Treatment of Ulnar Collateral Ligament Injuries in Athletes
Surgery, University of Southern California School of Medicine,
Kerlan-Jobe Orthopaedic Clinic, Los Angeles, California.
Interestingly, trauma to this ligament rarely leads to symptomatic
instability of the elbow in the majority of those injured (5,11).
However, athletes participating in overhead or throwing sports place
repetitious high valgus stress upon the medial aspect of the elbow
joint (9). This may result in symptomatic
valgus instability due to ulnar collateral ligament injury,
occasionally requiring operative treatment to restore overhead athletic
function.
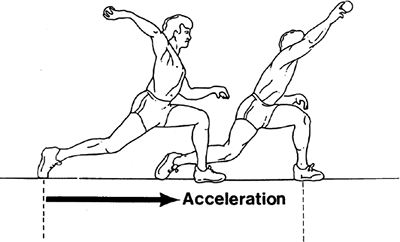
activities is the most common presentation. Pain is localized to the
medial side of the elbow, especially during the late cocking or
acceleration phases of the throwing motion (Fig. 14-2).
Significant injury requiring intervention may follow one of three
scenarios: the experience of an acute “pop” or sharp pain on the medial
aspect of the elbow leading to the inability to throw further, the
gradual onset of medial elbow pain over time with throwing, or pain
following an episode of heavy throwing with the inability on successive
attempts to throw above 50% to 75% of full function. The patient may
report associated recurrent pain or paresthesia radiating onto the
ulnar aspect of the forearm, hand, and fourth and fifth fingers,
especially with throwing.
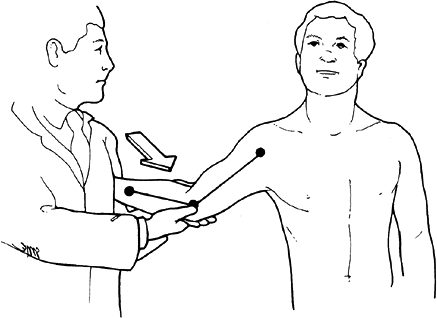
patient seated and the hand and wrist held securely between the
examiner’s forearm and trunk (Fig. 14-3). The
patient’s elbow is flexed beyond 25 degrees to unlock the olecranon
from its fossa and minimize the bony contribution to joint stability.
The ulnar collateral ligament is palpated while simultaneously
applying
a valgus stress. Local pain, tenderness, and end-point laxity are
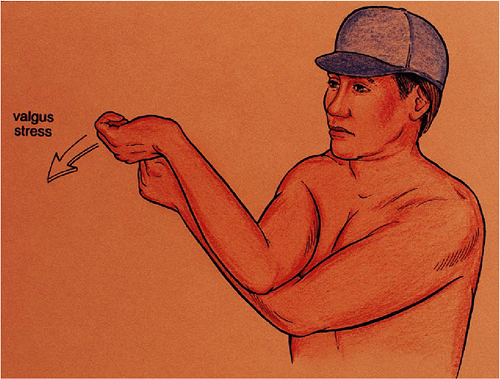
characterized with this maneuver. The “milking test” is a sensitive
test for damage to the ulnar collateral ligament and is performed with
the elbow at 70 to 90 degrees of flexion (Fig. 14-4).When
the valgus instability leads to degenerative or traumatic arthritis
with the formation of osteophytes and loose bodies posteriorly and
medially, surgical intervention is appropriate (6).
 |
|
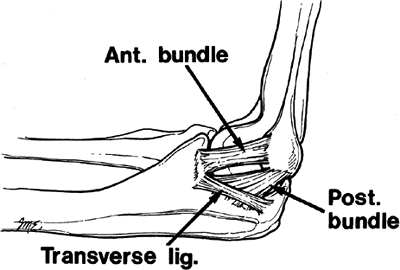
Figure 14-1.
Medial ulnar collateral ligament complex, right arm. Anterior bundle has an eccentric location across medial joint. It attaches to the coronoid tubercle and the base of the medial epicondyle. |
 |
|
Figure 14-2. Arm and elbow position during acceleration phase of throwing resulting in high valgus force.
|
 |
|
Figure 14-3. Valgus stress test produces pain and tenderness over ulnar collateral ligament.
|
 |
|
Figure 14-4.
O’Brien’s “milking test.” The elbow is flexed at 70 to 90 degrees and traction is placed on the thumb in a radial direction imparting a valgus force on the elbow. |
antiinflammatory medications, alternating ice and heat, and other
physical therapy modalities applied in the early symptomatic period,
may arrest the progression of instability and allow return to full
function without surgery (1). We have not found
steroid injection to be helpful. Rest periods with rehabilitation of up
to 3 months should be attempted and repeated at least once, especially
in those patients who have not experienced an acute rupture.
nonoperative treatment usually suffices. However, if the patient
desires to return to highly competitive overhead or throwing sports and
has failed to improve despite nonoperative treatment, surgical
intervention is indicated.
ligament and reconstruction using tendon graft. In our experience, the
indications for repair of the ulnar collateral ligament are limited.
This technique is reserved for those patients with an acute proximal
avulsion of the ulnar collateral ligament from its humeral attachment.
The avulsed ligament should be of good quality and without
calcifications presented within it. In this case, repair may be
attempted. However, this presentation occurs rarely (2).
stabilization. These symptoms are present in more than 40% of patients
with ulnar collateral ligament insufficiency (2). Symptoms of ulnar neuropathy may also be caused by traction, friction, and compression of the nerve (3,4).
The medial joint instability under valgus loading and the cubitus
valgus deformity lead to nerve traction injury, whereas friction
injuries result from recurrent subluxation of the nerve or abrasion by
posteromedial osteophytes. Elbow flexion deformities are often found
but usually do not adversely affect performance, since the throwing
motion involves elbow positions between 120 degrees and 20 degrees of
flexion (8). Calcifications within the injured ligament are also common but of themselves are not justification for surgery.
reconstruction should not be performed until a trial of work
modification has been performed.
to making the correct diagnosis of ulnar collateral ligament
insufficiency. It is important to record previous elbow injuries and
treatment.
over the ulnar collateral ligament complex, depending upon the degree
of inflammation at the time of examination. Such inflammation may also
irritate or compress the ulnar nerve locally as it traverses the
cubital tunnel (3). A positive Tinel’s sign
along the cubital tunnel is an indication of this focal ulnar nerve
irritability. A careful neurologic examination of the upper extremity
should be performed.
negative study should not rule out the diagnosis of ulnar collateral
ligament insufficiency. The importance of radiographs is to ensure
there is no associated pathology that may need to be addressed at the
time of surgery. Standard radiographs may identify ossification within
the ulnar collateral ligament, loose bodies in the posterior
compartment, marginal osteophytes about the radiocapitellar or the
ulnohumeral articulations, olecranon and condylar hypertrophy, or
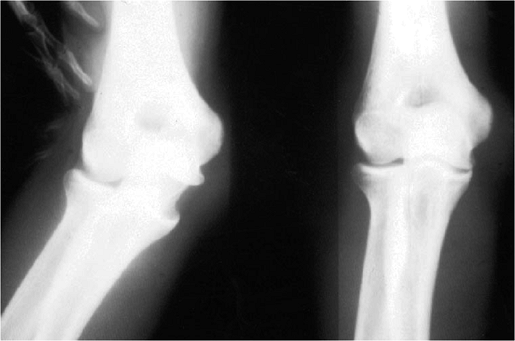
osteochondrotic lesions of the capitellum. Stress radiographs can show
excessive medial joint line opening, indicating ligament laxity (Fig. 14-5).
acute and chronic injury to the ulnar collateral ligament.
Intraarticular injection of contrast can increase sensitivity of the
test (Fig. 14-6).
been similar following repair or reconstruction, and the recommended
rehabilitation times are the same (2).
Therefore reconstruction of the insufficient ulnar collateral ligament
with free autologous tendon graft is our surgical treatment of choice.
 |
|
Figure 14-5. Valgus stress radiograph showing gross medial laxity. This degree of joint space opening is frequently absent.
|
 |
|
Figure 14-6. Magnetic resonance imaging (MRI) showing edema and fiber injury in the ulnar collateral ligament (arrowheads).
|
 |
|
Figure 14-7. The arm is placed on an arm board with the shoulder externally rotated to expose the medial aspect of the elbow.
|
free autologous tendon graft in all patients with ulnar collateral
ligament insufficiency who have symptomatic valgus instability
unresponsive to nonoperative treatment.
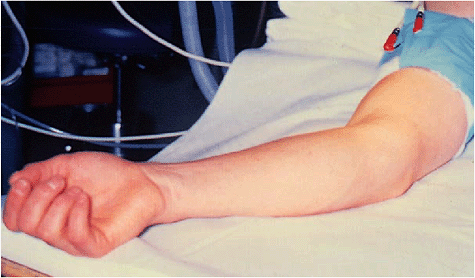
patient is given a general anesthetic and is placed supine with the arm
abducted to the side on a Parker arm board (Fig. 14-7).
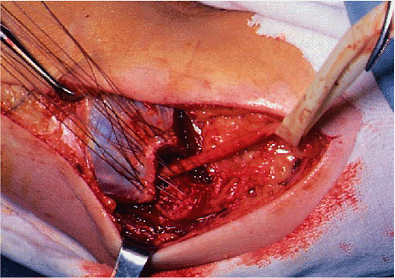
used to expose the myofascia and aponeurosis of the flexor pronator
muscle mass, the medial epicondyle, and the medial intermuscular septum
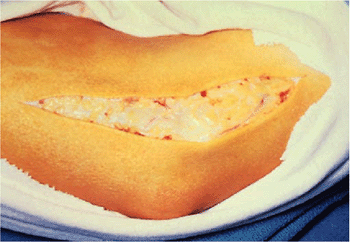
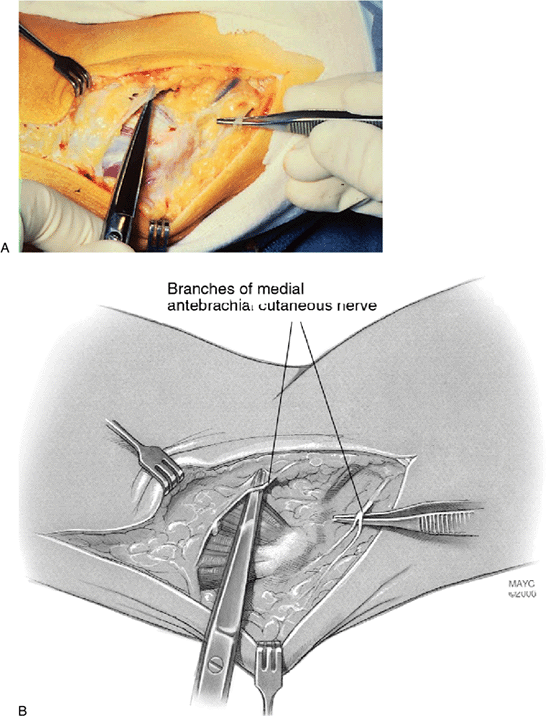
of the brachium (Fig. 14-8). Care is taken to
protect the medial antebrachial cutaneous nerve as it passes through
the medial aspect of the forearm across the surgical field (Fig. 14-9).
If there has been a previous anterior transposition of the ulnar nerve,
the nerve should be identified and protected before exposure of the
ulnar collateral ligament. For this exposure, a longitudinal split is
made in the myofascia, the underlying flexor pronator aponeurosis and
muscle mass at its more anterior origin from the medial epicondyle.
Retraction of the flexor mass to both sides provides access and
exposure to the anterior portion of the ulnar collateral ligament (Fig. 14-10).
 |
|
Figure 14-8. A 12-cm incision is centered over the distal aspect of the medial epicondyle and just anterior to it.
|
to inspect the medial aspect of the elbow joint. The elbow is flexed to
20 to 30 degrees and a valgus stress is applied. With insufficiency of
the medial collateral ligament, the medial joint should easily open
several millimeters (Fig. 14-11).
adequate ligamentous tissue remaining after debridement of calcific
deposits from the ligament, or in those with an acute injury causing an
avulsion of the ligament from the medial epicondyle. However, we feel
this is the exception and not the rule, especially in overhead and
throwing athletes. Usually it is necessary to reconstruct the ligament.
debrided and reattached to the periosteum of the medial epicondyle or
any substantial proximal remnant of ligamentous tissue. Slack in the
ligament can be imbricated and tightened by using a figure-of-eight
suture on both sides of the longitudinal split and then suturing the
two halves of the ligament together. An avulsion of the ligament from
its attachment to the medial epicondyle can be
repaired
by placing a Bunnell-type stitch through the body of the ligament and
then passing the two free ends of the suture through drill holes in the
medial epicondyle. The reattachment site should be prepared well with a
rongeur to provide a good base for healing. The sutures are then tied
securely on the posterior aspect of the medial epicondyle, with care
taken to protect the ulnar nerve.
 |
|
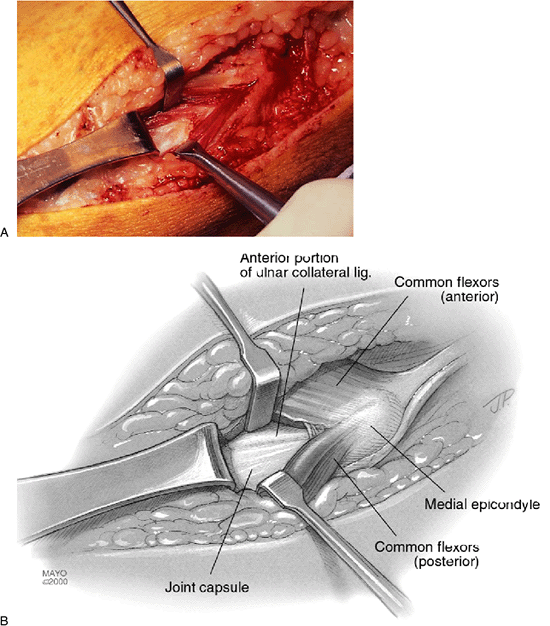
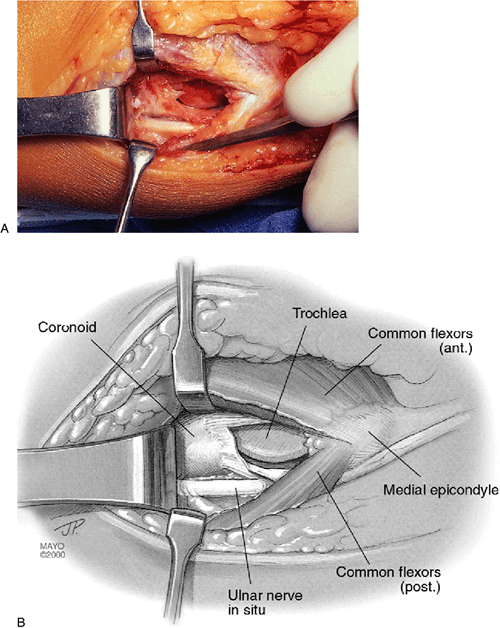
Figure 14-9. A,B:
The medial antebrachial cutaneous nerve is identified and protected as it crosses the surgical field. The common flexor pronator tendon is observed directly deep to the nerve. |
 |
|
Figure 14-10. A,B: Ulnar collateral ligament exposed through a longitudinal split in the flexor muscle mass at the base of the medial epicondyle.
|
necessary. In patients with associated preoperative ulnar motor
neuropathy or evidence suggesting posterior compartment osteophytes or
loose bodies, preparation is made to transpose the ulnar nerve
anteriorly. The tendinous origin of the flexor pronator muscle bundle
is transected 1 cm distal to the attachment of the aponeurosis on the
medial epicondyle, leaving a stump of tendon for reattachment. The
tendon and muscle are then reflected distally, leaving a thin layer of
muscle fibers attached to their bed of origin on the ulnar collateral
ligament itself. This provides excellent exposure of the entire ulnar
collateral ligament as well as its attachment to the tubercle on the
medial aspect of the coronoid process. Any calcification within the
remaining ligament and soft tissues is removed.
the cubital tunnel. The fascial arcade of Struthers, passing over the
ulnar nerve from the medial head of the triceps to the medial
intermuscular septum, is identified and released. The nerve is
dissected free and carefully
mobilized
proximally from the level of the arcade of Struthers and distally to
the interval between the two heads of the flexor carpi ulnaris. A loop
of 6.4-mm Penrose drain is placed about the nerve to protect it and to
manipulate it during mobilization (Fig. 14-12).
Care is taken to preserve any blood vessels intimately coursing with
the nerve, and as many vascular tributaries as possible to minimize
segmental devascularization of the nerve (8).
The articular branches of the nerve are sacrificed, but its motor
branches to the flexor carpi ulnaris muscle are preserved. A portion of
the medial intermuscular septum in the brachium is excised
sufficiently, allowing the transposed nerve to course anterior to the
epicondyle without contacting any remaining sharp edges of septum. With
the nerve anteriorly transposed, the posterior compartment of the elbow
is easily accessible through a thin veil of capsular tissue, and any
posterior loose bodies or osteophytes on the posteromedial margin of
the olecranon can be removed.
 |
|
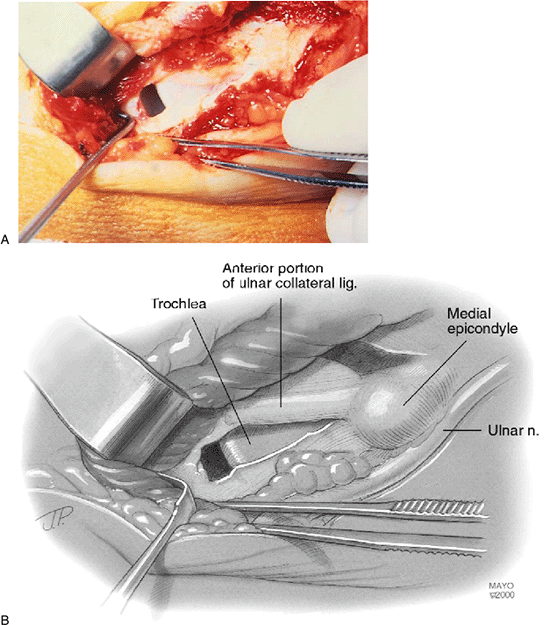
Figure 14-11. A,B: Longitudinal incision in the ulnar collateral ligament, revealing medial joint opening with valgus stress.
|
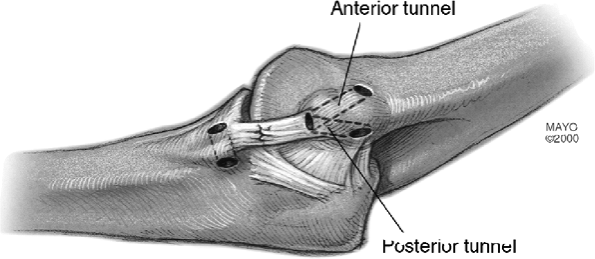
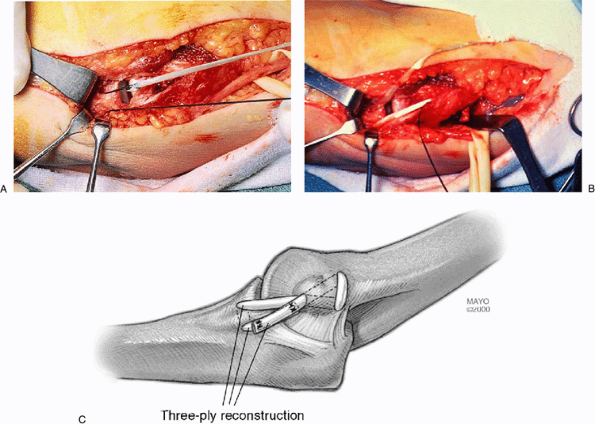
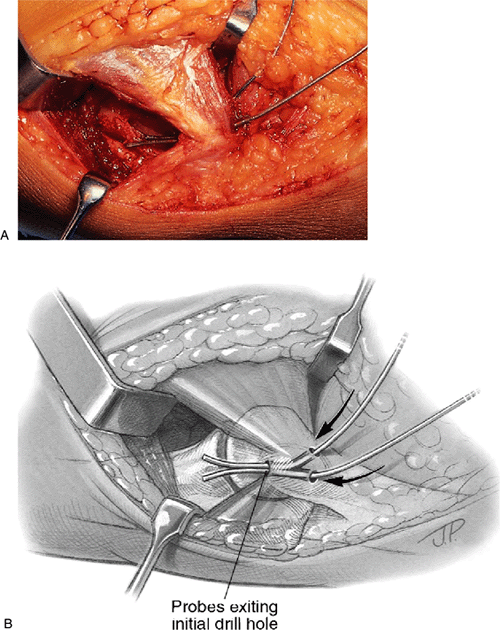
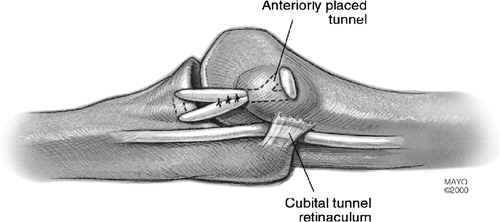
epicondyle, creating bone tunnels though which the graft will be
passed. A single entry hole is made anteriorly near the base of the
epicondyle. The drill holes diverge and exit separately in the cubital
tunnel posteriorly (Fig. 14-13).
located at the level of the tubercle on the medial aspect of the
coronoid process. These holes are separated by approximately 1 cm (Fig. 14-13).
 |
|
Figure 14-12. A,B:
Flexor pronator conjoint tendon transected 1 cm distal to epicondylar attachment and reflected distally. Muscle fibers can be seen originating from the ligament itself. The ulnar nerve is shown retracted from the cubital tunnel with a Penrose tubing. |
suitable tendon for autologous graft tissue. We prefer to use the
ipsilateral palmaris longus tendon for the free graft if available;
however, the contralateral tendon, the plantaris tendon, a 3- to 5-mm
medial strip of Achilles tendon, or tendon from lesser toe extensors
may be used. The palmaris longus tendon has been shown to fail at
higher loads with nearly four times the ultimate strength as compared
with the anterior band of the ulnar collateral ligament (10).
In our experience, the removal of palmaris tendon for reconstruction of
the ulnar collateral ligament causes minimal morbidity with superior
overall results as compared with repair of the ulnar collateral
ligament. The presence of a palmaris longus tendon must be documented
preoperatively. If absent, alternative autologous graft tissue may be
used as mentioned earlier.
creating a 2-cm transverse skin incision at the level of the distal
flexor crease of the wrist. The median nerve and its palmar cutaneous
branch are protected by isolating the tendon and identifying the
tendinous insertion into the palmar fascia. A second transverse skin
incision is made 10 cm proximal to the wrist at the level of the
palmaris longus musculotendinous junction. The tendon is then
transected distally and brought out through the proximal incision. It
is divided at the musculotendinous junction, providing a free
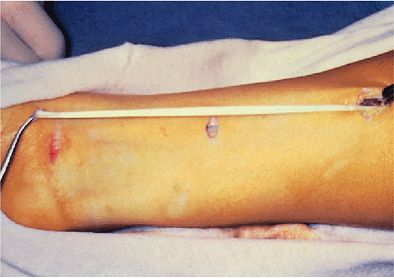
autogenous graft approximately 15 cm in length (Fig. 14-14). These incisions are irrigated and closed routinely.
 |
|
Figure 14-13. Drill hole orientation in the coronoid tubercle distally and epicondyle proximally.
|
 |
|
Figure 14-14. A 15- to 20-cm segment of palmaris longus tendon is harvested through three small incisions.
|
end of the graft, and a flexible suture passer is used to thread the
tendon through the bone tunnels in a figure-of-eight fashion. With the
elbow held in 45 degrees of flexion and neutral varus/valgus position,
the graft is pulled taut and sutured to itself (Fig. 14-15).
The graft is also sutured to the tough tissue of the intermuscular
septum near the epicondyle and to any remnants of the ulnar collateral
ligament. The elbow is then brought through a full passive range of
motion to verify isometricity and checked for abrasion of the graft on
the joint line. A gentle valgus stress is applied with the elbow in 30
and 70 degrees of flexion to test stability. A stable reconstruction
will prevent medial joint line opening.
osteophytes, or loose bodies, the ulnar nerve is not transposed. This
avoids the risk of perioperative nerve impairment caused by segmental
devascularization, intraoperative traction, or compression in the
transposed position. Also, the flexor pronator aponeurosis origin on
the medial epicondyle can be preserved.
under current study attempt to facilitate easier graft placement
tensioning and fixation (Figs. 14-17 and 14-18).
 |
|
Figure 14-15. A,B: The graft is secured at one end with nonabsorbable suture and pulled through the bone tunnels with a suture passer (C).
The graft is placed in a figure-of-eight fashion and sutured to itself. It can also be reinforced by suturing it to soft tissue around the epicondyle. |
 |
|
Figure 14-16.
The conjoint tendon is repaired to the 1-cm cuff of tendon on the epicondyle with the ulnar nerve transposed anteriorly in the submuscular position when indicated (see text). |
 |
|
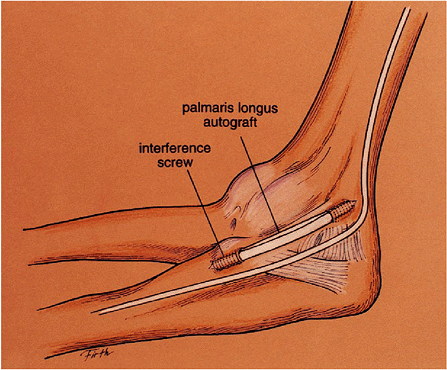
Figure 14-17.
The “docking procedure.” A two- or three-ply graft is placed through drill holes anterior and posterior to the ulnar tubercle. Then the proximal ends are “docked” into the epicondylar drill hole with attached sutures tensioned and tied over a proximal epicondylar bone bridge. |
 |
|
Figure 14-18.
Anatomic interference reconstruction. A three- or four-ply graft is inserted and fixed distally into a 4.0 drill hole with an interference screw. Then it is tensioned and fixed proximally into the epicondyle with a second screw. |
of the ulnar collateral ligament are identical. The patient begins
gentle hand grip exercises squeezing a sponge or soft ball on the first
postoperative day or as soon as it is comfortable to do so. The patient
is discharged from the hospital on the second postoperative day.
active elbow and shoulder and wrist range-of-motion exercises are
started. After 4 to 6 weeks, muscle-strengthening exercises of the
wrist and forearm are initiated, including flexion, extension,
pronation, and supination of the hand and wrist. At 6 weeks,
elbow-strengthening exercises are begun while avoiding valgus stress
until 4 months after the operation. Shoulder exercises, including those
for strengthening and maintaining the rotator cuff, are continued
throughout the rehabilitative period.
wind-up motion for a distance of 30 to 40 feet two to three times per
week for about 10 to 15 minutes per session. At 5 months after surgery,
the patient may increase the tossing distance to 60 feet and at 6
months the patient may perform an easy wind-up. Thereafter the patient
may perform exercises and tossing on alternate days. Ice is used
following all workouts to decrease swelling and inflammation.
strengthening exercises, as well as total body conditioning is
performed. Throwers and pitchers are carefully supervised, limiting
throwing to one-half full speed while gradually increasing the duration
of their sessions to 25 to 30 minutes. Pitchers are permitted to return
to the mound and progress to 70% of maximum velocity during the eighth
or ninth month.
the body mechanics of throwing, including the lower extremities and
torso. Duration of throwing sessions and velocity is slowly increased
to eventually simulate a game situation. Throwing in competition is
permitted at 1 year if the shoulder, elbow, and forearm are pain-free
while throwing and have returned to normal strength and range of
motion. Rhythm, proprioception, and accuracy are the last skills to be
regained in overhead athletes following reconstruction of the ulnar
collateral ligament of the elbow. In a professional pitcher, it may
require more than 18 months to regain preoperative ability and
competitive level, with relatively shorter periods required for other
player positions or overhead sports (4).
overhead or throwing athletes unable to compete due to valgus
instability of the elbow has been successful in returning most patients
to their previous level of participation (2,4).
Of 70 operations on 68 patients with valgus instability of the elbow
treated at the Kerlan-Jobe Orthopaedic Clinic, 14 had direct repair and
56 had a reconstruction of the torn or incompetent ligament, using a
free tendon graft (2). These patients were
followed for 6.3 years postoperatively. Fifty percent of the repair
group and 68% of the reconstruction group returned to their previous
level of participation. The mean time to return to competition was 9
months in the repair group and 12 months in the reconstruction group.
Twelve of 16 major league baseball players who underwent reconstruction
without previous elbow surgery returned to playing in the major
leagues. Two of seven major league players who had a direct repair as
their primary procedure returned to that level. Previous operations on
the elbow were shown to decrease the patients’ chances of return to
their preinjury level of participation in their sport.
considered, it appears that baseball pitchers are the most difficult
patients to return to their previous competitive level, with 62%
showing excellent results in the reconstruction group.
the mode of onset of symptoms (acute versus insidious), and the type of
ligament injury (avulsion versus attenuation) did not affect the
postoperative outcome. Also, postoperative flexion deformities of the
elbow up to 25 degrees may not decrease a thrower’s performance,
especially if present preoperatively.
the ulnar nerve constitute the most common complication following ulnar
collateral ligament repair or reconstruction in conjunction with nerve
transposition and may occur in up to 25% of patients (2).
Careful subcutaneous dissection may prevent inadvertent transection of
cutaneous nerves causing local paresthesia or painful neuroma
formation. Also, meticulous hemostasis and placement of surgical drains
help to prevent compression of the ulnar nerve secondary to hematoma
formation. Segmental devascularization of the transposed ulnar nerve
may play a major role in the occurrence of postoperative ulnar nerve
palsy (8,12). Therefore
in patients requiring ulnar nerve transposition, gentle handling of the
ulnar nerve and preservation of as much of its vascular leash as
possible may limit the incidence of this problem. To address the
incidence of postoperative ulnar nerve problems, dissection and
anterior transposition of the nerve are now performed only when
symptoms of ulnar neuropathy are present or when pathology in the
posterior compartment requires exposure through the cubital tunnel.
Rupture or stretch of the reconstruction is possible but is uncommon if
three strands of the graft cross the joint. If the joint becomes
dysfunctional, reoperation is indicated and a new autogenous graft is
used to construct the deficiency ligament.
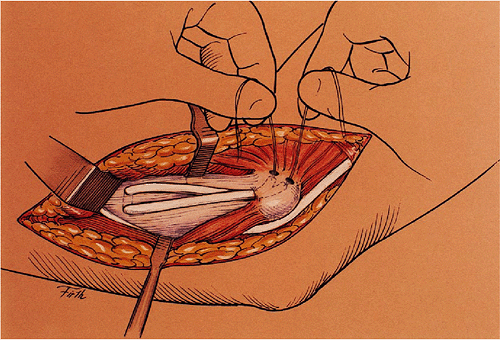
insufficiency but no ulnar nerve symptoms. The approach and exposure of
the flexor pronator conjoint tendon is the same as described earlier.
The conjoint tendon and muscle fibers of the flexor pronator group are
split longitudinally and retracted to expose the ulnar collateral
ligament. The ulnar nerve is not exposed and is left in position in the
cubital tunnel. The flexor pronator tendon origin is also left intact,
not transecting it at the epicondyle. The drill holes in the coronoid
tubercle of the ulna are fashioned as described earlier. However, care
should be taken to protect the ulnar nerve and its muscular branches at
the level of the coronoid tubercle as it courses within the muscle
fibers on the inferior and medial aspect of the exposure. The nerve may
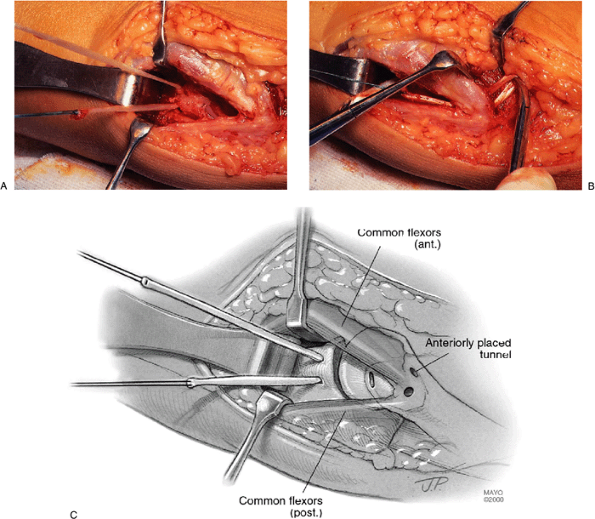
be visible at this level (Fig. 14-19). The
initial drill hole at the humeral epicondylar attachment of the
ligament is made and angled more superiorly and anteriorly than the
procedure described earlier. Two drill holes are then made on the
superior and anterior surface of the epicondyle approximately 1 cm
apart with both placed anterior to the intermuscular septum. They are
angled so that they communicate with each other and with the initial
entry hole within the substance of the epicondyle (Fig. 14-20).
In this way, the cubital tunnel is not penetrated and the ulnar nerve
is not disturbed. The tendon graft is harvested and placed through the
bone tunnels as described earlier (Figs. 14-21 and 14-22).
ends buried within the bone tunnels. The longitudinal split in the
flexor pronator wad may then be repaired if desired by simply closing
the superficial myofascia with absorbable suture.
A long-arm posterior plaster splint is used to immobilize the elbow in
90 degrees of flexion and neutral rotation, leaving the wrist and hand
free.
 |
|
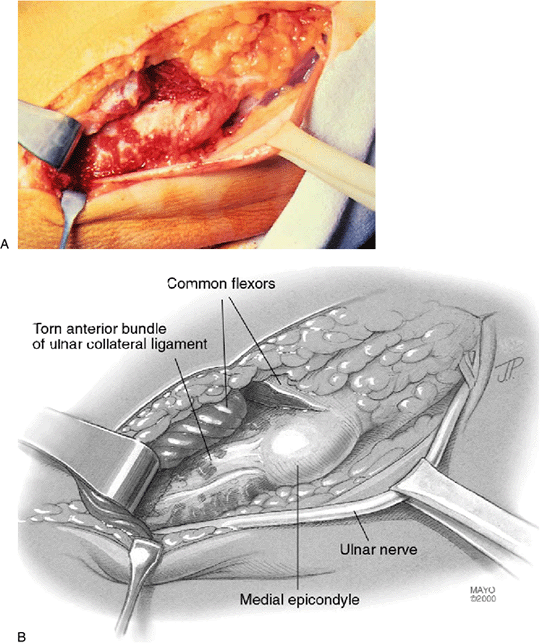
Figure 14-19. A,B:
When ulnar nerve transposition is not required, the procedure is performed through a longitudinal incision in the conjoint tendon and muscle instead of transecting the epicondylar attachment. Above, the calcified ligament that had been debrided and the coronoid tubercle is exposed for drilling. Note the ulnar nerve on the lower aspect of the exposed tubercle. |
 |
|
Figure 14-20. A,B: Epicondylar drill holes oriented anterior and superior to the intermuscular septum. Shown above with probes through the holes.
|
 |
|
Figure 14-21. A-C: The graft is placed and tensioned as described in the text.
|
 |
|
Figure 14-22. The epicondylar holes are anterior to the intermuscular septum with the ulnar nerve left in position in the cubital tunnel.
|
 |
|
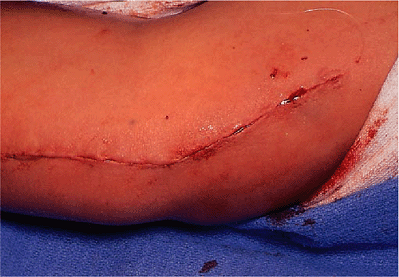
Figure 14-23. Skin closure.
|
JE, Jobe FW, Glousman RE, Pink, M. Medial instability of the elbow in
throwing athletes: surgical treatment by ulnar collateral ligament
repair or reconstruction. J Bone Joint Surg 1992;74:67–83.
RJ, Nevaiser RJ, Adams JP, et al. The effect of devascularization on
the regeneration of lacerated peripheral nerves: an experimental study.
J Hand Surg 1978;3:163.
