Developmental Dysplasia
– HIP > Part B – Evaluation and Treatment of Hip Disorders > 5 –
Developmental Dysplasia
most common neonatal orthopaedic problems, and it has variable
morphologic patterns. The term refers to an abnormal relationship
between the femoral head and the acetabulum and includes the fetal,
neonatal, and infantile periods. It results in anatomic abnormalities
leading to increased contact pressure in the joint and, eventually,
coxarthrosis. Abnormal mechanical forces on the head of the femur may
contribute to DDH; however, the primary cause is still unknown. The
pathomorphologic appearance commonly includes an increased femoral
neck/shaft angle, increased anteversion of the proximal femur and a
shallow acetabulum. In untreated or unsuccessfully treated cases, pain
and disability commonly necessitate reconstructive surgery or hip
replacement at some time during adult life. However, many patients with
hip dysplasia become symptomatic before the development of severe
degenerative changes because of abnormal hip biomechanics, hip
instability, impingement, or associated labral pathology. Several
nonarthroplasty treatment options are available. The primary deformity
is most commonly acetabular; therefore, for many patients; a
reconstructive osteotomy that restores more nearly normal pelvic
anatomy is often considered. Total hip arthroplasty for the treatment
of DDH can be complex with technical challenges on both the acetabular
and femoral sides.
pathogenesis of DDH. During embryonic development the hip joint, both
femoral head and acetabulum, develop from the same primitive
mesenchymal cells, and after 11 weeks the hip joint is fully formed. At
birth the femoral head is deeply seated in the acetabulum and is
difficult to dislocate. In a dysplastic hip, however, the femoral head
can easily be subluxated or dislocated. Several theories regarding the
cause of congenital dysplasia have been proposed, including mechanical
factors, hormone-induced joint laxity, primary acetabular dysplasia,
and genetic inheritance. Breech delivery, with the mechanical forces of
abnormal flexion of the hips, can be seen as a cause of dislocation of
the femoral head. It has been observed that in boys, DDH often occurs
in association with concomitant deformities and oligohydramnios,
whereas in girls it has been attributed to hormone-induced laxity of
the hip capsule.
weeks after birth, occasionally a dislocation will occur up to 1 year
of age in patients documented to be normal previously. This is
particularly true among infants with either a positive family history
of DDH, breech presentation, or a persistent hip click on clinical
examination. Hence, it is important to screen for DDH even after the
newborn period.
genetic factors, habits, and cultural practices of different
populations. The historical incidence was between 0.5 and 1.5 cases per
1,000 live births. By current clinical testing almost 10 to 20 newborns
per 1,000 are considered to have abnormal hips and therefore normally
receive some type of treatment. DDH is approximately five to eight
times more common in girls than in boys with the ratio of reported
prevalences ranging from 2.4:1 to 9.2:1. Breech deliveries make up
approximately 3% to 4% of all deliveries, and the incidence of
congenital dysplasia of the hip is increased in this patient
population. A family history of DDH of the hip increases the likelihood
of this condition to approximately 10%. The risk of a genetic influence
was noted by Ortolani, who reported a 70% incidence of a positive
family history in children with congenital dysplasia of the hip.
Infants treated in a neonatal intensive care unit are also at higher
risk. The incidence of DDH is as high as 50 per 1,000 births in Lapps
and North American Indians; however, it is almost nonexistent among
Chinese and those of African descent. In general, it is more common in
white children than in black children. An increased incidence of
congenital dysplasia of the hip has been reported in cultures that
place infants in swaddling clothes with the hip in constant extension.
femoral head, concentrically reduced in the acetabulum, is a very
important stimulus for the normal growth of the triradiate cartilage
and the three ossification centers of the acetabular portion of the
pubis, ilium, and ischium to form a concave acetabulum. The altered
growth and bony deformities characteristically include increased
neck/shaft and anteversion angles in the proximal femur. The femoral
head is usually small, the neck may be short, the greater trochanter is
displaced posteriorly, and the femoral canal is narrow. On the pelvic
side, the true acetabulum is typically shallow, lateralized,
anteverted, and deficient anteriorly and superiorly. Occasionally the
whole hemipelvis is underdeveloped. Retrotorsion problems of the
acetabulum and/or femur are also seen rarely and may lead to anterior
impingement. In combination, these abnormalities lead to a decreased
contact area between the femoral head and acetabulum and to
lateralization of the center of hip rotation, which increases the
body-weight lever arm.
however, the longer DDH goes undetected, the greater is the
developmental impairment of both the femoral head and the acetabulum.
In adults, the natural history of untreated complete dislocation
depends on the presence or absence of a well-developed false acetabulum
as well as bilaterality. Back pain eventually occurs in patients with
bilateral dislocations. This is thought to be secondary to associated
hyperlordosis of the lumbar spine. In unilateral hip dislocations,
secondary problems of limb-length inequality, deformity of the hip,
ipsilateral knee pain, scoliosis, and gait disturbances are common.
laxity to severe acetabular, femoral head, and femoral neck dysplasia.
The anatomical definition of dysplasia refers to inadequate development
of the acetabulum, the femoral head, or both. Anatomical classification
is performed using the system of Severin (Table 5-1).
It has been shown that this classification, a simultaneous evaluation
of acetabular dysplasia, femoral head deformity and subluxation,
correlates well with long-term radiographic, clinical, and functional
outcome.
|
TABLE 5-1 Severin Classification for Radiographic Results
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
TABLE 5-2 Classification of HIP Dysplasia by Hartofilakidis
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
the degree of dysplasia, i.e., the grade of subluxation. It is
calculated using an anteroposterior radiograph by measuring the
vertical distance between the interteardrop line and the junction
between the femoral head and the medial edge of the neck. The amount of
subluxation is the ratio between this distance and the vertical
diameter of the undeformed head. When the femoral head is deformed, the
predicted vertical diameter of the femoral head has been found to be
20% of the height of the pelvis as measured from the highest point on
the iliac crest to the inferior margin of the ischial tuberosity. It is
graded as grade I (<50% subluxation), grade II (50% to 75%
subluxation), grade III (75% to 100% subluxation), or grade IV
(>100% subluxation). An alternate classification by Hartofilakidis (Table 5-2) has also been suggested. 1
regularly to detect early signs of coxarthrosis following the increased
contact pressure in the joint secondary to the anatomic abnormalities.
Growth disturbance of the proximal femur, which may be associated with
femoral head avascular necrosis, may be a problem after treatment of
DDH. History should be taken, and differential diagnosis that includes
inflammatory disease, neuromuscular disease, traumatic epiphyseal slip,
congenital coxa vara, and abnormal joint laxity should be considered.
Incomplete femoral head coverage can also be observed in various
conditions other than DDH (cerebral palsy, pelvic tilt). The natural
history of dysplasia should be discussed with the patients and
radiographs evaluated periodically to monitor the joint for development
of arthritis.
have distinct features from that of the child. A careful documentation
of the leg length and evaluation of impingement signs should be
performed. A thorough examination is essential in eliciting signs that
confirm clinical suspicions. Clinical examination begins with
inspection of the lower
extremity and includes assessment of gait, limb lengths, muscle power, range of motion, and special tests.
should be noted. Quadriceps atrophy can be indicative of severe or
chronic hip problems. The position that the leg spontaneously takes
should be carefully observed. This is true not only for abduction and
adduction but also for rotation, as for example a leg maintained in
internal rotation can be associated with femoroacetabular impingement.
Range of hip motion is commonly normal in early hip dysplasia and will
begin to decrease as the degree of secondary coxarthrosis increases. A
fixed adduction contracture or very limited abduction that reproduces
hip pain and may produce a palpable clunk is a sign of hinge abduction
present in residual Perthes disease deformity.
described the “gear stick” sign, which will help differentiate
trochanteric overgrowth from other sources of decreased hip abduction.
With this test hip abduction is full in flexion but is limited in
extension by impingement of the greater trochanter on the ilium or
posterior wall of the acetabulum.
patient prone, the knee flexed, and the hip undergoing rotation. The
piriformis and the posterior border of the gluteus medius may be tender
on direct palpation, and occasionally this tenderness may extend to the
lateral border of the sacrum. In patients with coxa vara with decreased
femoral anteversion, tight external rotators as well as hamstrings may
be demonstrated. Tight external rotators can also be seen in patients
with acetabular retroversion because they maintain their leg in
external rotation to minimize anterior impingement and can subsequently
develop contractures.
external rotation in full extension, is seen in femoroacetabular
impingement of various causes. If there is already a lack of full
extension, the extension maneuver may force the hip into internal
rotation to avoid posteroinferior contact between the acetabulum and
the femoral head. If there is an osteophyte present on the posterior
aspect of the femoral head, then full extension may become possible
only with hip abduction.
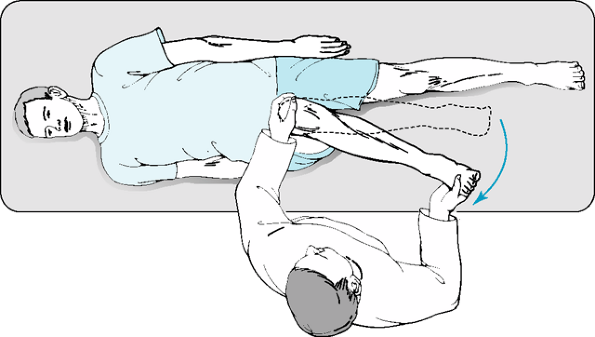
rim syndrome. The hip is internally rotated as it is flexed 90 degrees
and adducted 15 degrees (Fig. 5-1). This
combination of movement brings the proximal and anterior part of the
femoral neck into contact with the anterior rim of the acetabulum,
which is the usual location for labral disease. This will elicit sharp
pain from a mobile os acetabuli or a torn, degenerative, or ossified
anterior acetabular labrum. An uncommon cause for a positive
impingement test is acetabular retroversion or decreased femoral neck
anteversion, as both of these anatomic variants result in early
acetabular-femoral neck impingement with internal rotation.
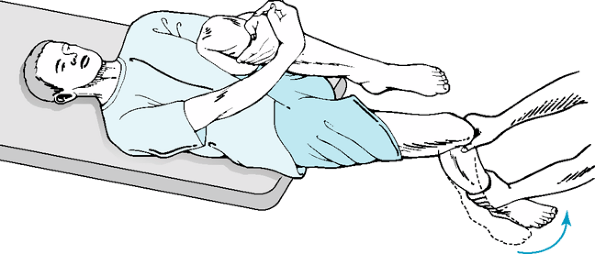
instability. The patient lies supine and the hip is adducted and
externally rotated, producing discomfort and a sense of instability as
the femoral head experiences deficient anterior acetabular coverage (Fig. 5-2).
In a very thin patient this external rotation in extension can produce
a mass in the inguinal region referred to as a “lump sign,” which
represents the femoral head pushing against the anterior hip capsule.
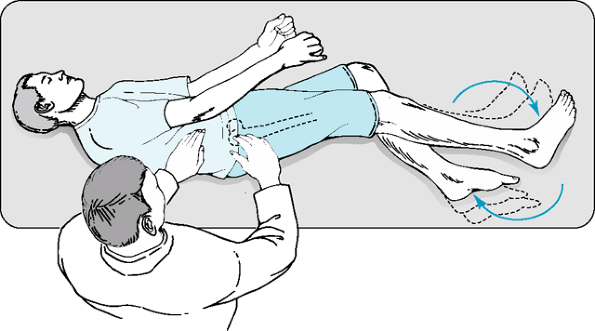
examined in the lateral position with the affected hip up and a bicycle
pedaling maneuver performed as the lateral and posterior margins of the
trochanter are palpated. Provocation of this maneuver can be performed
by increasing the load on the pedaling foot, which may exacerbate the
pain (Fig. 5-3).
border of the gluteus medius. Under direct palpation, often a
crepitation may be felt over the trochanteric bursa, which the patient
may have previously described as a sensation of “sand in the joint.”
authors as a sign of labral disease. Our experience, however, has
demonstrated that in dysplastic hips with deficient anterior coverage,
or in other causes of anterior femoral head prominence such as
increased femoral neck anteversion, if the extremity is actively flexed
and externally rotated and then brought back slowly toward extension
and neutral rotation, at between 40 degrees and 50 degrees of external
rotation, the iliopsoas tendon snaps over the uncovered femoral head.
With the same maneuver in neutral or internal rotation, this click is
eliminated.
with DDH. It is often reported with hyperextension and external
rotation of the hip and thought to be secondary to subluxation of the
femoral head. Locking, giving way symptoms, and catching may indicate
associated labral or chondral pathology. Patients with subluxated hips
usually have symptom onset at a younger age than those with complete
dislocations. Invariably, radiographic subluxation leads to
degenerative joint disease. The rate of deterioration is related
directly to the severity of the subluxation and the age of the patient.
Patients with the most severe subluxations usually develop symptoms
during the second decade of life. Those with moderate subluxation often
present at 30 to 40 years of age, and those with minimal subluxations
experience symptoms usually in their 40s or 50s. Patients with complete
dislocations and high-riding hips often will not develop problems until
the fifth or sixth decades of life. It is rare to see radiographic
changes of degenerative joint disease such as joint space narrowing,
osteophyte formation, or subchondral cysts at symptom onset. The only
radiographic signs may be subchondral sclerosis in the weight-bearing
area. After clinical symptoms and radiographic signs of degenerative
joint disease appear, progression is rapid.
clinical examination already described and the radiographic imaging as
described below. DDH-related problems such as back pain, secondary
problems of limb-length inequality,
deformity of the hip, ipsilateral knee pain, scoliosis, and gait disturbances need to be considered.
 |
|
Figure 5-1 Impingement test.
|
with DDH depends on age and differs for diagnostic versus management
situations. Plain radiographs, including an anteroposterior view of the
pelvis and lateral view of the hip, are the first steps in imaging
evaluation.
arthroplasty is indicated will not routinely require additional
imaging. However, occasionally with complex cases a three-dimensional
CT scan with reconstructions may give additional information. Further
imaging is required in patients in whom joint salvage procedures are
being considered. A false profile image, which is a standing lateral
hip image, will give valuable information on anterior femoral head
coverage and aids in preoperative planning. Abduction and adduction
views should also be obtained to assess joint congruency and
containment. Labral pathology is best evaluated with MR/MR arthrogram.
It is normally indicated in the rare patient presenting with labral
pathology with minimal dysplasia in whom arthroscopy alone may be given
consideration. MRI can also be helpful in the evaluation of loose
bodies, chondral defects, and synovial disease.
 |
|
Figure 5-2 Apprehension test.
|
the assessment of the Shenton line, the Tonnis angle, the center edge
(CE) angle, and the extrusion index. The Shenton line is drawn between
the medial border of the neck of the femur and the superior border of
the obturator foramen. In the normal hip this line is an even,
continuous arc, whereas in a dislocated hip with proximal displacement
of the femoral head, it is broken and interrupted.
demonstrate the full degree of hip dysplasia that is clearly present on
a false profile view. The false profile image should be evaluated with
regard to the ventral center edge angle.
evaluation of acetabular dysplasia, femoral head deformity, and
subluxation (Table 5-1). It has been shown to
correlate well with long-term radiographic, clinical, and functional
outcomes. Degenerative changes are classified according to Tonnis on a
scale from absent (grade 0) to severe (grade III).
dysplastic patients with regard to age, severity of radiographic
changes, symptoms, and patient expectations. Treatment alternatives
vary with each of these factors.
high-impact activities should be avoided. Although controversy does
exist, most would agree that the surgical alternatives should be
reserved for symptomatic patients with severe limitation of their daily
activities.
arthroscopic surgery, pelvic osteotomy, femoral osteotomy, arthrodesis,
and resection arthroplasty. The main goal of these procedures is to
decrease pain. Arthroscopy can be beneficial when symptoms seem to be
related only to labral tears or lose bodies in the absence of severe
structural abnormalities about the hip. Fusion and resection
arthroplasty are rarely, if ever, indicated given current treatment
alternatives. The operative treatment of residual dysplasia of the hip
after skeletal maturity is based on the assumption that the dysplasia,
if left untreated, will lead to secondary osteoarthritis of the hip.
described for late salvage in cases of persistent acetabular
maldevelopment and instability (Table 5-3). The
common goals of such interventions are the provision of improved
acetabular coverage, enhanced femoral head–acetabular congruence and
containment, and improved joint biomechanics. Some osteotomies are also
expected to slow down progression of degenerative changes by better
distributing forces applied through the hip joint, and they may provide
better distribution of bone stock that might facilitate further
reconstructive surgery if required in the future. In the presence of
severe degenerative changes, total joint arthroplasty gives the most
predictable outcomes.
 |
|
Figure 5-3 Abductor fatigue test (bicycle test).
|
dysplastic hips with mechanical symptoms related to either loose bodies
or labral tears. Retrotorsion problems of the acetabulum and femur
should be ruled out before offering this procedure. Arthroscopic
debridement and lavage in the presence of degenerative changes is a
less predictive procedure. Arthroscopy alone has limited applications
in the dysplastic hip because the underlying bony deformities cannot be
addressed.
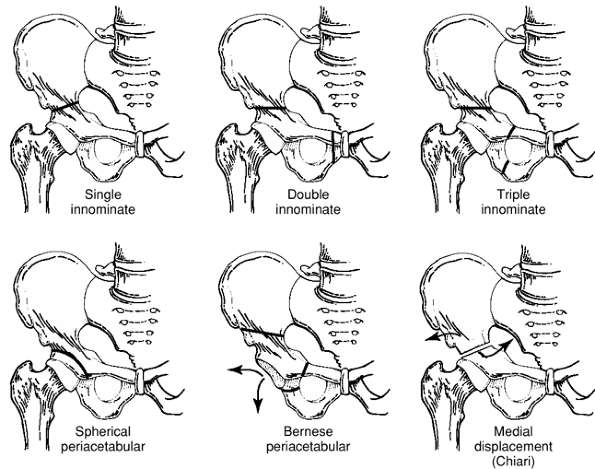
hip joint are attractive in the patient with hip dysplasia. Increased
joint congruity after reorientation of the osteotomized fragment allows
load transmission through a broader area, which can reduce articular
surface pressure. In general, osteotomies should be offered to young
patients who have symptomatic hip dysplasia without excessive proximal
migration of the center of rotation, reasonably well-preserved range of
motion, and no more than mild degenerative changes on the articular
surface (Fig. 5-4, Table 5-3).
The Salter single innominate osteotomy is beneficial in children, but
often is insufficient in adults because it allows limited correction
(approximately 10-degree change in Tonnis angle) owing to the decreased
flexibility of the symphysis pubis. It also lateralizes the hip joint,
which is undesirable in dysplastic hips. So-called salvage procedures
such as the Chiari iliac osteotomy and shelf procedures still may be
indicated in some severely dysplastic hips that cannot be rendered
congruent by a reconstructive osteotomy because of the discrepancy in
sizes and shapes between the femoral head and the acetabulum.
|
TABLE 5-3 Osteotomies for Developmental Dysplasia of the HIP (DDH) in Adults
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
preferred by many reconstructive surgeons. The procedure is indicated
in patients with a closed triradiate cartilage. It requires only one
incision and is performed with a series of straight, relatively
reproducible extra-articular cuts. 3
It allows large corrections of the osteotomized acetabular fragment in
all directions. The osteotomy includes a partial osteotomy of the
ischium, a complete osteotomy of the superior pubic ramus, an
incomplete osteotomy of the ilium, and a final cut connecting the ileal
cut to the ischial cut. The posterior column of the hemipelvis remains
intact, allowing early ambulation. The periacetabular fragment is
mobilized once the osteotomies are completed.
acetabular sourcil is horizontal, the femoral head is congruous,
appropriate version has been obtained, the femoral head is medialized
to within 5 to 15 mm of the ilioischial line, and the Shenton line is
near normal. The joint may be opened and evaluated for labral lesions.
effective technique for surgical correction of a severely dysplastic
acetabulum in adolescents and young adults (Fig. 5-5). The early clinical results have been reported in several series, including a series by Clohisy et al. 4
in which results were reported as very good at an average of 4.2 years
postoperatively. If a total hip arthroplasty is necessary at a later
stage, this can be done safely in patients with a previous
periacetabular osteotomy and should provide excellent results. 5
The Bernese periacetabular osteotomy can also be used successfully to
treat neurogenic acetabular dysplasian skeletally mature patients. 6
arthroplasty and should be considered only in those instances in which
other reconstructions are impossible: when the femoral head cannot be
centered adequately in the acetabulum or in painfully subluxated hips
with early signs of osteoarthritis. This procedure deepens the
deficient acetabulum by medial displacement of the distal pelvic
fragment and improves superolateral femoral coverage. The Chiari
procedure is an operation that places the femoral head beneath a
surface of joint capsule and cancellous bone with the capacity for
regeneration and corrects the lateral pathologic displacement of the
femur. The biomechanical effect of medial weight-bearing transfer is to
unload the femoral head and reduce the demands on the abductor
musculature. The angle of osteotomy is 10 to 20 degrees relative to the
plane of the upper acetabular margin, and the lower segment is
displaced medially by approximately half its width. The superior
fragment of the osteotomy then becomes a shelf, and the capsule is
interposed between it and the femoral head.
dislocations that have been reduced and in which no other osteotomy
will establish a congruous joint with apposition of the articular
cartilage of the acetabulum to the femoral head. In a classic shelf
operation, the acetabular roof is extended laterally, posteriorly, or
anteriorly, either by a graft or by turning the acetabular roof and
part of the lateral cortex of the ilium distally over the femoral head.
femur is the primary site of deformity or when a pelvic osteotomy alone
does not provide sufficient correction. Several requirements must be
fulfilled before proposing an isolated femoral osteotomy. First, the
osteotomy must be able to provide satisfactory correction of the
deformity. Second, the preoperative range of motion
should
be sufficient to allow a functional arc of hip motion after correction.
Third, the joint should be congruent in the proposed position of
correction. Most patients with hip dysplasia who are candidates for
isolated femoral osteotomy have coxa valga with mild acetabular
deformity.
 |
|
Figure 5-4 Osteotomy options.
|
secondary to hip dysplasia, total hip arthroplasty (THA) is the
procedure of choice. As described elsewhere in the text, there are
specific challenges on both the acetabular and femoral sides of the
reconstruction. Based on the severity of subluxation, a number of
different options are available for acetabular/femoral reconstruction (Table 5-4).
|
TABLE 5-4 Total HIP Arthroplasty Reconstruction Options Based on Severity of HIP Dysplasia (Crowe Classification)
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||
acetabular component in the true acetabulum. There may be bone stock
deficiency superiorly depending on the degree of dysplasia and
additionally the true acetabulum may have increased, or rarely
decreased,
version,
which has to be assessed at the time of component placement.
Occasionally the patient’s femoral head may be used as an autograft if
the component is excessively uncovered (>25%) superolaterally.
Cementless acetabulum components with screw fixation are preferred.
When choosing the optimal location of acetabular component placement,
the advantages of a normal anatomic location must be balanced with the
need to provide sufficient acetabular implant coverage. Whenever
possible, the acetabular reconstruction should seek normalization of
the hip center. Extra-small acetabular implant sizes often are
required. Small femoral head sizes to preserve adequate polyethylene
thickness may be needed. Because most of these patients are younger, an
alternate bearing such as highly cross-linked polyethylene, ceramic on
polyethylene, ceramic on ceramic, or metal on metal may be considered.
 |
|
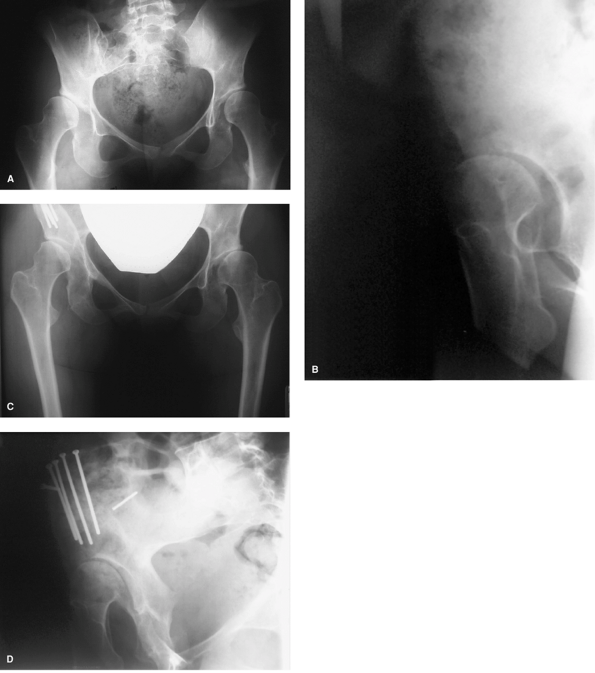
Figure 5-5
Preoperative anteroposterior and false views demonstrating acetabular dysplasia. Postoperative images 6 years following corrective Bernese pelvic osteotomy with preservation of joint space. |
neck anteversion, a valgus neck/shaft angle, metaphyseal-diaphyseal
mismatch (with a very narrow medullary canal) and prominent greater
trochanter in cases of high dislocation. A shortening femoral osteotomy
may have to be performed to minimize injury to the sciatic nerve owing
to leg lengthening. Often a modular cementless femoral component is
ideally suited to address the host bone abnormalities.
patients younger than 30 years of age, especially when other
alternatives such as arthrodesis or resection arthroplasty are
considered. Pain relief in patients with hip dysplasia after total hip
arthroplasty parallels the excellent results of total hip arthroplasty
in the general population. Long-term survivorship remains a challenge
in this often younger patient population; however, with the advent of
alternate bearings with improved wear characteristics this may improve
in the future.
varied and complex clinical scenario to the adult reconstruction
surgeon. A thorough knowledge of the natural history, the physical and
radiographic evaluation, and the various treatment alternatives is
required to manage these challenging cases.
G, Stamos K, Karachalios T, et al. Congenital hip disease in adults.
Classification of acetabular deficiencies and operative treatment with
acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg Am. 1997;78: 683–692.
R, Klaue K, Vinh TS, et al. A new periacetabular osteotomy for the
treatment of hip dysplasias: technique and preliminary results. 1988. Clin Orthop Relat Res. 2004;418:3–8.
J, Burmeister H, Ganz R. Previous Bernese periacetabular osteotomy does
not compromise the results of total hip arthroplasty. Clin Orthop Relat Res. 2004;423:118–122.
