 1982;145(3):661-665.
JD, Wolf AT, Wyss TF, et al. Stepped osteotomy of the trochanter for
stable, anatomic refixation. Clin Orthop Relat Res 2009;467(3):732-738.
MJ, Poka A, Reinert CM, et al. Heterotopic ossification as a
complication of acetabular fracture. Prophylaxis with low-dose
irradiation. J Bone Joint Surg Am 1988; 70(8):1231-1237.
EA. Traumatic dislocation of the hip: Army Experience and results over
twelve year period. J Bone Joint Surg Am 1962;44:1115-1134.
RW, Wheeless G. Irreducible posterior fracture—dislocations of the hip.
The role of the iliofemoral ligament and the rectus femoris muscle.
Clin Orthop Relat Res 1982;167:118-122.
M, Della Valle AG, Morandi A, et al. Insufficiency subchondral fracture
of the femoral head: report of 4 cases and review of the literature. J
Arthroplasty 2003;18(3): 377-382.
MC, Ambekar A, Lu Y, et al. MRI and CT of insufficiency fractures of
the pelvis and the proximal femur. AJR Am J Roentgenol
2008;191(4):995-1001.
MS, Zych G, Latta L, et al. Computed tomography evaluation of stability
in posterior fracture dislocation of the hip. Clin Orthop Relat Res
1988;227:152-163.
JF. Acetabular labrum entrapment associated with a femoral-head
fracture-dislocation. A case report. J Bone Joint Surg Am
1974;56(8):1735-1737.
LE, Hundley JD. Reduction of posterior hip dislocations in the lateral
position using traction-countertraction: safer for the surgeon? J
Orthop Trauma 1999;13(5): 373-374.
TB Jr. Bucket-handle tear of acetabular labrum accompanying posterior
dislocation of the hip. J Bone Joint Surg Am 1959;41A(1):131-134.
JC. Fractures and dislocations of the hip. In: Rockwood Jr CA, Green
DP, Bucholz RW, eds. Fractures in Adults. Philadelphia:
Lippincott-Raven, 1996:1756-1803.
JC, Evans JA, Thomas J. Anterior dislocation of the hip and associated
femoral-head fractures. J Bone Joint Surg Am 1980;62(6):960-964.
PS, Bibighaus AJ. Sciatic nerve entrapment by ectopic bone after
posterior fracture-dislocation of the hip. South Med J
1974;67(2):209-210.
KE, Schwarzkopf SR, Haas NP, et al. [Femur head dislocation fractures.
Long-term outcome of conservative and surgical therapy]. Unfallchirurg
1996;99(6): 400-409.
KE, Schwarzkopf SR, Haas NP, et al. Isolated traumatic dislocation of
the hip. Long-term results in 50 patients. J Bone Joint Surg Br
1994;76(1):6-12.
RG, Beauregard G, Fauteaux P, et al. Femoral head defect following
anterior hip dislocation. Radiology 1980;135(3):627-629.
NA, Savolaine ER, Skie MC, et al. Soft-tissue window to enhance
visualization of entrapped osteocartilaginous fragments in the hip
joint. Orthop Rev 1993;22(9): 1017-1021.
J, Ng de J, Tham SK. Chondrocyte apoptosis in response to dislocation
of the hip in the rat model. ANZ J Surg 2006;76(5):398-402.
HC. Traumatic anterior and simple posterior dislocations of the hip in
adults and children. Instr Course Lect 1973;22:115-145.
HC, Harvey JP. Traumatic anterior dislocations of the hip: management
and results, an analysis of fifty-five cases. J Bone Joint Surg Am
1972;54:1561-1562.
HC, Wiss DA, Cozen L. Posterior fracture dislocation of the hip with
fractures of the femoral head. Clin Orthop Relat Res 1985;201:9-17.
N, Rothenfluh DA, Beck M, et al. Treatment of femoro-acetabular
impingement: preliminary results of labral refixation. J Bone Joint
Surg Am 2006;88(5): 925-935.
KJ, Mulligan ME, Murphey MD, et al. Gas bubbles in the hip joint on CT:
an indication of recent dislocation. AJR Am J Roentgenol
1995;164(4):931-934.
VH, Pugh JW. Biomechanics of the hip. In: Tronzo RG, ed. Surgery of the
Hip Joint. Philadelphia: Lea & Febiger, 1973:115-131.
R, Gill TJ, Gautier E, et al. Surgical dislocation of the adult hip a
technique with full access to the femoral head and acetabulum without
the risk of avascular necrosis. J Bone Joint Surg Br
2001;83(8):1119-1124.
MJ, Suk M, Pearle A, et al. Surgical dislocation of the hip for
fractures of the femoral head. J Orthop Trauma 2005;19(5):334-342.
E, Ganz K, Krugel N, et al. Anatomy of the medial femoral circumflex
artery and its surgical implications. J Bone Joint Surg Br
2000;82(5):679-683.
AW, Gardner MJ, Sussmann PS, et al. The surgical anatomy of the blood
supply to the femoral head: description of the anastomosis between the
medial femoral circumflex and inferior gluteal arteries at the hip. J
Bone Joint Surg Br 2008;90(10): 1298-1303.
GS, Mears DC, Tauxe WN. Distinguishing avascular necrosis from
segmental impaction of the femoral head following an acetabular
fracture: preliminary report. J Orthop Trauma 1988;2(1):5-9.
JD, Mack LA, Winquist RA. CT of acetabular fractures: comparison with
conventional radiography. AJR Am J Roentgenol 1982;138(3):413-417.
RF, Fox J. Sciatic nerve injuries associated with traumatic posterior
hip dislocations. Am J Emerg Med 2003;21(7):545-548.
Y, Oda R, Nakatani K. Sciatic nerve paralysis in posterior dislocation
of the hip. A case report. Clin Orthop Relat Res 1977;126:172-175.
K, Lindequist S, Nielsen LB. Computerised tomography after posterior
dislocation of the hip. J Bone Joint Surg Br 1987;69(4):556-557.
K, Thomsen PB. Coxarthrosis following traumatic posterior dislocation
of the hip. J Bone Joint Surg Am 1987;69(5):679-683.
K, Thomsen PB. Traumatic posterior dislocation of the hip—prognostic
factors influencing the incidence of avascular necrosis of the femoral
head. Arch Orthop Trauma Surg 1986;106(1):32-35.
K, Thomsen PB. Traumatic posterior fracture-dislocation of the hip with
fracture of the femoral head or neck, or both. J Bone Joint Surg Am
1988;70(2): 233-239.
WW Jr, Lacey T, Schwartz RP. A study of the gross anatomy of the
arteries supplying the proximal portion of the femur and the
acetabulum. J Bone Joint Surg Am 1950;32A(4):856-866.
GA. Posterior dislocation and fracture-dislocation of the hip. A review
of fifty-seven patients. J Bone Joint Surg Br 1969;51(1):38-44.
JR, Rao JP, Ciccarelli C. Traumatic dislocation and fracture
dislocation of the hip. A long-term follow-up study. Clin Orthop Relat
Res 1987;214:249-263.
CC. Fracture dislocation of the hip with displacement of bone fragment
into acetabulum during closed reduction. J Bone Joint Surg Br
1957;39:310-312.
M, Beck M, Huff TW, et al. Capsular and pericapsular contributions to
acetabular and femoral head perfusion. J Bone Joint Surg Am
2009;91(2):409-418.
JE Jr, Brashear HR Jr, Guilford WB. Stability of posterior
fracture-dislocations of the hip. Quantitative assessment using
computed tomography. J Bone Joint Surg Am 1988;70(5):711-714.
RP, Yarbrough SH 3rd. Posterior fracture-dislocation of the femoral
head with retained medial head fragment. J Trauma 1971;11(2):97-108.
GE, Spivey CJ, Swanson SA, et al. Patterns of cartilage stiffness on
normal and degenerate human femoral heads. J Biomech 1971;4(6):597-609.
KI, Koo KH, Sharma R, et al. Concomitant fractures of the femoral head
and neck without hip dislocation. Clin Orthop Relat Res
2001;391:247-250.
YT, Ninomiya S, Tachibana Y, et al. Acetabular labrum entrapment
following traumatic posterior dislocation of the hip. J Orthop Sci
2003;8(2):232-235.
SG, Stevens J, Kolb L, et al. Late sciatic-nerve palsy following
posterior fracture-dislocation of the hip. A case report. J Bone Joint
Surg Am 1971;53(4):781-782.
GA, Hamel AJ, Guerin J, et al. The biomechanical consequences of
impaction injuries to the femoral head. Paper presented at: 14th Annual
Meeting of the Orthopaedic Trauma Association; October 8-11, 1998;
Vancouver, BC, Canada.
PJ, Vap AR, Zlowodzki M, et al. Acetabular fractures associated with
femoral head fractures (pipkin IV): treatment utilizing ganz
trochanteric flip osteotomy. Presented at: 22nd Annual Meeting of the
Orthopaedic Traumatology Association; 2006; Phoenix, Arizona.
O, Stougaard J. Traumatic dislocation of the hip. Results of
conservative treatment. Acta Orthop Scand 1974;45(2):206-212.
NA, Levinsohn EM, Yuan HA, et al. Computerized tomography in disorders
of the hip. J Bone Joint Surg Am 1978;60(8):1099-1102.
Gerot I, Demondion X, Louville AB, et al. Subchondral fractures of the
femoral head: a review of seven cases. Joint Bone Spine
2004;71(2):131-135.
PE. Hip dislocations. In: Browner BD, Jupiter JB, Levine AM, eds.
Skeletal Trauma. Philadelphia: WB Saunders, 1998:1329-1369.
DW Jr, Hartman JT. Traumatic dislocation of the hip with ipsilateral
femoral fractures. A case report. J Bone Joint Surg Am
1971;53(5):1012-1016.
LA, Harley JD, Winquist RA. CT of acetabular fractures: analysis of
fracture patterns. AJR Am J Roentgenol 1982;138(3):407-412.
ME, Steinberg GG, Coumas JM. Intermediate-term experience of Pipkin
fracture-dislocations of the hip. J Orthop Trauma 1996;10(7):455-461.
JV, Cotler HB, Harris JH Jr, et al. Posterior hip dislocation
associated with acute traumatic injury of the thoracic aorta: a
previously unrecognized injury complex. J Orthop Trauma
1990;4(4):383-387.
J, Koudela K. [Bilateral fractures of the femoral head (Pipkin I and
Pipkin II)]. Acta Chir Orthop Traumatol Cech 2002;69(6):369-371.
K, Sumi H, Sumi Y, et al. An analysis of hip dislocations among
snowboarders and skiers: a 10-year prospective study from 1992 to 2002.
J Trauma 2003;55(5): 946-948.
S, Routt ML Jr. Irreducible fracture-dislocations of the femoral head
without posterior wall acetabular fractures. J Orthop Trauma
2008;22(10):686-692.
BS, Wainwright AM. Fracture of the femoral head without associated hip
dislocation following low-energy trauma. A report of two cases. Arch
Orthop Trauma Surg 1996;115(5):300-302.
BR, Letournel E. Low-dose irradiation and indomethacin prevent
heterotopic ossification after acetabular fracture surgery. J Bone
Joint Surg Br 1994;76(6):895-900.
BR, Maxey JW. Evaluation of fractures of the femoral head using the
CT-directed pelvic oblique radiograph. Clin Orthop Relat Res
1993;296:161-167.
CT 3rd, Warren RF, Hershman EB, et al. Traumatic posterior hip
subluxation in American football. J Bone Joint Surg Am
2003;85A(7):1190-1196.
SA, Bay BK, Hamel A. Biomechanics of the hip joint and the effects of
fracture of the acetabulum. Clin Orthop Relat Res 1997;339:92-104.
SA, Bay BK, Pollak AN, et al. The effect of variable size posterior
wall acetabular fractures on contact characteristics of the hip joint.
J Orthop Trauma 1996;10(6): 395-402.
CB, Xeller CF. Transverse computerized axial tomography of patients
with posterior dislocation of the hip. J Trauma 1984;24(1):76-79.
HC, Rice J, Wolfram K, et al. Hip dislocation in patients with multiple
injuries. A followup investigation. Clin Orthop Relat Res
2000;377:99-105.
JJ, Callaghan JJ, Spritzer CE, et al. Changes on magnetic resonance
images after traumatic hip dislocation. Clin Orthop Relat Res
1995;319:249-259.
RE, Polesky FA. Intrapelvic dislocation of the femoral head following
anterior dislocation of the hip. A case report. J Bone Joint Surg Am
1972;54(5):1097-1098.
HG, Montgomery KD, Padgett DE, et al. Magnetic resonance imaging of the
pelvis. New orthopaedic applications. Clin Orthop Relat Res
1995;319:223-231.
JH, Edwards AH. Traumatic dislocation of the hip joint. An experimental
study on the cadaver. Glasgow Med J 1943;21:25-40.
TB, Nork SE, Routt ML. Surgical treatment of femoral head fractures.
Paper presented at: 17th Annual Meeting of the Orthopaedic Trauma
Association; San Diego, CA: October 18-20, 2001.
EM, Russell GV Jr, Washington WJ, et al. Gluteus minimus necrotic
muscle debridement diminishes heterotopic ossification after acetabular
fracture fixation. Injury 2002;33(9):751-756.
PD, Mann RW, Harris WH. Influence of cartilage geometry on the pressure
distribution in the human hip joint. Science 1979;204(4391):413-415.
O, Ozturk C, Dereboy F, et al. Asymmetrical bilateral traumatic hip
dislocation in an adult with bilateral acetabular fracture. Arch Orthop
Trauma Surg 2007;127(8): 643-646.
V, Karakas ES, Aksu S, et al. Traumatic dislocation and
fracture-dislocation of the hip: a long-term follow-up study. J Trauma
2003;54(3):520-529.
SJ, Anglen JO. The East Baltimore Lift: a simple and effective method
for reduction of posterior hip dislocations. J Orthop Trauma
1999;13(1):56-57.
W, Elsasser B, Mullaji AB, et al. Hip dislocation without fracture:
traction or mobilization after reduction? Injury 1993;24(1):27-31.
R, LaFrance AE, Oxland TR, et al. Does trochanteric step osteotomy
provide greater stability than classic slide osteotomy? A preliminary
study. Clin Orthop Relat Res 2009;467(3):775-782.
M, Sener U, Yildiz M, et al. Bilateral traumatic hip dislocation with
bilateral sciatic nerve injury. Arch Orthop Trauma Surg
1997;116(4):225-226.
SS. Circulatory and vascular changes in the hip following traumatic hip
dislocation. Clin Orthop Relat Res 1979;140:255-261.
KA, Gautier E, Woo AK, et al. Surgical dislocation of the femoral head
for joint debridement and accurate reduction of fractures of the
acetabulum. J Orthop Trauma 2002;16(8):543-552.
KA, Gautier E, Ziran BH, et al. Trochanteric flip osteotomy for cranial
extension and muscle protection in acetabular fracture fixation using a
Kocher-Langenbeck approach. J Orthop Trauma. 1998;12(6):387-391.
GR, Loop JW. Radiologic classification of posterior dislocations of the
hip: refinements and pitfalls. Radiology 1976;119(3):569-574.
BD, Moon CN, Franco DP. Use of a trochanteric flip osteotomy improves
outcomes in Pipkin IV fractures. Clin Orthop Relat Res
2009;467(4):929-933.
WS, Yoo JJ, Koo KH, et al. Subchondral fatigue fracture of the femoral
head in military recruits. J Bone Joint Surg Am 2004;86A(9):1917-1924.
J. Fracture-dislocation of the hip with entrapment of the femoral head
by impaction against the acetabular rim. Injury 1976;8(2):127-128.
JP, Harris HW, Volgas DA, et al. Functional outcome of patients with
femoral head fractures associated with hip dislocations. Clin Orthop
Relat Res 2000;377:44-56.
H. Computerized tomography for ascertaining osteocartilaginous
intraarticular (slice) fractures of the femoral head. Isr J Med Sci
1983;19(2):180-184.
CR. Recent traumatic dislocations of the hip: with a report of ten
cases and their end results. Ann Surg 1914;60(5):617-621.
MJ. Management of fractures of the head of the femur complicated by
dislocation of the hip. Orthop Clin North Am 1974;5(4):793-798.
WJ. Aseptic necrosis of the head of the femur following traumatic
dislocation of the hip joint. Case report and experimental studies. J
Bone Joint Surg Am 1933;15: 413-438.
AJ. Distribution and severity of injuries associated with hip
dislocations secondary to motor vehicle accidents. J Trauma
1986;26(5):458-460.
MF, Thorpe M, Seiler JG, et al. Operative management of displaced
femoral head fractures: case-matched comparison of anterior versus
posterior approaches for Pipkin I and Pipkin II fractures. J Orthop
Trauma 1992;6(4):437-442.
VP, Epstein HC. Traumatic dislocation of the hip; a survey of two
hundred and four cases covering a period of twenty-one years. J Bone
Joint Surg Am 1951; 33A(3):746-778; passim.
A, Gulino G, Baldini N, et al. Clinical and radiographic long term
results of acetabular fractures associated with dislocations of the
hip. Ital J Orthop Traumatol 1985;11(4):443-454.
P 3rd. Non-operative management of acetabular fractures. The use of
dynamic stress views. J Bone Joint Surg Br 1999;81(1):67-70.
PA, Grigiene R, Borrelli J Jr, et al. Effect of impact load on
articular cartilage: cell metabolism and viability, and matrix water
content. J Biomech Eng 1999;121(5): 433-441.
RG, Edwards GE, Bazant FJ. Post-traumatic recurrent dislocation of the
hip without fracture. J Bone Joint Surg Br 1969;51:194.
M, Hashmi R, Ito M, et al. Subchondral insufficiency fracture of the
femoral head: magnetic resonance imaging findings correlated with
micro-computed tomography and histopathology. J Comput Assist Tomogr
2003;27(2):189-193.
SS, Moulton A. The long-term results of traumatic posterior dislocation
of the hip. J Bone Joint Surg Br 1981;63B(4):548-551.
SS, Moulton A, Burwell RG. Biological factors predisposing to traumatic
posterior dislocation of the hip. A selection process in the mechanism
of injury. J Bone Joint Surg Br 1985;67(2):232-236.
SS, Moulton A, Srikrishnamurthy K. An analysis of the late effects of
traumatic posterior dislocation of the hip without fractures. J Bone
Joint Surg Br 1983; 65(2):150-152.
MR. Fracture-dislocation of the hip joint; the nature of the traumatic
lesion, treatment, late complications and end results. J Bone Joint
Surg Am 1948;30A(3): 699-727.
MR. Injuries to the hip joint: traumatic dislocations incurred chiefly
in jeep injuries in World War II. Am J Surg 1947;74:586-597.
JC, Hurwitz S, Wiesel SW. Posterior acetabular fracture-dislocations:
fragment size, joint capsule, and stability. J Trauma
1989;29(11):1494-1496.
T. Stress osteopathy of the femoral head. 10 military recruits followed
for 5-11 years. Acta Orthop Scand 1997;68(2):138-141.
PE. Dislocations. In: Edmonson AS, Crenshaw AH, eds. Campbell’s
Operative Orthopaedics. 6th ed. St. Louis: CV Mosby, 1980.
TR, Chung JY, Jung ST, et al. Malunion of femoral head fractures
treated by partial ostectomy: three case reports. J Orthop Trauma
2003;17(6):447-450.
JJ, Sontich JK, Miron SD, et al. Blood flow changes to the femoral head
after acetabular fracture or dislocation in the acute injury and
perioperative periods. J Orthop Trauma 2001;15(3):170-176.
JJ, Wilber JH, Lipuma JP, et al. Posterior hip dislocations: a
cadaveric angiographic study. J Orthop Trauma 1996;10(7):447-454.
M, Thomson A, Russell GV Jr, et al. Acetabular fractures associated
with femoral head fractures (pipkin IV injuries): long-term follow-up
of open reduction and internal fixation. Presented at: 19th Annual
Meeting of the Orthopaedic Traumatology Association. Salt Lake City,
Utah; 2003.
