Staying Out of Trouble while Treating Hand, Wrist, and Forearm Injury
|
|
common injuries sustained by children. Although not life threatening
and usually not debilitating, they may be a frequent source of
management trouble due to the sheer volume seen by most orthopaedists
caring for children. Most injuries can be treated successfully and will
heal uneventfully; however, careful attention to certain principles of
diagnosis and management is critical to a consistently good outcome.
orthopaedist caring for children can handle the vast majority of hand
injuries in children, it is important to know which cases should be
transferred directly to a hand surgeon.
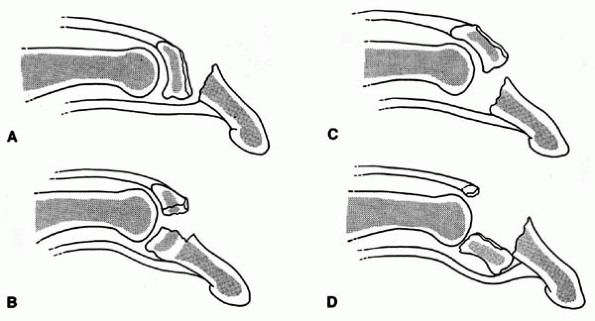
fractures. Fortunately, growth arrest is very rare. To stay out of
trouble, it is important to recognize that an apparent “tendon
disruption” may instead be a physeal fracture in a young child (Fig. 7-1).
The flexor digitorum profundus inserts onto the distal phalanx and the
flexor digitorum superficialis inserts onto the middle phalanx. The
extensor tendons insert onto the epiphysis of the distal phalanges.
 |
|
▪ FIGURE 7-1
What looks like a tendon avulsion can be a growth plate injury in children. (Reprinted with permission from Graham TJ, O’Brien ET. Fractures and Dislocations of the Hand and Carpus in Children. In Rockwood CA Jr., Wilkins KE, Beaty JH, eds. Fractures in Children, 4th ed. Philadelphia: Lippincott-Raven, 323-447.) |
First, the orthopaedist should assess for an open injury, which can be
subtle in the hand. Neurologic examination can be very difficult in
children. One clue to a possible nerve injury is excessive bleeding
from a wound around the area of the digital nerve, since the digital
artery and nerve are often lacerated together. To stay out of trouble
in assessing a nerve, it is helpful to do the “wrinkle test.” Immerse
the digit in warm water for about 5 minutes. Denervated digits will not
have any wrinkling of the volar skin.
control. Digital blocks are very effective for phalangeal fractures and
nail bed injuries. To stay out of trouble, do not use epinephrine for
digital block, as it may lead to distal ischemia. Also, never inject a
circular weal around the digit as the circulation of the digit can be
compromised.
 |
|
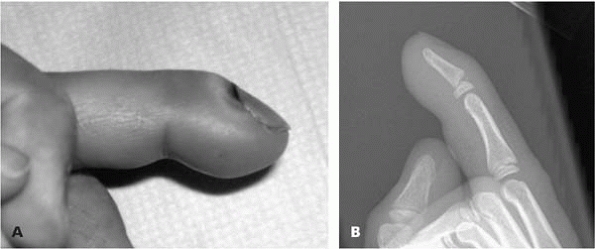
▪ FIGURE 7-2
The “closed” Seymour fracture. This child presented four days after sustaining an injury to his index finger. The clinical examination showed no nail avulsion but a mallet posture to the finger and blood under the eponychium (A), indicating nail bed laceration. The lateral radiograph (B) raised concern of a Seymour fracture. At operation, gross purulence was found in the physeal fracture. (Reprinted with permission from R. Cornwall, MD.) |
be missed. Plain radiographs should be obtained to assess for a
concomitant fracture. The nail should be removed if it is not already
off and the wound should be irrigated just like an open fracture.
(or “jersey finger”) injury. Mallet fingers in children are usually
avulsion fractures rather than tendon disruptions. In younger children
these will usually be a Salter Harris I or II injury with the flexor
tendon still attached to the distal piece. “Jersey finger” injuries
usually occur in adolescents near skeletal maturity. The classic
example is a football player whose finger gets caught in an opposing
player’s jersey, leading to a flexor tendon avulsion. AP, lateral, and
oblique radiographs should be obtained to look for avulsion fractures
entrapped in the pulley system or in the palm. To stay out of trouble,
surgical intervention, within 7 to 10 days after injury, is usually
required to reattach the tendon after a jersey finger injury.
gruesome injuries, brought in by hysterical parents. If the parent
brings the amputated part it is important to assess its quality to
decide whether replantation or a composite graft is warranted.
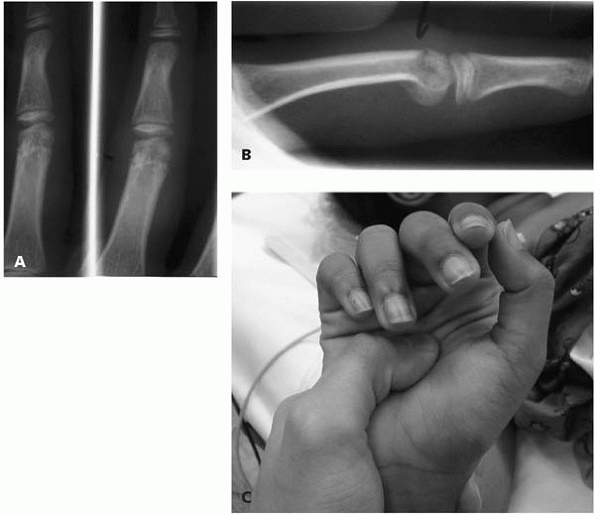
can generally be managed successfully, but do present a few specific
sources of trouble. One important cause of problems is failure to
recognize a rotational deformity (Fig. 7-3).
can be treated with nonoperative management utilizing reduction and
casting for 3 to 4 weeks.
is the neck. Most can be treated with closed reduction and splinting in
the safe position.
 |
|
▪ FIGURE 7-3
Perhaps the most classic source of trouble in pediatric hand fractures: the missed rotational deformity. The AP and oblique radiographs (A) of the proximal phalanx fracture look innocuous enough. The lateral radiograph (B) best shows the malrotation at the fracture site. This preoperative clinical photograph demonstrates the malrotation of the long finger. The key is the physical examination, which shows the problem in three dimensions. (Case courtesy of R. Cornwall, MD.) |
for malrotation. When the child makes a fist, all fingers should point
to the scaphoid and all nail beds should be parallel. Unstable
fractures with residual rotational malalignment may require closed
reduction and percutaneous pinning. Fractures at the base of the
metacarpal are infrequent in children. They are usually the result of
high-energy trauma.
present as simple transverse fractures or intraarticular fractures.
Salter Harris type III and IV fractures at the base most closely
resemble the adult Bennett’s fracture. Fractures at the base of the
thumb without intraarticular extension can be treated with closed
reduction and immobilization. Angulation of up to 20 degrees can be
accepted.
gamekeeper’s thumb) are typically encountered in adolescents rather
than young children. Similar to other injuries, the ulnar collateral
ligament will be stronger than the adjacent bone, resulting in a Salter
Harris III avulsion fracture rather than ligament disruption. This is a
“gamekeeper’s equivalent” and requires open reduction and internal
fixation if displaced.
children are exceedingly rare. The most common is a scaphoid fracture.
Be alert to the fact that the scapholunate space may be physiologically
wider in an immature child as there is unossified cartilage. This
should not be mistaken for a perilunate injury. Comparison views will
help define the normal space for the child that presents to you. To
stay
out
of trouble with carpal bone injuries, any patient with pain in the
snuffbox should be treated using a thumb spica cast for 10 to 14 days,
even if the radiographs are negative.
high risk of avascular necrosis (AVN). Distal pole fractures seem to
heal with no problem. Fractures at the scaphoid waist are similar risks
as in adults.
relatively rare, these injuries are not uncommon in the teenage
athlete. To stay out of trouble, look for areas of open injury and do a
good prereduction neurovascular examination. If the joint is
irreducible, it is possible that there is an interposed ligament or
volar plate hindering reduction. Open reduction may be necessary.
common in children. The keys to staying out of trouble include
understanding remodeling, avoiding overtreatment, putting your
reductions in good casts, and being alert for associated injuries.
Remodeling is greatest in young children, in fractures near a rapidly
growing physis, in fractures that are in the plane of motion of the
adjacent joint, and in fractures with greater amounts of angulation.
Typically, the child can correct about 10 degrees of apex-volar
angulation for each year of growth remaining. Radial-ward angulation of
the distal radius, caused by the pull of the brachioradialis, corrects
more slowly. Bayonet apposition remodels reliably in younger children,
especially those less than about 8 years old.
common growth plate injury in children. To stay out of trouble,
evaluate for open injuries, especially subtle pinpoint openings on the
volar skin. Higher energy injuries, such as when a teenager falls
rollerblading, can lead to neuropraxia of the median nerve, or even
acute carpal tunnel syndrome or compartment syndrome.1
To stay out of trouble, do a careful nerve exam and get these fractures
reduced as quickly as is practical. The easiest injury to miss is the second
injury, so be certain to evaluate the elbow and hand carefully when
confronted with a distal radius fracture. Minimally displaced fractures
are often placed in a splint and an ace wrap in the emergency
department and sent on to an orthopaedist office for management. A
tight ace wrap can be trouble (Fig. 7-4).
Children will shift in the splint, or play with their ace wrap, which
can become rolled and cause a tourniquet-like effect. The ace wrap can
create a row of blisters at the seams between the ace wrap or create a
tremendous amount of swelling distally. Alert your emergency room
colleagues about the potential dangers of tight ace wraps in children,
and get these children into a proper cast as soon as is practical.
sedation at the time of injury. It is a general principle to avoid
reductions or re-reductions of physeal injuries later than
approximately 10 days following injury, in order to avoid growth
arrest. Open or closed reduction with K-wire fixation is used in
special circumstances.2
should be taken to avoid the radial sensory nerve and the extensor
tendons. Most agree that smooth K-wires across the physis are not a
significant risk for growth arrest.3
 |
|
▪ FIGURE 7-4
This 5-year-old boy had a distal radius fracture, which was splinted in the emergency department two days prior to presentation. As often occurs, the ace wrap rolled up around his wrist, creating a tourniquet effect, and leading to dramatic hand swelling. His mother was more concerned about the hand than the wrist fracture. Fortunately it was only two days… |
of a distal radial physeal fracture will remodel satisfactorily in a
child with more than 3 years of growth remaining. Of course, this
should not be the goal at the first reduction. However, if an
8-year-old returns to your office with 30 degrees of angulation 10 days
later, that can be accepted with an excellent result. The risk of
growth arrest from a distal radius physeal fracture is considered to be
4%. However, the rate of growth arrest of a distal ulnar physeal
fracture4 is 60%.
metaphyseal fractures can be treated in many ways with a good result.
Some orthopaedists use splints and ace wraps, some use removal Velcro
splints and many cast. In our experience, the least trouble occurs when
a well-padded short arm cast is used.
reduction, it is important to understand the help and hindrance of
intact periosteum. In dorsally displaced fractures, the periosteum is
torn on the volar surface. With a good three-point mold, the intact
dorsal periosteum will help hold your reduction. However, the intact
dorsal periosteum also will make it impossible to reduce the fracture
with pure traction, as is done for an adult Colles fracture. Once
adequate conscious sedation is obtained, the fracture is reduced by
re-creation of the deformity, which may lead to fainting by one or both
parents. To avoid loss of reduction (Fig. 7-5),
a well-made cast is essential. There should be a three-point mold at
the distal radius. One common problem is a series of cast molds that
are so close together that they really are not working as three points,
but as just one diffuse, unhelpful pressure point. The cast should be
oval so that the anterior-posterior diameter is less than 0.7 of the
radioulnar diameter (this has been called the cast index). Extreme
pronation and supination should be avoided, as it is thought to
increase compartment pressures. A long-arm cast is used for completely
displaced fractures. A followup x-ray is often done about 5 to 10 days
after reduction.
of dorsal angulation or 20 degrees of radial-ward angulation will yield
a good result. One way to stay out of trouble with parents is to put a
chart up in your office or cast room that shows progressive radiographs
of a distal radius fracture remodeling over the course of several
months (Fig. 7-6). This will help to decrease
anxiety in parents when the parents see the crooked bone on radiograph.
It will also help you avoid the temptation to overtreat these injuries.
When a displaced distal radial metaphyseal fracture occurs with a
displaced ipsilateral supracondylar fracture, stay out of trouble by
pinning both.5,6
Growth arrest is possible after a metaphyseal fracture of the distal
radius, so at least one later followup visit may be advisable.7
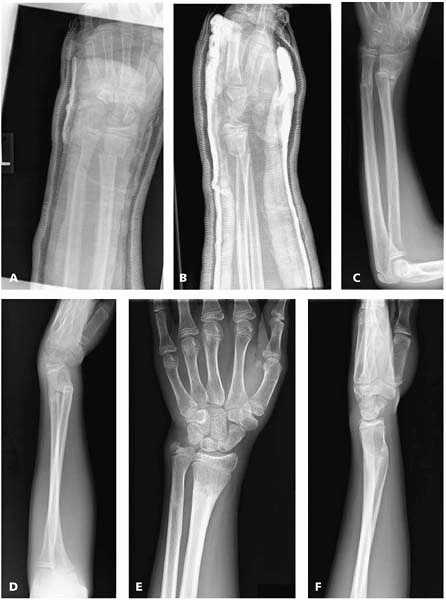 |
|
▪ FIGURE 7-5
This case illustrates the trouble from a bad cast, and the need to avoid overtreatment. This 12-year-old boy sustained a high-energy distal radius and ulna fracture. A,B: AP and lateral radiographs after reduction. The reduction is satisfactory, but the cast predicts trouble: there is no mold on the distal radius, either dorsally or radially. A prefabricated splint was used, rather than plaster splints. Predictably, he lost reduction. C,D: The boy neglected to follow up until 7 weeks after injury, when he presented with an ugly arm and angulation that textbooks say is unacceptable for a 12 year old. Mom wanted some corrective surgery “as soon as possible.” Instead, education was offered. E,F: 6 months after injury: dramatically better, but not yet good enough. He still lacks about 10 degrees of pronation and supination. Mom no longer wanted surgery; in fact, she probably won’t bring him back for further followup. |
disruption of the triangular fibrocartilage complex (TFCC). These are
very rare injuries in children. In children, the TFCC is rarely torn;
instead the distal ulnar physis is fractured and displaced (an
equivalent injury). Remember the 60% physeal arrest rate of displaced
distal ulnar physeal fractures. Most Galeazzi fractures can be treated
with closed reduction and a long-arm cast for about 6 weeks, with the
forearm in slight pronation.
trouble than distal radius and ulna fractures. The remodeling of the
shaft is much less extensive and the healing is slower. Much more
stringent reduction criteria are needed than for the distal fractures.
A significant malunion of a forearm diaphyseal fracture will lead
to
permanent loss of pronation and supination, and sometimes an unsightly
curvature or prominence in the forearm. To stay out of trouble,
understand that many of these fractures, especially greenstick
injuries, are rotational injuries and are reduced with derotation of
the forearm. Although upper extremity compartment syndrome is rare, the
most common cause in children today is a forearm fracture (and no
longer supracondylar fractures treated with flexion, causing Volkmann’s
ischemic contracture). Don’t be fooled by pseudo Volkmann’s contracture
due to tethering of the flexor digitorum profundus to fractures of the
ulna. One report described seven cases, detected 2 days to 16 years
after closed reductions of fractures of the shafts of the radius and
ulna. The children did not have nerve palsies or undue pain after the
reductions. Normal length, excursion, and function of the flexor
digitorum profundus were restored by untethering the muscle and its
tendons from the ulnar fracture by early manipulation or by late
localized myotenolysis. The authors recommended that the passive range
of motion of all fingers be routinely checked immediately after closed
reductions of fractures of the radius and ulna. If muscle tethering is
detected, the fracture is re-manipulated to release the muscle. If the
muscle is still tethered, then surgical release, through a small
incision, is recommended.8
 |
|
▪ FIGURE 7-6
Many pediatric orthopaedic practices hang a chart such as this one (from Children’s Hospital of Philadelphia) in their cast room to reassure parents and avoid overtreatment of distal radius fractures. |
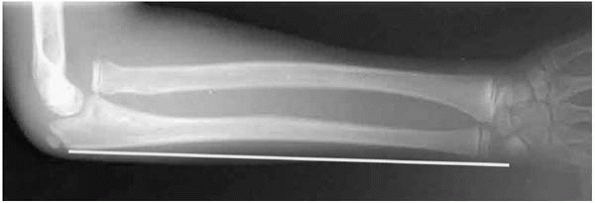
subtle injury. The most common and most important oversight is the
missed Monteggia fracture, especially in the apparently isolated ulna
injury. To stay out of trouble, the orthopaedist should insist on two
views of the entire forearm at right angles to one another, as well as
dedicated films of the elbow, to be assured that the radiocapitellar
relationship is satisfactory (Fig. 7-7). To
understand rotation, look at the width of the diaphyseal fragment at
the fracture site and study the relationship between the bicipital
tuberosity and the radial styloid (they should be opposite one
another). In all angulated or displaced radius and ulna diaphyseal
fractures, manipulative closed reduction under conscious sedation or
general anesthesia should be performed. Diaphyseal fractures in
children require 6 weeks of immobilization, at a minimum. In older
children, 8 weeks may be necessary. To stay out of trouble, warn
families that diaphyseal forearm fractures are among the rare fractures
in children that are at risk for refracture. Refracture seems to be a
risk in greenstick fractures and in the first 3 months after cast
removal. One study9 of 768 children
with displaced forearm fractures requiring reduction found a refracture
incidence of 4.9%. The median time to refracture was 8 weeks after
discontinuing cast immobilization. The authors found that diaphyseal
fractures were
eight
times more likely to refracture than metaphyseal fractures, and that
the risk of refracture was inversely proportional to the duration of
cast immobilization. Cast immobilization for a minimum of 6 weeks
reduces the risk of refracture by a factor of between four and six.
Midshaft forearm fractures are at risk of refracture for 16 weeks from
cast removal.
 |
|
▪ FIGURE 7-7 A missed Monteggia fracture presented 2 weeks after injury. All images done at the outside hospital (A,B)
showed only a greenstick fracture of the ulna, and mom’s hand covering the elbow. Suspicious for a Monteggia, we removed the cast and obtained good elbow images, revealing the dislocated radial head (C,D). |
increasingly used to stabilize one or both bones of pediatric
diaphyseal forearm fractures. The preferred entry site for the ulna is
proximal in most cases. For the radius, the best entry site is at
Lister’s tubercle, or on the radial side of the radius, with caution to
avoid injury to the radial nerve.
attempt to get the intramedullary wire across the fracture site. If you
don’t get the wire across in three attempts, it is safer to open the
fracture.10 Multiple missed passes
in a swollen forearm increase the risk for compartment syndrome. Single
bone fixation, usually with an ulnar intramedullary K-wire, is often a
simple solution, especially for fractures in the 8- to 12-year-old age
range. As children approach
maturity, adult style plating allowing rapid mobilization is usually the best way to stay out of trouble.
trouble. In young children in whom there is no cosmetic deformity in a
full range of motion, casting without reduction is acceptable. However,
if the arm appears bowed or motion is lost, reduction should be
attempted in the operating room. A great amount of force must be
applied at a very slow rate over a long period of time to correct
plastic deformation.11 After
reduction, a long-arm cast is used for 4 to 6 weeks. Again, beware of
the plastically deformed ulna that distracts your attention from an
associated radial capitellar dislocation.
represent less than 1% of all pediatric forearm fractures, they receive
great attention because they create so much trouble. Most of these
injuries occur in children younger than age 10. Many “isolated radial
head dislocations” that walk into your office as routine visits were
probably missed traumatic lesions rather than congenital dislocations.12
To stay out of trouble, high-quality radiographs are mandatory to
manage Monteggia fractures successfully. The views should include the
whole forearm, as well as isolated elbow radiographs. The ulna should
be “ruler straight”13 (Fig. 7-9).
A line drawn down the shaft of the radius should point to the center of
the capitellum. Be sure to assess this after initial reduction and at
each follow-up, as late dislocation of the radial head has been
reported.14 Remember, there is
normal angulation of the proximal ulna in children, and the proximal
radial neck can angulate up to about 12 degrees of valgus. Also, a
careful neurologic examination is essential, since up to 20% of
Monteggia fractures present with nerve palsy. The most common scenario
is a posterior interosseous nerve palsy associated with a Bado type III
lesion.
attempt at closed reduction with conscious sedation or general
anesthesia. If the injury is acute, a very satisfying reduction “clunk”
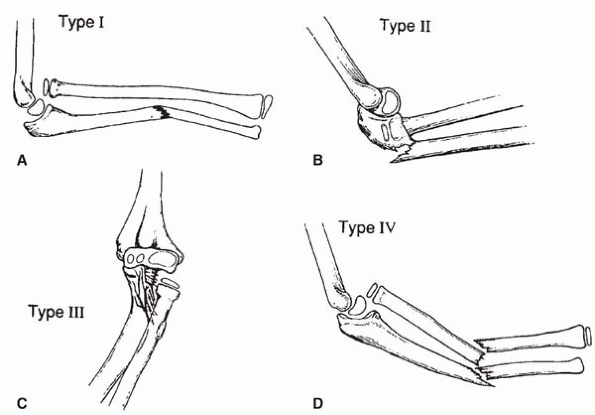
is usually felt. Type I fractures are reduced with forearm supination
and complete elbow flexion, but they should not be casted in
hyperflexion.
A well-molded long-arm cast at 90 degrees for about 4 to 6 weeks is
satisfactory. For Type II fractures, the fractures are reduced with
elbow extension. This can be a difficult position to maintain in a
long-arm cast. Often fixation of the ulna is necessary for stability.
Type III fractures require a correction of the varus angulation in
order to reduce the radial head. Type IV fractures are very difficult
to treat with a simple closed reduction. Often, the radial shaft
fracture must be internally fixed with either a plate or a wire in
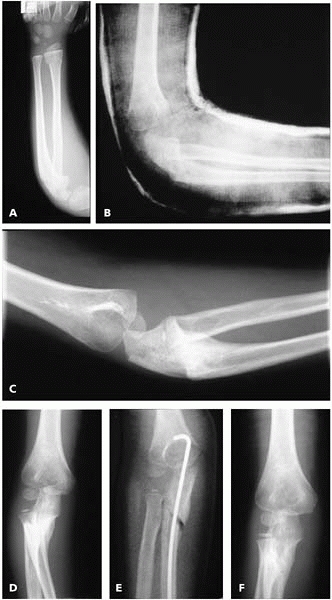
order to successfully reduce the radial head (Fig. 7-10).
 |
|
▪ FIGURE 7-8
Four types of Monteggia fractures, as described by Bado. (Reprinted with permission from Wilkins KE, O’Brien ET. Fractures of the Distal Radius and Ulna. In Rockwood CA Jr., Wilkins KE, Beaty JH, eds. Fractures in Children, 4th ed. Philadelphia: Lippincott-Raven, 451-651.) |
 |
|
▪ FIGURE 7-9
The ulna should be “ruler straight.” This radial head dislocation is associated with plastic deformation of the ulna (anterior bowing). Many of the children who present with “isolated” or “congenital” radial head dislocations actually had a Monteggia fracture of equivalent. (Reprinted with permission from Price CT, Flynn JF. Management of fractures. In Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopaedics, 6th ed. Philadelphia, Lippincott Williams & Wilkins, 2006.) |
mandatory in Monteggia fractures. To stay out of trouble during the
followup period, immobilize the Monteggia fracture in a cast with only
thin fiberglass at the elbow. In this way, you will be able to
visualize the elbow joint clearly without obscuring plaster. If there
is any question about the relationship of the radius and capitellum
during the postoperative period, it is better to take the cast off and
get good x-rays and risk loss of reduction, than to continue to cast a
malaligned radiocapitellar joint obscured by plaster.
of recognition, failure of initial reduction, loss of reduction, nerve
injury, late stiffness, radial head avascular necrosis, and radial
ulnar synostosis. If a Monteggia fracture is missed, late
reconstruction involves restoring ulnar length and alignment and an
open reduction of the radial head, often with angular ligament
reconstruction.15 Even in the best
of hands, results of late reconstruction are often disappointing if
more than 6 to 12 months has elapsed since the injury.16
unusual, but metaphyseal proximal radius fractures are not. Since the
radial head’s relationship with the capitellum is critical in
maintaining forearm rotation, optimal reduction of angulation—and more
important, translation—offers the best chance of a good functional
result. Proximal radius fractures cause a remarkable amount of trouble,
especially persistent loss of motion after injury. Even compartment
syndrome has been reported after these troublesome injuries.17
Pay careful attention to the radial nerve on the initial neurovascular
examination. An attempt should be made to reduce displaced proximal
radius fractures under conscious sedation or general anesthesia. This
can be aided by injecting a local anesthetic into the radiocapitellar
joint and evacuating the hematoma prior to reduction. After an attempt
at closed reduction, up to 30 degrees of angulation and 3 mm of
translation can be accepted. If reduction under conscious sedation
fails, additional attempts should be made with fluoroscopic guidance in
the operating room.
maneuvers to reduce a proximal radius fracture before resorting to open
reduction. Many of the complications described in the literature for
radial head and neck fractures are the result
of
open reduction. Of course, these are probably the worst proximal radius
fractures, but it is clear that once you open these injuries you are
inviting a lot of trouble. A recent prospective multicenter study
concluded that the restricted use of open interventions may be the key
to improving results.18
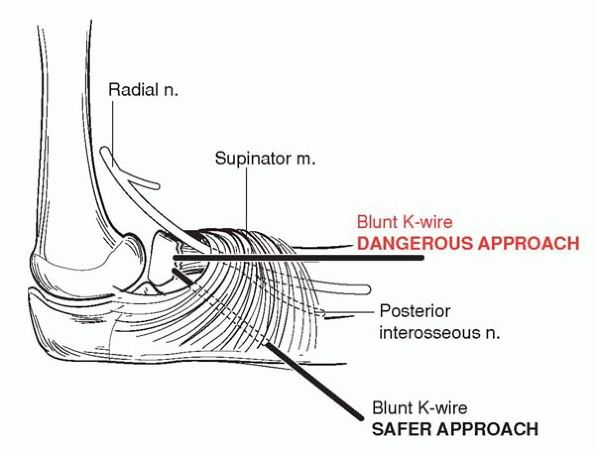
Before opening a radial head or neck fracture, attempt reduction with
the elbow extended in a valgus force, attempt closed reduction with the
Israeli technique (flexion and pronation), and attempt a reduction
aided by percutaneous manipulation using a small K-wire or an awl. To
stay out of trouble with the percutaneous manipulation maneuver, be
certain you understand where the posterior interosseous nerve is. There
are reports of radial nerve injury using this technique (Fig. 7-11).
If you open a proximal radius fracture, it is wise to stabilize the
fracture after reduction. To support this concept, one study reviewed
nine cases of radial neck nonunion.19
The authors concluded that the severity of initial fracture
displacement and inadequate fixation technique contributed to radial
neck nonunion. Healing of the nonunion did not necessarily lead to
improvement of clinical symptoms.
 |
|
▪ FIGURE 7-10
Getting out of trouble: an ulnar osteotomy to salvage a missed Monteggia fracture. Trouble: the focus was on the distal radius, so the radial head dislocation was missed (A). More trouble: they thought to get an elbow radiograph, but the cast obscured the radial head dislocation, so it was missed (B). The family presents for a second opinion a few weeks after injury. The ulna is healed and the radial head is out (C,D). After an ulnar osteotomy and intramedullary fixation with a Steinmann pin, the radial head was reduced and stable. The radiocapitellar joint was not opened (E). Six months later, all better (F). |
 |
|
▪ FIGURE 7-11 Drawing of the position of the radial nerve and how it is adjacent to a joystick pin or awl.
|
fractures, be sure to warn families at the time of injury that loss of
motion is common, regardless of treatment. These fractures should not
be immobilized for more than about 3 to 4 weeks.
 |
|
▪ FIGURE 7-12
This olecranon sleeve fracture was the first presentation of mild osteogenesis imperfecta in this child. (Reprinted with permission from Price CT, Flynn JF. Management of fractures. In Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopaedics, 6th ed. Philadelphia, Lippincott Williams & Wilkins, 2006.) |
Most are minimally displaced and involve the metaphysis without
significant articular disruption. Be alert that an olecranon sleeve
fracture may be the first presentation of mild osteogenesis imperfecta20 (Fig. 7-12).
Also beware that the fracture may have had a much more disruptive
effect on the articular surface than is seen on plain radiographs.21,22
Displaced intraarticular olecranon fractures are managed with open
reduction and internal fixation, using either a tension band technique
or compression fixation with an interfragmentary screw. In children,
the tension band can be a strong permanent suture rather than a wire.
The K-wires can be placed percutaneously. This technique can allow you
to remove the K-wires in the clinic and leave the suture, saving the
child a hardware removal in the late postoperative period. To stay out
of trouble, use a large nonabsorbable suture.
-
Seventy-five percent of finger fractures create no problems, but 25% need prompt treatment.
-
A “tendon disruption” may instead be a physeal fracture in a young child.
-
In assessing a nerve, the “wrinkle test” is helpful in young children.
-
Check the digital cascade at rest and with tenodesis wrist motion.
-
Get a true lateral of the injured digit.
-
Beware of germinal matrix entrapped in the distal phalanx physis.
-
Be aware that a jersey finger can be dismissed as a jammed finger.
-
MRI is the best test to find an occult scaphoid fracture.
-
After an injury to
the volar plate, move the joint early. Do not do extension block
splinting because you risk contracture of the child’s PIP joint.
-
Understand remodeling to avoid overtreatment
-
Be alert that high-energy distal radial physeal fractures can lead to acute carpal tunnel syndrome.
-
Look for a “2nd injury” elsewhere in the injured upper extremity.
-
With distal radius pinning, care should be taken to avoid the radial sensory nerve and the extensor tendons.
-
To avoid a loss of
reduction, a well made cast (oval, three-point mold) is essential to
maintaining reduction. Bad casts are a big source of trouble in these
fractures. -
Put up a remodeling fracture poster in your cast room to calm anxious parents and save them second-opinion trips.
-
Growth arrest is 60% for the distal ulna: counsel families as to that fact.
-
A significant malunion of a forearm diaphyseal fracture will lead to permanent loss of pronation and supination.
-
The most common cause of upper extremity compartment syndrome today is forearm fractures.
-
Watch out for the occult Monteggia fracture.
-
Insist on two views
of the entire forearm at right angles to one another, as well as
dedicated films of the elbow to be assured that the radiocapitellar
relationship is satisfactory. -
Don’t make multiple
passes in an attempt to get the intramedullary wire across the fracture
site. If you don’t get the wire across in three attempts, it is safer
to open the fracture. -
To manage Monteggia
fractures successfully, radiograph views should include the whole
forearm, as well as isolated elbow radiographs. The ulna should be
“ruler straight.” -
If there is any
question about the relationship of the radius and capitellum during the
postoperative period, it is better to take the cast off to get good
radiographs and risk loss of reduction rather than to continue to cast
a malaligned radiocapitellar joint obscured by plaster. -
The key to managing Monteggia fractures lies in ulnar stability.
-
Pay careful attention to the radial nerve on the initial neurovascular examination.
-
Attempt a variety of different maneuvers to reduce a proximal radius fracture before resorting to open reduction.
-
With the percutaneous manipulation maneuver for radial head fractures, be certain to avoid the posterior interosseous nerve.
-
With radial head and
neck fractures, be sure to warn families at the time of injury that
loss of motion is a problem. These fractures should not be immobilized
for more than about 3 to 4 weeks. -
An olecranon sleeve fracture may be the first presentation of mild osteogenesis imperfecta.
-
In children, the tension band can be a strong permanent suture rather than a wire (and don’t use absorbable suture).
KY, Chan WS, Lam TP, et al. Percutaneous Kirschner-wire pinning for
severely displaced distal radial fractures in children. A report of 157
cases. J Bone Joint Surg Br. 1995;77(5):797-801.
A, Reis M, Molina M, Davids J, et al. Supracondylar fractures of the
humerus associated with ipsilateral forearm fractures in children: a
report of forty-seven cases. J Pediatr Orthop. 2001;21(3):307-312.
CW, Kay RM, Skaggs DL. Growth arrest of the distal radius following a
metaphyseal fracture: case report and review of the literature. J Pediatr Orthop B. 2002;11(1):89-92.
VF, Kaye JJ, Geary SP, et al. Pseudo-Volkmann’s contracture due to
tethering of flexor digitorum profundus to fractures of the ulna in
children. J Pediatr Orthop. 1998;18(4):437-440.
S, De Schrijver F, De Smet L. Radial head dislocation with plastic
deformation of the ulna in children. A rare and frequently missed
condition. Acta Orthop Belg. 2000;66(4):359-362.
PP, Haevernick B, Herold A, et al. Treatment decision, method of
osteosynthesis, and outcome in radial neck fractures in children: a
multicenter study. J Pediatr Orthop. 2005;25(1):45-50.