Nonacute Shoulder Disorders
-
Anatomy. The
muscle tendon units of the supraspinatus, infraspinatus, and teres
minor compose the rotator cuff. Each has its own specific muscle body
but they coalesce together into one tendon as they pass through the
subacromial space. The borders of the subacromial space are as follows:
superiorly, the undersurface of the acromion and the acromioclavicular
(AC) joint; anteriorly, the coracoacromial ligament and coracoid;
inferiorly, the humeral head. The subacromial bursa also exists in the
subacromial space above the rotator cuff but underneath the acromion.
The long head of the bicep tendon and the subscapularis muscles are
important anterior stabilizers of the glenohumeral joint. -
Mechanism of injury.
Any anatomic influences that narrow the already confining subacromial
space have the potential to compromise, in particularly, the
superspinatus tendon and irritate the SA bursa. Thickening of the
bursa, undersurface spurring of the AC joint, instability of the
glenohumeral joint, or changes in the shape of the acromion (Fig. 16-1) are the most common reasons for rotator cuff compromise. This process of rotator cuff attrition is manifested as impingement syndrome.
The process of cuff disease begins with bursitis and reversible
tendinosis and gradually progresses to full-thickness cuff pathology
over time. -
History. The
typical patient with impingement syndrome is older than age 40 and
complains of anterolateral shoulder pain, which is worse with overhead
activities and positionally at night. -
Examination.
Examination begins by general inspection of the anterior and posterior
shoulder. Clearly visible atrophy of the posterior shoulder in the
region of the supraspinatus and/or infraspinatus muscle belly is an
indicator of a large rotator cuff tear. The differential diagnosis for
this atrophy would include suprascapular nerve entrapment. Shoulder
motion is often symmetric except for a loss of internal rotation.
Special tests include those for rotator cuff strength, impingement, and
instability. Supraspinatus weakness and pain is usually present to
strength testing. Tenderness is present over the anterior rotator cuff
and SA bursa. Significant weakness to external rotation strength
testing often indicates that a large rotator cuff tear is present. -
Roentgenograms.
Plain roentgenograms should be obtained in patients with a history of
acute trauma or in those who do not improve with standard nonoperative
treatment. Sclerosis of the greater tuberosity, narrowing of the
acromiohumeral distance, or spur formation at the AC joint or the
anterior acromion are all evidence of ongoing impingement syndrome. An
acromion that has an inferiorly directed hook at its anterior edge is
classified as a type III acromion (1) (Fig. 16-1).
This hooked acromion may predispose some patients to developing
anterior rotator cuff pathology by narrowing the SA space. Usually the
supraspinatus tendon is affected first. With patients in whom operative
intervention is indicated, further imaging studies may be obtained.
Arthrograms are widely available and easily used to detect the presence
of a rotator cuff tear. However, they do not give reliable information
regarding tear location, size, atrophy, or other associated subacromial
pathology. A magnetic resonance imaging (MRI) scan, gives more detailed
information regarding pathology in the SA space. It is more expensive
and may be susceptible to technical problems and misinterpretation. An
MRI
P.230
should only be ordered if it will change treatment recommendation (Table 16-1).
Physicians without adequate experience in the shoulder exam may wish to
refer prior to ordering the MRI. Ultrasonagraphy is another diagnostic
test that can, in the hands of an experienced ultrasonagrapher, give
good visualization of rotator cuff pathology.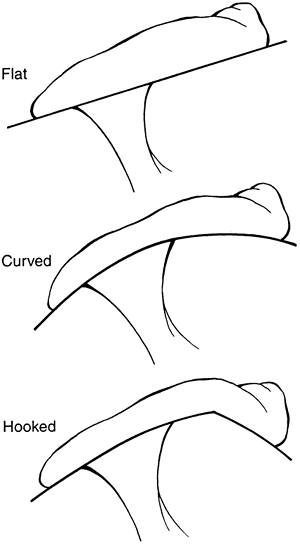 Figure 16-1.
Figure 16-1.
Bigliani classification of acromial morphology: type I, flat; type II,
curved; type III, hooked. (From Bigliani LU, Morrison DS, April EW. The
morphology of the acromion and rotator cuff impingement. Orthop Trans 1986; 10:288.) -
Diagnosis.
The topic of nonacute shoulder disorders often falls into the broad
categories of impingement and instability. While the former tends to
affect people older than age 30, and instability tends to affect those
younger than age 30, there is a large overlap. Additionally, both may
occur in the same patient. Impingement is generally the result of
either some bursitis, tendinopathy, or rotator cuff tears. These issues
will be addressed below. Instability, or a hyper-mobile glenohumeral
joint was addressed under the topic of shoulder dislocations in Chap. 15, II.C. Additional categories of
P.231
AC joint arthritis, adhesive capsulitis, arthritis, and scapulothoracic
disorders are causes of non-acute shoulder disorders and will be
discussed below.TABLE 16-1 MRI Scan Indications- Shoulder dislocation over age 40.
- Significant rotator cuff weakness.
- Family history of rotator cuff disease.
- Failure to respond to nonsurgical measures (physical therapy, injection).
-
Treatment
-
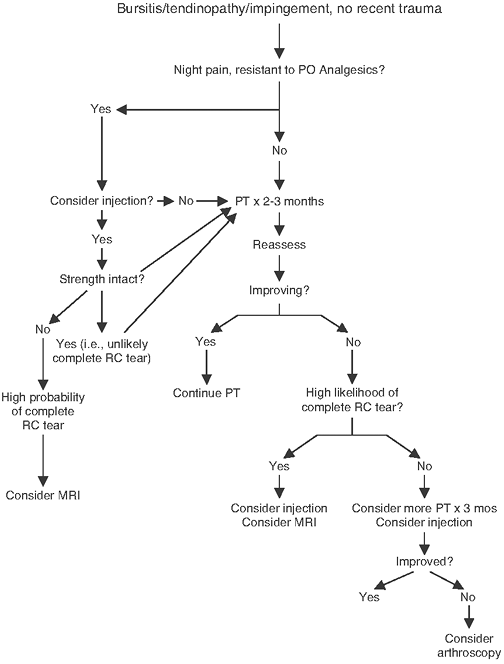
Bursitis/tendinopathy/impingement (Fig. 16-2).
The focus of treatment for chronic shoulder disorders is physical
therapy (PT). PT forms the basis for recovery for those who suffer from
impingement-type symptoms (e.g., with bursitis or rotator cuff
tendinopathy), instability, adhesive capulitis, scapulothoracic
dysfunction, and other nonacute shoulder pathology. The current
P.232
standard
for successful treatment is on returning the patient to his or her full
range of motion prior to focusing on strength. Poor posture associated
with our increasingly inactive lifestyles seems to be cause of poor
scapulothoracic stability and subsequent shoulder pain. It is important
to ask your physical therapists to address scapular stabilization in
the rehabilitation of most patients with chronic shoulder problems. The
scapula forms the starting point of the rotator cuff muscles (thus
important in rotator cuff tendinopathy), the origin of the acromion
(thus important in other causes of impingement), and of the glenoid
(thus important in shoulder instability). Our personal preference is
for the patient to have at least 6 to12 months of concentrated PT prior
to surgery unless otherwise indiciated (e.g., if there is a complete,
acute rotator cuff tear).![]() Figure 16-2.
Figure 16-2.
Diagram of treatment pathway for bursitis/tendinopathy/impingement with
no recent trauma. PT, physical therapy; RC, rotator cuff.Injections provide another important component in the treatment of nonacute shoulder problems (Table 16-2).
The most common is an SA injection, for which we prefer a
posterolateral approach due to its ease and avoidance of major
neurovascular structures (see chapter on injections for details). The
SA shoulder injection can be done with either diagnostic or therapeutic
goals. Diagnostically, one can theoretically “rule out” a complete
rotator cuff tear if a patient who had pain and weakness demonstrates
normal strength after an anesthetic injection. Therapeutically, pain
relief from an injection is for those who have pain that cannot be
treated adequately with oral medications (either due to a lack of
efficacy or side effects), those who are unable to perform PT due to
pain, and those with night pain that interrupts their sleep.-
Nonoperative treatment is successful in the majority of patients. The cornerstone of treatment is Physical therapy
to rehabilitate the rotator cuff muscles (especially the
supraspinatus), to regain scapulothoracic stability, and to correct any
contractures (typically loss of internal rotation). If physical therapy
alone is not successful, an injection of
corticosteroid and lidocaine into the SA space often brings the
patient’s symptoms under control. If the diagnosis of impingement
syndrome is correct, the lidocaine should give an excellent relief of
pain for 2 to 3 hours. If no lidocaine effect is obtained, alternative
diagnoses should be considered. The steroid typically takes 2 to 4 days
to take effect. The indications for an SA injection at the initial
visit include significant night pain or symptoms severe enough to make
progress in PT difficult. -
Operative treatment
is indicated in individuals who fail a minimum 6-month course of
nonoperative treatment. The goal of surgery is to open the SA space.
This is typically accomplished by excision of the thickened and
P.233
scarred
bursa, recession of the coracoacromial ligament, and an anterior
acromioplasty. Any other factors (AC joint hypertrophy or glenohumeral
instability) that may predispose the patient to impingement syndrome
should also be addressed. This opening of the SA space is termed a decompression.
A decompression may be completed through either open or arthroscopic
techniques. Arthroscopic techniques allow an evaluation of the
glenohumeral joint for any concomitant pathology. In addition, a
patient with an arthroscopic SA decompression recovers approximately 1
month sooner than an open SA decompression.
-
-
Rotator cuff tears
-
Younger patients
(younger than 55 years old) or those with true acute tears typically
undergo surgical repair. Repairs for complete tears are best done if
within 3 months of injury when possible. -
Older patients
often do well with physical therapy and nonoperative treatment. MRI
studies of asymptomatic patients older than 60 years of age have shown
that 50% have some form of rotator cuff pathology. An SA decompression
and rotator cuff repair are indicated only after nonoperative measures
have failed. In older, low functional demand patients with large
rotator cuff tears, an SA decompression alone often yields good pain
relief, but only limited improvement in function. Patients with a
massive, irreparable rotator cuff tear and glenohumeral arthritis often
respond well to physical therapy and an SA injection. If nonoperative
treatment fails, arthoscopic glenohumeral joint debridment and limited
SA decompression may be indicated. A hemi-arthroplasty is another
acceptable form of operative intervention.
-
-
Calcific bursitis.
involves deposition of a calcium salt into the substance of the rotator
cuff tendon. This paste-like material may escape into the SA bursa,
causing an acute inflammatory bursitis. Severe symptoms of impingement
syndrome result. An SA injection with corticosteroids with lidocaine
and PT are effective in controlling acute symptoms. If repetitive
episodes of pain occur, an arthroscopic excision of the calcific
deposit is indicated. -
Long head of biceps tendinitis (see Chap. 15, IV) often occurs as part of impingement syndrome and is treated with the same program.
-
range of motion may have a problem with their glenohumral joint, either
a bony obstruction (arthritis) or a capsular adhesion (adhesive
capsulitis or “frozen shoulder”). Note that these two problems can be
distinguished from a rotator cuff tear by noting differences between
active and passive range of motion. A patient with a rotator cuff tear
may have more passive than active range of motion, whereas, one with
true glenohumeral pathology will have equal passive and active range of
motion (Table 16-3).
-
Arthritis
-
Etiology.
Arthritis of the glenohumeral joint may be idiopathic (osteoarthritis),
secondary to inflammatory disease (rheumatoid or psoriatic arthritis),
or posttraumatic. Given that the shoulder is not a weight-bearing
joint, symptomatic arthritis of the
P.234
glenohumeral joint is not as common as arthritis of the knee and hip.TABLE 16-3 Diagnostic Range of MotionEtiology Range of motion Full thickness rotator cuff tear Passive may be greater than active Osteoarthritis Passive = Action Adhesion capsulitis Passive = Action -
History.
Nonspecific lateral shoulder pain is present, which is made worse with
increased activities. Stiffness is also a frequent complaint.
Polyarticular complaints should arouse the suspicion of an inflammatory
disorder. -
Examination
reveals loss of active and passive range of motion, crepitus on joint
motion, and mild diffuse muscle atrophy. Strength is usually not
significantly affected. Distal neurovascular changes are rare. -
Roentgenographic
studies should include an anteroposterior view of the shoulder in 30
degrees of external rotation and an axillary view. Narrowing of the
glenohumeral joint space and inferior spur formation on the humeral
head is an indication of osteoarthritis. Periarticular erosions are
suspicious for inflammatory disease. A computed tomography scan to
exactly determine glenoid version or an MRI scan to assess rotator cuff
status and glenoid version may be indicated preoperatively. -
Treatment
-
Nonoperative treatment
is directed toward controlling the pain with analgesics, injections of
the glenohumeral joint with anesthetics and corticosteroids, and
improvement of joint mechanics (especially range of motion) with PT and
lifestyle modification. -
Operative treatment.
In early cases of inflammatory arthritis, an arthroscopic synovectomy
may yield improvement of symptoms. Once the articular surface is eroded
to bone, either a hemiarthroplasty, a total shoulder replacement, or an
arthrodesis is indicated. A total shoulder replacement results in the
best function of the glenohumeral joint and pain relief (2) but may not be indicated in young patients or patients with heavy occupational demands.
-
-
-
Adhesive capsulitis (frozen shoulder)
-
Etiology
-
Idiopathic adhesive capsulitis results
from capsular fibrosis. The pathologic mechanism for this fibrosis is
not well understood (3). -
Adhesive capsulitis may result from
capsular fibrosis from a traumatic or surgical event or may be
associated with a systemic disease such as diabetes, thyroid disorders,
cervical disc disease, or neoplastic disorders of the thorax.
-
-
History. The
patient complains of a deep, achy pain in the shoulder that is present
at rest as well as with activities. Complaints of loss of motion follow
the onset of the pain by several weeks. A careful past medical history
and review of systems is necessary to rule out any systemic causes.
Diabetes mellitus and thyroid abnormalities often predispose people to
adhesive capsulitis. Distal neurovascular complaints are rare. -
Examination.
A global loss of active and passive range of motion is noted. Internal
and external rotation are typically affected first. Nonspecific
tenderness is usually present early in the disease process. Rotator
cuff strength is often normal but may be difficult to assess secondary
to the limited and painful range of motion. -
Roentgenographs are typically unremarkable.
-
Treatment
-
Nonoperative
management with a home-based stretching program as well as pain
medication if necessary is successful in 90% of patients. Symptoms may
take up to 18 months to resolve. Occasionally, an injection of the
glenohumeral joint with corticosteroid is necessary to control pain (4). -
Operative treatment
is directed at releasing the contracted capsule in a sequential fashion
to improve range of motion. This may be accomplished either closed or
arthroscopically. Any associated pathology (especially in the SA space)
should also be addressed (5). Operative intervention typically not indicated until the patient fails 12–18 months of nonoperative care.
-
-
-
Arthritis
-
Etiology. Osteoarthritis of the AC joint is extremely common in individuals older than 50 years of age and most are asymptomatic (6). Inflammatory
P.235
processes such as rheumatoid arthritis or fractures of the distal
clavicle can also cause AC joint symptoms. Younger patients may develop
nonacute AC joint pain from activities such as weight lifting. -
History. Pain
is localized to the superior aspect of the AC joint. Symptoms are worse
when sleeping on the affected side. Overlap symptoms with impingement
syndrome are common. -
Examination.
Tenderness over the subcutaneous aspect of the AC joint is present. The
extreme motions of forward flexion and cross body adduction are limited
and painful. Frequently, coexisting rotator cuff findings are present. -
Roentgenograms are similar to those obtained for patients with impingement syndrome. A Zanca view is helpful.
-
Treatment is
directed at controlling local symptoms with PT, analgesics, and, if
necessary, a corticosteroid and lidocaine injection into the AC joint.
A typical AC joint will accept 1 to 2 cc of volume. If nonoperative
treatment fails, a distal clavicle resection is indicated. This may be
completed either via arthroscopic or open techniques (7).
-
-
Osteolysis of
the clavicle may occur following a traumatic injury to the AC joint or
in individuals who place repeated unusual stress on the AC joint, such
as weight lifters. Radiographic changes consist of osteopenia and
erosive changes in the articular surface. Treatment is similar to that
described for arthritic conditions.
-
Scapulothoracic bursitis (snapping scapula)
-
Etiology. The
scapula has a significant excursion across the chest wall with range of
motion of the shoulder girdle. This motion requires the presence of a
large bursa between the scapula and the thorax. Inflammation of this
bursa can be caused by overuse of the shoulder, serratus anterior
contracture, or a bony deformity on the undersurface of the scapula (8). -
History.
Patients complain of pain deep and medial to the scapula on the thorax
posteriorly. The hallmark symptoms of this disorder are catching or
crepitus with motion of the scapula. -
Examination. Scapulothoracic motion may be limited. The patient can usually reproduce a palpable sensation of crepitus under the scapula.
-
Imaging studies are not typically useful unless there is a history of trauma or there is suspicion of an osteochondroma under the scapula.
-
Treatment is
directed at increasing motion of the superior medial angle of the
scapula away from the thorax and strengthening the periscapular
muscles, or noninvasive techniques may include deep friction massage
and ultrasound. Occasionally, a corticosteroid injection into the
scapulothoracic bursa is necessary. If nonoperative methods fail, an
arthroscopic or open excision of the bursa and the superior medial
angle of the scapula is indicated (9).
-
-
Winging of the scapula
-
Etiology. The
scapula is held against the thorax by the serratus anterior muscle,
which is innervated by the long thoracic nerve. Anything that disrupts
either of these two structures results in winging of the scapula.
Pseudo-winging of the scapula (scapular dyskinesia) is far more common
than true winging and develops when the periscapular muscles do not
work in a synchronized manner. -
History.
Weakness and loss of active motion of the shoulder is noticed first.
Secondary symptoms of rotator cuff inflammation (secondary impingement
syndrome) may develop. A history of trauma to the chest wall in the
location of the long thoracic nerve may be present. Most patients do
not have a readily identifiable cause for their serratus anterior
dysfunction (10). Fascioscapulohumeral muscular dystrophy often initially presents with isolated winging of one or both scapulae. -
Examination.
Winging of the scapula occurs when the medial border of the scapula is
rotated outward and laterally, causing the scapula to give the
appearance of “wings” on the patient’s back (Fig. 16-3).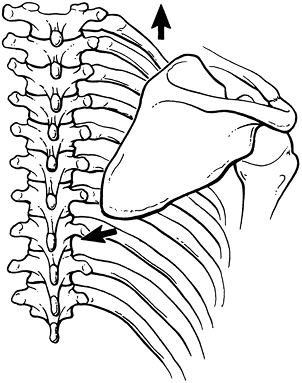 Figure 16-3.
Figure 16-3.
Position of the scapula with primary scapular winging due to serratus
anterior palsy. The scapula pulls away from the back and does not
protract on arm elevation. (From Kuhn JE, Hawkins, RJ. Evaluation and
treatment of scapular disorders. In: Warner JJP, Iannotti JP, Gerber C,
eds. Complex and revision problems in shoulder surgery. Philadelphia, PA: Lippincott-Raven, 1997: 357–375.) -
Treatment is
directed at strengthening the periscapular muscles and observation to
determine whether the long thoracic nerve will recover. If after 18
months no recovery is present, either a pectoralis major tendon
transfer or a scapulothoracic fusion is indicated.
P.236 -