Upper Extremity Multiple Stimulation Techniques
II – Single-Injection Peripheral Blocks > A – Upper Extremity > 9
– Upper Extremity Multiple Stimulation Techniques
using a single-injection technique require a large volume of local
anesthetics and their diffusion through several barriers before
reaching the nerves. In addition, it has been established that with a
single-injection technique the intensity of the block is not uniform
among the nerves. Thus, the block of the brachial plexus using a
single-injection technique with an interscalene approach often misses
the ulnar nerve, and with an axillary approach it often misses the
musculocutaneous or the radial nerve.
double-, and multiple-injection techniques for axillary brachial plexus
block, Handoll and Koscelniak-Nielsen (2006) reported a statistically
significant decrease in primary anesthesia failure (RR 0.24, 95% CI
0.13 to 0.46) and incomplete motor block (RR 0.61, 95% CI 0.39 to 0.96)
in the multiple-injection group as compared to those in the
single-injection group. Similarly, when comparing multiple with double
injections the meta-analysis showed a statistically significant
decrease in primary anaesthesia failure (RR 0.23, 95% CI 0.14 to 0.38)
and incomplete motor block (RR 0.55, 95% CI 0.36 to 0.85) in the
multiple-injection group versus the double-injection group.
for single and double injections compared with multiple injections, but
the requirement for supplementary blocks in these groups tended to
increase the time to readiness for surgery. This provides evidence that
multiple-injection techniques using nerve stimulation for axillary
plexus block provide more effective anesthesia than do either double-
or single-injection techniques.
for peripheral nerve block placement, the importance of needle
reorientation to optimize the diffusion of the local anesthetic
solution around different nerves and branches involved in the nerve
block has become even clearer.
multistimulation for the most commonly used approaches to the brachial
plexus block. Multistimulation has been reported with axillary,
interscalene, midhumeral and infraclavicular approaches to the brachial
plexus. However, considering the greater number of needle passes in the
proximity of the pleural cavity and large blood vessels that cannot be
compressed in case of unwanted vascular puncture, multistimulation with
the infraclavicular approach should be reserved for those with
significant experience.
multistimulation technique, three different muscular responses should
be elicited: (a) contraction of the deltoid muscle, induced by
stimulation of the superior trunk (C4-5 roots); (b) contraction of the
biceps with flexion of the forearm, induced by stimulation of the
middle trunk (C6 root); and (c) contraction of the triceps muscle with
extension of the forearm, induced by stimulation of the inferior trunk
(C7 root).
The interscalene groove formed by the anterior and middle scalene
muscles is palpated at the level of the cricoid cartilage (C6). This
can be facilitated by palpating the posterior border of the
sternocleidomastoid muscle and rolling the finger laterally and
posteriorly to feel the scalene muscle. If the groove is not palpated,
the patient can be asked to take a slow and deep breath to facilitate
its location. The interscalene groove is marked. Next a horizontal line
is drawn at the level of the cricoid cartilage. The site of
introduction of the needle is the intersection between these two lines.
The insulated needle connected to a nerve stimulator (1.5 mA, 2 Hz, 0.1
ms) is introduced at a 45° angle, in a caudal and posterior direction,
and is advanced slowly until it produces a specific motor response. The
first motor response usually observed is the contraction of the deltoid
muscle (superior trunk). The position of the needle is then adjusted to
maintain the same motor response with a current of 0.5 mA. For shoulder
surgery this is the most predictive response of a good block, deserving
a larger part of the local anesthetic volume. Thus, after negative
blood aspiration, 8 mL of local anesthetic solution is injected slowly.
Next, the insulated needle is withdrawn to the level of the skin and
the intensity of the current is increased to 1.5 mA. The needle is then
reintroduced in a slightly more caudal direction (3° to 5°) toward the
midpoint of the clavicle and the groove between the pectoralis major
and deltoid muscles, in search of stimulation of the middle trunk
(contraction of the biceps muscle with flexion of the forearm). After
positioning the needle to allow for an appropriate motor response with
a current of 0.5 mA, 6 mL of local anesthetic is injected following
negative aspiration for blood. The insulated needle is again withdrawn
to the level of the skin, and the intensity of the current set back to
1.5 mA. The needle is reintroduced in a slightly more caudal direction
(3° to 5°) in search of a stimulation of the inferior trunk
(contraction of the triceps muscle with the extension of the forearm).
After the appropriate motor response is maintained with a current of
0.5 mA, another 6 mL of local anesthetic is injected slowly following a
careful aspiration test.
-
The first motor response determines how the needle needs to be redirected next.
-
To extend the block posteriorly, it is
possible to block the scapular nerve by eliciting a contraction of
trapezium muscle and then injecting an additional 5 mL of local
anesthetic. This is especially useful when the block is used to provide
anesthesia for a shoulder arthroscopy, since a trocar is always placed
posteriorly. -
Sometimes it may be difficult to feel the
interscalene groove at the C6 level. In these cases the groove can be
more easily palpated distally immediately above the clavicle, where it
is larger. Then the fingers can be progressively moved along the
interscalene groove in the direction of C6.
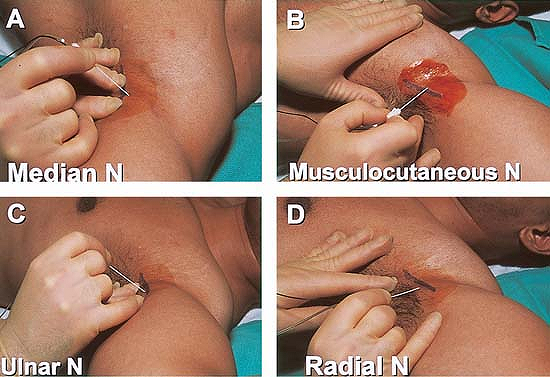
are based on the elicitation of motor responses associated with the
stimulation of four nerves (the median, ulnar, radial, and
musculocutaneous nerves). Accordingly, the muscular responses that need
to be elicited are: (a) flexion of the fingers, induced by the
stimulation of the median nerve; (b) extension of the fingers and
especially the thumb, induced by the stimulation of the radial nerve;
(c) flexion of the fourth and fifth fingers with opposition of the
first finger, induced by stimulation of the ulnar nerve; (d)
contraction of the biceps muscle with flexion of the forearm, induced
by the stimulation of the musculocutaneous nerve (Fig. 9-1).
Supine, with the arm to be blocked abducted at 90° and the forearm
flexed on the arm with another 90° angle while the head is slightly
turned toward the contralateral side.
At the level of the axilla, the axillary artery is surrounded by the
median, radial, and ulnar nerves within the neurovascular sheath. The
position of the nerves relative to the artery is variable. The
musculocutaneous nerve leaves the axilla more proximally and enters the
coracobrachialis muscle. The radial nerve is usually found posterior to
the artery, the ulnar nerve lies on the inferior or posterior border of
the artery, and the median nerve lies superior to the artery.
The axillary artery is identified and marked along with the inferior
border of the major pectoralis muscle, and the coracobrachialis muscle.
Then the insulated needle connected to a nerve stimulator (1.5 mA, 2
Hz, 0.1 ms) is introduced immediately above the axillary artery at a
45° angle as proximally as possible at the level of insertion of the
long head of the biceps muscle (Fig. 9-1)
in search of a stimulation of the median nerve (flexion of the
fingers). After the proper stimulation is elicited, the position of the
needle is adjusted to maintain the same motor response with a current
of 0.5 mA. After negative aspiration for blood, 5 to 6 mL of the
anesthetic solution is injected slowly. The needle is then withdrawn to
the level of the skin and the intensity of stimulating current is set
back to 1.5 mA. The needle is redirected toward the coracobrachialis
muscle at 30° and deeper in search of a stimulation of the
musculocutaneous nerve. After the proper stimulation is elicited, the
position of the needle is adjusted to maintain the same motor response
with a current of 0.5 mA. After negative aspiration for blood, 5 to 6
mL of the anesthetic solution is injected slowly. The needle is then
withdrawn to the level of the skin, and the intensity of stimulating
current is set back to 1.5 mA. The needle is reinserted through another
skin puncture inferior to the axillary artery and perpendicular to the
skin in search of the stimulation of the ulnar nerve (flexion of the
fourth and fifth fingers with opposition of the first finger). The
intensity of the current is progressively reduced to 0.5 mA. After a
negative aspiration test, 5 to 6 mL of the local anesthetic solution is
injected. The needle is withdrawn from the skin and then redirected
posteriorly to the axillary artery in search of the radial nerve
(extension of fingers including the thumb). After the proper
stimulation
is elicited, the position of the needle is adjusted to maintain the
same motor response with a current of 0.5 mA. After negative aspiration
for blood, 5 to 6 mL of the anesthetic solution is injected slowly.
 |
|
Figure 9-1.
An insulated needle connected to a nerve stimulator is introduced immediately above the axillary artery at a 45° angle as proximally as possible at the level of insertion of the long head of the biceps muscle in search of a stimulation of the median nerve. |
-
Because of the variability of nerve
distribution around the axillary artery it is important to not only
have an appropriate knowledge of the possible anatomic variations but
also the specific motor response associated with the stimulation of
each nerve. -
If the musculocutaneous nerve is first
blocked, the needle needs to be redirected more superficially and
proximal to the axillary in search of the median nerve. The median
nerve is contained in the brachial plexus sheath. The musculocutaneous
nerve exits early from this sheath. -
The intercostobrachialis nerve, a branch
of the T2 intercostal nerve, can be also blocked by subcutaneous
injection of 5 mL of local anesthetic inferior to the axillary artery
toward the inferior border of the axilla.
G, Casati A, Beccaria P, et al. Interscalene brachial plexus
anaesthesia with small volumes of ropivacaine 0.75%: effects of
injection technique on the onset time of nerve blockade. Eur J Anaesthesiol 2001;18:54–58.
G, Casati A, Garancini P, et al. Nerve stimulator and multiple
injection technique for upper and lower limb blockade: failure rate,
patient acceptance and neurologic complications. Anesth Analg 1999;88:847–852.
E, Kern O, Mahoudeau G, et al. Block of the brachial plexus branches by
the humeral route. A prospective study in 503 ambulatory patients.
Proposal of a nerve-blocking sequence. Acta Anaesthesiol Scand 1999;43:609–613.
HH, Koscielniak-Nielsen ZJ. Single, double or multiple injection
techniques for axillary brachial plexus block for hand, wrist or
forearm surgery. Cochrane Database Syst Rev. 2006 Jan 25;(1):CD003842.
ZJ, Hesselbjerg L, Fejlberg V. Comparison of transarterial and multiple
nerve stimulation techniques for an initial axillary block by 45 mL of
mepivacaine 1% with adrenaline. Acta Anaesthesiol Scand 1998;42:570–575.
ZJ, Rotboll Nielsen P, Sorensen T, et al. Low dose axillary block by
targeted injections of the terminal nerves. Can J Anaesth 1999;46:658–664.
ZJ, Stens-Pedersen HL, Lippert FK. Readiness for surgery after axillary
block: single or multiple injection techniques. Eur J Anaesth 1997;14:164–171.
J, Barcena M, Taboada-Muniz M, et al. A comparison of single versus
multiple injections on the extent of anesthesia with coracoid
infraclavicular brachial plexus block. Anesth Analg 2004;99:1225–1230.
S, Batoli M, Lepri A, et al. Multiple-injection axillary brachial
plexus block: a comparison of two methods of nerve localization–nerve
stimulation versus paresthesia. Anesth Analg 2000;91: 647–651.
