Leg Length Inequality
|
|
be considered normal. A study of 600 military recruits found a leg
length discrepancy of 0.5 to 1.5 cm in 32% of recruits, and 4% had a
difference of over 1.5 cm.1 While a
few small studies report an increased incidence of back or hip problems
with modest LLD, most large series do not report an increased incidence
of long-term problems with LLD ≤1 inch. However, the long-term effect
of LLD is not certain. Nor is there convincing evidence to support the
orthopaedic community’s position that an LLD ≤1 inch is acceptable
while LLD >1 inch warrants treatment. One thing that has been shown
by gait analysis is that in children LLDs <3% are not associated
with compensatory strategies.2 A 3% LLD in an average adult is about 1 inch.
appropriately concerned to families, be careful about minimizing the
importance of small leg length discrepancies at the beginning of the
visit. The families may have already been informed by trusted
non-physician healthcare providers that if untreated, their child’s LLD
will lead to long-term pain and disability.
abnormal. Is one leg too short, or the other one too long? This point
is not just academic, as a patient with idiopathic hemihypertrophy or
nonsyndromic Beckwith-Wiedemann syndrome warrants an ultrasound of the
abdomen to rule out associated Wilms or other tumor. Looking at the
proportions of the legs to the body can be helpful in determining which
limb is abnormal. Hint: pathologically short limbs often have
associated musculoskeletal abnormalities such as coxa vara, bowing,
absence of an ACL, lateral femoral hypoplasia, fibular hemimelia,
tumorous conditions such as fibrous dysplasia, etc. In contrast,
pathologically long limbs are often associated with cutaneous or
vascular anomalies as seen in Proteus syndrome, Klippel-Trenaunay
syndrome, neurofibromatosis or Beckwith-Wiedemann syndrome.
serious underlying causes such as neurofibromatosis, bone or
soft-tissue tumors, or neurologic disorders that may require treatment.
Do not be fooled by a child with hemiplegia cerebral palsy (CP), in
which a short leg is expected on the affected side, and serves a
beneficial effect of helping with leg clearance during the swing stage
of gait.
 |
|
▪ FIGURE 24-1 Pelvic obliquity can cause an apparent LLD; patient supine on examining table.
|
the assessment of LLD. Hip position can influence the apparent leg
length on exam and during gait. An adducted hip makes the leg appear
shorter, while an abducted hip makes the leg appear longer. In fact, an
apparent discrepancy of 3 cm is created for each 10 degrees of hip
adduction/abduction.3 Because of this, simply looking at the position of the feet of a supine patient is not accurate (Fig. 24-1). Measuring leg lengths from the anterior superior iliac spine to the medial malleolus is subject to extreme variability.
have the patient stand up, with knees straight, and place the
examiner’s fingers on the iliac crest. Placing blocks of various sizes
under the short leg until the pelvis is level provides a
reasonable
estimation of the LLD. This test is less accurate in the
circumferentially challenged (obese) child, as the pelvis is more
difficult to palpate. Beware that previous pelvic surgery, such as a
Salter osteotomy in which part of the iliac crest has been removed, may
make this test inaccurate. Another pitfall in evaluating for LLD by the
standing method is that a chronically short leg often develops an
equinus contracture. Make certain both feet are flat on the floor.
Beware that often children with significant LLDs will automatically
bend the knee of the longer leg to level the pelvis—this is another
pitfall.
particular attention during the physical exam to evaluate joint
stability of the hips, knees (ACL) and ankles (valgus/varus). An
unstable joint is best discovered before it dislocates during
lengthening.
such as patient positioning and joint contractures. If these
radiographs are going to be used to determine surgical treatment,
supervision of the x-ray technique by the surgeon may be best if
standardization is not certain. In a teleoroentgenogram (AP radiograph
of the lower extremities including the hips, knees and ankles on one
film) the x-ray beam is at an angle to the hip and ankle, thus is not
accurate. However, in an infant or toddler, the small parallax effects
may be preferable to the likelihood of movement between the three
images of a scanogram. Scanograms are preferable in children who can
lie still.
included, so a foot deformity that contributes to the overall LLD will
not be recognized by the scanogram. A second pitfall of the scanogram
is that the diaphysis of the femur and tibia are not imaged, so a tumor
or other cause of the LLD may be missed. At the initial assessment,
full-length radiographs of the lower extremities are beneficial in
establishing the diagnosis. For teleoroentgenograms and scanograms, a
hip or knee flexion contracture gives a falsely short reading of the
contracted limb. Computer axial tomography (CT) scanograms can more
accurately assess limb lengths in children with hip or knee
contractures, as well as rotational alignment. Additional benefits of
CT are lower radiation exposure and greater accuracy, particularly when
the patient is poorly positioned.
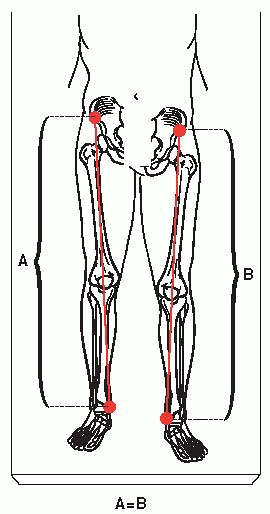
then confirm that the lengths and differences give the same total LLD
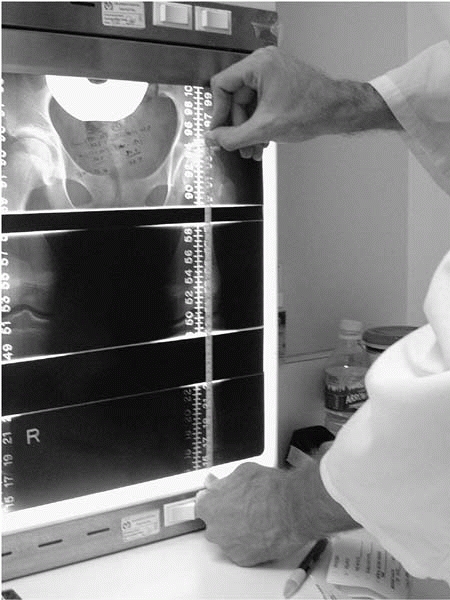
independently. This may be written directly on the scanogram (Fig. 24-2)
or dictated in the chart, so the accuracy may be later verified. While
this sounds elementary, most errors in LLD surgery are from
miscalculations (see box, Errors in Using Growth Charts).
|
TABLE 24-1 Useful Chart for Reading a Scanogram
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||
 |
|
▪ FIGURE 24-2
A quick way to double-check your calculated LLD from the scanogram: Measure the length from the top of the femur to the bottom of the tibia of both legs with a tape measure. The difference of these measurements should equal the formally calculated LLD. |
 |
|
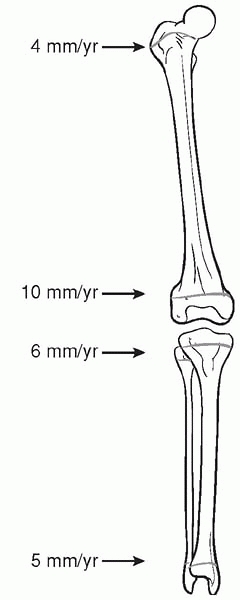
▪ FIGURE 24-3
Estimate of growth of the physes of the femur and tibia (proximal femur 4 mm/yr, distal femur 10 mm/yr, proximal tibia 6 mm/yr, distal tibia 5 mm/yr). |
common sense. Having a few rules of thumb at hand is very helpful to
double-check calculations. For example, the average total leg length in
adult males is 85 cm and in females is 78 cm. A rough estimate of the
growth of the physes of the lower extremity is proximal femur 4
mm/year, distal femur 10 mm/year, proximal tibia 6 mm/year and the
distal tibia 5 mm/year (Fig. 24-3). Skeletal
growth generally ends at 14 or 15 years in girls and 16 or 17 years in
boys. There are many measures of maturity: chronologic age, bone age,
radiologic appearance of physis, comparison of child’s height compared
to parents, and comparison to siblings’ and parents’ growth patterns
(e.g., Dad grew 4 inches in college). All of these are subject to
inaccuracies, thus consideration of all of them together may give the
most accurate picture. Also beware that underlying disorders may affect
maturation, for example, one third of children with spina bifida may
have precocious puberty.
treating is the LLD predicted at maturity, not the current LLD. The
three traditional methods of
predicting
LLD are the arithmetic method, the growth-remaining method, and the
straight-line method. These three all use data from one database by
Anderson and Green. A potential pitfall in using only the
growth-remaining method is that tall children obtain more correction
than short children after an epiphysiodesis, because they will have
more growth. Of these three methods, the Moseley straight line method
has several advantages to help minimize errors, such as using multiple
measurements at different times and taking into account growth
percentiles.4
While the Moseley straight-line method has been the gold standard,
multiple measurements should be obtained to use it, and there are many
potential sources of error.
introduced recently, which allows prediction of LLD with one
measurement of limb lengths, without the need for bone age or graphing.5 When used on congenital discrepancies, we have found this method quite simple and with few steps prone to errors.
as a femur fracture healing 3 cm short or growth stimulation from
osteomyelitis that has since healed, are not considered growth
inhibition, and do not exhibit a constant effect on a discrepancy. Thus
the above methods are applicable only when applied after the resolution
of the event.
method is subject to significant variability. Sixty hand radiographcs
were read by 4 radiologists, and 50% of the children were assigned a
skeletal age that differed by more than 1 year between radiologists;
10% varied by more than 2 years.8
|
Traditional Guidelines for Treatment of LLD*
|
||
|---|---|---|
|
walking on the toes of the short limb, prescribing a shoe lift or
orthotic may help prevent an equinus contracture. If there is
significant angular deformity in a limb, that must be taken into
account when predicting LLD, as correction of the angular deformity
will lengthen the leg.
and aim at 0.5 to 1.0 cm of undercorrection as discrepancies <2 cm
are well tolerated. Particularly when an epiphysiodesis has been
performed, families may be quite unhappy if the long leg was shortened
too much, and the child sacrificed more height than was necessary. It
is important to plan for a leg to end up shorter if the knee is stiff
in extension, or if there is weakness requiring the knee to be braced
in extension, to allow for clearance of the foot during the swing
through phase of gait.
lumbar-sacral obliquity may be compensated for by unequal leg lengths,
in which case equalizing the leg lengths could result in a functional
leg length discrepancy.
Extra periosteal stapling is usually reversible if there is
uncertainty, but this may require larger incisions and later hardware
prominence compared to percutaneous methods. Technically, when ablating
the physis with a drill or curette, there is a tendency for the
instrument to fall into the softer adjacent cancellous bone. Stay out
of trouble with liberal use of images to make certain you are ablating
the physis. The distal femoral physis in particular is not flat; make
certain the ablation follows the undulations of the physis.
performing a temporary epiphysiodesis. This phenomenon is well
described in temporary hemiepiphysiodesis for angular deformity, and we
suspect is underappreciated in the treatment of LLD. Dr. Moseley
recommends that the epiphyses of both tibia and femur should be
approached both medially and laterally since it is very difficult to
ablate the plate from only one aspect. In contrast Drs. Grill and
Skaggs have performed epiphysiodesis from only one side with
predictable good results. If performing an epiphysiodesis from one
side, it is essential to not miss the corners of the growth plate
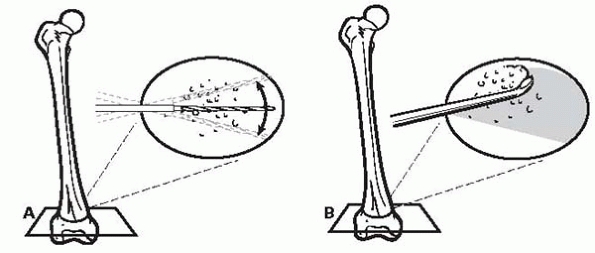
adjacent to the incision (Figs. 24-4A and B).
child with many years of remaining growth, consider concomitant
epiphysiodesis of the proximal fibula to avoid a prominent fibular
head. With proper respect for the peroneal nerve, this procedure has
been shown to be safe.10 Following ablation of the epiphysis,
the authors (both DLS and JMF) protect the limb with a knee immobilizer for about 4 weeks.
 |
|
▪ FIGURE 24-4 (A,B)
Minimalist technique of percutaneous epiphysiodesis. Drill from one side. Drill across the physis almost to the other side, then repeat with multiple passes at slightly different angles within the plane of the physis. When most of the physis is drilled, begin to windshield the drill back and forth. If too much force is used, the drill may break. A key part of staying out of trouble with this technique is to then use a curette to remove the portion of the physis adjacent to entrance of the drill. |
continued normal growth. These complications should usually be noted
within 6 months by serial radiographs. Stay out of trouble by
recognizing a partial growth arrest early, before significant angular
deformity develops. If recognized early, a repeat epiphysiodesis may be
all that is necessary, and the need for an osteotomy avoided.
insufficient growth remaining for an epiphysiodesis to work.
Complications of femoral shortening are more common and more serious
than epiphysiodesis; one way to stay out of trouble is to do the
epiphysiodesis early if possible. Femoral shortenings may be performed
open or closed. In general, avoid shortening greater than 5 to 6 cm, as
this may lead to muscular weakness.
equipment-heavy procedures prone to challenges. The posterior portion
of the cut along the linea aspera may require a separate incision. The
first osteotomy is easiest, as the intact femur acts as a lever arm. A
technical trick to help complete the second cut is to use the distal
femur as a (well-controlled) battering ram against the proximal piece.
Reaming is associated with respiratory distress syndrome, presumably
from fat emboli. Using fluted reamers and/or drilling a vent for canal
decompression have been suggested as possibly minimizing this
complication. Remember to pay attention to rotational alignment when
applying fixation to the segments. Knee heights will often end up
different, but that is not a functional problem and patients who expect
it ahead of time do not seem to be bothered.
have realistic expectations of the goals and challenges involved.
Families should expect a 100% complication rate at a minimum, with
multiple complications likely. They should understand that a
significantly lengthened leg will be thin, with ugly scars, decreased
ROM, and weakness—and unlikely to be exactly
the same length as the other leg. The surgeon and family must know
there is no way to reliably stay out of trouble with surgical
lengthening—it is just inherent in the procedure. Patient and family
selection is critical for this operation, both from a psychological and
physiologic perspective. Unstable parents provide inadequate support
for the program. In general, avoid heroic lengthenings if the foot is
bad, e.g., fibula hemimelia with a stiff 2-ray foot in rigid-equino
valgus is not an ideal candidate for lengthening.
Don’t be greedy. Consider making up half of the LLD with a
contralateral epiphysiodesis. If the family wants a “heroic”
lengthening, and you feel uncomfortable with this, refer the family to
a surgeon with a similar philosophy as the family. Having knees at
different levels is well-tolerated, so do not add significant surgery
or risk to avoid this “complication.” If a joint is potentially
unstable, which can conceivably be found in all congenital cases,
consider crossing the joint with the fixator prior to lengthening.
Acute injuries to nerves or blood vessels during application of device
is uncommon but potentially serious. Review of cross-sectional anatomy
is essential. As Dr. Vernon Tolo teaches, “You can invent an operation,
but not anatomy.”
dislocated at 1 cm of femoral lengthening. I wouldn’t want to give a
number, but there’s no question that complications that result from
soft-tissue tightness, such as knee flexion contracture and
subluxation, are more likely the longer the lengthening. I think it’s
best not to set a specific goal but to watch diligently for reasons to
stop.
-
Reliable time in frame (less infections, faster healing of the callus)
-
Frame fixation may loosen after a longer time
-
Joint stiffness present for a shorter time
Clinically the threshold of soft-tissue tolerance to gradual
lengthening is often limited to 15 to 20%.11
-
Use of monolateral
frames is OK if the joint does not need to be crossed. Start in some
valgus and expect to drift into varus with lengthening. Consider
prophylactic release of iliotibial band to help minimize varus drift. -
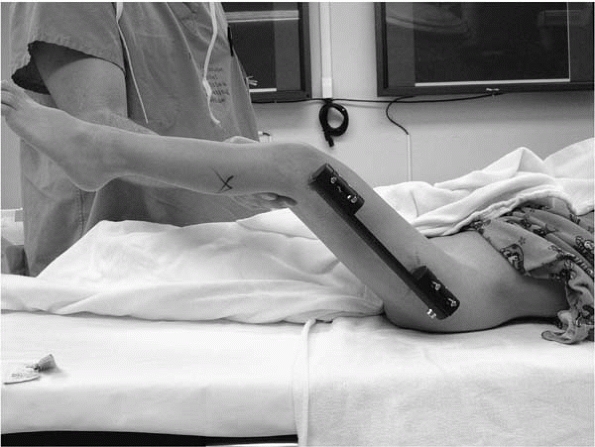
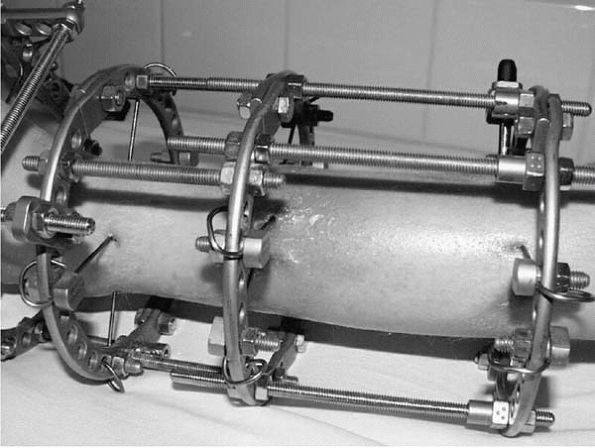
Ensure there is good knee motion at initial surgery. Release tensor fascia lata if tethering pins (Fig. 24-5).
-
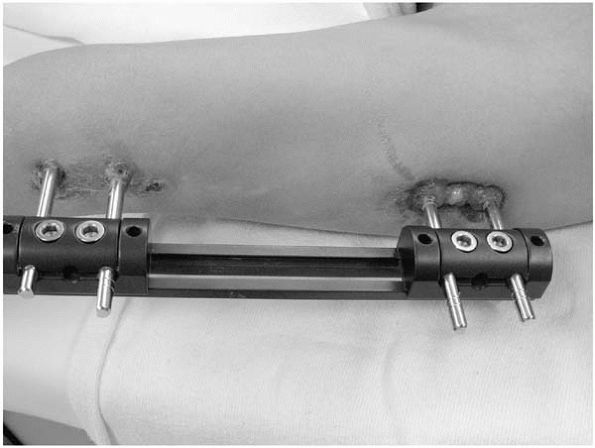
Surgeon and parents should expect poor knee ROM following femoral lengthening (Fig. 24-6).
 |
|
▪ FIGURE 24-5
Following placement of an external fixator for femoral lengthening, the knee is taken through a full range of motion. This minimizes soft-tissue tethering of the pins, in this case probably by allowing the distal pins to split the fibers of the iliotibial band. |
 |
|
▪ FIGURE 24-6
Despite physical therapy, and a modest 3-cm lengthening, the patient’s maximum knee flexion is 30 degrees even under anesthesia. With physical therapy this patient’s knee flexion returned to near normal within 6 months. |
-
Remove 1-cm section out of the fibula; a simple osteotomy may consolidate early (Fig. 24-7).
-
Pin or screw across ankle syndesmosis to prevent proximal migration of distal fibula.
-
For bilateral lengthenings especially, do not place unilateral devices medially, as they hit other devices during walking.
-
Consider Botox in gastrocnemius at initial surgery to prevent TAL equinus.
-
Don’t do bifocal lengthenings on tibia—higher nerve injury.12
 |
|
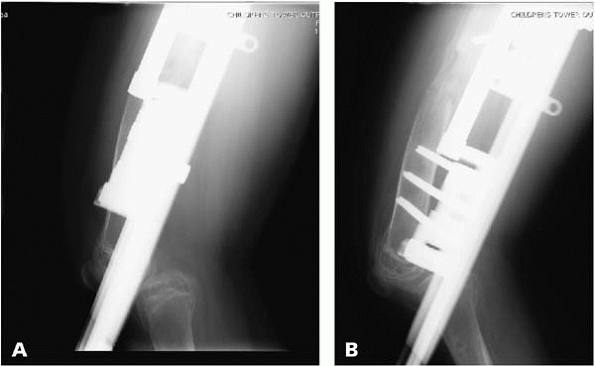
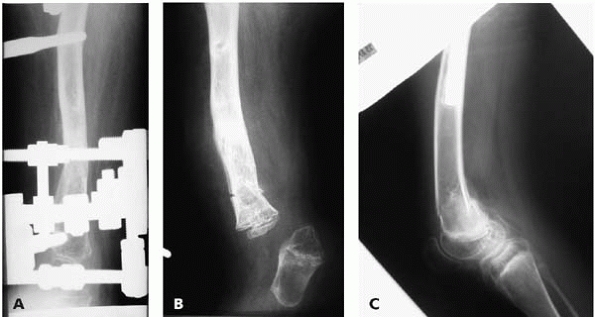
▪ FIGURE 24-7 The patient is undergoing a lengthening through a normal tibia and fibula. (A) Immediately post-operative period. Note that a fibular osteotomy was performed, but a section of the fibula was not removed. (B)
Patient 3.5 weeks later. There is more opening anteriorly at the tibial osteotomy site, and the pins are beginning to bend. These two findings should make one suspect that something is wrong. The fact that the fibula osteotomy has healed was not recognized at this time. (C) Lengthening was continued and 40 days later radiographs show that a separation of the proximal fibular physis has occurred. The bent pins and fibular healing were noted in this radiograph, but unfortunately the physeal separation was not appreciated. A second (and unneeded) fibula osteotomy was performed, but nothing needed to be done as the lengthening was proceeding nicely through the separated fibular physis. |
is the point at which most troubles occur. At followup visits look at
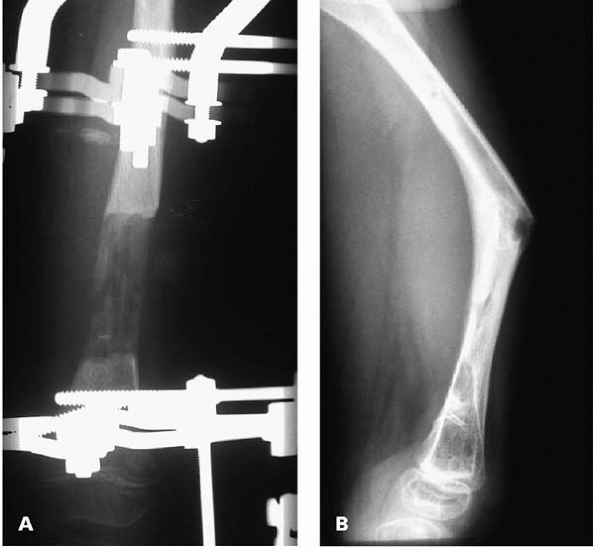
joint above and below for subluxation; the hip and knee are at risk (Figs. 24-8 and 24-9).
Knee subluxation is always preceded by a loss of full extension.
Persistent lengthening after a joint contracture has developed places
the joint at a higher risk for dislocation. At the point of persistent
significant lack of knee extension, stay out of trouble by stopping
lengthening, and even consider shortening. Surgical treatment in the
form of soft-tissue releases, and spanning the joint with the external
fixator, is often needed. Clearly label direction of turning on the
device, such as drawing an arrow on a piece of tape.
 |
|
▪ FIGURE 24-8
This child sustained a dislocated hip after a perhaps overenthusiastic femoral lengthening over an intramedullary rod in the setting of an abnormal hip. Note the severe osteopenia of the lengthened femur. |
 |
|
▪ FIGURE 24-9 (A,B)
After approximately 3.5 cm of lengthening, posterior subluxation of the knee was noted. Note that the lengthening apparatus may obscure the view of the knee, so extra attention to the adjacent joints is important in evaluation of radiographs. |
Avoid doing harm by recommending caustic agents. A reasonable primary
treatment of infected or inflamed pin sites is 10 days of an oral
antibiotic (cephalexin). Expect pin site infections, and give the
family a prescription for oral antibiotics so they can fill it when
needed (Figs. 24-10 and 24-11). Change the antibiotics if they are not working.
tethering over a pin, or entrapment in soft tissue—particularly the
peroneal nerve. Immediately stop
lengthening in this scenario. It has been shown that immediate
decompression of the affected nerve as soon as the injury is recognized
improves recovery.12
Do not hesitate to slow the rate of lengthening if there are
soft-tissue problems or poor distraction callus. Speed up lengthening
if there is concern over premature consolidation of callus.
 |
|
▪ FIGURE 24-10
This patient has cellulitis characterized by erythema, warmth, induration, and pain. Antibiotics at this point are mandatory. If there is not rapid improvement with oral antibiotics, hospital admission with intravenous antibiotics may be necessary. |
 |
|
▪ FIGURE 24-11
Pin sites may show local drainage and inflammatory tissue with the possibility of infection. Consider antibiotics and irrigation with whirlpool, Jacuzzi, etc. |
One method of helping to avoid this complication is to lengthen through
the metaphysis when possible, as the bending strength of bone is
related to the fourth power of the radius of the bone. There is
unfortunately no infallible method of predicting when the device can be
safely removed, though many have been studied. One criterion is that
radiographs should show cortical bone and the beginning of a medullary
canal of the regenerate in two planes. When removing the device in the
operating room, disconnect
the
device across the lengthened area but leave the pins in, while
stressing the callus, so the device may be easily replaced if the
callus is not yet sufficiently strong. Following removal of the
external fixator, stay out of trouble by recognizing (and sharing with
the parents) that the remaining bone is osteopenic and at risk for
fracture (see Fig. 24-10 and Fig. 24-13).
-
End of device
-
Bone consolidated
-
Turning the wrong way
 |
|
▪ FIGURE 24-12 (A,B) Fracture through the area of regenerate bone in a femoral lengthening and subsequent deformity.
|
 |
|
▪ FIGURE 24-13 (A,B) Fracture through a pin hole following device removal. (C)
Following removal of the external fixator, a distal femoral metaphyseal fracture occurred through the osteopenic bone. This is the same child seen in Figure 24-8. |
removed in the operating room, or the patient and surgeon will endure
much pain. As fracture through callus or pin-site is most likely
following device removal, consider protection of the lengthened bone
with a brace and/or crutches, although bracing is ineffective in
protecting the femur. Avoid forceful range of motion of the knee while
the patient is under anesthesia, as this may cause significant injury
to the cartilage.
showed that young adults who underwent a Symes amputation in childhood
showed no difference from normal adults in psychological testing,
quality of life or self esteem, and all 10 adults had no difficulty
walking or running. Before taking this obviously irreversible step,
consider a second opinion or having the patient presented at a
conference. When indicated, amputate early, before child and family
become attached to the limb.
-
Limb lengths must be verified by imaging and physical exam, as both methods are subject to error.
-
Adequate preparation of parental and patient expectations is essential.
-
Do not be greedy in lengthening; consider the middle way of combined contralateral epiphysiodesis and lengthening.
-
Assess family and patient for coping abilities—get a psychologist involved before surgery if in doubt.
-
Double-check
radiographic measurements and calculations of final LLD before
surgery—there is a high error rate in predicting final LLD. -
During lengthening focus on the soft tissues, alignment, and adjacent joints, not just radiographs of miraculous new bone.
-
Golden Rule: As in other aspects of life, function is more important than length.
JJ, Burke T, McCarthy MC. Need for concomitant proximal fibular
epiphysiodesis when performing a proximal tibial epiphysiodesis. J Pediatr Orthop. 2003;23(1):52-54.
JE, Kelly-Hahn J, Carpenter CJ, et al. Pin site care during external
fixation in children: results of a nihilistic approach. J Pediatr Orthop. 2000;20(2):163-165.
JG, Walsh SJ, Small JM, et al. Syme amputation for the treatment of
fibular deficiency. An evaluation of long-term physical and
psychological functional status. J Bone Joint Surg Am. 1999;81(11):1511-1518.