Trauma about the Elbow II: Other Fractures
have a well-earned reputation for complications such as nonunion, late
fracture displacement, and cubitus varus, which can most often be
avoided by early recognition and careful observation during treatment.
Soft-tissue injury is typically less severe than that seen in
supracondylar fractures, and acute neurovascular injury is uncommon.
These fractures are the second most common fracture about the elbow in
children after supracondylar fractures.
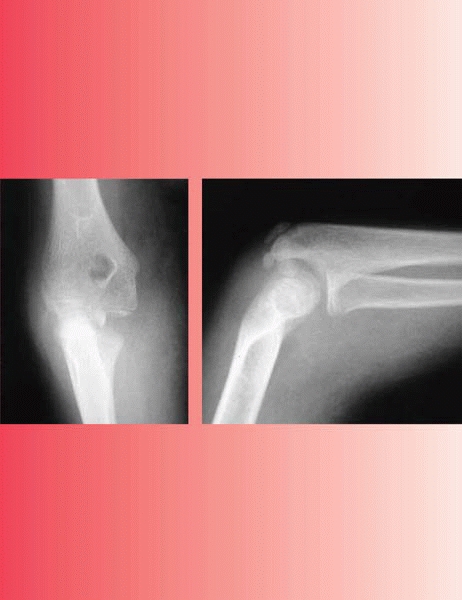
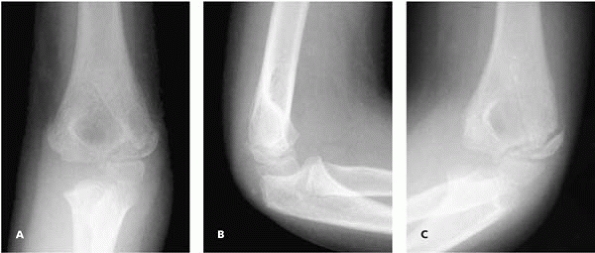
appreciating the amount of displacement of the fracture, on standard AP
and lateral radiographs of the elbow. As the plane of the fracture is
oblique, from anterior lateral to posterior medial, an internal oblique
view of the elbow usually shows the largest amount of displacement. In
addition, at times the metaphyseal fragment is such a thin wafer of
bone that it could easily be missed, and the fracture not appreciated.
 |
|
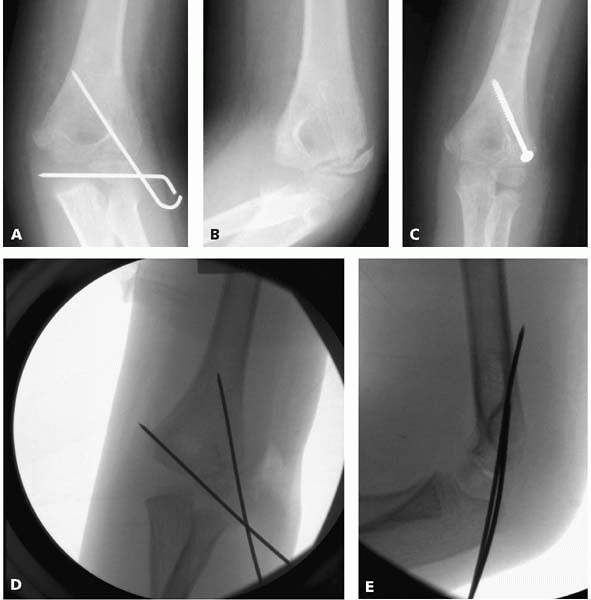
▪ FIGURE 6-1 A: AP view of a lateral condyle fracture demonstrating less than 2 mm displacement. B: Lateral view of a lateral condyle fracture demonstrating less than 2 mm of displacement. C:
Oblique view, looking at the lateral side of the elbow tangentially, showing greater than 2 mm of displacement. Without this radiograph, one may have assumed there was less than 2 mm of displacement, and treated the fracture nonoperatively. |
Salter II fracture with a lateral condyle fracture. In a lateral
condyle fracture, swelling and tenderness are predominantly in the
lateral region of the elbow. The radiographic appearance of a Salter II
fracture with a lateral metaphyseal fragment may be similar to that of
a lateral condyle fracture prior to ossification of the trochlea (see Fig. 5-6).
At times, differentiation may be made on physical exam. In contrast to
the lateral swelling and tenderness of the lateral condyle fracture,
the Salter II fracture has more swelling medially, where the periosteum
is torn, and not laterally, where the periosteum is intact. In
addition, tenderness is more diffuse with a Salter II fracture.
use in determining treatment or predicting outcome. If the amount of
maximum fracture displacement in all radiographs is ≤2 mm, then
nonoperative treatment with immobilization is indicated. Remember that
the AP and lateral views may underestimate the extent of fracture
displacement, so an oblique view is necessary (Fig. 6-1) when considering
nonoperative treatment. A prospective investigation of 112 lateral
condyle fractures with ≤2mm of displacement treated with splinting
reported that if the fracture line cannot be followed to the epiphysis,
the fracture is stable and not at risk for displacement1 (Fig. 6-2).
However, when the fracture line extended into the epiphysis, with the
lateral gap greater than the medial gap, 17% (6/35) of fractures
displaced (Fig. 6-3). When the fracture gap at the epiphysis was equal to the lateral gap, 42% (5/12) of fractures displaced (Fig. 6-4).
Thus, to stay out of trouble, pay special attention to fractures
extending into the epiphysis, and reassess these fractures with AP,
lateral and oblique views 5 to 9 days after injury to be certain
displacement has not occurred. To allow better radiographic
visualization of the fracture, fiberglass rather than plaster is
helpful, but do not hesitate to remove the cast in order to get good
quality radiographs. If it is so unstable that you are afraid to remove
the cast for a good x-ray, then it probably should be pinned.
of displacement operatively. The type of operative treatment depends on
the amount of displacement, and the integrity of the articular surface.
In young children the majority of the epiphysis is cartilage, which is
less brittle than bone. At times, the metaphyseal bone may fracture,
while the more malleable epiphyseal cartilage does not, thus leaving
the articular surface intact, acting as a hinge (Fig. 6-5).
further imaging such as arthrography or an MRI may be used to diagnose
this type of fracture. If the articular cartilage is intact, open
reduction is usually not needed, and closed reduction and pinning
should be sufficient. In cases in which one suspects the articular
surface may be intact, DLS and JMF prefer to perform an arthrogram
under general anesthesia, and if the articular surface is intact,
proceed with percutaneous pinning.
In questionable cases Dr. Beaty recommends using a gradient echo MRI in evaluating articular fractures of the elbow (Fig. 6-6).
A recent series of twelve children with lateral condylar fractures
displaced >2 mm and intact articular surfaces managed with
percutaneous pinning reported uniformly excellent results.2
If the articular surface is displaced, or if there is >2 mm of
fracture displacement, stay out of trouble and proceed with an open
reduction in this problematic fracture.
 |
|
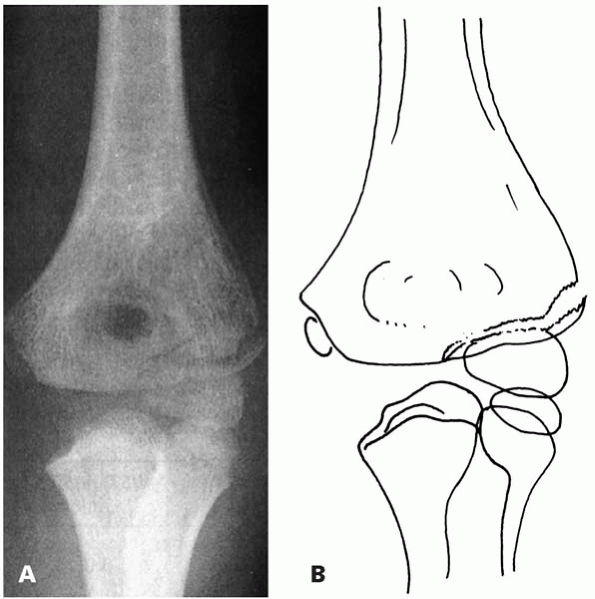
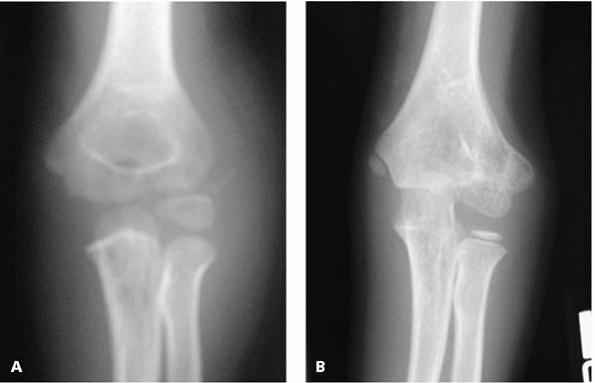
▪ FIGURE 6-2 A:
Type A fracture. Fracture through the lateral humeral condyle with a minimal gap laterally. The fracture cannot be followed to the epiphyseal cartilage. B: Outline of the radiograph. (Reprinted with permission from Finnbogason T, Karlsson G, Lindberg L, et al. Nondisplaced and minimally displaced fractures of the lateral humeral condyle in children: a prospective radiographic investigation of fracture stability. J Pediatr Orthop. 1995;15(4):422-425.) |
 |
|
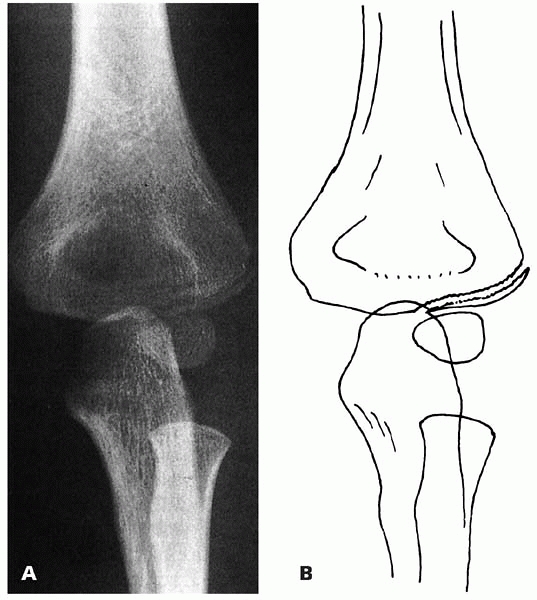
▪ FIGURE 6-3 A:
Type B fracture. Fracture through the lateral humeral condyle with a gap laterally. The fracture can be followed to the epiphyseal cartilage. B: Outline of the radiograph. (Reprinted with permission from Finnbogason T, Karlsson G, Lindberg L, et al. Nondisplaced and minimally displaced fractures of the lateral humeral condyle in children: a prospective radiographic investigation of fracture stability. J Pediatr Orthop. 1995;5(4):422-425.) |
 |
|
▪ FIGURE 6-4 A: Type C fracture. Fracture through the lateral humeral condyle. The fracture gap is as wide laterally as medially. B:
Outline of the radiograph. (Reprinted with permission from Finnbogason T, Karlsson G, Lindberg L, et al. Nondisplaced and minimally displaced fractures of the lateral humeral condyle in children: a prospective radiographic investigation of fracture stability. J Pediatr Orthop. 1995;15(4):422-425.) |
 |
|
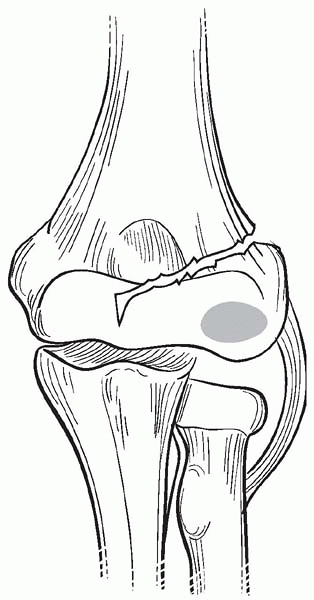
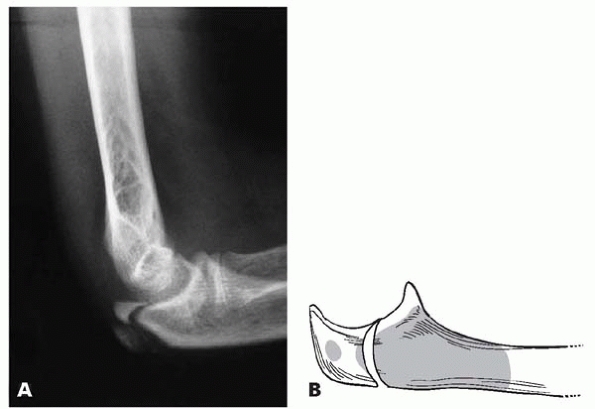
▪ FIGURE 6-5
Lateral condyle fracture may be completely through the ossified portion of the distal metaphysis, but not enter into the joint. This fracture pattern presumably occurs because of the flexible nature of the cartilaginous epiphysis. |
 |
|
▪ FIGURE 6-6
MRI of an elbow demonstrating a lateral condyle fracture in which the fracture line does not extend through the cartilage into the joint. Dr. Beaty reports that as time goes on some institutions will be utilizing MRI over arthrography in a number of cases. (Reprinted with permission from Horn BD, Herman MJ, Crisci K, et al. Fractures of the lateral humeral condyle: role of the cartilage hinge in fracture stability. J Pediatr Orthop. 2002;22(1):8-11.) |
arthrogram in this setting. First, the traditional approach for an
elbow arthrogram is via the lateral soft spot between the radial head,
olecranon, and lateral column. In the case of a lateral condyle
fracture, the anatomy of this area is distorted, and dye extravasation
in soft tissues makes visualization of the articular surface difficult,
or fracture hematoma may limit dye flow into the joint. An alternative
site for dye entry directly posterior into the olecranon fossa avoids
these problems3 (Fig. 6-7).
The second potential pitfall is mistaking dye in the olecranon fossa
for a vertical intraarticular fracture. The olecranon fossa may be
differentiated from an intraarticular fracture by rotating the arm
under live imaging.
posterior interosseous nerve and brachial artery is not too great.
Fortunately, once through superficial fascia a traumatic rent in the
wrist extensor muscle mass is usually present, which can allow one to
get to the fracture site with very little sharp dissection once through
skin. This opening may be enlarged to visualize the fracture site and
remove hematoma. To minimize the chances of avascular necrosis (AVN),
soft-tissue attachments on the posterior portion of the fracture
fragment should not be detached as the only blood supply to the lateral
trochlea and capitellum enter in the posterior nonarticular portion
(see Fig. 5-7).
 |
|
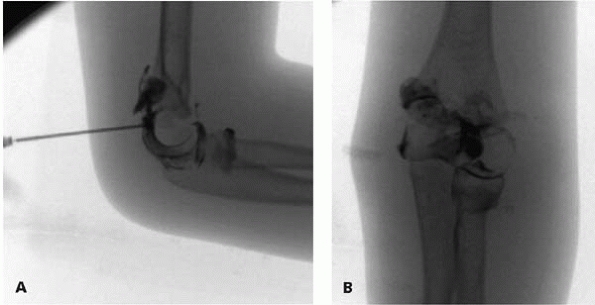
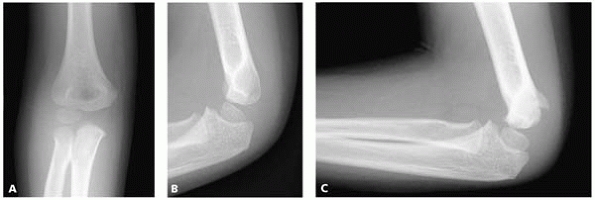
▪ FIGURE 6-7 A:
Lateral view of elbow with fluoroscopy in which an arthrogram is being performed by placing a needle into the olecranon fossa from a posterior approach. B: Anterior-posterior view of an arthrogram of the same elbow. This demonstrates that the articular surface is intact, so the fracture does not extend into the joint. Most frequently, closed pinning is sufficient when the articular surface is intact. |
and verified under direct visualization, at which time a headlight is
helpful. Dissection of about 5 mm of soft tissue from the lateral
portion of the distal fragment improves visualization of the fracture
line. Reduction can occasionally be surprisingly difficult, at which
time dorsiflexion of the wrist relaxes the wrist extensors attached to
the distal fragment and makes the reduction much easier. Two smooth
pins are placed percutaneously just posterior to the incision in a
parallel or divergent manner, and fixation stability is assessed. A
potential pitfall is having the more distal K-wire wholly in epiphyseal
cartilage, failing to engage cortex (Fig. 6-8).
 |
|
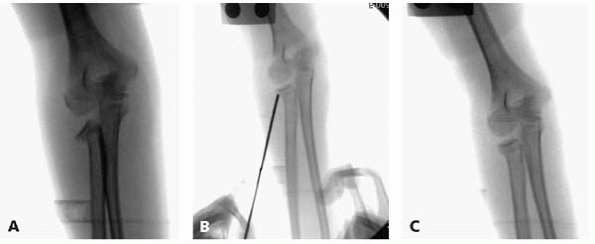
▪ FIGURE 6-8 A: Anterior-posterior radiograph demonstrating the horizontal pin failing to engage ossific bone in the proximal to the fracture. B: Ten weeks following surgery, the patient has elbow pain and stiffness, and the radiograph demonstrates a lack of union. C:
Rigid fixation with a compression screw was used at time of second surgery to allow early motion. Screw should be only in the lateral column and not in the olecranon fossa or terminal elbow extension would be compromised. D: Preferable pin configuration. Both cortices in the proximal fragment are engaged. Pins are not in the olecranon, allowing for early motion with full extension if desired. E: Lateral view showing the proximal pin exiting through the posterior cortex. This is common as the capitellum is an anterior structure, so pins may have an anterior to posterior direction. |
 |
|
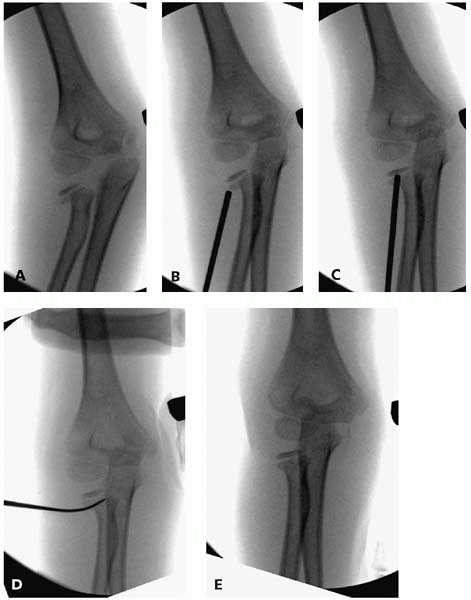
▪ FIGURE 6-9 A:
AP view of elbow of 3½-year-old boy 5 weeks following open reduction internal fixation of a displaced lateral condyle fracture. B: Lateral view of same boy at same time. C: Only the oblique view demonstrates persistent lack of callus at fracture site. Pins were kept in for 8 weeks, with eventual clinical and radiographic healing. Just as an oblique x-ray may be needed to see maximum fracture displacement at the time of injury, an oblique x-ray out of plaster may help detect a lack of healing that would have been missed on the anterior-posterior and lateral views. |
in three weeks, lateral condyle fractures occasionally require up to 12
weeks of immobilization despite pinning. A potential complication with
these intraarticular pins is pin infection with a subsequent septic
elbow, so carefully weigh the benefits versus risks of leaving pins in
longer than 3 to 4 weeks, and certainly examine the pin sites if you
choose to leave the pins in longer. Assess radiographs at 3 weeks
carefully, and do not hesitate to continue casting for more time to
help avoid a nonunion (Fig. 6-9).
duPont Hospital for Children reported that 50 of 55 patients with
lateral condyle fractures were not radiographically healed until 6
weeks of casting.4 The authors
recommended not removing pins until signs of healing. While this study
stresses the point that these fractures may heal slowly, we believe
most lateral condyle fractures can have implants removed in less than 6
weeks.
not be performed in fractures seen later than 3 weeks, as the risk of
poor results from stiffness and AVN increases. However, if one
carefully avoids posterior dissection to maintain blood supply of the
distal fragment, good results with open reduction of lateral condyle
fractures in children 8 weeks to 14 years after injury has been
reported.5
reduction in patients where extensive soft-tissue stripping would have
been required to improve the position of the fragment allowed the
surgeons in this series to avoid AVN.”5
late lateral condyle fractures is to not necessarily aim for anatomic
reduction; it is preferable to fix it where it lies with no posterior
stripping. Dr. Beaty reminds us this technique has been described as
“metaphyseal osteosynthesis in situ” in the past. These fractures are
similar to a slipped capital femoral epiphysis in that respect.
Consider rigid fixation with a screw(s) in compression in late cases to
maximize healing and early ROM, while remembering to avoid the
olecranon fossa.
appear unavoidable, but early recognition and explanation may keep you
out of trouble with parents. Cubitus varus is reported with surprising
frequency following both operative and nonoperative treatment, though
we suspect that this is usually apparent from lateral overgrowth, and
not true cubitus varus. Warn parents ahead of time that they may see a
lateral prominence when the cast comes off and the arm is atrophied. In
some cases, lateral overgrowth is clear (Fig. 6-10). Either way, assure parents it is rarely severe enough to require treatment.
 |
|
▪ FIGURE 6-10 A: X-ray at time of injury confirms previously normal growth. B: Example of lateral overgrowth following operative treatment of a lateral condyle fracture.
|
and nonoperative treatment. These seldom cause any problem other than
parental concern over the radiographs (Fig. 6-11).
condyle fractures much more frequently than supracondylar fractures.
Stay out of trouble by having a low
threshold for beginning physical therapy before too many weeks go by with poor motion. A dropout cast (Fig. 6-12) or dynamic splint can assist in gaining motion if progress in physical therapy plateaus.
 |
|
▪ FIGURE 6-11 A: Anteroposterior radiograph at time of injury. B: Lateral radiograph at time of injury. C: Osseous spur following treatment with casting for a minimally displaced lateral condyle fracture.
|
 |
|
▪ FIGURE 6-12
Drop out extension cast assists in gaining elbow extension. The cast is placed in maximum passive extension of the elbow, then the distal-dorsal quadrant is cut out of the cast to allow for more extension over time. |
injury radiographs of a child with a medial epicondyle fracture, have a
high index of suspicion for associated injuries. Simple fractures of
the medial epicondyle are extraarticular injuries with limited
soft-tissue injury, thus an elevated posterior fat pad should not be
present in an isolated medial epicondyle fracture. Gross instability of
the elbow or significant swelling of the joint suggests other injuries,
such as an intraarticular medial condyle fracture and an elbow
dislocation. The most important step in the evaluation of medial
epicondyle fractures is ruling out concomitant injury, as up to 50% of
these fractures may be associated with an elbow dislocation.
fracture associated with an elbow dislocation that has become
incarcerated in the joint, which occurs in about 15% of cases. It may
be quite difficult to see the fracture fragment in the joint, but one
should become suspicious if the ossification center for the medial
epicondyle is not appreciated after the ossification centers for the
trochlea and/or olecranon is present. Remember, the order of
ossification (see Fig. 5-1) is capitellum,
radial head and/or medial epicondyle, trochlea and/or olecranon, and
lastly the lateral condyle. Arthrography, MRI or CT may help diagnosis
this injury if needed.
isolated fractures should be treated conservatively. Three weeks of
protection, with possible mobilization after the first week should lead
to good results. Controversy surrounds the treatment of the displaced
medial epicondyle fractures. To stay out of trouble with displaced
fractures, make certain the parents are well informed about the above
controversies, risks and benefits of nonoperative vs. operative
treatment before their child has a fibrous nonunion and the second
opinion says it would have healed correctly if initially treated
surgically. Long-term studies report that
regardless
of displacement, medial epicondyle fractures may be treated
conservatively with virtually no functional limitations, though the
radiographic finding of fibrous union is common.6
Studies comparing operative treatment to nonoperative concluded that
children treated surgically will have better radiographs (better
reduction and higher union rate), though more minor symptoms than those
treated conservatively.7 The
literature does not suggest that there is a threshold of displacement
above which operative therapy leads to improved outcome over closed
treatment.
the opinion that displaced medial epicondylar fractures should be
treated operatively to avoid the possibility of late valgus
instability, particularly in patients who will be placing abnormal
valgus stress across the elbow, such as baseball pitchers or gymnasts.
The only two absolute indications for operative treatment of medial
epicondyle fractures are an irreducible incarceration of the medial
epicondyle in the joint and an open fracture. Partial ulnar nerve
injuries should recover with closed fracture treatment. In the rare
case of a complete ulnar nerve injury, exploration should be considered
as the nerve may be wrapped around the fracture fragment.
incarcerated within the elbow joint following either spontaneous or
supervised reduction of a dislocated elbow. One trick to help avoid
this is to verify that the ossification centers of the elbow are
occurring in the proper order (see Fig 5-1).
If the trochlea and olecranon centers are present (which ossify at 8 to
9 years old), but the medial epicondyle (ossifies at 4 to 5 years old)
is not in its proper place, be suspicious of an incarcerated medial
epicondyle fracture and look in the joint (Fig. 6-13).
 |
|
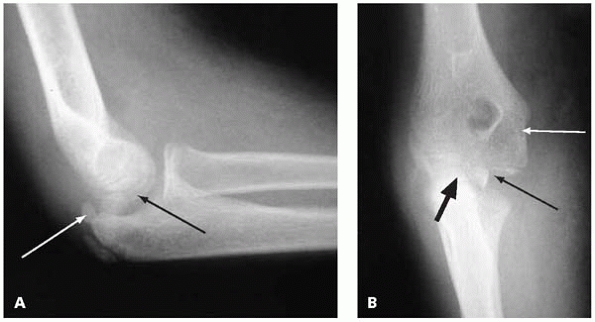
▪ FIGURE 6-13 A: Lateral view of elbow demonstrating an incarcerated medial epicondyle (black arrow) following spontaneous reduction of a dislocated elbow. Note that the olecranon apophysis is ossified (white arrow), suggesting the child is skeletally mature enough that the medial epicondyle should be ossified and visible on the AP view. B: Anteroposterior view of same elbow. Note that the trochlea is beginning to ossify (thin black arrow), suggesting the medial epicondyle should be visible, but is absent from its anatomic position (white arrow). The mystery is solved by identifying the medial epicondyle in the joint (thick black arrow).
|
closed means by opening the elbow with valgus stress, while extending
the wrist to place tension across the wrist flexors whose origin are on
the epicondyle. This maneuver should be performed gently with the
patient under general anesthesia. If unsuccessful, an open reduction
with internal fixation is necessary while protecting the ulna nerve.
When an open reduction is chosen, consider rigid fixation with a screw
to allow early motion, but warn the family this almost always is
prominent and requires later removal.
screw up the medial column, and not across the olecranon fossa, which
will limit elbow extension. Remember that this is different from
supracondylar and lateral condylar fractures, in which pins can be
placed across the olecranon fossa, but are removed at fracture healing.
posterior cortex (or any other cortex) and the bone is so hard that the
threads can shear off, causing a pigtail of metal to lodge in the
bone—that requires a long explanation to the parents.
olecranon fractures in children. The first is missing another fracture,
as most series report more than half of all olecranon fractures are
associated with another fracture about the elbow.8
The second pitfall to avoid is failing to recognize displacement of the
fracture during the course of treatment by cast immobilization.
Particularly at risk for displacement is the flexion-type fracture in
which the posterior portion of the olecranon fails in tension, and the
fracture line proceeds to the articular surface. If complete, this
fracture is potentially unstable as the torn posterior periosteum
cannot function as a tension band, and the pull of the biceps and
triceps may further displace the fracture over time. If closed
treatment is chosen, good quality radiographs at about one week after
injury are indicated to assess possible displacement.
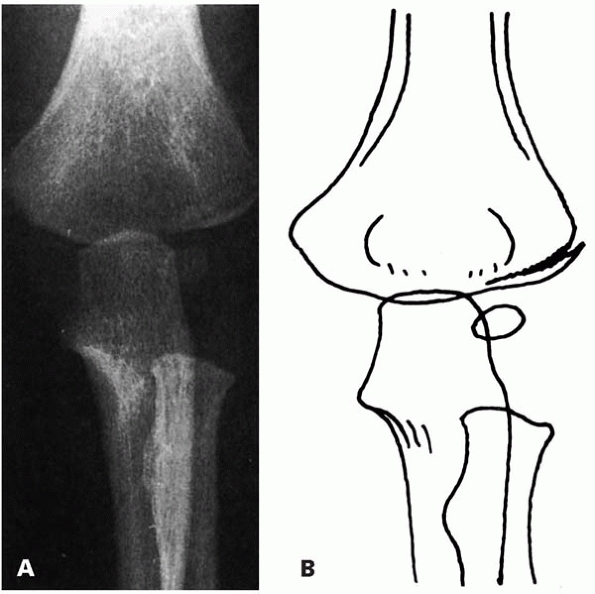
olecranon fracture that is almost pathognomonic for osteogenesis
imperfecta. This fracture is an avulsion of the proximal ulnar
metaphysis, and following one fracture, is eventually bilateral in 70%
of children with osteogenesis imperfecta. Most fractures require
operative treatment, and re-fracture is not uncommon (Fig. 6-14).9
 |
|
▪ FIGURE 6-14 A:
Lateral radiograph of 12-year-old boy with Type IA osteogenesis imperfecta demonstrating a characteristic olecranon fracture seen in children with osteogenesis imperfecta. B: Drawing shows characteristic fracture pattern involving the olecranon observed in children with osteogenesis imperfecta. (Reprinted with permission from Zionts LE, Moon CN. Olecranon apophysis fractures in children with osteogenesis imperfecta revisited. J Pediatr Orthop. 2002;22(6):745-750.) |
of elbow loss of motion is not as severe as in adults, so we usually
place the child in a long arm cast following open reduction and
internal fixation of olecranon fractures. Thus, the tension band can be
strong suture rather than wire, and the K-wires can be left
percutaneous. This technique obviates the need for return to the
operating room for hardware removal.
loss of supination and pronation, often in spite of correct treatment.
This should be discussed at the first visit with the parents, and
clearly limit expectations for a full range of motion.
common with proximal radius fractures, and missing a second fracture or
dislocation is a potential pitfall. A valgus injury may cause an
associated medial epicondyle avulsion or olecranon fracture. Proximal
radius fractures are also associated with posterior elbow dislocations,
with the radial head displacing anteriorly if the fracture occurs
during the dislocation, or posteriorly if the fracture occurs during
relocation. Fractures of the proximal radius in children tend to
involve the metaphyseal neck, or less commonly the physis (Salter type
I or II), rather than the head as seen in adults.
overlooked on radiographs, with only one cortex in one radiograph
showing too sharp of an angle where there should be a gentle curve. A
subtle radial neck fracture may be present without elevation of the
posterior fat pad as it may be extracapsular. There are two potential
radiographic fakeouts. First, the radial head is normally angulated up
to 15 degrees valgus, and thus is not necessarily perpendicular to the
diaphysis of the radius. Second, a bipartite ossification center may be
mistaken for a fracture. The physical exam is often quite helpful in
diagnosing subtle fractures, as tenderness is well localized in
isolated, nondisplaced fractures. Pronation and supination are usually
more painful than elbow flexion and extension when a proximal radius
fracture is present.
pronation and supination. The importance of early motion and physical
therapy should be discussed with the family at the first visit to help
ensure compliance. Good results can be expected in fractures with less
than 30 degrees angulation and less than three millimeters of
translation. It is generally recommended that fractures with greater
angulation or translation undergo an attempted reduction.
as it may help reduce scarring and maximize range of motion. One closed
reduction technique that appears particularly effective is the Israeli
technique: flex the elbow to 90 degrees, and apply direct pressure over
the radial head with your thumbs, while rotating the forearm between
full supination and pronation. We believe that the patient’s range of
motion is a more important criterion for the acceptability of reduction
than radiographic appearance, though support in the literature for this
opinion is lacking.
degrees after attempted closed reduction, percutaneous reduction may be
attempted by various maneuvers.
We
have had good results with a percutaneous K-wire, which is a simpler
technique than it looks. A few technical points are worthy of mention
with this technique.
-
Enter the K-wire into the skin at least 8
cm distal to the radial head, to allow a proximally directed force that
frees the fracture fragment. -
Using the sharp end of the wire is useful
to pierce skin, but use of the blunt end of the wire to push the
fracture fragment provides more pushing power as the sharp end may
simply penetrate the bone. -
Rotate the forearm until the maximum displacement of the fracture is visualized, and perform the reduction using that view.
-
Be cognizant of the small chance of
injuring the posterior interosseous nerve, with supination of the
forearm bringing the nerve posteriorly and under less tension (Fig. 6-15).
If percutaneous reduction with a K-wire is inadequate, consider making
a 4-mm incision and inserting a Freer elevator to lever the fragment in
place (Fig. 6-16). In the very young child
prior to robust ossification of the radial head, an arthrogram may help
in visualization and manipulation of the proximal radius (Fig. 6-17).
stable from locking interdigitations. In the rare case that internal
fixation is needed, avoid trouble by not placing a transcapitellar
K-wire, which have been known to break. Excision of a radial head
should be avoided at all cost at initial treatment in the immature
skeleton as synostosis, cubitus valgus and ulna deviation of the wrist
may develop.
 |
|
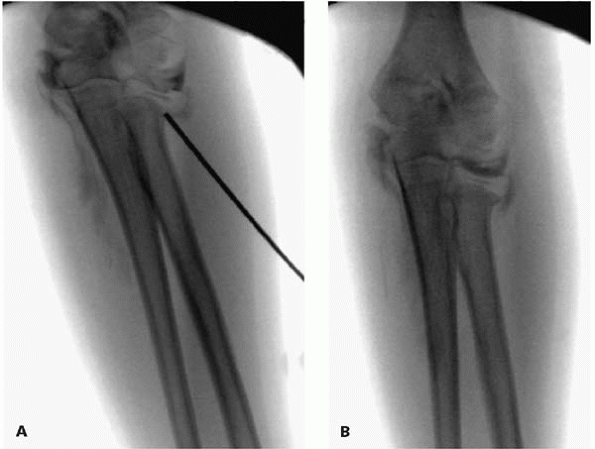
▪ FIGURE 6-15 A:
Displaced radial neck fracture in an 11-year-old girl. Attempts at closed reduction have failed. Rotate the forearm until the maximal displacement of the fracture is seen, and keep this position to visualize the reduction. B: A 2.4-mm K-wire is inserted proximal to fracture, then the blunt end of the wire is used to push the fracture fragment free. C: Final image showing near anatomic reduction. At this point, the patient had 80 degrees of pronation and supination. |
complication is a loss of pronation and supination. Loss of range of
motion may be minimized by early motion. Fractures not needing
reduction may begin active motion at about day 7 to 14; those requiring
reduction may postpone motion for 2 to 3 weeks. Both groups should be
protected with a splint for 3 weeks, and allowed out for motion
exercises. We suspect that as computer keyboards become more
ubiquitous, pronation will be more important than supination. For this
reason, casting in mild pronation is reasonable.
but pitfalls in this condition are worthy of mention. Over half of
posterior elbow dislocations are associated with other fractures, most
commonly the medial epicondyle, radial head and neck, and the coronoid
process. Following a stable reduction of a dislocated elbow, expect a
fairly large arc of motion without severe pain; if there is no motion
or severe pain with little motion, look for a fracture, particularly an
incarcerated medial epicondyle fracture (see Figs. 6-13A and B).
 |
|
▪ FIGURE 6-16 A: Injury film of a 6-year-old girl with a radial neck fracture. B: Attempting percutaneous reduction with a K-wire. C: Even when using the blunt end of the K-wire, the K-wire may become lodged in the bone, with incomplete reduction. D: Through a 4-mm incision a freer elevator can be used to lever the fracture fragment into place. E: Reduction with minimal dissection was possible.
|
 |
|
▪ FIGURE 6-17 A:
In the young child with little ossification of the radial head, an arthrogram may prove useful in visualizing the proximal radius during reduction. B: Same patient as in A, following reduction. |
careful pre- and postreduction neurologic exam is essential. Any
postreduction nerve deficit not recognized before reduction should be
considered an entrapped nerve until proven otherwise with an MRI or
surgical exploration. A median nerve deficit after reduction of an
elbow dislocation associated with a medial epicondylar fracture has
been well described.10
rare, as the physes tend to fail before the ligaments. Prior to
ossification of the capitellum, an injury with the radiographic
appearance of an elbow dislocation is most likely a transphyseal
fracture, and usually requires pinning. The diagnosis may be confirmed
with an intraoperative arthrogram (Fig 6-18). For further discussion of transphyseal injuries, see Chapter 5.
 |
|
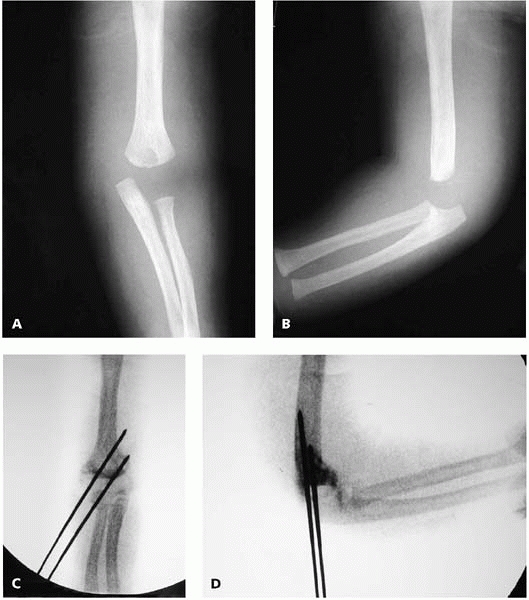
▪ FIGURE 6-18 A:
Anteroposterior radiograph of a 4-month-old boy. As there are no secondary ossification centers visible, a diagnostic pitfall is to call this an elbow dislocation. B: The lateral view may be similarly misinterpreted as an elbow dislocation. C, D: Arthrogram confirms diagnosis of transphyseal fracture, and aids in visualization of fracture during reduction and pinning. |
-
Lateral condyle fractures are intraarticular and need anatomic reduction for union and long-term good outcome.
-
With lateral condyle
fractures, at presentation and healing, internal oblique radiographs
often show a larger fracture displacement than the anterior-posterior
and lateral radiographs. -
Do not dissect posteriorly.
-
Prolonged casting may be needed.
-
Have a low threshold for radiographs out of plaster if loss of reduction is suspected.
-
Medial epicondyle fractures rarely require surgery, but discuss controversy with family at initial visit.
-
Proximal radius fractures are at great risk for loss of pronation and supination; warn parents at initial visit.
-
Begin early motion in elbow fractures when possible.
-
With olecranon and proximal radius fractures, as well as elbow dislocations, look for associated injuries.
T, Karlsson G, Lindberg L, et al. Nondisplaced and minimally displaced
fractures of the lateral humeral condyle in children: a prospective
radiographic investigation of fracture stability. J Pediatr Orthop. 1995;15(4):422-425.
P, Potenza V, Caterini R, et al. Long-term results of treatment of
fractures of the medial humeral epicondyle in children. J Bone Joint Surg Am. 2001;83-A(9):1299-1305.
SB, Crawford AH. Median nerve entrapment after dislocation of the elbow
in children. A report of 2 cases and review of literature. Clin Orthop Relat Res. 1995;(312):232-237.
S, Vaishya R, Klenerman L. Management of radial neck fractures in
children: a retrospective analysis of one hundred patients. J Pediatr Orthop. 1993;13(2):232-238