Achilles Tendinitis
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Achilles Tendinitis
Achilles Tendinitis
Dennis E. Kramer MD
Description
-
Common overuse injury
-
Represents a spectrum of disorders involving the Achilles tendon, paratenon, and retrocalcaneal bursa
-
Ranges from painful inflammation of the Achilles tendon and its sheath to chronic degenerative tendinosis and tearing
-
Definitions:
-
Retrocalcaneal bursitis: Inflammation of the retrocalcaneal bursa, sparing tendon
-
Paratenonitis: Paratenon inflammation
-
Achilles tendinitis: Acute inflammation of the tendon with paratenon inflammation
-
Tendinosis: Intrasubstance degeneration of the tendon
-
-
Location: Noninsertional (several
centimeters above attachment to the calcaneus) versus insertional (at
insertion point on the posterior calcaneus)
General Prevention
-
Avoid excessive running uphill.
-
Avoid training errors, such as overly rapid increase in running mileage.
Epidemiology
-
Occurs particularly in recreational and competitive athletes, especially long-distance runners
-
Common in active middle-aged individuals
-
The Male:Female predominance approximately parallels the percentage of Male:Female participation in a given athletic activity.
-
Degenerative tendinosis also occurs in middle-aged to elderly individuals, regardless of sports participation.
Incidence
Occurs in 6% of runners (1)
Risk Factors
-
Large posterosuperior calcaneal tuberosity (Haglund process)
-
Microvascular disease: Diabetes, lupus, rheumatoid disease
-
Hemodialysis or peritoneal dialysis: Renal disease
-
Connective-tissue disease
Pathophysiology
-
Achilles tendon anatomy (2):
-
95% type-I collagen
-
Wavy configuration at rest
-
Surrounded throughout its length by a
thin gliding paratenon that functions as an elastic sleeve, permitting
free tendon movement -
Achilles tendon blood supply:
-
Intrinsic vascular system at the musculotendinous and osteotendinous junctions
-
Extrinsic vascular supply via paratenon
-
Zone of hypovascularity 2–6 cm proximal to tendon insertion
-
-
Paratenonitis/tendinitis: Chronic inflammatory changes (uncommon)
-
Tendinosis: Chronic mucoid degenerative changes with disorganization of collagen fibers (common)
-
Etiology
-
Training errors (60–80%): Sudden increase in training regimen (mileage), change in shoe wear or terrain (2,3)
-
Rough terrain or uneven surfaces
-
Improper shoe wear
-
Adverse weather conditions (ice, snow, cold)
-
Biomechanical abnormalities of the lower extremity, from lumbar spine to foot (2,3)
-
Hyperpronation
-
Cavus foot
-
Leg-length discrepancy
-
-
Chronically inappropriate, short, or absent warm-up and stretching period
Associated Conditions
Achilles tendon rupture
 |
|
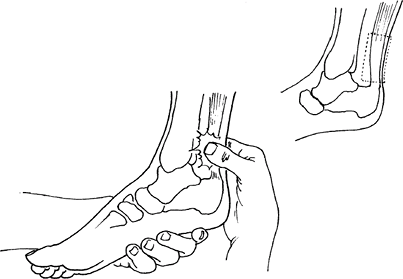
Fig. 1. The area of tenderness in Achilles tendinitis is above the heel, over a broad area.
|
Signs and Symptoms
-
A gradual increase in painful swelling
and warmth occurs at any point along the tendon substance, from the
musculotendinous junction to the bony insertion (os calcis). -
Most pain is 3–5 cm proximal to the insertion onto the calcaneus.
-
Microtrauma, such as continued running, or even gross trauma, such as a single leap (in jumpers), exacerbates the symptoms.
-
Pain is relieved somewhat by rest.
Physical Exam
-
Check for pain on dorsiflexion of the ankle.
-
Palpate the tendon to localize the pain.
-
In severe cases, the tendon sheath may be swollen and crepitant with ankle motion (Figs. 1 and 2).
-
-
Feel for nodular swelling in the tendon.
-
Use the Thompson test to rule out tendon rupture.
-
Swelling, warmth, or bogginess immediately anterior to the tendon insertion suggests retrocalcaneal bursitis.
-
Test single-limb heel rise.
-
Note any intrinsic foot, ankle, or leg deformities: Pes cavus, leg-length discrepancy, scoliosis, equinus deformity
Tests
Lab
-
Usually none are indicated.
-
Serum chemistry study with glucose is recommended if diabetes is suspected.
-
Evaluate for inflammatory arthritis if clinically indicated.
Imaging
-
Standing foot radiographs:
-
AP, lateral, oblique views
-
Assess Haglund prominence.
-
Identify:
-
Insertional spurring of the calcaneus
-
Intratendinous calcification, indicative of chronic tendinosis
 Fig. 2. Retrocalcaneal bursitis produces pain in the back of the heel, at the insertion of the Achilles tendon.
Fig. 2. Retrocalcaneal bursitis produces pain in the back of the heel, at the insertion of the Achilles tendon.
-
-
-
MRI is indicated if the clinical picture suggests tendinosis (4).
-
MRI of a normal Achilles tendon:
-
Homogenous low signal on all sequences
-
Flat or concave anterior margin
-
Crescentic shape
-
Ovoid shape at its insertion onto the calcaneus
-
Normal thickness <8 mm
-
-
MRI of acute paratenonitis:
-
Loss of sharp interface between tendon and pre-Achilles fat
-
On T2-weighted views, high signal intensity around the tendon and pre-Achilles fat
-
Low signal intensity within tendon itself
-
-
MRI of chronic Achilles tendinopathy:
-
Thickened >8 mm, enlarged tendon
-
Loss of normal concave margin anteriorly
-
On T1-weighted views, heterogeneous increased signal intensity within tendon
-
-
MRI of Achilles rupture:
-
Usually occurs 3–5 cm above calcaneal insertion
-
Partial rupture has focal areas of high
signal intensity on T2-weighted sequence images within the tendon
substance, with preservation of continuity of the tendon. -
Complete rupture shows loss of continuity with gap formation (high signal area on T2-weighted views).
-
-
-
Ultrasound:
-
Technique is technician-dependent.
-
Shows fluid around tendon or peritendinous adhesions
-
P.5
Differential Diagnosis
-
Precalcaneal bursitis
-
Retrocalcaneal bursitis
-
Peroneal tendinitis or rupture
-
Posterior tibialis tendinitis or rupture
-
Achilles tendon rupture, partial or complete, may represent terminal stage.
-
Inflammatory arthritis
General Measures
-
Early, acute phase:
-
NSAIDs, ice, rest, heel lift, foot-wear modification, and orthotic correction of the foot and leg abnormality
-
Modify activities; perform Achilles stretching.
-
Retrocalcaneal bursa injection also may help relieve symptoms and inflammation.
-
For patients unresponsive to the previously-listed treatments, a trial of cast or boot immobilization is appropriate.
-
Corticosteroid injection of the tendon sheath may precipitate rupture and should be avoided.
-
Special Therapy
Physical Therapy
-
Ultrasound therapy (during proliferative
phase healing), phonophoresis, iontophoresis, and short-term heel wedge
use (to unload tendon unit) -
Eventually, flexibility, strengthening, and conditioning through eccentric exercise to gain maximal benefit
Medication
First Line
-
NSAIDs
-
Analgesics
Surgery
-
For patients for whom nonoperative treatment for 3–6 months has failed:
-
Paratenonitis:
-
Treatment involves removal or release of the paratenon through a straight medial incision.
-
-
Achilles tendinosis:
-
Requires intratendinous débridement, retrocalcaneal bursectomy, and Haglund exostectomy (5,6)
-
May require augmentation or local tendon
transfer (e.g., plantaris or flexor hallucis longus) if Achilles tendon
has extensive disease (7)
-
-
Prognosis
The prognosis is good, but recovery can be prolonged.
Complications
Tendon degeneration and eventual rupture with loss of function, particularly with a high rate of surgical failure, are possible.
Patient Monitoring
Routine follow-up is indicated until the symptoms have resolved.
References
1. Clement DB, Taunton JE, Smart GW. Achilles tendinitis and peritendinitis: etiology and treatment. Am J Sports Med 1984;12:179–184.
2. Paavola M, Kannus P, Jarvinen TAH, et al. Achilles tendinopathy. J Bone Joint Surg 2002;84A: 2062–2076.
3. Schepsis AA, Jones H, Haas AL. Achilles tendon disorders in athletes. Am J Sports Med 2002;30:287–305.
4. Recht MP, Donley BG. Magnetic Resonance Imaging of the foot and ankle. J Am Acad Orthop Surg 2001;9:187–199.
5. McGarvey
WC, Palumbo RC, Baxter DE, et al. Insertional Achilles tendinosis:
surgical treatment through a central tendon splitting approach. Foot Ankle Int 2002;23:19–25.
WC, Palumbo RC, Baxter DE, et al. Insertional Achilles tendinosis:
surgical treatment through a central tendon splitting approach. Foot Ankle Int 2002;23:19–25.
6. Watson
AD, Anderson RB, Davis WH. Comparison of results of retrocalcaneal
decompression for retrocalcaneal bursitis and insertional Achilles
tendinosis with calcific spur. Foot Ankle Int 2000;21:638–642.
AD, Anderson RB, Davis WH. Comparison of results of retrocalcaneal
decompression for retrocalcaneal bursitis and insertional Achilles
tendinosis with calcific spur. Foot Ankle Int 2000;21:638–642.
7. Martin
RL, Manning CM, Carcia CR, et al. An outcome study of chronic Achilles
tendinosis after excision of the Achilles tendon and flexor hallucis
longus tendon transfer. Foot Ankle Int 2005;26:691–697.
RL, Manning CM, Carcia CR, et al. An outcome study of chronic Achilles
tendinosis after excision of the Achilles tendon and flexor hallucis
longus tendon transfer. Foot Ankle Int 2005;26:691–697.
Additional Reading
Clain MR, Baxter DE. Achilles tendinitis. Foot Ankle 1992;13:482–487.
Saltzman CL, Tearse DS. Achilles tendon injuries. J Am Acad Orthop Surg 1998;6:316–325.
Codes
ICD9-CM
-
726.71 Achilles tendinitis
-
727.82 Calcium deposits in tendon and bursa
Patient Teaching
Activity
Proper shoe wear and terrain adjustment, with avoidance of steep hills and stairs
Prevention
Adequate pretraining stretching and warm-up
FAQ
Q: What is the most common location for Achilles tendinosis?
A: In the zone of avascularity, 2–6 cm proximal to the tendon’s insertion onto the calcaneus.
Q: How long should nonoperative treatment be attempted for Achilles tendinosis before proceeding with surgery?
A: At least 6 months of nonoperative treatment are recommended before surgical treatment.
Q: What are the MRI findings in Achilles tendinopathy?
A:
On T1-weighted MRI images, a thickened (>8 mm) Achilles tendon with
loss of normal concave anterior margin and increased signal intensity
within the tendon.
On T1-weighted MRI images, a thickened (>8 mm) Achilles tendon with
loss of normal concave anterior margin and increased signal intensity
within the tendon.
