Examination of Facial Strength
– Neurologic Examination > Cranial Nerve Examination > Chapter 16
– Examination of Facial Strength
assess for lesions of the central or peripheral nervous system motor
pathways that move the face.
part of a complete neurologic examination. In most patients, the
examination of facial symmetry and strength can be limited to observing
the patient’s smile. For patients who present with a complaint of
facial weakness or who show evidence of facial weakness on examination,
a more detailed assessment to distinguish upper motor neuron from lower
motor neuron weakness should be performed, as described in How to
Examine Facial Strength.
begins in the motor cortex of each frontal lobe. Axons from these nerve
cells travel downward as the corticospinal tract, which then synapse at
the facial nerve nucleus in the pons. Axons from the facial nucleus—the
lower motor neuron for facial movement—leave the pons as the facial
nerve to innervate all of the muscles of facial expression on that side
of the face. The part of the facial nerve nucleus that moves the lower
part of the face (e.g., mouth movement) is innervated mainly by fibers
from the contralateral corticospinal tract. The part of the facial
nerve nucleus that moves the upper part of the face (e.g., forehead
wrinkling and eye closure) is innervated by fibers from both the
contralateral and the ipsilateral corticospinal tracts.
-
Ask the patient to smile. Assess for any
weakness or obvious asymmetry of mouth movement. If no significant
facial weakness is seen, the examination of facial strength can end at
this step; otherwise, proceed further. -
Ask the patient to raise his or her
eyebrows (show the patient what you mean by wrinkling your own
eyebrows). Look for any asymmetry of forehead movement. -
Ask the patient to close his or her eyes
tightly. Look for any obvious asymmetry of strength of eye closure, and
assess the ability of the patient to resist your attempt to open his or
her eyes.
 |
|
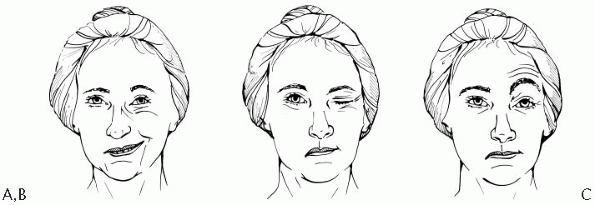
Figure 16-1 A patient with upper motor neuron facial weakness attempting to smile (A), close her eyes (B), and raise her eyebrows (C). The patient has a lesion of the left corticospinal tract causing right-sided facial weakness.
|
-
Weakness of the smile on one side of the
mouth with normal movement of the forehead muscles and normal eye
closure on that side (Fig. 16-1) is consistent
with a lesion of the corticospinal tract on the side contralateral to
the side of the facial weakness. In other words, a lesion of the left
hemisphere (or the left upper brainstem) involving the left
corticospinal tract causes weakness of the smile on the right side of
the mouth. This is called upper motor neuron facial weakness.
In upper motor neuron facial weakness, the muscles that move the
forehead and close the eye are spared because of the bilateral
corticospinal tract innervation to the part of the facial nerve nucleus
that performs these functions. -
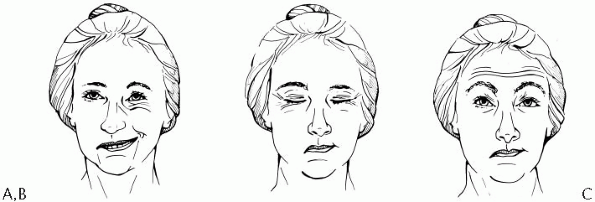
Weakness of an entire side of the face,
including weakness of the smile on one side of the mouth, one side of
the forehead, and weakness of closure of the eye (Fig. 16-2),
is consistent with a lesion of the facial nerve on that side. In other
words, a lesion of the right facial nerve (or its nucleus in the pons)
causes right lower motor neuron facial weakness. In lower motor neuron
facial weakness, all of the muscles that move the face on one side may
be affected because all of these muscles are innervated by the facial
nerve on that side.
-
The terminology describing facial
weakness can be confusing. Lesions of the upper motor neuron (the
corticospinal tract) cause weakness of the
P.54
lower
part of the face. Lesions of the lower motor neuron (the facial nerve)
cause weakness of the upper and lower parts of the face. Avoid
ambiguous terms such as “upper facial” and “lower facial” weakness.
It’s best to describe facial weakness as upper motor neuron type or
lower motor neuron type weakness.![]() Figure 16-2 A patient with lower motor neuron facial weakness attempting to smile (A), close her eyes (B), and raise her eyebrows (C). The patient has a lesion of the right facial nerve causing right-sided facial weakness.
Figure 16-2 A patient with lower motor neuron facial weakness attempting to smile (A), close her eyes (B), and raise her eyebrows (C). The patient has a lesion of the right facial nerve causing right-sided facial weakness. -
Patients commonly have a mild asymmetry (often described as flattening)
of the nasolabial fold on one side of the face compared to the other.
The nasolabial fold is the facial crease that extends from the nostril
to the corner of the mouth. Mild asymmetry of the nasolabial fold as an
isolated finding is usually of doubtful clinical significance. -
The evaluation of taste sensation in
patients with possible lower motor neuron facial weakness (such as in
Bell’s palsy) is described in Chapter 22, Examination of Taste. -
There are some additional unusual
findings that may be observed when looking at a patient’s resting
facial muscles; these should be looked for especially when there is a
complaint of abnormal involuntary facial movements.-
Hemifacial spasm
consists of intermittent twitches of the muscles on one side of the
face, characterized by unilateral eye blinking or twitching of the
muscles of one side of the cheek, or both; this generally occurs as a
result of compressive dysfunction of a facial nerve. -
Facial myokymia
consists of a continuous undulating and quivering movement of the
muscles on one side of the face, especially around one eye; this is
seen primarily in the setting of multiple sclerosis but has also been
described due to brainstem gliomas. -
Blepharospasm consists of intermittent involuntary tight blinking of both eyes; this is a form of focal dystonia (see Chapter 46, Examination of the Patient with a Movement Disorder).
-