Lower Limb
-
Gluteal region (L. regio glutealis).
This transitional region between the trunk and free lower limb includes
two parts of the lower limb: the rounded, prominent posterior region,
the buttocks (L. nates, clunes), and the lateral, usually less prominent hip (L. coxa) or hip region (L. regio coxae),
which overlies the hip joint and greater trochanter of the femur. Note
that the “width of the hips” in common terminology is a reference to
one’s transverse dimensions at the level of the greater trochanter. The
gluteal region is bounded superiorly by the iliac crest, medially by
the intergluteal (natal) cleft (L. natus, to be born), and inferiorly by the skin fold (groove) underlying the buttock, the gluteal fold (L. sulcus glutealis). The gluteal muscles constitute the bulk of this region. -
Thigh or femoral region (L. regio femoris).
This part/region of the free lower limb lies between the gluteal,
abdominal, and perineal regions proximally and the knee region
distally. It contains most of the femur (thigh bone), which connects the hip and knee.
P.556
The transition between the trunk and free lower limb is abrupt
anteriorly and medially. The boundary between the thigh and abdominal
regions is demarcated by the inguinal ligament anteriorly and the ischiopubic ramus of the hip bone (part of the pelvic girdle or skeleton of the pelvis) medially. The junction of these regions is the inguinal region or groin.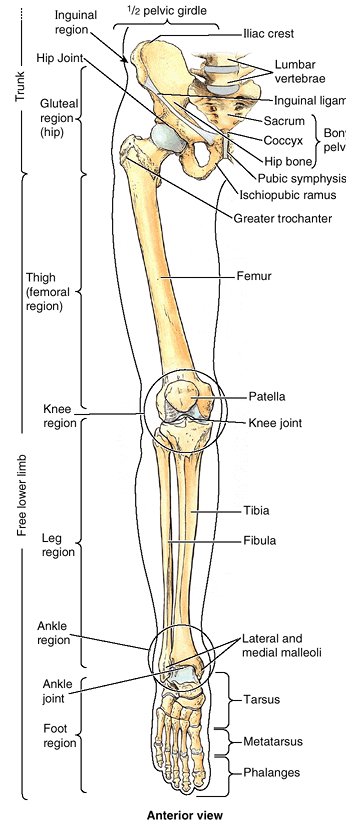 Figure 5.1. Regions and bones of lower limb.
Figure 5.1. Regions and bones of lower limb.
The pelvic girdle, consisting of the sacrum and right and left hip
bones united by the pubic symphysis, attaches the appendicular skeleton
of the free lower limb to the axial skeleton and transfers weight from
the axial skeleton to the lower limbs. -
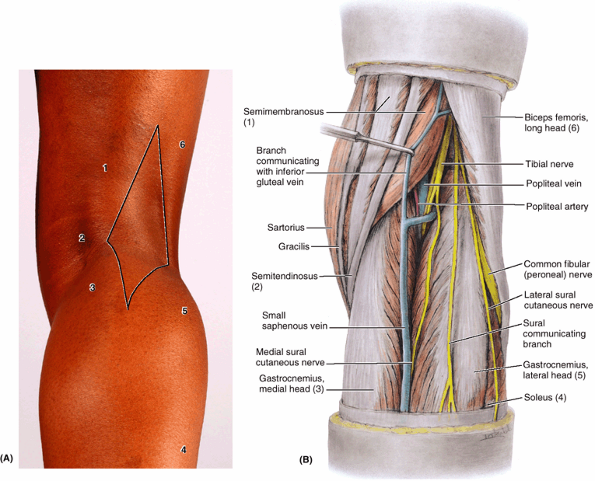
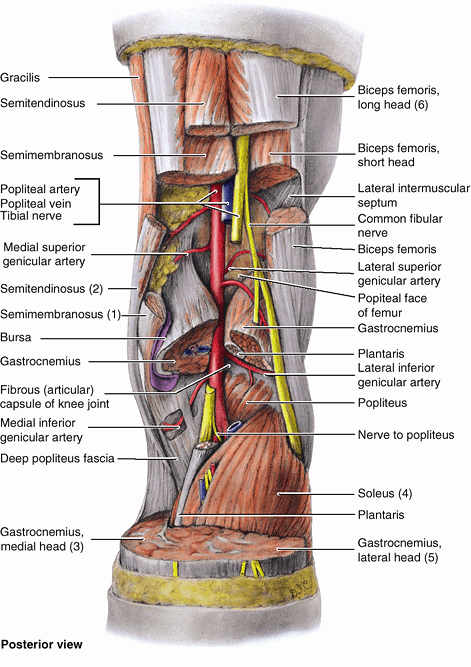
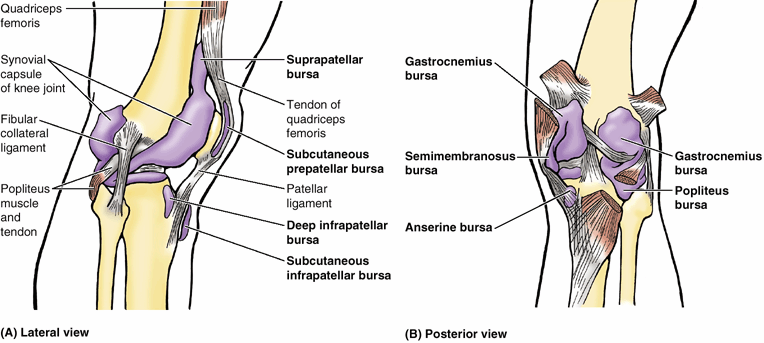
Knee (L. genu) or knee region (L. regio genus). This part/region includes the prominences (condyles) of the distal femur and proximal tibia, the head of the fibula, and the patella (knee cap, which lies anterior to the distal end of the femur) as well as the joints between these bony structures. The posterior part of the knee (L. poples) includes a well-defined, fat-filled hollow, transmitting neurovascular structures, called the popliteal fossa.
-
Leg (L. crus) or leg region (L. regio cruris).
Although laypersons refer incorrectly to the entire lower limb as “the
leg,” the leg is the part that lies between the knee and the rounded
medial and lateral prominences (malleoli) that flank the ankle joint. The leg contains the tibia (shin bone) and fibula (L. buckle) and connects the knee and foot. The calf (L. sura) of the leg is the posterior prominence caused by the triceps surae muscle, from which the calcaneal (Achilles) tendon extends to reach the heel. -
Ankle (L. tarsus) or talocrural region (L. regio talocruralis).
This includes the narrow, distal part of the leg and the malleoli; the
ankle (talocrural) joint is located between the malleoli. -
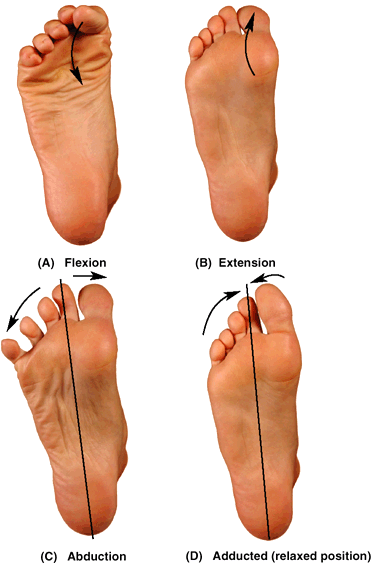
Foot (L. pes) or foot region (L. regio pedis). The foot is the distal part of the lower limb containing the tarsus, metatarsus, and phalanges (toe bones). The superior surface is the dorsum of the foot and the inferior, ground-contacting surface is the sole or plantar region. The toes are the digits of the foot. The great toe (L. hallux), like the thumb, has only two phalanges (digital bones); the other digits have three.
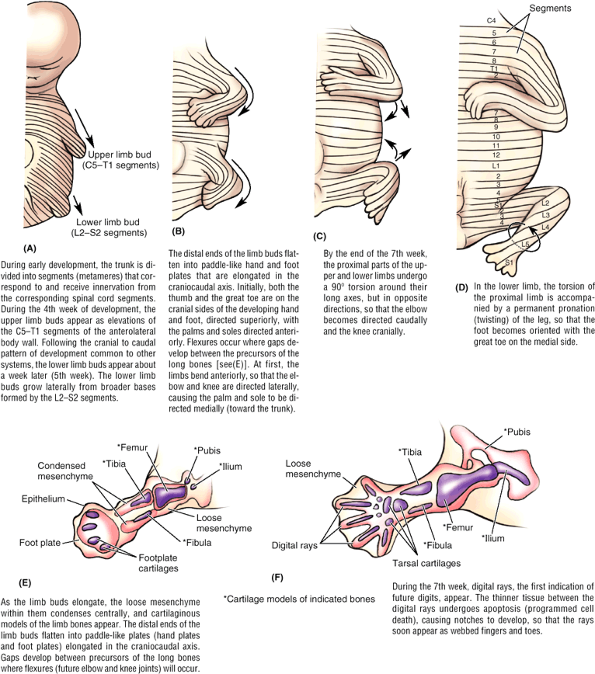
Initially, the development of the lower limb is similar to that of the
upper limb, although occurring about a week later. During the 5th week,
lower limb buds bulge from the lateral aspect of the L2–S2 segments of the trunk (a broader base than for the upper limbs) (Fig. 5.2A).
Both limbs initially extend from the trunk with their developing thumbs
and great toes directed superiorly and the palms and soles directed
anteriorly. Both limbs then undergo torsion around their long axes, but
in opposite directions (Fig. 5.2B–D).
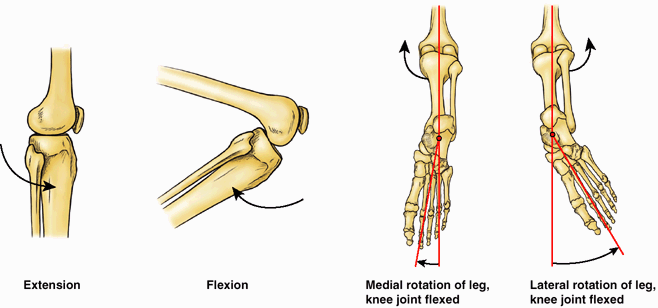
The medial rotation and the permanent pronation of the lower limb
explain (1) how the knee, unlike the joints superior to it, extends
anteriorly and flexes posteriorly, as do the joints inferior to the
knee (e.g., interphalangeal joints of the toes); (2) how the foot
becomes oriented with the great toe on the medial side (Fig. 5.2D),
whereas the hand (in the anatomical position) becomes oriented with the
thumb on the lateral side; and (3) the “barber-pole” pattern of the
segmental innervation of the skin (dermatomes) of the lower limb (see “Cutaneous Innervation of the Lower Limb,”
in this chapter). The torsion and twisting of the lower limb is still
in progress at birth (note the way babies’ feet tend to meet sole to
sole when they are brought together, like clapping). Completion of the
process coincides with the mastering of walking skills.
limb injuries. Injuries to the hips make up <3% of lower limb
injuries. In general, most injuries result from acute trauma during
contact sports such as hockey and football and from overuse during
endurance sports such as marathon races. Adolescents are most
vulnerable to these injuries because of the demands of sports on their
slowly maturing musculoskeletal systems. The cartilaginous models of
the bones in the developing lower limbs are transformed into bone by
endochondral ossification (see “Bone Development” in the Introduction) (Fig. 5.2E & F).
Because the process is not completed until early adulthood,
cartilaginous epiphysial plates still exist during the teenage years
when physical activity often peaks and involvement in competitive
sports is most common. During growth spurts, bones actually grow faster
than the attached muscle. The combined stress on the epiphysial plates
resulting from physical activity and rapid growth may result in
irritation and injury of the plates and developing bone
(osteochondrosis).
skeleton) may be divided into two functional components: the pelvic
girdle and the bones of the free lower limb (Fig. 5.1). The pelvic girdle
(bony pelvis) is a bony ring composed of the sacrum and right and left
hip bones joined anteriorly at the pubic symphysis. It attaches the
free lower limb to the axial skeleton, the sacrum being common to the
axial skeleton and the pelvic girdle. The pelvic girdle also makes up
the skeleton of the lower part of the trunk. Its protective and
supportive functions serve the abdomen, pelvis, and perineum as well as
the lower limb. The bones of the free lower limb are contained within
and specifically serve that part of the limb.
 |
|
Figure 5.2. Development of lower limb. A–D.
The upper and lower limbs develop from limb buds that arise from the lateral body wall during the 4th and 5th weeks, respectively. They then elongate, develop flexures, and rotate in opposite directions. Segmental innervation is maintained, the dermatomal pattern reflecting the elongation and spiraling of the limb. E and F. Future bones develop from cartilage models, demonstrated at the end of the 6th week (E) and beginning of the 7th week (F). |
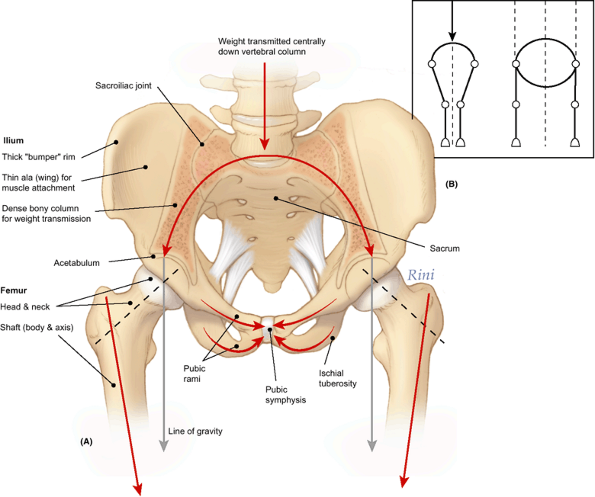
To support the erect bipedal posture better, the femurs are oblique
(directed inferomedially) within the thighs so that when standing the
knees are adjacent and are placed directly inferior to the trunk,
returning the center of gravity to the vertical lines of the supporting
legs and feet (Figs. 5.1, 5.3, and 5.4).
Compare this oblique position of the femurs with that of quadrupeds, in
whom the femurs are vertical and the knees are apart, with the trunk
mass suspended between the limbs (Fig. 5.3B).
The femurs of females are slightly more oblique than those of males,
reflecting the greater width of their pelves. At the knees, the distal
end of each femur articulates with the patella and tibia of the
corresponding leg. Weight is transferred from the knee joint to the
ankle joint by the tibia. The fibula does not articulate with the femur
and
does not bear or transfer weight, but it provides for muscle attachment and contributes to the formation of the ankle joint.
 |
|
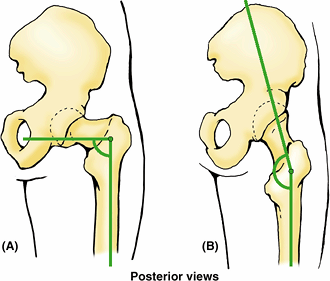
Figure 5.3. Pelvic Girdle and Related Joints, Demonstrating Transfer of Weight. A.
The weight of the upper body, transmitted centrally through the vertebral column, is divided and directed laterally by means of the bony arch formed by the sacrum and ilia. Thick portions of the ilia transfer the weight to the femurs. The pubic rami form “struts” or braces that help maintain the integrity of the arch. B. The arrangement of the lower limb bones of bipeds is compared to that of quadrupeds. The diagonal disposition of the femur recenters support directly inferior to the trunk (body mass) to make bipedal standing more efficient and to enable bipedal walking, in which the full weight is borne alternately by each limb. In quadrupeds, the trunk is suspended between essentially vertical limbs, requiring simultaneous support from each side. |
 |
|
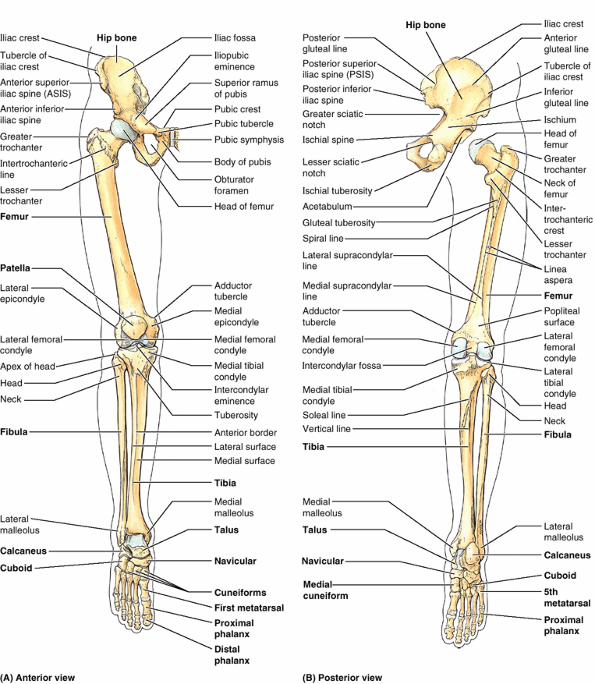
Figure 5.4. Bones of lower limb. A and B. Individual bones and bony formations are identified. The foot is in full plantarflexion. The hip joint is disarticulated (B) to demonstrate the acetabulum of the hip bone, which receives the head of the femur.
|
The talus is the keystone of a longitudinal arch formed by the tarsal
and metatarsal bones of each foot that distributes the weight evenly
between the heel and the forefoot when standing, creating a flexible
but stable platform to support the body.
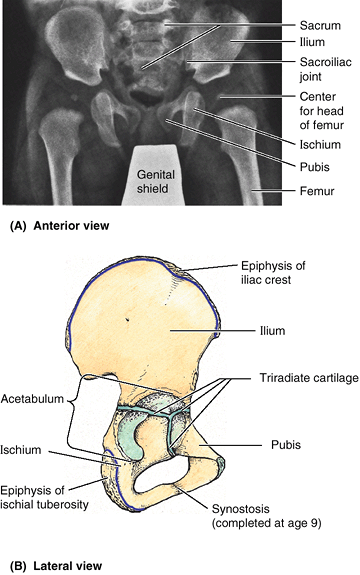
the end of the teenage years. Each of the three bones is formed from
its own primary center of ossification; five secondary centers of
ossification appear later. At birth, the three primary bones are joined
by hyaline cartilage; in children, they are incompletely ossified (Fig. 5.5). At puberty, the three bones are still separated by a Y-shaped triradiate cartilage centered in the acetabulum, although the two parts of the ischiopubic rami fuse by the 9th year (Fig. 5.5B).
The bones begin to fuse between 15 and 17 years of age; fusion is
complete between 20 and 25 years of age. Little or no trace of the
lines of fusion of the primary bones is visible in older adults (Fig. 5.6).
Although the bony components are rigidly fused, their names are still
used in adults to describe the three parts of the hip bone.
pelvis is primarily concerned with pelvic and perineal structures and
functions (Chapter 3) or their union with the vertebral column (Chapter 4),
it is described more thoroughly in those chapters. Aspects of the hip
bones concerned with lower limb structures and functions, mainly
involving their lateral aspects, are described in this chapter.
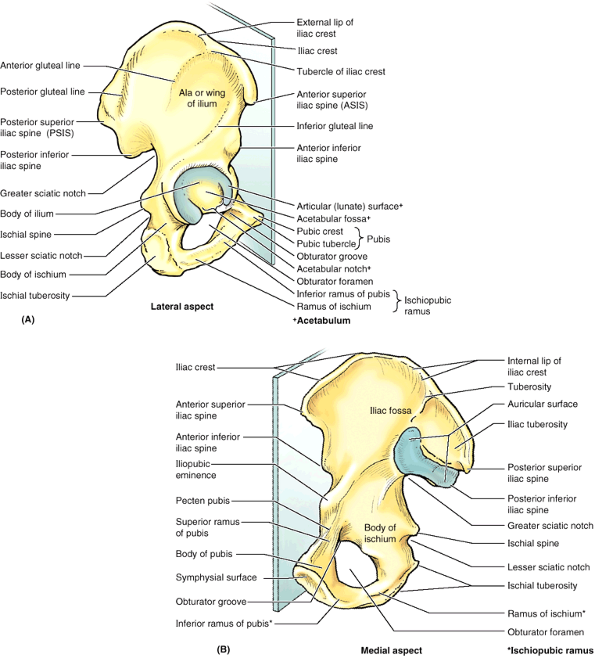
Beginning at the anterior superior iliac spine (ASIS), the long curved
and thickened superior border of the ala of the ilium, the iliac crest, extends posteriorly, terminating at the posterior superior iliac spine
(PSIS). The crest serves as a protective “bumper” and is an important
site of aponeurotic attachment for thin, sheet-like muscles and deep
fascia. A prominence on the external lip of the crest, the tubercle of the iliac crest (iliac tubercle), lies 5–6 cm posterior to the ASIS. The posterior inferior iliac spine marks the superior end of the greater sciatic notch.
 |
|
Figure 5.5. Parts of hip bones. A.
An anteroposterior radiograph of an infant’s hips shows the three parts of the incompletely ossified hip bones (ilium, ischium, and pubis). B. The right hip bone of a 13-year-old demonstrating the Y-shaped triradiate cartilage extending through the acetabulum, uniting the three primary parts of the bone, and the ossified epiphyses along the iliac crest and ischial tuberosity. These bony parts fuse to form the one-part mature hip bone of the adult between the 16th and 18th years. |
demarcate the proximal attachments of the three large gluteal muscles
(glutei). Medially, each ala has a large, smooth depression, the iliac fossa (Fig. 5.6B), that provides proximal attachment for the iliac muscle (L. iliacus).
The bone forming the superior part of this fossa may become thin and
translucent, especially in older women with osteoporosis. Posteriorly,
the medial aspect of the ilium has a rough, ear-shaped articular area
called the auricular surface (L. auricula, a little ear) and an even rougher iliac tuberosity
superior to it for synovial and syndesmotic articulation with the
reciprocal surfaces of the sacrum at the sacroiliac joint (see Chapter 4).
 |
|
Figure 5.6. Right hip bone of adult in anatomical position. In this position, the anterior superior iliac spine (ASIS) and the anterior aspect of the pubis lie in the same coronal plane. A. The large hip bone is constricted in the middle and expanded at its superior and inferior ends. B.
The symphysial surface of the pubis articulates with the corresponding surface of the contralateral hip bone. The auricular surface of the ilium articulates with a corresponding surface of the sacrum to form the sacroiliac joint. |
at the inferior margin of this notch provides ligamentous attachment.
This sharp demarcation separates the greater sciatic notch from a more
inferior, smaller, rounded, and smooth-surfaced indentation, the lesser sciatic notch.
The lesser sciatic notch serves as a trochlea or pulley for a muscle
that emerges from the bony pelvis here. The rough bony projection at
the junction of the inferior end of the body of the ischium and its
ramus is the large ischial tuberosity. The
body’s weight rests on this tuberosity when sitting, and it provides
the proximal, tendinous attachment of posterior thigh muscles.
anteromedial part of the hip bone, contributing the anterior part of
the acetabulum, and provides proximal attachment for muscles of the
medial thigh. The pubis is divided into a flattened body and two rami,
superior and inferior (Fig. 5.6). The rami are
strong yet relatively light skeletal “struts” (braces) that maintain
the arch composed of the sacrum and the two ilia, by which axial weight
is divided and transferred laterally to the limbs when standing and to
the ischial tuberosities when sitting (Fig. 5.3). Medially, the symphysial surface of the body of the pubis articulates with the corresponding surface of the body of the contralateral pubis by means of the pubic symphysis. The anterosuperior border of the united bodies and symphysis forms the pubic crest, which provides attachment for abdominal muscles. Small projections at the lateral ends of this crest, the pubic tubercles,
are important landmarks of the inguinal regions. The tubercles provide
attachment for the main part of the inguinal ligament and thereby
indirect muscle attachment. The posterior margin of the superior ramus of the pubis has a sharp raised edge, the pecten pubis, which forms part of the pelvic brim (see Chapter 3).
large oval or irregularly triangular aperture in the hip bone. It is
bounded by the pubis and ischium and their rami. Except for a small
passageway for the obturator nerve and vessels (the obturator canal), the obturator foramen is closed by the thin, strong obturator membrane (see Chapter 3).
The presence of the foramen minimizes bony mass (weight) while its
closure by the obturator membrane still provides extensive surface area
on both sides for fleshy muscle attachment.
cup-shaped cavity or socket on the lateral aspect of the hip bone that
articulates with the head of the femur to form the hip joint (Fig. 5.6A).
All three primary bones forming the hip bone contribute to the
formation of the acetabulum. The margin of the acetabulum is incomplete
inferiorly at the acetabular notch, which
makes the fossa resemble a cup with a piece of its lip missing. The
rough depression in the floor of the acetabulum extending superiorly
from the acetabular notch is the acetabular fossa. The acetabular notch and fossa also create a deficit in the smooth lunate surface of the acetabulum, which articulates with the head of the femur. The acetabulum is discussed further in relation to the hip joint.
ischium, and pubis), the hip bones are joined to the sacrum posteriorly
and to each other anteriorly (at the pubic symphysis) to form the
pelvic girdle. Each hip bone is specialized to receive half the weight
of the upper body when standing and all of it periodically during
walking. Thick parts of the bone transfer weight to the femur. Thin
parts of the bone provide a broad surface for attachment of powerful
muscles that move the femur. The pelvic girdle encircles and protects
pelvic viscera, particularly the reproductive organs.
-
ASIS and the anterosuperior aspect of the pubis lie in the same vertical plane.
-
Symphysial surface of the pubis is vertical, parallel to the median plane (Fig. 5.6).
-
Acetabulum faces inferolaterally, with the acetabular notch directed inferiorly.
-
Obturator foramen lies inferomedial to the acetabulum.
-
Internal aspect of the body of the pubis
faces almost directly superiorly (it essentially forms a floor on which
the urinary bladder rests). -
The superior pelvic aperture (pelvic
inlet) is more vertical than horizontal; in the anteroposterior (AP)
view, the tip of the coccyx appears near its center (Fig. 5.3).
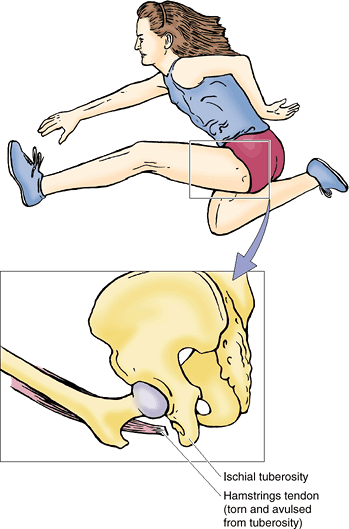
hip bone may occur during sports that require sudden acceleration or
deceleration forces, such as sprinting or kicking in football, soccer,
hurdle jumping, basketball, and martial arts (Fig. B5.1). A small part of bone with a piece of a tendon or ligament attached is “avulsed” (torn away). These fractures occur at apophyses
(bony projections that lack secondary ossification centers). Avulsion
fractures occur where muscles are attached: anterior superior and
inferior iliac spines, ischial tuberosities, and ischiopubic rami.
 |
|
Figure B5.1
|
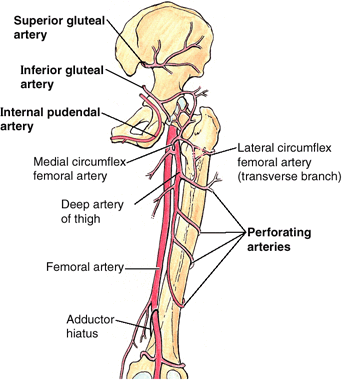
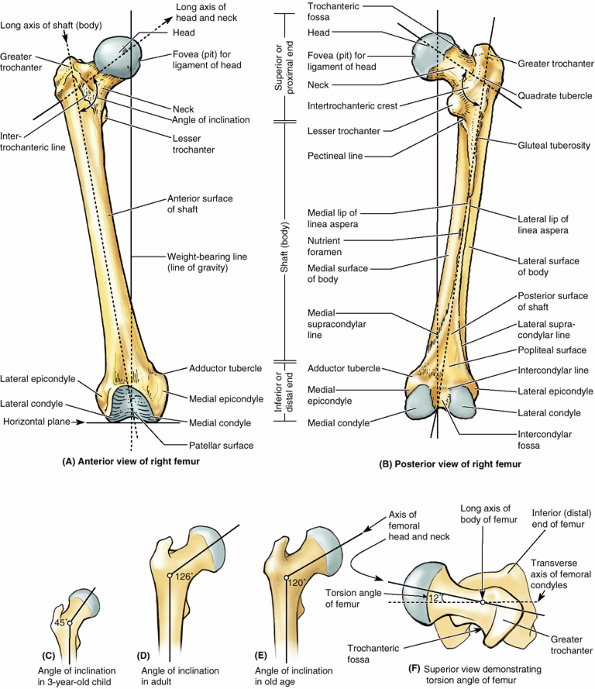
heaviest bone in the body. It transmits body weight from the hip bone
to the tibia when a person is standing (Fig. 5.4). Its length is approximately a quarter of the person’s height. The femur consists of a shaft (body) and two ends, superior or proximal and inferior or distal (Fig. 5.7). The superior (proximal) end of the femur consists of a head, neck, and two trochanters (greater and lesser). The round head of the femur makes up two thirds of a sphere that is covered with articular cartilage, except for a medially placed depression or pit, the fovea for the ligament of the head. In early life, the ligament gives passage to an artery supplying the epiphysis of the head. The neck of the femur
is trapezoidal, with its narrow end supporting the head and its broader
base being continuous with the shaft. Its average diameter is three
quarters that of the femoral head.
axis of the head and neck projects superomedially at an angle to that
of the obliquely oriented shaft (Fig. 5.7A & B). This obtuse angle of inclination
is greatest (most nearly straight) at birth and gradually diminishes
(becomes more acute) until the adult angle is reached (115–140°,
averaging 126°) (Fig. 5.7C–E).
The angle is less in females because of the increased width between the
acetabula (a consequence of a wider lesser pelvis) and the greater
obliquity of the shaft. The angle of inclination allows greater
mobility of the femur at the hip joint because it places the head and
neck more perpendicular to the acetabulum in the neutral position. The
abductors and rotators of the thigh attach mainly to the apex of the
angle (the greater trochanter) so they are pulling on a lever (the short limb of the L)
that is more laterally than vertically directed. This provides
increased leverage for the abductors and rotators of the thigh and
allows the considerable mass of the abductors of the thigh to be placed
superior to the femur (in the gluteal region) instead of lateral to it,
freeing the lateral aspect of the femoral shaft to provide increased
area for fleshy attachment of the extensors of the knee. The angle also
allows the obliquity of the femur within the thigh, which permits the
knees to be adjacent and inferior to the trunk, as explained
previously. All of this is advantageous for bipedal walking; however,
it imposes considerable strain on the neck of the femur. Consequently,
fractures of the femoral neck can occur in older people as a result of
a slight stumble if the neck has been weakened by osteoporosis.
occurred during development does not conclude with the long axis of the
superior end of the femur (head and neck) parallel to the transverse
axis of the inferior end (femoral condyles). When the femur is viewed
superiorly (so that one is looking along the long axis of the shaft),
it is apparent that the two axes lie at an angle (the torsion angle, or angle of declination),
the mean of which is 7° in males and 12° in females. The torsion angle,
combined with the angle of inclination, allows rotatory movements of
the femoral head within the obliquely placed acetabulum to convert into
flexion and
extension, abduction and adduction, and rotational movements of the thigh.
 |
|
Figure 5.7. Right femur. A and B.
The bony features of an adult femur are shown. Functionally and morphologically, the bone consists of highly modified superior and inferior ends and an intervening cylindrical shaft. The nutrient foramen (B) is demonstrated entering the femoral shaft near the linea aspera. A–E. The femur is “bent” so that the long axis of the head and neck lies at an angle (angle of inclination) to that of the shaft. When the massive femoral condyles rest on a horizontal surface, the femur assumes its oblique anatomical position in which the center of the round femoral head lies directly superior to the intercondylar fossa. C–E. The angle of inclination decreases (becomes more acute) with age, resulting in greater stress at a time when bone mass is reduced. When the femur is viewed along the long axis of the femoral shaft, so that the proximal end is superimposed over the distal end (F), it can be seen that the axis of the head and neck of the femur forms a 12° angle with the transverse axis of the femoral condyles (angle of torsion). |
(G. a runner) extends medially from the posteromedial part of the
junction of the neck and shaft to give tendinous attachment to the
primary flexor of the thigh (the iliopsoas). The greater trochanter
is a large, laterally placed bony mass that projects superiorly and
posteriorly where the neck joins the femoral shaft, providing
attachment and leverage for abductors and rotators of the thigh. The
site where the neck and shaft join is indicated by the intertrochanteric line,
a roughened ridge formed by the attachment of a powerful ligament
(iliofemoral ligament), that runs from the greater trochanter and winds
around the lesser trochanter to continue posteriorly and inferiorly as
a less distinct ridge, the spiral line. A similar but smoother and more prominent ridge, the intertrochanteric crest, joins the trochanters posteriorly. The rounded elevation on the crest is the quadrate tubercle. In anterior and posterior views (Fig. 5.7A & B), the greater trochanter is in line with the femoral shaft. In posterior and superior views (Fig. 5.7B & F), it overhangs a deep depression medially, the trochanteric fossa.
slightly bowed (convex) anteriorly. This convexity may increase
markedly, proceeding laterally as well as anteriorly, if the shaft is
weakened by a loss of calcium, as occurs in rickets. Most of the shaft
is smoothly rounded, providing fleshy origin to extensors of the knee,
except posteriorly where a broad, rough line, the linea aspera,
provides aponeurotic attachment for adductors of the thigh. This
vertical ridge is especially prominent in the middle third of the
femoral shaft, where it has medial and lateral lips (margins). Superiorly, the lateral lip blends with the broad, rough gluteal tuberosity, and the medial lip continues as a narrow, rough spiral line. The spiral line
extends toward the lesser trochanter but then passes to the anterior
surface of the femur, where it is continuous with the intertrochanteric
line. A prominent intermediate ridge, the pectineal line,
extends from the central part of the linea aspera to the base of the
lesser trochanter. Inferiorly, the linea aspera divides into medial and
lateral supracondylar lines, which lead to the spirally curved medial and lateral condyles (Fig. 5.7B).
make up nearly the entire inferior (distal) end of the femur. The two
condyles are on the same horizontal level when the bone is in its
anatomical position, so that if an isolated femur is placed upright
with both condyles contacting the floor or tabletop, the femoral shaft
will assume the same oblique position it occupies in the living body
(about 9° from vertical in males and slightly greater in females). The
femoral condyles articulate with menisci (crescentic plates of
cartilage) and tibial condyles to form the knee joint (Fig. 5.4).
The menisci and tibial condyles glide as a unit across the inferior and
posterior aspects of the femoral condyles during flexion and extension.
The convexity of the articular surface of the condyles increases as it
descends the anterior surface, covering the inferior end, and then
ascends posteriorly. The condyles are separated posteriorly and
inferiorly by an intercondylar fossa (intercondylar notch) but merge anteriorly, forming a shallow longitudinal depression, the patellar surface (Fig. 5.7), which articulates with the patella. The lateral surface of the lateral condyle has a central projection called the lateral epicondyle. The medial surface of the medial condyle has a larger and more prominent medial epicondyle, superior to which another elevation, the adductor tubercle,
forms in relation to a tendon attachment. The epicondyles provide
proximal attachment for the collateral ligaments of the knee joint.
femur, has developed a bend (angle of inclination) and has twisted
(medial rotation and torsion so that the knee and all joints inferior
to it flex posteriorly) to accommodate our erect posture and to enable
bipedal walking and running. The angle of inclination and attachment of
the abductors and rotators to the greater trochanter allow increased
leverage, superior placement of the abductors, and oblique orientation
of the femur in the thigh. Combined with the torsion angle, oblique
rotatory movements at the hip joint are converted into movements of
flexion–extension and abduction–adduction (in the sagittal and coronal
planes, respectively) as well as of rotation.
varies with age, sex, and development of the femur (e.g., a congenital
defect in the ossification of the femoral neck). It may also change
with any pathological process that weakens the neck of the femur (e.g.,
rickets). When the angle of inclination is decreased, the condition is coxa vara (Fig. B5.2A); when it is increased, it is coxa valga (Fig. B5.2B). Coxa vara causes a mild shortening of the lower limb and limits passive abduction of the hip.
the epiphysis of the femoral head may slip away from the femoral neck
because of a weakened epiphysial plate. This injury may be caused by
acute trauma or repetitive microtraumas that place increased shearing
stress on the epiphysis, especially with abduction and lateral rotation
of the thigh. The epiphysis often dislocates (slips) slowly and results
in a progressive coxa vara. The common
initial symptom of the injury is hip discomfort that may be referred to
the knee. Radiographic examination of the superior end of the femur is
usually required to confirm a diagnosis of a dislocated epiphysis of
the head of the femur.
 |
|
Figure B5.2.
|
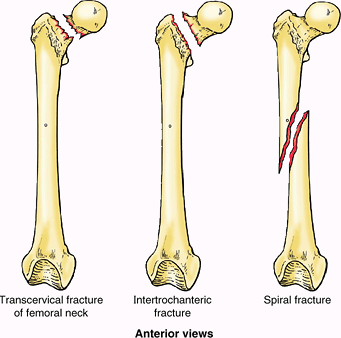
commonly fractured. The type of fracture sustained is frequently age-
and even sex-related. The neck of the femur is most frequently
fractured because it is the narrowest and weakest part of the bone and
it lies at a marked angle to the line of weight bearing (pull of
gravity). It becomes increasingly vulnerable with age, especially in
females, secondary to osteoporosis.
Fractures of the proximal femur occur at several locations; two
examples are trans-cervical (middle of neck) and intertrochanteric (Fig. B5.3).
These fractures usually occur as a result of indirect trauma (stumbling
or stepping down hard, as off a curb or step). Because of the angle of
inclination, these fractures are inherently unstable and impaction
(overriding of fragments resulting in foreshortening of the limb)
occurs. Muscle spasm also contributes to the shortening of the limb.
Intracapsular fractures (occurring within the hip joint capsule), are
complicated by degeneration of the femoral head owing to vascular
trauma (see clinical correlation [blue] boxes “Fractures of the Femoral Neck (‘Hip Fractures’)” and “Surgical Hip Replacement,” both later in this chapter).
usually result from direct trauma (direct blows sustained by the bone
resulting from falls or being hit) and are most common during the more
active years. They frequently occur during motor vehicle accidents and
sports such as skiing and climbing. In some cases, a spiral fracture
of the femoral shaft occurs, resulting in foreshortening as the
fragments override, or the fracture may be comminuted (broken into
several pieces), with the fragments displaced in various directions as
a result of muscle pull and depending on the level of the fracture.
Union of this serious type of fracture may take up to a year.
separation of the condyles, resulting in misalignment of the articular
surfaces of the knee joint, or by hemorrhage from the large popliteal
artery that runs directly on the surface of the bone, which compromises
the blood supply to the leg (an occurrence that should always be
considered in knee fractures–dislocations).
 |
|
Figure B5.3
|
articulates with the condyles of the femur superiorly and the talus
inferiorly and in so doing transmits the body’s weight. The fibula
mainly functions as an attachment for muscles, but it is also important
for the stability of the ankle joint. The shafts (bodies) of the tibia
and fibula are connected by a dense interosseous membrane composed of
strong oblique fibers.
(shin bone) is the second largest bone in the body. It flares outward
at both ends to provide an increased area for articulation and weight
transfer. The superior
(proximal) end widens to form medial and lateral condyles that overhang the shaft medially, laterally, and posteriorly, forming a relatively flat superior articular surface, or tibial plateau.
This plateau consists of two smooth articular surfaces (the medial one
slightly concave and the lateral one slightly convex) that articulate
with the large condyles of the femur. The articular surfaces are
separated by an intercondylar eminence formed by two intercondylar tubercles (medial and lateral) flanked by relatively rough anterior and posterior intercondylar areas. The tubercles fit into the intercondylar fossa between the femoral condyles (Fig. 5.7B).
The intercondylar tubercles and areas provide attachment for the
menisci and principal ligaments of the knee, which hold the femur and
tibia together, maintaining contact between their articular surfaces.
The anterolateral aspect of the lateral tibial condyle bears an anterolateral tibial tubercle (Gerdy tubercle) inferior to the articular surface (Fig. 5.8),
which provides the distal attachment for a dense thickening of the
fascia covering the lateral thigh, adding stability to the knee joint.
The lateral condyle also bears a fibular articular facet posterolaterally on its inferior aspect for the head of the fibula.
 |
|
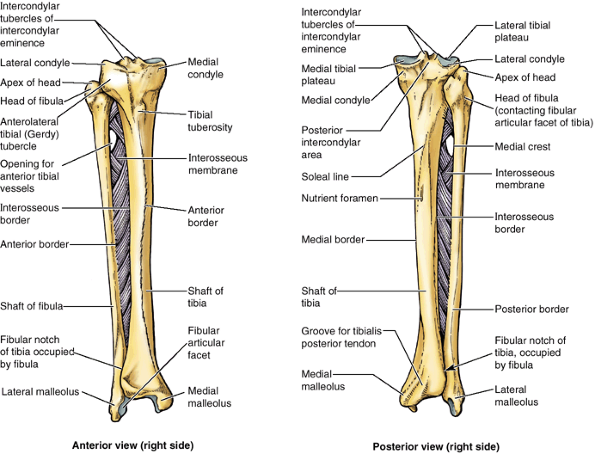
Figure 5.8. Right tibia and fibula.
Tibiofibular syndesmoses, including the dense interosseous membrane, tightly connect the tibia and fibula. The interosseous membrane provides additional surface area for muscular attachment. The anterior tibial vessels traverse the opening in the membrane to enter the anterior compartment of the leg (Fig. 5.10). |
is truly vertical within the leg and somewhat triangular in cross
section, having three surfaces and borders: medial,
lateral/interosseous, and posterior. The anterior border
of the tibia is the most prominent border; it and the adjacent anterior
surface are subcutaneous throughout their lengths and are commonly
known as the “shin” or “shin bone”; their periosteal covering and
overlying skin is vulnerable to bruising. At the superior end of the
anterior border, a broad, oblong tibial tuberosity
provides distal attachment for the patellar ligament, which stretches
between the inferior margin of the patella and the tibial tuberosity.
The tibial shaft is thinnest at the junction of its middle and distal
thirds. The distal end of the tibia is smaller than the proximal end,
flaring only medially; the medial expansion extends inferior to the
rest of the shaft as the medial malleolus.
The inferior surface of the shaft and the lateral surface of the medial
malleolus articulate with the talus and are covered with articular
cartilage (Fig. 5.4). The interosseous border of the tibia is sharp where it gives attachment to the interosseous membrane that unites the two leg bones. Inferiorly, the sharp border is replaced by a groove, the fibular notch, that
accommodates and provides fibrous attachment to the distal end of the fibula.
which runs inferomedially to the medial border; it is formed in
relationship to the aponeurotic origin of the soleus muscle
approximately one third of the way down the shaft. Immediately distal
to the soleal line is an obliquely directed vascular groove, which
leads to a large nutrient foramen. From it, the nutrient canal runs inferiorly in the tibia before it opens into the medullary (marrow) cavity.
Unlike the comparable bones of the forearm (radius and ulna), which are
joined to enable mobility (pronation and supination), the leg is fixed
in a permanently pronated position that places the great toe medially
and directs the sole of the foot inferiorly, toward the ground. The
fibula has no function in weight bearing; it serves mainly for muscle
attachment, providing distal attachment (insertion) for one muscle and
proximal attachment (origin) for eight muscles. The fibers of the
tibiofibular syndesmosis are arranged to resist the resulting net
downward pull on the fibula.
and provide attachment for the ligaments that stabilize the joint. The
lateral malleolus is more prominent and posterior than the medial
malleolus and extends approximately 1 cm more distally. The proximal
end of the fibula consists of an enlarged head and smaller neck; the head has a pointed apex
formed in relationship to a tendinous attachment. The head articulates
with the fibular facet on the posterolateral, inferior aspect of the
lateral tibial condyle. The shaft of the
fibula is twisted and marked by the sites of muscular attachments. Like
the shaft of the tibia, it is triangular in cross section, having three
borders (anterior, interosseous, and posterior) and three surfaces
(medial, posterior, and lateral).
bearing the weight of all superior to it. The slender fibula does not
bear weight but, along with the interosseous membrane that binds it to
the tibia, is accessory to the tibia in providing an additional surface
area for fleshy muscle attachment and in forming the socket of the
ankle joint. Through evolution and development, the two bones have
become permanently pronated to accommodate bipedalism.
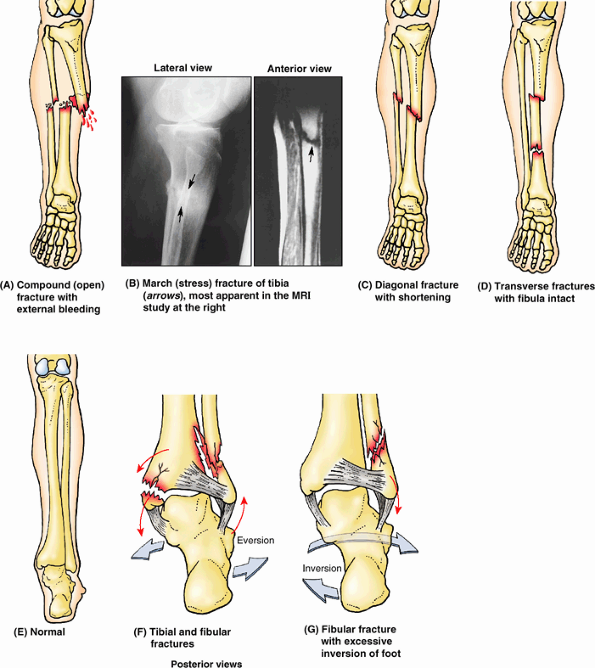
middle and inferior thirds, which is the most frequent site of
fracture. Unfortunately, this area of the bone also has the poorest
blood supply. Because its anterior surface is subcutaneous, the tibial
shaft is the most common site for a compound fracture (Fig. B5.4A).
Compound tibial fractures may also result from direct trauma (e.g., a
“bumper fracture” caused when a car bumper strikes the leg). Fracture
of the tibia through the nutrient canal predisposes the patient to
non-union of the bone fragments resulting from damage to the nutrient
artery.
are common in people who take long hikes before they are conditioned
for this activity. The strain may fracture the anterior cortex of the
tibia. Indirect violence applied to the tibial shaft when the bone
turns with the foot fixed during a fall may produce a fracture (e.g.,
when a person is tackled in football). In addition, severe torsion
during skiing may produce a diagonal fracture (Fig. B5.4C) of the tibial shaft at the junction of the middle and inferior thirds as well as a fracture of the fibula.
Diagonal fractures are often associated with limb shortening caused by
overriding of the fractured ends. Frequently during skiing, a fracture
results from a high-speed forward fall, which angles the leg over the
rigid ski boot, producing a “boot-top fracture” (Fig. B5.4D).
anterior tibia is accessible for obtaining pieces of bone for grafting
in children; it is also used as a site for intramedullary infusion in
dehydrated/shocked children.
the tibia appears shortly after birth and joins the shaft of the tibia
during adolescence (usually at 16–18 years of age). Tibial fractures in
children are more serious if they involve the epiphysial plates because
continued normal growth of the bone may be jeopardized. The tibial
tuberosity usually forms by inferior bone growth from the superior
epiphysial center at approximately 10 years of age, but a separate
center for the tibial tuberosity may appear at approximately 12 years
of age. Disruption of the epiphysial plate at the tibial tuberosity may
cause inflammation of the tuberosity and chronic recurring pain during
adolescence (Osgood-Schlatter disease), especially in young athletes.
When a person slips and the foot is forced into an excessively inverted
position, the ankle ligaments tear, forcibly tilting the talus against
the lateral malleolus and shearing it off (Fig. B5.4G). Fractures of the lateral and medial malleoli
are relatively common in soccer and basketball players. Fibular
fractures can be painful owing to disrupted muscle attachments; walking
is compromised because of the bone’s role in ankle stability.
 |
|
Figure B5.4
|
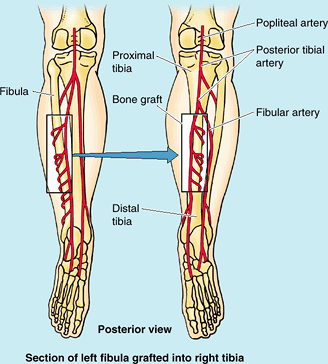
disease, the limb becomes useless. Replacement of the affected segment
by a bone transplant may avoid amputation. The fibula is a common
source of bone for grafting. Even after a segment of shaft has been
removed, walking, running, and jumping can be normal. Free vascularized
fibulas have been used to restore skeletal integrity to upper and lower
limbs in which congenital bone defects exist and to replace segments of
bone after trauma or excision of a malignant tumor (Fig. B5.5).
The remaining parts of the fibula usually do not regenerate because the
periosteum and nutrient artery are generally removed with the piece of
bone so that the graft will remain alive and grow when transplanted to
another site. Secured in its new site, the fibular segment restores the
blood supply of the bone to which it is now attached. Healing proceeds
as if a fracture had occurred at each of its ends.
fibula is important when performing free vascularized fibular
transfers. Because the nutrient foramen is located in the middle third
of the fibula in most cases, this segment of the bone is used for
transplanting when the graft must include a blood supply to the marrow
cavity as well as to the compact bone of the surface (via the
periosteum).
 |
|
Figure B5.5
|
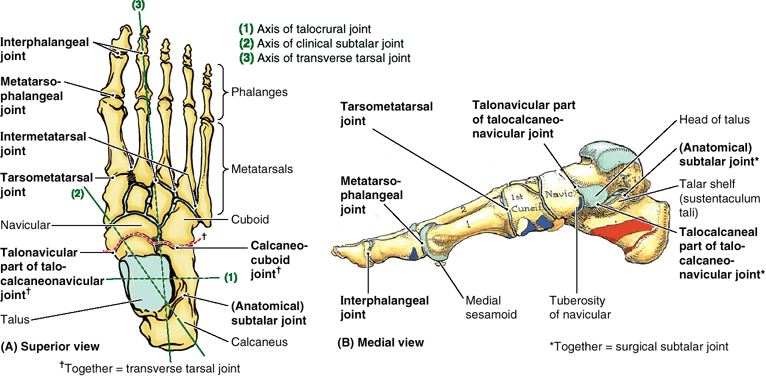
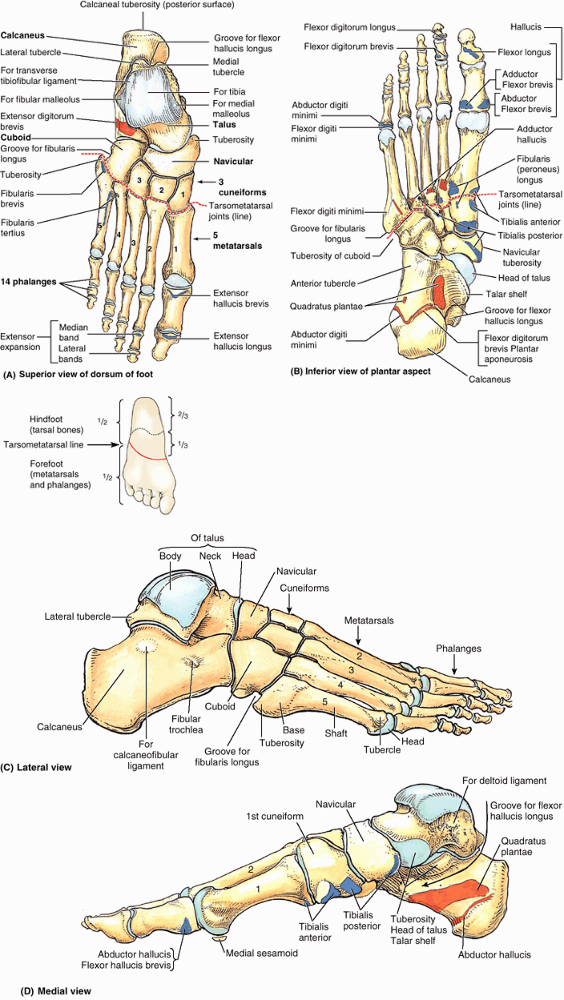
Although knowledge of the characteristics of individual bones is
necessary for an understanding of the structure of the foot, it is
important to study the skeleton of the foot as a whole and to identify
its principal bony landmarks in the living foot (see “Surface Anatomy of the Bones of the Foot,” later in this chapter).
and receives the weight of the body from the tibia. It transmits that
weight in turn, dividing it between the calcaneus, on which the talar body rests, and the forefoot, via an osseoligamentous “hammock’ that receives the rounded and anteromedially directed talar head. The hammock (spring ligament) is suspended across a gap between the talar shelf (a bracket-like lateral projection of the calcaneus) and the navicular bone, which lies anteriorly (Fig. 5.9B & D).
The talus is the only tarsal bone that has no muscular or tendinous
attachments. Most of its surface is covered with articular cartilage.
The talar body bears the trochlea superiorly and narrows into a posterior process that features a groove for the tendon of the flexor hallucis longus (Fig. 5.9D), flanked by a prominent lateral tubercle and a less prominent medial tubercle (Fig. 5.9A).
When standing, the calcaneus transmits the majority of the body’s
weight from the talus to the ground. The anterior two thirds of the
calcaneus’s superior surface articulates with the talus and its
anterior surface articulates with the cuboid. The lateral surface of
the calcaneus has an oblique ridge (Fig. 5.9C), the fibular trochlea,
that anchors a tendon pulley for the evertors of the foot (muscles that
move the sole of the foot away from the median plane). On the medial
side, the talar shelf (L. sustentaculum tali),
the shelf-like support of the talus, projects from the superior border
of the medial surface of the calcaneus and participates in supporting
the talar head (Fig. 5.9B & D). The posterior part of the calcaneus has a massive, weight-bearing prominence, the calcaneal tuberosity (L. tuber calcanei), which has medial, lateral, and anterior tubercles. Only the medial tubercle contacts the ground during standing.
ship) is a flattened, boat-shaped bone located between the talar head
posteriorly and the three cuneiforms anteriorly (Fig. 5.9). The medial surface of the navicular projects inferiorly to form the navicular tuberosity,
an important site for tendon attachment because the medial border of
the foot does not rest on the ground, as does the lateral border.
Instead, it forms a longitudinal arch of the foot,
which must be supported centrally. If this tuberosity is too prominent,
it may press against the medial part of the shoe and cause foot pain.
 |
|
Figure 5.9. Bones of right foot. A–D.
The seven bones of the tarsus make up the posterior half of the foot (hindfoot). The talus and calcaneus occupy the posterior two thirds of the hindfoot, and the cuboid; navicular; and medial, lateral, and intermediate cuneiforms occupy the anterior third. Only the talus articulates with the leg bones. The metatarsus connects the tarsus posteriorly with the phalanges anteriorly. Together, the metatarsus and phalanges make up the anterior half of the foot (forefoot). Sites of muscle attachment are shown in parts A, B, and D. Proximal attachments are shown in salmon color and distal attachments in blue. |
joining the midpoints of the medial and shorter lateral borders of the
foot; thus the metatarsals and phalanges are located in the anterior
half (forefoot) and the tarsals are in the posterior half (hindfoot) (Fig. 5.9A inset & B).
The base of each metatarsal is the larger, proximal end. The bases of
the metatarsals articulate with the cuneiform and cuboid bones, and the
heads articulate with the proximal phalanges. The bases of the 1st and
5th metatarsals have large tuberosities that provide for tendon
attachment; the tuberosity of the 5th metatarsal projects laterally over the cuboid. On the plantar surface of the head of the 1st metatarsal are prominent medial and lateral sesamoid bones (not shown); they are embedded in the tendons passing along the plantar surface (see “Bones of the Foot” in the following section on Surface Anatomy).
follows: the 1st digit (great toe) has 2 phalanges (proximal and
distal); the other four digits have 3 phalanges each: proximal, middle,
and distal (Fig. 5.9A & C). Each phalanx has a base (proximally), a shaft, and a head
(distally). The phalanges of the 1st digit are short, broad, and
strong. The middle and distal phalanges of the 5th digit may be fused
in elderly people.
allows weight to be distributed to a wide platform to maintain balance
when standing, enable conformation and adjustment to terrain
variations, and perform shock absorption. They also transfer weight
from the heel to the forefoot as required in walking and running.
and surgery because they can be used to evaluate normal development,
detect and assess fractures and dislocations, and locate structures
such as nerves and blood vessels.
The posterior two thirds of the crests are more difficult to palpate
because they are usually covered with fat. The iliac crest ends
anteriorly at the rounded anterior superior iliac spine,
which is easy to palpate by tracing the iliac crest anteroinferiorly.
The ASIS is often visible in thin individuals. In obese people these
spines are covered with fat and may be difficult to locate; however,
they are easier to palpate when the person is sitting and the muscles
attached to them are relaxed. The iliac tubercle,
5–6 cm posterior to the ASIS, marks the widest point of the iliac
crest. To palpate the iliac tubercle, place your thumb on the ASIS and
move your fingers posteriorly along the external lip of the iliac crest
(Fig. SA5.1B). The iliac tubercle lies at the level of the spinous process of L5 vertebra.
which may be difficult to palpate; however, its position is easy to
locate because it lies at the bottom of a skin dimple, approximately 4
cm lateral to the midline (see Chapter 4). The dimple exists because the skin and underlying fascia attach to the PSIS. The skin dimples
are useful landmarks when palpating the area of the sacroiliac joints
in search of edema (swelling) or local tenderness. These dimples also
indicate the termination of the iliac crests from which bone marrow and
pieces of bone for grafts can be obtained (e.g., to repair a fractured
tibia).
is covered with muscles and is not usually palpable. Only the superior
and inferior ends of the femur are palpable. The laterally placed greater trochanter
projects superior to the junction of the shaft with the femoral neck
and can be palpated on the lateral side of the thigh approximately 10
cm inferior to the iliac crest (Fig. SA5.1B).
The greater trochanter forms a prominence anterior to the hollow on the
lateral side of the buttock. The prominences of the greater trochanters
are normally responsible for the width of the adult pelvis. The
posterior edge of the greater trochanter is relatively uncovered and
most easily palpated when the limb is not weight bearing. The anterior
and lateral parts of the trochanter are not easy to palpate because
they are covered by fascia and muscle. Because it lies close to the
skin, the greater trochanter causes discomfort when you lie on your
side on a hard surface. In the anatomical position, a line joining the
tips of the greater trochanters normally passes through the pubic
tubercles and the center of the femoral heads. The lesser trochanter is indistinctly palpable superior to the lateral end of the gluteal fold.
|
Figure SA5.1
|
slides during flexion and extension of the leg at the knee joint. The
lateral and medial margins of the patellar surface can be palpated when
the leg is flexed. The adductor tubercle,
a small prominence of bone, may be felt at the superior part of the
medial femoral condyle by pushing your thumb inferiorly along the
medial side of the thigh until it encounters the tubercle.
oval elevation on the anterior surface of the tibia, is easily palpated
approximately 5 cm distal to the apex of the patella. The subcutaneous,
flat anteromedial surface of the tibia is also easy to palpate. The skin covering this surface is freely movable. The tibial condyles can be palpated anteriorly at the sides of the patellar ligament, especially when the knee is flexed. The head of the fibula
is prominent at the level of the superior part of the tibial tuberosity
because the knob-like head is subcutaneous at the posterolateral aspect
of the knee. The neck of the fibula can be
palpated just distal to the lateral side of the head. Doing so may
evoke a mildly unpleasant sensation because of the presence of a nerve
passing there.
Note that its inferior end is blunt and does not extend as far distally
as the lateral malleolus. The medial malleolus lies approximately 1.25
cm proximal to the level of the tip of the lateral malleolus. Only the
distal quarter of the shaft of the fibula is palpable. Feel your lateral malleolus, noting that it is subcutaneous and that its inferior end is sharp (Fig. SA5.1G & I).
Note that the tip of the lateral malleolus extends farther distally and
more posteriorly than does the tip of the medial malleolus.
anteromedial to the proximal part of the lateral malleolus when the
foot is inverted and anterior to the medial malleolus when the foot is
everted (Fig. SA5.1G).
Eversion of the foot makes the talar head more prominent as it moves
away from the navicular. The head occupies the space between the talar
shelf and the navicular tuberosity. If the talar head is difficult to
palpate, draw a line from the tip of the medial malleolus to the
navicular tuberosity; the talar head lies deep to the center of this
line. When the foot is plantarflexed, the superior surface of the body
of the talus can be palpated on the anterior aspect of the ankle,
anterior to the inferior end of the tibia.
is the only part of the medial aspect of the calcaneus that may be
palpated as a small prominence approximately a finger’s breadth distal
to the tip of the medial malleolus. The entire lateral surface of the
calcaneus is subcutaneous. The fibular trochlea,
a small lateral extension of the calcaneus, may be detectable as a
small tubercle on the lateral aspect of the calcaneus, anteroinferior
to the tip of the lateral malleolus.
surface of the foot is difficult because of the thick skin, fascia, and
pads of fat. The medial and lateral sesamoid bones inferior to the head of the 1st metatarsal can be felt to slide when the great toe is moved passively. The heads of the metatarsals can be palpated by placing the thumb on their plantar surfaces and the index finger on their dorsal surfaces. If callosities (calluses), thickenings of the keratin layer of the epidermis, are present, the metatarsal heads are difficult to palpate.
inferoanterior to the tip of the medial malleolus. The cuboid and
cuneiforms are difficult to identify individually by palpation.
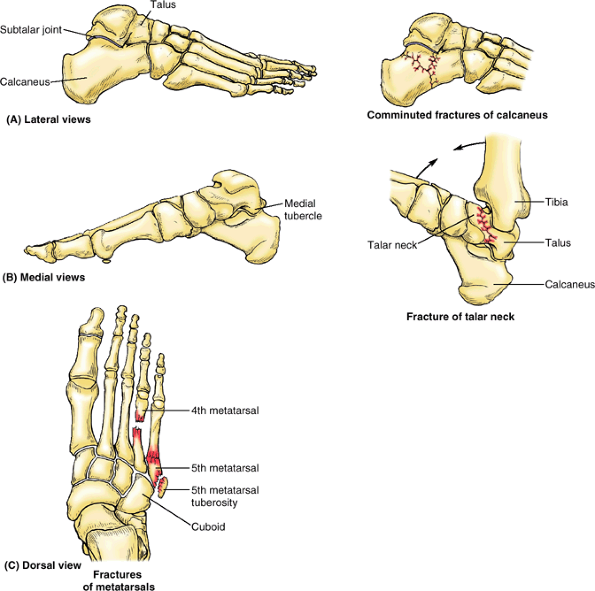
A calcaneal fracture is usually disabling because it disrupts the
subtalar (talocalcaneal) joint, where the talus articulates with the
calcaneus.
may occur during severe dorsiflexion of the ankle (e.g., when a person
is pressing extremely hard on the brake pedal of a vehicle during a
head-on collision). In some cases, the body of the talus dislocates
posteriorly.
the foot, for example or when it is run over by a heavy object such as
a metal wheel (Fig. B5.6C). Metatarsal fractures are also common in dancers, especially female ballet dancers who use the demi-pointe technique. The dancer’s fracture usually occurs when the dancer loses balance, putting the full body weight on the metatarsal and fracturing the bone. Fatigue fractures of the metatarsals may result from prolonged walking. These fractures, usually transverse, result from repeated stress on the metatarsals.
tuberosity of the 5th metatarsal may be avulsed by the tendon of the
fibularis brevis muscle. Avulsion fractures of the 5th metatarsal tuberosity (Fig. B5.6C)
are common in basketball and tennis players. Part of the tuberosity is
pulled off, producing pain and edema at the base of the 5th metatarsal.
 |
|
Figure B5.6
|
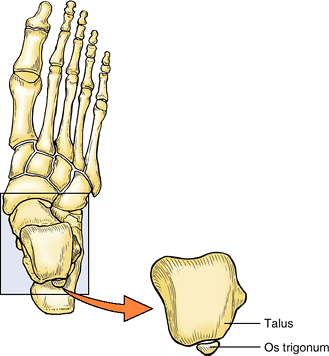
ossification center, which becomes the lateral tubercle of the talus,
occasionally fails to unite with the body of the talus. This failure
may be caused by applied stress (forceful plantarflexion) during the
early teens. Occasionally, a partly or even fully ossified center may
fracture and progress to non-union. Either event may result in a bone
(accessory ossicle) known as an os trigonum, which occurs in 14–25% of adults, more commonly bilaterally (Fig. B5.7).
It has an increased prevalence among soccer players and ballet dancers.
Patients with an os trigonum may be symptomatic or pain free.
Radionuclide bone scanning, which provides physiological as well as
anatomical evidence, is useful in distinguishing symptomatic and
asymptomatic ossicles. (Lawson, 1994)
 |
|
Figure B5.7
|
flexor hallucis longus bear the weight of the body, especially during
the latter part of the stance phase of walking (see “Posture and Gait,” in this chapter). The sesamoids develop before birth and begin to ossify during late childhood. Fracture of the sesamoids may result from a crushing injury (e.g., when a heavy object falls on the great toe).
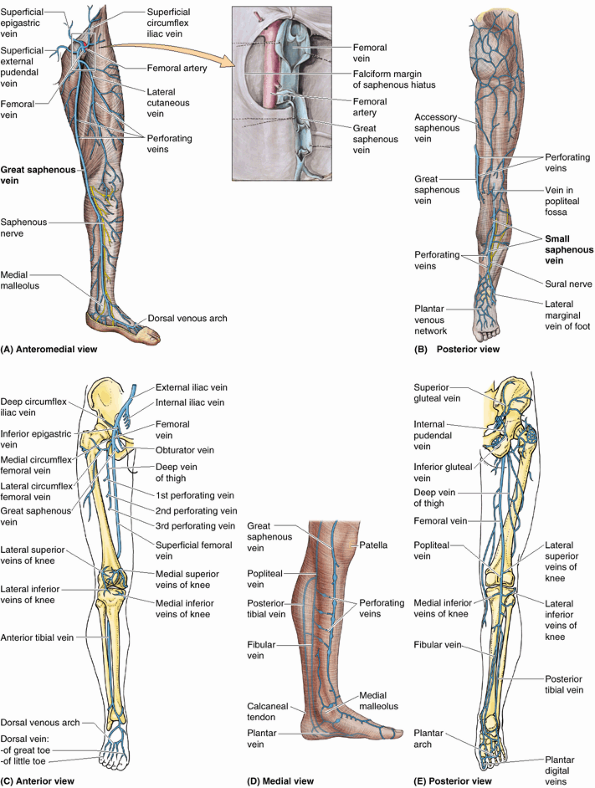
and consists of loose connective tissue that contains a variable amount
of fat, cutaneous nerves, superficial veins (great and small saphenous
veins and their tributaries), lymphatic vessels, and lymph nodes. The
subcutaneous tissue of the hip and thigh is continuous with that of the
inferior part of the anterolateral abdominal wall and buttock. At the
knee, the subcutaneous tissue loses its fat and blends with the deep
fascia, but fat is again present distal to the knee in the subcutaneous
tissue of the leg.
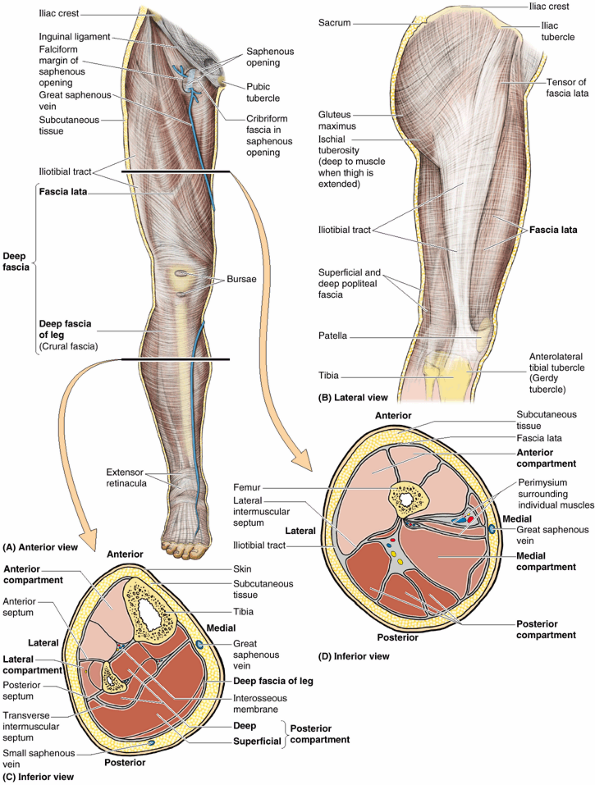
The deep fascia limits outward expansion of contracting muscles, making
muscular contraction more efficient in compressing veins to push blood
toward the heart. The deep fascia of the thigh is called fascia lata (L. lata, broad). It is continues inferior to the knee as the deep fascia of the leg.
-
The inguinal ligament, pubic arch, body
of pubis, and pubic tubercle superiorly; the membranous layer of
subcutaneous tissue (Scarpa fascia) of the inferior abdominal wall also
attaches to the fascia lata approximately a finger’s breadth inferior
to the inguinal ligament. -
The iliac crest laterally and posteriorly.
-
The sacrum, coccyx, sacrotuberous ligament, and ischial tuberosity posteriorly.
-
Exposed parts of bones around the knee and the deep fascia of the leg distally.
large thigh muscles, especially laterally where it is thickened and
strengthened by additional reinforcing longitudinal fibers to form the iliotibial tract (Fig. 5.10B). This broad band of fibers is the conjoint aponeurosis of the tensor of fascia lata and gluteus maximus muscles. The iliotibial tract extends from the iliac tubercle to the anterolateral tibial tubercle.
compartments—anterior, medial, and posterior. The walls of these
compartments are formed by the fascia lata and three fascial
intermuscular septa that arise from its deep aspect and attach to the
linea aspera of the femur (Fig. 5.10D). The lateral intermuscular septum
is especially strong; the other two septa are relatively weak. The
lateral intermuscular septum extends deeply from the iliotibial tract
to the lateral lip of the linea aspera and lateral supracondylar line
of the femur. This septum offers a welcome internervous plane to
surgeons needing wide exposure of the femur.
is a gap or hiatus in the fascia lata inferior to the medial part of
the inguinal ligament, approximately 4 cm inferolateral to the pubic
tubercle. The saphenous opening is usually approximately 3.75 cm in
length and 2.5 cm in breadth, and its long axis is vertical. Its medial
margin is smooth but its superior, lateral, and inferior margins form a
sharp crescentic edge, the falciform margin. This margin is joined at its medial margin by fibrofatty tissue, the cribriform fascia (L. cribrum,
a sieve). This sieve-like fascia is a localized membranous layer of
subcutaneous tissue that spreads over the saphenous opening, closing
it. This layer of spongy connective tissue is pierced by numerous
openings (thus its name) for the passage of efferent lymphatic vessels
from the superficial inguinal lymph nodes and by the great saphenous
vein and its tributaries. After passing through the saphenous opening
and cribriform fascia, the great saphenous
vein enters the femoral vein (Figs. 5.10A and 5.11A). The lymphatic vessels enter the deep inguinal lymph nodes.
 |
|
Figure 5.10. Fascia, intermuscular septa, and fascial compartments of lower limb. A.
The anterior skin and subcutaneous tissue have been removed to reveal the deep fascia of the thigh (fascia lata) and leg (crural fascia). B. The fascia lata is reinforced laterally with longitudinal fibers to form the iliotibial tract, which also serves as an aponeurosis for the gluteus maximus and tensor of fascia lata muscles. C and D. The fascial compartments of the thigh and leg, containing muscles sharing common functions and innervation, are demonstrated in transverse sections. |
leg), attaches to the anterior and medial borders of the tibia, where
it is continuous with its periosteum. The deep fascia of the leg is
thick in the proximal part of the anterior aspect of the leg, where it
forms part of the proximal attachments of the underlying muscles.
Although thinner distally, the deep fascia of the leg forms thickened
bands both superior and anterior to the ankle joint, the extensor retinacula (Fig. 5.10A). Anterior and posterior intermuscular septa pass from the deep surface of the lateral deep fascia of the leg and attach to the corresponding margins of the fibula. The interosseous membrane
and the intermuscular septa divide the leg into three compartments:
anterior (dorsiflexor), lateral (fibular), and posterior
(plantarflexor) (Fig. 5.10C). The muscles in the posterior compartment are subdivided into superficial and deep parts by the transverse intermuscular septum.
deep fascia. The former insulates, stores fat, and provides passage for
cutaneous nerves and superficial vessels (lymphatics and veins). The
deep fascia of the thigh (fascia lata) and leg (crural fascia) (1)
surround the thigh and leg, respectively, limiting outward bulging of
muscles and facilitating venous return in deep veins; (2) separate
muscles with similar functions and innervation into compartments, and
(3) surround individual muscles, allowing them to act independently.
Modifications of the deep fascia include openings that allow the
passage of neurovascular structures (e.g., the saphenous opening) and
thickenings that retain tendons close to the joints they act on
(retinacula).
superficial veins are in the subcutaneous tissue, and the deep veins
are deep to (beneath) the deep fascia and accompany all major arteries.
Superficial and deep veins have valves, which are more numerous in deep
veins.
-
Ascends anterior to the medial malleolus.
-
Passes posterior to the medial condyle of the femur (about a hand’s breadth posterior to the medial border of the patella) (Fig. 5.12 inset).
-
Anastomoses freely with the small saphenous vein.
-
Traverses the saphenous opening in the fascia lata.
-
Empties into the femoral vein.
10–12 valves, which are more numerous in the leg than in the thigh.
These valves are usually located just inferior to the perforating veins
(Fig. 5.11A). The perforating veins also have valves. Venous valves are cusps (flaps) of endothelium with cup-like valvular sinuses
that fill from above. When they are full, the valve cusps occlude the
lumen of the vein, thereby preventing reflux of blood distally, making
flow unidirectional. The valvular mechanism also breaks the column of
blood in the saphenous vein into shorter segments, reducing back
pressure. Both effects make it easier for the musculovenous pump to
overcome the force of gravity to return the blood to the heart.
vein receives numerous tributaries and communicates in several
locations with the small saphenous vein. Tributaries from the medial
and posterior aspects of the thigh frequently unite to form an accessory saphenous vein (Fig. 5.11B).
When present, this vein becomes the main communication between the
great and the small saphenous veins. Also, fairly large vessels, the lateral and anterior cutaneous veins,
arise from networks of veins in the inferior part of the thigh and
enter the great saphenous vein superiorly, just before it enters the
femoral vein. Near its termination, the great saphenous vein also
receives the superficial circumflex iliac, superficial epigastric, and
external pudendal veins (Fig. 5.11A).
-
Ascends posterior to the lateral malleolus as a continuation of the lateral marginal vein.
-
Passes along the lateral border of the calcaneal tendon.
-
Inclines to the midline of the fibula and penetrates the deep fascia.
-
Ascends between the heads of the gastrocnemius muscle.
-
Empties into the popliteal vein in the popliteal fossa.
veins, their diameters remain remarkably uniform as they ascend the
limb. This is possible because the blood received by the saphenous
veins is continuously shunted from these superficial veins in the
subcutaneous tissue to the deep veins by means of many perforating
veins.
penetrate the deep fascia close to their origin from the superficial
veins and contain valves that allow blood to flow only from the
superficial veins to the deep veins. The perforating veins pass through
the deep fascia at an oblique angle so that when muscles contract and
the pressure
increases
inside the deep fascia, the perforating veins are compressed.
Compression of the perforating veins also prevents blood from flowing
from the deep to the superficial veins. This pattern of venous blood
flow—from superficial to deep—is important for proper venous return
from the lower limb because it enables muscular contractions to propel
blood toward the heart against the pull of gravity (musculovenous pump; see the Introduction).
 |
|
Figure 5.11. Veins of lower limb. The veins are subdivided into superficial (A and B) and deep (C and E)
groups. The superficial veins, usually unaccompanied, course within the subcutaneous tissue; the deep veins are internal to the deep fascia and usually accompany arteries. A, inset. The proximal ends of the femoral and great saphenous veins are opened and spread apart to show the valves. Although depicted as single veins in parts C and E, the deep veins usually occur as duplicate or multiple accompanying veins. D. Multiple perforating veins pierce the deep fascia to shunt blood from the superficial veins (e.g., the great saphenous vein) to the deep veins (e.g., the posterior tibial and fibular veins). |
 |
|
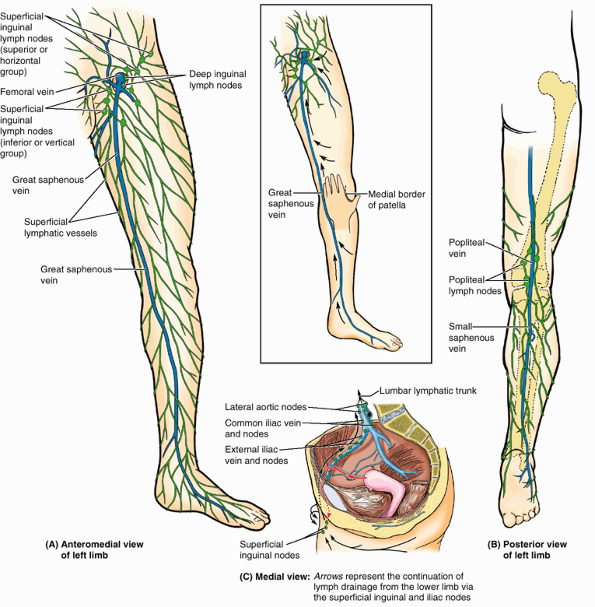
Figure 5.12. Superficial veins and lymphatics of lower limb. A.
The great saphenous vein ascends the medial aspect of the limb, passing anterior to the medial malleolus and approximately a hand’s breadth posterior to the patella (knee cap) (inset). The superficial lymphatic vessels from the medial foot, anteromedial leg, and thigh converge toward and accompany the great saphenous vein, draining into the inferior (vertical) group of superficial inguinal lymph nodes. B. Superficial lymphatic vessels of the lateral foot and posterolateral leg accompany the lesser saphenous vein and drain initially into the popliteal lymph nodes, which lie deep to the popliteal fascia. The efferent vessels from these nodes join other deep lymphatics, which accompany the femoral vessels to drain into the deep inguinal lymph nodes. C. Lymph from the superficial and deep inguinal lymph nodes traverses the external and common iliac nodes before entering the lateral aortic lymph nodes and the lumbar lymphatic trunk. |
and their branches. Instead of occurring as a single vein in the limbs
(although they are frequently illustrated as one and are often referred
to as a single vein), the deep veins usually occur as paired,
frequently interconnecting veins that flank the artery they accompany (Fig. 5.11C & E).
They are contained within the vascular sheath with the artery, whose
pulsations also help compress and move blood in the veins.
drains primarily via the superficial saphenous veins, perforating veins
penetrate the deep fascia, forming and continually supplying an
anterior tibial vein in the anterior leg. Medial and lateral plantar veins from the plantar aspect of the foot form the posterior tibial and fibular veins posterior to the medial and lateral malleoli (Fig. 5.11C–E). All three deep veins from the leg flow into the popliteal vein posterior to the knee, which becomes the femoral vein
in the thigh. Veins accompanying the perforating arteries of the deep
artery of the thigh drain blood from the thigh muscles and terminate in
the deep vein of the thigh (L. vena profunda femoris),
which joins the terminal portion of the femoral vein. The femoral vein
passes deep to the inguinal ligament to become the external iliac vein
of the trunk.
when a person stands quietly. During exercise, blood received from the
superficial veins by the deep veins is propelled by muscular
contraction to the femoral and then the external iliac veins. Flow in
the reverse direction—away from the heart or from the deep to the
superficial veins—is prevented if the venous valves are competent
(capable of performing their function). The deep veins are more
variable and anastomose much more frequently than the arteries they
accompany. Both superficial and deep veins can be ligated with impunity
if necessary.
the subcutaneous tissue) and deep (internal to the deep fascia) veins.
The superficial great and lesser saphenous veins mainly drain the
integument or skin and, via many perforating veins, continuously
shunting blood to the deep veins accompanying the arteries. Deep veins
are subject to muscle compression (musculovenous pump) to aid venous
return. All lower limb veins have valves to overcome the effects of
gravity.
Varicose veins form when the valves that usually prevent blood flow
from the deep veins through the perforating veins to the superficial
veins are incompetent. When the valves within the great saphenous vein
itself are incompetent, the pull of gravity on the uninterrupted column
of blood results in a higher intraluminal pressure, which also
exacerbates varicosities. As a result, the superficial veins become
tortuous and dilated.
 |
|
Figure B5.8
|
-
Incompetent, loose fascia that fails to resist muscle expansion, diminishing the effectiveness of the musculovenous pump.
-
External pressure on the veins from bedding during a prolonged hospital stay or from a tight cast or bandage.
-
Muscular inactivity (e.g., during an overseas flight).
arterial bypasses because (1) it is readily accessible, (2) sufficient
distance occurs between the tributaries and the perforating veins so
that usable lengths can be harvested, and (3) its wall contains a
higher percentage of muscular and elastic fibers than do other
superficial veins. Saphenous vein grafts are used to bypass
obstructions in blood vessels (e.g., in an intracoronary thrombus; see Chapter 1).
When part of the great saphenous vein is removed for a bypass, the vein
is reversed so that the valves do not obstruct blood flow in the graft.
Because there are so many other leg veins, removal of the great
saphenous vein rarely produces a significant problem in the lower limb
or seriously affects circulation, provided the deep veins are intact.
In fact, removal of this vein may facilitate the superficial to deep
drainage pattern to take advantage of the musculovenous pump.
or in patients in shock whose veins are collapsed, the great saphenous
vein can always be located by making a skin incision anterior to the
medial malleolus (Fig. 5.11A). This procedure, called a saphenous cutdown,
is used to insert a cannula for prolonged administration of blood,
plasma expanders, electrolytes, or drugs. The saphenous nerve
accompanies the great saphenous vein anterior to the medial malleolus.
Should this nerve be cut during a saphenous cutdown or caught by a
ligature during closure of a surgical wound, the patient may complain
of pain or numbness along the medial border of the foot.
These nodes lie under the deep fascia on the medial aspect of the
femoral vein. The lymphatic vessels accompanying the small saphenous
vein enter the popliteal lymph nodes, which surround the popliteal vein in the fat of the popliteal fossa (Fig. 5.12B). The deep lymphatic vessels
from the leg accompany deep veins and enter the popliteal lymph nodes.
Most lymph from these nodes ascends through deep lymphatic vessels to
the deep inguinal lymph nodes. Lymph from the deep nodes passes to the
external and common iliac lymph nodes and is then received by the lumbar lymphatic trunks (Fig. 5.12C).
that follow the superficial veins to the superficial inguinal nodes.
Some lymphatics follow deep veins to deep inguinal nodes. Lymph
drainage from the lower limb then passes deep to the external and
common iliac nodes of the trunk.
caused by pathogenic microorganisms or their toxins in the blood or
other tissues, may produce slight enlargement of the superficial
inguinal lymph nodes (lymphadenopathy) in
otherwise healthy people. Because these enlarged nodes are located in
the subcutaneous tissue, they are easy to palpate in healthy people.
Those who are unaware of this may be concerned when they feel these
nodes because they assume they have a serious genital disease, for
example. When inguinal lymph nodes are enlarged, their entire field of
drainage—the trunk inferior to the umbilicus, including the perineum,
as well as the entire lower limb—should be examined to determine the
cause of their enlargement. In female patients, the possibility of
metastasis of cancer from the uterus should also be considered because
some lymphatic drainage from the uterine fundus may flow along
lymphatics accompanying the round ligament of the uterus through the
inguinal canal to reach the superficial inguinal lymph nodes (see Chapter 3)
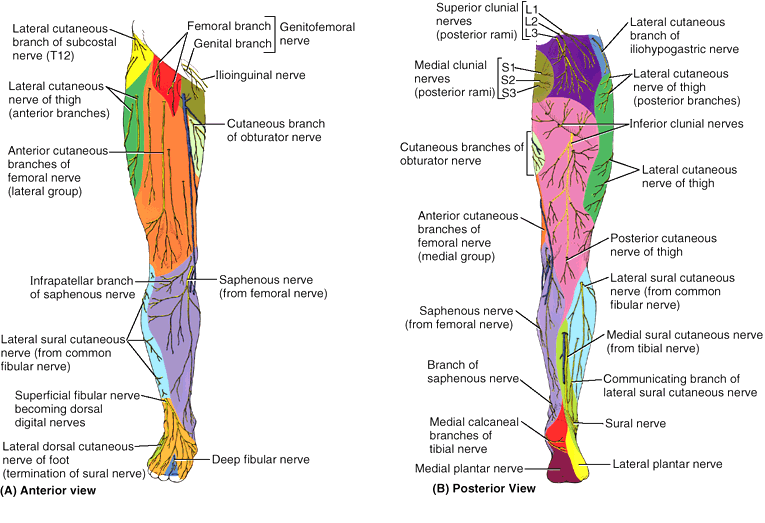
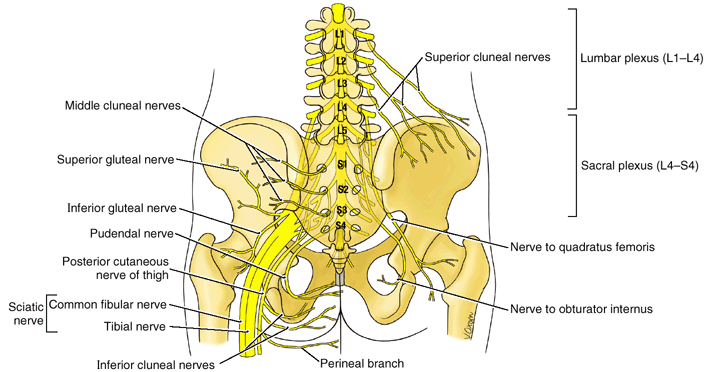
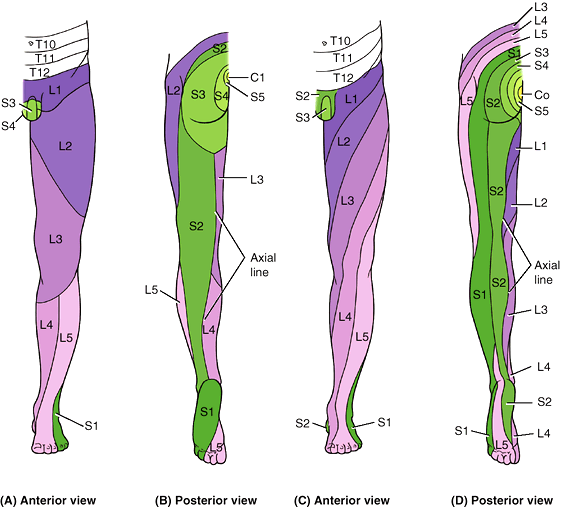
These nerves, except for some proximal unisegmental nerves arising from
the T12 or L1 spinal nerves, are branches of the lumbar and sacral
plexuses (see Chapters 3 and 4). The areas of skin supplied by the individual spinal nerves, including those contributing to the plexuses, are called dermatomes.
The dermatomal (segmental) pattern of skin innervation is retained
throughout life but is distorted by limb lengthening and the torsion of
the limb that occurs during development (Fig. 5.13). Although simplified into distinct zones in dermatome maps, adjacent dermatomes overlap, except at the axial line,
the line of junction of dermatomes supplied from discontinuous spinal
levels. Dermatomes L1–L5 extend as a series of bands from the posterior
midline of the trunk into the limbs, passing laterally and inferiorly
around the limb to its anterior and medial aspects, reflecting the
medial rotation that occurs developmentally. Dermatomes S1 and S2 pass
inferiorly down the posterior aspect of the limb, separating near the
ankle to pass to the lateral and medial margins of the foot. The
cutaneous nerves of the lower limb are illustrated and their origin
(including contributing spinal nerves), course, and distribution are
listed in Table 5.1.
 |
|
Figure 5.13. Dermatomes of lower limb.
The dermatomal or segmental pattern of distribution of sensory nerve fibers persists despite the merging of spinal nerves in plexus formation during development. Two different dermatome maps are commonly used. A and B. The dermatome pattern of the lower limb according to Foerster (1933) is preferred by many because of its correlation with clinical findings. C and D. The dermatome pattern of the lower limb according to Keegan and Garrett (1948) is preferred by others for its aesthetic uniformity and obvious correlation with development. Although depicted as distinct zones, adjacent dermatomes overlap considerably, except along the axial line. |
|
Table 5.1. Cutaneous Nerves of the Lower Limb
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
both the original segmental innervation of the skin via separate spinal
nerves in its dermatomal pattern and the result of plexus formation in
the distribution of multisegmental peripheral nerves. Most innervation
of the thigh is supplied by lateral and posterior cutaneous nerves of
the thigh and anterior cutaneous branches of the femoral nerve, the
names of which describe their distribution. The latter branches also
supply most of the medial aspect of the thigh. The innervation of the
leg and dorsum of the foot is supplied by saphenous (anteromedial leg),
sural (posterolateral leg), and fibular nerves (anterolateral leg and
dorsum of foot). The plantar aspect (sole) of the foot is supplied by
calcaneal branches of the tibial and sural nerves (heel region) and the
medial and lateral plantar nerves; the areas of distribution of the
latter are demarcated by a line bisecting the 4th toe.
blocked by injecting an anesthetic agent 4–6 cm posterior to the ASIS,
along the lateral aspect of the external lip of the iliac crest (see Chapter 2). This is where these nerves perforate the transverse abdominal (L. transversus abdominis)
muscle. The femoral nerve (L2–L4) can be blocked 2 cm inferior to the
inguinal ligament, approximately a finger’s breadth lateral to the
femoral artery. Paresthesia (tingling,
burning, tickling) radiates to the knee and over the medial side of the
leg if the saphenous nerve (terminal branch of femoral) is affected.
example, the iliohypogastric and ilioinguinal nerves may arise from a
common trunk of variable length, or the ilioinguinal nerve may join the
iliohypogastric nerve at the iliac crest. In the latter case, the
iliohypogastric nerve supplies the cutaneous branches for both nerves.
When the obturator nerve has a large cutaneous branch, the medial
anterior cutaneous branches of the femoral nerve are correspondingly
small.
area of skin represents more than one segment of the spinal cord.
Therefore, to interpret abnormalities of peripheral sensory function,
peripheral nerve distribution of the major cutaneous nerves must be
interpreted as anatomically different from dermatome distribution of
the spinal cord segments (Fig. 5.13).
Neighboring dermatomes may overlap. Pain sensation is tested by using a
sharp object and asking the patient if pain is felt. If there is no
sensation, the spinal cord segment(s) involved can be determined.
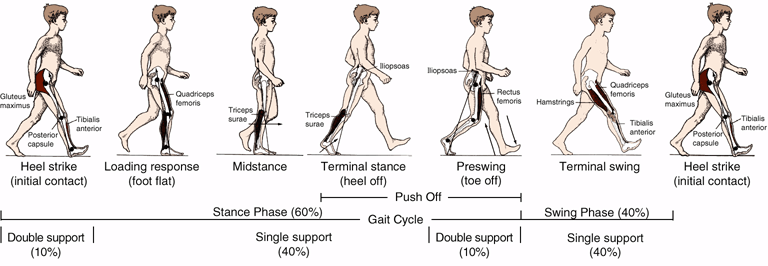
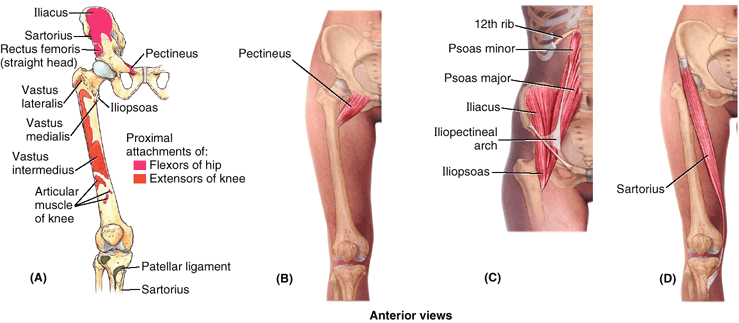
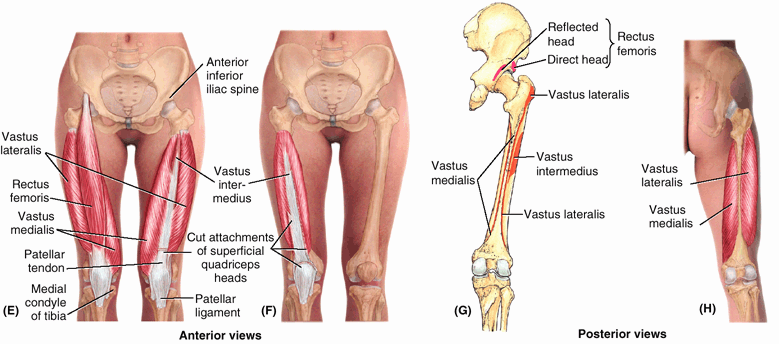
walking. Typically the actions of the lower limb muscles are described
as if the muscle were acting in isolation, which rarely occurs. In this
book, including the comments in the tables, the role of each muscle (or
of the functional group of which it is a member) is described in
typical activities, especially standing and walking. It is important to
be familiar with lower limb movements and concentric and eccentric
contractions of muscles, as described in the Introduction, and to have
a basic understanding of the processes of standing and walking.
apart and rotated laterally so the toes point outward, only a few of
the back and lower limb muscles are active (Fig. 5.14).
The mechanical arrangement of the joints and muscles are such that a
minimum of muscular activity is required to keep from falling. In the
stand-easy position, the hip and knee joints are extended and are in
their most stable positions (maximal contact of articular surfaces for
weight transfer, with supporting ligaments taut). The ankle joint is
less stable than the hip and knee joints, and the line of gravity falls
between the two limbs just anterior to the axis of rotation of the
ankle joints. Consequently, a tendency to fall forward (forward sway)
must be countered periodically by bilateral contraction of calf muscles
(plantarflexion). The spread and splay of the feet increase lateral
stability. However, when lateral sway
occurs, it is countered by the hip abductors (acting through the
iliotibial tract); fibular collateral ligament of the knee joint; and
the evertor muscles of one side acting with the thigh adductors, tibial
collateral ligament, and invertor muscles of the contralateral side.
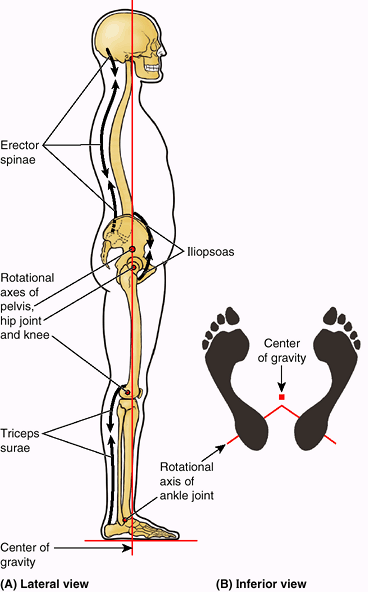 |
|
Figure 5.14. Relaxed standing. A.
The relationship of the line of gravity to the transverse rotational axes of the pelvis and lower limb in the relaxed standing (stand-easy) position is demonstrated. Only minor postural adjustments, mainly by the extensors of the back and the plantarflexors of ankle, are necessary to maintain this position because the ligaments of the hip and knee are being tightly stretched to provide passive support. B. A bipedal platform is formed by the feet during relaxed standing. The weight of the body is symmetrically distributed around the center of gravity, which falls in the posterior third of a median plane between the slightly parted and laterally rotated feet, anterior to the rotational axes of the ankle joints. |
function. The movements of the lower limbs during walking on a level
surface may be divided into alternating swing and stance phases (Table 5.2). The gait cycle consists of one cycle of swing and stance by one limb. The stance phase begins with heel strike, when the heel strikes the ground and begins to assume the body’s full weight (loading response), and ends with push off from the forefoot—a result of plantarflexion. The swing phase
begins after push off when the toes leave the ground and ends when the
heel strikes the ground. The swing phase occupies approximately 40% of
the walking cycle and the stance phase, 60%. The stance phase of
walking is longer than the swing phase because it begins and ends with
relatively short periods (each 10% of the cycle) of double support
(both feet are contacting the ground) as the weight is transferred from
one side to the other, with a more extended period of single support
(only one foot on the ground bearing all body weight) in between as the
contralateral limb swings forward. In running,
there is no period of double support; consequently, the time and
percentage of the gait cycle represented by the stance phase are
reduced.
advantage of gravity and momentum so that a minimum of physical
exertion is required. Most energy is used (1) in the eccentric
contraction of the dorsiflexors during the beginning (loading) phase of
stance as the heel is lowered to the ground following heel strike and
(2) especially at the end of stance as the plantarflexors
concentrically contract, pushing the forefoot (metatarsals and
phalanges) down to produce push off, thus providing most of the
propulsive force. During the last part of the stance phase (push off),
the toes flex to grip the ground and augment the push off initiated
from the ball of the foot (sole underlying the heads of the medial two
metatarsals). The long flexors and intrinsic muscles of the foot
stabilize the forefoot and toes so that the effect of plantarflexion at
the ankle and flexion of the toes is maximized.
the limb accelerates faster than the forward movement of the body.
Initially, the knee flexes almost simultaneously, owing to momentum
(without expenditure of energy), followed by dorsiflexion (lifting the
forefoot up) at the ankle joint. The latter two movements have the
effect of shortening the free limb so that it will clear the ground as
it swings forward; by midswing, knee extension is added to the flexion
and momentum of the thigh to realize anterior swing fully. The
extensors of the hip and flexors of the knee contract eccentrically at
the end of swing to decelerate the forward movement, while extensors of
the knee (quadriceps) contract as necessary to extend the leg for the
desired length of stride and to position the foot (present the heel)
for heel strike. Contraction of the knee extensors is maintained
through heel strike into the loading phase to absorb shock and keep the
knee from buckling until it reaches full extension. Because the
unsupported side of the hip tends to drop during the swing phase (which
would negate the effect of limb shortening), abductor muscles on the
supported side contract strongly during the single support part of the
stance phase, pulling on the fixed femur to resist the tilting and keep
the pelvis level. These same muscles also rotate (advance) the
contralateral side of the pelvis forward, concurrent with the swing of
its free limb.
with each step. The extensors of the hip normally make only minor
contributions to level walking. Primarily, the hip is passively
extended by momentum during stance, except when accelerating or walking
fast, and becomes increasingly active with increase in slope
(steepness) during walking uphill or up stairs. Concentric hip flexion
and knee extension are used during the swing phase of level walking and
so are not weight-bearing actions; however, they are effected by body
weight when their eccentric contraction is necessary for deceleration
or walking downhill or down stairs
locomotion. The invertors and evertors of the foot are principal
stabilizers of the foot during the stance phase. Their long tendons,
plus those of the flexors of the digits, also help support the arches
of the foot during the stance phase, assisting the intrinsic muscles of
the sole.
calcaneal tendon is ruptured, a much less effective and efficient push
off (from the midfoot) can still be accomplished by the actions of the
gluteus maximus and hamstrings in extending the thigh at the hip joint
and the quadriceps in extending the knee. Because push off from the
forefoot is not possible (in fact, the ankle will be passively
dorsiflexed as the body’s weight moves anterior to the foot), those
attempting to walk in the absence of plantarflexion often rotate the
foot as far laterally (externally) as possible during the stance phase
to disable passive dorsiflexion and allow a more effective push off
through hip and knee extension exerted at the midfoot.
region is closely associated with the assumption of bipedalism and an
erect posture. The prominent gluteal region is unique to humans.
Modification of the shape of the femur necessary for bipedal walking
and running (specifically the “bending” of the bone, creating the angle
of inclination and the trochanters, as discussed earlier in this
chapter) allows the superior placement of the abductors of the thigh
into the gluteal region. The remaining thigh muscles are organized into
three compartments by intermuscular septa that pass deeply between the
muscle groups from the inner surface of the fascia lata to the linea
aspera of the femur (Fig. 5.10D). The
compartments are anterior or extensor, medial or adductor, and posterior or flexor,
so named on the basis of their location or action at the knee joint.
Generally, the anterior group is innervated by the femoral nerve, the
medial group by the obturator nerve, and the posterior group by the
tibial portion of the sciatic nerve. Although the compartments vary in
absolute and relative size depending on level, the anterior compartment
is largest overall and includes the femur.
|
Table 5.2. Muscle Action during the Gait Cycle
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
used in dissection courses, the anterior and medial thigh is addressed
initially, followed by continuous examination of the posterior aspect
of the proximal limb: gluteal region, posterior thigh, and popliteal
fossa
The major muscles of the anterior compartment tend to atrophy
(diminish) rapidly with disease, and physical therapy is often
necessary to restore strength, tone, and symmetry with the opposite
limb after immobilization of the thigh or leg.
quadrangular muscle located in the anterior part of the superomedial
aspect of the thigh. It often appears to be composed of two layers,
superficial and deep, and these are generally innervated by two
different nerves. Because of the dual nerve supply and the muscle’s
actions (the pectineus adducts and flexes the thigh and assists in
medial rotation of the thigh), it is actually a transitional muscle
between the anterior and the medial compartments.
flexor of the thigh, the most powerful of the hip flexors with the
longest range. Although it is one of the body’s most powerful muscles,
it is relatively hidden, with most of its mass located in the posterior
wall of the abdomen and greater pelvis. Its broad lateral part, the iliacus, and its long medial part, the psoas major, arise from the iliac fossa and lumbar vertebrae, respectively (Table 5.3C).
Thus it is the only muscle attached to the vertebral column, pelvis,
and femur. It is in a unique position not only to produce movement but
to stabilize (fixate). However, it can also perpetuate and even
contribute to deformity and disability when it is malformed (especially
if it is shortened for various reasons), dysfunctional, or diseased.
the free limb, producing flexion at the hip to lift the limb and
initiate its forward swing during walking (i.e., during the preswing
and initial swing phases, as the opposite limb accepts weight; Table 5.2) or to elevate the limb during
climbing. However, it is also capable of moving the trunk. Bilateral
contraction initiates flexion of the trunk at the hip on the fixed
thigh—as when (incorrectly) doing sit-ups—and increases the lumbar
curvature of the vertebral column. It is active during walking
downhill, its eccentric contraction resisting acceleration. The
iliopsoas is also a postural muscle, active during standing in
maintaining normal lumbar lordosis (and indirectly the compensatory
thoracic kyphosis; see Chapter 4) and resisting hyperextension of the hip joint (Fig. 5.14). Unilateral weakness or spasticity may be a factor in the development of scoliosis.
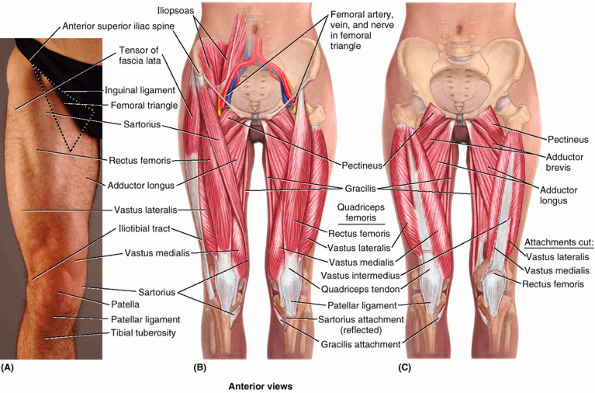 |
|
Figure 5.15. Muscles of anterior thigh. A. The surface anatomy of the anterior thigh muscles is shown. In B–C,
skin, subcutaneous tissue, and deep fascia have been removed to expose the anterior thigh muscles, the layers of which are demonstrated by removing the muscles sequentially, from superficial (B-right side) to deep (C-left side). |
patched or repaired), is long and ribbon-like. It passes obliquely
(lateral to medial) across the superoanterior part of the thigh (Fig. 5.15; Table 5.3D).
The sartorius lies superficially inside the anterior compartment,
within its own relatively distinct fascial sheath. This muscle descends
inferiorly as far as the side of the knee. The sartorius, the longest
muscle in the body, acts across two joints. It flexes the hip joint and
participates in flexion of the knee joint. It also weakly abducts the
thigh and laterally rotates it. The actions of both sartorius muscles
bring the lower limbs into the cross-legged sitting position. None of
the actions of the sartorius is strong; therefore, it is mainly a
synergist, acting with other thigh muscles that produce these movements.
four-headed femoral muscle) forms the main bulk of the anterior thigh
muscles and collectively constitutes the largest and one of the most
powerful muscles in the body. It may be three times stronger than its
antagonistic muscle group, the hamstrings. It covers almost all the
anterior aspect and sides of the femur. The quadriceps femoris
(quadriceps) consists of four parts: (1) rectus femoris, (2) vastus
lateralis, (3) vastus intermedius, and (4) vastus medialis.
Collectively, the quadriceps is a two-joint muscle capable of producing
action at both the hip and the knee. The two major components of the
quadriceps (rectus femoris and vasti) are discussed separately later in
this chapter.
Concentric contraction of the quadriceps to extend the knee against
gravity is important during rising from sitting or squatting, during
climbing and walking up stairs, and for acceleration and
projection
(running and jumping). In level walking, it becomes active during the
termination of the swing phase, preparing the knee to accept weight (Table 5.2).
It is primarily responsible for absorbing the jarring shock of heel
strike, and its activity continues as the weight is assumed during the
early stance phase (loading response). It also functions much of the
time as a fixator during bent-knee sports, such as skiing and tennis,
and contracts eccentrically during downhill walking and descending
stairs.
is the continuation of the quadriceps tendon in which the patella is
embedded. The patella is thus the largest sesamoid bone in the body.
The medial and lateral vasti muscles also attach independently to the
patella and form aponeuroses, the medial and lateral patellar retinacula,
which reinforce the joint capsule of the knee on each side of the
patella en route to attachment to the anterior border of the tibial
plateau. The retinacula also play a role in keeping the patella aligned
over the patellar articular surface of the femur.
during kneeling and the friction occurring when the knee is flexed and
extended during running. The patella also provides additional leverage
for the quadriceps in placing the tendon more anteriorly, farther from
the joint’s axis, causing it to approach the tibia from a position of
greater mechanical advantage. The inferiorly directed apex of the
patella indicates the level of the joint plane of the knee when the leg
is extended and the patellar ligament is taut.
|
Table 5.3-II. Muscles of the Anterior Thigh: Extensors of the Knee
|
|||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||
performed with the person in the supine position with the knee partly
flexed. The person extends the knee against resistance. During the
test, contraction of the rectus femoris should be observable and
palpable if the muscle is acting normally, indicating that its nerve
supply is intact.
straight). Because of its attachments to the hip bone and tibia, the
rectus femoris crosses two joints; hence it is capable of flexing the
thigh at the hip joint and extending the leg at the knee joint. The
rectus femoris is the only part of the quadriceps that crosses the hip
joint, and as a hip flexor it acts with and like the iliopsoas during
the preswing and initial swing phases of walking (Table 5.2).
The ability of the rectus femoris to extend the knee is compromised
during hip flexion, but it does contribute to the extension force
during the toe off phase, when the thigh is extended. It is
particularly efficient in movements combining knee extension and hip
flexion from a position of hip hyperextension and knee flexion, as in
the preparatory position for kicking a soccer ball. The rectus femoris,
the “kicking muscle,” is susceptible to injury and avulsion from the
anterior inferior iliac spine during kicking. A loss of function of the
rectus femoris may reduce thigh flexion strength by as much as 17% (Markhede and Stener, 1981).
-
Vastus lateralis, the largest component of the quadriceps, lies on the lateral side of the thigh.
-
Vastus medialis covers the medial side of the thigh.
-
Vastus intermedius lies deep to the rectus femoris, between the vastus medialis and the vastus lateralis.
superiorly to the inferior part of the anterior aspect of the femur and
inferiorly to the synovial membrane of the knee joint and the wall of
the suprapatellar bursa (Table 5.3A).
This muscle pulls the synovial membrane superiorly during extension of
the leg, thereby preventing folds of the membrane from being compressed
between the femur and the patella within the knee joint.
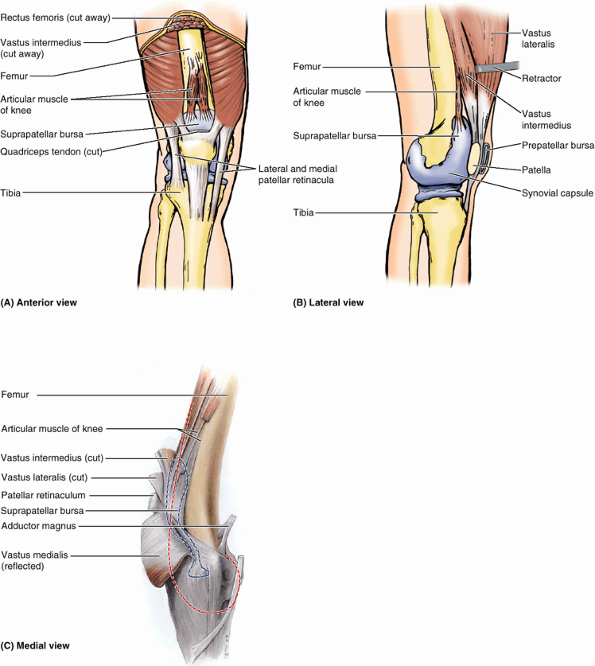 |
|
Figure 5.16. Suprapatellar bursa and articular muscle of knee. A and B.
The large suprapatellar bursa, normally a potential space extending between the quadriceps and the femur, is depicted as if injected with latex. C. In this deep dissection of the knee region, the projected outline of the femur is indicated by a red broken line and the extent of the suprapatellar bursa is indicated by a blue broken line. A–C. The articular muscle of the knee is shown as extending from the distal femur to attach to the bursa. This muscle blends with the deep aspect of the vastus intermedius. |
flexors of the hip and extensors of the knee, with most muscles
innervated by the femoral nerve. The quadriceps femoris accounts for
most of the mass of this compartment. It surrounds the femur on three
sides and has a common tendon of attachment to the tibia, which
includes the patella as a sesamoid bone. Major muscles of this
compartment atrophy rapidly with disease or disuse, requiring physical
therapy to retain or restore function.
that usually occurs at its anterior part (e.g., where the sartorius
attaches to the ASIS). This is one of the most common injuries to the
hip region, usually occurring in association with collision sports,
such as the various forms of football, ice hockey, and volleyball. Contusions cause bleeding from ruptured capillaries and infiltration of blood into the muscles, tendons, and other soft tissues. The term hip pointer
may also refer to avulsion of bony muscle attachments, for example, of
the sartorius or rectus femoris to the anterior iliac spines, of the
hamstrings from the ischium (see clinical correlation [blue] box “Hamstring Injuries,” in this chapter), or of the iliopsoas from the lesser trochanter of the femur). However, these injuries should be called avulsion fractures.
refer either to the cramping of an individual thigh muscle because of
ischemia or to contusion and rupture of blood vessels sufficient enough
to form a hematoma. The injury is usually
the consequence of tearing of fibers of the rectus femoris; sometimes
the quadriceps tendon is also partially torn. The most common site of a
thigh hematoma is in the quadriceps. A charley horse is associated with
localized pain and/or muscle stiffness and commonly follows direct
trauma (e.g., a stick slash in hockey or a tackle in football).
intervertebral discs, the sides of the T12–L5 vertebrae, and their
transverse processes. The medial arcuate ligament of the diaphragm
arches obliquely over the proximal part of the psoas major (see Chapter 2).
The transversalis fascia on the internal abdominal wall is continuous
with the psoas fascia, where it forms a fascial covering for the psoas
major that accompanies the muscle into the anterior region of the thigh.
(pus-forming) infection in the abdomen or greater pelvis,
characteristically occurring in association with TB of the vertebral
column, or secondary to regional enteritis of the ileum (Crohn
disease), may result in the formation of a psoas abscess.
When the abscess passes between the psoas and its fascia to the
inguinal and proximal thigh regions, severe pain may be referred to the
hip, thigh, or knee joint. Consequently, a psoas abscess should always
be considered when edema occurs in the proximal part of the thigh. Such
an abscess may be palpated or observed in the inguinal region, just
inferior or superior to the inguinal ligament, and may be mistaken for
an indirect inguinal hernia or a femoral hernia, an enlargement of the
inguinal lymph nodes, or a saphenous varix (see clinical correlation [blue] box “Saphenous Varix,”
in this chapter). The lateral border of the psoas is commonly visible
in radiographs of the abdomen; an obscured psoas shadow may be an
indication of abdominal pathology.
leg against resistance and usually presses on the distal end of the
thigh during walking to prevent inadvertent flexion of the knee joint.
Weakness of the vastus medialis or vastus lateralis, resulting from
arthritis or trauma to the knee joint, for example, can result in
abnormal patellar movement and loss of joint stability.
(runner’s knee) is a common knee problem for marathon runners. Such
overstressing of the knee can also occur in running sports such as
basketball. The soreness and aching around or deep to the patella
results from quadriceps imbalance.
Chondromalacia patellae may result from a blow to the patella or
extreme flexion of the knee (e.g., during squatting when power lifting).
may result from a blow to the knee or sudden contraction of the
quadriceps (e.g., when one slips and attempts to prevent a backward
fall). The proximal fragment is pulled superiorly with the quadriceps
tendon, and the distal fragment remains with the patellar ligament.
ossified during the 3rd–6th years, frequently from more than one
ossification center. Although these centers usually coalesce and form a
single bone, they may remain separate on one or both sides, giving rise
to a bipartite or tripartite patella (Fig. B5.9).
An unwary observer might interpret this condition on a radiograph or CT
as a patellar fracture. Ossification abnormalities are nearly always
bilateral; therefore, diagnostic images should be examined from both
sides. If the defects are bilateral, the abnormalities are likely
ossification abnormalities.
 |
|
Figure B5.9
|
(knee jerk). This myotatic (deep tendon) reflex is routinely tested
during a physical examination by having the person sit with legs
dangling. A firm strike on the ligament with a reflex hammer usually
causes the leg to extend. If the reflex is normal, a hand on the
person’s quadriceps should feel the muscle contract. This tendon reflex
tests the integrity of the femoral nerve and the L2–L4 spinal cord
segments. Tapping the ligament activates muscle spindles in the
quadriceps; afferent impulses from the spindles travel in the femoral
nerve to the L2–L4 segments of the spinal cord. From here, efferent
impulses are transmitted via motor fibers in the femoral nerve to the
quadriceps, resulting in a jerk-like contraction of the muscle and
extension of the leg at the knee joint. Diminution or absence of the patellar tendon reflex may result from any lesion that interrupts the innervation of the quadriceps (e.g., peripheral nerve disease).
The adductor group of thigh muscles consists of the adductor longus,
adductor brevis, adductor magnus, gracilis, and obturator externus. In
general, they attach proximally to the anteroinferior exterior of the
bony pelvis (pubic bone, ischiopubic ramus, and ischial tuberosity) and
adjacent obturator membrane and distally to the linea aspera of the
femur (Table 5.4A). All adductor muscles, except the “hamstring part” of the adductor magnus—plus part of the pectineus—are supplied by the obturator nerve
(L2–L4). The pectineus is supplied by the femoral nerve (L2–L4), and
the hamstring part of the adductor magnus is supplied by the tibial
part of the sciatic nerve (L4). The details of their attachments, nerve
supply, and actions of the muscles are provided in Table 5.4. While collectively these muscles are the adductors of the thigh, the actions of some of these muscles are more complex.
arises by a strong tendon from the anterior aspect of the body of the
pubis just inferior to the pubic tubercle (apex of triangle) and
expands to attach to the linea aspera of the femur (base of triangle);
in so doing it covers the anterior aspects of the adductor brevis and
middle of the adductor magnus.
lies deep to the pectineus and adductor longus where it arises from the
body and inferior ramus of the pubis. It widens as it passes distally
to attach to the uppermost part of the linea aspera. As the obturator
nerve emerges from the obturator canal to enter the medial compartment
of the thigh, it splits into an anterior and a posterior division, the
two divisions passing anterior and posterior to the adductor brevis.
This unique relationship is useful in identifying the muscle in
dissection and in anatomical cross sections.
The adductor part fans out widely for aponeurotic distal attachment
along the entire length of the linea aspera of the femur, extending
inferiorly onto the medial supracondylar ridge. The hamstring part has
a tendinous distal attachment to the adductor tubercle.
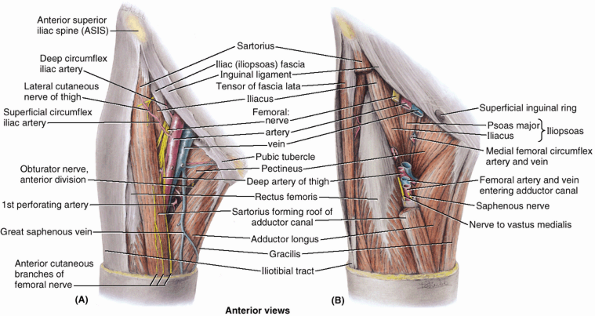 |
|
Figure 5.17. Femoral triangle. A.
The boundaries and contents of the femoral triangle are shown. Observe the structures that bound the triangle: the inguinal ligament superiorly, the adductor longus medially, and the sartorius laterally. Superiorly, the femoral nerve and vessels enter the base of the triangle; inferiorly, they exit from its apex. B. In this deeper dissection, sections have been removed from the sartorius and the femoral vessels and nerve. Observe the muscles forming the floor of the femoral triangle: the iliopsoas laterally and the pectineus medially. Of the neurovascular structures at the apex of the femoral triangle, the two anterior vessels (femoral artery and vein) and the two nerves enter the adductor canal (anterior to adductor longus), and the two posterior vessels (deep artery and vein of thigh) pass deep (posterior) to the adductor longus. |
a long, strap-like muscle and is the most medial muscle of the thigh.
It is the most superficial of the adductor group and the weakest
member. It is the only one of the group to cross the knee joint as well
as the hip joint, joining with two other two-joint muscles from the
other two compartments (the sartorius and semitendinosus muscles. Thus
the three muscles are innervated by three different nerves). They have
a common tendinous insertion, the pes anserinus
(L. goose’s foot), into the upper part of the medial surface of the
tibia. The gracilis is a synergist in adducting the thigh, flexing the
knee, and rotating the leg medially when the knee is flexed. It acts
with the other “pes anserinus” muscles to add stability to the medial
aspect of the extended knee, much as the gluteus maximus and tensor of
the fascia lata do via the iliotibial tract on the lateral side.
flat, relatively small, fan-shaped muscle that is deeply placed in the
superomedial part of the thigh. It extends from the external surface of
the obturator membrane and surrounding bone of the pelvis to the
posterior aspect of the greater trochanter, passing directly under the
acetabulum and neck of the femur.
adductor muscle group is to pull the thigh medially, toward or past the
median plane. Three adductors (longus, brevis, and magnus) are used in
all movements in which the thighs are adducted (e.g., pressed together
when riding a horse). They are used to stabilize the stance when
standing on both feet, to correct lateral sway of the trunk, or when
there is a side-to-side shift of the surface on which one is standing
(rocking a boat, standing on a balance board). They are also used in
kicking with the medial side of the foot in soccer and in swimming.
Finally, they contribute to flexion of the extended thigh and extension
of the flexed thigh when running or against resistance.
Although they are important in many activities, it has been shown that
a reduction of as much as 70% in their function will result in only a
slight to moderate impairment of hip function (Markhede and Stener, 1981).
is performed while the person is lying supine with the knee straight.
The person adducts the thigh against resistance, and if the adductors
are normal, the proximal ends of the gracilis and adductor longus can
easily be palpated.
|
Table 5.4. Muscles of the Medial Thigh: Adductors of the Thigh
|
||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||
attach proximally to the anteroinferior bony pelvis and distally to the
linea aspera of the femur. They are adductors of the thigh, innervated
primarily by the obturator nerve. Use of these muscles as prime movers
is relatively limited.
opening or gap between the aponeurotic distal attachment of the
adductor part of the adductor magnus and the tendinous distal
attachment of the hamstring part. The adductor hiatus transmits the
femoral artery and vein from the adductor canal in the thigh to the
popliteal fossa posterior to the knee (Table 5.4). The opening is located just lateral and superior to the adductor tubercle of the femur.
adductor group of muscles, it can be removed without noticeable loss of
its actions on the leg. Hence, surgeons often transplant the gracilis,
or part of it, with its nerve and blood vessels to replace a damaged
muscle in the hand, for example. Once the muscle is transplanted, it
soon produces good digital flexion and extension. Freed from its distal
attachment, the muscle has also been relocated and repositioned to
create a replacement for a non-functional external anal sphincter.
injury.” These terms mean that a strain, stretching, and probably some
tearing of the proximal attachments of the anteromedial thigh muscles
has occurred. The injury usually involves the flexor and adductor thigh
muscles. The proximal attachments of these muscles are in the inguinal
region (groin), the junction of the thigh and trunk. Groin pulls
usually occur in sports that require quick starts such as
short-distance racing (e.g., a 60-m sprint), base stealing in baseball,
and quick starts in basketball.
may occur in horseback riders and produce pain (rider’s strain).
Ossification sometimes occurs in the tendons of these muscles because
the horseback riders actively adduct their thighs to keep from falling
from their animals. The areas of the ossified tendons are sometimes
called “riders’ bones.”
triangular landmark useful in dissection and in understanding
relationships in the groin. (Figs. 5.15A & B, and 5.17, 5.18 and 5.19).
In living people it appears as a triangular depression inferior to the
inguinal ligament when the thigh is flexed, abducted, and laterally
rotated. (Fig. 5.15A) The femoral triangle is bounded:
-
Superiorly by the inguinal ligament (the thickened inferior margin of the external oblique aponeurosis) that forms the base of the femoral triangle.
-
Medially by the adductor longus.
-
Laterally by the sartorius; the apex is where the lateral border of the sartorius crosses the medial border of the adductor longus.
(created as the inguinal ligament spans the gap between the two bony
prominences to which it is attached, the ASIS and public tubercle) is
an important passageway connecting the trunk/abdominopelvic cavity to
the lower limb. The inguinal ligament actually serves as a flexor
retinaculum, retaining structures that pass anterior to the hip joint
against the joint during flexion of the thigh. The passageway posterior
to the ligament is divided into two compartments, or lacunae, by a
thickening of the iliopsoas fascia, the iliopectineal arch (Fig. 5.19), which passes between the deep surface of the inguinal ligament and the iliopubic eminence (Fig. 5.6B). Lateral to the arch is the muscular lacuna,
through which the iliopsoas muscle and femoral nerve pass from the
greater pelvis into the anterior thigh; medial to the arch, the vascular lacuna
allows passage of the major vascular structures (veins, artery, and
lymphatics) between the greater pelvis and the femoral triangle of the
anterior thigh. As they enter the femoral triangle, the names of the
vessels change from external iliac to femoral.
-
Femoral nerve and its (terminal) branches.
-
Femoral sheath and its contents:
-
Femoral artery and several of its branches.
-
Femoral vein and its proximal tributaries (e.g., the great saphenous and deep femoral veins).
-
Deep inguinal lymph nodes and associated lymphatic vessels.
-
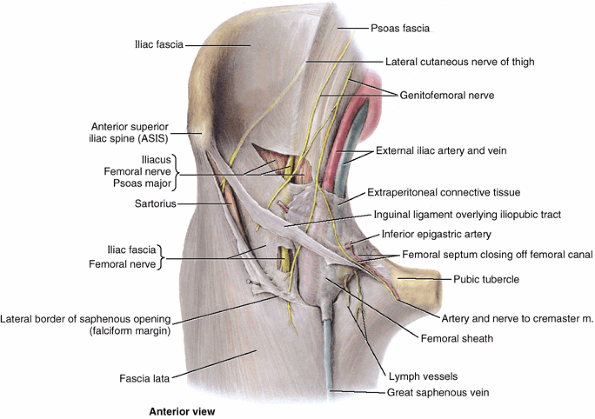 |
|
Figure 5.18. Dissection of femoral sheath in femoral triangle.
The falciform margin of the saphenous opening in the fascia lata is cut and reflected. Note that the femoral nerve is external and lateral to the femoral sheath, whereas the femoral artery and vein occupy the sheath. |
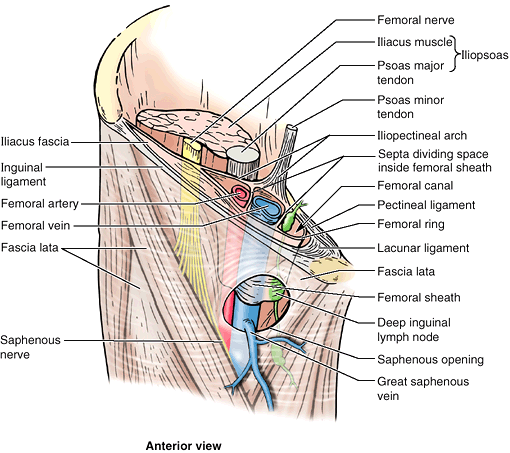 |
|
Figure 5.19. Structure and contents of femoral sheath.
This dissection is of the superior end of the anterior aspect of the right thigh. Note the compartments within the femoral sheath. The proximal end (abdominal opening) of the femoral canal is the femoral ring. |
and vein, which pass to and from the adductor canal inferiorly at its
apex (Fig. 5.17A). The adductor canal is an intramuscular passageway by which the major neurovascular bundle of the thigh traverses its middle third (Figs. 5.17B and 5.20).
the largest branch of the lumbar plexus. The nerve originates in the
abdomen within the psoas major and descends posterolaterally through
the pelvis to approximately the midpoint of the inguinal ligament (Figs. 5.17A, 5.18 and 5.19).
It then passes deep to this ligament and enters the femoral triangle,
lateral to the femoral vessels. After entering the triangle, the
femoral nerve divides into several branches to the anterior thigh
muscles. It also sends articular branches to the hip and knee joints
and provides several cutaneous branches to the anteromedial side of the
thigh (Table 5.1). The terminal cutaneous branch of the femoral nerve, the saphenous nerve, descends through the femoral triangle, lateral to the femoral sheath containing the femoral vessels (Fig. 5.17B and 5.19).
The saphenous nerve accompanies the femoral artery and vein through the
adductor canal and becomes superficial by passing between the sartorius
and the gracilis when the femoral vessels traverse the adductor hiatus
at the distal end of the canal. It runs anteroinferiorly to supply the
skin and fascia on the anteromedial aspects of the knee, leg, and foot.
It terminates inferiorly by blending with the adventitia of the femoral
vessels. The sheath encloses proximal parts of the femoral vessels and
creates the femoral canal medial to them (Figs. 5.18 and 5.19). The sheath is formed by an inferior prolongation of transversalis and iliopsoas fascia from the abdomen/greater pelvis (see Chapter 2).
The femoral sheath does not enclose the femoral nerve because it passes
through the muscular lacuna. When a long femoral sheath occurs (when it
extends farther distally), its medial wall is pierced by the great
saphenous vein and lymphatic vessels (Fig. 5.18).
The femoral sheath allows the femoral artery and vein to glide deep to
the inguinal ligament during movements of the hip joint.
compartments by vertical septa of extraperitoneal connective tissue
that extend from the abdomen along the femoral vessels (Fig. 5.19). The compartments of the femoral sheath are the:
-
Lateral compartment for the femoral artery.
-
Intermediate compartment for the femoral vein.
-
Medial compartment, which constitutes the femoral canal.
smallest of the three compartments. It is short (approximately 1.25 cm)
and conical and lies between the medial edge of the femoral sheath and
the femoral vein. The femoral canal (Fig. 5.19):
-
Extends distally to the level of the proximal edge of the saphenous opening.
-
Allows the femoral vein to expand when
venous return from the lower limb is increased or when increased
intra-abdominal pressure causes a temporary stasis in the vein (as
P.603
during a Valsalva maneuver, i.e., taking a breath and holding it, often while bearing down).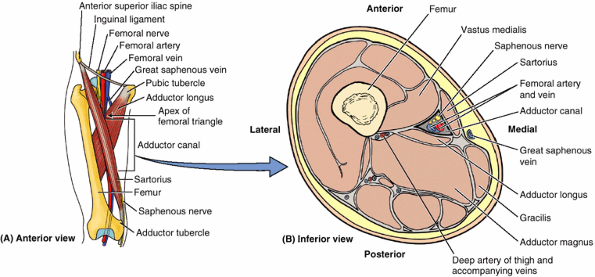 Figure 5.20. Adductor canal in medial part of middle third of thigh. A. Orientation drawing showing the canal formed between the three thigh muscles and the level of the section shown in part B. B. This transverse section of the thigh shows the muscles bounding the adductor canal and its neurovascular contents.
Figure 5.20. Adductor canal in medial part of middle third of thigh. A. Orientation drawing showing the canal formed between the three thigh muscles and the level of the section shown in part B. B. This transverse section of the thigh shows the muscles bounding the adductor canal and its neurovascular contents. -
Contains loose connective tissue, fat, a few lymphatic vessels, and sometimes a deep inguinal lymph node (Cloquet node).
-
Laterally, the vertical septum between the femoral canal and the femoral vein.
-
Posteriorly, the superior ramus of the pubis covered by the pectineus and its fascia.
-
Medially, the lacunar ligament.
-
Anteriorly, the medial part of the inguinal ligament.
It enters the femoral triangle deep to the midpoint of the inguinal
ligament (midway between the ASIS and the pubic tubercle), lateral to
the femoral vein (Fig. 5.20A).
Its pulsations are palpable within the triangle because of its
relatively superficial position deep (posterior) to the fascia lata,
where it lies and descends on the adjacent borders of the iliopsoas and
pectineus that make up the floor of the triangle. The superficial
epigastric artery, superficial (and sometimes the deep) circumflex
iliac arteries, and the superficial and deep external pudendal arteries
arise from the anterior aspect of the proximal part of the femoral
artery.
is the largest branch of the femoral artery and the chief artery to the
thigh. It arises from the lateral or posterior side of the femoral
artery in the femoral triangle. In the middle third of the thigh, where
it is separated from the femoral artery and vein by the adductor longus
(Figs. 5.17B and 5.20B),
it gives off perforating arteries that wrap around the posterior aspect
of the femur. The perforating arteries supply muscles of all three
fascial compartments (adductor magnus, hamstrings, and vastus
lateralis).
encircle the uppermost shaft of the femur and anastomose with each
other and other arteries, supplying the thigh muscles and the superior
(proximal) end of the femur. The medial circumflex femoral artery is especially important because it supplies most of the blood to the head and the neck of the femur via its branches, the posterior retinacular arteries. The retinacular arteries are often torn when the femoral neck is fractured or the hip joint is dislocated. The lateral circumflex femoral artery,
less able to supply the femoral head and neck as it passes laterally
across the thickest part of the joint capsule of the hip joint, mainly
supplies muscles on the lateral side of the thigh.
supply the adductor muscles via anterior and posterior branches, which
anastomose (Table 5.5). The posterior branch gives off an acetabular branch that supplies the head of the femur.
branching of the deep artery of the thigh, is superficial in position,
making it especially accessible and useful for a number of clinical
procedures. Some vascular surgeons refer to this part of the femoral
artery as the common femoral artery and to its continuation distally as the superficial femoral artery.
This terminology is not recommended by the Federative International
Committee on Anatomical Terminology and is not used in this book
because these terms may cause misunderstanding. Anterior to the initial
part of the femoral artery are the skin, subcutaneous tissue,
superficial inguinal lymph nodes, superficial circumflex iliac artery,
cribriform fascia, and the anterior part of the femoral sheath (Figs. 5.10, 5.12, and 5.18).
By placing the tip of the little finger (of the right hand when dealing
with the right side) on the ASIS and the tip of the thumb on the pubic
tubercle, the femoral pulse can be palpated with the midpalm just
inferior to the midpoint of the inguinal ligament by pressing firmly.
Normally the pulse is strong; however, if the common or external iliac
arteries are partially occluded, the pulse may be diminished.
may also be accomplished at this site by pressing directly posteriorly
against the superior pubic ramus, psoas major, and femoral head (Fig. B5.10C).
Compression at this point will reduce blood flow through the femoral
artery and its branches, such as the deep artery of the thigh.
a long, slender catheter is inserted into the artery and passed up the
external iliac artery, common iliac artery, and aorta to the left
ventricle of the heart (see Chapter 1).
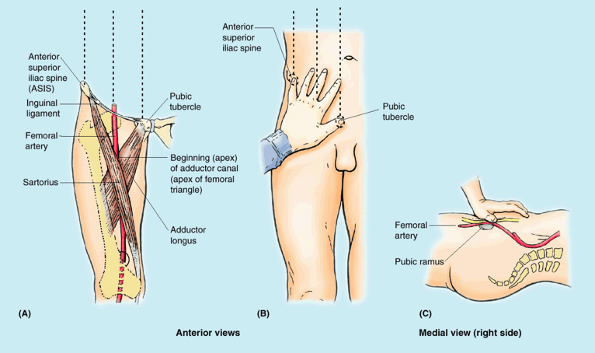 |
|
Figure B5.10
|
femoral triangle also makes it vulnerable to traumatic injury,
especially laceration. Commonly, both the femoral artery and vein are
lacerated in anterior thigh wounds because they lie close together. In
some cases, an arteriovenous shunt occurs as a result of communication
between the injured vessels. When it is necessary to ligate the femoral
artery, anastomosis of branches of the femoral artery with other
arteries that cross the hip joint, may supply blood to the lower limb.
However, the cruciate anastomosis,
consisting of a four-way common meeting of the medial and lateral
circumflex femoral arteries with the inferior gluteal artery superiorly
and the first perforating artery inferiorly posterior to the femur,
occurs less commonly than its frequent description in textbooks and
depiction in atlases implies.
in approximately 20% of people. This artery runs close to or across the
femoral ring to reach the obturator foramen and would be closely
related to the neck of a femoral hernia. Consequently, this artery
could be involved in a strangulated femoral hernia.
Surgeons placing staples during endoscopic repair of both inguinal and
femoral hernias must also be vigilant concerning the possible presence
of this common arterial variant.
continuation of the popliteal vein proximal to the adductor hiatus. As
it ascends through the adductor canal, the femoral vein lies
posterolateral and then posterior to the femoral artery (Figs. 5.17A & B and 5.19).
The femoral vein enters the femoral sheath lateral to the femoral canal
and ends posterior to the inguinal ligament, where it becomes the
external iliac vein. In the inferior part of the femoral triangle, the
femoral vein receives the deep vein of the thigh, the great saphenous
vein, and other tributaries. The deep vein of the thigh,
formed by the union of three or four perforating veins, enters the
femoral vein approximately 8 cm inferior to the inguinal ligament and
approximately 5 cm inferior to the termination of the great saphenous
vein.
|
Table 5.5. Arteries of the Anterior and Medial Thigh
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||
some text and reference books use the term “superficial femoral vein”
when referring to the femoral vein before it is joined by the
accompanying veins of the deep artery of the thigh (deep femoral
veins). Some primary care physicians may not have been taught and/or
may not realize that the so-called superficial femoral vein is actually
a deep vein and that acute thrombosis of this vessel is potentially
life threatening. The adjective superficial should not be used because it implies that this vein is a superficial vein. Most pulmonary emboli
originate in deep veins, not in superficial veins. The risk of embolism
can be greatly reduced by anticoagulant treatment. The use of imprecise
language here creates the possibility that an acute thrombosis of this
truly deep vessel could be overlooked as an acute clinical issue, and a
life-threatening situation created. Anatomical terminology used in
clinical reports must be accurate to avoid possible life-threatening
situations.
(L. dilated vein), may cause edema in the femoral triangle. A saphenous
varix may be confused with other groin swellings such as a psoas
abscess (see clinical correlation [blue] box “Psoas Abscess,” in this chapter); however, a varix should be considered when varicose veins are present in other parts of the lower limb.
position can be located inferior to the inguinal ligament by feeling
the pulsations of the femoral artery, which is immediately lateral to
the vein. In thin people, the femoral vein may be close to the surface
and may be mistaken for the great saphenous vein. It is important
therefore to know that the femoral vein has no tributaries at this
level, except for the great saphenous vein that joins it approximately
3 cm inferior to the inguinal ligament. In varicose vein operations, it is obviously important to identify the great saphenous vein correctly and not tie off the femoral vein by mistake.
from the chambers of the right side of the heart and/or from the
pulmonary artery and to perform right cardiac angiography,
a long, slender catheter is inserted into the femoral vein as it passes
through the femoral triangle. Under fluoroscopic control, the catheter
is passed superiorly through the external and common iliac veins into
the inferior vena cava and right atrium of the heart. Femoral venous
puncture may also be used for the administration of fluids.
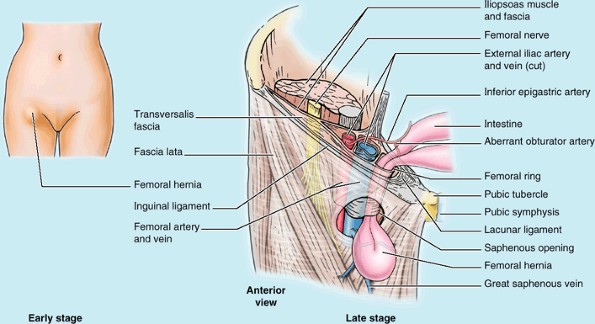 |
|
Figure B5.11
|
abdominal wall that normally is of a size sufficient to admit the tip
of the little finger. The femoral ring is the usual originating site of
a femoral hernia, a protrusion of
abdominal viscera (often a loop of small intestine) through the femoral
ring into the femoral canal. A femoral hernia appears as a mass, often
tender, in the femoral triangle, inferolateral to the pubic tubercle (Fig. B5.11).
The hernia is bounded by the femoral vein laterally and the lacunar
ligament medially. The hernial sac compresses the contents of the
femoral canal (loose connective tissue, fat, and lymphatics) and
distends the wall of the canal. Initially, the hernia is small because
it is contained within the canal; but it can enlarge by passing
inferiorly through the saphenous opening into the subcutaneous tissue
of the thigh. Femoral hernias are more common in females. Strangulation of a femoral hernia
may occur because of the sharp, rigid boundaries of the femoral ring,
particularly the concave margin of the lacunar ligament. Strangulation
of a femoral hernia interferes with the blood supply to the herniated
intestine. This vascular impairment may result in death of the tissues.
(subsartorial canal; Hunter canal) is a long (approximately 15 cm),
narrow passageway in the middle third of the thigh. It extends from the
apex of the femoral triangle, where the sartorius crosses over the
adductor longus, to the adductor hiatus in the tendon of the adductor magnus (Fig. 5.20).
The adductor canal provides an intermuscular passage for the femoral
artery and vein, the saphenous nerve, and the nerve to vastus medialis,
delivering the femoral vessels to the popliteal fossa where they become
the popliteal vessels.
-
Anteriorly and laterally by the vastus medialis.
-
Posteriorly by the adductors longus and magnus.
-
Medially by the sartorius, which overlies the groove between the above muscles, forming the roof of the canal.
subsartorial or vastoadductor fascia spans between the adductor longus
and the vastus medialis muscles, forming the anterior wall of the canal
deep to the sartorius. Because this fascia has a distinct superior
margin, novices dissecting in this area commonly assume when they see
the femoral vessels pass deep to this fascia that they are traversing
the adductor hiatus. The adductor hiatus, however, is located at a more
inferior level, just proximal to the medial supracondylar ridge. This
hiatus is a gap between the aponeurotic adductor and the tendinous
hamstrings attachments of the adductor magnus.
of the arm, is placed on the medial side of the limb for protection. In
the upper third of the thigh, the bundle is most superficial as it
enters deep to the inguinal ligament. This relatively superficial
position is important for clinical procedures. Although they are
essentially adjacent, the femoral nerve traverses the muscular lacunae
of the subinguinal space, whereas the femoral vessels traverse the
vascular lacunae within the femoral sheath. The femoral vessels bisect
the femoral triangle, where the primary vessels of the thigh, the deep
artery and vein of the thigh, arise and terminate, respectively. The
femoral nerve per se terminates within the triangle. However, two of
its branches, a motor branch (nerve to vastus medialis) and sensory
branch (saphenous nerve), are part of the neurovascular bundle that
traverses the adductor canal in the middle third of the thigh. The
vascular structures then pass through the adductor hiatus, becoming
popliteal in name and location in the distal thigh/posterior knee
region.
anteriorly at the inguinal ligament, posteriorly the gluteal region is
a large transitional zone between trunk and limb. Physically part of
the trunk, functionally the gluteal region is definitely part of the
limb. The gluteal region is the prominent area posterior to the pelvis
and inferior to the level of the iliac crests (the buttocks) and
extending laterally and anteriorly to the greater trochanter according
to some definitions and to the ASIS according to others (Fig. 5.21). The intergluteal cleft separates the buttocks from each other. The gluteal muscles
(gluteus maximus, medius, and minimus and tensor of the fascia lata) form the bulk of the region. The gluteal fold demarcates the inferior boundary of the buttock and the superior boundary of the thigh.
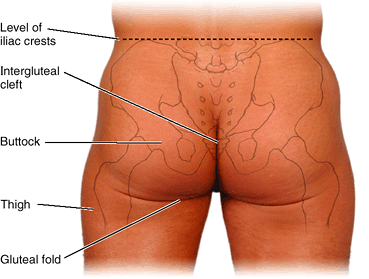 |
|
Figure 5.21. Gluteal region—buttocks area.
The intergluteal cleft separates the buttocks (right and left gluteal regions or prominences). The gluteal fold (sulcus) marks the lower limit of the buttock and the upper limit of the thigh. |
is the passageway for structures entering or leaving the perineum
(e.g., pudendal nerve). It is helpful to think of the greater sciatic
foramen as the “door” through which all lower limb arteries and nerves
leave the pelvis and enter the gluteal region. The piriformis (Table 5.6) also enters the gluteal region through the greater sciatic foramen and almost fills it.
-
The superficial layer
consists of the three large glutei (maximus, medius, and minimus) and
the tensor of the fascia lata. These muscles all have proximal
attachments to the posterolateral (external) surface and margins of the
ala of the ilium and are mainly extensors, abductors, and medial
rotators of the thigh. -
The deep layer
consists of smaller muscles (piriformis, obturator internus, externus
gemelli, and quadratus femoris) covered by the inferior half of the
gluteus maximus. They all have distal attachments on or adjacent to the
intertrochanteric crest of the femur. These muscles are lateral
rotators of the thigh but they also stabilize the hip joint, working
with the strong ligaments of the hip joint to steady the femoral head
in the acetabulum.
most superficial gluteal muscle. It is the largest, heaviest, and most
coarsely fibered muscle of the body. The gluteus maximus covers all of
the other gluteal muscles (Figs. 5.23A & C and 5.24A) except for the anterosuperior third of the gluteus medius. The ischial tuberosity
can be felt on deep palpation through the inferior part of the muscle,
just superior to the medial part of the gluteal fold. When the thigh is
flexed, the inferior border of the gluteus maximus moves superiorly,
leaving the ischial tuberosity subcutaneous. You do not sit on your
gluteus maximus; you sit on the fatty fibrous tissue and the ischial
bursa that lie between the ischial tuberosity and the skin.
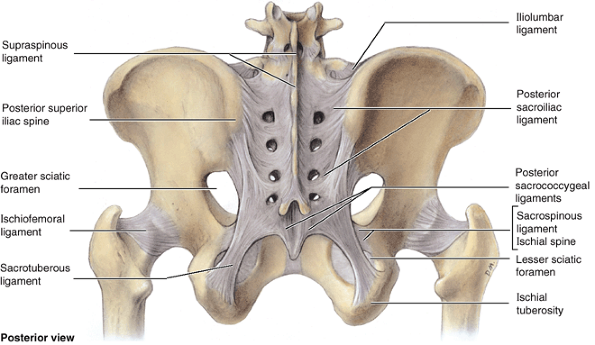 |
|
Figure 5.22. Ligaments of pelvic girdle.
The sacrotuberous and sacrospinous ligaments pass from the ischial tuberosity and ischial spine, respectively, to the side of the sacrum and coccyx. These ligaments convert the greater and lesser sciatic notches into foramina. The greater sciatic foramen is the doorway of the true pelvis; the lesser sciatic foramen, the entrance to the perineum. |
|
Table 5.6. Muscles of Gluteal Region: Abductors and Rotators of the Thigh
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
angle from the pelvis to the buttock. The fibers of the superior and
larger part of the gluteus maximus and superficial fibers of the
inferior part insert into the iliotibial tract (Fig. 5.23A, C, & D). Some deep fibers of the inferior part of the muscle (roughly the deep anterior and inferior quarter) attach to the gluteal tuberosity of the femur.
The inferior gluteal nerve and vessels enter the deep surface of the
gluteus maximus at its center. It is supplied by both the inferior and
superior gluteal arteries. In the superior part of its course, the sciatic nerve passes deep to the gluteus maximus (Fig. 5.24A).
and lateral rotation of the thigh. When the gluteus maximus is fixed
proximally, the muscle extends the trunk on the lower limb. Although it
is the strongest extensor of the hip, it acts mostly when force is
necessary (rapid movement or movement against resistance) and functions
primarily between the flexed and standing (straight) positions of the
thigh, as when rising from the sitting position, straightening from the
bending position, walking uphill and up stairs, and running. It is used
only briefly during casual walking and usually not at all when standing
motionless. Paralysis of the gluteus maximus does not seriously affect
walking on level ground. Verify this by placing your hand on your
buttock when walking slowly. The gluteus maximus contracts only briefly
during the earliest part of the stance phase (from heel strike to when
the foot is flat on the ground, to resist further flexion as weight is
assumed by the partially flexed limb) (Table 5.2). If you climb stairs and put your hand on your buttock, you will feel the gluteus maximus contract strongly.
the gluteus maximus and tensor of the fascia lata together are also
able to assist in making the extended knee stable, but they are not
usually called on to do so during normal standing. Because the
iliotibial tract attaches to the femur via the lateral intermuscular
septum, it does not have the freedom necessary to produce motion at the
knee.
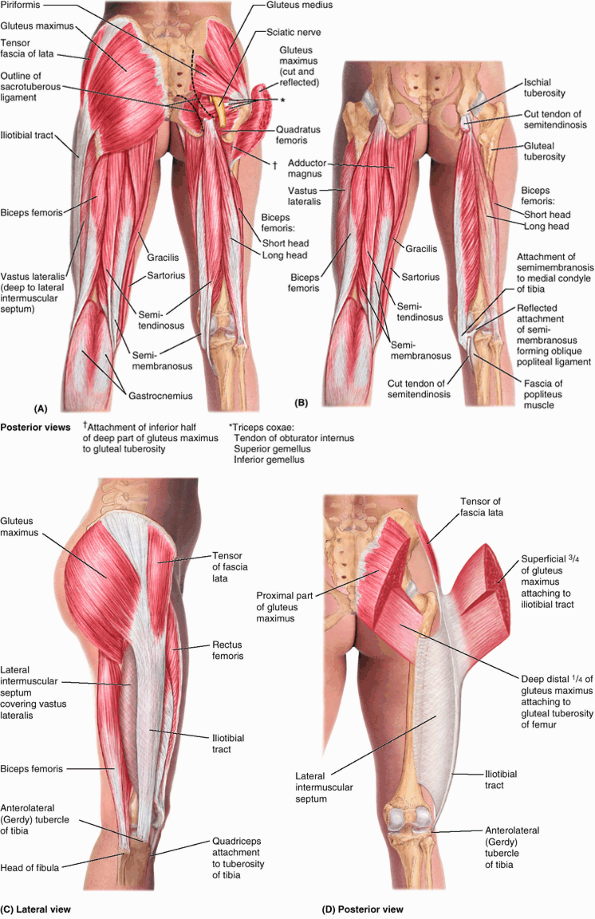 |
|
Figure 5.23. Muscles of gluteal region and posterior compartment of thigh. Superficial and deep dissections of the gluteal region (A) and the posterior compartment of the thigh (B) are demonstrated. Also shown are superficial (C) and deep (D)
views of the lateral musculofibrous complex formed by the tensor of the fascia lata and gluteus maximus muscles and their shared aponeurotic tendon, the iliotibial tract. The iliotibial tract is continuous (posteriorly and deeply) with the dense lateral intermuscular septum, by which the tract is attached to the linea aspera of the femur. |
is performed when the person is prone with the lower limb straight. The
person tightens the buttock and extends the hip joint as the examiner
observes and palpates the gluteus maximus.
Bursae are membranous sacs lined by a synovial membrane containing a
capillary layer of slippery fluid resembling egg white. Bursae are
located in areas subject to friction (e.g., where the iliotibial tract
crosses the greater trochanter); their purpose is to reduce friction
and permit free movement. Usually three bursae are associated with the
gluteus maximus:
-
The trochanteric bursa
separates superior fibers of the gluteus maximus from the greater
trochanter. The trochanteric bursa is commonly the largest of the
bursae formed in relation to bony prominences and is present at birth.
Other such bursae appear to form as a result of postnatal movement. -
The ischial bursa separates the inferior part of the gluteus maximus from the ischial tuberosity; it is often absent.
-
The gluteofemoral bursa separates the iliotibial tract from the superior part of the proximal attachment of the vastus lateralis, a thigh muscle.
and are supplied by the same blood vessel, the superior gluteal artery.
The gluteus minimus and most of the gluteus medius lie deep to the
gluteus maximus on the external surface of the ilium. The gluteus
medius and minimus abduct the thigh and rotate it medially (Fig. 5.26; Table 5.2).
is performed while the person is prone with the leg flexed to a right
angle. The person abducts the thigh against resistance. The gluteus
medius can be palpated inferior to the iliac crest, posterior to the
tensor of the fascia lata, which is also contracting during abduction
of the thigh.
The tensor and the superficial and anterior part of the gluteus maximus
share a common distal attachment to the anterolateral tibial condyle
via the iliotibial tract, which acts as
a long aponeurosis for the muscles. However, unlike the gluteus
maximus, the tensor is served by the superior gluteal neurovascular
bundle. Despite its gluteal innervation and shared attachment, the
tensor of the fascia lata is primarily a flexor of the thigh because of
its anterior location; however, it generally does not act
independently. To produce flexion, the tensor of the fascia lata acts
in concert with the iliopsoas and rectus femoris. When the iliopsoas is
paralyzed, the tensor of the fascia lata undergoes hypertrophy in an
attempt to compensate. It also works in conjunction with other
abductor/medial rotator muscles (gluteus medius and minimus) (Fig. 5.26). It lies too far anteriorly to be a strong abductor and thus probably contributes primarily as a synergist or fixator.
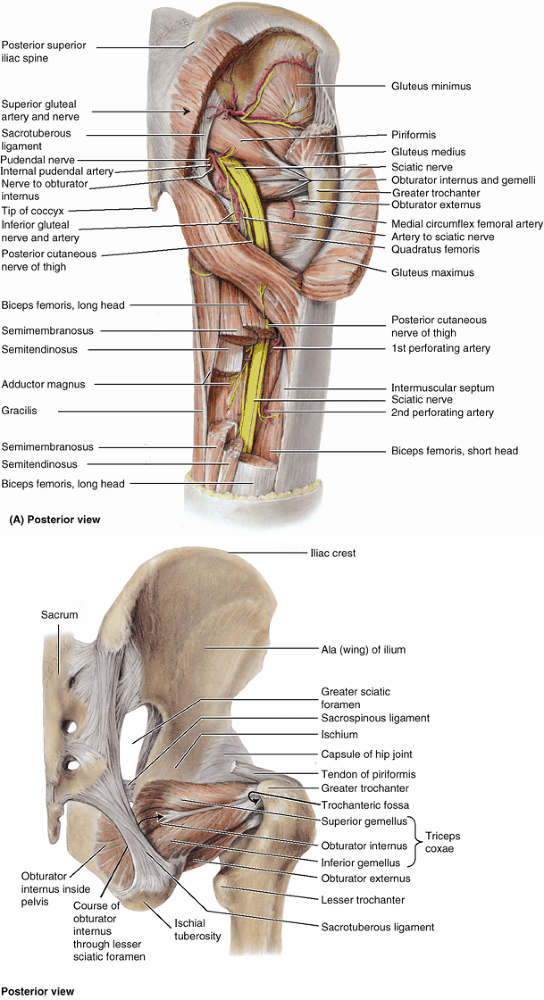 |
|
Figure 5.24. Dissection of gluteal region and abductors and rotators of thigh. A.
In this deep dissection, the neurovascular structures of the gluteal region and proximal posterior thigh are revealed. Most of the gluteus maximus and medius are removed, and segments of the hamstrings are excised. Except for the superior gluteal artery and nerve, the neurovascular structures supplying or traversing the gluteal region and posterior thigh emerge from the pelvis via the greater sciatic foramen inferior to the piriformis; however, exceptions occur (Fig. 5.28). The sciatic nerve runs deep (anterior) to and is protected by the overlying gluteus maximus initially and then the biceps femoris. B. This dissection shows some of the lateral rotators of the thigh: the piriformis (distal tendinous attachment only), the external and internal obturators (arising from opposite sides of the obturator membrane), and the gemelli muscles. Note that the components of the triceps coxae share a common attachment—adjacent to that of the obturator externus—into the trochanteric fossa. |
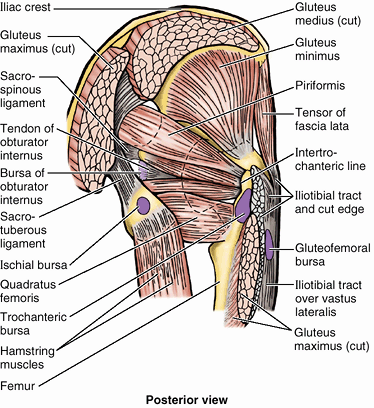 |
|
Figure 5.25. Gluteal muscles and bursae.
Three bursae (trochanteric, gluteofemoral, and ischial) usually separate the gluteus maximus from underlying bony prominences, allowing free muscular contraction or tendon movement. The bursa of the obturator internus allows the tendon of the obturator internus to glide freely over the lesser sciatic notch of the hip bone, which the muscle uses as a trochlea (pulley), changing its direction of pull by more than 90° before the gemelli muscles become attached to it. |
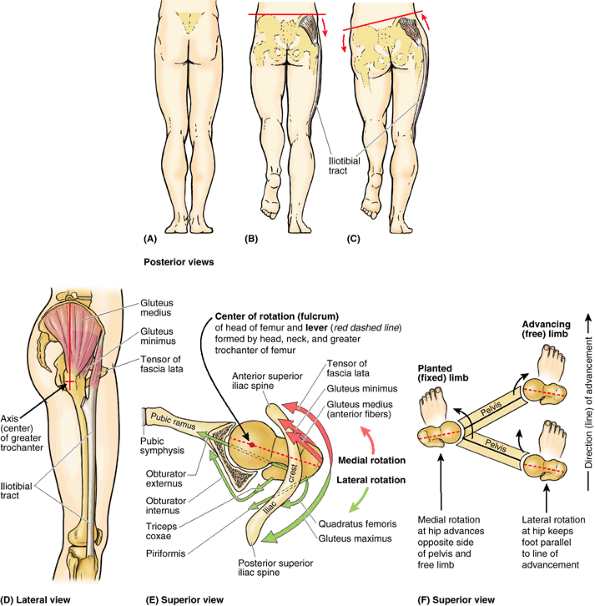 |
|
Figure 5.26. Action of abductors/medial rotators of thigh when walking. A–C.
The role of the abductors (gluteus medius and minimus, tensor of fascia lata) is demonstrated. When the weight is on both feet (A), the pelvis is evenly supported and does not sag. When the weight is borne by one limb (B), the muscles on the supported side fix the pelvis so that it does not sag to the unsupported side. Keeping the pelvis level enables the non-weight-bearing limb to clear the ground as it is brought forward during the swing phase. When the right abductors are paralyzed (C), owing to a lesion of the right superior gluteal nerve, fixation by these muscles is lost and the pelvis tilts to the unsupported left side (positive Trendelenburg sign). The net effect is that the limb becomes “too long” for the hip height, requiring a compensatory limp to prevent the foot from hitting the ground during swing phase. D–F. The role of the rotators of the thigh is demonstrated. In the lateral (D) and superior (E) views, note that most abductors—the tensor of the fascia lata, gluteus minimus, and most (the anterior fibers) of the gluteus medius—lie anterior to the lever provided by the axis of the head, neck, and greater trochanter of the femur to rotate the thigh around the vertical axis traversing the femoral head. The superior view of the right hip joint (E) includes the superior pubic ramus, acetabulum, and iliac crest; the inferior part of the ilium has been removed to reveal the head and neck of the femur. The lines of pull of the rotators of the hip are indicated by arrows, demonstrating the antagonistic relationship resulting from their positions relative to the lever and the center of rotation (fulcrum). The medial rotators pull the greater trochanter anteriorly and the lateral rotators pull the trochanter posteriorly, resulting in rotation of the thigh around the vertical axis. Note that all of these muscles also pull the head and neck of the femur medially into the acetabulum, strengthening the joint. In walking (F), the same muscles that act unilaterally during the stance phase (planted limb) to keep the pelvis level via abduction can simultaneously produce medial rotation at the hip joint, advancing the opposite unsupported side of the pelvis (augmenting advancement of the free limb). The lateral rotators of the advancing (free) limb act during the swing phase to keep the foot parallel to the direction (line) of advancement. |
lata and iliotibial tract, thereby helping support the femur on the
tibia when standing. Because the iliotibial tract is attached to the
femur via the lateral intermuscular septum, the tensor produces little
if any movement of the leg (Fig. 5.23D).
However, when the knee is fully extended, it contributes to (increases)
the extending force, adding stability. When the knee is flexed by other
muscles, the tensor can synergistically augment flexion and lateral
rotation of the leg.
essential role during locomotion, advancing and preventing the sagging
of the unsupported side of the pelvis during walking, as illustrated
and explained in Figure 5.26. The supportive and action-producing functions of the abductors/medial rotators depends on normal:
-
Muscular activity and innervation from the superior gluteal nerve.
-
Articulation of the hip joint components.
-
Strength and angulation of the femoral neck.
almost filling it, to reach its attachment to the superior border of
the greater trochanter. Because of its key position in the buttock, the
piriformis is the landmark of the gluteal region. The piriformis
provides the key to understanding relationships in the gluteal region
because it determines the names of the blood vessels and nerves:
-
The superior gluteal vessels and nerve emerge superior to it.
-
The inferior gluteal vessels and nerve emerge inferior to it.
-
The surface marking of the superior
border of the piriformis is indicated by a line joining the skin dimple
formed by the posterior superior iliac spine to the superior border of
the greater trochanter of the femur (Fig. SA5.2G).
becomes tendinous, and receives the distal attachments of the gemelli
before attaching to the medial surface of the greater trochanter
(trochanteric fossa). The small gemelli are narrow, triangular
extrapelvic reinforcements of the obturator internus. Although the
inferior gemellus receives separate innervation from the nerve to the
quadratus femoris, it is more realistic to consider these three muscles
as a unit (i.e., as the triceps coxae) because they are incapable of
independent action. The bursa of the obturator internus
allows free movement of the muscle over the posterior border of the
ischium, where the border forms the lesser sciatic notch and the
trochlea over which the tendon glides as it turns (Fig. 5.25).
the superior ends of the adductor muscles) and its innervation
(obturator nerve), the obturator externus was described earlier in this
chapter with the medial thigh muscles (Table 5.4).
However, it functions as a lateral rotator of the thigh, and its distal
attachment is visible only during dissection of the gluteal region (Fig. 5.24B)
or hip joint. Thus it is mentioned again in this context. It lies deep
in the proximal thigh, with its tendon passing deep to the quadratus
femoris on the way to its attachment to the trochanteric fossa of the
femur (Fig. 5.24A). The obturator externus, with other short muscles around the hip joint, stabilizes the head of the femur in the acetabulum (Fig. 5.26E). It is most effective as a lateral rotator of the thigh when the hip joint is flexed.
the relatively transverse lever formed by the proximal femur allows
superior placement of the abductors of the thigh and provides
mechanical advantage for the deeper medial and lateral rotators of the
thigh. This is critical for bipedal locomotion. Thus, despite their
designations, the abductors/medial rotators (the superficial gluteal
muscles) are most active during the stance phase when they
simultaneously elevate and advance the contralateral unsupported side
of the pelvis during ambulation. The lateral rotators (deep gluteal
muscles) of the unsupported side rotate the free limb during the swing
phase so that the foot remains parallel to the line of advancement.
(e.g., as from cycling, rowing, or other activities involving
repetitive hip extension while seated) may overwhelm the ischial
bursa’s ability to dissipate applied stress. The recurrent trauma
results in inflammation of the bursa (ischial bursitis). Ischial bursitis is a friction bursitis
resulting from excessive friction between the ischial bursae and the
ischial tuberosities. Localized pain occurs over the bursa, and the
pain increases with movement of the gluteus maximus. Calcification may
occur in the bursa with chronic bursitis. Because the ischial
tuberosities bear the body weight during sitting, these pressure points
may lead to pressure sores in debilitated people, particularly paraplegic persons with poor nursing care.
may result from repetitive actions such as climbing stairs while
carrying heavy objects or running on a steeply elevated treadmill.
These movements involve the gluteus maximus and move the superior
tendinous fibers repeatedly back and forth over the bursae of the
greater trochanter. Trochanteric bursitis causes deep diffuse pain in
the lateral thigh region. This type of friction bursitis
is characterized by point tenderness over the great trochanter;
however, the pain radiates along the iliotibial tract that extends from
the iliac tubercle to the tibia (Figs. 5.23C and 5.26D).
This thickening of the fascia lata receives tendinous reinforcements
from the tensor of the fascia lata and the gluteus maximus. The pain
from an inflamed trochanteric bursa, usually localized just posterior
to the greater trochanter, is generally elicited by manually resisting
abduction and lateral rotation of the thigh while the person is lying
on the unaffected side.
-
Proximal attachment to the ischial tuberosity deep to the gluteus maximus.
-
Spanning and acting on two joints: extension at the hip joint and flexion at the knee.
-
Innervation by the tibial division of the sciatic nerve.
but the short head of the biceps, the fourth muscle of the posterior
compartment, fails to meet any of them. The hamstrings received their
name because it is common to tie hams (pork thighs) up for curing
and/or smoking with a hook around these muscle tendons. This also
explains the expression “hamstringing the enemy” by slashing these
tendons lateral and medial to the knees.
maximally at the same time: full flexion of the knee requires so much
shortening of the hamstrings that they cannot provide the additional
contraction that would be necessary for simultaneous full extension of
the thigh; similarly, full extension of the hip shortens the hamstrings
so they cannot further contract to act fully on the knee. When the
thighs and legs are fixed, the hamstrings can help extend the trunk at
the hip joint. They are active in thigh extension under all situations
except full flexion of the knee, including maintenance of the relaxed
standing posture (standing at ease). A person with paralyzed hamstrings
tends to fall forward because the gluteus maximus muscles cannot
maintain the necessary muscle tone to stand straight.
on flat ground, when the gluteus maximus demonstrates minimal activity.
However, rather than producing either hip extension or knee flexion per
se during normal walking, the hamstrings demonstrate most activity when
they are eccentrically contracting, resisting (decelerating) hip
flexion and knee extension during terminal swing (between midswing and
heel strike) (Table 5.2).
a matter of conditioning. In some people, they are not long enough to
allow them to touch their toes when the knees are extended. Routine
stretch exercise can lengthen these muscles and tendons.
person flexes the leg against resistance. Normally, these
muscles—especially their tendons on each side of the popliteal
fossa—should be prominent as they bend the knee.
muscle is semitendinous. This muscle has a fusiform belly that is
usually interrupted by a tendinous intersection and a long, cord-like
tendon that begins approximately two thirds of the way down the thigh.
Distally, the tendon attaches to the medial surface of the superior
part of the tibia as part of the pes anserinus
formation in conjunction with the tendinous insertions of the sartorius and gracilis (discussed earlier in this chapter).
|
Table 5.7. Muscles of the Posterior Thigh: Extensors of the Hip, Flexors of the Knee
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||
broad muscle that is also aptly named because of the flattened
membranous form of its proximal attachment to the ischial tuberosity (Fig. 5.27A).
The tendon of the semimembranosus forms around the middle of the thigh
and descends to the posterior part of the medial tibial condyle. Its
tendon divides distally into three parts: (1) a direct attachment to
the posterior aspect of the medial tibial condyle, (2) a part that
blends with the popliteal fascia, and (3) a reflected part that
reinforces the intercondylar part of the joint capsule of the knee as
the oblique popliteal ligament (Figs. 5.23B and 5.60).
medial hamstrings or “semi-” muscles (semitendinosus and
semimembranosus) pass to the medial side of the tibia; in this
position, contraction of the medial hamstrings (and of synergists
including the gracilis, sartorius, and popliteus) produces a limited
amount (about 10°) of medial rotation of the tibia at the knee. The two
medial hamstrings are not as active as the lateral hamstring, the
biceps femoris, which is the “workhorse” of extension at the hip (Hamill and Knutzen, 1995).
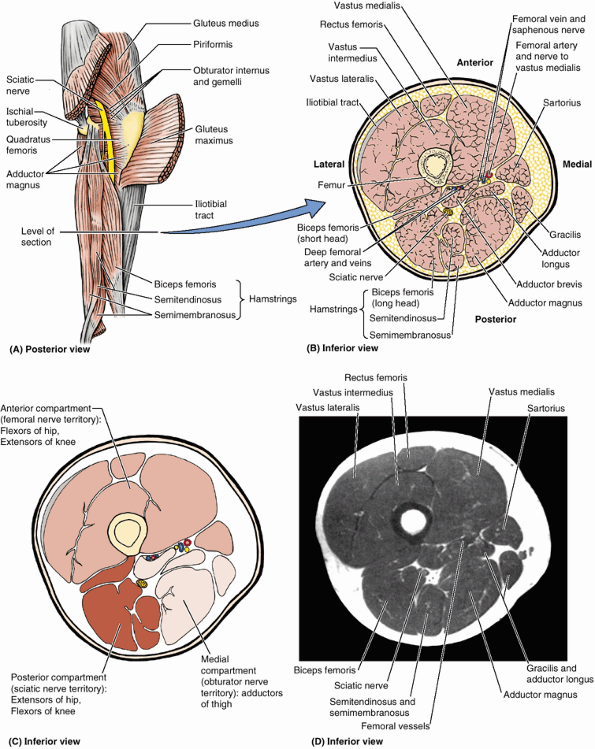 |
|
Figure 5.27. Muscles and fascial compartments of thigh. A.
The gluteus maximus has been reflected to reveal the sciatic nerve entering the proximal thigh and the attachments of the hamstrings. The level of the sections shown in parts B and C is indicated. B. An anatomical transverse section through the middle thigh, 10–15 cm inferior to the inguinal ligament. C. The three compartments of the thigh are shown. Note that each has its own nerve supply and functional group(s) of muscles. D. This transverse MRI of the right thigh indicates the muscles of each compartment. (Courtesy of Dr. W. Kucharczyk, Chair of Medical Imaging, Faculty of Medicine, University of Toronto and Clinical Director of the Tri-Hospital Resonance Centre, Toronto, Ontario, Canada.) |
In the inferior part of the thigh, the long head becomes tendinous and
is joined by the short head. The rounded common tendon attaches to the
head of the fibula and can easily be seen and felt as it passes the
knee, especially when the knee is flexed against resistance (see “Surface Anatomy of the Gluteal Region and Thigh,” in this chapter). The long head of the biceps femoris
crosses and provides protection for the sciatic nerve after it descends
from the gluteal region into the posterior aspect of the thigh (Fig. 5.27).
When the sciatic nerve divides into its terminal branches, the lateral
branch (common fibular nerve) continues this relationship, running with
the biceps tendon.
arises from the lateral lip of the inferior third of the linea aspera
and supracondylar ridge of the femur. Whereas the hamstrings have a
common nerve supply from the tibial division of the sciatic nerve, the
short head of the biceps is innervated by the fibular division (Table 5.7).
Because each of the two heads of the biceps femoris has a different
nerve supply, a wound in the posterior thigh with nerve injury may
paralyze one head and not the other.
lateral hamstring (biceps) as well as the iliotibial tract pass to the
lateral side of the tibia. In this position, contraction of the biceps
and tensor of the fascia lata produces about 40° lateral rotation of
the tibia at the knee. Rotation of the flexed knee is especially
important in snow skiing.
the gluteus maximus, the hamstrings are the main extensors of the hip
used in normal walking. They are two-joint muscles, and their
concentric contraction produces either extension of the hip or flexion
of the knee. However, in walking they are most active in eccentrically
contracting to decelerate hip flexion and knee extension during
terminal swing. The hamstrings also rotate the flexed knee. If
resistance to hip extension is increased, or more vigorous extension is
required, the gluteus maximus is called into action.
and/or torn hamstrings) are common in individuals who run and/or kick
hard (e.g., in running, jumping, and quick-start sports such as
baseball, basketball, football, and soccer). The violent muscular
exertion required to excel in these sports may tear part of the
proximal tendinous attachments of the hamstrings to the ischial
tuberosity. Hamstring strains are twice as common as quadriceps strains
(Levandowski and Difiori, 1994).
tearing of muscle fibers, resulting in rupture of the blood vessels
supplying the muscles. The resultant hematoma
is contained by the dense stocking-like fascia lata. Tearing of
hamstring fibers is often so painful when the athlete moves or
stretches the leg that he or she falls and writhes in pain. These
injuries often result from inadequate warming up before practice or
competition. Avulsion of the ischial tuberosity (see clinical correlation [blue] box “Injuries of the Hip Bone (Pelvic Injuries),”
in this chapter) at the proximal attachment of the biceps femoris and
semitendinosus (“hurdler’s injury”) may result from forcible flexion of
the hip with the knee extended (e.g., kicking a football).
and either supply the gluteal region (e.g., superior and inferior
gluteal nerves) or pass through it to supply the perineum and thigh
(e.g., the pudendal and sciatic nerves, respectively). Table 5.8 describes the origin, course, and distribution of the nerves of the gluteal region and posterior thigh.
buttocks). These superficial nerves supply the skin over the iliac
crest, between the posterior superior iliac spines and over the iliac
tubercles. Consequently, these nerves are vulnerable to injury when
bone is taken from the ilium for grafting.
gluteal nerves, sciatic nerve, nerve to quadratus femoris, posterior
cutaneous nerve of the thigh, nerve to obturator internus, and pudendal
nerve (Fig. 5.24A; Table 5.8,
figure). All of these nerves are branches of the sacral plexus and
leave the pelvis through the greater sciatic foramen. Except for the
superior gluteal nerve, they all emerge inferior to the piriformis.
runs laterally between the gluteus medius and minimus with the deep
branch of the superior gluteal artery. It divides into a superior
branch that supplies the gluteus medius and an inferior branch that
continues to pass between the gluteus medius and the gluteus minimus to
supply both muscles and the tensor of the fascia lata.
leaves the pelvis through the greater sciatic foramen, inferior to the
piriformis and superficial to the sciatic nerve, accompanied by
multiple branches of the inferior gluteal artery and vein. It
also divides into several branches, which provide motor innervation to the overlying gluteus maximus.
|
Table 5.8. Nerves of Gluteal Region and Posterior Thigh
|
||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||
largest nerve in the body and is the continuation of the main part of
the sacral plexus. The rami converge at the inferior border of the
piriformis to form the sciatic nerve, a thick, flattened band
approximately 2 cm wide. The sciatic nerve is the most lateral
structure emerging through the greater sciatic foramen inferior to the
piriformis. Medial to it are the inferior gluteal nerve and vessels,
the internal pudendal vessels, and the pudendal nerve. The sciatic
nerve runs inferolaterally under cover of the gluteus maximus, midway
between the greater trochanter and ischial tuberosity. The nerve rests
on the ischium and then passes posterior to the obturator internus,
quadratus femoris, and adductor magnus muscles. The sciatic nerve is so
large that it receives a named branch of the inferior gluteal artery,
the artery to the sciatic nerve (L. arteria comitans nervi ischiadici).
region. It supplies the posterior thigh muscles, all leg and foot
muscles, and the skin of most of the leg and the foot. It also supplies
the articular branches to all joints of the lower limb.
derived from posterior (postaxial) divisions of the anterior rami,
which are loosely bound together in the same connective tissue sheath (Fig. 5.28A). Perone is Greek for the fibula;
because of the close relationship of the nerve to the fibular neck, its
name has been changed internationally from common peroneal to common
fibular. The tibial and common fibular nerves usually separate
approximately halfway or more down the thigh (Fig. 5.33); however, in approximately 12% of people, the nerves separate as they leave the pelvis (Fig. 5.28B).
In these cases, the tibial nerve passes inferior to the piriformis, and
the common fibular nerve pierces this muscle or passes superior to it (Fig. 5.28C).
leaves the pelvis anterior to the sciatic nerve and obturator internus
and passes over the posterior surface of the hip joint. It supplies an
articular branch to this joint and innervates the inferior gemellus and
quadratus femoris.
supplies more skin than any other cutaneous nerve. Its fibers from the
anterior divisions of S2 and S3 supply the skin of the perineum. Some
of the fibers from the posterior divisions of the anterior rami of S1
and S2 supply the skin of the inferior part of the buttock (via the
inferior clunial nerves); others continue inferiorly in branches that
supply the skin of the posterior thigh and proximal part of the leg.
Unlike most nerves bearing the name cutaneous,
the main part of this nerve lies deep to the deep fascia (fascia lata),
with only its terminal branches penetrating the subcutaneous tissue for
distribution to the skin.
most medial structure to exit the pelvis through the greater sciatic
foramen inferior to the piriformis muscle. It descends posterolateral
to the sacrospinous ligament and enters the perineum through the lesser
sciatic foramen to supply structures in the perineum (see Chapter 3); it supplies no structures in the gluteal region or posterior thigh.
arises from the anterior divisions of the anterior rami of the L5–S2
nerves and parallels the course of the pudendal nerve. As it passes
around the base of the ischial spine, it supplies the superior
gemellus. After entering the perineum via the lesser sciatic foramen,
it supplies the obturator internus muscle.
a compensatory list of the body to the weakened gluteal side. This
compensation places the center of gravity over the supporting lower
limb. Medial rotation of the thigh is also severely impaired. When a
person is asked to stand on one leg, the gluteus medius and minimus
normally contract as soon as the contralateral foot leaves the floor,
preventing tipping of the pelvis to the unsupported side (Fig. B5.12A).
When a person who has suffered a lesion of the superior gluteal nerve
is asked to stand on one leg, the pelvis on the unsupported side
descends (Fig. B5.12B),
indicating that the gluteus medius and minimus on the supported side
are weak or non-functional. This observation is referred to clinically
as a positive Trendelenburg test. Other causes of this sign include fracture of the greater trochanter (the distal attachment of gluteus medius) and dislocation of the hip joint.
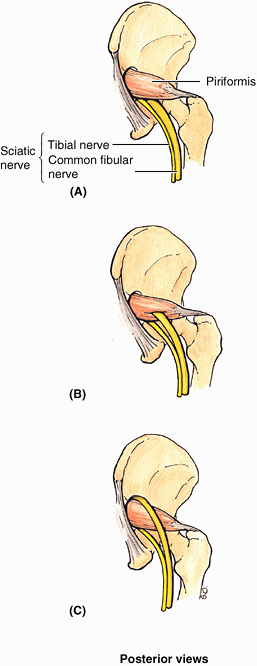 |
|
Figure 5.28. Relationship of sciatic nerve to piriformis. A. The sciatic nerve usually emerges from the greater sciatic foramen inferior to the piriformis. B.
In 12.2% of 640 limbs studied, the sciatic nerve divided before exiting the greater sciatic foramen, the common fibular division (yellow) passed through the piriformis. C. In 0.5% of cases, the common fibular division passed superior to the muscle, where it is especially vulnerable to injury during intragluteal injections. |
lower limb becomes, in effect, too long and does not clear the ground
when the foot is brought forward in the swing phase of walking. To
compensate, the individual leans away from the unsupported side,
raising the pelvis to allow adequate room for the foot to clear the
ground as it swings forward. This results in a characteristic
“waddling” or gluteal gait. Other ways to compensate is to lift the
foot higher as it is brought forward, resulting in the so-called
steppage gait, or to swing the foot outward (laterally), the so-called
swing-out gait. These same gaits are adopted to compensate for the footdrop that results from common fibular nerve paralysis (see clinical correlation [blue] box “Injury to the Common Fibular Nerve and Footdrop,” in this chapter), which also makes the limb too long.
by the injection of an anesthetic agent a few centimeters inferior to
the midpoint of the line joining the PSIS and the superior border of
the greater trochanter. Paresthesia radiates to the foot because of
anesthesia of the plantar nerves, which are terminal branches of the
tibial nerve derived from the sciatic nerve.
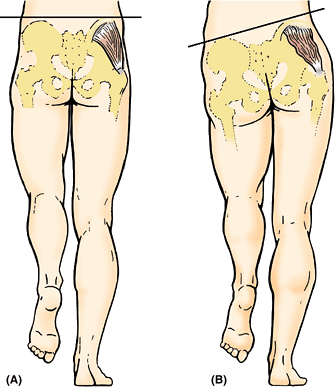 |
|
Figure B5.12
|
Individuals involved in sports that require excessive use of the
gluteal muscles (e.g., ice skaters, cyclists, and rock climbers) and
women are more likely to develop this syndrome. In approximately 50% of
cases, the case histories indicate trauma to the buttock associated
with hypertrophy and spasm of the piriformis. In the approximately 12% of people in whom the common fibular division of the sciatic nerve passes through the piriformis (Fig. 5.28B), this muscle may compress the nerve.
is uncommon. When this occurs, the leg is useless because extension of
the hip is impaired, as is flexion of the leg. All ankle and foot
movements are also lost. Incomplete section of the sciatic nerve
(e.g., from stab wounds) may also involve the inferior gluteal and/or
the posterior femoral cutaneous nerves. Recovery from a sciatic lesion
is slow and usually incomplete.
side of safety (its lateral side) and a side of danger (its medial
side). Wounds or surgery on the medial side of the buttock are liable
to injure the sciatic nerve and its branches to the hamstrings
(semitendinosus, semimembranosus, and biceps femoris) on the posterior
aspect of the thigh. Paralysis of these muscles results in impairment
of thigh extension and leg flexion.
penetrate the skin, fascia, and muscles. The gluteal region is a
favorable injection site because the muscles are thick and large;
consequently, they provide a substantial volume for absorption of
injected substances by intramuscular veins. It is important to be aware
of the extent of the gluteal region and the safe region for giving
injections. Some people restrict the area of the buttock to the most
prominent part, which may be dangerous because the sciatic nerve lies
deep to this area (Fig. B5.13A).
superolateral quadrant of the buttock or superior to a line extending
from the PSIS to the superior border of the greater trochanter
(approximating the superior border of the gluteus maximus).
Intramuscular injections can also be given safely into the
anterolateral part of the thigh, where the needle enters the tensor of
the fascia lata (Fig. 5.23C)
as it extends distally from the iliac crest and ASIS. The index finger
is placed on the ASIS, and the fingers are spread posteriorly along the
iliac crest until the tubercle of the crest is felt by the middle
finger (Fig. B5.13B).
An intragluteal injection can be made safely in the triangular area
between the fingers (just anterior to the proximal joint of the middle
finger) because it is superior to the sciatic nerve. Complications of
improper technique include nerve injury, hematoma, and abscess
formation.
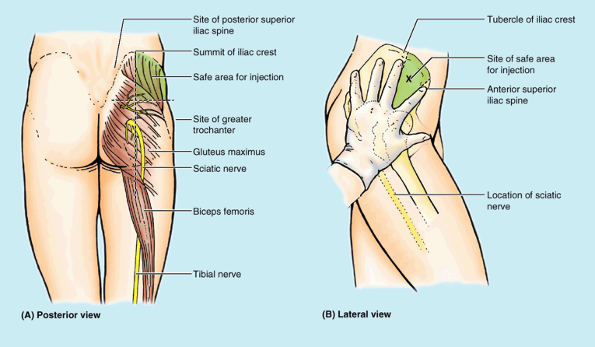 |
|
Figure B5.13.
|
sciatic foramen) by which derivatives of the sacral plexus exit the
bony pelvis, the gluteal region includes a disproportionate number of
nerves of all sizes, both motor and sensory. Fortunately, most are
placed in the inferomedial quadrant; thus properly administered
intramuscular injections avoid these structures. Because the sciatic
nerve includes fibers from the L4–S3 spinal nerves, it is affected by
the most common nerve compression syndromes (e.g., radiculopathies of
the L4 and L5 spinal nerve roots; see Chapter 4).
Even though occurring outside the lower limb per se, these syndromes
result in sciatica—pain that radiates down the lower limb along the
course of the nerve and its terminal branches. Pain experienced in the
lower limb may not necessarily arise from a problem in the limb!
The major branches of the internal iliac artery that supply or traverse
the gluteal region are the (1) superior gluteal artery, (2) inferior
gluteal artery, and (3) internal pudendal artery. After birth, the
posterior compartment of the thigh has no major artery exclusive to the
compartment; it receives blood from multiple sources: inferior gluteal,
medial circumflex femoral, perforating, and popliteal arteries.
is the largest branch of the internal iliac artery and passes
posteriorly between the lumbosacral trunk and the S1 nerve. The
superior gluteal artery leaves the pelvis through the greater sciatic
foramen, superior to the piriformis, and divides immediately into
superficial and deep branches. The superficial branch supplies the gluteus maximus and skin over the proximal attachment of this muscle; the deep branch
supplies the gluteus medius, gluteus minimus, and tensor of the fascia
lata. The superior gluteal artery anastomoses with the inferior gluteal
and medial circumflex femoral arteries.
arises from the internal iliac artery and passes posteriorly through
the parietal pelvic fascia, between the S1 and the S2 (or S2 and S3)
nerves. The inferior gluteal artery leaves the pelvis through the
greater sciatic foramen, inferior to the piriformis. It enters the
gluteal region deep to the gluteus maximus and descends medial to the
sciatic nerve.
maximus, obturator internus, quadratus femoris, and superior parts of
the hamstrings. It anastomoses with the superior gluteal artery and
frequently participates in the cruciate anastomosis of the thigh,
involving the first perforating arteries of the deep artery of the
thigh and the medial and lateral circumflex femoral arteries (Table 5.5).
Whether the cruciate anastomosis is formed or not, these vessels all
participate in supplying the structures of the proximal posterior thigh.
major artery of the posterior compartment, traversing its length and
becoming continuous with the popliteal artery. This part of the artery
diminishes, however, persisting postnatally as the artery to the sciatic nerve.
arises from the internal iliac artery and lies anterior to the inferior
gluteal artery. Its course parallels that of the pudendal nerve,
entering the gluteal region through the greater sciatic foramen
inferior to the piriformis. The internal pudendal artery leaves the
gluteal region immediately by crossing the ischial spine/sacrospinous
ligament and enters the perineum through the lesser sciatic foramen.
Like the pudendal nerve, it supplies the skin, external genitalia, and
muscles in the perineal region. It does not supply any structures in
the gluteal region or posterior thigh.
three arising in the anterior compartment and the fourth being the
terminal branch of the deep artery itself. The perforating arteries are
large vessels, unusual in the limbs for their transverse,
intercompartmental course. Surgeons operating in the posterior
compartment are careful to identify them to avoid inadvertent injury.
They perforate the aponeurotic portion of the distal attachment of the
adductor magnus to enter the posterior compartment. Within the
posterior compartment, they typically give rise to muscular branches to
the hamstrings and anastomotic branches that ascend or descend to unite
with those arising superiorly or inferiorly from the other perforating
arteries or the inferior gluteal and popliteal artery. A continuous
anastomotic chain thus extends from the gluteal to popliteal regions,
which gives rise to additional branches to muscles and to the sciatic
nerve. After giving off their posterior compartment branches, the
perforating arteries pierce the lateral intermuscular septum to enter
the anterior compartment, where they supply the vastus lateralis muscle.
|
Table 5.9. Arteries of the Gluteal Region and Posterior Thigh
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||
accompany the corresponding arteries through the greater sciatic
foramen, superior and inferior to the piriformis, respectively (Fig. 5.29A).
They communicate with tributaries of the femoral vein, thereby
providing alternate routes for the return of blood from the lower limb
if the femoral vein is occluded or has to be ligated. The internal pudendal veins
accompany the internal pudendal arteries and join to form a single vein
that enters the internal iliac vein. These veins drain blood from the
external genitalia or pudendum (L. pudere, to be ashamed). Perforating veins accompany the arteries of the same name to drain blood from the posterior compartment of the thigh into the deep vein of the thigh.
The perforating veins, like the arteries, usually also communicate
inferiorly with the popliteal vein and superiorly with the inferior
gluteal vein.
aortic lumbar (caval/lymph) nodes.
which also receive lymph from the thigh. All the superficial inguinal
nodes send efferent lymphatic vessels to the external iliac lymph nodes.
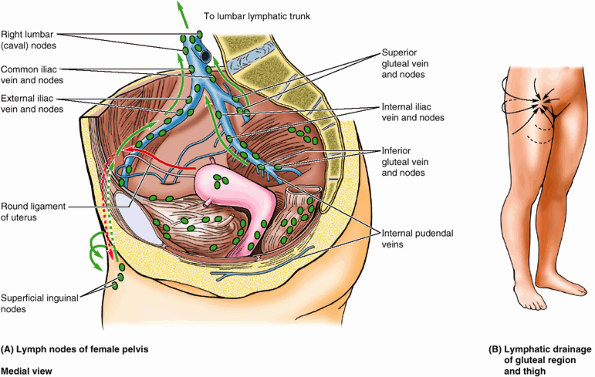 |
|
Figure 5.29. Lymphatic drainage of gluteal region and thigh. A.
Lymph from the deep tissues of the gluteal region enters the pelvis along the gluteal veins, draining to the superior and inferior gluteal lymph nodes; from them, it passes to the iliac and lateral lumbar (caval/aortic) lymph nodes. B. Lymph from superficial tissues of the gluteal region passes initially to the superficial inguinal nodes, which also receive lymph from the thigh. Lymph from all the superficial inguinal nodes passes via efferent lymph vessels to the external and common iliac and right and left lumbar (caval/aortic) lymph nodes, draining via lumbar lymphatic trunks to the chyle cistern. |
proximal part of the posterior compartment of the thigh are branches
and tributaries of the internal iliac artery and vein that pass to and
from the region via the greater sciatic foramen. All but the superior
gluteal vessels exit the foramen inferior to the piriformis muscle.
Although the pudendal vessels follow the same route, they traverse the
gluteal region only briefly en route to and from the perineum via the
lesser sciatic foramen. The posterior compartment of the thigh does not
have a major artery coursing through it with primary responsibility for
the compartment. Rather, branches are sent from several arteries in
other compartments to supply it.
whole, the majority of the arterial blood coming to the limb and most
of the venous blood and lymph exiting from it pass along the more
protected anteromedial aspect of the limb. Flexor aspects are generally
better protected than are extensor aspects, the latter being exposed
and therefore vulnerable in the flexed, defensive position.
course, especially in men, whereas the skin of the thigh is relatively
thin and loosely attached to the underlying subcutaneous tissue. A line
joining the highest points of the iliac crests (Fig. SA5.2A) crosses the L4–L5 intervertebral (IV) disc and is a useful landmark when a lumbar puncture is performed (see Chapter 4), indicating the middle of the lumbar cistern (Fig. SA5.2A–D). The intergluteal cleft,
beginning inferior to the apex of the sacrum, is the deep groove
between the buttocks. It extends as far superiorly as the S3 or S4
segment. The coccyx is palpable in the superior part of the
intergluteal cleft. The posterior superior iliac spines
are located at the posterior extremities of the iliac crests and may be
difficult to palpate; however, their position can always be located at
the bottom of the permanent skin dimples approximately 3.75 cm from
midline (Fig. SA5.2B).
A line joining these dimples, often more visible in women than in men,
passes through the S2 spinous process, indicating the level of the
lowest limit of the dural sac or lumbar cistern, the middle of the
sacroiliac joints, and the bifurcation of the common iliac arteries.
|
Figure SA5.2
|
covering most structures in the gluteal region can be felt to contract
when straightening up from bending over. The inferior edge of this
large muscle is located just superior to the gluteal fold, which contains a variable amount of subcutaneous fat (Fig. SA5.2A & C).
The gluteal fold disappears when the hip joint is flexed. The degree of
prominence of the gluteal fold changes in certain abnormal conditions,
such as atrophy of the gluteus maximus. An imaginary line drawn from
the coccyx to the ischial tuberosity indicates the inferior edge of the
gluteus maximus (Fig. SA5.2B).
Another line drawn from the PSIS to a point slightly superior to the
greater trochanter indicates the superior edge of this muscle.
is covered by the inferior part of the gluteus maximus; however, the
tuberosity is easy to palpate when the thigh is flexed because the
gluteus maximus slips superiorly off the tuberosity, which is then
subcutaneous. Feel the ischial tuberosity as you bend to sit. The
superior part of the gluteus medius can be palpated between the superior part of the gluteus maximus and the iliac crest (Fig. SA5.2E & F).
The gluteus medius of one buttock can be felt when all the body weight
shifts onto the ipsilateral limb (the one on the same side).
most lateral bony point in the gluteal region, may be felt on the
lateral aspect of the hip, especially its inferior part (Fig. SA5.2A–C).
It is easier to palpate when you passively abduct your lower limb to
relax the gluteus medius and minimus. The top of the trochanter lies
approximately a hand’s breadth inferior to the tubercle of the iliac
crest. The prominence of the trochanter increases when a dislocated hip
causes atrophy of the gluteal muscles and displacement of the
trochanter. A line drawn from the ASIS to the ischial tuberosity (Nélaton line), passing over the lateral aspect of the hip region, normally passes over or near the top of the greater trochanter (Fig. SA5.2D). The trochanter can be felt superior to this line in a person with a dislocated hip or a fractured femoral neck. The lesser trochanter is palpable with difficulty from the posterior aspect when the thigh is extended and rotated medially.
important structure inferior to the piriformis, is represented by a
line that extends from a point midway between the greater trochanter
and the ischial tuberosity (Fig. SA5.2G) down the middle of the posterior aspect of the thigh (Fig. SA5.2H).
The level of the bifurcation of the sciatic nerve into the tibial and
common fibular nerves varies. The separation usually occurs in the
inferior third of the thigh, but the division of the sciatic nerve may
occur as it passes through the sciatic foramen. The tibial nerve bisects the popliteal fossa, and the common fibular nerve
follows the biceps femoris, which covers it. The sciatic nerve
stretches when the thigh is flexed and the knee is extended, and it
relaxes when the thigh is extended and the knee is flexed.
as a group as they arise from the ischial tuberosity and extend along
the lateral and posterior aspects of the thigh (Fig. SA5.2E). The iliotibial tract,
the fibrous band that reinforces the fascia lata laterally, can be
observed on the lateral aspect of the thigh as it passes to the lateral tibial condyle.
While sitting down with your lower limb extended, raise your heel off
the floor and feel the anterior border of the iliotibial tract passing
a finger’s breadth posterior to the lateral border of the patella (Fig. SA5.2E & F). Note that the iliotibial tract is prominent and taut when the heel is raised and indistinct when the heel is lowered. The tendons of the hamstrings can be observed and palpated at the borders of the popliteal fossa (Fig. SA5.2I & J). The biceps femoris tendon
is on the lateral side of the fossa. The most lateral tendon on the
medial side when the knee is flexed against resistance is the semimembranosus tendon.
While sitting on a chair with your knee flexed, press your heel against
the leg of the chair and feel your biceps femoris tendon laterally and
trace it to the head of the fibula. Also feel the narrow and more
prominent semitendinosus tendon medially, which pulls away from the semimembranosus tendon that attaches to the superomedial part of the tibia.
may be easily observed as a ridge passing down the thigh when the lower
limb is raised from the floor while sitting. Observe the large bulges
formed by the vastus lateralis and medialis at the knee (Fig. SA5.2J). The patellar ligament
is easily observed, especially in thin people, as a thick band running
from the patella to the tibial tuberosity. You can also palpate the infrapatellar fat pads, the masses of loose fatty tissue on each side of the patellar ligament.
shortening (e.g., resulting from a femoral fracture). To make such
measurements, compare the affected limb with the corresponding limb.
Real limb shortening is detected by comparing the measurements from the
ASIS to the distal tip of the medial malleolus on both sides. To
determine if the shortening is in the thigh, the measurement is taken
from the top of the ASIS to the distal edge of the lateral femoral
condyle on both sides. Keep in mind that small differences between the
two sides—such as a difference of 1.25 cm in total length of the
limb—may be normal.
Approximately 3.75 cm along this line distal to the inguinal ligament,
the deep artery of the thigh arises from the femoral artery. The femoral vein is
-
Medial to the femoral artery at the base of the femoral triangle (indicated by inguinal ligament).
-
Posterior to the femoral artery at the apex of the femoral triangle.
-
Posterolateral to the artery in the adductor canal.
superoanterior aspect of the thigh, is not a prominent surface feature
in most people. When some people sit cross-legged, the sartorius and
adductor longus stand out, delineating the femoral triangle. The
surface anatomy of the femoral triangle is clinically important because
of its contents. The femoral artery can be felt pulsating just inferior at the midinguinal point. When you palpate the femoral pulse, the femoral vein is just medial, the femoral nerve is a finger’s breadth lateral, and the femoral head
is just posterior. The femoral artery runs a 5-cm superficial course
through the femoral triangle before it is covered by the sartorius in
the adductor canal.
The central point of this opening, where the great saphenous vein
enters the femoral vein, is located 3.75 cm inferior and 3.75 cm
lateral to the pubic tubercle.
mostly fat-filled compartment of the lower limb. Superficially, when
the knee is flexed, the popliteal fossa is evident as a diamond-shaped
depression posterior to the knee joint, bound superiorly by the
diverging hamstrings and inferiorly by the converging heads of the
gastrocnemius and plantaris (Fig. 5.30). The
size of this gap between muscles is misleading, however, in terms of
the actual size and extent of the popliteal fossa. Deeply, it is much
larger than the superficial depression indicates because the heads of
the gastrocnemius forming the inferior boundary superficially form a
roof over the inferior half of the deep part. When the knee is
extended, the fat within the fossa protrudes through the gap between
muscles, producing a rounded elevation flanked by shallow longitudinal
grooves overlying the hamstring tendons. In dissection, if the heads of
the gastrocnemius are separated and retracted (Fig. 5.31), a much larger space is revealed.
-
Superolaterally by the biceps femoris (superolateral border).
-
Superomedially by the semimembranosus, lateral to which is the semitendinosus (superomedial border).
![]() Figure 5.30. Superficial popliteal region. A. Numbers on the surface anatomy refer to structures identified in part B. The diamond-shaped gap in the roof of the popliteal fossa, formed by the overlying muscles, is outlined. B.
Figure 5.30. Superficial popliteal region. A. Numbers on the surface anatomy refer to structures identified in part B. The diamond-shaped gap in the roof of the popliteal fossa, formed by the overlying muscles, is outlined. B.
Superficial dissection of the popliteal region showing the muscles that
cover most of the popliteal fossa. The medial sural cutaneous nerve and
the sural communicating branch of the common fibular nerve unite at
various levels to form the sural nerve. In this specimen, the union
occurs inferior to the level of this dissection. Compare this with the
high union within the popliteal fossa in the specimen shown in Figure 5.31.P.633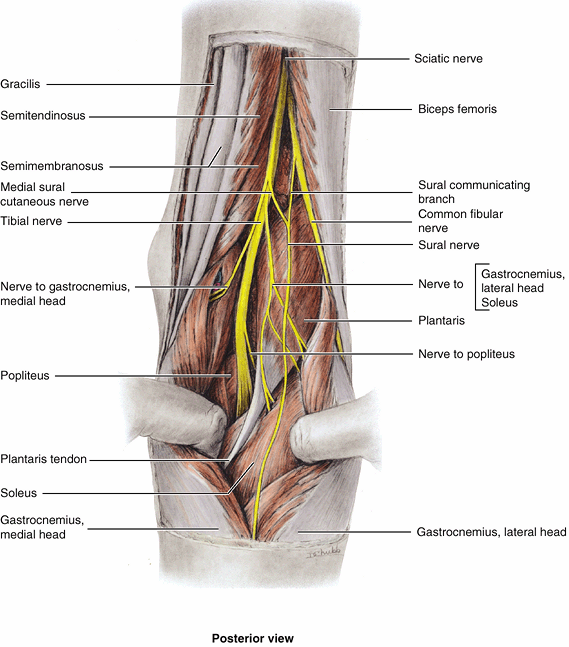 Figure 5.31. Exposure of popliteal fossa and nerves of fossa.
Figure 5.31. Exposure of popliteal fossa and nerves of fossa.
The two heads of the gastrocnemius muscle have been separated and are
being retracted. The sciatic nerve separates into its components at the
apex of the popliteal fossa (or higher; Fig. 5.28B).
The common fibular nerve courses along the medial border of the biceps
femoris. All the motor branches arising from the tibial nerve, except
one, arise from the lateral side; consequently, in surgery it is safer
to dissect on the medial side. The level at which the medial and
lateral sural nerves merge to form the sural nerve—occurring high
here—is quite variable; it may even occur at the level of the ankle. -
Inferolaterally and inferomedially by the
lateral and medial heads of the gastrocnemius, respectively
(inferolateral and inferomedial borders). -
Posteriorly by skin and popliteal fascia (roof).
boundaries are formed by the diverging medial and lateral supracondylar
lines of the femur. The inferior boundary is formed by the soleal line
of the tibia (Fig. 5.4B). These boundaries surround a relatively large diamond-shaped floor (anterior wall), formed by the popliteal surface
of the femur superiorly, the posterior capsule of the knee joint
centrally, and the popliteus fascia covering the popliteus muscle
inferiorly (Fig. 5.60).
-
Termination of the small saphenous vein.
-
Popliteal arteries and veins and their branches and tributaries.
-
Tibial and common fibular nerves.P.634
![]() Figure 5.32. Deep dissection of popliteal fossa.
Figure 5.32. Deep dissection of popliteal fossa.
The popliteal artery runs on the floor of the fossa, formed by the
popliteal surface of the femur, the joint capsule of the knee, and the
popliteus fascia. The floor of the fossa, which extends superiorly to
the diverging supracondylar lines of the femur and inferiorly to the
soleal line of (superior attachment of the soleus to) the tibia, is
much larger than the gap between the overlying muscles (outlined in Figure 5.30A), often mistaken as representing the extent of the fossa. Numbers refer to the surface anatomy shown in Figure 5.30A. -
Posterior cutaneous nerve of thigh (Table 5.1B).
-
Popliteal lymph nodes and lymphatic vessels (Fig. 5.13B).
contains the small saphenous vein (unless it has penetrated the deep
fascia at a more inferior level), and three cutaneous nerves: the
terminal branch(es) of the posterior cutaneous nerve of the thigh and the medial and lateral sural cutaneous nerves. The deep popliteal fascia is a strong sheet of deep fascia, continuous superiorly with the fascia lata and inferiorly with the deep fascia of the leg.
The popliteal fascia forms a protective covering for neurovascular
structures passing from the thigh through the popliteal fossa to the
leg and a relatively loose but functional retaining “retinaculum” for
the hamstring tendons. Often it is pierced by the small saphenous vein.
When the leg extends, the fat within the fossa is relatively compressed
as the popliteal fascia becomes taut, and the semimembranosus moves
laterally, providing further protection to the contents of the
popliteal fossa. The contents, most important the popliteal artery and
lymph nodes, are most easily palpated with the knee in semiflexion.
Because of the deep fascial roof and osseofibrous floor, the popliteal
fossa is a relatively confined space. Many disorders produce swelling
of the fossa, making knee extension painful.
Progressing from superficial to deep (posterior to anterior) within the
fossa, as in dissection, the nerves are encountered first, then the
veins. The arteries lie deepest, directly on the surface of the femur,
joint capsule, and popliteal fascia forming the floor of the fossa.
is the medial, larger terminal branch of the sciatic nerve derived from
anterior (preaxial) divisions of the anterior rami of the L4–S3 spinal
nerves. The tibial nerve is the most superficial of the three main
central components of the popliteal fossa (i.e., nerve, vein, and
artery); however, it is still in a deep and protected position. The
tibial nerve bisects the fossa as it passes from its superior to its
inferior angle. While in the fossa, the tibial nerve gives branches to
the soleus, gastrocnemius, plantaris, and popliteus muscles. The medial sural cutaneous nerve is also derived from the tibial nerve in the popliteal fossa and is joined by the sural communicating branch of the common fibular nerve at a highly variable level to form the sural nerve. This nerve supplies the lateral side of the leg and ankle.
the lateral, smaller terminal branch of the sciatic nerve derived from
posterior (postaxial) divisions of the anterior rami of the L4–S2
spinal nerves. It begins at the superior angle of the popliteal fossa
and follows closely the medial border of the biceps femoris and its
tendon along the superolateral boundary of the popliteal fossa. The
common fibular nerve leaves the fossa by passing superficial to the
lateral head of the gastrocnemius and then passes over the posterior
aspect of the head of the fibula. The common fibular nerve winds around
the fibular neck and divides into its terminal branches.
supply the skin that overlies the popliteal fossa. The nerve traverses
most of the length of the posterior compartment of the thigh deep to
the fascia lata; only its terminal branches enter the subcutaneous
tissue as cutaneous nerves per se.
begins when the latter passes through the adductor hiatus. The
popliteal artery passes inferolaterally through the fossa and ends at
the inferior border of the popliteus by dividing into the anterior and
posterior tibial arteries. The deepest (most anterior) structure in the
fossa, the popliteal artery, runs in close proximity to the joint
capsule of the knee as it spans the intercondylar fossa. Five genicular
branches of the popliteal artery supply the capsule and ligaments of
the knee joint. The genicular arteries are the superior lateral, superior medial, middle, inferior lateral, and inferior medial genicular arteries (Fig. 5.33). They participate in the formation of the periarticular genicular anastomosis,
a network of vessels surrounding the knee that provides collateral
circulation capable of maintaining blood supply to the leg during full
knee flexion, which may kink the popliteal artery. Other contributors
to this important anastomosis are the:
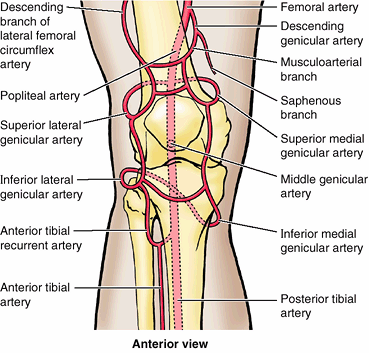 |
|
Figure 5.33. Genicular anastomosis.
The many arteries making up the periarticular anastomosis around the knee provide an important collateral circulation for bypassing the popliteal artery when the knee has been maintained too long in a fully flexed position or when the vessels are narrowed or occluded. |
-
Descending genicular branch of the femoral artery, superomedially.
-
Descending branch of the lateral femoral circumflex artery, superolaterally.
-
Anterior tibial recurrent branch of the anterior tibial artery, inferolaterally.
hamstring, gastrocnemius, soleus, and plantaris muscles. The superior
muscular branches of the popliteal artery have clinically important
anastomoses with the terminal part of the deep femoral and gluteal
arteries.
Throughout its course, the vein lies close to the popliteal artery,
lying superficial to it and in the same fibrous sheath. The popliteal
vein is initially posteromedial to the artery and lateral to the tibial
nerve. More superiorly, the popliteal vein lies posterior to the
artery, between this vessel and the overlying tibial nerve. Superiorly,
the popliteal vein, which has several valves, becomes the femoral vein
as it traverses the adductor hiatus. The small saphenous vein passes
from the posterior aspect of the lateral malleolus to the popliteal
fossa, where it pierces the deep popliteal fascia and enters the
popliteal vein.
expansion, pain from an abscess or tumor in the popliteal fossa is
usually severe. Popliteal abscesses tend to spread superiorly and inferiorly because of the toughness of the popliteal fascia. A popliteal cyst (Baker cyst), a saphenous varix, and an aneurysm of the popliteal artery should be considered in the differential diagnosis of masses within this space (see clinical correlation [blue] boxes “Popliteal Cysts,” “Saphenous Varix,” and “Popliteal Aneurysm and Hemorrhage,” in this chapter).
Palpation of this pulse is commonly performed with the person in the
prone position with the knee flexed to relax the popliteal fascia and
hamstrings. The pulsations are best felt in the inferior part of the
fossa where the popliteal artery is related to the tibia. Weakening or
loss of the popliteal pulse is a sign of a femoral artery obstruction.
(abnormal dilation of all or part of the popliteal artery) usually
causes edema and pain in the popliteal fossa. A popliteal aneurysm may
be distinguished from other masses by palpable pulsations (thrills) and abnormal arterial sounds (bruits)
detectable with a stethoscope. Because the artery lies deep to the
tibial nerve, an aneurysm may stretch the nerve or compress its blood
supply (vasa vasorum). Pain from such nerve compression is usually
referred, in this case to the skin overlying the medial aspect of the
calf, ankle or foot. Because the artery is closely applied to the
popliteal surface of the femur and the joint capsule, fractures of the
distal femur or dislocations of the knee may rupture the artery,
resulting in hemorrhage. Furthermore, because of their proximity and
confinement within the fossa, an injury of the artery and vein may
result in an arteriovenous fistula
(communication between an artery and a vein). Failure to recognize
these occurrences and to act promptly may result in the loss of the leg
and foot. If the femoral artery must be ligated, blood can bypass the
occlusion through the genicular anastomosis and reach the popliteal
artery distal to the ligation.
deep and protected position in the popliteal fossa; however, the nerve
may be injured by deep lacerations in the popliteal fossa. Posterior dislocation of the knee joint may also damage the tibial nerve. Severance of the tibial nerve
produces paralysis of the flexor muscles in the leg and the intrinsic
muscles in the sole of the foot. People with a tibial nerve injury are
unable to plantarflex their ankle or flex their toes. Loss of sensation
also occurs on the sole of the foot.
are usually small and lie in the subcutaneous tissue. A lymph node lies
at the termination of the small saphenous vein and receives lymph from
the lymphatic vessels that accompany this vein (Fig. 5.12B). The deep popliteal lymph nodes
surround the vessels and receive lymph from the joint capsule of the
knee and the lymphatic vessels that accompany the deep veins of the
leg. The lymphatic vessels from the popliteal lymph nodes follow the
femoral vessels to the deep inguinal lymph nodes.
confined compartment posterior to the knee that is traversed by all
neurovascular structures passing between the thigh and the leg. The
sciatic nerve bifurcates at the apex of the fossa, with the common
fibular nerve passing laterally along the biceps tendon. The tibial
nerve, popliteal vein, and popliteal artery bisect the fossa—in that
order, from superficial (posterior) to deep (anterior). Genicular
branches of the popliteal artery form a periarticular genicular
anastomosis around the knee, providing collateral circulation to
maintain blood flow in all positions of the knee.
and the two leg bones to which they attach, were discussed at the
beginning of this chapter and are illustrated in cross-section in Figure 5.34. It was pointed out that the muscles of each compartment share common functions and innervations.
closed spaces, ending proximally and distally at the joints.
Inflammations within the anterior and posterior compartments spread
chiefly in a distal direction. Suppuration (formation of pus) from
purulent (pus-forming) infections in the lateral compartment of the
leg, however, can ascend proximally into the popliteal fossa.
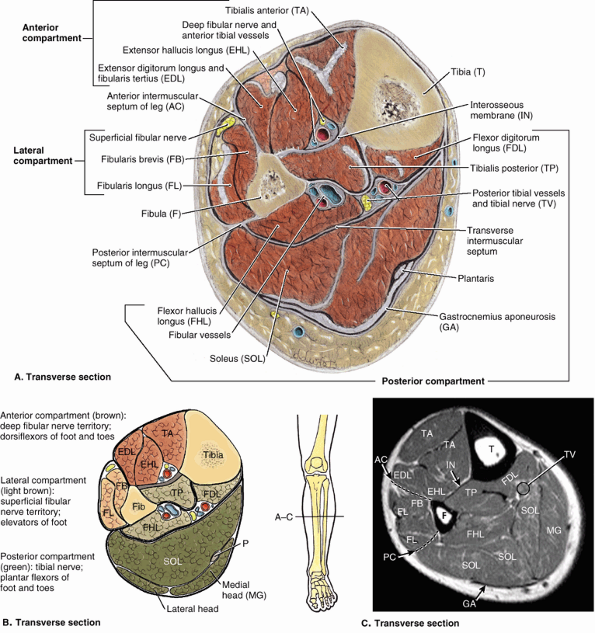 |
|
Figure 5.34. Compartments of leg at midcalf level in transverse anatomical section. A.
The anterior (dorsiflexor or extensor) compartment contains four muscles (the fibularis tertius lies inferior to the level of this section). The lateral (fibular) compartment contains two evertor muscles. The posterior (plantarflexor or flexor) compartment, containing seven muscles, is subdivided by an intracompartmental transverse intermuscular septum into a superficial group of three (two of which are commonly tendinous/aponeurotic at this level) and a deep group of four. The popliteus (part of the deep group) lies superior to the level of this section. B. Overview of compartments of leg. C. MRI of the leg. Abbreviations are defined in the labels for parts A and B. |
produce hemorrhage, edema, and inflammation of the muscles. Because the
septa and deep fascia of the leg forming the boundaries of the leg
compartments are strong, the increased volume consequent to any of
these processes increases intracompartmental pressure. With arterial
bleeding, the pressure may reach levels high enough to compress
structures significantly in the compartment(s) concerned. Structures
distal to the compressed area may become ischemic and permanently
injured (e.g., loss of motor function in muscles whose blood supply
and/or innervation is affected). These conditions, in which increased
pressure in a confined anatomical space adversely affects the
circulation and threatens the function and viability of tissue within
or distally, constitute compartment syndromes.
Loss of distal pulses is an obvious sign of arterial compression, as is
a lowering of the temperature of tissues distal to the compression. A fasciotomy (incision of the overlying fascia or a septum) may be performed to relieve the pressure in the compartment(s) concerned.
between the lateral surface of the tibial shaft and the medial surface
of the fibular shaft, and anterior to the intermuscular septum that
connects them. The anterior compartment is bounded anteriorly by the
deep fascia of the leg and skin. The deep fascia of the leg overlying
the anterior compartment is dense superiorly, providing part of the
proximal attachment of the muscle immediately deep to it. With
unyielding structures on three sides (the two bones and the
interosseous membrane) and a dense fascia on the remaining side, the
relatively small anterior compartment is especially confined and
therefore most susceptible to compartment syndromes. Inferiorly, two
band-like thickenings of the fascia form retinacula that bind the
tendons of the anterior compartment muscles before and after they cross
the ankle joint, preventing them from bowstringing anteriorly during
dorsiflexion of the joint (Fig. 5.35):
-
The superior extensor retinaculum is a strong, broad band of deep fascia, passing from the fibula to the tibia, proximal to the malleoli.
-
The inferior extensor retinaculum,
a Y-shaped band of deep fascia, attaches laterally to the
anterosuperior surface of the calcaneus. It forms a strong loop around
the tendons of the fibularis tertius and the extensor digitorum longus
muscles.
tibialis anterior, extensor digitorum longus, extensor hallucis longus,
and fibularis tertius (Fig. 5.34A & B; Table 5.10).
These muscles pass and insert anterior to the transversely oriented
axis of the ankle (talocrural) joint and, therefore, are dorsiflexors
of the ankle joint, elevating the forefoot and depressing the heel. The
long extensors also pass along and attach to the dorsal aspect of the
digits and are thus extensors (elevators) of the toes.
with a range of about 20° from neutral—dorsiflexion is actively used in
the swing phase of walking, when concentric contraction keeps the
forefoot elevated to clear the ground as the free limb swings forward,
and immediately after in the stance phase, as eccentric contraction
controls the lowering of the forefoot to the floor following heel
strike (Table 5.2). The latter is important to
a smooth gait and is important to deceleration (braking) relative to
running and walking downhill. During standing, the dorsiflexors
reflexively pull the leg (and thus the center of gravity) anteriorly on
the fixed foot when the body starts to lean (the center of gravity
begins to shift too far) posteriorly. When descending a slope,
especially if the surface is loose (sand, gravel or snow), dorsiflexion
is used to “dig in” one’s heels.
The long tendon of the TA begins halfway down the leg and descends
along the anterior surface of the tibia. The tendon passes within its
own synovial sheath deep to the superior and inferior extensor
retinacula (Fig. 5.35) to its attachment on the
medial side of the foot. In so doing, its tendon is located farthest
from the axis of the ankle joint, giving it the most mechanical
advantage and making it the strongest dorsiflexor. Although antagonists
at the ankle joint, the TA and the tibialis posterior (from the
posterior compartment) both cross the subtalar and transverse tarsal
joints to attach to the medial border of the foot and thus act
synergistically to invert the foot.
individual is asked to stand on the heels or dorsiflex the foot against
resistance; if normal, its tendon can be seen and palpated.
A small part of the proximal attachment of the muscle is to the lateral
tibial condyle; however, most of it attaches to the medial surface of
the fibula and the superior part of the anterior surface of the
interosseous membrane (Table 5.10A).
The muscle becomes tendinous superior to the ankle, forming four
tendons that attach to the phalanges of the lateral four toes. A common
synovial sheath surrounds the four tendons of the EDL (plus that of the
fibularis tertius) as they diverge on the dorsum of the foot and pass
to their distal attachments (Fig. 5.35B).
Each tendon forms a membranous extensor expansion
(dorsal aponeurosis) over the dorsum of the proximal phalanx of the
toe, which divides into two lateral bands and one central band (Fig. 5.35A).
The central band inserts into the base of the middle phalanx, and the
lateral slips converge to insert into the base of the distal phalanx.
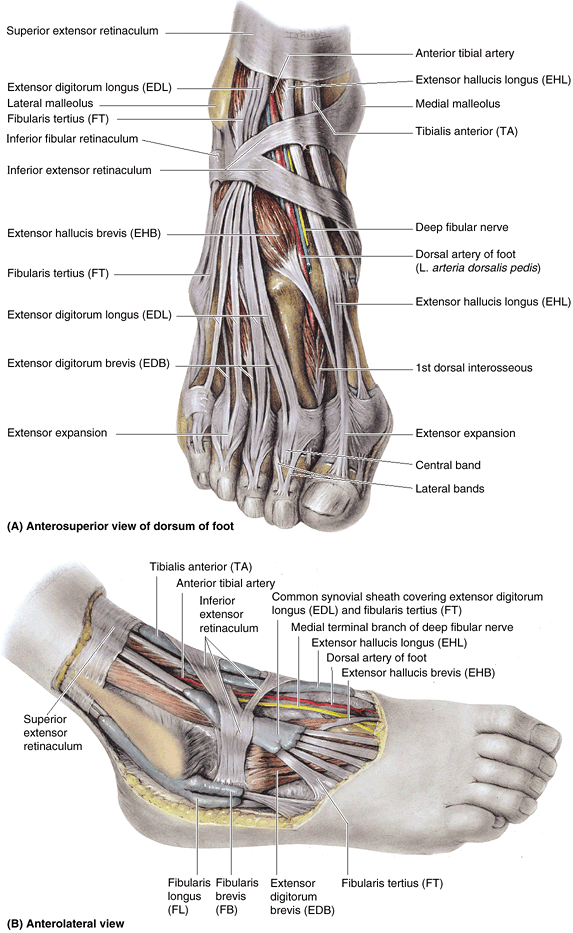 |
|
Figure 5.35. Dissections of foot.
These dissections demonstrate the continuation of the anterior and lateral leg muscles into the foot. The thinner portions of the deep fascia of the leg have been removed, leaving the thicker portions that make up the extensor and fibular retinacula, which retain the tendons as they cross the ankle. A. The vessels and nerves are cut short. At the ankle, the vessels and the deep fibular nerve lie midway between the malleoli and between the tendons of the long dorsiflexors of the toes. B. Synovial sheaths surround the tendons as they pass beneath the retinacula of the ankle. |
|
Table 5.10. Muscles of the Anterior and Lateral Compartments of the Leg
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
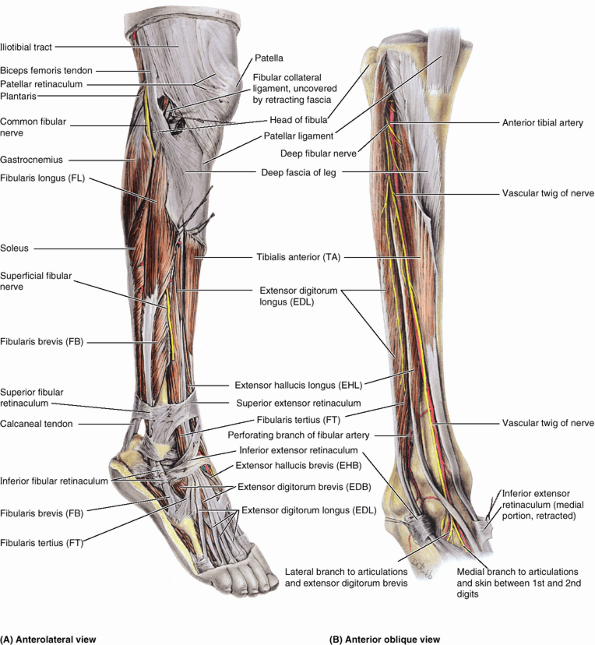 |
|
Figure 5.36. Dissections of anterior and lateral compartments of leg. A.
This dissection shows the muscles of the anterolateral leg and dorsum of the foot. The common fibular nerve, coursing subcutaneously across the lateral aspect of the head and neck of the fibula, is the most commonly injured peripheral nerve. B. In this deeper dissection of the anterior compartment, the muscles and inferior extensor retinaculum are retracted to display the arteries and nerves. |
Proximally, the attachments and fleshy parts of the EDL and FT are
continuous; however, distally, the FT tendon is separate and attaches
to the 5th metatarsal, not to a phalanx (Table 5.10F).
Although the FT does contribute (weakly) to dorsiflexion, it also acts
at the subtalar and transverse tarsal joints, contributing to pronation
(eversion) of the foot. It may play a special proprioceptive role in
sensing sudden inversion and then contracting reflexively to protect
the anterior tibiofibular ligament, the most commonly sprained ligament
of the body. The FT is not always present.
(EHL) is a thin muscle that lies deeply between the TA and the EDL at
its superior attachment to the middle half of the fibula and
interosseous membrane. The EHL rises to the surface in the distal third
of the leg, passing deep to the extensor retinacula (Figs. 5.35 and 5.36). It courses distally along the crest of the dorsum of the foot to the great toe.
It is one of the two terminal branches of the common fibular nerve,
arising between the fibularis longus muscle and the neck of the fibula.
After its entry into the anterior compartment, the deep fibular nerve
accompanies the anterior tibial artery, first between the TA and the
EDL and then between the TA and the EHL. It then exits the compartment,
continuing across the ankle joint to supply intrinsic muscles and a
small area of the skin of the foot. A lesion of this nerve results in
an inability to dorsiflex (footdrop).
The smaller terminal branch of the popliteal artery, the anterior
tibial artery, begins at the inferior border of the popliteus muscle
(i.e., as the popliteal artery passes deep to the tendinous arch of the
soleus) and immediately passes anteriorly through a gap in the superior
part of the interosseous membrane to descend on the anterior surface of
this membrane between the TA and the EDL muscles. At the ankle joint,
midway between the malleoli, the anterior tibial artery changes names,
becoming the dorsal artery of the foot (L. arteria dorsalis pedis).
in the area of the distal two-thirds of the tibia—result from
repetitive microtrauma of the TA, which causes small tears in the
periosteum covering the shaft of the tibia and/or of fleshy attachments
to the overlying deep fascia of the leg. Shin splints are a mild form
of the anterior compartment syndrome. Shin splints commonly occur
during traumatic injury or athletic overexertion of muscles in the
anterior compartment, especially the TA, by untrained persons. Often
persons who lead sedentary lives develop shin splints when they
participate in walk-a-thons (long-distance walks). Shin splints also
occur in trained runners who do not warm up and cool down sufficiently.
Muscles in the anterior compartment swell from sudden overuse, and the
edema and muscle–tendon inflammation reduce the blood flow to the
muscles. The swollen muscles are painful and tender to pressure.
nerve (e.g., during skiing, running, and dancing) may result in muscle
injury and edema in the anterior compartment. This entrapment may cause
compression of the deep fibular nerve and pain in the anterior
compartment. Compression of the nerve by tight-fitting ski boots, for
example, may occur where the nerve passes deep to the inferior extensor
retinaculum and the extensor hallucis brevis. Pain occurs in the dorsum
of the foot and usually radiates to the web space between the 1st and
2nd toes. Because ski boots are a common cause of this type of nerve
entrapment, this condition has been called the “ski boot syndrome”;
however, the syndrome also occurs in soccer players and runners and can
result from tight shoes.
bones and membranes, is susceptible to compartment syndromes. The
contained muscles are ankle dorsiflexors/toe extensors that are active
in walking as they (1) concentrically contract to raise the forefoot to
clear the ground during the swing phase of the gait cycle and (2)
eccentrically contract to lower the forefoot to the ground after the
heel strike of the stance phase. The deep fibular nerve and anterior
tibial artery course within and supply the compartment. Injury of the
common or deep fibular nerve results in footdrop (see clinical correlation [blue] box, “Injury to the Common Fibular Nerve and Footdrop,” in this chapter).
|
Table 5.11. Nerves of the Leg
|
||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||
|
Table 5.12. Arteries of the Leg
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||
is the smallest (narrowest) of the leg compartments, bounded by the
lateral surface of the fibula, the anterior and posterior intermuscular
septa, and the deep fascia of the leg (Fig. 5.34A & B; Table 5.10). The compartment ends inferiorly at the superior fibular retinaculum, which spans between the distal tip of the fibula and the calcaneus (Fig. 5.36A).
Here the tendons of the two muscles of the lateral compartment enter a
common synovial sheath to accommodate their passage between the
superior fibular retinaculum and the lateral
malleolus, using the latter as a trochlea as they cross the ankle joint.
and brevis muscles. These muscles have their fleshy bellies in the
lateral compartment but are tendinous as they exit the compartment
within the common synovial sheath deep to the superior fibular
retinaculum. Both muscles are evertors of the foot, elevating the
lateral margin of the foot. Developmentally, the fibularis muscles are
postaxial muscles, receiving innervation from the posterior divisions
of the spinal nerves, which contribute to the sciatic nerve. However,
because the fibularis longus and brevis pass posterior to the
transverse axis of the ankle (talocrural) joint, they contribute to
plantarflexion at the ankle—unlike the postaxial muscles of the
anterior compartment (including the fibularis tertius), which are
dorsiflexors.
and transverse tarsal joints. From the neutral position, only a few
degrees of eversion are possible. In practice, the primary function of
the evertors of the foot is not to elevate the lateral margin of the
foot (the common description of eversion) but to depress or fix the
medial margin of the foot in support of the toe off phase of walking
and, especially, running and to resist inadvertent or excessive
inversion of the foot (the position in which the ankle is most
vulnerable to injury). When standing (and particularly when balancing
on one foot), the fibularis muscles contract to resist medial sway (to
recenter a line of gravity, which has shifted medially) by pulling
laterally on the leg while depressing the medial margin of the foot.
the foot is everted strongly against resistance; if acting normally,
the muscle tendons can be seen and palpated inferior to the lateral
malleolus.
The narrow FL extends from the head of the fibula to the sole of the
foot. Its tendon can be palpated and observed proximal and posterior to
the lateral malleolus. Distal to the superior fibular retinaculum, the
common sheath shared by the fibular muscles splits to extend through
separate compartments deep to the inferior fibular retinaculum (Figs. 5.35A and 5.36). The FL passes through the inferior compartment—inferior to the fibular trochlea on the calcaneus—and enters a groove on the anteroinferior aspect of the cuboid bone (Fig. 5.9C).
It then crosses the sole of the foot, running obliquely and distally to
reach its attachment to the 1st metatarsal and medial cuneiform bones
(see Fig. 5.9B). When a person stands on one foot, the FL helps steady the leg on the foot.
a fusiform muscle that lies deep to the FL and, true to its name, the
FB is shorter than its partner in the lateral compartment (Figs. 5.34 and 5.36A; Table 5.10).
Its broad tendon grooves the posterior aspect of the lateral malleolus
and can be palpated inferior to it. The narrower tendon of the FL lies
on that of the FB and does not contact the lateral malleolus. The
tendon of the FB traverses the superior compartment of the inferior
fibular retinaculum, passing superior to the fibular trochlea of the
calcaneus; it can be easily traced to its distal attachment to the base
of the 5th metatarsal (Fig. 5.9C). The tendon of the fibularis tertius, a slip of muscle from the extensor digitorum longus, often merges with the tendon of the FB (Fig. 5.36A). Occasionally, however, the fibularis tertius passes anteriorly to attach directly to the proximal phalanx of the 5th digit.
After supplying the FL and FB, the superficial fibular nerve continues
as a cutaneous nerve, supplying the skin on the distal part of the
anterior surface of the leg and nearly all the dorsum of the foot.
through it. Instead, perforating branches and accompanying veins supply
blood to and drain blood from the compartment. Proximally, perforating
branches of the anterior tibial artery penetrate the anterior
intermuscular septum. Inferiorly, perforating branches of the fibular artery penetrate the posterior intermuscular septum, along with their accompanying veins (L. venae comitantes) (Table 5.12).
evertors of the foot and the superficial fibular nerve that supplies
them. Because no artery courses within the compartment, perforating
branches from the anterior tibial and fibular arteries (and their
accompanying veins) penetrate the intermuscular septa to supply (and
drain) blood. Eversion is used to support/depress the medial foot
during the toe off of the stance phase and to resist inadvertent
inversion, preventing injury.
inverted so that they walk on the outer border of the foot, feet of
humans are relatively everted (pronated) so that the soles lie more
fully on the ground. This pronation is the result, at least in part, to
the medial migration of the distal attachment of the fibularis longus
across the sole of the foot and the development of a fibularis tertius
that is attached to the base of the 5th metatarsal. These features are
unique to the human foot.
is the nerve most often injured in the lower limb, mainly because it
winds subcutaneously around the fibular neck, leaving it vulnerable to
direct trauma. This nerve may also be severed during fracture of the
fibular neck or severely stretched when the knee joint is injured or
dislocated. Severance of the common fibular nerve
results in flaccid paralysis of all muscles in the anterior and lateral
compartments of the leg (dorsiflexors of the ankle and evertors of the
foot). The loss of dorsiflexion of the ankle causes footdrop,
which is further exacerbated by unopposed inversion of the foot. This
has the effect of making the limb “too long”: The toes do not clear the
ground during the swing phase of walking (Fig. B5.14A).
-
A waddling gait, in which the individual leans to the side opposite the long limb, “hiking” the hip (Fig. B5.14B).
-
A swing-out gait, in which the long limb is swung out laterally (abducted) to allow the toes to clear the ground (Fig. B5.14C).
-
A high-stepping steppage gait,
in which extra flexion is employed at the hip and knee to raise the
foot as high as necessary to keep the toes from hitting the ground (Fig. B5.14D).
heel strike the ground first as in a normal gait, a steppage gait is
commonly employed in the case of flaccid paralysis. Sometimes an extra
“kick” is added as the free limb swings forward in an attempt to flip
the forefoot upward just before setting the foot down. In addition, the
braking action normally produced by eccentric contraction of the
dorsiflexors is also lost in flaccid paralysis footdrop. Therefore, the
foot is not lowered to the ground in a controlled manner after heel
strike but instead slaps the ground suddenly, producing a distinctive clop
and greatly increasing the shock both received by the forefoot and
transmitted up the tibia to the knee. Individuals with a fibular nerve
injury may also experience a variable loss of sensation on the
anterolateral aspect of the leg and the dorsum of the foot.
produce recurrent stretching of the superficial fibular nerve, which
may cause pain along the lateral side of the leg and the dorsum of the
ankle and foot. Numbness and paresthesia (tickling or tingling) may be present and increase with activity.
the distal attachment of fibularis brevis. This avulsion fracture is
associated with a severely sprained ankle. Injury to the associated
superficial fibular nerve causes inversion of the foot because of
paralysis of the fibular muscles in the lateral compartment.
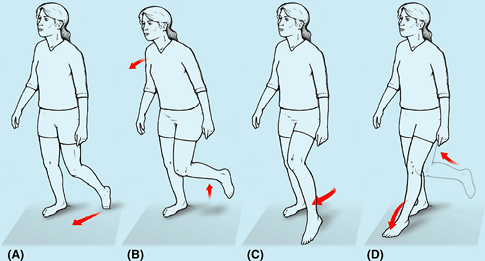 |
|
Figure B5.14
|
The tibial nerve and posterior tibial and fibular vessels supply both
parts of the posterior compartment but run in the deep subcompartment
deep (anterior) to the transverse intermuscular septum. The larger
superficial subcompartment is the least confined compartmental area.
The smaller deep subcompartment, like the anterior compartment, is
bounded by the two leg bones and the interosseous membrane
that binds them together plus the transverse intermuscular septum;
therefore, the deep subcompartment is quite tightly confined. Because
the nerve and blood vessels supplying the entire posterior compartment
and the sole of the foot pass through the deep subcompartment, when
swelling occurs it leads to a compartment syndrome that has serious
consequences.
muscles it contains become tendinous. The transverse intermuscular
septum ends as reinforcing transverse fibers that extend between the
tip of the medial malleolus and the calcaneus to form the flexor
retinaculum. The retinaculum is subdivided deeply, forming separate
compartments for each tendon of the deep muscle group, as well as for
the tibial nerve and posterior tibial artery as they bend around the
medial malleolus.
plantarflexion at the ankle, inversion at the subtalar and transverse
tarsal joints, and flexion of the toes. Plantarflexion is a powerful
movement (four times stronger than dorsiflexion) produced over a
relatively long range (approximately 50° from neutral) by muscles that
pass posterior to the transverse axis of the ankle joint. The movement
develops thrust, applied primarily at the ball of the foot, that is
used to propel the body forward and upward and is the major component
of the forces generated during the push-off (heel off and toe off)
parts of the stance phase of walking and running (Table 5.2).
gastrocnemius, soleus, and plantaris. Details concerning their
attachments, innervation and actions are provided in Table 5.13.
The two-headed gastrocnemius and soleus share a common tendon, the
calcaneal tendon, which attaches to the calcaneus. Collectively these
two muscles make up the three-headed triceps surae (L. sura, calf) (Fig. 5.37).
This powerful muscular mass tugs on the lever provided by the calcaneal
tuberosity, elevating the heel and thus depressing the forefoot,
generating as much as 93% of the plantarflexion force. The large size
of the gastrocnemius and soleus muscles is a human characteristic that
is directly related to our upright stance. These muscles are strong and
heavy because they lift, propel, and accelerate the weight of the body
when walking, running, jumping, or standing on the toes.
Achilles tendon) is the most powerful (thickest and strongest) tendon
in the body. Approximately 15 cm in length, it is a continuation of the
flat aponeurosis, formed halfway down the calf where the bellies of the
gastrocnemius terminate. The aponeurosis receives fleshy fibers of the
soleus directly on its deep surface proximally but thickens as the
soleus fibers become tendinous inferiorly. The tendon thus becomes
thicker (deeper) but narrower as it descends until it becomes
essentially round in cross-section superior to the calcaneus. It then
expands as it inserts centrally on the posterior surface of the calcaneal tuberosity.
It typically spirals a quarter turn (90°) during its descent, so that
the gastrocnemius fibers attach laterally and the soleal fibers attach
medially. This arrangement is thought to be significant to the tendon’s
elastic ability to absorb energy (shock) and recoil, releasing the
energy as part of the propulsive force it exerts. Although they share a
common tendon, the two muscles of the triceps surae are capable of
acting alone, and often do so: “You stroll with the soleus but win the
long jump with the gastrocnemius.”
the foot is plantarflexed against resistance (e.g., by “standing on the
toes,” in which case body weight [gravity] provides resistance). If
normal, the calcaneal tendon and triceps surae can be seen and palpated.
It is a fusiform, two-headed, two-joint muscle with the medial head
slightly larger and extending more distally than its lateral partner.
The heads come together at the inferior margin of the popliteal fossa,
where they form the inferolateral and inferomedial boundaries of this
fossa. Because its fibers are mainly vertical, and largely of the
white, fast-twitch (type 2) variety, contractions of the gastrocnemius
produce rapid movements during running and jumping (Table 5.13).
It is recruited into action only intermittently during symmetrical
standing. The gastrocnemius crosses and is capable of acting on both
the knee and the ankle joints; however, it cannot exert its full power
on both joints at the same time. It functions most effectively when the
knee is extended (and is maximally activated when knee extension is
combined with dorsiflexion, as in the sprint start). It is incapable of
producing plantarflexion when the knee is fully flexed.
to the gastrocnemius and is considered to be the “workhorse” of
plantarflexion. It is a large muscle, flatter than the gastrocnemius,
that is named for its resemblance to a sole—the flat fish that reclines
on its side on the sea floor. The soleus has a continuous proximal
attachment in the shape of an inverted U to the posterior aspects of
the fibula and tibia and a tendinous arch between them, the tendinous arch of the soleus (L. arcus tendineus
soleus
The popliteal artery and tibial nerve exit the popliteal fossa by
passing through this arch, the popliteal artery simultaneously
bifurcating into its terminal branches, the anterior and posterior
tibial arteries. The soleus can be palpated on each side of the
gastrocnemius when the individual is standing on the tiptoes.
|
Table 5.13-I. Superficial Muscles of the Posterior Compartment of the Leg
|
||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||
plantarflexing the ankle joint; it cannot act on the knee joint and
acts alone when the knee is flexed. The fibers of the soleus slope
posteriorly and inferomedially. When the foot is planted, it pulls
posteriorly on the bones of the leg. This is important to standing
because the line of gravity passes anterior to the leg’s bony axis. The
soleus is thus an antigravity muscle (the predominant plantarflexor for
standing and strolling), which contracts antagonistically but
cooperatively (alternately) with the dorsiflexor muscles of the leg to
maintain balance. Composed largely of red, fatigue-resistant,
slow-twitch (type 1) muscle fibers, it is a strong but relatively slow
plantarflexor of the ankle joint, capable of sustained contraction.
Electromyography (EMG) studies show that during symmetrical standing,
the soleus is continuously active.
highly variable in size and form when present (most commonly a tapering
slip about the size of the small finger). It acts with the
gastrocnemius but is insignificant as either a flexor of the knee or a
plantarflexor of the ankle. It has been considered to be an organ of
proprioception for the larger plantarflexors, as it has a high density
of muscle spindles (receptors for proprioception). Its long, slender
tendon is easily mistaken for a nerve (and hence dubbed by some the
“freshman’s nerve”). It runs distally between the gastrocnemius and the
soleus (Fig. 5.34A) and occasionally suddenly ruptures with a painful pop
during activities such as racquet sports. Because of its minor role,
the plantaris tendon can be removed for grafting (e.g., during
reconstructive surgery of the tendons of the hand) without causing
disability.
|
Table 5.13-II. Deep Muscles of the Posterior Compartment of the Leg
|
||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||
(L. bean), which articulates with the lateral femoral condyle and is
visible in lateral radiographs of the knee in 3–5% of people (Fig. B5.15).
of running injuries. Microscopic tears of collagen fibers in the
tendon, particularly just superior to its attachment to the calcaneus,
result in tendinitis, which causes pain
during walking, especially when wearing rigid-soled shoes. Calcaneal
tendinitis often occurs during repetitive activities, especially in
individuals who take up running after prolonged inactivity or suddenly
increase the intensity of their training, but it may also result from
poor footwear or training surfaces.
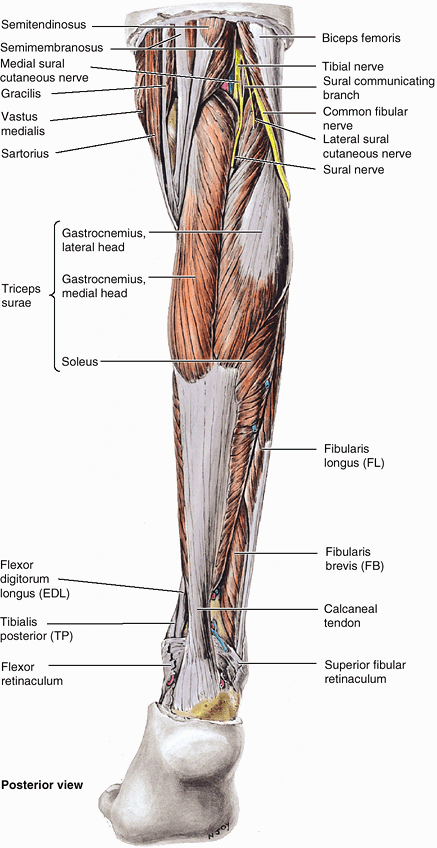 |
|
Figure 5.37. Superficial dissection of posterior aspect of leg.
Except for the retinacula in the ankle region, the deep fascia has been removed to reveal the nerves and muscles. Visible nerves include the tibial and common fibular nerves and their contributions to the formation of the sural nerve. The three heads of the triceps surae muscle attach distally to the calcaneus via the spiraling fibers of the calcaneal tendon. |
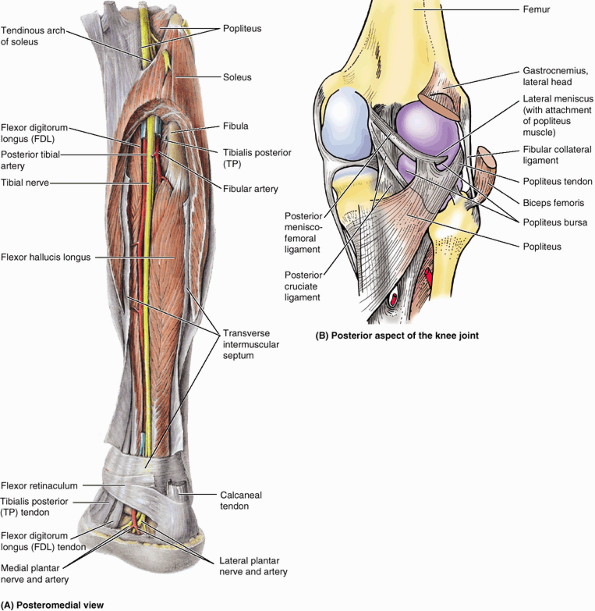 |
|
Figure 5.38. Deep dissection of posterior aspect of right leg and knee joint. A.
The gastrocnemius and most of the soleus are removed, leaving only a horseshoe-shaped section of the soleus close to its proximal attachments and the distal part of the calcaneal tendon in the superficial part of the posterior compartment The transverse intermuscular septum has been split to reveal the deep muscles, vessels, and nerves. B. The popliteus tendon attaches in part to the lateral meniscus and is separated from the proximal end of the tibia by the popliteus bursa. |
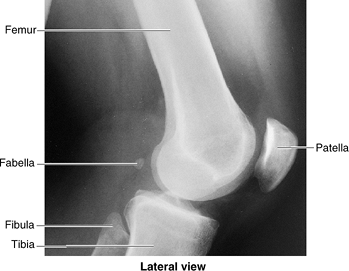 |
|
Figure B5.15
|
The injury is typically experienced as an audible snap during a
forceful push off (plantarflexion with the knee extended) followed
immediately by sudden calf pain and sudden dorsiflexion of the
plantarflexed foot. In a completely ruptured tendon, a gap is palpable,
usually 1–5 cm proximal to the calcaneal attachment.
probably the most severe acute muscular problem of the leg. Individuals
with this injury cannot plantarflex against resistance (cannot raise
the heel from the ground or balance on the affected side), and passive
dorsiflexion (usually limited to 20° from neutral) is excessive.
Ambulation is possible only when the limb is externally rotated,
rolling over the transversely placed foot during the stance phase
without push off. Bruising appears in the malleolar region, and a lump
usually appears in the calf owing to shortening of the triceps surae.
In older or non-athletic people, non-surgical repairs are often
adequate, but surgical intervention is usually advised for those with
active lifestyles.
a myotatic reflex elicited while the person’s legs are dangling over
the side of the examining table. The calcaneal tendon is struck briskly
with a reflex hammer just proximal to the calcaneus. The normal result
is plantarflexion of the ankle joint. The calcaneal tendon reflex tests
the S1 and S2 nerve roots. If the S1 nerve root is injured or
compressed, the ankle reflex is virtually absent.
leg) is a painful acute injury resulting from the partial tearing of
the medial belly of the gastrocnemius at or near its musculotendinous
junction, often seen in individuals older than 40 years of age. It is
caused by overstretching the muscle by concomitant full extension of
the knee and dorsiflexion of the ankle joint. Usually, an abrupt onset
of stabbing pain is followed by edema and spasm of the gastrocnemius.
Calcaneal bursitis causes pain posterior to the heel and occurs quite
commonly during long-distance running, basketball, and tennis. It is
caused by excessive friction on the bursa as the tendon continuously
slides over it. Inflammation of the subcutaneous calcaneal bursa also results from repetitive microtrauma from the backs of shoes, usually new ones.
the return of blood from the leg. When a person is standing, the venous
return from the leg depends largely on the muscular activity of the
triceps surae (see “Venous Drainage of the Lower Limb,”
earlier in this chapter). Contraction of the calf muscles pumps blood
superiorly in the deep veins. The efficiency of the calf pump is
improved by the deep fascia that invests the muscles like an elastic
stocking. Normally, blood is prevented from flowing into the
superficial veins by the valves in the perforating veins. If these
valves are incompetent, blood is forced into the superficial veins
during contraction of the triceps surae and by hydrostatic pressure
when straining or standing. As a consequence, the vessels become
dilated and tortuous varicose veins.
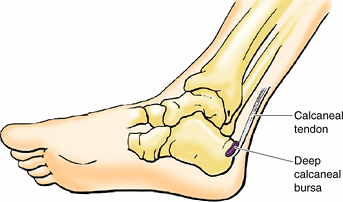 |
|
Figure B5.16
|
The accessory muscle usually appears as a distal belly medial to the
calcaneal tendon. Clinically, an accessory soleus may be associated
with pain and edema during prolonged exercise.
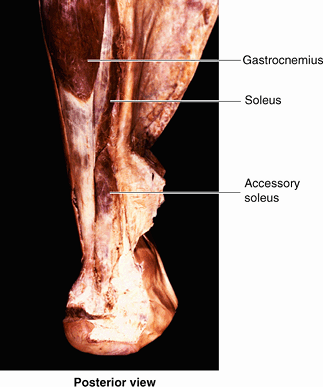 |
|
Figure B5.17
|
popliteus, flexor digitorum longus, flexor hallucis longus, and
tibialis posterior. Details concerning the attachments, innervation,
and actions of these muscles are provided in Table 5.13.
The popliteus acts on the knee joint, whereas the other muscles
plantarflex the ankle and flex the toes. However, because of their
smaller size and the close proximity of their tendons to the axis of
the ankle joint, the “non-triceps” plantarflexors collectively produce
only about 7% of the total force of plantarflexion, and in this the
fibularis longus and brevis are most significant. When the calcaneal
tendon is ruptured, these muscles cannot generate the power necessary
to lift the body’s weight (i.e., to stand on the toes).
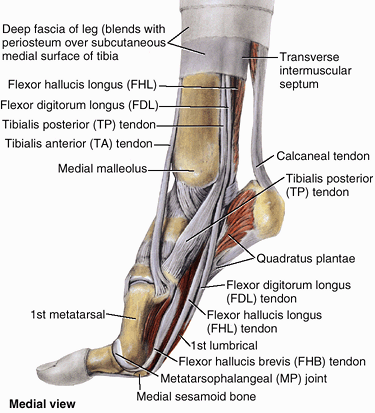 |
|
Figure 5.39. Dissection demonstrating continuation of plantarflexor tendons across ankle joint.
The foot is raised as in the push-off phase of walking. Observe the sesamoid bone acting as a “foot stool” for the 1st metatarsal, giving it extra height and protecting the flexor hallucis longus tendon. |
to the toes are criss-crossed—that is, the muscle attaching to the
medial (great) toe (flexor hallucis longus) arises laterally (from the
fibula) in the deep subcompartment, and the muscle attaching to the
lateral four toes (flexor digitorum longus) arises medially (from the
tibia) (Fig. 5.40). Their tendons cross in the sole of the foot.
Proximally, its tendinous attachment to the lateral aspect of the
lateral femoral condyle and its broader attachment to the lateral
meniscus occur between the fibrous layer and the synovial membrane of
the joint capsule of the knee. The apex of its fleshy belly emerges
from the joint capsule of the knee joint. It has a fleshy distal
attachment to the tibia that is covered by popliteal fascia reinforced
by a fibrous expansion from the semimembranosus muscle.
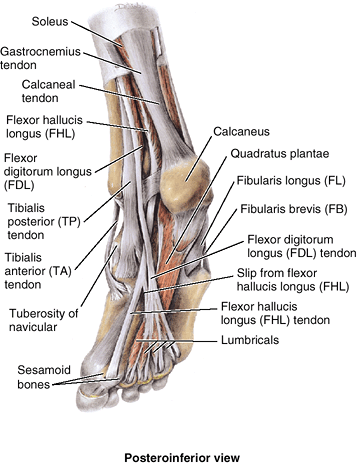 |
|
Figure 5.40. Dissection demonstrating continuation of plantarflexor tendons in second layer of sole of foot.
This layer of foot muscles includes the tendons of the flexor hallucis longus and flexor digitorum longus, the four lumbrical (L. lumbricus, earthworm) muscles, and the quadratus plantae. |
joint per se; but during flexion at the knee, it assists in pulling the
lateral meniscus posteriorly, a movement otherwise produced passively
by compression (as it is for the medial meniscus; some have claimed
this is part of the reason the lateral meniscus is injured less often).
When a person is standing with the knee partly flexed, the popliteus
contracts to assist the posterior cruciate ligament (PCL) in preventing
anterior displacement of the femur on the inclined tibial plateau.
When standing with the knees locked in the fully extended position, the
popliteus acts to rotate the femur laterally 5° on the tibial plateaus
(see “Tibia,” earlier in this chapter),
releasing the knee from its close-packed or locked position so that
flexion can occur. When the foot is off the ground and the knee is
flexed, the popliteus can aid the medial hamstrings (the “semimuscles”)
in rotating the tibia medially beneath the femoral condyles.
(FHL) is a powerful flexor of all of the joints of the great toe.
Immediately after the triceps surae has delivered the thrust of
plantarflexion to the ball of the foot
(the prominence of the sole underlying the heads of the 1st and 2nd
metatarsals), the FHL delivers a final thrust via flexion of the great
toe for the preswing phase (toe off) of the gait cycle (Table 5.2).
When barefoot, this thrust is delivered by the great toe; but with
soled shoes on, it becomes part of the thrust of plantarflexion
delivered by the forefoot. The tendon of the FHL passes posterior to
the distal end of the tibia and occupies a shallow groove on the
posterior surface of the talus, which is continuous with the groove on
the plantar surface of the talar shelf (Figs. 5.39 and 5.40).
The tendon then crosses deep to the tendon of the flexor digitorum
longus in the sole of the foot. As it passes to the distal phalanx of
the great toe, the FHL tendon runs between two sesamoid bones in the tendons of the flexor hallucis brevis (Fig. 5.40). These bones protect the tendon from the pressure of the head of the 1st metatarsal bone.
phalanx of the great toe is flexed against resistance; if normal, the
tendon can be seen and palpated on the plantar aspect of the great toe
as it crosses the joints of the toe.
It passes diagonally into the sole of the foot, superficial to the
tendon of the FHL. However, its direction of pull is realigned by the quadratus plantae muscle, which is attached to the posterolateral aspect of the FDL tendon as it divides into four tendons (Fig. 5.40), which in turn pass to the distal phalanges of the lateral four digits.
phalanges of the lateral four toes are flexed against resistance; if
they are acting normally, the tendons of the toes can be seen and
palpated.
the deepest (most anterior) muscle in the posterior compartment, lies
between the FDL and the FHL in the same plane as the tibia and fibula
within the deep subcompartment (Figs. 5.38A, 5.39, and 5.40).
Distally, the TP attaches primarily to the navicular bone (in close
proximity to the high point of the medial longitudinal arch of the
foot) but has attachments to other tarsal and metatarsal bones (Figs. 5.44D and 5.68A; Table 5.13).
foot. Indeed, when the foot is off the ground, it can act
synergistically with the TA to invert the foot, their otherwise
antagonistic functions canceling each other out. However, the primary
role of the TP is to support or maintain (fix) the medial longitudinal
arch during weight bearing; consequently, the muscle contracts
statically throughout the stance phase of gait (Fig. 5.69C & E; Table 5.2).
In so doing, it acts independently of the TA because, once the foot is
flat on the ground after heel strike, that muscle is relaxed during the
stance phase (the dorsiflexion that occurs as the body passes over the
planted foot is passive), unless braking requires its eccentric
contraction. While standing (especially on one foot),
however,
the two muscles may cooperate to depress the lateral side of the foot
and pull medially on the leg as needed to counteract lateral leaning
for balance.
the foot is inverted against resistance with the foot in slight
plantarflexion; if normal, the tendon can be seen and palpated
posterior to the medial malleolus.
It runs vertically through the popliteal fossa with the popliteal
artery, passing between the heads of the gastrocnemius, the two
structures exiting the fossa by passing deep to the tendinous arch of
the soleus. The tibial nerve supplies all muscles in the posterior
compartment of the leg (Figs. 5.34A and 5.38A; Table 5.11).
At the ankle, the nerve lies between the tendons of the FHL and the
FDL. Posteroinferior to the medial malleolus, the tibial nerve divides
into the medial and lateral plantar nerves. A branch of the tibial
nerve, the medial sural cutaneous nerve, is usually joined by the sural communicating branch of the common fibular nerve to form the sural nerve.
This nerve supplies the skin of the lateral and posterior part of the
inferior third of the leg and the lateral side of the foot. Articular
branches of the tibial nerve supply the knee joint, and medial
calcaneal branches supply the skin of the heel.
the larger and more direct terminal branch of the popliteal artery,
provides the blood supply to the posterior compartment of the leg and
to the foot (Figs. 5.34A, 5.38A, and 5.41; Table 5.12).
It begins at the distal border of the popliteus as the popliteal artery
passes deep to the tendinous arch of the soleus and simultaneously
bifurcates into its terminal branches. Close to its origin, the
posterior tibial artery gives rise to its largest branch, the fibular
artery (see below), which runs lateral and parallel to it, also within
the deep subcompartment. During its descent, the posterior tibial
artery is accompanied by the tibial nerve and veins. The artery runs
posterior to the medial malleolus, from which it is separated by the
tendons of the tibialis posterior and flexor digitorum longus. Inferior
to the medial malleolus, it runs between the tendons of the flexor
hallucis longus and flexor digitorum longus. Deep to the flexor
retinaculum and the origin of the abductor hallucis, the posterior
tibial artery divides into medial and lateral plantar arteries, the arteries of the sole of the foot.
largest and most important branch of the tibial artery, arises inferior
to the distal border of the popliteus and the tendinous arch of the
soleus (Figs. 5.38A and 5.41; Table 5.12).
It descends obliquely toward the fibula and passes along its medial
side, usually within the FHL. The fibular artery gives muscular
branches to the popliteus and other muscles in both the posterior and
the lateral compartments of the leg. It also gives rise to the nutrient artery of the fibula (Fig. 5.41).
Distally, the fibular artery gives rise to a perforating branch and
terminal lateral malleolar and calcaneal branches. The perforating
branch pierces the interosseous membrane and passes to the dorsum of the foot, where it anastomoses with the arcuate artery. The lateral calcaneal branches supply the heel, and the lateral malleolar branch joins other malleolar branches to form a periarticular arterial anastomosis of the ankle.
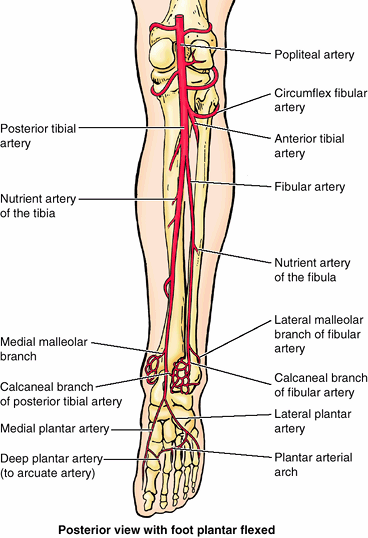 |
|
Figure 5.41. Arteries of knee, posterior leg, and sole of foot.
The popliteal artery bifurcates into the anterior and posterior tibial arteries; the latter gives rise to the fibular artery and terminates as it enters the foot, bifurcating into the medial and lateral plantar arteries. |
arises from the origin of the anterior or posterior tibial artery at
the knee and passes laterally over the neck of the fibula to the
anastomoses around the knee.
the largest nutrient artery in the body, arises from the origin of the
anterior or posterior tibial artery. It pierces the tibialis posterior,
to which it supplies branches, and enters the nutrient foramen in the
proximal third of the posterior surface of the tibia.
between the posterior surface of the medial malleolus and the medial
border of the calcaneal tendon (Fig. B5.18).
Because the posterior tibial artery passes deep to the flexor
retinaculum, it is important when palpating this pulse to have the
person invert the foot to relax the retinaculum. Failure to do so may
lead to the erroneous conclusion that the pulse is absent. Both
arteries are examined simultaneously for equality of force. Palpation
of the posterior tibial pulses is essential for examining patients with
occlusive peripheral arterial disease.
Although posterior tibial pulses are absent in approximately 15% of
normal young people, absence of posterior tibial pulses is considered
to be a sign of occlusive peripheral arterial disease in people older
than 60 years. For example, intermittent claudication,
characterized by leg pain and cramps, develops during walking and
disappears after rest. These conditions result from ischemia of the leg
muscles caused by narrowing or occlusion of the leg arteries.
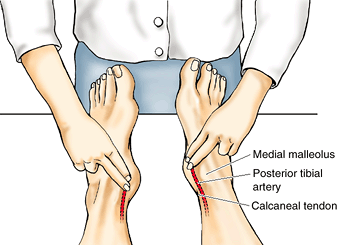 |
|
Figure B5.18
|
by the transverse intermuscular septum into superficial and deep
subcompartments. In the superficial subcompartment, the gastrocnemius
and soleus muscles (the triceps surae) share a common tendon (the
calcaneal tendon, the body’s strongest tendon). The triceps surae
provides the power of plantarflexion that propels the body in walking
and plays a major role in running and jumping via push off. The deep
muscles augment the action through flexion of the digits and support of
the longitudinal arch of the foot. The contents of the compartment are
supplied by the tibial nerve and two arteries, the (medial) posterior
tibial and fibular arteries. All three structures course within the
confined deep subcompartment, where swelling may have profound
consequences for the entire posterior compartment, the distal lateral
compartment, and the foot.
easily palpable elevation on the anterior aspect of the proximal part
of the tibia, approximately 5 cm distal to the apex of the patella (Fig. SA5.3A).
The tibial tuberosity indicates the level of the head of the fibula and
the bifurcation of the popliteal artery into the anterior and posterior
tibial arteries. The patellar ligament may
be felt as it extends from the inferior border of the apex of the
patella. It is most easily felt when the knee is extended. When the
knee flexes to a right angle, a depression may be felt on each side of
the patellar ligament. The joint cavity is superficial in these
depressions. The head of the fibula is subcutaneous and may be palpated at the posterolateral aspect of the knee, at the level of the tibial tuberosity. The neck of the fibula can be palpated just distal to the head. The tendon of the biceps femoris
may be traced by palpating its distal attachment to the lateral side of
the head of the fibula. This tendon and the neck of the fibula guide
the examining finger to the common fibular nerve (Fig. 5.37).
The nerve is indicated by a line along the biceps femoris tendon,
posterior to the head of the fibula, and around the lateral aspect of
the fibular neck to its anterior aspect, just distal to the fibular
head. The common fibular nerve can usually be palpated just posterior
to the fibular head and rolled against the fibular neck with the
fingertips.
is also subcutaneous, except at its proximal end. Its inferior third is
crossed obliquely by the great saphenous vein as it passes proximally
to the medial aspect of the knee.
superficially and is easily palpable just lateral to the anterior
border of the tibia. As the foot is inverted and dorsiflexed, the large
tendon of the TA can be seen and palpated
as it runs distally and slightly medially over the anterior surface of
the ankle joint to the medial side of the foot (Fig SA5.3C). If the 1st digit is dorsiflexed, the tendon of the EHL can be palpated just lateral to the tendon of the tibialis anterior. The tendon of the extensor hallucis brevis may also be visible. As the toes are dorsiflexed, the tendons of the EDL can be palpated lateral to the extensor hallucis longus and followed to the four lateral digits. The tendon of the FT may be palpable lateral to the tendons of the EDL, especially when the foot is dorsiflexed and everted.
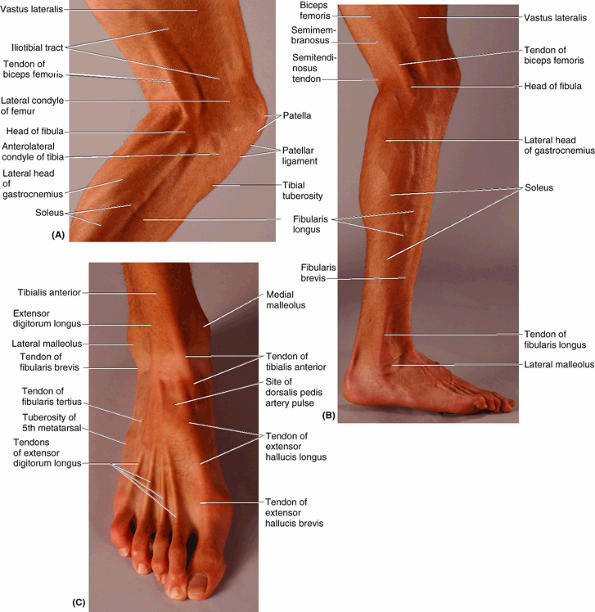 |
|
Figure SA5.3
|
are subcutaneous and prominent. Palpate them, noting that the tip of
the lateral malleolus extends farther distally and posteriorly than the
medial malleolus.
are palpable when the foot is everted as they pass around the posterior
aspect of the lateral malleolus. These tendons may be followed
anteriorly along the lateral side of the foot. The tendon of the
fibularis longus runs as far anteriorly as the cuboid and then
disappears by turning into the sole of the foot. The tendon of the FB may be traced to its attachment to the base of the 5th metatarsal.
easily followed to its attachment to the posterior part of the
calcaneus. The ankle joint is fairly superficial in the depression on
each side of the calcaneal tendon. The heads of the gastrocnemius are easily recognizable in the superior part of the calf of the leg (Fig. SA5.3A & B). The soleus can be palpated deep to and at the sides of the superior part of the calcaneal tendon. The triceps surae
(soleus and gastrocnemius together) is easy to palpate when the
individual is standing on the toes. The soleus can be distinguished
from the gastrocnemius during squatting (flexing the knees while
standing on toes) because flexion of the knee to approximately 90°
makes the gastrocnemius flaccid; plantarflexion in this position is
maintained by the soleus. The deep muscles of the posterior compartment
are not easily palpated, but their tendons can be observed just
posterior to the medial malleolus, especially when the foot is inverted
and the toes are flexed.
considerable amount of time primary care physicians devote to foot
problems. Podiatry is the specialized field that deals with the study and care of the feet.
narrowest and malleolar parts of the distal leg, proximal to the dorsum
and heel of the foot, including the ankle joint. The foot,
distal to the ankle, provides a platform for supporting the body when
standing and has an important role in locomotion. The skeleton of the
foot consists of 7 tarsals, 5 metatarsals, and 14 phalanges (Fig. 5.42; Table 5.14). The foot and its bones
may be considered in terms of three anatomical and functional parts:
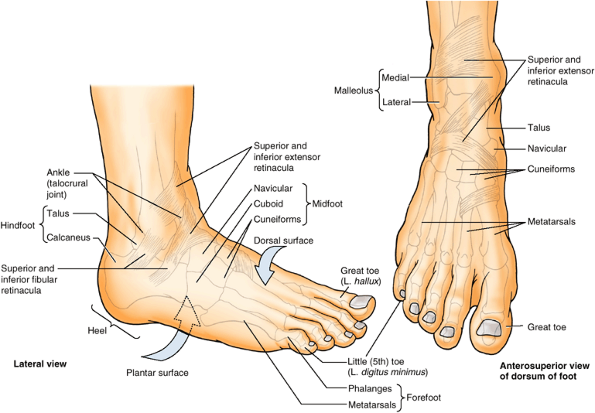 |
|
Figure 5.42. Retinacula of ankle and parts of foot.
The disposition of the bones of the foot and the superior and inferior extensor and fibular retinacula relative to surface features are demonstrated. |
|
Table 5.14-I. Muscles of the Foot: 1st and 2nd Layers of the Sole
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||
-
The hindfoot: talus and calcaneus.
-
The midfoot: navicular, cuboid, and cuneiforms.
-
The forefoot: metatarsals and phalanges.
(L. hallux) is also the 1st toe (L. digitus primus); the little toe (L. digitus minimus) is also the 5th toe (L. digitus quintus).
|
Table 5.14-II. Muscles of the Foot: 3rd and 4th layers of the Sole
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||
texture of skin, subcutaneous tissue (superficial fascia), and deep
fascia in relationship to weight bearing and distribution, ground
contact (grip, abrasion), and the need for containment or
compartmentalization.
tissue is loose deep to the dorsal skin; therefore, edema (G. oide–ma,
a swelling) is most marked over this surface, especially anterior to
and around the medial malleolus. The skin over the major weight-bearing
areas of the sole—the heel, lateral margin, and ball of the foot—is
thick. The subcutaneous tissue in the sole is more fibrous than in
other areas of the foot. Fibrous septa (highly developed skin ligaments, retinacula cutis; see Introduction)
divide this tissue into fat-filled areas, making it a shock-absorbing
pad, especially over the heel. The skin ligaments also anchor the skin
to the underlying deep fascia (plantar aponeurosis), improving the
“grip” of the sole. The skin of the sole is hairless and sweat glands
are numerous; the entire sole is sensitive (ticklish), especially the
thinner-skinned area underlying the arch.
|
Table 5.14-III. Muscles of the Foot: Dorsum of the Foot
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||
longitudinally arranged bundles of dense fibrous connective tissue
investing the central plantar muscles. It resembles the palmar
aponeurosis of the palm of the hand (Chapter 6)
but is tougher, denser, and elongated. The plantar fascia holds the
parts of the foot together, helps protect the sole from injury, and
helps support the longitudinal arches of the foot.
calcaneus and functions like a superficial ligament. Distally, the
longitudinal bundles of collagen fibers of the aponeurosis divide into
five bands that become continuous with the fibrous digital sheaths
that enclose the flexor tendons that pass to the toes. At the anterior
end of the sole, inferior to the heads of the metatarsals, the
aponeurosis is reinforced by transverse fibers forming the superficial transverse metatarsal ligament.
-
The medial compartment of the sole is covered superficially by thinner medial plantar fascia. It contains the
P.663
abductor hallucis, flexor hallucis brevis, the tendon of the flexor hallucis longus, and the medial plantar nerve and vessels.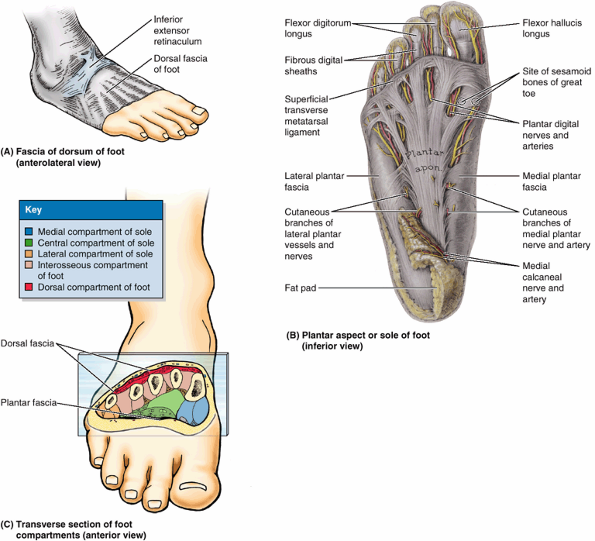 Figure 5.43. Fascia and compartments of foot. A. The skin and subcutaneous tissue have been removed to demonstrate the deep fascia of the leg and dorsum of the foot. B.
Figure 5.43. Fascia and compartments of foot. A. The skin and subcutaneous tissue have been removed to demonstrate the deep fascia of the leg and dorsum of the foot. B.
The deep plantar fascia consists of the thick plantar aponeurosis and
the thinner medial and lateral plantar fascia. The aponeurosis consists
of longitudinal bands of dense fibrous connective tissue. Thinner parts
of the plantar fascia have been removed, revealing the plantar digital
vessels and nerves. C. The bones and
muscles of the foot are surrounded by the deep dorsal and plantar
fascia. A large central and smaller medial and lateral compartments of
the sole are created by intermuscular septa that extend deeply from the
plantar aponeurosis. -
The central compartment of the sole is covered superficially by the dense plantar aponeurosis.
It contains the flexor digitorum brevis, the tendons of the flexor
hallucis longus and flexor digitorum longus plus the muscles associated
with the latter, the quadratus plantae and lumbricals, and the adductor
hallucis. The lateral plantar nerve and vessels are also located here. -
The lateral compartment of the sole is covered superficially by the thinner lateral plantar fascia and contains the abductor and flexor digiti minimi brevis.
is surrounded by the plantar and dorsal interosseous fascias. It
contains the metatarsals, the dorsal and plantar interosseous muscles,
and the deep plantar and metatarsal vessels. Whereas the plantar
interossei and plantar metatarsal vessels are distinctly plantar in
position, the remaining structures of the compartment are located
intermediate between the plantar and the dorsal aspects of the foot.
lies between the dorsal fascia of the foot and the tarsal bones and the
dorsal interosseous fascia of the midfoot and forefoot. It contains the
muscles (extensors hallucis brevis and extensor digitorum brevis) and
neurovascular structures of the dorsum of the foot.
may result from running and high-impact aerobics, especially when
inappropriate footwear is worn. Plantar fasciitis is the most common
hindfoot problem in runners (Middleton and Kolodon, 1992).
It causes pain on the plantar surface of the heel and on the medial
aspect of the foot. The pain is often most severe after sitting and
when beginning to walk in the morning, but dissipates after 5–10
minutes of activity, often recurring again following rest. Point
tenderness is located at the proximal attachment of the aponeurosis to
the medial tubercle of the calcaneus and on the medial surface of this
bone. The pain increases with passive extension of the great toe and
may be further exacerbated by dorsiflexion of the ankle and/or weight
bearing. If a calcaneal spur (abnormal
bony process) protrudes from the medial tubercle, plantar fasciitis is
likely to cause pain on the medial side of the foot when walking (Fig. B5.19). Usually a bursa develops at the end of the spur that may also become inflamed and tender.
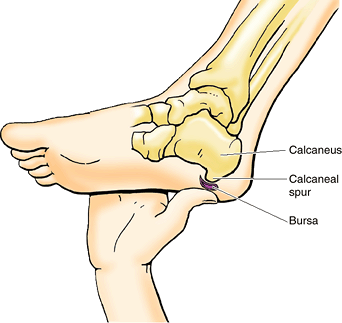 |
|
Figure B5.19
|
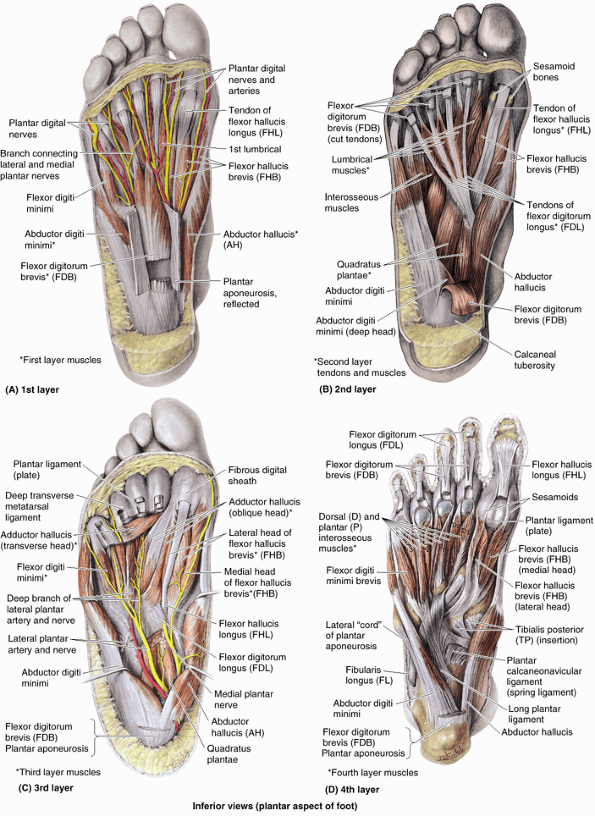 |
|
Figure 5.44. Layers of plantar muscles. A. The 1st layer consists of the abductors of the large and small toes, and the short flexor of the toes. B. The 2nd layer consists of the long flexor tendons and associated muscles: four lumbricals and the quadratus plantae. C.
The 3rd layer consists of the flexor of the little toe and the flexor and adductor of the great toe. Also demonstrated are the neurovascular structures that course in a plane between the 1st and 2nd layers. D. The 4th layer consists of the dorsal and plantar interosseous muscles. |
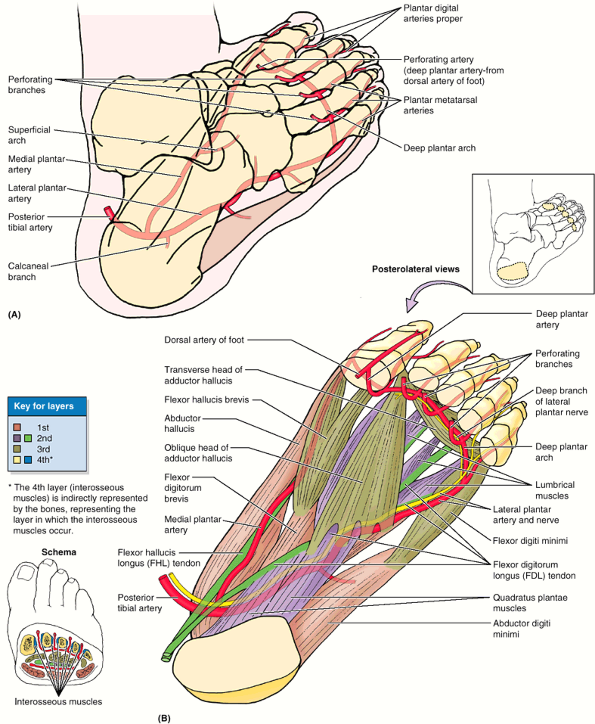 |
|
Figure 5.45. Arteries and muscle layers of foot. A and B.
The posterior tibial artery terminates as it enters the foot by dividing into the medial and lateral plantar arteries. Observe the distal anastomoses of these vessels with the deep plantar artery from the dorsal artery of the foot and the perforating branches to the arcuate artery on the dorsum of the foot (Fig. 5.47). Note that the plantar arteries enter and run in the plane between the 1st and the 2nd layers, with the lateral plantar artery passing from medial to lateral. The deep branches of the artery then pass from lateral to medial between the 3rd and the 4th layers. |
on the plantar aspect, 2 are on the dorsal aspect, and 4 are
intermediate in position. From the plantar aspect, muscles of the sole
are arranged in four layers within four compartments. The muscles of
the foot are illustrated and their attachments, innervation, and
actions are described by compartment and by layer in Figures 5.43C, 5.44, and 5.45B and Table 5.14.
plantar muscles function primarily as a group during the support phase
of stance, maintaining the arches of the foot (Table 5.2).
They basically resist forces that tend to reduce the longitudinal arch
as weight is received at the heel (posterior end of the arch) and is
then transferred to the ball of the foot and great toe (anterior end of
the arch). The muscles become most active in the later portion of the
movement to stabilize the foot for propulsion (push off), a time when
forces also tend to flatten the foot’s transverse arch. Concurrently,
they are also able to refine further the efforts of the long muscles,
producing supination and pronation in enabling the platform of the foot
to adjust to uneven ground. The muscles of the foot are of little
importance individually because fine control of the individual toes is
not important to most people. Rather than producing actual movement,
they are most active in fixing the foot or in increasing the pressure
applied against the ground by various aspects of the sole or toes to
maintain balance.
adductor hallucis is probably most active during the push-off phase of
stance in pulling the lateral four metatarsals toward the great toe,
fixing the transverse arch of the foot, and resisting forces that would
spread the metatarsal heads as weight and force are applied to the
forefoot (Table 5.2).
-
Plantar interossei ADduct (PAD) and arise from a single metatarsal as unipennate muscles.
-
Dorsal interossei ABduct (DAB) and arise from two metatarsals as bipennate muscles.
(1) a superficial one between the 1st and the 2nd muscular layers, and
(2) a deep one between the 3rd and the 4th muscular layers. The tibial nerve divides posterior to the medial malleolus into the medial and lateral plantar nerves (Figs. 5.38A and 5.46; Table 5.15).
These nerves supply the intrinsic muscles of the plantar aspect of the
foot. The medial plantar nerve courses within the medial compartment of
the sole between the 1st and the 2nd muscle layers. Initially, the
lateral plantar artery and nerve run laterally between the muscles of
the 1st and 2nd layers of plantar muscles (Figs. 5.44C and 5.45B). Their deep branches then pass medially between the muscles of the 3rd and 4th layers (Fig. 5.45B).
These thin, broad muscles form a fleshy mass on the lateral part of the
dorsum of the foot, anterior to the lateral malleolus. The EHB is
actually part of the EDB. Its small fleshy belly may be felt when the
toes are extended.
are arranged in four layers and divided into four fascial compartments.
A tough plantar aponeurosis overlies the central compartment, passively
contributing to arch maintenance and, along with firmly bound fat,
protecting the vessels and nerves from compression. There is similarity
to the arrangement of muscles in the palm of the hand, but the muscles
of the foot generally respond as a group rather than individually,
acting to fix the foot or push a portion of it harder against the
ground to maintain balance. The movements of abduction and adduction
produced by the interossei are toward or away from the 2nd digit. The
foot has two intrinsic muscles on its dorsum that augment the long
extensor muscles. The plantar intrinsic muscles function throughout the
stance phase of gait, from heel strike to toe off, resisting forces
that tend to spread the arches of the foot. They are especially active
in fixing the medial forefoot for the propulsive push off. The plantar
intrinsic muscles are innervated by the medial and lateral plantar
nerves, whereas the dorsal muscles are innervated by the deep fibular
nerve.
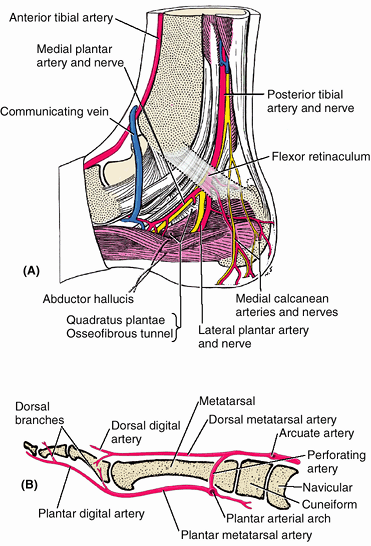 |
|
Figure 5.46. Arteries of foot: branching and communicating. A.
The arteries of the midfoot and forefoot resemble those of the hand in that (1) arches on the two aspects give rise to metatarsal (metacarpal) arteries, which in turn give rise to digital arteries; (2) the dorsal arteries are exhausted before reaching the distal ends of the digits, so the plantar (palmar) digital arteries send branches dorsally to supply the distal dorsal aspects of the digits, including the nail beds; and (3) perforating branches extend between the metatarsals (metacarpals) forming anastomoses between the arches of each side. B. The parent neurovascular structures giving rise to plantar vessels and nerves pass posterior to the medial malleolus and then divide, their terminal plantar branches entering the sole by passing deep to the abductor hallucis and coursing between the 1st and the 2nd muscle layers of the sole. |
climates, and cultures where shoes are less commonly worn. A neglected
puncture wound may lead to an extensive deep infection, resulting in
swelling, pain, and fever. Deep infections of the foot often localize
within the compartments between the muscular layers. A well-established
infection in one of the enclosed fascial or muscular spaces usually
requires surgical incision and drainage. When possible, the incision is
made on the medial side of the foot, passing superior to the abductor
hallucis to allow visualization of critical neurovascular structures,
while avoiding production of a painful scar in a weight-bearing area.
|
Table 5.15. Nerves of the Foot
|
|||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||
unimportant. Clinically, knowing the location of the belly of the EDB
is important for distinguishing it from abnormal edema. Contusion and
tearing of the muscle’s fibers and associated blood vessels result in a
hematoma, producing edema anteromedial to
the lateral malleolus. Most people who have not seen this inflamed
muscle assume they have a severely sprained ankle.
-
Medially by the saphenous nerve, which extends distally to the head of 1st metatarsal.
-
Superiorly (dorsum of foot) by the superficial (primarily) and deep fibular nerves.
-
Inferiorly (sole of foot) by the medial
and lateral plantar nerves; the common border of their distribution
extends along the 4th metacarpal and digit. (This is similar to the
pattern of innervation of the palm; see Chapter 6.) -
Laterally by the sural nerve, including part of the heel.
-
Posteriorly (heel) by calcaneal branches of the tibial and sural nerves.
largest (longest and most widely distributed) cutaneous branch of the
femoral nerve; it is the only branch to extend beyond the knee (Fig. 5.48B; Table 5.1).
In addition to supplying the skin and fascia on the anteromedial aspect
of the leg, the saphenous nerve passes anterior to the medial malleolus
to the dorsum of the foot, where it supplies articular branches to the
ankle joint and continues to supply skin along the medial side of the
foot as far anteriorly as the head of the 1st metatarsal (Table 5.15).
emerges as a cutaneous nerve about two thirds of the way down the leg.
It then supplies the skin on the anterolateral aspect of the leg and
divides into the medial and intermediate dorsal cutaneous nerves,
which continue across the ankle to supply most of the skin on the
dorsum of the foot. Its terminal branches are the dorsal digital nerves
(common and proper) that supply the skin of the proximal aspect of the
medial half of the great toe and that of the lateral three and a half
digits.
passes deep to the extensor retinaculum and supplies the intrinsic
muscles on the dorsum of the foot (extensors digitorum and hallucis
longus) and the tarsal and tarsometatarsal joints. When it finally
emerges as a cutaneous nerve, it is so far distal in the foot that only
a small area of skin remains available for innervation: the web of skin
between and contiguous sides of the 1st and 2nd toes. It innervates
this area as the 1st common dorsal (and then proper dorsal) digital nerve(s).
the larger and more anterior of the two terminal branches of the tibial
nerve, arises deep to the flexor retinaculum and enters the sole of the
foot by passing deep to the abductor hallucis (Figs. 5.44C and 5.46B).
It then runs anteriorly between this muscle and the flexor digitorum
brevis, supplying both with motor branches on the lateral side of the
medial plantar artery (Fig. 5.44A and C).
After sending motor branches to the flexor hallucis brevis and 1st
lumbrical muscle, the medial plantar nerve terminates near the bases of
the metatarsals by dividing into three sensory branches (common plantar
digital nerves). These branches supply the skin of the medial three and
a half digits (including the dorsal skin and nail beds of their distal
phalanges), and the skin of the sole proximal to them. Compared to the
other terminal branch of the tibial nerve, the medial plantar nerve
supplies more skin area but fewer muscles. Its distribution to both
skin and muscles of the foot is comparable to that of the median nerve
in the hand (Chapter 6).
The superficial branch divides, in turn, into two plantar digital
nerves (one common and one proper) that supply the skin of the plantar
aspects of the lateral one and a half digits, the dorsal skin and nail
beds of their distal phalanges, and skin of the sole proximal to them.
The deep branches of the lateral plantar nerve course with the plantar
arterial arch between the 3rd and the 4th muscle layers. The
superficial and deep branches supply all muscles of the sole not
supplied by the medial plantar
nerve.
Compared to the latter, the lateral plantar nerve supplies less skin
area but more individual muscles. Its distribution to both skin and
muscles of the foot is comparable to that of the ulnar nerve in the
hand (Chapter 6). The medial and lateral plantar nerves also provide innervation to the plantar aspects of all the joints of the foot.
The level of junction of these branches is variable; it may be high (in
the popliteal fossa) or low (proximal to heel), and sometimes the
branches do not join and, therefore, no sural nerve is formed. In these
people, the skin normally innervated by the sural nerve is supplied by
the medial and lateral sural cutaneous branches. The sural nerve
accompanies the small saphenous vein and enters the foot posterior to
the lateral malleolus to supply the ankle joint and skin along the
lateral margin of the foot (Table 5.15).
grafts in procedures such as repairing nerve defects resulting from
wounds. The surgeon is usually able to locate this nerve in relation to
the small saphenous vein (Fig. 5.48B).
Because of the variations in the level of formation of the sural nerve,
the surgeon may have to make incisions in both legs, and then select
the better specimen.
fascia to become a cutaneous nerve, it divides into medial and
intermediate cutaneous nerves. In thin people, these branches can often
be seen or felt as ridges under the skin when the foot is
plantarflexed. Injections of an anesthetic agent around these branches
in the ankle region, anterior to the palpable portion of the fibula,
anesthetizes the skin on the dorsum of the foot (except the web between
and adjacent surfaces of the 1st and 2nd toes) more broadly and
effectively than more local injections on the dorsum of the foot for
superficial surgery.
S1, and S2 nerve roots) is a myotatic (deep tendon) reflex that is
routinely tested during neurologic examinations. The lateral aspect of
the sole of the foot is stroked with a blunt object, such as a tongue
depressor, beginning at the heel and crossing to the base of the great
toe. The motion is firm and continuous but neither painful nor
ticklish. Flexion of the toes is a normal response. Slight fanning of
the lateral four toes and dorsiflexion of the great toe is an abnormal
response (Babinski sign), indicating brain
injury or cerebral disease, except in infants. Because the
corticospinal tracts are not fully developed in newborns, a Babinski
sign is usually elicited and may be present until children are 4 years
of age.
passes deep to the flexor retinaculum or curves deep to the abductor
hallucis may cause aching, burning, numbness, and tingling
(paresthesia) on the medial side of the sole and in the region of the
navicular tuberosity. Medial plantar nerve compression
may occur during repetitive eversion of the foot (e.g., during
gymnastics and running). Because of its frequency in runners, these
symptoms have been called “jogger’s foot.”
innervation from the superficial fibular nerve, the exception being the
skin of the web between and the adjacent sides of the 1st and 2nd toes.
The latter receives innervation from the deep fibular nerve after it
supplies the muscles on the dorsum of the foot. The skin of the medial
and lateral sides of the foot is innervated by the saphenous and sural
nerves, respectively. The plantar aspect of the foot receives
innervation from the larger medial and smaller lateral plantar nerves,
the former supplying more skin (the plantar aspect of the medial three
and half toes and adjacent sole) but fewer muscles (the medial hallux
and 1st lumbrical muscles only) than the latter, which supplies the
remaining muscles and skin of the plantar aspect. The distribution of
the medial and lateral plantar nerves is comparable to that of the
median and ulnar nerves in the palm.
a major source of blood supply to the forefoot (e.g., during extended
periods of standing)—is the direct continuation of the anterior tibial
artery (Fig. 5.47A).
The dorsal artery begins midway between the malleoli and runs
anteromedially, deep to the inferior extensor retinaculum between the
extensor hallucis longus and the extensor digitorum longus tendons on
the dorsum of the foot. The dorsal artery passes to the first
interosseous space, where
it divides into the 1st dorsal metatarsal artery and a deep plantar artery.
The latter passes deeply between the heads of the first dorsal
interosseous muscle to enter the sole of the foot, where it joins the
lateral plantar artery to form the deep plantar arch (Fig. 5.47B).
The course and destination of the dorsal artery and its major
continuation, the deep plantar artery, are comparable to the radial
artery of the hand, which completes a deep arterial arch in the palm (Chapter 6).
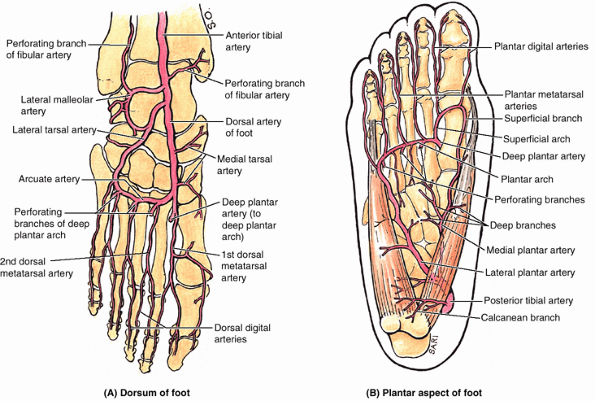 |
|
Figure 5.47. Arteries of foot: overview. A. Observe the anterior tibial artery becoming the dorsal artery of the foot (L. arteria dorsalis pedis) and the arcuate artery. B.
Observe the posterior tibial artery and its terminal branches, the medial and lateral plantar arteries. The deep plantar arch is formed by the lateral plantar artery. Note the anastomoses between the dorsal and the plantar arteries through the deep plantar artery and perforating branches of the deep plantar arch. |
branch of the dorsal artery of the foot, runs laterally in an arched
course beneath the extensor digitorum brevis to supply this muscle and
the underlying tarsals and joints (Fig. 5.47A). It anastomoses with other branches, such as the arcuate artery.
laterally across the bases of the lateral four metatarsals, deep to the
extensor tendons, to reach the lateral aspect of the forefoot where it
may anastomose with the lateral tarsal artery to form an arterial loop.
The arcuate artery gives rise to the 2nd, 3rd, and 4th dorsal metatarsal arteries.
These vessels run distally to the clefts of the toes and are connected
to the plantar arch and to the plantar metatarsal arteries by perforating branches (Figs. 5.45A & B, 5.46A, and 5.47B). Distally, each dorsal metatarsal artery divides into two dorsal digital arteries for the dorsal aspect of the sides of adjoining toes (Fig. 5.47A); however, these arteries generally end proximal to the distal interphalangeal joint (Fig. 5.46A) and are replaced by or receive replenishment from dorsal branches of the plantar digital arteries.
is evaluated during a physical examination of the peripheral vascular
system. Dorsalis pedis pulses may be palpated with the feet slightly
dorsiflexed. The pulses are usually easy to palpate because the dorsal
arteries of the foot are subcutaneous and pass along a line from the
extensor retinaculum to a point just lateral to the EHL tendons (Swartz, 2002) (Fig. B5.20).
A diminished or absent dorsalis pedis pulse usually suggests vascular
insufficiency resulting from arterial disease. The five P signs of acute arterial occlusion are pain, pallor, paresthesia, paralysis, and pulselessness. Some healthy adults (and even children) have congenitally non-palpable dorsalis pedis pulses;
the variation is usually bilateral. In these cases, the dorsal artery
of the foot is replaced by an enlarged perforating fibular artery.
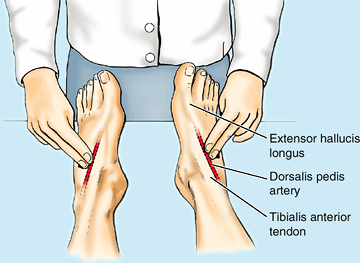 |
|
Figure B5.20
|
derived from the posterior tibial artery, which divides deep to the
flexor retinaculum (Figs. 5.44A, 5.46B, and 5.47B).
The terminal branches pass deep to the abductor hallucis as the medial
and lateral plantar arteries, which accompany the similarly named
nerves.
the smaller terminal branch of the posterior tibial artery. It gives
rise to a deep branch (or branches) that supplies mainly muscles of the
great toe. The larger superficial branch of the medial plantar artery
supplies the skin on the medial side of the sole and has digital
branches that accompany digital branches of the medial plantar nerve,
the more lateral of which anastomose with medial plantar metatarsal
arteries. Occasionally, a superficial plantar arch is formed when the superficial branch anastomoses with the lateral plantar artery or the (deep) plantar arch.
It runs laterally and anteriorly, at first deep to the adductor
hallucis and then between the flexor digitorum brevis and quadratus
plantae (Figs. 5.44C and 5.45B). The lateral plantar artery arches medially across the foot with the deep branch of the lateral plantar nerve to form the deep plantar arch, which is completed by union with the deep plantar artery, a branch of the dorsal artery of the foot (Figs. 5.44C, 5.45, and 5.47B). As it crosses the foot, the deep plantar arch gives rise to four plantar metatarsal arteries; three perforating branches (Figs. 5.45, 5.46A, and 5.47B);
and many branches to the skin, fascia, and muscles in the sole. The
plantar metatarsal arteries divide near the base of the proximal
phalanges to form the plantar digital arteries,
supplying the adjacent digits; the more medial metatarsal arteries are
joined by superficial digital branches of the medial plantar artery.
The plantar digital arteries typically provide most of the blood
reaching the distal toes, including the nail bed, via perforating and
dorsal branches (Fig. 5.46A)—an arrangement that also occurs in the fingers.
deep plantar arch and its branches usually result in severe bleeding,
typically from both ends of the cut artery because of the abundant
anastomoses. Ligature of the arch is difficult because of its depth and
the structures that surround it.
branches of the anterior and posterior tibial arteries, respectively.
The dorsal artery of the foot supplies all of the dorsum of the foot
and, via the arcuate artery, the proximal dorsal aspect of the toes. It
also contributes to formation of the plantar (arterial) arch via its
terminal deep plantar artery. The smaller medial and larger lateral
plantar arteries supply the plantar aspect of the foot, the latter
running in vascular planes between the 1st and 2nd and then, as the
plantar arch, the 3rd and 4th layers of the intrinsic muscles.
Anastomoses between the dorsal and the plantar arteries are abundant
and important for the health of the foot. Except for the scarcity of a
superficial arch, the arterial pattern of the foot is similar to that
of the hand.
superficial and deep veins in the foot. The deep veins take the form of
interanastomosing paired veins accompanying all arteries internal to
the deep fascia (Fig. 5.48A). The superficial veins are subcutaneous and unaccompanied by arteries (Fig. 5.48B).
Unlike the leg and thigh, however, the venous drainage in the foot is
primarily to the major superficial veins, both from the deep
accompanying veins and other smaller superficial veins. Perforating
veins begin the one-way shunting of blood from superficial to deep
veins, a pattern essential to operation of the musculovenous pump (see “Venous Drainage of the Lower Limb,” in this chapter), proximal to the ankle joint. Most blood is drained from the foot through the superficial veins.
covers the remainder of the dorsum of the foot. Both the arch and the
network are located in the subcutaneous tissue. For the main part,
superficial veins from a plantar venous network
either drain around the medial border of the foot to converge with the
medial part of the dorsal venous arch and network to form a medial marginal vein, which becomes the great saphenous vein, or drain around the lateral margin to converge with the lateral part of the dorsal venous arch and network to form the lateral marginal vein, which becomes the small saphenous vein (Fig. 5.48B).
Perforating veins from the great and small saphenous veins then
continuously shunt blood deeply as they ascend to take advantage of the
musculovenous pump.
plexuses. The collecting vessels consist of superficial and deep
lymphatic vessels that follow the superficial veins and major vascular
bundles, respectively. Superficial lymphatic vessels are most numerous
in the sole. The medial superficial lymphatic vessels, larger and more numerous than the lateral ones, drain the medial side of the dorsum and sole of the foot (Fig. 5.4). These vessels converge on the great saphenous vein and accompany it to the vertical group of superficial inguinal lymph nodes, located along the vein’s termination, and then to the deep inguinal lymph nodes along the proximal femoral vein. The lateral superficial lymphatic vessels
drain the lateral side of the dorsum and sole of the foot. Most of
these vessels pass posterior to the lateral malleolus and accompany the
small saphenous vein to the popliteal fossa, where they enter the popliteal lymph nodes (Fig. 5.12). The deep lymphatic vessels
from the foot follow the main blood vessels: fibular, anterior and
posterior tibial; then popliteal and femoral. The deep vessels from the
foot also drain into the popliteal lymph nodes. Lymphatic vessels from
them follow the femoral vessels, carrying lymph to the deep inguinal
lymph nodes. From the deep inguinal nodes, all lymph from the lower
limb passes deep to the inguinal ligament to the iliac nodes.
without popliteal lymphadenopathy can result from infection of medial
side of the foot, leg, or thigh; however, enlargement of these nodes
can also result from an infection or tumor in the vulva, penis,
scrotum, perineum, and gluteal region and from terminal parts of the
urethra, anal canal, and vagina.
superficial route, draining to the dorsum of the foot and then medially
via the greater or laterally via the lesser saphenous veins. From these
veins, blood is shunted by perforating veins to the deep veins of the
leg and thigh that participate in the musculovenous pump. The
lymphatics carrying lymph from the foot drain toward and then along the
superficial veins draining the foot. Lymph from the medial foot follows
the greater saphenous vein and drains directly to superficial inguinal
lymph nodes. Lymph from the lateral foot follows the lesser saphenous
vein and drains initially to the popliteal lymph nodes and then by deep
lymphatic channels to the deep inguinal nodes.
of the pelvic girdle—lumbosacral joints, sacroiliac joints, and pubic
symphysis, which are discussed in Chapter 3. The remaining joints of the lower limb are the hip joint, knee joint, tibiofibular joints, ankle joint, and foot joints (Fig. 5.50).
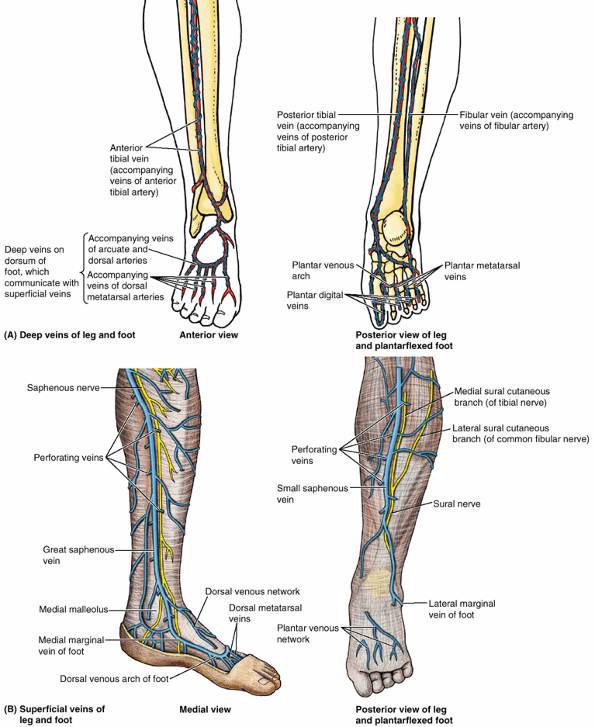 |
|
Figure 5.48. Veins of leg and foot. A. The deep veins accompany the arteries and their branches (L. venae comitantes); they anastomose frequently and have numerous valves. B.
The main superficial veins are the great and small saphenous veins, which drain into the deep veins as they ascend the limb by means of perforating veins so that muscular compression can propel blood toward the heart against the pull of gravity. Note that the distal great saphenous vein is accompanied by the saphenous nerve, and the small saphenous vein is accompanied by the sural nerve and its medial root (medial sural cutaneous nerve). |
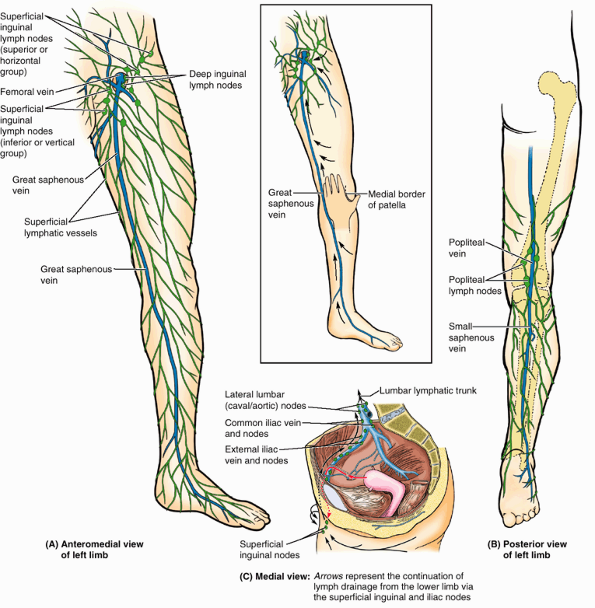 |
|
Figure 5.49. Lymphatic drainage of foot. A.
Superficial lymphatic vessels from the medial foot drain are joined by those from the anteromedial leg in draining to the superficial inguinal lymph nodes via lymphatics that accompany the greater saphenous vein. B. Superficial lymphatic vessels from the lateral foot join those from the posterolateral leg, converging to vessels accompanying the lesser saphenous vein and draining into the popliteal lymph nodes. The popliteal lymph nodes drain via lymphatics accompanying the femoral vein to the deep inguinal lymph nodes. |
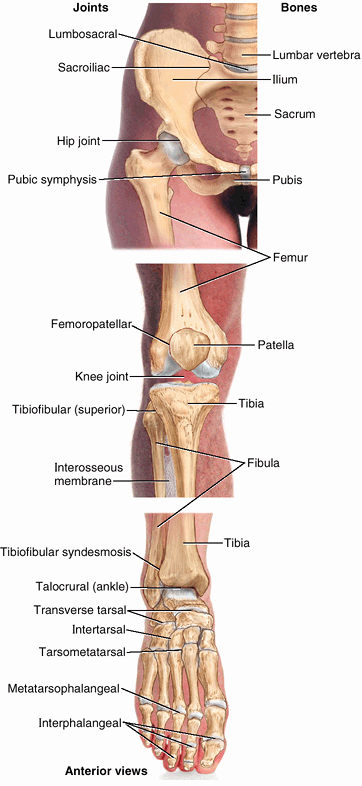 |
|
Figure 5.50. Joints of lower limb.
The joints are those of the pelvic girdle connecting the free lower limb to the vertebral column, the knee, the tibiofibular articulations, and the many joints of the foot. |
connection between the lower limb and the pelvic girdle. It is a strong
and stable multiaxial ball and socket type of synovial joint. The
femoral head is the ball, and the acetabulum is the socket (Fig. 5.51).
The hip joint is designed for stability over a wide range of movement.
Next to the glenohumeral (shoulder) joint, it is the most movable of
all joints. During standing, the entire weight of the upper body is
transmitted through the hip bones to the heads and necks of the femurs.
The acetabular rim and lunate surface form approximately three quarters
of a circle; the missing inferior segment of the circle is the acetabular notch.
a continuation of the acetabular labrum, bridges the acetabular notch.
As a result of the height of the rim and labrum, more than half of the
femoral head fits within the acetabulum (Fig. 5.52C).
In other words, the acetabular labrum enables the acetabulum to “grasp”
the femoral head beyond its equator; thus during dissection, the
femoral head must be cut from the acetabular rim to enable
disarticulation of the joint. Centrally a deep non-articular part,
called the acetabular fossa, is formed mainly by the ischium (Figs. 5.51 and 5.52C). This fossa is thin walled (often translucent) and continuous inferiorly with the acetabular notch.
anteriorly in humans. The weight-bearing iliac portion of the
acetabular rim overlies the femoral head, which is important for
transfer of weight to the femur in the erect (standing/walking)
position (Figs. 5.50A and 5.52C).
Consequently, of the positions commonly assumed by humans, the hip
joint is mechanically most stable when a person is bearing weight, as
when lifting a heavy object, for example. Decreases in the degree to
which the ilium overlies the femoral head (detectable radiographically
as the angle of Wiberg) may indicate joint
instability. Because of the anterior direction the axis of the
acetabulum and the posterior direction of the axis of the femoral head
and neck as it extends laterally (owing to the torsion angle—discussed
earlier in this chapter), there is an angle of 30–40° between their
axes (Fig. B5.21). Consequently, the articular
surfaces of the head and acetabulum are not fully congruent in the
erect (bipedal) posture. The anterior part of the femoral head is
“exposed” and articulates mostly with the joint capsule (Figs. 5.52B, 5.53A, and 5.56).
Nonetheless, rarely is <40% of the available articular surface of
the femoral head in contact with the surface of the acetabulum in any
position. Relative to other joints and in view of the large size of the
hip joint, this is extensive contact, contributing considerably to the
joint’s great stability.
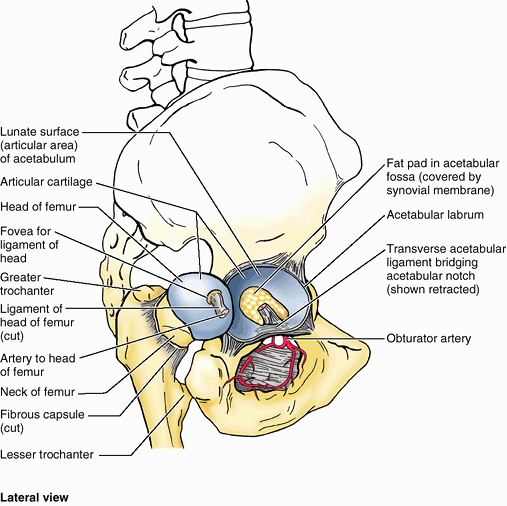 |
|
Figure 5.51. Hip joint.
The hip joint was disarticulated by cutting the ligament of the head of the femur and retracting the head from the acetabulum. The transverse acetabular ligament is retracted superiorly to show the obturator canal, which transmits the obturator nerve and vessels passing from the pelvic cavity to the medial thigh. |
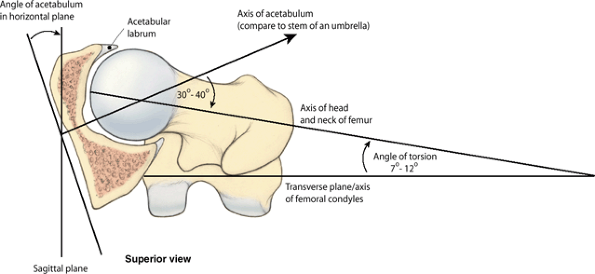 |
|
Figure B5.21
|
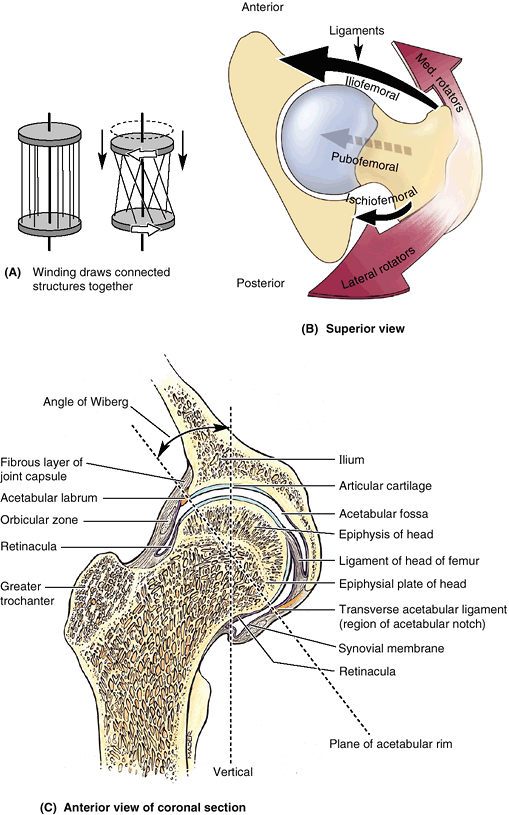 |
|
Figure 5.52. Factors increasing stability of hip joint. A.
Parallel fibers linking two discs resemble those making up the tube-like fibrous layer of the hip joint capsule. When one disc (the femur) rotates relative to the other (the acetabulum), the fibers become increasingly oblique and draw the two discs together. Similarly, extension of the hip joint winds (increases the obliquity of) the fibers of the fibrous layer, pulling the head and neck of the femur tightly into the acetabulum, increasing the stability of the joint. Flexion unwinds the fibers of the capsule. B. This transverse section through the hip joint demonstrates the medial and reciprocal pull of the periarticular muscles (medial and lateral rotators; reddish brown arrows) and intrinsic ligaments of the hip joint (black arrows) on the femur. Relative strengths are indicated by arrow width: Anteriorly, the muscles are less abundant but the ligaments are robust; posteriorly, the muscles predominate. C. In this coronal section of hip joint, the acetabular labrum and transverse acetabular ligament, spanning the acetabular notch (and included in the plane of section here), extend the acetabular rim so that a complete socket is formed. Thus the acetabular complex engulfs the head of the femur. The epiphysis of the femoral head is entirely within the joint capsule. The thick weight-bearing bone of the ilium normally lies directly superior to the head of the femur for efficient transfer of weight to the femur (Fig. 5.3). The angle of Wiberg (see text) is used radiographically to determine the degree to which the acetabulum overhangs the head of the femur. |
head are most congruent when the hip is flexed 90°, abducted 5°, and
rotated laterally 10° (the position in which the axis of the acetabulum
and the axis of the femoral head and neck are aligned), which is the
quadruped position! In other words, in assuming the upright position, a
relatively small degree of joint stability was sacrificed to maximize
weight bearing when erect. Even so, the hip joint is our most stable
joint, owing also to its complete ball and socket construction (depth
of the socket); the strength of its capsule; and the attachments of
muscles crossing the joint, many of which are located at some distance
from the center of movement (Palastanga et al., 2002).
Proximally, the fibrous layer attaches to the acetabulum, just
peripheral to the rim to which the labrum is attached, and to the
transverse acetabular ligament (Figs. 5.51, 5.52C, and 5.53). Distally, the fibrous layer attaches to the femoral neck only anteriorly at the intertrochanteric line and root of the greater trochanter (Fig. 5.55B). Posteriorly, the fibrous layer crosses the neck proximal to the intertrochanteric crest but is not attached to it (Fig. 5.55C).
from the hip bone to the intertrochanteric line, but some deep fibers
pass circularly around the neck, forming the orbicular zone. Thick parts of the fibrous layer of the capsule form the ligaments of the hip joint,
which pass in a spiral fashion from the pelvis to the femur. Extension
winds its spiraling ligaments and fibers more tightly, constricting the
capsule and drawing the femoral head tightly into the acetabulum (Fig. 5.52A).
The tightened fibrous layer increases the stability of the joint, but
restricts extension of the joint to 10–20° beyond the vertical
position. Flexion increasingly unwinds the spiraling ligaments and
fibers. This permits considerable flexion of the hip joint with
increasing mobility.
-
Anteriorly and superiorly is the strong, Y-shaped iliofemoral ligament
(Bigelow ligament), which attaches to the anterior inferior iliac spine
and the acetabular rim proximally and the intertrochanteric line
distally (Fig. 5.53A & B).
Said to be the body’s strongest ligament, the iliofemoral ligament
specifically prevents hyperextension of the hip joint during standing
by screwing the femoral head into the acetabulum via the mechanism
described above. -
Anteriorly and inferiorly is the pubofemoral ligament,
which arises from the obturator crest of the pubic bone and passes
laterally and inferiorly to merge with the fibrous layer of the joint
capsule (Fig. 5.53A).
This ligament blends with the medial part of the iliofemoral ligament
and tightens during both extension and abduction of the hip joint. The
pubofemoral ligament prevents overabduction of the hip joint. -
Posteriorly is the ischiofemoral ligament, which arises from the ischial part of the acetabular rim (Fig. 5.53C).
The weakest of the three ligaments, it spirals superolaterally to the
femoral neck, medial to the base of the greater trochanter.
The ligaments and periarticular muscles (the medial and lateral
rotators of the thigh) play a vital role in maintaining the structural
integrity of the joint, as demonstrated in the above figure. Both
muscles and ligaments pull the femoral head medially into the
acetabulum, and they are reciprocally balanced when doing so. The
medial flexors, located anteriorly, are fewer, weaker, and less
mechanically advantaged, whereas the anterior ligaments are strongest.
Conversely, the ligaments are weaker posteriorly where the medial
rotators are abundant, stronger, and more mechanically advantaged.
internal surfaces of the fibrous layer as well as any intracapsular
bony surfaces not lined with articular cartilage. Thus in the hip
joint, where the fibrous layer attaches to the femur distant from the
articular cartilage covering the femoral head, the synovial membrane of the hip joint reflects proximally along the femoral neck to the edge of the femoral head. Longitudinal synovial folds (retinacula) occur in the membrane covering the femoral neck (Fig. 5.52C). Subsynovial retinacular arteries
(branches of the medial, and a few of the lateral, circumflex femoral
artery) that supply the femoral head and neck course within the
synovial folds (Fig. 5.54).
primarily a synovial fold conducting a blood vessel, is weak and of
little importance in strengthening the hip joint. Its wide end attaches
to the margins of the acetabular notch and the transverse acetabular ligament; its narrow end attaches to the fovea for the ligament of the head. Usually, the ligament contains a small artery to the head of the femur. A fat pad in the acetabular fossa
fills the part of the acetabular fossa that is not occupied by the
ligament of the femoral head. Both the ligament and the fat-pad are
covered with synovial membrane. The malleable nature of the fat-pad
permits it to change shape to accommodate the variations in the
congruity of the femoral head and acetabulum as well as changes in the
position of the ligament of the head during joint movements. A synovial protrusion
beyond the free margin of the joint capsule onto the posterior aspect
of the femoral neck forms a bursa for the obturator externus tendon. (Fig. 5.53C)
Movements of the trunk at the hip joints are also important, such as
those occurring when a person lifts the trunk from the supine position
during sit-ups or keeps the pelvis level when one foot is off the
ground.
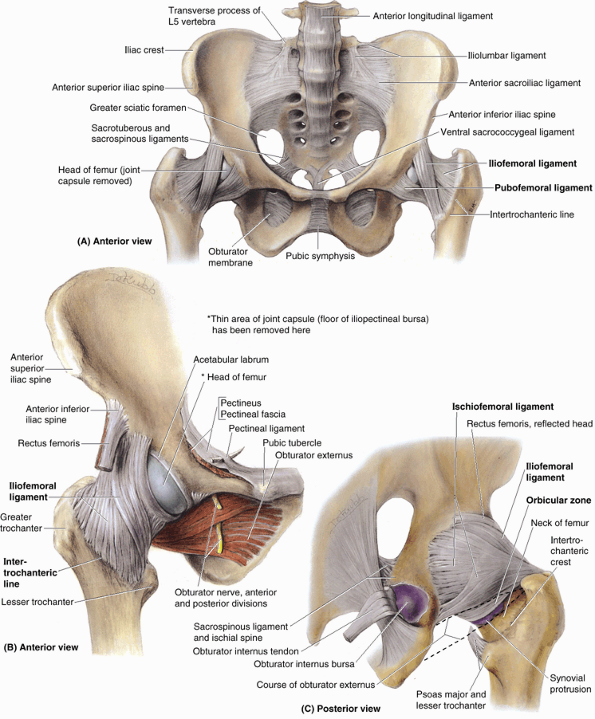 |
|
Figure 5.53. Ligaments of pelvis and hip joint. A.
Weight transfer from the vertebral column to the pelvic girdle is a function of the sacroiliac ligaments. Weight transfer at the hip joint is accomplished primarily by the disposition of the bones, with the ligaments limiting the range of movement and adding stability. B. The strong, triangular iliofemoral ligament attaches at its apex to the rim of the acetabulum inferior to the anterior inferior iliac spine and at its base to the anterior intertrochanteric line of the femur. The pubofemoral ligament, a thickened part of the fibrous layer of the joint capsule, extends from the superior ramus of the pubis to the intertrochanteric line of the femur, passing deep to the iliofemoral ligament. C. The ischiofemoral ligament, also a thickened part of the fibrous layer, passes superolaterally from the ischium over the neck of the femur. The joint capsule does not attach to the posterior aspect of the femur. Thus the synovial membrane is able to protrude from the joint capsule, forming the obturator externus bursa to facilitate movement of the tendon of the obturator externus (shown in part B) over the bone. |
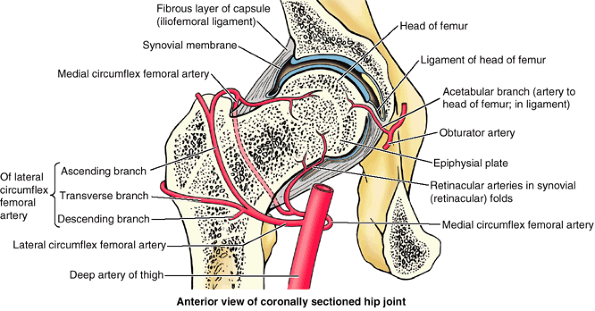 |
|
Figure 5.54. Blood supply of head and neck of femur.
Branches of the medial and lateral circumflex femoral arteries, branches of the deep artery of the thigh, and the artery to the femoral head (a branch of the obturator artery) supply the head and neck of the femur. In the adult, the medial circumflex femoral artery is the most important source of blood to the femoral head and adjacent (proximal) neck. |
joint depends on the position of the knee. If the knee is flexed,
relaxing the hamstrings, the thigh can be actively flexed until it
almost reaches the anterior abdominal wall, and can reach it via
further passive flexion. Not all this movement occurs at the hip joint;
some results from flexion of the vertebral column. During extension of
the hip joint, the fibrous layer of the joint capsule, especially the
iliofemoral ligament, is taut; therefore, the hip can usually be
extended only slightly beyond the vertical except by movement of the
bony pelvis (flexion of lumbar vertebrae).
the hip joint is usually somewhat greater than for adduction. About 60°
of abduction is possible when the thigh is extended, and more when it
is flexed. Lateral rotation is much more powerful than medial rotation.
The main muscles producing movements of the hip joint are listed in Figure 5.55B. Note that:
-
The iliopsoas is the strongest flexor of the hip.
-
In addition to its function as an adductor, the adductor magnus also serves as a flexor (anterior or aponeurotic part) and an extensor (posterior or hamstrings part).
-
Several muscles participate in both flexion and adduction (pectineus and gracilis as well all three “adductor” muscles).
-
In addition to serving as abductors, the anterior portions of the gluteus medius and minimus are also medial rotators.
-
The gluteus maximus
serves as the primary extensor from the flexed to the straight
(standing) position; and from this point posteriorly, extension is
achieved primarily by the hamstrings. The gluteus maximus is also a
lateral rotator.
-
The medial and lateral circumflex femoral arteries, which are usually branches of the deep artery of the thigh but occasionally arise as branches of the femoral artery.
-
The artery to the head of the femur, which is a branch of the obturator artery of variable size; it traverses the ligament of the head.
arising as branches of the circumflex femoral arteries. Retinacular
arteries arising from the medial circumflex femoral artery are most
abundant, bringing more blood to the head and neck of the femur because
they are able to pass beneath the unattached posterior border of the
joint capsule. Retinacular arteries arising from the lateral circumflex
femoral must penetrate the thick iliofemoral ligament and are smaller
and fewer.
nerves supplying the muscles extending directly across and acting at a
given joint also innervate the joint. Articular rami arise from the
intramuscular rami of the muscular branches and directly from named
nerves. A knowledge of the nerve supply of the muscles and their
relationship to the joints can allow one to deduce the nerve supply
of many joints. Possible deductions regarding the hip joint and its muscular relationships include (Fig. 5.55):
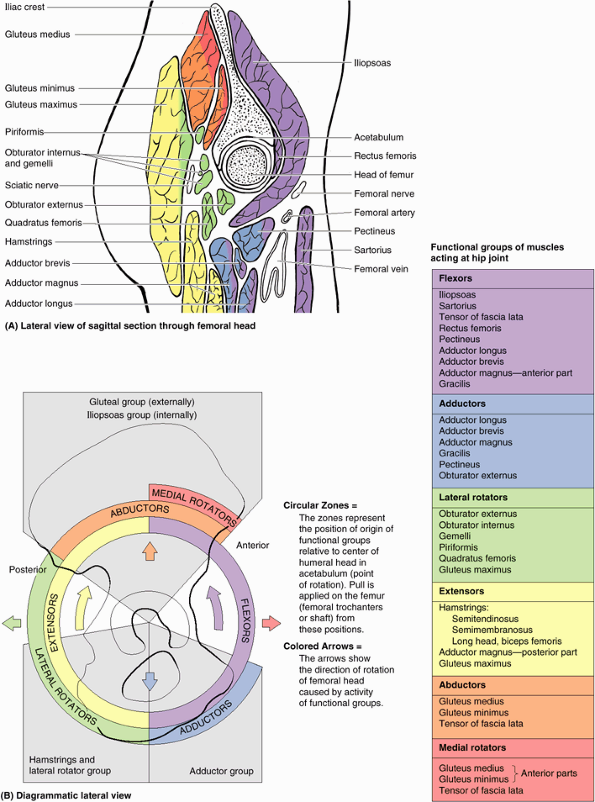 |
|
Figure 5.55. Relations of hip joint and muscles producing movements of joint. A.
Sagittal section of the hip joint showing the muscles, vessels, and nerves related to it. The muscles are color coded to indicate their function(s). Applying Hilton’s law, it is possible to deduce the innervation of the hip joint by knowing which muscles directly cross and act on the joint and their nerve supply. B. The relative positions of the muscles producing movements of the hip joint and the direction of the movement are demonstrated. |
-
Flexors innervated by the femoral nerve
pass anterior to the hip joint; the anterior aspect of the hip joint is
innervated by the femoral nerve (directly and via articular rami of the
muscular branches to the pectineus and rectus femoris). -
Lateral rotators pass inferior and
posterior to the hip joint; the inferior aspect of the joint is
innervated by the obturator nerve (directly and via articular rami of
the muscular branch to the obturator externus), and the posterior
aspect is innervated by the nerve to the quadratus femoris. -
Adductors innervated by the superior
gluteal nerve pass superior to the hip joint; the superior aspect of
the joint is innervated by the superior gluteal nerve.
(unfortunately referred to as “fractured hips,” implying that the hip
bone is broken) are uncommon in most contact sports because the
participants are usually young and the femoral neck is strong in people
<40 years of age. When they do occur in this age group, these
fractures usually result from high-energy impacts (e.g., during
race-car accidents, skiing, trampoline, and equestrian events) when the
lower limb is extended and the force of the impact is transmitted to
the hip joint, even if applied at some distance from the joint. For
example, if the foot is firmly braced against the car floor with the
knee locked, or if the knee is braced against the dashboard during a
head-on collision, the force of the impact may be transmitted
superiorly and produce a femoral neck fracture. These fractures are
especially common in individuals >60 years, especially in women
because their femoral necks are more often weak and brittle as a result
of osteoporosis (Fig. B5.22).
Fractures of the femoral neck are often intracapsular, and realignment
of the neck fragments requires internal skeletal fixation. Femoral neck
fractures are among the most troublesome and problematic of all
fractures (Salter, 1999).
supply to the head of the femur. Most of the blood to the head and neck
of the femur is supplied by the medial circumflex femoral artery (Fig. 5.54).
The retinacular arteries arising from this artery are often torn when
the femoral neck is fractured or the hip joint is dislocated. Following
some femoral neck fractures, the artery to the ligament of the femoral
head may be the only remaining source of blood to the proximal
fragment. This artery is frequently inadequate for maintaining the
femoral head; consequently, the fragment may undergo aseptic vascular necrosis.
 |
|
Figure B5.22
|
During hip replacement, a metal prosthesis anchored to the person’s
femur by bone cement replaces the femoral head and neck. A plastic
socket cemented to the hip bone replaces the acetabulum.
disrupt the artery to the head of the femur. Fractures that result in
separation of the superior femoral epiphysis (the growth plate between
the femoral head and neck) are also likely to result in an inadequate
blood supply to the femoral head and in post-traumatic avascular necrosis of the head.
As a result, incongruity of the joint surfaces develops, and growth at
the epiphysis is retarded. Such conditions, most common in children 3–9
years of age, produce hip pain that may radiate to the knee (Salter, 1999).
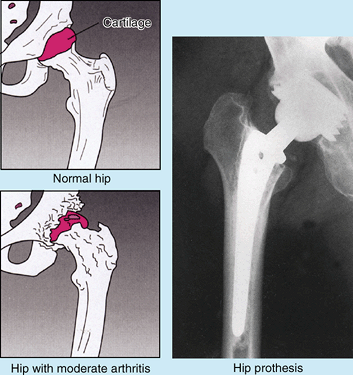 |
|
Figure B5.23
|
is common, occurring in approximately 1.5 per 1000 live births; it is
bilateral in approximately half the cases. Girls are affected at least
eight times more often than boys (Salter, 1999).
Dislocation occurs when the femoral head is not properly located in the
acetabulum. Inability to abduct the thigh is characteristic of
congenital dislocation. In addition, the affected limb appears (and
functions as if) shorter because the dislocated femoral head is more
superior than on the normal side, resulting in a positive Trendelenburg sign
(hip appears to drop on one side during walking). Approximately 25% of
all cases of arthritis of the hip in adults are the direct result of
residual defects from congenital dislocation of the hip.
is uncommon because this articulation is so strong and stable.
Nevertheless, dislocation may occur during an automobile accident when
the hip is flexed, adducted, and medially rotated, the usual position
of the lower limb when a person is riding in a car. Posterior
dislocations are most common. A head-on collision that causes the knee
to strike the dashboard may dislocate the hip when the femoral head is
forced out of the acetabulum (Fig. B5.24A).
The joint capsule ruptures inferiorly and posteriorly, allowing the
femoral head to pass through the tear in the capsule and over the
posterior margin of the acetabulum onto the lateral surface of the
ilium, shortening and medially rotating the affected limb (Fig. B5.24B). Because of the close relationship of the sciatic nerve to the hip joint (Fig. 5.56A),
it may be injured (stretched and/or compressed) during posterior
dislocations or fracture–dislocations of the hip joint. This kind of
injury may result in paralysis of the hamstrings and muscles distal to
the knee supplied by the sciatic nerve. Sensory changes may also occur
in the skin over the posterolateral aspects of the leg and over much of
the foot because of injury to sensory branches of the sciatic nerve.
results from a violent injury that forces the hip into extension,
abduction, and lateral rotation (e.g., catching a ski tip when snow
skiing). In these cases, the femoral head is inferior to the
acetabulum. Often, the acetabular margin fractures, producing a fracture–dislocation of the hip joint. When the femoral head dislocates, it usually carries the acetabular bone fragment and acetabular labrum with it.
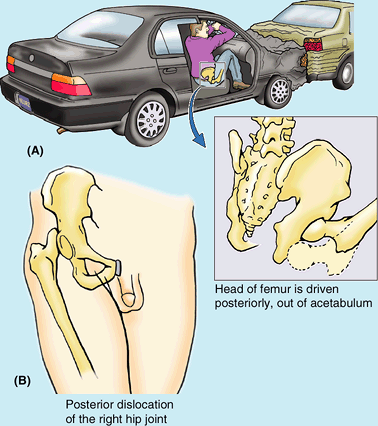 |
|
Figure B5.24
|
Its stability results from (1) the mechanical strength of its ball and
(deep) socket construction, allowing extensive articular surface
contact; (2) its strong joint capsule; and (3) its many surrounding
muscles. However, it remains vulnerable, especially in older age,
because of the angle of the femoral neck (inclination) and close
association of the blood supply of the femoral head to the neck. Thus
fractures result in avascular necrosis of the femoral head. Major
movements are flexion and extension, possible over a wide range; medial
and lateral rotation with abduction are part of every step of normal,
bipedal walking.
largest and most superficial joint. It is primarily a hinge type of
synovial joint, allowing flexion and extension; however, the hinge
movements are combined with gliding and rolling and with rotation about
a vertical axis. Although the knee joint is well constructed, its
function is commonly impaired when it is hyperextended (e.g., in body
contact sports, such as ice hockey).
including their articulating surfaces, were discussed in “Bones of the
Lower Limb,” earlier in this chapter. The articular surfaces of the
knee joint are characterized by their large size and their complicated
and incongruent shapes. The knee joint consists of three articulations (Fig. 5.56):
-
Two femorotibial articulations (lateral and medial) between the lateral and the medial femoral and tibial condyles.
-
One intermediate femoropatellar articulation between the patella and the femur.
of the incongruence of its articular surfaces, which has been compared
to two balls sitting on a warped tabletop. The stability of the knee
joint depends on (1) the strength and actions of the surrounding
muscles and their tendons and (2) the ligaments that connect the femur
and tibia. Of these supports, the muscles are most important;
therefore, many sport injuries are preventable through appropriate
conditioning and training. The most important muscle in stabilizing the
knee joint is the large quadriceps femoris, particularly the inferior fibers of the vastus medialis and lateralis (Fig. 5.57A). The knee joint will function surprisingly well after a ligament strain if the quadriceps is well conditioned.
of the knee. In this position the articular surfaces are most congruent
(contact is minimized in all other positions), the primary ligaments of
the joint (collateral and cruciate ligaments) are taut, and the many
tendons surrounding the joint provide a splinting effect.
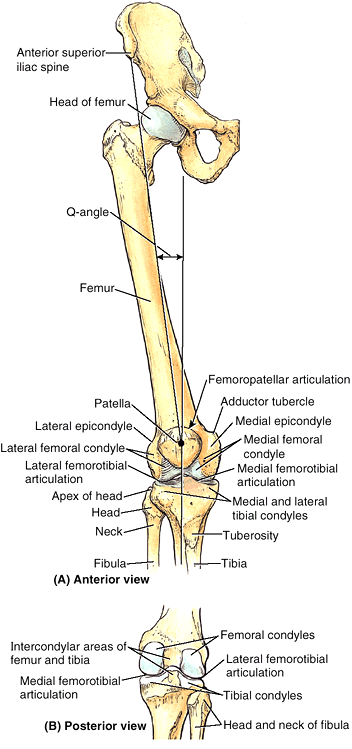 |
|
Figure 5.56. Bones of knee joint. A
The bones articulating at the knee joint are shown. The hip bone and proximal femur are included to demonstrate the Q-angle, determined during physical examination to indicate alignment of the femur and tibia and to evaluate valgus or varus stress at the knee. B. The bones and bony features of the posterior aspect of the knee joint and knee are shown. |
synovial membrane that lines all internal
surfaces of the articular cavity not covered with articular cartilage.
The fibrous layer has a few thickened parts that make up intrinsic
ligaments but, for the main part, it is thin and is actually incomplete
in some areas. The fibrous layer attaches to the femur superiorly, just
proximal to the articular margins of the condyles. Posteriorly, the
fibrous layer encloses the condyles and the intercondylar fossa (Fig. 5.57B).
The fibrous layer has an opening posterior to the lateral tibial
condyle to allow the tendon of the popliteus to pass out of the joint
capsule to attach to the tibia. Inferiorly, the fibrous layer attaches
to the margin of the superior articular surface (tibial plateau) of the
tibia, except where the tendon of the popliteus crosses the bone (Figs. 5.57A & B and 5.58A).
The quadriceps tendon, patella, and patellar ligament replace the
fibrous layer anteriorly—that is, the fibrous layer is continuous with
the lateral and medial margins of these structures, and there is no
separate fibrous layer in the region of these structures (Figs. 5.57A and 5.58A).
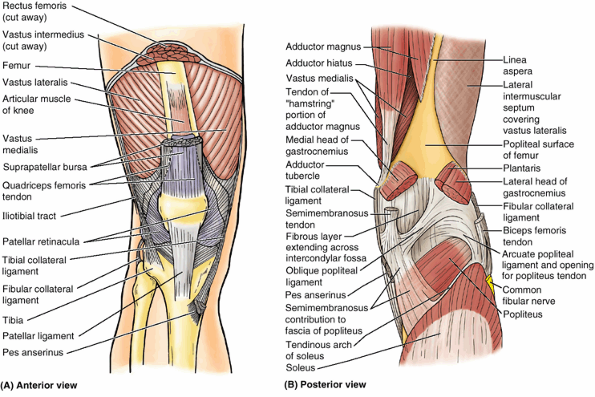 |
|
Figure 5.57. Joint capsule of knee.
The external aspect (fibrous layer) of the joint capsule is relatively thin in some places and thickened in others to form reinforcing intrinsic (capsular) ligaments. A. Modifications of the anterior aspect and sides of the fibrous layer include the patellar retinacula, which attach to the sides of the quadriceps tendon, patella, and patellar ligament, and incorporation of the iliotibial tract (laterally) and the medial collateral ligament (medially). B. The hamstring and gastrocnemius muscles and the posterior intermuscular septum have been cut and removed to expose the adductor magnus, lateral intermuscular septum, and the floor of the popliteal fossa. Posterior modifications of the fibrous layer include the oblique and arcuate popliteal ligaments and a perforation inferior to the arcuate popliteal ligament to allow passage of the popliteus tendon. |
Thus it attaches to the periphery of the articular cartilage covering
the femoral and tibial condyles; the posterior surface of the patella;
and the edges of the menisci, the
fibrocartilaginous discs between the tibial and the femoral articular
surfaces. It lines the internal surface of the fibrous layer laterally
and medially, but centrally it becomes separated from the fibrous
layer. From the posterior aspect of the joint, the synovial membrane
reflects anteriorly into the intercondylar region, covering the
cruciate ligaments and the infrapatellar fat-pad, so that they are excluded from the articular cavity. This creates a median infrapatellar synovial fold,
a vertical fold of synovial membrane that approaches the posterior
aspect of the patella, occupying all but the most anterior part of the
intercondylar region. Thus it almost subdivides the articular cavity
into right and left femorotibial articular cavities; indeed, this is
how arthroscopic surgeons consider the articular
cavity. Fat-filled lateral and medial alar folds cover the inner surface of fat-pads that occupy the space on each side of the patellar ligament internal to the fibrous layer.
 |
|
Figure 5.58. Layers of joint capsule, articular cavity, and articular surfaces of knee joint. A.
The attachments of the fibrous layer and synovial membrane to the tibia are shown. Note that, although they are adjacent on each side, they part company centrally to accommodate intercondylar and infrapatellar structures that are intracapsular (inside the fibrous layer) but extra-articular (excluded from the articular cavity by synovial membrane). B. The joint capsule was incised transversely, the patella was sawn through, and then the knee was flexed, opening the articular cavity. The infrapatellar fold of synovial membrane encloses the cruciate ligaments, excluding them from the joint cavity. All internal surfaces not covered with or made of articular cartilage (blue, or gray in the case of the menisci) are lined with synovial membrane (mostly purple, but transparent and colorless where it is covering non-articular surfaces of the femur). |
The synovial membrane of the joint capsule is continuous with the
synovial lining of this bursa. This large bursa usually extends
approximately 5 cm superior to the patella; however, it may extend
halfway up the anterior aspect of the femur. Muscle slips deep to the
vastus intermedius form the articular muscle of the knee, which attaches to the synovial membrane and retracts the bursa during extension of the knee (Figs. 5.16 and 5.57A).
or capsular (intrinsic) ligaments: patellar ligament, fibular
collateral ligament, tibial collateral ligament, oblique popliteal
ligament, and arcuate popliteal ligament (Fig. 5.57A & B). They are sometimes called external ligaments to differentiate them from internal ligaments, such as the cruciate ligaments.
distal part of the quadriceps tendon, is a strong, thick fibrous band
passing from the apex and adjoining margins of the patella to the
tibial tuberosity (Fig. 5.57A). The patellar ligament is the anterior ligament of the knee joint. Laterally, it receives the medial and lateral patellar retinacula,
aponeurotic expansions of the vastus medialis and lateralis and
overlying deep fascia. The retinacula make up the joint capsule of the
knee on each side of the patella (Figs. 5.57A and 5.58A)
and play an important role in maintaining alignment of the patella
relative to the patellar articular surface of the femur. The oblique
placement of the femur and/or line of pull of the quadriceps femoris
muscle relative to the axis of the patellar tendon and tibia, assessed
clinically as the Q-angle, favors lateral displacement of the patella (Fig. 5.56).
As flexion proceeds, they become increasingly slack, permitting and
limiting (serving as check ligaments for) rotation at the knee. The fibular collateral ligament
(FCL; lateral collateral ligament), a cord-like extracapsular ligament,
is strong. It extends inferiorly from the lateral epicondyle of the
femur to the lateral surface of the fibular head (Fig. 5.59A & B).
The tendon of the popliteus passes deep to the FCL, separating it from
the lateral meniscus. The tendon of the biceps femoris is split into
two parts by this ligament (Fig. 5.59A). The tibial collateral ligament
(TCL; medial collateral ligament) is a strong, flat, intrinsic
(capsular) band that extends from the medial epicondyle of the femur to
the medial condyle and the superior part of the medial surface of the
tibia (Fig. 5.59C & D).
At its midpoint, the deep fibers of the TCL are firmly attached to the
medial meniscus. The TCL, weaker than the FCL, is more often damaged.
As a result, the TCL and medial meniscus are commonly torn during
contact sports such as football and ice hockey.
is a recurrent expansion of the tendon of the semimembranosus that
reinforces the joint capsule posteriorly as it spans the intracondylar
fossa (Fig. 5.57B).
The ligament arises posterior to the medial tibial condyle and passes
superolaterally toward the lateral femoral condyle, blending with the
central part of the posterior aspect of the joint capsule.
also strengthens the joint capsule posterolaterally. It arises from the
posterior aspect of the fibular head, passes superomedially over the
tendon of the popliteus, and spreads over the posterior surface of the
knee joint. Its development appears to be inversely related to the
presence and size of a fabella in the proximal attachment of the
lateral head of gastrocnemius (see clinical correlation [blue] box “Fabella in the Gastrocnemius,” in this chapter). Both structures are thought to contribute to posterolateral stability of the knee.
the tibia is almost vertical within the leg, creating an angle at the
knee between the long axes of the bones (Fig. B5.25A). The angle between the two bones, referred to clinically as the Q-angle,
is assessed by drawing a line from the ASIS to the middle of the
patella and extrapolating a second (vertical) line passing through the
middle of the patella and tibial tuberosity (Fig. 5.56).
The Q-angle is typically greater in adult females, owing to their wider
pelves. When normal, the angle of the femur within the thigh places the
middle of the knee joint directly inferior to the head of the femur
when standing, centering the weight-bearing line in the intercondylar
region of the knee (Fig. B5.25A).
in which the femur is abnormally vertical and the Q-angle is small, is
a deformity called genu varum (bowleg) that causes unequal weight bearing: The line of weight bearing falls medial to the center of the knee (Fig. B5.25B). Excess pressure is placed on the medial aspect of the knee joint, which results in arthrosis (destruction of knee cartilages), and the fibular collateral ligament is overstressed (Fig. B.25D). A lateral angulation of the leg (large Q-angle, >17°) in relation to the thigh (exaggeration of the knee angle) is called genu valgum (knock-knee) (Fig. B5.25C).
Because of the exaggerated knee angle in genu valgum, the
weight-bearing line falls lateral to the center of the knee.
Consequently, the tibial collateral ligament is overstretched, and
there is excess stress on the lateral meniscus and cartilages of the
lateral femoral and tibial condyles. The patella, normally pulled
laterally by the tendon of the vastus lateralis, is pulled even farther
laterally when the leg is extended in the presence of genu valgum so
that its articulation with the femur is abnormal. Children commonly
appear bowlegged for 1–2 years after starting to walk, and knock-knees
are frequently observed in children 2–4 years of age. Persistence of
these abnormal knee angles in late childhood usually means congenital
deformities exist that may require correction. Any irregularity of a
joint eventually leads to wear and tear (arthrosis) of the articular
cartilages.
dislocates laterally. Patellar dislocation is more common in women,
presumably because of their greater Q-angle which, in addition to
representing the oblique placement of the femur relative to the tibia,
represents the angle of pull of the quadriceps relative to the axis of
the patella and tibia (the term Q-angle
was actually coined in reference to the angle of pull of the
quadriceps). The tendency toward lateral dislocation is normally
counterbalanced by the medial, more horizontal pull of the powerful
vastus medialis. In addition, the more anterior projection of the
lateral femoral condyle and deeper slope for the larger lateral
patellar facet provide a mechanical deterrent to lateral dislocation.
An imbalance of the lateral pull and the mechanisms resisting it result
in abnormal tracking of the patella within the patellar groove and
chronic patellar pain, even if actual dislocation does not occur.
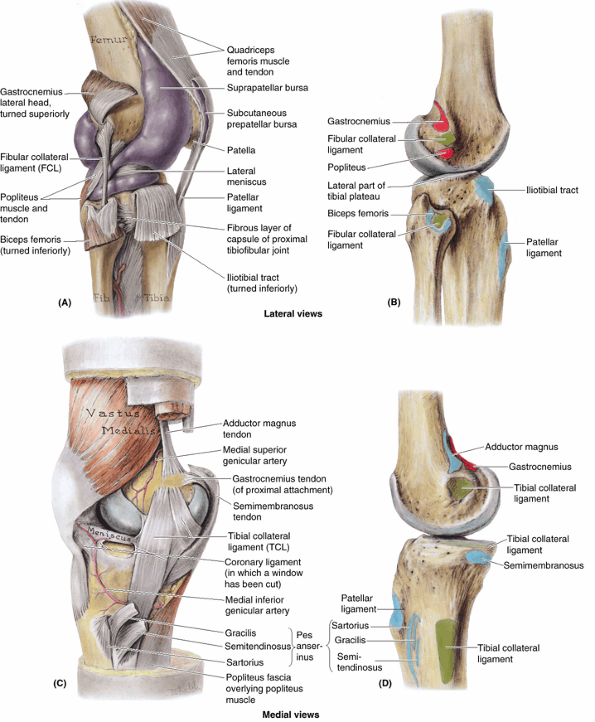 |
|
Figure 5.59. Collateral ligaments of knee joint. A.
The fibular collateral ligament is shown. Purple latex was injected into the articular cavity to demonstrate the extensive and complex synovial membrane surrounding it. The articular cavity/synovial membrane extends superiorly deep to the quadriceps, forming the suprapatellar bursa. B. The attachment sites of the FCL (green) and related muscles (red, proximal; blue, distal) on the lateral aspect of the bones of the knee region are indicated. The tendon of the biceps femoris bifurcates, its site of attachment embracing the inferior attachment of the FCL. C. The band-like part of the tibial collateral ligament (isolated here from the fibrous layer of the joint capsule, of which it is a part) attaches to the medial epicondyle (almost in line with the adductor magnus tendon); crosses the insertion of the semimembranosus muscle; and passes deep to the pes anserinus, the combined attachment sites of the tendinous distal attachment of the gracilis, semitendinosus, and sartorius muscles. D. The attachment sites of the TCL and related muscles on the medial aspect of the bones of the knee region are indicated. |
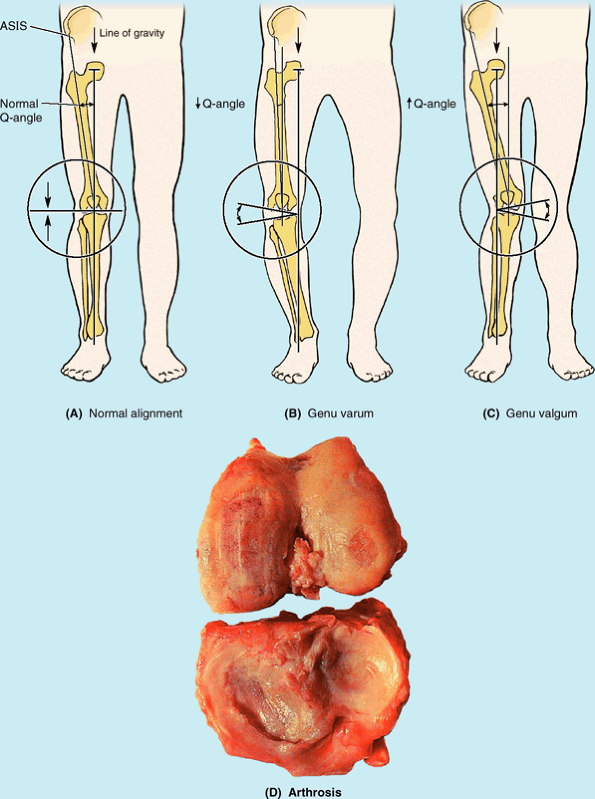 |
|
Figure B5.25
|
running, especially downhill; hence, this type of pain is often called
“runner’s knee.” The pain results from repetitive microtrauma caused by
abnormal tracking of the patella relative to the patellar surface of
the femur, a condition known as the patellofemoral syndrome. This syndrome may also result from a direct blow to the patella and from osteoarthritis of the patellofemoral compartment (degenerative wear and tear of articular cartilages). In some cases, strengthening of the vastus medialis corrects patellofemoral dysfunction.
This muscle tends to prevent lateral dislocation of the patella
resulting from the Q-angle because the vastus medialis attaches to and
pulls on the medial border of the patella. Hence, weakness of the
vastus medialis predisposes the individual to the patellofemoral
dysfunction and patellar dislocation.
consist of the cruciate ligaments and menisci. The popliteal tendon is
also intra-articular during part of its course.
During medial rotation of the tibia on the femur, the cruciate
ligaments wind around each other; thus the amount of medial rotation
possible is limited to about 10°. Because they become unwound during
lateral rotation, nearly 60° of lateral rotation is possible when the
knee is flexed >90°, the movement being ultimately limited by the
TCL. The chiasm (point of crossing) of the cruciate ligaments serves as
the pivot for rotatory movements at the knee. Because of their oblique
orientation, in every position one cruciate ligament, or parts of one
or both ligaments, is tense. It is the cruciate ligaments that maintain
contact with the femoral and tibial articular surfaces during flexion
of the knee.
(ACL), the weaker of the two cruciate ligaments, arises from the
anterior intercondylar area of the tibia, just posterior to the
attachment of the medial meniscus (Fig. 5.60A).
The ACL has a relatively poor blood supply. It extends superiorly,
posteriorly, and laterally to attach to the posterior part of the
medial side of the lateral condyle of the femur (Fig. 5.60C).
It limits posterior rolling (turning and traveling) of the femoral
condyles on the tibial plateau during flexion, converting it to spin
(turning in place). It also prevents posterior displacement of the
femur on the tibia and hyperextension of the knee joint. When the joint
is flexed at a right angle, the tibia cannot be pulled anteriorly (like
pulling out a drawer) because it is held by the ACL.
The PCL passes superiorly and anteriorly on the medial side of the ACL
to attach to the anterior part of the lateral surface of the medial
condyle of the femur (Fig. 5.60B & C).
The PCL limits anterior rolling of the femur on the tibial plateau
during extension, converting it to spin. It also prevents anterior
displacement of the femur on the tibia or posterior displacement of the
tibia on the femur and helps prevent hyperflexion of the knee joint. In
the weight-bearing flexed knee, the PCL is the main stabilizing factor
for the femur (e.g., when walking downhill).
are crescentic plates (“wafers”) of fibrocartilage on the articular
surface of the tibia that deepen the surface and play a role in shock
absorption (Fig. 5.61). The menisci (G. meniskos,
crescent) are thicker at their external margins and taper to thin,
unattached edges in the interior of the joint. Wedge shaped in
transverse section, the menisci are firmly attached at their ends to
the intercondylar area of the tibia (Fig. 5.60A). Their external margins attach to the joint capsule of the knee. The coronary ligaments
are portions of the joint capsule extending between the margins of the
menisci and most of the periphery of the tibial condyles (Fig. 5.60B). A slender fibrous band, the transverse ligament of the knee joins the anterior edges of the menisci (Fig. 5.61A), tethering them to each other during knee movements.
shaped, broader posteriorly than anteriorly. Its anterior end (horn) is
attached to the anterior intercondylar area of the tibia, anterior to
the attachment of the ACL (Fig. 5.60A).
Its posterior end is attached to the posterior intercondylar area,
anterior to the attachment of the PCL. The medial meniscus firmly
adheres to the deep surface of the TCL (Figs. 5.59C and 5.61).
Because of its widespread attachments laterally to the tibial
intercondylar area and medially to the TCL, the medial meniscus is less
mobile on the tibial plateau than is the lateral meniscus.
nearly circular, smaller, and more freely movable than the medial
meniscus. The tendon of the popliteus has two parts proximally. One
part attaches to the lateral epicondyle of the femur and passes between
the lateral meniscus and inferior part of the lateral epicondylar
surface of
the femur (on the tendon’s medial aspect) and the FCL that overlies its lateral aspect (Figs. 5.59A and 5.60B & D).
The other, more medial part of the popliteal tendon attaches to the
posterior limb of the lateral meniscus. A strong tendinous slip, the posterior meniscofemoral ligament, joins the lateral meniscus to the PCL and the medial femoral condyle (Figs. 5.60D and 5.61B).
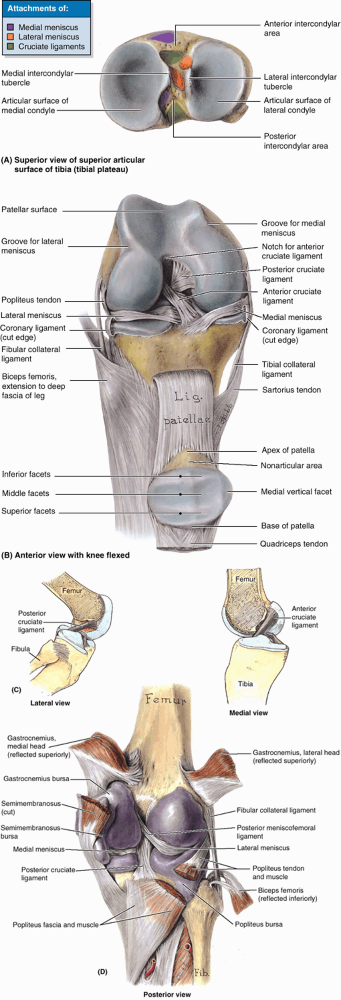 |
|
Figure 5.60. Cruciate ligaments of knee joint. A.
Superior aspect of the superior articular surface of the tibia (tibial plateau) showing the medial and lateral condyles (articular surfaces) and the intercondylar eminence between them. The sites of attachment of the cruciate ligaments are colored green; those of the medial meniscus, purple; and those of the lateral meniscus, orange. B. The quadriceps tendon has been severed and the patella (within the tendon and its continuation, the patellar ligament) has been reflected inferiorly. The knee is flexed to demonstrate the cruciate ligaments. C. In these lateral and medial views, the femur has been sectioned longitudinally and the near half has been removed with the proximal part of the corresponding cruciate ligament. The lateral view demonstrates how the posterior cruciate ligament resists anterior displacement of the femur on the tibial plateau. The medial view demonstrates how the anterior cruciate ligament resists posterior displacement of the femur on the tibial plateau. D. Both heads of the gastrocnemius are reflected superiorly, and the biceps femoris is reflected inferiorly. The articular cavity has been inflated with purple latex to demonstrate its continuity with the various bursae and the reflections and attachments of the complex synovial membrane. |
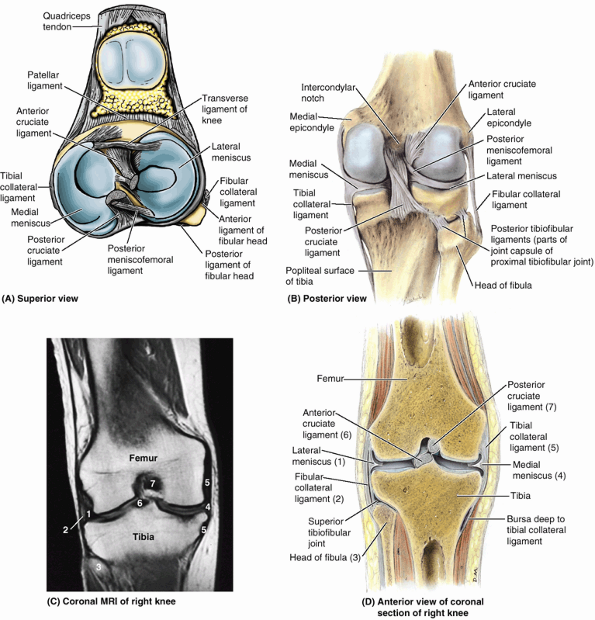 |
|
Figure 5.61. Menisci of knee joint. A.
The quadriceps tendon is cut, and the patella and patellar ligament are reflected inferiorly and anteriorly. The menisci, their attachments to the intercondylar area of the tibia, and the tibial attachments of the cruciate ligaments are shown. B. The band-like tibial collateral ligament is attached to the medial meniscus. The cord-like fibular collateral ligament is separated from the lateral meniscus. The posterior meniscofemoral ligament attaches the lateral meniscus to the medial femoral condyle. C and D. The numbers on the MRI study refer to the structures labeled in the corresponding anatomical coronal section. (Part C courtesy of Dr. W. Kucharczyk, Chair of Medical Imaging, University of Toronto, and Clinical Director of Tri-Hospital Magnetic Resonance Centre, Toronto, Ontario, Canada.) |
rotation occurs when the knee is flexed. When the knee is fully
extended with the foot on the ground, the knee passively “locks”
because of medial rotation of the femoral condyles on the tibial
plateau. This position makes the lower limb a solid column and more
adapted for weight bearing. When the knee is “locked,” the thigh and
leg muscles can relax briefly without making the knee joint too
unstable. To unlock the knee, the popliteus contracts, rotating the
femur laterally about 5° on the tibial plateau so that flexion of the
knee can occur. The main movements of the knee joint, the muscles
producing them, and relevant details are provided in Table 5.16.
|
Table 5.16. Movements of the Knee Joint and the Muscles Producing Them
|
||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||
during flexion and extension is limited (converted to spin) by the
cruciate ligaments, some
rolling
does occur, and the point of contact between the femur and the tibia
moves posteriorly with flexion and returns anteriorly with extension.
Furthermore, during rotation of the knee, one femoral condyle moves
anteriorly on the corresponding tibial condyle while the other femoral
condyle moves posteriorly, rotating about the chiasm of the cruciate
ligaments. The menisci must be able to migrate on the tibial plateau as
the points of contact between femur and tibia change.
around the knee: the genicular branches of the femoral, popliteal, and
anterior and posterior recurrent branches of the anterior tibial
recurrent and circumflex fibular arteries (Figs. 5.62 and 5.63B).
The middle genicular branches of the popliteal artery penetrate the
fibrous layer of the joint capsule and supply the cruciate ligaments,
synovial membrane, and peripheral margins of the menisci.
thus articular branches from the femoral (the branches to the vasti),
tibial, and common fibular nerves supply its anterior, posterior, and
lateral aspects, respectively. In addition, however, the obturator and
saphenous (cutaneous) nerves supply articular branches to its medial
aspect.
because most tendons run parallel to the bones and pull lengthwise
across the joint during knee movements. The subcutaneous prepatellar and infrapatellar bursae are located at the convex surface of the joint, allowing the skin to be able to move freely during movements of the knee (Figs. 5.58B and 5.59A). The main bursae of the knee are illustrated and described in Table 5.17.
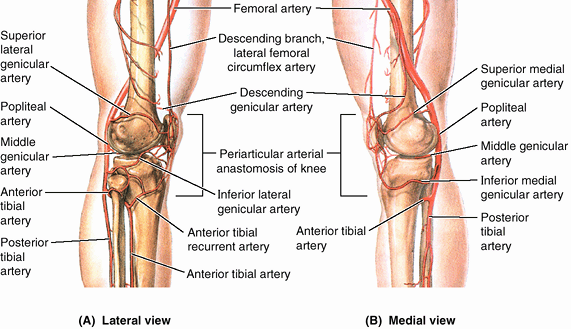 |
|
Figure 5.62. Arterial anastomoses around knee.
In addition to providing collateral circulation, the genicular arteries of the genicular anastomosis supply blood to the structures surrounding the joint as well as to the joint itself (e.g., its joint or articular capsule). Compare these views with the anterior view in Figure 5.63B. |
knee joint: suprapatellar bursa, popliteus bursa (deep to the distal
quadriceps), anserine bursa (deep to the tendinous distal attachments
of the sartorius, gracilis, and semitendinosus), and gastrocnemius
bursa (Figs. 5.59A and 5.60D). The large suprapatellar bursa (Figs. 5.57A and 5.59A)
is especially important because an infection in it may spread to the
knee joint cavity. Although it develops separately from the knee joint,
the bursa becomes continuous with it.
low-placed, mobile, weight-bearing joint, serving as a fulcrum between
two long levers (thigh and leg). Its stability depends almost entirely
on its associated ligaments and surrounding muscles. The knee joint is
essential for everyday activities such as standing, walking, and
climbing stairs. It is also a main joint for sports that involve
running, jumping, kicking, and changing directions. To perform these
activities, the knee joint must be mobile; however, this mobility makes
it susceptible to injuries. The most common knee injuries in contact
sports are ligament sprains, which occur when the foot is fixed in the ground (Fig. B5.26A).
If a force is applied against the knee when the foot cannot move,
ligament injuries are likely to occur. The tibial and fibular
collateral ligaments (TCL and FCL) are tightly stretched when the leg
is extended, normally preventing disruption of the sides of the knee
joint.
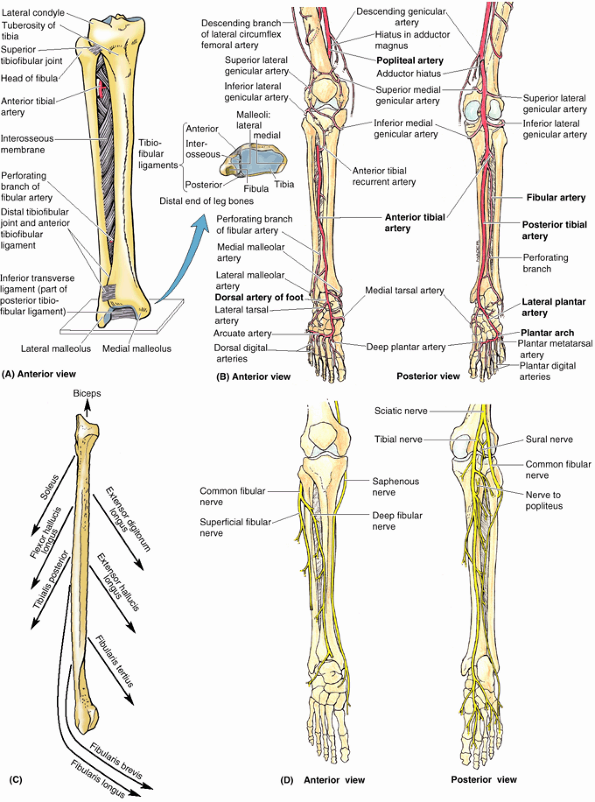 |
|
Figure 5.63. Joints and neurovascular structures of leg and foot. A.
The tibiofibular articulations include the synovial tibiofibular joint and the tibiofibular syndesmosis; the latter is made up of the interosseous membrane of the leg and the anterior and posterior tibiofibular ligaments. The oblique direction of the fibers of the interosseous membrane, primarily extending inferolaterally from the tibia, allows slight upward movement of the fibula but resists downward pull on it. B. The arterial supply of the joints of the leg and foot is demonstrated. Periarticular anastomoses surround the knee and ankle. C. Of the nine muscles attached to the fibula, all except one exert a downward pull on the fibula. D. The nerve supply of the leg and foot is demonstrated. Starting with the knee and progressing distally in the limb, cutaneous nerves become increasingly involved in providing innervation to joints, taking over completely in the distal foot and toes. |
|
Table 5.17. Bursae about the Knee Joint
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||
of considerable clinical significance because tearing of this ligament
frequently results in concomitant tearing of the medial meniscus. The
injury is frequently caused by a blow to the lateral side of the
extended knee or excessive lateral twisting of the flexed knee that
disrupts the TCL and concomitantly tears and/or detaches the medial
meniscus from the joint capsule (Fig. B5.26A).
This injury is common in athletes who twist their flexed knees while
running (e.g., in basketball, the various forms of football, and
volleyball). The ACL, which serves as a pivot for rotatory movements of
the knee and is taut during flexion, may also tear subsequent to the
rupture of the TCL, creating an “unhappy triad” of knee injuries.
Hyperextension and severe force directed anteriorly against the femur
with the knee semiflexed (e.g., a cross-body block in football) may
tear the ACL. ACL ruptures are also common
knee injuries in skiing accidents. This injury causes the free tibia to
slide anteriorly under the fixed femur, known as the anterior drawer sign (Fig. B5.26B). The ACL may tear away from the femur or tibia; however, tears commonly occur in the midportion of the ligament.
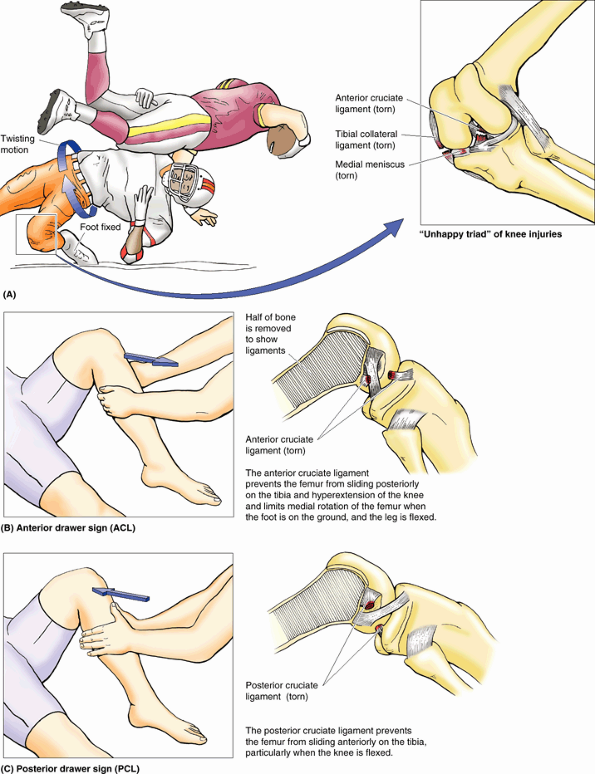 |
|
Figure B5.26
|
may occur when a player lands on the tibial tuberosity with the knee
flexed (e.g., when knocked to the floor in basketball). PCL ruptures
usually occur in conjunction with tibial or fibular ligament tears.
These injuries can also occur in head-on collisions when seat belts are
not worn and the proximal end of the tibia strikes the dashboard. PCL
ruptures allow the free tibia to slide posteriorly under the fixed
femur, known as the posterior drawer sign (Fig. B5.26C).
Most meniscal tears occur in conjunction with TCL or ACL tears.
Peripheral meniscal tears can often be repaired or may heal on their
own because of the generous blood supply to this area. Meniscal tears
that do not heal or cannot be repaired are usually removed (e.g., by
arthroscopic surgery). Knee joints from which the menisci have been
removed suffer no loss of mobility; however, the knee may be less
stable and the tibial plateaus often undergo inflammatory reactions.
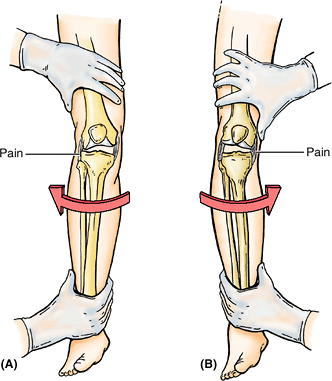 |
|
Figure B5.27
|
examination that allows visualization of the interior of the knee joint
cavity with minimal disruption of tissue (Fig. B5.28). The arthroscope and one (or more) additional canula(e) are inserted through tiny incisions, known as portals.
The second canula is for passage of specialized tools (e.g.,
manipulative probes or forceps) or equipment for trimming, shaping, or
removing damaged tissue. This technique allows removal of torn menisci,
loose bodies in the joint (such as bone chips), and débridement
(the excision of devitalized articular cartilaginous material) in
advanced cases of arthritis. Ligament repair or replacement may also be
performed using an arthroscope. Although general anesthesia is usually
preferable, knee arthroscopy can be performed using local or regional
anesthesia. During arthroscopy, the articular cavity of the knee must
be treated essentially as two separate (medial and lateral)
femorotibial articulations owing to the imposition of the synovial fold
around the cruciate ligaments. For further information see Soames (1995).
of the anterior thigh may involve the suprapatellar bursa and result in
infection of the knee joint. When the knee joint is infected and
inflamed, the amount of synovial fluid may increase. Joint effusions,
the escape of fluid from blood or lymphatic vessels, results in
increased amounts of fluid in the joint cavity. Because the
suprapatellar bursa communicates freely with the synovial cavity of the
knee joint, fullness of the thigh in the region of the suprapatellar
bursa may indicate increased synovial fluid. This bursa can be
aspirated to remove the fluid for examination. Direct aspiration of the knee joint
is usually performed with the patient sitting on a table with the knee
flexed. The joint is approached laterally, using three bony points as
landmarks for needle insertion: the anterolateral tibial (Gerdy)
tubercle, the lateral epicondyle of the femur, and the apex of the
patella. In addition to being the route for aspiration of serous and
sanguineous (bloody) fluid, this triangular area also lends itself to
drug injection for treating pathology of the knee joint.
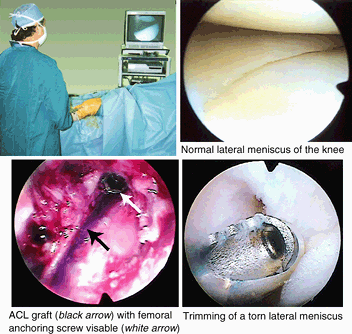 |
|
Figure B5.28
|
caused by friction between the skin and the patella; however, the bursa
may also be injured by compressive forces resulting from a direct blow
or from falling on the flexed knee (Anderson et al., 2000).
If the inflammation is chronic, the bursa becomes distended with fluid
and forms a swelling anterior to the knee. This condition has been
called “housemaid’s knee” (Fig. B5.29);
however, other people who work on their knees without knee pads, such
as hardwood floor and rug installers, may also develop prepatellar
bursitis.
is caused by excessive friction between the skin and the tibial
tuberosity; the edema occurs over the proximal end of the tibia. This
condition was formerly called “clergyman’s knee” because of frequent
genuflecting (L. genu, knee); however, it occurs more commonly in roofers and floor tilers if they do not wear knee pads. Deep infrapatellar bursitis
results in edema between the patellar ligament and the tibia, superior
to the tibial tuberosity. The inflammation is usually caused by overuse
and subsequent friction between the patellar tendon and the structures
posterior to it, the infrapatellar fat-pad and tibia (Anderson et al., 2000).
Enlargement of the deep infrapatellar bursa obliterates the dimples
normally occurring on each side of the patellar ligament when the leg
is extended.
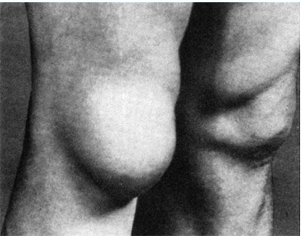 |
|
Figure B5.29
|
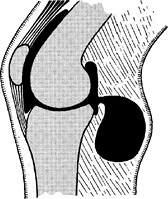 |
|
Figure B5.30
|
an infection caused by bacteria entering the bursa from the torn skin.
The infection may spread to the cavity of the knee joint, causing
localized redness and enlarged popliteal and inguinal lymph nodes.
cysts) are abnormal fluid-filled sacs of synovial membrane in the
region of the popliteal fossa. A popliteal cyst is almost always a
complication of chronic knee joint effusion (Slaby et al., 1994).
The cyst may be a herniation of the gastrocnemius or semimembranosus
bursa through the fibrous layer of the joint capsule into the popliteal
fossa, communicating with the synovial cavity of the knee joint by a
narrow stalk (Fig. B5.30). Synovial fluid may also escape from the knee joint (synovial effusion)
or a bursa around the knee and collect in the popliteal fossa. Here it
forms a new synovial-lined sac, or popliteal cyst. Popliteal cysts are
common in children but seldom cause symptoms. In adults, popliteal
cysts can be large, extending as far as the midcalf, and may interfere
with knee movements.
The artificial knee joint consists of plastic and metal components that
are cemented to the femoral and tibial bone ends after removal of the
defective areas. The combination of metal and plastic mimics the
smoothness of cartilage on cartilage and produces good results in
“low-demand” people who have a relatively sedentary life. In
“high-demand” people who are active in sports, the bone–cement
junctions may break down, and the artificial knee components may
loosen; however, improvements in bioengineering and surgical technique
have provided better results. For more information see Soames (1995).
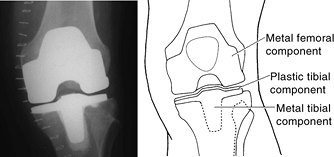 |
|
Figure B5.31
|
(primarily flexion and extension, with rotation increasingly possible
with flexion). It is our most vulnerable joint owing to its incongruous
articular surfaces and the mechanical disadvantage resulting from
bearing the body’s weight plus momentum while serving as a fulcrum
between two long levers. Compensation is attempted by several features,
including (1) strong intrinsic, extracapsular, and intracapsular
ligaments; (2) splinting by many surrounding tendons (including the
iliotibial tract); and (3) menisci that fill the spatial void,
providing mobile articular surfaces. Of particular clinical importance
are (1) collateral ligaments that are taut during (and limit) extension
and are relaxed during flexion, allowing rotation for which they serve
as check ligaments; (2) cruciate ligaments that maintain the joint
during flexion, providing the pivot for rotation; and (3) the medial
meniscus that is attached to the tibial collateral ligament and is
frequently injured because of this attachment.
The fibers of the interosseous membrane and all ligaments of both
tibiofibular articulations run inferiorly from the tibia to the fibula.
Thus the membrane and ligaments strongly resist the downward pull
placed on the fibula by eight of the nine muscles attached to it (Fig. 5.63C).
However, they allow slight upward movement of the fibula that occurs
when the wide (posterior) end of the trochlea of the talus is wedged
between the malleoli during dorsiflexion at the ankle. Movement at the
superior tibiofibular joint is impossible without movement at the
inferior tibiofibular syndesmosis.
is a plane type of synovial joint between the flat facet on the fibular
head and a similar articular facet located posterolaterally on the
lateral tibial condyle (Figs. 5.61B & D and 5.63A).
A tense joint capsule surrounds the joint and attaches to the margins
of the articular surfaces of the fibula and tibia. The joint capsule is
strengthened by anterior and posterior tibiofibular ligaments, which pass superomedially from the fibular head to the lateral tibial condyle (Fig. 5.61B). The joint is crossed posteriorly by the tendon of the popliteus. A pouch of synovial membrane from the knee joint, the popliteus bursa (Table 5.17),
passes between the tendon of the popliteus and the lateral condyle of
the tibia. About 20% of the time, the bursa also communicates with the
synovial cavity of the tibiofibular joint, enabling transmigration of
inflammatory processes between the two joints.
of the foot as a result of wedging of the trochlea of the talus between
the malleoli (see “Articular Surfaces of the Ankle Joint,” later in this chapter).
uniting the distal ends of the bones). The integrity of the inferior
tibiofibular joint is essential for the stability of the ankle joint
because it keeps the lateral malleolus firmly against the lateral
surface of the talus.
surface of the inferior end of the fibula articulates with a facet on
the inferior end of the tibia (Fig. 5.63A). The strong deep interosseous tibiofibular ligament,
continuous superiorly with the interosseous membrane, forms the
principal connection between the tibia and the fibula. The joint is
also strengthened anteriorly and posteriorly by the strong external anterior and posterior inferior tibiofibular ligaments. The distal deep continuation of the posterior inferior tibiofibular ligament, the inferior
transverse (tibiofibular) ligament
forms a strong connection between the distal ends of the tibia (medial
malleolus) and the fibula (lateral malleolus). It contacts the talus
and forms the posterior “wall” of a square socket (with three deep
walls and a shallow or open anterior wall), the malleolar mortise, for the trochlea of the talus. The lateral and medial walls of the mortise are formed by the respective malleoli (Fig. 5.64).
wedging of the wide portion of the trochlea of the talus between the
malleoli during dorsiflexion of the foot.
fibular artery and from medial malleolar branches of the anterior and
posterior tibial arteries (Fig. 5.63B).
joint and the tibiofibular syndesmosis, consisting of an interosseous
membrane and an inferior tibiofibular joint with anterior,
interosseous, and posterior tibiofibular ligaments. Together they make
up a compensatory system that allows a slight upward movement of the
fibula owing to forced transverse expansion of the malleolar mortise
(deep square socket) during maximal dorsiflexion of the ankle. All
fibrous tibiofibular connections run downward from tibia to fibula,
allowing this slight upward movement while strongly resisting the
downward pull applied to the fibula by the contraction of eight of the
nine muscles attached to it.
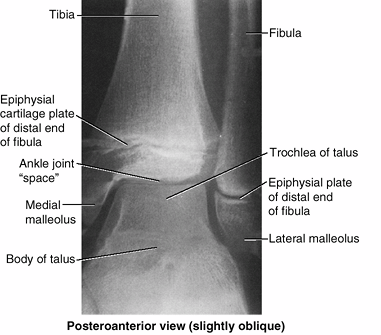 |
|
Figure 5.64. Radiograph of ankle joint of a 14-year-old boy.
The trochlea of the body of the talus fits into the mortise formed by the medial and lateral malleoli. Epiphysial (growth) plates are evident at this age. |
is a hinge-type synovial joint. It is located between the distal ends
of the tibia and the fibula and the superior part of the talus. The
ankle joint can be felt between the tendons on the anterior surface of
the ankle as a slight depression, approximately 1 cm proximal to the
tip of the medial malleolus.
The medial surface of the lateral malleolus articulates with the
lateral surface of the talus. The tibia articulates with the talus in
two places:
-
Its inferior surface forms the roof of the malleolar mortise, transferring the body’s weight to the talus.
-
Its medial malleolus articulates with the medial surface of the talus.
mortise during movements of the joint. The grip of the malleoli on the
trochlea is strongest during dorsiflexion of the foot (as when “digging
in one’s heels” when descending a steep slope or during tug-of-war)
because this movement forces the wider, anterior part of the trochlea
posteriorly between the malleoli, spreading the tibia and fibula
slightly apart. This spreading is limited especially by the strong
interosseous tibiofibular ligament as well as the anterior and
posterior tibiofibular ligaments that unite the tibia and fibula (Figs. 5.63A and 5.65).
The interosseous ligament is deeply placed between the nearly congruent
surfaces of the tibia and fibula; although demonstrated in the inset
for Figure 5.63A, the ligament can actually be observed only by rupturing it or in a cross section.
plantarflexion because the trochlea is narrower posteriorly and,
therefore, lies relatively loosely within the mortise. It is during
plantarflexion that most injuries of the ankle occur (usually as a
result of sudden, unexpected—and therefore inadequately
resisted—inversion of the foot).
leaving only the reinforced parts—the ligaments—and a synovial fold).
Its fibrous layer is attached superiorly to the borders of the
articular surfaces of the tibia and the malleoli and inferiorly to the
talus. The synovial membrane is loose and lines the fibrous layer of
the capsule. The synovial cavity often extends superiorly between the
tibia and the fibula as far as the interosseous tibiofibular ligament.
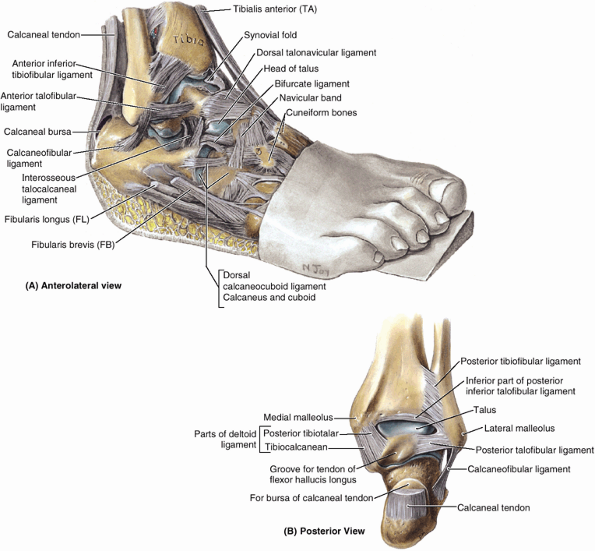 |
|
Figure 5.65. Dissection of ankle joint and joints of inversion and eversion. A and B.
The foot has been inverted (note wedge under foot) to demonstrate the articular areas and the lateral ligaments that become taut during inversion of the foot. |
-
Anterior talofibular ligament, a flat, weak band that extends anteromedially from the lateral malleolus to the neck of the talus,
-
Posterior talofibular ligament,
a thick, fairly strong band that runs horizontally medially and
slightly posteriorly from the malleolar fossa to the lateral tubercle
of the talus. -
Calcaneofibular ligament, a round cord that passes posteroinferiorly from the tip of the lateral malleolus to the lateral surface of the calcaneus.
The medial ligament fans out from the malleolus, attaching distally to
the talus, calcaneus, and navicular via four adjacent and continuous
parts: the tibionavicular part, the tibiocalcaneal part, and the anterior and posterior tibiotalar parts. The medial ligament stabilizes the ankle joint during eversion and prevents subluxation (partial dislocation) of the joint.
|
Table 5.18. Joints of Foot
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
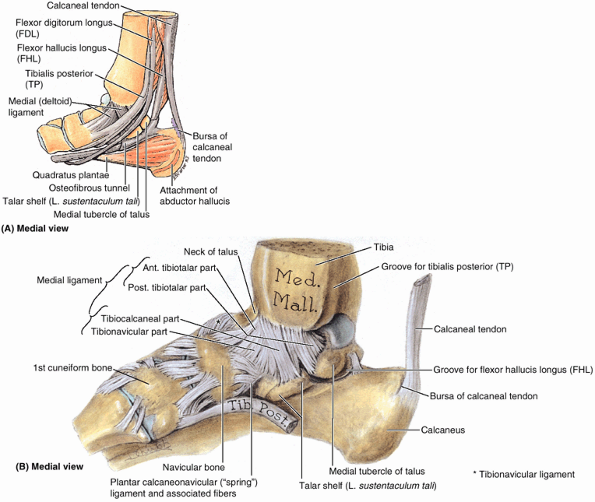 |
|
Figure 5.66. Ankle and tarsal joints. A.
The flexor tendons, which descend the posterolateral aspect of the ankle region and enter the foot, are shown as is their relationship to the medial malleolus and talar shelf. Except for the part tethering the flexor hallucis longus tendon, the flexor retinaculum has been removed. B. This dissection of the ankle and tarsal joints demonstrates the four parts of the medial (deltoid) ligament of the ankle. |
and plantarflexion of the foot, which occur around a transverse axis
passing through the talus (Table 5.18A).
Because the narrow end of the trochlea of the talus lies loosely
between the malleoli when the foot is plantarflexed, some “wobble”
(small amounts of abduction, adduction, inversion, and eversion) is
possible in this unstable position.
-
Dorsiflexion of the ankle is produced by the muscles in the anterior compartment of the leg (Table 5.10).
Dorsiflexion is usually limited by the passive resistance of the
triceps surae to stretching and by tension in the medial and lateral
ligaments. -
Plantarflexion of the ankle is produced by the muscles in the posterior compartment of the leg (Table 5.13). In toe dancing by ballet dancers, for example, the dorsum of the foot is in line with the anterior surface of the leg.
involving twisting of the weight-bearing plantarflexed foot. The person
steps on an uneven surface and the foot is forcibly inverted. Lateral ligament sprains
occur in sports in which running and jumping are common, particularly
basketball (70–80% of players have had at least one sprained ankle).
The lateral ligament is injured because it is much weaker than the
medial ligament and is the ligament that resists inversion at the
talocrural joint. The anterior talofibular ligament—part
of the lateral ligament—is most vulnerable and most commonly torn
during ankle sprains, either partially or completely, resulting in
instability of the ankle joint (Fig. B5.32). The calcaneofibular ligament may also be torn. In severe sprains, the lateral malleolus of the fibula may be fractured. Shearing injuries fracture the lateral malleolus at or superior to the ankle joint. Avulsion fractures break the malleolus inferior to the ankle joint; a fragment of bone is pulled off by the attached ligament(s).
This action pulls on the extremely strong medial ligament, often
tearing off the medial malleolus. The talus then moves laterally,
shearing off the lateral malleolus or, more commonly, breaking the
fibula superior to the tibiofibular syndesmosis. If the tibia is
carried anteriorly, the posterior margin of the distal end of the tibia
is also sheared off by the talus, producing a “trimalleolar fracture.”
In applying this term to this injury, the entire distal end of the
tibia is erroneously considered to be a “malleolus.”
leg by passing deep to the flexor retinaculum in the interval between
the medial malleolus and the calcaneus (Fig. 5.46B). Entrapment and compression of the tibial nerve (tarsal tunnel syndrome)
occurs when there is edema and tightness in the ankle involving the
synovial sheaths of the tendons of muscles in the posterior compartment
of the leg. The area involved is from the medial malleolus to the
calcaneus, and the heel pain results from compression of the tibial
nerve by the flexor retinaculum.
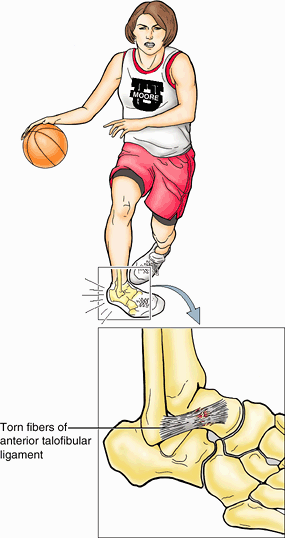 |
|
Figure B5.32
|
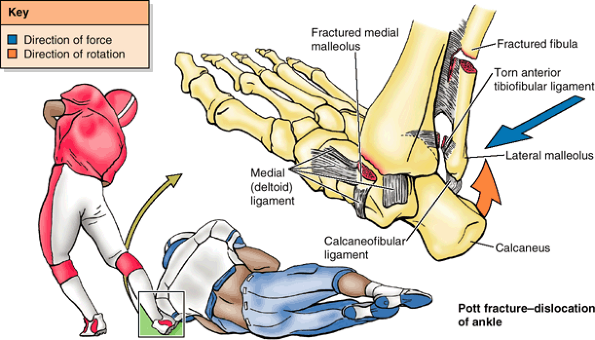 |
|
Figure B5.33
|
mortise, formed by the weight-bearing inferior surface of the tibia and
the two malleoli, which receive the trochlea of the talus. The joint is
maintained medially by a strong, medial (deltoid) ligament, and a much
weaker lateral ligament. The lateral ligament (specifically its
anterior talofibular ligament component) is the most frequently injured
ligament of the body. Injury occurs primarily by inadvertent inversion
of the plantarflexed, weight-bearing foot). About 70° of dorsiflexion
and plantarflexion is possible at the joint, in addition to which small
amounts of wobble occur in the less stable plantarflexed position.
are relatively small and are so tightly joined by ligaments that only
slight movement occurs between them. In the foot, flexion and extension
occurs in the forefoot at the metatarsophalangeal and interphalangeal
joints (Table 5.19) Inversion is augmented by
flexion of the toes (especially the great and 2nd toes), and eversion
by their extension (especially of the lateral toes). All bones of the
foot proximal to the metatarsophalangeal joints are united by dorsal
and plantar ligaments. The bones of the metatarsophalangeal and
interphalangeal joints are united by lateral and medial collateral
ligaments.
is a single synovial joint between the slightly concave posterior
calcaneal articular surface of the talus and the convex posterior
articular facet of the calcaneus (Table 5.18). The joint capsule is weak but is supported by medial, lateral, posterior, and interosseous talocalcaneal ligaments (Fig. 5.65). The interosseous talocalcaneal ligament lies within the tarsal sinus, which separates the subtalar and talocalcaneonavicular joints and is especially strong. Orthopaedic surgeons use the term subtalar joint for the compound functional joint consisting of the anatomical subtalar joint plus the talocalcaneal part of the talocalcaneonavicular joint. The two separate elements of the clinical subtalar joint
straddle the talocalcaneal interosseous ligament. Structurally, the
anatomical definition is logical because the anatomical subtalar joint
is a discrete joint, having its own joint capsule and articular cavity.
Functionally, however, the clinical definition is logical because the
two parts of the compound joint function as a unit; it is impossible
for them to function independently. The subtalar joint (by either
definition) is where the majority of inversion and eversion occurs,
around an axis that is oblique.
part of the talocalcaneonavicular joint
At this joint, the midfoot and forefoot rotate as a unit on the
hindfoot around a longitudinal (AP) axis, augmenting the inversion and
eversion movements occurring at the clinical subtalar joint.
Transection across the transverse tarsal joint is a standard method for
surgical amputation of the foot.
|
Table 5.19. Movements of the Joints of the Forefoot and the Muscles Producing Them
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||
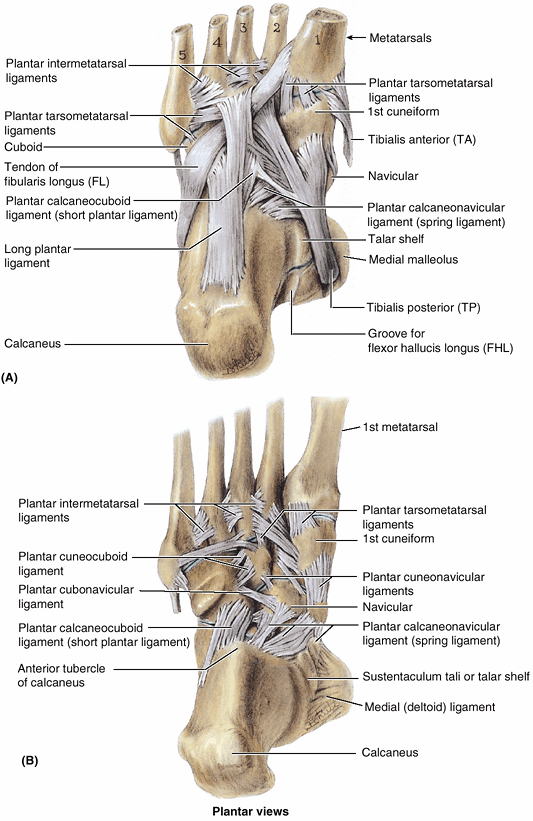 |
|
Figure 5.67. Plantar ligaments. A and B.
Deep dissection of the sole of the right foot showing the attachments of the ligaments and the long tendons of the long evertor and invertor muscles. The main ligaments from this view are the plantar calcaneonavicular and the long and short plantar ligaments. |
-
Plantar calcaneonavicular ligament (spring ligament), which extends across and fills a wedge-shaped gap between the talar shelf and the inferior margin of the posterior articular
P.710
surface of the navicular (Fig. 5.67A & B).
The spring ligament supports the head of the talus and plays important
roles in the transfer of weight from the talus and in maintaining the
longitudinal arch of the foot, of which it is the keystone
(superiormost element). -
Long plantar ligament,
which passes from the plantar surface of the calcaneus to the groove on
the cuboid. Some of its fibers extend to the bases of the metatarsals,
thereby forming a tunnel for the tendon of the fibularis longus (Fig. 5.67A). The long plantar ligament is important in maintaining the longitudinal arch of the foot. -
Plantar calcaneocuboid ligament (short plantar ligament), which is located on a plane between the plantar calcaneonavicular and the long plantar ligaments (Fig. 5.67B).
It extends from the anterior aspect of the inferior surface of the
calcaneus to the inferior surface of the cuboid. It is also involved in
maintaining the longitudinal arch of the foot.
the ground would generate extremely large forces of short duration
(shocks) that would be propagated through the skeletal system. Because
the foot is composed of numerous bones connected by ligaments, it has
considerable flexibility that allows it to deform with each ground
contact, thereby absorbing much of the shock. Furthermore, the tarsal
and metatarsal bones are arranged in longitudinal and transverse arches
passively supported and actively restrained by flexible tendons that
add to the weight-bearing capabilities and resiliency of the foot. Thus
much smaller forces of longer duration are transmitted through the
skeletal system.
(foot), acting not only as shock absorbers but also as springboards for
propelling it during walking, running, and jumping. The resilient
arches add to the foot’s ability to adapt to changes in surface
contour. The weight of the body is transmitted to the talus from the
tibia. Then it is transmitted posteriorly to the calcaneus and
anteriorly to the “ball of the foot” (the sesamoids of the 1st
metatarsal and the head of the 2nd metatarsal), and that
weight/pressure is shared laterally with the heads of the 3rd–5th
metatarsals as necessary for balance and comfort (Fig. 5.68).
Between these weight-bearing points are the relatively elastic arches
of the foot, which become slightly flattened by body weight during
standing. They normally resume their curvature (recoil) when body
weight is removed.
The tibialis anterior, attaching to the 1st metatarsal and medial
cuneiform, helps strengthen the medial longitudinal arch. The fibularis
longus tendon, passing from lateral to medial, also helps support this
arch (Fig. 5.69A). The lateral longitudinal arch is much flatter than the medial part of the arch and rests on the ground during standing (Fig. 5.69B & D). It is made up of the calcaneus, cuboid, and lateral two metatarsals.
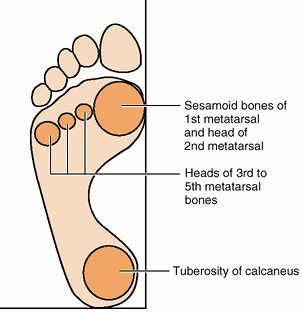 |
|
Figure 5.68. Weight-bearing areas of foot.
Body weight is divided approximately equally between the hindfoot (calcaneus) and the forefoot (heads of the metatarsals). The forefoot has five points of contact with the ground: a large medial one that includes the two sesamoid bones associated with the head of the 1st metatarsal and the heads of the lateral four metatarsals. The 1st metatarsal supports the major share of the load, with the lateral forefoot providing balance. |
It is formed by the cuboid, cuneiforms, and bases of the metatarsals.
The medial and lateral parts of the longitudinal arch serve as pillars
for the transverse arch. The tendons of the fibularis longus and
tibialis posterior, crossing under the sole of the foot like a stirrup (Fig. 5.69C),
help maintain the curvature of the transverse arch. The integrity of
the bony arches of the foot is maintained by both passive factors and
dynamic supports (Fig. 5.69E).
-
The shape of the united bones (both arches, but especially the transverse arch).
-
Four successive layers of fibrous tissue that bowstring the longitudinal arch (superficial to deep):
-
Plantar aponeurosis.
-
Long plantar ligament.
-
Plantar calcaneocuboid (short plantar) ligament.
-
Plantar calcaneonavicular (spring) ligament.
-
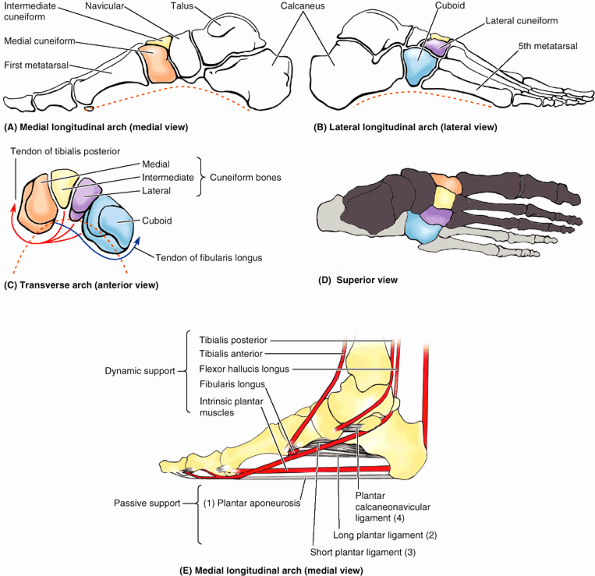 |
|
Figure 5.69. Arches of foot. A and B. The medial longitudinal arch is higher than the lateral longitudinal arch, which may contact the ground when standing erect. C.
The transverse arch is demonstrated at the level of the cuneiforms, receiving stirrup-like support from a major invertor (tibialis posterior) and evertor (fibularis longus). D. The components of the medial (dark gray) and lateral (light gray) longitudinal arches are indicated. The calcaneus (medium gray) is common to both. The medial arch is primarily weight bearing, whereas the lateral arch provides balance. E. The active (red lines) and passive (gray) supports of the longitudinal arches are represented. There are four layers of passive support (1–4). |
-
Active (reflexive) bracing action of intrinsic muscles of foot (longitudinal arch).
-
Active and tonic contraction of muscles with long tendons extending into foot:
-
Flexors hallucis and digitorum longus for the longitudinal arch.
-
Fibularis longus and tibialis posterior for the transverse arch.
-
aponeurosis bear the greatest stress and are most important in
maintaining the arches of the foot.
foot: (1) the clinical subtalar joint between the talus and the
calcaneus, where inversion and eversion occur about an oblique axis;
(2) the transverse tarsal joint, where the midfoot and forefoot rotate
as a unit on the hindfoot around a longitudinal axis, augmenting
inversion and eversion; and (3) the remaining joints of the foot, which
allow the pedal platform (foot) to form dynamic longitudinal and
transverse arches. The arches provide the resilience necessary for
walking, running, and jumping, and are maintained by four layers of
passive, fibrous support plus the dynamic support provided by the
intrinsic muscles of the foot and the long fibular, tibial, and flexor
tendons.
deformity caused by pressure from footwear and degenerative joint
disease; it is characterized by lateral deviation of the great toe (Fig. B5.34). The L in valgus indicates l ateral deviation. In some people, the painful deviation is so large that the great toe overlaps the 2nd toe (Fig. B5.34A),
and there is a decrease in the medial longitudinal arch. Such deviation
occurs especially in females, and its frequency increases with age.
These individuals cannot move their 1st digit away from their 2nd digit
because the sesamoids under the head of the 1st metatarsal are usually
displaced and lie in the space between the heads of the 1st and 2nd
metatarsals (Fig. B5.34B).
The 1st metatarsal shifts medially and the sesamoids shift laterally.
Often the surrounding tissues swell and the resultant pressure and
friction against the shoe cause a subcutaneous bursa to form; when
tender and inflamed, the bursa is called a bunion (Fig. B5.34A). Often hard corns (inflamed areas of thick skin) also form over the proximal interphalangeal joints, especially the little toe.
deformity in which the proximal phalanx is permanently and markedly
dorsiflexed (hyperextended) at the metatarsophalangeal joint and the
middle phalanx strongly plantarflexed at the proximal interphalangeal
joint. The distal phalanx of the digit is often also hyperextended.
This gives the digit (usually the 2nd) a hammer-like appearance (Fig. B5.35A).
This deformity of one or more toes may result from weakness of the
lumbrical and interosseous muscles, which flex the metatarsophalangeal
joints and extend the interphalangeal joints. A callosity or callus,
hard thickening of the keratin layer of the skin, often develops where
the dorsal surface of the toe repeatedly rubs on the shoe.
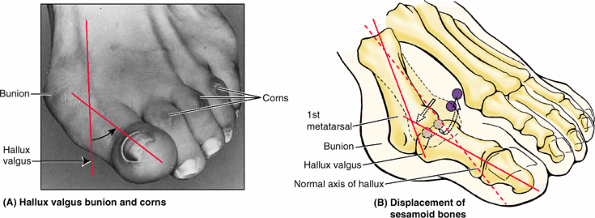 |
|
Figure B5.34
|
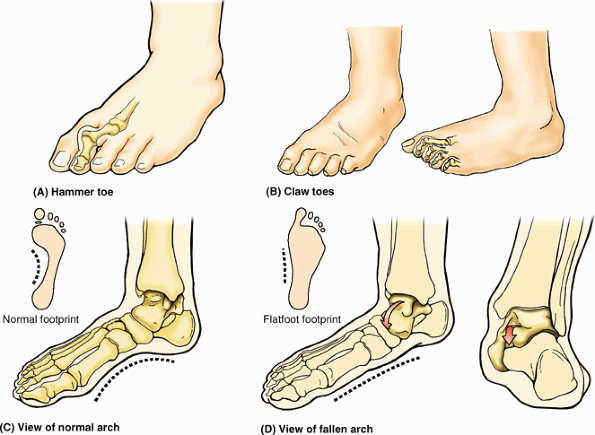 |
|
Figure B5.35
|
Usually, the lateral four toes are involved. Callosities develop on the
dorsal surfaces of the toes because of pressure of the shoe. They may
also form on the plantar surfaces of the metatarsal heads and the toe
tips because they bear extra weight when claw toes are present.
and results from the thick subcutaneous fat-pad in the sole. As
children get older, the fat is lost, and a normal medial longitudinal
arch becomes visible (Fig. B5.35C). Flatfeet can either be flexible (flat, lacking a medial arch, when weight bearing but normal in appearance when not bearing weight [Fig. B5.35D]) or rigid (flat even when not bearing weight). The more common flexible flatfeet
result from loose or degenerated intrinsic ligaments (inadequate
passive arch support). Flexible flatfoot is common in childhood but
usually resolves with age as the ligaments grow and mature. The
condition occasionally persists into adulthood and may or may not be
symptomatic.
history that goes back to childhood are likely to result from a bone
deformity (such as a fusion of adjacent tarsal bones). Acquired flatfeet
(“fallen arches”) are likely to be secondary to dysfunction of the
tibialis posterior (dynamic arch support) owing to trauma, degeneration
with age, or denervation. In the absence of normal passive or dynamic
support, the plantar calcaneonavicular ligament fails to support the
head of the talus. Consequently, the talar head displaces
inferomedially and becomes prominent (Fig. B5.35D, red arrow).
As a result, some flattening of the medial part of the longitudinal
arch occurs, along with lateral deviation of the forefoot. Flatfeet are
common in older people, particularly if they undertake much
unaccustomed standing or gain weight rapidly, adding stress on the
muscles and increasing the strain on the ligaments supporting the
arches.
the common type (2 per 1000 live births), involves the subtalar joint;
boys are affected twice as often as girls. The foot is inverted, the
ankle is plantarflexed, and the forefoot is adducted (turned toward the
midline in an abnormal manner) (Fig. B5.36). The foot assumes the position of a horse’s hoof, hence the prefix “equino” (L. equinus,
horse). In half of those affected, both feet are malformed. A person
with an uncorrected clubfoot cannot put the heel and sole flat and must
bear the weight on the lateral surface of the forefoot. Consequently,
walking is painful. The main abnormality is shortness and tightness of
the muscles, tendons, ligaments, and joint capsules on the medial side
and posterior aspect of the foot and ankle.
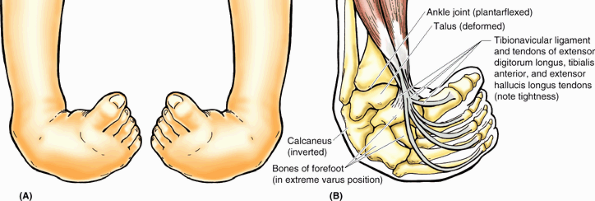 |
|
Figure B5.36
|
may be palpated as it passes posterior and distal to the medial
malleolus, then superior to the talar shelf, to reach its attachment to
the tuberosity of the navicular. Hence the tibialis posterior tendon is
the guide to the navicular. The tendon of the tibialis posterior also
indicates the site for palpating the posterior tibial pulse (halfway between the medial malleolus and the calcaneal tendon).
approximately 2 cm distal to the tip of the medial malleolus, is best
felt by palpating it from below where it is somewhat obscured by the tendon of the flexor digitorum longus, which crosses it (Fig. SA5.4B). On the lateral side, when the foot is inverted, the lateral margin of the anterior surface of the calcaneus is uncovered and palpable. This indicates the site of the calcaneocuboid joint. When the foot is plantarflexed, the head of the talus is exposed. Palpate it dorsal to where the anterior surface of the calcaneus is felt. The calcaneal tendon at the posterior aspect of the ankle is easily palpated and traced to its attachment to the calcaneal tuberosity.
In the depression on each side of the tendon, the ankle joint is
superficial. When the joint is overfilled with fluid, these depressions
may be obliterated.
satisfactorily only when their muscles are acting. The tendons of the
fibularis longus and brevis may be followed distally, posterior and
inferior to the lateral malleolus, and then anteriorly along the
lateral aspect of the foot (Fig. SA5.4C). The fibularis longus tendon can be palpated as far as the cuboid, and then it disappears as it turns into the sole. The fibularis brevis tendon
can easily be traced to its attachment to the dorsal surface of the
tuberosity on the base of the 5th metatarsal. This tuberosity is
located at the middle of the lateral border of the foot. With toes
actively extended, the small fleshy belly of the extensor digitorum brevis
may be seen and palpated anterior to the lateral malleolus. Its
position should be observed and palpated so that it may not be mistaken
subsequently for an abnormal edema.
-
The large tendon of the tibialis anterior leaves the cover of the superior extensor tendon (Fig. SA5.4A),
from which level the tendon is invested by a continuous synovial
sheath; the tendon may be traced to its attachment to the 1st cuneiform
and the base of the 1st metatarsal. -
The tendon of the extensor hallucis longus,
obvious when the great toe is dorsiflexed against resistance, may be
followed to its attachment to the base of the distal phalanx of the
great toe. -
The tendons of the extensor digitorum longus may be followed easily to their attachments to the lateral four toes (Fig. SA5.4C).
-
The tendon of the fibularis tertius may also be traced to its attachment to the base of the 5th metatarsal. This muscle is of minor importance and may be absent.
is indicated by a line from the posterior aspect of the tuberosity of
the navicular to a point halfway between the lateral malleolus and the
tuberosity of the 5th metatarsal (Table 5.18).
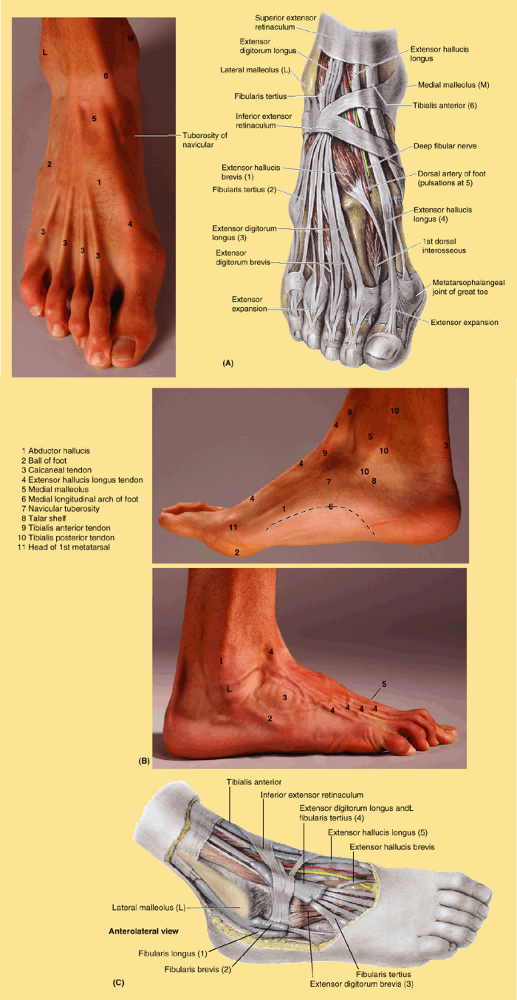 |
|
Figure SA5.4
|
abnormalities or malalignment. In the AP projection of the hip joint
shown in Figure 5.70A,
the patient is in the supine position on the radiographic table. The
central X-ray beam is centered over the hip joint (see orientation
figures). Superimposed on the femoral head is the posterior rim of the
acetabulum (PR). At the junction of the femoral neck and shaft, the
greater and lesser trochanters may be seen. Between the trochanters is
an oblique line cast by the superimposed intertrochanteric line and
crest (IC).
(i.e., on film or a monitor), observe the architecture of the
trabecular bone of the head, neck, and proximal shaft of the femur. The
strength of the angled bone depends on this structure. In a healthy
femur without osteoporosis, the trabeculae correspond to tension and
pressure lines reflecting the weight-bearing function of this bone. The
dense compact bone appears transparent (white), whereas the less dense
spongy bone appears dark.
in specific views are used to assess normal alignment of bony features.
Interrupted lines, irregular curve or lack of symmetry between left and
right sides indicates dislocations, fractures, or slipped epiphyses. To
ensure detection of a fracture of the femoral neck, several views must
be obtained (Fig. 5.70B).
oblique) are necessary to evaluate the knee properly. In an AP
projection of the knee joint (Fig. 5.71B),
the person is in the supine position with the knee extended. The
central X-ray beam is directed through the joint cavity. Outlines of
the femoral and tibial condyles and the shadows of the patella are
superimposed over the distal end of the femur. The joint cavity appears
large because the menisci are not visible. The menisci can be
visualized if air or opaque fluid is injected into the joint cavity.
The adductor tubercle is evident just superior to the medial epicondyle
of the femur. The lateral femoral epicondyle appears more prominent
than the medial one. The intercondylar fossa is opposite the medial and
lateral tubercles of the intercondylar eminence of the proximal tibia.
The articular surfaces of the condyles of the tibia are concave in an
AP view.
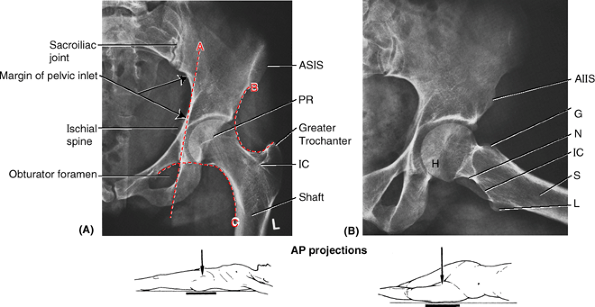 |
|
Figure 5.70. Radiographs of normal hip joint. A. On the femur, observe the head, neck, greater trochanter, intertrochanteric crest (IC), and shaft. On the hip bone, observe the lunate surface of the acetabulum, the posterior rim of the acetabulum (PR), the anterior superior iliac spine (ASIS),
the ischial spine, and the sacroiliac joint. Several different lines and curvatures are used in the detection of hip abnormalities (dislocations, fractures or slipped epiphyses). The Kohler line (A) is normally tangential to the pelvic inlet and the obturator foramen. The acetabular fossa should lie lateral to this line. A fossa that crosses the line suggests an acetabular fracture with inward displacement. The Shenton line (B) and the iliofemoral line (C) should appear in a normal AP radiograph as smooth, continuous lines that are bilaterally symmetrical. The Shenton line is a radiographic indication of the angle of inclination. B. In this view the left thigh was abducted. Observe the acetabular fossa, anterior inferior iliac spine (AIIS), head of the femur (H), neck of the femur (N), greater trochanter (G), lesser trochanter (L), intertrochanteric crest (IC), and shaft of femur (S). |
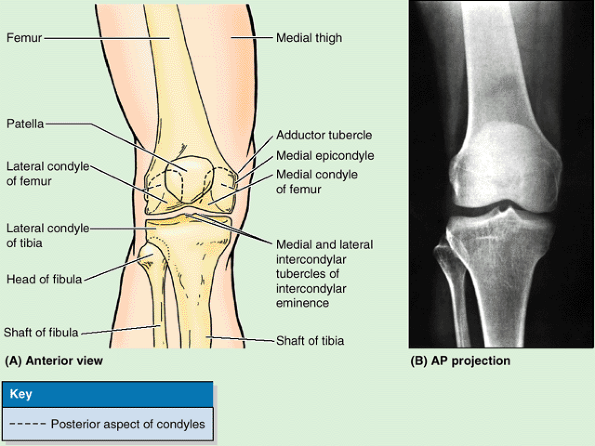 |
|
Figure 5.71. Knee joint. A and B. The orientation drawing depicts the structures visible in the AP radiograph of the right knee joint.
|
the knee is slightly flexed. A contrast medium was injected through the
joint capsule to show the joint cavity and the extent of the synovial
membrane. The articular cartilage on the femoral condyle is radiolucent
and the fibrous layer of the joint capsule, lined with synovial
membrane, is distinct. The large suprapatellar bursa is continuous with
the joint cavity. Although MRI has largely replaced arthrography, it is
sometimes useful for detecting loose articular bodies if the MRI is
inconclusive.
and foot are lateral and AP. A lateral radiograph is taken with the
lateral malleolus placed against the X-ray detector (Fig. 5.73A). In Figure 5.73,
the articulation of the convex surface of the trochlea of the talus (T)
with the malleoli of the tibia and fibula is apparent, and shadows of
the malleoli are visible. The neck (N) and head (H) of the talus, the
disc-shaped navicular (Na), and the talonavicular joint can be seen.
The calcaneus (Ca) and cuboid (C) articulate at the calcaneocuboid
joint. The tarsal sinus (TS), the space between the calcaneus and talus, contains the interosseous talocalcaneal ligament.
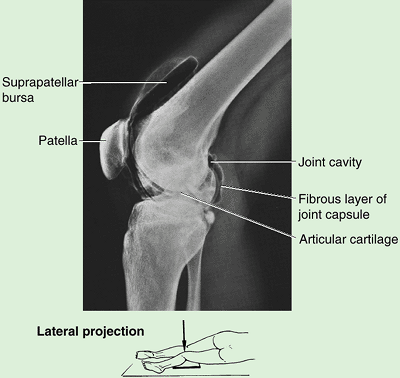 |
|
Figure 5.72. Arthrogram of knee joint.
Contrast medium was injected into the synovial cavity. The knee is slightly flexed. The large suprapatellar bursa communicates with the knee joint cavity. |
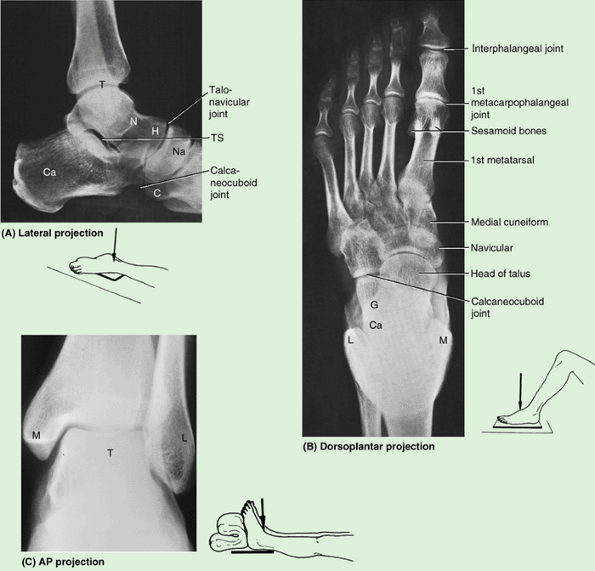 |
|
Figure 5.73. Radiographs of lower leg, ankle, and foot. A. The left foot is shown in a neutral position. B. The left foot, in slight plantarflexion, is shown. C. The left ankle is shown. C, cuboid; Ca, calcaneus; H, head of talus; L, lateral malleolus; M, medial malleolus; N, neck of talus; Na, navicular; T, talus; TS, tarsal sinus (tunnel). (Part C Courtesy of Dr. P. Bobechko and Dr. E. Becker, Department of Medical Imaging, University of Toronto, Toronto, Ontario, Canada.)
|
with the knee flexed, and the plantar surface of the foot is placed on
the X-ray detector (Fig. 5.73B).
The central X-ray beam is centered on the base of the 3rd metatarsal.
This view demonstrates the phalanges and interphalangeal joints.
However, because the toes are in slight flexion, the interphalangeal
joints of the 2nd–5th toes are not clear. The sesamoids on the plantar
surface of the head of the 1st metatarsal are evident, as is the
articulation of the base of the 1st metatarsal with the medial
cuneiform and the base of the 2nd metatarsal. The bases of the 2nd–5th
metatarsals overlap, so the intermetatarsal joints are easy to see. The
tarsal bones overlap somewhat because of the normal curvature of the
foot. Consequently, all the tarsal joints do not show clearly. Only
anterior parts of the talus and calcaneus are visible because of the
overlap of the malleoli.
position with the foot dorsiflexed to a right angle and the great toe
pointed slightly medially (Fig. 5.73C). To visualize all the bones and joints of the ankle and foot, other projections are required.
injection of a radiopaque contrast medium is a helpful way of studying
selected arteries to determine the existence of abnormalities such as popliteal aneurysm (circumscribed dilation of the popliteal artery). In a popliteal arteriogram (Fig. 5.74),
the radiopaque material is injected into the femoral artery and spreads
through the popliteal artery and its branches, the tibial and fibular
arteries.
angles; however, the images are created by computer reconstructions of
the data. CT scans can be set to display soft tissues or bone.
Hypodense areas on CT scans suggest strains (swelling), and hyperdense
areas suggest hematomas. CT of the knee (arthrotomography) provides a
reliable assessment of the cruciate ligaments, menisci, patellar
cartilage, and localizes of osteochondral defects and loose bodies.
without the use of radiation. MRI scanning requires the individual to
keep the limbs motionless for 5–10 min. MRIs show much more detail in
the soft tissues than do radiographs or CTs (Figs. 5.75, 5.76, 5.77 and 5.78).
joint capsule of the joint is thick near the iliofemoral ligament and
thin posterior to the psoas bursa and tendon. In sections at this
level, the femoral sheath, which encloses the femoral artery, vein,
lymph node, lymphatic vessels, and fat, protrudes into the subcutaneous
tissue. The loose connective tissue nearly surrounds it except
posteriorly where, between the iliopsoas and the pectineus, it is
attached to the capsule of the hip joint. The femoral artery is
separated from the hip joint by the iliopsoas muscle and/or tendon. In
the interval between the iliopsoas, the pectineus, and the femoral
nerve, the femoral vein lies between the iliopsoas and its fascia.
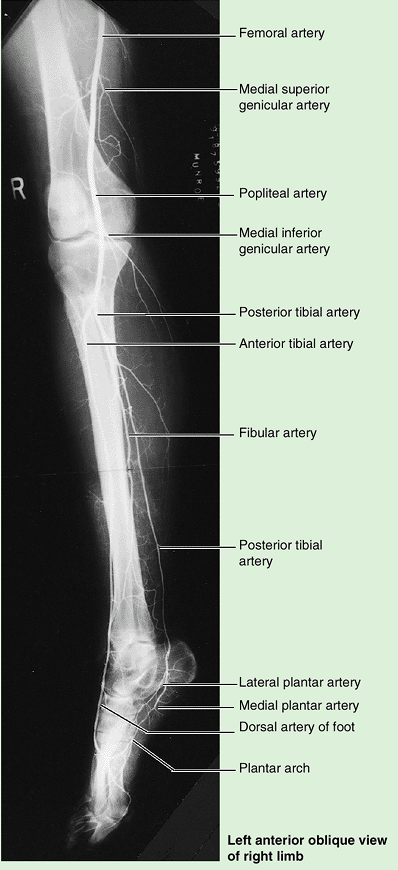 |
|
Figure 5.74. Popliteal arteriogram.
The popliteal artery begins at the site of the adductor hiatus (where it may be compressed) and then lies successively on the distal end of the femur, joint capsule of the knee joint, and popliteus muscle (not visible) before dividing into the anterior and posterior tibial arteries at the inferior angle of the popliteus fossa. Here it is subject to entrapment as it passes beneath the tendinous arch of the soleus muscle. (Courtesy of Dr. K. Sniderman, Associate Professor of Medical Imaging, University of Toronto, Toronto, Ontario, Canada) |
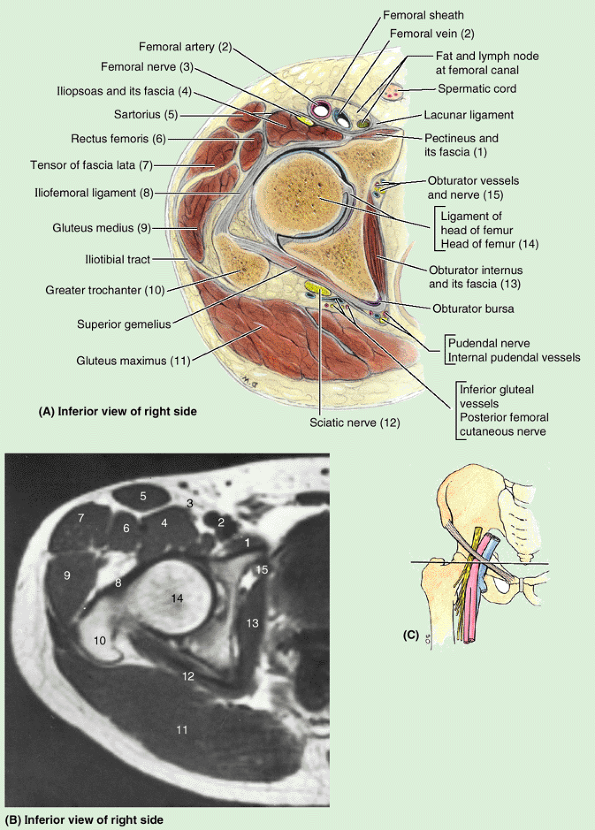 |
|
Figure 5.75. Sectional and radiographic anatomy of gluteal region and proximal anterior thigh at level of hip joint. A and B. A descriptive drawing and transverse (axial MRI) study of an anatomical section of the thigh are shown. C. The orientation drawing shows the level of the section.
|
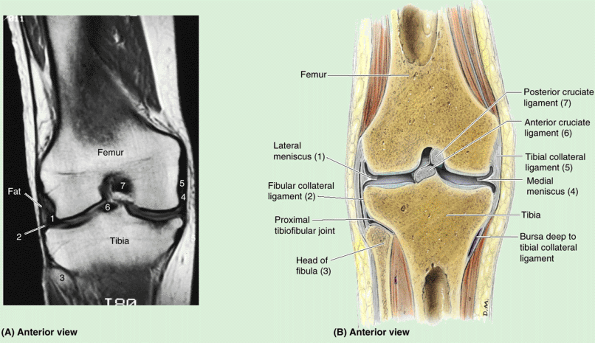 |
|
Figure 5.76. Sectional anatomy of knee joint. A and B.
The orientation drawing depicts the structures visible in the coronal MRI of the knee joint. (Courtesy of Dr. W. Kucharczyk, Professor and Chair of Medical Imaging, University of Toronto, and Clinical Director of Tri-Hospital Magnetic Resonance Centre, Toronto, Ontario, Canada.) |
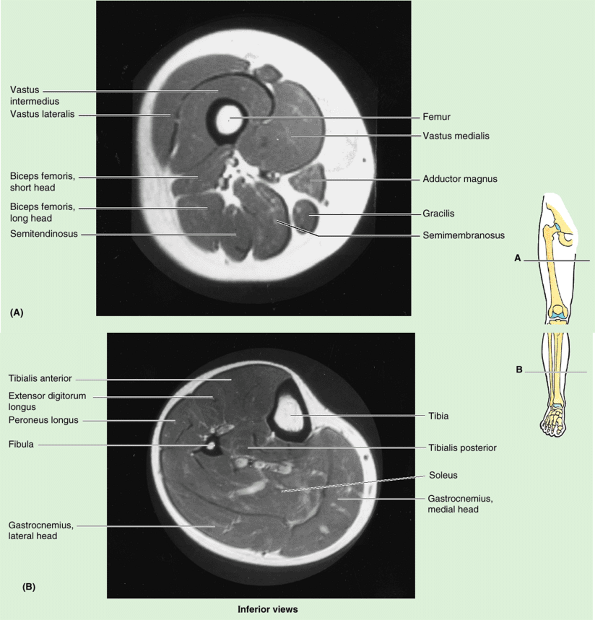 |
|
Figure 5.77. Transverse MRIs of lower limb, from below. A. Sections at the mid-thigh level (A) and mid-leg level (B) are shown.
|
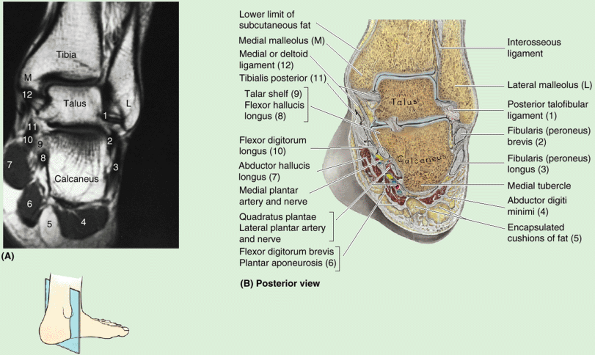 |
|
Figure 5.78. Sectional anatomy of ankle region. A and B.
The orientation drawing depicts the structures visible in the MRI of the ankle. (Courtesy of Dr. W. Kucharczyk, Professor and Chair of Medical Imaging, University of Toronto, and Clinical Director of Tri-Hospital Magnetic Resonance Centre, Toronto, Ontario, Canada.) |
the tibia rests on the talus and the talus rests on the calcaneus.
Between the calcaneus and the skin, several encapsulated cushions of
fat are evident. It is also clearly seen that the lateral malleolus
descends much farther inferiorly than the medial malleolus. In the
anatomical coronal section, the interosseous band between the talus and
calcaneus separates the subtalar joint from the talocalcaneonavicular
joint. Both the anatomical section and the MRI demonstrate the talar
shelf acting as a pulley for the flexor hallucis longus and giving
attachment to the calcaneotibial band of the medial ligament.
of its anterior position, the tensor of the fascia lata is often
studied with the anterior thigh muscles for convenience (i.e., when the
cadaver is supine); however, it is actually part of the gluteal group,
and will be included with that group in this book.