Periprosthetic Fractures
frequency. This is due, in part, to the increasing number of primary
and revision arthroplasties performed annually and also to the
increasing age and fragility of patients with such implants. All types
of periprosthetic fractures can present unique and substantial
treatment challenges. In each situation, the presence of an
arthroplasty component either obviates the use of, or increases the
difficulty of, standard fixation techniques. Additionally, these
fractures often occur in elderly patients with osteoporotic bone,
making stable fixation even more problematic.
fractures, regardless of location, is evidenced by the array of
treatment options described in the literature without a clear consensus
emerging on the most appropriate method.73,84,125,126,127
Most recently, treatment of the most common periprosthetic fractures,
those of the femoral shaft and the femoral supracondylar region, has
focused on open reduction with internal fixation (ORIF) or revision
arthroplasty procedures with or without supplementary autologous or
allogeneic bone grafting.22,54,121
Successful application of these strategies can be extrapolated to other
locations but must also consider the fracture location relative to the
arthroplasty component, the implant stability, the quality of the
surrounding bone, and the medical and functional status of the patient.34
patients with periprosthetic fractures of both the upper and lower
extremity.42,78,89,126
Lower extremity fractures tend to occur postoperatively and a
relatively larger proportion of upper extremity periprosthetic
fractures, especially those about humeral shoulder arthroplasty stems,
occur intraoperatively. Postoperative low-energy falls account for
greater than 75% of all periprosthetic femur fractures from the Swedish
registry database,89 whereas a majority, up to 76% of humeral fractures, have been reported to occur intraoperatively.19,148
Spontaneous fracture has been noted to be more common after revision
arthroplasty than after primary arthroplasty. This is likely due to the
reduced bone stock often present after revision.89
High-energy trauma accounts for only a small percentage of
periprosthetic fractures and these types are usually associated with a
more comminuted fracture pattern than seen with low-energy fractures.6
Intraoperative fractures of both the upper and lower extremities occur
more commonly during revision procedures and with implantation of large
noncemented stems.102,132 The risk increases when there is mismatch of the shape of long prosthetic stems and the shape of the bone.178
Given the predominance of low-energy injury mechanisms, associated
injuries are relatively uncommon. Of course, vigilance is required to
avoid missing the occasional associated injury.
periprosthetic fractures, the history should include a detailed account
of the status of the arthroplasty, including as much detail as possible
on the date of implantation, the specific prosthesis used, the index
diagnosis for implantation, and the relevant history related to the
associated arthroplasty. Additional secondary procedures should be
carefully cataloged as well as other complications, such as prior
infection. The baseline functional status specific to the involved
joint as well as to the patient as a whole, such as handedness,
occupation, ambulatory status, and any need for assist devices, are a
standard part of the history. The time course of any recent change in
status or symptoms related to the arthroplasty can be a clue to
heighten suspicion of a subtle periprosthetic fracture or prefracture
implant loosening.
with specific attention to prior surgical wounds about the joint in
question; the presence or absence of associated lesions, such as venous
stasis or diabetic ulcers of the ipsilateral or contralateral limbs;
limb length evaluation; as well as strength and neurologic evaluation.
Obviously, in cases of displaced fracture, many of these parameters
will be abnormal and not represent the patient’s baseline status.
However, it is still important to obtain a comprehensive history, as
clues to potential etiologic factors to the acute fracture such as
implant loosening, osteolysis, and infection may need to be addressed
during the course of fracture repair.
when the fracture happens intraoperatively. A pitch change during
malleting a trial or final prosthesis alerts the surgeon to the
possibility of fracture and should prompt an appropriate investigation
starting with direct observation. Similarly, an abrupt easing
of insertion resistance can be a subtle sign of fracture or perforation.
fracture, rather than an intraoperative fracture, is usually obvious.
The patient typically has an abrupt onset of pain and deformity
associated with trauma. However, more subtle fractures can occur,
especially when associated with significant osteopenia or osteolysis.
In these cases, a clinical suspicion is necessary to instigate a
specific radiographic evaluation to rule out fracture. The standard
radiographic evaluation should include plain radiographic
anteroposterior (AP) and lateral views to include the joint in question
and full-length radiographs of the bones above and below the joint.
Attention should be paid not only to fracture specifics but also to an
evaluation of the prosthesis relative to the fracture, as well as the
prosthesis relative to the native bone to which it is secured. It is
useful to assess for prosthetic loosening, presence of osteolysis, and
prosthetic and limb alignment. Prefracture radiographs, when available,
can provide insight to the time course of any existing or impending
prosthetic failure, specifically osteolysis, progression of cortical
erosions, and presence of any cortical penetrations or notching.
observation or indirectly based on suspicion from auditory changes in
the pitch of sounds coming from mallet blows of a broach or implant. In
such circumstances, intraoperative radiographs should be obtained to
define the extent of the fracture, which can be more extensive than
seen under direct vision.
evaluate periprosthetic fractures. However, significant advances have
been made to reduce metal artifact of both computed tomography scans
and magnetic resonance imaging scans, which may help in evaluating
subtle fractures or in evaluation of available bone stock for fracture
repair.109,111,166
fracture care are no different than the goals of treatment of any other
periarticular fracture. These goals include timely and uncomplicated
fracture union, restoration of alignment, and return to preinjury level
of pain and function. By definition, periprosthetic fractures are not
associated with normal joints. Therefore, baseline painless normal
joint function and normal anatomic alignment cannot be assumed nor can
return to normal function be the defacto goal. Instead, an accurate
history of prefracture function should be elicited to help guide goals
and prognosis. In the setting of a poorly functioning loose prosthesis,
return of the patient to a better functional level after fracture
fixation and revision arthroplasty may be a reasonable goal. If
prefracture malalignment existed, a careful determination must be made
whether restoring baseline alignment or normal alignment should be the
goal. This decision is often predicated on the alignment of the
prosthesis relative to the bone on the nonfractured side of the joint,
which may provide an inherent compensatory alignment. A unique
consideration when treating periprosthetic rather than native
periarticular fractures is consideration of prosthesis stability and
the potential need for future revision arthroplasty. The additional
goal here is to assure stability of the prosthesis and restoration of
adequate bone stock to maximize the potential success of any such
subsequent procedures.
frequency due to the increasing number of patients with hip
arthroplasties. The incidence of periprosthetic femur fracture after
primary hip arthroplasty has been generally considered to be less than
1%68,84 but has been reported to be as high as 2.3%.7,43,46,84
A recent survivorship analysis on 6458 primary cemented femoral hip
prostheses revealed a fracture incidence of 0.8% at 5 years and 3.5% at
10 years.26 After revision arthroplasty, the incidence climbs to between 1.5% and 7.8%.7,68,84,105 The risk further increases after an increasing number of revision surgeries.42 The lapsed time period from an index primary hip arthroplasty to periprosthetic femur fracture averages 6.3 to 7.4 years26,89 and is reduced to an interval of 2.3 years after a third revision procedure.89
about hip arthroplasty femoral stems are related to the age of the
patient, gender, index diagnosis, presence or absence of osteolysis,
presence or absence of aseptic loosening, primary or revision status,
the specific type of implant, and whether cemented or noncemented
technique was utilized. Identifying risk factors can both improve
patient counseling and potentially improve efforts at fracture
prevention. Furthermore, patients with periprosthetic femur fractures
have increased mortality.42 In a recent series, 11% of patients with periprosthetic fractures died within 1 year following surgical treatment.9
This mortality rate approached that of hip fracture patients (16.5%)
treated during the same time period and was significantly lower than
the mortality of patients undergoing primary joint replacement (2.9%).
periprosthetic femur fracture, is not clearly an independent risk
factor. Coexisting medical comorbidities such as osteoporosis,174 increased activity level,138
and fall risk also contribute. Furthermore, the number of years after
arthroplasty must be considered as each year after arthroplasty has
been associated with a 1.01 additional risk ratio per year.42
fractures among female patients (52% to 70%) has been reported in many
series,6,8,65,167
associated osteoporosis and a higher percentage of procedures being
performed in female patients makes gender less clear as an independent
risk factor. Accordingly, reports that account for such biases report
no increased,88,139 or even reduced, risk for females.42
rheumatoid arthritis and arthroplasty for hip fracture each being
identified as having increased risk ratios.42,139 Rheumatoid arthritis (RA) having an increased ratio of 1.56 to 2.142,139 and hip fracture having a reported risk ratio of 4.4.139
stem, represents an impending pathologic fracture, a growing problem in
arthroplasty, and a complex reconstructive problem. Fracture, deficient
bone stock, a loose implant, and an inciting particle generator may
each need to be addressed during fracture repair and reconstruction.
is most often associated with a loose prosthesis, with some data
indicating that the presence of a loose stem represents a risk factor
for subsequent fracture63,160 and other data showing no such association.89,157
associated risk factors. During primary total hip or hemiarthroplasty,
implantation of a cementless femoral component presents a reported 3%
to 5.4% risk of intraoperative fracture compared to 0% to 1.2% for a
cemented stem.7,41,143,154 Impaction grafting for revision of a femoral hip component carries up to a 22.4% perioperative risk for fracture.37,102,132
Most of these fractures, many incidental perforations, have been found
to occur with cement removal rather than the reconstructive procedure.37 Revision with large porus-coated diaphyseal stems has been reported to be associated with a nearly 30% risk,100
and long straight revision stems have an intermediate reported fracture
occurrence of 18% with an additional 55% of cases thought to be at
increased potential subsequent risk due to impingement of the distal
stem tip on the anterior femoral cortex.178
communication about and treatment of periprosthetic femoral shaft
fractures about hip arthroplasty stems.34
Its reliability and validity has been confirmed and therefore it
represents the current standard for assessing and reporting these
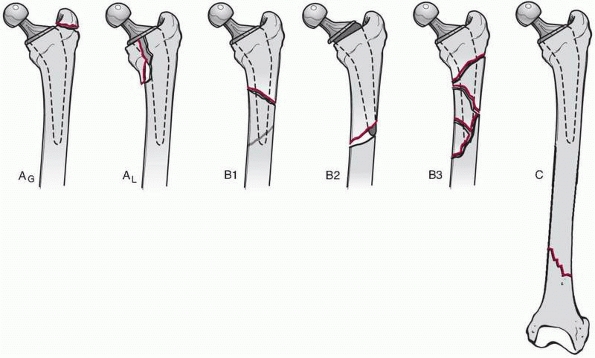
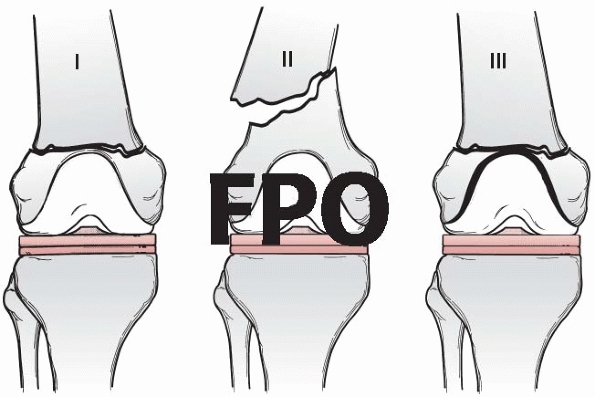
fractures.14,34 It considers the location of the fracture relative to the stem, the stability of the implant, and associated bone loss (Fig. 21-1).
Type A fractures are in the trochanteric region, type B fractures
involve the tip of the stem, and type C fractures are distant to the
tip of the stem such that their treatment is considered independent of
the hip prosthesis. Type A fractures are subdivided into fractures of
the greater trochanter, AG, which are frequently associated with osteolysis and remain stable, and those about the lesser trochanter, AL,
which are more likely to be associated with eventual implant loosening.
Type B fractures are also further subdivided: B1 fractures are
associated with a stable implant, B2 fractures are associated with an
unstable implant, and B3 fractures are associated with bone loss and
usually also a loose implant (Table 21-1).
 |
|
FIGURE 21-1
The Vancouver classification for periprosthetic fractures about femoral hip arthroplasty stems. Type B fractures are subdivided based on presence of a well fixed stem (Type B1), a loose stem (Type B2), or poor bone stock in the proximal fragment (Type B3). |
describe postoperative fractures, but has been expanded to address
intraoperative periprosthetic fractures.96
Similar to the original, the intraoperative Vancouver classification
divides fractures into three zones: type A being of the proximal
metaphysis without extension to the diaphysis, type B are diaphyseal
about the tip of the stem, and type C fractures extend beyond the
longest revision stem and include fractures of the distal metaphysis.
The subclassification of each type distinguishes the intraoperative
from the postoperative classification and reflects fracture stability:
subtype 1 represents a simple cortical perforation, subtype 2 is a
nondisplaced linear cortical crack, and subtype 3 is a displaced or
otherwise unstable fracture (Table 21-2). The
treatment options for fractures occurring intraoperatively varies
somewhat based on when the fracture was detected. Intraoperative
identification, in general, leads to more surgical interventions than
identification in the recovery room or later (see Table 21-2).
|
TABLE 21-1 Vancouver Postoperative Classification Scheme and Treatment Options
|
|||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||
are stable. They are usually non- or minimally displaced and are
stabilized by the opposite pull and continuity of the soft tissue
sleeve connecting the abductors and the vastus lateralis.162
Such stable fractures, when occurring postoperatively, can be managed
nonoperatively with symptomatic treatment. Weight bearing to tolerance
is generally allowed. Intraoperative stable fractures of the greater
trochanter can be managed similarly, especially when recognized after
wound closure. When recognized intraoperatively, internal fixation may
be considered. Widely displaced, or otherwise unstable, fractures of
the greater trochanter, especially when associated with substantial
pain, weakness, or limp, are generally treated operatively with ORIF,
typically with a claw plate that engages the soft tissue attachment of
the gluteus medius as well as the bone of the greater trochanter.
Results with these modern plates represent an improvement over earlier
wiring techniques.89,90
Distal fixation of these claw plates is with cables around the zone of
the femoral stem. There is usually no requirement to extend the plate
beyond the tip of the femoral prosthesis. However, very short plates
have been associated with fixation failure.90
Of course, the stability of the arthroplasty components are considered
and when loose they are revised. When these fractures are associated
with substantial osteolysis, bone grafting is indicated with care to
maintain the soft tissue stabilizers.162 There is very little in the way of published modern series of acute Vancouver Type AG
fractures to guide treatment and establish expected outcomes. Much of
the available information includes or is exclusively related to
treatment of greater trochanteric osteotomies or nonunions.52,87,89,90 In a recent series of 31 cases of claw plate fixation of the greater trochanter, only 8 were for acute fracture.90
Results for these patients were not distinguished. Overall, union
occurred in 28 of 31 patients with 3 having fibrous union of the
trochanter. Other complications included painful bursitis requiring
plate removal in 3 patients and deep infection in one. In the setting
of greater trochanteric nonunion, adjunctive vertically oriented wires
have resulted in better osseous contact and union.166
|
TABLE 21-2 Vancouver Intraoperative Classification Scheme and Treatment Options
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
shaft fractures is evidenced by the array of treatment options
described without a clear consensus emerging on the most appropriate
method.73,84
Most recently, treatment of these femur fractures has focused on ORIF
or revision arthroplasty procedures with or without supplementary
autologous or allogeneic bone grafting.22,54,121
Successful application of these techniques must consider the fracture
location relative to the femoral component, the implant stability, the
quality of the surrounding bone, and the medical and functional status
of the patient.34 In the context of
femoral shaft fractures about well-fixed implants (Vancouver Type B1
fractures), stabilization using ORIF techniques with plates and screws
or cortical onlay allografts or a combination of both has been
advocated.13,53,157,170
Newer indirect fracture reduction techniques have favorable biologic
features that minimize soft tissue disruption, preserve the vascular
supply to bone, enhance healing, and decrease the incidence of nonunion
for many fractures,61 often obviating the need for supplemental bone grafting.124
There is little role for revision arthroplasty for B1 fractures given
the stable prosthesis. Types B2 and B3 fractures are amendable to
femoral component revision with or without adjuvant plate and/or
allograft strut fixation.
 |
|
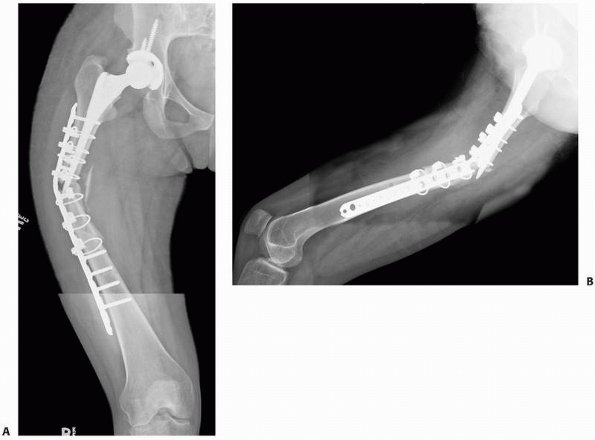
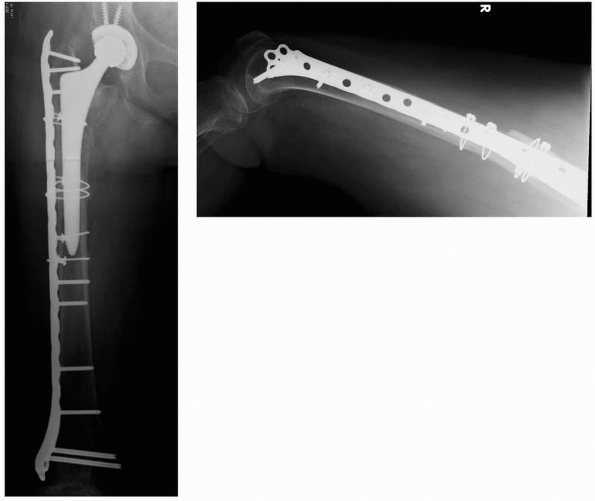
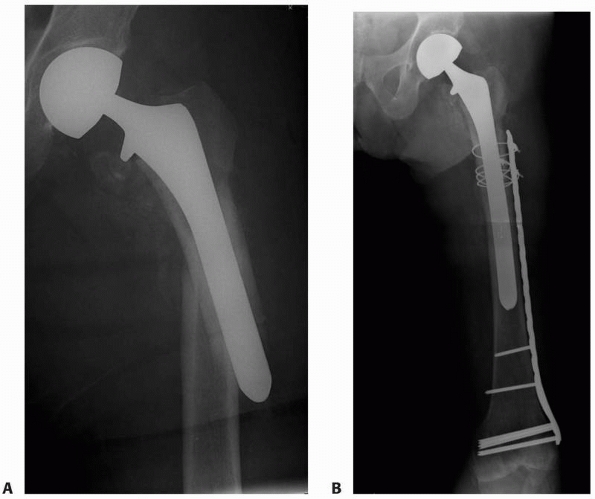
FIGURE 21-2 A,B:
High failure rates have been associated with lateral plate fixation when older direct, nonbiologically friendly reduction techniques are utilized. |
screw fixation for periprosthetic femoral shaft fractures using older
direct reduction techniques have been varied.17,28,40,47,101,103,104,152,157,164,180
Failure of traditional cable-plate constructs with cable fixation in
zone of intramedullary implant and nonlocked screws distally is likely
related, at least in part, to older direct reduction techniques and not
necessarily to the construct being inappropriate (Fig. 21-2).
Soft tissue stripping associated with direct reduction can delay
healing, which eventually manifests as implant failure. The addition of
strut grafts 90 degrees to a lateral plate offers prolonged construct
stability and improved results when these older direct reduction
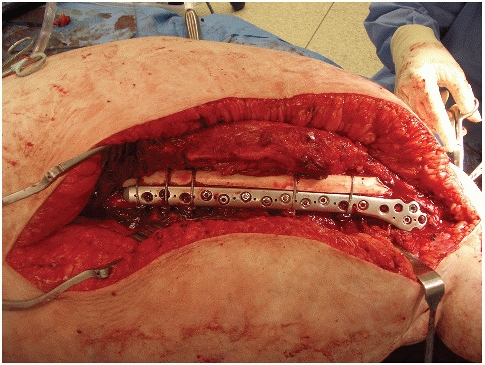
techniques are utilized (Fig. 21-3). In a
report on 40 patients, Haddad et al. concluded that cortical allografts
should be used routinely to augment fixation and healing of
periprosthetic femoral fracture around well fixed implants.53
Treatment methods varied in this study and included either cortical
onlay strut allograft alone, a plate and one cortical strut, or a plate
and two struts. The nonstandardized use of adjuvant bone grafting
materials in this study further increased the heterogeneity of the
treatment methods: 8 patients received autograft, 29 received
morselized allograft and 15 received demineralized bone matrix. Based
on 100% healing, it
is
logical to conclude that the use of strut allografts plus adjuvant bone
graft and/or lateral plate fixation can achieve good results. However,
it may be overstated to conclude from this study that allograft is a
requirement for treatment of Vancouver B1 fractures. Newer biologic
plating techniques that maximally preserve the soft tissue attachments
about a fracture have been shown to be successful without adjuvant bone
grafting for fractures in other anatomic areas that traditionally were
treated with adjuvant bone grafts.
 |
|
FIGURE 21-3 An intraoperative clinical photograph showing lateral plate fixation augmented with an anterior femoral strut allograft.
|
to apply these methods to Vancouver Type B1 periprosthetic femoral
shaft fractures.2,124
Indirect fracture reduction and a single, laterally applied plate
without the use of structural allograft nor any other substitute was
uniformly utilized in the series of Ricci et al.124
Union occurred after the index procedure in all of the 41 patients who
lived beyond the perioperative period. The average time required for
healing was relatively short, 11 weeks, and was very homogenous with
the standard deviation being only ± 4 weeks. All patients healed in
satisfactory alignment (less than 5 degrees of malalignment). Although
minor implant related complications, such as cable fracture, occurred
in 3 patients, this did not appear to complicate the healing process.
Each of these three fractures healed at between 10 and 12 weeks in
satisfactory alignment and without the need for further operation. Care
in preserving the soft tissue envelope around the fracture was
attributed to the consistent healing. These results compare favorably
to treatment of similar fractures using cortical onlay grafts alone,21,22,53,170 where nonunion requiring revision surgery has been reported in 8% to 10% of cases21,22,170 and where angular malunion has been reported to occur in 5% to 10% of cases.21,53
The reason for the higher malunion rate seen when allograft strut
fixation is used alone may be because these struts cannot be bent or
contoured as can plates. Fracture alignment, therefore, cannot be
adjusted with struts as precisely as with the use of plates.
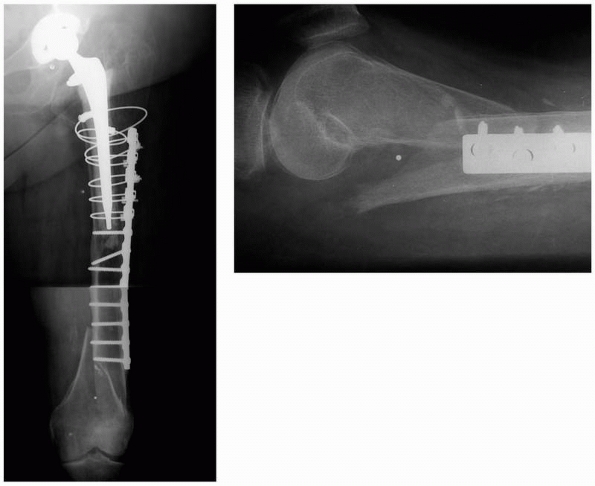
characteristics of various plate constructs used for Vancouver Type B
fractures.16,32,33,45,153,179 The Ogden type construct (Fig. 21-4),
cables proximally and standard nonlocked screws distally, is the
typical control construct. Prior to the advent of locking plates,
cortical allograft struts either in place of or in addition to the
Ogden concept were the focus of testing.32,33 More recently, proximal unicortical locking screws either in lieu of or in addition to cables have been investigated.45,153,179
In each of these studies, the stiffness of various experimental
constructs was greater than the Ogden construct, but the fatigue
characteristics were not investigated in the majority of studies,
limiting the clinical applicability of these investigations.32,33,45,179
The recent clinical series utilizing modern biologic plating techniques
have shown good results with slight modification of the Ogden
construct: addition of unicortical locked screws in the proximal
segment to augment (but not replace) cables, or bicortical locked
screws in the distal segment to augment nonlocked screws in the
presence of osteoporotic bone (Fig. 21-5).2,124
Unicortical locked screws alone, without cables; have not been shown to
provide adequate fixation for these fractures. This is primarily due to
the poor rotational stability of such short unicortical screws.
Therefore, locked screws should be used as an adjuvant but not as a
substitute for cable fixation in the zone of the hip prosthesis. Any
long-term detrimental effect of unicortical screws inserted into a
cement mantle remains unknown.
 |
|
FIGURE 21-4 AP view of the traditional Ogden type construct with cable fixation proximally and nonlocked screw fixation distally.
|
Minimum plate length is to obtain satisfactory distal fixation, usually
at least six plate holes with near and far holes to the fracture filled
with four or more screws. Locked screws should be considered when
osteoporotic bone is present. Longer plates that extend to the lateral
femoral condyle have recently been advocated to protect the entire
femur (see Fig. 21-5) and reduce risk of subsequent peri-implant fracture at the distal margin of the plate (Fig. 21-6).126
This strategy is at the expense of a likely increased risk of
plate-related pain over the subcutaneously located condylar extent of
the plate.
femoral shaft fractures is probably less important than the technique
utilized for its implantation. A number of designs that employ various
mechanisms for attachment of cables through or around the plate are
available (Fig. 21-7). However, good results have been achieved with standard plates.2,53,124,125
A plate that is bowed in the sagittal plane to match the anterior
femoral bow makes sense to assist in obtaining an anatomic reduction in
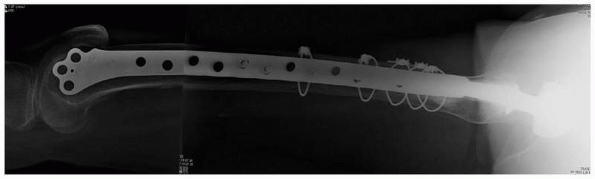
this plane (Fig. 21-8).
 |
|
FIGURE 21-5
AP view of a modern modification of the Ogden construct with a long distal femoral plate to protect the entire femur and with locked screws to augment fixation. |
 |
|
FIGURE 21-6
A Vancouver Type B femur fracture treated successfully with a lateral plate until fracture occurred at the distal tip of the plate. Constructs that span the entire femur (see Figure 21-5) avoid such complications. |
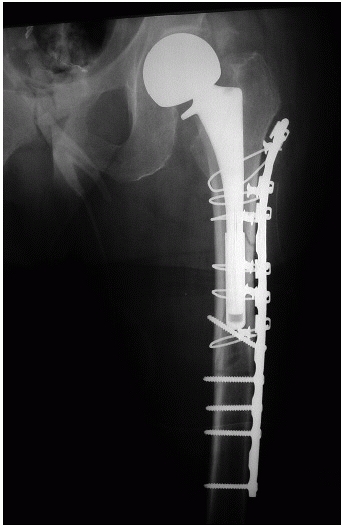
implant (Vancouver Types B2 and B3), revision of the femoral component
is typically recommended (Fig. 21-9). This strategy addresses
both the loose component and the fracture and provides intramedullary
stability by virtue of long femoral stems used for revision. Fracture
fixation with a lateral plate or reconstitution of bone stock with
allograft strut or sometimes a combination of both plates and struts
are utilized in addition to femoral component revision. In more severe
cases of bone loss, an allograft prosthesis composite, impaction bone
grafting technique, or proximal femoral replacement may be considered.80,106
The overall functional outcome based on the Oxford hip score for
revision arthroplasty in the setting of periprosthetic fracture have
been found, in a large comparative analysis (n = 232 revisions for
fracture), to be worse than when revision is for aseptic loosening.175
Further, this study demonstrated an eight-fold higher mortality rate
(7.3%) seen in the periprosthetic fracture patients. This data is
consistent with the high mortality rates (11%) seen in patients treated
with ORIF for periprosthetic femur fractures153 and together paint a sobering picture of the seriousness of these injuries.
 |
|
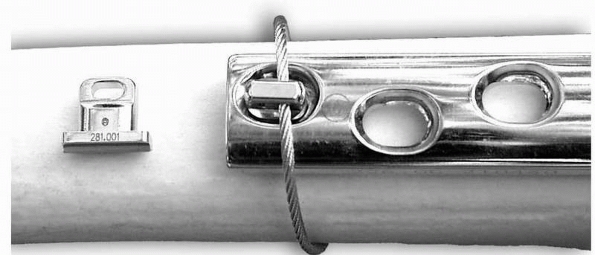
FIGURE 21-7
Grommet for stabilization of a cable about a plate. The grommets theoretically prevent slippage of the cable along the plate and reduce fretting of the cable. |
to effectively handle these challenging cases. In addition to the
aforementioned radiographic evaluation of the fracture and femoral stem
stability, quality orthogonal radiographs are also mandatory to
evaluate the fixation status of the acetabular component and remaining
acetabular and femoral bone stock. If possible, the operative note from
the original arthroplasty should be obtained to determine the
manufacturer of the components, so that new acetabular liners, if
needed, can be available. The presence of prefracture hip symptoms,
such as thigh or groin pain, can alert the surgeon to potential
component loosening, if the radiographs are equivocal. Serologies such
as sedimentation rate and C-reactive protein are of unknown benefit in
the presence of an acute fracture. If there is any concern for
infection, a preoperative hip aspiration should be considered.
quality of the remaining bone stock, the diameter of the femoral canal
distal to the fracture, and patient factors such as age and baseline
functional status. Through the fracture, cement and cement restrictors
can be removed. If necessary, the proximal fracture fragment can be
split coronally to allow excellent access for stem removal and direct
visualization of the distal canal to allow accurate reaming.149
The acetabular component is typically exposed after the femoral
component is removed. The liner is removed if modular, and the
acetabular component is manually tested for stability. If it is loose,
acetabular revision is performed. If it is well fixed, the liner is
typically exchanged, and the head size increased, if possible, to allow
improved hip stability.
 |
|
FIGURE 21-8 Fixation of midshaft femur fractures with a bowed plate helps preserve anatomic alignment in the sagittal plane.
|
rely on obtaining secure distal fixation. Only rarely is cemented long
stem revision considered. This can be useful in very osteopenic bone
with capacious canals.67 If the
fracture is anatomically reduced and fixed with cerclage cables and if
the cement is not vigorously pressurized, cement extravasation will not
typically occur. After cementation, intraoperative radiographs are
recommended to determine if any problematic cement extravasation has
occurred. It should be emphasized that cemented reconstructions are
rarely useful in the setting of periprosthetic fractures. The most
effective strategies include noncemented distal fixation techniques.
selection of the appropriate uncemented reconstruction. These include
the endosteal diameter and morphology of the distal fragment. If the
distal fragment demonstrates parallel endosteal cortices with 5 cm or
more of tubular diaphysis (usually with a diameter of less than 18 mm),
then extensively coated uncemented long stem prosthesis with or without
lateral plate augmentation is appropriate (see Fig. 21-9).
The distal canal is reamed and a trial stem is potted into the distal
fragment. The proximal fragments can then be reduced using the trial
implant as a template. Cerclage cables are applied, and a trial
reduction is performed. Once leg length and stability are acceptable,
the trial is removed and the femoral component is impacted. The
cerclage cables are then retensioned, crimped, and cut. The appropriate
femoral head length is selected, and the reconstruction completed.
These types of stems have demonstrated excellent long-term survivorship
in the revision setting and for periprosthetic fracture situations.73,84,107,110
Union occurs reliably and functional outcome is, as expected for
complex revision arthroplasty, modest. At a mean follow-up of 10.8
years, 17 of 22 patients treated with an extensively porous-coated
implant had a satisfactory functional result with delayed union
occurring in only 1.110 Concomitant
acetabular revision was required in 19 patients. Another similarly
treated group of 24 patients had an average Harris hip score of 69 with
91% of fractures uniting uneventfully.107
morphology, or large diameters (typically over 18 mm), fluted titanium
tapered modular stems can be used effectively. These stems are
commercially available in diameters up to 30 millimeters and can be
useful in capacious canals. Reaming under fluoroscopic
control
and “by hand,” especially in osteopenic bone, can help to avoid
anterior femoral cortical perforation. When axial stability is obtained
by diaphyseal reaming, the implant is impacted into place. It is wise
to place a prophylactic cable at the mouth of the distal fragment prior
to stem impaction. The proximal bodies of the modular implants are then
chosen to restore appropriate leg length, offset, and hip stability.
After trialing, the components are assembled and the hip reduced. The
proximal fragments are then reduced and cerclaged around the body of
the implant. The authors find this strategy effective for Vancouver
type B2 and even some B3 fractures; however, concerns remain about the
durability of the modular junction of such stems without proximal bony
support.
 |
|
FIGURE 21-9 Treatment of a periprosthetic femoral shaft fracture (A) with a porus-coated long stem prosthesis with an adjunctive lateral plate that spanned the entire remaining femur (B).
|
is appropriate. The former two methods are typically used in very
osteopenic bone; therefore, cemented distal fixation is recommended.
Preserving a sleeve of remaining proximal bone, albeit deficient,
provides some soft tissue attachment and assists in maintaining a
stable hip. A coronal split (Wagner type) of the proximal bone can
facilitate stem removal. The new implant is cemented into the distal
fragment, and then the proximal sleeve of remaining bone and soft
tissue can be cerclaged around the body of the proximal femoral
replacing prosthesis or the proximal femoral allograft/revision stem
composite with cable or heavy braided suture (Fig. 21-10).
Results of these extreme revision scenarios are not as good as seen
with the less complex revisions associated with type B1 fractures.
Patients should be counseled that neither bone healing nor function are
predictably good, but that both can be satisfactory. Twenty-three of 24
patients treated with such an allograft/implant composite for Vancouver
type B3 fractures were able to walk, but 15 required a walker.70,97
Osseous union of the allograft to host femur occurred in 80% and union
of the greater trochanter occurred in 68%. At a mean follow-up of 5.1
years, 16% had required a repeat revision. In a series of 21 similar
fractures treated with a proximal femoral replacement and followed for
3.2 years, all but one was able to walk.72
Despite a relatively high complication rate (2 wound drainage problems,
2 dislocations, 1 refracture distal to the femoral stem, 1 acetabular
cage failure), the authors concluded this was a viable option for
patients with a severe problem. When impaction grafting technique is
chosen, better results have been demonstrated with use of a long stem
femoral component that bypasses the fracture then with a short stem.161
It is important to note that if the abductors are deficient, any of
these constructs should include a constrained acetabular liner to
minimize the risk of postoperative dislocation. If the acetabular
component is of sufficient diameter and a compatible constrained liner
is not available, some surgeons have recommended cementing a
constrained liner into a well-fixed acetabular component. Good
containment of the locked liner by the acetabular component is
required, and cup position should be acceptable. Contouring the
backside of the liner to be cemented is recommended (if it is smooth)
to allow cement interdigitation.
It has been inferred that fixation of these fractures is independent of
the femoral prosthesis. This, however, is an oversimplification of the
typical situation. Distal shaft fractures in the absence of a hip
prosthesis are typically treated with intramedullary nails (either
antegrade or retrograde), and supracondylar or intercondylar fractures
are treated with either a lateral plate or retrograde nail. Vancouver
type C fractures, by virtue of the femoral stem, obviate standard nail
treatment options, and attempts to insert retrograde nails in this
short segment are ill-advised due to inadequate fixation within the
proximal fragment (Fig. 21-11). Ending the plate at (Fig. 21-12)
or just distal to the femoral stem should also be avoided to minimize
the stress rise effect. Additional principles and results of treating
these distal femoral shaft and metaphyseal fractures are presented in Chapters 50 and 51.
 |
|
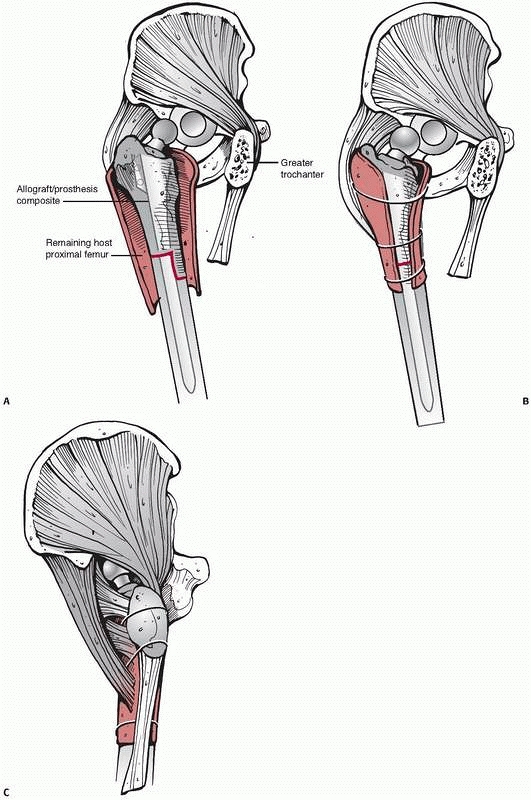
FIGURE 21-10 Proximal femoral allograft/revision stem composite for treatment of Vancouver type B3 periprosthetic femur fractures. A. The allograft/prosthesis composite is inserted into the native host distal femoral segment. B.
Any remaining proximal sleeves of host bone with soft tissue attachments are secured to the allograft and across the allografthost junction. C. The greater trochanter is separately attached to the allograft. |
 |
|
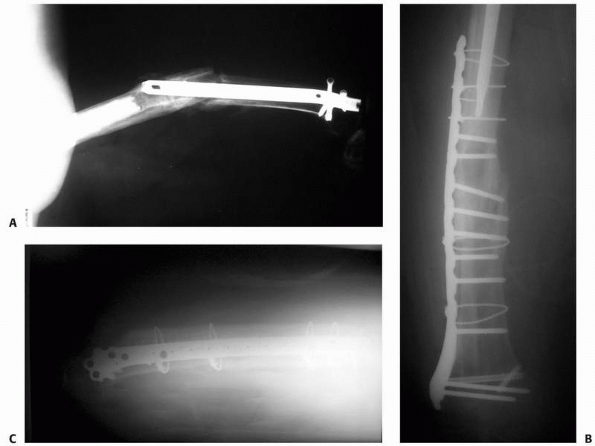
FIGURE 21-11 A.
Ill-advised treatment of a Vancouver type C femur fracture distal to a hip arthroplasty stem. The nail eroded through the anterior cortex and the fracture developed nonunion. This was treated with nail removal, ORIF with a lateral plate, autologus bone graft to stimulate nonunion healing, and an anterior strut graft to restore bone stock (B,C). |
 |
|
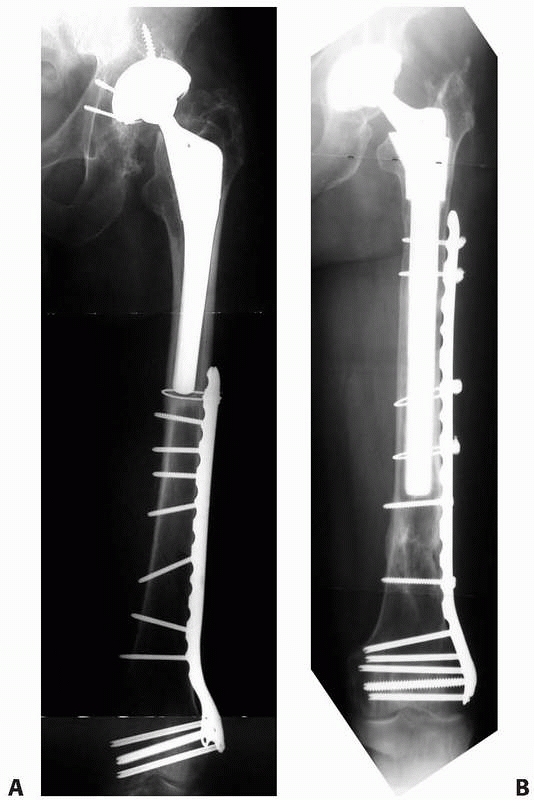
FIGURE 21-12 A.
Ill-advised treatment of a Vancouver type C fracture with a plate that is too short because it creates an unnecessary additional stress riser at the tip of the arthroplasty stem. B. More optimal plate constructs span the entire unprotected zone of the femur. |
fractures are generally treated nonoperatively with a limited period of
protected weight bearing. Assist devices are encouraged to preserve
mobility and balance and to help avoid subsequent falls. When fractures
of the medical calcar are noted intraoperatively, radiographs are
obtained to delineate the extent of fracture, as occasionally these
splits can spiral down toward the stem tip. Limited, nondisplaced
medial cracks noted intraoperatively are treated with one or two
cerclage cables. When propagation is present, a lateral plate is used
to bypass the distal extent of the fracture. Displaced fractures of
either the lesser or greater trochanter are treated operatively with an
anatomic ORIF. Limited sized lesser trochanteric fractures are cabled.
Claw plates are used for fixation of greater trochanteric fractures.
The tines of the claw are placed through the tendinous insertion of the
gluteus medius and impacted into the tip of the trochanter, thereby
gaining soft tissue and boney purchase. A plate long enough to bypass
the apex of the fracture by long enough to apply three well spaced
(approximately 2 cm apart) cables. A vertically applied cable is
recommended to augment the claw fixation proximally. Initial protected
weight bearing with use of a walker is encouraged with weight bearing
advanced thereafter as tolerated.
fractures includes a lateral plate contoured proximally to accommodate
the trochanteric flare. Distally, the plate should either have a
minimum of 6-8 holes covering the native femur distal to the stem or
extend to the condylar region (where a distal femoral plate design is
utilized). A bowed plate to accommodate the sagittal bow of the femur
is preferred. Three or more equally spaced cables are used proximally
between the lesser trochanter and the tip of the stem. We do not find
it necessary to use devices to attach or hold cables to the plate, the
cables are simply passed around the plate with the crimping connection
purposely positioned either just anterior or just posterior to the
plate to minimize prominence and to allow easy access for locking the
cable. The cables are sequentially tightened and provisionally secured
then retightened sequentially akin to the method of tightening lug nuts
on a car wheel. This assures that tightening one cable does not result
in loosening of an adjacent cable. Locked screws are placed in the
trochanteric region after all cables are tensioned. Distal plate
fixation is with screws. Two screws are placed immediately distal to
the prosthesis through the cement mantle, if present. The distal extent
of the plate is secured with two additional screws. If the fracture
pattern is amendable, lag screws are placed through the plate. The most
critical screws are those nearest and farthest from the fracture, so
between holes can be left empty. If the diaphyseal bone is
osteoporotic, as it is in many cases of periprosthetic fractures,
locked screws are indicated. Locked screws should be placed after
nonlocked screws and appear to be most advantageous near to the
fracture.
associated bone loss (Vancouver B3 fractures). The strut is secured
anteriorly with cables independent of an associated plate (cables over
the strut and under the plate) and with cables around both the plate
and strut.
implants, revision strategies should rely on diaphyseal, not proximal,
fixation. The diameter, geometry, and bone quality of the diaphyseal
bone will determine whether an extensively coated cylindrical stem or a
tapered modular stem is appropriate. Extensively coated cylindrical
stems are appropriate in smaller canals (<18 mm), simple fracture
patterns, and in situations where 5 cm of parallel diaphyseal endosteum
is available for fixation. This situation is rare; therefore, the
authors generally prefer to osteotomize the proximal femur, utilizing
existing fracture lines if possible for direct access to the diaphysis,
and then obtain distal fixation with a tapered modular stem. Modular
trials are used to restore leg length and hip stability. After the
assembly of the implant, the proximal fragments are stabilized with
cerclage, typically utilizing cables, using the intramedullary stem as
an “endoskeleton.” Rarely, the proximal bone is so deficient that
proximal femoral replacement with a modular megaprosthesis is
necessary. An effort should be made to preserve the proximal femoral
muscular attachments. The authors prefer to “wrap” any residual bony
fragments around the megaprosthesis with cerclage in an attempt to
improve construct stability. Obviously, if there are any acetabular
component issues, they can be addressed simultaneously, either with
modular liner exchange, or cup revision as indicated.
mobilization and knee range of motion with weight bearing being
protected for approximately 6 to 8 weeks. Patients are mobilized
postoperatively typically with 50% weight bearing initially followed by
full weight bearing at 6 to 8 weeks to allow some healing of the
proximal fragments. A brace to avoid hyperflexion and adduction is used
if necessary to protect trochanteric and other proximal fragments.
distal” to the femoral stem. These are usually in the supracondylar
femur region and are occasionally intercondylar. Although the fracture
fixation is not entirely dictated by the presence of the femoral stem,
the femoral stem must be considered. We do not recommend use of
retrograde nails for treatment of these distal femur fractures. There
is almost always not enough proximal shaft bone to allow stable
fixation of a retrograde nail. The mainstay of treatment of distal
femur fractures in the presence of a femoral stem is ORIF with lateral
plates. We prefer locked plates to provide fixed angle stability of the
end segment and improved fixation in an osteoporotic shaft segment.
General principles are anatomic reduction and fixation of any
intra-articular component. The articular block is then reduced and
fixed to the shaft restoring anatomic length alignment and rotation.
Great care is taken to preserve the soft tissue envelope in the zone of
the fracture and indirect fracture reduction techniques are generally
utilized. The main deviation from standard fixation of these fractures
due to the presence of the hip arthroplasty stem comes with fixation
proximally. It is rarely the case that a lateral plate to provide
stable fixation of the distal femur fracture is short enough to avoid a
stress riser effect between the top of the plate and the hip
arthroplasty femoral stem. Therefore, we recommend that plates utilized
for Vancouver type C fractures belong enough to overlap the femoral
stem. Fixation in the proximal fragment is with multiple screws distal
to the stem into the native shaft fragment and is supplemented with two
cables around the plate in the zone of the femoral prosthesis. This
construct provides satisfactory stability for fixation of the distal
femur fracture and protects the entire femur from future fracture.
They may occur intraoperatively or postoperatively. Intraoperative
fractures are most commonly associated with insertion of noncemented
components.55,145
The incidence of intraoperative fracture was found to be 0.3% in a
series of 7121 primary total hip arthroplasties (THAs) performed at the
Mayo Clinic between 1990 and 2000.55
All 21 fractures occurred during insertion of a noncemented component
resulting in a fracture incidence of 0.4% for noncemented components
and 0% for cemented components. The fracture occurrence was most common
during impaction of the final component (16/21) but fracture was also
noted to occur during reaming (3/21) and during initial dislocation
(2/21). This study also demonstrated that elliptical designs had a
significantly higher rate of fracture (0.7%) compared to hemispherical
designs (0.09%). This increased risk of fracture with elliptical
designs was largely related to the association with a monoblock design,
one with the liner bound to
the
shell such that visualization of implant seating through screw holes is
not possible. Monoblock elliptical components had a 3.5% incidence of
fracture, whereas modular elliptical components had a 0.3% incidence.
There was no statistical difference in fracture between the modular
elliptical and hemispherical designs supporting the theory that the
reduced feedback from the monoblock design may be a greater
contributing factor than the elliptical shape.
an exceedingly low rate of occurrence. In another large cohort study
from the Mayo Clinic (23,850 patients), the incidence of postoperative
acetabular fracture was 0.07%.119 A
number of factors have been implicated to be associated with
periprosthetic acetabular fracture. Although low-energy trauma, most
notably falls from a standing height, is the most common mechanism,119
fractures may also be seen without antecedent trauma or on occasion
from high-energy trauma. In some of these occult cases, especially
those diagnosed soon after arthroplasty, a missed intraoperative
fracture may be causative. De novo fractures in the postoperative
period that are not associated with trauma are normally associated with
reduced bone quality, quantity, or both. Osteolytic lesions clearly
reduce bone stock and, not surprisingly, fractures through such lesions
have been reported.136 Based on
indirect evidence, usually in the form of a disproportionately high
ratio of females, many authors have implicated osteoporosis as a risk
factor.55,145,147
Weakening of the pelvic bone stock associated with reaming required to
obtain a secure fit of a large diameter hemispherical component for
revision resulted in a 1.2% incidence of transverse acetabular fracture
without associated trauma.147 Stress
fracture has also been reported in association with revision
arthroplasty and should be considered with acute pain onset associated
with abrupt increased activity level.4
The prudent clinician should consider periprosthetic acetabular
fracture whenever there is acute onset of pain associated with total
hip arthroplasty, especially in situations with compromised bone stock.
periprosthetic acetabular fractures based on the stability of the
acetabular component.119 Type 1
fractures are associated with a radiographically stable component, one
where there was no change in the position of the component compared
with that seen on radiographs made before the fracture (if available)
and where gentle passive range of motion of hip caused little or no
pain. Fractures were considered type 2 if the acetabular component was
obviously displaced or radiographically loose and there was notable
pain with any motion of the hip. This classification scheme does not
account for the morphology of the fracture nor does it include the
relative location of the fracture. A modification of the acetabular
fracture classification system of Letournel (see Chapter 45)
that includes a category for fractures of the medial wall of the
acetabulum, a location that is common when these fractures occur
postoperatively, provides more insight into the fracture pattern and
location. In Peterson’s series of postoperative fractures occurring at
an average of 6.2 years after the index procedure, there were eight
type 1 fractures and three type 2 fractures.119
The medial wall was the most common pattern (5 of the 11 cases)
followed by posterior column in three, transverse in two, and anterior
column in one patient. Given the need to consider both the stability of
the component and the fracture location and pattern to determine a
treatment plan, it seems that neither classification system is
sufficient without consideration of the other.
requires consideration of many factors. In addition to the obvious
consideration of patient factors such as medical condition and
functional demands, the timing of the fracture (intraoperative or
postoperative), the displacement, the location, and the stability of
the component should be accounted for in the decision algorithm. The
overall goals are union of the fracture and return of the patient to
their prefracture functional level with a stable acetabular component.
Avoidance of fracture may be the first step. To this end, the degree of
reaming is of paramount importance. Too much reaming, especially in the
revision setting where bone stock is already compromised or in the
presence of serve osteoporosis, should be avoided. Careful reaming
without violation of the acetabular walls, including the medial wall,
will reduce risk for fracture and also provide the necessary foundation
for component stability.31 The
degree of reaming relative to the size of an uncemented implant is also
critical. Underreaming of the acetabulum more than 2 mm is ill-advised
unless the component is unusually large. Care must also be exercised
during insertion of the component. Excessive force should be avoided
and failure of the component to seat properly with successive mallet
blows should be an indication for increased caution and possibly
additional reaming.
with the evaluation of the acetabular component stability and defining
the fracture location and displacement. Intraoperative radiographs
including AP and obturator and iliac oblique views will help define the
location and degree of displacement. Small fractures of either the
anterior or posterior walls may not affect the stability of the implant
and can be treated without any further surgery. If the component is
relegated unstable by a large wall fracture or a fracture that
traverses one of the acetabular columns, then additional steps are
required to insure component stability that may involve adjunctive
fracture fixation. When the fracture is nondisplaced, screw fixation
through holes in the acetabular component may be sufficient to provide
component stability. However, if a column is involved, there should be
a low threshold for independent fracture reduction and plate and screw
fixation of the acetabular fracture, especially if the fracture is
displaced. Bone grafting of the fracture site with reamings or
morselized femoral head may be beneficial to speed fracture healing.145
After plate and screw fixation of the acetabulum, the acetabulum should
be reamed line-to-line for a new multihole component that is carefully
impacted and then stabilized with multiple screws. Weight bearing is
typically restricted for at least 6 weeks based on radiographic and
clinical evidence of fracture healing unless the fracture is of the
acetabular wall and is very small.
Two were small posterior wall fractures that did not compromise
component stability and therefore had no additional treatment and were
allowed immediate weight bearing. One similar fracture had no
additional intraoperative treatment but had restricted
postoperative
weight bearing. The other six were managed with screws either through
the component or placed peripherally outside the cup and in four of
these autograft was packed into the fracture site. Other than one
patient who required resection arthroplasty due to infection, all
fractures healed and no patient required revision at an average
follow-up of 42 months. Haidukewych et al. identified 21 intraoperative
fractures occurring during primary arthroplasty.55
Seventeen were judged not to compromise component stability and
received no additional intraoperative treatment. In 4 of their 21
patients, the component was found to be unstable necessitating a change
in component to one that provided supplemental screw fixation. No
adjunctive plates or screws outside the component were used. All
patients were treated with protected weight bearing. All fractures
healed and no patient required revision for loosening at an average
follow-up of 44 months.
very different than those occurring intraoperatively. Intraoperative
fractures are usually minimally displaced, most commonly involve the
acetabular walls rather than columns, generally require minimally
additional surgical management, and are generally associated with good
results. Postoperative fractures, on the other hand, are usually more
complex, require a greater degree of surgical intervention, and in
general have poorer results. Before treatment can be instituted,
etiologic factors should be considered, the stability of the cup
determined, and the available bone stock quantified.
stable components (type 1 fractures) with good bone stock can be
expected to have a high union rate with nonoperative management
consisting of protected weight bearing for 6 to 12 weeks. Despite union
and in distinction from similar intraoperative fractures, the fate of
the component is dubious. These components have a high likelihood of
loosening. In the series of Peterson et al., 75% of patients treated
nonoperatively for a type 1 fracture (stable component) eventually
required revision of their acetabular component.119
Of the eight fractures, six healed but four eventually required
revision of their acetabular component for loosening. The other 2
patients developed delayed or nonunion and both eventually required
revision. The 2 patients without their revision healed and had no
requirement for subsequent revision. All 8 patients had a stable
prosthesis at a mean of 36 months after their latest revision
procedure. Clearly, these results are far inferior to those seen for
type 1 fractures occurring intraoperatively. Immediate surgical
treatment for fractures with stable components in the absence of
osteolysis may be indicated for widely displaced fractures. Component
revision should be considered to accompany reduction and fixation of
the fracture in such instances; however, there is little in the way of
published results to guide this decision making. Springer et al.
reported seven displaced transverse periprosthetic acetabular fractures
after uncemented acetabular revision about well-fixed components.147
Two were identified on routine radiographs, were asymptomatic, treated
nonoperatively with the period of protective weight bearing, and
healed. Of the 5 symptomatic patients, all were treated operatively.
Four patients where the component was well fixed to the superior
portion of the ileum were treated with ORIF of the posterior column of
the acetabulum without revision of the acetabular component. In one
case where the cup was fixed to the inferior, ischial segment,
treatment was with a reconstruction cage. Of the 5 operatively treated
patients, 1 went on to nonunion and the other 4 healed and at the
latest follow-up had a stable, well-fixed cup.
associated with a loose acetabular component, type 2 fractures,
generally require revision of the acetabular component and supplemental
fracture fixation with plates and screws. The type of component
revision is highly dependent upon the available bone stock. In cases
with severe osteolysis or pelvic discontinuity, reconstruction
typically requires bone grafting, a reconstruction cage, or both. After
removal of the acetabular component, the fracture is fixed with plates
and screws based on the fracture pattern in order to restore, to the
extent possible, the integrity of the acetabular columns. Bone grafts,
either morselized or structural depending upon the size and location of
the defect, are used to reestablish any residual structural
deficiencies. A large multihole cup with screws or a cage are used to
complete the reconstruction. There is little published data to guide
subtle variations in treatment or to establish prognosis. Two patients
in the series of Peterson et al. with type 2 fractures had immediate
revision of the acetabular component without adjuvant plate and screw
fixation of the fracture.119 In one,
a cemented component was utilized and the fracture healed. The other
was revised with a noncemented component with screw fixation through
the shell. This patient went onto nonunion and required repeat revision
with a cemented acetabular component and plate and screw plate fixation
of the acetabular nonunion.
acetabular fractures in association with osteolysis have been the
subject of case reports.23,136
Regardless of the healing potential of the fracture, which in most
cases is nondisplaced, surgical management is indicated for the
underlying osteolytic process as well to deal with the loose component
that in most instances accompany these fractures. Treatment is
primarily directed to management of the osteolytic lesions with bone
graft. Revision of the acetabular component is usually required even if
stable so that adequate access to the lesions for bone grafting can be
accomplished.
associated with implantation of noncemented acetabular components
starts with identification of these fractures. Any change in pitch upon
implantation of these components or sudden loosening of a component
should alert the surgeon to the possible presence of such a fracture.
Direct observation usually identifies these fractures but if any doubt
remains, intraoperative plain film radiographs are recommended. When
fractures are occult and the cup remains stable, we generally
supplement cup fixation with multiple screws without formal plate
fixation of the periprosthetic acetabular fracture especially if the
fracture is small and of a wall. However, when fracture gaps exist,
displacement is wide, or the acetabular component is loose, we have a
low threshold to perform ORIF with plates and screws to first stabilize
the fracture.
Bone
graft from reamings or from the removed femoral head can be used to
fill any residual gaps. The acetabulum is reamed to a slightly larger
size and a new cup is gently inserted and fixed with multiple screws.
When possible, we prefer to have screws on either side of the fracture.
fractures, are generally treated nonoperatively with a period of
approximately 6 weeks of protected weight bearing. Patients that
sustain this type of fracture are monitored carefully at regular
intervals thereafter for any evidence of early loosening. Postoperative
fractures associated with osteolysis or a loose implant are treated
with revision. In these situations, the fracture is typically of
minimal consequence relative to the osteolytic process and therefore
principles of revision arthroplasty in the setting of osteolysis
prevail. As always, when revising one side of a total joint
arthroplasty, contingencies should be made in case intraoperative
factors indicate the other side requires revision also.
performed annually in the United States, and this number continues to
increase. It is estimated that 0.3% to 2.5% of patients will sustain a
periprosthetic fracture as a complication of primary total knee
arthroplasty (TKA).5,30,103 The prevalence of these fractures is substantially higher, up to 38%, after revision TKA.114
Patient-specific risk factors such as RA, osteolysis, osteopenic bone,
frequent falls common in the elderly population, and technique-specific
risk factors such as anterior femoral cortical notching have all been
implicated as potential causes of periprosthetic fractures.
major contributing factor to periprosthetic fractures in total knee
arthroplasty.1,17,28,101
Bone mineral density (BMD) in the distal femur has been shown to
decrease between 19% and 44% 1 year after TKA compared to initial value.117 Progressive loss in BMD has been reported in a follow-up study 2 years after surgery.118
The authors suggested that stress shielding in the anterior distal
femur is responsible and that these decreases in BMD may be an
important determinant of periprosthetic fracture. Neurologic disorders
have been implicated as etiologic factors,28,83 but this too may be related to osteopenia from associated disuse or neuroleptic medications.
a sudden increase in activity soon after TKA have been described and
may be related to relative disuse osteopenia occurring with extended
periods of inactivity prior to TKA.36
In the femur, these fractures may occur at any location and may present
a diagnostic challenge in a patient that complains of sudden onset of
pain without antecedent trauma and without signs of infection.27,56,79,83,113,123
Repeat plain radiographs a period of weeks after the onset of symptoms
may reveal the previously occult stress fracture or a bone scan may be
diagnostic earlier. With an index of suspicion, protected weight
bearing is prudent until stress fracture is ruled out. When ruled in,
protected weight bearing for approximately 6 weeks followed by gradual
advancements is usually a successful treatment plan.
factors may further contribute to the occurrence of periprosthetic
fractures above TKAs. Fractures through an osteolytic lesion about TKAs
are much less common than their occurrence about femoral hip
components, but these certainly may occur.116
Anterior femoral notching has been implicated as another risk factor
for subsequent periprosthetic supracondylar femur fracture.
Biomechanical evaluations in human cadaveric bone indicate that
anterior notching significantly reduces load to failure compared to
matched pairs without notching.82
When loaded in bending, notched femurs failed with a short oblique
fracture originating at the cortical defect while unnotched femora
sustained a midshaft fracture. No difference in failure mode was noted
with loading in torsion. The force to failure was significantly less
for notched femurs than unnotched: 18% less in bending and 39% less
than torsion. Finite element analysis has also yielded results that
indicate notching reduces the fracture threshold.177
Larger notches, sharper notches, and proximity to the prosthesis each
lead to increased local stresses. Despite commonsense and laboratory
investigations indicating notching as a risk factor for periprosthetic
supracondylar femur fractures, clinical data remains unconvincing. The
lack of statistical association between notching and fracture are
likely due to underpowered studies and extremely small number of
observed fractures. Lesh et al. reviewed 164 supracondylar
periprosthetic femur fractures reported in the literature and noted
more than 30% were associated with notching.82
Many of these patients, however, were noted to have other risk factors
for fracture. Ritter et al., in two separate studies, failed to find an
association between notching and fracture.130,131
However, with only two fractures in each of these cohorts, statistical
association would be difficult to determine. In the first study, one
fracture occurred from a group of 490 TKAs without notching and one
from a group of 180 TKAs with notching.130
In the second study, there were no fractures from a group of 325 with
notching and two fractures from a group of 764 without notching.131
component that removes bone from the intercondylar region has been
noted to increase risk for intraoperative fracture.134
Fracture, typically of the medial femoral condyle, is more likely to
occur if the component is not centered between the condyles. A
relatively new potential risk factor has been described in a case
report of periprosthetic supracondylar femur fractures through a
navigation pin hole.86 With the
increasing popularity of surgical navigation for TKA, this complication
should be considered when choosing a location for navigation
instruments.
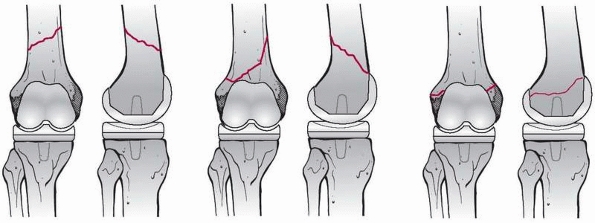
periprosthetic femur fractures about TKAs accounts for fracture
displacement and prosthesis stability (Fig. 21-13).85,133
Type I are stable fractures essentially nondisplaced and the
bone/prosthesis interface remains intact. Type II fractures are
displaced with an intact
interface and type III fractures have a loose or failing prosthesis regardless of the fracture displacement.
 |
|
FIGURE 21-13
Classification scheme for periprosthetic fractures about the femoral component of the knee. Type I fractures are minimally displaced with an intact prosthesis bone interface, type II fractures are displaced but maintain an intact bone prosthesis interface, and type III fractures may be displaced or nondisplaced, but have a loose femoral component. (Modified from Lewis PL, Rorabeck CH. Periprosthetic fractures. In: Engh GA, Roabeck CH, eds. Revision total knee arthroplasty. Baltimore: Williams & Wilkins, 1997:275-295). |
account for the fracture location relative to the prosthesis, a factor
that has the potential to dictate treatment. The classification scheme
of Su et al. is useful in this vein where fractures are divided into
three types according to the fracture location relative to the proximal
border of the femoral component.151
Type I fractures are proximal to the femoral component, type II
originate at the proximal end of the component and extend proximally,
and type III extend distal to the proximal border of the femoral
component (Fig. 21-14).
associated with TKA prostheses present unique challenges. Nonoperative
treatment has been associated with poor results for displaced
fractures, especially relative to results of operative fixation.17,28,40,47,101,104
The presence of a TKA prosthesis can complicate operative treatment of
these fractures by interfering with or precluding the use of standard
fixation methods. A TKA prosthesis with a narrow or closed
intracondylar space either limits the diameter for a retrograde nail or
completely obviates its use.93 Traditional plate fixation is prone to varus collapse,30
while blade plates or condylar screws have limited applicability for
very distal fractures or when associated with a TKA prosthesis that has
a deep intracondylar box. New locked plate devices offer many theoretic
advantages for these patients. The multiple locked distal screws
provide both a fixed angle to prevent varus collapse, and the ability
to address distal fractures even when associated with a deep
intracondylar box. The provision for locked screw insertion into the
diaphyseal fragment theoretically improves fixation in the often
associated osteoporotic bone. These devices can also be inserted with
relative ease and familiarity. The results of locked plate fixation for
treatment of periprosthetic supracondylar femur fractures above a TKA
have been investigated by several authors.59,120,125,127,155 Intramedullary nailing represents another slightly more limited but efficacious option for these fractures.3,48,59,168 Distal femoral replacement, although with limited longevity,74,104
has a role in certain subsets of patients. Patients with loose TKA
prostheses and in those where internal fixation is undesirable should
be considered for distal femoral replacement.
 |
|
FIGURE 21-14
The Su classification of periprosthetic distal femur fractures accounts for location of the fracture relative to the femoral TKA component. |
fixation of supracondylar femur fractures with traditional condylar
buttress type plates, are prone to complications. When comminution is
present, these nonfixed-angle implants are especially prone to varus
collapse. Davison reported more than 5 degrees of collapse to occur in
11 of 26 (42%) such comminuted distal femur fractures.30
These problems can be magnified in patients with fractures associated
with a TKA as these patients are often elderly with osteoporotic bone
making stable internal fixation even more unreliable. This is
confounded by the reduced ability to gain bicondylar screw purchase due
to interference of the TKA prosthesis. Figgie et al. reported failure
of internal fixation in 5 of 10 patients with periprosthetic femur
fractures above a
TKA treated with traditional plating methods40 and Merkel and Johnson reported satisfactory results in only 3 of 5 such patients.101
Traditional fixed angle plate constructs, such as 95-degree condylar
plates and blade plates, reduce the risk for varus collapse, but have
limited application for fractures about a TKA prosthesis due to
interference of the femoral component. More modern methods of fixation,
locked plating and retrograde nailing, have recently been shown in a
systematic review of 415 cases to provide superior results to
conventional treatment options for distal femur fractures above TKAs.59
The overall nonunion rate was 9%, fixation failure rate 4%, infection
rate 3%, and revision surgery rate 13%. Retrograde nailing was found to
offer relative risk reduction in nonunion (87%) and revision surgery
(70%) compared to traditional nonlocked plating. Locked plating showed
nonsignificant trends toward similar risk reductions (57% for
nonunions, 43% for revision surgery).
femur with the capacity for locking screws have potential advantages
for the fixation of supracondylar femur fractures associated with TKA (Fig. 21-15).
In contrast to traditional 95-degree plate devices, locking plates
offer multiple, rather than single, distal fixed angle screw options.
Ricci et al. showed that at least two such locked screws were typically
able to be placed across to the medial condyle despite the presence of
a TKA femoral component.127 When the
TKA blocked bicondylar screw fixation, unicondylar locked screws were
utilized. This combination of bicondylar and unicondylar locked screw
fixation provided excellent distal fixation as no distal fixation
failures occured in Ricci’s series. These results are consistent with
those of other locking plate devices used for fixation of native distal
femur fractures.140,142
With such secure distal fixation, repetitive stresses have led to plate
failure over the zone of fracture or to screw failure in the proximal
fragment in up to 33% of cases.59,120,127
Of note, three of the four proximal screw failures occurred when
exclusively nonlocking screws were used in the shaft fragment. This
study was the first to describe modern “hybrid” locked fixation, where
nonlocked and locked screws were used in the same construct. The
authors pointed out that inserting nonlocked screws prior to locked
screws in any given fragment allows the plate to be used as a reduction
aid where the contour of the plate helps dictate the reduction in the
coronal plane. Malreductions using this technique were present in only
2 of 22 cases (9%). This compares favorably with the reduction (6% to
20% malreductions) reported with internal fixator systems where
exclusive use of locked screws makes reduction independent of plate
contour.75,94,140,142
Only one such failure occurred among the 14 cases where locking screws
supplemented nonlocked fixation in the shaft, this being a patient with
diabetes and obesity who developed an aseptic nonunion. Biomechanical
investigations suggest that locked screws in the diaphysis may protect
from this type of screw failure, especially in osteoporotic bone.35,115
The 3 patients with healing complications in this series were at
exceedingly high risk for complications. All had insulin dependent
diabetes mellitus, neuropathy, and obesity as associated comorbidities.
 |
|
FIGURE 21-15 Treatment of a periprosthetic distal femur fracture (A,B) with a lateral locking plate (C,D).
|
satisfactory treatment option for fixation of supracondylar femur
fractures that are not associated with TKA. This fixation method is
advantageous because of the indirect nature of the fracture reduction
and associated minimization of soft tissue disruption about the
fracture. However, problems obtaining stable fixation with
intramedullary nails in patients with wide metaphyseal areas, with
osteopenia, or both can lead to loss of fixation and malalignment (Fig. 21-16A-C).3
When a TKA is present, the potential difficulties of retrograde nailing
of supracondylar femur fractures are also increased. Some TKA designs,
because of a closed or narrow intercondylar notch, preclude the use of
retrograde nails or limit their maximum diameter, respectively.
Furthermore, the specific prosthesis type may be unknown at
the
time of fracture fixation. In these cases, the choice of an anterior
surgical approach used for retrograde nailing may need to be aborted in
favor of a lateral approach for plate fixation if a nonaccommodating
prosthesis is encountered. Despite these potential pitfalls, retrograde
intramedullary nailing can be successfully applied to periprosthetic
supracondylar femur fractures that have adequate distal bone stock and
is the preferred method of treatment by some authors (see Fig. 21-16).48
Wick et al. found comparable results for retrograde nailing and locked
plating of these fractures in a small comparative series of nine
fractures each.168 They noted that
locked plates were preferred in cases with osteoporotic bone. Another
small series of 10 periprosthetic supracondylar femur fractures treated
with retrograde nailing resulted in 100% union.48
The one major complication was malunion in 35 degrees of valgus
requiring revision to a stemmed TKA. This may be related to the use of
a short nail which, because they do not benefit from the stability and
alignment control that comes from passing the nail across the femoral
isthmus, are not generally recommended any longer for treatment of
distal femur fractures. Recent advances in nail design that provide
multiple locked interlocks at multiple angles may provide improved
fixation of the distal segment and may therefore expand the indications
for this technique.
 |
|
FIGURE 21-16 Retrograde nailing of distal femur fractures with wide metaphyseal regions (A,B) runs the risk of malalignment (C).
Proper technique requires the nail be aligned with the axis of both the proximal and distal fragments. The isthmus of the femur helps align long nails within the proximal fragment, but it is incumbent upon the surgeon to establish alignment in the distal fragment. D,E. With attention to detail, successful alignment can be accomplished even with distal fractures. F,G. Nails with multiple distal locking options are recommended. (D-G courtesy of P. Tornetta, III, MD.) |
supracondylar fracture, revision is typically considered. Bony defects,
areas of osteolysis, osteopenia, and short periarticular fragments all
pose challenges to a successful revision arthroplasty in this setting.
In elderly patients, distal femoral replacement megaprostheses are
often required to reconstruct massive bony defects. Attention to
specific technical details is necessary for a successful result, and
the surgeon undertaking such reconstructions should be experienced in
both arthroplasty and fracture management
techniques.
In patients with a loose implant or a history of prefracture knee pain,
the routine preoperative evaluation of these patients should include a
complete blood count with manual differential, sedimentation rate,
C-reactive protein serologies, and a knee aspiration to exclude occult
infection.
arthroplasty should be obtained. This is especially important if
isolated component revision is contemplated. Older implant designs may
not offer varying degrees of constraint, augmentations, or polyethylene
insert sizes, and thus compatibility issues may necessitate complete
arthroplasty revision. Previous incisions and the status of the soft
tissues should be circumferentially evaluated and the neurovascular
status of the limb should be carefully documented.
fracture has become less common in the authors’ practices with the
advent of improved internal fixation devices such as locked plates.
Typically, revision arthroplasty is reserved for fractures around a
loose prosthesis, fractures with inadequate bone stock to allow for
stable internal fixation, or for recalcitrant supracondylar nonunions
that require resection and megaprosthesis implantation. Surgeons who
treat periprosthetic fractures around TKA must have the expertise and
technical support to be able to perform either long-stemmed revision
TKA or revision to a megaprosthesis, as one is often unable to
determine which reconstructive option is necessary until the fracture
has been exposed in the operating room. Bony defects secondary to
comminution, multiple previous procedures, the presence of broken
hardware, and the presence of deformity all may present technical
challenges to a successful outcome.
engage the diaphysis and simultaneously stabilize the fracture can be
used. Cemented stems may be used, but care must be taken to prevent
extrusion of cement into the fracture site. Allograft struts with
cerclage wiring can be used to reinforce the stability provided by a
long stem prosthesis. It is very unusual, however, to have distal
femoral bone stock that is inadequate for internal fixation yet
adequate for formal revision. The ideal indication for long stem
revision TKA would be the presence of adequate bone stock in the face
of a supracondylar fracture with a grossly loose femoral component.5,36
Most of the clinical data evaluating the outcomes of a simultaneous
revision arthroplasty with intramedullary stem fixation of a
supracondylar fracture have been gathered from the treatment of distal
femoral nonunion. Kress et al.76
reported a small series of nonunions about the knee treated
successfully with revision and uncemented femoral stems with bone
grafting. They used uncemented femoral stems and bone grafting and
achieved union in 6 months.
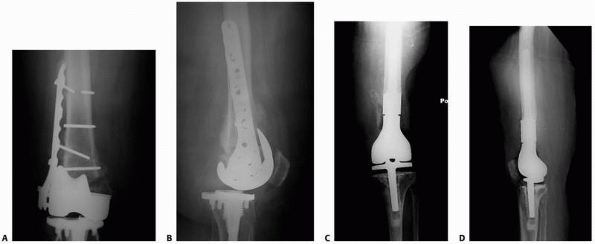 |
|
FIGURE 21-17 A periprosthetic distal femoral nonunion after ORIF (A,B) treated with a distal femoral replacement (C,D).
|
for salvage of failed internal fixation of supracondylar periprosthetic
femur fractures. The long-term results of the kinematic rotating hinge
prosthesis for oncologic resections about the knee have been good, with
a 10-year survivorship of approximately 90%. As their success becomes
more predictable, the indications for megaprostheses are expanding.
Elderly patients with refractory periprosthetic supracondylar nonunions
(Fig. 21-17) or those with acute fractures with
bone stock inadequate for internal fixation are reasonable candidates
for megaprostheses. Davila et al. have reported a small series of
supracondylar distal femoral nonunions treated with a megaprostheses in
elderly patients.29 They have shown
that a cemented megaprosthesis in this patient population permits early
ambulation and return to activities of daily living. Freedman performed
distal femoral replacement in 5 elderly patients with acute fractures
and reported four good results and one poor result secondary to
infection.44 The 4 patients with
good results regained ambulation in less than 1 month and had an
average arc of motion of 99 degrees. All patients had some degree of
extension lag.
composite may be a better alternative. Distal femoral reconstruction
with an allograft prosthetic composite, providing a biologic interface,
can help restore bone stock and potentially make future
revision easier.25,36
Kraay et al. have reported a series of allograft prosthetic
reconstructions for the treatment of supracondylar fractures in
patients with TKAs.74 At a minimum 2
year follow-up, the mean Knee Society score was 71 and the mean arc of
motion was 96 degrees. All femoral components were well fixed at
follow-up. Results of this study indicate that large segmental distal
femoral allograft prosthetic composites can be a reasonable treatment
method in this setting.
fractures about TKA are in the presence of a stable femoral component.
Therefore, ORIF is generally performed in this scenario. For fractures
that are at the diaphyseal-metaphyseal junction, retrograde
intramedullary nailing is usually our treatment of choice. Of course,
it is incumbent upon the surgeon to clearly identify the femoral
component type and to assure that retrograde nailing through the
intercondylar box is possible. If so, standard retrograde nailing
technique is utilized. A critical aspect of this procedure is the
trajectory of the starting point in the distal fragment. This
trajectory must be collinear with a long axis to the femur in both the
sagittal and coronal planes to assure proper alignment. Given the often
coexistent osteopenic bone and wide metaphyseal areas in this patient
population, an initial opening reamer passed in an ideal trajectory
will not necessarily guarantee that subsequent reamers and the
retrograde nail will follow the same path. Therefore, a surgeon must be
prepared to utilize supplementary techniques to assure that the nail is
aligned properly with the distal fragment. We prefer the use of
blocking screws. These screws are place anterior to posterior to
control varus-valgus alignment and from lateral to medial to control
flexion-extension alignment. The blocking screws should be placed
relatively near the fracture to optimally affect alignment. Additional
technical details of blocking screw placement can be found in multiple
chapters throughout this book including Chapter 7, Chapter 51, and Chapter 55.
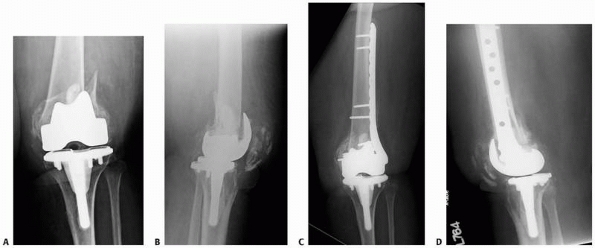 |
|
FIGURE 21-18 An extreme distal periprosthetic fracture above a TKA (A,B) treated successfully with a distal lateral femoral locking plate (C,D).
|
junction are treated with ORIF with locked plates, even when fracture
extension is extremely distal. We have found that locked plating
constructs offer satisfactory fixation distally even in these short
segments (Fig. 21-18). An important principle
for plate fixation of these fractures is the use of biologically
friendly, indirect, fracture reduction techniques. A lateral plate is
applied and fixed distally first with nonlocked then with locked
screws. Proximally, fixation is with nonlocked or locked screws
depending on the presence of osteoporosis.
is periprosthetic fracture between a TKA and THA, the so-called
interprosthetic fracture.92 These
fractures have been found to be in the supracondylar region above the
TKA about two times more frequently than in the shaft about the THA
stem. Treatment of these interprosthetic fractures should follow the
principles of the individual type of fracture encountered and
simultaneously protect against future fracture. This situation almost
universally lends to plate fixation with a long distal femoral locking
plate that spans from the distal femur to overlap with the region of
the femoral stem (Fig. 21-19) as described for
treatment of Vancouver type C fractures taking into account the issues
of distal fixation in the presence of the TKA femoral component
discussed in this section.
around loose implants and fractures of the distal femur with distal
fragments that offer no reasonable opportunity for internal fixation.
Revision of femoral components typically requires metal augmentation
due to the inevitable bone deficiency associated with component
removal. Stems should be used routinely, and it is recommended that the
stems engage the femoral diaphysis both for alignment and fixation
reasons. Commercially available metaphyseal sleeves and trabecular
metal cones can be useful for managing capacious metaphyseal defects.
It should be noted that implants with increased varus-valgus constraint
and hinged implants
should
be available, since ligamentous insufficiency is common in this
setting. More commonly, with a distal femoral fracture above a loose
implant, there is simply not enough bone to support a traditional
revision, even with the use of diaphyseal engaging stems. This
situation is not uncommon in the elderly, low demand patient. In these
cases, a modular megaprosthesis (distal femoral replacement) is
performed. Careful dissection of the residual distal femoral bone is
performed to avoid vascular injury. Various modular segments are
available to manage metaphyseal bone loss due to fracture comminution,
yet still allow restoration of appropriate leg length, limb alignment,
and knee stability. Cement fixation is typically used in this setting.
 |
|
FIGURE 21-19
An interprosthetic fracture located in the distal femur is treated with a long distal lateral femoral locking plate that protects the entire femur by overlapping with the hip arthroplasty stem. |
fractures about TKA is substantially less than that for fracture on the
femoral side of these prostheses. An analysis of fractures about TKAs
from the Mayo Clinic joint registry published in 1999 indicated that
postoperative fracture after primary TKA occurred with an incidence of
0.4% in the tibia, 0.7% in the patella, and 0.9% in the femur. In our
unpublished collective experience, however, periprosthetic fractures
above a TKA are much more than twice as common as those below, and in
several published series, the frequency of all three of these fractures
is substantially higher, with distal femur fractures occurring in up to
38% and patella fractures occurring in up to 21% of revision TKAs.5,30,114,128,158
patella fractures may be either systemic or local. Systemic risk
factors are not unique to these anatomic locations and are therefore
similar to those for other types of periprosthetic fractures and
primarily includes osteopenia from a variety of causes. Patients with
RA, especially those taking corticosteroids, are at a particularly high
risk for fracture about a TKA.10,17,60 BMD in the tibia below the tibial component has been shown to progressively decrease at 3 years follow-up after arthroplasty.118,165 Wang et. al found that alendronate taken for 6 months postoperatively improves BMD.165
periprosthetic fracture around the knee joint, and given the critical
nature of the extensor mechanism for knee function, these fractures are
significant to the ultimate arthroplasty success. Fractures of the
patella generally occur postoperatively and may occur with either
unresurfaced or resurfaced cases.20,146 Chalidi et al.,20
in a literature review, found that only 11.68% of 539 reported
fractures were directly associated with trauma. The remaining occurred
spontaneously and most fractures occurred during the first 2 years
after arthroplasty. Etiologic factors specific to the patella are
component design, excessive resection of bone, limb and prosthesis
alignment, and presence or absence of a lateral release.15,18,39,49,58
Intraoperative fractures, although uncommon, can occur with aggressive
clamping of the patella component, bone resection leaving less than 10
to 15 mm of bone, and in the setting of revision arthroplasty in cases
with poor remaining bone stock. Devascularization of the patella from
lateral retinacular release may be a risk factor for subsequent
fracture as well as for failure of subsequent fracture management. Tria
et al. reported that all 18 patella fractures in a series of 504
primary TKAs were associated with a prior lateral release.158
In this series, 4% of those with lateral release (n = 413) had
subsequent fracture of the patella compared to 0% of those without
lateral release (n = 91). The association of lateral release and
fracture was significant. However, opposite results were found in
another study by Ritter and Campbell.128
In this series, unlike Tria’s series, a vast majority of the 555
patients did not have a lateral release (n = 471). Fractures occurred
in 1.2% of cases with and 3.6% of those without lateral release. These
conflicting reports, both from large series, make it difficult to
determine if lateral release should be considered an independent risk
factor for patella fracture.
fractures may be related to technique as well as to implant design.
Osteotomy of the tibial tubercle facilitates exposure for the very
stiff knee but it reduces the structural integrity of the proximal
tibia. In a small series of nine TKAs with tibial tubercle osteotomy,
Ritter et. al reported two proximal tibia fractures.129
Both cases occurred soon after surgery (within 2 months) and each
healed with nonoperative management. Any prior bony defects, such as
from bone-patellar tendon-bone donor sites or tunnels from anterior
cruciate ligament reconstructions, are additional potential risk
factors for fracture of either the patella or the tibia. Also,
prior
fracture malunion and holes from prior fixation devices for high tibial
osteotomy or tibial plateau fracture fixation pose stress risers.
|
TABLE 21-3 Ortiguera and Berry Classification for Periprosthetic Patella Fractures112
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The technique used for implantation, reaming a conical hole for the
tibial stem without impaction and absence of trialing, rather than the
implant itself, may have been causative.
potential new situation related to periprosthetic fractures about knee
arthroplasty. A small number of these fractures have been reported
including both intraoperative and postoperative fractures.77,163 Surgical technique was held responsible for the three intraoperative fractures reported by Van Loon et al.163 All cases ended up being treated with revision to a TKA.
was utilized most frequently in the available literature. This
classification takes into account the integrity of the extensor
mechanism, the status of the patellar component (well-fixed or loose),
and the amount of available bone stock (Table 21-3).
Type I fractures have an intact extensor mechanism and a stable
implant, type II have disruption of the extensor mechanism with or
without a stable implant, and type III an intact extensor mechanism and
a loose implant. Type III subtype A has reasonable remaining bone
stock, and subtype B poor bone stock. Among 265 fractures in the
literature classified using this system, approximately 50% were type
III with the rest almost equally divided between types I and II.20
|
TABLE 21-4 Classification for Periprosthetic Tibia Fractures38,151
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
timing of the fracture (intra- or postoperative) are incorporated into
the classification of periprosthetic tibia fractures according to Felix
et al.38,150
Type I fractures occur in the tibial plateau, type II adjacent to the
stem tip, type III distal to the prosthesis, and type IV involve the
tibial tubercle. Subtype A have a well fixed implant, subtype B a loose
implant, and subtype C occur intraoperatively (Table 21-4 and Fig. 21-20).
patellar fractures. The integrity and tracking of the extensor
mechanism, locations and displacement of the fracture, stability of the
implant, and the available remaining bone stock must all be considered.
As with management of other periprosthetic fractures, the determination
of the optimal method can be complex and fracture management can be
difficult. A clear vision of the ultimate management goals, typically
restoration of the extensor mechanism and at least return to baseline
function and pain levels, helps define the optimal individual
management scheme. Treatment options include a range from nonoperative
management, ORIF, component resection, and patellectomy (partial or
complete). Nonoperative management is usually appropriate in a majority
of patients. When the extensor mechanism is intact and even sometimes
when it is not, nonoperative management is recommended. Surgical
management is usually reserved for disturbance of the extensor
mechanism integrity, a loose patellar component, and patellar
maltracking. The results of surgical management is, however, marginal.
ORIF with tension band technique or cerclage wiring results in nonunion
in a very large
proportion of patients in many reports, with an overall average nonunion rate of 92%.15,20,24,50,62,69,112,144
Although fibrous union can on occasion restore painless extensor
mechanism function, in general poor results in the face of nonunion can
be expected. The relatively small and avascular fracture fragments have
limited healing potential, which can be negatively influenced by
surgical dissection, potentially leading to nonunion and infection.
Therefore, nonoperative management is not an unreasonable consideration
even in the face of a disrupted extensor mechanism. The presence of
fracture and a loose implant is understandably associated with high
complication rates regardless of treatment method. These situations
usually leads to surgery for either removal or revision of the
component. When there is adequate bone stock (more than 10 mm),
revision of the patellar component is reasonable. Severe bone
deficiency, however, mandates patellar resection arthroplasty with
partial or complete patellectomy. Knee function among all patients
treated for periprosthetic patella fracture reveals an extensor lag of
no more than 10 degrees and a limitation of approximately 20 to 30
degrees of flexion in most patients.20 However, function is highly variable and related to the ultimate status of the extensor mechanism.
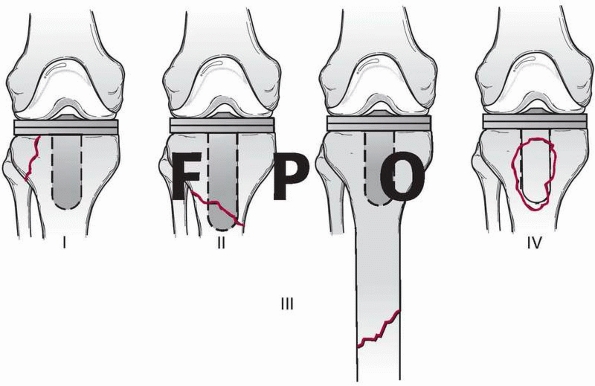 |
|
FIGURE 21-20
Classification scheme for periprosthetic tibia fractures about a TKA: type I fractures involve only a small portion of the tibial plateau, type II fractures are about the stem, type III fractures are distal to the stem, and type IV fractures are of the tibial tubercle. The subtypes are described in Table 21-4. |
TKA are extremely uncommon, and the tibial component is almost always
loose. Tibial fractures associated with loose components are best
treated with revision arthroplasty, frequently utilizing a long stem to
bypass the fracture.5,36,38
It is wise to have an entire revision system available because often
the femoral component will need to be revised as well for sizing,
constraint, exposure, or gap balancing reasons. Often, these fractures
are associated with extensive osteolysis and therefore may require
structural or morselized bone grafting, the use of metal wedges, or in
the most severe cases proximal tibial megaprosthesis or allograft
prosthetic composites. Maximizing host bone support is critical for a
good result. General principles include the use of stem extensions with
either metaphyseal cementation or longer, diaphyseal press-fit
strategies. More contemporary techniques utilize metaphyseal filling
sleeves that provide rotational and axial stability; however, long-term
data on such reconstructions is lacking. The largest series of
periprosthetic tibial fractures around loose prostheses was reported by
Rand and Coventry.122 They reported
that all 15 knees had varus axial malalignment when compared to a
control group. Similar studies have confirmed that varus malalignment
may be a potential risk factor for periprosthetic tibial fracture.91,169
Specific technical considerations include careful soft tissue
dissection and retraction to minimize soft tissue trauma to the already
compromised skin flaps. It is important that the surgeon undertaking
these reconstructions be experienced in revision arthroplasty
techniques and fracture management techniques to achieve a successful
outcome.
associated with a well-fixed component, nonoperative management with a
cast or brace is indicated for nondisplaced fractures and ORIF is
indicated for displaced fractures. If cast management is chosen, great
care should be taken to monitor for pressure sores especially in
patients with RA and those with diabetes. Maintenance of limb alignment
is important, therefore frequent, usually weekly, radiographic
surveillance is advisable with conversion to ORIF considered for
failure to maintain satisfactory alignment. As with any other
immobilized joint, arthrofibrosis is a potential risk factor. ORIF is
advisable for displaced fractures involving the metaphyseal-diaphyseal
junction (Fig. 21-21) and those more distal (Fig. 21-22).
Plate and screw constructs are limited by the available bone proximally
to pass bicortical screws. This is highly dependent upon the prosthesis
design with regard to the degree of metaphyseal filling. The inability
to pass multiple screws across the proximal fragment calls for
adjunctive fixation with unicortical locked screws, cables, secondary
posteriormedial plates, or some combination thereof.
periprosthetic fractures to manage. Operative management is associated
with relatively high nonunion and infection rates, and nonoperative
management
may require prolonged immobilization and does not address loose
components. We tend to lean toward nonoperative management for these
fractures unless displacement is severe or the component so loose that
is it may dislodge. A staged management protocol that treats a
periprosthetic patellar fracture associated with a loose component
sequentially rather than simultaneously is sometimes prudent to avoid
major complications. Nonoperative fracture management to healing
followed by surgical management of a loose component, if symptomatic,
is a strategy that takes longer to complete but may ultimately result
in fewer complications. When acute operative management is undertaken
in the face of a stable component, we have a low threshold for excision
of small- to moderate-sized superior or inferior pole fragments with
suture repair of the associated tendon to the remaining bone.
Patellectomy is our operative treatment of choice for cases with loose
prosthesis and poor bone stock.
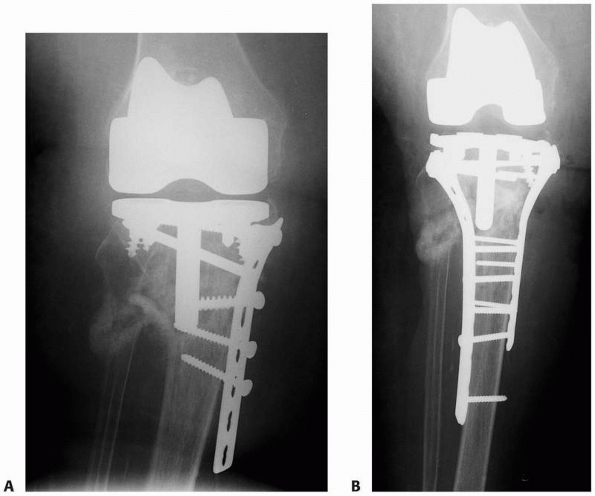 |
|
FIGURE 21-21 A proximal tibial periprosthetic nonunion (A) is treated with a combination of lateral locked plating, posterior medial locked plating, bone grafting, and adjuvant BMP (B).
|
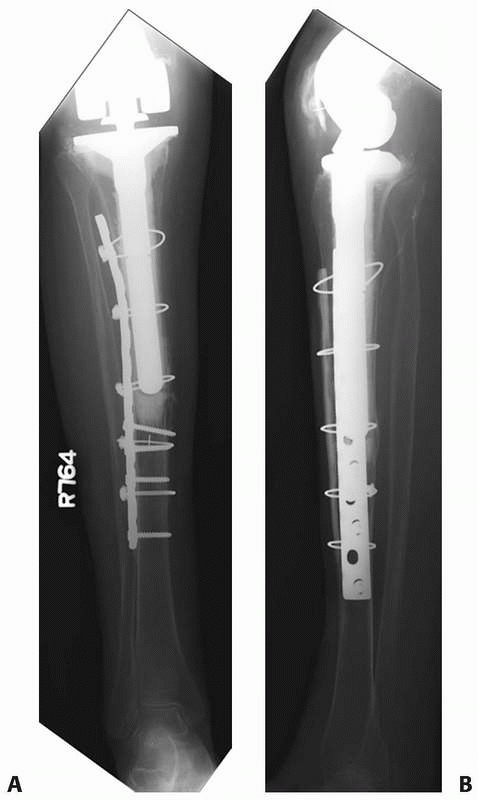 |
|
FIGURE 21-22 A,B:
A fracture about a well-fixed tibial stemmed tibial component of a TKA had a previously untreated perforation near the tip of the stem. This was managed with a lateral plate and an anterior medial strut allograft. |
are relatively uncommon. When they do occur, most often they are
associated with a loose tibial component; therefore, revision is
preferred in these situations. Tibial revision for periprosthetic
fracture requires the routine use of stems and augments and metaphyseal
filling metal implants can be useful for managing bone deficiencies.
The tibial base trays have often subsided into varus, and anticipating
medial and central defects is wise. The surgeon should be aware that
isolated tibial component revision is rare, and commonly, one should be
prepared to revise the entire arthroplasty.
stable, our preferred method of treatment is with locked plates.
Although there is scant literature supporting this practice, it is our
feeling that locked plates are invaluable for these fractures. The
amount and quality of bone proximally is usually marginal, where
nonlocked screws rarely obtain adequate fixation purchase. Locked
screws proximally and either locked or nonlocked screws distally
through a lateral plate provide sufficient stability. We, however, have
a low threshold to supplement a lateral plate with a posterior medial
plate (see Fig. 21-21). It is critical that these exposures
be through separate incisions so as to maximally preserve the soft
tissue envelope. Even in the presence of a midline incision from the
TKA, separate lateral and medial incisions can provide an adequate skin
bridge in all but the thinnest of patients.
arthroplasty or hemiarthroplasty occur with intermediate frequency
relative to other periprosthetic fractures. Among series that focus
exclusively on fractures that occurred postoperatively, the incidence
has been remarkably consistent at between 0.6% and 2.3%.12,78,172,173
With only limited data to rely on, the incidence of intraoperative
fracture may be substantially higher. Two studies that distinguish
between intraoperative and postoperative fractures both found two times
more fractures occurred intraoperatively.19,51
Many risk factors for fracture have been postulated, but the limited
number of fractures in most series, usually less than 10, make
scientific analysis impossible. It is logical, however, that conditions
that further weaken a bone that already has a stress riser would put
that patient at a particularly high risk of fracture after even minor
trauma.
Boyd’s series of seven postoperative fractures, 5 patients had RA. The
incidence of fracture among those treated with their initial
arthroplasty due to RA (1.8%), however, was only slightly higher than
for those treated for other diagnoses (1.5%). Studies from the Mayo
clinic, where a large proportion of patients had a primary diagnosis of
RA, have shown higher incidences of fracture among patients with RA.
Wright and Cofield reported on nine postoperative fractures from a
cohort of 499, 144 of whom had RA.173
The incidence of fracture was 3.4% among those with RA and 1.1% among
the rest. A more recent study from the Mayo clinic that included a
larger cohort of patients found a relatively low overall incidence of
postoperative fracture (0.6%). Nineteen fractures among 3091 patients.78
The proportion of fractures that occurred in patients with RA was high
(31%) but the relative numbers of patients in the entire cohort who had
RA was not reported, so evaluation of RA as a risk factor is impossible.
a risk factor for fracture, especially among patients with revision
arthroplasty stems.19,51,148 It should be noted, however, that such statement has been made without sufficient data in some series.19,51
Campell et al. quantified the degree of osteopenia as the ratio of the
combined width of the middiaphyseal cortices to the diameter of the
diaphysis.19 Normal bone was
considered to have a ratio of greater than 50%, mild osteopenia was a
ratio of between 25% and 50%, and severe osteopenia less than 25%. The
validity of these criteria and definitions, it should be noted, are
unsubstantiated. Using this criteria, 25% of their 20 patients with a
fracture had normal bone, 45% mild osteopenia, and 30% severe
osteopenia. It is useful to note that their 75% prevalence of
osteopenia in this cohort is very high; however, without data on the
bone quality of those without fracture, it is inaccurate to conclude
that this truly represents a risk factor for fracture. Kumar et al.
utilized this system to grade bone quality and found all of their
patients with fracture had osteopenia (44% severe).78
The presence or degree of osteopenia has not been correlated with a
particular injury mechanism, outcome, nor a particular treatment
strategy. It seems intuitive, however, that any treatment algorithm in
a patient with severely compromised bone stock should include
consideration of minimizing the presence of stress risers in the final
fracture treatment construct in order to avoid subsequent additional
fractures.
are also subject to limitations of a general lack of data for patients
without fracture. When such data is available, age in particular does
not appear to be substantially different in those with and without
fracture. The average age of all 3091 patients who had undergone
shoulder arthroplasty at the Mayo Clinic between 1976 and 2001 was 63
years and the age of those who sustained a fracture was also 63 years.78 The female to male ratio was slightly higher in those with fracture (63%) compared to the entire group (56%).
intraoperative fracture. Most notably to manipulations of the humerus
during surgical exposure or to preparation of the canal with reamers or
an oversized broach.19,51
Excessive external rotation required to provide exposure in patients
with large muscles or scars was causative for half of all
intraoperative fractures in one series.19
In half of these, associated overreaming of the diaphysis caused
notching of the endosteum resulting in a stress riser for spiral
fracture formation during subsequent external rotation. Hoop stresses
associated with an oversized broach or prosthesis can cause transverse
or oblique fractures.19,51 Fracture during revision shoulder arthroplasty may be intentional19
as a less destructive method to remove a stem. Unintentional fracture
may occur during explantation of the prosthesis, removal of associated
cement, or during implantation of the revision prosthesis.
periprosthetic humeral shaft fractures about shoulder arthroplasty
stems. Most distinguish fractures by their location relative to the tip
of the stem,19,51,173 and a smaller subset account for fractures of the tuberocities or the stability of the stem.172
None are universally accepted. Wright and Cofield described three
fracture patterns occurring in their series of nine postoperative
fractures: type A centered at the tip of the stem and extending
proximally more than one-third the length of the stem, type B also
centered at the tip of the stem but with less proximal extension, and
type C involving the distal humeral diaphysis, distal to the tip of the
stem, and extending into the metaphysis (Fig. 21-23).173 Campbell et al. categorized fractures into one of four regions (Fig. 21-24).19
Region 1 included the greater or lesser tuberosities, region 2 the
proximal metaphysis, region 3 the proximal humeral diaphysis, and
region 4 the mid- and distal diaphysis. They classified their 21
fractures based on the distal most fracture extent. Groh et al., like
Wright and Cofield, classified fractures of the shaft into three types (Fig. 21-25).51
Type I occur proximal to the tip of the prosthesis, Type II fractures
originate proximal to the tip and extend distal to it, and Type
III
fractures originate below the tip. Worland et al. considered each
fracture location, fracture obliquity, and implant stability (Fig. 21-26).172
They also made treatment recommendations based on the fracture
classification. Types A, B, and C were designated by the location of
the fracture: A about the tuberosities, B around the stem, and C well
distal to the stem. Type B fractures were subdivided. B1 fractures were
spiral with a stable stem, B2 transverse or short oblique with a stable
stem, and B3 were any fracture associated with a loose stem. Their
recommended treatment was very general, with conservative management or
ORIF recommended for all but B2 and B3 types where long stem revision
was recommended.
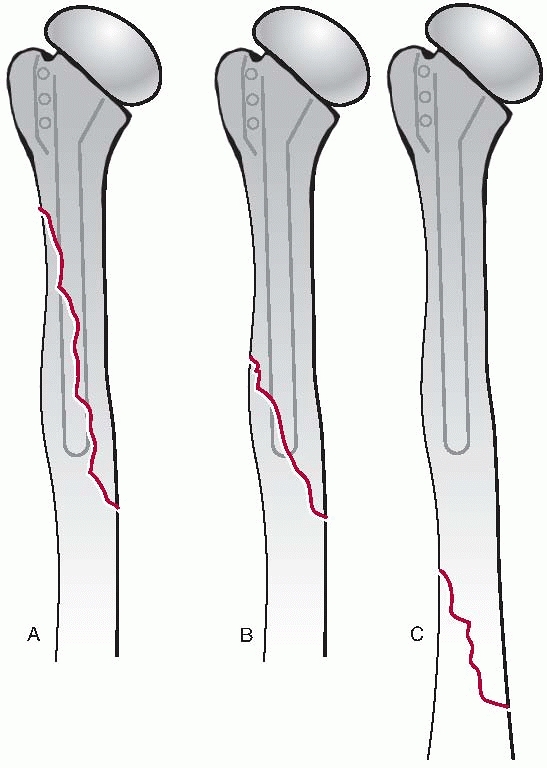 |
|
FIGURE 21-23 The Wright and Cofield classification of periprosthetic humeral fractures.173
|
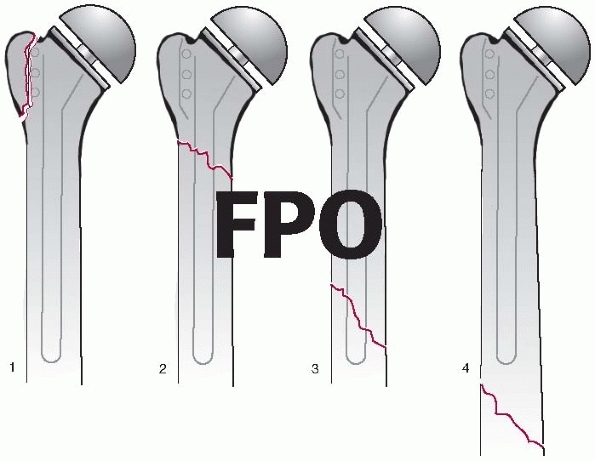 |
|
FIGURE 21-24 The Campbell classification of periprosthetic humeral fractures.19
|
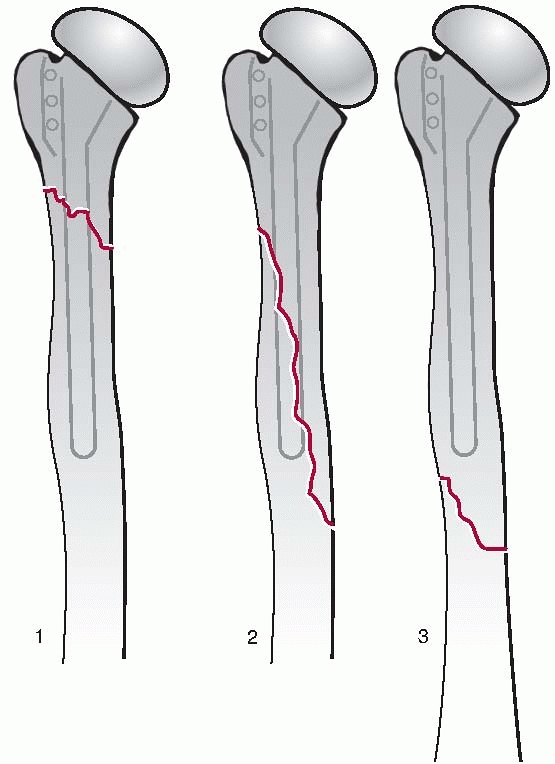 |
|
FIGURE 21-25 Groh classification of periprosthetic humeral fractures.51
|
much as any other periprosthetic fracture, starts with prevention of
intraoperative fracture. Steps include detailed preoperative
planning
particularly with regard to templating stem diameter. This requires
good quality preoperative radiographs taking into account
magnification. Substantive soft tissue releases reduce risk of fracture
by reducing stresses that accompany arm manipulations during
arthroplasty. Capsular contractures as well as scar formations in the
subacromial and subdeltoid spaces should be addressed to allow gentle
delivery of the bone so stress free preparation and implantation can
occur. Proper sizing of the implant and meticulous care to be colinear
with the long axis of the bone during canal preparation will help to
avoid perforation. Small perforations that are diagnosed
intraoperatively can easily be treated with a stem that bypasses the
defect by two or more bone diameters. There should be a low threshold
for intraoperative radiographs to assure a split that propagated
distally did not accompany the perforation, as this might require
additional treatment to stabilize the distal extent of such a fracture.
Non- or minimally displaced fractures of the lesser tuberosity can
occur with some frequency during placement of the trial component.
Treatment of these is generally with suture repair using heavy
nonabsorbable sutures placed through the subscapularis tendon and
either through or around the lesser tuberosity then into the adjacent
intact bone on the other side of the fracture. Similarly, cracks about
the greater tuberosity are stabilized with sutures to assure
displacement does not ensue.
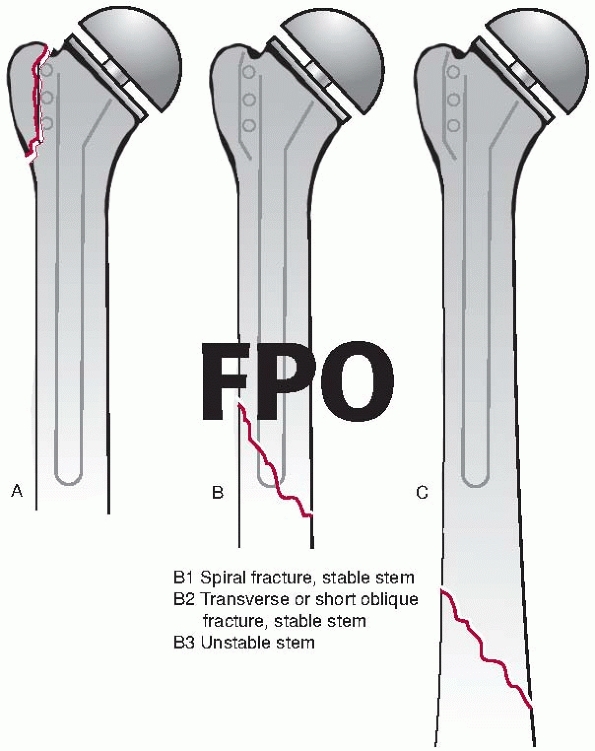 |
|
FIGURE 21-26 Worland classification of periprosthetic humeral fractures.172
|
of uneventful fracture healing and implant stability. This can be
accomplished by a variety of means. Intraoperative fractures of the
shaft are carefully examined with intraoperative radiographs. A long
stemmed noncemented prosthesis with adjunctive cerclage cables are
useful for these spiral fractures. More transverse intraoperative
fractures that are not amenable to cable stabilization are more
appropriately treated with a long stemmed prostheses and either plate
or strut stabilization. When there is compromised bone stock, strut
allografts are utilized.
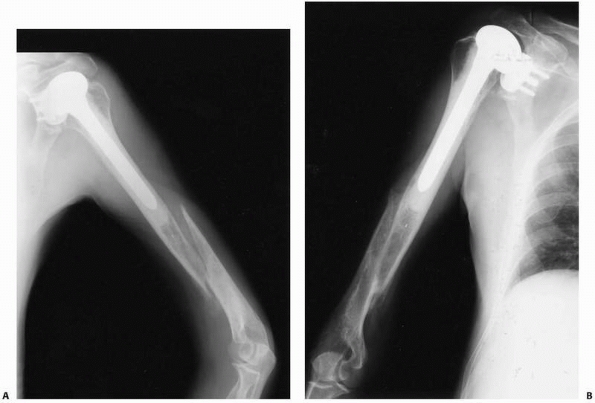 |
|
FIGURE 21-27 A humeral shaft fracture distal to a humeral prosthesis (A) treated nonoperatively to union (B).
|
nonoperatively if the implant is stable and the fracture is otherwise
amenable to bracing (Fig. 21-27). This usually
means the fracture is middiaphyseal, spiral, or short oblique (not
transverse), and there is not drastic displacement, where interposed
muscle may inhibit fracture healing. The results of treating these
fractures nonoperatively is mixed in the literature and some advocate
ORIF in this setting (Fig. 21-28).11,12,19,51,71,78,98,148,172,173 Kumar et al. treated 11 postoperative periprosthetic humeral shaft fractures nonoperatively.78
Six healed uneventfully but five required eventual operative
intervention: three had ORIF with bone grafting and two underwent
revision arthroplasty with a long stem for associated loosening.
Failure of nonoperative management in this series may be related to the
presence of loose implants. Immediate ORIF was performed in only 2
patients with stable prostheses: both had uneventful union. Similarly,
marginal results were reported by Boyd et al. in a small series where
nonunion occurred in 4 of 7 patients treated nonoperatively and radial
nerve palsy occurred in another 2.12 To the contrary, Groh et al. reported union in all five postoperative fractures treated nonoperatively.51
Nonunion after nonoperative treatment is typically managed with a
combination of bone grafting, ORIF, and revision to a long stemmed
arthroplasty.78,173
osteolysis, revision arthroplasty is indicated. A revision stem that
crosses the fracture provides intramedullary stabilization and is
usually accompanied by plate fixation in the absence of bone loss.
Strut grafts (Fig. 21-29), with or without plates are used to restore any associated deficient bone stock. Kumar et al.78
treated five periprosthetic humeral fractures or nonunions after
nonoperative treatment with revision arthroplasty (three with adjuvant
allograft). One of the patients with nonunion had persistent nonunion
after revision arthroplasty and ultimately required free fibular
transfer, further demonstrating the complexity of treating
periprosthetic nonunions.
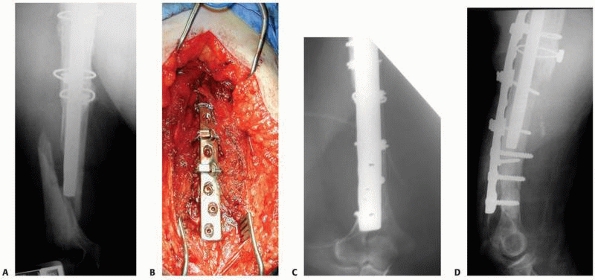 |
|
FIGURE 21-28 A.
A periprosthetic humeral shaft fracture distal to a revision humeral component. The proximal allograft was used previously during the revision arthroplasty. The acute periprosthetic fracture was treated via the posterior approach using biologic reduction techniques seen in an intraoperative photograph (B) that preserved the majority of the soft tissue attachments. C,D. A posterior plate with cables proximally and screws distally were used for fixation. |
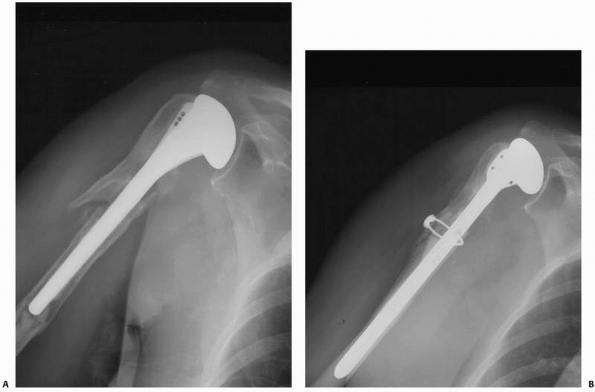 |
|
FIGURE 21-29 Treatment of a periprosthetic humeral shaft fracture associated with a loose prosthesis (A) with a long stem revision, allograft, and a cerclage cable (B).
|
Our preferred exposure is through a posterior approach. This is
extensile and allows visualization of the entire shaft of the humerus.
Furthermore, this exposure allows clear identification and protection
of the radial nerve during reduction, plating, and most importantly
cable fixation in the zone of the prosthesis. Applying cables through
an anterior exposure is dangerous with regard to potential injury and
entrapment of the radial nerve and in our opinion should be avoided. On
occasion, the non- or minimally displaced fracture, especially in
elderly patients that are otherwise poor candidates for surgery, are
treated nonoperatively with a fracture brace. Consideration is given to
the timing of the fracture relative to the arthroplasty. When the
fracture occurs shortly after joint replacement, surgical fixation
offers better capability to perform shoulder rehabilitation and
therefore we tend to treat these fractures operatively.
long stem revision component that bypasses the fracture is used. We
prefer to use noncemented technique whenever there is good quality bone
to provide a reasonably tight fit. We also have a low threshold for
supplemental plate fixation applied using the technique described
above. If either of the fragments has poor quality bone, cemented
technique can be utilized in that fragment (usually the distal
fragment) and noncemented technique in the other. When osteolysis is
severe, either impaction bone grafting technique, an allograft
prosthesis composite, or a tumor prosthesis is utilized. These are
extremely technically demanding cases that are individualized based on
secondary factors and should be undertaken by surgeons and in centers
familiar with and stocked with appropriate equipment, respectively.
occur intraoperatively and are related to retraction. A retractor that
is on the posterior glenoid margin to retract the humerus posteriorly
during preparation of the glenoid articular surface can cause fracture.
Patients undergoing revision surgery and those with severe osteopenia
are at a particularly high risk. Due to the relative rarity of these
fractures and absence of large series dealing with them, no generally
accepted fracture classification exists. Large fragments may be treated
with screws or plates. However, commonly, the fragments are small and
comminuted and are not amenable to screw fixation. With inadequate bone
support, glenoid resurfacing should be abandoned and the defect bone
grafted. After fracture healing, conversion of the hemiarthroplasty to
a total shoulder arthroplasty can be contemplated if symptoms require.
fractures about total elbow prostheses. One notable exception is the
Mayo Clinic experience with 1072 linked Coonrad-Morrey procedures
performed between 1983 and 2003. Periprosthetic fractures occurred with
9% of primary and 23% of revision procedures. These were equally
distributed between fractures of the humerus and those of the ulna (Table 21-5).
Specific risk factors have not been clearly elucidated due to the
relative paucity of published data related to this topic. However, it
is probably safe to consider that systemic or local conditions that
reduce or weaken the bone stock in the proximity to total elbow
arthroplasty (TEAs) would predispose to periprosthetic fracture.
periprosthetic fractures according to fracture location, component
fixation, and bone quality (Fig. 21-30). Type I
fractures are metaphyseal, type II are of the shaft and in the zone of
the stem, and type III are beyond the stem. As popularized by the
Vancouver Classification of periprosthetic femur fractures,
periprosthetic elbow fractures are further subdivided by the status of
the stem fixation. Subtype A fractures are well-fixed, and B fractures
are associated with a loose implant.
arthroplasties depends upon the location and displacement of the
fracture, the time of occurrence (intra- or postoperative), the status
of the implant (well-fixed or loose), and the type of
prosthesis
(constrained or unconstrained). Subtype A fractures are typically
treated by either nonoperative means if non- or minimally displaced,
otherwise they are treated with ORIF. Type B fractures, those with a
loose prosthesis, merit revision arthroplasty.
|
TABLE 21-5 Frequency of Periprosthetic Fractures About Total Elbow Arthroplasty by Anatomic Location
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||
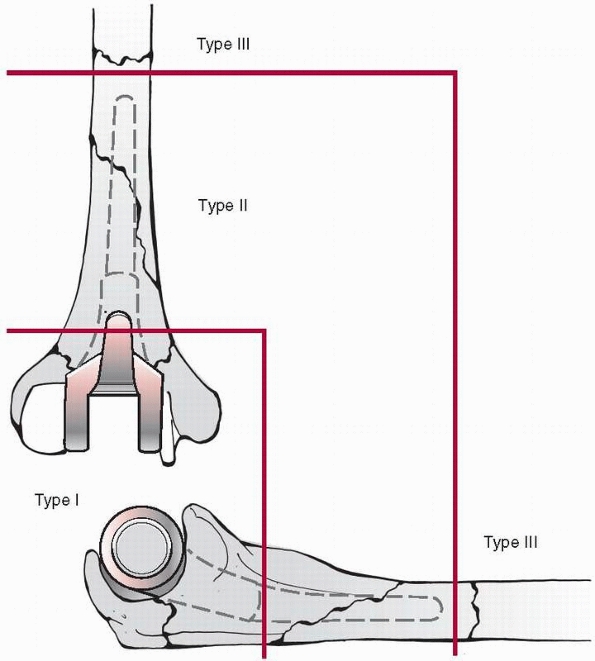 |
|
FIGURE 21-30
The Mayo classification of periprosthetic fractures about total elbow arthroplasty. Type I fractures are metaphyseal, type II involve bone occupied by the implant, and type III fractures extend beyond the stem. The subdivisions of these fractures is presented in the text. |
represent condylar fractures and may occur intraoperatively or
postoperatively. Intraoperative fractures are associated with implant
preparation in the metaphyseal region. Avulsion fracture of either the
medial or lateral condyle can occur with stressing the collateral
ligaments, especially if bone resection was generous. This weakened
area may be subject to spontaneous postoperative fracture or with minor
trauma. Treatment of these fractures depends upon the prosthesis being
used. A linked prosthesis such as the Coonrad-Morray device does not
rely upon the collateral ligaments for stability; therefore, these
fractures with this implant type have little implications regarding
prognosis. Nonoperative management is the mainstay so long as
displacement is not so great to compromise eventual union as nonunion
may cause pain. In the setting of prostheses that rely upon the
collateral ligaments for elbow stability, surgical fixation of these
fractures is indicated. Peer reviewed data for results of these
fractures is lacking.
olecranon or coronoid. Coronoid fractures are very uncommon and usually
occur intraoperatively. If the fragment is large, extends towards the
diaphysis, or compromises ulnar stem fixation, then cable or wire
fixation is performed. Type I fractures involving the olecranon are
more likely to affect function as these fractures may disrupt the
extensor mechanism. Thinning of the olecranon either due to systemic
disease such as from RA or from intraoperative bone resection
predisposes to fracture, and in these instances extreme care must be
taken to avoid critical stress on the olecranon, particularly during
intraoperative forearm manipulation. Postoperative fracture can, of
course, be related to direct trauma but may also occur spontaneously
due to the force generated by triceps muscle contraction when there is
compromised bone. Treatment is generally with ORIF utilizing a tension
band technique for intraoperative fractures. Postoperative fractures
are typically treated nonoperatively unless displacement is greater
than approximately 2 cm. Nonunion has been reported in up to 50% of
these fractures, but fibrous union and lack of displacement of more
than 1 cm has been attributed to the generally good results despite
lack of healing.95
very uncommon. They can theoretically occur at the time of
implantation, especially if a long humeral component is inserted into
an excessively bowed humerus. Fractures around the stem of the implant
are more likely to occur postoperatively and be associated with
osteolysis (type IIB) or with relatively high-energy trauma. Treatment
of these fractures should provide fracture stabilization, restoration
of bone stock, and a stable prosthesis. The treatment principles follow
that for the much more common and extensively studied Vancouver Type B
femoral fractures. In the absence of a loose prosthesis, ORIF with a
strut
allograft
or plate can provide the required stability. When the prosthesis is
loose, implant revision with a long stem that bypasses the fracture
provides intramedullary stability. Unlike the femur where canal filling
fully porous-coated stems is mainstream, long humeral stems do not
reliably provide such stabilization. Therefore, plate or strut fixation
is used. When bone deficiencies are present, strut allografts are
indicated with or without an adjunctive plate. Results of strut
fixation of 11 humeral and 22 ulnar fractures revealed approximately
99% success at 3 to 5 years of both anatomic sites.66,137
are relatively uncommon and are usually associated with trauma and a
loose stem. By definition, these fractures of the humerus are
relatively proximal and may be difficult to control with splints or
braces. Control of such fractures of the ulna is generally easier by
closed means. Operative treatment is indicated for displaced fractures
and those associated with a loose prosthesis (Fig. 21-31).
Goals are to obtain stable fixation, adequate bone stock, and a stable
prosthesis. When revision is indicated, a long stem is inserted across
the fracture if practical. Regardless of stem position, ORIF with
plates and struts are relied on to provide fracture stability.
arthroplasties are generally treated with ORIF with a plate and cable
construct applied through a posterior approach. The critical aspects of
this procedure are identification and protection of the ulnar nerve
distally and the radial nerve proximally. Formal exposure of the median
nerve is generally not necessary as long as great care is taken to pass
cables around the anterior aspect of the distal humerus adjacent to the
anterior surface of the bone. Proximal fixation is with standard screws
or, if the bone is osteoporotic, locked screws. We generally choose a
plate long enough to extend proximal to the radial neurovascular
bundle. The plate is gently slid beneath the bundle and fixed to the
proximal fragment above and below the bundle. Historically, large
fragment broad plates have been advocated for plating humeral
fractures. However, with utilization of modern biologic fracture
reduction techniques, the strength and associated bulk of these
implants is somewhat excessive. We now use narrow large fragment
plates. Occasionally, fractures about the stem of the humeral component
are non- or minimally displaced or the patient is otherwise not a
candidate for surgery. In these cases, nonoperative treatment of the
periprosthetic shaft fracture follows standard means with a fracture
brace. In cases with associated bone loss, strut allografts can be
utilized in lieu of or as an adjunct to a posteriorly applied plate. We
prefer using a strut directly over the zone of bone deficiency and a
plate adjacent to the strut. For periprosthetic ulna fractures, the
strategy is similar. Plates are preferred if there is a stable implant
with no associated bone loss. However, if there is significantly
diminished bone stock, a strut allograft with or without supplemental
plate is typically utilized. Revision arthroplasty is indicated when
there is a loose prosthesis on either side of the joint, osteolysis, or
both.
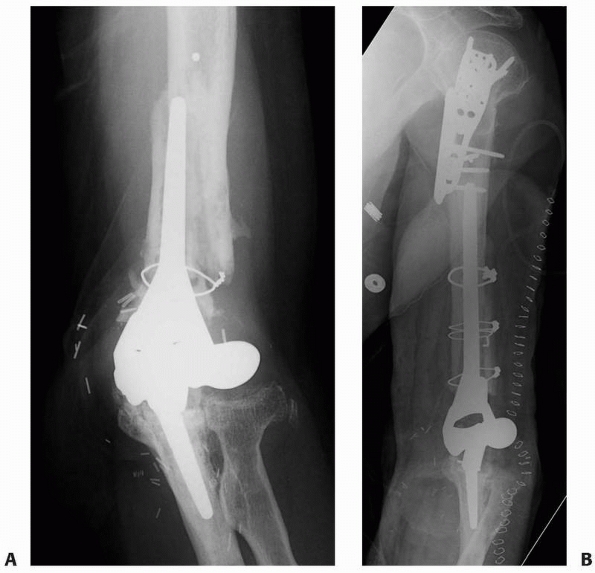 |
|
FIGURE 21-31 A periprosthetic humerus fracture about the humeral component of a total elbow arthroplasty (A) treated with ORIF (B).
|
fractures complicating total ankle arthroplasty (TAA), but no large
series have been published to date clearly elucidating specific
etiological factors or classification schemes.57,81,99,108,135,141,171
One risk factor, however, seems to be clear. Multiple studies have
demonstrated that fracture of the malleoli decrease with increasing
surgeon experience with the procedure. Lee et al.81 and Myerson and Mroczak108
each compared results of their first 25 cases to their next 25. Both
showed substantial reduction in intraoperative malleolar fractures with
experience: Lee et al. had 4 fractures among the first 25 cases (16%)
and 1 in the subsequent 25 (4%), and Myerson and Mroczak had 5 from the
initial group (20%) and 2 from the second group (8%). These results are
similar to those of several other authors. Haskell and Mann57
found a reduction in intraoperative fracture from 12% in the initial 50
cases to 9% in the subsequent 137 cases, and Schuberth et al.141 reported 19 intraoperative fractures from 50 cases (38%) and noted that this complication decreased with experience.
intraoperative fracture, occurring approximately twice as frequently as
lateral malleolus fractures.57,99,135,171
The vast majority of periprosthetic fractures about TAAs occur
intraoperatively; however, postoperative malleolar fracture has been
reported.57,99,171 Wood and Deakin171
had 10 postoperative fractures occur between 3 days and 23 months in
their series of 200 TAAs. Two of the 10 were associated with implant
loosening.
periprosthetic fractures about TAA. However, the general principles of
management of other periprosthetic fractures can be applied. Fracture
union, implant stability, and re-establishment of any associated loss
of bone stock are general goals of management with the hope of
restoring baseline function. Several authors describe internal fixation
for intraoperative malleolar fractures that compromised implant
stability,57,99 and yet others treated many of these fractures nonoperatively.81,108,171 Nonunion occurred after intraoperative fracture in 1 of 6 nonoperatively treated from one study57 and in 1 of 5 treated with ORIF from another.99
Most postoperative fractures are also of the malleolus and are
typically treated nonoperatively unless associated with implant
loosening or osteolysis.57,99,171
compilation of the typical complication seen after acute fracture
through native bone and the complications associated with joint
arthroplasty. Such complications can occur in isolation or in
combination. Clearly, treatment must consider both the implications
relative to the periprosthetic fracture and the implication with regard
to arthroplasty stability and function. It is sometimes useful to
prioritize the goals of treatment and decide if outcome for the
periprosthetic fracture is paramount or if preservation of the
arthroplasty function is the primary goal. These are sometimes
conflicting goals.
associated with periprosthetic fractures. Nonunion rates for
periprosthetic fracture fixation is generally higher than the rate for
treatment of the same fracture in the absence of a prosthesis. It has
been postulated that damage to the endosteal blood supply related to
the intramedullary implant could alter the healing response to
fracture, but this remains theory. A more influential cause of higher
nonunion rates is the potentially compromised fixation caused by the
prosthesis inhibiting optimal fixation. Cable fixation is the mainstay
for plate or strut fixation around the zone of prostheses and has
inferior strength compared to bicortical screws. However, advances in
surgical technique and implant technologies have led to recent
improvement in union rates. These advancements include biologic
reduction techniques and locked plates where locking screws augment
cable fixation in the zone of the implant and also augment fixation
when osteopenic bone is encountered. Treatment of nonunion can be
extremely challenging. Results of nonunion repair of periprosthetic
fracture are marginal. A multimodal approach is required.64
Correction of any systemic processes that could inhibit fracture
healing is done prior to nonunion repair. This consists of smoking
cessation, discontinuation of nonsteroidal anti-inflammatory drugs,
strict control of diabetes, and discontinuation of any other
dispensable medications that could alter bone metabolism. Operative
strategies include utilization of long stem prostheses in conjunction
with extramedullary strut and plate fixation. Generous use of
osteogenic and osteoinductive grafts and graft substitutes are
imperative. Autologous iliac crest bone graft remains the criterion
standard, but supplementation with BMP is a growing part of the
armamentarium for these difficult cases. It goes without saying that
restoration of anatomic limb alignment is another critical step.
fractures is reported in a number of series especially with fixation of
humeral fractures. One partial radial and two partial ulnar nerve
pulses were reported in a series of 11 periprosthetic humeral shaft
fractures.137 The proximity of the
radial and ulnar nerves to the fracture, the fixation devices, and
securing cerclage cables put these structures at particular risk for
injury. The best strategy for dealing with neurologic injury is one
based on prevention. Appropriate choice of surgical approach is the
first step. We prefer to directly expose any and all nerves that are
potentially compromised. Therefore, the posterior approach is preferred
for access to the humeral shaft. This way, the radial nerve is
precisely located and can be protected throughout the procedure. Gentle
soft tissue handling is also important with avoidance of forceful or
prolonged retraction of nerves. Passing cerclage cables can be a
harrowing experience. There is no substitute for knowledge of nerve
location and direct protection during passage of cables.
when infection is associated with periprosthetic fracture it can be
particularly devastating. Not only is fracture healing compromised but
also the survivorship of the associated arthroplasty. Relatively
aggressive early surgical treatment with irrigation and débridement and
parental organism specific antibiotics followed by long-term oral
suppression has a potential to spare the fracture fixation and
arthroplasty implants. Failure to control infection can have serious
results including resection arthroplasty or amputation at or above the
involved joint.
temporary or permanent stiffness of the involved joint due to
contracture and scar of the surrounding soft tissues from the original
injury as well as from the trauma of surgery. Immobilization of the
joint as part of fracture care can compound the tendency for stiffness.
These issues are also relevant to the treatment of periprosthetic
fractures. Fortunately, by nature most periprosthetic fractures are at
some distance from the involved joint and by definition are not
intraarticular. Nevertheless, every effort should be made to obtain
stable enough fixation to minimize the requirement for joint
immobilization and to allow as early as possible range of motion
exercises.
S, Elliott DS. Percutaneous plate fixation for periprosthetic femoral
fractures —a preliminary report. Injury 2000;31:627-630.
PL, Lee MA, Finkemeier CG, et al. Operative stabilization of
supracondylar femur fractures above total knee arthroplasty: a
comparison of four treatment methods. J Arthroplasty 2003;18:834-839.
P, Barrack RL, Harris WH. Stress fracture of the medial wall of the
acetabulum adjacent to a cementless acetabular component. J
Arthroplasty 2002;17:117-120.
JS, III, DeAndrade JR, Fleming LL, et al. Proximal femoral fractures
following total hip arthroplasty. Clin Orthop Relat Res 1982;95-106.
T, Chang D, Meigs JB, et al. Mortality after periprosthetic fracture of
the femur. J Bone Joint Surg Am 2007;89:2658-2662.
E, Hastings D, Gross A, et al. Supracondylar fractures of the femur
adjacent to resurfacing and MacIntosh arthroplasties of the knee in
patients with rheumatoid arthritis. Clin Orthop Relat Res 1988;213-220.
PM, Hawkins RJ. Fracture of the humeral shaft associated with total
replacement arthroplasty of the shoulder. A case report. J Bone Joint
Surg Am 1992;74:617-618.
OH, Garbuz DS, Masri BA, et al. The treatment of periprosthetic
fractures of the femur using cortical onlay allograft struts. Orthop
Clin North Am 1999;30:249-257.
OH, Garbuz DS, Masri BA, et al. The reliability and validity of the
Vancouver classification of femoral fractures after hip replacement. J
Arthroplasty 2000;15:59-62.
MA, Farfalli G, Paredes NM, et al. Locking compression plate fixation
of Vancouver type-B1 periprosthetic femoral fractures. J Bone Joint
Surg Am 2007;89: 1964-1969.
PR, Rubash HE, Wissinger HA, et al. Periprosthetic femoral fractures
following total knee arthroplasty. Clin Orthop Relat Res 1986;205-214.
HU, Jung YB. Noncemented stem tibial component in total knee
replacement: the 2- to 6-year results. Can J Surg 1993;36:555-559.
JT, Moore RS, Iannotti JP, et al. Periprosthetic humeral fractures:
mechanisms of fracture and treatment options. J Shoulder Elbow Surg
1998;7:406-413.
BE, Tsiridis E, Tragas AA, et al. Management of periprosthetic patellar
fractures. A systematic review of literature. Injury 2007;38:714-724.
HP, King D, Limbird R, et al. The use of cortical allograft struts for
fixation of fractures associated with well-fixed total joint
prostheses. Semin Arthroplasty 1993; 4:99-107.
HP, Tigges RG. The role of allografts in the treatment of
periprosthetic femoral fractures. Instr Course Lect 1998;47:257-264.
M, Parfitt J, Pearse MF: Periprosthetic acetabular fracture associated
with extensive osteolysis. J Arthroplasty 1998;13:843-845.
MG, Ballance J, Brick GW, et al. The use of structural allograft for
uncontained defects in revision total knee arthroplasty. A minimum
five-year review. J Bone Joint Surg Am 2001;83-A:404-411.
RE, Jenkins PJ, Walmsley PJ, et al. Risk factors for periprosthetic
fractures of the hip: a survivorship analysis. Clin Orthop Relat Res
2008;466:1652-1656.
A. Stress fractures of the pelvis as a cause of hip pain following
total hip and knee arthroplasty. Arthritis Rheum 1981;24:740-742.
RW, Schmidt RG, Hanks G, et al. Supracondylar fracture of the femur
following prosthetic knee arthroplasty. Clin Orthop Relat Res
1987;212-222.
J, Malkani A, Paiso JM. Supracondylar distal femoral nonunions treated
with a megaprosthesis in elderly patients: a report of two cases. J
Orthop Trauma 2001;15: 574-578.
BL. Varus collapse of comminuted distal femur fractures after open
reduction and internal fixation with a lateral condylar buttress plate.
Am J Orthop 2003;32: 27-30.
Valle CJ, Momberger NG, Paprosky WG. Periprosthetic fractures of the
acetabulum associated with a total hip arthroplasty. Instr Course Lect
2003;52:281-290.
MG, Simon JA, Kummer FJ, et al. Fixation of periprosthetic femoral
shaft fractures: a biomechanical comparison of two techniques. J Orthop
Trauma 2001;15: 177-180.
MG, Simon JA, Kummer FJ, et al. Fixation of periprosthetic femoral
shaft fractures occurring at the tip of the stem: a biomechanical study
of 5 techniques. J Arthroplasty 2000;15:523-528.
GA, Ammeen DJ. Periprosthetic fractures adjacent to total knee
implants: treatment and clinical results. Instr Course Lect
1998;47:437-448.
GL, Buttaro MA, Piccaluga F. Femoral fractures in revision hip
surgeries with impacted bone allograft. Clin Orthop Relat Res
2007;462:130-136.
NA, Stuart MJ, Hanssen AD. Periprosthetic fractures of the tibia
associated with total knee arthroplasty. Clin Orthop Relat Res
1997;113-124.
HE, III, Goldberg VM, Figgie MP, et al. The effect of alignment of the
implant on fractures of the patella after condylar total knee
arthroplasty. J Bone Joint Surg Am 1989;71:1031-1039.
MP, Goldberg VM, Figgie HE, III, et al. The results of treatment of
supracondylar fracture above total knee arthroplasty. J Arthroplasty
1990;5:267-276.
AP, Thompson NW, Wong J, et al. Periprosthetic femoral fractures—a
comparison between cemented and uncemented hemiarthroplasties. Injury
2005;36:424-429.
EL, Hak DJ, Johnson EE, et al. Total knee replacement including a
modular distal femoral component in elderly patients with acute
fracture or nonunion. J Orthop Trauma 1995;9:231-237.
E, Koval K, Preston CF, et al. Fixation of periprosthetic femoral shaft
fractures associated with cemented femoral stems: a biomechanical
comparison of locked plating and conventional cable plates. J Orthop
Trauma 2006;20:89-93.
E, Munuera L, Gil-Garay E. Femoral shaft fractures after cemented total
hip arthroplasty. Int Orthop 1992;16:97-100.
C, Rafiq M, Henry AP. Treatment of femoral fracture above a knee
prosthesis. 18 cases followed 0.5-14 years. Acta Orthop Scand
1994;65:610-614.
J, Megas P, Panagiotopoulos E, et al. Midterm results of treatment with
a retrograde nail for supracondylar periprosthetic fractures of the
femur following total knee arthroplasty. J Orthop Trauma
2005;19:164-170.
VM, Figgie HE III, Inglis AE, et al. Patellar fracture type and
prognosis in condylar total knee arthroplasty. Clin Orthop Relat Res
1988;115-122.
GI, Heckman MM, Wirth MA, et al. Treatment of fractures adjacent to
humeral prostheses. J Shoulder Elbow Surg 2008;17:85-89.
FS, Duncan CP, Berry DJ, et al. Periprosthetic femoral fractures around
well-fixed implants: use of cortical onlay allografts with or without a
plate. J Bone Joint Surg Am 2002;84-A:945-950.
FS, Marston RA, Muirhead-Allwood SK. The Dall-Miles cable and plate
system for periprosthetic femoral fractures. Injury 1997;28:445-447.
GJ, Jacofsky DJ, Hanssen AD, et al. Intraoperative fractures of the
acetabulum during primary total hip arthroplasty. J Bone Joint Surg Am
2006;88:1952-1956.
DC, Delince PE, Yasik E, et al. Stress fracture of the hip. An unusual
complication of total knee arthroplasty. Clin Orthop Relat Res
1992;140-144.
A, Mann RA. Perioperative complication rate of total ankle replacement
is reduced by surgeon experience. Foot Ankle Int 2004;25:283-289.
WL, Wasilewski SA, Takei R, et al. Patellofemoral complications
following total knee arthroplasty. Correlation with implant design and
patient risk factors. J Arthroplasty 1995;10:197-201.
DA, Kregor PJ, Cole PA, et al. Treatment of acute distal femur
fractures above a total knee arthroplasty: systematic review of 415
cases (1981-2006). Acta Orthop 2008;79:22-27.
DM, Bhalla S, Roffman M. Supracondylar fracture of the femur following
total knee replacement. Report of four cases. J Bone Joint Surg Am
1981;63:162-163.
CE. The role of blood supply to soft tissue in the healing of
diaphyseal fractures. An experimental study. J Bone Joint Surg Am
1972;54:993-1000.
WJ, Goll SR, Lotke PA, et al. The treatment of patellar fractures after
total knee arthroplasty. Clin Orthop Relat Res 1988;123-127.
SJ, Beard DM, Pupparo F, et al. One-stage revision of periprosthetic
fractures around loose cemented total hip arthroplasty. Am J Orthop
1998;27:35-41.
MM, Ricci WM, Borrelli J Jr, et al. A protocol for treatment of
unstable ankle fractures using transarticular fixation in patients with
diabetes mellitus and loss of protective sensibility. Foot Ankle Int
2003;24:838-844.
JE, McBroom R, Barrington TW, et al. Fracture of the ipsilateral femur
in patients wih total hip replacement. J Bone Joint Surg Am
1981;63:1435-1442.
S, Morrey BF. Proximal ulnar reconstruction with strut allograft in
revision total elbow arthroplasty. J Bone Joint Surg Am
2004;86-A:1223-1229.
A, Ince A, Wodtke J, et al. Component exchange in treatment of
periprosthetic femoral fractures. J Arthroplasty 2006;21:572-579.
CF, Boscainos PJ, Maury AC, et al. Proximal femoral allograft treatment
of Vancouver type-B3 periprosthetic femoral fractures after total hip
arthroplasty. Surgical technique. J Bone Joint Surg Am 2007;89(Suppl 2
Pt1):68-79.
DH, Clavert P, Warner JJ. Displaced periprosthetic humeral fracture
treated with functional bracing: a report of two cases. J Shoulder
Elbow Surg 2005;14:221-223.
GR, Parvizi J, Rapuri V, et al. Proximal femoral replacement for the
treatment of periprosthetic fractures. J Bone Joint Surg Am
2005;87:1777-1781.
MJ, Goldberg VM, Figgie MP, et al. Distal femoral replacement with
allograft/prosthetic reconstruction for treatment of supracondylar
fractures in patients with total knee arthroplasty. J Arthroplasty
1992;7:7-16.
PJ, Stannard JA, Zlowodzki M, et al. Treatment of distal femur
fractures using the less invasive stabilization system: surgical
experience and early clinical results in 103 fractures. J Orthop Trauma
2004;18:509-520.
KJ, Scuderi GR, Windsor RE, et al. Treatment of Nonunions About the
Knee Utilizing Custom Total Knee Arthroplasty With Press-fit
Intramedullary Stems. J Arthroplasty 1995;8(1):49-55.
A, Chambers I, Wong P. Periprosthetic fracture of the proximal tibia
after lateral unicompartmental knee arthroplasty. J Arthroplasty
2008;23:615-618.
S, Sperling JW, Haidukewych GH, et al. Periprosthetic humeral fractures
after shoulder arthroplasty. J Bone Joint Surg Am 2004;86-A:680-689.
DA, Rack C, Rutt J. Subtrochanteric stress fracture of the femur
following total knee arthroplasty. J Arthroplasty 1997;12:580-583.
GC, Nelson CL, Virmani S, et al. Management of periprosthetic femur
fractures with severe bone loss using impaction bone grafting
technique. J Arthroplasty 2009.
KB, Cho SG, Hur CI, et al. Perioperative complications of HINTEGRA
total ankle replacement: our initial 50 cases. Foot Ankle Int
2008;29:978-984.
ML, Schneider DJ, Deol G, et al. The consequences of anterior femoral
notching in total knee arthroplasty. A biomechanical study. J Bone
Joint Surg Am 2000;82-A: 1096-1101.
PJ, Testa NN. Stress fracture of the hip as a complication of total
knee replacement. Case report. J Bone Joint Surg Am 1982;64:304-306.
DG, Berry DJ. Periprosthetic fracture of the femur after total hip
arthroplasty: treatment and results to date. Instr Course Lect
1998;47:243-249.
PL, Rorabeck CH. Periprosthetic Fractures. In: Engh GA, Rorabeck CH,
Eds. Revision total knee arthroplasty. Baltimore: Williams &
Wilkins; 2007:275-295.
CH, Chen TH, Su YP, et al. Periprosthetic femoral supracondylar
fracture after total knee arthroplasty with navigation system. J
Arthroplasty 2008;23:304-307.
H, Garellick G, Regner H, et al. Three hundred and twenty-one
periprosthetic femoral fractures. J Bone Joint Surg Am
2006;88:1215-1222.
H, Malchau H, Herberts P, et al. Periprosthetic femoral fractures
classification and demographics of 1049 periprosthetic femoral
fractures from the Swedish National Hip Arthroplasty Register. J
Arthroplasty 2005;20:857-865.
H, Oden A, Garellick G, et al. The excess mortality due to
periprosthetic femur fracture. A study from the Swedish national hip
arthroplasty register. Bone 2007;40: 1294-1298.
RN, Umlas ME, Rodriguez JA, et al. Supracondylar femoral fracture above
a PFC posterior cruciate—substituting total knee arthroplasty treated
with supracondylar nailing. A unique technical problem. J Arthroplasty
1996;11:637-639.
M, Konrad G, Sudkamp N. Femur-LISS and distal femoral nail for fixation
of distal femoral fractures: are there differences in outcome and
complications? Clin Orthop Relat Res 2004;252-257.
G, Morrey BF, Gallay SH, et al. Fracture and nonunion of the olecranon
in total elbow arthroplasty. J Shoulder Elbow Surg 2006;15:486-494.
AC, Pressman A, Cayen B, et al. Proximal femoral allograft treatment of
Vancouver type-B3 periprosthetic femoral fractures after total hip
arthroplasty. J Bone Joint Surg Am 2006;88:953-958.
WC, Clanton TO, Lunz D. Malleolar fracture after total ankle
arthroplasty: a comparison of two designs. Clin Orthop Relat Res
2004;104-110.
RM, Garbuz DS, Masri BA, et al. Intraoperative fracture of the femur in
revision total hip arthroplasty with a diaphyseal fitting stem. J Bone
Joint Surg Am 2004;86-A:480-485.
WE, Wretenberg PF, Weidenhielm LR, et al. Complex cemented revision
using polished stem and morselized allograft.Minimum 5-years’
follow-up. Arch Orthop Trauma Surg 1999;119:288-291.
MA, Maar DC. Fractures of the ipsilateral femur after hip arthroplasty.
A statistical analysis of outcome based on 487 patients. J Arthroplasty
1994;9:511-519.
MC, Brick GW, Sledge CB, et al. Supracondylar femoral fracture
following total knee arthroplasty. Clin Orthop Relat Res 1996;196-209.
BF, Kavanagh BF. Complications with revision of the femoral component
of total hip arthroplasty. Comparison between cemented and uncemented
techniques. J Arthroplasty 1992;7:71-79.
C, Rayan F, Kheir E, Macdonald D. Management of late periprosthetic
femur fractures: a retrospective cohort of 72 patients. Int Orthop 2009.
S, Hassan T, Birtwistle S, et al. Management of types B2 and B3 femoral
periprosthetic fractures by a tapered, fluted, and distally fixed stem.
J Arthroplasty 2005;20: 751-756.
K, Quinlan JF, Kutty S, et al. The use of uncemented extensively
porous-coated femoral components in the management of Vancouver B2 and
B3 periprosthetic femoral fractures. J Bone Joint Surg Br
2005;87:1617-1621.
MD, Albareda J, Seral F. Subcapital stress fracture of the femoral neck
after total knee arthroplasty. Int Orthop 1994;18:308-309.
SM, Linke B, Schwieger K, et al. Aspects of internal fixation of
fractures in porotic bone. Principles, technologies and procedures
using locked plate screws. Acta Chir Orthop Traumatol Cech
2005;72:89-97.
CL, Hennessey R, Barden RM, et al. Revision total knee arthroplasty
with a cemented posterior—stabilized or constrained condylar
prosthesis: a minimum 3-year and average 5-year follow-up study. J
Arthroplasty 1997;12:896-903.
MM, Lauritzen JB, Pedersen JG, et al. Decreased bone density of the
distal femur after uncemented knee arthroplasty. A 1-year follow-up of
29 knees. Acta Orthop Scand 1996;67:339-344.
MM, Olsen C, Lauritzen JB, et al. Changes in bone mineral density of
the distal femur following uncemented total knee arthroplasty. J
Arthroplasty 1995;10: 7-11.
CA, Lewallen DG. Periprosthetic fracture of the acetabulum after total
hip arthroplasty. J Bone Joint Surg Am 1996;78:1206-1213.
J, Macholz F, Merkert W, et al. [Results and complications in the
treatment of periprosthetic femur fractures with a locked plate
system.] Unfallchirurg 2009.
ML, Patsalis T, Gregg PJ. Subcapital stress fractures of the hip
complicating total knee replacement. Injury 1995;26:421-423.
WM, Bolhofner BR, Loftus T, et al. Indirect reduction and plate
fixation, without grafting, for periprosthetic femoral shaft fractures
about a stable intramedullary implant. J Bone Joint Surg Am
2005;87:2240-2245.
WM, Borrelli J Jr. Operative management of periprosthetic femur
fractures in the elderly using biological fracture reduction and
fixation techniques. Injury 2007; 38(Suppl 3):S53-58.
WM, Loftus T, Cox C, et al. Locked plates combined with minimally
invasive insertion technique for the treatment of periprosthetic
supracondylar femur fractures above a total knee arthroplasty. J Orthop
Trauma 2006;20:190-196.
MA, Campbell ED. Postoperative patellar complications with or without
lateral release during total knee arthroplasty. Clin Orthop Relat Res
1987;163-168.
MA, Carr K, Keating EM, Faris PM, Meding JB. Tibial shaft fracture
following tibial tubercle osteotomy. J Arthroplasty 1996;11:117-119.
MA, Faris PM, Keating EM. Anterior femoral notching and ipsilateral
supracondylar femur fracture in total knee arthroplasty. J Arthroplasty
1988;3:185-187.
MA, Thong AE, Keating EM, et al. The effect of femoral notching during
total knee arthroplasty on the prevalence of postoperative femoral
fractures and on clinical outcome. J Bone Joint Surg Am
2005;87:2411-2414.
DE, Lee MB, Smith EJ, et al. Femoral impaction grafting in revision hip
arthroplasty with irradiated bone. J Arthroplasty 2002;17:834-840.
CH, Taylor JW. Classification of periprosthetic fractures complicating
total knee arthroplasty. Orthop Clin North Am 1999;30:209-214.
CH, Taylor JW. Periprosthetic fractures of the femur complicating total
knee arthroplasty. Orthop Clin North Am 1999;30:265-277.
CL, Amendola A, Anderson R, et al. Surgeon training and complications
in total ankle arthroplasty. Foot Ankle Int 2003;24:514-518.
J, McGrory BJ, Berry DJ. Acute periprosthetic fracture of the
acetabulum associated with osteolytic pelvic lesions: a report of 3
cases. J Arthroplasty 2000;15: 126-130.
J, O’Driscoll S, Morrey BF. Periprosthetic humeral fractures after
total elbow arthroplasty: treatment with implant revision and strut
allograft augmentation. J Bone Joint Surg Am 2002;84-A:1642-1650.
R, Huhtala H, Pajamaki J. Young age and wedge stem design are risk
factors for periprosthetic fracture after arthroplasty due to hip
fracture. A case-control study. Acta Orthop 2005;76:56-60.
R, Huhtala HS, Sovelius RT, et al. Factors predisposing to
periprosthetic fracture after hip arthroplasty: a case (n = 31)-control
study. Acta Orthop Scand 2004;75:16-20.
P, Partenheimer A, Koenemann B, et al. Distal femoral fractures and
LISS stabilization. Injury 2001;32(Suppl 3):SC55-63.
JM, Patel S, Zarutsky E. Perioperative complications of the Agility
total ankle replacement in 50 initial, consecutive cases. J Foot Ankle
Surg 2006;45:139-146.
M, Muller M, Krettek C, et al. Minimally invasive fracture
stabilization of distal femoral fractures with the LISS: a prospective
multicenter study. Results of a clinical study with special emphasis on
difficult cases. Injury 2001;32(Suppl 3):SC48-54.
JT Jr, Mayer JG, Engh CA. Femoral fracture during non-cemented total
hip arthroplasty. J Bone Joint Surg Am 1989;71:1135-1142.
RD, Turoff N, Ewald FC. Stress fracture of the patella following
duopatellar total knee arthroplasty with patellar resurfacing. Clin
Orthop Relat Res 1982;147-151.
PF, Hozack WJ, Callaghan JJ, et al. Acetabular fracture associated with
cementless acetabular component insertion: a report of 13 cases. J
Arthroplasty 1999; 14:426-431.
BD, Berry DJ, Cabanela ME, et al. Early postoperative transverse pelvic
fracture: a new complication related to revision arthroplasty with an
uncemented cup. J Bone Joint Surg Am 2005;87:2626-2631.
SP, Cheung EV. Treatment of periprosthetic humerus fractures associated
with shoulder arthroplasty. J Am Acad Orthop Surg 2008;16:199-207.
ET, DeWal H, Di Cesare PE. Periprosthetic femoral fractures above total
knee replacements. J Am Acad Orthop Surg 2004;12:12-20.
TS, Nanu AM, Buchanan MJ, et al. Dall-Miles plating for periprosthetic
B1 fractures of the femur. J Arthroplasty 2000;15(1):47-51.
MM, Meyers MH, Harvey JP Jr. Intraoperative femur fractures during
total hip replacement. Clin Orthop Relat Res 1978;96-103.
NW, McAlinden MG, Breslin E, et al. Periprosthetic tibial fractures
after cementless low contact stress total knee arthroplasty. J
Arthroplasty 2001;16:984-990.
AJ Jr, Harwood DA, Alicea JA, et al. Patellar fractures in posterior
stabilized knee arthroplasties. Clin Orthop Relat Res 1994;131-138.
E, Amin MS, Charity J, et al. Impaction allografting revision for B3
periprosthetic femoral fractures using a Mennen plate to contain the
graft: a technical report. Acta Orthop Belg 2007;73:332-338.
E, Haddad FS, Gie GA. The management of periprosthetic femoral
fractures around hip replacements. Injury 2003;34:95-105.
E, Narvani AA, Haddad FS, et al. Impaction femoral allografting and
cemented revision for periprosthetic femoral fractures. J Bone Joint
Surg Br 2004;86:1124-1132.
E, Spence G, Gamie Z, et al. Grafting for periprosthetic femoral
fractures: strut, impaction or femoral replacement. Injury
2007;38:688-697.
Loon P, de Munnynck B, Bellemans J. Periprosthetic fracture of the
tibial plateau after unicompartmental knee arthroplasty. Acta Orthop
Belg 2006;72:369-374.
KM, Koka R, Garikipati R, et al. Dall-Miles cable and plate fixation
for the treatment of peri-prosthetic femoral fractures—analysis of
results in 13 cases. Injury 2001; 32:395-400.
CJ, Wang JW, Weng LH, et al. The effect of alendronate on bone mineral
density in the distal part of the femur and proximal part of the tibia
after total knee arthroplasty. J Bone Joint Surg Am 2003;85-A:2121-2126.
LM, Kim JK, Mehta M, et al. Complications of total hip arthroplasty: MR
imaging-initial experience. Radiology 2000;215:254-262.
M, Muller EJ, Kutscha-Lissberg F, et al. [Periprosthetic supracondylar
femoral fractures: LISS or retrograde intramedullary nailing? Problems
with the use of minimally invasive technique]. Unfallchirurg
2004;107:181-188.
FC, Venters GC. Results of knee replacement with the Walldius
prosthesis: an interim report. Clin Orthop Relat Res 1976;39-46.
P, Gross AE. The use of structural allografts for treating
periprosthetic fractures about the hip and knee. Orthop Clin North Am
1999;30:259-264.
RL, Kim DY, Arredondo J. Periprosthetic humeral fractures: management
and classification. J Shoulder Elbow Surg 1999;8:590-594.
CC, Au MK, Wu SS, et al. Risk factors for postoperative femoral
fracture in cementless hip arthroplasty. J Formos Med Assoc
1999;98:190-194.
SW, Walker CG, Pitto RP. Functional outcome of femoral peri prosthetic
fracture and revision hip arthroplasty: a matched-pair study from the
New Zealand Registry. Acta Orthop 2008;79:483-488.
SH, Sadiq S, Purbach B, et al. Periprosthetic femoral fractures treated
with a modular distally cemented stem. J Orthop Surg (Hong Kong)
2007;15:163-166.
P, Backstein D, Gross AE, et al. Notching of the anterior femoral
cortex during total knee arthroplasty characteristics that increase
local stresses. J Arthroplasty 2006; 21:737-743.
P, Gandhi R, Petruccelli D, et al. Fractures at the tip of long-stem
prostheses used for revision hip arthroplasty. J Arthroplasty
2003;18:741-745.
R, Walker R, Waddell JP, et al. Biomechanical evaluation of
periprosthetic femoral fracture fixation. J Bone Joint Surg Am
2008;90:1068-1077.
EJ Jr, Pomeroy DL, Caudle RJ Ogden plate and other fixations for
fractures complicating femoral endoprostheses. Clin Orthop 1988;83-90.
