Staying Out of Trouble with the Hip: Legg-Calvé-Perthes, Slipped Capital Femoral Epiphysis, and Transient Synovitis vs. Septic Arthritis
– Spine and Hip > 22 – Staying Out of Trouble with the Hip:
Legg-Calvé-Perthes, Slipped Capital Femoral Epiphysis, and Transient
Synovitis vs. Septic Arthritis
Legg-Calvé-Perthes, Slipped Capital Femoral Epiphysis, and Transient
Synovitis vs. Septic Arthritis
|
|
(AVN) of the capital femoral epiphysis in a young child. The condition
tends to run a fairly predictable time course. It affects both hips in
about 10% of cases and is much more common in boys (about 4 to 1).
Children with Legg-Calvé-Perthes disease most commonly present between
the ages of 4 and 8 years, but the condition may be seen in children
less than 2 years old and as old as skeletal maturity. Most of the
trouble with Legg-Calvé-Perthes disease revolves around making the
diagnosis, dealing with the parents, and being selective about surgical
treatment. Without careful selection, the orthopaedist can get into
trouble by overtreating the young or the mildly affected, or the
untreatable severe cases, or conversely, get into trouble by missing
the more involved older child who would really benefit from surgical
management (Fig. 22-1).
diagnosis of Legg-Calvé-Perthes is to recognize that the presentation
can be very subtle and may be mistaken for transient synovitis in the
early stages.1 The most common experience of
the orthopaedist at diagnosis is a mom who says “I notice a slight limp
at the end of the day, but he wasn’t complaining of pain.”
 |
|
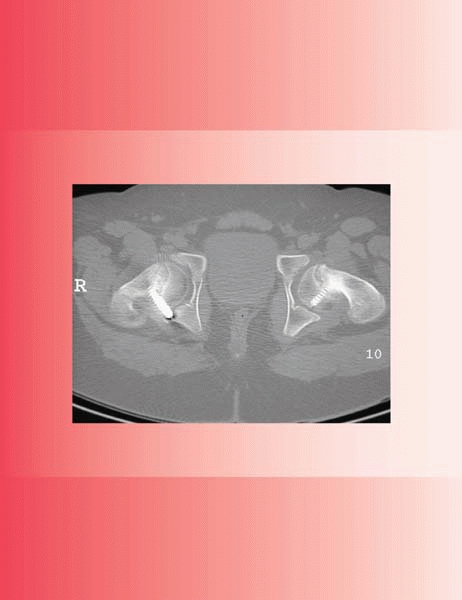
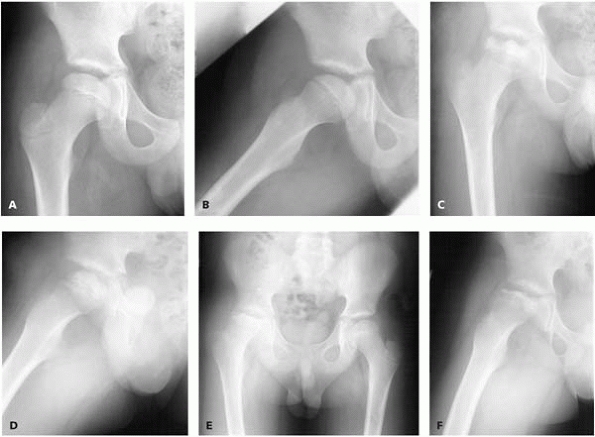
▪ FIGURE 22-1 An 11-year-old boy presented with Perthes involving the entire femoral head (A,B).
His prognosis is poor. Although it may be premature to assign a Herring type, it is not too early to intervene. No treatment was offered. (C,D) Six months later, the hip is still contained. Most would call it a Herring B/C. No treatment was offered. (E,F) Now 10 months after presentation, there is subluxation. He has very little motion. Now the family was offered surgical management. Could the surgeon have stayed out of trouble with surgical management at presentation? |
-
Transient synovitis
-
Septic arthritis
-
Sickle cell disease
-
Osteomyelitis of the femoral neck
-
Chondrolysis
-
Gaucher diseases/Mucopolysaccharidosis
-
Juvenile rheumatoid arthritis
-
Multiple epiphyseal dysplasia
-
Spondyloepiphyseal dysplasia
-
Myers dysplasia
be a subtle asymmetry in hip motion, typically a loss of hip abduction
and/or internal rotation. In a young child in the early stages of the
disease, the examiner should carefully control the pelvis during
examination to avoid missing subtle asymmetry between the hips.
flexion contracture and a positive Thomas test. Contracture or spasm of
the adductor tendon can also be seen. Just as it is easy to miss a
subtle loss of hip motion, it is easy to miss gait abnormalities early
in the condition. If there is a subchondral fracture or a hip effusion,
the child may walk with either an antalgic gait or with the foot
somewhat externally rotated. Later in the condition, the child may
develop a Trendelenburg gait and have a Trendelenburg sign.
frog lateral plain radiograph at the first visit for any child who
presents complaining of hip or thigh pain.
pelvic shift to obliquity on frog lateral. If there is no synovitis,
the pelvis will be level. If there is a synovitis, the pelvis is
shifted to the affected side because the x-ray technician is trying to
abduct that side but since the hip won’t abduct, the child elevates
that pelvis and it appears “catawampus,” or out of line. Beware of the
appearance of joint effusion, which might be evidence of early growth
failure or growth of the femoral head. Be aware that even high-quality
plain radiographs may be normal at the first visit.
involvement of the femoral epiphysis, paying particular attention to
the lateral pillar, which increasingly has been shown to be a key for
prognosis. Advanced imaging, such as technician 99 bone scan or MRI,
are not typically ordered when a child presents with Perthes. If the
differential diagnosis is concerning and the physician needs to search
for the source the hip or thigh pain, a bone scan, especially with pin
hole views, can be a good locator.
head involvement early in the disease process. However, some believe
that the MRI will exaggerate the involvement without contributing
significantly to the treatment decision.
controversial, and has been dominated in the past more by personal
preference and local customs than good
data.
There are several keys to staying out of trouble when treating Perthes.
First, it is important to understand how much the concept of a “dead
hip” terrifies parents. Parents who present to you, especially for a
second opinion, can be bewildered by information on the Internet and
the multiple varying opinions that they get from experienced “experts.”
To stay out of trouble, you will need more time with these families to
explain the pathophysiology of the condition, the expected time course,
and the limited amount of long-term natural history and treatment data.
It is disconcerting to families to learn how little we know about this
condition. The recent publication of better studies2,3
has shown us that staying out of trouble means more than adhering to
the time-honored principles of just motion and containment.
attention on children 8 years and older, and on those with moderate hip
involvement (Herring B, or B/C). Surgeons and children get in trouble
when a complication occurs in the process of overtreating one of the
60+% of children who would do perfectly well without ever seeing a
doctor.
boy or girl with Legg-Calvé-Perthes can create trouble for the family
and the doctor. Children less than 6 or 7 years are usually not
coordinated enough to be able to use crutches. Even children old enough
to use crutches cannot be expected to be completely compliant with
them. Therefore, when resting the hip seems important, many prefer to
use abduction (Petrie casts) (Fig. 22-2) for a
period of 6 weeks, followed by physical therapy to work on hip and knee
range of motion. To stay out of trouble with Petrie casts, be careful
to pad carefully around the Achilles tendon, as this is a common site
of cast pressure sores. Also, prepare the family for a child who is
difficult to transport and move around the house.
 |
|
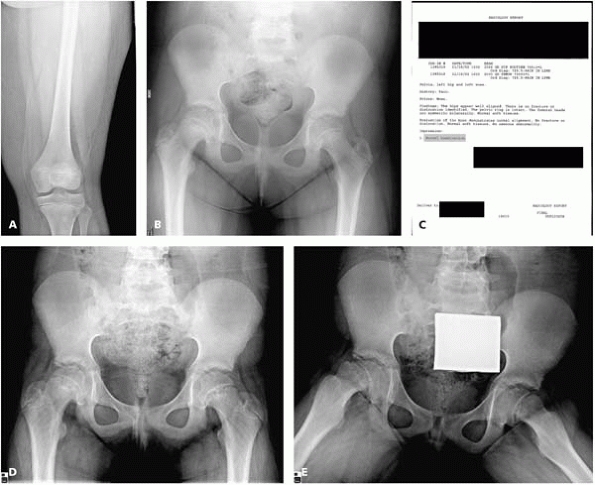
▪ FIGURE 22-2
Petrie casting. Many consider it a good way to rest the hip and gain motion. This picture demonstrates two problems: the left hip is not abducted in relation to the pelvis, and transportation can create trouble for families. |
are certainly several areas that can be sources of trouble for any of
the operations: shelf arthroplasty, Salter osteotomy, or varus
derotational osteotomy (VDRO). Each of these surgical options has one
or more champions who promote it as the best option for most kids. Each
method has pros and cons and sources of trouble (see next page). A
common theme for any procedure is to avoid surgery on a very stiff hip.
-
Don’t do a shelf arthroplasty if there is hinge abduction.
-
Don’t put too much bone anteriorly. This may block hip flexion.
-
Build the shelf flush on the hip capsule and make it substantial, or all of your shelf may reabsorb (Fig. 22-3) over the first two years after surgery.
-
After a shelf arthroplasty, beware of
putting the child in a spica cast for 6 weeks. A spica can create a
spectacular hip flexion contracture that can be slow to resolve. For
this reason, a Petrie cast is better as it allows some hip
flexion/extension but still will protect the shelf as it heals down to
the capsule of the hip.
 |
|
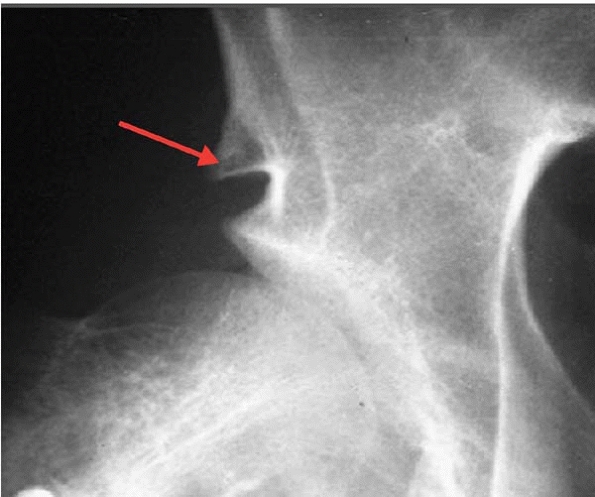
▪ FIGURE 22-3 This magnified AP radiograph shows the remnants of a shelf that has almost completely resorbed (arrow).
The bone graft was inserted too high above the subchondral bone of the acetabulum, so it saw no stress. (Case courtesy of R. Bowen, MD.) |
-
Be certain the child has full hip motion preoperatively, and use an arthrogram to check that the hip is congruent.
-
Salter osteotomy is better early in the diagnosis, not during the late remodeling stages.
-
Be certain not to block hip flexion with your osteotomy.
-
Warn the family preoperatively that either real or apparent limb shortening may be seen postoperatively.
-
Be certain the child has full hip motion, and use an arthrogram to check that the hip is congruent.
-
Do the osteotomy fairly early after the diagnosis, not during the remodeling stage.
-
Warn the family that a valgus osteotomy may be needed later to improve hip abduction.
-
Do not create too much varus. Keep the
neck shaft angle at 115° (or more) or the child will limp for a long
time (warn the parents!).5
| Age of Onset | |
|---|---|
| Before 8th Birthday | After 8th Birthday |
| Treat symptomatically Reduce activities Determine lateral pillar Out of organized activities Limited running and jumping NSAIDS prn 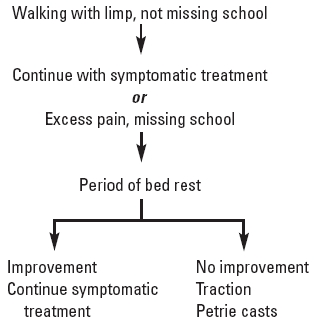 |
Treat symptomatically until classification is determined A, C: treat symptomatically B, B/C border: do Salter or VDRO |
one adolescent hip disease, estimated at 1 per 10,000 in the United
States, and is probably increasing with the epidemic of pediatric
obesity. About 80% of the cases occur during the adolescent growth
spurt (at approximately 12 years old for girls and 13.5 years old for
boy). The condition is said to be more common in obese African American
boys, and more common on the left side. One key to staying out of
trouble with SCFE is to recognize the child who is an outlier in terms
of these demographic criteria. If the child is not in the typical age
range, consider a possible underlying cause such as renal
osteodystrophy, hypothyroidism, panhypopituitarism, and hypogonadal
conditions.
some experts believe that up to 60 to 80% are bilateral, many being
silent cases that are not discovered until much later. Perhaps the
greatest source of trouble with SCFE is a delay in diagnosis (Fig. 22-4). In one series, the mean time from first seeing a physician until the correct diagnosis was nearly 4 months.6 Remember that in SCFE associated with renal failure, the SCFEs are bilateral in 95% of cases.7
It is also important to remember that the age at the time of
presentation of SCFE is predictive of whether a contralateral SCFE will
occur.8,9
 |
|
▪ FIGURE 22-4 This 9-year-old girl presented to her primary care doctor with a 4-month history of left hip and knee pain. He obtained knee (A) and hip (B)
films, but relied on the radiologist to detect a problem. Unfortunately for the child and doctor, the radiologist read the films as “normal examination” (C). The child was finally referred to the pediatric orthopaedist two months later. There is now a moderately displaced SCFE bilaterally (D,E). |
to target the primary care audience. The authors determined that
patients who present with primarily knee or distal thigh pain, patients
with Medicaid coverage, and patients with stable slips have longer
delays in diagnosis of SCFE.
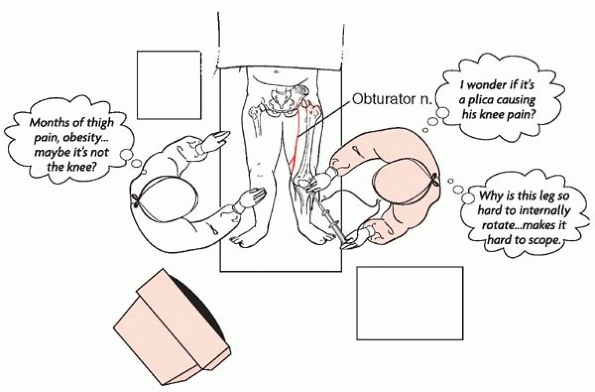
there are plenty of anecdotal stories about orthopaedic surgeons
missing the diagnosis. These include stories in which the surgeon first
thinks of SCFE while trying to get the externally rotated hip into the
leg holder for a knee arthroscopy, or worse, discovering a SCFE at one
of the knee arthroscopy postop visits (Fig. 22-5).
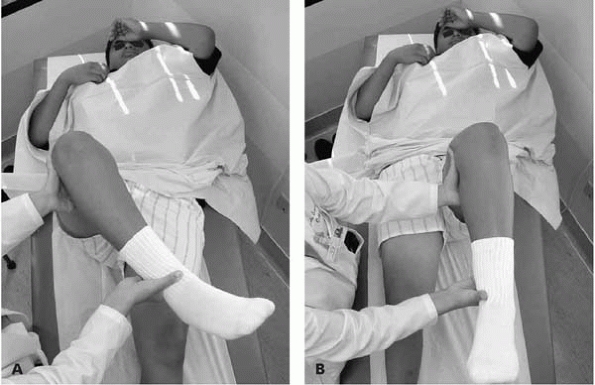
On physical examination, these children will often have an abductor
lurch or an antalgic gait. The foot is usually externally rotated. On
the table-top exam, the patient will demonstrate obligate external
rotation and abduction with attempts to flex the hip (Fig. 22-6). To stay out of trouble, recognize
the signs of an acute unstable SCFE. Children will not be able to walk
and may have pain just with gentle log rolling of the hip. This is
considered by many to be an orthopaedic emergency.
 |
|
▪ FIGURE 22-5
“It’s an SCFE, Stupid!!”—SCFE can present as knee pain instead of hip pain. The reason this is thought to occur is that the obturator nerve picks up the inflammation around the hip and refers the pain to the medial thigh. If the physician examines the knee instead of the hip, the child may be subjected to unnecessary knee arthroscopy when in fact the proper diagnosis is SCFE in the hip. |
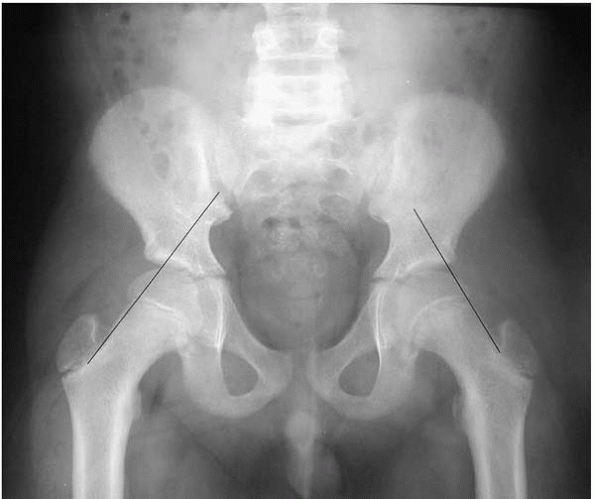
a source of trouble with SCFE. An AP and frog lateral of both hips
should be obtained. Although some believe that the true lateral
radiograph is more sensitive, it is much harder to obtain in a morbidly
obese adolescent with hip pain. Often, the AP view will show important
signs of a mild SCFE for the careful observer, such as subtle physeal
widening, a break in Klein’s line (Fig. 22-7) or a decrease in femoral epiphyseal height of the involved side compared to the opposite side.
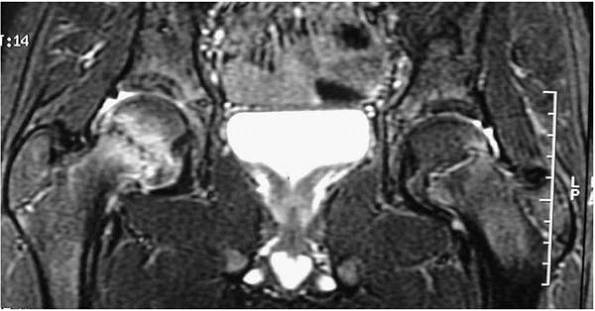
rarely necessary in SCFE. In some select cases, when there is a very
high clinical suspicion, but no confirming evidence on good quality
plain radiographs, an MRI can be helpful to
make the diagnosis12 (Fig. 22-8).
The surgeon should look for edema on either side of the physes. Other
signs on MRI may be slight widening of the physes and a hip effusion.
Beware, however, that an obese adolescent with a hip effusion could
certainly have some other condition.
 |
|
▪ FIGURE 22-6 In this boy with a right SCFE, the examination demonstrates obligate external rotation as the hip is flexed (A). No rotation with hip flexion on the normal side (B).
|
 |
|
▪ FIGURE 22-7
Using Klein’s line will help keep you out of trouble. The line drawn along the superior neck on the AP radiograph intersects less epiphysis on the left (SCFE) side. |
physis before more epiphyseal displacement occurs and avoid AVN or some
procedure or hardware-related complication. There is general agreement
that an unstable SCFE should be treated as an emergency, and admitted
and operated on as soon as possible. Stable SCFEs should be treated
promptly as well. Every institution has stories about mild stable SCFE
patients who went home for the weekend and had significant progression.
surgeon should aim to have a screw (7 mm or bigger) into the center of
the femoral head on every radiographic view, perpendicular to the
physis, stopping about 5 mm from the subchondral bone of the epiphyseal
articular cartilage. To stay out of trouble, avoid the posterior,
superior portion of the femoral head where the blood supply enters the
epiphysis. If you are going to miss in one direction or another, miss
with your screw inferior to the center of the head.
of trouble. You should be able to clearly visualize the femoral head on
both the AP and lateral views. Many surgeons have discovered that it is
easier to obtain good visualization of the
femoral head on the lateral view in an obese adolescent using a radiolucent table.13
The same visualization can be very difficult on the fracture table.
Using the radiolucent table is a somewhat more demanding technique,
because it is easy to bend the guide pin as the hip is taken into the
frog lateral position. In very obese kids, an arthrogram can help to
keep you out of trouble.14
 |
|
▪ FIGURE 22-8
An MRI is rarely needed, but can keep you out of trouble on the most questionable cases. This image of a child with a right early SCFE shows slight physeal widening and edema on both sides of the physis. (Case courtesy of L. Wells, MD.) |
 |
|
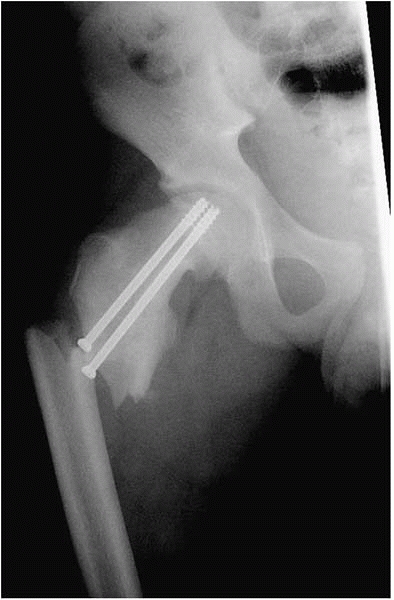
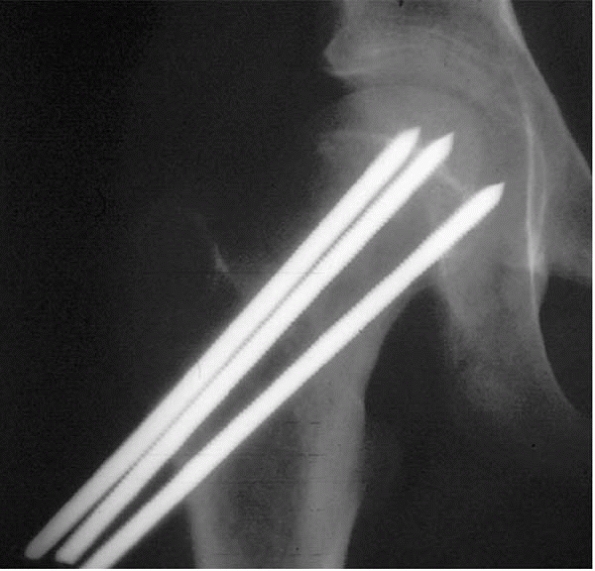
▪ FIGURE 22-9
This SCFE was stabilized using an adult hip fracture technique, with a very low subtrochanteric starting point for two screws. The screws were not perpendicular to the physis, and they created a stress riser leading to a subtrochanteric fracture. |
entering the anterior femoral neck as proximal as is necessary in order
to place the guide in perpendicular to the physes. If you use the same
technique as for pinning an adult hip fracture, you may not be
perpendicular to the physis and you risk subtrochanteric fracture (Fig. 22-9).
Such recommendations, however, can lead to several sources of trouble
in severe SCFEs. As the entry site for the screw gets closer and closer
to the physis, there is less metaphyseal bone of the femoral neck to
hold the screw. This can lead to cut out of the screw, progression of
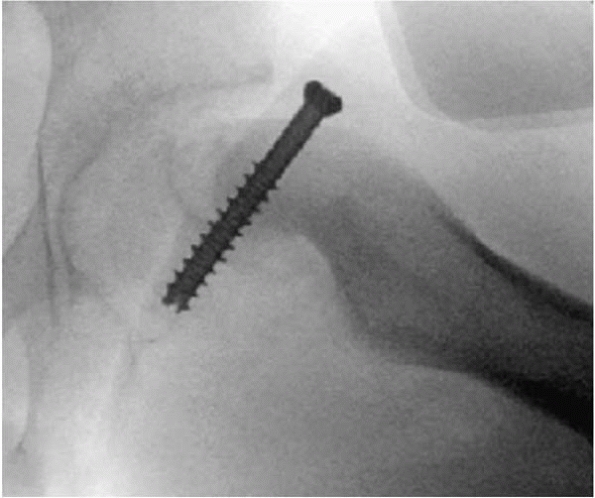
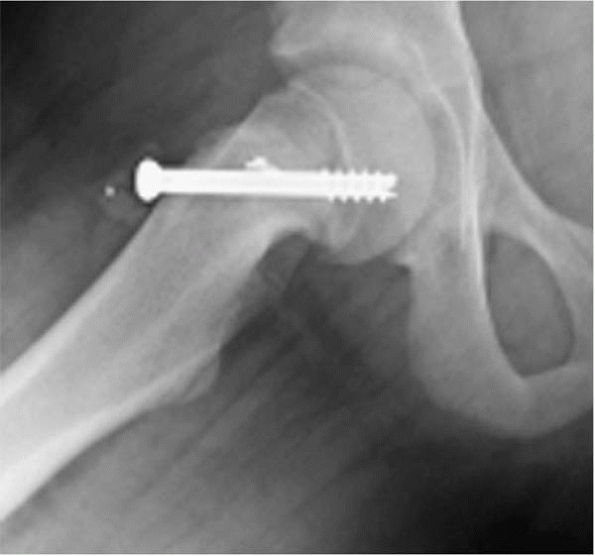
the slip after pinning, or femoral neck fracture.15 Likewise, the anterior screw can also abut against the edge of the acetabulum (Fig. 22-10) during flexion and extension, leading to damage. Hard bone can be a problem as well (Fig. 22-11).
In chronic SCFE, the bone just distal to the physes can become very
dense, as the region is subjected to high shear forces during the
progression of the slip. When drilling your guide pin, don’t allow it
to stop in this dense bone: it can be very difficult to restart the
guide pin. Judicious use of live fluoroscopic imaging and continuous
drilling can avoid this problem. In most cases, it is unnecessary to
overdrill the guide pin. However, if you like to overdrill, be very
alert that any bend in the pin could lead to shearing of the pin during
over drilling. Robb, et al.16 described six cases in which the guidewire was damaged by the cannulated drill (Fig. 22-12).
In five of those cases, the wire broke off within the femur. The broken
wire was retrieved in two of the cases but not in the remaining three.
Although there is controversy about how far the screw should be across
the physis, most experts and studies recommend 4 to 5 threads into the
epiphysis. One recent study17 found
that slip progression is inversely related to the number of screw
threads engaging the epiphysis on the postoperative frog-leg lateral
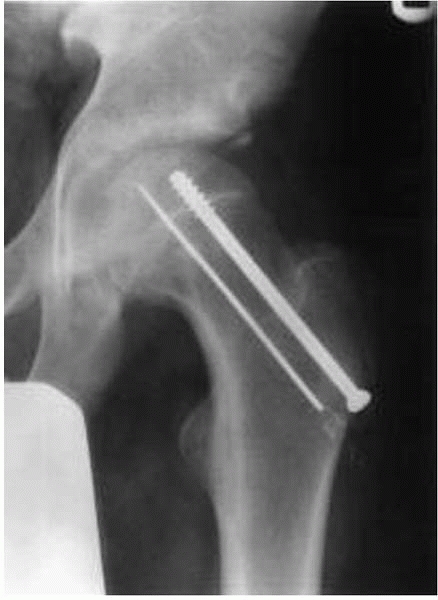
radiograph. Finally, after the screw is in place, it is essential to be
certain that the most proximal tip of the screw is not in the joint
itself. Use of the approach and withdrawal technique can assure proper
screw positioning at the end of the case (Fig. 22-13).
 |
|
▪ FIGURE 22-10 This screw was left a little proud, and it abuts the acetabulum when the hip is flexed. (Case courtesy of R. Davidson, MD.)
|
 |
|
▪ FIGURE 22-11
Obese teenagers can have extremely hard bone. This image demonstrates a metal fragment adjacent to the screw. The fragment was the thread of the first attempted screw that unraveled in the hard bone of the calcar portion of the femoral neck. (Case courtesy of R. Davidson, MD.) |
 |
|
▪ FIGURE 22-12
A shearedoff guidewire in SCFE. Overdrilling is preferred by some, but this is the downside. (Reprinted with permission from Robb JE, Annan IH, Macnicol MF. Guidewire damage during cannulated screw fixation for slipped capital femoral epiphysis. J Pediatr Orthop B. 2003;12(3):219-221.) |
trouble in atypical SCFEs. If the SCFE is related to renal
osteodystrophy, the keys are combined medical management and surgery
with custom-machined pins preventing slip progression while allowing
continued physeal growth.18 Warn
parents of children with Down syndrome that there is a much higher
incidence of AVN in Down kids, and look for hypothyroidism.19,20
Because most patients experience a rapid relief of their preoperative
symptoms, the surgeon should carefully look for problems if the patient
returns for a followup visit and there is persistent hip pain.
 |
|
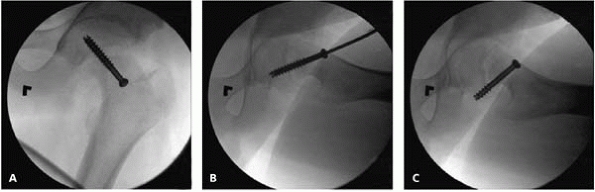
▪ FIGURE 22-13
An essential part of staying out of trouble after SCFE fixation is careful intraoperative evaluation of the screw placement. Importance of a true lateral approachwithdrawal technique. This screw looks perfect on the AP (A) and semilateral (B). However, this image (C) shows threads out. The time to discover this is in the operating room, not months later in the clinic (see Fig. 22-14). |
-
Persistent instability of the physis with inadequate fixation
-
Pin penetrating into the joint (Fig. 22-14)
-
Superficial or deep infection
-
AVN of the capital femoral epiphysis
 |
|
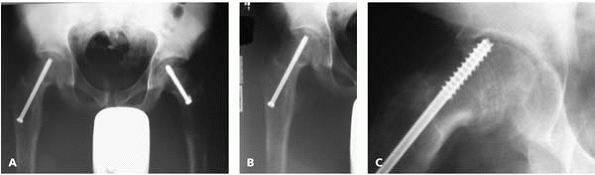
▪ FIGURE 22-14 Persistent hip pain after internal fixation of an SCFE requires careful evaluation. This AP pelvis image (A) and this AP of the right hip (B) do not show a clear source of the pain. This oblique image (C) shows the screw in the joint, with damage to the acetabulum. That certainly explains this patient’s persistent pain.
|
that screw removal is generally not indicated. Because symptoms are
rare, and will probably not complicate a total hip in the future, the
removal procedure can be a major source of problems. Another important
counseling discussion regards whether the asymptomatic side should be
stabilized with a screw. A recent study showed that in cases in which
the probability of contralateral SCFE exceeds 27%, or in cases in which
reliable followup is not feasible, pinning of the contralateral hip is
favored.21 Another study showed that
the triradiate cartilage was a good clue: if it is closed, there is
only a 4% chance of contralateral slip.22
The decision as to whether to pin one or both hips thus depends heavily
on the interaction between the surgeon and the parents. To stay out of
trouble, if the child is from a typical demographic group and followup
will be reliable, observation is generally preferred to the risk of
creating a complication on the asymptomatic side (which is uniformly
unappreciated by families and exploited by plaintiff attorneys). On the
other hand, if the child has renal osteodystrophy, hypothyroidism or
some other endocrine problem, cannot be relied on for followup, or has
parents who aggressively want both hips fixed, it is probably best to
offer bilateral internal fixation at the time of the initial
presentation.
 |
|
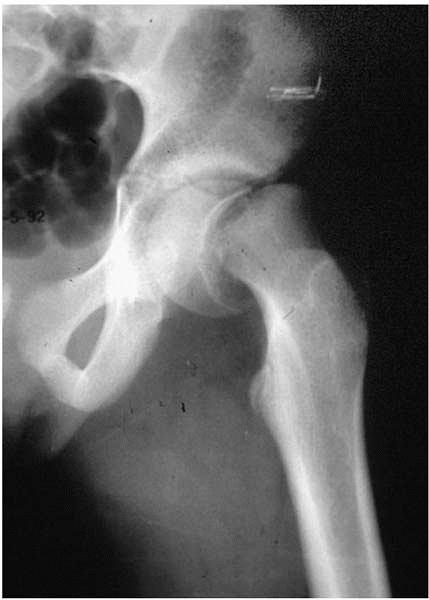
▪ FIGURE 22-15 The unstable SCFE—a major source of trouble.
|
they certainly cause more than 5 to 10% of the problems. To stay out of
trouble, an unstable SCFE should be treated as an emergency, and the
family should be counseled at the time of presentation about the high
risk of AVN. A second screw for additional internal fixation may be
considered, and the child should be followed very closely in the
postoperative period. At the time of fixation, “inadvertent” reduction
is the standard practice at many centers. Many believe that “the damage
is
done” to the blood supply to the epiphysis, so reduction (to unkink the vessels and create a more physiologic hip) is performed.23 Such empiric beliefs and observations have been supported by a recent angiographic study.24 There is also some evidence that a capsulotomy may decrease the risk of AVN after reduction.25 Unfortunately, the trial lawyers have evidence in the literature to condemn reduction,26 and thus many surgeons feel the need to use the words “inadvertent reduction” in the operative note.
 |
|
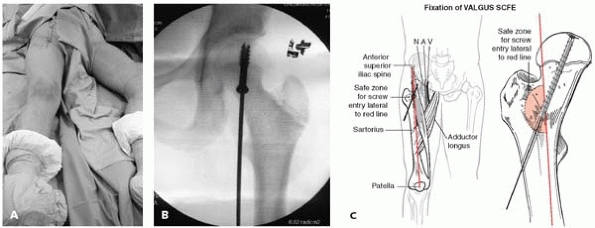
▪ FIGURE 22-16
The “valgus SCFE” can be trouble. Achieving fixation with proper screw orientation may put the neurovascular bundle at risk. This photo (A) shows positioning of the guidewire in the anterior thigh. The fluoroscopic image (B) shows the screw oriented perpendicular to the physis. (C) The relationship between the guidewire trajectory and the neurovascular bundle. (Case and pinning concepts courtesy of R. Davidson, MD.) (C) Staying out of trouble pinning a valgus SCFE. The safe zone for the screw is just lateral to the red line drawn here between the anterior-superior iliac spine and the center of the patella. The femoral head sits very superiorly and almost laterally on the neck of the femur. A very vertical track should be taken from distal to proximal in order to get a screw across the physis. |
epiphysis presents certain challenges. The perfect trajectory for a pin
may put the neurovascular bundle at risk27 (Fig. 22-16).
improper fixation of a slipped capital femoral epiphysis, or possible
loss of reduction, a CT scan can be a very valuable study to understand
the problem in three dimensions (Fig. 22-17).
It may be necessary to exchange screws or add a second screw for
further fixation. Any time a screw is removed, protective weight
bearing should be considered to avoid a pathologic fracture. This is
particularly true if the screw entered the subtrochanteric area of the
femur, where it can create a stress-riser, leading to fracture.28
Infection around the screw fixing a SCFE is rare but has been reported.
These children will often present with persistent pain and possibly an
elevated C-reactive protein (CRP) and radiolucency around the screw on
plain radiographs. Early after surgery, every effort should be made to
avoid removing the screw. The area should be cultured and the child
should be placed on appropriate antibiotics. If that fails, the screw
should be removed, the area debrided, and a new screw should be placed
in a different position.
 |
|
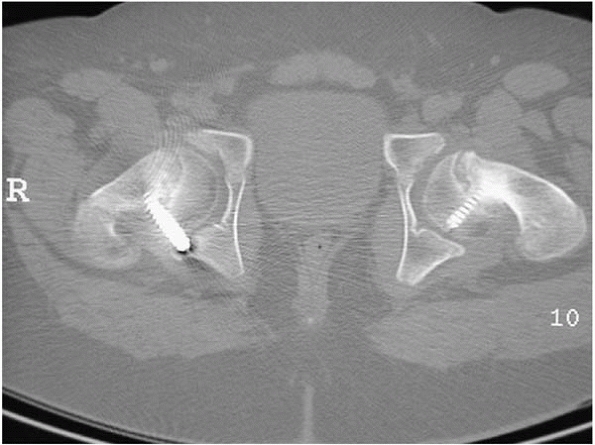
▪ FIGURE 22-17
This CT cut demonstrates why this boy had so much pain and stiffness after SCFE fixation. Persistent postoperative pain must be investigated. |
AVN in acute SCFE, and consider a bone scan or MRI early after surgery.
Non-weight bearing is recommended until the presence or absence of AVN
is confirmed. If AVN occurs, the decision to change screws depends on
the status of the physis. If the physis is closed, any penetrating
screws should be removed promptly. If the physis is still open, any
penetrating screws should be backed off or a new screw should be placed
in a different position. Treatment of AVN in SCFE with a vascularized
fibula graft is controversial. Success depends on many factors,
particularly the experience of the person performing the vascularized
fibular grafting. In most cases, AVN after SCFE is treated with
protective weight bearing, activity restrictions, and use of
nonsteroidal antiinflammatory drugs. In most cases, the final result is
unsatisfactory. A redirecting osteotomy is an option if there is just a
small segment of the head affected.
is clear now that many previous cases were related to intraarticular
hardware. The surgeon should be certain when making the diagnosis of
chondrolysis that there is no persistent pin penetration (Fig. 22-18).29 A CT-scan may be best for this assessment. Otherwise,
the treatment of chondrolysis is physical therapy, antiinflammatory
drugs, and possibly an epidural anesthetic with physical therapy.
 |
|
▪ FIGURE 22-18
This patient presented with a stiff hip and was diagnosed with chondrolysis, caused by the inferior pin tip in the joint. Before the days of reliable intraoperative imaging and screw fixation, pictures such as this were much more common. (Case courtesy of R. Davidson, MD.) |
unstable SCFEs, especially if SCFE is severely displaced. Observation
only is recommended for the first 18 to 24 months, because remodeling
of the femoral neck can occur. However, there is also a growing body of
evidence that the displaced metaphysis of a severe slip damages the
acetabular cartilage, leading to early arthritis.30
A variety of proximal femoral osteotomies have been proposed for the
proximal femoral deformity that occurs after an SCFE. Many of these
osteotomies restore internal rotation and flexion. Some of them may be
able to alter the likelihood of osteoarthritis. The closer the
osteotomy is to the physis, the better the correction of the deformity,
but also the higher risk of complications. Intertrochanteric osteotomy
with internal/external fixation has been the most widely used. However,
this creates a very complex shape to the proximal femur and may
challenge our total hip colleagues in the future.
in school-age children. Conversely, septic arthritis of the hip is rare
but is a potentially crippling disaster if the diagnosis is delayed or
not made at all. Distinguishing transient synovitis from septic
arthritis is an essential skill for staying out of trouble in pediatric
orthopaedics. Although recent studies have provided some clinical
predication rules,31, 32, 33 they are no substitute for experience, good judgment, and a careful history and physical examination.
worse by the hour, and will not bear weight on the involved side. There
is usually pain with simple log-rolling of the hip. Usually the CRP is
up even early in the condition. Erythrocyte sedimentation rate (ESR)
may not be elevated in the first 24 hours of infection.34
followed by an aspiration of any hip that is suspicious for septic
arthritis. Beware of the possibility of a false-negative ultrasound,
especially if the symptoms have been present for less than 24 hours.35
aggressive in the indications for irrigation/debridement. Most authors
recommend that if the white count is higher than 50,000 in the fluid,
the rest of the clinical picture suggests septic arthritis; a formal
open irrigation and debridement of the hip through an anterior approach
is then recommended.
irrigation and debridement than to miss a case of septic arthritis. In
this way, it is much like the philosophy the general surgeons have for
treating appendicitis.
-
Psoas abscess36,37
-
Pelvic abscess38
-
Appendicitis
-
Septic sacroiliac joint
-
Osteomyelitis of the pelvis39
-
Gynecologic conditions
-
Osteomyelitis
-
Acetabulum
-
Femur
-
familiar to most pediatric orthopaedists. To stay out of trouble, it is
important to avoid the blood supply, which comes in posteriorly. For
this reason, the approach is anteriorly through the tensor fascia
lata/sartorius interval. It is important to have a very definite
capsulotomy. Many surgeons recommend actually taking a small piece of
the capsule out to be certain that the joint has been decompressed. It
is important to irrigate the joint aggressively and decompress the
femoral neck if there is associated femoral neck osteomyelitis. A drain
is usually placed around the femoral neck and pulled a few days later.
Without a drain, the hip arthrotomy can close quickly and there can be
a reaccumulation of the fluid, necessitating repeat surgery. The child
should rest in bed for a couple of days to keep the drain in and allow
the hip to quiet down. Antibiotic management lasts 4 to
6
weeks, based on the organism that is cultured and the recommendation of
the infectious disease experts. CRP is the most valuable test to follow
in the postoperative period.
does not rapidly normalize in the first week after surgery. In the face
of either persistent symptoms or an elevated CRP, the surgeon reflect
on these questions: Could there be another collection in another area?
Could the fluid have reaccumulated? Is the diagnosis right? Are the
antibiotics right?
years is valuable, to study growth and the risk of AVN. For neonates
who experience sepsis, it is the orthopaedist’s job to prove that there
are not two septic hips or septic arthritis elsewhere. Multifocal
septic arthritis is very common in the neonate and can be a major
source of trouble. It is best to aspirate both hips and perhaps other
joints in order to make the diagnosis as soon as possible.
JA, Kim HT, Browne R. Legg-Calvé-Perthes disease. Part I:
Classification of radiographs with use of the modified lateral pillar
and Stulberg classifications. J Bone Joint Surg Am. 2004;86-A(10):2103-2120.
JA, Kim HT, Browne R. Legg-Calvé-Perthes disease. Part II: Prospective
multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004;86-A(10):2121-2134.
DL, Roy AK, Vitale MG, et al. Quality of evaluation and management of
children requiring timely orthopaedic surgery before admission to a
tertiary pediatric facility. J Pediatr Orthop. 2002;22(2):265-267.
RT, Greenfield ML. Clinical characteristics of children with atypical
and idiopathic slipped capital femoral epiphysis: description of the
age-weight test and implications for further diagnostic investigation. J Pediatr Orthop. 2001;21(4):481-487.
MJ, Patton CM, Luhmann S, et al. Knee pain as the initial symptom of
slipped capital femoral epiphysis: an analysis of initial presentation
and treatment. J Pediatr Orthop. 1999;19(4):455-460.
T, Suzuki S, Seto Y, et al. Sequential magnetic resonance imaging in
slipped capital femoral epiphysis: assessment of preslip in the
contralateral hip. J Pediatr Orthop B. 2001;10(4):298-303.
ST, Casillas M, Banta JV. Displaced femoral neck fractures at the
bone-screw interface after in situ fixation of slipped capital femoral
epiphysis. J Pediatr Orthop. 1997;17(2):212-215.
BT, Birnbaum P, Minter C. Slip progression after in situ single screw
fixation for stable slipped capital femoral epiphysis. J Pediatr Orthop. 2003;23(5):584-589.
MS, Bishop JA, Hresko MT, et al. Prophylactic pinning of the
contralateral hip after unilateral slipped capital femoral epiphysis. J Bone Joint Surg Am. 2004;86-A(12):2658-2665.
D, Dimeglio A, Bentahar T. Staging puberty in slipped capital femoral
epiphysis: importance of the triradiate cartilage. J Pediatr Orthop. 2004;24(2):144-147.
MD, Weiner DS, Green NE, et al. Acute slipped capital femoral
epiphysis: the value and safety of urgent manipulative reduction. J Pediatr Orthop. 1997;17(5):648-654.
JE, Abrahams MS, Dobbs MB, et al. Early reduction, arthrotomy, and
cannulated screw fixation in unstable slipped capital femoral epiphysis
treatment. J Pediatr Orthop. 2002;22(3): 352-358.
KP, Stanton RP, Mason DE. Factors influencing the development of
osteonecrosis in patients treated for slipped capital femoral
epiphysis. J Bone Joint Surg Am. 2003;85-A(5):798-801.
M, Casillas MM, Hamlet M, et al. Slipped capital femoral epiphysis:
early mechanical damage to the acetabular cartilage by a prominent
femoral metaphysis. Acta Orthop Scand. 2000;71(4):370-375.
MS, Mandiga R, Zurakowski D, et al. Validation of a clinical prediction
rule for the differentiation between septic arthritis and transient
synovitis of the hip in children. J Bone Joint Surg Am. 2004;86-A(8):1629-1635.
SJ, Jones A, Schootman M, et al. Differentiation between septic
arthritis and transient synovitis of the hip in children with clinical
prediction algorithms. J Bone Joint Surg Am. 2004;86-A(5):956-962.
ST, Rowe SM. Moon ES, et al. Significance of laboratory and radiologic
findings for differentiating between septic arthritis and transient
synovitis of the hip. J Pediatr Orthop. 2003;23(3):368-372.
MJ, Unkila-Kallio L, Aalto K, et al. Serum C-reactive protein,
erythrocyte sedimentation rate and white blood cell count in septic
arthritis of children. Pediatr Infect Dis J. 1997;16(4):411-413.
JE, Huang M, Dobbs M, et al. Causes of false-negative ultrasound scans
in the diagnosis of septic arthritis of the hip in children. J Pediatr Orthop. 2002;22(3):312-316.
J, Bagali M, Kaneker S. Physical signs in pyomyositis presenting as a
painful hip in children: a case report and review of the literature. J Pediatr Orthop B. 2004;(3):211-213.