Knees Bow Out, Feet Turn In, Who Cares?
|
|
for angular deformities of the legs are within normal limits. To stay
out of trouble the physician must be able to pick out the “problem.”
The first defense is to understand normal physiologic progression:1,2
-
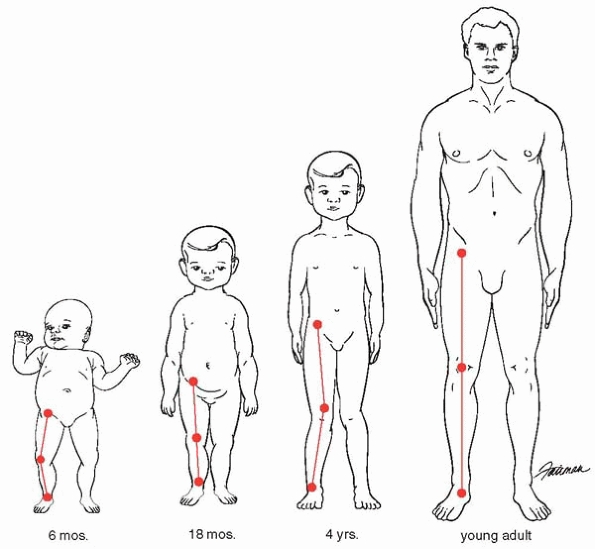
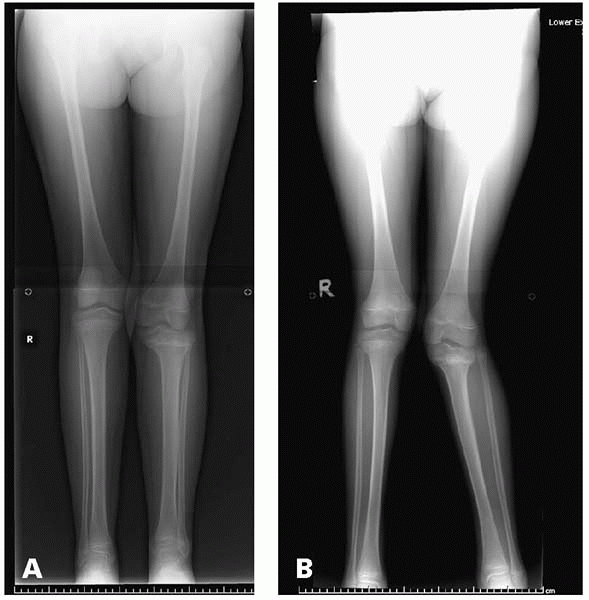
Maximum genu varum (bowlegs) at birth (Fig. 23-1A)
-
Legs straight at 18 months (Fig. 23-1B)
-
Maximum genu valgum (knock knees) around age 4 (Fig. 23-1C)
-
Straight to slight valgus at maturity (Fig. 23-1D)
 |
|
▪ FIGURE 23-1 (A) 6-month-old with genu varum. (B)
18-month-old with straight legs. At some point in most children, usually around 18 months of age, the legs are perfectly straight as their developmental stage passes from genu varum to genu valgum. (C) 4-year-old with genu valgum. (D) Adult with nearly straight legs, erring on the side of slight valgus. |
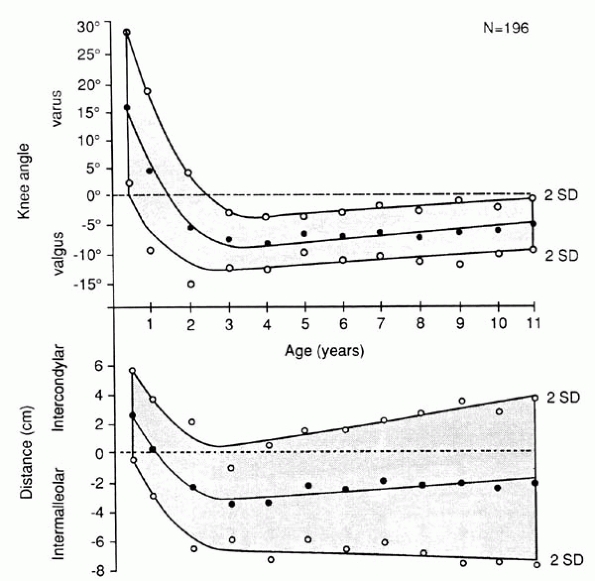
physiologic, measure the intermalleolar distance (for knock knees) or
intercondylar distance (for bow legs). Two useful facts to remember
from Heath and Staheli’s study2 are
that normal children aged 2 to 11 years may have knock knees up to 12
degrees and an intermalleolar distance up to 8 cm; and the existence of
bowlegs after age 2 years was abnormal. The graph in Fig. 23-2
can help you decide if this is within 2 standard deviations. This
measurement can be assessed 6 months later to provide some objective
evidence regarding progression or improvement. The technique of
measurement can be readily taught to the family members; they will then
feel that
the
situation is being monitored and taken seriously. In younger children,
the distances may have to be measured supine, and future measurements
must occur in the same position for consistency. A good screening tool
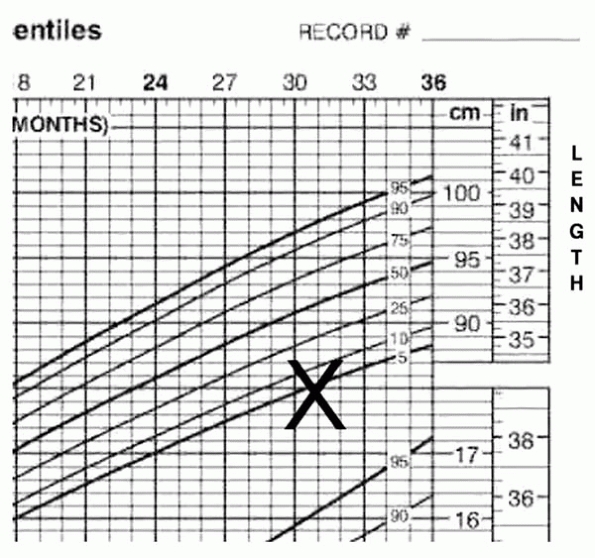
is to plot the child’s height on a growth curve (Fig. 23-3).
A child with abnormal angulation of the legs, whose height is more than
two standard deviations below normal, should be evaluated for an
underlying condition such as rickets or a skeletal dysplasia.
 |
|
▪ FIGURE 23-2 For each of the 12 age groups, mean values (solid circles) and 2 SD (pen circles) were plotted for knee angle (A) and intercondylar or intermalleolar distance (B).
Lines and shaded areas show general trends. (Reprinted with permission from Heath CH, Staheli LT. Normal limits of knee angle in white children—genu varum and genu valgum. J Pediatr Orthop. 1993;13(2):259-262.) |
 |
|
▪ FIGURE 23-3
Any child with abnormal angulation of the legs, whose height is greater than two standard deviations below normal, probably has an underlying condition such as rickets or a skeletal dysplasia. |
comparison. However, technique is important, and there are a couple of
pitfalls to avoid. The child should be standing if possible; this will
demonstrate greater deformity than seen on non-weight bearing
radiographs. Beware when comparing radiographs over time, that the
weight-bearing status of the radiographs are the same, or differences
in deformity may be falsely attributed to progression or improvement.
While taking radiographs, it is important that the patellas (not feet)
are pointing forwards (Fig. 23-4). In the case
of a child with tibial torsion, if the feet point forward, the patellas
point laterally and may give a false impression of genu varum
radiographically and clinically (Fig. 23-5A).
 |
|
▪ FIGURE 23-4 (A)
This radiograph was taken of a child with clinical unilateral genu valgum of the left leg, but the leg was externally rotated and the genu valum is not evident. (B) After the doctor drew an “X” on the patella and instructed the radiology technician to take the radiograph with the “X” pointing forwards, the true genu valgum was evident radiographically. |
 |
|
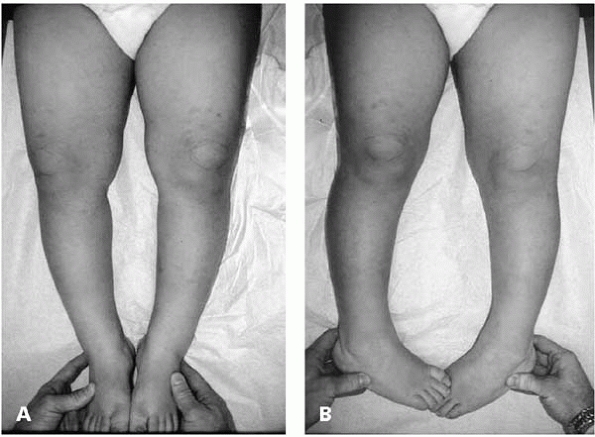
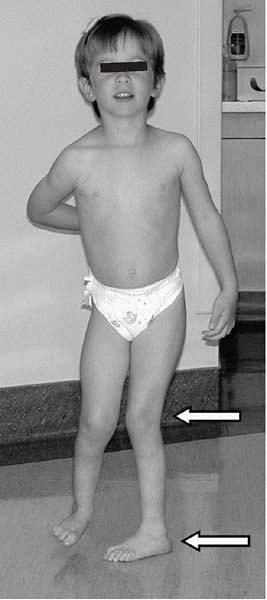
▪ FIGURE 23-5 (A)
Child demonstrating the apparent genu varum of tibial torsion. The chief complaint of this child’s parents was bowed legs. With the feet pointing forward the legs have the appearance of genu varum when the child is supine or walking. The apparent “bowing” is a product of the knees pointing laterally, so knee flexion gives the appearance of bowing. (B) When the child’s patellas point anteriorly it is clear that there is not significant genu varum present. This demonstration often helps alleviate parental anxiety. |
demonstrates, turning the legs inward so the patella points straight
anterior allows assessment and demonstration of varus/valgus alignment.
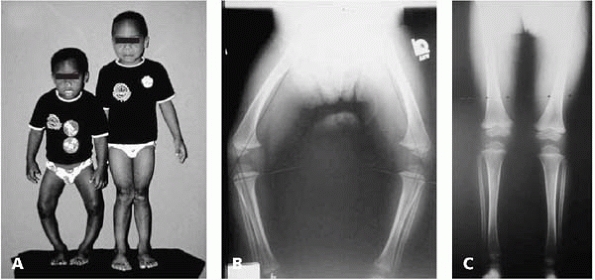
Blount disease is often quite difficult. This may be problematic with
respect to confirming the diagnosis and selecting the optimal timing
and method of treatment (Fig. 23-6). A
metaphyseal-diaphyseal angle >10 to 16 degrees increases the
likelihood of a diagnosis of Blount disease, but is by no means
definitive. Stay out of trouble by not relying too heavily on a
radiographic measurement in the diagnosis of Blount disease.
 |
|
▪ FIGURE 23-6 (A)
A 3-year-old with bowed legs next to his older brother. The mother reported the older brother had bowed legs just as bad as his younger brother but grew out of it without any treatment. (B) Radiographs of the 3-year-old show generalized bowing of the femurs and tibia. There is not a focal deformity of the proximal tibia that would be expected with Blount disease, and the physes appear normal. (C) Given the 3-year-old’s severity of bowing and age, treatment would generally be indicated for genu varum; however, in the context of the family history and radiographs suggestive of physiologic bowing, the child was followed up with close observation only. Radiograph of the same child at age 5 years demonstrates resolution of the genu varum without treatment (photographs courtesy of John T. Killian, MD). |
 |
|
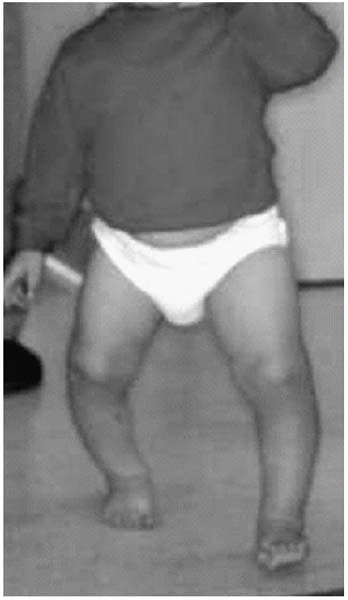
▪ FIGURE 23-7 During weight bearing, a lateral thrust of the knee is suggestive of Blount disease.
|
-
Child is older than 2 years
-
There is lateral thrust (as weight is placed on a leg during the stance phase of gait, the knee abruptly translates laterally) (Fig. 23-7)
-
Focal angulation on exam and radiograph at proximal tibia is observed (Fig. 23-8)
-
There is medial beaking and downward slope of the proximal tibial metaphysis (Fig. 23-9)
-
Parents report it is not improving
-
Obesity
-
African American ethnicity
-
Early walker
-
Unilateral occurrence
 |
|
▪ FIGURE 23-8 Focal angulation at the proximal tibia and medial beaking of the tibia are suggestive of Blount disease.
|
 |
|
▪ FIGURE 23-9 Medial tibial beaking and downwards sloping of the metaphysis is characteristic of Blount disease.
|
-
Parents report it is improving
-
It’s symmetrical
-
Generalized bowing on exam and radiographs over femur and tibia is observed (see Fig. 23-6)
may, according to some investigators, alter the natural history of
Blount disease. While many aspects of orthotic treatment are
controversial, most agree that bracing should be started before the age
of 3 years.3 In addition to issues
of compliance, this is also due to the fact that surgery should be done
by age 4 years to minimize the risk of recurrence of deformity.4,5
areas of potential trouble that the surgeon should be aware of.
Proximal tibia and fibula osteotomies have significant risk of
compartment syndrome. The anterior tibial artery passes through the
interosseous membrane near the level of the osteotomy. Acute correction
through the osteotomy site is believed to cause occlusion of the artery
and lead to compartment syndrome at times. Acutely lessening the degree
of correction has relieved signs of ischemia in some cases.6
Compartment release at time of correction should be considered, and
careful postoperative monitoring is essential. It may be wise to avoid
an epidural catheter because it might mask symptoms of compartment
syndrome.
 |
|
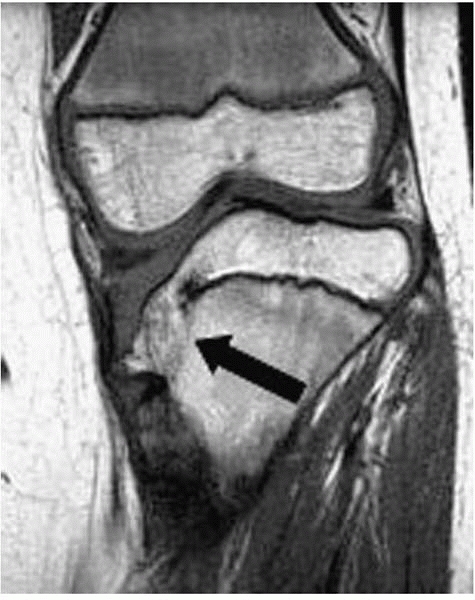
▪ FIGURE 23-10
MRI of a child with Blount disease demonstrating that a bony bridge has formed. An osteotomy alone is not sufficient treatment as the deformity will recur relatively rapidly when there is growth remaining. |
in the treatment of Blount disease, including that of simple K-wire
fixation and casting in the young child. The old technique of
incorporating pins into plaster is best avoided due to the risk of
infection and osteomyelitis. Rab popularized a method of an oblique
osteotomy stabilized by a single anteroposterior screw and an
above-knee cast. An alternative to this is plate fixation; a cast is
generally required regardless of internal fixation technique because
the child is otherwise likely to walk on the leg as soon as diminishing
pain permits.
time with specialized external fixators may help prevent compartment
syndrome and soft-tissue problems. With severe deformity, consider
preoperative evaluation of the physis with MRI (Fig. 23-10).
If a bony bridge has already developed on the medial side, it may be
excised at the time of the primary surgery, rather than waiting to
excise it following a recurrence of deformity. If the medial bar is
extensive, you may need to ablate the lateral physis to prevent
recurrence following osteotomy. Aiming for slight overcorrection into
mild valgus will probably decrease the risk of recurrence, and not
cause harm. Assess the mechanical axis in the operating room with a
Bovie cord and C-arm. When the cord is over the center of the hip and
ankle, it should pass just through the center of the knee or just
lateral to this to achieve slight overcorrection. Remember to cut the
fibula and to correct torsion at the same time.
-
Distal femur may be in varus as well, but it’s unclear when that requires correction as well.7
-
Hemiepiphysiodesis
of the tibia may be best in some cases with significant growth
remaining, provided there is no medial physeal bar. In such cases the
fibula can be ignored. Dr. Stevens adds that you may be pleasantly
surprised to find that the malrotation spontaneously corrects as the
limb straightens. -
Consider preoperative pulmonary consultation in adolescents with extreme obesity.
-
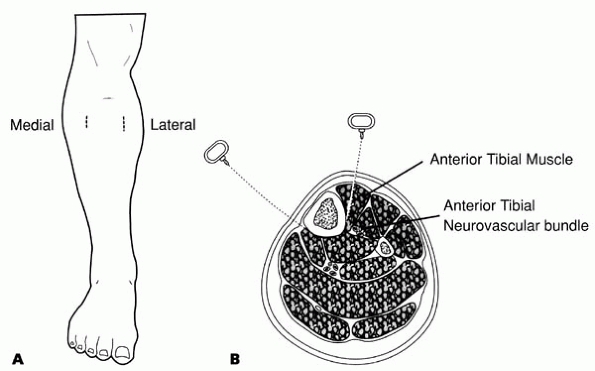
One of us (DLS) has found the Afghan percutaneous osteotomy described by Paktiss and Gross8
to be safe and effective, with less postoperative pain allowing for
earlier mobilization. This technique using a Gigli saw and two 1- to
1.5-cm incisions is well described in the cited reference (Fig. 23-11).
 |
|
▪ FIGURE 23-11 (A) Location of incisions for proximal tibial osteotomy. (B)
Position of the Gigli saw just before performance of the osteotomy. (Reprinted with permission from Paktiss AS, Gross RH. Afghan percutaneous osteotomy. J Pediatr Orthop. 1993;13(4):531-533.) |
Rickets may be due to many conditions, and be associated with genu
varum or genu valgum. Radiographs should demonstrate widened and cupped
physes, though this is difficult to discern at times. In cases of
rickets, do not do surgery until the child’s underlying condition is
medically controlled, or the deformity is likely to recur. Focal injury
to the growth plate from trauma, infection (especially neonatal
infection or meningococcemia) should be suspected, particularly in
deformities outside of the usual age and type.
 |
|
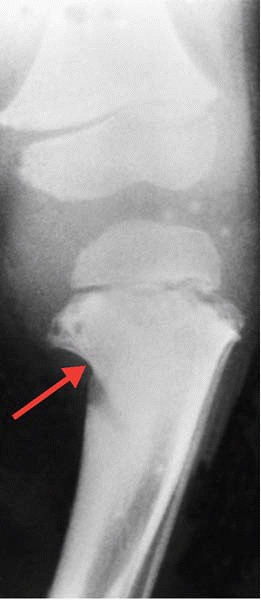
▪ FIGURE 23-12 Radiograph in a 39-month-old boy shows a characteristic focal defect in the medial aspect of the proximal tibia (arrow).
Note that there is no sloping of the medial metaphysis, which helps differentiate this from Blount disease. (Reprinted with permission from Choi IH, Kim CJ, Cho TJ, et al. Focal fibrocartilaginous dysplasia of long bones: report of eight additional cases and literature review. J Pediatr Orthop. 2000;20(4):421-427.) |
focal fibrocartilaginous dysplasia. In this condition there is focal
indentation of bone, most often the medial proximal tibia, which may be
confused with Blount disease, though involvement of the distal femur
and upper extremities have been reported as well (Fig. 23-12).
The physis and epiphysis appear radiographically normal. The deformity
associated with focal fibrocartilaginous dysplasia has been shown to
resolve spontaneously in at least 45% of tibial cases, so initial
observation may be warranted.9
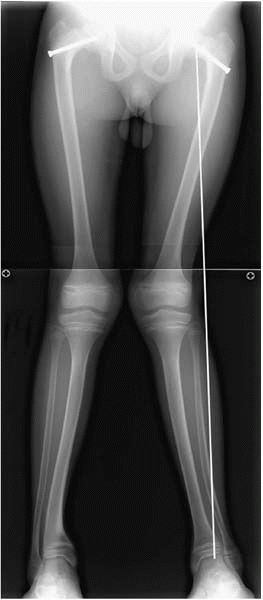
4-year-olds. It is usually symmetrical and demonstrates spontaneous
resolution. If the genu valgum is severe, or seen in children of other
age groups, suspect underlying disorders such as renal osteodystrophy,
skeletal dysplasias, or a posttraumatic origin following an incomplete
tibial metaphysis (Cozen) fracture (Fig. 23-13).
While there is no good science to suggest when genu valgum should be
corrected operatively, we consider it when children are symptomatic
(gait or running problems, pain) or for a mechanical axis passing
lateral to the knee. Gait analysis has demonstrated objective
improvement in gait following hemiepiphysiodesis for correction of genu
valgum.10 Adolescents with severe genu valgum report difficulty running and may
have associated patella pain; these symptoms may resolve with
normalization of the mechanical axis via hemiepiphysiodesis of the
distal femur.11
 |
|
▪ FIGURE 23-13
Radiograph of a 14-year-old boy with renal osteodystrophy. Widened growth physis is characteristic of rickets. The mechanical axis drawn from the center of the hip to the center of the ankle is lateral to the knee. This child also had bilateral SCFE, which is also associated with renal osteodystrophy. |
-
Use a permanent
hemiepiphysis only with great caution, as this is irreversible. A
recent series has reported overcorrection in 15/125 knees (12%) of
children treated with a permanent hemiepiphysiodesis12 -
Series of
hemiepiphysiodeses with staples conclude that the staples can be
removed without permanent injury to the growth plate, though rebound
growth can be expected particularly in young children.11,13,14 -
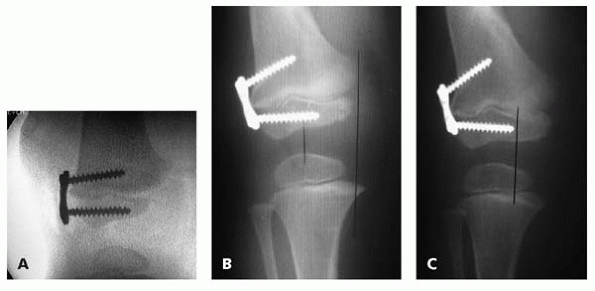
Plan on a temporary hemiepiphysiodesis only in children likely to return to followup appointments (Fig. 23-14).
-
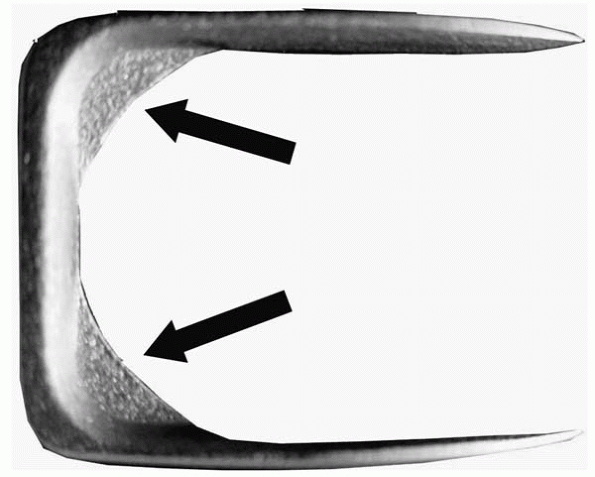
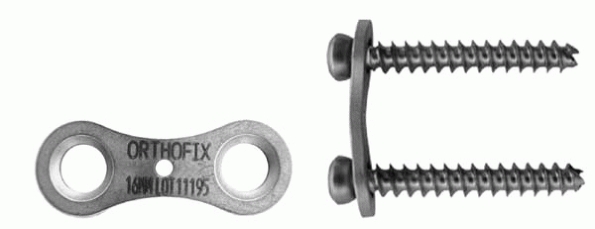
Use only staples with shoulders (Fig. 23-15),
or they will not be strong enough to withstand significant forces
generated by growth or instrumentation specifically designed for
hemiepiphysiodesis (“8” plate, Figs. 23-16 and 23-17). Keep dissection and implants superficial to perichondrial ring to prevent irreversible damage to physis. -
Generally, use two staples (or a single 8-plate) for the proximal tibia and/or distal femur.
 |
|
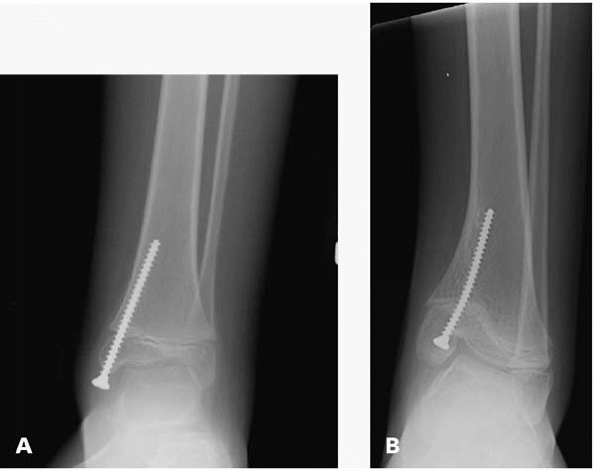
▪ FIGURE 23-14
This 12-year-old boy with spina bifida had a medial malleus screw placed to perform a temporary hemiepiphysiodesis for a valgus ankle. (A) The ankle is almost in a neutral position after some correction has already occurred. (B) The child was lost to followup and returned 4 years later with this radiograph. Temporary hemiepiphysiodesis is perhaps best reserved for patients likely to comply with followup instructions. |
 |
|
▪ FIGURE 23-15 This staple has “shoulders” (black arrows) designed to withstand the forces generated when spanning an active growth plate.
|
 |
|
▪ FIGURE 23-16
An “8” plate is specifically designed for hemiepiphysiodesis. Growth is prevented at the plate, but angulation of the screws within the plate permits asymmetric growth of the physis and angular correction. |
 |
|
▪ FIGURE 23-17 With asymmetric growth of the physis, progressive angulation of the screws (or staples) is expected with angular correction. (A) Intraoperative image at time of implantation of “8” plate. (B) Same patient 2 months after surgery. (C) Same patient 9 months after surgery.
|
trouble by not overreacting or overtreating. There is almost always an
associated calcaneovalgus foot in which the dorsum of the foot often
touches the skin over the tibia (see Fig. 23-19).
The foot deformity rapidly resolves with stretching, and the bowing
spontaneously resolves within the first year or two of life. The most
frequently encountered problem needing treatment (both in real life and
standardized tests) is a leg length discrepancy of 3- to 8-cm expected
at maturity, of which the parents should be forewarned.
seriously. About 50% of patients have neurofibromatosis; early
recognition of neurofibromatosis can help a child receive early
treatment for problems associated with it. Beware that many of the
cutaneous manifestations of neurofibromatosis, such as axillary and
inguinal freckling and café-au-lait spots, may not be present in
infancy, so it may be reasonable to consider a genetics referral for
all infants with anterolateral bowing of the tibia. If pseudarthrosis
is not congenital (present at birth) it may ensue following fracture.
Fractures are common, so help prevent them with an AFO or KAFO to be
used whenever the child is weight bearing. These braces should be used
from the onset of weight bearing. While there is not a clearly
established “best” surgical treatment for this condition, it is
generally accepted not to do a resection
of the pseudarthrosis and bone graph prophylactically. Try to hold off
surgery as long as possible with braces. When surgery becomes
inevitable, make certain the parents understand that multiple surgeries
are likely, and that they may ultimately come to a time when amputation
may provide better function than multiple heroic procedures.
the parents, grandparents, friends, and even concerned strangers will
think you are not taking the problem seriously enough (see Chapter 3, Dealing with Families).
To avoid this, simply verbalize the logical risk/benefit analysis we
consider obvious and the parents almost always come to the same
conclusion you do, and choose observation. But letting them make the
choice may make all the difference between a satisfied and disgruntled
family. For families seeking second opinions, because the first doctor
would not do anything, one approach is: “Yes, Sally’s feet certainly do turn in. I can fix that by simply cutting her bones in half and drilling some steel pins
through them. You understand, of course, such a surgery will leave
scars. And although it is rare, her nerves, blood vessels or other
structures may be permanently damaged, so her legs may not work as well
after surgery. On the other hand, this problem usually resolves over time by itself without surgery…”
 |
|
▪ FIGURE 23-18 There is no evidence to suggest that bracing affects the natural history of torsional deformities.
|
bracing influences the natural history of torsional deformities. While
it may be tempting to placate demanding family members, it has shown
that even corrective shoes have detrimental psychological effects on
children, with lasting lowered self-esteem as adults15 (Fig. 23-18). Maintaining a good relationship with the family is important, but cannot be at the expense of the child.
watching a professional basketball game on television. There is usually
a lot of intoeing going on, but the players nevertheless seem to
function adequately. Torsional deformities are different from angular
deformities in that torsional deformities are not associated with
long-term problems in otherwise normal children. Thus measuring the
extent or progression of deformity is usually a moot point.
also soft-tissue external rotation contractures present at birth that
may mask bony torsion. Thus, intoeing may appear to worsen during the
normal resolution of external rotation contractures of the hip. Femoral
anteversion and hip rotation improves spontaneously over the first
decade16,17 (Fig. 23-19).
When running knees point in and feet fly outwards, and it looks very
clumsy. The truth is, there is very little trouble one can get into
over femoral torsion. Even if the torsion does not resolve, there is
little evidence that persistent femoral torsion causes problems. A
cadaveric study18 of adult 110 cadavers from Africa reports an association of arthritis of the distal femur with decreased
anteversion. Other studies (conducted on live adults) have found no
association between increased femoral anteversion and abnormal
patellofemoral characteristics.18
 |
|
▪ FIGURE 23-19 In femoral anteversion, the knee and foot both point inward (arrows).
|
at birth normally, and spontaneous improvement can be expected in most
children.17 Acknowledge to parents
that this may lead to more tripping in young children. It has been
demonstrated that high-performance sprinters have more internal tibial
torsion than controls. Once the parents understand the true nature of
their child’s superior genetic gift, they may leave your office with
pride.19
-
If feet turn outward, consider a SCFE or coxa vara, or tibial torsion.
-
If one foot turns in, consider hemiplegia or other neuromuscular disorder.
-
Limping—torsion usually does not cause a limp, which by definition is an asymmetry of gait. Search for other causes of the limp.
-
Pain—torsional
disorders generally are not painful, so search for other causes with
one exception: miserable malalignment syndrome. This is defined by
excessive femoral anteversion, excessive tibial outward rotation, and
patellofemoral pain. There are two reports of a total of 40 extremities
treated by ipsilateral femoral and tibial osteotomies with good results.20,21 (Delgado, Schoenecker et al. 1996; Bruce and Stevens 2004)
-
Suspect rickets if child with bowed legs is of small stature.
-
Use staples with shoulders for hemiepiphysiodesis or screw and plate.
-
For Blount disease, surgery should be done by age 4 years to minimize the risk of recurrence of deformity.
-
The most common pitfall of torsional deformities is the parental perception of you not taking the problem seriously enough.
-
Residual inward tibial torsion may be associated with faster running.
HH, Sandrow RE, Sullivan PD. Complications of tibial osteotomy in
children for genu varum or valgum: evidence that neurological changes
are due to ischemia. J Bone Joint Surg Am. 1971;53(8):1629-1635.
IH, Kim CJ, Cho TJ, et al. Focal fibrocartilaginous dysplasia of long
bones: report of eight additional cases and literature review. J Pediatr Orthop. 2000;20(4):421-427.
RK, Dickens DR, Cole WG. Medial physeal stapling for primary and
secondary genu valgum in late childhood and adolescence. J Bone Joint Surg Br. 1995;77(5):733-735.