Sympathetic Blocks
Diagnosis and treatment of sympathetically mediated pain of the face,
neck, and upper extremity; treatment of postherpetic neuralgia of the
cervical dermatomes.
Stellate ganglion, which is composed of the fusion of C7 and T1
sympathetic ganglia, which lies anterior to the transverse process of
C7 and T1 on the anterior surface of the longus colli muscles, lateral
to the trachea and esophagus, anteromedial to the vertebral artery, and
medial to the common carotid artery. The block is performed lateral to
the cricoid cartilage at the level of the C6 transverse process
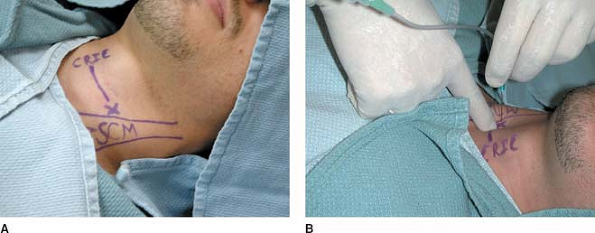
(Chassaignac tubercle) (Fig. 63-1A).
Prepare the skin with a sterile solution lateral to the cricoid
cartilage. Insert the needle perpendicular to the skin plane
approximately one fingerbreadth lateral to the cricoid cartilage to
make contact with the C6 transverse process (Fig. 63-1B).
After negative aspiration, inject 0.5 mL of 0.25% bupivacaine test
dose. After the negative aspiration and the injection of a test dose,
inject the remaining 5 to 10 mL of 0.25% bupivacaine. Under
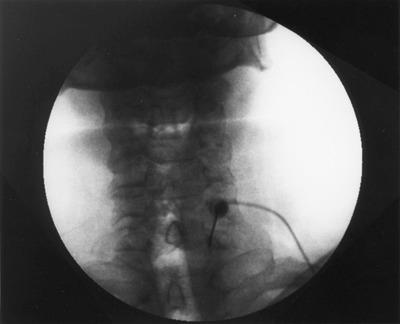
fluoroscopy, insert the needle at the junction of the transverse
process and the C7 vertebral body (Fig. 63-2). Use 2 mL of Isovue-200 (Bracco Diagnostics, Princeton, NJ) for verification of needle position. Figure 63-3 presents an anteroposterior (A) and lateral view (B).
 |
|
Figure 63-1. Stellate ganglion block anatomic landmarks.
|
 |
|
Figure 63-2. Insert the needle at the junction of the transverse process and the C7 vertebral body.
|
 |
|
Figure 63-3. A: Anteroposterior view. B: Lateral view.
|
Bleeding, infection, intravascular injection, pneumothorax, hoarseness
and dysphagia, and epidural, subdural, or subarachnoid injection.
-
Application of routine monitors, including blood pressure and pulse oxygen, is required.
-
Having the patient’s mouth slightly open decreases skin tension and facilitates palpation of the landmarks.
-
To avoid the risk for aspiration, the
patient should avoid oral intake for 4 to 6 hours after the block and
then resume with clear liquids as tolerated.
For diagnostic purposes: 15–20 cc of bupivacaine 0.5%, lidocaine 2%, or
ropivacaine 0.5%. For neurolysis: 10–15 cc of alcohol 50–100% or phenol
6.5%.
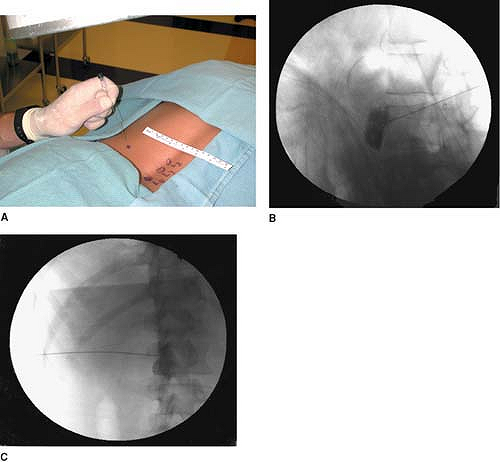
vertebral body. A slight cephalad–caudad tilt of the beam may be
necessary to square the endplates. This point should be marked and is
approximately 6–8 cm from midline. After skin wheal and deep
infiltration of local anesthetics, advance the needle parallel to the
x-ray beam. Of great importance is taking frequent AP views to assess
needle direction and lateral views (Fig. 63-4B)
to assess depth. Once the anterior third of the vertebral body is
reached, the stylet is removed from the needle and 0.1 cc–0.2 cc of
PFNS is injected to occupy the needle and prevent air embolization.
Once the aorta is pierced, very gentle aspiration is continuously
applied until negative aspiration for blood. Advance 2–3 mm. Inject a
small amount of the dye. Injection should be very slow and you should
not feel any resistance. Resistance to injection may indicate injection
in the wall of the aorta and may cause dissection. Injection of the
local anesthetic should commence after desirable AP (Figs. 63-4D and E) and lateral (Figs. 63-4C and F)
views are obtained with adequate propagation of the dye without
intravascular runoff. Following the local anesthetic, absolute alcohol
is injected slowly. Needle tip is about 1½ -2cm anterior to the
vertebral body. The same is done on the right side, stopping just
anterior to the vertebral body.
-
Alternatively, a right-sided needle can
be placed at the same level to block the splanchnic nerves retrocrural
in conjunction with the celiac plexus block or anterocrural as some
fibers from the celiac plexus may be blocked as well. -
Before performing this blocks, it is essential to confirm that the patient’s coagulation is normal.P.422
 Figure 63-4. A: Needle position at T12-L1 AP view. B: Lateral view. C and F: Lateral view with contrast. D and E: AP view with contrast.
Figure 63-4. A: Needle position at T12-L1 AP view. B: Lateral view. C and F: Lateral view with contrast. D and E: AP view with contrast. -
Frequent AP and lateral views assure certainty of needle position.
-
After injecting the dye, monitor the
spread and watch for backtracking through the foramina to the spinal
cord. This is especially important if splanchnic nerves are blocked. -
Use a diagnostic block prior to neurolytic blocks, preferably on different days, to test for signs of sensory or motor deficits.
-
Chiba type needle with a blocker may be used to secure the needle position.
-
Obtain informed consent and explain possible complications to both the patient and the family.
-
This block is not very useful or practical for the treatment of chronic nonmalignant pain.
-
If the tumor is occupying the space
adjacent to the celiac plexus, pain relief may not be obtained. In this
case, a splanchnic block is indicated, or radiofrequency ablation after
a successful diagnostic block.
The patient is placed in a prone position. A pillow may be used to flex
the lumbar spine to reduce the lumbar lordosis. We usually rest the
head and chest of the patient on the pillow.
Evaluation and management of sympathetically mediated pain (reflex
sympathetic dystrophy and causalgia) in the genitalia or lower
extremity. In addition, phantom limb pain, peripheral neuropathies,
lower extremity pain secondary to vascular insufficiency, and acute
herpes zoster or postherpetic neuralgia involving lumbar and sacral
dermatomes. It can also be used as a prognostic indicator for the
degree of pain relief before a destructive block or radiofrequency.
A 22-gauge, 178-mm Quincke spinal needle is used for this procedure.
The needle tip is bent about 1 cm from the tip at an angle of 20° to
30°, and care is taken so that the stylet can be removed after bending
the needle (Fig. 63-5).
5 mL of 0.5% bupivacaine. It may be mixed with 40 mg of Depo-Medrol
(Pharmacia Canada, Inc., Hamilton, Ontario, Canada) during the first
few blocks to give prolonged pain relief. For a diagnostic block, we
use only bupivacaine.
The lumbar sympathetic chain lies at the anterolateral border of the
vertebral bodies. The lumbar sympathetic chain consists of
preganglionic axons and postganglionic neurons. The cell bodies of the
preganglionic nerves arise from the intermediolateral column of the
spinal cord at T11, T12, L1, and L2 and occasionally from T10 and L3.
The preganglionic fibers pass by way of the ventral root from T11 to L2
to a white rami communicants and then to a paravertebral sympathetic
chain ganglion. The postganglionic fibers depart the chain either
directly to form a diffuse plexus around the iliac and femoral
arteries, or more commonly as gray rami communicants to combine with
spinal nerves of the lumbosacral plexus. They join all the major nerves
of the lower extremity and ultimately end with the corresponding
vessels.
with the inferior three thoracic and first lumbar ganglia. They join
the hypogastric and aortic plexuses en route to the pelvic viscera.
Afferent nociceptive fibers in this region accompany the sympathetic
fibers and relay pain sensations from the kidney, ureter, bladder, and
distal portions of the transverse colon, left descending colon, rectum,
prostate, testicle, cervix, and uterus. There are four sets (one on
each side) of lumbar sympathetic ganglia rather than five due to the
fusion
of the T12 and L1 ganglia. The position of the ganglia is variable and
can be segmentally located or closely grouped between L2 and L4.
 |
|
Figure 63-5.
The needle tip is bent about 1 cm from the tip at an angle of 20° to 30°, and care is taken so that the stylet can be removed after bending the needle. |
plane immediately anterolateral to the lumbar vertebral bodies. The
sympathetic chain is separated from the somatic nerves by the psoas
muscle and fascia, the psoas muscle being situated posteriorly and
laterally to the sympathetic chain. The aorta is positioned anteriorly
and slightly medially to the chain on the left side. The inferior vena
cava is in closer proximity to the chain on the right in an anterior
plane.
The lumbar region is prepared and draped using sterile techniques. The
block is performed at the L3 level. The fluoroscopy beam is rotated 25°
to 30° lateral to the midline toward the side to be blocked, and a
fluoroscopic view is obtained. The upper lateral edge of the L3
vertebra is then isolated by keeping a sterile clamp tip at that point
on the skin, and local anesthesia is applied to the skin and underlying
tissues (Fig. 63-6A). The bent 22-gauge spinal needle is then introduced under the skin with the
tip pointing laterally. The needle is advanced gradually toward the
upper lateral border of L3 with the bevel pointing laterally. The
lateral (Fig. 63-6B) and anteroposterior (Fig. 63-6C)
views are taken to confirm the depth of the needle and its distance
from the midline. The needle is advanced until it approaches the
anterolateral margin of the vertebral body in the lateral view, taking
care that the needle does not cross the facet line in the
anteroposterior view. The bevel is then directed medially to hug the
vertebral body anterolaterally. After negative aspiration for blood and
cerebrospinal fluid, 5 mL of Isovue-200 is injected. After confirming
spread of the dye in anteroposterior and lateral views, 5 mL of 0.5%
bupivacaine is injected. Temperature recordings are obtained 5 to 10
minutes after the block and compared with the temperatures before.
 |
|
Figure 63-6. Lumbar sympathetic block.
|
Epidural or spinal block, intravascular injection of local anesthetic,
puncture of the aorta and the inferior vena cava, backache (the most
common complication) from placement of the needle through the
paravertebral muscles, needle entry into a disc, and renal trauma. A
block of the genitofemoral nerve or lumbar plexus within the psoas
muscle can occur if the needle is placed too far laterally or
posteriorly.
-
Intravenous access is obtained for administering monitored anesthetic care.
-
The anteroposterior view is taken to
assess the direction of the needle, and the lateral view is taken to
assess the depth of the needle.
Pelvic visceral pain, testicular pain not responding to ilioinguinal
and genitofemoral nerve blocks, postradiation pelvic pain, prostatic
pain, and rectal pain not responding to other blocks, such as ganglion
impar.
10 mL of 0.5% bupivacaine with or without 40 mg of Depo-Medrol; 3 to 5
mL of Isovue-200 or 300; 1% lidocaine for skin wheal and deep
infiltration.
 |
|
Figure 63-7. Hypogastric plexus block.
|
The lumbar region is prepared and draped using sterile techniques.
Using fluoroscopy in a 10° to 20° cephalad caudad and ipsilateral 15°
to 30° oblique view, identify the triangular shape formed by shadows of
L5 transverse process and sacral and iliac crest. Using a gun-barrel
technique (i.e., the needle parallel to x-ray beam), take frequent
anteroposterior views (Fig. 63-7A with dye, Fig. 63-7C without dye) to assess direction and lateral views (Fig. 63-7B)
to assess depth. The tip of the needle is placed at the anterolateral
upper edge of the sacral promontory in the lateral view and medial to
the facet line in the anteroposterior view. Confirm placement using
Isovue-200, 3 to 5 mL, and take anteroposterior and lateral views.
-
As always, monitoring, working intravenous lines, and sterile techniques are essential.
-
If sedation is used, make sure the patient is able to communicate.
-
The needle is usually bent 1 cm from the tip to facilitate steering.
-
If the patient complains of pain in the
L5 distribution, the needle needs to be withdrawn to the level of the
skin and repositioned away from L5 in a more medial position. -
If the needle still cannot be passed, the procedure needs to be aborted.
-
Alternatively, it is possible to use a
blunt Racz-Finch Kit (Radionics, Burlington, MA) radiofrequency needle,
which may minimize the risks for L5 root or vascular injuries. -
For optimal results, it is necessary to
take the time to optimize the view of the lumbar triangle to allow
adequate visualization of the needle, aiming anterior medial and caudad.
Evaluation and management of sympathetically mediated pain of the
perineum, rectum, and genitalia. Also can be used in cases of
malignancy, endometriosis, reflex sympathetic dystrophy/causalgia,
proctalgia fugax, and radiation enteritis.
2 to 3 mL of radiocontrast dye Isovue-M 200; 3 to 5 mL of 1% lidocaine
or 0.25% bupivacaine, along with 80 mg of methylprednisolone, if an
inflammatory component is present; and 4 to 6 mL of 10% phenol for
neurolytic blockade.
The ganglion impar is a solitary retroperitoneal structure situated at
the level of the sacrococcygeal junction and in front of it. This
structure marks the termination of the paired paravertebral sympathetic
chains. It receives fibers from the lumbar and sacral portions of the
sympathetic and parasympathetic systems.
The lumbosacral region is prepared and draped using sterile techniques.
The sacrococcygeal junction and the tip of the coccyx are located using
fluoroscopy. The midline is identified and a skin wheal using a
25-gauge needle with 1% lidocaine is performed. The spinal needle is
advanced perpendicular to the skin at the sacrococcygeal junction, and
its tip is placed anterior to the sacrococcygeal junction using
fluoroscopy, confirming appropriate position using anteroposterior and
lateral views. After careful aspirate for blood, air, or feces, and
after negative aspiration, the radiocontrast dye is injected to confirm
the spread of contrast medium just anterior to the sacrococcygeal
junction. This is then followed with injection of the local anesthetic
mixture/phenol. Figure 63-8 presents the anteroposterior (A) and lateral view (B).
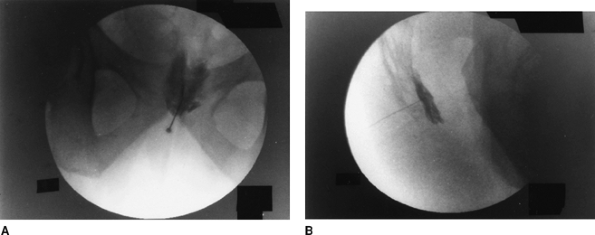 |
|
Figure 63-8. Anteroposterior (A) and lateral (B) view of ganglion impar block.
|
-
Rectal perforation with tracking of contaminants back to the rectum.
-
Infection and fistula formation,
especially in patients who are immunocompromised or who underwent prior
radiation therapy to the perineum. -
Epidural spread within the caudal canal.
-
Periosteal injection.
H, Cousins MJ, Löfström JB. Sympathetic neural blockade of upper and
lower extremity. In: Cousins MJ, Bridenbaugh PO, eds. Neural blockade in clinical anesthesia and management of pain, 3rd ed. Philadelphia: Lippincott-Raven, 1998.
