MANAGEMENT OF VOLKMANN’S CONTRACTURE
III – THE HAND > Reconstructive Procedures > CHAPTER 65 –
MANAGEMENT OF VOLKMANN’S CONTRACTURE
tissue fluid pressures that can reduce capillary perfusion below the
level necessary for tissue viability (1,3,7,8 and 9,11,22,26,29,35,36,58,59,68,81,93,97,98 and 99). If the compartment syndrome is sustained or untreated, ischemia results in irreversible muscle and nerve damage (12,19,23,25,28,33,34,35 and 36,40,64,70,74,77,79,86,87,96).
Muscle then undergoes necrosis, fibrosis, and contracture. Concomitant
nerve injury results in further muscle dysfunction, sensibility
deficits, or chronic pain. The result is a dysfunctional limb with
varying amounts of deformity, stiffness, or paralysis, known as
Volkmann’s ischemic contracture (4,5,10,13,25,30,31 and 32,37,39,40 and 41,44,45,46,47 and 48,50,51,56,61,62,63,64,65,66,67 and 68,71,72,74,75,76,77 and 78,80,81,84,85,90,91,92 and 93,97,100,101). See Chapter 13 on Compartment Syndrome.
condition, noting paralysis and subsequent limb contracture that
followed the application of tight, constricting bandages to an injured
limb (93). In 1922, Brooks described a similar condition and believed venous obstruction was a factor in the contracture formation (12). Arterial spasm or injury were subsequently indicated as causes by Leriche and Griffiths (32,49). In an attempt to prevent the contracture described by Volkmann, Bardenheur in 1911 discussed the use of forearm fasciotomy (2).
His “aponeurectomy” consisted of division of the deep antecubital and
forearm fascia. In 1922, Murphy also suggested fasciotomy as a means of
prevention of paralysis and contracture when pressure was increased
within a fascia-enclosed muscle space following hemorrhage or edema (65).
Although the pathogenesis was not clearly understood, in 1926 Jepson
objectively demonstrated the beneficial effects of early fascial
decompression of injured muscle (44).
discussed the various aspects of ischemic contracture formation and
prevention, including the need for immediate fasciotomy, and the role
of median and ulnar nerve decompression and brachial artery
exploration. The operative
technique and appreciation of surgical anatomy evolved from reports by Benjamin (3), Eichler and Lipscomb (22), Henry (38), Eaton and Green (21), Whitesides et al. (98), Newmeyer and Kilgore (66), and Gelberman (24,25,26,27 and 28).
The relationships between increased tissue fluid pressure and myoneural
dysfunction, as well as the use of fasciotomy to prevent ischemic
contracture, are now well established (1,2,3,4 and 5,7,8,9,10,11,12 and 13,19,20,21,22,23,24,25,26,27,28 and 29,33,34,35 and 36,40,41,46,50,51 and 52,58,59,63,64,78,84,86,94,98,99).
management of acute compartment syndrome, delays in treatment still
occur; these result in patients developing the full sequelae of
Volkmann’s ischemic contracture. The deficits can be devastating, and
management is challenging. Treatment can require a prolonged
rehabilitation program and/or operative management. A comprehensive
rehabilitation program includes active and passive exercises,
strengthening, splinting, desensitization, and pain management.
Operative management includes nerve decompression, infarct excision,
contracture release, myotendon lengthening, tendon transfers, or free
tissue transfers (4,5,10,13,14,15,16,17 and 18,21,22 and 23,25,30,31 and 32,37,39,40,41,42,43,44,45,46,47 and 48,50,51,53,54,55,56 and 57,60,61,62,63,64,65,66,67,68 and 69,73,74,75,76,77 and 78,80,81,82,83,84 and 85,88,89,90,91,92 and 93,95,97,100,101).
The following discussion reviews the general features of Volkmann’s
ischemic contracture, the classification of deformities, and the
methods of management.
tension. Muscle undergoes necrosis after 4 hours of ischemia produced
experimentally by application of a tourniquet (33,34).
With prolonged ischemia, muscle necrosis leads to fibroblastic
proliferation within the muscle infarct. A variable amount of
longitudinal and horizontal contraction may progress over a 6- to
12-month period following the ischemic insult. The necrotic muscle
adheres to surrounding structures, fixes muscle position, and reduces
excursion and mobility. Limitation of muscle excursion may lead to loss
of joint motion with subsequent joint contracture.
from the original ischemic insult, as well as from subsequent
compression resulting from muscle fibrosis, or from the chronic stretch
of limb deformity. The developing fibrosis may surround, tether, or
impinge on adjacent peripheral nerves, leading to local compression.
Hyperflexion at the elbow or wrist can lead to secondary neuropathy of
the ulnar nerve or the median nerve, respectively. In addition to the
associated motor loss, neuropathy following ischemic contracture can
lead to paresthesias, loss of limb sensibility, and chronic pain.
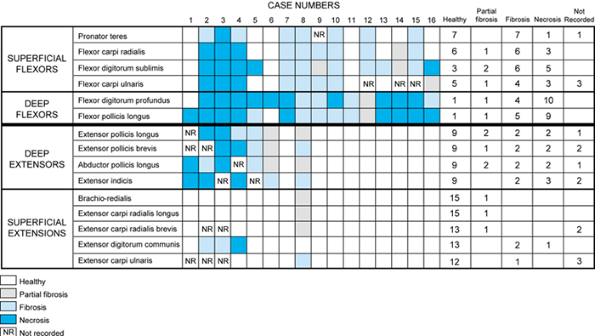
bone on the volar forearm, usually have the highest interstitial
pressure during an acute compartment syndrome (7,8,9 and 10,91,92).
Subsequent injury that leads to ischemic necrosis is most marked in
these deep compartments, more commonly involving the flexor digitorum
profundus and flexor pollicis longus (Fig. 65.1 and Fig. 65.2).
In the mildest contractures, only part of the flexor digitorum
profundus undergoes necrosis, usually to the ring and long fingers. In
severe contractures, all four digits are involved. The flexor digitorum
superficialis and pronator teres are generally less severely affected.
In the most severe cases, the wrist flexors, the wrist and digital
extensors, and the compartments proximal to the elbow may also undergo
varying degrees of fibrosis and contracture.
 |
|
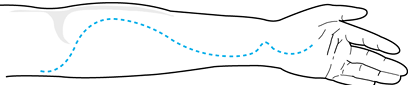
Figure 65.1.
The muscles affected in 16 cases of Volkmann’s contracture of the forearm. (Adapted from Seddon HJ. Volkmann’s Contracture: Treatment by Incision of the Infarct. J Bone Joint Surg Br 1956;38:152, with permission.) |
 |
|
Figure 65.2. Cross section of Volkmann’s contracture of the forearm. A: The shading represents the degree of involvement of the various muscles. The diagram is based on the data provided in Figure 65.1. B: Key to muscles. The plane of section is through the upper third of the forearm. E, EX, extensor; DIG, digiti; FL, flexor; POL, POLL, pollicis; L, longus; BREV, brevis; BR, brachio; ABD, abductor; C, carpi; R, radialis. (Adapted from Seddon HJ. Volkmann’s Contracture: Treatment by Incision of the Infarct. J Bone Joint Surg Br 1956;38:152, with permission.)
|
forearm is attributed to their deep location, a factor that increases
their vulnerability to ischemia (79). These deep compartments, particularly the regions adjacent to bone, usually have the highest interstitial pressures (34).
With compression from within the compartment, the circulation to the
deep portions of the muscle belly are compromised, whereas collateral
circulation to the more superficial parts of the muscle is retained. In
the forearm, the most severe muscle damage usually occurs in the middle
third of the muscle belly, with more injury closer to bone, and less
injury toward the proximal and distal surfaces. When a compartment
syndrome remains untreated, swelling may eventually resolve, but the
injured, necrotic muscle becomes fibrotic. An ellipsoid section or cord
of cicatrix can develop within the muscle or group of muscles. The
characteristic deformity of ischemic contracture may take weeks or
months to completely develop. When the forearm, hand, and arm are
significantly involved, the deformity in the upper extremity often
consists of varying amounts of elbow flexion, forearm pronation, wrist
flexion, thumb flexion and adduction, digital metacarpophalangeal (MP)
joint extension, and interphalangeal joint flexion (Fig. 65.3).
The MP joint extension and proximal interphalangeal joint flexion give
rise to a “claw hand” deformity. The extremity may initially be
flexible, especially in milder cases. Chronic muscle imbalance and lack
of joint motion may ultimately lead to fixed deformity from secondary
joint capsule, ligament, and skin contracture.
 |
|
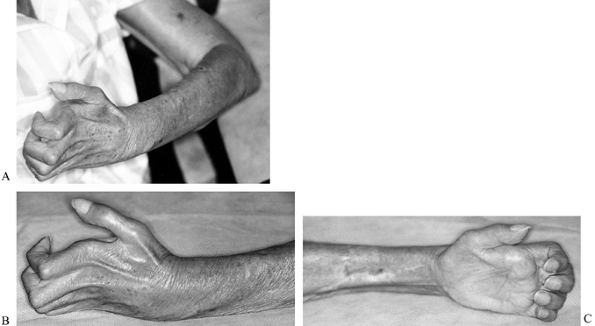
Figure 65.3. A,B,C:
Upper extremity of a patient with severe ischemic contracture. Unrecognized compartment syndrome developed after revascularization of the extremity for a brachial artery injury. The deformity includes hyperextension at the metacarpophalangeal joints and flexion at the interphalangeal joints. The forearm muscle mass is fibrotic, with a firm, “woody” consistency. Fixed myotendinous contractures exist that involve the extrinsic flexor and extensor muscles. The elbow flexors are also involved, with a fixed flexion deformity at the elbow and associated fibrosis of the brachium. Patients with established ischemic contracture often also show wrist flexion, forearm pronation, and adduction or flexion of the thumb. |
are complex. Although there may be an apparent similarity between the
ischemic contracture and the intrinsic muscle contracture in some
patients, the actual deformities are considerably different. Intrinsic
muscle contracture results in an intrinsic-plus deformity, with flexion
at the MP joints and extension at the proximal interphalangeal joints.
Volkmann’s contracture often leads to an intrinsic-minus deformity,
with hyperextension at the MP joints and flexion at the interphalangeal
joints. Although the two entities are associated and may occur
simultaneously, the resultant claw-hand deformity is determined by
contracture
of the more powerful extrinsic finger flexors. A paradoxical situation
of a claw-hand deformity with intrinsic tightness can exist (82).
The intrinsic contracture may not become apparent until the extrinsic
flexors have been released by a muscle slide, tendon lengthening, or
tenotomy. Only then does intrinsic tightness become evident.
extremity deformity is the amount of peripheral nerve injury
superimposed on the muscle. Ischemic injury to the muscle usually
results in muscle contracture (from fibrosis of the necrotic muscle).
Nerve injury, conversely, results in muscle paralysis. Concomitant
median and ulnar neuropathy in the forearm or wrist therefore
contribute to intrinsic muscle weakness and, in turn, to an
intrinsic-minus deformity. The final clinical outcome is dependent on
the relative amount of extrinsic and intrinsic muscle contracture (from
muscle ischemia) and on the amount of extrinsic and intrinsic muscle
paralysis (from nerve injury) (9,10).
of the deep extrinsic finger flexors, usually involving only two or
three fingers. Hand sensibility and strength are normal. The intrinsic
muscles are not involved, and fixed joint contractures are not present.
Most mild types of ischemic contracture are caused by fractures or
crush injuries to the forearm or elbow, and they usually occur in young
adults (40,91).
involves the flexor digitorum profundus and flexor pollicis longus
muscles. Less frequently, the flexor digitorum superficialis, flexor
carpi radialis, and flexor carpi ulnaris are involved. The wrist and
thumb become flexed and the hand assumes a claw-hand deformity from
contracture of the long finger flexors.
specific locations where nerves pass beneath ligaments or fibrous
arcades or through contracted muscles. The median
nerve
is most frequently compressed, usually at the lacertus fibrosus,
pronator teres, or flexor digitorum superficialis, or within the carpal
tunnel. The ulnar nerve may be compressed within the cubital tunnel or
between the two heads of the flexor carpi ulnaris. The radial nerve is
rarely involved, but it may be compressed at the arcade of Frohse or
within the supinator muscle.
fracture of the humerus. These fractures occur most commonly at 5 to 10
years of age (40,62,63,91).
Complications, including loss of nerve function, malunion or nonunion
of forearm fractures, and cutaneous scarring and contracture, are often
encountered. The most common causes of severe contracture are prolonged
ischemia secondary to brachial artery injury, and prolonged external
compression secondary to drug overdose.
severity of the deformity and the time interval between injury and
initiation of treatment. Contractures of the deep forearm flexors, with
normal hand sensibility and strength, may be treated conservatively.
Occupational therapy, including passive and dynamic extension
splinting, is designed to maintain wrist and interphalangeal joint
extension, to maintain or improve thumb web-space width, and to
strengthen weak thumb intrinsic muscles. Alternate the use of bivalved
pancake plaster casts or custom-molded synthetic orthoses with
low-profile digital extension, and thumb opposition splints. A C-bar
may be incorporated into the splint to maintain thumb position. In the
early stages, have the patient alternate passive and dynamic splints at
2-hour intervals during the day and, at night, wear extension splints.
Splinting techniques for Volkmann’s contracture have been described in
detail by Goldner (30). A satisfactory outcome
can be expected when mild contractures are treated soon after their
development using these techniques.
If the contracture is limited to one or two digits and a cordlike area
is palpable, simple excision of the infarcted muscle or lengthening of
the involved flexor tendons is recommended.
-
Perform excision of the infarcted muscle through a curved, longitudinal incision on the palmar forearm.
-
Identify and protect the radial artery, median nerve, and ulnar artery and nerve.
-
Retract the flexor digitorum
superficialis and flexor carpi radialis radially, and the flexor carpi
ulnaris ulnarly, to expose the flexor digitorum profundus. -
Isolate and excise the palpable, cordlike
areas of indurated muscle. The flexor digitorum profundus of the ring
and long fingers is most commonly affected. -
If the contracture is localized to the
pronator teres, this muscle may be excised. If the contracture and
induration involve three or four digits, flexor tendon lengthening may
be required. -
Perform Z-lengthening of the involved tendons in the distal two thirds of the forearm.
-
Begin the Z-lengthening incisions
proximally, near the musculotendinous junctions, to ensure adequate
tendon length for satisfactory correction. Repair the tendons using 4-0
nonabsorbable suture. -
Following the surgery, immobilize the
forearm in supination, the wrist in extension, and the digits in the
corrected amount of extension.
-
Release of secondary nerve compression
-
Treatment of contractures
-
Tendon transfers for substitution and reinforcement
-
Salvage procedures for the severely contracted or neglected forearm
within a constricting cicatrix, or at specific anatomic locations where
space is minimal. Secondary compressive neuropathies require attention
in the earliest stages of treatment. Improvement of nerve function is
related to the severity and duration of compression, as nerves may
sustain compression for longer periods than muscle and still show some
reversibility, particularly in sensory function (11,79). When continuity is maintained, nerves may show signs of gradual recovery over a 12-month period (80,85).
If both fibrosis and contracture are severe, all three major forearm
nerves may become constricted. Careful clinical assessment is essential
before the first phase of treatment.
restoring a useful functional extremity. This nerve lies in the center
of the constricting cicatrix and may become compressed in four anatomic
regions: the lacertus fibrosus, the pronator teres, the proximal
arch
of the flexor digitorum superficialis, and the carpal tunnel. Sensory
and motor loss consistent with median neuropathy warrant aggressive
management for decompression.
-
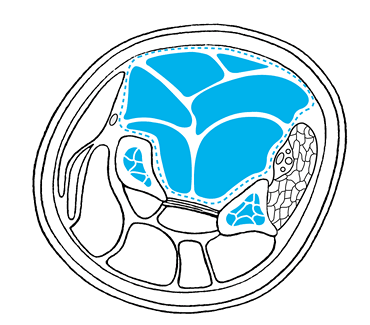
Use an incision similar to that used for decompression of an acute forearm compartment syndrome (24) (Fig. 65.4).
Begin the incision on the palmar aspect of the medial arm, about 2 cm
proximal to the medial epicondyle. Extend it obliquely across the
antecubital fossa to the mobile wad. Continue the incision
longitudinally, curving slightly ulnarly to reach the palmar distal
forearm. Extend the incision into the palm for carpal tunnel release.
Locate the distal portion of the incision ulnar to the palmaris longus
to avoid injury to the palmar cutaneous branch of the median nerve.![]() Figure 65.4.
Figure 65.4.
The incision used for decompression of the median nerve in the forearm
and hand. (Adapted from Gelberman RH, et al. Decompression of Forearm
Compartment Syndromes. Clin Orthop 1978;134:225, with permission.) -
Identify the median nerve in the proximal
portion of the incision and trace it distally to the lacertus fibrosus.
The lacertus fibrosus is a fascial extension of the biceps tendon and
lies anterior to the median nerve at the elbow. Nerve compression
occurs frequently in this area in the acute stages of a forearm
compartment syndrome, and it may also occur in the later stages of
contracture. -
If signs of proximal median nerve
compression are present, release the lacertus fibrosus. Incise the
fascia of the lacertus fibrosus in a longitudinal fashion along the
course of the median nerve to allow complete decompression and exposure
of the nerve. -
Continuing distally, the median nerve
will pass between the two heads of the pronator teres muscle. Nerve
compression can occur between these two heads. The ulnar head lies deep
to the nerve, and the humeral head is superficial to the nerve. A
tendinous band, which often lies along the deep head, may contribute to
compression. -
Completely release the nerve throughout
the entire length of its passage through the pronator teres. This often
requires division of the humeral head of the pronator teres and
division of any tendinous bands, deep or superficial, that may impinge
on the nerve. -
Distal to the pronator teres, the median
nerve continues beneath and within the fascia of the flexor digitorum
superficialis muscle, passing deep to the arch formed by the ulnar and
radial origins. The nerve is most frequently compressed beneath the
fibrous origin of this muscle (72). -
Decompress the nerve by either incising
the investing fascia or by dissecting the flexor digitorum
superficialis from the underlying flexor digitorum profundus.
Completely release the nerve from the investing fascia (72). -
Despite the proximal location of muscle
necrosis in Volkmann’s contracture, the incidence of median nerve
compression in the carpal tunnel is high. Extend the incision for
forearm decompression and expose the palmar fascia and transverse
carpal ligament (24,87). -
Incise these structures to decompress the median nerve decompression from the distal arm to the midpalm.
than that of median nerve compression. It is often compressed at the
elbow as it passes between the ulnar and humeral heads of the flexor
carpi ulnaris. Decompress it if there are signs of ulnar neuropathy.
neuropathies following Volkmann’s contracture. Occasionally, however,
it may require decompression as it passes under the tendinous origin of
the supinator muscle (arcade of Frohse) or within the muscle itself.
Nerve compression is manifested by motor loss of the digital and thumb
extensors and the ulnar wrist extensors. Radial wrist extensor strength
and radial nerve sensibility remain intact, as these neural branches
arise proximal to the area of compression (10).
-
To decompress the radial nerve, make a
straight, longitudinal incision on the proximal half of the posterior
forearm along an imaginary line extending between the lateral
epicondyle and the radial styloid. -
Develop the interval between the extensor
carpi radialis brevis and the extensor digitorum communis. This
interval is most easily defined in the distal portion of the incision
and should be developed here first and traced proximally. -
Retract the extensor carpi radialis brevis radially and the extensor digitorum communis ulnarly.
-
Identify the supinator.
-
Identify the radial nerve proximally
where it enters the supinator. The nerve may be found to be compressed
by the tendinous bands of the arcade of Frohse, by a vascular leash
that crosses the nerve transversely in this region, or by the supinator
muscle itself. Carefully divide the appropriate structures to
decompress the nerve (10).
as the patient’s condition permits. A nerve stimulator may be helpful
for verification of conductivity, especially
in
heavily scarred areas. Early return of sensibility and a decrease in
pain may be expected when decompression is undertaken in a timely
manner. Motor function return, although variable, can progress over
several days or weeks, depending on whether neuropraxia or axontemesis
is present. If nerves are irreparably damaged or have lost continuity
(neurotemesis), secondary excision of damaged segments and
microsurgical repair or reconstruction may offer some return of nerve
function. Alternatively, reconstruction may be accomplished with
appropriate tendon transfers.
clawing, and thumb adduction are fixed deformities that develop over
time. Procedures used to help correct established forearm contractures
include infarct incision, flexor tendon lengthening or excision, and
flexor pronator slide. These procedures should be performed at the time
of, or subsequent to, nerve decompression.
 |
|
Figure 65.5.
Excision of an infarct in the forearm, with preservation of the flexor carpi ulnaris and ulnar neurovascular bundle. (Adapted from Seddon HJ. Rev Chir Orthop Reparatrice Appar Mot 1960;46:149, with permission.) |
-
Excise the frequently encountered ellipsoid infarct through a long palmar forearm incision (80).
-
Excise fibrotic muscle and contracted
scar tissue. The deep digital flexors and thumb flexor are usually most
extensively involved. The pronator teres and pronator quadratus may be
released or, if they are fibrotic, excised. -
Gently manipulate the forearm and wrist
into supination and extension, respectively, and immobilize in this
corrected position following surgery.
necessary and advocates Z-lengthening of the forearm flexors proximal
to the wrist (30). The flexor digitorum
profundus, flexor digitorum superficialis, flexor pollicis longus, and
pronator teres may be lengthened to accomplish digital and thumb
extension, and forearm supination (6,30). If severe forearm fibrosis is encountered and digital contracture is severe, excise the flexor digitorum superficialis.
the forearm is further weakening of an already weakened muscle.
However, contracture release is usually functionally advantageous to
the maintenance of maximal strength. Tendon transfers, if needed, may
be performed at a later date.
-
Make a skin incision on the medial side
of the elbow, 6 cm proximal to the medial humeral condyle and extending
to the junction of the middle and distal thirds of the forearm.
Separate the subcutaneous tissue from the deep fascia on the ulnar and
radial sides of the incision. -
Isolate the ulnar nerve at the level of the elbow and transpose it anteriorly.
-
Proceed with systematic, complete
operative detachment of the origins of the flexor muscles of the
forearm. Dissect the muscles subperiosteally using a scalpel. -
Release the origins of the pronator
teres, flexor carpi radialis, palmaris longus, and the humeral head of
the flexor carpi ulnaris, and then detach the flexor digitorum
superficialis. -
Detach the ulnar head of the flexor carpi
ulnaris and the broad origin of the flexor digitorum profundus from the
anterior aspect of the ulna. -
Carry the dissection across the
interosseous membrane and release the origin of the flexor pollicis
longus from the anterior aspect of the radius. -
Take care to avoid injury to the
interosseous artery, vein, and nerves when detaching the flexors from
the interosseous membrane. -
Allow the muscles to slide distally 2–3 cm.
-
Postoperatively, immobilize the extremity
for 2–3 weeks with the elbow at 90° flexion, the forearm supinated, and
the wrist and digits extended.
unpredictability of correction achieved, the risk of recurrence of
deformity with growth, and the resultant decrease in grip strength,
particularly at the distal interphalangeal joint (52,91,92).
Despite these criticisms, the procedure has gained popularity and has
been shown to be effective in achieving satisfactory to excellent
results in a large group of patients with moderate to severe
contractures (91,92).
patients with Volkmann’s contracture are finger and thumb flexion and
thumb opposition. Tendon transfers are usually delayed until nerve
recovery has plateaued and the contractures have been corrected
maximally with mobilization and splinting, or with operative releases.
In 1947, Phalen and Miller described a series of tendon transfers
designed to provide digital flexion and thumb opposition (73).
-
Transfer the extensor carpi radialis
longus to the flexor digitorum profundus, and transfer the extensor
carpi ulnaris, lengthened by tendon graft, to the thumb for opposition (71,73). -
Excise the tendons of the flexor
digitorum superficialis if they are nonfunctional. The extensor
pollicis brevis may be used to reinforce the extensor carpi
ulnaris–opponens transfer. -
Alternative transfers to augment thumb opposition include the abductor digiti quinti opponensplasty described by Huber (42,52) and the extensor indicis proprius opponensplasty described by Zancolli (100) and Burkhalter et al. (14).
-
To reinforce thumb flexion, the brachioradialis may be transferred to the flexor pollicis longus (91,92).
-
When flexor tendons have been weakened
severely by previous Z-lengthening, reinforcement by transfer of the
extensor carpi radialis longus to the flexor digitorum profundus, and
transfer of the extensor carpi ulnaris to the flexor pollicis longus,
can be performed (30).
satisfactory results, and further procedures are seldom necessary.
Occasionally, however, additional measures may be required for
satisfactory correction of the severely contracted or neglected
forearm. Operations that have proved useful include proximal or distal
row carpectomy, radial and ulnar shortening, wrist fusion, and digital
joint fusion.
shortening that allows wrist extension while maintaining flexibility.
In severe deformities, carpectomy may be performed before tendon
transfer. If adequate donor muscles are not available for transfer,
interphalangeal joint fusion can be performed. The stabilized limb can
then function as a hook, which is generally superior to a prosthesis,
especially if some sensibility is retained (30). Radial and ulnar shortening and wrist fusion are rarely indicated for the treatment or salvage of Volkmann’s contracture.
contracture is complex, requiring a systematic approach. Intrinsic
contractures should be addressed only after extrinsic finger flexors
have been released. Fixed extrinsic contractures create a claw-hand
deformity (hyperextension of the MP joints and flexion of the
interphalangeal joints). Following extrinsic muscle release, intrinsic
tightness may become apparent. Complete release of intrinsic
contractures may not be desirable, since preservation of some MP joint
flexion will prevent recurrence of the claw-hand deformity. If the
intrinsic contracture is severe, the oblique fibers of the extensor
hood may be released to permit flexion of the interphalangeal joints (82).
in Volkmann’s contracture. The deformity may be caused by both
intrinsic and extrinsic contractures. Flexion contracture at the
interphalangeal joint may be corrected with flexor pollicis longus
lengthening. Residual deformity following tendon lengthening is
attributable to intrinsic muscle contracture, joint contracture, or
skin contracture of the first web. Recommended procedures for
correction of a severe thumb-in-palm deformity include release of the
adductor pollicis, deepening of the thumb web space, fusion of the MP
joint or interphalangeal joint, or excision of the trapezium (6,30).
Thenar origin release (recession) and release of the first dorsal
interosseous muscle may also be necessary for additional correction (6,57).
by intrinsic contractures but rather by secondary problems from sequela
of extrinsic muscle contractures in the forearm or by associated
neuropathy. Loss of median and ulnar nerve sensibility, intrinsic
paralysis secondary to median and ulnar motor nerve paralysis, and
interphalangeal joint flexion deformity secondary to contracture of the
extrinsic flexors cause severe functional deficits. Proper management
of these problems, as described in
Phase 1 and Phase 2, should significantly improve hand function.
contracture remains a challenging problem despite the available methods
of management. Advances in the free transfer of vascularized muscle,
nerve, and skin have offered potential additional methods of
reconstruction (15,16,17 and 18,43,88).
One of the early uses of these techniques for reconstruction of
Volkmann’s contracture was the transfer of the lateral head of the
pectoralis major to the flexor forearm, reported by Chien et al. in
1977 (15). Subsequently, Taylor and Daniel
achieved satisfactory results with a free vascularized superficial
radial nerve graft transfer to an irreparably damaged median nerve (89).
Chuang et al. have obtained an 80% success rate in free muscle transfer
in nine patients undergoing 10 transfers for Volkmann’s contracture (16,17 and 18).
As free tissue transfer has become more popular, reconstruction of
forearm muscles has now included the use of the gracilis, rectus
femorus, latissimus dorsi, or pectoralis muscles (15,16,17,18,43,53,54 and 55,60).
The early results of these procedures are promising, especially in
their role in the reconstruction of severe or neglected Volkmann’s
contracture in which few adequate donor muscles are available for
tendon transfer.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
B. Pathological Changes in Muscle as a Result of Disturbances of
Circulation: An Experimental Study of Volkmann’s Ischemic Paralysis. Arch Surg 1922;5:188.
DCC, Chen HC, Wei FC, et al. Compound Functioning Free Muscle Flap
Transplantation (Lateral Half of Soleus, Fibula and Skin Flap). Plast Reconstr Surg 1992;89:335.
DCC, Strauch RJ, Wei FC. Technical Consideration in Two-stage Function
Free Muscle Transplantation (FFMT) Reconstruction of Both Flexor and
Extensor Function of the Forearm. Microsurgery 1994;15:338.
AR, Evans KL, Hagen PL, et al. Quantitation of Skeletal-Muscle Necrosis
in a Model Compartment Syndrome. Presented at a meeting of the
Orthopedic Research Society, Dallas, TX, February 1978.
AR, Akeson WH, Mubarak SJ, et al. Kappa Delta Award Paper. Tissue Fluid
Pressures: From Basic Research Tools to Clinical Applications. J Orthop Res 1989;7:902.
FA III, Wyss CR, Drugmire RB Jr, et al. The Effects of Limb Elevation
and Dependency on Local Arteriovenous Gradients in Normal Human Limbs
with Particular Reference to Limbs with Increased Tissue Pressure. Clin Orthop 1980;150:187.
GS, Miller RC. The Transfer of Wrist and Extensor Muscles to Restore or
Reinforce Flexion Power of the Fingers and Opposition of the Thumb. J Bone Joint Surg 1947;29:993.
RM, Gelberman RH, Williamson RV, et al. Effects of Increased Systemic
Blood Pressure on Tissue Fluid Pressure Threshold of Peripheral Nerve. J Orthop Res 1983;1:172.
Schroeder HP, Botte MJ. Definitions and Terminology of Compartment
Syndrome and Volkmann’s Ischemic Contracture of the Upper Extremity. Hand Clin 1998;14:331.
E. Tendon Transfers after Ischemic Contracture of the Forearm:
Classification in Relation to Intrinsic Muscle Disorders. Am J Surg 1965;109:356.