The Wrist and Hand
posturing of the digit. The deformity may follow trauma to the central
slip portion of the extensor mechanism. It may occur from a laceration
involving the proximal interphalangeal (PIP) joint or from a closed,
axial force applied to the digit resulting in a rupture of the central
slip. More commonly, the boutonnière deformity is caused by central
slip attenuation due to PIP joint destruction from rheumatoid
arthritis. Much like a small bouquet of flowers protruding through a
buttonhole in the lapel of a suit, the proximal interphalangeal joint
protrudes through the attenuated extensor mechanism of the digit.
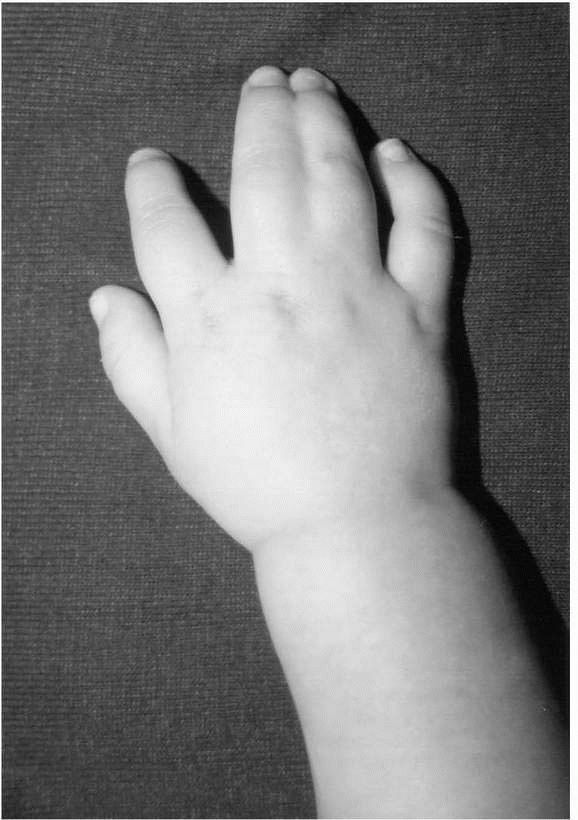
include hyperextension of the metacarpal phalangeal (MCP) joint,
flexion contracture of the proximal interphalangeal (PIP) joint,
hyperextension of the distal interphalangeal (DIP) joint, and
incompetence or attenuation of the central portion of the extensor
mechanism (Figure 14-1). The deformity can be
classified as either mild, moderate, or severe. The PIP joint
contracture in the mild or moderate varieties is considered passively
correctable, while the PIP joint contracture in the severe boutonnière
deformity is rigid or fixed and is not passively correctable.
prophylactic in the case of open or closed trauma of the extensor
mechanism. Lacerations of the central slip demand careful scrutiny and
prompt attention to prevent flexion posturing of the PIP joint and
ultimate failure of the extensor mechanism. In the event of a closed
rupture, the central slip is treated by splinting. Alternatively, the
boutonniere deformity seen in rheumatoid arthritis may be treated with
PIP joint synovectomy or reconstruction of the extensor mechanism when
the deformity is mild or moderate. In advanced cases, PIP joint
arthrodesis (fusion) or joint replacement arthroplasty is needed. In
general, soft tissue reconstruction of the boutonnière deformity has
been disappointing. The results from treatment with arthrodesis have
been more predictable.
entity seen by the hand surgeon, with some reporting that the condition
affects up to 10% of the general population—an estimated cost to the
U.S. medical system well beyond $1,000,000,000. When considering time
lost from work, the cost to society as a whole is substantial. Risk
factors for the condition include female, diabetes, hypothyroidism,
obesity, pregnancy, rheumatoid arthritis, gout, precious trauma,
acromegaly, smoking, old age, peripheral neuropathy, occupational
vibrational exposure, and renal disease.
 |
|
FIGURE 14-1. Posttraumatic Boutonnière deformity.
|
axonal transport within the median nerve is compromised with carpal
tunnel pressures of 30 mm Hg. This is a carpal canal pressure
clinically achievable in the carpal tunnel patient. Pressures in excess
of 30 m Hg have been shown in the patient who frequently flexes and
extends the wrist, pronates and supinates the forearm, or repeatedly
grasps objects. The consequence of chronic compression is damage to the
epineural covering of the median nerve resulting in diminished
conduction velocity.
information gathered from the history, physical examination, and
electrodiagnostic studies. The classic complaint from the patient
bothered by carpal tunnel syndrome is paresthesias at night.
Paresthesias are typically tingling or numbness in the median nerve
distribution of the hand. However, paresthesias can be characterized by
some patients as “pins and needles,” burning, or simply pain. Secondary
symptoms include paresthesias encountered while holding a book or
newspaper (“reading paresthesias”) or paresthesias encountered while
driving (“driving paresthesias”). Other complaints vary from
“clumsiness” of the hands, such that objects are often dropped and fine
digital tasks are difficult, to
generalized hand weakness. In the elderly complaints of “constant numbness” are often heard.
at the wrist, or the carpal tunnel compression test (Durkan’s test).
The carpal tunnel compression test is generally regarded as the most
sensitive. This test is administered by holding pressure directly over
the median nerve at the wrist. A positive test is acknowledged when the
patient experiences paresthesias in the median nerve distribution
within 30 seconds of the onset of the test. The most predictable
sensory test to evaluate carpal tunnel syndrome is the Semmes-Weinstein
monofilament test, where threshold testing of sensation is performed
using various sizes of nylon filaments. Vibrometry has also been shown
to be a useful sensory test for carpal tunnel syndrome.
electrodiagnostic testing for diagnosing carpal tunnel syndrome is
debated by some. Finsen et al. reported in one
series that 22% of patients who had normal nerve electrodiagnostic
studies had a good outcome following carpal tunnel release surgery,
indicating a substantial false-positive rate for the testing.
Electrodiagnostic tests include the nerve conduction velocity (NCV)
measurements and the electromyogram (EMG). The NCV is considered
positive for carpal tunnel syndrome when the median motor distal
latency is >4.5 ms or the distal sensory latency is >3.5 ms. In
more advanced cases, diminished action potential may also be seen. On
the EMG portion of the study, the presence of positive sharp waves,
increased insertional activity, decreased muscle recruitment, or
polyphasic activity is indicative of substantial nerve dysfunction.
splinting, particularly for mild or moderate carpal tunnel syndrome.
When consistently used for a period of 4 to 6 weeks, permanent relief
of symptoms can ensue. Other nonoperative measures include nonsteroidal
anti-inflammatory agents (NSAIDs), carpal tunnel injections,
ultrasound, phonophoresis, nerve gliding or stretching, and vitamin B6.
No data shows any clear advantage of adding these measures with or
instead of splinting. Corticosteroid injections have been shown to have
long-term efficacy in only 22% of patients with symptoms longer than 1
year. Relief of symptoms following injections has been shown to
correlate as a predictor of surgical success. Work modifications to
prevent sustained wrist movements or provocative wrist positioning may
play a greater role than any of the nonoperative measures except
splinting. Some studies have suggested the preventative effect of wrist
and hand exercises in certain occupational environments.
considered when two of the following criteria are meet following at
least a 3-month course of nonoperative care: persisting symptoms,
positive physical examination, and positive electrodiagnostic testing.
Absolute indications for surgery are constant paresthesias, thenar
atrophy, and markedly delayed median motor nerve conduction velocity or
abnormal EMG testing. The surgical procedure consists of increasing the
volume of the carpal canal by transecting the transverse carpal
ligament. An MRI study has shown that division of the transverse carpal
ligament expands the volume of the carpal canal by as much as 25%. In
some instances, such as in rheumatoid arthritis, the addition of a
flexor tenosynovectomy is needed. The surgical procedure is most
commonly performed through a small longitudinal incision at the base of
the palm, in line with the ring finger. Care must be taken to avoid
injury to the thenar motor branch of the median nerve, which has
variable anatomy. Misplaced or transverse incisions about the wrist may
jeopardize the palmar cutaneous branch of the median nerve. Other
reported complications with open carpal tunnel decompression include
ulnar nerve and artery injury.
decompression is the endoscopic carpal tunnel release. Various authors
have reported success rates equal to the open carpal tunnel release
with less scar tenderness and quicker return to work. Concerns still,
however, remain regarding the safety and efficacy of the endoscopic
technique. Van Heest et al., Lee et al., and Schwartz et al., have
reported incomplete release of the transverse carpal ligament using the
endoscopic technique in cadaver models. Devastating complications such
as median nerve transection and flexor tendon transection have been
reported causing some to carefully scrutinize the routine use of the
endoscopic technique.
chosen, it has been well established that success from carpal tunnel
surgery can approach 98% when only subjective complaints are
considered. It has been generally held that these results diminish with
age. It has been shown that workers applying for worker’s compensation
can be anticipated to have worse overall results and a slower recovery
compared to a similar group of patients not submitting worker’s
compensation claims.
(RSD) to identify a condition that included pain, swelling,
hyperhydrosis, skin color changes, skin temperature changes, stiffness,
and underlying osteoporosis, with all symptoms potentially reversible
with stellate ganglion blockade. Other terms often used in place of RSD
include Sudeck’s atrophy, shoulder-hand syndrome, or “allodynia.”
These complex and often confusing terms for pain of uncertain origin
has lead to the classification system of complex regional pain syndrome
(CRPS) typed I and II. Simply stated, CRPS type I is a condition
whereby pain had developed following an inciting painful circumstance.
In this condition the pain, however, seems to develop out of proportion
to the clinical situation. Associated findings include edema, skin
blood flow changes, and abnormal sudomotor activity such as
hyperhydrosis. CRPS type II has a similar clinical presentation but is
associated with a known nerve injury. The predominant symptoms and
findings of the initial stage are constant pain, hyperhydrosis, and a
hypersensitivity to touch. The second stage of the condition is
characterized more by stiffness and pain, while in stage III patients
experience diminished pain but overall disuse of the extremity. The
pathophysiology of CRPS is still unknown.
is the physical examination. Other less reliable tests include the
three-phase bone scan, thermography, the quantitative sudomotor axon
reflex test (QSART), and plain radiography. Increased uptake is
anticipated in the later phases of the bone scan while osteopenia is a
later finding in the CRPS patient. CRPS I has been reported to occur
following as many as 25% of all distal radius fractures. A risk factor
is displacement requiring reduction. It is generally regarded that
those patients experiencing CRPS of an extremity are at greater risk of
recurrent symptoms following a surgical procedure.
recognition and diagnosis. Most patients diagnosed within the first 6
to 8 weeks respond favorably to treatment. Initially, hand therapy
plays an important role in the treatment of CRPS. Such techniques as
massage, edema control, gentle passive motion (to prevent contracture),
contrast baths, and use of the transelectrical stimulator unit (TENS)
have proven effective. The key concept to remember when embarking on
hand therapy is the patient must be exercised within the limits of
pain, otherwise a flare-up of the condition may result. Initial drug
therapies have included the use of β-blocker medication (propranolol),
calcium channel blockers medication (nifedipine), guanethidine,
neurontin (anticonvulsant medication), nasal calcitonin, and 6-day
medrol dose packs—all with some limited success. The role of NSAIDs,
although theoretically attractive, has shown limited benefit.
sympathetically mediated or sympathetically independent. In those with
sympathetically mediated pain, stellate ganglion blocks may be
diagnostic as well as curative for the condition. Multiple such
injections may be necessary to realize a benefit and are indicated when
other above-mentioned measures are not effective. Surgical stellate
ganglion ablation is yet another treatment alternative.
10% of all birth defects. The limb bud forms adjacent to the fifth
through seventh cervical somites and can be visualized at day 25
following fertilization. During the ensuing 25 days the limb develops
rapidly with individual digits and web spaces well defined. It is
during this period of embryogenesis that anomalies occur due to either
malformation, deformation, disruption, or dysplasia. Syndactyly
(incompletely separated digits) and polydactyly (extra digits) are
generally considered the most common forms of congenital hand
anomalies. Certain anomalies may be associated with midline congenital
defects such as those affecting the heart, lungs, or kidneys, while
other congenital hand anomalies may appear as isolated events.
Appropriate pediatric and medical genetic workup is recommended in all
patients with upper extremity congenital anomalies. Surgery is often
necessary in these children with a goal of completing all hand
reconstruction by the time hand preference is established, which is
approximately 2 years of age.
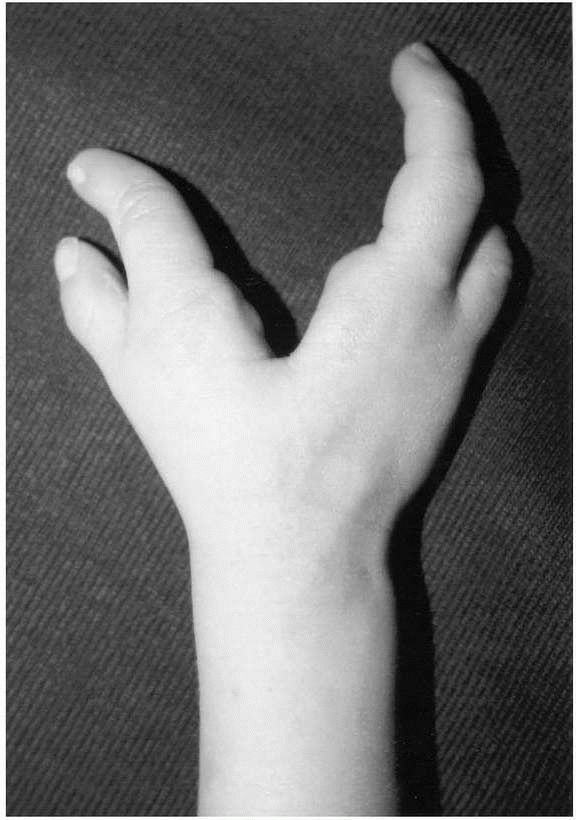
may be classified as type 1—short radius, type 2—hypoplastic radius
(radius growth substantially retarded), type 3—partial absence of the
radius (miniature radius), or type 4—completely absent radius. Type 4
is the most common variant. The condition is frequently associated with
thumb hypoplasia or complete thumb absence. In types 2-4 hypoplastic or
absent radial-sided structures—including the radial artery, flexor
carpi radialis tendon, or the radial wrist extensors—may contribute to
the condition. Radial aplasia often associated with other conditions
such as Holt-Oram syndrome, TAR syndrome (thrombocytopenia absent
radius), VATER (vertebral defects, anal atresia, tracheo-esophageal
atresia, esophageal atresia, and renal defects), and Fanconi’s anemia.
The condition occurs in 1/100,000 live births and is bilateral in 50%
of children affected.
 |
|
FIGURE 14-2. Radial aplasia with absence of entire radius.
|
surgery. More severe radial inclination of the hand is seen in the type
3 and type 4 radial aplasia patients, resulting in a hand that is
poorly functioning and cosmetically objectionable. Contraindication to
surgical correction includes poor general health, severely compromised
overall functional ability, or ipsilateral elbow extension contracture.
In the situation of the elbow extension contracture, the radial club
hand allows the patient to reach the mouth.
correction of the soft tissue contractures by either closed
manipulation and serial casting, or by ring external fixator
application. The second stage consists of centralization of the carpus
on the ulna with pin stabilization and sometimes ulnar osteotomy. At
the same time, radial extensor tendon releases and transfers to the
ulnar side of the wrist is frequently needed. Thumb hypoplasia surgery
is also commonly needed in the patients requiring surgical correction
of the radial club hand. The failure of correction or recurrent
deformity is the most common problem following reconstruction of radial
aplasia.
The hypoplastic thumb may have varying degrees of intrinsic muscle
deficiency, first web space narrowing, ulnar collateral ligament
instability, generalized short bones, or instability of the thumb
carpometacarpal (CMC) joint. In general, those hypoplastic thumbs with
an unstable thumb CMC joint are not reconstructable and require
ablation. Reconstructive procedures for salvageable hypoplastic thumbs
include web space deepening, ulnar collateral ligament reconstruction,
and tendon transfers. For the unreconstructable thumb, the index finger
may be transposed to create a stable, opposable thumb. This procedure
is known as pollicization.
of the ulnar and palmar portions of the distal radial metaphysis
resulting in relative overgrowth and dorsal subluxation of the ulna (Figure 14-4). Patients present some time during
adolescence due to wrist deformity and sometimes due to pain.
Radiographically, a steep ulnar slope with a deficient ulnar margin of
the radius characterizes the condition. The carpus translates volar and
ulnar resulting in the lunate being relatively “uncovered.” If the
condition is identified early in adolescence, a distal radius
physiolysis can restore a relatively normal growth pattern, correcting
the deformity. Traditionally, the treatment for Madelung’s deformity
has commenced at the end of growth and has included a distal radius
joint leveling procedure along with an ulnar shortening procedure.
 |
|
FIGURE 14-3. Unstable, hypoplastic thumb in patient with radial aplasia.
|
 |
|
FIGURE 14-4.
Madelung’s deformity with growth arrest of ulnar and volar aspect of the distal radial physis and relative overgrowth of the ulna. |
“dactylos” (digit). The condition may occur as frequently as 1 in 2,000
live births. The syndactyly may be simple (skin webbing only) or
complex (skin webbing plus bony fusion); and incomplete (digits with
partial separation) or complete (digits with no areas of separation).
The most common digits involved are the long and ring fingers (Figure 14-5).
Surgery is indicated to separate the syndactalized digits. This
procedure involves a complex incision with dorsal and volar limbs that
interdigitate. Skin is invariably deficient and full thickness skin
grafting from the ipsilateral groin is typically needed. Surgery is
performed at or around 18 months of age. The exception in syndactyly is
the patient with syndactyly of the thumb/index or the ring/small. In
these situations, surgery is indicated by 6 months in order to prevent
deformity due to differential bone lengths of these digits.
side of the hand, on the small finger side of the hand or in the center
portion of the hand. Thumb
polydactyly
may occur as several different types with the goal of treatment being
the creation of one stable and cosmetically normal appearing thumb. The
more ulnar of the two thumbs is the more robust digit and elements from
the radial-most thumb are harvested to supplement it. Common
post-reconstruction problems can include MCP joint instability. Small
finger polydactyly is more common in black newborns. In these babies
the duplicate digit may be well developed with a bony skeleton or a
vestigial skin tag. The well-formed digit requires a formal surgical
ablation at a later age. Vestigial polydactylous digits may simply be
tied off in the nursery. Central polydactyly is an extra digit that
affects the index, long, or more commonly, the ring finger. It is often
associated with syndactyly or the cleft hand.
 |
|
FIGURE 14-5. Complete, simple syndactyly of the long and ring fingers.
|
Flatt as “a functional triumph and a social disaster.” This congenital
defect is characterized by a V-shaped cleft in the central portion of
the hand associated with the absence of one or more digital rays (Figure 14-6).
The cause is not known but most likely suppression of the growth of the
central rays occurring at or about the seventh week of fetal
development. Additional anomalies seen with this condition include
polydactyly, syndactyly, and cleft palate. The principles of treatment
include closure of the cleft, reconstruction of any syndactylous
digits, and deepening of the first web space.
 |
|
FIGURE 14-6. Cleft hand.
|
uric acid that leads to the deposition of monosodium urate crystals and
intermittent acute articular swelling, which is termed acute gouty
arthritis. Occasionally the syndrome can also occur due to the
overproduction of uric acid. Gout is approximately 10 times more common
in men than women and has a predilection for middle-aged
males.
The attacks often occur suddenly and are characterized by severe pain,
warmth, and erythema. The consumption of alcohol, trauma, or acute
medical illnesses can cause an attack. Attacks often also occur
following a surgical procedure. Monosodium urate crystals have a lower
solubility quotient at colder temperatures; therefore some have
speculated that this is the cause for the gout commonly affecting the
distal aspects of the extremities. Gout can affect the wrist, MCP, PIP,
and DIP joints. In fact, its sudden onset can lure the unsuspecting
medical student toward acute septic arthritis. The diagnosis of acute
gouty arthritis is made by joint aspiration of negative birefringent,
monosodium urate crystals. The treatment of gout generally does not
require surgery. Colchicine, NSAIDS, or corticosteroid medication is
used in the treatment of acute gout. Chronic tophaceous gout is treated
with allopurinol. Occasionally, gouty tophi require surgical
debridement, particularly from the carpal tunnel following the
development of secondary carpal tunnel syndrome.
pseudogout, occurs due to the deposition of birefringent CPPD crystals
into the joint, activating an inflammatory cascade. In these patients,
sudden swelling, pain, and warmth occur. The wrist and the MCP joints
are the most commonly affected joints of the upper extremity. And like
gout, it can be misdiagnosed as infection. The condition more
frequently occurs in the older age groups, particularly females. In
these patients, chondrocalcinosis is frequently seen on plain
radiographs, particularly in the triangular fibrocartilage of the wrist
(Figure 14-7). Trauma and acute medical
illnesses can trigger attacks. Similar to gout, treatment is primarily
nonsurgical. For the wrist, joint aspiration with injection of 10 mg of
Kenalog is generally successful in minimizing an acute attack. For
other joints in the hand, NSAIDS may be useful.
 |
|
FIGURE 14-7.
PA wrist radiograph showing chondrocalcinosis within the fibrocartilage of the triangular fibrocartilage complex (TFCC) of the wrist. |
wrist is one of the more common afflictions seen in society. Causes
include posttraumatic, post-repetitive stress, or idiopathic, and may
be symmetrical or bilateral. This condition distinguishes itself from
the systemic and symmetrical inflammatory arthropathies. Patients often
complain of localized pain following certain provocative activities.
There may be swelling and pain with passive range of motion, which are
hallmarks of arthritis in general. A history of fracture may be related
but this is not always the case. Scapholunate advanced collapse (SLAC)
wrist is a type of degenerative arthritis of the wrist that primarily
affects the radio-scaphoid articulation and spares the radiolunate
articulation (Figure 14-8). Advanced cases have
midcarpal joint involvement with resulting loss of carpal height and
migration of the capitate proximally between the scaphoid and lunate
articulation. This is easily identifiable on plain wrist radiographs.
Patients may relate a history of wrist ligamentous injury, such as a
scapholunate ligament disruption, or radiographs may reveal an old
scaphoid nonunion. Most of these patients display weak grip and
diminished range of motion. In a study of over 200 wrists with primary
osteoarthritis of the wrist, the SLAC wrist pattern was identified as
the most common pattern. Initial nonoperative measures include activity
restriction, splinting, NSAIDs, and injections. Although many patients
may remain without symptoms for years, some patients require operative
intervention for relief of pain. Temporizing operative treatment
includes wrist debridement and de-innervation procedures where the
radiocarpal articular branches of the anterior and posterior
interosseous are cut in an effort to relieve pain. Salvage procedures
for SLAC wrist include removal of the scaphoid with midcarpal fusion
(scaphoidectomy with four-corner fusion); removal of the scaphoid,
lunate, and triquetrum thus shortening the carpus and allowing the head
of the capitate to articulate in the lunate fossa (proximal
row carpectomy); and complete wrist fusion. The choice of operative treatment is individualized.
 |
|
FIGURE 14-8. Scapholunate advanced collapse of the wrist (SLAC), the most common pattern of primary degenerative arthritis of the wrist.
|
is a form of thumb base arthritis. In these patients articulation
involving the scaphoid, the trapezium, and the trapezoid degenerates.
These patients may localize their discomfort at the base of the thumb
joint or in the wrist in general. This form of degenerative arthritis
is less common than SLAC wrist but is also recognized as either
posttraumatic or idiopathic. Patients will experience difficulties with
pinch tasks in particular. Initial treatment is also nonoperative
similar to the treatment for SLAC wrist. Operative treatment has
classically been the STT fusion. Problems with this operation have
included persistant pain and nonunion of the fusion mass. This outcome
has prompted some authors to recommend the same treatment that will be
discussed for degenerative arthritis of the thumb: removal of the
trapezium and tendon reconstruction of the ligaments of the base of the
thumb.
most common forms of arthritis in the body. Females in the sixth and
seventh decade of life are approximately eight times more likely to
develop the condition than males. Patients complain of pain at the base
of the thumb with most activities of daily living, such as turning keys
or pinching objects between the thumb and index finger. The thumb axis
itself may be misshapen with the first web space narrowed and the thumb
MCP joint hyperextended to aid in grasping objects. Radiographs show
narrowing of the carpometacarpal joint of the thumb (Figure 14-9). Initial nonoperative treatment includes thumb-spica splinting,
NSAIDs, and injections. If patients fail to respond to these
nonoperative measures, surgery may prove helpful. Surgery entails
removal of the arthritic CMC joint by complete trapezium removal and
harvest of the flexor carpi radialis (FCR) tendon. The FCR tendon is
used to recontruct the primary ligamentous stabilizer of the basilar
thumb joint—the anterior oblique retinacular ligament. One long-term
study showed high patient satisfaction at 10 years average follow-up.
Although initial success was reported, long-term failures with the
Silastic trapezial implant has been well recognized, due primarily to
wear debris from the implant and subsequent fracture. The use of the
Silastic trapezial implant is no longer recommended.
 |
|
FIGURE 14-9. Thumb carpometacarpal degenerative arthritis of the wrist (white arrow).
|
lengths occurs between the ulna and the radius such that the ulna is
longer than the radius. The result is that the ulna impales the lunate
or possibly the triquetrum during ulnar deviation of the wrist.
Coincident with ulnar impaction, the triangular fibrocartilage complex
(TFCC) is generally torn or frayed due to the impaction process. The
patients complain of ulnar-sided wrist pain with strong grip, which
results in ulnar deviation of the wrist. Causes of ulnar impaction
syndrome may be posttraumatic or developmental. Initial treatment is
nonoperative and includes long arm splinting and NSAIDs. Failure of
nonoperative treatment may indicate the patient for operative
intervention. The principle of surgical treatment is ulnar shortening.
This joint-leveling procedure requires an osteotomy of the ulna at the
metaphyseal or diaphyseal junction, necessitating internal fixation
with plates and screws. Another less desirable option is distal ulnar
resection, also referred to as Darrach procedure. The Darrach procedure
is more appropriately performed in the elderly, debilitated individual,
as it is not as well tolerated in the young active patient.
abductor pollicis longus (APL) tendons are generally contained within
the most radial condensation of the extensor retinaculum system, the
first dorsal compartment. DeQuervain’s syndrome generally occurs
following certain repetitive wrist movements that cause friction within
the first dorsal compartment. Anatomic variations such as more than two
APL tendons or multiple septations within the first dorsal compartment
may predispose to development of the syndrome. In cadaver studies,
first dorsal compartment septations have been found in approximately
one-third of individuals. In one study, Jackson et al.,
reported 67% incidence in patients undergoing surgical treatment for
DeQuervain’s syndrome. Space occupying lesions such as ganglion cysts
also contribute to narrowing of the first dorsal compartment.
of the compartment resulting in radial-sided wrist pain. Patients will
complain of soreness and tenderness at the base of the thumb
exacerbated by ulnar deviation of the wrist, strong grasp, or thumb
pinch. Inspection will find swelling of the radial side of the wrist in
most cases. Physical examination will find tenderness and often warmth
directly over the first dorsal compartment. In certain advanced cases,
audible squeaking occurs with active thumb movements. The classic test
confirming the diagnosis of DeQuervain’s syndrome is Finklestein’s
test. This test is performed with the thumb slightly flexed and
abducted into the palm and the wrist ulnarly deviated. A positive test
is one where pain is reproduced compared to the contralateral,
unaffected side. Often the test is performed incorrectly with the
patient clasping the thumb into the palm and the wrist ulnarly
deviated. This maneuver, if done vigorously, causes pain in most
anyone. If the reader doubts this, he is encouraged to try the maneuver
on himself.
nonoperative. The patient is fitted with a volar forearm-based,
thumb-spica splint for nighttime use. A small, lower profile,
hand-based splint may be used for daily activities if suited to the
patient’s lifestyle. NSAIDS may also be of value and should be
considered if not contraindicated due to GI intolerance. Additionally,
a corticosteriod injection into the first dorsal compartment may
provide sustained relief. In one study, Weiss et al.
reported that injection was just as effective in DeQuervain’s syndrome
as splinting alone or splinting combined with injection. In another
study of 63 patients, 71% of patients had sustained relief of their
symptoms with one first dorsal compartment injection. Skin
depigmentation and fat atrophy are known complications of
corticosteroid injections of the wrist.
fails, then operative intervention can be considered. Surgical
treatment is release of the first dorsal compartment under local
anesthesia. This is performed through a longitudinal incision directly
overlaying the first dorsal compartment. Branches
of
the superficial radial nerve are particularly vulnerable with this
procedure. Care must be exercised in protecting these branches as
injury to them can cause substantial disability. Other reported
complications of this procedure include volar subluxation of the first
dorsal compartment contents and hypertrophic scar formation. It is for
these reasons most prefer a prolonged trial of nonoperative therapy.
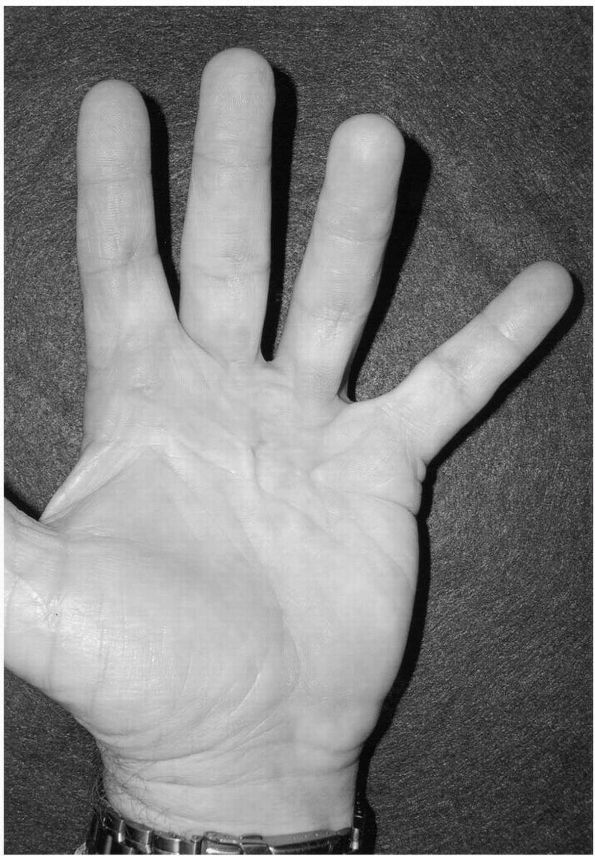
Due to factors that are poorly understood, fibroblasts transform to
myofibroblasts with contractile elements (smooth muscle actin) and
attach to the cells of the palmar aponeurosis. Trauma has also been
mentioned as a possible cause. As the disease progresses, the affected
tissues shorten as a unit, ultimately resulting in digital
contractures. Along with the digital contracture, skin dimpling may
occur. Dupuytren’s diathesis generally implies a more advanced form of
the disease, including “knuckle pads” (thickening over the extensor
surfaces of the PIP joints), plantar fibromas (lederhosen disease), and
fasciitis of the penis (Peyronie’s disease). The disease has a genetic
predisposition, as males of Northern European descent are more commonly
affected. Incidence among affected families has been reported to
approach 70%. Although the genetic predisposition in Dupuytren’s
disease has been well established, the condition is seen more commonly
in patients with seizures, patients who use alcohol and tobacco, and
patients with diabetes. Also, the combination of carpal tunnel
syndrome, trigger finger, and Dupuytren’s contracture has been
appreciated in the diabetic population. The most commonly affected
digit is the ring finger, but any finger can be affected. The prodrome
of Dupuytren’s contracture is inflammation with tenderness in the palm.
Later, contracture ensues on an unpredictable course. The bands of
palmar fascia are termed cords when
affected by Dupuytren’s disease. The most common pattern of cord
development is the pretendinous cord in the palm, which progresses to
cause a MCP joint contracture. The pretendinous cord develops directly
over the flexor tendon system in the palm. Secondarily, a PIP joint
contracture may develop due to the formation of a spiral cord that is
the condensation of several diseased fascial bands in the finger. The
most notable is Grayson’s ligament that is a digital aponeurotic
element attaching to skin volar to the digital nerve and artery. The
spiral cord is so named because it often entraps the digital nerve and
the digital artery along the radial or ulnar borders of the finger.
Following the acute inflammatory prodrome stage of the disease, pain is
usually not encountered as the contracture progresses. At some point,
patients seek medical attention due to the inability to straighten
their hands, making tasks such as shaking hands or donning gloves
difficult. In extreme cases, the contracture can become so severe that
palmar maceration develops, posing a hygiene problem.
 |
|
FIGURE 14-10. Dupuytren’s disease involving the ring finger.
|
disease that came to bear his name, although the nature of this disease
had been described years earlier by Felix Plater, Henry Cline, and Sir
Ashley Cooper. For many years a variety of nonoperative treatments have
been tried, all without success but, as Dupuytren first described,
surgery is the preferred treatment for this condition. Although simple
transection of the pretendinous cords is a viable option in the elderly
or the debilitated patient, the
surgery
for symptomatic Dupuytren’s contracture has evolved into a formal
fasciectomy of the involved palmar tissue. The indications for surgery
are debilitating contracture of the MCP joints or any contracture of
the PIP joint. Contractures of the MCP joints are easily corrected
under most circumstances. In contrast, contractures of the PIP joints
are often incompletely corrected and are fraught with recurrence.
standard zigzag Bruner incisions, unless the deformity is severe. With
severe contracture, the fundamental problem becomes one of skin
coverage after the fascia is removed and the contracture corrected. In
severe cases of Dupuytren’s contracture, a longitudinal incision with
multiple opposing Z-plasties can be utilized to expand the coverage
potential of the existing skin. Alternatively, McCash described a
technique whereby fasciectomy skin incisions can be made in the
transverse skin creases of the palm and the digits, without closure.
The wounds then heal by secondary intention so motion is not inhibited
following complex wound coverage procedures. Another alternative is
performing the standard Bruner incision and leaving portions of that
wound open following fasciectomy, either in the palm or in the digit.
Yet another option is dermofasciectomy where diseased fascial elements
are excised along with overlying skin and the resulting defect skin
grafted. Whatever the surgical technique employed, the dissection of
the palmar fascial can be tedious, particularly in advanced or
recurrent cases. Extreme care must be exercised in dissecting the
diseased fascial cords from the digital nerves and arteries because
nerve injury or even nerve division can result.
hand surgeon is maintaining the improvements in MCP and PIP motion
following fasciectomy. Maintaining motion improvements requires close
postoperative supervision by a hand therapist. Within the first 3 to 5
days the dressing is changed, and the patient is placed in an extension
splint. Care is taken to not cause ischemia of the palmar skin flaps.
It is important to also start active flexion exercises of the MCP and
PIP joints. The patient’s progress must be closely monitored and the
exercise protocol modified as necessary to achieve the optimal balance
between achieving digital extension and maintaining composite finger
flexion.
palmar fasciectomy, although complete corrections of PIP joint
contractures are rarely achieved. Recurrence of Dupuytren’s contracture
following fasciectomy has been well recognized with the incidence
approaching 50% in some series. Complications of fasciectomy surgery
for Dupuytren’s contracture include digital nerve neuropraxia and
digital sensory compromise, digital nerve division, digital ischemia,
wound healing problems, and complex regional pain syndrome type 1 or
type 2. Surgery for recurrent disease can be challenging even for the
most experienced surgeons, with complications such as amputation having
been reported.
infections of the hand. These infections are localized in the digit.
The felon is an abscess of the pulp on the pad of the fingertip. Due to
the multiple septa present within the pad of the finger, an infection
in this region can gain substantial pressure and become quite painful.
The most commonly encountered organism is Staphylococcus aureus.
The infection occurs secondary to direct inoculation, such as might
occur following the introduction of a foreign body. Like the treatment
of any other abscess, incision and drainage is the most effective
treatment. The surgical decompression is best done through straight
lateral incisions. Incisions directly over the finger pad are often
painful and should be avoided. When the pulp is decompressed, care
should be taken to break up all the septae within the pulp of the
fingertip to assure that no loculation is missed. The treatment is
originally supplemented with oral S. aureus
coverage, and antibiotics should be changed if cultures show a
different infection organism. Generally antibiotics are continued for 7
to 10 days. In severe infections with ascending lymphangitis, IV
antibiotics may be necessary.
about the nail fold (eponychium). Bacteria colonize underneath the nail
fold and adhere to the nailplate. The most common organism is S. aureus.
Causes of the paronychial infection include direct trauma, nail biting,
artificial nails, and manicures. Patients with diabetes mellitus are
more susceptible to developing these infections. Most paronychial
infections respond to warm soaks and oral S. aureus
coverage. Surgical drainage about the eponychial fold is indicated if
an abscess is identified. Chronic or recurrent infections typically
require removal of the nailplate because bacteria or fugal elements
notoriously adhere to the nailplate beneath the nail fold. Candida
albicans is one of the more common causes of recurrent of chronic
paronychial infections. In patients not responsive to incision and
drainage, nail removal, and culture-specific antibiotic therapy,
eponychial marsupialization (wide debridement) leaving the wound open
may be necessary.
often devastating, leaving scar within the flexor tendon sheath and
leading to substantial digital dysfunction. Septic flexor tenosynovitis
often occurs secondary to a puncture wound or a deep digital cut that
never receives proper attention. The diagnosis is made on clinical
grounds. Patients typically present with one or more Kanaval signs:
tenderness along the flexor tendon sheath, flexed digital posture,
fusiform swelling of the digit, and pain with passive stretching of the
digit. There is generally a history of trauma, particularly a puncture
wound. Treatment must be initiated early if scarring of the flexor
tendon sheath and ultimate disability is to be avoided. Infrequently,
symptoms may be identified within 24 hours of onset; these patients
will occasionally respond promptly to IV antibiotic therapy. Patients,
however, must be carefully observed for recurrence. Those patients not
promptly responding to IV antibiotics or those patients who have had
symptoms longer than 24 hours are indicated for emergent surgical
drainage. Surgical treatment consists of closed flexor tendon sheath
irrigation using a small catheter inserted in the palm at the A1 pulley
and the sheath drained at the level of the A5 pulley through an
midaxial incision along the lateral aspect of the finger. No clear
advantage has been shown with open tendon sheath irrigation or from
postoperative tendon sheath irrigation accomplished by leaving the
catheter in place.
abscess formation. The deep spaces of the hand are actually “potential
spaces” and consist of the thenar space (located deep to the flexor
pollicis longus tendon), hypothenar space (containing the hypothenar
muscles), the adductor space (located posterior to the adductor
pollicis muscle), and the midpalmar space (located deep to the flexor
tendons). Palmar abscesses are the result of a deep puncture wound.
Patients often present 2 to 3 days after the event, complaining of
pain, warmth, tenderness, and redness. Surgical drainage is indicated
followed by culture-specific antibiotics. These infections can endanger
the entire upper extremity and, especially in the immunocompromised
host, are surgical emergencies.
bacterial infections and ultimate complications are less severe than
the bacterial infections from human bites. From dog and cat bites, the
most common organisms are streptococcus. Pasturella multocida
is also a common infecting organism. Due to the sharp nature of the cat
tooth, cat bites tend to become infected more often than dog bites. The
initial treatment for any animal bite is prophylactic with cleansing of
the wound and broad spectrum oral antibiotic coverage. Any bite
developing a local abscess with or without ascending lymphangitis is
indicated for emergent surgical debridement. Patients with ascending
lymphangitis following a cat or dog bite should be admitted to the
hospital for IV antibiotic therapy and close observation.
for infection, are colonized by more virulent organisms, and have a
greater number of potential pathogens than animal bite wounds. The most
common bacteria are streptococcus and staphylococcus. Eikenella is
another common human oral flora that is notorious for causing infection
following a clinched fist injury that strikes an opponent’s tooth.
Uncomplicated human bite wounds, which do not involve a joint, tendon,
or nerve, may be treated with local wound care. Alternatively, a
penetrating bite wound, such as occurs following a clinched fist
injury, demands surgical exploration and debridement to inspect for
extensor tendon injury, metacarpal phalangeal joint capsule
penetration, and articular surface abrasions or defects. The wound is
left open. Obvious infections seen following human bite injuries
require surgical debridement and culture-specific antibiotics. While
cultures are maturing following initial debridement, broad empiric
antibiotic coverage should
begin, covering staph, strep, and anaerobic bacteria. Eikenella infections are usually sensitive to penicillin G.
osteomyelitis of the hand is rare, representing less than 5% of all
cases of infection in the hand. Of the bones of the hand and wrist, the
distal phalanx is the most commonly affected. The origin of
osteomyelitis of the hand is often related to trauma with open
fractures of the hand the most common situation. Penetrating wounds
such as bites or puncture wounds are other common vehicles. But
osteomyelitis can also be seen following elective hand surgery.
Patients with diabetes or who are immunocompromised are the most
susceptible to developing osteomyelitis. The most common infecting
organism is S. aureus. Methicillin-resistant S. aureus
is seen with increasing frequency. Clinical signs include pain,
swelling, and often an open draining wound. Radiographic signs include
a lucency with a sclerotic rim (Figure 14-11).
Extensive surgical debridement and sustained use with culture-specific
antibiotic therapy under the direction of an infectious disease
specialist is the necessary treatment of this condition.
bacilli. Infections from the atypical mycobacterial organisms are often
slow growing and underappreciated. The most widely recognized among
these bacteria is the Mycobacterium marinum
species. These bacteria are most commonly harbored on fresh or
particularly saltwater environments. Infection usually requires some
penetrating injury from aquatic equipment or marine organisms.
Clinically the patients present with or are sent in referral due to
painless cutaneous lesions. Draining skin lesions may also be present.
The slow-growing nature of these bacteria makes their culturing
difficult. Therefore, the bacteria should be cultured on
Lowenstein-Jensen plates incubated at a cooler temperature (31°C). A
culture time of 6 weeks is sometimes necessary to demonstrate growth.
An exception to this is the Mycobacterium fortuitum
species that is a more rapid growing variety that typically can be
isolated within 1 week of culture. Surgical debridement is necessary
for the subdermal infections. Complete surgical debridement is rarely
accomplished as the infection can be very infiltrating. Combination
therapy is the preferred antibiotic treatment. Empiric drug therapy
must be started following biopsy and culture because the time needed to
grow the organism is long. Antibiotic therapy may include a combination
of minocycline, clarithromycin, rifampin, ethambutol, or
trimethoprim-sulfamethoxazole. Alternatively, single drug therapy may
be used. Duration of antibiotic therapy can last 1 year. Recurrence is
common.
 |
|
FIGURE 14-11. Osteomyelitis of the ulna following a pintract infection (lytic lesion depicted by white arrow).
|
life-threatening infection involving the fascia and subcutaneous
tissues. As the name implies, the affected fascia and fat becomes
necrotic. Consequently, the nutrient blood supply to the skin is
compromised, and skin blistering and sloughing can also occur. The most
common causative organism is β-hemolytic streptococcus. Patients may
present with a localized
area of erythema or an abscess that rapidly progresses as the infection dissects along superficial and deep fascial planes (Figure 14-12).
The situation can occur following relatively innocuous wounds or trauma
in otherwise healthy individuals. However, the infection is more common
among those patients with immunocompromising conditions such as
diabetes, IV drug abuse, and inflammatory arthritic disorders. Severe
pain and edema may ensue and gas may be present on plain film
radiography. Patients may become critically ill, requiring
resuscitative measures due to septic shock, respiratory distress, and
multisystem organ failure. Nearly one-third of all patients who develop
necrotizing fasciitis die. The mortality rate may approach 75% where
the infection spreads to the chest wall.
debridement and early multimodal antibiotic therapy. Specifically,
clindamycin may be considered for strep and staph species, penicillin
for anaerobic bacteria, and gentamycin to cover Gram-negative bacteria.
Multiple debridements are frequently needed to remove all necrotic
tissue. Above elbow amputation, shoulder disarticulation, or
four-quarter amputation is often necessary to control the infection and
prevent death.
a toxin-producing, Gram-positive bacteria. As the name implies, toxins
cause necrosis of muscle as well as subcutaneous tissue and fat. The
infection then “snow balls” as local nutrient vessels are destroyed and
relative local tissue hypoxia occurs. Culture of the clostridia species
is difficult and requires sodium glycolate agar and an anaerobic
environment. Predisposing factors for development of clostridial
myonecrosis include crush injuries with open fractures and devitalized
muscle, foreign contamination, immunosuppression, and hypovolemic
shock. Patients develop massive edema and skin discoloration. Plain
radiographs show gas formation within the soft tissue shadow of the
muscle. Septic shock often ensues. In patients suspected of clostridial
myonecrosis, aggressive surgical debridement is necessary with
particular attention to the removal of any devitalized muscle. If
Gram’s stain shows Gram-positive rods, high dose penicillin therapy is
started. Amputation is performed for life threatening situations.
Several authors have reported success with the use of hyperbaric oxygen
(HBO) treatment in patients with clostridial myonecrosis. Randomized,
controlled studies, however, are lacking. With aggressive surgical
debridement, antibiotic therapy, and HBO, mortality in the range of 20%
can be expected. Fortunately, the incidence of clostridial myonecrosis
is rare.
 |
|
FIGURE 14-12.
The rapid progression of necrotizing fasciitis of the arm (black arrows) following the development of a septic olecranon bursa in an immunocompromised patient. |
most common inciting event is penetrating trauma, however, hematogenous
spread may also be the cause, especially in the immunocompromised host.
Like most other infections of the hand and wrist, predisposing factors
include diabetes, alcoholism, IV drug abuse, chronic renal failure,
advanced age, enteral corticosteroid usage, and inflammatory arthritis.
When the bacterial count within a synovial joint exceeds 100,000/cm3
a clinical infection will develop. Once infection develops, bacterial
toxins and proteolytic enzymes are released that destroy cartilage. As
the articular proteolytic enzymes are broken down the host mounts an
inflammatory response, which consists of polymorphonuclear lymphocytes,
lymphocytes, and macrophages. The end result of this process is the
production of pus. As pus collects, pressure increases causing further
articular damage due to inhibition of slowed articular blood flow and
ultimate articular oxygen exchange. Ultimately joint ankylosis and
contiguous osteomyelitis result if the condition is left untreated. Staphylococcus aureus
is the most common cause of septic arthritis of the joints of the hand
and wrist. Physical examination reveals warmth, swelling, and joint
tenderness. The patient may complain of pain and a recent febrile
illness. Laboratory examination reveals an elevated white blood cell
(WBC) count in only half of the cases. The sedimentation rate and the
C-reactive protein levels, however, are consistently elevated.
Diagnosis is confirmed by joint aspiration with a WBC above 50,000/mm3. Additionally, cloudy synovial fluid aspirate also suggests the diagnosis of a septic arthritis.
should be initiated immediately after cultures are obtained. The
differential diagnosis of the acutely swollen wrist should include
CPPD. CPPD of the wrist is often misdiagnosed as a septic wrist.
Patients with CPPD of the wrist will likewise have a painful, swollen,
and warm wrist joint. These patients will often have notable
calcifications within the triangular fibrocartilage complex and a
normal WBC count. Joint aspiration will demonstrate positive
birefringent crystal and a WBC well less than the 50,000/mm3
expected for a septic wrist. Patients with an acute attack of CPPD of
the wrist will respond quite promptly to immobilization and NSAIDs.
mechanism that still is not entirely understood, the blood flow to the
lunate bone of the wrist is compromised to such an extent that
osteonecrosis ensues and collapse and fragmentation of the bone occurs
over time. The end result can be degenerative arthritis of the
radiocarpal joint and pain. Various predisposing factors exist.
Approximately 75% of wrists with Keinbock’s disease have a shorter ulna
compared to the radius, as measured at the wrist (ulnar negative
variance). Also, the slope of the distal radius articular surface has
been shown to be more horizontal in patients with Keinbock’s disease.
Approximately one-fourth of lunate are thought to have a single vessel
blood supply. Some believe that osteonecrosis of the lunate occurs
subsequent to a single fracture although others have suggested
repetitive microfracture of the bone. In reality, cause of Keinbock’s
is most likely multifactorial.
Approximately 50% of patients relate a history of trauma. Most complain
of dorsal wrist pain and stiffness. Physical examination may reveal
diminished range of motion, grip weakness, and tenderness over the
radiocarpal joint. Some patients present with symptoms of carpal tunnel
syndrome. Keinbock’s can be staged radiographically into one of six
categories. Stage 0: normal plain radiographs of the wrist with
abnormal MRI scan of the lunate. Stage 1: fracture of the lunate
without collapse of the bone. Stage 2: sclerosis of the lunate without
collapse of the bone. Stage 3a: lunate collapse without loss of height
of the wrist (Figure 14-13). Stage 3b: Collapse of the wrist. Stage 4: degenerative changes of the wrist joint secondary to Keinbock’sdisease.
entirely known. In patients with stage 0 and stage 1 disease,
immobilization and nonoperative support may suffice. Patients with
stage 2 and stage 3a disease
who
continue with symptoms are generally indicated for surgery. The
surgical procedures for patients with stage 2 and stage 3a Keinbock’s
disease can be divided into two broad categories: joint-leveling
procedures and revascularization procedures. The most commonly
performed among these procedures is the radial shortening osteotomy.
This procedure is indicated in patients who have a short ulna and the
goal of surgery is to shorten the radius to “level” it with the ulna.
The exact reason why this procedure is effective is still unknown. The
most commonly performed revascularization procedures for Keinbock’s
disease is a pedicled vascularized bone graft harvested from the
dorsal, distal radius. For patients with symptomatic stage 4 disease
and some patients with stage 3b disease, reconstructive salvage surgery
of the wrist is indicated. This salvage surgery may include a partial
(maintains some element of wrist range of motion), or a complete wrist
fusion or a proximal row carpectomy (removal of the lunate bone along
with the scaphoid and triquetral bone). Proximal row carpectomy allows
the capitate to articulate in the lunate fossa. A prerequisite for this
operation is maintenance of a good distal radius articular surface.
 |
|
FIGURE 14-13. Stage 3a, osteonecrosis of the lunate (Keinbock’s disease).
|
and wrist as median, ulnar, or radial nerve palsies. The vast majority
of radial nerve palsy is posttraumatic, but can also occur as a
complication of elective surgery of the upper extremity, a residual of
birth palsy, or the consequence of cervical spine disc disease. Tendon
transfers provide an option to restore lost motor function. The ideal
tendon transfer is one in which the tendon’s muscle has normal
strength, has a straight line of pull, and provides adequate excursion.
Additionally, the tendon should originally have a function synergistic
or “opposite” to the tendon function for which it is substituted.
Naturally, the tendon to be transferred must be expendable.
results in a high median nerve palsy. The consequences of a high median
nerve palsy is loss of palmar sensation along the volar aspect of the
thumb, index, long, and radial border of the ring finger. Motor
strength deficits include loss of thumb opposition (loss of abductor
pollicis brevis), loss of thumb interphalangeal (IP) joint flexion
(loss of flexor pollicis longus muscle function), and loss of index
distal interphalangeal joint flexion (flexor digitorum profundus
function). Restoration of thumb IP joint flexion can be restored using
a transferred brachioradialis muscle (radial nerve innervated) to the
FPL tendon. Restoration of FDP function of the index finger can be
accomplished using the extensor carpi radialis longus (radial nerve
innervated) tendon rerouted to the index FDP tendon in the mid forearm.
Lastly, thumb opposition can be restored with transfer of the abductor
digiti minimi muscle (ulnar nerve innervated).
function of the hand because extension posturing of the wrist (the
prehensile position) is lost. This positioning of the hand increases
grip power as well as the all-important hand function of grasp and
release. The radial nerve is particularly vulnerable as it spirals
around the humerus midshaft, against which it is closely applied. The
radial nerve palsy is most often caused by injuries following a spiral
fracture of the humerus. The sharp bony ends of the fracture can impale
the radial nerve along its course. Loss of radial nerve function at
this level results in loss of wrist and finger extension. This is known
as “wrist drop.” Tendon transfers for radial nerve palsy include flexor
carpi radialis (FCR) transfer to extensor digitorum communus (EDC)
tendons, pronator teres to extensor carpi radialis brevis tendon, and
palmaris longus to the rerouted extensor pollicis longus (EPL) tendon.
These transfers are then subsequently fired by flexion of the wrist
causing tension on the transferred tendons (tenodesis) of the wrist.
hand is the ulnar nerve palsy. The ulnar nerve supplies sensation to
the volar aspect of the small finger as well as the small finger side
of the ring finger. Motor function deficits following ulnar nerve palsy
include loss of hand muscle function (intrinsic muscle function), which
includes digital side-to-side movements as well as “thumb pinch”
function. This results in substantial impairment in hand strength and
digital mobility. Ulnar nerve injuries higher (more proximal) in the
arm result in the loss of DIP joint flexion. Profound hand wasting
accompanies ulnar nerve dysfunction.
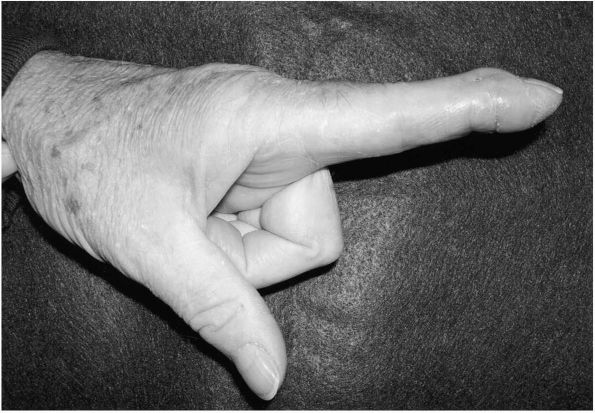
The classic “clawhand” of ulnar nerve palsy is known as Duchenne’s
sign. Wartenberg’s sign is the inability to pull in (adduct) the small
finger against the ring finger. Froment’s sign is the hyperflexion of
the thumb IP joint to substitute for the lack of thumb-pinch power
against the index finger. Weakness of DIP joint flexion due to loss of
FDP
function
of the ring and small finger is known as Pollock’s sign. The flattening
of the natural metacarpal arch of the hand seen in association with
hand muscle wasting is known as Masse’s sign.
their ability to restore hand strength. The ECRB tendon can be
transferred to the thumb proximal phalanx to provide thumb pinch
(adduction) while the extensor pollicis brevis (EPB) tendon is
transferred to the index interosseous muscle. Additionally, the thumb
MCP joint may be fused to prevent thumb hyperextension and instability.
The combination of these surgeries has been reported to restore
approximately 50% of the lost pinch strength.
population with females affected twice as often as males. It is a
systemic condition that causes a symmetrical polyarthritis. In the hand
and the wrist joint, the distal radioulnar joint and the
metacarpophalangeal joints are commonly affected. Patients usually
present between ages 40 and 60 with joint pain and stiffness and
occasionally fever. In the hand, synovial swelling is first seen
followed by ligamentous failure, joint subluxation, and ultimately
joint erosions and destruction. Initial treatment of rheumatoid
arthritis in the hand includes medical therapy and resting night
splints. Early on, medical therapy may consist of NSAIDs and rest
splints but potential remittive therapy is usually necessary.
Aggressive medical management often includes low dose oral
corticosteroids and immunosuppressive agents such as methotrexate,
Imuran (azathioprine), or Arava (leflunomide). Newer biological agents
include Enbrel (etanercept), Humira (adalimumab), and Remicade
(infliximab), which act by inhibiting tumor necrosis factor. These
biologic response modifiers may be combined with more traditional
agents such as methotrexate. Whether or not these treatments will make
surgery less necessary has been suggested but not yet established.
medical management, then surgical synovectomy is indicated to prevent
extensor tendon rupture. Similarly, synovitis of the wrist joint or the
metacarpophalangeal joints may not respond to medical management and
surgical synovectomy may be indicated. The indications for MCP and
wrist joint synovectomy are less clear but in the absence of joint
destruction, most agree that joint surgery can be delayed. MCP joint
synovectomy should be considered in those patients with recalcitrant
synovitis who have no radiographic evidence of joint destruction.
joint affected in patients with rheumatoid arthritis. DRUJ subluxation
is often observed and as the distal ulna becomes eroded, rupture of the
overlying extensor digiti quinti minimi (EDQM) tendon can occur. The
result is the Vaughan-Jackson sign, which is a prominent distal ulna
with the inability to extend the small finger. In these patients,
extensor tenosynovectomy is indicated with EDQM reconstruction. A
side-to-side tendon repair to the adjacent EDC to ring finger can
accomplish EDQM reconstruction. In these patients it is also incumbent
to stabilize the distal radioulnar joint. This is most commonly done
with a distal radioulnar joint fusion with the creation of a more
proximal pseudoarthrosis (Suave-Kapandji procedure). As disease
progresses, the remainder of the wrist joint becomes involved, further
destruction of the wrist may occur, and wrist arthrodesis may be
necessary. Wrist arthrodesis is a reliable procedure well suited for
providing pain relief. Alternatively, a total wrist replacement can be
considered in low demand individuals with bilateral disease. Total
wrist arthroplasty is contraindicated in patients with previous
infection. The failure rate with total wrist replacement approaches 25%
at intermediate-term follow-up in one recent series. The most common
mode of failure is distal component loosening.
MCP joint destruction with subluxation of the joint and drift of the
digits toward the small finger side of the hand (ulnar drift).
Tightness of the surrounding soft tissue structures ultimately prevents
correction of this deformity (intrinsic muscle tightness). Wrist
involvement may also occur with sliding of the carpal bones toward the
ulna (ulnar translation of the carpus) as ligamentous destruction
occurs (Figure 14-14). These patients also
commonly have pain and have noticed a recent decline in overall hand
performance. These patients are reasonable candidates for MCP joint
arthroplasties. The Swanson flexible silicone implant that has been in
service for well over 35 years functions as a spacer following
resection of the destroyed MCP joint. It has been well recognized that
these implants typically fracture but remain in service for
years, continuing to function as a spacer. Hansraj et al.
has reported a 90% 10-year survival rate with this spacer. The
biomechanical shortfall of the Swanson Silastic implant is the amount
of bone and soft tissue resection needed for implantation of the
device. Current alternatives to the Silastic implants are surface
replacement arthroplasties that attempt to recreate the normal
articular surface anatomy while requiring less soft tissue resection
for implantation of the device. Further follow-up data on these newer
generation devices are needed.
 |
|
FIGURE 14-14. Ulnar deviation deformity of the wrist and digits in a patient with advanced rheumatoid arthritis.
|
problem of a mismatch in size of the flexor tendons within their flexor
tendon sheath. The result is a bunching or catching of the tendons as
they pass through the orifice of the A1 pulley. This mismatch in size
results in the mechanical problem of triggering that is the clinical
hallmark of the condition. A fibrocartilagenous dysplasia develops at
the A1 pulley, leading to a similar lesion on the corresponding surface
of the flexor tendon. This results in degenerative tendinopathy over
time. The process can occur at any digit but more commonly affects the
ring finger. Patients usually present with a complaint of a painful
catching of the finger with gripping. In more advanced cases, the
finger may be locked in flexion and very painful to reduce. The
patients may complain of the occurrence more in the morning hours than
later in the day. Prior to experiencing the triggering or catching
symptoms, patients may just have a tender and sore flexor tendon sheath
that is aggravated by activities. On physical examination, actual
triggering may not be elicited but tenderness directly over the A1
pulley usually is. The condition is more frequently seen in patients
with rheumatoid arthritis, gout, diabetes, and degenerative arthritis.
Patients usually present in the fifth to seventh decade of life.
the use of NSAIDs has been shown to be effective in some patients.
Injection of corticosteroid into the flexor tendon sheath has been
shown to be effective in 70% of patients. Another study has shown the
percentage to increase to 84% when a regimen of two injections is used.
Alternatively, reports of splint therapy alone have yielded improvement
in 66% of patients. The trigger finger injection is performed using a
25-gauge needle and 1 cc of lidocaine and 10 mg of Kenalog solution or
an equivalent of another water insoluble steroid preparation. Water
insoluble steroid preparations are longer acting. The lidocaine steroid
preparation is injected into the flexor tendon sheath at the level of
the A2 pulley, and the examiner palpates the filling of the sheath.
Flexor tendon sheath release or trigger finger release is indicated
when nonoperative management fails. This is done at the opening of the
flexor tendon sheath, or at the level of the A1 pulley. Results
approaching 100% in appropriately indicated patients were recently
reported by Turowski et al. An alternative to
open trigger finger release is percutaneous flexor tendon sheath
release. This technique employs a 20-gauge needle placed percutaneously
at the level of the A1 pulley. The needle is manipulated such that the
A1 pulley is cut by the bevel of the needle. Complications of this
technique include scoring of the tendon.
swan-neck deformity may cause substantial functional limitation. It can
arise following trauma but more typically is seen in the context of the
rheumatoid hand. The essential features of the digital swan-neck
deformity include hyperextension of the PIP joint and flexion of the
DIP joint subsequent to incompetence of the PIP joint volar plate (Figure 14-15).
The swan-neck deformity is often accompanied by the presence of
intrinsic tightness. In this condition the interosseous muscles of the
hand become contracted, which causes tightness of the lateral band
portion of the extensor mechanism. With the metacarpal phalangeal (MCP)
joint extended, the lateral band portion of the extensor mechanism is
placed on stretch, causing tightness of the terminal tendon. This
imbalance then causes restriction in the passive or active flexion of
the PIP joint. A simple test for intrinsic tightness involves
hyperextending the PIP joint and then examining the passive range of
motion (ROM) of the PIP joint. Patients with intrinsic tightness of a
digit experience diminished passive range of motion at the PIP joint
when the test is performed.
four stages. Stage 1 is a finger with a swan-neck deformity and no
limitation of PIP joint ROM. Stage 2 is a swan-neck digit with
limitation of ROM with certain positions of the MCP joint. Stage 3 is a
digit with limitations of PIP ROM in any MCP position. Stage 4 is fixed
and rigid swan-neck deformity. The stage 4 swan-neck deformity in the
rheumatoid is characterized by advance PIP joint destruction.
 |
|
FIGURE 14-15. Swan-neck deformity of the index finger following trauma.
|
for the stage 1 deformity, and extensor mechanism reconstruction or
release of tight intrinsic muscles for the stage 2 and 3 deformities.
Arthrodesis or arthroplasty is required for the stage 4 condition. In
general, results for soft tissue reconstruction of the rheumatoid
swan-neck deformity has been disappointing while treatment with
arthrodesis has been more predictable.
is the ganglion cyst. The most common location is the dorsal aspect of
the wrist (originating from the scapholunate interosseous ligament. One
study found MRI-associated pathology in 30% of wrist ganglia imaged,
suggesting a traumatic origin for this lesion. The pathogenesis of
ganglions remains unclear. Recent series have documented enhanced
success rates using serial aspiration treatments. However, recurrence
rates with aspiration exceed 40%. Definitive management is open
surgical excision. Recurrence rates with surgical removal are as low as
5%. Arthroscopic ganglion removal is gaining increasing popularity for
dorsal wrist ganglions. When treating ganglion cysts it is important to
consider the patients perspective. In one study, 28% of patients sought
medical attention for their ganglion over concern of malignancy.
and even metastasize causing death, but are regarded as benign.
Eighty-five percent of giant cell tumors are diagnosed in patients
older than 20 years in age, occurring slightly more often in females.
Only 2% of giant cell tumors arise in the hand bones while
approximately 14% originate in wrist. The patient with a giant cell
tumor of the hand or wrist presents with pain and localized swelling.
The tumor is lytic radiographically with cortical expansion and
indistinct borders. Mitotic activity is quite common.
should be treated with wide excision and reconstruction. A recurrence
rate of 79% has been reported with curettage within the margins of the
lesion (intralesional). Curettage beyond the limits of the lesion is
permissible when the giant cell tumor has not violated the cortex of
the bone and extended into the soft tissue. No recurrences were
reported in 10 patients treated with wide excision and arthrodesis of
the wrist. Other than arthrodesis, other reconstructive surgeries about
the wrist that can be considered are vascularized or nonvascularized
bone grafting and composite osteoarticular allograft reconstruction of
the distal radius joint surface. Cementation and cryosurgery can also
be considered in place of bone grafting when curettage is chosen as a
primary treatment.
 |
|
FIGURE 14-16. Giant cell tumor of bone.
|
common soft tissue tumors of the hand. It is a slowly progressive,
painless, rubbery mass predominating on the radial three digits of the
hand and is typically identified adherent to the digital flexor tendon
sheath of the hand. The histology is variable but the tumors
consistently contain multinucleated giant cells and xanthoma cells.
Some lesions possess increased cellularity and mitotic activity.
Recurrence rates as high as 44 to 50% have been reported in series with
extended follow-up. A recent study of 43 patients found that following
surgical excision, the only lesions that recurred were those that
originally had multiple discrete tumors. Tumors composed of single
masses did not recur following surgical excision. MRI may be helpful in
determining the anatomic extent of the lesion.
soft tissue lesions of the hand. This tumor-like condition results from
the puncture of epithelium beneath the skin. The resulting growth of
epithelial cells is typically painless and seldom functionally
limiting. The fingertip is the most common location for epidermal
inclusion cysts. Marginal surgical excision is curative and indicated
when the lesion is bothersome to the patient. Involvement of the distal
phalanx has been mistaken for malignancy.
and wrist. It is seen in all age groups and has an equal male and
female distribution. These benign tumors may present due to a
pathologic fracture or may be observed incidentally on routine hand
radiographs. Analysis of over 5,500 bone tumors from Bauer et al.,
found that nearly 90% of
all
primary hand tumors were enchondromas. The most common location of the
enchondroma is the proximal phalanx, followed by the metacarpal and the
middle phalanx.
distortion of the cortex and punctate calcification. Multiple
enchondromas in the same extremity is known as the nonhereditary
condition, Ollier’s disease. In Ollier’s disease the enchondromas are
larger, causing notable cosmetic and functional problems. Growth of
enchondromas usually stops after skeletal maturity. Enchondroma growth
after skeletal maturity, particularly when associated with radiographic
progression and pain, raises the question of malignancy. Malignant
transformation of enchondromas to chondrosarcoma in Ollier’s disease is
much more likely than solitary enchondroma transformation and is
considered to be approximately 30%. Maffucci’s syndrome is an extremely
rare nonhereditary condition composed of multiple enchondromas and
associated hemangiomatas.
treatment. If lesions grow and become painful, biopsy should be
obtained. Pathologic fractures (fractures through tumor) occurring
through enchondromas are treated as fractures first. Once fracture
healing has occurred, formal treatment of the enchondroma is initiated.
Enchondromas that reach substantial size are excised to prevent
pathologic fracture. Enchondroma removal involves thorough curettage
(intralesional scrapping of the tumor) followed by packing of the
defect with bone graft. The recurrence rate with this method is
approximately 4.5%.
The most common primary malignant bone tumor of the hand and wrist is
the chondrosarcoma. The chondrosarcoma often develops in relationship
to a preexisting enchondroma, particularly enchondromas associated with
Ollier’s disease. Osteosarcoma is seen less frequently in the hand by
comparison to the lower extremities and is typically seen in an older
population than the classic young adult presentation. Radiation
exposure has been suggested as a possible cause for osteosarcoma
development in the hand. Metastatic tumors to the hand may present as
the original presentation of a previously undiagnosed cancer. The most
common metastatic tumor to the hand is lung and the most common site is
the distal phalanx. Other reported primary sites include the esophagus,
colon, breast, ovary, prostate, bladder, uterus, and thyroid. In one
study, there was only a 6-month average life expectancy of patients
with tumors metastatic to the hand. The most common soft tissue
sarcomas of the hand and upper extremity is the epithelioid sarcoma,
the malignant fibrous histiocytoma (MFH), and the synovial cell
sarcoma. The epithelioid sarcoma is often misdiagnosed at original
presentation leading to delays in treatment. Synovial cell sarcoma
presents associated with the synovial joints of the wrist. They are
slow growing and may go undiagnosed for years. MFH is becoming
increasingly more recognized in the hand, particularly in older adults.
It is often painless, also leading to original misdiagnosis and
treatment delays. Treatment for bone and soft tissue sarcomas are wide
tumor resection and limb salvage reconstruction. Adjuvant chemotherapy
and external beam radiation may prolong survival, depending on the
histologic diagnosis and grade of the tumor.
as result of penetrating trauma, repetitive trauma, primary vasospastic
disease (Raynaud’s disease), or vasospastic disease secondary to
another disorder (Raynaud’s phenomena). Whatever the cause, patients
complain of color changes of the digits anywhere from pale white to
bluish purple. They often experience pain and particularly cold
intolerance. In some advanced conditions, fingertip soft tissue
necrosis may result. Important information to be gained from the
patient is any history of smoking, penetrating or blunt trauma,
repetitive trauma, or excessive occupational vibration exposure. Also,
the examiner should query the patient for a history of malignancy,
blood dyscrasias, or any other hypercoagulable condition. Physical
examination should include an Allen’s test, which assesses the patency
of both the radial and ulnar arteries. In this test, the examiner
occludes both arteries at the wrist and then has the patient
repetitively make a fist in an effort to remove blood from the palm.
Sequentially, the examiner releases pressure from one of the arteries
while continuing to occlude the other. The return of capillary refill
to the palm of the hand is then assessed. The test is then repeated for
the
other
artery. The test can also be performed using a Doppler probe.
Symptomatic, chronic vascular insufficiency of the hand warrants a
workup that includes an upper extremity arteriogram and includes images
of the aortic arch and subclavian arteries. The arteriogram is obtained
to rule out the presence of vascular occlusion anywhere in the vascular
system of the upper extremity. Additionally, an echocardiogram is
obtained to rule out mural thombi in the ventricles of the heart. Other
testing includes the use of noninvasive vascular studies such as
color-duplex imaging, cold immersion testing, and magnetic resonance
angiography.
symmetric discoloration of the digits occur, primarily in females under
the age of 40 is known as Raynaud’s disease. These patients seldom
experience any trophic changes of the digits and have no clinical
evidence of occlusive arterial disease or connective tissue disorder.
The diagnosis is established following 2 years of symptoms.
Alternatively, secondary vasospastic conditions resulting from such
conditions as connective tissue disorders (including scleroderma,
rheumatoid arthritis, systemic lupus erythematosus, vasculitis, and
CREST syndrome), occlusive arterial disease, hematologic disorders, and
occupational trauma is referred to as Raynaud’s phenomena. Patients
developing Raynaud’s phenomena, are typically over age 40, have some
underlying disease, and often experience progressive trophic changes of
the digits. Raynaud’s phenomena is seen in approximately 80% of
patients with scleroderma, 25% of patients with systemic lupus
erythematosus, and 10% of patients with rheumatoid arthritis. Initial
nonoperative treatment of Raynaud’s phenomena includes oral calcium
channel blockers and axillary sympathetic blocks. Anticoagulation
therapy may also have some merit. Patients with continued symptoms but
a favorable response to axillary sympathetic blocks may be good
candidates for peripheral arterial sympathectomy.
inflammatory vascular occlusive disorder related to the use of
nicotine. The condition is more common in men. In these patients,
narrowing of the digital arteries generally occurs resulting in
ischemic finger pain and Raynaud’s phenomena. Smoking cessation arrests
the progression of the disease in most instances.
repetitive trauma to the ulnar side of the wrist, resulting in
thrombosis of the ulnar artery and Raynaud’s phenomena. These patients
often have engaged in activities such as drywall hanging, carpentry, or
other construction activities. In some instances, patients will give a
dramatic history of how they have used the ulnar border of the wrist as
a “hammer” to secure or stabilize objects. These patients often
complain of coldness in the digits, color changes, or frank pain while
engaged in certain occupational maneuvers. Arteriogram shows an ulnar
artery devoid of flow and in many instances markedly diminished or
absent blood flow to the ring and small digits (Figure 14-17).
Treatment in symptomatic individuals requires resection of the
thrombosed ulnar artery segment and superficial palmar arch
reconstruction using a reverse flow vein graft, normally harvested from
a dorsal foot vein. Following ulnar artery reconstruction, symptoms of
ring and small finger ischemia can be expected to improve.
 |
|
FIGURE 14-17. Posttraumatic ulnar artery occlusion (hypothenar hammer syndrome).
|
TR, Strickland JW. Soft tissue reconstruction for rheumatoid swan-neck
and boutonnière deformities: long-term results. J Hand Surg
1993;18A:984-989. Ninety-two digits were treated
with soft tissue reconstruction for rheumatoid swan-neck deformity and
19 digits for boutonnière deformity. Overall the results were mediocre
and unpredictable leading the authors to conclude that arthrodesis is
the best treatment of advanced rheumatoid digital deformities.
RJ. Intrinsic Contracture. In: Green, DP, Hotchkiss, RN, Pederson WC,
eds. Green’s Operative Hand Surgery. 4th ed. New York: Churchill
Livingstone, 1999:604-618. This chapter has been
included in every edition of this textbook and has been left unaltered
from the author’s original version. Digital contractures of the hand
are outlines with an emphasis on pathologic anatomy and treatment.
RJ. Intrinsic muscles of the fingers: Function, dysfunction and
surgical reconstruction. In: AAOS Instr Course Lect, vol. 24. St.
Louis: CV Mosby, 1975:200-220. This is a classic
review defining the anatomy and pathologic anatomy of the intrinsic
muscle system of the hand. The specific characteristic of boutonnière
and swan neck deformities are discussed and illustrated.
RA, Gelberman RH, Seiler JG III et al. Carpal tunnel release: a
prospective, randomized assessment of open and endoscopic methods. J
Bone Joint Surg 1993;75A:1265-1275. In a
prospective, randomized fashion, this study examined the results in 169
hands having either open or endoscopic carpal tunnel release surgery.
Overall, 90 to 98% of patients experienced relief of paresthesias.
There was no significant difference in objective outcome measures. The
open method resulted in more scar tenderness and a longer return to
work than did the endoscopic method. A greater complication rate was
found with the endoscopic carpal tunnel release surgery.
V, Russwurm H. Neurophysiology not required before surgery for typical
carpal tunnel syndrome. J Hand Surg 2001;26B:61-64. In
this study, 14 of 63 patients who had successful carpal tunnel release
surgery had preoperative electrodiagnostic testing that were normal.
RH, Aronson D, Weisman MH. Carpal tunnel syndrome: results of a
prospective trial of steroid injection and splinting. J Bone Joint Surg
1980;62A:1181-1184. In patients with carpal
tunnel syndrome, 80% of patients receiving a carpal tunnel steroid
injection experience relief of their symptoms but only 22% will still
be symptom free at 1 year. Patients who had symptoms for less than 1
year were likely to have sustained relief.
PM, Gelberman RH, Dimick MP. Sensibility testing in patients with
carpal tunnel syndrome. J Bone and Joint Surg 1984;66A:60-64. Clinical
threshold testing, such as Semmes-Weinstein monofilament testing and
vibrational testing, are more sensitive in detecting abnormalities in
hand sensory dysfunction. Overall, the Semmes-Weinstein monofilament
testing was found to provide the most reliable sensory test.
RM, Slater RR II, Farver TB et al. The value of diagnostic testing in
carpal tunnel syndrome. J Hand Surg 1999;24A:704-714. The
authors evaluated a variety of diagnostic tests for carpal tunnel
syndrome. They concluded that there is an 86% chance of patients having
carpal tunnel syndrome when there is the combination of a positive
carpal tunnel compression test, abnormal monofilament testing,
subjective night pain, and a positive hand diagram. The results of
electrodiagnostic studies did not add to the diagnostic accuracy.
rationale for the use of nerve blocks is discussed as well as the nerve
block options available for complex regional pain syndrome. The
techniques for various nerve blocks are discussed and illustration
provided.
SE, Holder LE. The use of three-phase radionuclide bone scanning in the
diagnosis of reflex sympathetic dystrophy. J Hand Surg 1984;9A:556-563.
In 145 patients, the three-phase bone scan was
used to diagnose RSD. The authors found that increased radiotracer
uptake in phase III of the scan was diagnostic for RSD with a
sensitivity of 96% and specificity of 98%.
M, Janig W, Hassenbusch S et al. Reflex sympathetic dystrophy: changing
concepts and taxonomy. Pain 1995;63:127-133. This
article discusses the various terms associated with pain of uncertain
origin and redefines pain as either complex regional pain syndrome type
I or type II. The term sympathetic mediated pain is also explained.
D. Pollicization of the index finger: methods and results in aplasia
and hypoplasia of the thumb. J Bone Joint Surg 1971;53A:1605-1617. This
article provides the original technical description of index finger
pollicization for thumb hypoplasia along with early results.
hands in 23 patients that were treated with a radialization technique
are presented with the need for overcorrection stressed as well as soft
tissue balancing from releases and tendon transfers. The indications
for ulnar osteotomy are also discussed.
E, Kozin SH, Thoder JJ, Porter S. The recurrence of deformity after
surgical centralization for radial club hand. J Hand Surg
2000;25A:745-751. The authors review the results
of centralization of 19 radial club hands in 14 patients treated over
an 18-year period. The follow-up averaged 6.5 years. Sixteen of the
cases have radial aplasia. On average the patients lost a 38° of the
correction obtained at surgery. A correlation was found between the
preoperative angle and the final angle achieved. Better results were
obtained when complete correction could be obtained at initial surgery.
AE. Cleft hand and central defects. In: Flatt AE, ed. The Care of
Congenital Hand Anomalies. 2nd Ed. St. Louis: Quality Medical
Publishing, 1994:337-365. This chapter provides a
comprehensive and detailed discussion of all aspects of cleft hand and
is considered a classic. The etiology, classification, and operative
treatment are discussed. The primary surgical procedures are
illustrated.
article reviews the genetics and etiology of the condition as well as
the classification and indications for surgical treatment. Surgical
decision making is also discussed with emphasis on the technique of
syndactyly release. Associated conditions such as Poland’s syndrome,
constriction band syndrome, central deficiency, and Apert’s syndrome
are discussed. Complications of treatment are also discussed.
PR, Rotman MB, Dailey LA. Long-term functional results after
pollicization for the congenitally deficient thumb. J Hand Surg
1992;17A:1064-1072. This is a review of 28 index
finger pollicizations following correction of congenital hypoplastic
thumb. The final total active range of motion was approximately 50% of
the contralateral normal thumb and the average grip 21%. The pollicized
digit was used as a thumb in 84% of cases with a 22% prolonged time
period to accomplish standard tasks. Patients having radial club hand
had significantly poorer results. Age at the time of surgery did not
correlate with final results.
Y. Crystalline arthritis and other arthritides. In: Berger RA, Weiss
APC, eds. Hand Surgery, vol. II, ch. 70. Philadelphia: Lippincott
Williams & Wilkins, 2004:1241-1252. This
chapter provides a complete overview of the crystalline arthropathy
conditions of the wrist. The pathogenesis, epidemiology, natural
history, and treatment are outlined.
MM. Pellegrini VD, Burton RI. Arthroplasty of the basal joint of the
thumb: long-term follow-up after ligament reconstruction with tendon
interposition. J Bone Joint Surg 1995;77A:346-355. Twenty-four
thumbs in 22 patients were reviewed at an average follow-up of 9 years.
Over 95% of the patients had relief of their pain. Grip strength and
pinch strength both improved. Follow-up radiographs showed loss of
carpal height compared to preoperative evaluation but this did not
portend a poor outcome.
HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern
of degenerative arthritis. J Hand Surg 1984;9A:358-365. This
is a review of over 200 patients presenting to the authors’ clinic with
a primary degenerative arthritis of the wrist. One of the more common
patterns of degenerative arthritis observed was the scapholunate
advanced collapse pattern whereby the scaphoid-distal radius
articulation becomes primarily involved. In the more advance condition,
the midcarpal joint becomes involved with proximal migration of the
capitate and diastasis of the scaphoid and lunate. This condition
results in a loss of carpal height.
wrists treated for De Quervain’s disease were retrospectively reviewed.
Seventy-one percent of the wrists treated with one wrist corticosteroid
injection achieved sustained relief of symptoms. An additional 11% of
the wrists gained relief with a second injection. Of the 11 wrists that
ultimately underwent first dorsal compartment release, 10 had
septations within the first dorsal compartment.
WT, Viegas SF, Coon TM et al. Anatomical variations in the first
extensor compartment of the wrist. J Bone Joint Surg 1986;68A:923-926. Three
hundred cadaver wrists were examined for anatomic variations in the
first dorsal compartment. In 40% of the wrists, a septum divided the
first dorsal compartment. In a separate clinical series, patients
undergoing release of the first dorsal compartment for DeQuervain’s
syndrome, there was a 67% incidence of septations within the first
dorsal compartment.
patients with DeQuervain’s disease were treated with either injection
alone, injection plus splinting, or splinting alone. The results from
injection alone were superior to splinting alone and not significantly
different from the combination of splinting and injection.
review examines the history of Dupuytren’s disease and dating its
origin somewhere between 1200 BC-200 BC. The author concludes that the
disease is probably not due to a single gene but is most likely
multifactorial.
MA, Hurst LC, Grandia SK et al. Platelet-derived growth factor in
Dupuytren’s disease. J Hand Surg 1992;17A:317-323. Palmar
facia obtained from surgical release of Dupuytren’s contracture release
was analyzed in 28 patients. An association between platelet-derived
growth factor (PDGF) and myofibroblasts found in the proliferative
stages of Dupuytren’s disease. The results of the study suggest that
the PDGF is bound to a cell membrane. The authors conclude that PGDF
may play a role in the proliferative events of myofibroblasts.
digits in 19 patients were treated surgically for recurrent Dupuytren’s
contracture and followed up at a median of 4 years. Dermatofasciectomy
and full-thickness skin grafting did not prevent recurrent contracture.
Three of the digits were anesthetic at follow-up. At follow-up, 18 of
19 patients were pleased with their results. There were no vascular
injuries, infections, flap, or graft losses.
J, Rayan GM. Correlation of alpha-smooth muscle actin expression and
contraction in Dupuytren’s disease fibroblasts. J Hand Surg
1995;20A:450-455. Eleven specimens from the
palmar fascia from patients with Dupuytren’s disease where analyzed for
smooth muscle actin. The results of the study show that fibroblasts in
patients with Dupuytren’s disease can acquire contractile
characteristics and the increased presence of smooth muscle actin in
these fibroblasts correlates with increased contractile activity.
retrospective study reviewed the results of 12 patients with
necrotizing fasciitis of the upper extremity. Eleven of the 12
infections were caused by β-hemolytic strep organisms. Ten of the
patients had a history of IV drug abuse and 2 patients were diabetic.
An average of 3 surgical debridements were necessary to control the
infection. Two patients required shoulder disarticulation and all
patients resolved their infection. The authors stress the importance of
early recognition of this condition as well as the need for aggressive
surgical debridement and appropriate antibiotic therapy.
review article discusses the anatomy of the nailbed and the distal
fingertip as well as the various infection forms seen in this area
including the acute paronychial infection, the chronic paronychial
infection, and the felon.
review of 700 patients with hand infections found 6% with osteomyelitis
of the hand bones. Fifty-seven percent were caused by trauma while 13%
were hematogenous. Twenty-two percent were immunocompromised or had
peripheral vascular disease. Cultures were positive in 74% with 35%
having multiple organisms and 35% Gram-positive organisms. The overall
amputation rate was 39%.
comprehensive review of the spectrum of animal bite injuries covers
such common bite wounds as dogs and cats as well as more obscure bite
wounds such as those from wolves, badgers, bears, skunks, snakes,
spiders, scorpions, and various marine species.
patients with Keinbock’s disease were examined to determine the
relationship if any with the presence of ulnar negative variance. The
patients were compared to a group of 99 control patients and the
authors determined that an association did exist between Keinbock’s and
the presence of ulnar negative variance.
J, Stanley JK, Trail IA. Keinbock’s disease: conservative management
versus radial shortening. J Bone Joint Surg 2000;82(B):820-823. The
results of 18 patients with stage 2 or 3 Keinbock’s treated
conservatively were compared with 15 patients treated operatively. The
mean follow-up was 3.6 years. The patients treated with radial
shortening had better pain relief and a stronger grip than patients
treated conservatively. Some patients treated conservatively rapidly
progressed to carpal collapse. Patients treated with radial shortening
osteotomy had a slower progression to carpal collapse.
AY, Bishop AT. Pedicled vascularized bone grafts for disorders of the
carpus: scaphoid nonunion and Keinbock’s disease. J Am Acad Orthop Surg
2002;10:210-216. This article reviews the anatomy
and indications of the reverse flow, pedicled vascularized bone graft
options of the dorsal aspect of the distal radius. These vascularized
bone grafts can be adapted for revascularization of the lunate in
patients with Keinbock’s disease.
DP. Radial nerve palsy. In: Green DP, Hotchkiss RN, Pederson WC, eds.
Green’s Operative Hand Surgery, 4th Ed., vol. 2. New York: Churchill
Livingstone, 1999:1481-1496. Extensive review of the subject with detailed discussion of the techniques for transfer.
G. Ulnar nerve palsy. In: Green DP, Hotchkiss RN, Pederson WC, eds.,
Green’s Operative Hand Surgery, 4th Ed., vol. 2. New York: Churchill
Livingstone, 1999:1526-1541. Comprehensive review
of the ulnar nerve palsy condition, including a detailed discussion of
physical examination findings and techniques for restoring function.
O, Saels P, Rombouts JJ et al. Long-term functional results of wrist
arthrodesis in rheumatoid arthritis. J Hand Surg 1999;24(B):27-31. Eighteen
patients were reviewed at an average of years following wrist
arthrodesis. All patients were pleased with the procedure and had
satisfactory pain relief.
patients followed-up at an average of 6.5 years with the biaxial total
wrist arthroplasty. Ninety-two percent of the patients rated themselves
as better. Eleven cases had failures, 8 of these at the distal implant.
Survival analysis determined an 83% probability of survival at last
follow-up.
SD, Beckenbaugh RD, Redondo J et al. Long-term follow-up of pyrolytic
carbon metacarpophalangeal implants. J Bone Joint Surg
1999;81(A):635-648. Twenty-six patients were
followed up at an average of 11.7 years after placement of pyrolytic
carbon MCP implants. Ninety-four of the implants showed
osteointegration. The 16-year survival rate was 70.3%. Ulnar drift was
unchanged from preoperative and digital range of motion was improved to
a relatively extended position.
KK, Ashworth CR, Ebramzadeh E et al. Swanson metacarpophalangeal joint
arthroplasty in patients with rheumatoid arthritis. Clin Orthop
1997;342:11-15. The results of 170 Swanson
Silastic MCP implants were evaluated at a mean of 5.2 years. No pain
was reported in 54% of the joints. Mean postoperative range of motion
was 27° compared to 38° preoperatively. Prosthesis survivorship at 10
years was 90%.
patients with trigger finger were treated with MCP joint splinting, and
another 50 trigger fingers were treated with injection. All patients
were followed up at one year. Treatment was successful in 66% of the
splinted patients and 84% of the injected patients. Patients with
multiple trigger fingers and symptoms greater than 6 months had worse
results in both groups.
patients were assessed after open release of A1 pulley for trigger
finger. One hundred percent of patients had either complete relief or
substantial relief of their symptoms. Only 3% had recurrence.
metastatic lesions in 18 patients were reviewed. The most common
location was the distal phalanx while the most common primary tumors
were in the lung and kidney. Over 50% of the patients in this series
died within 6 months of hand metastasis diagnosis.
P. Primary bone tumors. In: Berger RA, Weiss A-PC, eds. Hand Surgery.
Philadelphia: Lippincott Williams & Wilkins; 2004. Comprehensive
review of the most common benign and malignant bone tumors of the hand
and wrist. The chapter also reviews the important features of the tumor
workup and staging. An algorithm is provided for malignant bone tumor
decision making.
observation is an acceptable form of treatment, aspiration or surgical
excision is indicated for lesions causing pain, skin ulcerations,
functional limitations, or nerve compression. Recurrence rates of
greater then 50% are common following aspiration and puncture of most
ganglions. Aspiration is most successful for ganglion of the flexor
tendon sheath. When performed properly, the recurrence rate following
surgical excision is less than 5%.
Griend RA, Funderburk CH. The treatment of giant-cell tumors of the
distal part of the radius. J Bone Joint Surg 1993;75A:899-908. The
results of treatment for giant cell tumor of the distal radius were
studied in 23 patients. Extended curettage and cementation was
performed in 5 patients who had limited or no extraosseous tumor
extension. Eighteen patients having extraosseous tumor extension were
treated by distal radius resection and arthrodesis. At a follow-up
there were no recurrences.
patients with Raynaud’s phenomena due to a systemic process had
refractory pain and digital tip ulcerations. Following microvascular
peripheral sympathectomy, all patients had improved pain, and
improvement in the digital ulcerations. Although total blood flow was
not appreciatively improved, the sympathectomy increased overall
nutritional flow to the digit.
review article discusses Raynaud’s phenomenon and Raynaud’s disease
including the pathophysiology of each condition. Various vasospastic
disorders causing secondary Raynaud’s phenomenon are categorized and
listed. Treatment options including digital sympathectomy are
discussed. A digital algorithm is provided.
