Tibial Plateau Fractures
surface of the proximal tibia. Proximal tibia fractures that do not
involve the articular surface present different issues and are
discussed in Chapter 55. Small rim avulsions occur in conjunction with knee dislocations and other knee ligament injuries and are discussed in Chapter 54.
Despite these exclusions, tibial plateau fractures, as discussed in
this chapter, are a diverse group of fractures that represent a wide
spectrum of severity that ranges from simple injuries with predictably
excellent outcomes after nonoperative treatment to complex fracture
patterns that challenge even the most experienced surgeons (Fig. 53-1).
Imaging studies need to be of good quality to demonstrate the location
of the fracture, the fracture pattern, and the degree of displacement
and there is controversy on which type of imaging is optimal. Assessing
associated soft tissue injuries around the knee is critically
important. Certain fracture patterns have a high risk of
limb-threatening complications such as compartment syndrome and, for
other patterns, these risks are negligible. Treatment concepts based on
restoring or preserving limb alignment will lead to a satisfactory
outcome for most patients; poor alignment often will result in a less
satisfactory result. New methods have changed the surgical management
of both low-energy lateral plateau fractures and high-energy medial and
bicondylar fractures, but more data are necessary to determine if these
new methods are improving patient outcomes.
fractures have evolved dramatically over the past 50 years. In the
decades
of
the 1950s, 1960s, and 1970s, these fractures were predominantly treated
nonoperatively and published results indicated that favorable outcomes
were possible using a variety of techniques, including traction, cast
bracing, and even spica casting.8,9,42,47 Apley8,9
controlled deformity using longitudinal traction, encouraged early knee
motion, and reported satisfactory results. Lansinger et al.,99 in a 20-year follow-up of patients originally reported by Rasumssen,131
showed that nonoperative treatment for fractures with less than 10
degrees of coronal instability resulted in favorable outcomes. Duwelius
and Connolly48 treated patients with
closed reduction with or without percutaneous pin fixation and
mobilized them early in a cast brace and reported an 89% rate of good
or excellent clinical results. Spica casting after closed reduction led
to good and excellent results in 85% of patients.47 Cast bracing was frequently used for tibial plateau fractures as an isolated treatment with satisfactory results.42
Although mostly of historical interest, the favorable results in these
reports provide indirect evidence that the articular surface of the
proximal tibia is tolerant of modest deformities and treatment will
result in favorable outcomes if external forces are used to achieve
reasonable limb alignment even without a perfectly reduced articular
surface.
 |
|
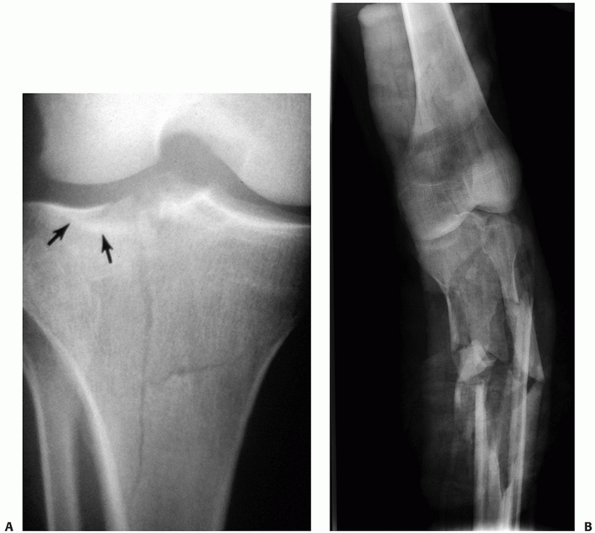
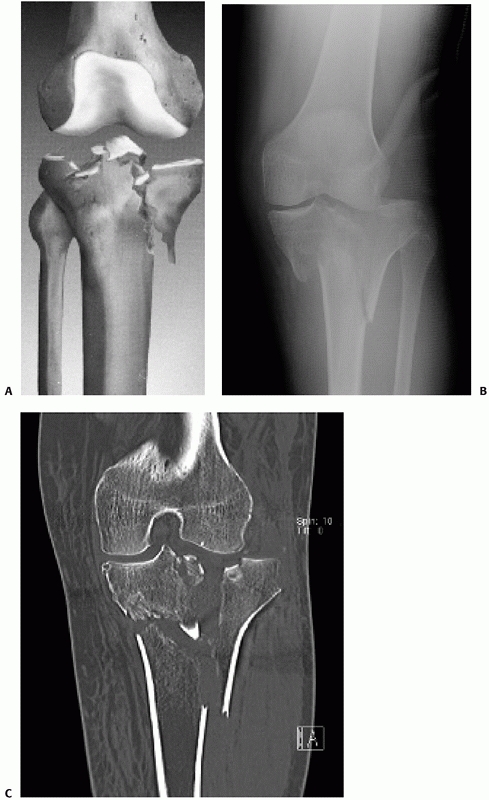
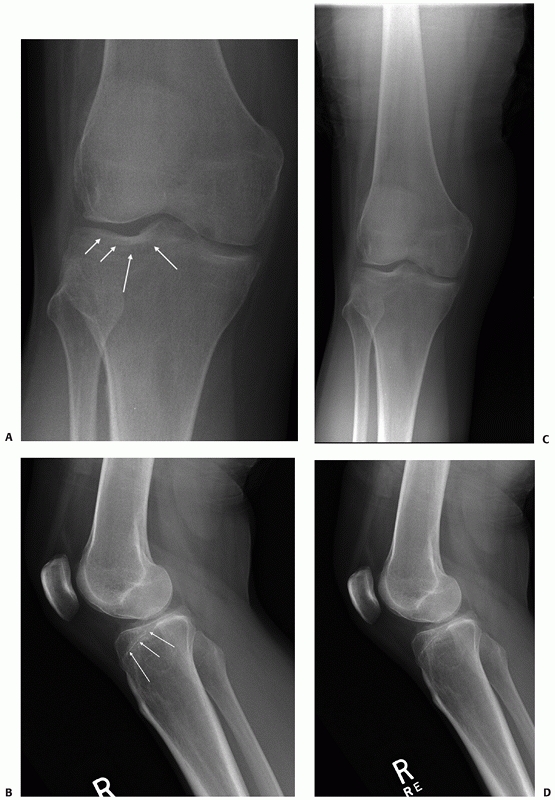
FIGURE 53-1
Two anteroposterior images illustrate the range of injury severity that occur in tibial plateau fractures. They also illustrate how fracture classifications do not always capture this wide range. A. Technically a bicondylar fracture classified as AO/OTA type C1 or Schatzker 6. It is minimally displaced, has a low risk for complications, and will be relatively easily treated. B. Also technically a bicondylar fracture classified as AO/OTA type C2 and Schatzker 6. The differences in appearances, displacement, comminution, risks, and required treatment techniques are obvious. |
reducing and fixing tibial plateau fractures became common in the
1980s. These techniques had the advantages of reducing the articular
surface, aligning the limb, and mobilizing the knee early after injury
with less-encumbering external devices. Similar to nonoperative
techniques, favorable results were reported for the majority of
patients.140,143,164
Criteria were developed for which fractures needed to be surgically
reduced, but this remains an area of controversy even today and
different surgeons continue to use different criteria for operative
intervention.112 Guidelines for
treatment based on measured millimeters of displacement of the
articular surface were proposed but have never been based on anything
more than opinion.
optimal treatment became of increased importance. The Schatzker
classification defined pathoanatomy and suggested treatment strategies,
and this classification remains central to the language of tibial
plateau fractures and is discussed here.142,143 The AO/OTA classification also works well for the proximal tibia and remains the key international classification of fractures.
treated, surgical complications, some of them severe, became relatively
common. Surgical methods for reducing and fixing tibial plateau
fractures have evolved over the last three or four decades, in
part
from the need to identify techniques that minimize complications and
other techniques that optimize the treatment of complications when they
occur.
thinking and are leading to better understanding, management, and
better outcomes for patients with tibial plateau fractures. Clinical
research is needed to provide evidence so these new trends can be most
appropriately integrated into the traditional surgical armamentarium.
visualize both the fracture and the associated injuries to important
soft tissue structures around the knee. High-quality computed
tomography (CT) scans including three-dimensional imaging assists in
preoperative planning particularly for complex patterns. The frequency
of associated meniscal and ligament injuries and the fracture patterns
in which these injuries are most likely to occur have been elucidated
with the use of magnetic resonance imaging (MRI). Although to some
clinicians the value of the information these studies provide seems
intuitively obvious, their role in improving patient outcome remains to
be fully defined.
techniques are being used to optimally support the reduced articular
surface, including better implants, better methods to position
implants, and better methods to fill the metaphyseal void created after
reducing the articular fragments. These new techniques are important
since some loss of articular reduction remains an important problem. In
fractures that involve both condyles and those with shaft instability,
plates with locked screws provide fixed angle stability and have become
important adjuncts to maintain fracture alignment and have
substantively changed practice patterns. When fixation is necessary on
both the medial and lateral side of the knee, using two separate
approaches appears to be as effective as and much safer than extensile
approaches. In severe patterns with displacement and soft tissue
injury, the use of a joint-spanning external fixator has facilitated
maintaining length and alignment during a delay awaiting soft tissue
recovery, which has led to safer definitive surgery.
of the proximal tibia that occur in adults, with the highest incidence
in the third through the fifth decades of life. Fractures in men occur
at a younger age and women have increasing incidence with advancing
age, particularly in the sixth and seventh decades, which indicates
these fractures are occurring in osteopenic bone.
the knee sustains one of a variety of mechanisms of injury. In
middle-aged or elderly patients, simple falls lead most commonly to
lateral or, less commonly, medial side fracture patterns. Split
depression fractures of the lateral plateau are most common. When the
bone is very osteopenic, insufficiency fractures in elderly patients
can occur and be missed on plain radiographs.129
Higher-speed injuries in younger patients from sports or similar
mechanism can cause split fractures or rim avulsion fractures
associated with knee ligament injuries. Motor vehicle accidents and
falls from heights and pedestrian struck injuries often produce more
severe patterns, which may involve both condyles and have a high risk
for associated neurovascular injuries, compartment syndrome, and
communicating open wounds. In one study of severe plateau fractures
treated with external fixation, 16 of 21 injuries were motor vehicle
related, and in another study of bicondylar fractures treated with dual
approaches, 68 of 83 were motor vehicle related or caused by a fall
from a height.11,111
In contrast, a study of elderly patients with a mean age of 74 years
reported that 58% of fractures were caused by a simple fall.87
the knee dictate the fracture pattern. The greater the energy absorbed
by the proximal tibia, the more severe is the fracture and the more the
fragments are displaced and comminuted. The energy of fracture results
from a combination of the forces applied and the quality of the bone.7
Generally, axially loading forces are more rapid and release greater
energy than angular forces. In cadavers, it is possible to produce
typical split fractures with pure valgus forces, local compression
fractures with axial forces, and split depression fractures with
combinations of both forces.91 The
intact medial collateral ligament (MCL) acts like a hinge for the
lateral femoral condyle, and in this cadaver study it needed to be
present for the lateral plateau to fracture.91 This means that clinically the MCL should not be torn in these lateral patterns.
valgus force because of the normal 5 to 7 degrees of valgus alignment
of the knee and because of a propensity to be struck from the lateral
side. A valgus force loads the lateral tibial plateau to failure from
direct impact with the lateral femoral condyle. A combination of valgus
and axial compression produces lateral side depression, split
depression, or, less commonly, lateral split or total lateral condyle
fractures.104 Younger patients with
good bone tend to have split fractures with less depression, and
elderly patients with osteopenic bone have a greater component of
compression with a less prominent split fragment. Most commonly in
lateral fracture patterns, there is at least a small component of both
a split fracture and depression at the peripheral margin of the
fracture. Less commonly than in lateral side fractures, varus injuries
lead to failure of the medial plateau. These injuries can involve the
entire medial plateau and, in some cases, the fracture-shearing plane
may extend well into the lateral plateau. In other cases, the fracture
involves lesser portions of the medial plateau. A posteromedial
shearing fracture of the medial plateau is a common medial side pattern
and can occur as an isolated split fracture, or in as many as one third
of bicondylar fractures, and it is part of the bicondylar fracture
pattern.13 The mechanism has been described as knee flexion, varus, and internal rotation of the medial femoral condyle.39,162
in a weight-bearing position so axial load is typically some component
of the injuring force. Generally, the greater the axial load component,
the more energy there is at failure and the more severe is the fracture
pattern. Bicondylar patterns result when axial load predominates, with
the severity varying based on the magnitude of the axial forces.
Occasionally in a patient with a
valgus knee, an axial force may shear the medial tibial condyle and produce a medial plateau fracture or fracture dislocation.
at the metaphyseal region as a result of direct trauma and/or a
combination of axial load and bending forces. These are classic bumper
injuries or other crush, direct blow, or similar mechanisms where the
tibial shaft is separated from the condyles with proximal extensions of
fracture lines into the plateau. These severe injuries have a high risk
of complications because of both the area of the injury and the high
degree of energy transfer. Open fractures, severe closed soft tissue
injury, trifurcation injury, and compartment syndrome are all
associated with this mechanism.166,177
injuries. These may be other ipsilateral or contralateral skeletal
injuries and injuries to other systems that may influence how the
plateau fracture is managed. In one recent study of bicondylar tibial
plateau fractures, 13 of 41 patients had other major skeletal injuries
in addition to the plateau fracture, and these associated injuries were
found to affect the patient’s functional outcome.11
High-energy tibial plateau fractures have a small risk of vascular
injury and a high risk for compartment syndrome. These associated
injuries are discussed in the next section on history and physical
examination.
tissue injuries that are important to recognize because they may
influence fracture management and prognosis. Not surprisingly, the
force that produces medial or lateral plateau fractures may lead to
associated collateral ligament injuries. MCL injuries can be associated
with lateral plateau fractures from valgus forces. These associated
collateral ligament injuries were once thought to be common because of
the instability apparent on exam, but this instability can occur
because of the loss of osseous support from the depression of the
lateral plateau articular surface. The bony failure on one side of the
joint actually protects the collateral ligament on the opposite side.
One mechanical study indicated that an intact MCL functioning as a
pivot point of the lateral femoral condyle was a necessary requirement
to produce a lateral plateau fracture.91
In one recent study, the incidence of associated collateral ligament
injury was only 3% each for both MCL and lateral collateral ligament
(LCL).1 The diagnosis can be made with MRI or with a stress view demonstrating medial joint opening.
These injuries play a role in managing tibial plateau fractures and are
further discussed in the section on current management. Certain
peripheral fractures of the margins of the tibial plateau are virtually
pathognomonic of cruciate ligament injury, and in these injured knees,
it is appropriate to emphasize treating the ligament injuries rather
than the plateau fracture itself. These fractures include the Segond
fracture, reverse Segond fracture, anteromedial tibial margin
fractures, and semimembranosus tendon insertion site fractures.31,37
pattern and should direct the necessary degree of vigilance for
associated injuries. Split lateral plateau fractures typically result
from low-energy forces from falls and twisting injuries. The risk of
associated neurovascular injury or compartment syndrome is very low. On
the other hand, patients whose injuries result from falls from a
height, motor vehicle accidents, or being struck as a pedestrian are
more likely to have tibial plateau fracture patterns that have a much
higher risk of these associated injuries that must be managed urgently
or emergently. Although the history is important, it is the fracture
pattern that guides treatment decisions and determines the risks for
complications. The clinician should be aware that the mechanism of
injury in isolation might be deceiving. Relatively high-energy
fractures can occur when the history suggests more innocuous mechanisms.
critically important to diagnose associated injuries and complications,
to plan for surgical treatment, and to decide on optimal timing of
interventions. In all injured limbs, but particularly in patients with
certain fracture patterns, a thorough neurovascular examination is
mandatory. Metaphyseal-diaphyseal dissociation patterns and fracture
dislocations are such injuries that are at particular risk for vascular
or neurologic injury.
risk for compartment syndrome. In one study, 10% of all tibial plateau
fractures were diagnosed with an associated compartment syndrome and
the risk was particularly high in the high-energy fractures, with 30%
in Schatzker 6 patterns.34 The
compartments of the lower leg should be evaluated with serial
examinations for signs of compartment syndrome. Presence of the
well-recognized signs, including tense compartments and pain with
passive stretching, should raise the suspicion of an associated
compartment syndrome and measurement of compartment pressures is
indicated. If the diagnosis is clear on physical examination,
fasciotomy may be performed without pressure measurements. Patients who
have high-energy fracture patterns who are not able to provide a
history and who are difficult to examine should have compartment
pressures measured at presentation, and these measurements may need to
be repeated based on the clinical findings and the results of the
initial measurement.
wounds that need to be identified on physical examination of the
injured limb (Fig. 53-2).
the knee after fracture healing is determined by a combination of the
presence or absence of extra-articular fracture deformity, residual
articular depression, and knee instability. Initial assessments of limb
alignment are frequently made based on the appearances of the fracture
on radiographs, but deformity may be apparent on inspection. In lateral
tibial plateau fractures, assessing for valgus instability of the knee
may provide a guide to the need for surgical treatment.50,174
If instability is present, it is likely caused by fracture displacement
and will not resolve without reducing the fracture. However, pain from
the injury often makes it difficult to examine the knee for coronal
instability, limiting the value of this assessment.
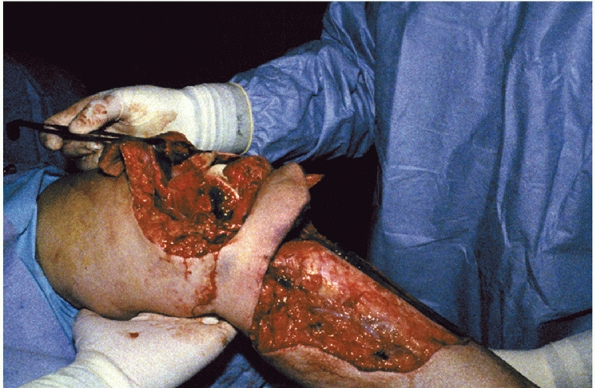 |
|
FIGURE 53-2 Open tibial plateau fracture with extensor mechanism disruption caused by a lawnmower blade.
|
is planned, the soft tissue envelope around the knee must be carefully
examined. The timing and, in some fractures, the type of surgical
approach will be dictated by this examination. High-energy tibial
plateau fractures have a significant risk of soft tissue complications
from surgical approaches, so the examination of the soft tissues is
very important. Important features of the soft tissues are the severity
of swelling, visible contusions, and the size, character, and location
of fracture blisters (Fig. 53-3).
made on plain radiographs, and for some fractures this may be the only
imaging necessary. Anteroposterior (AP), lateral, and an AP view in the
plane of the plateau (10- to 15-degree caudal view) are the standard
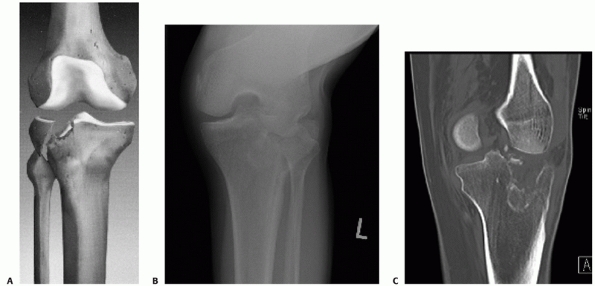
examinations (Fig. 53-4). The caudal view
provides a better view of the articular surface and helps assess
displacement and depression better than the standard AP view.82,115
Hohl found that the standard AP view could not reliably determine the
amount of articular depression but that a 14-degree caudal view
accurately estimated central and posterior displacement but could
overestimate anterior displacement and depression.115
Less frequently, oblique views are obtained to assess the location of
fracture lines or degree of displacement but are not routine. CT scans
have largely supplanted the need for these adjunctive views. When there
is substantial fracture displacement, particularly in bicondylar or
fracture dislocation patterns, radiographs in traction will better
assess the fracture anatomy (Fig. 53-5).
Traction restores the gross geometry of the proximal tibia, decreases
overlap, and better defines the fracture pattern than the original
radiographs. Manual traction may be applied solely for the purposes of
such radiographs, but in severe fractures, radiographs obtained after
applying a joint-spanning external fixator will provide the necessary
traction for assessment of fracture anatomy. When applying the fixator,
care should be taken to avoid having metal bars or clamps overlying the
proximal tibia in the plane of the important radiographic views.
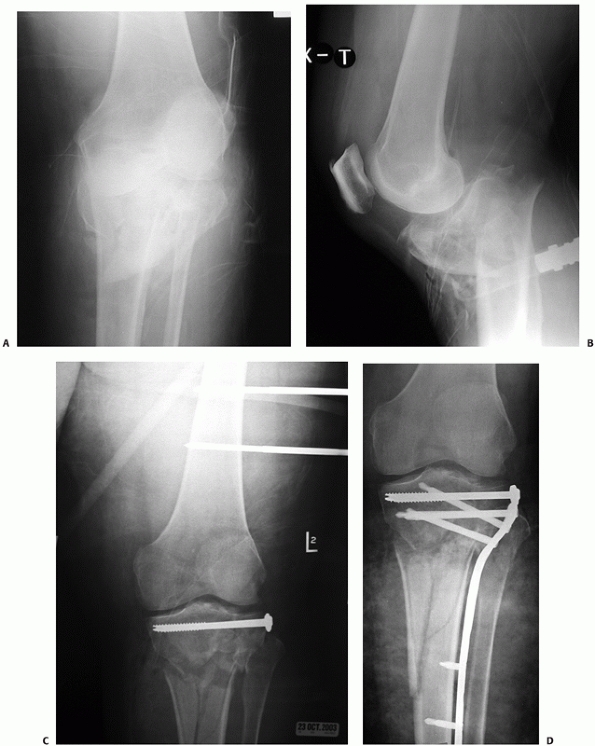
 |
|
FIGURE 53-3
Severe closed soft tissue injury associated with a high-energy tibial plateau fracture. There are hemorrhagic fracture blisters. |
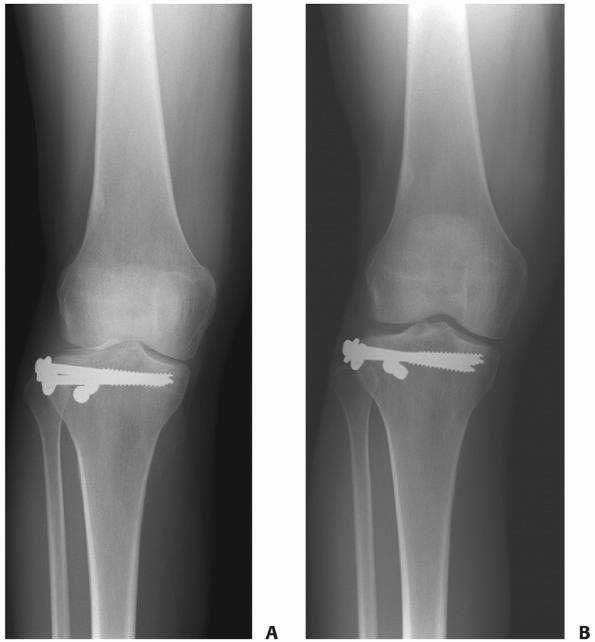 |
|
FIGURE 53-4 A.
Anteroposterior radiograph of this patient after treatment of a tibial plateau fracture shows slight ellipses of the nonprofiled medial and lateral plateaus. The anterior margin projects more superiorly than the posterior margin. In the 10-degree, caudal view (B), the proximal articular surface is nearly a single radiodense line, providing better assessment of the articular surface. |
tibial plateau fractures. They provide excellent detail of the fracture
pathoanatomy and serve as a critically important aid to preoperative
planning for operative approaches and fixation techniques. Although CT
may be used to help decide on the need for surgery, there are no good
data to indicate that the additional detail apparent on CT helps
determine which fractures will benefit from surgery. CT typically
demonstrates more articular displacement and comminution than is
apparent on plain films.102 CT has
been shown to help surgical planning and to lead to more reliability in
classifying the fracture and deciding on a treatment plan.32,176
The location of depressed fragments, the size of articular segments,
and the location and orientation of fracture lines are important
details in planning an operative strategy, and they are best visualized
on CT. Three-dimensional reconstructions have been increasingly used
and found to demonstrate spatial relationships of fracture fragments
better than plain radiographs.18 In one study, the addition of spiral CT with three-dimensional reconstructions frequently resulted in
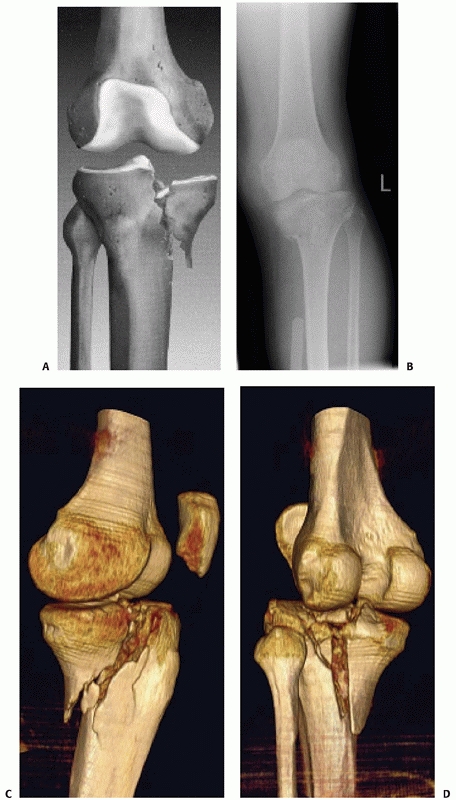
modifications and adjustments in operative plans compared with using plain radiographs alone102,176 (Fig. 53-6).
 |
|
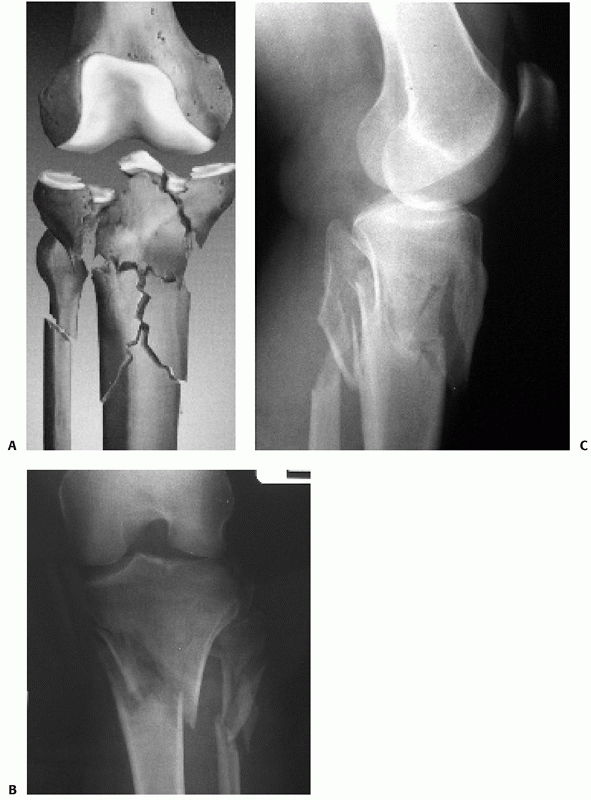
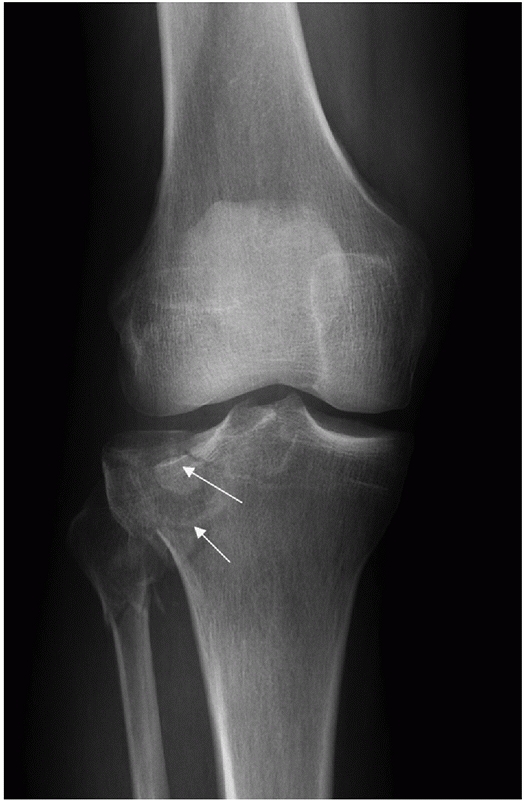
FIGURE 53-5
Advantages of traction in realigning a fractured tibial plateau. Distraction allows better imaging and facilitates fixing the fracture. The initial anteroposterior (AP) (A) and lateral (B) images show a severe fracture but little additional information can be gained because of the malalignment and overlap. C. An AP film after distraction with a spanning fixator dramatically improves the ability to assess this injury. D. A single screw was placed between the condyles, and 10 days later, the fracture was treated with a locking plate. |
 |
|
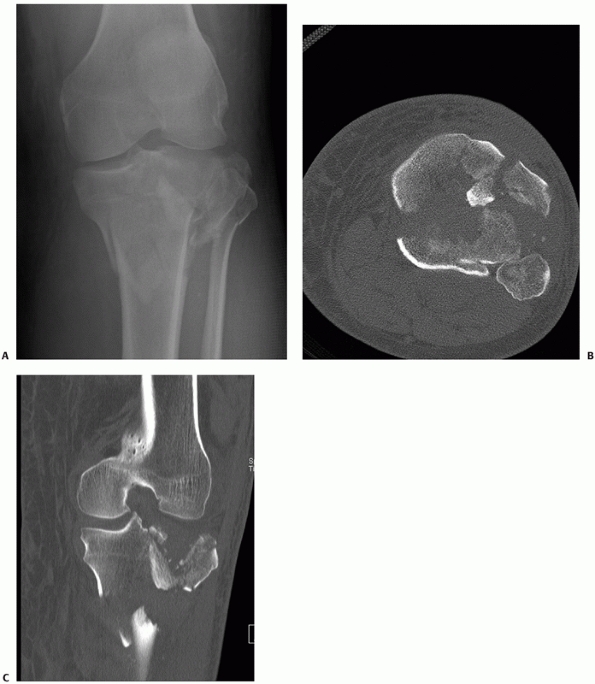
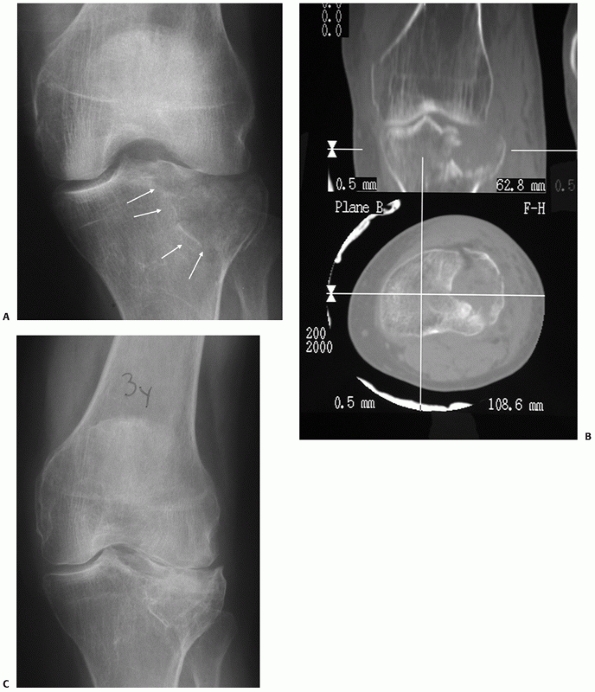
FIGURE 53-6 A.
AP radiograph shows a high-energy bicondylar tibial plateau fracture but further characteristics of the injury are difficult to define. An axial CT (B) and coronal reconstruction (C) show the degree of comminution and identify major fragments but do not provide detail about the overall size and alignment of the fragments. (continues) |
fractured plateau that may be visualized in any two-dimensional plane
or with high-quality three-dimensional images.52
Three-dimensional images from multidetector CT scans provide detail of
the fractured proximal tibia, which enables the surgeon to assess
comminution, depression, and fracture location more accurately than
previously possible.100,106
Similar to plain films, realigning the fracture with a spanning fixator
or other traction techniques before scanning will enhance the quality
of the information available from the study.
multiplaner reconstruction may increasingly be part of operatively
reducing and fixing displaced tibial plateau fractures. Early reports
indicate that this imaging technology allows the surgeon to better
assess the articular surface reduction and the placement of hardware
during the operation than is possible with standard C-arm fluoroscopy.90,93
Although the future role of these devices is currently uncertain, it is
likely that better intraoperative imaging will continue to improve the
ability to accurately and minimally invasively reduce and fix tibial
plateau fractures.
degree of articular displacement and also identifies occult fracture
areas better than plain films and has been found to be equivalent
to traditional two-dimensional CT.94
MRI provides additional information about injuries to the soft tissue
structures of the knee that is not obtained with other imaging
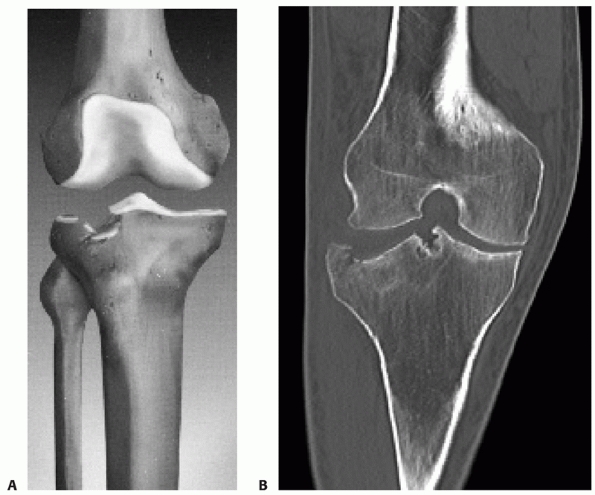
modalities (Fig. 53-7). However, whether MRI
should be a routine part of evaluating tibial plateau fractures or
whether it should be used instead of CT scanning is controversial. CT
scans better visualize the fracture anatomy than do MR images but MRI
demonstrates associated soft tissue injuries, particularly those of the
menisci and ligaments, that are not visualized on CT. When tibial
plateau fractures were assessed with both techniques, CT was found to
be sensitive and specific in identifying ligament injuries because most
of them had at least small bony avulsions, but MRI was necessary to
detect meniscal injuries.121
 |
|
FIGURE 53-6 (continued) (D,E)
High-quality three-dimensional reconstructions provide additional assessment of the fracture morphology for preoperative planning. |
surgeon incorporates management of these soft tissue injuries into a
treatment strategy, but whether this strategy improves patient outcome
is an area of controversy. MRI was shown to lead to higher observer
agreement for both fracture classification and treatment plan than
either plain films alone or plain films with the addition of CT.178 When a proximal tibia stress fracture is suspected and plain films are negative, MRI is the imaging modality of choice.26
risk for complications and, to some extent, the patient outcome.
Because different fracture patterns require very different treatment
strategies, it is important to group together similar injuries and to
separate different injuries from each other. In this way, treatments
can be matched to fracture patterns to optimize outcomes. To accomplish
these goals, fracture classifications must be reasonably reliabile and
reproducibile.
injury patterns are frequently used substituting for formal
classification. The AO/OTA110,122
and Schatzker classifications are both important and widely used in
current practice. Other fracture classifications are of historical
interest.
classifications of tibial plateau fractures, most surgeons still
classify fractures by describing them. Word descriptions provide more
meaning than lettered or numbered classifications, particularly because
many surgeons are not familiar with the exact numbers or letters of a
classification. Fracture descriptions in the tibial plateau work well
for management decisions and convey information necessary for patient
care but do not work for databases or for clinical research.
localize the fracture and then convey the general characteristics of
the fracture. For instance, whether the medial or lateral or both
plateaus are involved provides a reasonable start in describing the
fracture. The terms split, split depression, local compression, and bicondylar fracture
are well-accepted, commonly used terms and convey meaning that is
understood by most surgeons. These terms are incorportated in the
Schatzker classification, which is described later. Similar to other
fractures, the amount the fracture is displaced, angulated, or
comminuted and the presence or absence of subluxation or dislocation
are standard descriptions used for tibial plateau fractures. The amount
of articular surface depression, usually measured in millimeters, is a
quantitative method to assess and characterize the severity of tibial
plateau fractures. Surgical indications for local compression and split
depression fractures have been based on this measurement.
Unfortunately, this
measuremnt cannot be made very reliably between observers, significantly limiting its usefulness.114
 |
|
FIGURE 53-7 A. Lateral radiograph shows an unusual anterior fracture subluxation (AO/OTA type B3). B. Sagittal MR images show the fracture (black arrow) and (C) the torn posterior collateral ligament (white arrow).
|
It has several advantages over the commonly used Schatzker
classification. It identifies both articular and nonarticular fractures
of the proximal tibia, and by the use of the rule of squares, it
provides a way to distinguish proximal tibia from tibial shaft
fractures.122 The rule of squares
identifies a proximal tibia fracture as one where the center of the
fracture is within a square with one side along the articular surface
and the length of a side defined by the width of the metaphyseal
segment. Fractures outside of this square are tibial shaft fractures.
There is more than one category of medial plateau fracture, which is
desirable because it is clinically important to distinguish subtypes of
medial plateau fractures for treatment. For the total articular C
patterns, the degree of comminution of both the metaphysis and the
articular surface is subcategorized, providing important distinctions
for treatment and prognosis. The AO/OTA classification therefore
distinguishes ranges of severity in high-energy patterns better than
the Schatzker classification. It is well accepted for trauma databases
and has been frequently used in recent publications on tibial plateau
fractures.53,136,142,166
It is increasingly becoming a standard and well-accepted way to
classify proximal tibia fractures. The entire classification was
recently updated and republished, and there were no changes made to the
proximal tibia section.110
tibia is 1, so the plateau region is 41. The rule of squares is used to
distinguish these fractures from tibial shaft fractures, 42. The
subtypes of 41 are similar to the ends of the other long bones:
nonarticular fractures of the proximal tibia. Technically, they are not
tibial plateau fractures because the articular surface is not involved.
used because the verbal descriptions of split and split depression are
more common. However, these are lateral side terms and the AO/OTA
classification allows similar, although less common, medial side
injuries to be classified.
 |
|
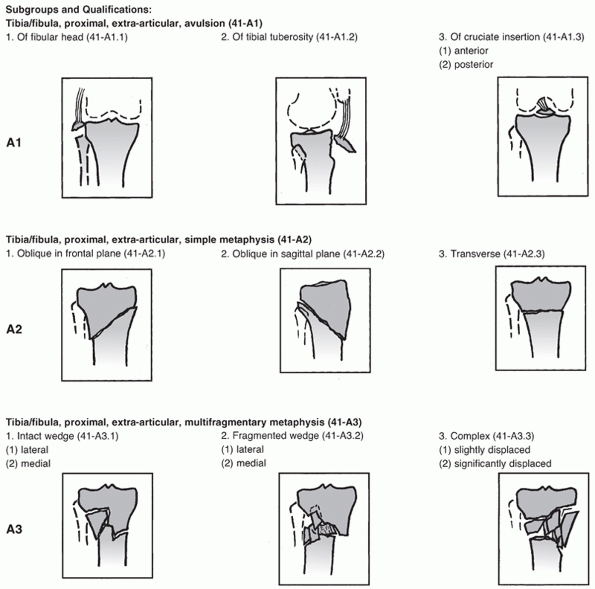
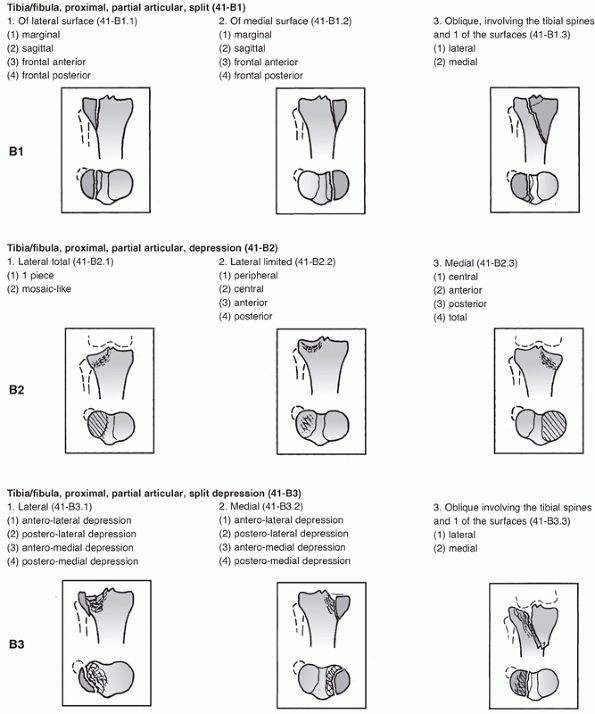
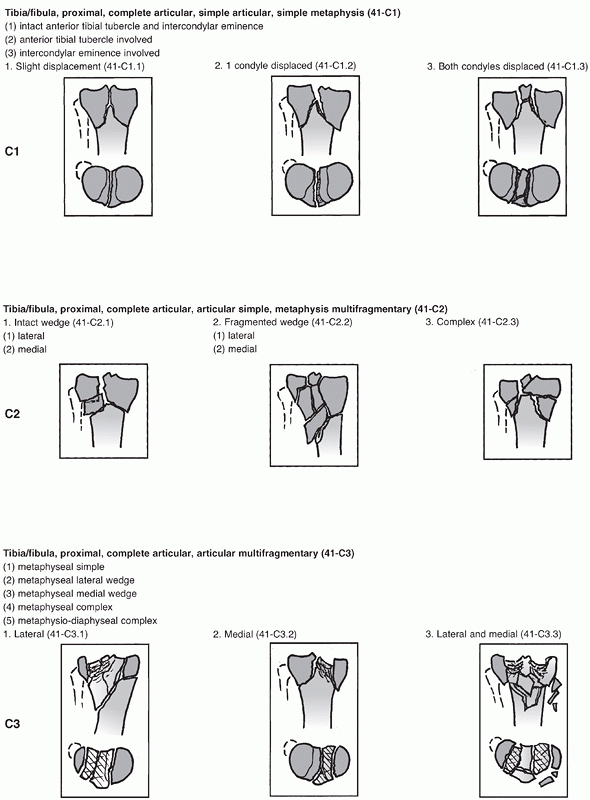
FIGURE 53-8
The AO/OTA classification of proximal tibia fractures. (Redrawn from Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 2007;21(10 Suppl):S1-133, with permission.) (continues) |
articular fractures and, in the proximal tibia, are frequently called
bicondylar fractures. The advantage of the AO/OTA is the ability to
subclassify these fractures based on comminution.
used classification of tibial plateau fractures and is familiar to most
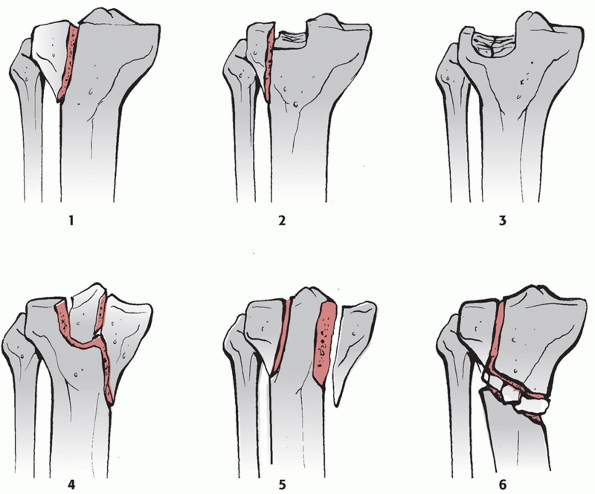
surgeons (Fig. 53-9). Some of the categories
are similar to those of previous classifications. For instance, Hohl in
1969 classified split, split depression, and central depression
fractures.71 Many surgeons may not
be familiar with the numbers of the six types, but most are familiar
with the meaning of the verbal descriptions of each type and this is an
important advantage of the Schatzker classification. Because the six
types are typically treated differently,
the
classification fufills some of the goals of an ideal classification.
Types 1 through 3 were described as lateral and less severe. These
three categories reasonably identify the types of fractures that occur
on the lateral side of the plateau.
 |
|
FIGURE 53-8 (continued)
|
 |
|
FIGURE 53-8 (continued)
|
 |
|
FIGURE 53-9 The Schatzker classification of tibial plateau fractures.
|
classification with regard to types 4 through 6, which are the medial
(type 4) and the more severe higher-energy bicondylar (type 5) and
shaft dissociated (type 6) patterns. Type 4 is the only category for a
medial sided fracture, but medial plateau fractures occur in several
distinct patterns. For instance, there is no way to distinguish a
posteromedial split fracture from a medial total condylar fracture. In
reporting a series of posteromedial plateau fractures treated by
internal fixation, Bhattacharyya et al.19 point out difficulties with categorizing these fractures in the Schatzker classification.
and most subsequent diagrams of the Schatzker 5 pattern, the
intercondylar eminences are intact with fractures of both condyles.
This pattern occurs only rarely if at all. The category Schatzker 6 is
important because it identifies a pattern where the diaphysis is
separated from the metaphysis with fractures proximally involving the
articular surface. Complications are frequent and treatment must be
designed to minimize risks. However, because of the problems with the
Schatzker 5 category, the 6 category is often used for any bicondylar
fracture. The common bicondylar pattern where both condyles are broken
without any intact articular surface or intercondylar eminences but the
shaft is not separated from the metaphysis is not easily classified in
the Schatzker classification. Despite these problems, the terms in the
Schatzker classification appear frequently in this chapter and in the
vernacular of most surgeons, so it is important to be familiar with
them:
split fractures have a single fracture line creating a marginal
fracture across the lateral plateau. These fractures are less common
than type 2 because any split is usually accompanied by some degree of
marginal depression along the split fracture line. They occur more
commonly in younger patients. Schatzker et al.143 identified four of these fractures from among 70 reviewed, and Hohl71 found them in only 3% of plateau fractures (Fig. 53-10).
found them to occur with equal frequency. The depression is the
marginal impaction at the edges of the split fragment. The relative
size of the split fragment and the amount of depression vary, ranging
from minimally displaced fractures to explosion fractures of the entire
lateral side of the joint and with a fractured fibular head (Fig. 53-11).
compression fractures are lateral. Although it is implied that this
type of fracture does not have a split fragment, only local depression,
there frequently is a small split through the lateral cortex. However,
the split is small enough and minimally displaced and does not provide
an easy window of access to the depression. This fracture tends to
occur in an older age group143 (Fig. 53-12).
entire condyle is split as a single fragment or it may have a
comminuted joint depression component. The fracture line is usually
through the intercondylar region although it may be through the
opposite lateral condyle, but some portion of the lateral
condyle
is left unfractured. With large medial condyle fractures, the intact
lateral condyle displaces laterally from the femur, leading to a
fracture dislocation pattern. These severe injuries have a risk of
associated injuries, including compartment syndrome, peroneal nerve,
and vascular injury. Wahlquist et al.165
found that the more the fracture line moves laterally, the greater is
the risk for these associated complications. Schatzker et al.143 thought that these fractures had the worst prognosis. Chan et al.31 found a high incidence of associated anterior cruciate ligament (ACL) tears with posteromedial fracture patterns (Fig. 53-13).
 |
|
FIGURE 53-10 A split fracture (AO/OTA type B-1, Schatzker 1) illustrated in (A) a drawing, (B) an anteroposterior radiograph, and (C) a coronal CT cut.
|
pattern was originally described by Schatzker as a fracture where both
the medial and lateral tibial plateaus are fractured. The
distinguishing feature was that the metaphysis and diaphysis remain
intact and not fractured. The intercondylar eminences may or may not be
fractured. The diagram in Schatzker et al.143
from 1979 shows them to be intact. The type 5 fracture in this diagram
has fractures of both plateaus with the intercondylar area intact. This
is extremely uncommon, and in the original paper Schatzker et al.143
identified only 2 of 70. There are patterns where some portion of both
condyles are fractured and some portion of one or both condyles remains
intact. For instance, there are medial and lateral partial condylar
fractures but typically the intact portion is not the area of the
intercondylar eminences. More commonly, these are posterior or anterior
fracture patterns where the fractures of the
two plateaus are mostly in the coronal plane, leaving the anterior or posterior portion of both intact29 (Fig. 53-14). Barei et al.13
noted that approximately one third of bicondylar fractures have a
posteromedial fracture and described the characteristics of this
associated pattern. This information is important when a surgeon is
planning to treat a bicondylar fracture with laterally based locking
plates.
 |
|
FIGURE 53-11 A split depression fracture (AO/OTA B-2 and -3, Schatzker 2) illustrated in (A) a drawing, (B) an anteroposterior radiograph, and (C)
a coronal CT cut. These images show a more severe high-energy pattern than is typical. Note the lateral femoral condyle impaled in the lateral tibial plateau, illustrating the mechanism of injury (B). |
 |
|
FIGURE 53-12 A local compression fracture (AO/OTA B-2, Schatzker 3) illustrated in (A) a drawing and (B) a coronal CT cut. There may be a subtle split fragment.
|
most classic bicondylar patterns, the shaft is separated from the
condyles (there is no articular surface intact or in continuity with
the shaft below). The defining characteristic of the Schatzker 6
pattern was a diaphyseal metaphyseal dissociation with varying
comminution of the articular surface.143 According to this definition, the distal extent of the fracture is more distal in type
6 than in type 5. Unfortunately, just when the change from 5 to 6
should occur is not precisely defined and is subject to observer
interpretation and therefore variability. The degrees of displacement
and comminution of the two articular surfaces vary, and there is no
subclassification of this pattern. The classic Schatzker 6 from the
original diagrams is a proximal shaft fracture with extension into the
joint. One of the weaknesses of this classification is the wide range
of patterns requiring different management strategies that all fit in
the 6 category. These are mostly high-energy fractures (Fig. 53-15).
 |
|
FIGURE 53-13 A medial condylar fracture dislocation (AO/OTA type B-3, Schatzker 4) illustrated in (A) a drawing, (B) an anteroposterior radiograph, and in two rotations of three-dimensional imaging (C,D). Note the dislocation of the lateral plateau from the femoral condyle.
|
 |
|
FIGURE 53-14 A bicondylar fracture. The illustration (A)
shows the intercondylar eminence intact but in most bicondylar fractures the entire proximal tibia is completely fractured (AO/OTA type C3) (B,C). If the shaft is dissociated from the metaphysis, this would be a Schatzker 6. This distinction would lead to differences of opinion among experienced observers. |
classifying tibial plateau fractures. Similar to many fracture
classifications, the AO/OTA and the Schatzker classifications of tibial
plateau fractures have been found to have less than excellent
interobserver reliability. In one study, the AO/OTA was found to be
more reliable than the Schatzker classification and to be more reliable
at the type than the group level.166 Another study found that simple use of unicondylar versus bicondylar and split versus split depression was more reliable than either the Schatzker or the
AO/OTA classification.35
One study looked at fracture characteristics that form the bases of all
plateau classifications and found that even simple terms like displaced versus nondisplaced and comminuted versus not comminuted led to significant observer disagreement.114
These studies indicate that the common fracture classifications and
even the terminology used for tibial plateau fractures are only
modestly reliable.
 |
|
FIGURE 53-15 A shaft dissociated fracture (AO/OTA type C-2, Schatzker 6) illustrated in a drawing (A) and in anteroposterior and lateral radiographs (B,C).
|
the forces applied combined with the osseous anatomy of the proximal
tibia. Occasionally, muscle forces or ligament attachments play a part
in the fracture pattern.
diaphysis to the proximal tibia. In the proximal quarter, the anterior
proximal tibia widens to become the tibial tubercle for attachment of
the patellar tendon. Just above this, the proximal lateral tibia
abruptly flares from the smooth anterolateral surface to form the
lateral tibial condyle, which serves as the origin of the anterior
compartment muscles, and more proximally has Gerdy’s tubercle for the
insertion of the iliotibial band. Posteriorly on the lateral side, the
fibular head serves as a palpable landmark and as the site of
attachment of the fibular collateral ligament and the biceps tendon. It
defines the position of the peroneal nerve, which rests on the
posterior neck of the fibula. The proximal fibula buttresses the
lateral plateau, and associated fractures of the proximal fibula result
in a greater degree of
valgus
instability and indicate a more severe lateral fracture. The proximal
tibiofibular joint is a synovial joint that may communicate with the
knee joint.
condyle is more gradual directly medial and more abrupt and flared
posteromedial. Angular forces to the knee and compression and axial
loading lead to failure through these flared condyles on the lateral or
medial sides or with straight axial loading on both sides. The medial
plateau is more resistant to failure than the lateral plateau.
flat or slightly convex in relation to the medial tibial plateau that
is concave, which provides greater congruity with the medial femoral
condyle than on the lateral side. This anatomy is important when using
radiographs and fluoroscopy during surgical treatment because it allows
separate assessment of the two plateaus on the lateral radiographs. The
lateral plateau is also higher than the medial plateau, accounting for
the few degrees of varus of the tibial plateau in relation to the
shaft. The proximal articular surface slopes in relation to the shaft
from the front, which is high, to the back, which is low. In a study
using MRI, Hashemi et al.68 found
that the average values were around 5 degrees for sagittal slope and 3
degrees for coronal slope. However, these angular relationships of the
tibial plateau had significant variation between individuals, with the
range of varus coronal slope between -1 and +6 degrees and the sagittal
slope from 0-14 degrees on the lateral side and -3 to +10 degrees on
the medial side.68 These variations
between individuals are potentially important for tibial plateau
fracture surgery since small degrees of malalignment may be considered
important. Assessing alignment in comparison to the nonfractured side
is prudent.
covered by hyaline cartilage and are partially covered by the
fibrocartilaginous menisci, both of which are attached to their
respective plateaus by the meniscotibial ligaments (coronary
ligaments). There is greater meniscal coverage of the lateral plateau
than the medial plateau. The intercondylar eminence and medial and
lateral tibial spines, which are nonarticular, separate the two
plateaus. They also serve as attachment for the ACL anterior to the
medial spine and the posterior cruciate ligament (PCL) that extends
down to the posterior surface of the proximal tibia.
largely subcutaneous. The posterior tibia is deep beneath the
structures crossing the popliteal fossa, making direct surgical
exposures in this area difficult. The anterior tibia is more accessible
but particularly the medial surface is at risk for surgical incisions
in high-energy fractures. The pes tendons, gracilis, sartorius, and
semitendinosis insert on the anteromedial portion of the proximal tibia
distal to the insertion of the patellar tendon on the tibial tubercle.
Before the insertion, these tendons give off expansions to the fascia
of the lower leg. The posterior aspect of the pes expansions must be
incised to retract the pes tendons anteriorly during the posteromedial
approach. The anterior compartment muscles, tibialis anterior and
extensor digitorum longus, arise from the inferior surface of the
lateral condyle of the tibia. The origin must be elevated to place an
anterolateral tibial plate. The medial head of the gastrocnemius arises
from the posterior femur just above the posterior medial femoral
condyle. It can be retracted laterally or, if necessary, the origin can
be incised to enhance exposure of the posteromedial and posterior
tibial plateau.
biceps femoris and is on the back of the neck of the fibula. It is not
at risk during most surgery for tibial plateau fractures as long as the
surgeon remains aware of the position of the fibula. Rarely, a
posterolateral approach may be chosen in which case the peroneal nerve
must be identified and mobilized. It is at risk from direct lateral
impact mechanisms and with high-energy fractures of the tibial plateau,
particularly medial plateau fractures which produce varus alignment.
The tibial nerve in the popliteal fossa is rarely injured and rarely
part of surgical approaches for tibial plateau fractures.
dislocations, is rarely injured with tibial plateau fractures. However,
the trifurcation of the popliteal artery occurs in an area where
plateau displacement is likely with certain fracture patterns and the
anterior tibial artery is bound at the interosseous membrane and is at
particular risk in shaft-dissociated patterns. Occult injury to the
anterior tibial artery may account in part for the compartment
syndromes frequently associated with these fracture patterns.
reduce and internally fix tibial plateau fractures: the anterolateral
approach and the posteromedial approach. They are used in isolation for
fractures on the lateral and medial side of the knee, respectively,
and, not uncommonly, they are used together for patterns that involve
both condyles. These two approaches with common variants can be used to
treat virtually all tibial plateau fractures. In current practice, most
other approaches have become unusual or reserved for special
circumstances.
It is the workhorse approach for split depression fractures of the
lateral plateau. The incision is based over Gerdy’s tubercle and is
extended distally over the anterior compartment. An L-shaped incision
in the origin of the anterior compartment muscles provides access to
the anterolateral surface of the tibia. Care should be taken along the
posterolateral border of the tibia as the anterior tibial artery passes
through the interosseous membrane from back to front.
variable based on surgeon preferences for joint exposure. For
fluoroscopic or arthroscopic reductions, the proximal exposure develops
subcutaneous access posteriorly toward the fibular head for placement
of a lateral tibial plate. The knee joint is not opened or further
exposed. Alternatively, two different exposures can be used to directly
visualize the lateral joint. In one of them, the deep dissection is
brought posteriorly along the tibial margin of the joint line, incising
the coronary ligament to create a submeniscal arthrotomy. With a long
enough inframeniscal incision, the meniscus can be retracted proximally
to expose the tibial side of the lateral joint beneath the meniscus.
Cross-joint distraction facilitates visualizing the joint through this
submeniscal arthrotomy. This approach has been credited
to the AO group.120
The coronary ligament is repaired at the end of the procedure and has
been found to heal in a dog model of this submeniscal arthrotomy.30
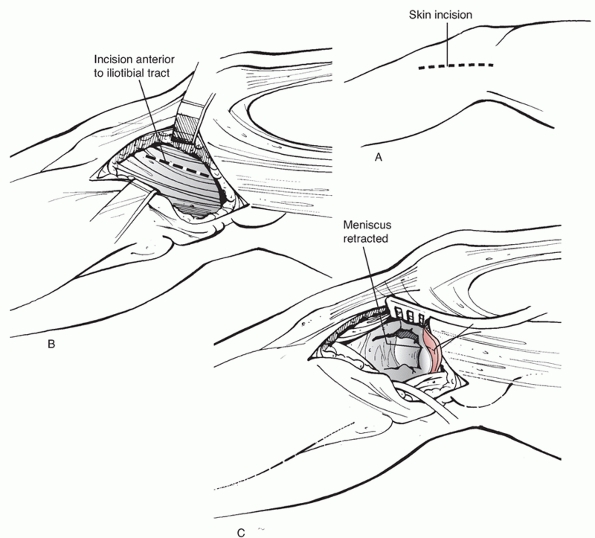 |
|
FIGURE 53-16 A. Anterolateral approach to the tibial plateau with alternate techniques to expose the lateral joint. B. A submeniscal arthrotomy through the coronary ligament. C. An anterior joint arthrotomy with detachment of the anterior horn of the meniscus.
|
and an anterolateral joint arthrotomy is created. In this approach,
exposure of the joint is from above the meniscus. The ability to
visualize the tibial fragments is increased by incising the anterior
portion of the coronary ligament and the intermeniscal ligament
detaching the anterior horn of the lateral meniscus that can then be
retracted laterally with the split fragment opening the joint through
the fracture. These are repaired with sutures at the end of the
procedure.127 Arthroscopic evaluation of the anterior horn has shown that the incised meniscus heals.125,127
approach, is used to reduce and fix the medial side of the proximal
tibia and particularly the posteromedial fragment (Fig. 53-17).
It has the advantage of relatively good soft tissue cover and it is
widely separated from the anterolateral approach allowing these two
approaches to be combined when necessary. In addition, the fracture
fragments often have extra-articular fracture lines, which are not
comminuted and are relatively easy to reduce. A posteromedial plate
when optimally positioned is well suited to resist deforming forces. An
antiglide plate is placed directly over the area of maximal
displacement at the apex of the fracture.
the tibia. The patient is most commonly positioned supine, which allows
access to the front of the knee for a second anterolateral approach or
to apply a distracter.62 The leg is
externally rotated, allowing easy access. Alternatively, the patient
can be positioned prone, which makes the posterior to anterior hardware
easier to place and facilitates fracture reduction by knee extension.40
The subcutaneous dissection must avoid the saphenous nerve and vein,
and the incision must be posterior enough to allow hardware to be
placed from the posterior aspect of the tibia without the posterior
skin flap obstructing the screw paths. The deep interval is between the
posterior border of the pes anserine tendons and the medial head of the
gastrocnemius. A retractor under the medial head protects the popliteal
fossa structures. The origin of the medial head may be incised to
increase exposure, but this is rarely necessary.19,40
To directly visualize the bone, the popliteus origin must be lifted and
retracted laterally. This often directly exposes the apex of the
fracture.
 |
|
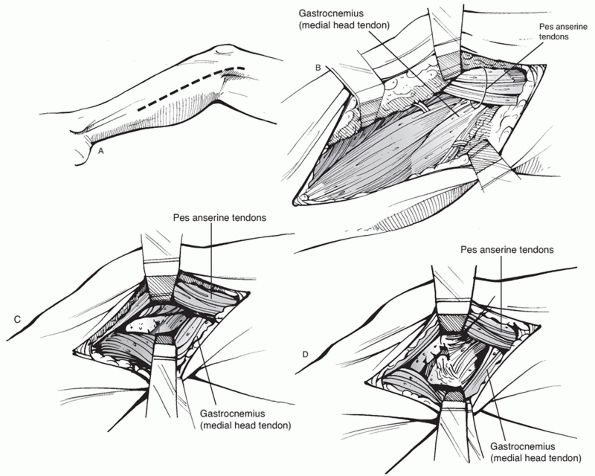
FIGURE 53-17
Posteromedial approach to the medial tibial plateau. The pes is retracted anteriorly and the medial gastrocnemius is retracted posteriorly. |
through distal extension of a medial arthrotomy similar to a total knee
approach. However, it is unusual for fracture patterns to involve the
anteromedial tibia in isolation. An anteromedial approach should not be
used in conjunction with the common anterolateral approach. Usually,
medial patterns involve the posteromedial plateau, which requires a
posteromedial approach. Occasionally through the same incision, a
separate anteromedial interval in front of or between the pes tendons
can be used to reduce and fix the front of the medial joint through the
posteromedial approach.
which is difficult to stabilize from an anterolateral approach with the
fibular head in the way. If the posterior plateau is comminuted far
onto the lateral side, it cannot be reached through the posteromedial
approach. In these cases, a posterolateral approach between the lateral
gastrocnemius and the biceps femoris with mobilization of the peroneal
nerve will provide access to the posterolateral tibial plateau. This
can be combined with a posteromedial approach as described by Carlson.28,29
The exposure obtained is similar to familiar approaches for knee
arthroplasty. They provide simultaneous access to both the medial and
lateral sides of the tibial plateau. Exposures where the extensor
mechanism is elevated with a tibial tubercle fracture or through
incision of the patellar tendon combined with anterior meniscal
incision provide an intra-articular exposure to reduce fractures that
are not possible with any other approach. Unfortunately, these
exposures, when combined with dual plating, lead to excessive soft
tissue stripping and devascularization of damaged fracture fragments,
and when they resulted in infection and/or wound breakdown, disastrous
results followed. For these reasons, alternate techniques should be
chosen if at all possible. Current opinion and data indicate that dual
plates can be reasonably safely applied to the fractured proximal tibia
but that dual approaches are safer than extensile approaches.
used the Lobenhoffer approach for posteromedial fractures. This
approach uses the same interval as the previously described
posteromedial approach between the pes tendons and the medial
gastrocnemius. Carlson28,29
described combined posteromedial and posterolateral approaches to the
back of the tibial plateau. These are efficacious for posterior
shearing patterns where direct posterior plating is mechanically
optimal. A posterior approach in the prone position has the advantage
of reducing the fracture with the knee in extension with a more direct
view of the fracture and screw paths. In addition, taking the medial
head down makes for a more extensile exposure to visualize comminuted
fractures. These advantages are offset by the more difficult
positioning compared to the supine posteromedial approach and lack of
readily available access to the lateral side for bicondylar fractures.
combined approaches using an anterolateral approach and posteromedial
approach as described earlier.62
Dual approaches provide access to complex bicondylar fractures but
strip less soft tissue attachments than extensile anterior approaches.
The patient is positioned supine and the leg must externally rotate for
the posteromedial portion of the approach. Anterolateral and
posteromedial incisions are nearly at 180 degrees from each other, so
short skin bridges are not an issue. Direct access to each injured
condyle to reduce the fracture and to place implants is obtained, which
minimizes the soft tissue dissection required.
surface require surgery and not all displaced intra-articular fractures
need to be surgically reduced. The proximal tibial articular surface
tolerates small to modest articular displacements and, in properly
selected fractures, nonoperative treatment results in predictably
excellent outcomes despite articular irregularities. Progressive
incapacitating posttraumatic arthritis is actually very unusual.
maintain a closed reduction of the proximal tibia and, for many
displaced fractures, it is impossible. Nonoperative treatment is
therefore indicated for tibial plateau fractures that will heal without
a significant deformity or for elderly patients or patients with
associated medical problems where operative intervention is high risk
or otherwise undesirable and for whom a deformity will be clinically
acceptable.
predicting the presence or absence of a deformity after treatment is
very important (Fig. 53-18). Angular deformity
is not well tolerated by the articular surface since typically the knee
will be malaligned in a direction that increases the weight-bearing
load on the most damaged portion of the articular surface. Malalignment
increases the propensity for knee instability and is cosmetically
objectionable.
be difficult. To make this judgment, a surgeon must use information
about the fracture pattern, knowledge of outcomes of various types of
fractures, and the alignment both on injury radiographs and on clinical
examination. The type of fracture is critically important to choosing
nonoperative treatment and to achieving a good result. Although the
amount of articular displacement and the risk for deformity have some
relationship to each other, it is not a direct relationship. Localized
depressions of up to 10 or more millimeters of the lateral plateau may
result in stable knees and good outcomes when treated nonoperatively,
if the depression involves a small portion of the articular surface.
Depressions with associated displaced split fragments or those that
involve larger portions of the lateral articular surface will be more
likely to lead to valgus malalignment. Different from the lateral
plateau, a minimally displaced medial total condylar fracture has a
greater potential for displacement that may lead to unacceptable varus
deformity. The medial articular surface is less well protected by the
meniscus, so it is more important to minimize the amount of articular
steps or other displacements on this side of the knee.
operative versus nonoperative treatment for tibial plateau fractures on
a predetermined number of millimeters of displacement of the articular
surface is not sensible and does not account for important knowledge
about how different tibial plateau fracture patterns have more or less
propensity to lead to deformity and subsequent favorable or unfavorable
outcomes.
side of the joint. They once were commonly used to stabilize the
injured joint while permitting some degree of joint mobility.42,43,146 DeCoster et al.42
showed that alignment within 7 degrees of normal was obtained in all 30
plateau fractures treated with a cast brace. Delmarter and Hohl43
used cast bracing as both a primary nonoperative treatment and as an
adjunct to open reduction and internal fixation and showed that 85%
maintained alignment in the cast brace. Currently, cast braces are not
commonly used since most unstable plateau fractures are treated
surgically and most surgical techniques achieve enough stability that a
cast brace is not necessary. Tibial plateau fractures that are
inherently stable or stabilized surgically do not need this additional
protection and a lighter, removable brace is preferred.
tolerate up to 6 weeks of cast immobilization, most surgeons prefer
early mobilization with a hinged brace, which allows joint mobility and
provides some coronal support.
nonoperatively treated tibial plateau fractures should be kept
non-weight bearing during the initial weeks after injury. The duration
of non-weight bearing depends on the fracture pattern but is typically
4 to 8 weeks. Scotland and Wardlaw146 reported that plateau fractures treated in a cast brace could weight bear early,
within a few days or weeks after injury; however, this technique is not often used in current practice.
 |
|
FIGURE 53-18
Anteroposterior and lateral radiographs of a 28-year-old patient who slipped and fell. The fracture of the lateral plateau is hard to see on the anteroposterior radiograph (A) but the lateral radiograph (B) shows the anterior plateau depression. Follow-up radiographs 6 months after injury (C,D) show healing. The patient was back to work, the clinical outcome was excellent, and the leg remained well aligned. |
nonoperatively have been reported. Although there are no recent
reports, older series provide important information. Since the
indications to treat plateau fractures nonoperatively have narrowed
considerably, the older series can be considered worst case compared
with those treated nonoperatively in current practice.
thought early joint mobility and exercises contributed to their favorable outcomes. Jensen et al.83
compared traction to surgery and found equivalent outcomes, although
not surprisingly surgery led to shorter hospital stays. On the other
hand, motion must not be critical because Drennan et al.47
reported 85% good and excellent results with good motion at follow-up
in patients treated with closed reduction and a spica cast for 6 weeks.
reported on a 20-year follow-up of nonoperatively treated patients
originally reported by Rassmusen. Surgical treatment was reserved for
patients with greater than 10 degrees of coronal plane instability in
full extension.131 The patients
achieved 90% good and excellent results, which indicate that lack of
significant instability in full extension is associated with good
results after nonoperative treatment. Although this information is
helpful in clinical decision-making in some cases, it is of limited
value since it is often difficult to reliably examine an acutely
injured knee to determine the degree of instability.
found that 5 mm of widening and 3 mm of step-off were well tolerated
but that any medial side displacement or tilt should be avoided.
reported excellent results for 29 patients treated in a cast brace and
emphasized early weight bearing and return to function. DeCoster et al.42
followed 30 plateau fractures treated with a cast brace and found that
the outcome of the knee was less favorable for more complex bicondylar
fractures.
reported good results after nonoperative or limited surgical approaches
and noted that excellent clinical outcomes did not correlate well with
the radiographic appearances of the knee.
possible for many tibial plateau fractures without surgery, despite
articular incongruities and displacements. It is important to maintain
limb alignment, and this may require external support with a cast brace
and, for some fractures, traction or other methods. In current
practice, patients with fractures similar to those in many of the cited
studies are treated operatively, which ensures accurate limb alignment,
early motion, and better reductions with less external support.
However, the favorable results of nonoperative treatment should be
considered when a patient with a tibial plateau fracture has
significant comorbidities, is elderly with osteopenic bone, has poor
skin, or does not want an operation. An excellent outcome without
surgery is possible for many tibial plateau fracture patterns.
tibial plateau fractures where near-normal limb alignment cannot be
predicted based on the fracture pattern or physcial examination. In
young healthy patients, this will include almost all bicondylar and
shaft dissociated patterns, and all but minimally displaced medial
plateau fractures and lateral plateau fracture patterns where valgus
alignment will occur without surgically reducing and fixing the
fracture. For the lateral patterns, the presence of a split fragment, a
depression affecting over half of the lateral articular surface, a
fibular head fracture, valgus alignment on injury radiographs, and
clinical valgus alignment on examination are all strong indications for
surgery.
surface measured on radiographs has been frequently used to indicate
surgery. Unfortunately, depression is difficult to measure accurately
and reliably on plain radiographs (Fig. 53-19). Martin et al.112
found that when observers make measurements independently of each
other, their measurements are different from each other by at least 12
mm 10% of the time. In addition, the size and location of the depressed
area all make a difference in whether a certain amount of depression
will be clinically significant. The number of millimeters is not
reliable and too simplistic to be a good way to determine surgical
indications.
unfit patients, the indications for operative treatment are narrower
and the risks and benefits of surgical intervention must be carefully
assessed on a case-by-case basis. In these patients, a deformity will
be less significant, functional demands are less, and surgery is
potentially more difficult with more osteopenic bone (Fig. 53-20). The results of surgery in elderly patients are generally less satisfactory than in young patients.11,75,88,145,170
favorable patient outcomes depend on the patient and the fracture
pattern. A variety of techniques are currently popular and have good
results reported in the literature, and new techniques continue to be
developed. However, for a given patient with a given
fracture
pattern, there is little evidence to indicate one technique is superior
to others. For instance, for one of the most common fracture patterns,
a split depression lateral plateau fracture, currently acceptable
techniques for visualizing the articular surface reduction include
fluoroscopic, arthroscopic, and joint arthrotomy with meniscal
incision. The same fracture might be stabilized with either small or
large plates and screws, or screws alone. Numerous materials to fill
the void created after reducing the fracture would be considered
acceptable choices. As another example, there has been a wave of
popularity for treating AO/OTA C fractures and Schatzker 6 patterns
with locking plates without any evidence that outcomes are better than
with previous techniques. It is even difficult to know which fractures
are benefited by surgical management.
 |
|
FIGURE 53-19
This anteroposterior radiograph demonstrates a typical split depression fracture of the lateral plateau. If different surgeons measured the number of millimeters of articular depression, there would be wide variability in the results. For example, which arrow represents the maximal articular depression? |
 |
|
FIGURE 53-20
Nonoperative treatment plays a greater role in elderly patients with limited function, medical comorbidities, and osteopenic bone. A 76-year-old woman with medical comorbidities slips and falls. Anteroposterior and computed tomography cuts (A,B) show a significant joint depression lateral plateau fracture. (C) Three years after nonoperative treatment, radiographs show slight valgus alignment with a relatively preserved joint. The patient returned to her previous level of activity. |
fracture, the fracture pattern will dictate the operative approach, the
technique of reducing the fracture, and the appropriate use of internal
or external fixation devices. In addition to assessing the fracture
pattern, the surgeon must decide how to visualize the articular
reduction and whether to assess and manage associated meniscal and
ligament injuries as part of an operative treatment plan.
an important aspect of treating displaced plateau fractures. In
planning a surgical case, the surgeon has choices on how to assess and
visualize the reduction. The articular reduction can be assessed
indirectly by fluoroscopy, with an arthroscope, or directly through an
arthrotomy to see the articular surface. Some surgeons favor one
approach over another, and others choose different approaches based on
the fracture pattern.
directly assess the fracture reduction through a joint arthrotomy. In
lateral side patterns, the meniscus can either be incised anteriorly or
elevated with a submeniscal arthrotomy. Both approaches allow the
articular reduction to be directly assessed under direct vision. The
meniscus and arthrotomy are repaired during closure.
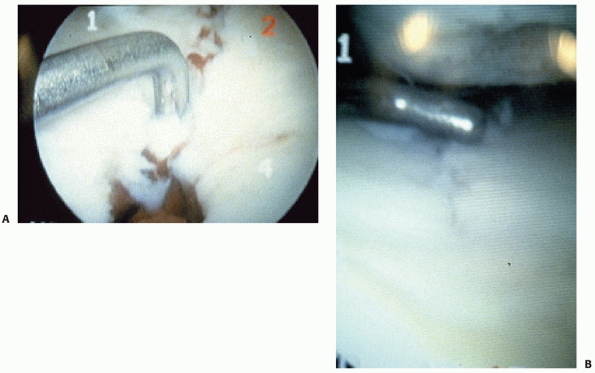
reduction have been used by some surgeons for a wide range of fracture
patterns for more than two decades81 (Fig. 53-21).
With arthroscopic techniques, the fractured articular surface is
visualized less invasively than with wide arthrotomies and detaching or
elevating the meniscus. In addition to assisting with fracture
reduction, arthrosocpy has the further advantage of allowing associated
intra-articular soft tissue injuries to be directly assessed and
treated.163 Faster rehabilitation and more accurate reductions compared to open techniques with arthrotomy have been reported.24 Most authors have reported results that are similar to or better than more traditional open procedures,56,79,101,105 but directly comparing the two techniques is difficult because of potential differences in case selection.74,105
Although mostly used for split, split depression, and local compression
fractures, arthroscopy has been used for higher energy fractures.33,81 Good results have been reported for arthroscopic treatment for elderly patients, mostly for lower energy fractures.37
plateau fractures because it is used to assess the placement and final
position of hardware in relation to fracture lines and the articular
surface. Final assessment of fracture reduction is frequently by
fluoroscopy. Therefore, using fluoroscopy to assess the reduction is
frequently part of the operative plan. However, using fluoroscopy
exclusively as a guide to reducing depressed fragments is challenging
and not universally accepted. It has the advantage of being less
invasive than joint arthrotomy and does not require the extra equipment
and joint distention required for arthroscopy. Koval et al.96
indirectly reduced 18 plateau fractures using fluoroscopy and fixed
them with screws and had 13 excellent reductions. They noted more
difficulty accurately reducing fractures with depressed fragments,
although, interestingly, all cases with incomplete reductions had
excellent outcomes. Other authors have reported similar experiences
with simple cases amenable to fluoroscopic assessment alone and more
complex cases requiring adjunctive arthrotomies or arthroscopy.49,67,92
In a comparative study, Loebenhofer et al. found that fluoroscopic
assessment of the plateau with a C-arm was equivalent to and
technically easier than assessing it with an arthroscope. Patients
assessed with fluoroscopy alone did not have clinical problems
secondary to unrecognized soft tissue injuries.104
 |
|
FIGURE 53-21 Arthroscopic assessment of a split fracture (A) and the fracture line after it has been reduced (B).
|
fractures and may or may not need to be incorporated into an operative
plan. There are two important types of soft tissue injuries. First
there are injuries to menisci and ligaments and second there is the
injury to the surrounding soft tissue envelope that increases the risks
for complications and must be considered when managing tibial plateau
fractures.
incidence of ligament and meniscal injuries associated with tibial
plateau fractures. When assessed by MRI, one study found that even
minimally displaced tibial plateau fractures indicated for nonoperative
treatment had a high percentage of these injuries (meniscal 80%, ligament 40%).152
In another study of MRI findings in 103 patients with operatively
treated tibial plateau fractures, all but one patient had some soft
tissue injury with lateral meniscus (91%), most commonly followed by
ACL (77%), posterolateral corner (68%), and medial meniscus (44%).58
Similarly, in knees evaluated arthroscopically during operative
treatment of a tibial plateau fractures, 71% (70 of 98) were found to
have meniscal or ligament injuries at a rate of 57% for meniscal, 25%
for ACL, 5% PCL, and 3% each for MCL and LCL.1
The authors of this study could not demonstrate a strong association
with fracture type although ACL injuries were more common in total
condylar and Schatzker 6 patterns. In another study, the incidence of
meniscal injury in split depression patterns was found to correlate
with the degree of depression and condylar widening.57 Looking specifically at ligament injuries using stress radiographs and intraoperative findings, Delamarter et al.44
found that in 39 tibial plateau fractures evaluated there were 22 MCL,
8 LCL, 1 ACL, and 8 combined ligament injuries. Unfortunately, the
clinical significance of these soft tissue injuries when associated
with a tibial plateau fracture is not known.
is controversial. Conservatively managing MCL injuries is generally
favored so most surgeons do not currently advocate diagnostic or
treatment strategies for an associated MCL injury. In addition, the
medial ligament does not present long-term problems and residual laxity
usually relates to bony depression rather than collateral ligament
laxity. At an average of nearly 3 years after injury, Moore at al.116
tested 208 patients with unicondylar tibial plateau fractures for varus
or valgus laxity using stress radiographs. They found that compared to
the uninjured knee, there was no increased laxity to suggest chronic
collateral ligament damage. This was despite calcification in
collateral ligaments in one of seven knees. This information suggests
that after reducing and fixing a lateral plateau fracture, a brace is
sufficient to treat the associated collateral ligament injury.
and ligament injuries that are frequently present is controversial.
Some authors recommend an aggressive approach to both diagnosis and
surgical repair.17,81,163 Other authors have found that the patient’s function and outcome are excellent without addressing these injuries.27,111
The meniscus is important in preventing posttraumatic osteoarthritis
(OA), and many operative techniques stress meniscal repair.14
However, the vast majority of minimally displaced tibial plateau
fractures have excellent outcomes without addressing associated
meniscal or ligament injuries. For these minimally displaced fractures,
as for all tibial plateau fractures, it is difficult to know which soft
tissue injuries need to be managed surgically to improve patient
outcome. Many severe tibial plateau fractures have excellent outcomes
after being treated surgically with techniques that do not routinely
evaluate or repair meniscal injuries.111
These results indicate that meniscal injuries either heal or are not
symptomatic in patients after tibial plateau fractures. Reattaching an
avulsed ACL or PCL, particularly when it is associated with a fracture
fragment, is recommended by the authors of some series of high-energy
fractures.16,37
In one comparative study, better results were found in fractures where
the ligaments were surgically repaired compared to fractures treated
without ligament repair.178 However, other series of high-energy fractures have reported good results without ligament repair,159,177 and many reports on high-energy fractures do not indicate whether ligament injuries were addressed surgically.53,164,166
Some surgeons order MRI routinely to assess tibial plateau fractures
and the associated soft tissue injuries, and others reserve it for
cases where there is a particular concern about the status of the
ligaments or the menisci that would not be otherwise assessed through
the operative approach.
a severe injury to the overlying soft tissues. The worst soft tissue
injuries typically occur with bicondylar fractures,
fracture-dislocations, and shaft dissociated patterns. These
high-energy patterns may require extensive surgical approaches with
substantial implants, and the risk of these procedures is increased
because of the injury to the soft tissues. Open tibial plateau
fractures may be clinically obvious, but subtle wounds or abrasions in
the zone of injury must be assessed with suspicion for being an open
fracture. When there is doubt, these suspicious wounds should be
explored. Fracture blisters occur when the soft tissue injury is severe
and may be red or white; red blisters represent a deeper dermal injury.
Tense swelling and deep contusions are additional signs of severe
fracture associated soft tissue injury. Severe closed soft tissue
injuries take many days or even weeks after the injury to recover. If
mismanaged, surgical approaches that are performed during the period of
intense swelling before recovery pose a high risk for wound
complications.
the operating room. Soft tissue coverage may be needed, and this can
frequently be accomplished with a rotational flap from the medial or,
less commonly, lateral head of the gastrocnemius.
frequent implants used to stabilize tibial plateau fractures, and all
major manufacturers have recently developed precontoured periarticular
plates and locking plates, resulting in more plate choices than have
ever been available in the past. The simplest implants are lag screws
used to compress simple fracture lines in isolation or in conjunction
with other fixation devices. For compression, partially threaded screws
are most common and 6.5-mm screws work well for major plateau fracture
lines, although smaller screws may work equally well.
fracture pattern and where they are anatomically placed. A common plate
application is for the anterolateral proximal tibia where it is used as
a buttress and to substitute for the damaged lateral cortex that occurs
with lateral split depression plateau fractures. These plates are
precontoured for this anatomic region, which makes obtaining an
accurate fit for buttressing the lateral tibial condyle much easier.
The 3.5-mm implants and screws are the most common size, having largely
supplanted the 4.5-mm implants that were common in the past. The 3.5-mm
implants are less bulky and easier to fit on the bone, and the smaller
3.5-mm screws allow more screws to be placed closer to the articular
surface to support reduced fragments. In cancellous bone, 3.5-mm screws
have been shown to have equivalent pullout strength in comparison to
6.5-mm and 4.5-mm screws.174 Multiple holes in the head of the plate allow 3.5-mm screws to be placed parallel and close to the articular surface to support
the reduced articular surface and minimize the chances for
postoperative settling. This technique has been called “rafting screws.”85,95 It is similar to a technique that used multiple K-wires beneath a lateral fragment as a way to prevent secondary displacement.18
The high incidence of some loss of the articular reduction after
surgically treating lateral plateau fractures, reported in 31% of cases
in one series, means that newer techniques not used in this series,
such as rafting screws, should be very seriously considered.4
function than anterolateral plates. In this area, the plate must
function as an antiglide device to resist shearing forces. Again,
3.5-mm implants are most common and specially contoured plates are
becoming available from several manufacturers. In this area, the plate
position in relation to the apex of the fracture is more important than
the exact placement of screws.
have several advantages. They decrease time spent for intraoperative
plate contouring, facilitate limited approaches when the bone is not
completely visualized to allow contouring, and may assist with
reduction by fitting the fractured bone to the precontoured plate.
However, Goyal et al.65 have shown
that there is significant normal variation in the shape of the proximal
tibia leading to suboptimal fit of precontoured plates to cadaver
specimens, even in ideal laboratory settings. The relevance of this
finding to maintaining fracture reduction is uncertain, but surgeons
can be certain that perfect plate contact with the bone will not
frequently be obtained.
fractures must resist axial, rotational, and bending forces. Locking
screws to the plate has been a great advance in resisting these
mechanical forces, and these implants are currently very popular. They
are larger and use larger screws than those used for unicondylar
fractures based on the need to resist substantial deforming forces.
From their lateral position, they must prevent the tendency of bending
forces to create a varus deformity. By resisting varus collapse, they
have decreased the need for dual plates and for definitive external
fixation.
limited approach with external targeting of the distal screws. They can
now be used with either locked or nonlocked screws. So-called hybrid
techniques use nonlocked screws to pull the bone to the precontoured
plate, and then locked screws are added to resist angular deviation.
Some manufacturers now offer polyaxial designs with flexibility in the
direction of screw insertion combined with fixed angle stability.66
Although many manufacturers have made locking technology for many of
their implants, the use of locking screws for unicondylar tibial
plateau fractures where the plate functions as a buttress (lateral
plateau) or for antiglide (posteromedial plateau) is of uncertain value.
used for tibial plateau fractures has dramatically changed in the past
decade. The advent of locking plates applied through limited approaches
has significantly decreased the amount of external fixation used for
definitive treatment of shaft dissociated and bicondylar patterns.
However, external fixation is now frequently used as temporary
treatment by spanning the knee. This noninvasively restores length and
aligns the fracture during soft tissue recovery before definitive
treatment with internal fixation.
tibial plateau fractures based on surgeon preference or in cases with
severe soft tissue injury, when, despite delay, internal fixation is
not thought to be safe. Most data indicate that external fixation is
equally as effective or more so than plate fixation.170
One recent randomized study of bicondylar fractures by the Canadian
Orthopaedic Trauma Association found that patients treated with
external fixation had similar or better outcomes with less
complications than those treated with dual plating.27
Definitive external fixation can be performed using a variety of
different frames and both wires and pins have been effective. The frame
and the bone fixation elements must be designed to overcome the
deforming forces. Some fixator constructs may be as effective at
resisting deforming forces in bicondylar fractures as dual plates5 (Fig. 53-22).
easily applied. Pin bar frames are most common, allowing pin spread and
frame geometry to be designed based on the needs of the fracture and
associated soft tissue injury (Fig. 53-23). The
tibial pins should be placed in a way so not to interfere with
subsequent procedures for internal fixation, keeping potentially
contaminated pin sites away from future incisions and internal fixation
devices. Radiolucent carbon bars facilitate imaging after the frame is
applied. The major goal is to restore and then maintain length and
align the fracture and knee joint. This may require significant
distraction forces. Spanning frames need to be used only for severe
fractures with marked displacement, shortening, or joint subluxation.
They are rarely necessary for routine lateral plateau fractures and
usually are not needed for medial plateau and bicondylar fractures that
are only minimally displaced. Widely displaced fractures with soft
tissue injuries such as tense swelling, fracture blisters, compartment
syndrome, or open wounds are the best indications for temporary
spanning frames. The use of a staged protocol has been reported to
decrease the wound complication rate, but there are no comparative
studies.51
reducing depressed tibial plateau articular fragments, typically those
of the lateral plateau, leads to empty areas in bone or voids beneath
the reduced fragments. The cancellous trabeculae are compressed by the
injury resulting in loss of substance after the articular fragments are
reduced. Given the excellent healing potential of these cancellous
fractures, these voids do not present a risk for failure of healing.
Rather, they are an area that lacks support for the reduced articular
fragments, increasing the risk that the articular fragments will
redisplace despite internal fixation. To minimize this risk, it has
been a principle of lateral plateau fracture surgery to fill the void
to increase stability and prevent redisplacement. Classically, the most
common material for “grafting” the void has been autograft, most
frequently from the iliac crest.98,140,164 In severe cases, tricortical iliac graft has been recommended147 and, where support of reduced fragments is not possible, replacement of the lateral plateau with a patellar graft.80,177
For many surgeons, allograft has supplanted autograft. It has the
advantage of being readily available in unlimited quantities and offers
similar handling properties to autograft without donor site morbidity.149
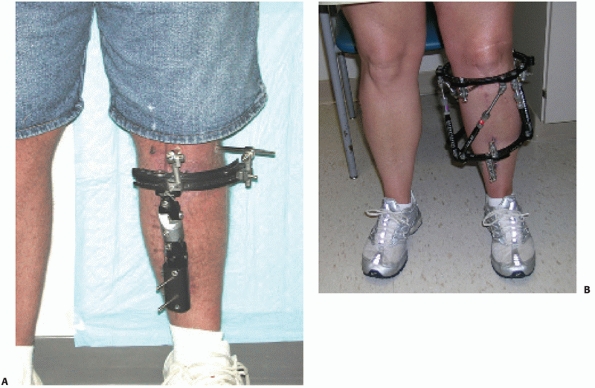 |
|
FIGURE 53-22 Two examples of definitive external fixation frames for tibial plateau fractures. A pin frame (A) with a one third ring and hinges for fracture alignment and a ring frame (B) with spatial hinges.
|
available graft substitutes in mechanical and clinical studies. The
optimal material is currently uncertain, but this is an area of
changing practice. Since subsidence after surgically reducing and
fixing lateral plateau fractures is a real problem, new methods to
support the reduced articular surface are important. Interporous
coralline hydroxyapatite has excellent bone in growth properties72 and, in 1989, Bucholz et al.25
found it to be equivalent to autograft in patients with tibial plateau
fractures. In goats, 3 months after creating a cylindrical defect and
filling it with beta tricalcium phosphate, investigators found less
collapse and more new bone than in similar defects filled with
autograft.175
 |
|
FIGURE 53-23 A simple pin to bar joint-spanning external fixator.
|
which have been shown to have better rather than equivalent mechanical
properties to bone grafts. In a split depression fracture model in
cadavers, a calcium phosphate (Ca-P) cement was significantly stiffer
in compression to cancellous bone.160
In a goat lateral plateau model without internal fixation, Ca-P cement
augmentation led to less secondary displacement than cancellous bone.173
reported in several level 4 studies, and the results have been
generally favorable.78,89,103,153
However, in all of these studies, there remains a small but persistent
rate of subsidence of the lateral articular surface. For instance,
Lobenhoffer et al.103 noted partial
loss of reduction 4 to 8 weeks after surgery in 2 of 25 patients
treated with Ca-P cement. In a randomized controlled trial, Russel et
al.139 found that Ca-P cement
resulted in less articular subsidence than autograft. In a
metaanalysis, fractures in metaphyseal regions treated with Ca-P cement
maintained the reduction better than those treated with autograft and
patients treated with Ca-P cement had less symptoms than control
subjects treated without graft.10
Further clinical investigation will be necessary to confirm these
results, and it will be challenging to prove that outcomes are
improved. However, the potential for better support for the reduced
articular surface should be welcomed because loss of reduction remains
one of the problems with surgery for these fractures.
dictates the operative approach, fixation technique, risk for
complications,
and,
to some extent, outcome. These differences stratify nicely based on the
AO/OTA and Schatzker classifications. There is some variability in the
procedures recommended in the literature for each of these patterns,
but the general principles are similar enough to allow a pattern-based
discussion. For details of surgical approaches, assessment, and
management of meniscal and ligamentous injuries; techniques to assess
reduction; and void fillers, see the previous sections. The following
sections will outline the general range of surgical techniques and
implants used for each of these basic patterns and the fracture
specific results reported in the literature.
 |
|
FIGURE 53-24 A high-energy Schatzker 6 tibial plateau fracture (A) was treated with a spanning fixator (B) and then nailing (C,D).
Although an unusual indication, nailing can be used for patterns such as this one where there is significant distal extension of the fracture into the shaft. |
Lateral Plateau—Limited Approach Techniques With Arthroscopic or
Fluoroscopic Assessment of Reduction. Simple split fractures of the
medial and lateral plateau are the strongest indications for limited
approach techniques that assess the reduction with arthroscopy or
fluoroscopy (Fig. 53-25). These fracture
patterns do not have large depressed fragments, and reducing the split
fragment will accurately align and stabilize the joint and restore the
congruity of the articular surface. The fracture can often be fixed
with percutaneous applied cannulated screws alone. The location and
orientation of the fracture lines can be accurately determined
preoperatively with a CT scan. This information can guide the surgeon
to apply reduction forceps and direct screw paths to optimally reduce
and securely fix the split fracture. Large reduction forceps with a
span to extend between the two plateaus are helpful.
the optimal technique to assess the accuracy of the reduction (see
techniques to visualize the articular reduction). Arthroscopic
techniques directly visualize the articular fracture through a
minimally invasive approach, but fluoroscopic techniques, when used
well, may be equally as effective. To fix the fracture with screws
only, the split fragment needs to be compressed to prevent
displacement. Plate fixation requires an open approach and applies more
bulky hardware. A mechanical study in cadavers has shown no difference
between pure split fractures fixed with 6.5-mm interfragmentary screws
alone and those fixed with screws with the addition of a buttress plate
or the addition of an antiglide screw and washer at the apex of the
fracture.95
 |
|
FIGURE 53-25 A. Injury and (B)
postoperative anteroposterior radiographs of a split fracture that was treated with fluoroscopically assisted percutaneous reduction and 6.5-mm cannulated screws. C. Large reduction forceps assisted in reducing the fracture. This is the most common approach for this fracture pattern and could be combined with an arthroscopic assessment of the reduction. |
fracture through percutaneous techniques is an isolated oblique
shearing fracture of the posteromedial condyle. A split fracture in
this area is less amenable to percutaneous techniques because of more
difficult posterior access and relatively higher deforming shearing
forces. These fractures will more often be handled by a posteromedial
open approach and an antiglide plate.
have reported satisfactory results after closed reduction and screw
fixation alone for split fractures and combinations of split and split
depression fractures and even for relatively minimally displaced
bicondylar fractures.49,67,92,96
The results of treatment of Schatzker type 1 or AO/OTA type B-1
fractures in isolation are difficult to report with great precision
because they are combined with other lateral side patterns. However, in
most series, these fractures seem to have close to or the best outcomes
of all plateau fracture types studied. For instance, Honkonen,75
in a study of seven types of tibial plateau fractures treated with
various operative and nonoperative techniques and followed an average
of 7.6 years, found the least incidence of secondary arthritis in
lateral split fractures. In Schatzker’s orginal report, which described
the six fracture types, the only type that had all satisfactory results
was the type 1 lateral split fracture.22 Koval et al.96
treated 18 displaced fractures by closed reduction and percutaneous
screw fixation; the seven type 1 fractures had four excellent, two
good, and one fair result.
Fractures of the Lateral Plateau—Reduction and Buttress Plate Fixation
and Void Filler. This is the most common operation for displaced tibial
plateau fractures. In this fracture pattern, lateral split fragments
are associated with varying amounts of articular depression. The split
fragment may be large and the depression small, or a small split
fragment may be part of a large
joint
depression fracture. An associated fibular head fracture increases the
degree of knee instability and may be a negative factor for prognosis.23
By accurately reducing the lateral plateau, the goal of preventing or
minimizing the valgus alignment that would occur without surgical
treatment is realized.
depressed tibial plateau fractures is fairly straightforward and
familiar to most surgeons, the tendency to postoperative settling of
the articular fragments is significant, leading to a knee aligned in
valgus despite surgery4 (Fig. 53-26).
The more severe the split depression fracture and the more osteopenic
the bone, the greater are the risk and severity of this problem. To
avoid these problems, surgical techniques need to accurately and
completely reduce the fracture, the implant needs to be placed to
support the reduced fragments, and the void must be filled with the
optimal material. Newer techniques with 3.5-mm plates, multiple
“rafting screws,” and Ca-P cements to fill the void may be better than
the previous techniques.
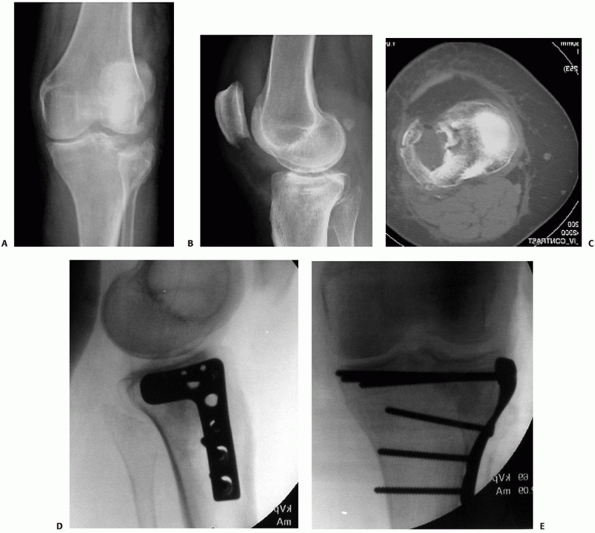 |
|
FIGURE 53-26 A,B. Anteroposterior (AP) and lateral radiographs and (C)
axial computed tomography cut show a low-energy split lateral plateau fracture (AO/OTA type B3, Schatzker 2) that was treated with fluoroscopically assisted reduction, a 3.5-mm lateral plate, rafting screws, and Ca-P cement (D,E). (continues) |
the C-arm should be on the medial side, leaving the lateral side free
for the surgeons to work while the knee is assessed fluoroscopically.
The anterolateral approach is used and the anterior compartment fascia
is incised proximally and anteriorly to allow a buttress plate to be
applied to the anterolateral tibia. The lateral split fragment will be
exposed and partially reflected during the approach, but care should be
taken to minimize the stripping of soft tissues from this fragment,
particularly posteriorly. When the split fracture is reduced, the
capsule and iliotibial band that remain attached to the fragment will
likewise be restored to their normal position and tension.
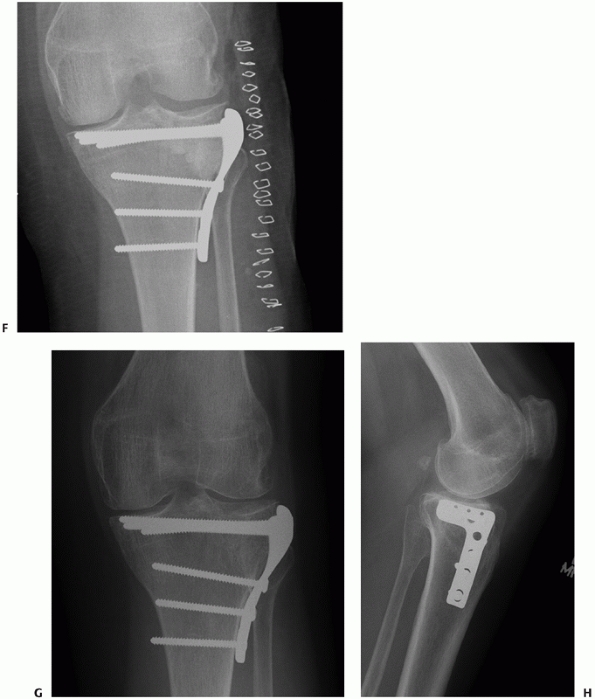 |
|
FIGURE 53-26 (continued) In comparison to the postoperative AP film (F), the fracture at 1 year appears to have settled slightly (G,H). The clinical outcome was excellent.
|
to assist in reducing the fracture, it is accomplished through the
anterior fracture line in the lateral split fragment augmented with a
proximal anterolateral arthrotomy with incision of the anterior lateral
meniscus or a posteriorly directed horizontal arthrotomy beneath the
lateral meniscus. Either approach allows the depressed lateral
articular surface to be directly visualized. A cross-joint distractor
or external fixator may be used to further open the joint.
the depressed fragments to be manipulated and directly reduced to align
with the margins of the intact areas of the plateau. Care should be
taken to work from below, with tamps and elevators keeping as much of
the cancellous bone beneath fragments intact as possible. Generally
speaking, the more fragments that can be elevated in situ from below
and the less they are completely freed and placed on the back table,
the more favorable the eventual reduction will be. The surgeon must
carefully assess for and reduce marginal impactions of the articular
surface remaining attached to the split fragment. Otherwise, the
depressed central fragment will be incompletely elevated, to match a
marginally depressed area, leading to an unsatisfactory reduction. The
fragments may be temporarily fixed with K-wires. When assessed with
fluoroscopy, the lateral side needs to be restored to its normal
position, slightly higher than the medial side. Overreduction is better
than underreduction, given a tendency to postoperative settling.
Comparative images of the opposite side may be helpful.
plate positioned over the split fragment. Current practice favors
3.5-mm plates with 3.5-mm screws. Screws are placed close to the
articular surface to help support the reduced articular fragments.
Three or four of these so-called rafting screws may be used. AP and
lateral fluoroscopy assists in obtaining optimal implant position.
Mechanically, multiple smaller screws provide better support to reduced
articular fragments than a smaller number of larger screws.126 Precontoured plates facilitate implant fit to the bone, but they must be carefully positioned
to optimally achieve this. The proximity of the plate to the
subchondral bone partially dictates the screw support for the articular
fragments.
screws facilitate compressing the plate to bone, enhancing its buttress
effect and narrowing the condylar width. Fixation in firm uninjured
bone on the medial side prevents the screws from settling. They do not
have to resist the bending and rotational forces as do lateral plates
used to treat bicondylar fractures. Some surgeons might advocate that
optimal support for the articular fragment is obtained by locking a
rafting screw to the plate.
operative approach. After reducing but before internally fixing the
fracture or after both of these steps, the void created by the fracture
and the reduction process can be filled with one of several materials
to support the articular fragment. If Ca-P cements are used, the screws
should be placed before the cement to avoid fracture of the material,
which is brittle when it is set. If graft is used, it should be firmly
impacted beneath the reduced fragments.
of lateral plateau fractures, split depression fractures have slightly
poorer outcomes than split or local compression fractures partially
because of the likelihood of these occurring in elderly patients and
partly because some very severe lateral plateau injuries are in this
category. In elderly patients, Keating88
found that split depression had worse outcomes than all other types
except the shaft dissociated pattern. To a certain extent, the results
depend on the ability to reduce and maintain the articular reduction of
the lateral plateau and for some fractures, and in patients with
osteopenic bone, this can be difficult. Ali et al.4 reported a high percentage of patients who lost reduction after surgical treatment, particularly elderly patients.
Techniques With Arthroscopic or Fluoroscopic Assessment of Reduction
and Screw Fixation or Plate Fixation and Possible Void Filler. The
issues that this lateral side fracture pattern present are intermediate
to the previous two. Usually, substantial lateral joint depression
fractures are accompanied by at least a marginal split fragment and the
appropriate operative techniques are described above. Very small
isolated depressions of the lateral articular surface may or may not
need to be treated operatively. To reduce a local depression fracture
without a significant split fragment, the lateral wall should be left
intact, which then requires a technique to access the depressed area.
This can be accomplished with a cannulated drill system where a
guidewire is placed into the depressed cavity from the exterior surface
of the tibia (Fig. 53-27). Once the position is
confirmed either arthroscopically or fluoroscopically, the cortex can
then be opened over the wire, providing access for tamps or awls to
reduce the articular fragments. The cortex can be opened either
anterolaterally or anteromedially depending on the direction of
displacement of the articular fragment. The reduction is judged either
fluoroscopically or arthroscopically. The reduced fragment is supported
with subchondral screws targeted to the correct location beneath the
fragment and void filler can be used to fill the resulting cavity. This
entire procedure can be accomplished using minimally invasive
techniques.
fractures are less severe injuries than most of the other plateau
patterns and for this reason have generally favorable outcomes. Keating88 found that in elderly patients split and local compression fractures had better outcomes than all other types. Lachiewicz98 found that all the local compression fractures treated surgically had excellent outcomes. Savoie et al.140
found all good and excellent outcomes in surgically treated patients
with local compression fractures. In one series, better results were
reported with arthroscopic treatment than with open reduction.
Schatzker 4, Total Condylar—Posteromedial Surgical Approach Antiglide
Plate. In these patterns, at a minimum, the far side of the lateral
plateau is intact and will serve as the fixation point for the
displaced medial side. The fracture line may be through the medial
plateau only or may extend to the intercondylar eminences or into the
articular surface of the lateral plateau. Fractures may be minimally
displaced or present as fracture dislocations where the forces that
fracture the medial condyle are continued and dislocate the lateral
plateau from the lateral femoral condyle. Comminution at the margin of
the fracture is common and may be severe in medial fracture dislocation
patterns and involve the lateral plateau.
but these fractures are difficult to accurately reduce and small errors
may lead to significant articular step-offs or angular malalignment.
Nondisplaced or minimally displaced fractures may be stabilized with
cannulated screws to prevent displacement. When the fracture needs to
be reduced, the forces on these large fragments are significant and the
fracture needs to be fixed with plates (Fig. 53-28).
positioned supine or prone based on surgeon preference. When
substantially displaced, reducing the fracture is difficult and using
aids such as large and small reduction forceps, awls and elevators, and
intraoperative distraction techniques manually or with fixed skeletal
distraction is often necessary. The primary shearing fracture line may
be associated with locally depressed fragments. Depending on their size
and location, their reduction may need to be incorporated into the
operative plan. Usually, this can be accomplished with the
posteromedial approach through the major posterior fracture line even
when the depressed fragments are in the lateral plateau. As with all
plateau fractures, the techniques to visualize and ensure accurate
reduction should be planned ahead and executed intraoperatively.
Despite accurately reducing an extra-articular fracture line, large
medial plateau fractures may have residual tilts or other joint
malreductions that need to be assessed and corrected because they will
lead to limb malalignment. Fluoroscopic techniques are usually
necessary because visualizing the joint through the posteromedial
approach is difficult unless important posterior soft tissue structures
are incised.19 Fixing the fracture
with an antiglide plate will supplement interfragmentary screws that,
depending on the plate configuration, may be applied through proximal
portions of the plate. Most commonly, 3.5-mm plates will be strong
enough to provide the antiglide effect necessary. If the plate is
narrow, two plates may be used to support a total
condylar fracture (Fig. 53-29).
Placing the plate at the apex of the fracture is mechanically optimal.
Mechanical studies and common sense would indicate that the temptation
to try to stabilize a displaced medial plateau fracture with a lateral
side locking plate should be resisted.132
 |
|
FIGURE 53-27 Intraoperative fluoroscopy show K-wires (A,B) targeting a lateral plateau joint depression and a curette elevating the fragment (C,D). The reduction was supported with screws and Ca-P cement (E).
|
there are few results reported for these difficult and less common
fractures when they occur in isolation. In many series, there are too
few medial patterns to meaningfully report results. Schatzker et al.143 thought that the medial side patterns had the worst prognosis of the six types. Honkonen75
found less satisfactory outcomes and a high percentage of posttraumatic
OA in medially tilted fractures and bicondylar patterns with a medial
tilt. Both Bhattacharyya et al.19 and Carlson29 warned of the possibility of flexion deformities, particularly after posterior approaches for these fractures.
6—Bicondylar or Metaphyseal Diaphyseal Dissociation—Lateral Locking
Plate; Adjunctive Medial Plate Based on Characteristics of Medial Side
Injury or External Fixation. These are the most difficult and complex
fracture patterns and have a wide range of injury severity. All AO/OTA
type 41-C and Schatzker 5 and 6 patterns are presented together in this
section because distinguishing between them is not clear enough to
merit separate discussions of treatment and results. The advent of
locking plates has brought new information and controversy and
increased the variety of operative strategies for these complex
fracture patterns. Without a
plate
with fixed angle stability from the lateral side, surgeons had two
choices: (a) a lateral plate combined with a medial plate or
occasionally combined with a medial external fixator136
or (b) an external fixator with enough stability to support the entire
fracture. Many of these fracture patterns are now effectively
stabilized with a laterally based locking plate as the only major
implant. The shift to this technique has been rapid and dramatic.
However, there are issues to be considered in planning and executing
this strategy. Important decisions that require good judgment include
knowing which patterns are amenable to a lateral locking plate alone
and which need to be fixed on both sides with two plates and which
would be safer with an external fixator. Case selection is critical and
new information and new generations of locking implants may continue to
change which fractures can be stably fixed with a lateral locked plate
only. The currently available information on these fractures will be
presented in the following categories: mechanical studies, soft tissue
injury and management, definitive external fixation, dual plates,
lateral locking plates, and comparative studies.
 |
|
FIGURE 53-28 A,B.
Even subtle medial plateau fractures tend to align in varus as seen in the initial radiographs in this case. The medial joint has several coronal fracture lines seen on the lateral view (arrows in B). C. A posteromedial approach and two small fragment plates, one between the pes tendons, were supplemented by 4 weeks of adjunctive cross-joint external fixation. D,E. Three-year follow-up radiographs show neutral alignment and a preserved joint. |
Mechanical studies have compared lateral locking plates alone to dual
plates in bicondylar tibial plateau fracture models and the results
have been mixed. In paired cadaver models, Gosling et al.63 and Muellar et al.119 found no significant difference with vertical loading between dual plates and lateral locking plates. Egol et al.50
found that dual plates were better at resisting displacement but did
not think the differences were likely to be clinically important. In a
matched-pair cadaver model of bicondylar fracture, Higgens et al.69 found that that subsidence was sufficiently greater with lateral locked
plates compared to dual plates to raise clinical concerns about using
lateral locked plates alone for these fractures. In a medial plateau
fracture model, medial buttress plating was found to be stronger than a
lateral locked plate.132
One study demonstrated that bone quality was the most important
parameter in determining fixation strength regardless of the technique
to stabilize the fracture.6 The
clinical relevance of these types of studies is predicated on knowing
how stiff and how much deforming force must be resisted to promote
healing while not allowing secondary displacement.
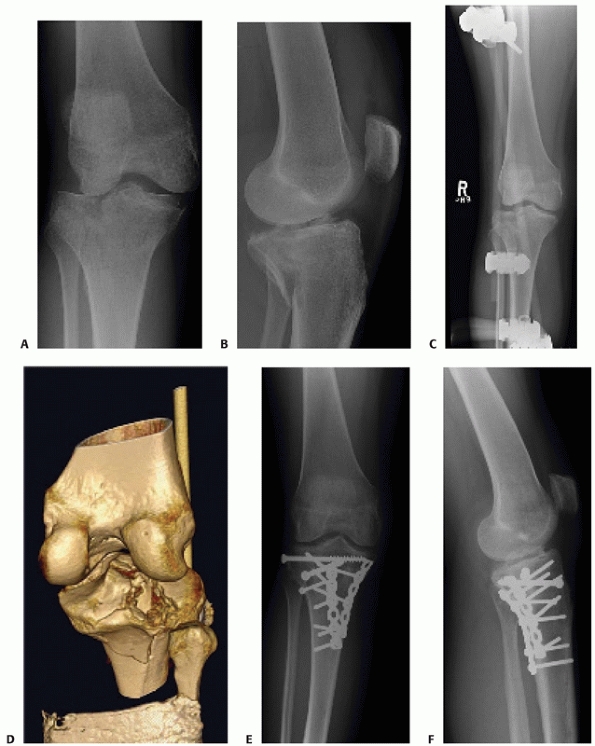 |
|
FIGURE 53-29
The posteromedial approach allows access to the entire posterior aspect of the knee. Anteroposterior and lateral images show a comminuted posterior medial fracture pattern (A,B) treated with a spanning fixator, which restored provisional length and alignment (C). D. A computed tomography scan in traction shows a comminuted posterior fracture pattern. A posteromedial approach, with fracture reduction and two 3.5-mm pelvic reconstruction plates, was used for surgery 10 days later. E,F. At 8 months after the injury, the fracture is healed and alignment is excellent. Note that the most posterior plate is past the midline and that the lateral comminution was reduced through the posteromedial approach. |
The soft tissues must be carefully assessed and managed with respect to
minimize soft tissue complications from the substantive implants
required for these fractures. Surgical timing, temporary spanning
external fixation, and recognizing the risk for compartment syndrome
are all important to optimizing outcomes. In addition, these fractures
are effectively and relatively safely managed with definitive external
fixation, so when a surgeon chooses a locking plate, he or she must be
confident that the risk for severe complications can be minimized.
important role for initially managing some of these fractures. The
external fixator spans both the fracture and the knee, and as much as
possible the pins avoid the entire zone of injury. Frames are most
commonly constructed from pin to bar components. When placing pins, the
location of future incisions and implants should be considered. The
goal is to maintain length and alignment in the days or weeks after
injury while the soft tissue injury recovers and the definitive
procedures can be planned. However, careful attention to technique is
required to achieve these goals. A knee-spanning fixator applied with
pins in poor position and the fracture short and/or malaligned may
cause more harm than benefit. Case selection for this technique is
important because not all of these fractures require a joint-spanning
external fixator. Proximal tibia fractures that have the greatest
potential to benefit have one or more of the following: significant
displacement and shortening, open fracture, a severe closed soft tissue
injury, compartment syndrome, a fracture-dislocation, and/or a long
anticipated delay to definitive surgery.
In some bicondylar patterns, the fracture needs to be fixed on two
sides based on the characteristics of the medial side injury. A medial
plate is necessary when the medial condyle is comminuted, is very
displaced, or is a relatively small fragment. If the medial condyle is
split coronally, creating a posteromedial fragment, this may need to be
separately fixed with a posteromedial plate. The choice between a
lateral locking plate alone and dual plates is largely driven by these
characteristics of the medial side injury. The exact fracture pattern
must be carefully assessed, and the correct choice does not easily
divide along classic classification categories or subcategories.
fracture, the first important factor is the associated soft tissue
injury. Periods of joint spanning external fixation are frequently
chosen, and delays of 3 weeks or longer before definitive surgery are
not uncommon. The fixator should be placed so pins avoid the region of
the subsequent dual plating approach.
Although each side must take into account the other side, they are
modestly separate techniques. The medial side is typically approached
first. Reducing and fixing the medial side restores this section of the
plateau and the lateral side will then be reduced and buttressed
against it. Additional points to consider in planning this dual
approach include the following: (a) the incisions should be nearly 180
degrees from each other anterolateral and posteromedial; (b) this is a
lot of surgery—be prepared with enough time; (c) the initial stages of
the operation on the medial side must be accurate or the final result
will be unsatisfactory; (d) medial side screws must account for the
lateral side injury—they can usually be targeted anteriorly, avoiding
the lateral fracture zone; (e) limit the number of screws early in the
case—there will be a lot of screws in the end and the lateral screws
can be used to lock in the provisionally fixed medial side, decreasing
the need for excessive medial-to-lateral screws; and (f) consider that
access is required to both sides when positioning the patient.
plating of fractures of the proximal tibia has been reported in
numerous case series and was compared to external fixation in one
randomized controlled trial. In the 1980s and early 1990s, this
technique developed a bad reputation because of a high incidence of
wound breakdown and devastating infections when dual plates were
applied via a single midline incision with medial and lateral
dissections. The term “dead bone sandwich” was used as a way to
criticize this technique. A variety of advances have decreased the
complication rates. One of the most important of these is adopting a
staged protocol, which initially manages the fracture with a
joint-spanning external fixator, allowing a delay to the dual plating
procedure for soft tissue recovery. This staged technique is the most
valuable in the most severe fractures with the highest risk for the
soft tissues.51 Another important change has been the use of dual approaches rather than a single anterior extensile approach.
fractures treated with modern medial and lateral plating techniques
have reported deep infection rates of between 8.4% and 18%.12,27,150 Multiple surgical procedures are often necessary after a patient develops a deep infection. Shah and Karunaker150
noted that the risk might be particularly high in cases where a
fasciotomy had been necessary. These infection rates are still not
trivial and every effort should be made to minimize these complications.
the general sense of the literature is that the healing rate after dual
plating is high. With a careful technique, alignment is usually
satisfactory. Barei et al.12
reported 91% and 72% satisfactory coronal and sagittal alignment,
respectively. The accuracy of reducing the articular surface is hard to
measure or judge. The COT study demonstrated a significant proportion
of articular malreductions despite dual approach open reductions. The
authors did not believe the outcome was compromised by these malreduced
articular surface.27 However, Barei et al.11 found that the accuracy of articular reduction correlated with outcome.
When the timing is optimal for the definitive procedure, the techniques
for either a laterally based locking plate or a definitive external
fixator are similar. Obtaining length and alignment during the
procedure is important, and this may be accomplished by a preexisting
joint spanning external fixator. Alternatively, a fixator or femoral
distracter may be applied at the time of the surgery or an able
assistant may be able to apply the necessary traction forces.
tibial articular surface and fix the medial and lateral condyles to
each other, building a proximal articular block. The techniques
required depend on the intra-articular fracture pattern. In AO/OTA type
A fractures, the proximal tibia is not fractured. In cases with
nondisplaced or minimally displaced articular extensions, cannulated
screws to fix the split are satisfactory. As the fracture becomes more
complex, there is an increased need to incorporate other previously
described techniques of joint reduction and fixation (Fig. 53-31). Void filler may occasionally be necessary when significant joint depressions have been reduced.66
The severity of these injuries and the risks for complications should
lean the cautious toward approaches that are more limited than those
for isolated medial and lateral injuries.
the tibial shaft must be reduced and fixed to each other restoring
length and alignment. This is facilitated by distraction, a
fluoroscopically compatible table, and careful implant position on the
proximal
and distal fragment. To decrease complications and to speed healing,
the area of the metaphyseal injury should be largely skipped and
treated with a no-touch technique spanned by the locking implant.
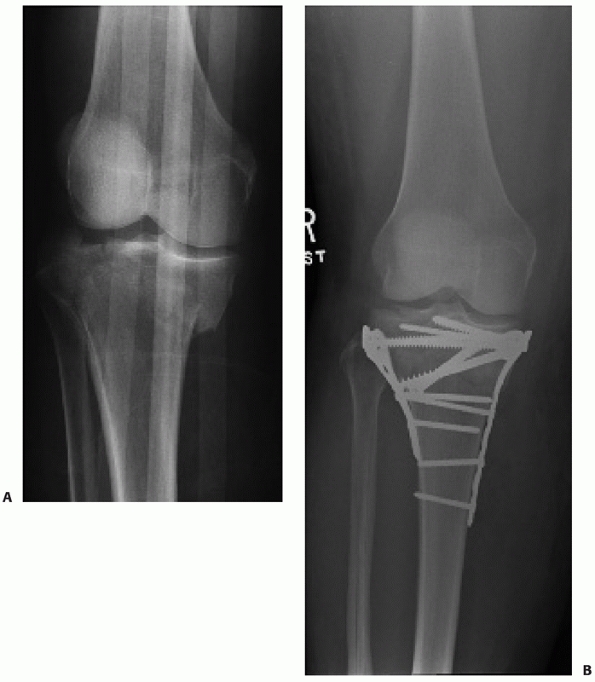 |
|
FIGURE 53-30
Some bicondylar fractures are still best treated with medial and lateral plates, particularly if the medial side fracture is small, comminuted, or split in the coronal plane. A,B. This case was treated with dual plates through separate posteromedial and anterolateral approaches. |
plates made by different manufacturers. The technique is fairly similar
for all of them. An incision over the anterolateral tibia must be long
enough and appropriately positioned to accommodate the head of the
tibial plate and the insertion of the proximal screws into the plate
head. The top of the plate will be just below the joint line, and in
the sagittal plane it must be in line with the shaft and avoid being
too anterior. A small incision in the fascia at the top of the anterior
compartment is necessary to allow the plate to slide along the
anterolateral tibia. Care should be taken to keep the plate directly on
bone. This can be felt as the plate is inserted and assessed
fluoroscopically.
and distally. If the fracture is reduced, the implant may just be
placed on the bone using it to secure the reduction. If the implant
will be used to assist in reducing the fracture, each step in fixing
the implant proximally and distally must be sequentially assessed.
Accurate plate position proximally and distally will reduce the
fracture. If the plate will extend farther distal than the middle of
the tibia, care must be taken to not injure the superficial peroneal
nerve or the anterior tibial neurovascular bundle when inserting the
distal screws.41 Final fixation will be with locked screws in the head of the tibial plate and either locked or nonlocked screws distally.
Treating tibial plateau fractures with lateral locking plates is still
a relatively new treatment concept, so assessing the results and
comparing them to previous techniques is important. The results
reported in case series have been generally satisfactory but there have
been some concerns with loss of alignment and with hardware problems
related to either the position of the proximal portion of the implant
or to cold welding of the locked screws. There has been some
variability in the reported incidence of infection.
first locking plate system that began to popularize this technique, and
most of the results for the proximal tibia have been reported with this
implant. Infection has been reported in between 0% and 22% of cases,
postoperative malalignment in 0% to 23% of cases, and hardware
irritation in 5% to 18%.22,38,50,64,128,135,144,155 Gosling et al.64
reported a 23% malreduction rate and noted the challenges of limited
approach surgery for complex proximal tibia fractures, particularly
with less experienced surgeons. Postoperative compartment syndrome was
reported in two series, accounting for 3% to 5% of cases.12,136 Peroneal nerve injury has been a rare complication.38,128 Cold welded screws during hardware removal was reported in 4 of 94 screws in one series38 and in 2 of 88 screws in another series.128 Phistikul
et al.128
stressed the risk for complications such as deep infection which
occurred in 22% of fractures in their series. The risk of infection of
a lateral locking plate was thought to be particularly high in patients
with compartment syndrome with open fasciotomy wounds.
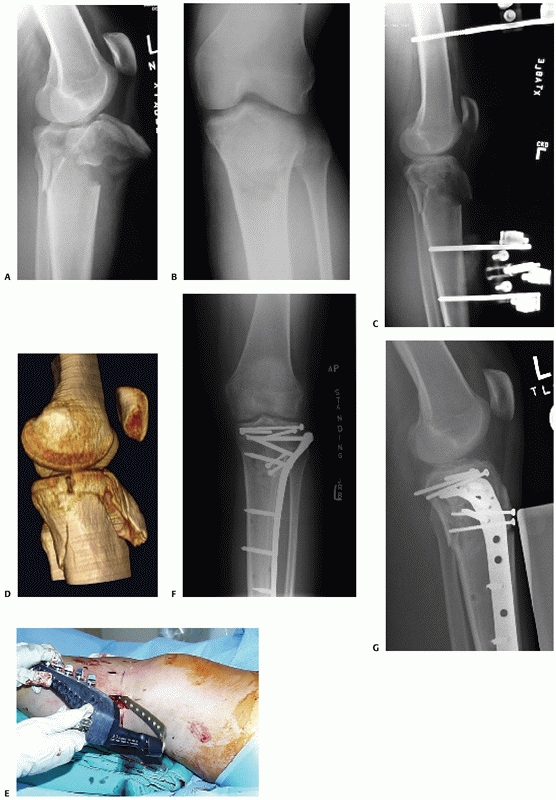 |
|
FIGURE 53-31
For many bicondylar fractures, the reduction can be maintained with a laterally based locking plate alone. This unusual bicondylar fracture with extensor mechanism disruption (AO/OTA type C-3) had anterior skin pressure and needed urgent spanning external fixation (A-C). D. CT scanning showed a split in the medial plateau, but it was minimally displaced, allowing the fracture to be treated with a lateral locking plate through a limited anterior lateral approach with indirect reduction and screw fixation of the medial side. E. The photograph shows the small anterior incisions for reduction instruments and screws and the locking plate placed through the anterolateral incision. F,G. At 6 months after the injury, the patient’s fracture has healed and alignment has been maintained. |
whether lateral locked plates are strong enough to prevent varus
displacement in bicondylar fractures. Some authors have found no loss
of alignment,50,144,155 where Gosling et al.64 and Phisitkul et al.128
reported 14% and 8% loss of alignment, respectively. Watson indicated
that if the medial column was not comminuted and could be accurately
reduced, then a lateral locking plate would suffice but otherwise dual
plating was necessary168 (Fig. 53-32).
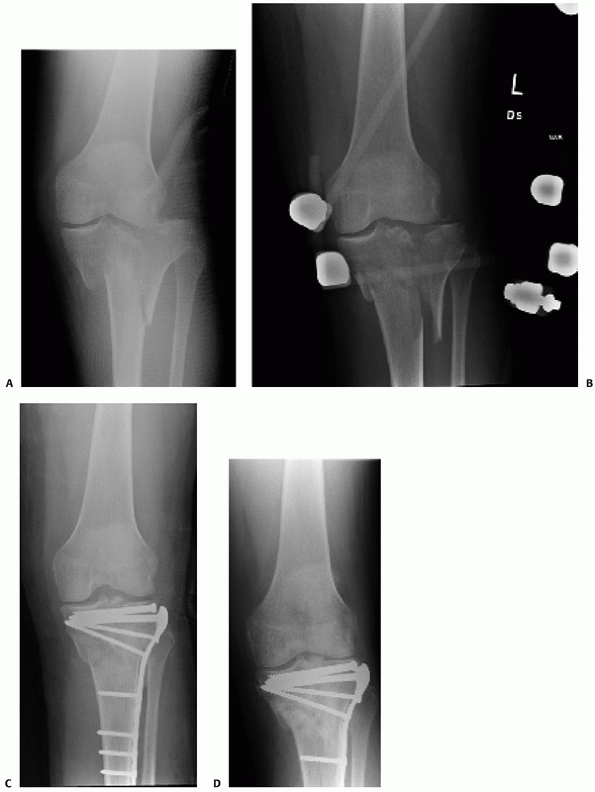 |
|
FIGURE 53-32
In bicondylar fractures treated with a lateral locking plate, it is difficult to predict the need for additional medial fixation. An initial anteroposterior (AP) radiograph shows a widely displaced fracture dislocation pattern (A) with improved alignment after a spanning fixator was applied (B). A laterally based locking plate stabilized the fracture. An immediate postoperative (C) and a 4-month AP (D) radiograph shows slight loss of reduction into varus. |
reported the results of 24 type 41-A or -C and 7 type B proximal tibia
fractures treated with a polyaxial locked plate, which allows variable
trajectories of the screws before locking. Seven patients had
adjunctive posteromedial plates. The authors found no loss of
alignment. Two patients developed deep infections. Hardware removal was
not reported.
When definitive treatment is with an external fixator, the first step
in the procedure uses the same preliminary steps of reducing and
internally fixing the two condyles to each other as described for
lateral locking plates. Occasionally proximal fixation can be
supplemented by direct incisions over the area of joint involvement and
adjunctive antiglide plating.167
Similar to a locking plate, the external fixator will span the
metaphyseal area of the fracture and stabilize the tibial condyles to
the tibial shaft. The metaphyseal fracture is reduced indirectly. A
wide variety of frames can be used to accomplish this. These include
circular external fixators, monolateral fixators, and hybrid fixators.
Many of these fixators have an adjustable frame to facilitate
accurately aligning the limb because this is one of the most important
technical aspects of the procedure.
constructing a frame and securing the frame to the bone proximal and
distal to the fracture, to ensure stability is optimized.169
Because of the limited extent of proximal tibia available for fixation
and because of the presence of fracture lines and relatively small
fracture fragments and the proximity of capsular reflections from the
knee, securing adequate proximal fixation is the most difficult
challenge. Adequate preoperative planning for frame application is very
important and should include a CT scan. If a pin fixator is used,
hydroxyapatite-coated pins provide longer lasting purchase to the
metaphyseal bone than standard noncoated pins.118
Pins may be placed medial, anteromedial, or anterolateral. The patellar
tendon must be avoided. Fluoroscopy should be used to assist in placing
pins in the best bone, avoiding fracture lines to the extent possible,
and to ensure that they are placed deeply through the bone without
being prominent on the opposite side. There must be two or preferably
three proximal pins to have adequate purchase in the proximal tibia. If
a circular wire frame is used, maximum wire spread is facilitated by
using a fibular head wire combined with a
posteromedial-to-anterolateral wire. Fluoroscopy is also important for
accurate wire placement. Three tensioned wires are typically used and
they may be augmented by a single half-pin. The use of olive wires
increases the stability of proximal fixation and may be used to
compress major fracture lines. Both pins and wires should be kept as
far from the joint as possible to minimize the chances of septic
arthritis, but the fracture pattern also has a role in the proximal
distal location of pins and wires.
alignment with stable fixation with less soft tissue dissection and
without a bulky implant.171 With
some frame constructs using tensioned wires and circular frames,
earlier weight bearing than with other techniques may be possible.2
reported satisfactory results using an all-pin fixator. Pins or wires
should be kept as far away from the articular surface as possible to
minimize the chances of septic arthritis that has been reported after
both pins and wires.55,111,123
In severe cases with soft tissue injuries, fracture instability, and
small periarticular fragments, a cross-knee-spanning frame may be used
to augment the primary frame and removed after a few weeks of
neutralizing the cross-joint forces. In one series of fine wire
external fixation for bicondylar tibial plateau fractures, the knee was
bridged as part of the frame in 63% of cases without adverse outcomes.
Neutralizing the forces across the knee may decrease the risk for
proximal pin- or wire-related septic arthritis.
Definitive external fixation as treatment for high-energy tibial
plateau fractures has been reported in the literature since the early
1990s.111,123,154,171
Case selection for these techniques have been biased toward the
high-energy bicondylar or shaft dissociated patterns with a high
incidence of open fractures and compartment syndrome. For instance, in
three recent series treated by definitive external fixation, the
percentage of open fractures ranged between 33% and 100%.36,87,158
Most of the results are reported in case series, and most authors have
found satisfactory results considering the severity of the fractures
treated. The union rate without additional procedures has been high,
ranging between 85% and 100% in recent series.3,36,45,158,167,170
Although stable fixation leading to good alignment is usually achieved,
one author reported 4 of 15 open plateau fractures lost reduction
during treatment and recommended limited internal fixation as an
adjunct to prevent this problem.111 Another author reported loss of reduction into valgus in 3 of 11 elderly patients treated with a hybrid fixator,3 and in another, 3 of 16 healed fractures had a varus deformity.60 The knee range of motion is generally good; Kateria et al.86 reported an average of 132 degrees in 48 patients with Schatzker 5 and 6 fractures. Marsh et al.111
reported that patients averaged 138 degrees of flexion. Most patients
have achieved knee scores averaging 85 to 90 on 100-point scales.111,169 Weigel and Marsh170
found that the initial results were maintained at longer follow-up. All
patients with sequential follow-up to 5 to 11 years after injury were
found to improve with longer follow-up. Pin tract infections are common
and septic arthritis is an unusual but feared complication of external
fixation for tibial plateau fractures.60,111
The treatment of tibial plateau fracture patterns has been extensively
reported in the literature. Despite this, the optimal technique for a
given fracture is uncertain. With the complexity of these fractures and
the difficulty of the techniques, there clearly is room for treatment
to be based on the personal preferences and experiences of the surgeon.
In addition, in most of the literature there is overlap between
bicondylar patterns treated with dual plates and shaft dissociated
patterns treated with locking plates alone or external fixation, which
makes it hard to compare the treatment methods.
fixation for AO/OTA type C fractures (Schatzker 5 and 6) in a
randomized controlled trial performed by the Canadian Orthopaedic
Trauma Association.27 They found
that dual plating resulted in a greater incidence of deep infection
(18%) and repeat operations, longer hospitalization, and a marginally
longer return to function. The reductions and patient outcomes were
similar in the two groups, both of which had decreased general health
status compared to age-matched control groups. In another
study, Jiang et al.84
found that the LISS lateral locking plate and dual plating resulted in
similar outcomes. There was a trend to a slightly higher malalignment
rate and more symptomatic hardware with the LISS.84
A metaanalysis compared fractures fixed with plates to those fixed with
external fixators and found that there was not enough evidence to
distinguish between the two techniques.107
not been the subject of many studies. The optimal postoperative program
should minimize complications and loss of reduction of the fracture and
maximize knee motion while speeding recovery and return to function.
is necessary to minimize the chances of displacing the reduced
fracture. The duration depends on the fracture pattern and the strength
of the fixation but it probably takes 6 to 12 weeks for any meaningful
increase in resistince to displacement from fracture healing, so most
surgeons will not progress weight bearing until sometime in this range.
One paper recommended early weight bearing for operatively and
nonoperatively treated lateral plateau fractures with a cast brace to
unload the lateral side and demonstrated little secondary displacement.148
Although cast braces are less commonly used in current practice, this
information should be considered when poor patient compliance with
weight-bearing restrictions is anticipated.
that is potentially important in the postoperative care of tibial
plateau fractures. Fractures treated nonoperatively can regain
excellent knee motion after being immobilized for up to 6 weeks.47,61
However, because most fractures treated nonoperatively in current
practice can be safely moved postinjury, most surgeons will recommend
knee motion immediately or within a few weeks, usually in a hinged
brace.
thought that that early motion was much more important after operative
treatment, because knees immobilized for longer than 2 weeks tended to
be stiff. In current practice, surgeons strive to fix fractures in a
way that will allow motion during the early weeks of recovery sometimes
in a hinged brace. In recent years, temporary periods of immobilizing
injured joints with a spanning fixator have been used with increased
frequency for some severe tibial plateau fractures. Marsh et al.111
have shown that the knee can recover excellent motion (range of flexion
greater than 130 degrees) after up to 6 weeks of immobility using
spanning fixation. Other investigators have also found that cross-joint
external fixation does not seem to be a frequent obstacle to regaining
motion.51
possible to reduce and fix the fracture as long as it is compatible
with a well-aligned limb and a fracture that is fixed well enough to
start early motion. The more limited an approach, the more important is
preoperative planning to understand the fracture pattern and the
important fragments and how they are displaced. Complex imaging with a
CT scan is indispensible, and in difficult patterns, I usually review
three-dimensional images on the computer work station to optimally
assess the pathoanatomy of the proximal tibia. Because I only rarely
directly assess or treat associated intra-articular meniscal injuries,
I usually do not obtain an MR image.
severe injuries, because many fractures of the tibial plateau do not
need or benefit from this two-stage approach. However, in appropriately
selected cases, it has been an important part of my practice for many
years.111 A simple anterior pin to
single bar frame with two spread pins in both the tibia and femur
usually suffices, although I find strong distraction is required in
difficult cases. I spread the pins widely to increase frame stability
but occasionally will build a more complex frame. I always prefer
anterior femoral pins since they are in the plane of motion and in my
opinion do not bind the quadriceps any more than other possible pin
orientations.
antiglide plating, and locking screws are not necessary or helpful and
only serve to increase costs. On the other hand, lateral locked plating
has largely replaced definitive external fixation in my practice for
most bicondylar and shaft dissociated patterns.
injuries is to prevent valgus deformity. Some fracture patterns with
large split fragments are amenable to screw fixation only. These are
treated with true percutaneous techniques. It is important to have the
screws perpendicular to the fracture line for compression and
stability. I find that plate fixation is not necessary for split
fractures.
control and supported with cannulated screws. Split depression
fractures, where the split fragment is small or of poor quality, need a
buttress plate. I use 3.5-mm precontoured plates and try to place the
implant so the screws can be close under the elevated fragments. The
extent of the approach is only what is required to place the plate and
this approach is accomplished as the first step in the procedure. I do
not open or visualize the joint. The depressed fragments are reduced
through the split fracture line and visualized fluoroscopically. Small
residual articular irregularities are accepted. I do not incise or
elevate the meniscus. The reduced fragments are supported with
subchondral 3.5-mm rafting screws, and if there is an obvious void, it
is filled with calcium phosphate cement, because current data indicate
it has the best mechanical properties of the currently available void
fillers.
fluoroscopically. This avoids an arthrotomy and in my hands leads to
equally satisfactory reductions and minimizes disruption of the soft
tissues. I rarely use arthroscopy. I do not obtain preoperative MR
images for routine injuries. Despite the high incidence of meniscal
injuries, in my experience these do not need to be routinely assessed
or managed since they do not make a difference in patient outcome. This
approach is consistent with the good results reported for a variety of
other strategies to treat plateau fractures that have not addressed
meniscal pathology.17,65,174
injuries on the medial side and most posterior injuries. I never do
direct posterior approaches. The medial gastrocnemius is easily
mobilized and access well past the posterior midline is possible. When
the plate will be posterior or even posteromedial, I take care to make
the incision on the posterior side of the posteromedial tibia to
prevent the skin from becoming an impediment to screw paths. An
incision too anterior is one of the biggest obstacles to reducing and
fixing posterior patterns from the posteromedial approach. For more
anterior medial patterns, I still use a posteromedial approach and the
work is done between the pes tendons.
lead to unacceptable limb alignment. Despite directly reducing a
posteromedial spike, alignment must be assessed fluoroscopically and
compared to the opposite side. I always obtain fluoroscopic images of
the opposite side at the start of the case. The limb is best visualized
when it is extended and in the standard AP position. The fragment must
be provisionally fixed with reduction forceps during this step. Flexion
and external rotation may recreate deformity so I often achieve screw
fixation in the extended nonrotated position from anterior or anterior
lateral, before reexposing the posteromedial surface for plating in
flexion and external rotation. To fix the posteromedial fragment, I
have used a number of different 3.5-mm plates and frequently favor one
or two pelvic reconstruction plates. They contour easily to any
location and are narrow enough that two can be used if necessary to
broaden the support over the back of the proximal tibia.
with a combination of the two approaches: anterolateral for the lateral
side injury and posteromedial for the medial side injury. For most
patterns with a coronal split of the medial condyle creating a
displaced posteromedial fragment, I will choose to approach both sides
rather than using a lateral locked plate alone. These are difficult
fracture patterns, but
possible. The procedure is performed with the patient supine on a
radiolucent table. The posteromedial approach and medial side fracture
are reduced and fixed first with the leg externally rotated. It is
critically important to reduce the medial side as accurately as
possible because it is the first step in a sequential procedure, of
which the end result is to have a well-reduced and -aligned knee.
During plating, care must be taken that posteromedial screw paths do
not interfere with the subsequent lateral side procedure. In addition,
I try to be conservative with the amount of fixation screws,
recognizing that there will be plates on both sides. With plates on
both sides, 3.5-mm implants are usually sufficient and locking screws
are rarely necessary or helpful. I also try to move along as quickly as
possible—with two full procedures on both sides of the joint, there is
a lot of work to do.
treated by a lateral side locking plate only. The decision is based on
the characteristics of the medial side injury. If the medial side is
nondisplaced or if the fragment is large and not comminuted, I will
reduce it indirectly and stabilize it from the lateral side with a
locking plate. In more complex medial side patterns, I prefer two
approaches to avoid varus collapse or inaccurate medial side reduction.
limited approaches—only what is necessary to place the head of the
implant and to open the anterior compartment to slide it distally.
Articular reductions are performed through limited approaches based on
the fracture pattern. Distal screws are placed through the external
targeting jig. I usually first use nonlocked screws proximal and distal
to bring the plate to the bone. Proximal fixation is then completed
with locking screws and distally the shaft is fixed with nonlocked
screws. In my opinion, this hybrid-type construct has the advantages of
both locked and nonlocked plates.
fractures, some fractures are associated with compartment syndrome, I
use definitive external fixation with a monolateral frame or a Taylor
Spatial Frame. Frames are usually needed for 3 to 4 months, and I
encourage weight bearing in the second half of this time in the frame.
Frames are removed in the outpatient clinic unless hydroxyapatite pins
are used, in which case they are removed in the operating room.
severe complications, but significantly displaced split, split
depression, and local compression fractures of the lateral plateau, if
untreated, have a high incidence of valgus alignment of the knee.
Because optimal outcome requires a well-aligned knee, one of the goals
of treating lateral plateau fractures is to prevent valgus deformity.
The evidence indicates that even with current techniques, surgically
managing these fractures is frequently complicated by losing some of
the reduction postoperatively. In one study, 31% of operated knees had
loss of position after surgical treatment, and in patients older than
60 this percentage rose to 79%.4 The
clinical significance of loss of reduction is uncertain, but when it
leads to malalignment, patient outcome may be compromised (Fig. 53-33).
Improved methods of fixing low-energy fractures such as smaller
precontoured plates allowing subchondral screws to raft under the
reduced articular surface may decrease the tendency for postoperative
displacement.85 Calcium phosphate
cement used as a void filler after reducing the articular fragments may
be stronger than traditional techniques such as bone grafting.160
Whether these new techniques will decrease the incidence of loss of
reduction and thereby lead to improved patient outcome is uncertain,
but given the high tendency toward postoperative displacement, these
refinements of technique seem warranted.
severely injured soft tissue envelope. Surgical approaches through the
damaged soft tissues present a considerable risk for complications.
Wound
breakdown,
exposed hardware, and proximal tibial infection are devastating
complications of surgery. Fortunately, current techniques have
decreased the risk. These techniques include delays to definitive
surgery, the use of temporary spanning external fixation, dual
approaches instead of extensile surgical approaches for plate fixation,
and definitive external fixation. However, in high-energy fractures,
some risk remains despite careful technique.
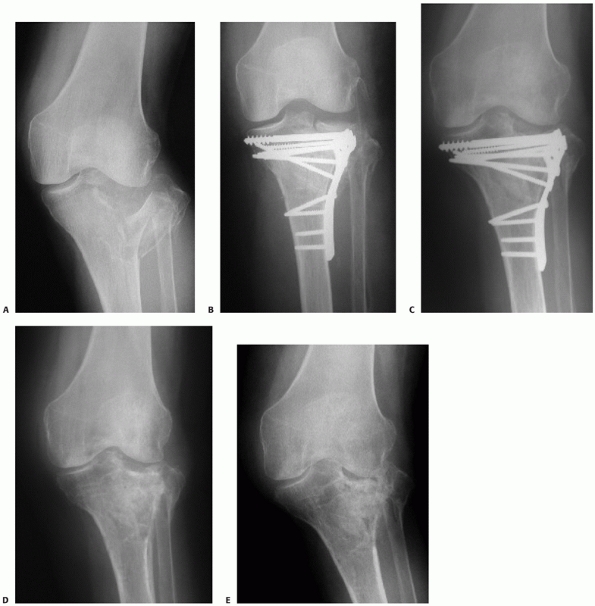 |
|
FIGURE 53-33 A.
Difficulty in maintaining reduction of split plateau fractures is dramatically illustrated in an elderly woman with a severe split depressed lateral fracture. Postoperative (B) and 6-month (C) films show incomplete initial reduction and subsidence at 6 months. D,E. The hardware was removed at 1 year, and at 18 months, the patient is in need of a complex reconstruction. |
complications means the importance of avoiding them cannot be
overemphasized. Previous techniques using extensile approaches, poorly
timed surgery, and excessive stripping of soft tissues to place medial
and lateral implants led to an unacceptably high risk of these
complications. Mallick et al.108 reported deep infection in four of five bicondylar fractures treated with internal fixation with plates. Young and Barrack179
reported deep infection in seven of eight cases treated with dual
plates, which resulted in two amputations and five ankylosis or
arthrodesis. In both of these series, the surgical approach was not
specified.
changes have been important in decreasing complications. Surgery for
internal fixation is not performed until the soft tissues recover from
the initial injury and, if necessary, length and
alignment are maintained with a temporary joint-spanning external fixator.51
Extensile anterior approaches, where a single incision is used to
expose the medial and lateral tibia with or without extensor mechanism
elevation, devascularized both the skin and the bone. These extensile
approaches have been largely abandoned in favor of direct approaches to
the injured proximal tibia and, if necessary, two approaches—one
anterolateral and one posteromedial. These direct approaches leave the
soft tissue envelope as minimally disturbed as possible while still
providing access to reduce and stabilize complex fractures. However,
despite these techniques, recent studies have reported infection rates
of greater than 10% in severe fractures treated with medial and lateral
plating.12,27,150
These authors have documented that multiple surgical procedures are
often necessary after a patient develops a deep infection. Shah and
Karunaker’s150 data indicated that
the risk might be particularly high in cases where a fasciotmy had been
necessary. While these complication rates may be less than earlier
reports, they are not trivial.
been an important advance that has in part been responsible for
decreasing complications of high-energy proximal tibia fractures. For
low-energy fractures, delays are less important, and if necessary, the
knee can be safely splinted. For displaced and shortened high-energy
fractures, surgical delays have been facilitated by the use of
joint-spanning external fixators, which restore length and alignment in
a minimally invasive fashion. Definitive surgery is then delayed to
wait for soft tissue recovery. Even severely injured knees appear to
tolerate cross-knee immobility for 6 weeks or longer and can still
regain good motion and have reasonable function in the short and long
term.145
should decrease the need for dual plating in unstable bicondylar
fractures since the fixed angle screw plate device can resist common
deforming forces. In addition, external screw targeting allows the
plates to be applied through limited approaches. In combination, these
advantages may decrease the incidence of wound complications and some
publications indicate the wound complication rate is low.12,29,93 However, Phistikuhl reported a 22% rate of infection in high-energy proximal tibias treated with an LISS plate.128 Open fasciotomy incisions are frequently present and may complicate treatment and increase the risk for infection.
the clinical presentation. The authors of a recent paper speculated
that current infections were easier to treat and less severe because of
more limited approaches for reducing the fracture and inserting the
implant.128 Irrigation and debridement in the operating room and organism-specific antibiotics are central to all treatment techniques.
may be maintained and the wound packed open. If the infection can be
suppressed until fracture healing, hardware removal will then give a
chance for a cure. However, if the infection is aggressive or the bone
is involved, hardware removal followed by external fixation may be
prudent. Associated soft tissue defects may require flap coverage.
Definitive stabilization can be with external fixation or repeat
internal fixation after infection control and soft tissue coverage are
accomplished.
tibial plateau fractures that involve the joint and the bone may be
very difficult to control and cure. Proximal tibial resection with a
cement spacer and subsequent arthroplasty, knee arthrodesis, or even
above-knee amputation may be necessary to eradicate infection.
tibial plateau fractures has complications unique to that method.
Septic arthritis of the knee related to proximal tibial external
fixation wires or pins has been reported as an occasional complication.
Rates have been as high as 10%.111
Studies have assessed the capsular reflections around the knee in an
effort to define a safe zone for pins or wires. One study indicated
that to be certain capsular reflections were not violated, pins and
wires should be kept a minimum of 14 mm below the joint.134
to keep external fixation pins or wires as far from the articular
surface as possible. In severely comminuted fractures with multiple
small fragments close to the joint or large joint depression cavities,
a prolonged period of cross-knee external fixation will minimize the
risk of joint sepsis in the early weeks after injury.
plates, external fixation with pins or wires in the very proximal tibia
is used less commonly. For this reason, this complication is now rarely
seen. The joint-spanning external fixators that are commonly used for
temporary treatment do not pose a risk for knee septic arthritis,
because pins are remote from the knee and the zone of injury.
after tibial plateau fractures. Current techniques emphasize early
motion in stable fractures or after operatively fixing unstable
fractures. In one study of 202 operatively treated patients with 1 year
of follow-up, the average knee range of motion was 130 degrees (range,
10 to 145 degrees).130 In another
study of all high energy fractures treated with external fixation, the
knee range of motion at greater than 5 years after injury averaged 3
degrees of extension and 120 degrees of flexion.170
Early motion after surgical treatment is standard care, although
fixation must be strong enough to permit motion. Some patients may
benefit from physical therapy, but there are no data that a therapy
program improves motion.
external fixation is commonly used before freeing the knee. Even with
this enforced immobility, most patients have restored knee motion. Egol
et al.51 reported that after a mean
of 15 days of cross-knee external fixation before definitive internal
or external fixation on the same side of the knee, patients averaged
106 degrees of knee flexion. Although the authors thought that the
results were satisfactory, they speculated that the external fixator
might have contributed to the decreased range of flexion seen in some
of their patients. Marsh et al.111
reported that even 6 weeks of cross-knee immobilization before external
fixation on the tibial side of the knee resulted in excellent knee
motion.
fracture, it is challenging to treat. Knee manipulation may improve
motion in some knees that are not progressing. It is preferable to wait
until healing has likely occurred, usually around 3 months. After 4
months, a surgical lysis of intra-articular adhesions, either open or
arthroscopic, may be necessary.
must be taken to place implants in optimal positions to minimize
prominent painful hardware. Screws through laterally based plates can
easily be too long and prominent on the subcutaneous medial border of
the tibia, irritating the pes tendons. The relative, triangular shape
of the proximal tibia can make anterior screws that are too long appear
within bone on AP radiographs. Rarely, long anterior to posterior
screws cause neurovascular injury.133
more frequent hardware problems than traditional lower profile plates
that were compressed to the bone, and when necessary hardware may be
difficult to remove because of cold welding of screws and because these
plates are frequently long and are beneath a long length of the
anterior compartment. These plates are large enough to treat unstable
metaphyseal and diaphyseal fractures, which makes them more prominent
in the proximal lateral subcutaneous area than 3.5-mm lateral buttress
plates (Fig. 53-34). These plates are inserted
through the anterior compartment. During acute treatment of the
fracture, the plate can be applied to the bone and the screws inserted
using a minimally invasive approach. Hardware removal may be more
difficult than insertion through such limited incisions and may have
greater risks than the original implant insertion. These problems are
compounded if locked screws are cold welded to the plate. The incidence
and severity of these problems are currently not well known but cold
welded screws have been reported primarily with the LISS system.38,128
difficulty. Split depression fractures need void filler solely for the
purpose of support of the reduced articular surface and not to ensure
union, which occurs reliably. High-energy AO/OTA type C-3 and Schatzker
6 fractures, particularly when widely displaced and open, have a risk
for healing delays or nonunion.
challenging. As in any nonunion, the presence or absence of infection
is the first issue in deciding on treatment techniques. Infection is
suspected based on the history, clinical examination, imaging, and
laboratory studies. In periarticular nonunions of the proximal tibia,
both the mobility of the joint and the presence or absence of
posttraumatic arthritis must be considered. If the joint is
salvageable, the nonunion is repaired with internal or external
fixation and usually some osteoinductive material such as autologous
bone graft or bone morphogenic protein is added. Accurate alignment
must be restored. If the joint cannot be salvaged, the nonunion should
be treated along with the knee by arthrodesis or arthroplasty.
 |
|
FIGURE 53-34
Photograph of the lateral side of the knee of a patient 9 months after a open reduction with internal fixation shows the prominence from a locking plate, which can be problematic for the patient. |
treating tibial plateau fractures. Tibial plateau fractures can lead to
extra-articular angular malunion, intra-articular malunions, or
combinations of both. Angular malunion may occur in any plane. If
angular deformity is significant, it will cause functional problems, be
cosmetically objectionable, and increase the risk for posttraumatic OA.
The degree of deformity that will predictably cause these problems is
uncertain and must be assessed on a case-by-case basis. If correction
is necessary, the surgical approach and technique will depend on the
direction and amount of the deformity, the presence of preexisting
implants, and the condition of the soft tissue envelope. Preoperative
planning is critically important. Either opening or closing wedge
osteotomies may be chosen and can be fixed internally or with an
external fixator.
evaluate and to surgically correct. Intra-articular malunions can
contribute to limb malalignment. For instance, a major split depression
lateral plateau fracture that heals with the lateral joint
significantly depressed will result in a limb aligned in valgus. If the
alignment is unacceptable, it can be corrected through an
intra-articular osteotomy to restore the lateral articular surface and
support the lateral femoral condyle. An alternate approach accepts the
intra-articular deformity and aligns the limb with an extra-articular
osteotomy. In certain challenging deformities, combined intra- and
extra-articular osteotomies may be the best approach113 (Fig. 53-35). Toro-Arbelaez et al.159
reported a small series of five patients where deformity was corrected
through an intra-articular nonunion by nonunion takedown, fragment
repositioning, grafting, and internal fixation.
to develop severe arthrosis than the hip after acetabular fracture or
the ankle after tibial plafond fracture.109
In two series from the same institution, both with 5 to 11 years of
follow-up, the ankle after tibial plafond fracture had developed
arthrosis in over 90% of patients with the majority being moderate or
severe, whereas the knee after high-energy tibial plateau fracture had
arthrosis in only 36% of patients and over half of these cases were
only mild or moderate.112,170 At 7 years of follow-up of patients treated operatively and nonoperatively, Rasmussen131 found arthrosis in only 17%. Lachiewicz98
found that 10 of 43 operatively treated knees had arthrosis at almost 3
years of follow up. In operatively treated plateaus with 5 to 27 years
of follow-up, Rademakers et al.130 found arthrosis in 27% of malaligned
knees and only 9% with anatomic alignment. Honkonen75
found that arthrosis was increased with menisectomy and with
malalignment, but it correlated poorly with articular step-offs. Keating88
found arthrosis in 68% of knees after tibial plateau fracture in
patients over age 60, demonstrating the effect of older age on
increasing the likelihood of secondary arthritis.
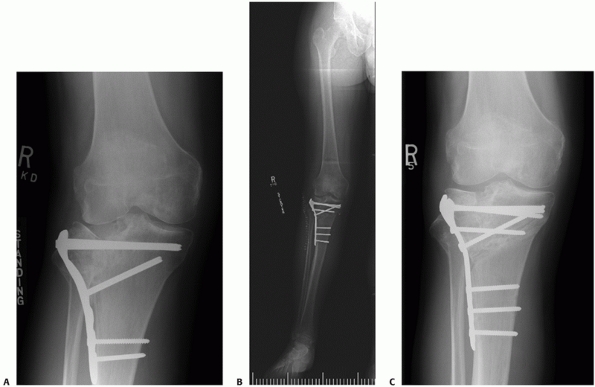 |
|
FIGURE 53-35 A,B.
Failed lateral plating of a split depression tibial plateau fracture demonstrates severe lateral articular deficiency and valgus alignment on long leg films. C. The joint was reconstructed through an intra-articular osteotomy of the depressed articular surface and an extra-articular varus osteotomy. |
treat failed tibial plateau fractures have been reported with long
follow-up (mean, 12 years).151 In
this time interval, one third of knees had been converted to prosthetic
arthroplasty and 40% of remaining knees had moderate or severe
degenerative changes. Despite this, most surviving grafts continued to
provide reasonable function. A tibial osteotomy to change alignment was
a frequent associated procedure and there was a trend to better results
with concomitant meniscal transplantation. Mosaicplasty has been
reported as another possibility to reconstruct defects in the lateral
tibial plateau after fracture.138
elderly patients with painful posttraumatic arthritis and/or deformity
after a tibial plateau fracture. Recent case series have shown that
relief of pain and improved function are predictably achieved but that
there is a high incidence of postoperative complications and
reoperations including infection, component revisions, and knee
manipulation.172 In addition, these
are frequently technically demanding arthroplasties due to hardware,
proximal tibial deformity, scarred soft tissues, and stiffness. Weiss
et al.172 reported a 21% reoperation
rate for knee arthroplasty after tibial plateau fracture. These results
indicate that conversion of a symptomatic knee after a tibial plateau
fracture to a knee arthroplasty should not be undertaken lightly (Fig. 53-36).
tibial plateau fractures is difficult since the wide range of fracture
patterns leads to variable results and the factors that potentially
affect outcome are different for different patterns. Certain split
fractures may be percutaneously stabilized to prevent displacement with
minimal risk and near-perfect outcomes after a relatively rapid
recovery. On the other hand, high-energy Schatzker 6 patterns with
AO/OTA type C-3 comminution have high risks of injury and
treatment-related complications and a recovery time that may last
years, leading to variable functional outcomes.
outcomes are also controversial. They include patient factors, injury
factors, and then factors involved with treatment. Because treatment is
under the surgeon’s control, it leads to the most controversy and the
relative importance of limb alignment, articular reduction, and
associated ligament and meniscal injuries are all areas that spark
controversy.
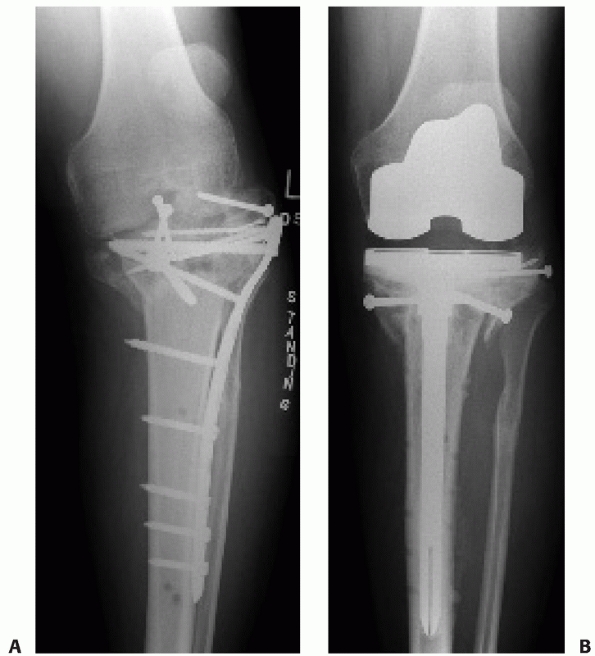 |
|
FIGURE 53-36
Total knee replacement after tibial plateau fracture is unusual. It is often more difficult and complicated than after routine primaries, as illustrated in this case where removal of the failed lateral locking plate was complicated and difficult (A,B). |
outcomes if knee alignment is maintained and complications are avoided.
The proximal articular surface of the tibia is relatively resistant to
posttraumatic arthrosis and most patients recover knee function and do
not need reconstructive surgery. Knee replacement after a tibial
plateau fracture is very rare, indicating that pain is relatively
minimal and that reasonable and long-lasting knee function is restored
in most patients. Over an 11-year period during which 13,821 knee
arthroplasties were performed at the Mayo Clinic, only 62 knee
arthroplasties were performed in patients with a prior fracture of the
tibial plateau.172 In another study of tibial plateau fracture patients older than 60 years, only 2 of 151 required knee arthroplasty.172
lower extremity articular fractures, the articular surface of the
proximal tibia appears to be more tolerant to fractures than the ankle
or hip.170 At 5 to 11 years after
injury, a series of high-energy plateau fractures treated by external
fixation were found to have good knee function and a low rate of
arthrosis. The general health status of the patients equaled
age-matched controls and the knee score averaged 90 on a 100-point
scale.112 These results are in
contradistinction to another group of patients with 5 to 11 years of
follow-up after high-energy tibial plafond fractures where patients had
decreased general health status compared to age-matched control
subjects and significant residual ankle pain and decreased function.
This may be due to the less congruent nature of the articulation, the
characteristics of the cartilage, a load-sharing effect of the menisci,
or perhaps other factors.
clearly depends on the fracture pattern but as a general rule can be
expected to take at least 1 year. One study found significant residual
strength deficits at 1 year after plateau fracture in the majority of
patients tested.59 Another study showed that recovery stabilized after 2 years.170
In one study, medial condylar fractures and bicondylar fractures with a
medial tilt were found to have less favorable results than lateral side
patterns and varus was more poorly tolerated than valgus.23
One study showed that the presence of a proximal fibula fracture was a
poor prognostic sign. Another study showed better results in
monocondylar than bicondylar fractures.130
As an exception in one study of internal fixation of tibial plateau
fractures with an average of 2.7 years of follow-up, there was no
association between fracture pattern and outcome.98
found that removal of the meniscus for exposure led to posttraumatic
degenerative arthritis in 74% of cases. However, identifying and
repairing injured menisci, although advocated, have insufficient data
to show that this leads to better outcomes.
For instance, one study showed dramatically different outcomes in
patients older than 40 compared to those younger than 40. At 8 years
after injury, only 12 of 21 patients in the over-40 age group were
equal to age-matched control subjects on patient-derived outcome
measures.170 Another study of
patients older than 50 years with tibial plateau fractures found that
regardless of fracture pattern or operative or nonoperative treatment,
only 35% (14 of 40 patients) were satisfied with their result.145 In another study, patients older than 60 were found to have mediocre functional outcomes and frequent degenerative changes.88
One study reported that favorable results were achieved in 82% of
operatively treated patients older than 55 but increasing age still
correlated with poorer outcomes.157 One study found recovery of knee function was slower in patients older than 40.59
As an exception to these studies, a recent study of operative
treatment, with 5 to 27 years of follow-up, did not find a negative
effect with increased age.130
outcome represent an important and controversial issue. In a cadaver
model, Brown et al.24 showed that
articular step-offs increased contact loading but less than they
expected. Some clinical studies have identified that the quality of
articular reduction is an important determinant of outcome,11,19,21
but other authors have thought that limb alignment is the most critical
factor and that, in a well-aligned limb, articular step-offs are less
important.20,39,46,48,75,99,130,145
Some of this controversy can be resolved by the fact that in many
fracture patterns the articular reduction and eventual alignment of the
knee are fairly closely linked to each other because large residual
articular displacements lead to limb malalignment. One study of open
reduction and internal fixation of plateau fractures found that neither
the fracture pattern nor the quality of reduction affected patient
outcome at an average of more than 8 years after injury.170
Two studies followed similar high-energy fractures treated by external
fixation, and one found that knee scores were significantly better in
patients with anatomic articular reductions, while the other found that
good outcomes were predictable in well-aligned stable knees.97,145 Another recent study found that
malalignment of greater than 5 degrees led to a higher incidence of
arthrosis (27% versus 9%) at follow-up of between 5 and 27 years after
operative treatment.130
correlate with preventing deformity, avoiding complications, and
younger age. For these reasons, further advances will require better
methods to control limb alignment and minimize complications. Recent
innovations in locked plating and buttressing with small fragment
precontoured plates indicate that further hardware improvements may
continue to emerge; however, the most promising area for future
advances is in new materials to fill metaphyseal voids as ways to
prevent postsurgical settling while avoiding the morbidity of iliac
crest grafts.
without increased soft tissue injury and increasingly without large
joint arthrotomies will continue to be developed. This will require
further improvements in intraoperative imaging. Currently available
intraoperative three-dimensional imaging is just a start.
better preservation of articular cartilage surfaces will need to be
developed. Since we are near the limits of what can be done
mechanically, major advances will need to be in biologic methods to
help restore and preserve damaged articular surfaces.
function in elderly patients will need to be developed and clinical
research will need to define the reasons for poorer outcome in this
patient group. Only in this way will treatment advances be directed at
improving the poor results frequently seen in these patients.
MZ, Chang CH, Chan YS, et al. Arthroscopic evaluation of soft tissue
injuries in tibial plateau fractures: retrospective analysis of 98
cases. Arthroscopy 2006;22:669-675.
AM, Burton M, Hashmi M, et al. Outcome of complex fractures of the
tibial plateau treated with a beam-loading ring fixation system. J Bone
Joint Surg Br 2003;85:691-699.
AM, Burton M, Hashmi M, et al. Treatment of displaced bicondylar tibial
plateau fractures (OTA-41C2&3) in patients older than 60 years of
age. J Orthop Trauma 2003;17:346-352.
AM, Saleh M, Bolongaro S, et al. The strength of different fixation
techniques for bicondylar tibial plateau fractures: a biomechanical
study. Clin Biomech (Bristol, Avon) 2003;18:864-870.
AM, Saleh M, Eastell R, et al. Influence of bone quality on the
strength of internal and external fixation of tibial plateau fractures.
J Orthop Res 2006;24:2080-2086.
DD, Mosqueda T, Thomas T, et al. Quantifying tibial plafond fracture
severity: absorbed energy and fragment displacement agree with clinical
rank ordering. J Orthop Res 2008;26:1046-1052.
AG. Fractures of the lateral tibial condyle treated by skeletal
traction and early mobilisation; a review of sixty cases with special
reference to the long-term results. J Bone Joint Surg Br
1956;38B:699-708.
SS, Zlowodzki M, Lelwica A, et al. The use of calcium phosphate bone
cement in fracture treatment. A meta-analysis of randomized trials. J
Bone Joint Surg Am 2008;90A:1186-1196.
DP, Nork SE, Mills WJ, et al. Functional outcomes of severe bicondylar
tibial plateau fractures treated with dual incisions and medial and
lateral plates. J Bone Joint Surg Am 2006;88A:1713-1721.
DP, Nork SE, Mills WJ, et al. Complications associated with internal
fixation of high-energy bicondylar tibial plateau fractures utilizing a
two-incision technique. J Orthop Trauma 2004;18:649-657.
DP, O’Mara TJ, Taitsman LA, et al. Frequency and fracture morphology of
the posteromedial fragment in bicondylar tibial plateau fracture
patterns. J Orthop Trauma 2008;22:176-182.
MO, Kazmier P, Anglen JO. Repair or reattachment of the meniscus after
fixation of a tibial plateau fracture. J Orthop Trauma 2005;19:198-200.
J, Noblin JD, Freeland AE. Posteromedial second incision to reduce and
stabilize a displaced posterior fragment that can occur in Schatzker
type V bicondylar tibial plateau fractures. Orthopedics 1996;19:903-904.
SK, Agnew SG, Mayo KA, et al. Immediate internal fixation of open,
complex tibial plateau fractures: treatment by a standard protocol. J
Orthop Trauma 1992;6:78-86.
AE, Soucacos PN, Glisson RR, et al. Load tolerance of tibial plateau
depressions reinforced with a cluster of K-wires. Bull Hosp Jt Dis
1996;55:12-15.
T, McCarty LP 3rd, Harris MB, et al. The posterior shearing tibial
plateau fracture: treatment and results via a posterior approach. J
Orthop Trauma 2005;19:305-310.
A, Reddy NS, Chaudhury J, et al. The results of surgical management of
displaced tibial plateau fractures in the elderly. Injury
1995;26:291-297.
CP, Rorabeck CH, Bourne RB. Tibial plateau fractures. An analysis of
the results of treatment in 60 patients. Clin Orthop Relat Res
1984:193-199.
C, Fankhauser F, Hofer HP, et al. Three-year results of proximal tibia
fractures treated with the LISS. Clin Orthop Relat Res 2006;445:222-229.
M, Turanli S, Doral MN, et al. The impact of proximal fibula fractures
in the prognosis of tibial plateau fractures: a novel classification.
Knee Surg Sports Traumatol Arthrosc 2005;13:323-328.
TD, Anderson DD, Nepola JV, et al. Contact stress aberrations following
imprecise reduction of simple tibial plateau fractures. J Orthop Res
1988;6:851-862.
RW, Carlton A, Holmes R. Interporous hydroxyapatite as a bone graft
substitute in tibial plateau fractures. Clin Orthop Relat Res
1989:53-62.
P, Tamim H. Occult fractures of tibial plateau detected employing
magnetic resonance imaging. Arch Orthop Trauma Surg 2000;120:355-357.
Orthopaedic Trauma Society. Open reduction and internal fixation
compared with circular fixator application for bicondylar tibial
plateau fractures. Results of a multicenter, prospective, randomized
clinical trial. J Bone Joint Surg Am 2006;88A:2613-2623.
DA. Bicondylar fracture of the posterior aspect of the tibial plateau.
A case report and a modified operative approach. J Bone Joint Surg Am
1998;80A:1049-1052.
ML, McGee JP, Ebraheim NA, et al. Response of the lateral meniscus of
the dog to wide incision and repair of the meniscotibial ligament. J
Orthop Trauma 1995;9:141-144.
KK, Resnick D, Goodwin D, et al. Posteromedial tibial plateau injury
including avulsion fracture of the semimembranous tendon insertion
site: ancillary sign of anterior cruciate ligament tear at MR imaging.
Radiology 1999;211:754-758.
PS, Klimkiewicz JJ, Luchetti WT, et al. Impact of CT scan on treatment
plan and fracture classification of tibial plateau fractures. J Orthop
Trauma 1997;11:484-489.
YS, Yuan LJ, Hung SS, et al. Arthroscopic-assisted reduction with
bilateral buttress plate fixation of complex tibial plateau fractures.
Arthroscopy 2003;19:974-984.
YH, Tu YK, Yeh WL, et al. Tibial plateau fracture with compartment
syndrome: a complication of higher incidence in Taiwan. Chang Gung Med
J 2000;23:149-155.
CP, Tryfonidis M, Alvi F, et al. Inter- and intra-observer variation of
the Schatzker and AO/OTA classifications of tibial plateau fractures
and a proposal of a new classification system. Ann R Coll Surg Engl
2007;89:400-404.
TY, Bardana D, Bailey M, et al. Functional outcome of tibial plateau
fractures treated with the fine-wire fixator. Injury 2005;36:1467-1475.
AP, King D, Gibbon AJ. Impingement fracture of the anteromedial tibial
margin: a radiographic sign of combined posterolateral complex and
posterior cruciate ligament disruption. Skeletal Radiol 2001;30:114-116.
PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using
the less invasive stabilization system: surgical experience and early
clinical results in 77 fractures. J Orthop Trauma 2004;18:528-535.
JF. The posterior shearing tibial plateau fracture: treatment and
results via a posterior approach. J Orthop Trauma 2005;19:508; author
reply.
Boeck H, Opdecam P. Posteromedial tibial plateau fractures. Operative
treatment by posterior approach. Clin Orthop Relat Res
1995;(320):125-128.
JP, Deangelis NA, Anderson R. Anatomy of the superficial peroneal nerve
in relation to fixation of tibia fractures with the less invasive
stabilization system. J Orthop Trauma 2004;18:536-539.
TA, Nepola JV, el-Khoury GY. Cast brace treatment of proximal tibia
fractures. A ten-year follow-up study. Clin Orthop Relat Res
1988;(231):196-204.
RB, Hohl M, Hopp E Jr. Ligament injuries associated with tibial plateau
fractures. Clin Orthop Relat Res 1990:226-233.
GK, Kontos S, Katsenis D, et al. Treatment of high-energy tibial
plateau fractures by the Ilizarov circular fixator. J Bone Joint Surg
Br 1996;78B:710-717.
DB, Locher FG, Maylahn DJ. Fractures of the tibial plateau. Treatment
by closed reduction and spica cast. J Bone Joint Surg Am
1979;61A:989-995.
PJ, Connolly JF. Closed reduction of tibial plateau fractures. A
comparison of functional and roentgenographic end results. Clin Orthop
Relat Res 1988:116-126.
PJ, Rangitsch MR, Colville MR, et al. Treatment of tibial plateau
fractures by limited internal fixation. Clin Orthop Relat Res
1997:47-57.
KA, Su E, Tejwani NC, et al. Treatment of complex tibial plateau
fractures using the less invasive stabilization system plate: clinical
experience and a laboratory comparison with double plating. J Trauma
2004;57:340-346.
KA, Tejwani NC, Capla EL, et al. Staged management of high-energy
proximal tibia fractures (OTA types 41): the results of a prospective,
standardized protocol. J Orthop Trauma 2005;19:448-455; discussion 56.
JK, Ryzewicz M, Hartshorn C, et al. Optimizing the management of Moore
type I postero-medial split fracture dislocations of the tibial head:
description of the Lobenhoffer approach. J Orthop Trauma
2007;21:330-336.
DL. Anterior approach to the knee with osteotomy of the tibial tubercle
for bicondylar tibial fractures. J Bone Joint Surg Am 1988;70A:208-219.
DC, Sommers MB, Kam BC, et al. Knee stability after articulated
external fixation. Am J Sports Med 2005;33:1735-1741.
CD, Zimmer JW, Schepsis AA. The role of arthroscopy in the assessment
and treatment of tibial plateau fractures. Arthroscopy 1993;9:584-590.
MJ, Yacoubian S, Geller D, et al. Prediction of soft-tissue injuries in
Schatzker II tibial plateau fractures based on measurements of plain
radiographs. J Trauma 2006;60:319-323; discussion 24.
MJ, Yacoubian S, Geller D, et al. The incidence of soft tissue injury
in operative tibial plateau fractures: a magnetic resonance imaging
analysis of 103 patients. J Orthop Trauma 2005;19:79-84.
P, Will EM, Keating JF. Recovery of knee function following fracture of
the tibial plateau. J Bone Joint Surg Br 2005;87B:1233-1236.
RF, Mallik AR, Szporn M. Hybrid external fixation of comminuted tibial
plateau fractures. Clin Orthop Relat Res 1996:203-210.
S, Hohl M. The significance of early motion in the treatment of tibial
plateau fractures. Clin Orthop Relat Res 1986:135-138.
GM. Combined anterior and posterior approaches for complex tibial
plateau fractures. J Bone Joint Surg Br 1994;76B:285-289.
T, Schandelmaier P, Marti A, et al. Less invasive stabilization of
complex tibial plateau fractures: a biomechanical evaluation of a
unilateral locked screw plate and double plating. J Orthop Trauma
2004;18:546-551.
T, Schandelmaier P, Muller M, et al. Single lateral locked screw
plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res
2005;439:207-214.
KS, Skalak AS, Marcus RE, et al. Analysis of anatomic periarticular
tibial plate fit on normal adults. Clin Orthop Relat Res
2007;461:245-257.
G, Sems SA, Huebner D, et al. Results of polyaxial locked-plate
fixation of periarticular fractures of the knee. J Bone Joint Surg Am
2007;89A:614-620.
MC, Henstorf JE, Vessely MB, et al. Closed reduction and percutaneous
stabilization of tibial plateau fractures. Orthopedics 1995;18:623-626.
J, Chandrashekar N, Gill B, et al. The geometry of the tibial plateau
and its influence on the biomechanics of the tibiofemoral joint. J Bone
Joint Surg Am 2008;90A:2724-2734.
TF, Klatt J, Bachus KN. Biomechanical analysis of bicondylar tibial
plateau fixation: how does lateral locking plate fixation compare to
dual plate fixation? J Orthop Trauma 2007;21:301-306.
M. Articular fractures of the proximal tibia. In: Evarts C, ed. Surgery
of the Musculoskeletal System. New York: Churchill-Livingstone,
1993:3471-3497.
RE, Bucholz RW, Mooney V. Porous hydroxyapatite as a bone-graft
substitute in metaphyseal defects. A histometric study. J Bone Joint
Surg Am 1986;68A:904-911.
P, Matter P, Minter J. Arthroscopically assisted treatment of lateral
tibial plateau fractures in skiers: use of a cannulated reduction
system. J Orthop Trauma 1994;8:273-281.
WG, Verheyen CC, Leemans R. An injectable calcium phosphate cement as a
bone-graft substitute in the treatment of displaced lateral tibial
plateau fractures. Injury 2003;34:141-144.
SS, Chao EK, Chan YS, et al. Arthroscopically assisted osteosynthesis
for tibial plateau fractures. J Trauma 2003;54:356-363.
JE. Patellar Graft for severely depressed comminuted fractures of the
lateral tibial condyle. J Bone Joint Surg Am 1965;47A:842-847.
DB, Bjerg-Nielsen A, Laursen N. Conventional radiographic examination
in the evaluation of sequelae after tibial plateau fractures. Skeletal
Radiol 1988;17:330-332.
DB, Rude C, Duus B, et al. Tibial plateau fractures. A comparison of
conservative and surgical treatment. J Bone Joint Surg Br
1990;72B:49-52.
R, Luo CF, Wang MC, et al. A comparative study of Less Invasive
Stabilization System (LISS) fixation and two-incision double plating
for the treatment of bicondylar tibial plateau fractures. Knee
2008;15:139-143.
MA, Egol KA, Peindl R, et al. Split depression tibial plateau
fractures: a biomechanical study. J Orthop Trauma 2002;16:172-177.
H, Sharma N, Kanojia RK. Small wire external fixation for high-energy
tibial plateau fractures. J Orthop Surg (Hong Kong) 2007;15:137-143.
D, Athanasiou V, Megas P, et al. Minimal internal fixation augmented by
small wire transfixion frames for high-energy tibial plateau fractures.
J Orthop Trauma 2005;19:241-248.
JF, Hajducka CL, Harper J. Minimal internal fixation and
calcium-phosphate cement in the treatment of fractures of the tibial
plateau. A pilot study. J Bone Joint Surg Br 2003;85B:68-73.
D, Pearle A, Hufner T, et al. First clinical results and consequences
of intraoperative three-dimensional imaging at tibial plateau
fractures. J Trauma 2007;63:239-244.
JC, Bailey WH. Experimental tibial-plateau fractures. Studies of the
mechanism and a classification. J Bone Joint Surg Am 1968;50A:1522-1534.
A, Siewerdsen JH, Whyne CM, et al. Intraoperative cone-beam CT for
imageguided tibial plateau fracture reduction. Comput Aided Surg
2007;12:195-207.
L, Lieberman JM, Motta AO, et al. Evaluation of tibial plateau
fractures: efficacy of MR imaging compared with CT. AJR Am J Roentgenol
1994;163:141-147.
KJ, Polatsch D, Kummer FJ, et al. Split fractures of the lateral tibial
plateau: evaluation of three fixation methods. J Orthop Trauma
1996;10:304-308.
KJ, Sanders R, Borrelli J, et al. Indirect reduction and percutaneous
screw fixation of displaced tibial plateau fractures. J Orthop Trauma
1992;6:340-346.
A, Whittle AP. Treatment of complex (Schatzker type VI) fractures of
the tibial plateau with circular wire external fixation: retrospective
case review. J Orthop Trauma 2000;14:339-344.
PF, Funcik T. Factors influencing the results of open reduction and
internal fixation of tibial plateau fractures. Clin Orthop Relat Res
1990:210-215.
O, Bergman B, Korner L, et al. Tibial condylar fractures. A twenty-year
follow-up. J Bone Joint Surg Am 1986;68A:13-19.
LP, Corl FM, Fishman EK. Multi- and single detector CT with 3D volume
rendering in tibial plateau fracture imaging and management. Crit Rev
Comput Tomogr 2002;43:251-282.
BA, Herrera DA, Macdonald P, et al. The medial approach for
arthroscopic-assisted fixation of lateral tibial plateau fractures:
patient selection and mid- to long-term results. J Orthop Trauma
2008;22:201-205.
RY, Birdsall PD, Mucci B, et al. Spiral computed tomography with two-
and three-dimensional reconstruction in the management of tibial
plateau fractures. Orthopedics 1999;22:929-932.
P, Gerich T, Witte F, et al. Use of an injectable calcium phosphate
bone cement in the treatment of tibial plateau fractures: a prospective
study of twenty-six cases with twenty-month mean follow-up. J Orthop
Trauma 2002;16:143-149.
P, Schulze M, Gerich T, et al. Closed reduction/percutaneous fixation
of tibial plateau fractures: arthroscopic versus fluoroscopic control
of reduction. J Orthop Trauma 1999;13:426-431.
L, Murrone M, Marini S, et al. Tibial plateau fractures: evaluation
with multidetector-CT. Radiol Med (Torino) 2004;108:503-514.
D, Costa ML, Gaffey A. Open reduction and internal fixation versus
hybrid fixation for bicondylar/severe tibial plateau fractures: a
systematic review of the literature. Arch Orthop Trauma Surg 2008 Jan 4.
AR, Covall DJ, Whitelaw GP. Internal versus external fixation of
bicondylar tibial plateau fractures. Orthop Rev 1992;21:1433-1436.
JL, Buckwalter J, Gelberman R, et al. Articular fractures: does an
anatomic reduction really change the result? J Bone Joint Surg Am
2002;84A:1259-1271.
JL, Slongo TF, Agel J, et al. Fracture and dislocation classification
compendium—2007: Orthopaedic Trauma Association classification,
database and outcomes committee. J Orthop Trauma 2007;21(suppl):S1-S133.
JL, Smith ST, Do TT. External fixation and limited internal fixation
for complex fractures of the tibial plateau. J Bone Joint Surg Am
1995;77A:661-673.
JL, Weigel DP, Dirschl DR. Tibial plafond fractures. How do these
ankles function over time? J Bone Joint Surg Am 2003;85A:287-295.
RK, Kerkhoffs GM, Rademakers MV. Correction of lateral tibial plateau
depression and valgus malunion of the proximal tibia. Oper Orthop
Traumatol 2007;19:101-113.
J, Marsh JL, Nepola JV, et al. Radiographic fracture assessments: which
ones can we reliably make? J Orthop Trauma 2000;14:379-385.
TM, Harvey JP Jr. Roentgenographic measurement of tibial-plateau
depression due to fracture. J Bone Joint Surg Am 1974;56A:155-160.
TM, Meyers MH, Harvey JP Jr. Collateral ligament laxity of the knee.
Long-term comparison between plateau fractures and normal. J Bone Joint
Surg Am 1976;58A:594-598.
TM, Patzakis MJ, Harvey JP. Tibial plateau fractures: definition,
demographics, treatment rationale, and long-term results of closed
traction management or operative reduction. J Orthop Trauma
1987;1:97-119.
A, Heikkila J, Magyar G, et al. Fixation strength and pin tract
infection of hydroxyapatite-coated tapered pins. Clin Orthop Relat Res
2001:209-217.
KL, Karunakar MA, Frankenburg EP, et al. Bicondylar tibial plateau
fractures: a biomechanical study. Clin Orthop Relat Res 2003:189-195.
ME, Allgower M, Schneider R, et al. Manual of internal fixation.
Technique recommended by the AO group 1979 (ed 2):256-257.
LW, Engelsohn E, Umans H. Comparison of CT and MRI in patients with
tibial plateau fracture: can CT findings predict ligament tear or
meniscal injury? Skeletal Radiol 2007;36:145-151.
ME, Nazarian S, Koch P, et al. The Comprehensive Classification of
Fractures of Long Bones. New York: Springer-Verlag, 1990.
CP, D’Ambrosia R, Dabezies EJ. The small pin circular fixator for
proximal tibial fractures with soft tissue compromise. Orthopedics
1991;14:273-280.
T, Tokunaga M, Hiroshima S, et al. Arthroscopic management of tibial
plateau fractures: comparison with open reduction method. Arch Orthop
Trauma Surg 2003;123:489-493.
TG, Ebraheim NA, Frogameni A. Meniscal detachment to approach lateral
tibial plateau fractures. Clin Orthop Relat Res 1995 May:192-198.
S, Mahon A, Green S, et al. A biomechanical study comparing a raft of
3.5 mm cortical screws with 6.5 mm cancellous screws in depressed
tibial plateau fractures. Knee 2006;13:231-235.
CR, Evans LG, Rice S, et al. A new surgical approach to fractures of
the lateral tibial plateau. J Bone Joint Surg Am 1984;66A:1236-1240.
P, McKinley TO, Nepola JV, et al. Complications of locking plate
fixation in complex proximal tibia injuries. J Orthop Trauma
2007;21:83-91.
N, Murray JM, Kumar D, et al. Insufficiency fracture of the tibial
plateau: an often missed diagnosis. Acta Orthop Belg 2006;72:587-591.
MV, Kerkhoffs GM, Sierevelt IN, et al. Operative treatment of 109
tibial plateau fractures: five- to 27-year follow-up results. J Orthop
Trauma 2007;21:5-10.
PS. Tibial condylar fractures. Impairment of knee joint stability as an
indication for surgical treatment. J Bone Joint Surg Am
1973;55A:1331-1350.
JR, Werner FW, Green JK, et al. Medial buttress versus lateral locked
plating in a cadaver medial tibial plateau fracture model. J Orthop
Trauma 2007;21:444-448.
ML, Harper WH, Oni OO. A serious vascular complication of internal
fixation of a tibial plateau fracture: a cautionary tale from which
several lessons can be learned. J Trauma 1996;40:323-325.
JS, Van Slyke MA, Moulton MJ, et al. Safe placement of proximal tibial
transfixation wires with respect to intracapsular penetration. J Orthop
Trauma 2001;15:10-17.
WM, Rudzki JR, Borrelli J Jr. Treatment of complex proximal tibia
fractures with the less invasive skeletal stabilization system. J
Orthop Trauma 2004;18:521-527.
MD, Meinhard BP. Medial external fixation with lateral plate internal
fixation in metaphyseal tibia fractures. A report of eight cases
associated with severe soft-tissue injury. Clin Orthop Relat Res
1990:215-223.
WH, Oskam J, Vierhout PA. Arthroscopically assisted osteosynthesis of
tibial plateau fractures in patients older than 55 years. Arthroscopy
2001;17:826-831.
T, Lill H, Hepp P, et al. Autologous osteochondral mosaicplasty for
treatment of a posttraumatic defect of the lateral tibial plateau: a
case report with two-year follow-up. J Orthop Trauma 2005;19:217-222.
TA, Leighton RK. Comparison of autogenous bone graft and endothermic
calcium phosphate cement for defect augmentation in tibial plateau
fractures. A multicenter, prospective, randomized study. J Bone Joint
Surg Am 2008;90A:2057-2061.
FH, Vander Griend RA, Ward EF, et al. Tibial plateau fractures. A
review of operative treatment using AO technique. Orthopedics
1987;10:745-750.
J. Fractures of the tibial plateau. In: Schatzker JT, Tile M, eds.
Rationale of Operative Fracture Care. Berlin: Springer-Verlag,
1987:279-295.
J. Fractures of the tibial plateau. In: Schatzker J, Tile M, eds.
Rationale of Operative Fracture Care. Berlin:, Springer-Verlag,
1988:279.
J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto
experience 1968—1975. Clin Orthop Relat Res 1979:94-104.
M, Kaab MJ, Haas N. Stabilization of proximal tibial fractures with the
LIS-System: early clinical experience in Berlin. Injury 2003;34(suppl
1):A30-A35.
R, Brinker MR, Beaver R, et al. Patient self-assessment of tibial
plateau fractures in 40 older adults. Am J Orthop 1998;27:512-519.
T, Wardlaw D. The use of cast-bracing as treatment for fractures of the
tibial plateau. J Bone Joint Surg Br 1981;63B:575-578.
D, Franchi AV, Campanile J. Iliac autograft for reconstruction of
severely depressed fracture of a lateral tibial plateau. Brief note. J
Bone Joint Surg Am 1985;67A:1270-1272.
D, Mallik AR, Wetzler MJ, et al. Early weight bearing of lateral tibial
plateau fractures. Clin Orthop Relat Res 1993:232-237.
JM, Torner P, Garcia S, et al. Use of bone allograft in tibial plateau
fractures. Arch Orthop Trauma Surg 1998;117:357-359.
SN, Karunakar MA. Early wound complications after operative treatment
of high energy tibial plateau fractures through two incisions. Bull NYU
Hosp Jt Dis 2007;65:115-119.
N, Krywulak S, Backstein D, et al. Long-term follow-up of fresh tibial
osteochondral allografts for failed tibial plateau fractures. J Bone
Joint Surg Am 2003;85A(suppl 2):33-39.
L, Abdollahi K, Lee J, et al. The prevalence of soft tissue injuries in
nonoperative tibial plateau fractures as determined by magnetic
resonance imaging. J Orthop Trauma 2002;16:628-631.
ST, Marsh JL, Nepola JV, et al. Tibial plateau fractures treated with
external fixation and minimal internal fixation. Iowa Orthop J
1991;11:69-77.
JP, Wilson TC, Volgas DA, et al. The less invasive stabilization system
in the treatment of complex fractures of the tibial plateau: short-term
results. J Orthop Trauma 2004;18:552-558.
EP, Westrich GH, Rana AJ, et al. Operative treatment of tibial plateau
fractures in patients older than 55 years. Clin Orthop Relat Res
2004:240-248.
M, Kapukaya A, Arslan H, et al. Outcome of open comminuted tibial
plateau fractures treated using an external fixator. J Orthop Sci
2007;12:347-353.
JB, Gardner MJ, Shindle MK, et al. Open reduction and internal fixation
of intraarticular tibial plateau nonunions. Injury 2007;38:378-383.
A, Landry S, McLaughlin K, et al. Comparative fixation of tibial
plateau fractures using alpha-BSM, a calcium phosphate cement, versus
cancellous bone graft. J Orthop Trauma 2005;19:698-702.
J. Posteromedial fracture of the tibial plateau is not an avulsion
injury. A case report and experimental study. J Bone Joint Surg Br
1994;76B:290-292.
CT Jr, Ghaderi B, Hohl M, et al. Arthroscopy of meniscal injuries with
tibial plateau fractures. J Bone Joint Surg Br 1994;76B:488-490.
JP, Johnston DW, Neidre A. Fractures of the tibial plateau: a review of
ninety-five patients and comparison of treatment methods. J Trauma
1981;21:376-381.
M, Iaguilli N, Ebraheim N, et al. Medial tibial plateau fractures: a
new classification system. J Trauma 2007;63:1418-1421.
NP, Harish S, Roberts C, et al. AO or Schatzker? How reliable is
classification of tibial plateau fractures? Arch Orthop Trauma Surg
2003;123:396-398.
JT, Coufal C. Treatment of complex lateral plateau fractures using
Ilizarov techniques. Clin Orthop Relat Res 1998:97-106.
JT, Phillips M, Karges D, et al. Lateral locking plates for the
treatment of bicondylar tibial plateau fractures: treatment protocol,
indications, and results. Presented at the 23rd Annual Meeting OTA
2007, October 19, 2007, Boston, MA.
JT, Ripple S, Hoshaw SJ, et al. Hybrid external fixation for tibial
plateau fractures: clinical and biomechanical correlation. Orthop Clin
North Am 2002;33: 199-209, ix.
DP, Marsh JL. High-energy fractures of the tibial plateau. Knee
function after longer follow-up. J Bone Joint Surg Am
2002;84A:1541-1551.
LS, Kelley M, Yang E, et al. The use of combination internal fixation
and hybrid external fixation in severe proximal tibia fractures. J
Orthop Trauma 1995;9:244-250.
NG, Parvizi J, Trousdale RT, et al. Total knee arthroplasty in patients
with a prior fracture of the tibial plateau. J Bone Joint Surg Am
2003;85A:218-221.
RD, Zhang H, Bronson DG. Experimental tibial plateau fractures
augmented with calcium phosphate cement or autologous bone graft. J
Bone Joint Surg Am 2003;85A:222-231.
GL, McLaurin TM, Hutton WC. Screw pullout strength: a biomechanical
comparison of large-fragment and small-fragment fixation in the tibial
plateau. J Orthop Trauma 2002;16:178-181.
DL, Cross AR, Eschbach EJ, et al. Grafting of massive tibial
subchondral bone defects in a caprine model using beta-tricalcium
phosphate versus autograft. J Orthop Trauma 2005;19:85-91.
S, Blaser PF, Blanc CH, et al. Comparison between standard radiography
and spiral CT with 3D reconstruction in the evaluation, classification
and management of tibial plateau fractures. Eur Radiol
2000;10:1227-1232.
WJ, Jacobs JE. Patellar graft for severely depressed comminuted
fractures of the lateral tibial condyle. J Bone Joint Surg Am
1952;34A:436-442.
SV, Nevins RT, Sallis JG, et al. Impact of MRI on treatment plan and
fracture classification of tibial plateau fractures. J Orthop Trauma
2002;16:632-637.
