Trauma about the Pelvis/Hip/Femur
|
|
usually result from significant trauma. Although low-energy hip and
femur fractures are seen, as the treating surgeon you are usually
assuming care of a child whose body has been subjected to significant
force. Perhaps the most important guideline for staying out of trouble
with these fractures is to look for injuries to other organ systems. In
many cases, help from a traumatologist will best serve you and the
child. Although we have grouped pelvis, hip, and femur fractures
together anatomically, the management philosophy of these injuries is
quite different: the vast majority of pediatric pelvic fractures are
treated without surgical intervention, while most pediatric hip and
femur fractures are optimally managed with surgery.
In the adult literature, the pelvis is often compared to the ring of a
pretzel. A break in the ring in one location generally indicates a
break in a second location (either through the ligaments, or through
another part of the bony ring). In children, think of the pelvis as a
soft Philadelphia-style pretzel. The ring can indent, or break in one
place, or in two or more places. The abdominal and pelvic contents are
not as well protected in kids as in adults. The ligaments tend to be
stronger than bone, so CT scans (to define ligamentous disruption) play
a smaller role than in adults.3 Look
for iliac wing fractures rather than sacroiliac joint disruption, and
pubic rami fractures rather than pubic symphysis disruption. Most
important, work with your trauma surgeon to rule out abdominal,
urologic, chest, and head injuries (Fig. 8-2). For this reason, almost all children with a pelvic fracture are evaluated with an MRI.
 |
|
▪ FIGURE 8-1
Torode and Zieg classification of pelvic fractures in children. Type I, avulsion fractures; type II, iliac wing fractures; type III, simple ring fractures; type IV, ring disruption fractures. (Reprinted with permission from Canale ST, Beaty JH. Fractures of the Pelvis. In Beaty JH, Kasser JR, eds. Rockwood and Wilkins’ Fractures in Children, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:883-911.) |
leg length discrepancy, nerve palsies, heterotopic ossification, and
triradiate cartilage growth arrests have been the most frequently
reported problems. Schwarz, et al. reported leg length discrepancies up
to 5 cm in a small series of children with unstable pelvic fractures
treated with nonoperative methods.4
Sacral nerve root injuries have been reported after pediatric sacral
fractures. There are also isolated reports of common sciatic nerve
injury after pediatric pelvic fractures. A careful neurologic exam at
presentation is essential. Heterotopic ossification occurs
occasionally, but is rarely disabling. Therefore, counsel parents about
the risk of persistent hip stiffness after a
severe
hip or pelvic fracture. Displaced acetabular fractures through the
triradiate cartilage are rare injuries. Like any growth plate fracture,
early anatomic alignment is recommended. Families should be counseled
at the time of injury about triradiate cartilage growth arrest and the
possibility of later acetabular dysplasia.
 |
|
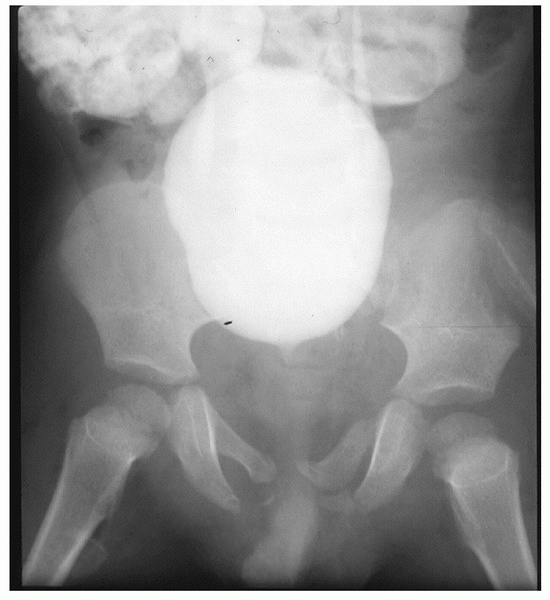
▪ FIGURE 8-2
Like a soft pretzel, the pelvis of a young child can absorb considerable force, bending, or breaking in just one place. In this child, who was run over by a car, the apparently minor bony injury belies the tremendous force that impacted the pelvis—and more important—its visceral contents. This child didn’t need plates and screws, he needed a trauma surgeon and a urologist. |
fracture recover well from their bone injuries. Their hospital course
and rehabilitation is often dominated by associated injuries. On
occasion, a child may have an adult-type injury or may present with
hemodynamic instability. In these cases, adult principles of external
fixation, possibly augmented by internal fixation, should be utilized
to close and stabilize the pelvic ring. Follow pelvic fractures for a
year after injury to assure there is no triradiate cartilage growth
arrest, leg length inequality, heterotopic ossification or other
potential long-term problem.
On your first encounter with the parents, you should counsel
extensively about the long list of risks that have been so well
described. These injuries often occur in children who fall from heights
or are struck by vehicles. Search for other injuries before focusing on
the femoral neck. Results reported since the advent of intraoperative
fluoroscopic imaging and stable internal fixation are far superior to
the old, classic series of
reports on children.5
Early anatomic reduction, stable internal fixation with screws and 4 to
6 weeks in a spica cast (for the young child) is the best way to stay
out of trouble.6 Early capsular
decompression may reduce the risk of femoral head necrosis, and there
is little morbidity from adding this to the treatment plan. In
teenagers, you can use the same principles as adults and cross the
growth plate with stable fixation. This allows them to be partial
weight bearing without cast immobilization.
The risk of AVN is related to fracture type: the closer the fracture to
the proximal femoral epiphysis, the more likely it will result in AVN.
There is not yet convincing evidence to support the notion that AVN can
be consistently prevented after a pediatric femoral neck fracture.
However, prompt anatomic reduction and internal fixation, perhaps with
capsulotomy or aspiration of the fracture hematoma, is the best the
orthopaedic surgeon can offer the child with a femoral neck fracture.
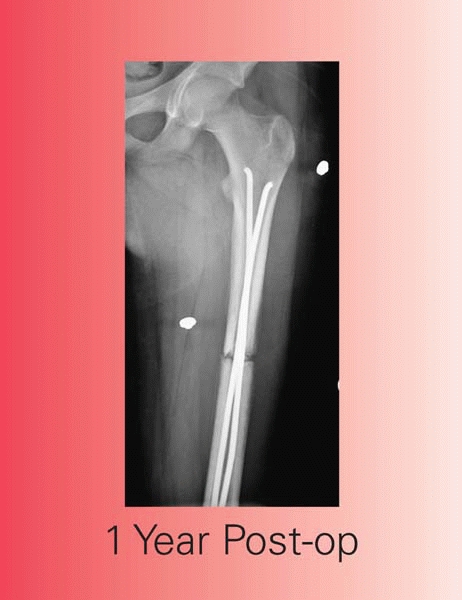
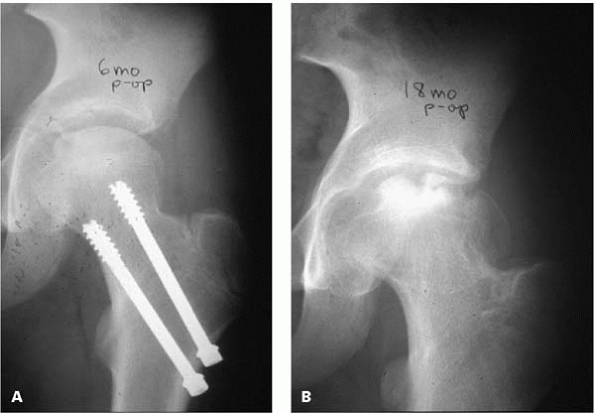
AVN may take 12 months or more to manifest itself. Good quality AP and
frog-lateral radiographs up to 2 years after injury are recommended.
 |
|
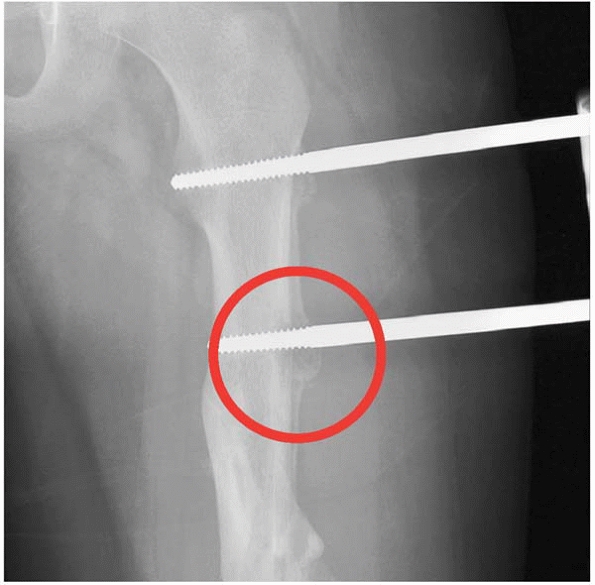
▪ FIGURE 8-3
(a) Plain radiograph taken 6 months after screw implantation. (b) Plain radiographs taken after screw removal at 18 months shows avascular necrosis of the femoral head. |
not well defined in AVN after pediatric femoral neck fracture, but it
is reasonable to assume that children would do as well or better than
adults when these methods are used prior to femoral head collapse.
Many believe that modern imaging and fixation have markedly reduced
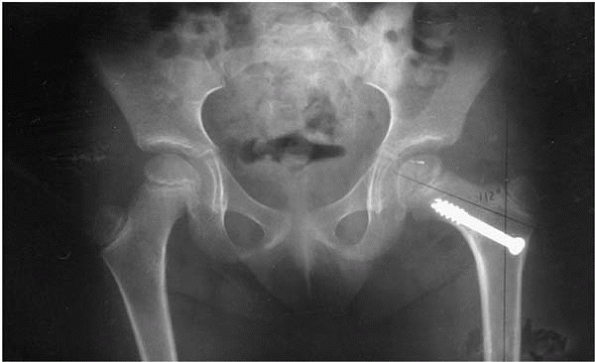
this complication. Probably the most important cause of coxa vara is
malunion. AVN or damage to the physis in the proximal femur can also
cause coxa vara. Many children will tolerate a neck shaft angle down to
120 degrees and still function at a very high level. Especially in
younger children, some improvement of the neck shaft angle over time
may be noted. If an older child (>8 years old) has a persistent
abductor lurch more than 2 years after injury and a neck shaft angle
less than 110 degrees, a valgus osteotomy may be helpful.
 |
|
▪ FIGURE 8-4 Plain radiograph showing coxa vara 2 years after surgery.
|
 |
|
▪ FIGURE 8-5 Physeal closure after type II femoral neck fracture.
|
In most cases, AVN is the culprit. Although an abductor lurch and
altered hip mechanics are common, functionally important leg length
inequality is rarely seen, except when there is physeal arrest in very
young children. In cases of leg length inequality, a contralateral
epiphysiodesis can be performed.
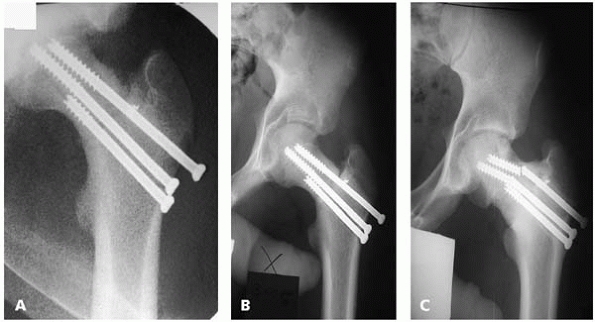
If there is persistent pain and no evidence of healing by 3 months
after injury, a nonunion should be suspected. Operative treatment is
recommended, with removal of initial internal fixation, repeat internal
fixation and possibly a subtrochanteric valgus osteotomy.
 |
|
▪ FIGURE 8-6 A:
Plain radiographs taken after screw fixation. There are signs of a struggle: note the small metal fragment adjacent to the most superior screw, indicating that a prior attempt with a screw here was hampered by unraveling of the thread on the dense bone. The screws are not parallel, probably holding the fracture in some distraction. B: Plain radiograph three months later shows early nonunion. The boy was lost to followup for two years. When he returned (C) he was healed because the screws broke. He had coax vara with a limp and a small leg length inequality. |
varieties: toddlers/young children who have dislocation with trivial
trauma; and older children/teens with hip dislocation, often with
significant trauma. In younger children, closed reduction is generally
easy, associated injuries are unusual, and AVN is rare. Traumatic hip
dislocation in older children presents much more trouble (Fig. 8-7).
 |
|
▪ FIGURE 8-7 Plain radiograph showing patient 2.5 years after hip dislocation.
|
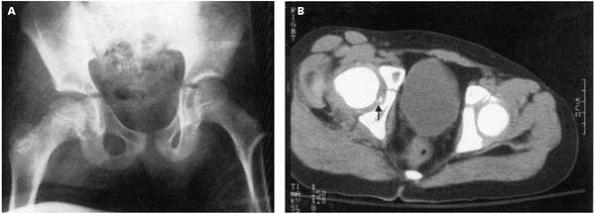
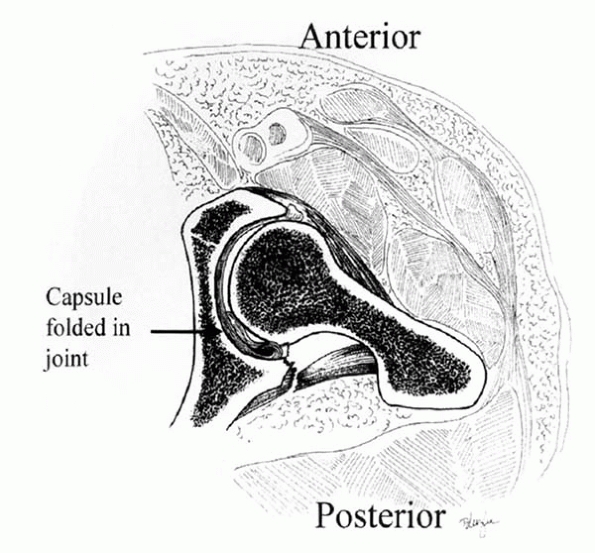
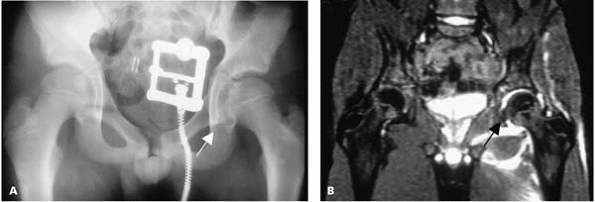
athletic injuries, or in pedestrian or motor vehicle accidents. The
best way to stay out of trouble is by recognizing that the injury has
occurred (sometimes spontaneous reduction may be unrecognized), by
being sure the reduction is done early and produces an anatomic
reconstitution of the joint, and using an MRI or CT scan, if necessary,
to assure that there is no interposed tissue after reduction (Figs. 8-8 and 8-9).
track or any other running and jumping sport. Consider this possibility
when presented with a teenage athlete who experienced sudden hip pain
during sports and has persistent groin pain or other associated
symptoms a few days later. Use a careful physical examination and good
quality radiographs to be certain that the hip is reduced, stable and
not affected by tissue interposed in the joint. If there is persistent
pain or any sign of joint space widening, or possible fragments seen on
the x-ray in the vicinity of the femoral epiphysis, an MRI is
recommended. Sometimes a widened joint space without radiographic
density is the only sign of an interposed capsule or labrum.
 |
|
▪ FIGURE 8-8 A: Plain radiograph of a 12-year-old boy who sustained a traumatic hip dislocation. B: CT scans showed labrum, capsule and cartilage (arrow)
from posterior wall interposed. (Reprinted with permission from Price CT, Pyevich MT, Knapp DR, et al. Traumatic hip dislocation with spontaneous incomplete reduction: a diagnostic trap. J Orthop Trauma. 2002;16-10:730-735.) |
epiphysis can be unstable. Before going to the operating room to reduce
a dislocated hip in a teenage patient with an open proximal physis,
warn the parents that there may be an unrecognized fracture at the
proximal femoral physis. There are reports of displacement through the
physis, giving the appearance of an acute slipped capital femoral
epiphysis, at the time of attempted closed reduction.8 It may be best to perform the reduction in the operating room with maximum relaxation and pain control.
 |
|
▪ FIGURE 8-9
Be suspicious of potential hip dislocation with spontaneous reduction; there may be tissue in the joint, as seen on this artist’s rendering. Check CT or MRI. (Reprinted with permission from Price CT, Pyevich MT, Knapp DR, et al. Traumatic hip dislocation with spontaneous incomplete reduction: a diagnostic trap. J Orthop Trauma. 2002;16-10:730-735.) |
commonly in older children and teenagers. It is probably related to the
severity of the initial trauma. As for femoral neck fractures,
reduction within 6 hours after injury may be beneficial in preventing
AVN.9
 |
|
▪ FIGURE 8-10 A: Plain radiograph taken at presentation of a hip injury (arrow) acquired while playing soccer. B: MRI scans showed the presence of interposed tissue (arrow).
|
forgiving than their adult counterparts. In children, particularly very
young children, the periosteum is thick, remodeling potential is
excellent, and small leg length differences may correct spontaneously.
However, treatment decisions are often complex due to concern about
damaging the physis or the blood supply to the proximal femoral
epiphysis. In adults, you slam down an intramedullary nail, interlock
it, and move on. In children, several options offer a variety of risks
and benefits. Different fracture patterns and clinical situations may
dictate that the best option is either a cast, traction followed by
casting, flexible intramedullary nailing, external fixation, or plating.10 Trochanteric-entry nails and submuscular plates are also finding a place in the management of pediatric femoral fractures.
management principles that should be heeded. First, although most
pediatric femur fractures heal without any long-term sequelae (often
regardless of treatment method), complications are a frequent source of
bad outcomes and professional liability claims. According to the AAOS
monograph Managing Orthopaedic Malpractice Risk,11
“The closed treatment of children’s (femur) fractures resulted in the
most frequent and expensive complications, including foot drop, skin
loss, compartment syndrome and malrotation/shortening.” Therefore, in
the small set of pediatric femur fractures that have complications, the
trouble can be enormous. Second, pediatric femur fractures are managed
with an aged-based algorithm. In the vast majority of cases, children
less than 6 years of age are optimally managed with closed reduction
and early spica casting. Children older than 6 years generally benefit
from some form of fixation. Third, infants who present with femur
fractures should be evaluated carefully for the possibility of
nonaccidental injury. This is a source of potentially great danger for
the child, agony for the family, and significant trouble for the
medical team. Surround yourself and the child with experts in this
clinical scenario.
Remember that the alignment and shortening recommendations are
age-based, and reflect acceptable standards abstracted from several
retrospective series.12 Understand
that many children do well functionally—even when these standards are
exceeded—but that may be difficult to explain in a courtroom setting.
Regarding acceptable angulation, accept less around the knee than
around the hip. Even 5 degrees or 10 degrees of angulation in the
distal femur of a teenager can cause trouble. In general, families tend
to be more forgiving when an injured side is longer after a fracture
rather than when the injured side is shorter after a fracture. Although
you should counsel extensively about the concept of overgrowth and
remodeling in pediatric femur fractures, it is wise to achieve the best
possible alignment with the safest clinical method and then deal with
potential overgrowth later.
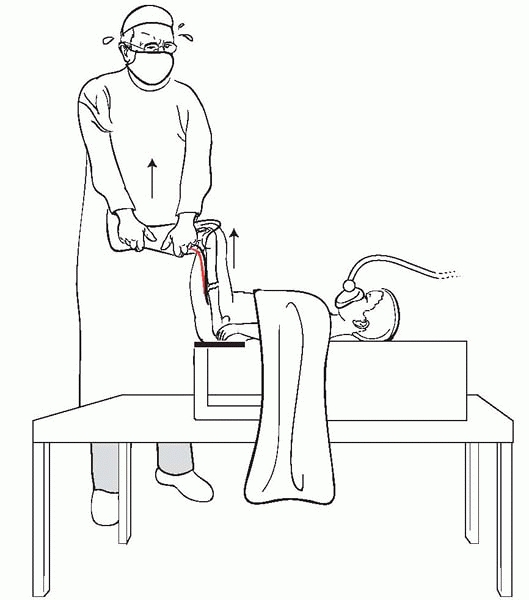
treat a pediatric fracture, but it is an art and can cause a remarkable
amount of trouble in even the best, most experienced hands. The
long-term results are excellent with this method but the first six
months can be very tough on the child and family (especially in the
child older than 4 years). In a high-energy trauma situation, perform
the telescope test before applying a spica cast.13
If the fracture shortens, more than 3 cm with gentle axial load, it has
a high likelihood of shortening if the cast was applied without a
period of traction. Traction and casting is relatively contraindicated
in children who are obese, in adolescents, and in children who have had
multiple trauma, a significant head injury, a floating knee injury, or
a very distal fracture. The traction pin should be put in the distal
femur, not in the proximal tibia where a proximal tibial growth arrest
is a risk. Apply the first section of the cast so that it includes the
foot, ankle, and calf, and goes just above the knee. Using this first
step, there is less risk that you will put excessive pressure or force
on the popliteal fossa or peroneal nerve as the rest of the cast is
applied (Fig. 8-11).14,15 Shortening is less likely if the hip and knee are flexed
to 90 degrees.16 A valgus mold should be made laterally, as most of these fractures will drift into varus if the cast is put on improperly (Fig. 8-12).
Assure that there is enough padding over bony prominences and along the
path that your cast saw will take at the time of removal. In bigger,
stronger children connecting the legs with a bar will prevent failure
of the cast at the hip. If there is any concern about leg swelling,
leave the foot out of the cast, and perhaps bivalve the cast. In some
cases, it may be wise to observe the child overnight after casting.
Teach the parents to prop up the head of the crib or bed in children in
diapers so that urine, etc., flows downhill. When it is time to remove
the cast, take an x-ray in the cast first to assure that there is
satisfactory callus. Be very careful about cast saw burns. The blade
becomes extremely hot, especially in the area of the hip. Stop
frequently to allow the cast saw to cool. After the cast is removed,
avoid the temptation to send the child immediately to physical therapy.
Most children fresh out of a body cast do not like to have a therapist
manipulating their joints, and early callus may fail. Keep the child in
the wheelchair and non-weight bearing for a week or two, reassess with
a radiograph, and then begin physical therapy if necessary. Warn the
family that the child may limp for up to a year after the injury.
|
TABLE 8-1 Femur Fractures: Acceptable Alignment at Union
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
▪ FIGURE 8-11
The dangers of pulling upward on the calf when applying a spica: this upward pull, which is used to reduce the fracture, can be dangerous, because it puts pressure on the gastrocnemius muscle and the other posterior leg structures, such as the femoral artery and femoral vein. |
 |
|
▪ FIGURE 8-12
Despite the incorporation of a traction pin into the spica cast, this fracture went into varus because there was no valgus mold on the cast. |
 |
|
▪ FIGURE 8-13
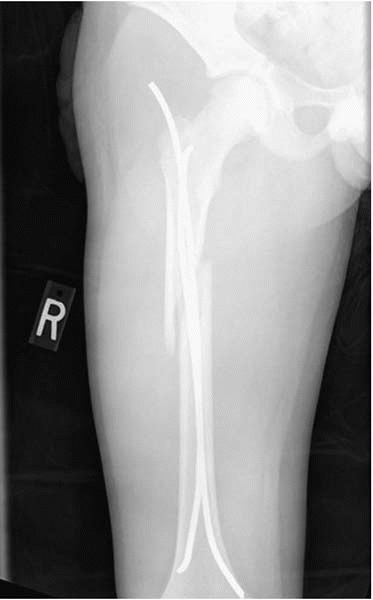
Flexible nails have several advantages, including rapid mobilization, maintaining length and alignment, good callus formation, and minimal risk for AVN, physeal injury, and refracture. |
popular way to treat pediatric femur fractures in children between the
ages of 6 and skeletal maturity. Although Enders nails have been used
for decades, and the French have used titanium nails since the 1970s,
the release of titanium elastic nails in the United States has made
flexible nailing perhaps the most popular method for treating stable
pediatric femur fractures in older children. The principles outlined by
the French are important: there should be symmetry of nail entry site,
nail size, and nail length in order to have two opposing internal
splints that stabilize the fracture. Ender nail principles include both
optimal nail bending and “stacking” of the nails to create stability.
Flexible intramedullary nailing is best for children from ages 6 to 14
who have a stable transverse fracture pattern in the mid-70% of the
diaphysis.17 These implants allow
rapid mobilization; they are good at holding length and alignment while
a large amount of callus is formed (Fig. 8-13). There
is minimal risk of AVN, physeal injury and refracture with these implants.18,19
After several cases, many orthopaedic surgeons become so enthusiastic
with the excellent results that they extend the indications to much
less stable fracture patterns. Long spiral fractures, comminuted
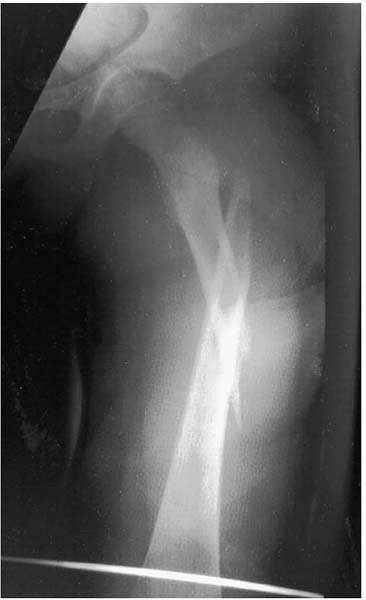
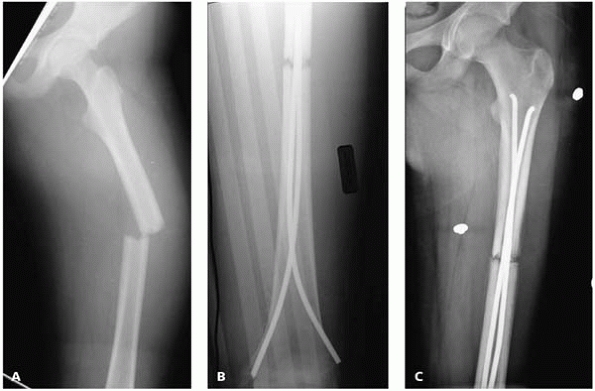
fractures, and proximal (Fig. 8-14) and distal
fractures can be treated with flexible intramedullary nailing; however,
supplemental immobilization is strongly recommended. Shortening, nail
back out, and malunion occur more often than is noted in the literature
published to date. In such unstable fractures, a long leg cast with a
pelvic band (one-legged spica) can be used for 4 to 6 weeks until
callus is sufficient to allow weight bearing as tolerated. Recent
attention has focused on the upper age and weight limits for these
implants.20, 21, 22
Complications, such as malunion, increase when titanium nailing is used
in children older than 11 years and heavier than about 50 kg. Although
flexible nailing may be the best option for such children, the family
and surgeon should be aware of the higher rate of trouble.
 |
|
▪ FIGURE 8-14
Injuries such as this long oblique proximal femur fracture can be managed very successfully with titanium nails, but the surgeon may have to alter technique and aftercare to get the best result. In this case, a proximal lateral entry was used, along with a distal medial entry, creating an excellent internal splint. A single leg “walking spica” was used for four weeks to prevent shortening or excessive angulation. |
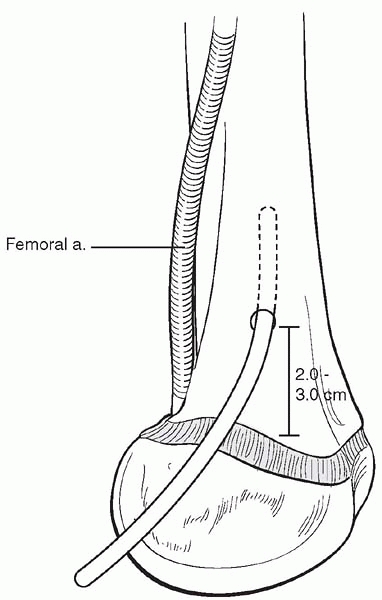
trouble with titanium elastic nailing. The nails are generally placed
retrograde, with a starting point about 2.5 cm above the distal femoral
physis (Fig. 8-15). Avoid any deep dissection
in the area of the distal femoral physis to minimize the chance of
growth arrest, and posterior to the femur, as vascular injury may
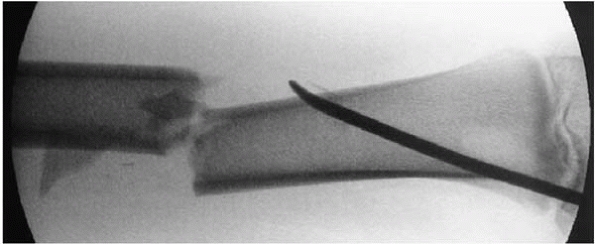
result. The tip of the titanium elastic nail is sharp enough to
penetrate the cortical bone in the area of the distal femoral
metaphysis (Fig. 8-16); image frequently if you
meet resistance as the nail is started up the canal. Leave only 1 to
1.5 cm of nail outside the bone, and don’t bend the nail tip away from
the metaphysis (Fig. 8-17). The most frequent
complication of these devices is soft-tissue irritation by the distal,
extraosseous portion of the nail. Be certain that rotation and
distraction are eliminated before leaving the operating room. There are
a few cases of delayed union or nonunion that resulted when
tight-fitting titanium elastic nails held the fracture site distracted
in the first couple of months after surgery (Fig. 8-18). In most centers, titanium
elastic nails are removed once the fracture is healed. Once the
fracture line is gone, the nails can be removed, but protect the child
in a knee immobilizer for at least a month or two after nail removal in
order to avoid refracture through the nail entry site.
 |
|
▪ FIGURE 8-15 The nails are generally placed retrograde, with a starting point about 2.5 cm above the distal femoral physis.
|
 |
|
▪ FIGURE 8-16 To avoid trouble with titanium elastic nailing, image frequently during nail passage.
|
 |
|
▪ FIGURE 8-17 To avoid irritation, leave only 1 to 1.5 cm of nail out distally and don’t bend the tip away from the bone.
|
select pediatric femur fractures. External fixation provides rapid and
rigid immobilization and allows for minimal incisions, minimal blood
loss, and a low risk of physeal injury or AVN.23
It is best used for severe soft tissue injuries or length-unstable
fractures (spiral or commuted fractures). In this way, it complements
elastic nailing nicely. The troubles surrounding the use of external
fixators for pediatric femur fractures have
limited its use, however. External fixation can produce pin site irritation, infection (Fig. 8-19), and unsightly pin track scars.24
 |
|
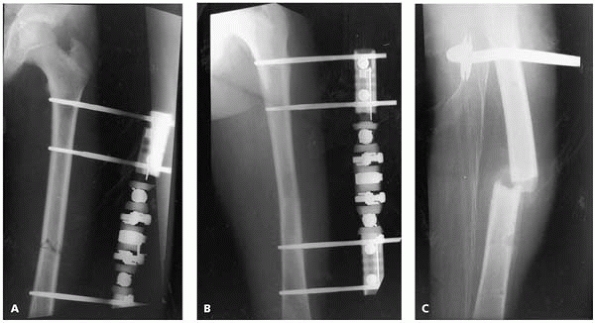
▪ FIGURE 8-18 A, B, C:
Delayed union after the fracture was fixed in distraction; this 14 year old refused to bear weight because of distal nail irritation of the knee. |
 |
|
▪ FIGURE 8-19 To avoid pin site infection, avoid bone necrosis and motion at pin site. Administer oral antibiotics.
|
Several series have reported this problem, despite the best efforts to
dynamize the device. If weight bearing is going to be allowed
immediately after fixator removal, at least three cortices should be
united on two views of the fracture site.25
As an alternative strategy, the device can be removed as soon as the
fracture is length stable (usually 6 to 8 weeks) and the child can be
placed in a one-legged spica cast until the callus matures and the ex-fix pin sites fill in (6+ weeks).
 |
|
▪ FIGURE 8-20 A: This patient was treated with external fixation. B: At three months, the fracture appears to have healed. C:
However, one week after removal of the device, refracture occurred. Avoid end-to-end reduction of transverse or short oblique fractures. |
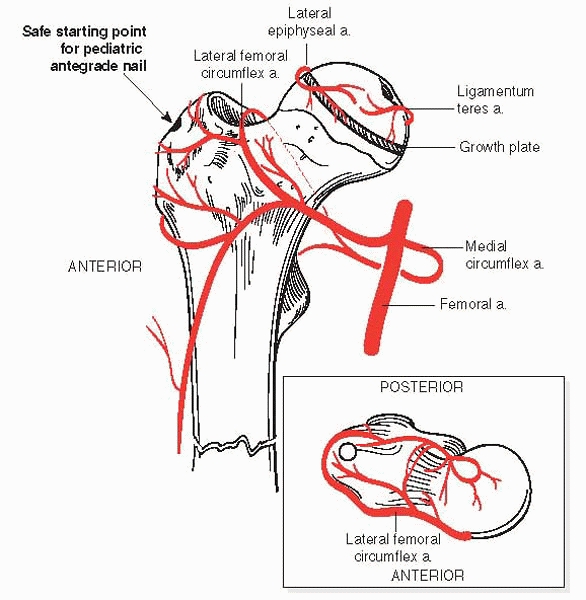
skeletally mature teen, just as it is for an adult. It offers maximum
stability and load sharing and maintains perfect alignment.
Unfortunately, there have been many reported cases of AVN of the
capital femoral epiphysis when a solid antegrade nail is used in a
skeletally immature patient. Casting, flexible nails and external
fixation are mainly complicated by malunion, shortening, refracture, or
soft-tissue problems; these are rare in intramedullary nailing.
However, problems such as leg length inequality and malunion can be
successfully corrected with later surgery, but AVN of the proximal
femur is trouble that should be avoided, not treated. Newer generations
of antegrade nail, most using a trochanteric or lateral starting point,
may fulfill the need to manage length-unstable pediatric femur
fractures without risking AVN. Until then, current recommendations
include avoiding the piriformis fossa (Fig. 8-21)
with a trochanteric starting point and using a smaller diameter femoral
nail in children. Most important, the surgeon should ask: is there a
better treatment option for this child with an open proximal femoral
physis in a femur fracture?
plate fixation is used infrequently for pediatric femur fractures.
Although it does give rapid and rigid fixation with widely available
equipment, problems with hardware failure, large incisions, significant
blood loss, the need for hardware removal, and refracture after
hardware removal have limited the use of plates. Recently, there has
been a wave of enthusiasm for submuscular plating employing a minimally
invasive approach. This method is technically demanding and unnecessary
for most pediatric femur fractures, but it may address some of the
shortcomings of standard open plating. Overgrowth has been reported
after plate fixation, so the family should be counseled appropriately.
 |
|
▪ FIGURE 8-21
To avoid trouble when using solid intramedullary nails and to avoid AVN, ensure no awl in the piriformis fossa; a trochanteric starting point, and use smaller diameter nails. |
-
Search for associated trauma.
-
Counsel at presentation: leg length discrepancy, heterotopic ossification.
-
Perform a thorough neurologic examination at presentation.
-
Follow patient for at least 1 year.
-
Counsel at presentation: AVN, coxa vara, growth arrest.
-
Early, anatomic reduction.
-
Use screws, not K-wires or spica alone.
-
Protect younger children in a spica for a few weeks after internal fixation.
-
Follow patient for at least 2 years.
-
Counsel at presentation: leg length discrepancy, limping for up to 1 year
-
Consider child abuse, especially in children younger than 1 year old.
-
Follow standards for length/alignment.
-
Spica: don’t use excessive traction on leg and protect popliteal fossa.
-
Titanium Elastic
Nailing: symmetrical configuration, no excessive bend at entry, no
distraction/rotation, knee immobilizer (stable fracture), 1-leg spica
(unstable fracture) for 4 to 6 weeks. Be careful with bigger, older
kids (especially >11 years old, >50 kg) -
External fixation:
protect the pin-bone interface, release skin at pin sites, dynamize,
assure 3 cortices healed, or protect in walking spica. -
Intramedullary nail: stay out of the piriformis fossa.
JS, Flynn JM. Changing patterns of pediatric pelvic fractures with
skeletal maturation: implications for classification and management. J Pediatr Orthop. 2002;22-1:22-2-6.
JS, Flynn JM, Koffler KM, et al. Analysis of the cause, classification,
and associated injuries of 166 consecutive pediatric pelvic fractures. J Pediatr Orthop. 2001;21-4:446-450.
JS, Flynn JM, Katz MA, et al. Role of computed tomography in the
classification and management of pediatric pelvic fractures. J Pediatr Orthop. 2001;21-2:148-151.
JM, Wong KL, Yeh GL, et al. Displaced fractures of the hip in children.
Management by early operation and immobilisation in a hip spica cast. J Bone Joint Surg Br. 2002;84-1:108-112.
KC, Thompson JD, Sponseller PD, et al. A prospective study of early
spica casting outcomes in the treatment of femoral shaft fractures in
children. J Pediatr Orthop. 1995;15-1:30-35.
AP, Schenck RC, Jr., Sponseller PD, et al. Peroneal nerve palsy after
early cast application for femoral fractures in children. J Pediatr Orthop. 1992;12-1:25-28.
TM, Frick SL. Compartment syndrome of the leg after treatment of a
femoral fracture with an early sitting spica cast. A report of two
cases. J Bone Joint Surg Am. 2003;85-A-11: 2207-2210.
JM, Hresko T, Reynolds RA, et al. Titanium elastic nails for pediatric
femur fractures: a multicenter study of early results with analysis of
complications. J Pediatr Orthop. 2001;21-1: 4-8.
JM, Launay F, Moroz L, et al. Titanium elastic nailing of pediatric
femur fractures: predictors of complications and poor outcomes. American Academy of Orthopaedic Surgeons. Washington DC, 2005.
CT, Foad SL, Crawford AH, et al. Weight ≥99 pounds (45 kg) and age ≥12
years predict malunion following elastic stable intramedullary nailing
(nancy nailing) of femoral shaft fractures in children. Presented at Pediatric Orthopaedic Society of North America. St. Louis, MO, 2004.