SURGERY OF THE THORACIC OUTLET
result from compression of the neurovascular structures as they exit
the chest and neck and pass through the costoclavicular interval and
down into the axilla. The clinical presentation in each patient
reflects the degree of compression of the brachial plexus and of the
subclavian artery and vein. Historically, the interscalene area was
considered the primary site of compression, but subsequent experience
has shown that treatment of this disorder requires understanding the
dynamic anatomy of the entire region of the neck and shoulder region.
normal development, age, and disease complicate the problem
considerably but also provide a way to understand how signs and
symptoms are produced (39). Specifically,
exaggeration of the normal caudad descent of the shoulder girdle
produced by poor posture or local injury can cause compression of the
lower trunk of the brachial plexus and of the subclavian artery and
vein (Fig. 61.1). This mechanism can explain the emergence of symptoms of TOS in patients who are asymptomatic before motor vehicle accidents (6,20,26).
Congenital anatomic abnormalities such as cervical ribs, long
transverse processes, or congenital bands can increase the severity of
the effect.
 |
|
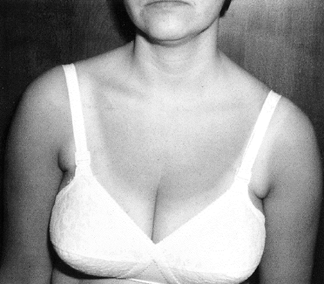
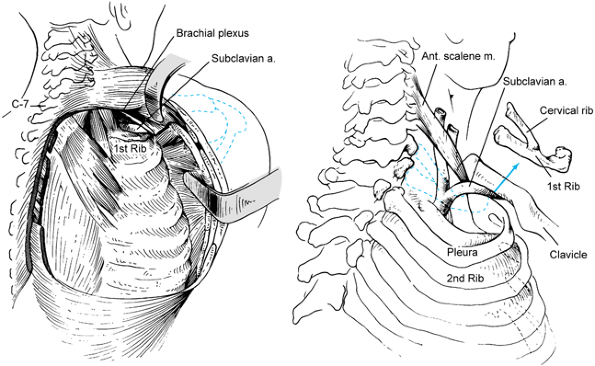
Figure 61.1.
This patient was asymptomatic before a motor vehicle accident in which she sustained what was termed a whiplash injury. This caused pain in the shoulder girdle, which led to a postural droop of her scapula and subsequent thoracic outlet compression. She was overweight with large breasts, which added to the downward pull on her shoulder girdle. Ultimately, after failure of conservative treatment, she underwent first rib resection with relief of her symptoms but required extensive postoperative muscle reeducation to correct her posture. |
population has been reported in different studies to range from 0.056%
to l.5% (35), nine types of congenital fibrous
bands have been described that can cause neurovascular compression
within the thoracic outlet (30). Malunions and nonunions of the clavicle can also lead to thoracic outlet compression (14). Instability of the glenohumeral joint (33) can be associated with numbness and tingling within the limb or with secondary TOS (17).
with TOS outnumber males by about four to one. The disorder is seen
most commonly between puberty and the
fourth
decade of life. Although there are scattered case reports of girls who
have developed TOS in childhood, the authors do not report whether the
patients had attained menarche. A postmenopausal woman who develops
symptoms thought to be due to thoracic outlet compression should be
carefully examined to be certain that the symptoms are not due to
another condition.
chapter, I believe that the diagnosis of TOS is primarily clinical.
Although some laboratory examinations are helpful, diagnosis is usually
made on the basis of a careful history and physical examination.
which structures are being compressed. The majority of patients
complain of pain and paresthesias that radiate from the neck, upper
chest, or shoulder region, down the medial aspect of the arm and into
the little and ring fingers, although some experience numbness of the
entire upper limb. Much less commonly, it is the radial aspect of the
arm and hand that is numb. Symptoms are often nocturnal; elevation of
the arm in sleep or during activities aggravates them. Complaints such
as the inability to hold a hair dryer or to work with the arms above
the head are common. Some patients have numbness when driving or when
carrying heavy objects. These symptoms are caused by compression of the
lower trunk of the brachial plexus.
weakness of the ulnar-innervated intrinsic muscles unless compression
is severe. There may be weakness of all the intrinsic musculature and
loss of power of the long flexors of the little and ring fingers. When
the upper trunk of the brachial plexus is involved, differential
diagnosis becomes more difficult, and there may be confusion with
cervical radiculopathy or carpal tunnel syndrome.
insufficiency or gangrene in the hand, but such severe symptoms are
rarely seen in an orthopaedic practice. Such patients usually have
acute occlusion of the subclavian or axillary arteries and often have
aneurysms caused by compression by significant cervical ribs (13,27). This complication is more often found in older patients with long histories of often undiagnosed symptoms.
upper limb, which, if intermittent, is difficult to document until its
severity motivates the patient to have it examined. Intermittent venous
compression in the absence of thrombosis produces cyanosis as well as
swelling in the limb.
This “effort thrombosis” of the subclavian and axillary veins results
from underlying subclinical thoracic outlet compression and repetitive
or strenuous use of the arms, particularly in the overhead position.
The symptoms are acute pain and swelling of the limb and ipsilateral
chest wall. Prompt recognition of the condition is imperative—delay may
result in considerable disability due to chronic pain and swelling.
Acute therapy consists of administration of intravenous thrombolytics
by catheter, with mechanical dilatation, if needed. Maintain the
patient on anticoagulants for 3 or 4 months, and follow up with
elective first rib resection to diminish the likelihood of recurrent
thrombosis (35).
diagnosed as being consistent with TOS. In this case, it is attributed
to selective compression of the sympathetic innervation of the limb
within the lower trunk of the brachial plexus. The etiology of
unilateral Raynaud’s phenomenon is not collagen disease. More likely,
this phenomenon represents episodes of distal embolization from an
aneurysm located within the subclavian artery (13).
pain. When TOS is in the left hemithorax, such pain may mimic angina or
myocardial infarction and bring the patient repeatedly to the emergency
room or cardiac care unit (42).
achieve a positive diagnosis but also to rule out other conditions that
may be confused with TOS or that may coexist with it. Cervical
radiculopathy is unusual in the C8—T1 distribution in the arm and hand (5).
Nevertheless, when the symptoms are difficult to interpret, the
cervical spine must be ruled out as a site of disease. There may be
tenderness over the brachial plexus in the supraclavicular fossa, but
this nonspecific finding may accompany either thoracic outlet
compression or cervical radiculopathy.
thoracic outlet compression, the overhead exercise test and Wright’s
maneuver (49) are the most consistently
positive. The first test is performed by having the patient, in the
“hands-up” position, rapidly flex and extend the fingers. In
susceptible patients, this exercise produces cramping on the affected
side within 30 seconds. In addition, placing the arm in the abducted
and laterally rotated position not only obliterates the pulse at the
wrist but also reproduces the symptoms. Lowering the arm to the side
restores the pulse and alleviates the symptoms.
provocative positions is not diagnostic of TOS, because in many young
women, some position of the arm can obliterate a pulse. The
reproduction of the symptoms is crucial! Sometimes they can be elicited
by rotating the neck to the opposite side or by having the patient take
a deep breath, particularly while the affected extremity is abducted
and externally rotated at the shoulder.
reproduces symptoms in patients whose costoclavicular interval has been
narrowed, particularly by a clavicular fracture. The classic Adson’s
maneuver is performed by having the patient, with the arm dependent,
rotate and hyperextend the neck to the affected side and take a deep
breath. In my experience, this has been the least rewarding of the
provocative tests.
to verify the stability of the glenohumeral joint, because patients
with instability may complain that the arm “feels dead” (33).
In addition, finding an increased venous pattern on the side of the
lesion is presumptive evidence of venous hypertension and possible
compression or thrombosis.
of the hand. The only motor deficit may be just-perceptible atrophy of
the hypothenar muscles and weakness of adduction of the little finger
to the ring finger. Rarely, all of the intrinsics are weak or atrophic.
The cutaneous distribution of the first thoracic nerve is the medial
aspect of the forearm, thus it is differentiated from the distribution
of the ulnar nerve.
to assess the lower cervical spine for the presence of adventitious
ribs or long transverse processes at C7 because the patient’s
identification plate may have been placed there. Hypoplastic, true
first ribs may be present, and sometimes, a cervical rib can be
confused with a hypoplastic rib unless you are sure of the vertebral
level. Count from the atlas caudalward to establish that there is, in
fact, a cervical rib. Look carefully at the disc spaces and the
intervertebral foramina, and note abnormalities. In the lateral view of
patients with droopy shoulders, the physician may be able to clearly
define the second dorsal vertebra. Such patients may resemble those
with TOS but may have no peripheral neural deficits in the limbs (37).
lung tumors, which can mimic TOS in their presentation. Adequate
radiographs of the shoulder are also necessary. When there is
significant concern about possible cervical radiculopathy, magnetic
resonance imaging (MRI) or myelography may be indicated. They are not
needed in most cases.
reliable diagnostic test for TOS. In my experience, however, because
pulses can be positionally obliterated in many normal people, the
incidence of false-positive results is substantial. Interpret such
studies with caution. For patients with intrinsic vascular disease,
noninvasive studies can be extremely useful.
the general diagnosis of TOS, and I do not routinely use them. Because
the occlusion of arterial outflow with the position of the arm may be
observed in asymptomatic patients, an arteriogram would provide little
information unless there is serious consideration of the presence of an
aneurysm in the subclavian artery or intrinsic vascular disease.
Patients with complete cervical ribs may have an increased incidence of
such aneurysms (13,27).
Therefore, in such patients, it is prudent to obtain arteriographic
studies if the surgeon intends to explore the thoracic outlet through
the axilla. Venography is useful in demonstrating thrombosis of the
axillary or subclavian vein and in following the process of
recanalization, should it occur. Noninvasive testing may be of value in
this situation as well.
the velocity of conduction of the ulnar nerve through the thoracic
outlet to diagnose TOS, the experience of many workers has failed to
substantiate this claim (40,42,44).
Reports from electrodiagnostic laboratories may say, “There is no
evidence of TOS”; interpret such statements based on nerve conduction
velocity (NCV) with caution, however, because the test is not of value
in this situation.
Conditions such as ulnar neuropathy at the elbow and carpal tunnel
syndrome are readily identified by means of
NCV
determinations. Because NCV determination is not a reliable means of
assessing the plexus within the thoracic outlet, the use of
somatosensory evoked potentials and F responses has received attention
as a means of obtaining further objective evidence of neural
dysfunction to diagnose TOS (10,23).
Some workers have found the measurement of the amplitude of the evoked
response of the medial cutaneous nerve of the forearm and C8 root
stimulation to be of value in making the diagnosis (24).
In my opinion, the diagnostic value of such measurements has not yet
been firmly established, and the diagnosis remains clinical (4,44).
usually not markedly abnormal unless there has been sufficient
compression to cause denervation. In such cases, it is often possible
clinically to detect atrophy and weakness of the ulnar-innervated
interosseous and hypothenar muscles. In other patients, however, these
muscles may show fibrillation potentials at rest that appear to be
clinically normal (36).
have written that the coexistence of TOS and carpal tunnel syndrome is
rare if it exists at all, patients are seen nonetheless with
well-demonstrated signs of both entities (47). Ulnar neuropathy may coexist with TOS (16).
Patients may have hard-to-define combinations of signs and symptoms
that appear to be the result of more than TOS. I these cases, look for
additional lesions to explain the entire picture; otherwise treatment
will fail.
enormously, and in many cases, the symptoms have been present for
months or years. Not uncommonly, such patients have been told that
their symptoms are of emotional origin, or they have been subjected to
unsuccessful conservative or operative treatment. Such patients require
objective, sympathetic evaluation and sometimes psychological
consultation. Some patients with TOS are clinically depressed. The very
deleterious effect depression has on their posture aggravates the
anatomic problem. If such is the case, the surgeon may, according to
training and inclination, treat the patient with antidepressants or
refer him or her for psychotherapy. It is not rare to see patients
whose symptoms of TOS can be lessened by such measures, even though
some may ultimately require surgery.
often poor. It is worthwhile to inquire about their level of physical
activity; often, it is quite limited. Sometimes, patients are afraid to
exercise for fear of worsening the condition, or they have been so
advised by their physicians. If the patients have no other serious
medical problems, make an effort to mobilize them with aerobic
exercises. Probably the easiest generalized exercise for such patients
is walking, because it does not usually cause much discomfort. Some
patients may experience increased symptoms with walking, and in these
cases, the use of a shoulder support such as the Biomet Hook
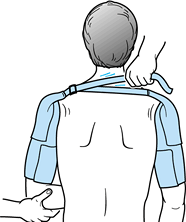
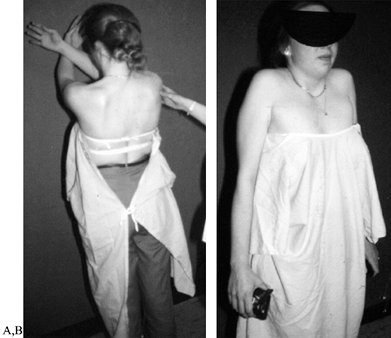
Hemi-Harness (Biomet, Warsaw, IN) (Fig. 61.2) or the Roylan sling (Smith & Nephew, Germantown, WI) (Fig. 61.3) may help. Also, such patients may be able to benefit from use of a stationary bicycle.
 |
|
Figure 61.2.
The Biomet Hook Hemi-Harness as seen from behind is shown. It consists of two cloth sleeves with Velcro closures and an adjustable strap that can be tightened or loosened as needed to support the shoulder girdles. In addition to the height of the shoulders, the degree of retropulsion is determined by where the strap is attached to the sleeves, and this, too, may be varied according to the correction required. |
 |
|
Figure 61.3. The Roylan sling as seen from the back (A) and the front (B).
|
manage; patients do not like to be told that they are overweight. Yet,
excess soft tissue can place additional strain on the shoulders,
particularly in women who have large breasts, which can aggravate TOS
by increasing traction on the structures crossing the first rib. In
cases of gigantomastia, reduction mammoplasty as a first step in the
treatment of very debilitating TOS may be successful. Kay has reported
on neurologic deficits in women with large breasts (15).
The mechanism of thoracic outlet compression makes it likely that this
is the locus of the problem. Even if weight reduction does not produce
the desired alleviation of compression, the patient who is thinner will
be easier and safer to operate on, especially through the axilla.
of TOS involves correcting postural abnormalities that can be
identified as contributing to the compression, and exercises to
strengthen the shoulder girdle when it is determined that weakened
muscles are a significant factor (Fig. 61.4).
Unfortunately, when the physician refers patients with TOS to a
physical therapy department, it is not always guaranteed that the
therapist caring for the
patient will understand the genesis of the problem and apply appropriate therapy. Very often, stereotyped routines (25)
such as stretching, soft-tissue massage, “nerve mobilization,” and
cervical traction are used, and these methods will actually worsen the
symptoms in many patients. The TOS patient must have a thorough
analysis by a knowledgeable therapist, and an individual therapy
program should be designed, implemented, and monitored to avoid
provocative maneuvers (25).
 |
|
Figure 61.4. A:
The therapist is instructing the patient in the correct way to exercise. Note that the arms are held in front of the plane of the body and that they are below shoulder height. The trapezius, rhomboids, and levator scapulae can be strengthened in this way without bracing the shoulders back or provoking symptoms. The therapeutic plan must be individualized to the specific patient’s needs, and most often it can be carried out as a home program with occasional visits to the therapist. B: Exercises for the upper trapezius that are tolerated by most patients with TOS. |
not tolerate even the most gentle conservative program. Particularly in
the case of anterior glenohumeral instability, the exercises often
prove provocative because they tend to reproduce the subluxations. Such
patients may be differentiated from those with dead arm syndrome. In
all likelihood, many patients with the diagnosis of dead arm syndrome
owing to glenohumeral instability really have TOS. If the condition
goes unrecognized, the patients will
continue
to be symptomatic even after shoulder repair. Leffert and Gumley
studied an interesting series of patients in whom these two entities
coexisted (17).
related to symptoms of TOS, modify such activities, if possible.
Overhead activities, the carrying of heavy loads, or the use of
backpacks can be quite provocative to patients with compression within
the thoracic outlet.
periodically so that the condition does not drag on interminably. The
conservative approach with periodic review is particularly important in
patients whose cases are complicated by litigation, insurance, or open
workers’ compensation cases. Caregivers must try to be objective in
interpreting symptoms so that patients are not unfairly deprived of the
benefits of treatment. In addition to periodic reviews, set a time
limit beyond which conservative therapy should be viewed as having
failed. If there is no positive response, the clinician must decide
whether to advise surgery or to accept the status quo with hopes that
the condition may improve with time.
the previously described treatment measures is the usual indication for
surgery.
the intrinsic muscles of the hand but sometimes in the long flexors as
well—almost never respond positively to conservative therapy. If they
are subjected to surgery, however, they should know preoperatively that
postoperative improvement in the power of the long flexors may actually
increase the muscle imbalance in the fingers and cause clawing or make
it worse. Advise such patients that they may require secondary hand
reconstruction for the muscle imbalance if it occurs. For those who
have significant sensory loss, the outlook is somewhat unpredictable
but generally favorable.
hand are candidates for immediate surgery. Fortunately, they are rare
and usually are not seen primarily by the orthopaedic surgeon but more
likely by vascular surgeons.
thoracic outlet is intractable pain. Only the patient can feel and
describe the pain; the surgeon must be able to interpret these reports
appropriately. Constraints of daily routine, vocational or avocational
adjustments, sleep disturbance, and history of analgesic use are all
important avenues of inquiry necessary to formulate a decision for
surgery. A complete and in-depth review of what was done in prior
physical therapy sessions is most important, because the patient may
not have had optimal care, or may actually have gotten worse because of
provocative positioning the exercises require (25).
records. Review the differential diagnosis very carefully before
proceeding. Discuss with the patient and family the mechanics and
objectives of surgery. Explain all possible complications in detail so
that the patient can give an informed consent. If you believe that a
second opinion would be useful, made certain that the surgeon or
physician rendering this opinion has sufficient experience in the area
to provide a valid opinion. Too often that opinion may be rendered on
the basis of little personal experience or knowledge.
lose weight despite specific evaluation for the cause of obesity and
instructions to correct it evinces poor cooperation. I have found it
prudent to inform such patients that their surgery is elective and will
not be done until they demonstrate genuine evidence of being willing or
able to participate in their own rehabilitation.
hemorrhage, the patient’s blood should be typed and cross-matched
before surgery. Whether to operate on a patient who will not accept
blood transfusion or blood products, should they be needed
intraoperatively, is a difficult and individual decision for which I do
not have a confident answer.
local custom, as well as the nature of the surgery to be performed,
either a vascular or general thoracic surgeon may be part of the
operating team. Although I have performed the vast majority of my
surgeries without need for such assistance, it is valuable to ensure
that such help is available on an if-needed basis. For patients who
have particular problems such as successive surgeries in which
complications can be anticipated, consultants may be invited to
participate at the beginning of the case. In addition, the operating
team should be experienced and adequate in number. I require three
scrubbed assistants for surgery by the axillary route. Do not use
overhead arm traction with weights, as is used in shoulder arthroscopy;
it carries a risk of inducing an intraoperative traction injury of the
brachial plexus.
in working order before you make the skin incision. Have vascular and
thoracic surgical instrument packs in the operating room should they be
needed.
the transaxillary route requires that the patient be profoundly
relaxed. The newer, short-acting muscle relaxants are particularly well
suited to this situation. Discuss the time frame for the surgery with
the anesthesiologist before commencing surgery so that muscular
relaxation may be reversed by the time the incision is closed, thus
allowing extubation without delay.
not undertake thoracic outlet surgery because it has the potential for
very serious complications. However, with proper identification of
patients suffering from significant compression and technically
adequate surgery, the results are very gratifying in most cases.
procedure is best for the treatment of TOS. Scalenotomy was the first
procedure to gain favor. If the pathology resided entirely between the
scalene muscles (1,2 and 3),
as was theorized, release of the anterior scalene should have
permanently cured the condition. Unfortunately, the incidence of
recurrence following scalenotomy was sufficiently high that surgeons
had to develop other procedures.
common denominator of compression and have concentrated their efforts
on eliminating it as well as adventitious ribs or congenital bands that
might be encountered in the course of exploration (9).
Since Roos reported his experience with the transaxillary first rib
resection in 1966, this approach has been the procedure most often
performed, and as the mainstay of the surgical approach to the problem,
it is described in detail (28,29,30,31 and 32). A variety of anatomic approaches, however, may be used for exploration of the thoracic outlet and removal of the first rib.
due to fracture angulation or hypertrophic subclavicular callus may
occasionally necessitate claviculectomy. It is worth considerable
effort to retain the clavicle if to do so does not materially increase
the surgical risks (14). Removal of the strut
function of the intact clavicle from a shoulder girdle with poor
muscular support can markedly increase symptoms because of the
superimposed traction effect of the ptotic shoulder. Patients with a
good trapezius may function well following claviculectomy, but they
experience weakness in overhead use of the arm. The enthusiasm for
claviculectomy for uncomplicated thoracic outlet compression has been
very limited. The procedure is not recommended (19).
local pathology. Some authors consider it the preferred method of
surgical treatment in certain cases (31).
Although it is desirable to avoid reattachment of the scalenes to the
bed of the first rib after it has been resected, I do not routinely
resect a portion of the anterior and middle scalenes because of the
possibility of injury to branches of the brachial plexus, which may
actually pass through the middle scalene. The phrenic nerve must be out
of harm’s way if you elect to resect part of the anterior scalene.
recurrence has been deemed due to scarring within the scalene muscles
themselves. An anterior approach is best. In addition to obvious
branches of the brachial plexus and phrenic nerve, the long thoracic
nerve is particularly vulnerable, because it may not always be located
lateral to the middle scalene. It may pierce the muscle or even present
as two branches, each of which must be gently retracted and preserved.
operative approaches to the thoracic outlet specifically for resection
of the first rib and then will comment briefly on the others.
 |
|
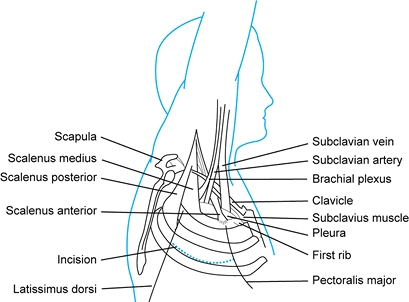
Figure 61.5.
Anatomy of the right thoracic outlet from the axillary view with the upper extremity and shoulder elevated. (From Roos DB. Experience with First Rib Resection for Thoracic Outlet Syndrome. Ann Surg 1971;173:429, with permission.) |
-
Place the patient, under general
endotracheal anesthesia, on the operating table in the lateral
decubitus position with the head tilted up. Face the patient’s back. I
place a high standing stool obliquely toward the head of the table near
me so that a sterilely gowned assistant can maintain the arm abducted
during the procedure. This assistant can lower the arm or change its
position as required lest a brachial plexus injury occur from excessive
traction, such as might occur if the arm were suspended from the
ceiling. Two other scrubbed assistants are necessary, one on either
side of the table, to retract the latissimus dorsi and pectoralis major
muscles during the procedure. -
Make a transverse skin incision between
the pectoralis major and latissimus dorsi muscles over the third
interspace, just below the axillary hairline. If the incision is
prolonged into the tail or body of the female breast, it can cause a
hypertrophic scar. I spread self-retaining retractors horizontally in
the wound to dissect the fat and render the tissues temporarily
ischemic, thus eliminating the need to ligate superficial vessels. -
Incise the fascia longitudinally in the
midline and bluntly spread the tissues with your fingers. Dissect
through the subcutaneous tissues to the level of the rib cage. Retract
the latissimus and pectoralis muscles. -
Overhead lights will not provide sufficient illumination to perform the surgery safely. Use a headlight or lighted retractors.The intercostobrachial nerve arises from the second
intercostal nerve and crosses the axilla embedded in fat to ultimately
reach the medial aspect of the arm. If possible, mobilize and retract
it, because trauma to the nerve can result in annoying dysesthesia on
the posteromedial aspect of the upper arm and axilla. -
Bluntly dissect with the fingers by touch
until the surface of the first rib can be palpated. Have the assistant
elevate the arm obliquely to open the outlet. -
Ligate the supreme thoracic arterial
branch to allow mobilization of the artery, which is done under direct
vision with nonabsorbable sutures or malleable clips. -
Now identify the important structures in
the field. The anterior scalene muscle attaches to the scalene
tubercle, which is located toward the inner border of the first rib
rather than extensively on its cephalic surface, although occasionally
the muscle may extend over it. Use a small wad or “palm” of gauze and
blunt dissection to delineate the muscle from the adjacent subclavian
artery and vein. -
Have assistants on each side of the table
retract the muscles using Deaver or similar retractors. If the muscle
relaxant wears off, the surgeon and assistants will become aware that
the muscles are getting tighter and the operative field is collapsing.
Close cooperation with the anesthesiologist is vital to the success of
the surgery. -
The most anterior structure in the wound
is the subclavius muscle with the costoclavicular ligaments and their
insertion into the superior surface of the first rib. Just behind and
adjacent to them is the subclavian vein. Use a blunt periosteal
elevator (Fig. 61.6) and dissecting sponges to clear the surface of the first rib of its soft tissues anterior to the middle scalene.![]() Figure 61.6. Instruments for transaxillary first rib resection are shown. Penosteal elevator (A), rasp for first rib (B), and Roos rib cutter (C) are illustrated.
Figure 61.6. Instruments for transaxillary first rib resection are shown. Penosteal elevator (A), rasp for first rib (B), and Roos rib cutter (C) are illustrated. -
Turn attention to the superior surface of
the first rib. Define and detach the anterior scalene. The phrenic
nerve is not usually at risk with this approach, because it is located
at least 2 cm cephalad to the tubercle. Using gentle, blunt dissection,
tease the subclavian artery and vein away from the anterior scalene.
Because the pleura may rise posteriorly and be adherent to the
posterior surface of the muscle, it is helpful to use a long
right-angled clamp to dissect behind the muscle and to shield each
vessel in turn as, alternately, half of the muscle is cut sharply at
its insertion to the bone. Obviously, all of this must be done very
carefully under direct vision. When the muscle has been cut, it
retracts. -
At this stage, visualization is limited
by the middle scalene, which can be elevated off the first rib with the
elevator. It is tempting to sharply divide this muscle at its
insertion, but the possibility of injury to the nerve to the serratus
anterior makes penetration inadvisable. As the muscle is elevated, it
can also be partially retracted with the blunt retractor. -
Using a rasp with a cutting edge that
conforms to the outer curvature of the first rib, separate the soft
tissues from the bone. Often, the first digitation of the serratus
anterior muscle may overlap the insertion of the middle scalene on the
first rib, and it must be bluntly separated. Alternate the rasp, the
periosteal elevator, and gauze sponges to clear the surface of the rib
of its muscle attachments. The undersurface should be similarly
cleared, although it is not desirable to perform the entire dissection
subperiosteally because of the possibility of later regeneration of the
rib, particularly in young patients. -
The periosteum of the first rib must be
disrupted and as much of it removed as possible. This procedure may
result in a tear in the adjacent pleura, causing a pneumothorax. During
this maneuver, ask the anesthesiologist to control respiration so that
the lung is retracted from the pleura in exhalation. About 30 seconds
of apnea should be required. Then controlled respiration may be resumed. -
Flood the wound with normal saline to
demonstrate the integrity of the pleura. If the pleura has been
breached, there will be air bubbles with respiration, or the fluid will
simply funnel down into the pleural cavity. If there is a pneumothorax,
drain it with a soft rubber catheter at wound closure or insert a chest
tube. Usually, a #26 tube can be inserted below the incision and into
the rent in the pleura without difficulty. Connect it to underwater
seal and suction. A pneumothorax does not significantly prejudice the
remainder of the operative procedure, and the tube can be placed just
before closure. It usually needs to be retained for 24 hours. -
Next, address the tendon of the
subclavius muscle and costoclavicular ligament. Make an incision at the
insertion onto the bone, which covers the superior surface of the rib.
Keep the subclavian vein constantly under direct vision because it is
immediately adjacent to the tendon and at significant risk. Once the
plane of dissection has been established, however, it is possible to
use the periosteal elevator and direct it away from the vein as the
tendon is elevated from the rib. Failure to perform this part of the
procedure properly will cause the line of section of the rib to lie at
the level of the subclavian vein, where a sharp edge of bone will
adhere to it. -
Having detached all the important soft
tissue from the first rib, thoroughly explore the outlet for the
presence of fibrous bands that are radiographically invisible but that
may be quite significant in causing compression of the neurovascular
structures. Never retract the neurovascular structures themselves with
any considerable tension because of the very real possibility of
injury. By positioning the arm appropriately, it is possible to lift
the structures off the surface of the rib so that a retractor is
usually not necessary. -
In addition to fibrous bands of various types, other important variations in the local anatomy can be observed (30).
For example, the anterior scalene may actually be overlapped in its
insertion by the middle scalene. There may be additional vascular
branches, or a cervical rib. A complete cervical rib may actually
attach to the manubrium, but a lesser one may reach to the scalene
tubercle. The attachment of the two ribs, which can be fibrous or
actually fused, can create significant problems, especially if the
subclavian artery is located at the juncture.I recently encountered such a situation that had
resulted in a symptomatic aneurysm with emboli in the arm of a
24-year-old woman. After the bone had been removed, I had the valuable
assistance of a vascular surgeon (prearranged) who did a vein graft to
the thrombosed aneurysm, with an excellent clinical result. This
dissection required both a supraclavicular and an infraclavicular
exposure—which is usually not necessary, because most cervical ribs can
be removed without having to make a supraclavicular incision. I always
obtain preoperative permission to make one, however, should it be
necessary. The rib may have to be removed piecemeal with rongeurs
rather than being resectable by means of two neat cuts of a rib cutter.
Piecemeal removal, of course, adds to the time necessary for the
procedure, as well as its difficulty. -
Once the anatomy is clear, decide which
instruments will be used to remove the rib. Ideally, a rib cutter can
be placed posterior to the lower trunk of the brachial plexus, almost
to the level of the transverse process, and the rib can be cut at that
level. If a straight rib cutter is used, however, the resulting
osteotomy will be oblique, leaving a very sharp point on the posterior
portion of rib, a most undesirable situation. For that reason, I have
used the rib cutter designed by Roos (see Fig. 61.6), which produces a transverse cut, owing to the inclination of its cutting surfaces.When used on the left side, introduce the rib cutter
with its point facing upward, hooking it beneath the rib and closing
the jaws before sliding it posteriorly. For a rib on the right side,
the point will face caudad, placing the pleura at risk. In either case,
the jaws should be almost closed and under direct vision so that they
will be safely beneath the neurovascular structures and posterior to
them. During this period, the anesthesiologist should maintain apnea in
expiration. -
After verifying that nothing has been
caught in the jaws of the rib cutter, firmly close the blades and cut
the rib. Then gently slide the instrument forward and open it in the
reverse manner in which it was inserted. Grasp the rib with a Kocher
forceps and visualize the anterior attachment to cartilage. Using a
standard rib cutter with its blades pointed away from the subclavian
vein, divide the rib and gently remove it from the wound. Complete as
close to total rib resection as possible. There should be at least 1.5
cm of space behind the lower trunk of the brachial plexus; in most
patients there will be 2 cm or less of posterior rib fragment
(measuring from the transverse process). Anteriorly, the line of
resection should be medial to the subclavian vein and disarticulation
is optimal. -
At this point, retest the integrity of
the pleura. Achieve complete hemostasis. Digitally explore the outlet
and place the patient’s arm in all positions to assess whether there is
any compression of the neurovascular structures. Usually there is not,
although if the second rib is very prominent, it could cause
compression. Relieve it by removing the middle third of the rib.P.1730If there is a pneumothorax, insert a chest tube at this
point and then prepare for closure. Give antibiotics if there has been
a pleural leak but not in an otherwise uncomplicated case.Return the arm, which the assistant has intermittently
raised and lowered, to the side. Drains are not used, nor should they
be needed.Complete a subcutaneous closure, followed by a
subcuticular closure using nonabsorbable suture, which is removed at 2
weeks postoperatively. Apply a small dressing. A sling is not needed.
thoracic outlet have been advised for resection of cervical ribs and
resection of the first thoracic rib as well as for scalenectomy (3,9,21,22).
In my experience, the exposure obtained for subtotal resection of the
first rib is less satisfactory than that gained with the axillary
approach, although this is not a universally held opinion.
-
Make a 7 to 9 cm incision 1 to 2 cm above
and parallel to the clavicle, extending from the midpoint of the
clavicular attachment of the sternomastoid muscle to the anterior edge
of the trapezius. Identify the platysma muscle for later careful
reapproximation. -
The external jugular vein must usually be
ligated. To facilitate exposure, divide about half of the sternomastoid
anteriorly, just above its insertion; 1 to 2 cm of trapezius may be
similarly cut. Divide the omohyoid muscle at its midpoint. The
suprascapular and transverse cervical vessels run horizontally and must
usually be ligated. -
Identify the phrenic nerve on the surface
of the anterior scalene muscle as it proceeds distally. Carefully
retract and preserve it. Detach the anterior scalene muscle and allow
it to retract. The belly of the muscle may then be safely resected. To
detach the muscle safely, carefully dissect the subclavian artery and
vein away from it and the pleura posteriorly. The internal jugular vein
is on the medial side of the muscle. Mobilize the subclavian artery in
its extraadventitial plane and retract it medially, while retracting
the brachial plexus laterally. -
If a cervical rib is present, remove it
from its periosteal envelope and resect it. Remove as much of the
periosteum as possible. Elevate the middle scalene off the first rib,
and then remove the rib. -
Reserve the transclavicular approach for
postoperative recurrences of thoracic outlet compression in which
adherence of the subclavian artery or vein to the anterior edge of the
resected rib is strongly suspected. -
In the subclavicular approach, make a 7
cm skin incision over the cartilage of the first rib, midway between
the clavicle and second rib (12). Split the
pectoralis major in the line of its fibers, exposing the cartilage of
the first rib. Open the periosteum of the anterior portion of the first
rib with a scissors, and carry out further dissection with a finger or
gauze. -
After the costochondral junction is
divided, remove the cartilage with a rongeur. The rib may then be
grasped and levered, either caudally or cephalad, for stripping of the
anterior and middle scalene muscles. Use a rasp, if necessary, to
denude the rib further, then cut the rib posteriorly with Sauerbruch
rib shears.
any abnormalities of the first rib encountered, including abnormal
width or a cervical rib, are difficult to manage because of limited
access. The presence of anomalous bands cannot be easily verified or
dealt with, and the vessels must be constantly retracted and are at
risk in an extremely confined space. Other than for access to the
anterior portion of the first rib, this is not a useful incision and is
not recommended.
Although it is considered a technique that does not involve any
disability or disfigurement, it is an extensive approach that traverses
the trapezius muscle, the levator scapulae, and rhomboids. For this
reason, I believe that it should be used infrequently; it should
particularly be avoided in patients who already have weakness of these
muscles and sagging shoulders, as well as those who must do heavy labor
following their convalescence.
 |
|
Figure 61.7. A: Posterior approach for resection of the first thoracic rib is shown. B: A cervical rib has been removed with the first thoracic rib. (From Clagett OT. Presidential Address: Research and Prosearch. J Thorac Cardiovasc Surg 1962;44:153, with permission.)
|
decompression of the thoracic outlet in patients who are extremely
muscular or obese and in whom the axillary approach would be
technically difficult. It is the preferred approach for reoperations in
which a retained posterior segment of rib has become adherent to the
brachial plexus and is causing symptoms.
-
Place the patient in the lateral
decubitus position, with the affected side up. Prep and drape the arm
free. Drape the entire hemithorax posteriorly past the midline,
including the neck to the hairline. -
Make a long incision from the superior
angle of the scapula, 2 cm medial to its vertebral border, for the
length of the bone. An incision too close to the scapula will encounter
the anastomotic scapular vessels, causing annoying bleeding. -
Introduce a scapular retractor beneath the scapula, which can then be retracted anteriorly and laterally (see Fig. 61.7).
-
The first rib must be identified from the
level of its transverse process; the rib is not horizontal in most
patients, and the second rib may partially obscure it. The posterior
scalene may blend with the middle scalene and is attached to the outer
surface of the second rib. It is easily detached. Identify and
carefully section the middle scalene, which inserts onto the superior
surface of the first rib. Anterior to it, the lower trunk of the
brachial plexus lies in contact with the rib, with the subclavian
artery immediately anterior to it, restrained by the insertion of the
anterior scalene to the scalene tubercle. The first digitation of the
serratus anterior originates from the outer aspect of the first rib and
can be freed with a rasp. The subclavian vein is, of course, anterior
to the anterior scalene and must be carefully protected. -
Remove the first rib. If a cervical rib
is present, it can be easily removed through the same incision. It is
impossible, however, to deal with a subclavian aneurysm through this
approach. Although the rib is resected subperiosteally to protect the
adjacent structures, remove as much of the periosteum as possible to
prevent regeneration of the bone. -
If a pneumothorax has been produced, insert a chest tube.
-
Perform closure in layers, taking care to
approximate anatomically the very important suspensory muscles of the
scapula, including the levator scapulae, rhomboids, and trapezius.
Place the patient in a sling for 3 weeks postoperatively and then begin
exercises to strengthen shoulder girdle muscles.
thoracic outlet by the axillary route, there is minimal blood loss and
physiologic disturbance. Although there may be moderate postoperative
pain, within a day most patients are sufficiently comfortable to move
about without the support of a sling. If a pleural tear has occurred
intraoperatively, then a chest tube is used for 24 hours. Most patients
are discharged from the hospital on the second or third day after
surgery.
to a single layer of gauze or removed altogether. Patients may shower
as long as the wound is kept dry; underarm deodorants and powders are
prohibited until the sutures are removed. Patients may be ambulatory at
home but are cautioned against heavy lifting or any strenuous
activities
for 4 weeks after surgery. Then they may resume their preoperative
exercise program, if there is no significant postural abnormality or
weakness of the scapular muscles. It is most important that these
exercises do not involve either overhead use of the arms or shoulder
bracing, because both of these types of exercises essentially duplicate
the provocative maneuvers that are used in diagnosis. Unfortunately,
they are still prescribed and used in many physical therapy facilities (25).
from the surgeon’s inexperience or timidity. Failure to resect the
subclavius tendon anteriorly produces a line of resection of the first
rib at the level of the subclavian vein that will then adhere and cause
symptoms of venous compression. Because the vein has a thin wall and is
easily torn, reoperation is hazardous. It is best performed, if
necessary, by the transclavicular route.
the lower trunk of the brachial plexus by 2 cm is most common with an
anterior approach, but it may also occur with a transaxillary
procedure. In most cases, less than 2 cm of rib should remain from the
level of the transverse process, but it is unnecessary to disarticulate
the rib. If recurrence is believed to be due to adherence of the lower
trunk of the plexus to the rib remnant, this problem is best approached
through a posterior, high thoracoplasty approach (8,41).
The hazards of this procedure stem from the difficulty of separating
the periosteum and scar from the nerves, which must be carefully
defined and lysed while the rib remnant is removed. Preliminary
resection of the second rib is an aid to the dissection, which then
proceeds to the bed of the first rib with a wider and clearer field.
regeneration of a resected rib, particularly in a young patient, it is
advantageous to remove or displace as much of the periosteum as
possible. The close adherence of the pleura, however, makes rents in
this filmy structure common during the course of the dissection.
Because the pleura cannot be directly repaired, either a rubber
catheter may be used to drain the pleural cavity during closure and
then withdrawn, or a chest tube may be placed through a separate stab
wound and connected to underwater suction for 24 hours. Then, after a
radiograph confirms the absence of a pneumothorax, the tube may be
removed. If a patient has sustained an intraoperative pneumothorax, he
or she should be restricted from air travel for 7 to 10 days.
the subcutaneous tissues of the arm and innervates the posterior
brachium, in many patients, down to the level of the olecranon. Because
it is located at the midpoint of the axillary incision made over the
third interspace, it is liable to injury, either by laceration or
traction. Even if care is taken to protect it, in many cases, there is
some transient numbness along the posterior aspect of the arm, which
gradually fades with time. If the nerve is cut, however, the patient
may experience very annoying dysesthesia that can be permanent.
Prevention is the best means of dealing with the problem. If there is a
neuroma, local nerve blocks are of occasional value.
Occasionally, patients have varying degrees of neural dysfunction in
excess of what was present preoperatively. The patient with increased
postoperative loss of intrinsic function in the hand and numbness of
the little and ring fingers may have sustained either a direct
laceration of the lower trunk or a traction injury. In the first
situation, repair is impossible, and no improvement is expected. In the
second situation, often there is little spontaneous recovery, although
it may occur. This complication can be avoided by gentle handling of
the nerves with minimal or no direct retraction.
the entire arm and significant motor weakness that was not present
preoperatively has sustained a traction injury to the brachial plexus,
which usually results from excessive pull on the arm during surgery.
This complication can result in permanent neurologic loss and pain, and
can largely be avoided by carefully monitoring the amount of
intraoperative traction. During the procedure, arm traction must be
periodically lessened so that a constant pull is not maintained.
comes around or through the middle scalene can result in permanent
winging of the scapula owing to paralysis of the serratus anterior (48).
The nerve should be sought and carefully protected. Sometimes, separate
branches to the digitations of the serratus anterior are seen, in which
case these must
be preserved. This complication weakens the patient’s ability to lift the arm in front of the plane of the body.
any procedure performed within the thoracic outlet. The surgeon must
have available appropriate technical ability or surgical assistance for
all eventualities. As stated earlier, appropriate instruments must be
present in the room, and the sterile field should be draped to allow
for additional procedures, including thoracotomy, if necessary.
demanding, sometimes frustrating, and technically challenging. However,
many carefully selected patients get good results from surgical
treatment when conservative therapy has been strenuously employed and
failed. The nature of the patient population is such that attempting to
compare the results of different series of surgically treated patients
can lead to markedly divergent impressions of the effectiveness of
surgery. In my own experience, about three quarters of the patients
that I have operated on have had good to excellent results. Despite the
fact that these surgical patients represent less than 20% of all the
patients I have seen with this entity, I believe that the surgery of
TOS has a rightful place in the armamentarium of orthopaedics.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
AW. Cervical Ribs: Symptoms, Differential Diagnosis and Indications for
Section of the Insertion of the Scalenus Anticus Muscle. J Internat Coll Surg 1951;16:546.
MJ, Olney RK, Parry GJ, et al. Relative Utility of Different
Electrophysiologic Techniques in the Evaluation of Brachial
Plexopathies. Neurology 1988;38:546.
P, Kazmier FJ, Hollier LH. Axillary-Subclavian Venous Occlusion: The
Morbidity of a Non-Lethal Disease. J Vasc Surg 1986;4:333.
Forestier N, Moulonguet A, Maisonobe T, et al. True Neurogenic Thoracic
Outlet Syndrome: Electrophysiological Diagnosis in Six Cases. Muscle Nerve 1998;21:1129.
A, Papagapiou M, Vanderlinden RG, et al. Thoracic Outlet Syndrome after
Motor Vehicle Accidents in a Canadian Pain Clinic Population. Clin J Pain 1995;11:316.
S, Paradiso C, Giannini F, et al. Diagnosis of Thoracic Outlet
Syndrome. Relative Value of Electrophysiological Studies [see
comments]. Acta Neurol Scand 1994;90:179.
AP, Ignacio DR, Gargour GW, et al. Assessment of Conduction from C8
Nerve Root Exit to Supraclavicular Fossa—Its Value in the Diagnosis of
Thoracic Outlet Syndrome. Electromyog Clin Neurophysiol 1989;29:445.
DM, Wassel HD. Traffic Accident Induced Thoracic Outlet Syndrome:
Decompression without Rib Resection, Correction of Associated Recurrent
Thoracic Aneurysm. Int Surg 1993;78:25.
RD, van der Merwe DM, Mitchell WL. Subclavian Vein Stenosis and
Axillary Vein “Effort Thrombosis.” Age and the First Rib Bypass
Collateral, Thrombolytic Therapy and First Rib Resection. S Afr Med J 1987;71:564.
T, Trojaborg W. Diagnosis of Thoracic Outlet Syndrome. Value of Sensory
and Motor Conduction Studies and Quantitative Electromyography. Arch Neurol 1987;44:1161.

