The Pediatric Leg and Knee
common and obvious abnormalities to affect the child’s lower
extremities. Trauma is the major concern; however, the understanding of
other congenital or acquired deformities is important to minimize or
prevent the long-term sequelae in later life. Some of the deformities
are physiologic and periodic observation and reassurance of the parents that the deformity
is a variant of normal but not a disease. In this chapter, the various
physiologic and pathologic conditions affecting the leg and knee are
discussed, and the trauma affecting the physis and impacting on both
the growth and development of the child’s leg and knee are also
addressed.
presents as recurvatum and is evident at birth. The incidence is
approximately 1% of the incidence of congenital dislocation of the hip.
It may be an isolated entity or may occur with associated
problems, such as dislocated hips, clubfoot, myelodysplasia, Larsen’s syndrome, or arthrogryposis (Figure 18-1).
Special attention must be paid to the hip joint because approximately
50% of children have congenital dislocation of the hip. Several
terminologies have been used in describing congenital hyperextension of
the knee, a descriptive term indicating recurvatum of the knees at
birth. Hyperextension of the knee in newborn infants may be caused by
aberrations in intrauterine positions, such as the frank breech
position, which slowly stretches the hamstrings and soft tissues of the
posterior aspect of the knee. Fibrosis of the quadriceps mechanism is
generally believed to be secondary to the dislocation rather than its
cause. At least half of all babies presenting with this clinical
appearance have some passive knee flexion at birth, and the severity of
the deformity is variable.
relationship. In type I, hyperextension is minimal, and the knee can
passively be flexed to 90°. In type II, or moderate type, in which
there is subluxation of the tibia anteriorly on the femoral condyles,
the knee can be flexed up to 45°. In type III, or severe type, there is
complete anterior dislocation of the proximal tibia on the femoral
condyles with no contact between the tibia and the femur. Most of type
I and type II cases respond quickly to a gentle manipulation and serial
casting program or Pavlik harness to maintain knee flexion for a few
weeks. However, treatment of congenital dislocation of the knee or hip
associated with Larsen’s syndrome or myelodysplasia is difficult.
Fibrosis of the quadriceps is present in this type, and this is the
change that separates congenital knee dislocations from the more easily
treatable postural deformations. In patients unresponsive to
nonoperative treatment and in most of type III cases, early open
reduction and quadricepsplasty are required. Surgical lengthening of
the quadricepspatellar tendon complex is the first step, and then the
knees can be flexed and reduced. Knee dislocation must be resolved
prior to treatment of congenital hip instability. Postoperative
management includes initial positioning of the knee in slight flexion
to remove tension on the skin incision and then progressive flexion to
obtain at least 90° of knee flexion. Long-term outlook is variable;
however, lack of complete flexion is common.
 |
|
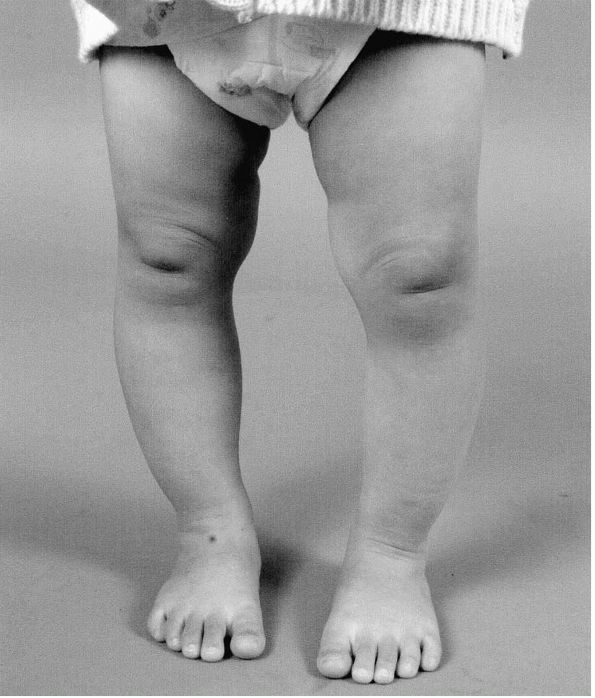
FIGURE 18-1. Clinical appearance of congenital dislocation of the right knee in a child with arthrogryposis and hyperextended knee.
|
condition, where hypoplasia of the patella, lateral femoral condyle,
trochlea groove, and quadriceps mechanism are seen along with lateral
displacement and fixation of the patella (Figure 18-2).
There is a fixed flexion contracture of the knee, and the patella is
laterally displaced with genu valgum and the tibia is externally
rotated. Nonoperative treatment is futile. Surgical correction includes
extensive lateral release, advancement of the vastus medialis obliquus,
semitendinosus tenodesis to the patella and the centralization of the
patella tendon insertion.
 |
|
FIGURE 18-2.
Anteroposterior radiograph of the congenital dislocation of the patella demonstrates lateral displacement of the patella and externally rotated tibia. |
young children are frequent causes of anxiety in parents and a common
cause of referral to the orthopaedic surgeons. In the vast majority of
cases, genu varum corrects by itself with growth. Evaluating angular
malalignment is simplified, if one is familiar with the normal
development of the tibio-femoral angle. Normal knee alignment is
approximately 10 to 15° of varus at birth, which progresses to neutral
alignment at about 18 months of age. The appearance of genu varum
frequently is exacerbated or accentuated by concurrent internal tibia
torsion (Figures 18.3 and 18.4).
Most report that persistence of genu varum beyond 2 years of age is
abnormal. However, spontaneous correction of the physiologic genu varum
will occasionally be delayed until 30 months of age, and even
pronounced physiologic genu varum greater than 30° can correct with
continuing growth. Overcorrection to excessive genu valgum is maximal
at 4 years of age, and the valgus angulation averages 8°. Correction to
physiologic valgus is usually by 5 or 6 years of age.
 |
|
FIGURE 18-3. Clinical appearance of physiologic genu varum in a 26-month-old boy.
|
however, if there is a concern that this falls outside the normal range
in a child 18 to
36
months old, or is associated with short stature or asymmetric
involvement, standing anteroposterior radiographs should be taken to
rule out any pathologic conditions. The treatment of physiologic genu
varum and valgum is periodic observation and examination, together with
education and reassurance of the parents that the deformity
is a variant of normal but not a disease. Fat thighs, ligamentous
laxity, and flatfoot often result in toed-out habitus, and can
accentuate the knock-kneed appearance and make physiologic genu valgum
appear more severe. Torsional malalignment can have a similar effect.
In rare cases of uncorrected physiologic genu valgum greater than 20°,
hemiepiphysiodesis or osteotomy may be indicated.
 |
|
FIGURE 18-4. Thigh-foot angle. Concurrent internal tibial torsion exacerbates the clinical appearance of physiologic genu varum.
|
genu varum in children and adolescents. It is considered to be a
developmental condition, which affects posteromedial aspect of the
proximal medial tibial physis, resulting in a progressive varus
deformity. Biopsy of the lesions reveals disorganized physeal cartilage
with abnormally large groups of capillaries, densely packed
hypertrophic chondrocytes, and islands of almost acellular fibrous
tissue. Both fibrovascular and cartilaginous reparative tissue can be
found at the physeal-metaphyseal junction. Infants affected by this
condition are usually of black or Mediterranean origin, often have a
history of early walking, and are in the upper percentile of weight for
height. Examination of the child with tibia vara reveals an angular
deformity discernable just below the knee. In contrast, young child
with physiologic genu varum will have a more gentle curvature of the
entire extremity. A lateral thrust, indicating laxity of the lateral
ligamentous complex, may be seen in children over the age of 3 with
tibia vara.
forms. Infantile Blount’s disease may be difficult to diagnose in its
early form until 2 years of age, when the radiographic changes
suggestive of infantile tibia vara are more evident (Figure 18-5).
The Langenskiöld radiographic staging classification reflects the
progression of tibia vara in untreated cases. The natural history of
untreated cases is to progress to complete medial physeal arrest, which
can occur by the age of 6 (Figure 18-6). In
such an event, subsequent treatment is difficult, because both angular
deformity and tibial shortening must be addressed. Other radiographic
criteria have been developed, such as the metaphyseal-diaphyseal angle
for the early diagnosis of Blount’s disease. Some children with
metaphyseal-diaphyseal angles described as compatible with infantile
tibia vara (an angle of 16° is currently accepted) spontaneously
improve without treatment; at the present, this differentiation
continues to be very difficult in the early Langenskiöld stages.
 |
|
FIGURE 18-5.
Anteroposterior radiograph of a 3-year-old boy with infantile tibia vara. Prominent beaking of the medial metaphysis and varus angulation at the epiphyseal-metaphyseal junction are evident. |
management in patients younger than 3 years old may be successful in
correcting the mild deformity. Obesity, instability, and delayed
bracing are considered as risk factors for failure. Early valgus
osteotomy before 4 years of age is strongly recommended to minimize
deformity of the proximal medial physis. With this in mind,
overcorrection into 5 to 10° valgus angulation beyond normal should be
the goal. The pathology of late onset tibia vara between the ages of 6
and 13 is similar to that of
infantile
tibial vara; however, because growth at the tibia is closer to maturity
in the adolescent, bracing is not effective. Various techniques,
including plate, monolateral, or circular external fixation, have been
described to maintain position after osteotomy. Use of rigid external
fixation with acute or gradual correction allows accurate alignment of
the lower extremity and prevents complications such as nerve palsy,
compartment syndrome, overcorrection, or undercorrection. For those
adolescent patients with significant growth remaining, consider
selective lateral epiphysiodesis. The rate of correction following this
procedure has been reported to be 4° per year.
 |
|
FIGURE 18-6.
Anteroposterior radiograph of a 7-year-old boy with untreated infantile tibia vara demonstrates complete medial physeal arrest of the proximal tibia. |
to intrauterine position. The posture of the newborn with posteromedial
bowing of the leg is characteristic (Figure 18-7),
with marked calcaneo-valgus and dorsiflexion of the foot, which may
even be opposed to the tibia. The natural history of this condition
would be gradual resolution of the foot deformity and the tibial bowing
with growth. In general, the severity of initial deformity is related
to the amount of ultimate leg shortening, and final leg length
discrepancies at the maturity vary from 5 to 27% relative to the
contralateral normal side. No treatment for bowing is necessary or
indicated. Serial documentation of discrepancy throughout childhood is
advisable, and physeal arrest of the contralateral leg or lengthening
of affected tibia should be performed, if the discrepancy is projected
to exceed 2.5 cm at maturity.
 |
|
FIGURE 18-7. Anteroposterior radiograph of a 4-year-old girl with posteromedial bowing of the tibia.
|
to congenital posteromedial bowing, is not a benign condition and is
the heralding physical sign
of actual or impending fracture with subsequent pseudoarthrosis of the tibia (Figure 18-8).
Congenital pseudoarthrosis of the tibia is relatively rare, occurring
in 1 in 190,000 live births. The cause of congenital pseudoarthrosis of
the tibia is unknown and appears to be the end expression of several
different pathologic conditions. Neurofibromatosis is linked to about
50% of cases, and the pathology is not particularly different from
other causes of pseudoarthrosis, with a cuff of harmartous tissue
surrounding the lesions. Congenital pseudoarthrosis, which is not
associated with neurofibromatosis, develops often after a seemingly
innocuous fracture in what appears to be reasonably normal bone.
the tibia: dysplastic, cystic, sclerotic, fibular, and clubfoot or
congenital band type. The most common type is dysplastic, where the
tibia is tapered at the defective site; an hourglass constriction
is more often associated with neurofibromatosis. Furthermore, this type
has a poor natural history with regard to fracture healing, and
recurrent fracture is common even if union is achieved. In the
sclerotic type, the medullary canal is absent, and the fracture often
appears transverse and incomplete initially, like a stress fracture.
Late onset fractures seem to have a better prognosis.
 |
|
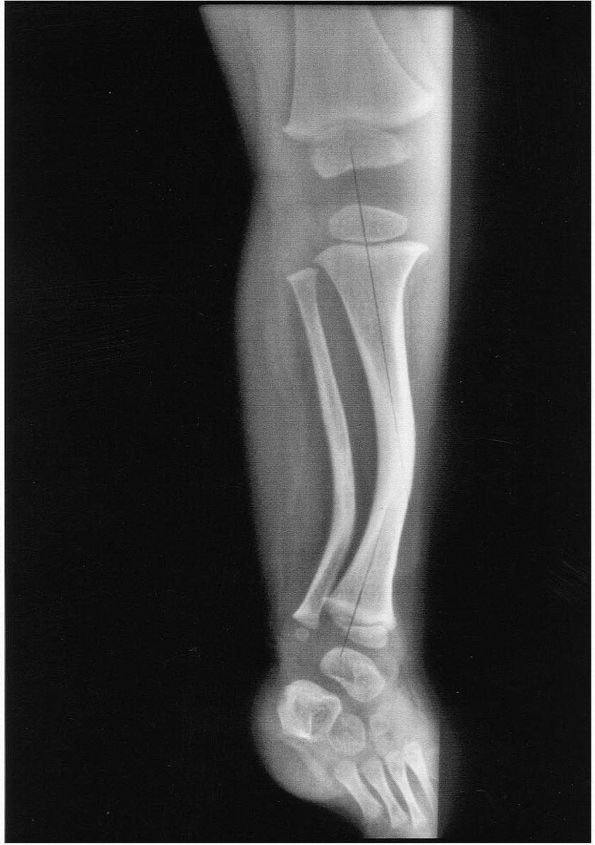
FIGURE 18-8.
Lateral radiograph of a 5-year-old girl with congenital pseudoarthrosis of tibia demonstrates anterior bowing of the tibia and the fracture occurred in the cystic lesion. |
orthosis may prevent or delay fracture, however, after the fracture has
occurred, cast immobilization is generally unsuccessful. The management
of established pseudoarthrosis remains controversial, and currently
popular methods include excision of the lesion followed by compression
with external fixator, vascularized fibular grafts, or intramedullary
rodding. When treatment fails, Syme amputation and prosthetic fitting
are needed for a functional limb. Treatment and follow-up through
adolescence are appropriate, because a high rate of refractures often
need retreatment, and delayed fracture of the tibia in late adolescence
is frequent. Patients with union at skeletal maturity usually, but not
necessarily, fare well in adult life.
lower extremity with or without a terminal deficiency at the foot. It
is a paraxial deficiency, and the spectrum varies from complete absence
of the fibula with missing lateral rays to a fibula that is slightly
short with a ball and socket type of ankle joint (Figure 9-2).
The tibia has an anterolateral bow, and the femoral shortening may
accompany fibular hemimelia. If it does, the lateral femoral condyle is
always deficient. The magnitude of the projected shortening usually is
related to the severity of fibular and lateral ray absence. Tarsal
coalition may exist with a mass representing the talus and calcaneus.
rendered stable weight-bearing surface or there is excessive predicted
leg length discrepancy, patient satisfaction following Syme’s
amputation and prosthetic fitting is high. This procedure is optimally
performed before the time when children would normally ambulate. Staged
limb lengthening in some cases has been demonstrated to be successful
in achieving limb-length equality in children with less than 35%
projected shortening of the tibia and fibula, when undertaken carefully
with protection of the ankle and foot to avoid exacerbation of the
valgus position of the hind foot. Complex assemblies for lengthening
are required to protect the foot from further deformity during the
lengthening for fibular hemimelia.
the knee in which the lateral meniscus is discoid in shape rather than
normal semilunar configuration. It is seen in 1 to 3% of normal
population with a higher frequency in Asians. It can be complete,
incomplete, or the Wrisberg type. The latter is characterized by the
absence of a menisco-tibial attachment, and the increased mobility
allows the development of a discoid configuration as a secondary event.
in the knee in the infant, especially when the child is agitated. Most
patients present in childhood and early in adolescence. The hallmark
complaint in the Wrisberg type is a snap or clunk in the knee with
motion. Symptoms of snapping and popping usually occur between the ages
of 6 and 12 years. There may be associated pain or limp. Routine
radiographs may show a widened lateral joint space and tibial eminence
flattening. Three or more cuts of MRI showing a meniscus 5 mm thick
from anterior to posterior are indicative of a discoid meniscus (Figure 18-9). In addition, the meniscus may extend into the notch and demonstrate intrasubstance degeneration.
full mobility, and no effusion. Most discoid meniscal surgery is
performed by arthroscopic techniques. The first goal is to establish
the presence of stability. Arthroscopy-assisted sculpturing of the
meniscus to a normal configuration is attempted for the complete and
incomplete types. If the meniscus is unstable, this should be repaired;
however, complete menisectomy should be avoided.
 |
|
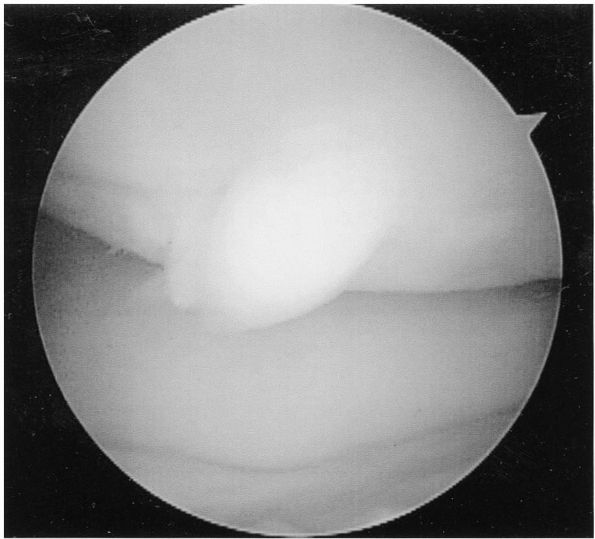
FIGURE 18-9.
T2-weighted magnetic resonance image of a discoid lateral meniscus shows a continuous bow-tied or slab appearance of lateral meniscus and degenerative changes within the posterior horn of meniscus. |
portion of the articular cartilage of the knee and its underlying
subchondral bone becomes separated from the remaining articular
cartilage. Its origin is unknown. Repetitive trauma imposed by the
tibial spine on the medial femoral condyle has been suggested as a
principal cause. Symptoms are related to the condition’s acuity, may be
present only with activity, and may be associated with recurrent
effusions. Occasionally, there are symptoms of locking or catching of
the knee when an osteochondritis dissecans fragment is a free loose
body. Local tenderness may be present with direct pressure at the
lesion, if it is unstable.
tunnel view, demonstrate the lesion. The most common site is in the
non-weight-bearing, posterior lateral aspect of the medial femoral
condyle, and the lesion is seen as an osseous fragment surrounded by a
lucent defect. A portion of lateral femoral condyle or patella can also
be involved. MRI or arthroscopy helps determine the fragment’s
articular cartilage continuity, size, and integrity of its subchondral
bone (Figure 18-10).
based on the age and status of the fragment. In children and
adolescents in whom the lesion is not yet separated from the remaining
subchondral bone, cast immobilization for a period of 6 to 12 weeks is
warranted, with healing in most patients. Conversely, instability or
loss of continuity of the articular surface compromise healing. When
the articular surface of the condyle is disrupted, it is important to
stabilize the fragment and to encourage revascularization by drilling
the base of the lesion or by bone grafting of large osteochondral
defects. Currently, these procedures are performed arthroscopically in
most cases. Excision of irregular lesions with curettage of the
underlying bone may be of value in some cases. When a large portion of
the weight-bearing surface of the medial compartment of the knee is
involved, degenerative arthritis of the knee with narrowing and
sclerosis of the joint can be expected to occur at an early age.
 |
|
FIGURE 18-10.
Arthroscopic examination of the knee in a 12-year-old boy with osteochondritis dissecans. The lesion is partially detached and a hinge of intact cartilage on one edge of the femoral condyle. |
typically seen in athletic boys between the ages of 10 and 15. The
lesion is considered secondary to unresolved, submaximal avulsion
fractures at the patella tendon-tibial tubercle junction. As the
apophysis of tibial tubercle matures, ossification changes from
membranous to endochondral. During the endochondral phase, the physis
is less resistant to tensile stress, and failure may manifest by
fragmentation of bone at this site.
anterior tibial tubercle, and pain with kneeling or activity involving
quadriceps contraction. Symptoms may span the spectrum from pain solely
with direct contact of the tibial tubercle to pain during physical
activities such as running and jumping, to chronic pain associated with
activities of daily living. Radiographs show fragmentation or
prominence of tibial tubercle (Figure 18-11).
Ossicle formation occurs in nearly 40% of patients within the patella
ligament, and the radiographic findings do not necessarily correlate
with clinical symptoms.
almost all cases asymptomatic by skeletal maturity. In children who
have pain merely with contact and are able to be athletically active
without symptoms, no intervention is required except for provision of
knee pads during sports. In patients who have pain during sports
activity in the absence of direct knee contact or who have pain with
activities
of daily living, rest from offending activities and temporary
substitution of nonoffensive activities are recommended. Surgical
excision of a residual loose ossicle remaining at skeletal maturity has
been described with good outcome; however, skeletal maturity does not
necessarily need to be reached before the ossicle is enucleated.
Debulking of the tibial tubercle may be done at the time of ossicle
excision in patients who are mature.
 |
|
FIGURE 18-11. Lateral radiograph of a 13-year-old boy with Osgood-Schlatter disease shows fragmentary ossification of the tibial tubercle.
|
radiographic curiosities are noted incidentally. An incompletely
ossified portion of the patella is a radiographic characteristic.
Involvement of the superolateral corner of the patella occurs in 75% of
cases. Symptoms may occur at the patella-fragment junction due to acute
trauma or repetitive microtrauma causing separation.
radiographic findings but may present in patients with knee pain.
Typically, cysts are bilateral and well circumscribed in the patella.
Biopsy of patellar cysts reveals nothing more than a cyst with synovial
fluid. Surgical intervention is not indicated.
the inferior patella pole-superior patellar ligament junction and
represents a sequelae of chronic tensile stresses at that site. Healthy
athletic boys are commonly affected. In the adolescent, signs and
symptoms occur at the proximal patella ligament, the so-called jumper’s knee.
Radiographic evaluation of the knee may be normal or may demonstrate
variable changes in distal patellar pole ossification. Treatment
consists of ice, massage, anti-inflammatory medication, and rest from
running and jumping activities with resolution of the pain in 2 to 4
weeks. Healing of the lesion may be ascertained radiographically by
increased ossification at the pole of the patella with increased
longitudinal length of the patella. Surgical intervention is not
indicated.
complaint among the skeletally immature adolescents, but it is not rare
in preadolescence. The symptoms are usually well localized to the
peripatellar region, and giving way is a common complaint. Knee pain in
the skeletally immature patient must be considered referred hip pain
until proven otherwise, and a thorough hip examination must be a part
of the evaluation of knee complaints.
pain and swelling associated with activities such as prolonged walking,
running, or jumping. Pain gets worse by prolonged sitting, stair
climbing, squatting, and inclement weather, and the patient has a sense
that the involved knee will give way. Patients with anterior knee pain
demonstrate full range of motion of the knee and no instability. There
may be low grade synovitis, and significant muscle weakness of the
lower extremity is frequently present. A comprehensive rehabilitation
program is the treatment of choice with no need for bracing,
arthroscopic evaluation, or other interventional modalities.
most commonly occur laterally. The loss of articular continuity occurs
during a phase of patellar excursion, usually at 0 to 25° of flexion.
The most common cause is lateral malalignment of the quadriceps
mechanism, and ligamentous laxity in Down syndrome or Ehlers-Danlos
syndrome, lateral soft tissue contractures, external tibial torsion, a
shallow intercondylar notch of the femur, patella alta, or vastus
medialis insufficiency may be contributing factors (Figure 18-12).
In recurrent patella instability, the frequency and magnitude of
precipitating events and any previous treatment need to be addressed.
The patient presents with a complaint of sudden knee pain and a
sensation of instability or giving way of the knee. With recurrent
subluxation or dislocation, the vicious cycle of pain and reflex
weakness of the dynamic stabilizers of the knee result in
activity-related pain, swelling, and instability.
extremity alignment, joint motion, patella alta, ligamentous laxity,
muscle strength, and quadriceps retinacular competence. It reveals a
hypermobile patella with lateral displacement of the patella and may
reveal contracture of lateral retinaculum with only minimal medial
displacement of the lateral edge of the patella from the lateral
femoral condyle. The quadriceps complex, patella, and femur must be
thought of as a unit. The Q angle is formed by a line drawn along the
quadriceps
tendon
and a line drawn along the patella ligament, and a large Q angle is
associated with a tendency toward lateral subluxation of the patella.
Patellofemoral sulcus incongruity may be due to anatomic
maldevelopment. Four-view knee radiographs should be obtained. A
tangential view obtained with the knee in 40° of flexion shows the
relationship of the patella to the anterior part of the femoral
intercondylar groove, and may also demonstrate loose bodies and
fractures of the patella or lateral condyle. CT scan is helpful in
assessing the relationship of the patellofemoral joint in terms of tilt
or translation, or both.
 |
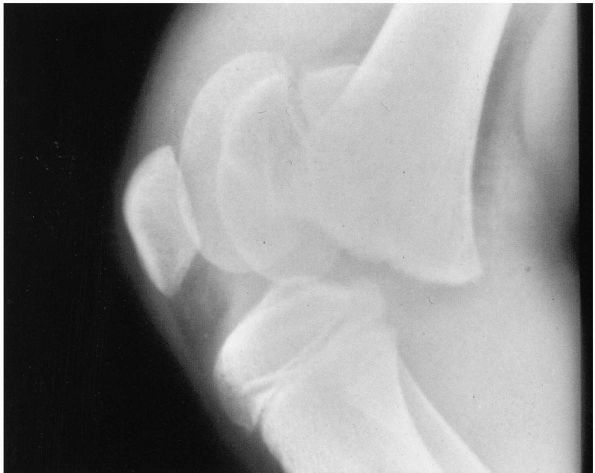
|
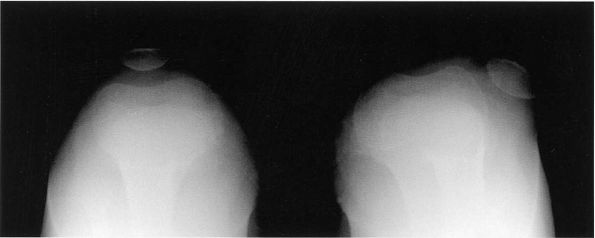
FIGURE 18-12. A skyline view of the knee shows lateral dislocation of the patella with hypoplastic lateral femoral condyle.
|
pathology, the initial management should be nonoperative. Strengthening
the vastus medialis is of the utmost importance and may reduce the
frequency of dislocation. If conservative treatment fails, the surgical
approaches to growing children should be focused on realigning the
quadriceps mechanism, usually in combination with a lateral release and
the creation of a medial patella restraint. However, the surgeon’s
options are limited by the open growth plate of the tibial tubercle,
which prohibits operations that transfer the origin of the patellar
tendon. To date, proximal realignment of the quadriceps and the
transfer of the semitendinosus tendon to the patella has been the best
option to recurrent dislocating patella in skeletally immature
children, even in cases with ligamentous laxity. Tibial tubercle
rotational realignment, described by Elmslie and Trillat, has proven
successful without drastically altering patellar realignment. After
operation, an intensive physical therapy program is required.
of the medial collateral ligament and may require stress radiographs
for definitive diagnosis. Minimally displaced fractures of the distal
femoral epiphysis may be treated by immobilization in a long-leg cast,
while those fractures that are completely displaced, such as in
Salter-Harris type II, have unexpectedly higher incidences of physeal
arrest than epiphyseal fractures in other locations (Figure 18-13).
Closed reduction can often be obtained; however, because of inherent
instability, percutaneous internal fixation with the aid of an image
intensifier may be necessary to maintain reduction of Salter-Harris
types I and II fractures. Premature closure of the distal femoral
physis is common due to the significant energy required to produce such
a fracture. Complete cessation of growth of the distal femoral physis
may occur, resulting in leg length discrepancy; partial closure of the
physis results in progressive angular deformity of the knee.
in adults, and usually occur in older children. Avulsion fractures may
involve the superior, medial, inferior, or lateral patella. A sleeve
fracture of the distal pole of patella is actually the most common type
in children, and often appears benign on a radiograph, because only a
fleck of bone is seen. However, a rather large cartilaginous sleeve is
avulsed along with the periosteum and retinaculum. Displaced transverse
fractures are treated as in adults, with open reduction and tension
band wiring.
the anterior spine is fractured many times more often than the
posterior. By placing the knee in extension, the displaced fragment can
generally be reduced, although the medial meniscus has been found
interposed with completely displaced fragments. If radiographs of the
knee in full extension demonstrate anatomic reduction of the fracture,
immobilization of the knee in this position is expected to result in an
excellent return of function. However, an unreduced fragment is managed
either
arthroscopically
or with open reduction. Anterior cruciate ligament laxity has often
been noted on follow-up of completely displaced fractures, but
complaints or subjective instability is infrequent.
 |
|
FIGURE 18-13. Lateral radiograph of the knee shows anteriorly displaced Salter-Harris type II fracture of the distal femoral physis.
|
tremendous amount of energy and carries poor prognosis, because the
metaphysis can be displaced posteriorly and peripheral ischemia occurs
in 15% of the patients. Most Salter-Harris types I and II fractures are
treated with closed means, but types III and IV injuries are usually
treated with open reduction and internal fixation. Angular deformity
can occur due to asymmetrical growth arrest or malunion, and this is
treated with physeal bar excision if less than 50% of the physis is
involved.
The mechanism of injury for avulsion of the tubercle is forceful
quadriceps contraction against resistance. Treatment for all but
minimally displaced fractures consists of open reduction and internal
fixation. Posttraumatic genu recurvatum can occur in younger children
due to premature arrest of the anterior aspect of the growth plate.
nondisplaced, with or without fibular fracture, may result in a valgus
angular deformity. Although exact mechanism of this phenomenon is
unknown, the deformity worsens for about 2 years and then improves
gradually. Osteotomy at the time of the greatest deformity is very
often unrewarding, as the osteotomy can induce the same reaction as the
fracture, producing recurrent valgus.
lower extremity in children, and the shaft fractures can generally be
managed with casting. Less than 10° of angulation should be the goal in
older children, and varus angulation remodels better than
valgus
or posterior angulation. Reports also indicate that the incidence of
compartment syndrome, vascular injury, infection, and delayed union in
children is similar to that in adults.
 |
|
FIGURE 18-14. Anteroposterior radiograph of the knee shows displaced fracture fragment of tibial eminence.
|
being recognized more frequently, and tears of both cruciate and
collateral ligaments have been reported. Hemarthrosis without fracture
implies significant soft tissue injuries. The natural history of
anterior cruciate ligament (ACL) injuries is simply not good. There is
no doubt at present regarding whether operative reconstruction is
necessary; the question is rather on a technique that will not
interfere with subsequent growth. Many ACL injuries in skeletally
immature patients occur at the tibial insertion. The substantial series
of untreated posterior cruciate injuries in children has not been
reported.
 |
|
FIGURE 18-15. Lateral radiograph of the knee shows Salter-Harris type II fracture of the tibial tubercle.
|
authors reported arthroscopically documented anterior cruciate ligament
tears, and recommended arthroscopic assessment for any patient with an
acute hemarthrosis.
article describes congenital dislocation of the knee and its associated
abnormalities and expected outcomes. The authors emphasize the need for
treatment of knee dislocation before treatment of hip or foot
deformities.
and treatment of subluxation, tilt plus subluxation, and tilt alone are
suggested. In addition to the author’s recommended treatment of
realignment of the quadriceps mechanism, a comprehensive review of the
literature is presented.
HW, Weinstein SL. Intramedullary fixation and bone grafting for
congenital pseudarthrosis of the tibia. Clin Orthop 2002;405:250-257. This
article reports good results with intramedullary rod fixation and bone
grafting, and suggests the indications and technical aspects of
intramedullary fixation.
is an excellent review of the commonly encountered angular and
torsional problems in early childhood and discusses presentation,
differential diagnosis, and recommended treatment.
large series documenting the natural history of Osgood-Schlatter
disease provides a valuable baseline for comparison. Results in
patients with or without immobilization were the same.
growth and development of 33 patients with congenital posteromedial
bowing of the tibia and fibula are documented with the demonstration of
progressive improvement and leg length discrepancy.
EJ, Barrett IR, Shapiro F. Growth disturbances following distal femoral
physeal fracture-separations. J Bone Joint Surg 1983;65A:885-893. This article demonstrates the high incidence of early growth plate disorders associated with this injury.
PD, Stanitski CL. Fractures and dislocations about the knee. In: Beaty
JH, Kasser JR, eds. Fractures in Children. Philadelphia: Lippincott
Williams & Wilkins 2001:981-1076. This
chapter clearly describes the pathophysiology of the
fractures/dislocations around the knee and suggests the treatment
guidelines.
LT, Corbett M, Wyss C et al. Lower-extremity rotational problems in
children: normal values to guide management. J Bone Joint Surg
1985;67A:39-47. This classic study of clinical
changes in the rotational profile of 500 subjects presents data on
individuals from infancy through the eighth decade. Graphs include
changes by age in foot progression angle, tibial version, and femoral
version, and provide mean ± 2 standard deviations for each parameter at each age.
article reviews potential causes of anterior knee pain in adolescents
(Osgood-Schlatter disease, Sinding-Larsen Johansson disease,
multipartite patellae, pathologic plica, and reflex sympathetic
dystrophy). The need for a search for a specific diagnosis in
idiopathic anterior knee pain is emphasized.
